Abstract
A research team from Boston Children's Hospital and Harvard Medical School conducted a community-based feeding study in collaboration with Framingham State University (FSU) and Sodexo, the food service contractor at FSU. The study was a randomized controlled trial, implemented on the FSU campus. For the final year of the study, a satellite feeding site was established at Assabet Valley Regional Technical High School. The purpose of the study was to assess the biological effects of different macronutrient diets. An academia-industry partnership was developed to overcome common challenges associated with hospital-based feeding studies. Benefits included the following: a study site outside of Boston (reducing inconvenience for participants), access to a large commercial kitchen and study-specific kiosk (promoting efficiency), collaboration with Sodexo chefs (ensuring palatability of meals), and opportunity to procure food from contracted vendors. The research (academia) and food service (industry) teams worked together to design, plan, and execute intervention protocols using an integrated approach. During execution, the research team was primarily responsible for overseeing treatment fidelity, whereas the food service team provided culinary expertise, with a strong focus on hospitality and food quality. The study was conducted in 3 cohorts between August 2014 and May 2017. Participants received all of their food for ∼30 wk, totaling >160,000 meals. For all 3 cohorts combined, 234 participants provided informed consent, 229 started a standard run-in weight-loss diet, 164 lost a mean ± SD 12% ± 2% of baseline body weight and were randomly assigned to different macronutrient diets for weight-loss maintenance, and 148 completed the study. During the final and largest cohort, as many as 114 participants received daily meals concurrently. The daily cost per participant for preparation and service of weighed meals and snacks was ∼$65. This academia-industry partnership provides a model for controlled feeding protocols in nutrition research, potentially with enhanced cost-effectiveness, practicality, and generalizability. This trial was registered at http://www.clinicaltrials.gov as NCT02068885.
Keywords: dietary intervention, different macronutrient diets, feeding protocol, meal service, randomized controlled trial, research partnership, treatment fidelity
Introduction
Data from randomized controlled trials are arguably the strongest level of evidence for developing dietary recommendations (1, 2). A systematic approach to addressing a nutrition research question begins with explanatory (efficacy) trials to test hypotheses pertaining to biological mechanisms and culminates with pragmatic (effectiveness) trials (1, 3). Explanatory trials are conducted under ideal conditions to minimize the likelihood of confounding and thus have high internal validity, whereas pragmatic trials have high external validity or generalizability to real-world settings.
Very few dietary intervention trials are entirely explanatory or pragmatic, and steps along the study design continuum are not well defined for nutrition research (as compared, for example, with standardized phases for pharmaceutical research). Careful attention to study design is imperative when interpreting results from a completed trial or aligning methods with specific aims for a new trial. The scientific literature on the impact of different macronutrient diets provides a case in point on interpreting results. A much-debated question focuses on whether biological adaptations, elicited by different macronutrient diets, influence long-term weight-loss maintenance. Small short-term feeding studies conducted in metabolic wards, to maximize internal validity, provide information on acute biological responses (4) but may be irrelevant when questioning long-term effects. Conversely, long-term studies that rely on psycho-educational intervention strategies provide generalizable data but often lack adequate dietary adherence to draw strong conclusions with regard to biological adaptations (5–7).
In this context, an academia-industry partnership was developed to design, plan, and execute a feeding protocol in a community-based trial. The purpose of the trial was to assess biological effects of different macronutrient diets with the use of an intervention approach that can be applied when addressing other nutrition research questions. Through the partnership, participants received all of their food freshly prepared for a full academic year (∼30 wk), thereby increasing sample size and extending intervention duration beyond what is feasible in metabolic wards and promoting adherence beyond what can be expected when relying solely on psycho-educational intervention strategies. In this research methodology article, we first describe the benefits of the academia-industry partnership and integrated execution of feeding protocols. Then, we take a step back and describe how the research (academia) and food service (industry) teams collaborated to design different macronutrient diets, establish infrastructure for food preparation and meal service, and develop systems for tracking meals, monitoring adherence, and participant support.
