Abstract
Objectives:
To characterize in a large, community cohort of patients with HF, the individual and combined effects of multimorbidity and functional limitation on healthcare utilization and mortality.
Design:
Prospective cohort study.
Setting:
11 southeastern Minnesota counties.
Participants:
Patients with a first-ever HF code (ICD-9 code 428 or ICD-10 code I50) between 1/1/2013 and 3/31/2016 (n=2692).
Measurements:
8 activities of daily living measured by survey on a Likert scale (1=without any difficulty, 5= unable to do; median=8). Patients with a score >8 were categorized as having functional limitation. Multimorbidity was defined as having ≥2 non-cardiac comorbidities.
Results:
Among 2692 patients (mean age 74, 54% male), 25% had neither multimorbidity nor functional limitation, 35% had multimorbidity, 9% had functional limitation and 31% had both. After adjustment, patients with both multimorbidity and functional limitation had increased risks of all outcomes (death HR: 4.92, 95% CI: 3.03–8.00; ED visit HR: 3.67, 95% CI: 2.94–4.59; hospitalization HR: 3.66, 95% CI: 2.85–4.70; outpatient visit HR: 1.73, 95% CI: 1.52–1.96) compared to those with neither. Patients with functional limitation alone had increased risks of death, ED visits and hospitalizations (HR: 4.84, 95% CI: 2.78–8.43; HR: 2.35, 95% CI: 1.75–3.16; HR: 2.10, 95% CI: 1.52–2.88, respectively) but not outpatient visits. Those with multimorbidity alone experienced similar risks of ED visits and hospitalizations as those with functional limitation alone, but were more likely to have outpatient visits (HR: 1.50, 95% CI: 1.34–1.67).
Conclusions:
Patients with both multimorbidity and functional limitation have the highest risk of death and healthcare utilization. Patients with only functional limitation have similar hospitalization and ED visit utilization as those with only with multimorbidity, underscoring the need to consider both when managing patients with HF.
Keywords: heart failure, multimorbidity, functional limitation, outcomes
INTRODUCTION
Heart failure (HF) affects more than 6 million individuals in the US.1 It is predominantly a disease of the elderly and thus multimorbidity and functional limitation are important concerns. Roughly half of patients with HF have 5 or more additional chronic conditions.2–5 Multimorbidity in patients with HF has been shown to be associated with worse outcomes, including increased healthcare utilization and death.6–8 Specifically, non-cardiovascular (CV) conditions have been shown to be more strongly associated with poor outcomes compared to CV-related conditions.8 Additionally, functional limitation is commonly reported among patients with HF and has also been shown to be associated with poor outcomes.9–11
While the individual effects of multimorbidity and poor physical functioning on outcomes among patients with HF have been studied, the combined effect of these conditions on outcomes has not been rigorously evaluated. Emerging evidence suggests that adults with both multimorbidity and functional limitation are high users of healthcare and incur significant healthcare costs.12 Indeed, these patients had twice the hospital use and visited the doctor more frequently than patients with multimorbidity alone and their annual healthcare expenditures were nearly three times as high.12 We aimed to characterize, among a large, community cohort of patients with HF, the individual and combined effects of multimorbidity and functional limitation on healthcare utilization (including hospitalizations, emergency department (ED) visits and outpatient visits) and mortality.
METHODS
This study was conducted in southeast Minnesota, within the 11 counties of Dodge, Fillmore, Freeborn, Goodhue, Houston, Mower, Olmsted, Rice, Steele, Wabasha, and Winona, incorporating data from Mayo Clinic, Mayo Clinic Health System clinics and hospitals, and Olmsted Medical Center and its affiliated clinics. Our study utilized the Rochester Epidemiology Project (REP), a records linkage system which allows retrieval of nearly all healthcare utilization and outcomes of residents living in southeastern Minnesota.13, 14 This region has similar age, sex and ethnic characteristics as the state of Minnesota and the Upper Midwest region of the US.14
Case Identification
Residents age 18 or older with a first-ever International Classification of Diseases, Ninth Revision (ICD-9) code 428 or ICD-10 code I50 for heart failure within the REP records of the 11-county area in southeast Minnesota between January 1, 2013 and March 31, 2016 were identified. These patients were asked to complete a survey to measure functional status. Patients were first mailed a survey packet containing the survey, an introductory letter and HIPAA form. The survey packet was then resent to initial non-responders approximately 1 month after the first mailing. Finally, a telephone interview was attempted approximately 1 month after the second mailing for the remaining non-responders.
