Short abstract
Introduction
Maternal health and the performance of health workers is a key concern in low- and middle-income countries. Mobile health technologies are reportedly able to improve workers’ performance. However, how this has been achieved for maternal health workers in low-resource settings is not fully substantiated. To address this gap by building theoretical explanations, two questions were posed: How does mobile health influence the performance of maternal health care workers in low- and middle-income countries? What mechanisms and contextual factors are associated with mobile health use for maternal health service delivery in low- and middle-income countries?
Methods
Guided by established guidelines, a realist review was conducted. Five databases were searched for relevant English language articles published between 2009 and 2016. A three-stage framework was developed and populated with explanatory configurations of Intervention–Context–Actors–Mechanism–Outcome. Articles were analyzed retroductively, with identified factors grouped into meaningful clusters.
Results
Of 1254 records identified, 23 articles representing 16 studies were retained. Four main mechanisms were identified: usability and empowerment explaining mobile health adoption, third-party recognition explaining mobile health utilization, and empowerment of health workers explaining improved competence. Evidence was skewed toward the adoption and utilization stage of the framework, with weak explanations for performance outcomes.
Conclusions
Findings suggest that health workers can be empowered to adopt and utilize mobile health in contexts where it is aligned to their needs, workload, training, and skills. In turn, mobile health can empower health workers with skills and confidence when it is perceived as useful and easy to use, in contexts that foster recognition from clients, peers, or supervisors.
Keywords: Mobile health, maternal health services, health personnel, work performance, developing countries
Introduction
Maternal health remains a major challenge in low- and middle-income countries (LMICs). In 2015, an estimated 303,000 women and young girls died from pregnancy and childbirth-related complications, with 99% of these deaths occurring in LMICs. Access to and availability of skilled health care workers (HCWs) throughout the maternal care continuum (antenatal, delivery, and postnatal), is necessary for reducing preventable mortality and improving quality of maternal health services.1–3 However, LMICs are plagued by chronic workforce shortages, most predominantly in rural and remote areas.4–6
While efforts to increase availability of health workers in low resource settings through training, task shifting, and retention programs have shown promise,7–9 there are concerns that health workers’ performance remains suboptimal.10 This has also been linked to poor access to appropriate training and supervision11,12 and the “know-do” gap, i.e. the inability to apply acquired knowledge and skills. Therefore, while health workers may have been trained to perform assigned tasks, they sometimes underperform for a myriad of reasons including environmental, client, or provider-related.10 This presents a significant challenge for effective decentralization of health services to the primary and secondary levels of care while maintaining quality care.
Information and communication technologies (ICTs) such as mobile health technology are increasingly recommended as a means to bridge the know-do gap and by extension improve health worker performance and quality of maternal health.13,14 Mobile health (mHealth), specifically, is defined as medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices.15 These technologies are currently developing at a rate that outpaces other infrastructural development, expanding the range of mHealth projects targeting health workers as users.16 In Ghana and Thailand, for example, mHealth has been notably reported to improve data collection and surveillance.17,18 In Malawi, mHealth was found to significantly reduce delays in data transmission when compared to a paper-based system.19 Reviews of literature have also documented its use for supporting referral linkages, point-of-care services, health promotion, and behavior change for maternal and child health.20,21 Technology interacts with actors, health systems and the unique intervention contexts. The delivery of mHealth-supported maternal care with the expectation of optimal health workers’ performance is therefore a complex issue.
As the body of literature on mHealth use by health workers has grown, so has the need to better understand what works or not. A recent review by Gagnon et al.22 highlighted factors that could facilitate or limit the utilization of mHealth by HCWs. These included individual- and organizational-level factors. A separate study broadly examined the effect of mHealth on maternal health, including interventions targeted at pregnant women or health workers.23 While reviewers concluded that mHealth interventions could be effective, they highlighted the need for further studies. In assessing how mHealth can improve the professional experiences of health workers in developing countries, authors found that diversity among cadres in levels of education, service experience, and status, affected service delivery.24 Aforementioned reviews have either focused on a large geographical area—using data from both LMIC and high-income countries,24 synthesized evidence from multiple health domains, or included various user groups within LMICs.22 In addition, they tend to concentrate on questions related to effectiveness, i.e. if mHealth leads to expected outcomes.
Despite the existence of theories on technology usage in the workplace,25–27 how exactly mHealth interventions affect performance of maternal HCWs in LMICs is yet to be established. This review therefore aimed to build plausible theoretical explanations underlying how mHealth influences the performance of HCWs, specifically for delivering maternal health services in LMIC. The review questions were as follows: How does mHealth influence the performance of maternal HCWs in LMIC? What mechanisms and contextual factors are associated with the outcomes of mHealth use in maternal health service delivery in LMIC?
Methods
Study design
To address the knowledge gap of how mHealth interventions influence performance of maternal HCWs in LMICs, a methodological approach to evidence synthesis that embraces complexity is needed. Guided by the principles of scientific realism, realist review has been proposed as a method for opening the “black box” of complex interventions.28–31 Using theoretical reasoning, it aims to explain the conditions under which complex interventions lead to outcomes and the reasoning behind these associations. This approach has been applied in a wide range of studies including those related to health and policy.32–35 We therefore considered realist methodology a useful approach to synthesize studies on how mHealth interacts with social and health systems to achieve program outcomes.
The five-stage method for conducting realist reviews30 was adopted to guide the review process. This was supported by the evolving publication standards on Realist and Meta-narrative Evidence Syntheses.29
Search strategy and process
First, we defined the main concepts of the review: mHealth, health workers, LMICs, and performance. Next, a systematic search strategy was developed using the keywords: mHealth, HCWs, LMICs. An additional file shows these in detail (see supplementary file 1).
In September 2016 the syntax was run across five electronic databases of peer-reviewed literature—PubMed, Web of Science Core Collection, CINAHL, International Bibliography of the Social Sciences (IBSS), and Cochrane Library. We aimed to identify studies in English language published from 1999 onward because this was when the term eHealth, a broader term that encompasses mHealth, was introduced into common usage.36 All references were managed using EndNote©.
After deduplication and discussions to establish selection criteria, two authors (IOA, OI) screened the title and abstract (TIAB) of each record for relevance. A third author (MD) made TIAB decisions on a random number (20%) of records and full text reading was carried out by at least two authors, with a third reading every fifth paper. During full text reading, we preliminarily scoped the literature guided by our knowledge on the subject matter with the intention of developing a framework to guide the review. By “snowballing” the reference sections of preselected studies, we also expanded the search to identify additional relevant articles. Only primary studies, including theoretical papers were retained for extraction. See supplementary file 1 for exclusion criteria.