Methods
Methodologic details for the overall study are presented in a previous protocol article (8). Participants were aged 18–65 y with a BMI (kg/m2) ≥25. A run-in phase was designed to promote weight loss corresponding to 12% ± 2% (mean ± SD) of baseline body weight over 9–10 wk with a standard diet (60% of estimated energy needs; 45% of energy from carbohydrate, 30% from fat, 25% from protein), and then weight stabilization (100% of estimated energy needs, same macronutrient composition) for ≥2 wk. Participants achieving ≥10% weight loss were randomly assigned to 1 of 3 different macronutrient diets (described below) for a 20-wk test phase. The research team adjusted energy intake as needed to promote weight loss during the run-in phase and weight-loss maintenance (no more than ±2 kg deviation from the post–weight-loss anchor) during the test phase. The study was conducted between August 2014 and May 2017, with recruitment for each of 3 cohorts during the spring semester before the respective academic year (August–May) of study participation. All study protocols were approved by the Institutional Review Board at Boston Children's Hospital (BCH).
Treatment fidelity was a primary consideration and encompassed differentiation, consistency, and integrity (9). When planning the dietary interventions, focus was on developing protocols to achieve optimal differentiation (extent to which calculated diets were distinct, allowing meaningful comparisons between diets) and appropriate consistency (control across interventions when considering intake of certain nutrients, methods for preparing food and serving meals, and strategies for providing support to participants). Monitoring protocols were developed to ensure intervention integrity (extent to which dietary interventions were executed according to established protocols).
Benefits of the partnership
A research team from BCH and Harvard Medical School conducted the study in collaboration with Framingham State University (FSU), located 20 miles west of Boston, and Sodexo, the food service contractor at FSU. The study was known as the Framingham State Food Study [(FS)2]. An academia-industry partnership was developed to overcome common challenges associated with hospital-based feeding studies (10):
To reduce participant burden, the study was conducted in a metropolitan area outside of Boston, thereby eliminating inconvenience and frustration often associated with traveling to research facilities in the city on a daily basis.
To efficiently prepare and serve meals, the food service team used a well-equipped commercial kitchen and built a study-specific kiosk, known as the (FS)2 kitchen (described below).
To ensure production of fresh, visually appealing, and maximally palatable meals and snacks—while maintaining tight control over dietary composition—the research team worked closely with Sodexo chefs when calculating the diets.
To procure a wide variety of study foods and beverages, the food service team ordered products from contracted vendors, with particular attention to ensuring freshness and brand consistency so that nutrient profiles of provided meals and snacks reflected calculated menus.
For the final year of the study, a satellite site at Assabet Valley Regional Technical High School (AV), located 10 miles north of Framingham, was established to extend the reach of the partnership. Food was prepared in the school nutrition kitchen, and participants dined in restaurant space made available through the AV culinary arts and hospitality management program. To ensure consistency in menu cycles, nutrient profiles, and food quality between sites, a centralized food-procurement system was implemented by which Sodexo purchased food for distribution to AV.
