Abstract
There is increased recognition that lifestyle factors, including nutrition, physical activity, emotional well-being and stress management, tobacco use, alcohol consumption, and sleep habits, are major determinants of health. There is a need to teach practicing physicians, medical trainees, and other health care providers how to perform a “lifestyle history.” This article proposes 13 screening questions physicians should consider exploring with patients. It provides the rationale and scientific evidence supporting each question and includes key lifestyle counseling points for clinicians to consider.
Keywords: lifestyle medicine, medical education, clinical skills
‘However, it is important to recognize that simply asking the questions conveys to the patient that the physician values and recognizes the role of lifestyle modification in reducing risk for chronic disease.’
Introduction
Medical education has traditionally focused on the management of acute and chronic disease rather than on disease prevention and health promotion through lifestyle changes. However, there has been increased recognition in recent years that lifestyle factors, including nutrition, physical activity, tobacco use, alcohol consumption, emotional well-being and stress management, and sleep habits, are major determinants of health.1 A robust body of research has implicated modifiable lifestyle factors in the causes of many of the major chronic diseases, including cardiovascular disease, hypertension, cancer, and type 2 diabetes.1 In one study, adhering to 4 healthy lifestyle factors (never smoking, having a body mass index less than 30 kg/m2, performing 3.5 h/wk or more of physical activity, and adhering to healthy dietary principles of high intake of fruits, vegetables, and whole-grain bread and low meat consumption) was shown to lower the risk of developing chronic disease by 78%.2 This knowledge is important because the World Health Organization has predicted that by 2020, two-thirds of all diseases worldwide will be the result of lifestyle choices.3
Although physicians would benefit from the help of allied health professionals with lifestyle counseling, access to these services is often limited. A national survey of 11 170 Canadian physicians working in an office or community clinic revealed that only 17% of them had access to a registered dietitian in their practice.4 Availability of exercise physiologists and kinesiologists is even more scarce.5 In light of this, there is a critical need for physicians to become knowledgeable in lifestyle medicine.6 This has been defined as the “evidence-based practice of assisting individuals and their families to adopt and sustain behaviors that can improve health and quality of life.”7 (p202)
In a survey of 9 Canadian medical schools, most medical students reported a lack of comfort in discussing the role of nutrition in the treatment of disease.8 More than 87% reported that undergraduate medical education should dedicate more time to teaching on nutrition.8 In a recent study, primary care physicians identified time constraints and a lack of familiarity with lifestyle counseling as the main barriers to discussions around the primary and secondary prevention of childhood obesity.9 A review of the websites of medical schools in the United States identified that more than half of the physicians trained in 2013 received no formal education in physical activity.10
This article proposes 13 screening questions physicians can explore with their patients as part of the standard medical history (Table 1). It also outlines the rationale and scientific evidence behind each question. Key lifestyle counseling points are also included because the asking of the questions can serve as powerful stimulus for lifestyle medical patient education. However, it is important to recognize that simply asking the questions conveys to the patient that the physician values and recognizes the role of lifestyle modification in reducing risk for chronic disease.
Table 1.
Queen’s Lifestyle History.
| Lifestyle Medicine Domain | Screening Questions | Expanded Screening Tools |
|---|---|---|
| Nutrition | 1. Do you follow any specific dietary pattern? (eg, vegetarian, vegan, gluten free, lactose free) | IRCM Lifestyle Questionnairea |
| 2. Are you currently dieting for weight loss? | ||
| 3. How many meals do you cook from scratch versus eat out/order in/take out (including prepared supermarket counter foods) each week? | ||
| 4. What do you drink for thirst? | ||
| 5. Do personal finances influence your food choices? | ||
| Physical activity | 6. How many hours a day do you spend doing sedentary activity such as TV watching, playing/working on the computer? | IRCM Lifestyle Questionnaire |
| 7. On average, how many minutes a week are you engaged in moderate to vigorous physical activity, such as a brisk walk? | ||
| 8. How often do you do muscle and bone-strengthening activities using major muscle groups each week? | ||
| Tobacco and alcohol use | 9. Do you currently smoke or have you ever smoked tobacco? | IRCM Lifestyle Questionnaire |
| 10. How many alcoholic beverages do you consume on an average day? | CAGE Test47
AUDIT Test48 MAST Test49 T-ACE Test50 RAPS4 Test51 |
|
| Stress management | 11. In the past month, how often have you felt your stress level was not manageable? | Perceived Stress Scale58
Ardell Wellness Stress Test59 |
| Healthy relationships | 12. What personal support do you have in your life? | |
| Sleep habits | 13. How many hours do you sleep in a typical night? | Sleep Timing Questionnaire73 |
Abbreviations: ICRM, Institut de recherches cliniques de Montréal; AUDIT, Alcohol Use Disorders Identification Test; MAST, Michigan Alcoholism Screening Test; RAPS4, Rapid Alcohol Problems Screen.
