Key Points
Question
What are the trends and variations in cataract surgery access associated with a central reimbursement policy in Thailand?
Findings
In this time series analysis, after implementing a central reimbursement policy, the national cataract surgery rate increased substantially to 765.3 cases per 100 000 population in 2015. The subnational cataract surgery rate gap widened because of rapid uptake in areas with high rates of cataract surgery initially and decreased as overall coverage became adequately large.
Meaning
A central reimbursement policy that mitigated financial constraints of individual health care professionals in a developing country reduced backlogs for cataract surgery and was associated with improved access.
Abstract
Importance
Uptake of cataract surgery in developing countries is much lower than that in developed countries. Cataract unawareness and financial barriers have been cited as the main causes. Under the Universal Coverage Scheme (UCS), Thailand introduced a central reimbursement (CR) system for cataract surgery. It is unknown if this financial arrangement could incentivize service provision (private or public) in areas that are hard to reach.
Objective
To examine the association between the CR policy and access to cataract surgery in Thailand.
Design, Setting, and Participants
Using time series analysis, hospitalization data during 2005 to 2015 for UCS members were analyzed for time trends and subnational variations in the cataract surgery rate (CSR) before and after the CR implementation.
Main Outcomes and Measures
The annual growth in access was estimated using segmented regression. The CSR gap across regions was determined by the slope index of inequality (SII). Unequal access across districts was represented by the gap between the top and bottom quintiles.
Results
During 2005 to 2015, a total of 0.98 million UCS members (mean [SD] age, 67.4 [11.2] years; 58.7% female) received cataract surgery. The number of cases increased from 77 897 in 2005 to 192 290 in 2015. At the national level, the CSR per 100 000 population increased from 352.0 to 378.7 cases in 2005 to 2008, to 716.3 cases in 2013, and then to 765.3 cases in 2015. With the use of mobile services through an exclusive CR, 3 private hospitals took the lead in service growth, sharing 79.2% of cases in the private sector in 2009. From 2010, the number of cases in public hospitals grew yearly by 12.6% to 13.6% until 2012, rose 21.7% in 2013, and then the rate of increase declined to that of 8.2% to 8.3% in 2014-2015. During the periods of an increase in overall access, the CSR gap across regions widened as indicated by the SII of 755.4 cases per 100 000 population in 2010 because of rapid uptake in areas with mobile services. When the national CSR became adequately large and mobile services were discouraged in 2013, the gap in 2014-2015 narrowed.
Conclusions and Relevance
This study found that the appropriate payment and service designs helped reduce the cataract surgery backlog. With an adequately high CSR, Thailand is on track to reach the VISION 2020 goal, aiming for blindness elimination by the year 2020, which has been achieved by most developed countries.
This time series analysis examines the association between the central reimbursement policy of a universal health coverage scheme and access to cataract surgery in Thailand.
Introduction
Cataract is a high-burden disease in developing countries and is responsible for almost half of all cases of blindness.1,2 In Thailand, the National Survey of Blindness, Low Vision and Visual Impairment from 2006 to2007 and the Rapid Assessment of Avoidable Blindness Survey from 2012 to 2013 reported that 0.6% of adults 50 years or older were blind.3,4 In both surveys, the leading cause of blindness was untreated cataract, estimated at 51.6% and 69.7%, respectively.
In 1999, the World Health Organization5 launched VISION 2020, a global initiative for eliminating avoidable blindness by the year 2020. In developed countries, the cataract surgery rate (CSR) was beyond the 3000 per million minimum set by the World Health Organization for blindness elimination.6 The CSR per 1000 population increased from 4.47 in 1992 to 7.26 in 2000 in Sweden.7 In England, the CSR per 100 000 population rose from 62 cases in 1968 to 637 cases in 2004, with wide geographic variation.8 In the United States (Wisconsin), the age- and sex-adjusted incidence of lens extraction in 2008 to 2010 was 11.7% and was much higher in persons with less visual impairment.9 The rising CSR in recent decades has been attributed to a reduced visual impairment threshold and improved techniques for cataract surgery unrelated to demographic transition.10 Despite being a proven cost-effective intervention,11,12 cataract surgery in developing countries has faced backlogs, with major causes being lack of cataract awareness and financial barriers.13,14,15
Thailand implemented universal health coverage in 2002, when uninsured and medically indigent people became eligible for the Universal Coverage Scheme (UCS). Each year, the UCS budget is allocated through networks of predominantly public hospitals, known as contracting units for primary care (CUPs). At district levels, more than 1000 CUPs receive a prospective per capita budget for ambulatory visits. Hospitalization is paid under global budgeting by diagnosis-related groups across 13 administrative regions. With the prepaid arrangement, each CUP takes full responsibility for costs of services rendered to its population inside or outside of the catchment areas.
