Abstract
Human granulocytic anaplasmosis (HGA) is a debilitating, non-specific febrile illness caused by the granulocytotropic obligate intracellular bacterium called Anaplasma phagocytophilum. Surveillance studies indicate a higher prevalence of HGA in male versus female patients. Whether this discrepancy correlates with differential susceptibility of males and females to A. phagocytophilum infection is unknown. Laboratory mice have long been used to study granulocytic anaplasmosis. Yet, sex as a biological variable (SABV) in this model has not been evaluated. In this paper, groups of male and female C57Bl/6 mice that had been infected with A. phagocytophilum were assessed for the bacterial DNA load in the peripheral blood, the percentage of neutrophils harboring bacterial inclusions called morulae, and splenomegaly. Infected male mice exhibited as much as a 1.85-fold increase in the number of infected neutrophils, which is up to a 1.88-fold increase in the A. phagocytophilum DNA load, and a significant increase in spleen size when compared to infected female mice. The propensity of male mice to develop a higher level of A. phagocytophilum infection is relevant for studies utilizing the mouse model. This stresses the importance of including SABV and aligns with the observed higher incidence of infection in male versus female patients.
Keywords: anaplasmosis, anaplasmataceae, mouse model, sex as a biological variable, morula, intracellular bacteria, gender differences to infection
1. Introduction
Sex as a biological variable (SABV) is an important criterion to include in vertebrate animal studies. As part of its approach to increase rigor and reproducibility, the United States (USA) National Institutes of Health recently changed its guidelines to ensure that its funded vertebrate animal studies address SABV. As many as 37% of published preclinical animal studies and 9% of published cell culture studies may have been affected by these new guidelines [1]. Biological differences between males and females have been shown to affect infection rates and variable gene transcription of multiple pathogens including Mycobacterium tuberculosis [2,3], Legionella spp. [4], and Coxiella burnetii [5]. Even though infections caused by bacteria in the order Rickettsiales have led to the loss of millions of lives throughout history, have impacted wars, and continue to threaten global health today [6,7,8,9,10,11,12,13], no study to date has addressed SABV for any rickettsial organism.
Anaplasma phagocytophilum is a tick-transmitted obligate intracellular bacterium of the order Rickettsiales that preferentially infects granulocytes and bone marrow progenitor cells to cause human granulocytic anaplasmosis (HGA). The emerging infection typically presents as a non-specific febrile illness that is self-limiting in otherwise healthy individuals. In the elderly, the immunocompromised, and, in some instances, when proper antibiotic therapy is delayed, HGA can result in potentially deadly sequelae including rhabdomyolysis, septic shock, and pneumonia [14]. The first HGA case was documented in Minnesota, USA in 1994 [15]. Since then, the disease has been increasingly reported in the USA, Europe, and Asia [14]. From the year 2000, when HGA was reported to the USA Centers for Disease Control (CDC), up to 2016, the number of annually reported cases rose from 350 to 4151, which represents a 1186% increase [16]. Seroepidemiologic data indicate that its incidence may be several-fold higher in some endemic areas [17,18]. Notably, it has been reported that male HGA patients outnumber female HGA patients three to one [19].
The mouse model has been utilized to study A. phagocytophilum infection in vivo for more than 20 years. Infected mice develop laboratory markers that occur during HGA. One of these markers shows that neutrophils harboring intravacuolar A. phagocytophilum colonies, called morulae, can be detected in peripheral blood smears using light microscopy. A. phagocytophilum infected mice also develop splenomegaly [20,21,22,23,24,25,26]. Whether male or female mice exhibit differential susceptibility to infection with the bacterium has yet to be explored. This fact has led to the current study. In this paper, we demonstrate that male mice exhibit significantly higher peripheral blood bacterial burdens and splenomegaly than female mice after infection with A. phagocytophilum.
2. Materials and Methods
2.1. Cultivation of Uninfected and A. phagocytophilum Infected Cell Lines
Uninfected and A. phagocytophilum (NCH-1 strain) infected human promyelocytic HL-60 cells, CCL-240 (American Type Culture Collection (ATCC), Manassas, VA, USA) were cultured as described previously [27].
2.2. Literature Search
To determine if prior publications that utilized the mouse model of granulocytic anaplasmosis examined the influence of SABV on A. phagocytophilum infection, queries of PubMed (https://www.ncbi.nlm.nih.gov/m/pubmed) were performed using combinations of the following keywords or keyword combinations: A. phagocytophilum, granulocytic anaplasmosis, granulocytic ehrlichiosis, human granulocytic anaplasmosis, human granulocytic ehrlichiosis, agent of human granulocytic ehrlichiosis, mouse, murine, and in vivo. The time period examined was 1980 to present. The searches returned a total of 61 different publications.
2.3. Infection of C57/Bl6J Mice
Seven-week-old female and male C57Bl/6J mice (Jackson Laboratories, Bar Harbor, ME, USA) were housed in animal biosafety level-2 laboratories prior to and during all experiments. Mice were intraperitoneally inoculated with 1 × 108 A. phagocytophilum organisms that had been recovered following sonication of infected HL-60 cells and differential centrifugation, which is a method that specifically isolates the infectious dense-core but not the non-infectious reticulate cell form [28]. Sterile PBS was used as a mock inoculum to inject negative control animals. Blood was collected from the tail vein on days 0, 4, 8, 12, 16, 21, and/or 28. On day 28, the mice were euthanized, blood was collected via cardiac puncture, and spleens were harvested. All animal research was performed under the approval of the Institutional Animal Care and Use Committee at Virginia Commonwealth University (Protocol Number AM10220).
