Abstract
Background
High myopia is a common ocular disease worldwide. To expand our current understanding of the genetic basis of high myopia, we carried out a whole exome sequencing (WES) study to identify potential causal gene mutations.
Methods
A total of 20 individuals with high myopia were exome sequenced. A novel filtering strategy combining phenotypes and functional impact of variants was applied to identify candidate genes by multi-step bioinformatics analyses. Network and enrichment analysis were employed to examine the biological pathways involved in the candidate genes.
Results
In 16 out of 20 patients, we identified 20 potential pathogenic gene variants for high myopia. A total of 18 variants were located in myopia-associated chromosomal regions. In addition to the novel mutations found in five known myopia genes (ADAMTS18, CSMD1, P3H2, RPGR, and SLC39A5), we also identified pathogenic variants in seven ocular disease genes (ABCA4, CEP290, HSPG2, PCDH15, SAG, SEMA4A, and USH2A) as novel candidate genes. The biological processes associated with vision were significantly enriched in our candidate genes, including visual perception, photoreceptor cell maintenance, retinoid metabolic process, and cellular response to zinc ion starvation.
Discussion
Systematic mutation analysis of candidate genes was performed using WES data, functional interaction (FI) network, Gene Ontology and pathway enrichment. FI network analysis revealed important network modules and regulator linker genes (EP300, CTNNB1) potentially related to high myopia development. Our study expanded the list of candidate genes associated with high myopia, which increased the genetic screening performance and provided implications for future studies on the molecular genetics of myopia.
Keywords: Whole exome sequencing, High myopia, Pathway enrichment, GO and FI network enrichment, QTL, Genomics, Bioinformatics
Introduction
Myopia, recognized as the most common ocular disease (Holden et al., 2016; Shi et al., 2011; Vitale, Sperduto & Ferris, 2009), has a prevalence in 20–30% of Australian, American, and Western European populations (Kempen et al., 2004). One extreme type of myopia is high myopia, defined as a refractive error of at least −6.0 diopters (D) or axial length >26 mm (Young et al., 1998). It occurred in about 2.7% of the world population in 2000 and has shown significant increase in prevalence over the last two decades (Holden et al., 2016). Although myopia is usually a benign disorder that can be corrected by glasses and contact lenses, patients with high myopia are at increased risk of other complications, such as cataracts, glaucoma, retinal detachment, and posterior staphyloma (Morgan, Ohno-Matsui & Saw, 2012; Saw et al., 2005; Xu et al., 2006).
Genetic factors play a critical role in the development of high myopia based on family aggregation and twin studies (Hammond et al., 2001; Katz, Tielsch & Sommer, 1997), with its heritability estimated to be over 70% in large twin studies (Dirani et al., 2006; Lopes et al., 2009). Family linkage studies have identified 26 Quantitative Trait Loci (QTLs) (OMIM: 160700) so far (Andrew et al., 2008; Li et al., 2009; Nakanishi et al., 2009; Schwartz, Haim & Skarsholm, 1990; Young et al., 1998). However, only seven QTLs are fine-mapped to the causal genes (Table S1), a large proportion of linkage signal found in family studies still remain to be elucidated.
The inheritance mode for familial form of high myopia is complex. It may be inherited in an autosomal recessive, autosomal dominant, or X-linked recessive manner (Ng et al., 2009; Zhang, 2015). Quite a few disease-associated genes have been identified in individual studies, such as dominant genes SCO2 (Tran-Viet et al., 2013), ZNF644 (Shi et al., 2011), and P4HA2 (Guo et al., 2015); recessive genes LRPAP1 (Aldahmesh et al., 2013) and LEPREL1 (Mordechai et al., 2011); X-linked gene ARR3 (Xiao et al., 2016). As the sequencing costs keep dropping, whole exome sequencing (WES) has been gradually adopted in studies of familial or early-onset high myopia. Variants in LRPAP1, CTSH, LEPREL1, ZNF644, SLC39A5, and SCO2 genes were comprehensively screened in 298 families with early-onset high myopia (Jiang et al., 2014). However, only a small proportion of patients were found to have deleterious mutations in these six genes. Sun et al. (2015) investigated mutations in 234 genes associated with retinal dystrophies in 298 patients with early-onset high myopia. They found that 34 of 234 genes had potential pathogenic mutations including GNAT1, GUCY2D, COL2A1, COL11A1, PRPH2, FBN1, TSPAN12, CACNA1F, OPA1, PAX2, and RPGR. Recently, Kloss et al. (2017) analyzed 14 families of high myopia through WES combining with QTL overlapping analysis and identified 73 rare and 31 novel pathogenic variant candidates. Jin et al. (2017) took another approach searching for de novo mutations through WES in 18 family trios with healthy parents and early-onset high myopia children. In addition to the novel pathogenic gene BSG, two known high myopia candidate genes (LEPREL1 and GRM6), three oculopathy-related genes (FAM161A, GLA, and CACNA1F), and a further possible gene (MAOA) were also identified in this trio study.
The high prevalence of high myopia in East Asian population (Holden et al., 2016; Wu et al., 2015) and previous WES studies suggested the complex genetic mechanisms behind the disease despite its strong heritability in families. In this study, we applied a novel phenotype driven variant filtering approach on the WES data of 20 patients with familial high myopia to search for potential causal mutations. We also explored the functions of the candidate genes through gene expression profiling, network and pathway enrichment analysis.
Materials and Methods
Human subjects
This study included a total of 20 samples from 19 families (nine males and 11 females) of Han Chinese ancestry with non-syndromic familial high myopia. The human subjects were recruited at the ophthalmic clinic at Sichuan Academy of Medical Sciences & Sichuan Provincial People’s Hospital, Chengdu, China. Approval for the study was provided by the Institutional Review Board of Sichuan Provincial People’s Hospital. Written informed consent forms were signed by all patients before the collection of peripheral blood and clinical data. The refractive errors of all patients were greater than −6.00 D, as diagnosed by a team of high myopia specialists.
Exome sequencing and variant calling
Genomic DNA was isolated from peripheral blood samples of patients by using Genomic DNA Extraction Kit (Invitrogen, South San Francisco, CA, USA). The sequencing libraries were prepared and captured using SureSelect Human All Exon V6 kit (Agilent Technologies, Santa Clara, CA, USA) following the manufacturer’s instructions. Paired-end (2 × 150 bp) NGS was performed using HiSeq X-10 (Illumina, San Diego, CA, USA) according to the manufacturer’s protocol.
Raw sequencing reads were filtered using the Trimmomatic program (http://www.usadellab.org/cms/index.php?page=trimmomatic) to remove reads with low sequencing quality at both ends. The cleaned reads were mapped to human reference genome (GRCH37) by the BWA-MEM software (Li & Durbin, 2009), and Polymerase Chain Reaction (PCR) duplications were removed by Picards (http://broadinstitute.github.io/picard). Variant calling was performed by a consensus call method to reach a good balance of high sensitivity and low false positive rate. Only variants detected by at least two methods out of four haplotype-based calling algorithms (Platypus, samtools, freebayes, and GATK haplotype caller) were kept in the final variant file. Variant annotation including gene functional consequence (gene context, amino acid change, splicing effect etc.), pathogenicity predictions by multiple computational methods (SIFT, Polyphen2, MutationTaster, CADD etc.), as well as healthy population allele frequencies from 1000G (Sudmant et al., 2015), ExAC (http://exac.broadinstitute.org/), and ESP (http://evs.gs.washington.edu/) database (Lek et al., 2016) were performed using the VEP software (McLaren et al., 2016).