Multimorbidity and Functional Limitation
Comorbidities were ascertained electronically by retrieving diagnostic codes from inpatient and outpatient encounters at all providers indexed in the REP. We selected comorbidities that were identified by the US Department of Health and Human Services (US-DHHS) for studying multimorbidity.15, 16 This list contains 20 comorbidities: heart failure, hyperlipidemia, hypertension, arrhythmias, coronary artery disease (CAD), autism, arthritis, asthma, cancer, chronic kidney disease, chronic pulmonary disease, dementia, depression, diabetes, hepatitis, human immunodeficiency virus (HIV), osteoporosis, schizophrenia, substance abuse disorder, and stroke. In our study we excluded HIV (n=2) and autism (n=0) due to low prevalence and HF because all of the patients have HF. We added anxiety as an important chronic condition that was not included in the US-DHHS list, resulting in a total of 18 chronic conditions. Two occurrences of a code (either the same code or two different codes within the code set for a given disease) separated by more than 30 days and occurring within 4 years prior to the index date were required for diagnosis. Conditions were characterized as CV-related (hyperlipidemia, hypertension, arrhythmias and CAD) and non-CV (all other conditions). Because the majority of HF patients had multiple CV comorbidities, and non-CV comorbidities are more strongly related to poor outcomes than CV comorbidities, we defined multimorbidity as the presence of ≥2 non-CV comorbidities.
Functional limitation was measured by activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Patients were asked to self-report their performance of 8 ADLs/IADLs on a 5-point Likert scale (1=without any difficulty to 5= unable to do; score range 8–40; median: 8). Patients were asked how much difficulty they had performing the following without assistance: bathing, getting in and out of bed, feeding yourself, dressing, using the toilet, preparing meals, managing medications and using transportation. Adopting an approach used in previous research,12 functional limitation was defined as having a ADL/IADL score greater than the median (>8), which also corresponds to reporting any limitation in at least 1 of the 8 ADLs/IADLs. Patients were categorized into 4 groups by multimorbidity (Yes/No) and functional limitation (Yes/No).
Outcomes
Participants were followed from survey completion through 12/31/2016 for vital status, hospitalizations, ED visits and outpatient visits. Deaths were identified from medical records and death certificates received from the state of Minnesota. Hospitalizations, ED visits and outpatient visits were collected through the REP, which, as described above, collects information from all in- and outpatient care in the 11 counties. Outpatient visits for tests, imaging, or outpatient procedures were not included. ED visits which resulted in a hospitalization were counted as both an ED visit and a hospitalization. In-hospital transfers were counted as one hospitalization.
Statistical Analysis
Patients who answered at least 6 out of the 8 ADLs/IADLs (≥75% of the questions) were retained for analysis. For those who did not answer all the ADLs/IADLs, the mean of the responses were used to replace the missing responses. Baseline characteristics are presented as frequency (percentage) for categorical variables, mean (standard deviation) for normally-distributed continuous variables, or median (25th, 75th percentile) for continuous variables with a skewed distribution. Chi-square tests for categorical variables and ANOVA for continuous variables were used to test trends in characteristics across the 4 multimorbidity/functional limitation groups.
Cox proportional hazards regression was used to examine the association between the groups and death. Models were run unadjusted and while controlling for age, sex, education and marital status. To account for repeated events, associations between groups and all-cause outpatient visits, ED visits and hospitalizations were analyzed with Andersen-Gill models, univariately and adjusted as for death. Pairwise comparisons among the 4 groups were tested controlling for the false discovery rate to account for multiple comparisons.17 The proportional hazard assumption was tested using the scaled Schoenfeld residuals and was found to be valid.
All analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc, Cary, NC). This study was approved by the Mayo Clinic and Olmsted Medical Center Institutional Review Boards.
RESULTS
Among 6346 patients identified with HF who were mailed a survey, 803 were excluded for the following reasons: deceased (n=270), lost to follow-up (n=23), physically/mentally unable (n=447) and language barrier (n=63), resulting in 5543 patients. Among these patients, 2866 returned the survey (response rate 52%). Survey respondents were slightly older (72.4 vs. 71.2; p=0.002) than non-respondents, but had a similar sex distribution (p=0.90).
Patients with incomplete survey data (n=53; 2%) and those that returned their survey after 12/31/2016 (n=121; 4%) were excluded from the analysis resulting in the sample size of N=2692 (mean age 73.6 years; 53.7% male, Table 1). In total, 674 (25%) patients had neither multimorbidity nor functional limitation, 932 (35%) had multimorbidity only, 248 (9%) had functional limitation only and 838 (31%) had both multimorbidity and functional limitation. The most common non-CV related conditions were diabetes (45%), arthritis (40%) and cancer (31%). Of the 8 ADLs and IADLs that were measured, patients most frequently reported that they had much difficulty with or were unable to do the following on their own: using transportation (37%), preparing meals (28%) and bathing (23%).
Table 1.
Baseline characteristics overall and by categories of multimorbidity and functional limitation
| Multimorbidity/Functional Limitationa | |||||
|---|---|---|---|---|---|
| Overall (N=2692) | No/No (N=674) |
Yes/No (N=932) |
No/Yes (N=248) |
Yes/Yes (N=838) |
|
| Demographics | |||||
| Age, Mean (SD) | 73.6 (12.6) | 69.5 (13.3) | 72.8 (11.2) | 77.9 (12.7) | 76.5 (12.3) |
| Male | 1445 (53.7) | 409 (60.7) | 504 (54.1) | 131 (52.8) | 401 (47.9) |
| Education | |||||
| Non-high school graduate | 304 (11.5) | 52 (7.8) | 100 (10.9) | 32 (13.1) | 120 (14.5) |
| High school graduate | 941 (35.5) | 217 (32.6) | 333 (36.4) | 93 (38.1) | 298 (36.1) |
| Some college/college degree | 1111 (41.9) | 313 (47.0) | 386 (42.1) | 85 (34.8) | 327 (39.6) |
| Graduate school | 296 (11.2) | 84 (12.6) | 97 (10.6) | 34 (13.9) | 81 (9.8) |
| Married | 1564 (58.7) | 431 (64.5) | 590 (63.9) | 124 (50.6) | 419 (50.5) |
| Cardiovascular conditions | |||||
| Hypertension | 2164 (80.4) | 444 (65.9) | 814 (87.3) | 168 (67.7) | 738 (88.1) |
| Coronary artery disease | 1398 (51.9) | 291 (43.2) | 528 (56.7) | 110 (44.4) | 469 (56.0) |
| Arrhythmia | 1846 (68.6) | 403 (59.8) | 668 (71.7) | 147 (59.3) | 628 (74.9) |