Unlike systematic reviews, realist reviews do not typically appraise the risk of bias, but instead focus on the relevance of papers, the methodological credibility of the data, and the conclusions authors draw from them.37 Discussions during our review process therefore included indicative assessments of the validity of conclusions reflected in each paper. Papers deemed relevant for answering all or part of the review questions were included, irrespective of study design or format of evidence. Bias was minimized by the multidisciplinary (health policy and systems research, behavioral sciences, global public health, medicine, social science) nature of the five-person review team.
Data extraction
Theoretical findings from a realist review are typically presented in series of statements with a Context (C), Mechanism (M), and Outcome (O) configuration, i.e. C–M–O. To answer review questions along the lines of: What works, for whom, in what contexts, to what extents, how and why? we took an extended approach using an I–C–A–M–O configuration, i.e. Intervention–Context–Actors–Mechanism–Outcome.38,39 Definitions of these concepts are presented in Table 1. In so doing, we distinguish between the features and characteristics of the mHealth Intervention (I), the HCW or actors (A) who use it, the unique layers of context identified from our exploratory reading of articles- environmental context (C1) and organizational/health system context (C2), and the outcomes of interest (O). We differentiated contextual levels because of the complex dynamic nature of health systems. Additionally, due to common features of health systems in LMICs, we expected to find more similarities at C2 level than at C1 across intervention countries.
Table 1.
Definitions of realist concepts.
| Concept | Definition/description |
|---|---|
| Intervention (I) | Refers to the features and characteristics of the various mHealth interventions such as type of technology, cointerventions, and mode of delivery. |
| Context (C) | Refers to “… features of the conditions in which programmes are introduced, that are relevant to the operation [of] the programme mechanisms”40 p. 7, and answers the question: in what circumstances will a program work?We differentiate two layers of context:ii) Environmental (C1): the broad external environment in which interventions are situated, following a PESTELI typology, i.e. political, economic, social, technological, environmental, legal, and infrastructural.iii) Organizational/Health System (C2): resources, policies, and structures directly related to the unique health facility settings in which mobile technology is introduced. |
| Actors (A): | This describes the individual users of mHealth—in this case, health workers of varying cadres and levels of experience and skills, who are expected to use mHealth for maternal health service delivery. |
| Mechanism (M) | Mechanisms are behavioral, cognitive, affective, and social responses to mHealth which can explain the (un)intended outcomes of its use.41They refer to the ways in which the resources offered through mHealth in a given context may permeate into the reasoning of the actors, leading to various outcomes.40,42 |
| Outcome (O) | Outcomes include changes due to mHealth interventions and their intended or unintended consequences.Although the review started off with a focus on health worker performance as an outcome of mHealth use, further on we explain the rationale behind expanding the scope of the review to explore more proximal outcomes. |
mHealth: Mobile health.
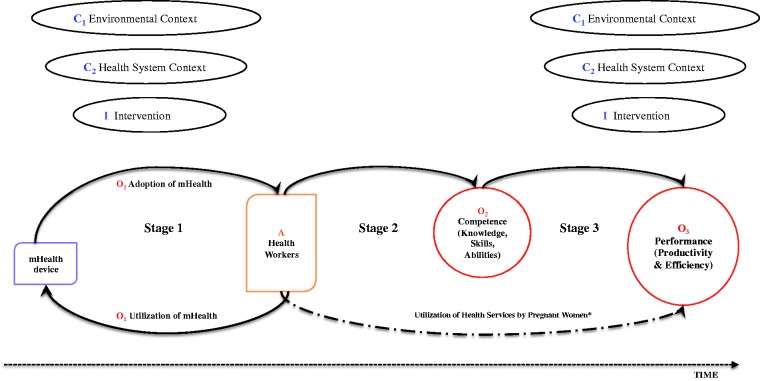
The initial round of full reading of preselected articles motivated review refinement. We only found few papers that focused explicitly on health workers’ performance as an outcome of mHealth use in maternal care. In light of this, the review team retained the initial focus of the review on performance as an outcome of interest but decided to map the pathway of effect by considering more proximal outcomes. Consequently, we developed a framework that could potentially explain how and at what stages mHealth interacts with actors, progressing to improved health worker performance. The framework mapped three stages in mHealth use, each related to an outcome (O): (i) Stage 1 (O1)—adoption and utilization of mHealth by health workers, where utilization is a feedback process that reflects continuous use over time; (ii) Stage 2 (O2)—effect of mHealth on the knowledge, skills, and attitudes (i.e. competence) of health workers; and (iii) Stage 3 (O3)—change in performance of health workers. The initial framework depicted in Figure 1 was modified as the review progressed.
Figure 1.
Initial framework. mHealth: mobile health. Contextual factors are labelled C1 and C2. Outcomes are labelled O1, O2, and O3 for adoption/utilization, competence and performance outcomes respectively. Actor or user characteristics are labelled ‘A’. The label ‘Time’ denotes progression from mHealth adoption towards other outcomes. Note that this is a preliminary version of the framework. *Utilization of health services by pregnant women recognises the demand-side influence of mHealth use on health worker performance.
Data extraction was conducted using multiple tools: (i) an Excel data extraction template which included general study information, type and characteristics of intervention, duration, expected and reported outcomes, intervention process, and theoretical models applied; (ii) verbatim extractions of text relevant to understanding the embedded nature of theoretical configurations. Color coding of text extractions guided our understanding of how separate parts make up a whole configuration as shown in Box 1; (iii) Identified indicators of I–C–A–M–O were “populated” into the framework alongside a numerical code assigned to each article, to facilitate backtracking of sources.
The data extraction process was piloted using a couple of papers. For quality assurance, two authors carried out double-data extraction, meeting together after independently extracting three articles. The review team held discussion meetings after data from batches of five papers were extracted.
Identifying ICAMO configurations: Thinking in categories and levels
Articles were read using a retroductive approach, that is shuttling between empirical data and theory using inductive and deductive reasoning to explain observed outcomes.43 We identified the levels at which authors were describing the intervention and its outcomes and worked backward to the process and inputs in an attempt to identify underlying mechanisms. Where multiple papers described a single study, we triangulated the data, filling information gaps across papers.
In order to manage data heterogeneity and the task of “thinking through” the data, we initially populated the framework with “raw” data, using the information as given in the articles. Supplementary file 2 shows the framework in progress. During discussions, we identified patterns and similar clusters such that information became grouped and categorized as higher level constructs, i.e. going from the more detailed to the abstract. Given that the papers we identified were not written with a theory-based or realist perspective in mind, we often had to reconceptualize information presented by authors using a realist interpretive lens. In our process log, we took care to differentiate mechanisms and other factors directly identified in the papers from our interpretations. Where identified, less favorable factors and outcomes were denoted with a negative (−) sign. This effectively meant the framework was iteratively modified throughout the process, with subsequent stages leading to higher levels of abstraction and clarity.