IRCM Lifestyle Questionnaire is available at https://www.ircm.qc.ca/CLINIQUE/educoeur/Documents/questionnaire_EN.pdf.
The Lifestyle History represents an expansion of the traditional “Social History” and “Habits” of the clinical history to reflect the larger spheres of lifestyle medicine. The 13 screening questions are meant to quickly identify problem areas in lifestyle that can be later explored in more detail similar to other questions taught to medical students as part of the standard medical history. The authors recognize that it may be difficult to ask all 13 screening questions in a clinical encounter given time constraints, particularly because many of the questions are open-ended to invite reflection, discussion, and goal setting. Strategies to overcome this could include targeting lifestyle medicine questions to patients perceived to be at high risk for unhealthy lifestyle issues, asking a few lifestyle questions at ongoing clinical encounters with a patient, and/or scheduling a separate lifestyle medicine visit, potentially as a shared appointment with other members of the interdisciplinary lifestyle medicine team. Suggestions for expanded screening tools are also provided. An example of a lifestyle medicine note is provided in Figure 1.
Figure 1.
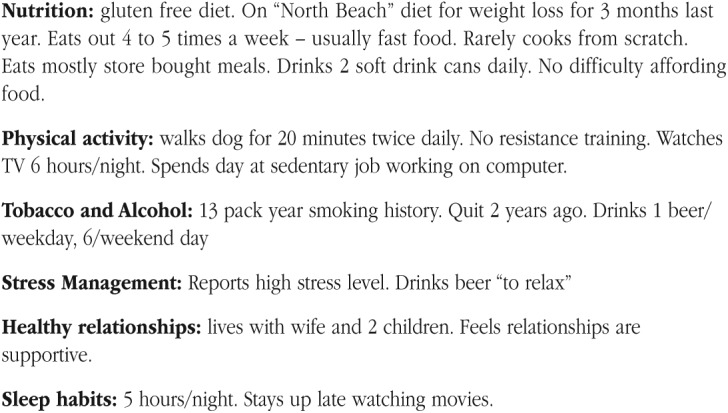
Sample lifestyle medicine history note.
Lifestyle History Questions
Do You Follow Any Specific Dietary Pattern? (eg, Vegetarian, Vegan, Gluten Free, Lactose Free)
Rationale
Nutrition science has recognized that there is no single dietary pattern that is optimal for everyone.11 Moreover, the dietary pattern that is more appropriate for someone may change throughout their life. There has been a movement away from a “good food/bad food” approach toward a focus on overall dietary patterns. Recent research suggests that optimal dietary patterns are characterized by (1) high intake of fruits, vegetables, whole grains, and water as a preferred beverage; (2) moderate intakes of dairy products, plant-based proteins, poultry, fish, and fats; and (3) limited intakes of red meat, alcohol, refined grains, and sweets.12
Canada’s Food Guide provides a pattern of healthy eating appropriate for most adults13; however, many Canadians do not follow the recommendations, with the majority eating fewer than the recommended minimum of 5 daily servings of vegetables and fruits.14 In recent years, it has become increasingly common for people to omit or limit foods from one or more food groups. Examples include omitting milk and alternatives as a result of perceived lactose intolerance and limiting grains for perceived gluten intolerance or to follow a low-carbohydrate diet. Most people should be encouraged to eat a balanced diet and not eliminate entire food groups. Consider referring patients avoiding one or more food groups to a registered dietitian to ensure that missing nutrients are obtained through other foods and/or supplements. A more comprehensive screening tool prepared by Institut de recherches cliniques de Montreal (IRCM) to assess eating, physical activity, and smoking habits is available at https://www.ircm.qc.ca/CLINIQUE/educoeur/Documents/questionnaire_EN.pdf.
