Abstract
Rationale: There is no standardized education program for patients with interstitial lung disease (ILD). Pulmonary rehabilitation is a resource for structured disease education that is still geared primarily toward patients with chronic obstructive pulmonary disease.
Objectives: The goals of this qualitative study were to identify the educational needs of patients with ILD and explore how pulmonary rehabilitation can become an appropriate setting for ILD education.
Methods: Four focus groups including 24 patients with ILD and 10 semistructured interviews with healthcare professionals with expertise in ILD and/or pulmonary rehabilitation were conducted in two academic centers (University of California San Francisco and Centre Hospitalier de l’Université de Montréal). We conducted a qualitative thematic analysis of the transcripts using an iteratively developed codebook.
Measurements and Main Results: The transcript analysis highlighted four major themes: patient dissatisfaction with the current educational model, lack of attention to emotional well-being, specific recommendations for educational content, and operationalizing education in the context of pulmonary rehabilitation. Seven key topics to be included an ILD-specific, pulmonary rehabilitation–based education program were identified: disease education, symptom management, clinical tests, autonomy, oxygen use, medications, and end-of-life counseling.
Conclusions: This study provides a better understanding of the needs of patients and healthcare providers regarding education of patients with ILD. It lays the foundation for the development of a structured education intervention that could be delivered in the context of pulmonary rehabilitation.
Keywords: interstitial lung disease, education, patient knowledge, pulmonary rehabilitation
Interstitial lung diseases (ILDs) form a heterogeneous group of disorders that negatively impact patients’ survival and health-related quality of life (1, 2). Although they may have similar clinical and radiological features, the ILDs comprise a wide range of diagnoses with different etiologies and pathophysiologies (3). Understanding ILDs can be challenging due to their generally uncommon prevalence and complex terminology. For patients with ILD, there are few educational resources currently available and none that have been systematically developed and meant to be delivered in person.
Comprehensive pulmonary rehabilitation, including educational intervention, plays a central role in the management of patients with chronic obstructive pulmonary disease (COPD) (4, 5). Likewise, pulmonary rehabilitation should be integrated into the comprehensive care of patients with ILD (6), and, as in COPD, pulmonary rehabilitation has been shown to improve exercise tolerance, health-related quality of life, and dyspnea (6–11). However, whether ILD-specific education leads to better understanding of the condition and behavioral changes, including symptom awareness, that ultimately influence clinical outcomes in patients with ILD is unknown.
Pulmonary rehabilitation presents a unique opportunity to implement an in-person education program tailored to patients with ILD. We performed a qualitative study to understand the educational needs of patients with ILD and to explore whether and how ILD-specific education can be delivered in pulmonary rehabilitation. The results of this analysis lay the foundation for the development of a structured ILD patient–targeted education program to be implemented and evaluated in the real-world setting of pulmonary rehabilitation.
Methods
This qualitative study was conducted from March to July 2015 and consisted of four focus groups of patients with ILD and 10 semistructured individual interviews of healthcare professionals with expertise in either ILD or pulmonary rehabilitation.
Participants
Patients receiving medical care at the ILD clinics at the University of California San Francisco (UCSF) or the Centre Hospitalier de l’Université de Montréal (CHUM) were invited to participate. We used purposive sampling to recruit participants with a range of ILD diagnoses, disease severities, ages, and genders. A diverse group of healthcare professionals with an expertise in either ILD or pulmonary rehabilitation were approached to participate in the individual interviews.
Procedures
An interview guide (Table 1), including a series of key open- and closed-ended questions, was developed and used for all focus groups and interviews to facilitate the discussion and ensure that all topics of interest were covered. Follow-up probes were used to gather details of responses. The same interviewer (J.M.), a pulmonologist with 3 years of experience in the care of patients with ILD and who has had training in qualitative research, conducted all of the focus groups and interviews. Sessions were digitally recorded and transcribed verbatim. Focus groups and interviews were conducted in private rooms in French at CHUM and in English at UCSF. Analysis of the transcripts was performed after each focus group and interview session to look for theme saturation. Demographics and medical information of focus group participants were obtained with a short questionnaire at the time of the focus group and completed with chart review. The institutional review boards of UCSF and the CHUM approved the study before its initiation. Written informed consent was obtained from patients and healthcare professionals before each focus group and interview.
Table 1.