The National Health Security Office (NHSO), the UCS administrative body, has introduced a retrospective payment (a central reimbursement [CR]) for selective medical and surgical procedures. The CR policy would draw financial risks from individual CUPs into an adequately large national pool. Through a reasonable cost recovery rate, financial constraints to health facilities could be mitigated and hence stimulate scaling up of priority services that had low uptake.
Committing to the global movement, The Royal College of Ophthalmologists of Thailand campaigned for the first time on cataract awareness, which resulted in a surge during 2004 to 2006 of 60 000 to 80 000 cataract surgical procedures.16 In 2006, the NHSO introduced the CR system for cataract surgery by paying an exclusive lump sum for mobile services on case finding and treatment in remote areas. The usual hospitalized surgery was paid by regular diagnosis related groups. In district areas where ophthalmologists were in shortage, hospitals were able to outsource the treatment to mobile services from the private sector or collaborate with tertiary care facilities. Foreseeing trouble from system fragmentation, the NHSO in 2011 substituted the dual-payment methods with fixed fee schedules for both surgical procedures and intraocular lens insertion and extraction.17 A subsequent policy adjustment was implemented in 2013, when cross-region mobile services were discouraged.
During 9 years (2007-2015) of the CR implementation, spending on cataract surgery accrued to US $354 million. Cataract surgery alone accounts for 2.8% of payments for all hospitalizations and 0.7% of the UCS budget.18 With 2 years left in the global eye health agenda, it is timely to examine if the CR policy can help Thailand achieve universal access to the cost-effective intervention of cataract surgery.
Methods
Data Sources
The UCS hospitalization data during 2005 to 2015 were obtained from the NHSO. Patients were included if they had the following International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) or International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes: senile cataract (ICD-10 codes H25.0, H25.1, H25.2, H25.8, and H25.9) or unspecified cataract (ICD-10 code H26.9), plus lens extraction procedures (ICD-9-CM codes 13.19, 13.2, 13.41, 13.42, 13.43, 13.51, 13.59, 13.69, and 13.71). Additional data included location and type of admitting hospitals, the total UCS population, and CUPs area where the patients registered.
The study was approved by the Ethics Committee for Human Research, Khon Kaen University (HE 602150). Informed consent was not sought because the data were provided by the NHSO.
Measurement
Access to cataract surgery was measured in terms of service volume and population coverage or the CSR. For a given year, hospitalizations for cataract surgery were disaggregated by private and public sectors. The CSR was calculated as a ratio between the number of cases and the UCS population 40 years or older who resided in the same districts.
In addition, the CSR was examined for subnational variations. Two subnational areas were chosen because they were associated with the UCS financial arrangement. The first was a cluster of 4 to 8 provinces forming 13 administrative regions of the NHSO. The regions where the mobile services had operated were analyzed for the subnational trend and compared with the whole country. The second was the functional district area where each CUP was located. Distribution of the CSR across the 13 regions and more than 1000 districts was determined using an inequality measure and quintile ranking, respectively.
The absolute inequality in the CSR, representing a gap between the regional extremes, was calculated as the slope index of inequality (SII).19 The SII captured the CSR gradient on descending ranks across all regions.
For the quintile ranking, the district-level CSR at baseline (2005) was ranked and formed 5 equally sized groups. The first quintile (Q1) represented the 20% of districts with the lowest CSR, whereas the fifth quintile (Q5) represented the 20% of districts with the highest CSR. The median and interquartile range (IQR) of Q1 and Q5 were tracked until 2015.
Statistical Analysis
To assess time trends in overall access, data on the CSR at the national level and the regions where the mobile services had operated were submitted to an interrupted time series analysis.20 The CSR was regressed on yearly time points, which were separated into segments to differentiate annual changes before and after the CR implementation. The Durbin-Watson (DW) statistic was calculated for a serial correlation that followed the first-order autoregressive process.21 If the DW test result was statistically significant or inconclusive, a generalized least square that accounted for the serial correlation was applied using Prais-Winsten transformation.22 Two-sided P < .05 was considered statistically significant.