Useful Counseling Points
Eat a variety of nutrient-rich foods, including whole grains, lean protein (eg, plant-based proteins), fruits and vegetables, and low-fat or fat-free dairy. Eat less food high in solid fats, added sugars, and sodium (salt).14
Make as much of your grain products whole grain as possible each day. Eat a variety of whole grains, such as barley, oats, quinoa, and wild rice. Enjoy whole grain breads, oatmeal, or whole wheat pasta.15
Try to eat 6 to 8 servings of fruits and vegetables in a variety of colors each day. Choose fresh, frozen, low-sodium canned, or dried options.13
Choose lean sources of protein: have meat alternatives such as beans and peas (kidney, pinto, black or white beans; split peas; chickpeas; hummus), soy products (tofu, tempeh, veggie burgers), and unsalted nuts and seeds. When choosing animal proteins, use low-fat cuts of beef or pork and skinless chicken or poultry. Eat at least 2 servings of fish each week. Use cooking methods such as roasting, baking, or poaching that require little or no added fat, and when using oils, choose olive, vegetable, or canola oils.15
Use the Harvard Healthy Plate to learn more about portion sizes and how to eat a balanced diet (available at http://www.health.harvard.edu/healthy-eating-plate), but generally at least half of every meal should be vegetables, and the remainder should be divided evenly between grains and a protein source.
A registered dietitian can assist patient how to eat well with a specific dietary pattern.
Are You Currently Dieting for Weight Loss?
Rationale
In 2014, 40% of Canadian men and 27.5% of women reported height and weight that classified them as overweight; 20.2% of Canadians aged 18 years and older reported figures that would classify them as obese.16 As a result, excess energy intake is a common nutritional concern. Although many adults consume too many calories, they may not be consuming sufficient macronutrients or micronutrients, particularly if they are making nutrient-poor calorie-dense choices or omitting entire food groups as part of a fad diet. As the use of fad diets is common, physicians need to be familiar with the popular ones.
Useful Counseling Points
How Many Meals Do You Cook From Scratch Versus Eat Out/Order In/Take Out (Including Prepared Supermarket Counter Foods) Each Week?
Rationale
Nutrient density is a useful concept to evaluate how healthy a food is. Nutrient-dense foods are defined as foods that provide substantial amounts of vitamins and minerals and have relatively few calories.19 Energy-dense foods provide more energy in a given quantity of food. Patients should be encouraged to get more nutrients from their calories by minimizing intake of energy-dense, nutrient-poor foods because consumption of these foods is known to be associated with increased risk of obesity and chronic disease risk.20 Fast and prepared foods are typically energy dense and associated with excessive portion size, and their consumption is contributing to the escalating rates of overweight and obesity in North America.17,21
Useful Counseling Points
What Do You Drink for Thirst?
Rationale
Sugar-sweetened beverages, such as soft drinks, fruit drinks, sports drinks, energy drinks, iced tea, and lemonade are common fluid sources. These beverages provide calories but few or no nutrients; also, calories from fluids have been proposed to be less satiating and may lead to calorie overconsumption.22 Their intake has been linked to obesity.23
Useful Counseling Points
Do Personal Finances Influence Your Food Choices?
Rationale
Food insecurity exists within a household when one or more members do not have access to the variety or quantity of food that they need because of financial strain.24 About 8% of adults and 5% of children experienced food insecurity in Canada in 2012.25 Physicians need to be aware of the importance of food insecurity as a determinant of health. The most common strategy to address food insecurity in Western countries relies on food distribution primarily in the form of food banks26; however, physicians need to be advocates for more comprehensive strategies, including government commitments to living wages and welfare, taxation reforms, and new approaches to agricultural food and nutritional policies.27
Useful Counseling Points
Become knowledgeable of food distribution resources in your community (eg, food banks, soup kitchens, community gardens, good food baskets, school breakfast/lunch programs).26
How Many Hours a Day Do You Spend Doing Sedentary Activity Such as TV Watching, Playing/Working on the Computer?
Rationale
The World Health Organization has identified physical inactivity as the fourth leading contributor to global mortality, with an estimated 3.2 million annual attributable deaths globally.28 In addition, physical inactivity is estimated to be the main driver for approximately 21% to 25% of breast and colon cancers, 27% of diabetes, and approximately 30% of ischemic heart disease burden.28 Common sedentary activities include television watching, playing video/computer games, car travel, and reading. Many modern occupations involve prolonged sitting. A recent 12-year study of 17 000 Canadians found that people spending 50% or more of their time sitting had higher mortality rates, even after controlling for age, smoking, and physical activity levels.29
The Canadian Sedentary Behavior Guidelines advice limiting how much time children spend being sedentary in front of screens or in vehicles.30 They recommend that children <2 years have no screen time and children 2 to 4 years old should limit screen time to less than 1 h/d. Although there are no sedentary time guidelines for adults, they should be encouraged to limit sedentary behavior and include physical activity breaks during sedentary time.