Interview and focus group guide
| Healthcare professionals interview |
|---|
| Do you think patients are satisfied with the level of information they are given about ILD when they receive the diagnosis of pulmonary fibrosis or interstitial lung disease? |
| How well would you say patients understand the disease? |
| What topics do you think should be included in an ILD education program included in pulmonary rehabilitation? |
| Do you think some topics should not be addressed? |
| Given the heterogeneous nature, evolution, and treatment options of ILDs, how do you think tailored educational information should be delivered to groups of patients undergoing pulmonary rehabilitation? |
| Do you think ILD patients should be grouped and separated from COPD patients in the setting of pulmonary rehabilitation? |
| ILD patient focus group |
| Are you satisfied with the level of information you were given about ILD when you received the diagnosis of pulmonary fibrosis or interstitial lung disease? |
| Did you look for information elsewhere? |
| Did you look on the Internet to get additional information? |
| How well would you say you understand the disease? |
| What topics do you think should be included in an ILD education program in pulmonary rehabilitation? |
| Do you think some topics should not be addressed? |
| How would you want this information to be delivered (group discussion, written material, online resources, formal education program)? |
| Do you think ILD patients should be grouped and separated from COPD patients in the setting of pulmonary rehabilitation? |
Definition of abbreviations: COPD = chronic obstructive pulmonary disease; ILD = interstitial lung disease.
Data Analysis
The interviews and focus group transcripts were analyzed using grounded theory (12). Two different researchers fluent in French and English (J.M. and B.-P.D.) performed the analysis. A qualitative researcher (J.J.S., who has 12 years of experience in clinical research and care of patients with ILD) was also involved in the interpretation of the data.
Transcripts were analyzed in their original language to prevent potential translational losses. First, transcripts were independently read and reread by both coders to achieve immersion. Once immersion was achieved, each investigator identified code categories within transcripts using an emergent approach. Codes were shared, compared, and modified as necessary to achieve consensus around a draft English codebook. Codes were organized into major themes within the codebook. Using the codebook, codes were applied to three healthcare professional interviews and one patient focus group; this ensured appropriate coverage of existing codes and allowed refinement of existing codes, discussion of emergent new codes, and revision of the codebook. Each investigator then used the updated codebook to independently code all transcripts.
Interrater agreement was evaluated using Cohen’s κ. We obtained theme saturation, where no additional themes emerged, after six interviews and three focus groups. Finally, consensus on the final key themes was obtained using iterative discussion.
We made no a priori assumption that the results obtained from healthcare professionals’ interviews were going to be different from those of the patients’ focus groups. Some of the codes in the codebook were found only in transcripts of patients’ focus groups and were absent in the healthcare professionals’ interviews and vice versa. Representative quotes were identified for each of these themes. Meaningful French quotes were translated to English.
Results
A total of 24 patients participated in the four focus groups. Table 2 shows the characteristics of all patients and those for each of the focus groups. Participants had a range of ILD diagnoses; the majority had idiopathic pulmonary fibrosis (IPF). They had a wide array of physiological impairments, and nearly half required supplemental oxygen.
Table 2.
Characteristics of focus group participants
| Characteristic | Focus Group |
Total | |||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Center | UCSF | UCSF | UCSF | CHUM | — |
| Number of patients | 9 | 6 | 4 | 5 | 24 |
| Male sex, n | 5 | 4 | 2 | 2 | 13 |
| Age, yr (SD) | 67 (8) | 68 (7) | 73 (10) | 61 (8) | 67 (9) |
| Diagnosis | |||||
| IPF, n | 4 | 5 | 1 | 2 | 12 |
| HP, n | 1 | 1 | 2 | 0 | 4 |
| CTD-ILD, n | 3 | — | 1 | 1 | 5 |
| Others, n | 1 | — | — | 2 | 3 |
| FVC, % predicted (SD) | 74 (20) | 79 (18) | 61 (10) | 66 (14) | 70 (20) |
| DlCO, % predicted (SD) | 49 (12) | 54 (3) | 40 (11) | 57 (10) | 52 (10) |
| Long-term oxygen therapy, n | 5 | 3 | 1 | 1 | 10 |
| Previous participation in pulmonary rehabilitation, n | 4 | 5 | 4 | 1 | 14 |
| Previous participation in support group, n | 8 | 5 | 2 | 0 | 15 |
| Current therapy | |||||
| Prednisone | — | 1 | — | 1 | 2 |
| Azathioprine | — | 1 | — | — | 1 |
| Mycophenolate mofetil | 3 | — | 1 | 1 | 5 |
| Nintedanib | — | 1 | 1 | — | 2 |
| Pirfenidone | 3 | 3 | — | 2 | 8 |
Definition of abbreviations: CHUM = Centre Hospitalier de L’Université de Montréal; CTD-ILD = connective tissue disease–related interstitial lung disease; DlCO = diffusing capacity of the lung for carbon monoxide; HP = hypersensitivity pneumonitis; IPF = idiopathic pulmonary fibrosis; UCSF = University of California San Francisco.