Variant filtering
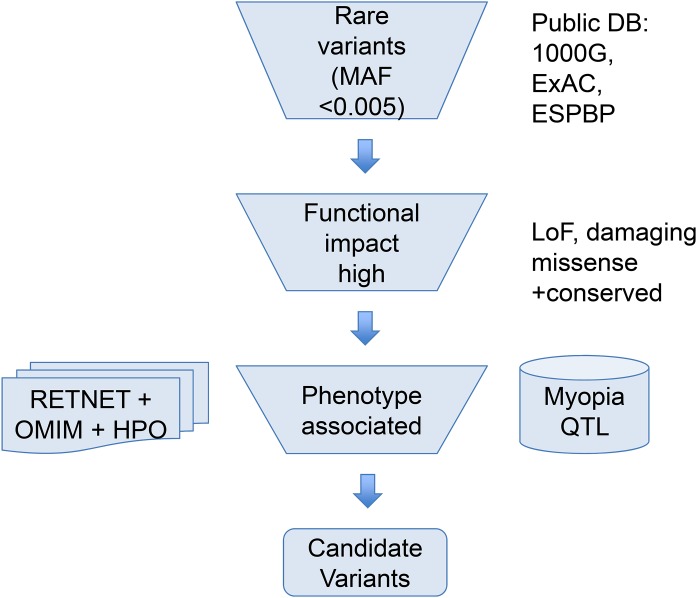
To help narrow down the potential candidate variants for high myopia, we took a phenotype driven strategy focusing on rare variants in ocular diseases and high myopia phenotype related genes as illustrated in Fig. 1. First, we used a maximum allele frequency of 0.005 in any of the three public population databases: 1000G (http://browser.1000genomes.org/index.html), ExAC, and ESP dataset to filter out common variants. Then, only variants with high functional impact (loss-of-function, or computationally predicted pathogenic missense variants) were considered. Pathogenicity of missense mutations was assumed if predicted pathogenic by at least six out of eight computational methods (SIFT, PolyPhen2, LRT, MutatationTaster, MutationAssessor, FATHMM, CADD, DANN). Lastly, we focused on phenotype relevant genes. We considered only genes meeting both of the following two criteria. Firstly, genes must be associated with eye-related diseases. The ocular disease genes were assembled from the following three databases: genes associated with the myopia phenotype term (HP:0000545) in Human Phenotype Ontology (HPO: http://human-phenotype-ontology.github.io), or ocular disease genes from RetNet database (http://www.sph.uth.tmc.edu/retnet/) and OMIM (https://www.omim.org/). Secondly, genes must be known high myopia genes from previous publications (Aldahmesh et al., 2013; Chen et al., 2013; Jiang et al., 2014; Jin et al., 2017; Kloss et al., 2017; Shi et al., 2011; Sun et al., 2015; Tran-Viet et al., 2013) (complete gene list of known genes and ocular disease genes in Table S2) or within the myopia-associated (MYP) QTL regions (Table S1). Because not all patients have syndromic severe ocular diseases, a few variants in genes causing dominant OMIM ocular diseases not satisfying clinical phenotypes were excluded.
Figure 1. Overview of the variant filtering strategy and analysis of WES data.
We applied a phenotype driven strategy to filter the potential candidate variants for high myopia. Variant frequency in populations, mutation functional impact, and phenotype associations from RetNet, HPO, and OMIM are combined to narrow down the candidate variants.
Functional enrichment and network analysis
We chose a recent RNA-seq expression profile GSE94437 and a gene microarray expression profile GSE41102 to explore the expression pattern of the compiled complete list of ocular disease genes. For the GSE94437, RPKM was transformed by log2(RPKM + 0.001). To test the expression differences of the 709 ocular disease genes versus other genes, one-sided t-test was applied to obtain the statistical significance. The Gene Ontology (GO) is a hierarchically organized, controlled vocabulary to consistently describe and annotate gene products (Ashburner et al., 2000). Joint terms may give insight on the shared biological processes, and enrichment analysis can make use of term–term relationships (Huang, Sherman & Lempicki, 2009; Kuleshov et al., 2016). The ReactomeFIViz app (Wu et al., 2014) was designed to find GO, pathways and network patterns. Thus we used the ReactomeFIViz app and Cytoscape 3.5.1 to perform GO enrichment analysis of candidate genes. Using all the protein-coding genes in the genome as background, we carried out the GO enrichment for both the 12 candidate gene set and the 709 eye disease gene set. ReactomeFIViz was also used to explore the network features of candidate genes in the manually curated pathway-based protein functional interaction (FI) network covering over 60% of human proteins (Wu, Feng & Stein, 2010).
Results
In this study, WES from 20 patients with high myopia were performed to find disease-associated mutations, followed by pathway, GO enrichment and network analysis (Materials and Methods). From WES, we generated an average of 10.7 Gb of sequence with 121× mean target coverage for each individual as paired-end, 150 bp reads. All samples had more than 95% of target bases covered by at least 10 reads. There are an average of 49,904 Single Nucleotide Polymorphisms (SNPs) and small indels called per sample. After multiple steps of variant filtering considering Minor Allele Frequency (MAF), functional impact, phenotype associations and QTL overlapping information, a total of 20 potential pathogenic (three splicing, one frame-shift, and 16 deleterious missense) heterozygous variants in 12 genes were identified in 16 patients (Table 1).
Table 1. Variants identified in patients with high myopia.
| Gene | Inheritance | Type | Patient ID | Position | Variations | dbSNP | QTL | |
|---|---|---|---|---|---|---|---|---|
| Nucleotide | Amino acid | |||||||
| ABCA4 | AR | Ocular disease gene | R0025 | 1:94490591 | c.4553G>A | p.Ser1518Asn | – | MYP14 |
| ADAMTS18 | AR | Known HM gene | R0017 | 16:77334288 | c.2546G>A | p.Gly849Asp | – | – |
| CEP290 | AR | Ocular disease gene | R0031 | 12:88519100 | c.1112T>C | p.Val371Ala | – | MYP3 |
| R0026 | 8:2975943 | c.6408C>G | p.Asn2136Lys | rs778164827 | MYP10 | |||
| CSMD1 | Known HM gene | R0027 | 8:3165341 | c.3826G>A | p.Glu1276Lys | rs534926586 | MYP10 | |
| R0029 | 8:3165341 | c.3826G>A | p.Glu1276Lys | rs534926586 | MYP10 | |||
| HSPG2 | AR | Ocular disease gene | R0023 | 1:22154919 | c.12238G>A | p.Val4080Met | – | MYP14 |
| R0011 | 1:22207207 | c.1940G>A | p.Arg647Gln | – | MYP14 | |||
| P3H2 | AR | Known HM gene | R0031 | 3:189692463 | c.1336C>T | p.Leu446Phe | – | – |
| PCDH15 | AR | Ocular disease gene | R0018 | 10:55973726 | c.1081_1082delGA | p.Asp361LeufsTer6 | – | MYP15 |
| RPGR | X-linked | Known HM gene | R0016 | X:38147035 | c.1832A>G | p.Asn611Ser | rs774982456 | MYP13 |
| R0015 | X:38182648 | c.154+4A>G | Splicing | rs764483977 | MYP13 | |||
| SAG | AR | Ocular disease gene | R0021 | 2:234217902 | c.72_75+15delATCGGTGAGTGGTGCACAA | Splicing | rs771810575 | MYP12 |
| SEMA4A | AR/AD | Ocular disease gene | R0019 | 1:156146474 | c.1972C>T | p.Arg658Trp | rs756847201 | MYP14 |
| R0012 | 1:156126310 | c.245A>G | p.Glu82Gly | – | MYP14 | |||
| SLC39A5 | AD | Known HM gene | R0020 | 12:56629416 | c.877G>A | p.Gly293Arg | rs756666376 | MYP24 |
| R0018 | 1:216419965 | c.2771C>T | p.Pro924Leu | – | MYP14 | |||
| USH2A | AR | Ocular disease gene | R0019 | 1:216372968 | c.3811+1G>A | Splicing | – | MYP14 |
| R0014 | 1:215821999 | c.14453C>T | p.Pro4818Leu | rs143344549 | MYP14 | |||
| R0015 | 1:216498726 | c.1064T>C | p.Val355Ala | rs746683099 | MYP14 | |||
Notes:
Chromosome position in accordance with GRCh37/hg19 assembly.
The HM is abbreviation of the high myopia.
There were eight pathogenic variants identified from five known high myopia genes, including ADAMTS18, CSMD1, P3H2, RPGR and SLC39A5. Patient R0020 had a clear molecular diagnosis with one missense variant rs756666376 in gene SLC39A5 (MYP24, autosomal dominant inheritance). Rs756666376 (p.Gly293Arg) is extremely rare in healthy populations, absent in 1000G data, with only one heterozygote in 4,325 East Asians (MAF = 0.00012) and two heterozygotes in 33,359 Non-Finnish Europeans (MAF = 0.00003) in the ExAC database. The SNP is highly conserved and predicted to be deleterious by all of the eight computational methods in our variant annotation. The RPGR gene is located on the Xp21.1 and plays a role in ciliogenesis and photoreceptor integrity. In gene RPGR, sample R0015 had a heterozygous loss-of-function mutation in the second intron (c.154+4A>G) potentially affecting splicing as predicted by the adaptive boosting method in the splicing consensus region (Jian, Boerwinkle & Liu, 2014) and sample R0016 had a rare heterozygous pathogenic missense mutation (rs774982456, c.1832A>G).