Useful Counseling Points
Try to limit sedentary behaviors that involve very little physical movement while awake, such as sitting or reclining while watching television or playing with nonactive electronic devices such as video games, tablets, computers, or phones.
If your work is sedentary in nature, organize physical activity breaks throughout your day.
On Average, How Many Minutes Per Week Are You Engaged in Moderate to Vigorous Physical Activity, Such as a Brisk Walk?
Rationale
Physical activity is movement that increases heart rate and breathing. It requires energy expenditure by skeletal muscle. Like appropriate nutrition, physical activity enhances health and well-being and decreases risk factors for chronic diseases.31,32 Recent research indicates that for the primary prevention of diabetes and secondary prevention of coronary heart disease, stroke, and heart failure, physical activity is as effective as, or more effective, than many drug interventions.31
On a scale relative to an individual’s personal capacity, moderate-intensity physical activity is usually a 5 or 6 on a scale of 10. As a rule of thumb, persons doing moderate-intensity activity can talk, but not sing their favorite song, during the activity. Heart rate should be 50% to 70% of maximum heart rate.33 On a scale relative to an individual’s personal capacity, vigorous-intensity physical activity is usually a 7 or 8 on a scale of 10. If a patient is doing vigorous-intensity activity, he or she will not be able to say more than a few words without pausing for a breath. Heart rate will have increased to 70% to 85% of maximum heart rate.33
Canadian guidelines for physical activity have been developed by the Canadian Society for Exercise Physiology (CSEP) and provide advice on the minimum physical activity that Canadians need to engage daily for maintaining health and well-being.30 Before starting a new exercise program, participants may use a self-guided questionnaire such as the Physical Activity Readiness Questionnaire to alert those with elevated risk to consult a health care provider before participation.34
Useful Counseling Points
Explore barriers and problem solve solutions to participation in physical activity. Commonly perceived barriers include lack of time; lack of energy or fatigue; lack of interest or motivation; long-term illness, injury, or disability; cost; feeling ill at ease or uncomfortable; fear of injury; and lack of physical skill.30
Encourage patients to do at least 150 minutes of moderate- to vigorous-intensity aerobic physical activity per week, in bouts of 10 minutes or more.30
Brisk walking is an easy activity to incorporate for most people.30
How Often Do You Do Muscle and Bone-Strengthening Activities Using Major Muscle Groups Each Week?
Rationale
Resistance training has been shown to increase lean muscle mass and muscle strength,35,36 and bone mineral density reducing risk of osteoporosis.37-39 In individuals with diabetes, it has been shown to improve glycemic control.40 The CSEP guidelines provide advice on frequency of muscle and bone-strengthening activities. They also provide advice on including physical activities to enhance balance and prevent falls in individuals older than 65 years.30
Useful Counseling Point
Try to add muscle and bone-strengthening activities using major muscle groups at least 2 d/wk.30
Do You Currently or Have You Ever Smoked Tobacco?
Rationale
Cigarette smoking is the leading preventable cause of mortality.41 The major causes of tobacco-related mortality are atherosclerotic cardiovascular disease, lung cancer, and chronic obstructive pulmonary disease.42 Screening patients for tobacco use and providing smokers with behavioral counseling and pharmacotherapy to stop smoking has been identified as one of the most valuable preventive services in health care.43
Useful Counseling Points
How Many Alcoholic Beverages Do You Consume on an Average Day?
Rationale
Excessive alcohol intake is associated with increased mortality as well as a number of adverse health and social consequences.45 Unhealthy alcohol use has been identified as the fourth leading cause of preventable death in the United States.46 A variety of validated screening tests for problem drinking exist, including the CAGE Test,47 AUDIT Alcohol Consumption Questions,48 Michigan Alcoholism Screening Test (MAST),49 T-ACE,50 and the Rapid Alcohol Problems Screen (RAPS4).51
Useful Counseling Points
According to the Dietary Guidelines for Americans 2015-2020, the US Department of Health and Human Services, and US Department of Agriculture, moderate drinking is defined as up to 1 drink per day for women and up to 2 drinks per day for men.52
According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), for men up to age 65 years, drinking at low risk for developing an alcohol use disorder is defined as no more than 4 drinks on any single day and no more than 14 drinks per week.53 For women, who tend to have lower volumes of distribution, and men older than 65 years, lower-risk alcohol use is no more than 3 drinks on any single day and no more than 7 drinks per week.53
In the Past Month, How Often Have You Felt That Your Stress Level Was Not Manageable?