Ten healthcare professionals (five from UCSF and five from CHUM) participated in the individual interviews, including four pulmonologists (three ILD physicians and one pulmonary rehabilitation physician), four nurses (two ILD nurses and two nurses conducting pulmonary rehabilitation programs), and two kinesiotherapists. All had over 5 years of experience in caring for patients with ILD in their respective fields (Table 3). One of the healthcare professionals was also an investigator in this study (C.G.).
Table 3.
Characteristics of participating healthcare professionals
| Healthcare Professional | Center | Profession | Years of Experience Caring for Patients with ILD |
|---|---|---|---|
| 1 | UCSF | Nurse | 26 |
| 2 | UCSF | Nurse | 38 |
| 3 | UCSF | Nurse | 32 |
| 4 | UCSF | Pulmonologist | 17 |
| 5 | UCSF | Pulmonologist | 39 |
| 6 | CHUM | Kinesiologist | 7 |
| 7 | CHUM | Kinesiologist | 10 |
| 8 | CHUM | Nurse | 15 |
| 9 | CHUM | Pulmonologist | 13 |
| 10 | CHUM | Pulmonologist | 11 |
Definition of abbreviations: CHUM = Centre Hospitalier de L’Université de Montréal; ILD = interstitial lung disease; UCSF = University of California San Francisco.
The transcript analysis highlighted four major themes. Themes identified in the transcriptions were similar between study sites. Within-transcript Cohen’s κ values between the two coders ranged from 0.81 to 1.0 (13, 14).
Theme 1: Patient Dissatisfaction with the Lack of Available, Decipherable Information
Unanimously, patients expressed their dissatisfaction regarding the amount and quality of information and education they received during their standard medical care. They consistently described a desire for knowledge that was not met. They wished there were more online resources, written documentation, or booklets and more education delivered by physicians during clinic visits. Many patients had difficulty stating their specific diagnosis. “I am dissatisfied; the disease was not explained to me. I feel like people assumed I know, but in general it felt like you were left, like, in the corner” (non-IPF patient, focus group 4). Patients with non-IPF diagnoses reported that they felt the majority of the educational material they came across was targeted toward IPF, highlighting the need for resources that include education on a wider range of ILD diagnoses.
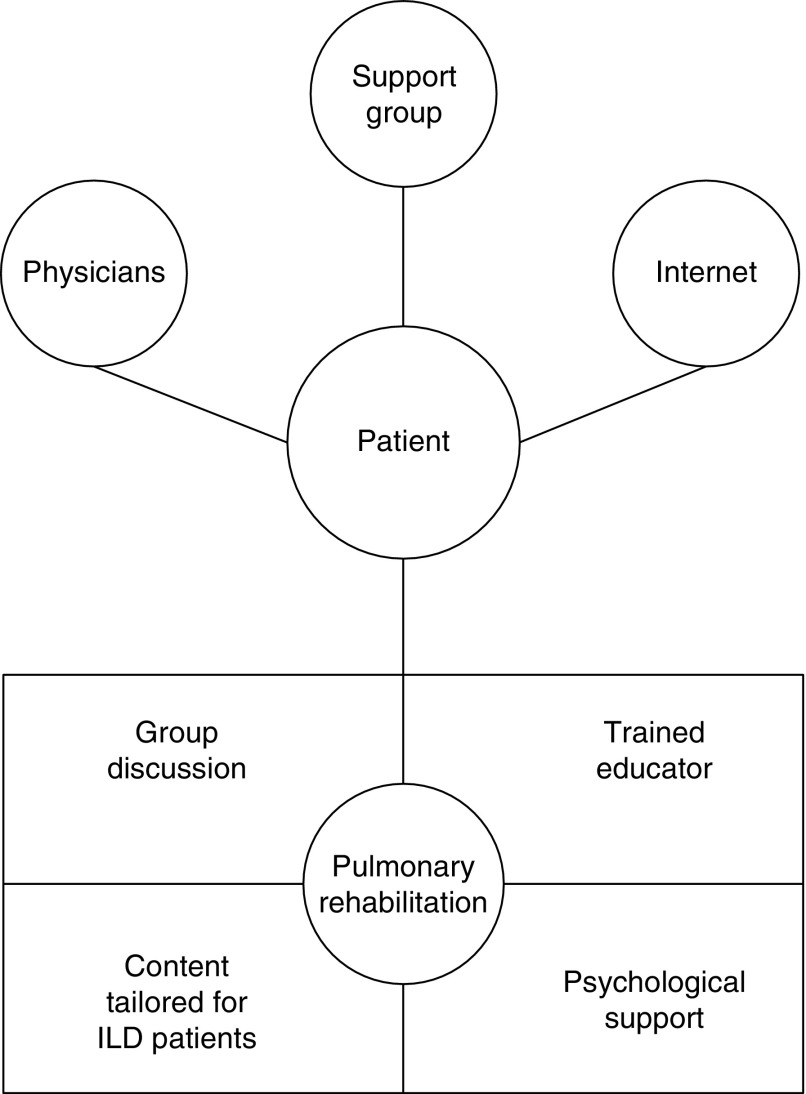
Patients described feelings of isolation, of being “left out in the dark” and lamented that they often had to acquire knowledge on the disease by themselves. They realized the information obtained in such a manner was often imprecise or unclear. They mentioned reaching out to sources such as their physicians, support group meetings; pulmonary rehabilitation; or, most frequently, the Internet (Figure 1). Patients reported that, although the Internet was an easy and accessible source of education, they had significant difficulties identifying information that was pertinent to their own diagnosis. They felt that they could easily get lost in the available content, and many patients described their overall Internet experience as “scary.” “[R]eally, I had no information, and the Internet was terrifying. Terrifying” (IPF patient, focus group 1).
Figure 1.
How pulmonary rehabilitation can enrich the available sources of education for patients with interstitial lung disease (ILD). An education program included within pulmonary rehabilitation should be built on a strong foundation of appropriately tailored topics and adequate session format. This proposed framework could address unmet educational needs and contribute to comprehensive care of the patient with ILD.