| Hyperlipidemia | 1981 (73.6) | 417 (61.9) | 765 (82.1) | 122 (49.2) | 677 (80.8) |
| Non-cardiovascular conditions | |||||
| Arthritis | 1078 (40.0) | 82 (12.2) | 460 (49.4) | 32 (12.9) | 504 (60.1) |
| Asthma | 306 (11.4) | 7 (1.0) | 141 (15.1) | 4 (1.6) | 154 (18.4) |
| Cancer | 835 (31.0) | 78 (11.6) | 406 (43.6) | 27 (10.9) | 324 (38.7) |
| Chronic kidney disease | 764 (28.4) | 36 (5.3) | 320 (34.3) | 12 (4.8) | 396 (47.3) |
| Chronic pulmonary disease | 548 (20.4) | 28 (4.2) | 234 (25.1) | 17 (6.9) | 269 (32.1) |
| Dementia | 92 (3.4) | 3 (0.5) | 25 (2.7) | 4 (1.6) | 60 (7.2) |
| Depression | 527 (19.6) | 12 (1.8) | 228 (24.5) | 8 (3.2) | 279 (33.3) |
| Diabetes | 1224 (45.5) | 119 (17.7) | 560 (60.1) | 49 (19.8) | 496 (59.2) |
| Hepatitis | 19 (0.71) | 2 (0.30) | 5 (0.54) | 0 (0.00) | 12 (1.43) |
| Osteoporosis | 256 (9.5) | 13 (1.9) | 111 (11.9) | 4 (1.6) | 128 (15.3) |
| Schizophrenia | 33 (1.2) | 0 (0.00) | 9 (1.0) | 1 (0.40) | 23 (2.7) |
| Substance abuse disorder | 125 (4.6) | 11 (1.6) | 53 (5.7) | 3 (1.2) | 58 (6.9) |
| Stroke | 354 (13.2) | 15 (2.2) | 151 (16.2) | 7 (2.8) | 181 (21.6) |
| Anxiety | 311 (11.6) | 15 (2.2) | 144 (15.5) | 5 (2.0) | 147 (17.5) |
| ADLs, Median (Q1–Q3) | 8.00 (8–11) | 8.00 (8–8) | 8.00(8–8) | 11.00(10–15) | 12.00 (10–16) |
Data are presented as N (%) unless otherwise specified.
all p<0.05 for 3 df chi-square test for categorical variables and one way ANOVA for continuous variables.
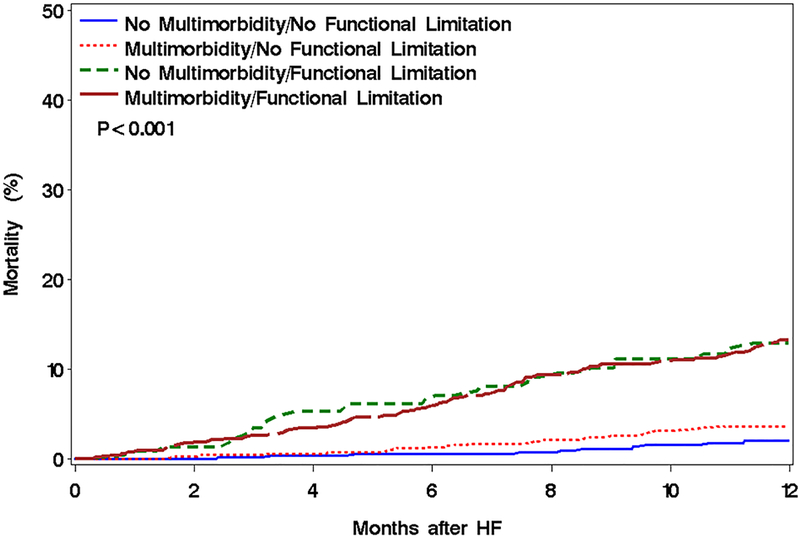
After a mean±SD follow-up of 14.6±7.8 months, 249 deaths occurred. Mortality in the groups with both multimorbidity and functional limitation and only functional limitation were significantly greater than in the other groups (Figure 1, p<0.001). After adjustment for age, sex, education and marital status, patients with both multimorbidity and functional limitation had a 5-fold increased risk of death (HR 4.92; 95% CI: 3.03–8.00; Table 2); those with functional limitation alone also had nearly a 5-fold increased risk (HR 4.84; 95% CI: 2.78–8.43) compared to those with neither. Patients with multimorbidity alone had a 72% increased risk of death (HR: 1.72; 95% CI: 1.01–2.92). Testing the pairwise comparisons among the 4 groups while controlling for the false discovery rate resulted in statistically significant differences between all pairs except for those with multimorbidity only vs. those with neither multimorbidity or functional limitation and for those with functional limitation only vs. those with both multimorbidity and functional limitation.
Figure 1.
Mortality by multimorbidity and functional limitation categories.
Table 2.