Rationale
Stress is a common patient complaint; 60% to 80% of primary care visits may have a stress-related component.54 Meta-analyses have indicated that chronic stress is associated with reduced quality of life55 and increased cardiovascular risk.56 However, one study of more than 33 000 primary care office visits found that only 3% included stress management counseling.57 It was the least common type of counseling, compared with counseling about nutrition (16.8%), physical activity (12.3%), weight reduction (6.3%), and tobacco cessation (3.7%) The Perceived Stress Scale (10 questions)58 and the Ardell Wellness Stress test (25 questions)59 are 2 tools that can be used to screen for stress in more depth.
Useful Counseling Points
What Personal Support Do You Have in Your Life?
Rationale
Several studies have shown that people who have satisfying relationships with family, friends, and their community are happier, have fewer health problems, and live longer.63-65 Conversely, a relative lack of social ties is associated with depression and later-life cognitive decline as well as increased mortality.66,67 One meta-analysis, which examined data from more than 309 000 people, found that lack of strong relationships increased the risk of premature death from all causes by 50%.67 In view of this, the patient’s personal support system should be explored.
Useful Counseling Points
How Many Hours Do You Sleep in a Typical Night?
Rationale
A sufficient amount of sleep is essential for optimal physical health. The American Academy of Sleep Medicine and Sleep Research Society recommends that those aged 18 to 60 years should sleep 7 or more hours per night on a regular basis for optimal sleep health.68 Similarly, the National Sleep Foundation consensus report specifies that 7 to 9 hours is recommended for adults aged 18 to 64 years and 7 to 8 hours is recommended for those 65 years of age and older.69 Infants, children, and teenagers require substantially more sleep than adults.69 Insufficient sleep is a common problem. According to data from the National Health Interview Survey, nearly 30% of US adults reported sleeping 6 or fewer hours per day, and rates are even higher among younger adults, racial and ethnic minorities, and patients with low socioeconomic status.70 Short sleep duration has been associated with increased risk of cardiovascular disease, obesity, and all-cause mortality.71,72
The Sleep Timing Questionnaire is a tool that can be used to explore sleep habits in more depth. It includes questions about habitual wake times and bedtimes on weekdays and weekends, similar to those obtained from a sleep diary.73
Useful Counseling Points
Stick to the same sleep schedule, even on the weekends.68
Exercise daily.68
Maintain a sleep environment conducive to sleep (eg, comfortably cool temperature, reduction of environmental light and noise).68
Wind down with quiet activities that may promote sleep, such as reading with a dim light.68
If you cannot sleep, do not look at a clock. Go into another room and do something relaxing until you feel drowsy enough to fall asleep again.68
Conclusion
Given the global pandemics of chronic disease and the role of modifiable health behaviors in their prevention, lifestyle history needs to become an essential part of the standard medical history. Instruction on appropriate screening questions and counseling points should become a standard component of the curriculum of undergraduate clinical skills training and clinical encounters. A total of 13 lifestyle history standard screening questions have been proposed in this article to help identify unhealthy behaviors and replace them with ones that promote health. The number has been kept small to ensure their adoption, recognizing the reality of common time constraints in medical history taking. However, the authors hope that as medical students, physicians, and other health care providers become more comfortable and competent in taking a lifestyle history and with continuity of care, the breadth and depth of questioning and counseling can steadily expand.