A large proportion of the available information on the Internet is about IPF. Patients who had diagnoses other than IPF had difficulty distinguishing general data on “ILD” from specific data on “IPF,” particularly information regarding prognosis. Overall, patients found information obtained on the Internet too difficult to comprehend or contextualize to be considered a satisfactory source of usable information. Patients’ uncertainty (or lack of understanding) about their specific diagnoses, confusion over the information they found, and the lack of general public awareness regarding ILD (especially compared with other diseases such as cancer, heart disease, or COPD) made it frustratingly difficult for them to adequately explain ILD to their families and friends. “The gap that we have in our knowledge is that much greater with the individuals that surround us, friends and family, and it took awhile for me to be able to describe it in such a way [so] other people could understand it” (non-IPF patient, focus group 3).
Finally, many patients mentioned that obtaining a specific diagnosis was a long journey. Several reported having to meet multiple physicians before a clear diagnosis could be made. Many were told “I don’t know what you have.” They felt that not all physicians had the same level of experience or sufficient knowledge about how to diagnose and care for patients with ILD.
Healthcare professionals were generally aware of the high level of patient dissatisfaction regarding their care and education. “I don’t think they are satisfied. I believe they are less satisfied than a patient with COPD would be” (pulmonologist, interview 9). They recognized that patients often used the Internet to fill their knowledge gaps, which often resulted in misleading information that may or may not have been appropriate for their individual diagnosis. “I think they are nearly always online and rarely picking the best resources, credible resources. Some of them that have IPF, they go on the internet and see it’s a fatal disease and stop reading. Some of them are somewhat misinformed of the reason for their disorder” (nurse, interview 2). In addition, healthcare professionals also wished there was a wider selection of education resources for patients with ILD with clearer, diagnosis-specific content.
Theme 2: Lack of Attention to Emotional Well-Being
Dissatisfaction with available, easily understood, patient-friendly educational material and the general lack of societal awareness of their diagnoses contributed to the almost universal symptoms of anxiety and/or depression patients reported. “The emotional component is not addressed at all at any point in time, and it’s probably the most important thing that you need at that point, since you can’t change the physical. You have to overcome it or compensate for it in some other ways. That never comes into play” (non-IPF patient, focus group 1). Receiving a diagnosis of ILD can be devastating, and patients felt that they were not systematically receiving the emotional support they wanted or needed. They wished there were resources, such as an available counseling psychologist or social worker, to help them immediately after they received the diagnosis and subsequently to help them deal with the anxiety associated with living with a progressive disease. “I mean, the emotional terror that you go through. The not being able to sleep at night and not being able to breath and not being able to envision a future” (IPF patient, focus group 1).