2.4. Evaluation of A. phagocytophilum Infection
Peripheral blood smears were fixed and stained with FisherBrand Hema 3 solutions (ThermoFisher, Waltham, MA, USA) and examined by light microscopy for the presence of neutrophils with morulae. Three blood smears were examined per time point per mouse in order for the percentage of infected neutrophils to be determined from a total of at least 300 neutrophils. DNA was isolated from heparin-treated blood using the DNeasy Blood and Tissue Kit (Qiagen, Valencia, CA, USA). Fifty nanograms of DNA were subjected to quantitative PCR (qPCR) using primers targeting A. phagocytophilum 16S rDNA and mouse β-actin [29], SsoFast EvaGreen Supermix (Biorad, Hercules, CA, USA), and the CFX384 Detection System (Biorad). Thermal cycling conditions consisted of an initial denaturation step of 98 °C for 2 min and was followed by 40 cycles at 98 °C for 5 s and 60 °C for 30 s. The relative 16 S rDNA levels were normalized to that of β-actin using the 2−ΔΔCT method [30]. To assess for splenomegaly, spleen-to-body weight ratios were determined on day 28.
2.5. Statistical Analysis
Statistical analyses were performed using the Prism 5.0 software package (Graphpad, San Diego, CA, USA). Two-way analysis of variance (ANOVA) with the Sidek’s post-hoc test was used to test for a significant difference among the groups. A paired student’s t-test was used to test for statistical significance between paired data. Statistical significance was set at p values of <0.05.
3. Results
3.1. A. phagocytophilum Infected Male Mice Have Higher Peripheral Blood Bacterial DNA Levels than Infected Female Mice
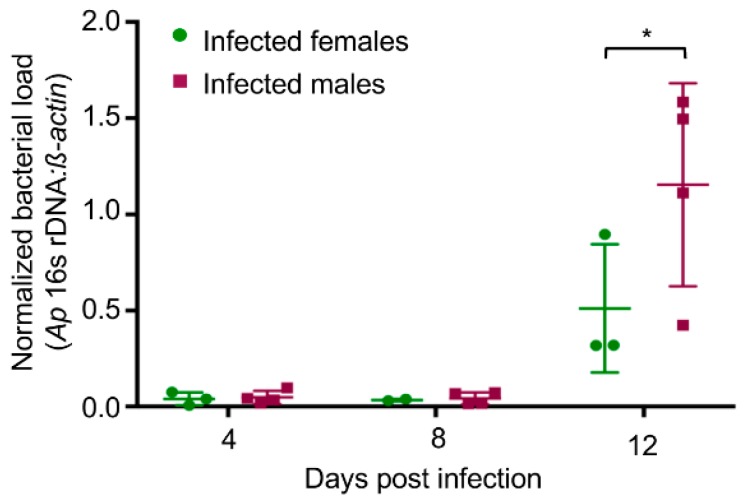
An examination of the literature revealed 61 publications that used the mouse model of granulocytic anaplasmosis. Of the 61 reports, 31 did not disclose the gender, 13 used only females, 9 used only males, 6 included both sexes, 1 used females for one group and males for another, and 1 used females for the experimental group but male and females for the control group [20,21,22,23,25,26,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83] (Table 1). None of the six studies that included males and females examined for a correlation between sex and differential susceptibility to A. phagocytophilum infection [25,39,41,62,65,73]. We sought to determine if such a correlation exists. Following inoculation, the A. phagocytophilum peripheral blood burden in immunocompetent wild-type mice tends to peak by day 12 and subsides thereafter to undetectable or near undetectable levels by days 21 to 28 [23,26,38,45,52,58,60,64,68,71,73,75,78,81,84]. C57Bl/6 mice are commonly used for studying A. phagocytophilum infection [26,34,36,38,39,40,41,52,61,62,65,68,70,73,75,76,78,84,85]. Male and female C57Bl/6 mice were intraperitoneally inoculated with host cell-free A. phagocytophilum organisms. DNA was isolated from blood obtained on days 4, 8, and 12 and subjected to qPCR using primers targeting A. phagocytophilum 16S rDNA and mouse β-actin. On day 12, the relative bacterial load in the peripheral blood of male mice exhibited a statistically significant 1.88-fold increase relative to bacterial load in the peripheral blood of female mice (Figure 1).
Table 1.
Published studies using the mouse model of granulocytic anaplasmosis.
| References | Usage of Female and/or Male Mice |
|---|---|
| [20,21,22,26,31,32,34,35,36,38,40,42,45,46,47,48,49,51,54,55,56,59,60,63,66,72,74,75,78,79,80] | Not disclosed |
| [23,43,52,53,58,64,67,68,69,70,71,81,82] | Females |
| [33,37,44,50,57,61,77,83,84] | Males |
| [25,39,41,62,65,73] | Males and females |
| [85] | Females used for experimental group and males used for control group |
| [76] | Females used for experimental group and males and females used for controls |
Figure 1.
A. phagocytophilum infected male mice exhibit higher peripheral A. phagocytophilum DNA levels than female mice. Male and female C57Bl/6 mice were intraperitoneally injected with A. phagocytophilum organisms. DNA samples isolated from heparin-treated blood recovered on days 4, 8, and 12 and were then subjected to qPCR using gene-specific primers. Relative A. phagocytophilum 16S rDNA-to-murine β-actin DNA levels for each mouse generated using the 2−ΔΔCT method along with their standard deviations are presented. Statistically significant (* p < 0.05) values are indicated.