Rates (95% CI) and Hazard ratios (95% CI) for Outcomes by Categories of Multimorbidity and Functional Limitationa
| Multimorbidity/Functional Limitation | ||||
|---|---|---|---|---|
| Models | No/No (N=643) |
Yes/No (N=920) |
No/Yes (N=238) |
Yes/Yes (N=824) |
|
All cause death
(249 events) |
||||
| Event rate b | 3.11 (1.90–4.80) | 5.54 (4.13–7.29) | 16.81 (12.01–22.89) | 16.75 (14.07–19.79) |
| Unadjusted model | 1.00 | 1.78 (1.06–2.98) | 5.54 (3.24–9.47) | 5.44 (3.40–8.70) |
| Adjusted Model c | 1.00 | 1.70 (1.02–2.86) | 4.66 (2.70–8.04) | 4.83 (3.00–7.75) |
| Adjusted Model d | 1.00 | 1.72 (1.01–2.92) | 4.84 (2.78–8.43) | 4.92 (3.03–8.00) |
|
All Cause Hospitalizations
(1584 events) |
||||
| Event rate b | 16.95(13.92–20.45) | 27.50 (24.22–31.11) | 31.09 (24.4–39.03) | 43.69 (39.29–48.44) |
| Unadjusted model | 1.00 | 2.01(1.56–2.59) | 2.08 (1.51–2.86) | 3.70 (2.92–4.70) |
| Adjusted Model c | 1.00 | 2.00 (1.55–2.59) | 2.08 (1.51–2.87) | 3.69 (2.88–4.72) |
| Adjusted Model d | 1.00 | 2.00 (1.54–2.59) | 2.10 (1.52–2.88) | 3.66 (2.85–4.70) |
|
All cause ED Visits
(3068 events) |
||||
| Event rate b | 24.88 (21.18–29.05) | 43.37 (39.22– 47.84) | 41.60 (33.81–50.64) | 56.07 (51.07–61.42) |
| Unadjusted model | 1.00 | 2.35 (1.89–2.92) | 2.24 (1.66–3.03) | 3.56 (2.87–4.42) |
| Adjusted Model c | 1.00 | 2.37 (1.90–2.96) | 2.33 (1.72–3.16) | 3.66 (2.91–4.60) |
| Adjusted Model d | 1.00 | 2.40 (1.93–2.98) | 2.35 (1.75–3.16) | 3.67 (2.94–4.59) |
|
Outpatient Visits
(34301 events) |
||||
| Event rate b | 90.20 (83.01–97.85) | 95.65(89.44–102.19) | 88.66 (77.10–101.46) | 93.81 (87.31–100.66) |
| Unadjusted model | 1.00 | 1.50 (1.35–1.67) | 1.06 (0.90–1.25) | 1.76 (1.56–1.99) |
| Adjusted Model c | 1.00 | 1.49 (1.34–1.66) | 1.03 (0.87–1.22) | 1.73 (1.52–1.96) |
| Adjusted Model d | 1.00 | 1.50 (1.34–1.67) | 1.02 (0.86–1.20) | 1.73 (1.52–1.96) |
67 patients without follow-up data were excluded from this analysis.
unadjusted rate per 100 person-years
Adjusted for age and sex.
Adjusted for age, sex, education and marital status.