Integrated execution of feeding protocols
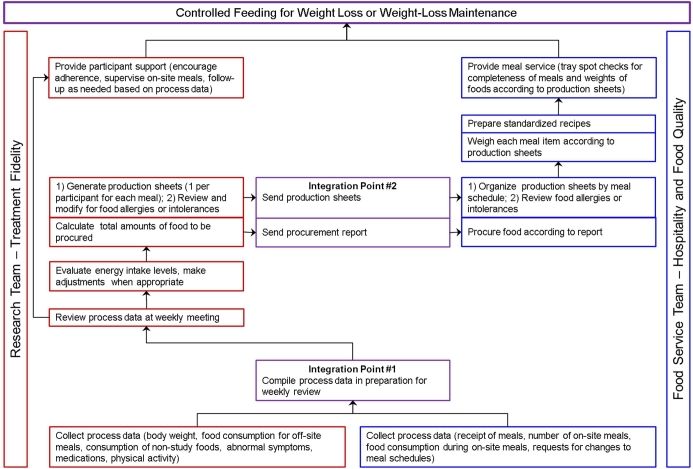
Figure 1 provides an overview of integration between the research and food service teams, highlighting distinct responsibilities and integration points. The research team primarily focused on treatment fidelity, whereas the food service team focused on hospitality and food quality. Daily collection and weekly compilation of process data by both teams was the foundation for integration. The research team reviewed process data, evaluated energy intake levels (and made adjustments when appropriate), calculated total amounts of foods to be procured, generated production sheets, and provided ongoing participant support. The procurement report and production sheets were sent to the food service team. In turn, the food service team procured food and organized production sheets, prepared recipes and weighed each menu item according to production sheets, and provided meal service. Integrated execution of controlled-feeding protocols ensured that participants received quality meals on different macronutrient diets at their prescribed energy intake levels.
FIGURE 1.
Integrated execution of feeding protocols.
Different macronutrient diets
Establishing macronutrient targets
The 3 diets were high-carbohydrate (60% of energy from carbohydrate, 20% from fat), moderate-carbohydrate (40% from carbohydrate, 40% from fat), and low-carbohydrate (20% from carbohydrate, 60% from fat) (8). Protein was held constant across diets at 20% of energy. Saturated fat was set at 35% of total fat, and added sugar was set at 15% of total carbohydrate. Total fiber content was consistent with recommendations from the Institute of Medicine (11) and reflected a gradient across the 3 diets (17.5, 15, and 12.5 g/1000 kcal with the high-, moderate-, and low-carbohydrate diets).
Retrieving Sodexo recipes and calculating diets
The food service team provided existing menus, used by FSU dining services, to the research team as a starting point for calculating diets. The research team also was given access to the corporate food management platform, which housed a proprietary library of additional standardized Sodexo recipes. Recipes were selected to reflect cuisines from different cultures, with consideration for the scope of food production systems and differentiation and consistency across diets. Ingredients in selected recipes were retrieved from a food service information technology system (CBORD; Ithaca, New York), which contained detailed information on weights, cooking and handling losses, and yields. These were entered into the (FS)2 recipe database, built with the use of Food Processor software (ESHA Research) and housed at BCH. The availability of specific brands, when needed to achieve nutrient targets, was confirmed via the campus food-procurement and production system. Recipe instructions were retrieved from the corporate food management platform. With the use of Food Processor software, dietitians on the research team calculated diets using standardized recipes, as much as possible, and other foods to meet nutrient targets.
The research team developed cycle menus for the 2 study phases. There were 42 meals (14 breakfasts, 14 lunches, and 14 dinners) and 14 snacks incorporated into three 1-wk-cycle menus during the run-in phase. Another 42 meals and 14 snacks for each of the different macronutrient diets, totaling 126 meals and 42 snacks, were incorporated into six 1-wk-cycle menus during the test phase. The Sodexo chefs reviewed menu cycles for appropriate meal variety and feasibility with food production systems. When dietitians on the research team made significant changes to recipes to meet nutrient targets, the recipes were tested by Sodexo chefs to ensure palatability and quality. The food service and research teams selected a subset of meals with each diet that were best suited for freezing, for use as emergency meals. Participants were provided with ≥2 sets of frozen emergency meals, according to their randomly assigned diet, that were consumed only under the direction of the study dietitians during extreme unexpected circumstances (e.g., snow days).