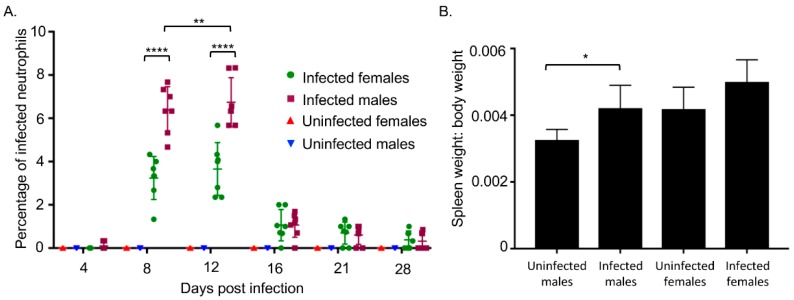
3.2. A. phagocytophilum Infected Male Mice Exhibit Higher Percentages of Neutrophils Harboring Morulae and Splenomegaly Compared to Infected Female Mice
The infection experiment was repeated except that each sex group consisted of seven mice. To address the possibility that A. phagocytophilum might achieve its highest peripheral load in female mice at a later time point than day 12, blood was drawn on days 4, 8, 12, 16, 21, and 28. In addition, since qPCR measures the DNA load and, therefore, cannot distinguish DNA derived from live versus dead bacteria, blood smears were generated and examined for the presence of neutrophils harboring morulae. Consistent with the qPCR data, both sexes had the highest mean percentage ± SD of neutrophils with morulae on day 12 (Figure 2A). However, the percentages of infected neutrophils in female mice never became as high as that observed in male mice, which were significantly 1.97-fold and 1.85-fold greater on days 8 and 12, respectively. Little to no infected peripheral blood neutrophils were detectable for either sex by day 28. Overall, these data indicate that, while the kinetics of A. phagocytophilum infection do not differ between male and female mice over the course of infection, the bacterium achieves a significantly higher load in the peripheral blood in male mice. On day 28, the mice were euthanized, spleens harvested, and their spleen-to-body weight ratios determined. The mean spleen-to-body weight ratio of infected to uninfected male mice increased significantly while the mean spleen-to-body weight ratio of infected to uninfected female mice did not (Figure 2B).
Figure 2.
A. phagocytophilum infected male mice have higher percentages of peripheral blood neutrophils harboring morulae and greater degrees of splenomegaly than infected female mice. Male and female C57Bl/6 mice were intraperitoneally injected with A. phagocytophilum bacteria. (A) Peripheral blood smears were microscopically examined for neutrophils that contained morulae. Each dot corresponds to the mean percentage of infected neutrophils determined from counting a total of at least 300 neutrophils from three separate blood smears per mouse. Error bars correspond to the mean ± standard deviation of the percentages determined for all seven mice per group. Data are representative of two experiments with similar results; (B) On day 28, the mice were euthanized, the spleens were harvested, and the spleen-to-body weight ratios were calculated. Data are the mean ± standard deviation of the ratios determined from seven mice per group. Statistically significant (* p < 0.05, ** p < 0.01, **** p < 0.0001 values are indicated.
4. Discussion
This study demonstrates for the first time that A. phagocytophilum achieves a higher peripheral blood load and causes a greater degree of splenomegaly in male versus female mice using the C57Bl/6 strain, which is the most-commonly used murine model of granulocytic anaplasmosis. These results are consistent with a higher case incidence in males among HGA patients [19]. The biological basis for this difference is unclear. Given that A. phagocytophilum incorporates cholesterol into its cell wall [86], replicates better in the presence of cholesterol [61,87,88], and specifically exploits the low-density lipoprotein (LDL) uptake pathway [88], it is reasonable to speculate that the better infection the bacterium exhibits in males could be at least partially linked to the fact that men tend to have higher LDL-cholesterol levels than women [89]. A report using apolipoprotein E-deficient mice and mice fed high cholesterol diets conspicuously demonstrated that high blood cholesterol levels facilitate A. phagocytophilum infection. However, that study, which only assessed the relevance of cholesterol to A. phagocytophilum infection, exclusively utilized male mice [61]. It would be worth revisiting this study using males and females. Another possible gender-based difference that could account for the reduced permissiveness of females to A. phagocytophilum is that female mice and humans tend to produce higher levels of IFNγ and exhibit more robust innate and adaptive immune responses than males. This difference translates to better clearance, reduced susceptibility, and lower disease incidence of viral and fungal infections in female mice [90,91,92,93]. An IFNγ dominated immune response is critical for clearing A. phagocytophilum infection [59].
Whether a similar sex bias for better A. phagocytophilum infection exists in other laboratory mouse strains remains to be determined. Due to the importance of including SABV as a criterion when designing vertebrate animal experiments unless a sex bias in the model exists, the differential susceptibility of male versus female mice to A. phagocytophilum infection demonstrated in this paper should be kept in mind for future experiments using the C57Bl/6 strain.
Author Contributions
J.A.C., W.A.N., R.S.G. and C.L.C. conceived and designed the experiments. W.A.N., R.S.G. and C.L.C. performed the experiments. W.A.N., R.S.G., C.L.C. and J.A.C. analyzed the data. J.A.C., C.L.C. and W.A.N. wrote the manuscript.