Finally, the recommendations outlined above for lifestyle and dietary modifications would best be approached with motivational interviewing techniques with the goal of developing specific, measurable, achievable, realistic, and trackable (SMART) goals with evolving targets and appropriately timed follow-up to produce sustainable and effective lifestyle behavior change.74
It can also act as an important gateway to involve other members of the interdisciplinary lifestyle medicine team, including registered dietitians, exercise physiologists/exercise coaches/personal trainers/kinesiologists, psychologist/licensed therapists/health coaches, nurses, pharmacists, and lifestyle medicine physician specialists.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation. Geneva, Switzerland: WHO; 2003. WHO Technical Report, Series 916. [PubMed] [Google Scholar]
- 2. Ford ES, Bergmann MM, Kroger J, et al. Healthy living is the best revenge: findings from the European Prospective Investigation into Cancer and Nutrition-Potsdam Study. Arch Intern Med. 2009;169:1353-1362. [DOI] [PubMed] [Google Scholar]
- 3. Chopra M, Galbraith S, Damton-Hill I. A global response to a global problem: the epidemic of over nutrition. Bull World Health Organ. 2001;80:952-958. [PMC free article] [PubMed] [Google Scholar]
- 4. Rosser W. Nutritional advice in Canadian family practice. Am J Clin Nutr. 2003;77(suppl):1011S-1015S. [DOI] [PubMed] [Google Scholar]
- 5. Moore C, Lee J, Milligan J, Giangregorio L. Physical activity as medicine among family health teams: an environmental scan of physical activity services in an interdisciplinary primary care setting. Appl Physiol Nutr Metab. 2015;40:302-305. [DOI] [PubMed] [Google Scholar]
- 6. Polak R, Pojednic RM, Phillips EM. Lifestyle medicine education. Am J Lifestyle Med. 2015;9:361-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA. 2010;304:202-203. [DOI] [PubMed] [Google Scholar]
- 8. Gramlich LM, Olstad DL, Nasser R, et al. Medical students’ perceptions of nutrition education in Canadian universities. Appl Physiol Nutr Metab. 2010;35:336-343. [DOI] [PubMed] [Google Scholar]
- 9. Bourgeois N, Brauer P, Randall Simpson J, et al. Interventions for prevention of childhood obesity in primary care: a qualitative study. CMAJ Open. 2016;4:E194-E199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cardinal BJ, Park EA, Kim M, et al. If exercise is medicine, where is exercise in medicine? Review of US medical education curricula for physical activity-related content. J Phys Act Health. 2015;12:1336-1343. [DOI] [PubMed] [Google Scholar]
- 11. Office of Disease Prevention and Health Promotion. Scientific report of the 2015 Dietary Guidelines Advisory Committee: part D. Chapter 2: dietary patterns, foods and nutrients, and health outcomes. http://health.gov/dietaryguidelines/2015/qanda.asp. Published January 6, 2016. Accessed June 1, 2016.
- 12. Willett WC, Stampfer MJ. Current evidence on healthy eating. Annu Rev Public Health. 2013;34:77-95. [DOI] [PubMed] [Google Scholar]
- 13. Health Canada. Eating well with Canada’s Food Guide. http://www.hc-sc.gc.ca/fn-an/food-guide-aliment/index-eng.php. Published September 1, 2011. Accessed June 1, 2016.
- 14. Garriguet D. Nutrition: findings from the Canadian Community Health Survey. Overview of Canadians’ eating habits. Catalogue n. 82-620-MIE No. 2. http://publications.gc.ca/Collection/Statcan/82-620-M/82-620-MIE2006002.pdf. Accessed March 29, 2017.
- 15. Gonzalez-Campoy JM, St Jeor ST, Castorino K, et al. Clinical practice guidelines for healthy eating for the prevention and treatment of metabolic and endocrine diseases in adults: cosponsored by the American Association of Clinical Endocrinologists/the American College of Endocrinology and the Obesity Society. Endocr Pract. 2013;19(suppl 3):1-82. [DOI] [PubMed] [Google Scholar]
- 16. Statistics Canada. Overweight and obese adults (self-reported), 2014. http://www.statcan.gc.ca/pub/82-625-x/2015001/article/14185-eng.htm. Published November 27, 2015. Accessed June 1, 2016.
- 17. Kong A, Beresford SA, Alfano CM, et al. Self-monitoring and eating-related behaviours are associated with 12-month weight loss in postmenopausal overweight-to-obese women. J Acad Nutr Diet. 2012;112:1428-1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Freedhoff Y, Sharma AM. Best weight: a practical guide of office-based management. Canadian Obesity Network, 2010. http://www.obesitynetwork.ca/best-weight. Accessed March 31, 2017. [Google Scholar]
- 19. US Department of Health and Human Services, and US Department of Agriculture. Dietary Guidelines for Americans, 2005. 6th ed. Washington, DC: US Government Printing Office; 2005. [Google Scholar]
- 20. Nickalas TA. Nutrient profiling: the new environment. J Am Coll Nutr. 2009;28:416S-420S. [DOI] [PubMed] [Google Scholar]
- 21. Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008;9:535-547. [DOI] [PubMed] [Google Scholar]
- 22. Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health. 2007;97:667-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Buhler S, Raine KD, Arango M, Pellerin S, Neary NE. Building a strategy for obesity prevention one piece at a time: the case of sugar-sweetened beverage taxation. Can J Diabetes. 2013;37:97-102. [DOI] [PubMed] [Google Scholar]
- 24. Health Canada. 2012. Household food insecurity in Canada: overview. http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/insecurit/index-eng.php. Published July 25, 2012. Accessed June 1, 2016.