Results
Overview and characteristics of selections
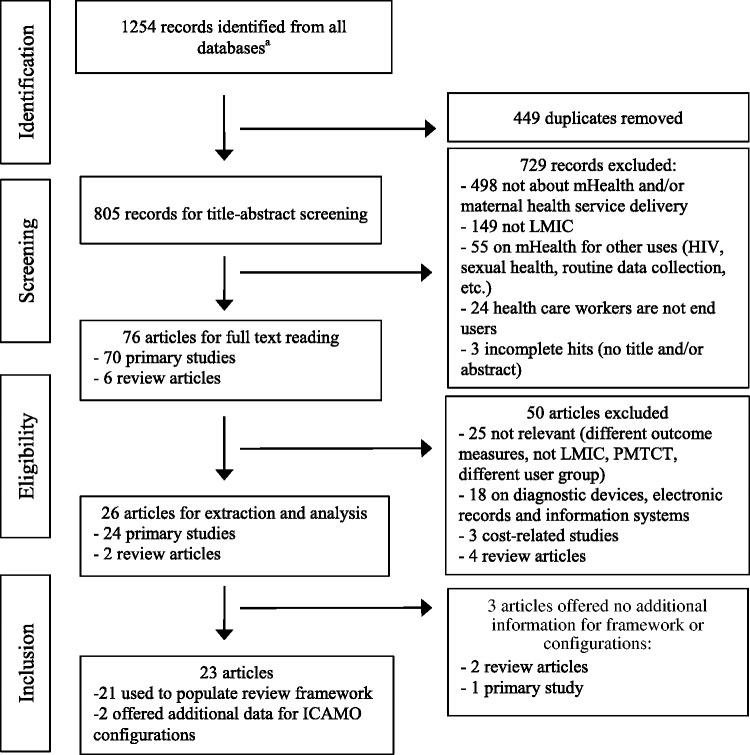
A total of 1254 records were identified from the five databases, and 23 articles published between the years 2008 and 2016 were deemed relevant. Figure 2 outlines the stepwise selection of articles.
Figure 2.
Identification, selection, and inclusion of studies. aPubMed—524; Web of Science—443; CINAHL—151; Cochrane Database—98; IBSS—38. ICAMO: Intervention–Context–Actors–Mechanism–Outcome; LMIC: low- and middle-income countries; mHealth: mobile health; PMTCT: Prevention of mother-to-child transmission of HIV.
Of the 23 primary papers retained, 12 represented independent studies and 11 were related to four different studies: five papers for the multicountry QUALMAT project,44–48 and two papers each related to the Aceh Besar midwives mobile phone project in Indonesia,49,50 use of mHealth forms in Ethiopia,51,52 and the mClinic study in Ghana.53,54 For convenience, we subsequently refer to these as groups of papers (i.e. n = 16) referencing the individual articles only where necessary.
Studies covered 13 LMICs: one each in Uganda, Burkina Faso, Rwanda, Tanzania, Indonesia, Sri Lanka, Liberia, Ethiopia and Papua New Guinea; South Africa, Ghana, and Nigeria had two studies each; three of the 16 studies were focused on India. A multicountry study tagged “QUALMAT” covered three countries—Ghana, Tanzania, and Burkina Faso. Included studies were broadly heterogeneous with respect to their sample size, type of mHealth intervention, as well as in their design and expected outcomes. The framework was populated using data from only 21 of the 23 articles retained, with the remaining two papers providing supplementary project information for further understanding the configurations identified. Empirical papers reported interventions delivered mostly through mobile phones (n = 10) and less frequently laptops (n = 1), tablets or PDAs (n = 3).
mHealth functionality ranged from its use for short messaging service (SMS)50,55,56 or voice calls57 to clinical decision support systems44–48 and health information systems.52,54,58 Common to all studies, however, was their use in rural or remote geographical areas with only two studies including semiurban locations.44–48,59 The cadres of health worker represented were mainly midwives and community health (extension) workers. In addition, a few studies included other cadres such as nurses, nurse assistants, and auxiliary staff.
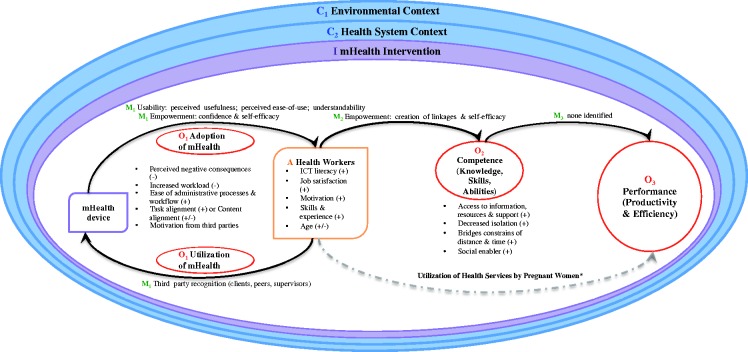
Presentation of findings
Results are pictorially presented in the final framework (see Figure 3). Findings focus on mechanisms related to adoption and utilization of mHealth and its influence on the competence of maternal health workers in LMIC. Although there was no evidence to sufficiently inform ICAMO configurations on maternal health workers’ performance, it is retained in the framework because this gap is an important finding.
Figure 3.
Final framework. The final framework depicts a progressive dynamic process of how mHealth influences performance within a complex context (concentric circles C1 and C2). The implemented technology (I) inevitably introduces an additional layer of context by providing infrastructural support, training, technical components, and tools. O1, O2, and O3 are the outcomes of adoption/utilization, competence, and performance, respectively. Utilization is the continued use of the adopted mHealth device by health workers (A). M1, M2, or M3 are explanatory mechanisms related to outcomes O1, O2, and O3, respectively. The bullet points highlight some factors that facilitate (+) or inhibit (−) outcomes at various stages. The framework evolved through the review process: compare initial framework (Figure 1), framework in progress (supplementary file 2) and final framework (Figure 3).
ICT: Information and communication technology; mHealth: mobile health.
*Utilization of health services by pregnant women was not explored in this review. However, the framework recognizes the demand-side component of maternal health services which might explain how mHealth influences health worker performance.
ICAMO configurations are presented in narrative format in the following subsections. Contextual factors are denoted “C1” and “C2” for environmental and health system context, respectively. Outcomes are denoted “O1” or “O2,” representing adoption/utilization and competence, respectively. Mechanisms are identified “M1” or “M2” following the outcomes they are linked to, with related explanatory mechanisms depicted “m1”or “m2,” respectively. Actor or user characteristics are denoted “A.”