Funding
This study was supported by the National Institutes of Health (grant AI072683-11A1 to Jason A. Carlyon).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Potluri T., Engle K., Fink A.L., Vom Steeg L.G., Klein S.L. Sex reporting in preclinical microbiological and immunological research. MBio. 2017;8:e01868-17. doi: 10.1128/mBio.01868-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holmes C.B., Hausler H., Nunn P. A review of sex differences in the epidemiology of tuberculosis. Int. J. Tuberc. Lung Dis. 1998;2:96–104. [PubMed] [Google Scholar]
- 3.Jimenez-Corona M.E., Garcia-Garcia L., DeRiemer K., Ferreyra-Reyes L., Bobadilla-del-Valle M., Cano-Arellano B., Canizales-Quintero S., Martínez-Gamboa A., Small P.M., Sifuentes-Osornio J., et al. Gender differentials of pulmonary tuberculosis transmission and reactivation in an endemic area. Thorax. 2006;61:348–353. doi: 10.1136/thx.2005.049452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greig J.E., Carnie J.A., Tallis G.F., Ryan N.J., Tan A.G., Gordon I.R., Zwolak B., Leydon J.A., Guest C.S., Hart W.G. An outbreak of Legionnaires’ disease at the Melbourne Aquarium, April 2000: Investigation and case-control studies. Med. J. Aust. 2004;180:566–572. doi: 10.5694/j.1326-5377.2004.tb06093.x. [DOI] [PubMed] [Google Scholar]
- 5.Textoris J., Ban L.H., Capo C., Raoult D., Leone M., Mege J.L. Sex-related differences in gene expression following Coxiella burnetii infection in mice: Potential role of circadian rhythm. PLoS ONE. 2010;5:e12190. doi: 10.1371/journal.pone.0012190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berman S.J., Kundin W.D. Scrub typhus in South Vietnam: A study of 87 cases. Ann. Intern. Med. 1973;79:26–30. doi: 10.7326/0003-4819-79-1-26. [DOI] [PubMed] [Google Scholar]
- 7.Chattopadhyay S., Richards A.L. Scrub typhus vaccines: Past history and recent developments. Hum. Vaccin. 2007;3:73–80. doi: 10.4161/hv.3.3.4009. [DOI] [PubMed] [Google Scholar]
- 8.Deller J.J., Jr., Russell P.K. An analysis of fevers of unknown origin in American soldiers in Vietnam. Ann. Intern. Med. 1967;66:1129–1143. doi: 10.7326/0003-4819-66-6-1129. [DOI] [PubMed] [Google Scholar]
- 9.Gormley T.S. A diagnosis of scrub typhus. Navy Med. 1996;87:20–22. [Google Scholar]
- 10.Kelly D.J., Fuerst P.A., Ching W.M., Richards A.L. Scrub typhus: The geographic distribution of phenotypic and genotypic variants of Orientia tsutsugamushi. Clin. Infect. Dis. 2009;48(Suppl. 3):S203–S230. doi: 10.1086/596576. [DOI] [PubMed] [Google Scholar]
- 11.Kelly D.J., Richards A.L., Temenak J., Strickman D., Dasch G.A. The past and present threat of rickettsial diseases to military medicine and international public health. Clin. Infect. Dis. 2002;34(Suppl. 4):S145–S169. doi: 10.1086/339908. [DOI] [PubMed] [Google Scholar]
- 12.Sahni S.K., Narra H.P., Sahni A., Walker D.H. Recent molecular insights into rickettsial pathogenesis and immunity. Future Microbiol. 2013;8:1265–1288. doi: 10.2217/fmb.13.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Valbuena G., Walker D.H. Approaches to vaccines against Orientia tsutsugamushi. Front. Cell. Infect. Microbiol. 2012;2:170. doi: 10.3389/fcimb.2012.00170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bakken J.S., Dumler J.S. Human granulocytic anaplasmosis. Infect. Dis. Clin. N. Am. 2015;29:341–355. doi: 10.1016/j.idc.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen S.M., Dumler J.S., Bakken J.S., Walker D.H. Identification of a granulocytotropic Ehrlichia species as the etiologic agent of human disease. J. Clin. Microbiol. 1994;32:589–595. doi: 10.1128/jcm.32.3.589-595.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Number of Reported Anaplasmosis Cases by Month of Onset, 2000–2016. [(accessed on 27 June 2018)]; Available online: https://www.cdc.gov/anaplasmosis/stats/index.html.
- 17.Johan S.B., Paul G., Mark Van E., Denise Z.B., Oscar L.S., Sandy M., Krueth J., Tilden R.L., Asanovich K., Walls J., et al. Seroprevalence of human granulocytic ehrlichiosis among permanent residents of northwestern Wisconsin. Clin. Infect. Dis. 1998;27:1491–1496. doi: 10.1086/515048. [DOI] [PubMed] [Google Scholar]
- 18.Aguero-Rosenfeld M.E., Donnarumma L., Zentmaier L., Jacob J., Frey M., Noto R., Carbonaro C.A., Wormser G.P. Seroprevalence of antibodies that react with Anaplasma phagocytophila, the agent of human granulocytic ehrlichiosis, in different populations in Westchester County, New York. J. Clin. Microbiol. 2002;40:2612–2615. doi: 10.1128/JCM.40.7.2612-2615.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bakken J.S., Dumler J.S. Clinical diagnosis and treatment of human granulocytotropic anaplasmosis. Ann. N. Y. Acad. Sci. 2006;1078:236–247. doi: 10.1196/annals.1374.042. [DOI] [PubMed] [Google Scholar]
- 20.Hodzic E., Fish D., Maretzki C.M., De Silva A.M., Feng S., Barthold S.W. Acquisition and transmission of the agent of human granulocytic ehrlichiosis by Ixodes scapularis ticks. J. Clin. Microbiol. 1998;36:3574–3578. doi: 10.1128/jcm.36.12.3574-3578.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hodzic E., Ijdo J.W.I., Feng S., Katavolos P., Sun W., Maretzki C.H., Fish D., Fikrig E., Telford S.R., III, Barthold W.S. Granulocytic ehrlichiosis in the laboratory mouse. J. Infect. Dis. 1998;177:737–745. doi: 10.1086/514236. [DOI] [PubMed] [Google Scholar]