- 25. Statistics Canada. Health at a glance: food insecurity in Canada. https://www.scribd.com/document/260080624/Statistics-Canada-Food-Insecurity-in-Canada. Published March 25, 2015. Accessed March 31, 2017. Statistics Canada Catalogue no.82-624-X.
- 26. Roncarolo F, Potvin L. Food insecurity as a symptom of social disease. Can Fam Physician. 2016;62:291-292. [PMC free article] [PubMed] [Google Scholar]
- 27. Riches G. Food banks and food security: welfare reform, human rights and social policy: lessons from Canada? Soc Policy Adm. 2002;36:648-663. [Google Scholar]
- 28. World Health Organization. Physical activity. http://www.who.int/topics/physical_activity/en/. Accessed June 1, 2016.
- 29. Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41:998-1005. [DOI] [PubMed] [Google Scholar]
- 30. Canadian Society for Exercise Physiology. Canadian physical activity guidelines and Canadian sedentary behavioural guidelines: your plan to get active every day. http://www.csep.ca/cmfiles/guidelines/csep_guidelines_handbook.pdf. Accessed June 1, 2016.
- 31. Warburton DE, Charlesworth S, Ivey A, Nettlefold L, Bredin SS. A systematic review of the evidence for Canada’s physical activity guidelines for adults. Int J Behav Nutr Phys Act. 2010;7:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Blair SN, Brodney S. Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. Med Sci Sports Exerc. 1999;31(11, suppl):S646-S662. [DOI] [PubMed] [Google Scholar]
- 33. Centre for Disease Control. Target heart rate and estimated maximum heart rate. http://www.cdc.gov/physicalactivity/basics/measuring/heartrate.htm. Published August 10, 2015. Accessed June 1, 2016.
- 34. Bredin SS, Gledhill N, Jamnik VK, Warburton DE. PAR-Q+ and ePARmed-X+: New risk stratification and physical activity clearance strategy for physicians and patients alike. Can Fam Physician. 2013;59:273-277. [PMC free article] [PubMed] [Google Scholar]
- 35. Ryan AS, Hurlbut DE, Lott ME. Insulin action after resistive training in insulin resistant older men and women. J Am Geriatr Soc. 2001;49:247-253. [DOI] [PubMed] [Google Scholar]
- 36. Schwingshackl L, Dias S, Strasser B, Hoffmann G. Impact of different training modalities on anthropometric and metabolic characteristics in overweight/obese subjects: a systematic review and network meta-analysis. PLoS One. 2013;8:e82853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nelson ME, Fiatarone MA, Morganti CM. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. JAMA. 1994;272:1909-1914. [DOI] [PubMed] [Google Scholar]
- 38. Engelke K, Kemmler W, Lauber D. Exercise maintains bone density at spine and hip EFOPS: a 3-year longitudinal study in early postmenopausal women. Osteoporos Int. 2006;17:133-142. [DOI] [PubMed] [Google Scholar]
- 39. Howe TE, Shea B, Dawson LJ, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011;(7):CD000333. [DOI] [PubMed] [Google Scholar]
- 40. Gordon BA, Benson AC, Bird SR, Fraser SF. Resistance training improves metabolic health in type 2 diabetes: a systematic review. Diabetes Res Clin Pract. 2009;83:157-175. [DOI] [PubMed] [Google Scholar]
- 41. World Health Organization. World Health Organization Report on the Global Tobacco Epidemic, 2011: warning about the dangers of tobacco. http://whqlibdoc.who.int/publications/2011/9789240687813_eng.pdf. Accessed November 28, 2016.