When receiving their diagnoses, patients are typically told they have an irreversible, progressive, and life-threatening disease. Patients mentioned that hearing this diagnosis created a state a shock in which they tended to focus only on the bad prognosis. This news often comes after months of tests and evaluations by many different doctors who may lack sufficient knowledge of ILD. Patients struggle with the unknown: uncertainty over what the future holds for them, not knowing what is going to happen in the upcoming weeks, let alone months or years. Even after learning more about the disease, patients found ILD difficult to comprehend and its emotional consequences a constant challenge.
Theme 3: Key Topics for Education in Pulmonary Rehabilitation
Patients and healthcare professionals globally agreed on the key topics that they believed should be included in an education program within pulmonary rehabilitation. Table 4 lists the seven key topics (pathophysiology of ILD, management of symptoms, clinical tests, autonomy, oxygen use, medications, and end-of-life counseling) and representative quotes regarding them.
Table 4.
Key educational topics
| Theme | Quotes |
|
|---|---|---|
| Patients | Healthcare Professionals | |
| Pathophysiology of ILD | “I don’t know what interstitial lung disease is. I would have liked a more basic approach in saying this is what’s going on and this is where you can learn more about it....” IPF patient (focus group 1) | “[T]alk about what’s known about it in terms of known causes, if any, and then anatomy, inflammation or fibrosis, depending on what the disorder is. Then get into specifics about each disease.” Pulmonologist (interview 5) |
| Management of symptoms | “Especially how to cope on a day-to-day basis because you basically, with this progressive disease, you’re basically constantly making adjustments for your lack of function. I guess you use the word coping, you use the word compromising or accommodating yourself. What are some of the tricks in doing that to alleviate the frustration and to be able to function as well as you can for as long as you can?” Non-IPF patient (focus group 1) | “What do you do if your symptoms are starting to overwhelm you? I think that’s really important for IPF. I [teach] it [to] everybody, but I know IPF patients can go from basically feeling healthy to really symptomatic on a dime.” Nurse (interview 3) |
| Clinical tests | “We live and die by lung capacity and DlCO. You should know what your lung capacity and your DlCO is so that you can follow your own progress.…” IPF patient (focus group 2) | “[P]atients often have questions regarding the investigation they need to go through, ‘Why do I need to see a rheumatologist?’ They want to know what tests they need to do and why.…” Pulmonologist (interview 10) |
| Autonomy | “[R]ehab should promote self-sufficiency. We’ve really talked about all of this. What are the resources? What are the websites? What can you do to enhance your health? One the things that has helped me is to understand the diagnosis and its progression and its possible origins, and all those things are, whatever pieces there are, help me to understand how I can construct this program to enhance my health.” IPF patient (focus group 2) | “I wish patients could be able to define the disease and consider all of the modifiable factors, be able to recognize them. Better yet, in the program we want patients to be able to name those behaviors and also change their behaviors and integrate this knowledge to their everyday life; we want them to be as self-sufficient as possible and be able adequately take charge [of] their disease.” Pulmonologist (interview 9) |
| Oxygen use | “The one thing that I’ve always struggled with is oxygen use and things of that sort and what are the goals.” Non-IPF patient (focus group 4) | “Why is the oxygen equipment so important? And they [say], ‘Because it’s our lifeline.’ Oxygen moves from being something sort of repulsive to them to being a lifeline for them. It becomes a very important thing.…” Nurse (interview 1) |
| Medications | “All of us probably take something that is pill form, and there was no particular discussion of those and the side effects.…” Non-IPF patient (focus group 3) | “I think people need to know how to take these and what to watch out for. People on immunosuppressants need to be reminded that they need monthly blood draws and why, and what to watch out for, so I think it’s an important topic, definitely.” Nurse (interview 8) |
| End-of-life counseling | “[I]n the back of my mind, forever since my diagnosis was, how does one die from this disease? Nobody ever explained to me how do you die. I mean, what’s the reality of it? Does it hurt? Does it not hurt? Is it like drowning? All that stuff. Is there anything that can be done to alleviate the suffering in the process? I think that has to be explained.…” IPF patient (focus group 1) | “I feel like patients appreciate when we discuss end of life. At first it may scare them, but when we develop a relationship with them, they feel more comfortable. It answers many of their questions, and they talk about it with their families…. They feel more confident to address the issue with their families, and that is important….” Kinesiologist (interview 6) |
Definition of abbreviations: DlCO = diffusing capacity of the lung for carbon monoxide; ILD = interstitial lung disease; IPF = idiopathic pulmonary fibrosis.