Results
In total, 0.98 million people who were UCS members received cataract surgery over 11 years (2005-2015) of the study period. Most patients were older (mean [SD] age, 67.4 [11.2] years) and female (58.7%).
Service Volume
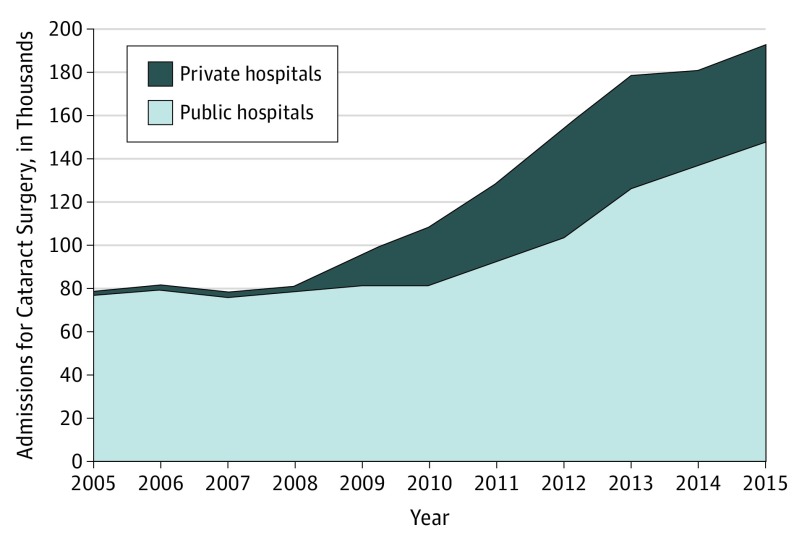
The number of facilities that performed cataract surgery for UCS members was stable at 229 to 232 hospitals during 2005 to 2008. Since 2009, the numbers rose by almost 60% to 365 hospitals in 2015. An expanding availability on the supply side translated into increasing services such that the total cataract surgical procedures increased by more than 2 times, from 77 897 cases in 2005 to 192 290 cases in 2015 (Figure 1).
Figure 1. Number of Admissions for Cataract Surgery in Private and Public Hospitals, 2005-2015.
Private health care professionals took the lead in service growth during 2009 to 2013. Before 2009, only a handful of 28 to 31 private hospitals performed cataract surgery for UCS members. In 2009, admissions for cataract surgery in the private sector increased substantially to 14 822, of which 79.2% were serviced by 3 hospitals. These leading private hospitals used mobile services to reach the target population beyond the catchment areas. As the number of private hospitals increased gradually to 43 hospitals in 2013, the number of services grew rapidly and reached a peak of 52 376. The private sector services decreased during the last 2 years (2014-2015).
Almost all cataract surgical procedures were performed in approximately 200 public hospitals during 2005 to 2008 and remained stable at up to 80 775 per year until 2010. An increase in the public sector services began in 2011, representing a 2-year lag behind the private sector. The number of public hospitals performing the surgery increased to 230 during 2011 to 2013 and peaked at 290 in 2015. From 2010, the number of cases in public hospitals grew yearly by 12.6% to 13.6% until 2012, rose 21.7% in 2013, and then the rate of increase declined to that of 8.2% to 8.3% in 2014-2015. In 2015, the surgical procedures in public hospitals shared 76.7% of the combined private and public 192 290 admissions.
Population Coverage
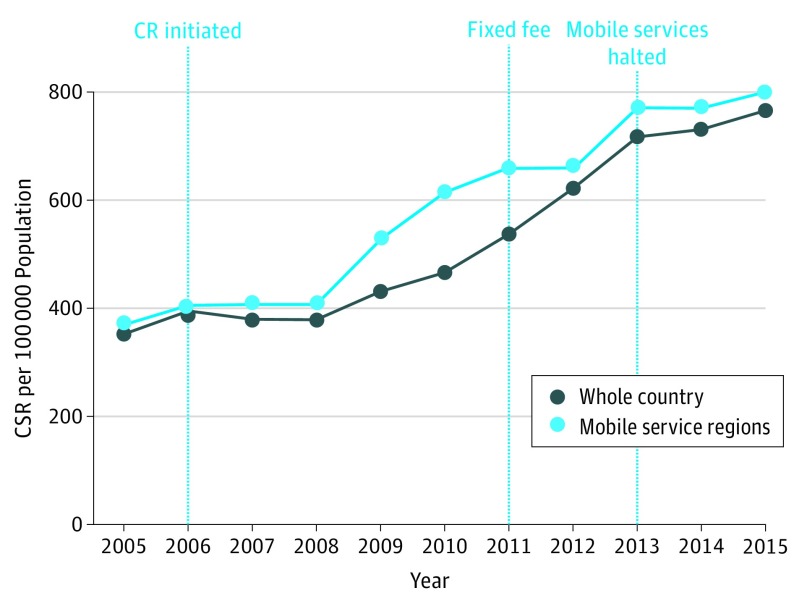
At the national level, the CSR per 100 000 population increased from 352.0 to 378.7 cases in 2005 to 2008, to 716.3 cases in 2013, and then to 765.3 cases in 2015 (Figure 2). The combined regions where the mobile services were available had a yearly CSR and time trend similar to those of the whole country until 2008; the 2 diverged thereafter.