Other than the known high myopia genes, we also discovered 12 rare potentially pathogenic heterozygous variants located in other MYP QTL regions, suggesting potential new candidate genes explaining these QTLs. Among these ocular disease related or direct high myopia related genes, five genes (CSMD1, HSPG2, RPGR, SEMA4A and USH2A) have pathogenic variants in multiple patients.
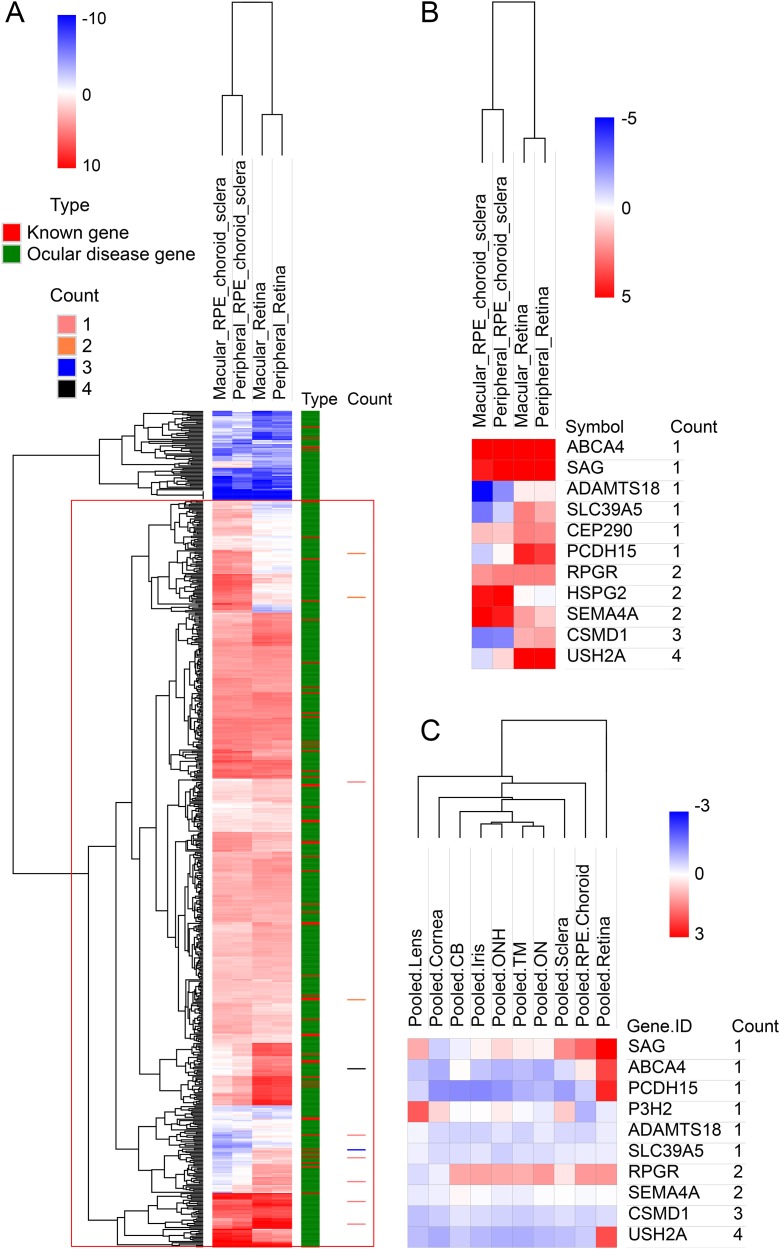
To look deep into the genes with pathogenic variants associated with high myopia, we assembled a list of 709 genes associated with eye diseases (details in variant filtering section of Materials and Methods), including 58 known high myopia genes and 651 ocular disease genes (Table S2). Clinical phenotype related studies have shown that retinal, choroidal, and scleral lesions are high-frequency phenotypes in high myopia patients (Brussee et al., 2014; Gupta et al., 2015, 2017). It would be natural to assume that myopia related genes would be highly expressed in retina and sclera tissues. To test this hypothesis, we first explored the expression pattern of all the 709 eye disease genes. The results showed that in the RNA-seq dataset, the expression of 709 genes was significantly higher than that of other genes in retina, retinal pigment epithelium, choroid and sclera (p < 0.001; Fig. S1). All candidate genes in our own high myopia cohort were located in the positive expression class when using the 709 eye disease genes as background (Fig. 2A). Looking further into the candidate gene expression differences among the three tissues, we found that five genes (PCDH15, CEP290, SLC39A5, CSMD1 and USH2A) have much higher expression in retinas (macular retina and peripheral retina), while ABCA4, SAG, RPGR, and SEMA4A are highly expressed in both sclera and retina (Fig. 2B). Microarray dataset confirmed the higher expression in retina for genes PCDH15 and USH2A (Fig. 2C).
Figure 2. Hierarchical cluster analysis of gene expression.
(A) The heatmap of 709 known genes associated with eye diseases in RNA-seq expression profile. The 709 genes were divided into known high myopia genes and ocular disease genes, as shown in different colors in type column. Count column represents the sample count of pathogenic variants for our candidate genes. (B) The heatmap of candidate genes in RNA-seq expression profile. (C) The heatmap of candidate genes in microarray expression profile.
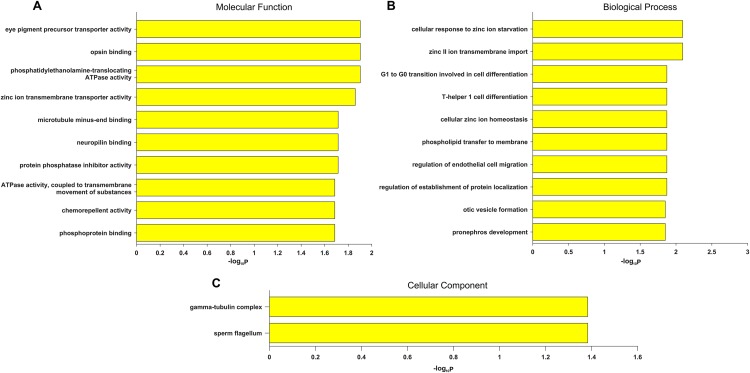
Gene Ontology term enrichment was carried out for a comprehensive functional analysis of the 12 genes found in this study. Because our bioinformatics pipeline has a filtering step to include only eye disease related genes, this could lead to potential bias in the enrichment signal. Thus we did two GO enrichment analyses using either our 12 genes, or the 709 eye disease genes (complete list of enriched GO terms from both analyses are in Table S3). Other than the enriched GO terms like visual perception, photoreceptor cell maintenance, retinoid metabolic process shared with the 709 genes, significant enrichment was uniquely observed in our candidate genes in eye pigment precursor transporter activity, opsin binding, zinc ion transmembrane related processes, microtubule binding etc. (Fig. 3). Interestingly, the visual phototransduction pathway was enriched by pathway analysis. Visual phototransduction is the photochemical reaction that takes place when light is converted to an electric signal in the retina (Smith, Sivaprasad & Chong, 2016). It’s not surprising the malfunction of genes in this pathway will potentially lead to myopia. This pathway was also found highly enriched in differentially expressed genes during myopia development in a mouse study (Metlapally et al., 2016), which corroborated these genes’ potential causal roles in high myopia.
Figure 3. Top 10 significantly enriched GO terms only in candidate genes and not in the 709 eye disease genes.
(A) Molecular function. (B) Biological process. (C) Cellular component. x-axis is the −log10 (BH adjusted P-value) from hypergeometric test of enrichment analysis. Complete list of enriched GO terms in Table S3.