Because participants dined together, regardless of the diet to which they were randomly assigned, the research and food service teams worked together to make meal experiences similar. When possible, the same main dishes were used in differing portions, with addition of or reduction in food items to main dishes as well as side dishes, to maximize differentiation among diets. For example, the chicken burrito rice bowl in the high- and moderate-carbohydrate diets was replaced with a chicken burrito lettuce wrap in the low-carbohydrate diet (sample meal shown in Table 1). To achieve nutrient targets, common ingredients varied in the chicken burrito, with the addition of items to the burrito and side dishes, depending on the diet. As another example, pancakes made with wheat flour for participants assigned to the high- and moderate-carbohydrate diets were replaced with grain-free waffles made with chickpea flour for those assigned to the low-carbohydrate diet. Holiday meals were created to support maximum dietary adherence during special times of the year while maintaining nutrient targets of the different macronutrient diets (holiday meal shown in Table 1).
TABLE 1.
Example meals (per 2000-kcal/d menu)
| High-carbohydrate | Moderate-carbohydrate | Low-carbohydrate | |
|---|---|---|---|
| Sample meal | |||
| Main dish | Chicken burrito rice bowl: | Chicken burrito rice bowl: | Chicken burrito lettuce wrap: |
| Cilantro lime chicken, 91 g | Cilantro lime chicken, 91 g | Cilantro lime chicken, 64 g | |
| Santa Fe black beans, 70 g | Santa Fe black beans, 80 g | Santa Fe black beans, 70 g | |
| Salt (for chicken and beans), 0.4 g | |||
| Mild chunky salsa, 25 g | Mild chunky salsa, 25 g | Mild chunky salsa, 25 g | |
| Sour cream, 8 g | Sour cream, 20 g | Sour cream, 22 g | |
| Brown basmati rice, 145 g | Brown basmati rice, 115 g | ||
| Butter (salted, for rice), 4 g | Butter (salted, for rice), 5 g | ||
| Bibb lettuce, 30 g | |||
| Items added to main dish | Cheddar cheese (shredded), 20 g | Cheddar cheese (shredded), 38 g | |
| Guacamole, 29 g | Guacamole, 41 g | ||
| Cucumber (sliced), 30 g | |||
| Chipotle mayonnaise, 17 g | |||
| Sides | Fresh pineapple chunks, 204 g | Fresh pineapple chunks, 149 g | Fresh pineapple chunks, 55 g |
| Whole-wheat pita, 47 g | |||
| Milk (whole), 124 g | |||
| Holiday meal | |||
| Main dish | Classic roasted turkey, green beans, and mashed potatoes: | Classic roasted turkey, green beans, and mashed potatoes: | Classic roasted turkey, green beans, and mashed cauliflower “potatoes”: |
| Roasted turkey breast, 90 g | Roasted turkey breast, 122 g | Roasted turkey breast, 103 g | |
| Gravy, 15 g | Gravy, 20 g | Gravy, 27 g | |
| Whole green beans, 60 g | Whole green beans, 60 g | Whole green beans, 100 g | |
| Butter (salted, for green beans), 7 g | |||
| Mashed potatoes, 70 g | Mashed potatoes, 65 g | ||
| Mashed cauliflower, 110 g | |||
| Butter (salted, for potatoes), 12 g | Butter (salted, for cauliflower), 6 g | ||
| Whole-berry cranberry sauce, 26 g | Whole-berry cranberry sauce, 13 g | ||
| Dried cranberries, 21 g | |||
| Sides | Roasted butternut squash, 90 g | Roasted butternut squash, 60 g | |
| Bread stuffing, 34 g | Bread stuffing, 50 g | ||
| Greek yogurt (vanilla, nonfat), 70 g | |||
| Dessert | Pumpkin pie, 70 g | Pumpkin pie, 70 g | |
| Pumpkin custard, 60 g | |||
| Dark chocolate (70%), 14 g | |||
| Almonds (dry roasted), 15 g |
Classifying recipes
Recipes were classified as batch, breakdown, or point-of-service. Batch recipes were those with a homogenous distribution of ingredients, allowing high confidence in nutrient composition per gram weight of each portion. These recipes were prepared in bulk and weighed and portioned for each participant on the basis of their energy intake levels. Examples of batch recipes included herb grilled salmon and cauliflower soup. Breakdown recipes were those in which ingredients were not homogenously distributed across portions. These recipes were broken down into subrecipes to ensure that each participant received the targeted nutrients. For example, a marinated bean salad recipe was divided into 2 subrecipes: bean mixture and oil dressing. For each participant, the portions of beans and dressing were weighed and then combined to complete the salad. Point-of-service recipes were similar to breakdown recipes, but the final preparation was not completed until a participant arrived at mealtime. For example, a spinach and cheese omelet was divided into 3 subrecipes: spinach and mushroom mixture, cheese, and raw eggs. The portions of each subrecipe were weighed in advance, and the omelet was cooked at the (FS)2 kitchen.