Figure 2. Cataract Surgery Rate (CSR) in Mobile Service Regions and in the Whole Country, 2005-2015.
CR indicates central reimbursement.
Three distinct segments of time trends in the CSR were detected. The first segment represented the secular trend around the CR introduction from 2005 to 2006 and 2007 to 2008, when a lagged policy association was observed. The second and third segments captured the 7-year trend from 2009 onward. The post-CR period was delineated by early and late phases because of a policy change in 2013, when mobile clinics were barred from most regions.
The serial correlation of the data between adjacent years was examined. For 11 time points with 3 variables, representing 1 prepolicy period and 2 postpolicy periods to be estimated, the lower and upper bounds for the 5% significance level of the DW statistic were 0.595 and 1.928, respectively. The DW statistic for the data from regions with mobile services was 1.694, which suggested an inconclusive serial correlation; in contrast, the DW on the national time series of 0.419 was statistically significant (P < .05). Therefore, the Prais-Winsten method that assumed the first-order autoregressive process was applied to both the national and subnational series.
The national CSR had a nonsignificant, increasing trend that preexisted during 2005 to 2008, around the time of CR introduction (Table 1). However, during the early post-CR period in 2009 to 2013, the CSR increased rapidly by 64.9 cases per 100 000 population per year, which was statistically significant (P < .01). In the late post-CR period (2014-2015), the annual growth slowed to 34.8 cases per 100 000 population on average.
Table 1. Estimated Baseline and Mean Annual Changes in the Cataract Surgery Rate per 100 000 Population.
| Period | Whole Country | Mobile Service Regions |
|---|---|---|
| Baseline (2005)a | 364.6 | 348.7 |
| Secular trend (2005-2008) | +0.82 | +23.4b |
| Post-CR | ||
| Early (2009-2013)a | +64.9 | +64.6 |
| Late (2014-2015) | +34.8c | +16.4b |
Abbreviation: CR, central reimbursement.
P < .01.
P < .10.
P < .05.
By the time of CR introduction, the CSR in the regions where the mobile services were available had already increased by 23.4 cases per 100 000 population per year (P < .10). Five years later (2009-2013), although the annual rate was comparable with that of the national level on average, an acceleration in the mobile service regions provided a head start. The increase in the CSR during the last 2 years (2014-2015) was slower than that in the national series by half.
Subnational Variations
When the national CSR increased during the early period of CR, unequal distribution in the CSR across subnational areas was noted. The CSR gap between the regional extremes as measured by the SII was 314.6 to 337.6 cases per 100 000 population during 2005 to 2008, then widened (SII, 464.7 cases per 100 000 population) in 2009, and remained large (SII, 755.4-800.4 cases per 100 000 population) during 2010 to 2012 (eTable in the Supplement). The absolute inequality across 13 regions decreased to 681.0 cases per 100 000 population in 2013 and reached a minimum of 502.9 cases per 100 000 population in the last year (2015).
When the inequality in the CSR reached a peak in 2010, three administrative regions (3, 4, and 5, located in the central part of Thailand) were notable for high coverage (750-1100 cases per 100 000 population) (eFigure in the Supplement, middle panel), whereas the rest remained low similar to the 2005 baseline (eFigure in the Supplement, top panel). A substantial increase in the top 3 regional CSRs steepened the slope, widening the gap. In 2015, when regions (especially those having low CSR levels) surpassed the top of the baseline (500 cases per 100 000 population), the CSR gradient became flatter (eFigure in the Supplement, bottom panel). This helped reduce the inequality across regions.