Adoption of mHealth by HCWs
mHealth adoption is a complex social process that is modified by cognitive, emotional, and contextual factors, and in which individuals decide to accept or reject a given innovation.60 The introduction of innovative technology in health facilities triggers immediate positive responses due to the novelty effect from a sense of newness and innovation. This is reflected in welcoming attitudes,44,61 general enthusiasm, and willingness to adopt.44,45 We identified two major mechanisms—usability and empowerment—by which adoption of mHealth by maternal health workers in LMICs occur.
Usability
Usability can be defined as the extent to which an mHealth application could be used to achieve specific goals with effectiveness, efficiency, and satisfaction, in a specified context by specific types of users.62 If maternal health workers in LMICs perceive mHealth to be useful for their work, easy to use, and/or easy to understand, they adopt it (O1) as a first step toward improving service delivery tasks due to its high usability (M1). This is in the context of necessary infrastructural and technical resources (C1) and adequate training and support (I) during implementation. Adoption response is modified by individual-level characteristics such as technological literacy (A), skills and experience (A), as well as the age (A) and level of education (A) of the user. In health facilities with staff shortages (C2), high workload (C2), and inadequate peer support (C2), adoption mechanisms are suppressed, overriding the perceived usefulness (m1) and ease of use (m1) of mHealth which is dependent on the extent to which the innovation is aligned (I) to the service delivery and skills needs of users. In contexts of codependence (C2) and openness for peer learning, challenges with ease of use in (older) users (A) and those with low technological literacy (A) were minimized by peer support (C2). mHealth interface and communication fit (with respect to system design and use of local languages) (I) fosters ease of use and understandability (m1) in health workers with little formal training and low technological skills (A).
Analysis revealed three explanatory components linked to usability as a mechanism for mHealth adoption by health workers. These include perceived usefulness, perceived ease of use, and understandability of device:
Perceived usefulness: if the functions of an intervention are aligned to the maternal health services (e.g. antenatal care, postnatal care) it is intended for, and there are infrastructural resources (e.g. internet availability, electricity) to support its use, its perceived usefulness leads to adoption by maternal health workers. In one study, the decision support intervention was more aligned to the needs of midwives, while community health extension workers preferred easy-to-use data entry applications.63 Conditions such as increased workload, workflow misalignment, and longer client waiting times overshadow the perceived usefulness of mHealth and deter its adoption.
Perceived ease of use: relates to how easy or effortless users anticipate a mHealth device to be. Our analysis showed that health workers perception of ease of use was positive44,61 or negative,55,64 depending on users’ level of technological “savviness.” Evidence indicated that there is no agreement on the relationship between perceived ease of use and the age or level of experience of the health worker. In interventions involving data entry or record keeping where simultaneous use of pilot mHealth and standard paper systems was unavoidable, health workers had negative perceptions of mHealth due to concerns about increased workload, workflow interruptions, and prolonged client waiting times (QUALMAT).57,59,65 Contrarily, when users already perceive a mHealth intervention as a beneficial means to hasten or lighten administrative processes,54 it is welcome and adopted.
In addition to perceived complexity and workload burden,45,47 the usability of mHealth by maternal health workers appeared to be modified by prior exposure to ICTs or newly acquired technological literacy due to intervention exposure and training.55,63 Users reported interventions to be complicated and inconveniencing based on mHealth type, i.e. technical presentation of the software (interface, touch screen functions, size of key pad, portability, etc.) and the availability of training and technical supervision prior to and during the intervention.44,45,47 Contextual factors included technical and infrastructural resources such as electricity, cell phone penetration, and signal coverage. Cointerventions or supportive strategies to remove or minimize structural and systemic barriers to adoption included provision of electricity support in the form of solar or monthly mobile credit.50,51,65,66
c. Understandability: the extent to which a user understands the content, message, or information provided by mHealth level influences its usability and by extension its adoption. The appropriateness of content varies between health workers and is a function of the alignment between the level and style of information offered, and their cognitive or technical capabilities. Short and easy-to-read SMS were easily adopted by workers with less formal education or those with concerns that mHealth was too complex. This was because text messages required little time and effort, reduced risk of workload increase, and are perceived as not “too hard.”67 However, some higher cadre and more experienced health workers felt the information offered through the SMS information system was too simple and below their information support needs.67 Availability of mHealth content in local languages can facilitate mHealth adoption.47,51,55,65,68 Where interventions offer sufficient training on technology use and the software includes local language support, workers with lower level of training and lower ICT skills can still find mHealth content understandable and easy to adopt, especially when the process is fostered by close-knit and codependent peer relationships at an organizational (i.e. health facility) level.
Empowerment
Empowerment and its consequential effect on adoption is summarily related to users’ perceptions of mHealth, individual-level characteristics, implementation strategies, and supportive organizational structures. Analysis showed that mHealth triggers empowerment as a process—when technical literacy skills are acquired through training and support, as well as an outcome—reflected in the ability of health workers to leverage resources provided by the innovation for service delivery.
When mHealth is introduced in health facilities with a supportive organizational culture (C2) characterized by adequate supervision,65 clinical support,59 and peer cooperation,44,49 and the intervention is accompanied with sufficient training (I) on how to use the innovation, alongside regular technical support (I) during the implementation process; HCWs who are computer literate (A) or (become) sufficiently skilled in using the specific device (A) demonstrate innovation adoption (O1) because they feel empowered (M1). Empowerment is the result of increased computer literacy skills (m1) (e.g. QUALMAT study), increased confidence (m1) in their problem-solving capabilities, professional credibility (m1) as service providers,44,49,57 or enhanced self-efficacy (m1) in performing service delivery tasks supported by mHealth.55,61 This response is modified by individual-level characteristics such as technological literacy (A), motivation (A), and job satisfaction (A).
Utilization of mHealth by HCWs
We differentiated adoption (initial use) from utilization (continued or prolonged use over time), based on the expectation that the short-term novelty effect associated with initial use of technology wears off over time.69 Identification of utilization as a feedback loop following adoption was based on references to “prolonged use,” “continued use,” “frequently used,” or “utilized.” Where explicitly identified, positive reports of utilization were recorded in three studies44,49,61 with some reports of resistance and underuse in one of these.44
In contexts with the necessary infrastructural and technical resources (C1) to support optimal functioning of a specific innovative device, enhanced by enabling features and characteristics of the intervention (I) such as (i) training, monitoring, and supervision; (ii) alignment to task and needs; and (iii) collaborative engagement, mHealth is utilized (O1). Utilization is promoted when health worker users feel recognized (M1) by third-party actors (peers, supervisors, and clients). For example, in health facilities where mHealth users lacked the organizational support (C2) for technology use from peers or supervisors such as facility managers, they became demotivated (m1), resulting in mHealth underutilization.44,57 Despite this, HCWs with low job satisfaction (A), who feel unappreciated (A), were motivated to continue using mHealth devices if patients (or peers) supported its use, leading to feelings of improved social (or professional) status (m1).57 The level of support or discouragement received from third-party actors, respectively, triggered or suppressed recognition as a form of motivation (m1) in HCWs.