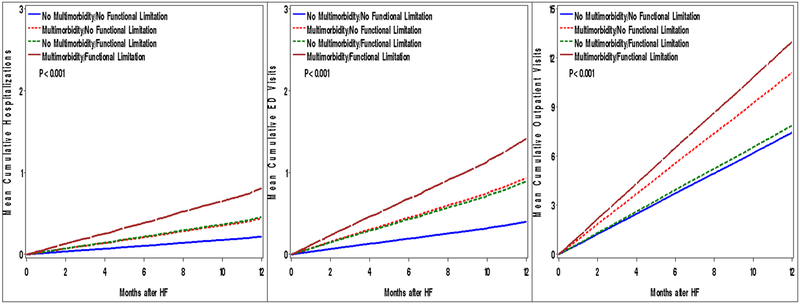
After a mean±SD follow-up of 14.6±7.8 months 1,584 hospitalizations, 3,086 ED visits and 34,301 outpatient visits occurred. Mean cumulative incidence of hospitalizations, ED visits and outpatient visits was highest among the multimorbidity/functional limitation group (Figure 2, p<0.001 for all outcomes). After adjustment, patients with both multimorbidity and functional limitation were 1.7 times more likely to have an outpatient visit (HR: 1.73; 95% CI: 1.52–1.96) and had an approximately 3.6-fold increased risk of ED visits and hospitalizations compared to patients with neither (ED visit HR: 3.67; 95% CI: 2.94–4.59; hospitalization HR: 3.66; 95% CI: 2.85–4.70; Table 2). Patients with functional limitation alone did not have an increase in outpatient visits, but had an approximately 2.4- and 2.1-fold increased risks of ED visits and hospitalizations, respectively (outpatient HR: 1.02; 95% CI: 0.86–1.20; ED visit HR: 2.35; HR: 1.75–3.16; hospitalization HR: 2.10; 95% CI: 1.52–2.88; Table 2). Those with multimorbidity alone experienced similar risks of ED visits and hospitalizations as those with functional limitation alone, although they were 50% more likely to have an outpatient visit (HR: 1.50; 95% CI: 1.34–1.67; Table 2). Testing the pairwise comparisons among the 4 groups while controlling for the false discovery rate resulted in statistically significant differences between all pairs for outpatient visits except for those with functional limitation only vs. those with neither multimorbidity or functional limitation. For ED visits and hospitalizations, all comparisons were significantly different except for multimorbidity alone vs functional limitation alone.
Figure 2.
Mean cumulative number of hospitalizations (left), ED visits (center) and outpatient visits (right) by multimorbidity and functional limitation categories.
In ancillary analyses where functional limitation was defined using only the basic ADLs, similar results were obtained when analyzing the associations between the multimorbidity/functional limitation groups and outcomes, albeit the associations were slightly attenuated for death, hospitalization and ED visits.
DISCUSSION
In our large, contemporary cohort of patients with HF, 31% had both multimorbidity and functional limitation, 35% had multimorbidity alone, 9% had functional limitation alone and 25% had neither. Patients with both multimorbidity and functional limitation had the highest risk for death and hospitalization, ED visits and outpatient visits. For those with functional limitation only, their risk of death was comparable to those with both multimorbidity and functional limitation and higher than those with multimorbidity alone. In addition, their risk of hospitalizations and ED visits was comparable to those with multimorbidity only. Finally, the risk of outpatient visits for those with multimorbidity only was higher than those with functional limitation only. These results have important implications for targeting interventions to those most likely to benefit.
The individual effects of multimorbidity have been studied in patients with HF. We previously studied a community cohort of patients with HF and found that on average these patients have 4 additional comorbid conditions.8 Furthermore, while the most common comorbidities were CV in nature, the burden of other physical or mental conditions was more strongly associated with death and hospitalizations. A study of Medicare beneficiaries with HF found that a higher number of comorbidities was associated with mortality and also found that several non-cardiac conditions were associated with death.3 In another study of Medicare beneficiaries it was reported that nearly 40% of patients with HF have 5 or more non-cardiac conditions and the risk of hospitalization increased with the number of these conditions.6
Functional limitation has also been found to be associated with adverse outcomes in HF patients. We previously found that over half of patients with HF report difficulty with one or more ADLs and increasing ADL difficulty was associated with increased mortality.9 ADL difficulty was also associated with increased risk for hospitalization. In a study of HF patients from the Cardiovascular Health Study, instrumental ADLs were associated with increased mortality, while other measures of functional impairments including basic ADLs and 15-foot walk time were not.11
The combined effects of multimorbidity and functional limitation on outcomes in HF patients are less well known. In our large, community cohort of HF patients, 31% of patients have both multimorbidity and functional limitation. These patients had the highest risk of death and hospitalizations, ED visits and outpatient visits. Our results augment a recent analysis of data from the 2009–2011 Medical Expenditure Panel Survey, which found that adults aged 18 or older with both multimorbidity (defined as 3 or more chronic conditions) and functional limitation (defined as self-reported limitation in an ADL or instrumental ADL) had annual healthcare expenditures that were nearly three times higher than those with multimorbidity alone.12 Rates of hospital use were twice as high and doctor visits were more frequent for patients with both multimorbidity and functional limitation compared to patients with multimorbidity alone.12 In a recent study of the Health and Retirement Study, patients were classified into 4 groups: 1) having one or more severe medical conditions and/or receiving assistance with ADLs (functional limitation); 2) having one or more condition and/or functional limitation and hospital admission in the last 12 months and/or residing in a nursing home; 3) having a condition and functional limitation and hospital admission in the last 12 months and/or residing in a nursing home; 4) meeting none of the above criteria.18 Patients in group 3 had the highest proportion of hospitalizations, highest total Medicare expenditures and highest mortality after 1 year.18
Furthermore, we found that patients with either multimorbidity or functional limitation alone had similar risk for hospitalizations and ED visits. This is important as it provides further evidence that both multimorbidity and functional limitation should be considered when managing patients with HF. Another interesting finding was that having functional limitation only was associated with a large increased risk of death, however having multimorbidity only was not, which also underscores the importance of functional limitation in the prognosis of HF patients.