- 22.Hodzic E., Feng S., Fish D., Leutenegger C.M., Freet K.J., Barthold S.W. Infection of mice with the agent of human granulocytic ehrlichiosis after different routes of inoculation. J. Infect. Dis. 2001;183:1781–1786. doi: 10.1086/320735. [DOI] [PubMed] [Google Scholar]
- 23.Sun W., Ijdo J.W., Telford S.R., III, Hodzic E., Zhang Y., Barthold S.W., Fikrig E. Immunization against the agent of human granulocytic ehrlichiosis in a murine model. J. Clin. Investig. 1997;100:3014–3018. doi: 10.1172/JCI119855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borjesson D.L., Barthold S.W. The mouse as a model for investigation of human granulocytic ehrlichiosis: Current knowledge and future directions. Comp. Med. 2002;52:403–413. [PubMed] [Google Scholar]
- 25.Wang X., Shaw D.K., Hammond H.L., Sutterwala F.S., Rayamajhi M., Shirey K.A., Perkins D.J., Bonventre J.V., Velayutham T.S., Evans S.M., et al. The prostaglandin E2-EP3 receptor axis regulates Anaplasma phagocytophilum-mediated NLRC4 inflammasome activation. PLoS Pathog. 2016;12:e1005803. doi: 10.1371/journal.ppat.1005803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carlyon J.A., Akkoyunlu M., Xia L., Yago T., Wang T., Cummings R.D., McEver R.P., Fikrig E. Murine neutrophils require alpha1,3-fucosylation but not PSGL-1 for productive infection with Anaplasma phagocytophilum. Blood. 2003;102:3387–3395. doi: 10.1182/blood-2003-02-0621. [DOI] [PubMed] [Google Scholar]
- 27.Truchan H.K., VieBrock L., Cockburn C.L., Ojogun N., Griffin B.P., Wijesinghe D.S., Chalfant C.E., Carlyon J.A. Anaplasma phagocytophilum Rab10-dependent parasitism of the trans-Golgi network is critical for completion of the infection cycle. Cell. Microbiol. 2016;18:260–281. doi: 10.1111/cmi.12500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Troese M.J., Carlyon J.A. Anaplasma phagocytophilum dense-cored organisms mediate cellular adherence through recognition of human P-selectin glycoprotein ligand 1. Infect. Immun. 2009;77:4018–4027. doi: 10.1128/IAI.00527-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ojogun N., Kahlon A., Ragland S.A., Troese M.J., Mastronunzio J.E., Walker N.J., VieBrock L., Thomas R.J., Borjesson D.L., Fikrig E., et al. Anaplasma phagocytophilum outer membrane protein A interacts with sialylated glycoproteins to promote infection of mammalian host cells. Infect. Immun. 2012;80:3748–3760. doi: 10.1128/IAI.00654-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 31.Hodzic E., Borjesson D.L., Feng S., Barthold S.W. Acquisition dynamics of Borrelia burgdorferi and the agent of human granulocytic ehrlichiosis at the host-vector interface. Vector Borne Zoonotic Dis. 2001;1:149–158. doi: 10.1089/153036601316977750. [DOI] [PubMed] [Google Scholar]
- 32.Levin M.L., Ross D.E. Acquisition of different isolates of Anaplasma phagocytophilum by Ixodes scapularis from a model animal. Vector Borne Zoonotic Dis. 2004;4:53–59. doi: 10.1089/153036604773082997. [DOI] [PubMed] [Google Scholar]
- 33.Lin Q., Zhang C., Rikihisa Y. Analysis of involvement of the RecF pathway in p44 recombination in Anaplasma phagocytophilum and in Escherichia coli by using a plasmid carrying the p44 expression and p44 donor loci. Infect. Immun. 2006;74:2052–2062. doi: 10.1128/IAI.74.4.2052-2062.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen G., Severo M.S., Sakhon O.S., Choy A., Herron M.J., Felsheim R.F., Wiryawanc H., Liaoc J., Johnsd J.L., Munderlohb U.G., et al. Anaplasma phagocytophilum dihydrolipoamide dehydrogenase 1 affects host-derived immunopathology during microbial colonization. Infect. Immun. 2012;80:3194–3205. doi: 10.1128/IAI.00532-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhan L., Cao W.-C., Jiang J.-F., Zhang X.-A., Liu Y.-X., Wu X.-M., Zhang W.-Y., Zhang P.-H., Bian C.-L., Dumler J.S., et al. Anaplasma phagocytophilum from rodents and sheep, China. Emerg. Infect. Dis. 2010;16:764–768. doi: 10.3201/eid1605.021293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi K.S., Scorpio D.G., Dumler J.S. Anaplasma phagocytophilum ligation to toll-like receptor (TLR) 2, but not to TLR4, activates macrophages for nuclear factor-kappa B nuclear translocation. J. Infect. Dis. 2004;189:1921–1925. doi: 10.1086/386284. [DOI] [PubMed] [Google Scholar]
- 37.Wang X., Cheng Z., Zhang C., Kikuchi T., Rikihisa Y. Anaplasma phagocytophilum p44 mRNA expression is differentially regulated in mammalian and tick host cells: Involvement of the DNA binding protein ApxR. J. Bacteriol. 2007;189:8651–8659. doi: 10.1128/JB.00881-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scorpio D.G., Choi K.-S., Dumler J.S. Anaplasma phagocytophilum-related defects in CD8, NKT, and NK lymphocyte cytotoxicity. Front. Immunol. 2018;9:710. doi: 10.3389/fimmu.2018.00710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pedra J.H., Sutterwala F.S., Sukumaran B., Ogura Y., Qian F., Montgomery R.R., Flavell R.A., Fikrig E. ASC/PYCARD and caspase-1 regulate the IL-18/IFN-gamma axis during Anaplasma phagocytophilum infection. J. Immunol. 2007;179:4783–4791. doi: 10.4049/jimmunol.179.7.4783. [DOI] [PubMed] [Google Scholar]