Emphasizing their desire to obtain honest and comprehensive information, most patients stated that no topics should be considered off-limits. They specifically insisted on needing to understand the basic mechanisms of the disease and the relationship between pathophysiological abnormalities and clinical symptoms. They felt that gaining a better understanding of their disease would help them face their illness and have more control over their lives.
Patients also highlighted their need to gain insight about the interpretation of their clinical tests (i.e., pulmonary function tests [PFTs]). They perceived the importance that physicians give to PFTs and expressed frustration at their incomprehension of these numbers, by which they felt they “live and die.” While acknowledging that the interpretation of PFTs remains a medical prerogative, patients mentioned that having more knowledge regarding the basic meaning of variables such as FVC or diffusing capacity of the lung for carbon monoxide would reassure them, in particular when trying to interpret the meaning of a temporal change in these parameters.
Patients wanted education on their medications, the use of oxygen, and how to be self-sufficient (i.e., autonomy). Oxygen therapy was a topic of high interest to all patients. Those who did not need oxygen were interested in learning how it could affect their everyday lives, while those on oxygen therapy liked to share their experiences in dealing with the equipment or about the logistics of traveling with oxygen. All patients, whether on oxygen therapy or not, found value in an education session on the topic of oxygen therapy. Patients were motivated to develop autonomy and symptom awareness skills by requesting clear, concrete, and realistic strategies to cope with their symptoms on a day-to-day basis. Healthcare professionals also believed that these skills should be central aspects of patient-focused education in pulmonary rehabilitation.
End-of-life issues were often the first education theme patients mentioned in focus groups and were felt to be one of the greatest unmet educational needs. Both patients and healthcare professionals asserted that end-of-life issues are an important topic for education, but their opinions about what should be included in the discussion was somewhat different. Healthcare professionals tended to have a more systematic approach, covering topics such as prognosis, and discussion of end-of-life issues and advanced planning with families. Patients tended to focus on the lack of information regarding the concrete sequence of events that leads to death in ILD. They also reported anxiety and had a common impression that clinicians withheld information regarding end-of-life issues. They expressed a desire to know how death would happen to them (Table 4), whether they would suffer, and whether they would feel like they were suffocating. Only one felt end-of-life issues were a sensitive and private subject for which group education was not the appropriate setting.
Theme 4: Format of an Education Session
The last key theme of the analysis concerned the organization and format of an educational intervention within pulmonary rehabilitation. Patients strongly believed in the benefits of group discussion and thought education sessions should include time for them to share and discuss matters among themselves, under supervision of a competent healthcare professional. “You’re sharing coping skills. That’s essentially what you’re doing. You’re sharing coping skills, and this is where you learn a lot how some people cope and you say to yourself, ‘I never thought about that and that’s important’” (non-IPF patient, focus group 1).
Healthcare professionals agreed that group discussion should be integrated into the education curriculum of pulmonary rehabilitation. They observed the beneficial effects of peer interaction to provide support and education through shared experiences. “That’s the positive aspect of group teaching. Patients can always find someone they can relate to who is going through similar things; they get the feeling that they are not alone. It’s helpful; it has a positive impact on the participants” (kinesiologist, interview 7). They also found value in using written material during education sessions to provide visual support. They also wished patients could have some documents to take home to consult later or to share with their families.
In addition, patients spontaneously expressed that the providers leading the education session should receive some training in adult learning theory, in addition to content expertise, to ensure the education sessions are built to enhance the learning experience of participants. For example, when asked about previous experience in pulmonary rehabilitation, one patient emphasized the need for trained educators: “They don’t understand adult learning theory, how to engage the participants, how to activate their prior knowledge, which is just part of that engagement piece, designing the lessons. They were just bubbles, sort of different topics, and you really had to work to try to connect the pieces to make it a complete necklace. I would hope that part of the result of this is [a] more standardized curriculum that also provides instructional strategies to the people that are delivering [the content] (non-IPF patient, focus group 3).
Finally, patients and healthcare professionals shared the same vision of the ideal group composition for pulmonary rehabilitation. When possible, they advised grouping patients with ILD together for education. “In an ideal world, I’d separate ILD patients from patients with COPD or asthma. ILD patients shared symptoms, shared anxiety; the diseases are just different” (nurse, interview 1). However, all agreed it might not be possible to operationalize this in clinical practice, so that having a mixed group of ILD and COPD patients together would be a reasonable alternative (as long as patients with ILD could benefit from appropriate, tailored education).