Clinical Implications
This work has important clinical implications because we expand upon previous work by studying not only the individual effects but also the combined effects of multimorbidity and functional limitations on outcomes in HF. Our results indicate that both multimorbidity and functional limitation are common among patients with HF and have important prognostic value. Patients experiencing both multimorbidity and functional limitation have the highest risk of death and healthcare utilization. Thus, interventions should be targeted to these patients in order to improve their outcomes. There is evidence that interventions to improve physical functioning appear to be effective among patients with HF.19–21 Furthermore, the importance of recognizing the complexity of caring for patients with multiple chronic conditions has been recently highlighted22 as has incorporating principles of geriatrics to the care of patients with cardiovascular disease.23 Indeed, the presence of multiple conditions increases the challenges for health care providers and patients, and can affect patient safety if recommendations for one condition conflict with those of another condition.22 Thus these complex patients should be the target of future interventions in order to undercover ways to best manage them and improve their outcomes.
Limitations and Strengths
Some limitations to the study should be noted. As in any survey study, non-responder bias could be an issue, although baseline characteristics were similar between those who completed the survey and those who did not. We may have missed some healthcare encounters that occurred outside of the 11-county REP area. Our study was conducted in a population of mostly white race; thus, the generalizability may be limited. However, prior epidemiological study has demonstrated that the population from which our cohort was derived is similar to the population of the upper Midwest in terms of age, sex, and ethnic characteristics.24
Our study also has notable strengths. This is a large, community-based cohort study and we have comprehensive ascertainment of comorbidities, death and healthcare utilization in a large area of southeast Minnesota.13 We are one of the first studies to report on the combined effects of multimorbidity and functional limitation in patients with HF. Furthermore, our response rate was somewhat higher than response rates in national surveys.25
Conclusions
Patients with both multimorbidity and functional limitation have the highest risk for death and healthcare utilization. Patients with functional limitation alone have similar hospitalizations and ED visits but an increased risk of death compared with those with multimorbidity alone. This underscores the need to consider both multimorbidity and functional limitation when managing patients with HF.
Impact Statement:
We certify that this work is novel.
To the best of our knowledge, this research is novel because it reports on not only the individual effects, but also the combined effects of multimorbidity and functional limitation in patients with heart failure.
ACKNOWLEDGMENTS
We thank Ellen Koepsell, RN, Dawn Schubert, RN, Sandra Severson, RN, and Deborah Strain for their study support.
Sources of Funding:This work was supported by grants from the National Heart, Lung and Blood Institute (R01 HL120859) and the Patient Centered Outcomes Research Institute - PCORI (CDRN-1501–26638) and was made possible by the Rochester Epidemiology Project, Rochester, MN (R01 AG034676) from the National Institute on Aging. The funding sources played no role in the design, conduct, or reporting of this study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Sponsor’s Role:The funding sources played no role in the design, conduct, or reporting of this study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: None.