- 40.Niu H., Xiong Q., Yamamoto A., Hayashi-Nishino M., Rikihisa Y. Autophagosomes induced by a bacterial Beclin 1 binding protein facilitate obligatory intracellular infection. Proc. Natl. Acad. Sci. USA. 2012;109:20800–20807. doi: 10.1073/pnas.1218674109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pedra J.H.F., Mattner J., Tao J., Kerfoot S.M., Davis R.J., Flavell R.A., Askenase P.W., Yin Z., Fikrig E. c-Jun NH2-terminal kinase 2 inhibits gamma interferon production during Anaplasma phagocytophilum infection. Infect. Immun. 2008;76:308–316. doi: 10.1128/IAI.00599-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kolbert C.P., Bruinsma E.S., Abdulkarim A.S., Hofmeister E.K., Tompkins R.B., Telford S.R., III, Mitchell P.D., Adams-Stich J., Persing D.H. Characterization of an immunoreactive protein from the agent of human granulocytic ehrlichiosis. J. Clin. Microbiol. 1997;35:1172–1178. doi: 10.1128/jcm.35.5.1172-1178.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ravyn M.D., Lamb L.J., Jemmerson R., Goodman J.L., Johnson R.C. Characterization of monoclonal antibodies to an immunodominant protein of the etiologic agent of human granulocytic ehrlichiosis. Am. J. Trop. Med. Hyg. 1999;61:171–176. doi: 10.4269/ajtmh.1999.61.171. [DOI] [PubMed] [Google Scholar]
- 44.Kim H.Y., Rikihisa Y. Characterization of monoclonal antibodies to the 44-kilodalton major outer membrane protein of the human granulocytic ehrlichiosis agent. J. Clin. Microbiol. 1998;36:3278–3284. doi: 10.1128/jcm.36.11.3278-3284.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Holden K., Hodzic E., Feng S., Freet K.J., Lefebvre R.B., Barthold S.W. Coinfection with Anaplasma phagocytophilum alters Borrelia burgdorferi population distribution in C3H/HeN mice. Infect. Immun. 2005;73:3440–3444. doi: 10.1128/IAI.73.6.3440-3444.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thomas V., Anguita J., Barthold S.W., Fikrig E. Coinfection with Borrelia burgdorferi and the agent of human granulocytic ehrlichiosis alters murine immune responses, pathogen burden, and severity of Lyme arthritis. Infect. Immun. 2001;69:3359–3371. doi: 10.1128/IAI.69.5.3359-3371.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Banerjee R., Anguita J., Roos D., Fikrig E. Cutting edge: Infection by the agent of human granulocytic ehrlichiosis prevents the respiratory burst by down-regulating gp91phox. J. Immunol. 2000;164:3946–3949. doi: 10.4049/jimmunol.164.8.3946. [DOI] [PubMed] [Google Scholar]
- 48.Scorpio D.G., Akkoyunlu M., Fikrig E., Dumler J.S. CXCR2 blockade influences Anaplasma phagocytophilum propagation but not histopathology in the mouse model of human granulocytic anaplasmosis. Clin. Diagn. Lab. Immunol. 2004;11:963–968. doi: 10.1128/CDLI.11.5.963-968.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bunnell J.E., Trigiani E.R., Srinivas S.R., Dumler J.S. Development and distribution of pathologic lesions are related to immune status and tissue deposition of human granulocytic ehrlichiosis agent-infected cells in a murine model system. J. Infect. Dis. 1999;180:546–550. doi: 10.1086/314902. [DOI] [PubMed] [Google Scholar]
- 50.Teglas M.B., Foley J. Differences in the transmissibility of two Anaplasma phagocytophilum strains by the North American tick vector species, Ixodes pacificus and Ixodes scapularis (Acari: Ixodidae) Exp. Appl. Acarol. 2006;38:47–58. doi: 10.1007/s10493-005-5293-5. [DOI] [PubMed] [Google Scholar]
- 51.Ijdo J.W., Wu C., Telford Iii S.R., Fikrig E. Differential expression of the p44 gene family in the agent of human granulocytic ehrlichiosis. Infect. Immun. 2002;70:5295–5298. doi: 10.1128/IAI.70.9.5295-5298.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Choi K.-S., Webb T., Oelke M., Scorpio D.G., Dumler J.S. Differential innate immune cell activation and proinflammatory response in Anaplasma phagocytophilum infection. Infect. Immun. 2007;75:3124–3130. doi: 10.1128/IAI.00098-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johns J.L., Borjesson D.L. Downregulation of CXCL12 signaling and altered hematopoietic stem and progenitor cell trafficking in a murine model of acute Anaplasma phagocytophilum infection. Innate Immun. 2012;18:418–428. doi: 10.1177/1753425911413794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ijdo J.W., Zhang Y., Hodzic E., Magnarelli L.A., Wilson M.L., Telford S.R., Barthold S.W., Fikrig E. The early humoral response in human granulocytic ehrlichiosis. J. Infect. Dis. 1997;176:687–692. doi: 10.1086/514091. [DOI] [PubMed] [Google Scholar]
- 55.Carlyon J.A., Ryan D., Archer K., Fikrig E. Effects of Anaplasma phagocytophilum on host cell ferritin mrna and protein levels. Infect. Immun. 2005;73:7629–7636. doi: 10.1128/IAI.73.11.7629-7636.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Birkner K., Steiner B., Rinkler C., Kern Y., Aichele P., Bogdan C., von Loewenich F.D. The elimination of Anaplasma phagocytophilum requires CD4+ T cells, but is independent of Th1 cytokines and a wide spectrum of effector mechanisms. Eur. J. Immunol. 2008;38:3395–3410. doi: 10.1002/eji.200838615. [DOI] [PubMed] [Google Scholar]