Discussion
In this qualitative study, we collected the perspectives of patients and healthcare providers regarding patient education in ILD and how it might be implemented in the clinical context, particularly in pulmonary rehabilitation. We identified four major themes: patient dissatisfaction over the lack of available, decipherable information; lack of attention to emotional well-being; key topics for education in pulmonary rehabilitation; and the suggested format of an educational session. Our findings suggest that an educational intervention for patients with ILD could reasonably be delivered in pulmonary rehabilitation. Such a program should include not only appropriately tailored, disease-based content but also, importantly, psychological support. Suggestions for the format of the program included delivery of some information by providers trained in both ILD content and adult learning theory (Figure 1) and allotment of time for group discussion and sharing of experiences between participants. Participants believed that such a program could fill glaring gaps in education currently available for patients with ILD.
Our findings reflect and extend the results of work by other investigators (15–17). Schoenheit and coworkers (15) conducted a qualitative survey of 45 patients with IPF living in Europe and identified unmet needs among this population, including easily accessible, reliable, patient-friendly learning material. In another study (18), researchers used individual interviews to collect patients’ and providers’ perspectives on themes to be included in education for patients with ILD. Like our patients, their patients identified similar topics, such as the pathophysiology of ILD, medications, management of symptoms, and end-of-life counseling. In contrast to the participants in our study, patients and healthcare professionals in that study were not in agreement about what important topics should be included in the curriculum of pulmonary rehabilitation. Specifically, patients wanted end-of-life issues to be discussed in the context of pulmonary rehabilitation, but healthcare professionals disagreed on whether this topic should be addressed. In addition, participants in our study believed that education around clinical testing (i.e., PFT interpretation) and developing skills for autonomy and symptom awareness were additional important topics not included in previous studies.
Subjects in our study noted a conspicuous absence of resources targeting mental well-being and emotional support among patients with ILD. They highlighted the emotional struggles associated with receiving a diagnosis of ILD and living with ILD on a day-to-day basis. These results are similar to those of a study aimed at understanding the perspective of patients regarding the impact of IPF on their quality of life (2). Contributing to their anxiety was the sense of insufficient ILD knowledge in some of their physicians. The relative rarity of ILDs, the need for multidisciplinary discussion of diagnosis, and the confusing, frequently changing terminology make it difficult for many physicians to gain the expertise that patients desire.
The finding of insufficient education regarding end-of-life care and management was not surprising. Although the majority of patients felt that these educational needs were a priority and could be addressed in a group setting, this feeling was not shared by all patients. In light of the sensitive nature of end-of-life counseling, a better approach may be to have an optional session geared toward this topic, allowing for accommodation of personal preferences.
Strengths and Limitations
Strengths of this study include the participation of patients and healthcare providers from two countries and the recruitment of patients with an array of fibrotic ILD diagnoses and disease severities. In addition, the data were analyzed and processed using a rigorous application of grounded theory. Limitations include the primary enrollment of patients from two academic centers. Patients seen in these ILD clinics may differ from the overall population of patients with ILD, which may limit the generalizability of some of our findings. However, the experiences shared by patients probably reflects their past experiences, including time before being seen in a specialized center. In addition, although a range of disease severities were included, the sickest population of patients with ILD could not participate, owing to limitations in their health and mobility. Finally, we used both open- and closed-ended questions in our interview guide. This could have limited the richness of the data we collected.
Implications
This study provides a better understanding of the perspective of patients and healthcare providers regarding educational needs in ILD. These findings lay the foundation for an educational framework that can be developed into a targeted educational intervention in patients with ILD. An ideal education program would include sessions with rich ILD-specific content that addresses the patients’ needs. This curriculum could be structured to enhance the participants’ learning experience. The educational intervention needs to go beyond pure education and/or advice-giving approaches, and it should also help patients learn and adopt sustainable symptom awareness skills. In such a program, patients would have the opportunity to share skills and experiences in well-led group discussions. Due to the multimodal nature of pulmonary rehabilitation, an educational intervention embedded in pulmonary rehabilitation is a promising way to provide structured education and support that is not available elsewhere. Further studies are needed to explore the impact of such an educational intervention on ILD patient–reported outcomes such as health-related quality of life.
Acknowledgments
Acknowledgment
The authors thank the healthcare professionals and patients from the UCSF Interstitial Lung Disease Program and the Centre Hospitalier de l’Université de Montréal who generously agreed to participate in this study.