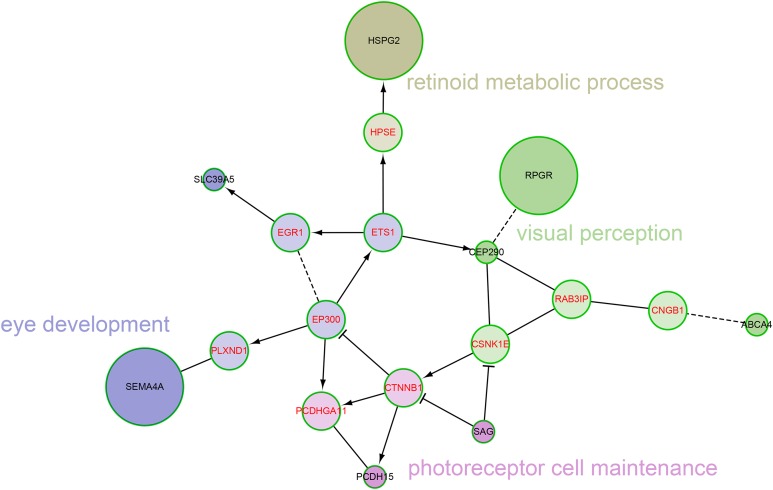
We also explored the network characteristics in a FI network (Wu, Feng & Stein, 2010). Focused on the 12 genes from our own cohort, except for the direct interaction between RPGR and CEP290, other genes are scattered, but all genes can be linked to form a large network by some linker genes, such as EP300, CTNNB1 (Fig. 4). A network clustering algorithm (Newman, 2006) divided this network into four network modules. The principal biological process of each module was eye development, retinoid metabolic process, visual perception and photoreceptor cell maintenance, respectively. There were some differences between modules in biological processes, but they were all related to vision. When using the 709 genes as background, only GO term photoreceptor cell cilium was found enriched in the modules (Fig. S2). EP300 encodes protein p300, which is a transcriptional co-activator regulating hundreds of genes’ transcription via chromatin remodeling, and is important in the processes of cell proliferation and differentiation. Mutations in EP300 are known to cause Rubinstein–Taybi syndrome (RTS). Interestingly, RTS patients with EP300 mutations were frequently documented with severe myopia phenotype (Bartholdi et al., 2007; Fergelot et al., 2016). Various visual defects (including familial exudative vitreoretinopathy, retina detachment and myopia etc.) have also been reported in recent WES studies of people with mutations in CTNNB1 (Li et al., 2017; Panagiotou et al., 2017).
Figure 4. The network modules associated with high myopia candidate genes and linker genes in the functional interaction (FI) network.
This network can be divided into four network modules. The background colors of genes represent different modules. Principal biological process of each module was described. The candidate genes are black in text color, and the linker genes are red in text color. The circle size of each candidate gene is proportional to the number of samples with pathogenic variants for the gene.
Discussion
Whole genome sequencing and WES have now entered medical practice (Biesecker & Green, 2014). Whole genome sequencing is the most powerful method of disease gene identification, because this method targets both coding and regulatory non-coding variants, and can identify disease genes caused by SNVs, large indels, and other large structure variants as well. However, its cost is still daunting. Some previous studies have estimated that ∼85% of Mendelian disease mutations are located within the coding region, canonical splice acceptor and donor sites (Stenson et al., 2017). Thus the WES becomes the sweet spot rather than Whole Genome Sequencing (WGS) (Teer & Mullikin, 2010). We used WES to identify causal gene mutations in 20 patients with high myopia. Potential pathogenic mutations were identified in 16 patients (80.0%, 16/20). A total of 20 mutations in 12 genes were potentially pathogenic variants for high myopia. Compared to the discovery rate in previous studies (Chen et al., 2013; Kloss et al., 2017; Sun et al., 2015), our phenotype driven filtering method yielded higher diagnostic rate.
In our study, SEMA4A, RPGR, and HSPG2 each had two pathogenic mutations detected in our probands. Gene SEMA4A encodes a member of the semaphorin family of soluble and transmembrane proteins. This gene maps to chromosome 1p36, which is located within the MYP14 locus (Abid et al., 2006; Wojciechowski et al., 2006). Mutation in codon 345 from G to C and in codon 350 from T to G in exon 10 of the SEMA4A gene resulted in an asp345-to-his (D345H) and a phe350-to-cys (F350C) substitution, respectively. A link between those two mutations and retinitis pigmentosa and retinal degeneration has been demonstrated (Abid et al., 2006; Berger, Kloeckener-Gruissem & Neidhardt, 2010). Retinitis pigmentosa GTPase regulator (RPGR) is one of the main genes causing X-linked retinitis pigmentosa (XLRP). It was suggested that over 70% of XLRP cases were caused by RPGR mutations (Breuer et al., 2002; Sharon et al., 2003). Multiple studies have shown that female heterozygous RPGR mutation carriers had early-onset high myopia in one of two eyes, especially those with protein truncating variants (Jin et al., 2006; Yokoyama et al., 2001). Some families showed even full penetrance of high myopia in heterozygous carriers (Parmeggiani et al., 2016). Both patients with a RPGR mutation are female carriers in our study. The incomplete penetrance of XLRP phenotype of other RPGR carriers suggested that annual follow up examinations checking symptoms of Retinitis Pigmentosa (RP) is warranted. Gene HSPG2 encodes a protein called perlecan (Farach-Carson & Carson, 2007; Warren et al., 2015). Perlecan is a heparan sulfate proteoglycan, which interacts with many other proteins and has a variety of functions, such that mutation of the gene has pleiotropic effects. Schwartz–Jampel syndrome is a rare autosomal recessive skeletal dysplasia with myotonia, short stature, and low-set ears and myopia (Kubrey, Solanki & Agrawal, 2015). The two damaging missense mutations (c.12238G>A and c.1940G>A) in HSPG2 each occurred in one patient. In our current cohort, four heterozygote variants in gene USH2A were identified, which fall within QTL MYP14. USH2A is a large gene with 73 exons and encodes at least two different isoforms. The mutations in the USH2A genes are responsible for 5∼10% of the cases with retinitis pigmentosa and 60∼90% of the cases with Usher syndrome type II (Baux et al., 2014; Pennings et al., 2004; Slijkerman et al., 2016).
Gene ABCA4 is specifically expressed in cone and rod photoreceptor outer segments (Molday, Rabin & Molday, 2000). The ABCA4 protein is active following phototransduction. ABCA4 mutations can result in multiple vision related phenotypes (Cideciyan et al., 2009; Klevering et al., 2004; Shroyer et al., 1999; Valverde et al., 2007) including Retinitis pigmentosa, Fundus flavimaculatus, Cone-rod dystrophy, and Stargardt disease (Lin et al., 2016), which is characterized by juvenile macular degeneration. In addition, a missense variant c.1268A>G in ABCA4 was recently found to be responsible for myopia (D’Angelo et al., 2017). A novel missense rare variant (not observed in 1000G, ESP, or ExAC database) c.4553G>A (p.Ser1518Asn) was found in our patient R0025. Yzer et al. (2012) made a mutation analysis for gene CEP290 and found that patients with a different mutation c.5587–1G>C showed myopia. Based on linkage and haplotype analysis, Nallasamy et al. (2007) identified a presumptive myopia locus in gene PCDH15. A novel frameshift mutation (c.1081_1082delGA) was found in one patient R0018. These functional evidences suggested that carriers of high impact variants in these severe recessive inheritance ocular disease genes might be at higher risk for high myopia. When we relaxed the computational prediction filtering criteria for missense variants to at least five or four out of eight methods, we obtained one or two extra candidate variants (Table S4). This suggested that our pipeline is relatively robust to the computational prediction cut-offs. Despite published evidences of the connections with myopia for the genes found in our cohort, none of the candidate variants were found in previous published sequencing studies of myopia (Aldahmesh et al., 2013; Chen et al., 2013; Jiang et al., 2014; Jin et al., 2017; Kloss et al., 2017; Shi et al., 2011; Sun et al., 2015; Tran-Viet et al., 2013), which highlighted the strong heterogeneity even in familial high myopia. The molecular functional impact of these mutations on the penetrance and severity of various ocular disease phenotypes would need further functional studies.
There are some limitations to our current study due to the small sample size and availability of family genetic data. Although our phenotype driven analysis approach has boosted the probabilities of the final variants associated with high myopia, the statistical significance of any genuine associated genes would need a large sample size gene-level burden test (Lee et al., 2014). Alternatively, extra genetic validation of the causal relationship of these variants with high myopia would require family segregation analysis with extended family phenotyping and genotyping. In our study, R0027 (daughter) and R0029 (father) are the only two samples from the same family. After our bioinformatics filtering process, there are two candidate variants left in both patients and both variants are shared and consistent with Mendelian inheritance. One is the heterozygote c.3826G>A SNP in CSMD1 listed in Table 1, the other is a missense variant c.2338C>G (p.Pro780Ala) in COL4A5 on chromosome X with the daughter’s genotype being a heterozygote and the father’s genotype being a hemizygote. Deletions or pathogenic missense variants in COL4A5 are known to cause X-linked dominant Alport syndrome (Knebelmann et al., 1996), however, neither patient exhibits the clinical phenotypes of Alport syndrome. Therefore, this COL4A5 variant was excluded from our final candidate list.