ICAMO configurations showed that while mHealth adoption is mostly related to individual-level factors, health workers utilized mHealth in response to the behavior and reactions of other important actors in the care process, specifically other health workers (peers or higher cadre professionals), administrative supervisors, and clients (pregnant women). At the intervention level, health workers felt supported to utilize mHealth in routine practice when implementation strategies included refresher training and continued technical support44–48 or regular feedback meetings.57
Effect of mHealth on HCWs’ competence
Competence (operationalized as skills, knowledge, and abilities) in health service delivery refers to the possession of a sufficient level of skills and knowledge for executing tasks in line with evidence-based standards of care. Evidence on this outcome was derived from studies which measured or discussed improved knowledge,49,50,57,61,67 skills,54,55 and overall competence.
mHealth increases health workers’ access to task-related support and information directly (e.g. SMS or electronic clinical decision support system) or indirectly (e.g. calling a supervisor or peer). Through the creation of linkages (m2), adoption and utilization of mHealth improves the competence (O2) of maternal health workers by empowering (M2) them to take appropriate action when they do not know what to do or how to do it. This is especially in workers with gaps in knowledge and skills (A), as well as in workers experiencing professional isolation (C2) or geographic isolation (C1). This leads to increased knowledge,54,61,67 self-confidence,49 and ability,44–48,55 while decreasing feelings of isolation.54
Interventions that allow direct linkage to information and resources (I) are especially useful in understaffed health facilities (C2), while third-party interventions (I) require availability and access to trusted skilled informants who possess the required information49,59,65 or are perceived as approachable. Therefore, while the former model creates user dependency on mHealth, the latter requires supportive organizational contexts (C2) that encourage codependence and shared learning.49,50
However, competence cannot lead to improved performance without resources (e.g. drugs, ambulance, consumables) to act on the information acquired (i.e. shift from ability to capability). Although some projects provided ICT infrastructure (I) to fill gaps in the broader context (C1), lack of resources (C2) limits health workers’ actionability.
Discussion
Overview
This realist review was conducted to identify theoretical explanations connecting mHealth with the performance of maternal HCWs in LMICs. Three main preperformance outcomes (mHealth adoption, utilization, and competence) were identified (Figure 3). Overall, the evidence was concentrated within the adoption and utilization stage with limited evidence for the competence stage.
We identified four main mechanisms connecting the use of mHealth to maternal health service delivery under various contextual conditions. These include usability and empowerment related to mHealth adoption, recognition by a third party for mHealth utilization, and the empowerment of health workers with competence through the creation of linkages.
Reflecting on existing theories
Since identified ICAMO configurations are plausible theories, we reflect on the review findings against some frameworks or theories from the fields of technology and the behavioral sciences.
mHealth adoption and the FITT framework
We identified four groups of factors crucial to the successful adoption and utilization of mHealth—general environment, health system organization, intervention, and individual. These categories are partly captured in the Fit between Individuals, Task and Technology (FITT) framework which links adoption behavior to an alignment or fit.25 Our review findings expand on this theory by providing additional information on explanatory mechanisms (i.e. the “how”) linking individual, technology and organizational factors to performance expectations. Additionally while the FITT highlights the influence of motivation in mHealth adoption and given established knowledge on the role of motivation in job performance,33,70 only few of the studies we reviewed referred to motivation as an influencer of either mHealth adoption, utilization, competence, or performance.51,52,57,58,61 Although motivation was a key factor in the candidate theory of the QUALMAT project44 for example, changes in motivation over time were not measured. It should also be emphasized that for mHealth adoption to eventually translate to improved performance, essential health system resources (e.g. medical consumables; effective referral structures) are necessary.71 Interventions failing to take both motivational and health system factors into account may fall short of expectations.
mHealth utilization and the technology acceptance model (TAM)
Another theory, from the field of information systems—the TAM, applies the theory of reasoned action to explain information technology adoption or rejection by users.26 Our findings showed that mHealth utilization by health workers appears interlinked with motivation acquired through recognition by third-party actors (patients, supervisors, or peers). The third-party effect has been tested under a modified version of the TAM.72 According to Venkatesh and Davis,72 this effect is valid only in contexts of mandatory use of technology. This may explain our findings on the role supervision plays in adoption behavior, i.e. the absence of supervisory support for mHealth led to underutilization because workers were not monitored by their superiors. Because LMIC settings often have top-down administrative structures,73 adoption could be better achieved by increasing extrinsic motivation through supervisory support and oversight. Patient or peer recognition, on the other hand, is likely effective because it triggers intrinsic motivation in mHealth users. Intrinsic motivation has been shown to be a significant predictor of performance and compared to extrinsic rewards, it is a better predictor of performance quality.74
Maternal health workers’ competence and the self-efficacy theory
Findings by Jimoh et al.63 of lower mHealth knowledge among workers despite higher perceived ease of use and usefulness of mHealth indicate that mHealth adoption does not automatically progress to improved competence. Bandura’s self-efficacy theory75—the belief in one’s ability to succeed in a task—offers insight on how the adoption/utilization and competence stages of our framework may be connected. It considers constructs such as motivation, human agency, prior experience, and supportive contexts that influence the mechanisms identified in this realist analysis. By enabling higher health worker confidence and improving knowledge, mHealth can lead to increased self-efficacy for both ICT-related and maternal health tasks, which is manifested in improved skills.55 Self-efficacy may also explain how mHealth empowers health workers and leads to improved competence through changes in knowledge and abilities.49
Maternal health workers’ performance and the technology-to-performance (TPC) chain
As mentioned, we found insufficient links between mHealths’ effect on competence and improved maternal health worker performance (Figure 3). However, building upon studies related to technology utilization and fit, the TPC chain posits that utilization of mHealth and its alignment to the tasks it supports predicts changes in performance and expected improvements in service delivery.76 Studies involving empirical testing of the TPC have shown that the combination of task and technology characteristics and technology utilization strongly establishes the connection between technology and performance.76,77 The context of use, that is mandatory versus voluntary, is said to influence the extent to which constructs of the model play a role77 such that in mandatory settings, user characteristics such as individual perceptions and beliefs about mHealth would otherwise not play a significant role in predicting usage behavior and subsequent changes in performance. Validating and testing the TPC specifically related to mHealth use in LMIC health service providers may aid addressing evidence gaps that our review and its correspondent framework could not.
Strengths and limitations
Realist approach offers the opportunity to synthesize heterogonous data in gaining useful insights on a complex question. A strength of this methodology is that it facilitated “teasing” out the reasoning behind mHealth interventions and factors that explain current knowledge in this domain.