Developing diet-specific unit bars
Recipes for three 100-kcal unit bars, matching the macronutrient composition of each test diet, were developed by the research team and then tested and reformulated in collaboration with Sodexo chefs from the food service team. The purpose of providing unit bars to certain participants was 2-fold: 1) to replace some of the meal calories, when large portions were a barrier to consuming all provided food, and thereby meet energy and nutrient targets, and 2) to immediately increase or decrease calories before an energy adjustment could be implemented by the food service team according to the cycles (described below), to achieve weight-loss maintenance (±2 kg of the post–weight-loss anchor weight).
Infrastructure for food preparation and meal service
The infrastructure for preparing food and meal service was designed for efficiency, quality control, and participant satisfaction and safety.
(FS)2 kitchen
Recognizing that additional space was needed for weighing menu items and point-of-service food preparation, the food service director worked closely with an architectural firm to conceptualize, design, and build the (FS)2 kitchen (Figure 2) on the basis of several considerations:
The study protocol mandated preparation and service of weighed meals and snacks on a daily basis at designated times, in compliance with intervention protocols and all public health regulations and codes.
The location and layout of the (FS)2 kitchen were based on the need for timely and efficient flow of operations (e.g., transporting food from the larger commercial kitchen, food and recipe preparation, meal assembly, participant check-in, meal service and pick-up, participant check-out and distribution of any take-out meals, weighing any leftover menu items to document participant adherence, transporting dirty wares to a cleaning and sanitation area).
Space for the (FS)2 kitchen was limited to 500 square feet to minimize impact on surrounding campus operations and infrastructure. The (FS)2 kitchen was built primarily off-site with only final assembly conducted on-site.
A wide range of cooking equipment was needed in a space without a commercial kitchen exhaust. Installation of electrical and plumbing services requiring structural changes or disruption to proximal foodservice platforms was not an option.
An open kitchen was designed to showcase culinary techniques, thereby offering transparency and generating interest in the study.
Capacity for point-of-service preparation of meals was necessary for some recipes to ensure optimal freshness and food quality.
A comfortable dining space around the (FS)2 kitchen, where participants could eat and socialize while adhering to randomly assigned diets, was important for participant satisfaction. A smaller (FS)2 kitchen was built for the AV satellite feeding site.
FIGURE 2.
Framingham State Food Study kitchen.
The (FS)2 kitchen was designed with the use of a food service solution, known as Food on Demand, in the Sodexo portfolio. Food on Demand has a mission to service smaller populations and produce restaurant-quality plated meals prepared on an individual rather than a bulk basis. It relies primarily on microconvection ovens, rather than usual commercial equipment, to re-thermalize food and finish meal preparation. Microconvection ovens provide the quick heating function of microwave ovens and roasting, grilling, and baking functions of conventional ovens. In addition to microconvection ovens and cookware (e.g., roasters, skillets, Dutch ovens, casseroles, stockpots), the (FS)2 kitchen was equipped with induction burners and a griddle for sautéing and searing, a commercial freezer and refrigerators, rolling racks for organizing trays, balances and scales for weighing recipe ingredients and portioning menu items, storage shelves, meal preparation tools (e.g., knives, spatulas, ladles, tongs), and a hand-washing sink. Much of the food preparation and meal assembly occurred before designated mealtimes, so that nutrition research assistants had uninterrupted time for weighing each menu item. Assembled meals were stored on trays in refrigerators until meal service.