- 57.Lin Q., Rikihisa Y. Establishment of cloned Anaplasma phagocytophilum and analysis of p44 gene conversion within an infected horse and infected SCID mice. Infect. Immun. 2005;73:5106–5114. doi: 10.1128/IAI.73.8.5106-5114.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Blas-Machado U., de la Fuente J., Blouin E.F., Almazan C., Kocan K.M., Mysore J.V. Experimental infection of C3H/HeJ mice with the NY18 isolate of Anaplasma phagocytophilum. Vet. Pathol. 2007;44:64–73. doi: 10.1354/vp.44-1-64. [DOI] [PubMed] [Google Scholar]
- 59.Akkoyunlu M., Malawista S.E., Anguita J., Fikrig E. Exploitation of interleukin-8-induced neutrophil chemotaxis by the agent of human granulocytic ehrlichiosis. Infect. Immun. 2001;69:5577–5588. doi: 10.1128/IAI.69.9.5577-5588.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Banerjee R., Anguita J., Fikrig E. Granulocytic ehrlichiosis in mice deficient in phagocyte oxidase or inducible nitric oxide synthase. Infect. Immun. 2000;68:4361–4362. doi: 10.1128/IAI.68.7.4361-4362.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Xiong Q., Wang X., Rikihisa Y. High-cholesterol diet facilitates Anaplasma phagocytophilum infection and up-regulates macrophage inflammatory protein-2 and CXCR2 expression in apolipoprotein e-deficient mice. J. Infect. Dis. 2007;195:1497–1503. doi: 10.1086/514819. [DOI] [PubMed] [Google Scholar]
- 62.Pedra J.H., Tao J., Sutterwala F.S., Sukumaran B., Berliner N., Bockenstedt L.K., Flavell R.A., Yin Z., Fikrig E. IL-12/23p40-dependent clearance of Anaplasma phagocytophilum in the murine model of human anaplasmosis. FEMS Immunol. Med. Microbiol. 2007;50:401–410. doi: 10.1111/j.1574-695X.2007.00270.x. [DOI] [PubMed] [Google Scholar]
- 63.Bunnell J.E., Magnarelli L.A., Dumler J.S. Infection of laboratory mice with the human granulocytic ehrlichiosis agent does not induce antibodies to diagnostically significant Borrelia burgdorferi antigens. J. Clin. Microbiol. 1999;37:2077–2079. doi: 10.1128/jcm.37.6.2077-2079.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Johns J.L., MacNamara K.C., Walker N.J., Winslow G.M., Borjesson D.L. Infection with Anaplasma phagocytophilum induces multilineage alterations in hematopoietic progenitor cells and peripheral blood cells. Infect. Immun. 2009;77:4070–4080. doi: 10.1128/IAI.00570-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Johns J.L., Discipulo M.L., Koehne A.L., Moorhead K.A., Nagamine C.M. Influence of genetic background on hematologic and histopathologic alterations during acute granulocytic anaplasmosis in 129/SvEv and C57BL/6J mice lacking type I and type II interferon signaling. Comp. Med. 2017;67:127–137. [PMC free article] [PubMed] [Google Scholar]
- 66.Scorpio D.G., von Loewenich F.D., Göbel H., Bogdan C., Dumler J.S. Innate immune response to Anaplasma phagocytophilum contributes to hepatic injury. Clin. Vaccin. Immunol. 2006;13:806–809. doi: 10.1128/CVI.00092-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Herron M.J., Ericson M.E., Kurtti T.J., Munderloh U.G. The interactions of Anaplasma phagocytophilum, endothelial cells, and human neutrophils. Ann. N. Y. Acad. Sci. 2005;1063:374–382. doi: 10.1196/annals.1355.090. [DOI] [PubMed] [Google Scholar]
- 68.Wang T., Akkoyunlu M., Banerjee R., Fikrig E. Interferon-γ deficiency reveals that 129Sv mice are inherently more susceptible to Anaplasma phagocytophilum than C57BL/6 mice. FEMS Immunol. Med. Microbiol. 2004;42:299–305. doi: 10.1016/j.femsim.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 69.Sukumaran B., Narasimhan S., Anderson J.F., DePonte K., Marcantonio N., Krishnan M.N., Fish D., Telford S.R., Kantor F.S., Fikrig E. An Ixodes scapularis protein required for survival of Anaplasma phagocytophilum in tick salivary glands. J. Exp. Med. 2006;203:1507–1517. doi: 10.1084/jem.20060208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Borjesson D.L., Simon S.I., Hodzic E., Ballantyne C.M., Barthold S.W. Kinetics of CD11b/CD18 up-regulation during infection with the agent of human granulocytic ehrlichiosis in mice. Lab. Investig. 2002;82:303–311. doi: 10.1038/labinvest.3780424. [DOI] [PubMed] [Google Scholar]
- 71.Martin M.E., Bunnell J.E., Dumler J.S. Pathology, immunohistology, and cytokine responses in early phases of human granulocytic ehrlichiosis in a murine model. J. Infect. Dis. 2000;181:374–378. doi: 10.1086/315206. [DOI] [PubMed] [Google Scholar]
- 72.Mastronunzio J.E., Kurscheid S., Fikrig E. Postgenomic analyses reveal development of infectious Anaplasma phagocytophilum during transmission from ticks to mice. J. Bacteriol. 2012;194:2238–2247. doi: 10.1128/JB.06791-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sukumaran B., Ogura Y., Pedra J.H., Kobayashi K.S., Flavell R.A., Fikrig E. Receptor interacting protein-2 contributes to host defense against Anaplasma phagocytophilum infection. FEMS Immunol. Med. Microbiol. 2012;66:211–219. doi: 10.1111/j.1574-695X.2012.01001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Levin M.L., Coble D.J., Ross D.E. Reinfection with Anaplasma phagocytophilum in BALB/c mice and cross-protection between two sympatric isolates. Infect. Immun. 2004;72:4723–4730. doi: 10.1128/IAI.72.8.4723-4730.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Browning M.D., Garyu J.W., Dumler J.S., Scorpio D.G. Role of reactive nitrogen species in development of hepatic injury in a C57bl/6 mouse model of human granulocytic anaplasmosis. Comp. Med. 2006;56:55–62. [PubMed] [Google Scholar]