Conclusions
There is a large proportion of genetic heritability of high myopia still unexplained by known myopia genes. WES enables thorough and unbiased genetic analysis of candidate genes as well as novel gene discoveries. In this study, we took a novel bioinformatics screening approach combining ocular disease gene annotation, myopia phenotype to gene association, and rare variant functional effect filtering narrowing down potential causal variants. Systematic mutation analysis of high myopia genes was further analyzed by FI network, GO and pathway enrichment, which expanded our current understanding of high myopia. These variants, especially those on novel high myopia genes, expanded the mutation spectrum of myopia genes and provided clues for further genetic screening targets.
Supplemental Information
Positions are QTL positions on human genome assembly GRCh37.
Known genes are genes known to be associated with high myopia based on OMIM (https://www.omim.org/) or previous publications. Ocular disease genes are genes associated with eye diseases excluding the known genes, assembled from RetNet database (http://www.sph.uth.tmc.edu/retnet/) or OMIM.
Only GO terms with an BH adjusted FDR <0.05 were included in the table. MF, Molecular Function; BP, Biological Process; CC, Cellular Component.
Chromosome position is based on GRCh37/hg19 assembly. HM stands for high myopia.
Compare to other genes in the genome, HM know genes and ocular disease genes are highly expressed in retina, retinal pigment epithelium (RPE), choroid and sclera. The values shown in the heatmap are log2(RPKM+0.001).
This network can be divided into 4 network modules. Principal biological process of each module was calculated using the eye disease genes as background instead of the genomic background as in Fig. 4. The rest is the same as in Fig. 4.
Acknowledgments
We would like to thank all the patients for participating in this study, and Dr. Yongcheng Dong and Xin Ma for feedback on bioinformatics analysis.
Funding Statement
This work was supported by Specialized Research Fund for the Doctoral Program of Higher Education (Grant No. 20130181110079) and the National Major Scientific Equipment program (Grant No. 2012YQ12008005). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Ling Wan conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Boling Deng performed the experiments, approved the final draft.
Zhengzheng Wu performed the experiments, approved the final draft.
Xiaoming Chen conceived and designed the experiments, contributed reagents/materials/analysis tools, authored or reviewed drafts of the paper, approved the final draft.
Human Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
Approval for the study was provided by the Institutional Review Board of Sichuan Provincial People’s Hospital.
Data Availability
The following information was supplied regarding data availability:
The raw sequence data reported in this paper are deposited in the Genome Sequence Archive (Genomics, Proteomics & Bioinformatics 2017), Beijing Institute of Genomics (BIG), Chinese Academy of Sciences, under accession numbers CRA000764 and CRA000769, publicly accessible at http://bigd.big.ac.cn/gsa.
References
- Abid et al. (2006).Abid A, Ismail M, Mehdi SQ, Khaliq S. Identification of novel mutations in the SEMA4A gene associated with retinal degenerative diseases. Journal of Medical Genetics. 2006;43(4):378–381. doi: 10.1136/jmg.2005.035055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldahmesh et al. (2013).Aldahmesh MA, Khan AO, Alkuraya H, Adly N, Anazi S, Al-Saleh AA, Mohamed JY, Hijazi H, Prabakaran S, Tacke M, Al-Khrashi A, Hashem M, Reinheckel T, Assiri A, Alkuraya FS. Mutations in LRPAP1 are associated with severe myopia in humans. American Journal of Human Genetics. 2013;93(2):313–320. doi: 10.1016/j.ajhg.2013.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrew et al. (2008).Andrew T, Maniatis N, Carbonaro F, Liew SH, Lau W, Spector TD, Hammond CJ. Identification and replication of three novel myopia common susceptibility gene loci on chromosome 3q26 using linkage and linkage disequilibrium mapping. PLOS Genetics. 2008;4(10):e1000220. doi: 10.1371/journal.pgen.1000220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashburner et al. (2000).Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, Davis AP, Dolinski K, Dwight SS, Eppig JT, Harris MA, Hill DP, Issel-Tarver L, Kasarskis A, Lewis S, Matese JC, Richardson JE, Ringwald M, Rubin GM, Sherlock G, The Gene Ontology Consortium Gene ontology: tool for the unification of biology. Nature Genetics. 2000;25(1):25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholdi et al. (2007).Bartholdi D, Roelfsema JH, Papadia F, Breuning MH, Niedrist D, Hennekam RC, Schinzel A, Peters DJM. Genetic heterogeneity in Rubinstein–Taybi syndrome: delineation of the phenotype of the first patients carrying mutations in EP300. Journal of Medical Genetics. 2007;44(5):327–333. doi: 10.1136/jmg.2006.046698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baux et al. (2014).Baux D, Blanchet C, Hamel C, Meunier I, Larrieu L, Faugere V, Vache C, Castorina P, Puech B, Bonneau D, Malcolm S, Claustres M, Roux AF. Enrichment of LOVD-USHbases with 152 USH2A genotypes defines an extensive mutational spectrum and highlights missense hotspots. Human Mutation. 2014;35(10):1179–1186. doi: 10.1002/humu.22608. [DOI] [PubMed] [Google Scholar]
- Berger, Kloeckener-Gruissem & Neidhardt (2010).Berger W, Kloeckener-Gruissem B, Neidhardt J. The molecular basis of human retinal and vitreoretinal diseases. Progress in Retinal and Eye Research. 2010;29(5):335–375. doi: 10.1016/j.preteyeres.2010.03.004. [DOI] [PubMed] [Google Scholar]
- Biesecker & Green (2014).Biesecker LG, Green RC. Diagnostic clinical genome and exome sequencing. New England Journal of Medicine. 2014;370(25):2418–2425. doi: 10.1056/NEJMra1312543. [DOI] [PubMed] [Google Scholar]
- Breuer et al. (2002).Breuer DK, Yashar BM, Filippova E, Hiriyanna S, Lyons RH, Mears AJ, Asaye B, Acar C, Vervoort R, Wright AF, Musarella MA, Wheeler P, MacDonald I, Iannaccone A, Birch D, Hoffman DR, Fishman GA, Heckenlively JR, Jacobson SG, Sieving PA, Swaroop A. A comprehensive mutation analysis of RP2 and RPGR in a North American cohort of families with X-linked retinitis pigmentosa. American Journal of Human Genetics. 2002;70(6):1545–1554. doi: 10.1086/340848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brussee et al. (2014).Brussee C, Buitendijk GHS, Springelkamp H, Snabel M, Luyten GPM, Van Rijn GA, Boon CJF, Geerards A, Verhoeven VJM, Klaver CCW. Frequency of retinal pathology in high myopia. The MYST study. Investigative Ophthalmology & Visual Science. 2014;55:3617. [Google Scholar]
- Chen et al. (2013).Chen Y, Zhang Q, Shen T, Xiao X, Li S, Guan L, Zhang J, Zhu Z, Yin Y, Wang P, Guo X, Wang J, Zhang Q. Comprehensive mutation analysis by whole-exome sequencing in 41 Chinese families with Leber congenital amaurosis. Investigative Opthalmology & Visual Science. 2013;54(6):4351–4357. doi: 10.1167/iovs.13-11606. [DOI] [PubMed] [Google Scholar]
- Cideciyan et al. (2009).Cideciyan AV, Swider M, Aleman TS, Tsybovsky Y, Schwartz SB, Windsor EA, Roman AJ, Sumaroka A, Steinberg JD, Jacobson SG, Stone EM, Palczewski K. ABCA4 disease progression and a proposed strategy for gene therapy. Human Molecular Genetics. 2009;18(5):931–941. doi: 10.1093/hmg/ddn421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Angelo et al. (2017).D’Angelo R, Donato L, Venza I, Scimone C, Aragona P, Sidoti A. Possible protective role of the ABCA4 gene c.1268A>G missense variant in Stargardt disease and syndromic retinitis pigmentosa in a Sicilian family: preliminary data. International Journal of Molecular Medicine. 2017;39(4):1011–1020. doi: 10.3892/ijmm.2017.2917. [DOI] [PubMed] [Google Scholar]