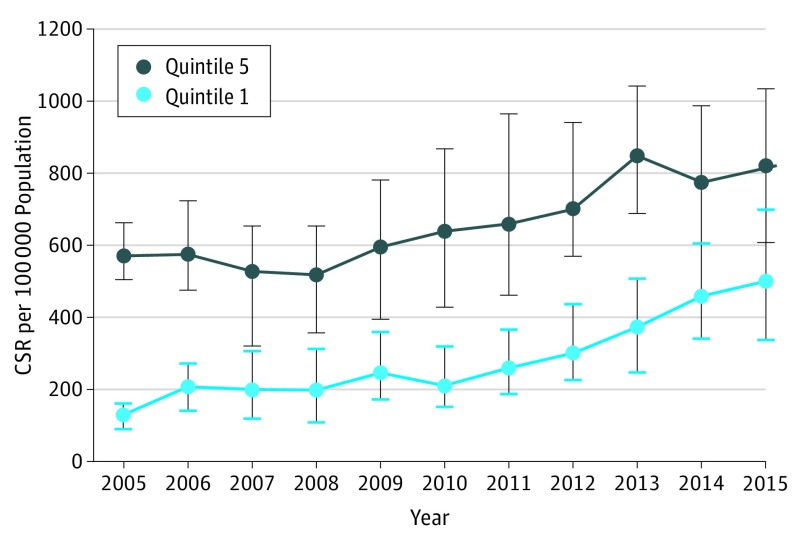
For variations in the CSR across district areas, data from 921 districts where UCS members obtained cataract surgery in 2005 were divided into quintiles. The median CSR at baseline was 568.0 cases per 100 000 population in the top quintile (Q5), which was 4 times higher than the 128.1 cases per 100 000 population in the bottom quintile (Q1).
Table 2 summarizes the baseline characteristics of the UCS population and the patients in the cataract surgery cases who were 40 years or older in each CSR quintile. Although the female majority (52.6%-53.6%) was distributed similarly across subgroups, the population at the high end (Q5) had a larger share of elderly individuals than that at the low end (Q1) (32.7% vs 30.7%). For the cataract surgery cases, Q5 had a female majority (61.5% vs 55.7%) and more elderly individuals (84.3% vs 80.0%) than Q1.
Table 2. Characteristics of the Population and Cases in 2005 and Private Hospitalization by Cataract Surgery Rate (CSR) Quintile.
| Variable | Quintile 1 (n = 185)a | Quintile 2 (n = 184)a | Quintile 3 (n = 184)a | Quintile 4 (n = 184)a | Quintile 5 (n = 184)a |
|---|---|---|---|---|---|
| CSR per 100 000 population, median (IQR) | 128.1 (89.8-160.0) | 220.1 (200.1-240.1) | 291.1 (270.8-307.8) | 382.6 (360.9-412.4) | 568.0 (502.7-659.8) |
| Population, median (IQR), % | |||||
| Female | 53.0 (51.7-54.3) | 52.6 (51.4-53.7) | 52.7 (51.6-54.5) | 53.3 (52.0-54.6) | 53.6 (52.2-55.3) |
| Age ≥60 y | 30.7 (29.3-33.7) | 31.3 (28.9-33.6) | 31.8 (29.8-34.6) | 31.9 (30.3-34.1) | 32.7 (31.0-35.7) |
| Cataract surgery cases, median (IQR), % | |||||
| Female | 55.7 (45.5-62.5) | 57.2 (51.0-63.2) | 58.1 (53.4-63.0) | 59.5 (54.6-63.6) | 61.5 (57.2-64.7) |
| Age ≥60 y | 80.0 (72.4-88.4) | 80.3 (75.0-86.2) | 83.8 (78.7-86.9) | 84.1 (80.1-86.9) | 84.3 (81.2-86.8) |
| Private hospitalization, median (IQR), % | |||||
| 2005 | 0 | 0 (0-0.9) | 0 (0-0.2) | 0 | 0 (0-0.5) |
| 2013 | 3.3 (0-37.5) | 14.3 (0-56.5) | 11.6 (0-50.3) | 13.6 (0.4-53.2) | 10.8 (0.7-50.7) |
| 2015 | 1.3 (0-29.1) | 4.1 (0-48.2) | 4.9 (0-37.5) | 1.7 (0-25.0) | 2.4 (0-27.0) |
Abbreviations: CSR, cataract surgery rate; IQR, interquartile range.