REFERENCES
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133: e38–360. [DOI] [PubMed] [Google Scholar]
- 2.Chamberlain AM, St Sauver JL, Gerber Y, et al. Multimorbidity in heart failure: a community perspective. Am J Med. 2015;128: 38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahluwalia SC, Gross CP, Chaudhry SI, et al. Impact of comorbidity on mortality among older persons with advanced heart failure. J Gen Intern Med. 2012;27: 513–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong CY, Chaudhry SI, Desai MM, et al. Trends in comorbidity, disability, and polypharmacy in heart failure. Am J Med. 2011;124: 136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saczynski JS, Go AS, Magid DJ, et al. Patterns of comorbidity in older adults with heart failure: the Cardiovascular Research Network PRESERVE study. J Am Geriatr Soc. 2013;61: 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braunstein JB, Anderson GF, Gerstenblith G, et al. Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure. J Am Coll Cardiol. 2003;42: 1226–1233. [DOI] [PubMed] [Google Scholar]
- 7.Mentz RJ, Kelly JP, von Lueder TG, et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol. 2014;64: 2281–2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manemann SM, Chamberlain AM, Boyd CM, et al. Multimorbidity in Heart Failure: Effect on Outcomes. J Am Geriatr Soc. 2016;64: 1469–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunlay SM, Manemann SM, Chamberlain AM, et al. Activities of daily living and outcomes in heart failure. Circ Heart Fail. 2015;8: 261–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chamberlain AM, McNallan SM, Dunlay SM, et al. Physical health status measures predict all-cause mortality in patients with heart failure. Circ Heart Fail. 2013;6: 669–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murad K, Goff DC Jr., Morgan TM, et al. Burden of Comorbidities and Functional and Cognitive Impairments in Elderly Patients at the Initial Diagnosis of Heart Failure and Their Impact on Total Mortality: The Cardiovascular Health Study. JACC Heart Fail. 2015;3: 542–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayes SL, Salzberg CA, McCarthy D, et al. High-Need, High-Cost Patients: Who Are They and How Do They Use Health Care? A Population-Based Comparison of Demographics, Health Care Use, and Expenditures. Issue Brief (Commonw Fund). 2016;26: 1–14. [PubMed] [Google Scholar]
- 13.Rocca WA, Yawn BP, St Sauver JL, et al. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87: 1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.JL Sauver, Grossardt BR, Leibson CL, et al. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87: 151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goodman RA, Posner SF, Huang ES, et al. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Preventing chronic disease. 2013;10: E66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Department of Health and Human Services. Multiple chronic conditions - a strategic framework: optimum health and quality of life for individuals with multiple chronic conditions. Washington, DC, December, 2010. [Google Scholar]
- 17.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B (Methodological). 1995;57: 289–300. [Google Scholar]
- 18.Kelley AS, Covinsky KE, Gorges RJ, et al. Identifying Older Adults with Serious Illness: A Critical Step toward Improving the Value of Health Care. Health Serv Res. 2017;52: 113–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson L, Oldridge N, Thompson DR, et al. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. J Am Coll Cardiol. 2016;67: 1–12. [DOI] [PubMed] [Google Scholar]
- 20.O’Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301: 1439–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor RS, Sagar VA, Davies EJ, et al. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014: CD003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arnett DK, Goodman RA, Halperin JL, et al. AHA/ACC/HHS strategies to enhance application of clinical practice guidelines in patients with cardiovascular disease and comorbid conditions: from the American Heart Association, American College of Cardiology, and US Department of Health and Human Services. Circulation. 2014;130: 1662–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell SP, Orr NM, Dodson JA, et al. What to Expect From the Evolving Field of Geriatric Cardiology. J Am Coll Cardiol. 2015;66: 1286–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.St Sauver JL, Grossardt BR, Leibson CL, et al. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87: 151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Czajki J, Beyler A. Declining Response Rates in Federal Surveys: Trends and Applications. 2016. Accessed at: https://aspe.hhs.gov/system/files/pdf/255531/Decliningresponserates.pdf Accessed November 15, 2017