Despite support for the inclusion of gray literature78 we focused the review by excluding them and may have missed other relevant studies. The wide range of interventions in the studies we assessed also limited the possibility to differentiate configurations based on intervention features (e.g. clinical decision support systems, text messaging, etc.). It was also impossible to disentangle the effects of cointerventions such as financial incentives or home visits, or to analyze at a subgroup level (e.g. health worker cadre, location).
Because our review was intended for theory building and informed only by evidence from the 16 interventions reviewed, the final review framework is only a foundation and is not conclusive for the topic domain. Refinement of identified plausible theories by empirical testing or established theoretical explanations and middle range theories from other fields are therefore necessary. Nonetheless, in reflecting on our findings we have highlighted some theories and frameworks that could serve as a starting point.
Recommendations for policy, research, and practice
This review corroborates evidence that an mHealth intervention is only as effective as the system it is imbedded within.59,79,80 Program success is very contextual and the lack of health system resources to support the actionability of acquired skills and knowledge predisposes well-intentioned interventions to failure. In an era of building resilient and adaptive systems, it does not augur well for the future of health systems in developing countries if mHealth is pushed as a magic agenda even in ill-suited contexts. Practitioners and funders should therefore reflect a priori on the critical contextual factors (C1 and C2) that influence the survival of mHealth interventions beyond the pilot phase.
Even though social programs are inevitably rooted in behavioral theories,28 most studies identified in this review did not explicate or reflect on their underlying theoretical assumptions. Policy makers rely on evidence presented by implementers, but disjointed or weak reporting could lead to scenarios where mHealth policies are not aligned to health workers’ needs, leading to adoption resistance.63 In order to strengthen the evidence base, reports on interventions should include explanatory linkages (i.e. how, for whom, and in what contexts) about what works or does not work.
The framework presented can be used to guide the lens through which future studies are designed, implemented, and reported. For example, understanding that the support of peers and supervisors is associated with mHealth utilization helps inform selection criteria for intervention sites with viable contexts. A large gap in the mechanisms that explain the final stage of the continuum (i.e. performance) indicates where additional empirical studies are needed.
Conclusion
A realist design proved valuable for establishing the depth of evidence regarding mHealth use for maternal health in LMIC. The review showed that the literature is skewed toward the adoption and utilization of mHealth by health workers, and there is limited evidence on how exactly mHealth influences their competence and performance. Findings suggest that health workers can be empowered to adopt and utilize mHealth in contexts where it is aligned to their needs, workload, training, and skills. In turn, mHealth can empower health workers with skills and confidence when it is perceived as useful and easy to use, in contexts that foster recognition from clients, peers, or supervisors.
Supplemental Material
Supplemental material 1 for Mobile health and the performance of maternal health care workers in low- and middle-income countries: A realist review by Ibukun-Oluwa Omolade Abejirinde, Onaedo Ilozumba, Bruno Marchal, Marjolein Zweekhorst and Marjolein Dieleman in International Journal of Care Coordination
Supplemental Material
Supplemental material 2 for Mobile health and the performance of maternal health care workers in low- and middle-income countries: A realist review by Ibukun-Oluwa Omolade Abejirinde, Onaedo Ilozumba, Bruno Marchal, Marjolein Zweekhorst and Marjolein Dieleman in International Journal of Care Coordination
Acknowledgements
The authors would like to thank Ralph de Vries, Vrije Universiteit Library, for his assistance in refining the search strategy and modifying it across databases. We would also like to thank Elsbet Lodenstein for contributing her expertise on realist reviews. Finally, the authors appreciate the constructive feedback from reviewers, which helped improve the manuscript.
Authors’ contributions
The review was designed and performed by IOA and OI with support from MZ, MD, and BM. IOA played a lead role in all stages of the review and in drafting the manuscript, seconded by OI, with other authors contributing to its revision. All authors have read and approved the final manuscript.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Erasmus Mundus Joint Doctorate Fellowship Specific Grant Agreement 2015-1595, which IOA is a beneficiary of. The funding agency had no role in study design, analysis, or preparation of the manuscript.
Supplementary materials
Additional supplementary information on the review process, formulation of ICAMO configurations, and population of the review framework are available on request.
References
- 1.Aahman E, Abou ZC, Amoako JF.et al. Make every mother and child count Geneva: WHO Press. http://www.who.int/whr/2005/whr2005_en.pdf (2005, accessed 2 April 2017).
- 2.Friberg IK, Kinney MV, Lawn JE, et al. Sub-Saharan Africa’s mothers, newborns, and children: how many lives could be saved with targeted health interventions? PLoS Med .Epub ahead of print2010.DOI: 10.1371/journal.pmed.1000295. 7(6): e1000295. [DOI] [PMC free article] [PubMed]
- 3.Lassi ZS, Musavi NB, Maliqi B, et al. Systematic review on human resources for health interventions to improve maternal health outcomes: evidence from low- and middle-income countries. Hum Resour Health 2016; 14: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leach MJ. Using role substitution to address the health workforce shortage and to facilitate integration? J Complement Integr Med 2012; 9: Article 30. [DOI] [PubMed] [Google Scholar]
- 5.Alcalde-Rabanal JE, Nigenda G, Bärnighausen T, et al. The gap in human resources to deliver the guaranteed package of prevention and health promotion services at urban and rural primary care facilities in Mexico. Hum Resour Health 2017; 15: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aluttis C, Bishaw T, Frank MW. The workforce for health in a globalized context – global shortages and international migration. Global Health Action 2014; 7: 23611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organisation. World health report: working together for health Geneva: WHO Press 2006.
- 8.Seidman G, Atun R. Does task shifting yield cost savings and improve efficiency for health systems? A systematic review of evidence from low-income and middle-income countries. Hum Resour Health 2017; 15: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okyere E, Mwanri L, Ward P. Is task-shifting a solution to the health workers’ shortage in Northern Ghana? PLoS One 2017; 12(3): e0174631. [DOI] [PMC free article] [PubMed]
- 10.Rowe AK, De Savigny D, Lanata CF, et al. How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet 2005; 366: 1026–1035. [DOI] [PubMed] [Google Scholar]
- 11.Narasimhan V, Brown H, Pablos-Mendez A, et al. Responding to the global human resources crisis. Lancet 2004; 363: 1469–1472. [DOI] [PubMed] [Google Scholar]
- 12.ten Hoope-Bender P, Liljestrand J, MacDonagh S. Human resources and access to maternal health care. Int J Gynaecol Obstet 2006; 94: 226–233. [DOI] [PubMed] [Google Scholar]
- 13.Bollinger R, Chang L, Jafari R, et al. Leveraging information technology to bridge the health workforce gap. Bull World Health Organ 2013; 91: 890–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Braun R, Catalani C, Wimbush J, et al. Community health workers and mobile technology: a systematic review of the literature. PLoS One 2013; 8: e65772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO. mHealth: new horizons for health through mobile technologies: 2nd Global Survey on eHealth Geneva: WHO Press, 2011.