Represents the number of contracting units for primary care per quintile of the CSR at district levels. Population and cases were Universal Coverage Scheme members 40 years or older.
The baseline CSR in Q1 was lower than that in Q5 not only by the median but also by within-group variation (IQR, 90-160 vs 503-660 cases per 100 000 population) (Figure 3). During 2009 to 2013, when the overall CSR rose rapidly, growth in the CSR in Q5 was faster than that in Q1. As a consequence, the Q5 to Q1 gap by the median and by either the lower or upper bounds of the IQR increased during this 5-year period. In addition, the IQR within each quintile increased in tandem with an increase in the median CSR. Notably, the IQR within Q5 was much larger than that in Q1. The median CSR for Q1 continued to grow until reaching a peak in 2015. Over the same period, growth in the median CSR for Q5 ceased, and consequently the Q5 to Q1 gap decreased.
Figure 3. Disparities and Trends in the District-Level Cataract Surgery Rate (CSR) Between the Baseline Q1 and Q5, 2005-2015.
The dot represents the median CSR (labeled inside) per quintile. The vertical line represents an interquartile range of the CSR within each quintile. Q1 indicates quintile 1 (20% of districts with the lowest CSR); Q5, quintile 5 (20% of districts with the highest CSR).
Discussion
During 9 years (2007-2015) of the CR implementation, the national CSR more than doubled, reaching 765.3 cases per 100 000 population, which was comparable with that in developed countries.7,8,23,24 This finding is evidence that Thailand is advancing its course toward meeting the VISION 2020 goal. The post-CR growth was faster than that in Latin America, a region where the ophthalmologist to population ratio (6.2 cases per 100 000 population) is much higher than that in Thailand.14,25 The design of the CR mitigated financial constraints on the supply side, which effectively complemented the social protection role of the UCS on the demand side.
However, the association lagged 2 to 4 years after the policy introduction, which reflected time-consuming responses by health care professionals. Rapid uptake occurred in the private sector in 2009, when a few facilities were adept in engaging service outreach paid by an exclusive CR. Three private hospitals were able to acquire 79% of cases in the private sector in 2009 within the first-year growth. The use of mobile services is a diversion from the UCS service arrangement that relied mostly on public hospitals. As a result, during 2009 to 2011, the CSR was higher and grew faster in the mobile service regions than the national average. When both mobile and hospitalized services were paid by the fee schedule in 2011, the private sector had fully engaged, and the public sector began to take off. The CSR in the regions where the mobile services used to operate continued with steady growth until 2013, when the NHSO no longer advocated mobile services. During 2014-2015, growth in the national CSR slowed down, largely because of decreasing private sector services. In Ontario, Canada, the mean number of cataract operations performed by recently graduating ophthalmologists dropped significantly after a policy of zero growth was mandated.26
Rapid uptake by the private sector has raised concern whether cataract surgery performance has missed the target for eliminating avoidable blindness by the year 2020. To mitigate the performance of surgery too early, the NHSO has mandated that for health care professionals since 2014 at least 30% of the reimbursed surgical procedures must be performed in patients with blinding cataract. This requirement was well complied with; evidence showed that almost all cases were recorded for visual impairment using explicit ICD-10 codes. In 2014 and 2015, blindness (ICD-10 codes H54.0 and H54.4) accounted for 28.8% and 37.2% of cases, respectively, with the blinding fraction being a little lower in the private sector compared with the public sector.
Another concern is whether improved access to cataract surgery would result in increased inequality in the CSR. The 2010 to 2012 peak of the inequality gap in the CSR across regions was largely driven by a notably high CSR in the top 3 administrative regions. The increasing gap seemed to be temporary, most likely because of the predominant role of mobile services in limited areas. Increased inequality in tandem with a rise in overall access has been observed in other essential services in developing countries such that well-off subgroups tended to be the first group to reap benefits from the progress. The gap between rich and poor individuals in skilled birth attendance was widening when a country’s average coverage progressed from a low rank toward the middle rank.27 Once a country reached high coverage, the top and bottom quintiles converged, and the gap narrowed. In 2015, the CSR gap in the UCS was much lower than gaps in outpatient and inpatient services (SII, 2.20% and 4.06%, respectively).28
Limitations
This study has some limitations. First, the study population was limited to UCS members. The rest of the Thai population was covered by other insurance, one for public employees and their dependents and another for employees in formal private sectors. The UCS population, mostly comprising a lower socioeconomic status, tended to have less access to high-cost health technology than members of the other 2 insurance programs.29,30 Therefore, the CSR in this study could be considered as the lower bound. Second, without control groups, this study did not demonstrate causality in the CR effect. However, the study estimated annual changes in the CSR before and after the CR implementation. By comparing across subnational areas, differential CSR trends were linked to service arrangements associated with policy interventions. Third, physical and financial barriers, knowledge, and attitude on the demand side were not examined in the present study. However, the demographics of both service recipients and the target population were compared across districts with respect to the CSR quintiles.