- Dirani et al. (2006).Dirani M, Chamberlain M, Shekar SN, Islam AF, Garoufalis P, Chen CY, Guymer RH, Baird PN. Heritability of refractive error and ocular biometrics: the Genes in Myopia (GEM) twin study. Investigative Opthalmology & Visual Science. 2006;47(11):4756–4761. doi: 10.1167/iovs.06-0270. [DOI] [PubMed] [Google Scholar]
- Farach-Carson & Carson (2007).Farach-Carson MC, Carson DD. Perlecan—a multifunctional extracellular proteoglycan scaffold. Glycobiology. 2007;17(9):897–905. doi: 10.1093/glycob/cwm043. [DOI] [PubMed] [Google Scholar]
- Fergelot et al. (2016).Fergelot P, Van Belzen M, Van Gils J, Afenjar A, Armour CM, Arveiler B, Beets L, Burglen L, Busa T, Collet M, Deforges J, De Vries BB, Dominguez Garrido E, Dorison N, Dupont J, Francannet C, Garcia-Minaur S, Gabau Vila E, Gebre-Medhin S, Gener Querol B, Genevieve D, Gerard M, Gervasini CG, Goldenberg A, Josifova D, Lachlan K, Maas S, Maranda B, Moilanen JS, Nordgren A, Parent P, Rankin J, Reardon W, Rio M, Roume J, Shaw A, Smigiel R, Sojo A, Solomon B, Stembalska A, Stumpel C, Suarez F, Terhal P, Thomas S, Touraine R, Verloes A, Vincent-Delorme C, Wincent J, Peters DJ, Bartsch O, Larizza L, Lacombe D, Hennekam RC. Phenotype and genotype in 52 patients with Rubinstein-Taybi syndrome caused by EP300 mutations. American Journal of Medical Genetics Part A. 2016;170(12):3069–3082. doi: 10.1002/ajmg.a.37940. [DOI] [PubMed] [Google Scholar]
- Guo et al. (2015).Guo H, Tong P, Liu Y, Xia L, Wang T, Tian Q, Li Y, Hu Y, Zheng Y, Jin X, Li Y, Xiong W, Tang B, Feng Y, Li J, Pan Q, Hu Z, Xia K. Mutations of P4HA2 encoding prolyl 4-hydroxylase 2 are associated with nonsyndromic high myopia. Genetics in Medicine. 2015;17(4):300–306. doi: 10.1038/gim.2015.28. [DOI] [PubMed] [Google Scholar]
- Gupta et al. (2015).Gupta P, Saw SM, Cheung CY, Girard MJA, Mari JM, Bhargava M, Tan C, Tan M, Yang A, Tey F, Nah G, Zhao P, Yin Wong T, Cheng C-Y. Choroidal thickness and high myopia: a case–control study of young Chinese men in Singapore. Acta Ophthalmologica. 2015;93(7):e585–e592. doi: 10.1111/aos.12631. [DOI] [PubMed] [Google Scholar]
- Gupta et al. (2017).Gupta P, Thakku SG, Saw SM, Tan M, Lim E, Tan M, Cheung CMG, Wong TY, Cheng CY. Characterization of choroidal morphologic and vascular features in young men with high myopia using spectral-domain optical coherence tomography. American Journal of Ophthalmology. 2017;177:27–33. doi: 10.1016/j.ajo.2017.02.001. [DOI] [PubMed] [Google Scholar]
- Hammond et al. (2001).Hammond CJ, Snieder H, Gilbert CE, Spector TD. Genes and environment in refractive error: the twin eye study. Investigative Ophthalmology & Visual Science. 2001;42(6):1232–1236. [PubMed] [Google Scholar]
- Holden et al. (2016).Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- Huang, Sherman & Lempicki (2009).Huang DW, Sherman BT, Lempicki RA. Bioinformatics enrichment tools: paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Research. 2009;37(1):1–13. doi: 10.1093/nar/gkn923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jian, Boerwinkle & Liu (2014).Jian X, Boerwinkle E, Liu X. In silico prediction of splice-altering single nucleotide variants in the human genome. Nucleic Acids Research. 2014;42(22):13534–13544. doi: 10.1093/nar/gku1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang et al. (2014).Jiang D, Li J, Xiao X, Li S, Jia X, Sun W, Guo X, Zhang Q. Detection of mutations in LRPAP1, CTSH, LEPREL1, ZNF644, SLC39A5, and SCO2 in 298 families with early-onset high myopia by exome sequencing. Investigative Ophthalmology & Visual Science. 2014;56(1):339–345. doi: 10.1167/iovs.14-14850. [DOI] [PubMed] [Google Scholar]
- Jin et al. (2006).Jin ZB, Liu XQ, Hayakawa M, Murakami A, Nao-i N. Mutational analysis of RPGR and RP2 genes in Japanese patients with retinitis pigmentosa: identification of four mutations. Molecular Vision. 2006;12:1167–1174. [PubMed] [Google Scholar]
- Jin et al. (2017).Jin ZB, Wu J, Huang XF, Feng CY, Cai XB, Mao JY, Xiang L, Wu KC, Xiao X, Kloss BA, Li Z, Liu Z, Huang S, Shen M, Cheng FF, Cheng XW, Zheng ZL, Chen X, Zhuang W, Zhang Q, Young TL, Xie T, Lu F, Qu J. Trio-based exome sequencing arrests de novo mutations in early-onset high myopia. Proceedings of the National Academy of Sciences of the United States of America. 2017;114(16):4219–4224. doi: 10.1073/pnas.1615970114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz, Tielsch & Sommer (1997).Katz J, Tielsch JM, Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Investigative Ophthalmology & Visual Science. 1997;38:334–340. [PubMed] [Google Scholar]
- Kempen et al. (2004).Kempen JH, Mitchell P, Lee KE, Tielsch JM, Broman AT, Taylor HR, Ikram MK, Congdon NG, O’Colmain BJ. The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Archives of Ophthalmology. 2004;122(4):495–505. doi: 10.1001/archopht.122.4.495. [DOI] [PubMed] [Google Scholar]
- Klevering et al. (2004).Klevering BJ, Maugeri A, Wagner A, Go SL, Vink C, Cremers FP, Hoyng CB. Three families displaying the combination of Stargardt’s disease with cone–rod dystrophy or retinitis pigmentosa. Ophthalmology. 2004;111(3):546–553. doi: 10.1016/j.ophtha.2003.06.010. [DOI] [PubMed] [Google Scholar]
- Kloss et al. (2017).Kloss BA, Tompson SW, Whisenhunt KN, Quow KL, Huang SJ, Pavelec DM, Rosenberg T, Young TL. Exome sequence analysis of 14 families with high myopia. Investigative Ophthalmology & Visual Science. 2017;58(4):1982–1990. doi: 10.1167/iovs.16-20883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knebelmann et al. (1996).Knebelmann B, Breillat C, Forestier L, Arrondel C, Jacassier D, Giatras I, Drouot L, Deschenes G, Grunfeld JP, Broyer M, Gubler MC, Antignac C. Spectrum of mutations in the COL4A5 collagen gene in X-linked Alport syndrome. American Journal of Human Genetics. 1996;59(6):1221–1232. [PMC free article] [PubMed] [Google Scholar]
- Kubrey, Solanki & Agrawal (2015).Kubrey S, Solanki D, Agrawal S. Schwartz-Jampel Syndrome (SJS) a rare entity: case report. Journal of Evolution of Medical and Dental Sciences. 2015;4(43):7538–7546. doi: 10.14260/jemds/2015/1093. [DOI] [Google Scholar]
- Kuleshov et al. (2016).Kuleshov MV, Jones MR, Rouillard AD, Fernandez NF, Duan Q, Wang Z, Koplev S, Jenkins SL, Jagodnik KM, Lachmann A, McDermott MG, Monteiro CD, Gundersen GW, Ma’ayan A. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Research. 2016;44(W1):W90–W97. doi: 10.1093/nar/gkw377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2014).Lee S, Abecasis GR, Boehnke M, Lin X. Rare-variant association analysis: study designs and statistical tests. American Journal of Human Genetics. 2014;95(1):5–23. doi: 10.1016/j.ajhg.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lek et al. (2016).Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, O’Donnell-Luria AH, Ware JS, Hill AJ, Cummings BB, Tukiainen T, Birnbaum DP, Kosmicki JA, Duncan LE, Estrada K, Zhao F, Zou J, Pierce-Hoffman E, Berghout J, Cooper DN, Deflaux N, DePristo M, Do R, Flannick J, Fromer M, Gauthier L, Goldstein J, Gupta N, Howrigan D, Kiezun A, Kurki MI, Moonshine AL, Natarajan P, Orozco L, Peloso GM, Poplin R, Rivas MA, Ruano-Rubio V, Rose SA, Ruderfer DM, Shakir K, Stenson PD, Stevens C, Thomas BP, Tiao G, Tusie-Luna MT, Weisburd B, Won HH, Yu D, Altshuler DM, Ardissino D, Boehnke M, Danesh J, Donnelly S, Elosua R, Florez JC, Gabriel SB, Getz G, Glatt SJ, Hultman CM, Kathiresan S, Laakso M, McCarroll S, McCarthy MI, McGovern D, McPherson R, Neale BM, Palotie A, Purcell SM, Saleheen D, Scharf JM, Sklar P, Sullivan PF, Tuomilehto J, Tsuang MT, Watkins HC, Wilson JG, Daly MJ, MacArthur DG, Exome Aggregation Consortium Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536(7616):285–291. doi: 10.1038/nature19057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li & Durbin (2009).Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25(14):1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2009).Li YJ, Guggenheim JA, Bulusu A, Metlapally R, Abbott D, Malecaze F, Calvas P, Rosenberg T, Paget S, Creer RC, Kirov G, Owen MJ, Zhao B, White T, Mackey DA, Young TL. An international collaborative family-based whole-genome linkage scan for high-grade myopia. Investigative Ophthalmology & Visual Science. 2009;50(7):3116–3127. doi: 10.1167/iovs.08-2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2017).Li N, Xu Y, Li G, Yu T, Yao RE, Wang X, Wang J. Exome sequencing identifies a de novo mutation of CTNNB1 gene in a patient mainly presented with retinal detachment, lens and vitreous opacities, microcephaly, and developmental delay: case report and literature review. Medicine. 2017;96(20):e6914. doi: 10.1097/md.0000000000006914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin et al. (2016).Lin B, Cai XB, Zheng ZL, Huang XF, Liu XL, Qu J, Jin ZB. Clinical and genetic analyses reveal novel pathogenic ABCA4 mutations in Stargardt disease families. Scientific Reports. 2016;6(1):35414. doi: 10.1038/srep35414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes et al. (2009).Lopes MC, Andrew T, Carbonaro F, Spector TD, Hammond CJ. Estimating heritability and shared environmental effects for refractive error in twin and family studies. Investigative Ophthalmology & Visual Science. 2009;50(1):126–131. doi: 10.1167/iovs.08-2385. [DOI] [PubMed] [Google Scholar]
- McLaren et al. (2016).McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GR, Thormann A, Flicek P, Cunningham F. The ensembl variant effect predictor. Genome Biology. 2016;17(1):122. doi: 10.1186/s13059-016-0974-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metlapally et al. (2016).Metlapally R, Park HN, Chakraborty R, Wang KK, Tan CC, Light JG, Pardue MT, Wildsoet CF. Genome-wide scleral micro- and messenger-RNA regulation during myopia development in the mouse. Investigative Ophthalmology & Visual Science. 2016;57(14):6089–6097. doi: 10.1167/iovs.16-19563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molday, Rabin & Molday (2000).Molday LL, Rabin AR, Molday RS. ABCR expression in foveal cone photoreceptors and its role in Stargardt macular dystrophy. Nature Genetics. 2000;25(3):257–258. doi: 10.1038/77004. [DOI] [PubMed] [Google Scholar]
- Mordechai et al. (2011).Mordechai S, Gradstein L, Pasanen A, Ofir R, El Amour K, Levy J, Belfair N, Lifshitz T, Joshua S, Narkis G, Elbedour K, Myllyharju J, Birk OS. High myopia caused by a mutation in LEPREL1, encoding prolyl 3-hydroxylase 2. American Journal of Human Genetics. 2011;89(3):438–445. doi: 10.1016/j.ajhg.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan, Ohno-Matsui & Saw (2012).Morgan IG, Ohno-Matsui K, Saw S-M. Myopia. Lancet. 2012;379(9827):1739–1748. doi: 10.1016/s0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- Nakanishi et al. (2009).Nakanishi H, Yamada R, Gotoh N, Hayashi H, Yamashiro K, Shimada N, Ohno-Matsui K, Mochizuki M, Saito M, Iida T, Matsuo K, Tajima K, Yoshimura N, Matsuda F. A genome-wide association analysis identified a novel susceptible locus for pathological myopia at 11q24.1. PLOS Genetics. 2009;5(9):e1000660. doi: 10.1371/journal.pgen.1000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nallasamy et al. (2007).Nallasamy S, Paluru PC, Devoto M, Wasserman NF, Zhou J, Young TL. Genetic linkage study of high-grade myopia in a Hutterite population from South Dakota. Molecular Vision. 2007;13(26):229–236. [PMC free article] [PubMed] [Google Scholar]
- Newman (2006).Newman MEJ. Modularity and community structure in networks. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(23):8577–8582. doi: 10.1073/pnas.0601602103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng et al. (2009).Ng SB, Turner EH, Robertson PD, Flygare SD, Bigham AW, Lee C, Shaffer T, Wong M, Bhattacharjee A, Eichler EE, Bamshad M, Nickerson DA, Shendure J. Targeted capture and massively parallel sequencing of 12 human exomes. Nature. 2009;461(7261):272–276. doi: 10.1038/nature08250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panagiotou et al. (2017).Panagiotou ES, Sanjurjo Soriano C, Poulter JA, Lord EC, Dzulova D, Kondo H, Hiyoshi A, Chung BH, Chu YW, Lai CHY, Tafoya ME, Karjosukarso D, Collin RWJ, Topping J, Downey LM, Ali M, Inglehearn CF, Toomes C. Defects in the cell signaling mediator β-catenin cause the retinal vascular condition FEVR. American Journal of Human Genetics. 2017;100(6):960–968. doi: 10.1016/j.ajhg.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmeggiani et al. (2016).Parmeggiani F, Barbaro V, De Nadai K, Lavezzo E, Toppo S, Chizzolini M, Palu G, Parolin C, Di Iorio E. Identification of novel X-linked gain-of-function RPGR-ORF15 mutation in Italian family with retinitis pigmentosa and pathologic myopia. Scientific Reports. 2016;6(1):39179. doi: 10.1038/srep39179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennings et al. (2004).Pennings RJ, Te Brinke H, Weston MD, Claassen A, Orten DJ, Weekamp H, Van Aarem A, Huygen PL, Deutman AF, Hoefsloot LH, Cremers FP, Cremers CW, Kimberling WJ, Kremer H. USH2A mutation analysis in 70 Dutch families with Usher syndrome type II. Human Mutation. 2004;24(2):185. doi: 10.1002/humu.9259. [DOI] [PubMed] [Google Scholar]
- Saw et al. (2005).Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic and Physiological Optics. 2005;25(5):381–391. doi: 10.1111/j.1475-1313.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- Schwartz, Haim & Skarsholm (1990).Schwartz M, Haim M, Skarsholm D. X-linked myopia: Bornholm eye disease. Linkage to DNA markers on the distal part of Xq. Clinical Genetics. 1990;38(4):281–286. doi: 10.1111/j.1399-0004.1990.tb03582.x. [DOI] [PubMed] [Google Scholar]
- Sharon et al. (2003).Sharon D, Sandberg MA, Rabe VW, Stillberger M, Dryja TP, Berson EL. RP2 and RPGR mutations and clinical correlations in patients with X-linked retinitis pigmentosa. American Journal of Human Genetics. 2003;73(5):1131–1146. doi: 10.1086/379379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi et al. (2011).Shi Y, Li Y, Zhang D, Zhang H, Li Y, Lu F, Liu X, He F, Gong B, Cai L, Li R, Liao S, Ma S, Lin H, Cheng J, Zheng H, Shan Y, Chen B, Hu J, Jin X, Zhao P, Chen Y, Zhang Y, Lin Y, Li X, Fan Y, Yang H, Wang J, Yang Z. Exome sequencing identifies ZNF644 mutations in high myopia. PLOS Genetics. 2011;7(6):e1002084. doi: 10.1371/journal.pgen.1002084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shroyer et al. (1999).Shroyer NF, Lewis RA, Allikmets R, Singh N, Dean M, Leppert M, Lupski JR. The rod photoreceptor ATP-binding cassette transporter gene, ABCR, and retinal disease: from monogenic to multifactorial. Vision Research. 1999;39(15):2537–2544. doi: 10.1016/s0042-6989(99)00037-1. [DOI] [PubMed] [Google Scholar]
- Slijkerman et al. (2016).Slijkerman RW, Vache C, Dona M, Garcia-Garcia G, Claustres M, Hetterschijt L, Peters TA, Hartel BP, Pennings RJ, Millan JM, Aller E, Garanto A, Collin RW, Kremer H, Roux AF, Van Wijk E. Antisense oligonucleotide-based splice correction for USH2A-associated retinal degeneration caused by a frequent deep-intronic mutation. Molecular Therapy—Nucleic Acids. 2016;5:e381. doi: 10.1038/mtna.2016.89. [DOI] [PubMed] [Google Scholar]
- Smith, Sivaprasad & Chong (2016).Smith RL, Sivaprasad S, Chong V. Retinal biochemistry, physiology and cell biology. Developments in Ophthalmology. 2016;55:18–27. doi: 10.1159/000431118. [DOI] [PubMed] [Google Scholar]