- 16.Sanou B. ICT facts & figures: The world in 2015. Geneva: ICT Data and Statistics Division, Telecommunication Development Bureau, International Telecommunication Union. https://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2015.pdf (2015, accessed 26 March 2017).
- 17.Andreatta P, Debpuur D, Danquah A, et al. Using cell phones to collect postpartum hemorrhage outcome data in rural Ghana. Int J Gynecol Obstet 2011; 113: 148–151. [DOI] [PubMed] [Google Scholar]
- 18.Kaewkungwal J, Singhasivanon P, Khamsiriwatchara A, et al. Application of smart phone in ‘Better Border Healthcare Program’: a module for mother and child care. BMC Med Inform Decis Mak 2010; 10: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joos O, Silva R, Amouzou A, et al. Evaluation of a mhealth data quality intervention to improve documentation of pregnancy outcomes by health surveillance assistants in Malawi: a cluster randomized trial. PLoS One 2016; 11: e0145238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tamrat T, Kachnowski S. Special delivery: an analysis of mHealth in maternal and newborn health programs and their outcomes around the world. Matern Child Health J 2012; 16: 1092–1101. [DOI] [PubMed] [Google Scholar]
- 21.Lee SH, Nurmatov UB, Nwaru BI, et al. Effectiveness of mHealth interventions for maternal, newborn and child health in low- and middle-income countries: systematic review and meta-analysis. J Glob Health 2016; 6: 10401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gagnon MP, Ngangue P, Payne-Gagnon J, et al. M-Health adoption by healthcare professionals: a systematic review. J Am Med Inform Assoc 2016; 23: 212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sondaal SFV, Browne JL, Amoakoh-Coleman M, et al. Assessing the effect of mHealth interventions in improving maternal and neonatal care in low- and middle-income countries: a systematic review. PLoS One 2016; 11: e0154664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White A, Thomas DSK, Ezeanochie N, et al. Health worker mHealth utilization. Comput Inform Nurs 2016; 34: 206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ammenwerth E, Iller C, Mahler C. IT-adoption and the interaction of task, technology and individuals: a fit framework and a case study. BMC Med Inform Decis Mak 2006; 6: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 1989; 13: 319–340. [Google Scholar]
- 27.Lee Y, Kozar KA, Larsen KRT. The technology acceptance model: past, present, and future. Commun Assoc Inf Syst 2003; 12: 50. [Google Scholar]
- 28.Pawson R. Evidence-based policy: a realist perspective. London: Sage Publications, 2006. [Google Scholar]
- 29.Wong G, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: realist syntheses. BMC Med 2013; 11: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pawson R, Greenhalgh T, Harvey G, et al. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005; 10: 21–34. [DOI] [PubMed] [Google Scholar]
- 31.Pawson R, Tilley N. Realistic evaluation. London: Sage, : 1997. [Google Scholar]
- 32.Vareilles G, Pommier J, Marchal B, et al. Understanding the performance of community health volunteers involved in the delivery of health programmes in underserved areas: a realist synthesis. Implement Sci 2017; 12: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dieleman M, Harnmeijer JW. Improving health worker performance: in search of promising practices. Geneva: WHO Evidence and Information for Policy, Department of Human Resources for Health. www.who.int/hrh/resources/improving_hw_performance.pdf (2006, accessed 10 March 2017).
- 34.Opoku D, Stephani V, Quentin W. A realist review of mobile phone-based health interventions for non-communicable disease management in sub-Saharan Africa. BMC Med 2017; 15: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McVeigh J, MacLachlan M, Gilmore B, et al. Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis. Global Health 2016; 12: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bashshur R, Shannon G, Krupinski E, et al. The taxonomy of telemedicine. Telemed J E Health 17: 484–494. [DOI] [PubMed] [Google Scholar]
- 37.Pawson R, Greenhalgh T, Harvey G.et al. Realist synthesis: an introduction. Manchester. https://pdfs.semanticscholar.org/4351/46e6e6617491ff1c4b32b76e0a534c86d6c7.pdf (2004, accessed 10 March 2017).
- 38.Van Belle S. Accountability in sexual and reproductive health. How relations between INGOs and state actors shape public accountability. A study of two local health systems in Ghana. United Kingdom: London School of Hygiene and Tropical Medicine University of London 2014: 1–382.
- 39.Marchal B, Kegels G, Van Belle S, et al. Realist evaluation in health policy and systems research: a fad, a fashion or here to stay? In: Nick E, Greenhalgh T, Manzano A et al. (eds) Doing realist research. London: Sage Publications expected June 2018.
- 40.Pawson R, Tilley N. Realist evaluation, www.communitymatters.com.au/RE_chapter.pdf (2004, accessed 10 March 2017).