Energy adjustment cycles
Three-week cycles were developed for adjusting energy intake levels to achieve weight loss (run-in phase) or weight-loss maintenance (test phase). During the first 2 wk of the cycle, the research team monitored body weight using Wi-Fi scales (see below) and then transferred daily weight data to a SAS data set (SAS Institute, Inc.) for systematically identifying participants who needed an energy adjustment. During the third week of the cycle, the research team calculated energy adjustments and the food service team implemented the adjustments for the next 3-wk cycle, according to production sheets. For the run-in phase, the research team made adjustments to achieve weight loss equating to 12% ± 2% of baseline body weight over 9–10 wk. For the test phase, the research team regressed weight on time over 14 d and made an energy adjustment to achieve weight-loss maintenance when the slope of the line was ≥15 g/d and/or body weight was not within ±2 kg of the post–weight-loss anchor weight. Meal production sheets, generated by the research team using SAS, indicated exact amounts of each food for individual participants to achieve appropriate energy intake levels. The food service team procured food on the basis of total amounts, automatically calculated from production sheets, for cohorts of participants.
Quality control of assembled meals
Nutrition research assistants were instructed to weigh menu items within narrow tolerance limits (±0.1 g of the target weight for items ≤10 g and ±0.5 g for items >10 g). Real-time quality control of menu items before meal service or pick-up involved checking actual weights, compared with target weights indicated on production sheets, for assembled meals selected at random (spot weight checks, 3 d/wk, 2–4 meals/d depending on cohort size). Additional random samples of take-out meals were checked for content (packaged menu item checks, 3 d/wk, 5–7 meals/d depending on cohort size). Any quality-control issues were addressed immediately.
System for managing food allergies, intolerances, and preferences
Before the start of the run-in and test diets, the research team reviewed all food allergies and intolerances reported by participants to generate a master list specifying participant names, menu items causing allergic reactions or food-intolerance symptoms, and substitute items. Additional SAS programming allowed for automatic substitution of menu items in production sheets, according to the master list, with items that maintained the macronutrient composition of the meal. The food service team reviewed each production sheet before food preparation and flagged any meal that contained a substitute menu item. The flag was an additional alert for food service staff to be extra vigilant. This system maximized participant safety, without compromising differentiation between diets.
Accommodation of most food allergies and intolerances was within the scope of the research protocol. However, peanut allergy was exclusionary due to the risk of cross-contamination. In addition, individuals with a gluten allergy or intolerance were not enrolled because all gluten-containing menu items could not be eliminated or substituted without significantly compromising differentiation between diets. Participants with lactose intolerance received lactose-free milk and instructions to take lactase pills at their own discretion with other dairy products.
Individual food preferences were assessed on a case-by-case basis. Vegetarianism was not accommodated, due to infeasibility of producing an additional menu for each of the 3 different macronutrient diets. However, one protein source [i.e., chicken, beef, pork, tofu, or seafood (fish or shellfish)] could be removed from the menu for any participant due to personal or religious beliefs.
Tracking, monitoring, and support
Participants were asked to eat ≥1 meal/d, Monday through Friday, in the dining area at FSU or AV. Electronic systems were used to track meals and monitor adherence. Data compiled from these systems provided prompts for supporting participants.
Tracking meals
Two systems were used for tracking receipt of meals, as follows:
The FSU photograph identification card system was used for participant check-in at the (FS)2 kitchen. Using this system, the food service team confirmed participant identity, tracked consumption of supervised on-site meals, and documented pick-up of unsupervised take-out meals.