- 42. Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses; United States, 2000-2004. MMWR Morb Mortal Wkly Rep. 2008;57:1226-1228. [PubMed] [Google Scholar]
- 43. Maciosek MV, Coffield AB, Edwards NM, et al. Priorities among effective clinical preventative services: results of a systematic review and analysis. Am J Prev Med. 2006;31:52-61. [DOI] [PubMed] [Google Scholar]
- 44. Siu AL. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women; U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2015;163;622-634. [DOI] [PubMed] [Google Scholar]
- 45. Edelman EJ, Fiellin DA. In the clinic: alcohol use. Ann Intern Med. 2016;164:ITC1. [DOI] [PubMed] [Google Scholar]
- 46. Stahre M, Roeber J, Kanny D, et al. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Prev Chronic Dis. 2014;11:E109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ewing JA. Detecting alcoholism: the CAGE questionnaire. J Am Med Assoc. 1984;252:1905-1907. [DOI] [PubMed] [Google Scholar]
- 48. Bush K, Kivlahan DR, McDonell MB. The AUDIT Alcohol Consumptions Questions (AUDIT-C). Arch Intern Med. 1998;158:1789-1795. [DOI] [PubMed] [Google Scholar]
- 49. Selzer ML. The Michigan Alcoholism Screening Test: the quest for a new diagnostic instrument. Am J Psychiatry. 1971;127:1653-1658. [DOI] [PubMed] [Google Scholar]
- 50. Sokol RJ, Martier SS, Ager JW. The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol. 1989;160:863-871. [DOI] [PubMed] [Google Scholar]
- 51. Cherpitel CJ. Screening for alcohol problems in the emergency room: a rapid alcohol problems screen. Drug Alcohol Depend. 1995;40:133-137. [DOI] [PubMed] [Google Scholar]
- 52. Office of Disease Prevention and Health Promotion. 2015-2020 Dietary guidelines for Americans. https://health.gov/dietaryguidelines/2015/. Accessed December 28, 2016.
- 53. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinician’s guide; 2005. https://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessed March 31, 2017.
- 54. Avey H, Matheny KB, Robbins A, Jacobson TA. Health care providers’ training, perceptions, and practices regarding stress and health outcomes. J Natl Med Assoc. 2003;95:836-845. [PMC free article] [PubMed] [Google Scholar]
- 55. Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: a meta-analytic review. Clin Psychol Rev. 2007;27:572-581. [DOI] [PubMed] [Google Scholar]
- 56. Roest AM, Marten EJ, de Jonge P, et al. Anxiety and risk of incident coronary heart disease; a meta-analysis. J Am Coll Cardiol. 2010;56:38-46. [DOI] [PubMed] [Google Scholar]
- 57. Nerurkar A, Bitton A, Davis RB, et al. When physicians counsel about stress: results of a national study. JAMA Intern Med. 2013;173:76-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50:613-621. [DOI] [PubMed] [Google Scholar]
- 59. Ardell DB. High Level Wellness: An Alternative to Doctors, Drugs and Disease. New York, NY: Bantam Books; 1969. [Google Scholar]
- 60. Pilkington K, Kirkwood G, Rampes H, et al. Yoga for depression: the research evidence. J Affect Disord. 2005;89:13-24. [DOI] [PubMed] [Google Scholar]
- 61. Yin J, Dishman RK. The effect of Tai Chi and Qigong practice on depression and anxiety symptoms: a systematic review and meta-regression analysis of randomized controlled trials. Ment Health Phys Act. 2014;7:135-146. [Google Scholar]
- 62. Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174:357-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377-387. [DOI] [PubMed] [Google Scholar]
- 64. Shor E, Roelfs DJ, Yogev T. The strength of family ties: a meta-analysis and meta-regression of self-reported social support and mortality. Soc Netw. 2013;35:626-638. [Google Scholar]
- 65. Yang YC, Boen C, Gerken K, et al. Social relationships and physiological determinants of longevity across the human life span. Proc Natl Acad Sci USA. 2016;113:578-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Donovan NJ, Wu Q, Rentz DM, et al. Loneliness, depression and cognitive function in older U.S. adults [published May 9, 2016]. Int J Geriat Psychiatry. doi: 10.1002/gps.4495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med. 2015;11:591-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 201;1:40-43. [DOI] [PubMed] [Google Scholar]
- 70. Schoenborn CA, Adams PF. Health behaviors of adults: United States, 2005–2007. Vital Health Stat 10. 2010;(245):1-132. http://www.cdc.gov/nchs/data/series/sr_10/sr10_245.pdf. Accessed November 29, 2016. [PubMed]
- 71. Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep. 2010;33:1037-1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, et al. Sufficient sleep duration contributes to lower cardiovascular disease risk in addition to four traditional lifestyle factors: the MORGEN study. Eur J Prev Cardiol. 2014;21:1367-1375. [DOI] [PubMed] [Google Scholar]
- 73. Monk TH, Buysse DJ, Kennedy KS, et al. Measuring sleep habits without using a diary: the sleep timing questionnaire. Sleep. 2003;26:208-212. [DOI] [PubMed] [Google Scholar]
- 74. Sim MG, Wain T, Khong E. Influencing behaviour change in general practice: part 2. Motivational interviewing approaches. Aust Fam Physician. 2009;38:986-989. [PubMed] [Google Scholar]