- 41.Weiss CH. Theory-based evaluation: past, present, and future. New Dir Eval 1997; 76: 41–55. [Google Scholar]
- 42.Lacouture A, Breton E, Guichard A, et al. The concept of mechanism from a realist approach: a scoping review to facilitate its operationalization in public health program evaluation. Implement Sci 2015; 10: 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010; 31: 363–381. [Google Scholar]
- 44.Sukums F, Mensah N, Mpembeni R, et al. Promising adoption of an electronic clinical decision support system for antenatal and intrapartum care in rural primary healthcare facilities in sub-Saharan Africa: the QUALMAT experience. Int J Med Inform 2015; 84: 647–657. [DOI] [PubMed] [Google Scholar]
- 45.Zakane SA, Gustafsson LL, Tomson G, et al. Guidelines for maternal and neonatal ‘point of care’: needs of and attitudes towards a computerized clinical decision support system in rural Burkina Faso. Int J Med Inform 2014; 83: 459–469. [DOI] [PubMed] [Google Scholar]
- 46.Mensah N, Sukums F, Awine T, et al. Impact of an electronic clinical decision support system on workflow in antenatal care: the QUALMAT eCDSS in rural health care facilities in Ghana and Tanzania. Glob Health Action 2015; 8: 25756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Duysburgh E, Temmerman M, Yé M, et al. Quality of antenatal and childbirth care in rural health facilities in Burkina Faso, Ghana and Tanzania: an intervention study. Trop Med Int Health 2016; 21: 70–83. [DOI] [PubMed] [Google Scholar]
- 48.Blank A, Prytherch H, Kaltschmidt J, et al. ‘ Quality of prenatal and maternal care: bridging the know-do gap’ (QUALMAT study): an electronic clinical decision support system for rural sub-Saharan Africa. BMC Med Inform Decis Mak 2013; 13: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee S. Midwives’ cell phone use and health knowledge in rural communities. J Health Commun 2011; 16: 1006–1023. [DOI] [PubMed] [Google Scholar]
- 50.Chib A, Lwin MO, Ang J, et al. Midwives and mobiles: using ICTs to improve healthcare in Aceh Besar, Indonesia. Asian J Commun 2008; 18: 348–364. [Google Scholar]
- 51.Medhanyie AA, Little A, Yebyo H, et al. Health workers’ experiences, barriers, preferences and motivating factors in using mHealth forms in Ethiopia. Hum Resour Health 2015; 13: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Little A, Medhanyie A, Yebyo H, et al. Meeting community health worker needs for maternal health care service delivery using appropriate mobile technologies in Ethiopia. PLoS One 2013; 8(10): e77563. [DOI] [PMC free article] [PubMed]
- 53.Velez O, Okyere PB, Kanter AS, et al. A usability study of a mobile health application for rural Ghanaian midwives. J Midwifery Womens Health 2014; 59: 184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Velez O. Design and usability testing of an mHealth application for midwives in rural Ghana. New York: Columbia University Academic Commons. 10.7916/D8X354DC. (2011, accessed 11 March 2017). [DOI]
- 55.Mwendwa P. Assessing the fit of RapidSMS for maternal and new-born health: perspectives of community health workers in rural Rwanda. Dev Pract 2016; 26: 38–51. [Google Scholar]
- 56.Perosky JE, Munro ML, Kay JL, et al. Texting from the bush: data collection using SMS text messaging in areas of low network coverage from low-literacy providers. J Health Commun 2015; 20: 1052–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mangwi Ayiasi R, Atuyambe LM, Kiguli J, et al. Use of mobile phone consultations during home visits by community health workers for maternal and newborn care: community experiences from Masindi and Kiryandongo districts, Uganda. BMC Public Health 2015; 15: 560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rodrigo ESS, Wimalaratne SRU, Marasinghe RB, et al. A pilot health information management system for public health midwives serving in a remote area of Sri Lanka. J Telemed Telecare 2012; 18: 159–163. [DOI] [PubMed] [Google Scholar]
- 59.McNabb M, Chukwu E, Ojo O, et al. Assessment of the quality of antenatal care services provided by health workers using a mobile phone decision support application in Northern Nigeria: a pre/post-intervention study. PLoS One 2015; 10: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Straub ET. Understanding technology adoption: theory and future directions for informal learning. Rev Educ Res 2009; 79: 625–649. [Google Scholar]
- 61.Kaphle S, Chaturvedi S, Chaudhuri I, et al. Adoption and usage of mHealth technology on quality and experience of care provided by frontline workers: observations from Rural India. JMIR mHealth uHealth 2015; 3: e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. British Standards Institution. Ergonomic requirements for office work with Visual Display Terminals (VDTs): guidance on usability 1st ed Geneva: International Organization for Standardization, 1998.
- 63.Jimoh L, Pate MA, Lin L, et al. A model for the adoption of {ICT} by health workers in Africa. Int J Med Inform 2012; 81: 773–781. [DOI] [PubMed] [Google Scholar]
- 64.Lim J, Cloete G, Dunsmuir DT, et al. Usability and feasibility of PIERS on the move: an mHealth app for pre-eclampsia triage. JMIR mHealth uHealth 2015; 3: e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Modi D, Gopalan R, Shah S, et al. Development and formative evaluation of an innovative mHealth intervention for improving coverage of community-based maternal, newborn and child health services in rural areas of India. Glob Health Action 2015; 8: 26769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Watson AHA, Sabumei G, Mola G, et al. Maternal health phone line: saving women in Papua New Guinea. J Pers Med 2015; 5: 120–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Woods DD. Text messages as a learning tool for midwives. S Afr Med J 2012; 102: 100–101. [DOI] [PubMed] [Google Scholar]
- 68.Balakrishnan R, Gopichandran V, Chaturvedi S, et al. Continuum of care services for maternal and child health using mobile technology – a health system strengthening strategy in low and middle income countries. BMC Med Inform Decis Mak 2016; 16: 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Atkins MJ. Evaluating interactive technologies for learning. J Curric Stud 1993; 25: 333–342. [Google Scholar]
- 70.Franco LM, Bennett S, Kanfer R. Health sector reform and public sector health worker motivation: a conceptual framework. Soc Sci Med 2002; 54: 1255–1266. [DOI] [PubMed] [Google Scholar]
- 71.Ag Ahmed MA, Gagnon M-P, Hamelin-Brabant L, et al. A mixed methods systematic review of success factors of mhealth and telehealth for maternal health in Sub-Saharan Africa. mHealth 2017; 3: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Venkatesh N, Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manage Sci 2000; 46: 186–204. [Google Scholar]
- 73.Chib A. The Aceh Besar midwives with mobile phones project: design and evaluation perspectives using the information and communication technologies for healthcare development model. J Comput Commun 2010; 15: 500–525. [Google Scholar]
- 74.Cerasoli CP, Nicklin JM, Ford MT. Intrinsic motivation and extrinsic incentives jointly predict performance: a 40-year meta-analysis. Psychol Bull 2014; 140: 980. [DOI] [PubMed] [Google Scholar]
- 75.Bandura A. Exercise of human agency through collective efficacy. Curr Dir Psychol Sci 2000; 9: 75–78. [Google Scholar]
- 76.Goodhue DL, Thompson RL. Task-technology fit and individual performance. MIS Q 1995; 19: 213. [Google Scholar]
- 77.Staples DS, Seddon P. Testing the technology-to-performance chain model. J Organ End User Comput 2004; 16: 17–36. [Google Scholar]
- 78.Booth A, Harris J, Croot E, et al. Towards a methodology for cluster searching to provide conceptual and contextual “richness” for systematic reviews of complex interventions: case study (CLUSTER). BMC Med Res Methodol 2013; 13: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shao AF, Rambaud-Althaus C, Swai N, et al. Can smartphones and tablets improve the management of childhood illness in Tanzania? A qualitative study from a primary health care worker’s perspective. BMC Health Serv Res 2015; 15: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Labrique AB, Vasudevan L, Kochi E, et al. mHealth innovations as health system strengthening tools: 12 common applications and a visual framework. Glob Health Sci Pract 2013; 1: 160–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material 1 for Mobile health and the performance of maternal health care workers in low- and middle-income countries: A realist review by Ibukun-Oluwa Omolade Abejirinde, Onaedo Ilozumba, Bruno Marchal, Marjolein Zweekhorst and Marjolein Dieleman in International Journal of Care Coordination
Supplemental material 2 for Mobile health and the performance of maternal health care workers in low- and middle-income countries: A realist review by Ibukun-Oluwa Omolade Abejirinde, Onaedo Ilozumba, Bruno Marchal, Marjolein Zweekhorst and Marjolein Dieleman in International Journal of Care Coordination