Footnotes
Supported by the National Center for Advancing Translational Science under National Institutes of Health grant UCSF-CTI KL2TR000143 and by the research fund of the Interstitial Lung Disease Program of the Centre Hospitalier de l’Université de Montréal.
Author Contributions: Involvement in conception, hypothesis, and design of the study: J.M., B.-P.D., C.G., J.B., H.R.C., J.J.S., and J.S.L.; acquisition of the data: J.M. and B.-P.D.; analysis and interpretation of the data: J.M., B.-P.D., H.R.C., J.J.S., and J.S.L.; and substantial involvement in the writing and/or revision of the manuscript: J.M., B.-P.D., C.G., J.B., H.R.C., J.J.S., and J.S.L.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Travis WD, Costabel U, Hansell DM, King TE, Jr, Lynch DA, Nicholson AG, Ryerson CJ, Ryu JH, Selman M, Wells AU, et al. ATS/ERS Committee on Idiopathic Interstitial Pneumonias. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–748. doi: 10.1164/rccm.201308-1483ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swigris JJ, Stewart AL, Gould MK, Wilson SR. Patients’ perspectives on how idiopathic pulmonary fibrosis affects the quality of their lives. Health Qual Life Outcomes. 2005;3:61. doi: 10.1186/1477-7525-3-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwarz MI, King TE. Interstitial lung disease. 5th ed. Shelton, CT: People’s Medical Publishing House USA; 2010. [Google Scholar]
- 4.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ, Nishimura M, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 5.McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2:CD003793. doi: 10.1002/14651858.CD003793.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, et al. ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryerson CJ, Cayou C, Topp F, Hilling L, Camp PG, Wilcox PG, Khalil N, Collard HR, Garvey C. Pulmonary rehabilitation improves long-term outcomes in interstitial lung disease: a prospective cohort study. Respir Med. 2014;108:203–210. doi: 10.1016/j.rmed.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 8.Dowman L, Hill CJ, Holland AE. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst Rev. 2014;10:CD006322. doi: 10.1002/14651858.CD006322.pub3. [DOI] [PubMed] [Google Scholar]
- 9.Ferreira A, Garvey C, Connors GL, Hilling L, Rigler J, Farrell S, Cayou C, Shariat C, Collard HR. Pulmonary rehabilitation in interstitial lung disease: benefits and predictors of response. Chest. 2009;135:442–447. doi: 10.1378/chest.08-1458. [DOI] [PubMed] [Google Scholar]
- 10.Huppmann P, Sczepanski B, Boensch M, Winterkamp S, Schönheit-Kenn U, Neurohr C, Behr J, Kenn K. Effects of inpatient pulmonary rehabilitation in patients with interstitial lung disease. Eur Respir J. 2013;42:444–453. doi: 10.1183/09031936.00081512. [DOI] [PubMed] [Google Scholar]
- 11.Swigris JJ, Fairclough DL, Morrison M, Make B, Kozora E, Brown KK, Wamboldt FS. Benefits of pulmonary rehabilitation in idiopathic pulmonary fibrosis. Respir Care. 2011;56:783–789. doi: 10.4187/respcare.00939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strauss AL, Juliet JM. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 13.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 14.Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363–374. [PubMed] [Google Scholar]
- 15.Schoenheit G, Becattelli I, Cohen AH. Living with idiopathic pulmonary fibrosis: an in-depth qualitative survey of European patients. Chron Respir Dis. 2011;8:225–231. doi: 10.1177/1479972311416382. [DOI] [PubMed] [Google Scholar]
- 16.Duck A, Spencer LG, Bailey S, Leonard C, Ormes J, Caress AL. Perceptions, experiences and needs of patients with idiopathic pulmonary fibrosis. J Adv Nurs. 2015;71:1055–1065. doi: 10.1111/jan.12587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Collard HR, Tino G, Noble PW, Shreve MA, Michaels M, Carlson B, Schwarz MI. Patient experiences with pulmonary fibrosis. Respir Med. 2007;101:1350–1354. doi: 10.1016/j.rmed.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Holland AE, Fiore JF, Jr, Goh N, Symons K, Dowman L, Westall G, Hazard A, Glaspole I. Be honest and help me prepare for the future: what people with interstitial lung disease want from education in pulmonary rehabilitation. Chron Respir Dis. 2015;12:93–101. doi: 10.1177/1479972315571925. [DOI] [PubMed] [Google Scholar]