- Stenson et al. (2017).Stenson PD, Mort M, Ball EV, Evans K, Hayden M, Heywood S, Hussain M, Phillips AD, Cooper DN. The human gene mutation database: towards a comprehensive repository of inherited mutation data for medical research, genetic diagnosis and next-generation sequencing studies. Human Genetics. 2017;136(6):665–677. doi: 10.1007/s00439-017-1779-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudmant et al. (2015).Sudmant PH, Rausch T, Gardner EJ, Handsaker RE, Abyzov A, Huddleston J, Zhang Y, Ye K, Jun G, Fritz MH, Konkel MK, Malhotra A, Stutz AM, Shi X, Casale FP, Chen J, Hormozdiari F, Dayama G, Chen K, Malig M, Chaisson MJP, Walter K, Meiers S, Kashin S, Garrison E, Auton A, Lam HYK, Mu XJ, Alkan C, Antaki D, Bae T, Cerveira E, Chines P, Chong Z, Clarke L, Dal E, Ding L, Emery S, Fan X, Gujral M, Kahveci F, Kidd JM, Kong Y, Lameijer EW, McCarthy S, Flicek P, Gibbs RA, Marth G, Mason CE, Menelaou A, Muzny DM, Nelson BJ, Noor A, Parrish NF, Pendleton M, Quitadamo A, Raeder B, Schadt EE, Romanovitch M, Schlattl A, Sebra R, Shabalin AA, Untergasser A, Walker JA, Wang M, Yu F, Zhang C, Zhang J, Zheng-Bradley X, Zhou W, Zichner T, Sebat J, Batzer MA, McCarroll SA, Mills RE, Gerstein MB, Bashir A, Stegle O, Devine SE, Lee C, Eichler EE, Korbel JO, The 1000 Genomes Project Consortium An integrated map of structural variation in 2,504 human genomes. Nature. 2015;526(7571):75–81. doi: 10.1038/nature15394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun et al. (2015).Sun W, Huang L, Xu Y, Xiao X, Li S, Jia X, Gao B, Wang P, Guo X, Zhang Q. Exome sequencing on 298 probands with early-onset high myopia: approximately one-fourth show potential pathogenic mutations in RetNet genes. Investigative Ophthalmology & Visual Science. 2015;56(13):8365–8372. doi: 10.1167/iovs.15-17555. [DOI] [PubMed] [Google Scholar]
- Teer & Mullikin (2010).Teer JK, Mullikin JC. Exome sequencing: the sweet spot before whole genomes. Human Molecular Genetics. 2010;19(R2):R145–R151. doi: 10.1093/hmg/ddq333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran-Viet et al. (2013).Tran-Viet KN, Powell C, Barathi VA, Klemm T, Maurer-Stroh S, Limviphuvadh V, Soler V, Ho C, Yanovitch T, Schneider G, Li YJ, Nading E, Metlapally R, Saw SM, Goh L, Rozen S, Young TL. Mutations in SCO2 are associated with autosomal-dominant high-grade myopia. American Journal of Human Genetics. 2013;92(5):820–826. doi: 10.1016/j.ajhg.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valverde et al. (2007).Valverde D, Riveiro-Alvarez R, Aguirre-Lamban J, Baiget M, Carballo M, Antinolo G, Millan JM, Garcia Sandoval B, Ayuso C. Spectrum of the ABCA4 gene mutations implicated in severe retinopathies in Spanish patients. Investigative Ophthalmology & Visual Science. 2007;48(3):985–990. doi: 10.1167/iovs.06-0307. [DOI] [PubMed] [Google Scholar]
- Vitale, Sperduto & Ferris (2009).Vitale S, Sperduto RD, Ferris FL., III Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Archives of Ophthalmology. 2009;127(12):1632–1639. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- Warren et al. (2015).Warren CR, Kassir E, Spurlin J, Martinez J, Putnam NH, Farach-Carson MC. Evolution of the perlecan/HSPG2 gene and its activation in regenerating Nematostella vectensis. PLOS ONE. 2015;10(4):e0124578. doi: 10.1371/journal.pone.0124578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojciechowski et al. (2006).Wojciechowski R, Moy C, Ciner E, Ibay G, Reider L, Bailey-Wilson JE, Stambolian D. Genomewide scan in Ashkenazi Jewish families demonstrates evidence of linkage of ocular refraction to a QTL on chromosome 1p36. Human Genetics. 2006;119(4):389–399. doi: 10.1007/s00439-006-0153-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu et al. (2014).Wu G, Dawson E, Duong A, Haw R, Stein L. ReactomeFIViz: a Cytoscape app for pathway and network-based data analysis. F1000Research. 2014;3:146. doi: 10.12688/f1000research.4431.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, Feng & Stein (2010).Wu G, Feng X, Stein L. A human functional protein interaction network and its application to cancer data analysis. Genome Biology. 2010;11(5):R53. doi: 10.1186/gb-2010-11-5-r53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu et al. (2015).Wu LJ, You QS, Duan JL, Luo YX, Liu LJ, Li X, Gao Q, Zhu HP, He Y, Xu L, Jonas JB, Wang W, Guo XH. Prevalence and associated factors of myopia in high-school students in Beijing. PLOS ONE. 2015;10(3):e0120764. doi: 10.1371/journal.pone.0120764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao et al. (2016).Xiao X, Li S, Jia X, Guo X, Zhang Q. X-linked heterozygous mutations in ARR3 cause female-limited early onset high myopia. Molecular Vision. 2016;22:1257–1266. [PMC free article] [PubMed] [Google Scholar]
- Xu et al. (2006).Xu L, Wang Y, Li Y, Wang Y, Cui T, Li J, Jonas JB. Causes of blindness and visual impairment in urban and rural areas in Beijing: the Beijing eye study. Ophthalmology. 2006;113(7):1134.e1–1134.e11. doi: 10.1016/j.ophtha.2006.01.035. [DOI] [PubMed] [Google Scholar]
- Yokoyama et al. (2001).Yokoyama A, Maruiwa F, Hayakawa M, Kanai A, Vervoort R, Wright AF, Yamada K, Niikawa N, Naoi N. Three novel mutations of the RPGR gene exon ORF15 in three Japanese families with X-linked retinitis pigmentosa. American Journal of Medical Genetics. 2001;104(3):232–238. doi: 10.1002/ajmg.10035. [DOI] [PubMed] [Google Scholar]
- Young et al. (1998).Young TL, Ronan SM, Drahozal LA, Wildenberg SC, Alvear AB, Oetting WS, Atwood LD, Wilkin DJ, King RA. Evidence that a locus for familial high myopia maps to chromosome 18p. American Journal of Human Genetics. 1998;63(1):109–119. doi: 10.1086/301907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yzer et al. (2012).Yzer S, Hollander AI, Lopez I, Pott JW, De Faber JT, Cremers FP, Koenekoop RK, Van Den Born LI. Ocular and extra-ocular features of patients with Leber congenital amaurosis and mutations in CEP290. Molecular Vision. 2012;18:412–425. [PMC free article] [PubMed] [Google Scholar]
- Zhang (2015).Zhang Q. Genetics of refraction and myopia. Progress in Molecular Biology and Translational Science. 2015;134:269–279. doi: 10.1016/bs.pmbts.2015.05.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Positions are QTL positions on human genome assembly GRCh37.
Known genes are genes known to be associated with high myopia based on OMIM (https://www.omim.org/) or previous publications. Ocular disease genes are genes associated with eye diseases excluding the known genes, assembled from RetNet database (http://www.sph.uth.tmc.edu/retnet/) or OMIM.
Only GO terms with an BH adjusted FDR <0.05 were included in the table. MF, Molecular Function; BP, Biological Process; CC, Cellular Component.
Chromosome position is based on GRCh37/hg19 assembly. HM stands for high myopia.
Compare to other genes in the genome, HM know genes and ocular disease genes are highly expressed in retina, retinal pigment epithelium (RPE), choroid and sclera. The values shown in the heatmap are log2(RPKM+0.001).
This network can be divided into 4 network modules. Principal biological process of each module was calculated using the eye disease genes as background instead of the genomic background as in Fig. 4. The rest is the same as in Fig. 4.
Data Availability Statement
The following information was supplied regarding data availability:
The raw sequence data reported in this paper are deposited in the Genome Sequence Archive (Genomics, Proteomics & Bioinformatics 2017), Beijing Institute of Genomics (BIG), Chinese Academy of Sciences, under accession numbers CRA000764 and CRA000769, publicly accessible at http://bigd.big.ac.cn/gsa.