A Quick Response Code (QRC) system was used to label trays for on-site meals and boxes for take-out meals. Color-coded labels were made using a label maker (Brady Corporation) for each diet, and each label specified participant name, menu cycle, day of the week, and meal (breakfast, lunch, dinner, snack). The QRC for each study meal received by a participant was scanned into a prepopulated meal-tracking file. Reports from both systems were generated at the end of each week and used by the research team to identify participants who needed support in adhering to study protocols (e.g., coming for required supervised on-site meals, pick-up of take-out meals) and by the food service team to identify any protocol deviations that could affect treatment fidelity (e.g., making sure that participants received the correct trays and take-out boxes).
Monitoring adherence
As noted previously (8), a study-specific online portal was developed for tracking adherence (SetPoint Health). The research team tracked body weight using Wi-Fi scales (Withings, Inc.), dietary intake, and information obtained from daily questionnaires. Participants were asked to weigh themselves in the morning, after getting out of bed and emptying their bladders, before breakfast. For supervised on-site meals at the (FS)2 kitchen, nutrition research assistants entered the weights of leftover menu items into the portal; for unsupervised take-out meals, participants were asked to record the proportion of each provided menu item consumed by using a form on the portal that was prepopulated a week in advance with daily menus from production sheets. Participants also were asked to complete questionnaires on the portal with regard to consumption of any nonstudy foods and beverages, abnormal symptoms, medications, and physical activity. Participants could view tables and graphs of real-time weight data and daily menus at any time.
The research team systematically reviewed data downloaded from the portal during weekly meetings. Large fluctuations in body weight, discrepancies between prescribed and actual energy intake levels (calculated by using a food and nutrient library in the portal), inability to consume all study foods, or consumption of nonstudy foods prompted follow-up by the research team. A study physician addressed abnormal symptoms and medication changes.
Participant support
Study dietitians on the research team built and maintained rapport with study participants to 1) encourage adherence, 2) supervise on-site meals, and 3) follow up as needed on the basis of review of weekly process data. Strategies used to encourage adherence included monthly group workshops, weekly educational handouts posted at the (FS)2 kitchen, personalized notes, and special activities during major holidays or events. Participants also received individualized quarterly progress reports detailing their weight loss or weight-loss maintenance (depending on study phase) and daily compliance with weighing themselves and providing self-report data via the study portal. The consistent presence of study dietitians at the (FS)2 kitchen allowed for open communication and direct observation of dietary intake during on-site meals. Individual follow-up sessions with regard to adherence issues were conducted in-person in a private space at FSU or AV, or by telephone, using a patient-centered counseling model (12).
Results and Discussion
An academia-industry partnership was successful for conducting a community-based feeding study. The partnership was built on a strong commitment from personnel at all levels of their career ladders. In addition to those engaged in developing logistical protocols and implementing the interventions, as described in Methods, study leaders from BCH (i.e., principal investigators, study director) and FSU (i.e., study director) provided oversight, and executive staff from Sodexo (i.e., product development director for wellness, dietitian for on-site service solutions, recipe/menu contractor) and FSU (i.e., provost/vice president of academic affairs, executive vice president) and AV (superintendent-director, director of business operations) were involved as needed to offer guidance, address challenges, and thereby promote success. The availability of a large on-site student population to fill per-diem nutrition research assistant positions and cover shifts at the (FS)2 kitchen was a benefit of conducting the study at FSU. Many students with an interest in nutrition and clinical research gained valuable work experience, some over multiple academic years.
Participant retention rates compared favorably with previous feeding studies. For all 3 cohorts combined, 234 participants provided informed consent, 229 started a standard run-in weight-loss diet, 164 lost 12% ± 2% of baseline body weight and were randomly assigned to different macronutrient diets for weight-loss maintenance, and 148 completed the study (8). As such, retention rates were 71.6% during the run-in phase (among those who started the run-in diet) and 90.2% during the test phase (among those who were randomly assigned). These rates are similar to those observed in a smaller hospital-based feeding study with a similar run-in phase (32 participants started, 75.0% retention) and a shorter test phase (3 different diets × 4 wk/diet, 24 participants randomly assigned, 87.5% retention) (10). Retention rates in multicenter crossover studies, with sample sizes similar to (FS)2, were 83.2% for 18 wk of feeding (3 different diets × 6 wk/diet, with 2–4 wk between diets, 191 participants randomly assigned) (13) and 71.4% for 20 wk of feeding (4 different diets × 5 wk/diet, with ≥2 wk between diets, 189 participants randomly assigned) (14).