Conclusions
Two primary conclusions can be drawn from this study. First, financial constraints of individual health care professionals could be mitigated by an adequate funding pool with appropriate payment rates. Second, engagement with private health care professionals regarding service arrangements could help accelerate access to cataract surgery, especially in settings where health services were dominated by the public sector, making it cumbersome to reach out to areas that are difficult to access. Surveys by the NHSO31 found that the waiting time for cataract surgery was reduced by half in private hospitals. In rural India, mobile surgical units were a viable alternative associated with improved outcomes and modest complications.32 Once the backlog is cleared, cataract surgery should be performed within established infrastructures. Finally, a country’s population-based data are the key to success in the monitoring and evaluation of health priority policies.33 These include such examples as a national registry in Sweden,7 electronic health records in the present study and in the United Kingdom,8 and cohort investigations in United States,9,10 as well as institutional capacity to conduct health systems research.
eTable. Point Estimates and 95% CI of SII on CSR Across 13 Regions, 2005-2015
eFigure. Gradients in CSR Across 13 Administrative Regions; 2005, 2010 and 2015
References
- 1.West S, Sommer A. Prevention of blindness and priorities for the future. Bull World Health Organ. 2001;79(3):244-248. [PMC free article] [PubMed] [Google Scholar]
- 2.Resnikoff S, Pascolini D, Etya’ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11):844-851. [PMC free article] [PubMed] [Google Scholar]
- 3.Jenchitr W, Hanutsaha P, Iamsirithaworn S, Parnrat U, Choosri P. The National Survey of Blindness, Low Vision and Visual Impairment in Thailand 2006-2007. Thai J Pub Hlth Ophthalmol. 2007;21:11-94. [Google Scholar]
- 4.Isipradit S, Sirimaharaj M, Charukamnoetkanok P, et al. The first rapid assessment of avoidable blindness (RAAB) in Thailand. PLoS One. 2014;9(12):e114245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization What is VISION 2020? https://www.who.int/blindness/partnerships/vision2020/en/. Accessed February 21, 2017.
- 6.World Health Organization Global Initiative for Elimination of Avoidable Blindness. Geneva, Switzerland: World Health Organization; 2000. Document WHO/PBL/97.61 Rev.2. [Google Scholar]
- 7.Lundström M, Stenevi U, Thorburn W. The Swedish National Cataract Register: a 9-year review. Acta Ophthalmol Scand. 2002;80(3):248-257. [DOI] [PubMed] [Google Scholar]
- 8.Keenan T, Rosen P, Yeates D, Goldacre M. Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. Br J Ophthalmol. 2007;91(7):901-904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klein BE, Howard KP, Lee KE, Klein R. Changing incidence of lens extraction over 20 years: the Beaver Dam Eye Study. Ophthalmology. 2014;121(1):5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erie JC. Rising cataract surgery rates: demand and supply. Ophthalmology. 2014;121(1):2-4. [DOI] [PubMed] [Google Scholar]
- 11.Baltussen R, Sylla M, Mariotti SP. Cost-effectiveness analysis of cataract surgery: a global and regional analysis. Bull World Health Organ. 2004;82(5):338-345. [PMC free article] [PubMed] [Google Scholar]
- 12.Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114(9):1670-1678. [DOI] [PubMed] [Google Scholar]
- 13.Boudville AI, Anjou MD, Taylor HR. Indigenous access to cataract surgery: an assessment of the barriers and solutions within the Australian health system. Clin Exp Ophthalmol. 2013;41(2):148-154. [DOI] [PubMed] [Google Scholar]
- 14.Batlle JF, Lansingh VC, Silva JC, Eckert KA, Resnikoff S. The cataract situation in Latin America: barriers to cataract surgery. Am J Ophthalmol. 2014;158(2):242-250.e1. [DOI] [PubMed] [Google Scholar]
- 15.Aboobaker S, Courtright P. Barriers to cataract surgery in Africa: a systematic review. Middle East Afr J Ophthalmol. 2016;23(1):145-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teerawattananon K, Butchon R, Wongkittiruk K, et al. Factors associated with an accessibility of undergoing cataract surgery in Thailand [in Thai]. J Health Sci. 2011;20(S):53-68. [Google Scholar]
- 17.Mass Communication Organization of Thailand Patients are now happy that the NHSO introduced the reimbursement for cataract surgery [in Thai]. http://www.manager.co.th/QOL/ViewNews.aspx?NewsID=9530000183743. Published December 30, 2011. Accessed February 21, 2017.