- 76.Borjesson D.L., Simon S.I., Hodzic E., DeCock H.E., Ballantyne C.M., Barthold S.W. Roles of neutrophil beta 2 integrins in kinetics of bacteremia, extravasation, and tick acquisition of Anaplasma phagocytophila in mice. Blood. 2003;101:3257–3264. doi: 10.1182/blood-2002-04-1019. [DOI] [PubMed] [Google Scholar]
- 77.Felek S., Telford S., III, Falco R.C., Rikihisa Y. Sequence analysis of p44 homologs expressed by Anaplasma phagocytophilum in infected ticks feeding on naive hosts and in mice infected by tick attachment. Infect. Immun. 2004;72:659–666. doi: 10.1128/IAI.72.2.659-666.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Scorpio D.G., Leutenegger C., Berger J., Barat N., Madigan J.E., Dumler J.S. Sequential analysis of Anaplasma phagocytophilum msp2 transcription in murine and equine models of human granulocytic anaplasmosis. Clin. Vaccine Immunol. 2008;15:418–424. doi: 10.1128/CVI.00417-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Choi K.-S., Scorpio D.G., Dumler J.S. Stat1 negatively regulates immune-mediated injury with Anaplasma phagocytophilum infection. J. Immunol. 2014;193:5088–5098. doi: 10.4049/jimmunol.1401381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang T., Malawista S.E., Pal U., Grey M., Meek J., Akkoyunlu M., Thomas V., Fikrig E. Superoxide anion production during Anaplasma phagocytophila infection. J. Infect. Dis. 2002;186:274–280. doi: 10.1086/341451. [DOI] [PubMed] [Google Scholar]
- 81.Zeidner N.S., Massung R.F., Dolan M.C., Dadey E., Gabitzsch E., Dietrich G., Levin M.L. A sustained-release formulation of doxycycline hyclate (Atridox) prevents simultaneous infection of Anaplasma phagocytophilum and Borrelia burgdorferi transmitted by tick bite. Pt 4J. Med. Microbiol. 2008;57:463–468. doi: 10.1099/jmm.0.47535-0. [DOI] [PubMed] [Google Scholar]
- 82.Borjesson D.L., Simon S.I., Tablin F., Barthold S.W. Thrombocytopenia in a mouse model of human granulocytic ehrlichiosis. J. Infect. Dis. 2001;184:1475–1479. doi: 10.1086/324518. [DOI] [PubMed] [Google Scholar]
- 83.Zhi N., Ohashi N., Tajima T., Mott J., Stich R.W., Grover D., Telford S.R., III, Lin Q., Rikihisa Y. Transcript heterogeneity of the p44 multigene family in a human granulocytic ehrlichiosis agent transmitted by ticks. Infect. Immun. 2002;70:1175–1184. doi: 10.1128/IAI.70.3.1175-1184.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Martin M.E., Caspersen K., Dumler J.S. Immunopathology and ehrlichial propagation are regulated by interferon-gamma and interleukin-10 in a murine model of human granulocytic ehrlichiosis. Am. J. Pathol. 2001;158:1881–1888. doi: 10.1016/S0002-9440(10)64145-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Akkoyunlu M., Fikrig E. Gamma interferon dominates the murine cytokine response to the agent of human granulocytic ehrlichiosis and helps to control the degree of early rickettsemia. Infect. Immun. 2000;68:1827–1833. doi: 10.1128/IAI.68.4.1827-1833.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lin M., Rikihisa Y. Ehrlichia chaffeensis and Anaplasma phagocytophilum lack genes for lipid A biosynthesis and incorporate cholesterol for their survival. Infect. Immun. 2003;71:5324–5331. doi: 10.1128/IAI.71.9.5324-5331.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xiong Q., Rikihisa Y. Subversion of NPC1 pathway of cholesterol transport by Anaplasma phagocytophilum. Cell. Microbiol. 2012;14:560–576. doi: 10.1111/j.1462-5822.2011.01742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xiong Q., Lin M., Rikihisa Y. Cholesterol-dependent Anaplasma phagocytophilum exploits the low-density lipoprotein uptake pathway. PLoS Pathog. 2009;5:e1000329. doi: 10.1371/journal.ppat.1000329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 90.Klein S.L. Sex influences immune responses to viruses, and efficacy of prophylaxis and treatments for viral diseases. Bioessays. 2012;34:1050–1059. doi: 10.1002/bies.201200099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pinzan C.F., Ruas L.P., Casabona-Fortunato A.S., Carvalho F.C., Roque-Barreira M.C. Immunological basis for the gender differences in murine Paracoccidioides brasiliensis infection. PLoS ONE. 2010;5:e10757. doi: 10.1371/journal.pone.0010757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Villacres M.C., Longmate J., Auge C., Diamond D.J. Predominant type 1 CMV-specific memory T-helper response in humans: Evidence for gender differences in cytokine secretion. Hum. Immunol. 2004;65:476–485. doi: 10.1016/j.humimm.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 93.Zhang M.A., Rego D., Moshkova M., Kebir H., Chruscinski A., Nguyen H., Akkermann R., Stanczyk F.Z., Prat A., Steinman L., et al. Peroxisome proliferator-activated receptor (PPAR) alpha and -gamma regulate IFNgamma and IL-17A production by human T cells in a sex-specific way. Proc. Natl. Acad. Sci. USA. 2012;109:9505–9510. doi: 10.1073/pnas.1118458109. [DOI] [PMC free article] [PubMed] [Google Scholar]