- 18.National Health Security Office Annual report. https://www.nhso.go.th/files/userfiles/file. Published 2013. Accessed February 21, 2017.
- 19.Low A, Low A. Measuring the gap: quantifying and comparing local health inequalities. J Public Health (Oxf). 2004;26(4):388-395. [DOI] [PubMed] [Google Scholar]
- 20.Lagarde M. How to do (or not to do) …: assessing the impact of a policy change with routine longitudinal data. Health Policy Plan. 2012;27(1):76-83. [DOI] [PubMed] [Google Scholar]
- 21.Savin NE, White KJ. The Durbin-Watson test for serial correlation with extreme sample sizes or many regressors. Econometrica. 1977;45(8):1989-1996. [Google Scholar]
- 22.Judge GG, Griffiths WE, Hill RC, Lutkepohl H, Lee TC, eds. The Theory and Practice of Econometrics. New York, NY: John Wiley & Sons; 1985. [Google Scholar]
- 23.World Health Organization Cataract surgical rate (CSR). https://www.who.int/blindness/data_maps/cataract_surgery_rate/en/. Accessed March 15, 2017.
- 24.Sparrow JM. Cataract surgical rates: is there overprovision in certain areas? Br J Ophthalmol. 2007;91(7):852-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Medical Council of Thailand Physician statistics. https://www.tmc.or.th/pdf/stat-tmc04-14022018.pdf. Accessed April 16, 2018.
- 26.Campbell RJ, El-Defrawy SR, Bell CM, et al. Effect of cataract surgery volume constraints on recently graduated ophthalmologists: a population-based cohort study. CMAJ. 2017;189(11):E424-E430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Houweling TA, Ronsmans C, Campbell OM, Kunst AE. Huge poor-rich inequalities in maternity care: an international comparative study of maternity and child care in developing countries. Bull World Health Organ. 2007;85(10):745-754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Limwattananon S, Limwattananon C. Development of Slope Index of Inequalities in the use of public health services by population in health regions [in Thai]. J Health Systems Res. 2017;11(3):427-434. [Google Scholar]
- 29.Limwattananon C, Limwattananon S, Sakulpanit T, Greetong T, Mills A, Tangcharoensathien V. Different Provider Payment Methods: Variation in Clinical Practice: Lessons From Thailand. Bangkok, Thailand: World Bank Country Office; 2008. Country Development Partnership in Health (CDP-H) Research Report. [Google Scholar]
- 30.Limwattananon S, Limwattananon C, Cheawchanwattana A, Silkavute P, Tangcharoensathien V. Forecasted expenditure due to the use of expensive drugs in Civil Servant Medical Benefit Scheme: a comparison with Universal Health Coverage Scheme [in Thai]. J Health Systems Res. 2011;5(2):170-180. [Google Scholar]
- 31.National Health Security Office Cataract surgery waiting time survey. https://www.nhso.go.th/files/userfiles/file. Accessed March 15, 2017.
- 32.Sangameswaran RP, Verma GK, Raghavan N, Joseph J, Sivaprakasam M. Cataract surgery in mobile eye surgical unit: safe and viable alternative. Indian J Ophthalmol. 2016;64(11):835-839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bennett S, Agyepong IA, Sheikh K, Hanson K, Ssengooba F, Gilson L. Building the field of health policy and systems research: an agenda for action. PLoS Med. 2011;8(8):e1001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Point Estimates and 95% CI of SII on CSR Across 13 Regions, 2005-2015
eFigure. Gradients in CSR Across 13 Administrative Regions; 2005, 2010 and 2015