General metrics on menu design and meal service provide insights on the scope of planning and operations. The meals comprised 130 individual standardized recipes of which 36 were unique to the run-in diet, 48 to the test diets, and 46 common among all diets. The recipes were classified as follows: 101 batch, 16 breakdown, and 13 point-of-service. More than 80% (n = 110) were Sodexo recipes. By the end of the study, >160,000 meals (including breakfasts, lunches, dinners, and snacks) were prepared and served at the (FS)2 kitchens. During the final and largest cohort, as many as 114 participants, across 2 sites (FSU, AV), received daily meals concurrently. The daily cost per participant for preparation and service of weighed meals and snacks for this cohort was ∼$65 (fiscal year 2017), including food, packaging of take-out meals, and labor (i.e., chefs, nutrition research assistants, dishwashers). This estimate compares favorably with posted rates for the provision of weighed meals from metabolic kitchens in clinical research centers (15–18). In Boston, for example, the daily cost per participant was $72 (3 meals, 1 snack) in fiscal year 2016 (18).
To monitor intervention integrity, spot weight checks and packaged menu item checks were conducted throughout the study. On the basis of data compiled during the final cohort at FSU, food service staff completed 95% and 97% of the intended spot weight and packaged menu item checks, respectively. For the completed spot weight checks, comparing actual weights with target weights, 67% of the menu items were within the narrow tolerance limits (±0.1 g of the target weight for items ≤10 g and ±0.5 g for items >10 g) and 98% were within ±5 g (a level of deviation that would not compromise macronutrient differentiation). Packaged menu item checks indicated that 99% of the take-out meals contained all of the intended menu items.
Direct observation of all meals and snacks provides the best measure of dietary adherence, often used for inpatient feeding studies of short duration (19, 20) but not feasible in this longer study in free-living participants. Thus, change in body weight was used as an objective indicator of adherence, rather than relying on self-report of dietary intake. Among 148 participants who completed the study, 110 achieved weight-loss maintenance within ±2 kg of the post–weight-loss anchor weight. For these participants, the mean ± SD change in body weight at the end of the study was −0.23 ± 1.00 kg, and the median (IQR) was −0.21 kg (−0.97, 0.33 kg), indicating a high level of adherence for a priori per-protocol analyses (8).
Access to standardized recipes and integration of food and nutrition platforms are important considerations for efficiency of workflow between research and food service teams. With support from Sodexo executive staff, the research team was privileged to have access to a proprietary library of standardized recipes. However, a method for integrating different platforms was not available, necessitating adaptation of available systems (Sodexo's corporate food management platform, CBORD food service information technology system, ESHA Food Processor software) to ensure success of the academia-industry partnership. Availability of compatible academia-industry platforms could enhance the efficiency of workflow between integrated research and food service teams.
In conclusion, the academia-industry partnership described herein provides a model for controlled-feeding studies in nutrition research. Some may argue that, even if a controlled feeding study provides interesting data to explain biological adaptations to dietary interventions, results are irrelevant if the interventions are not feasible in real-world settings. However, concerns about feasibility are premature without a clear understanding of biological adaptations. When interventions have beneficial biological effects in controlled-feeding studies, then researchers must address the challenges associated with implementation in real-world settings, recognizing that expanded perspectives on feasibility and changes to real-world settings may be prerequisites. Academia-industry partnerships for controlled-feeding studies may help to lay the foundation for trials aimed at evaluating generalizability.
Acknowledgments
The authors acknowledge Lisa Robinson, Nicole Chenard, and Kaitlyn Shannon (participant support, BCH); Kimberly Chin, Henry Feldman, and Carly Milliren (SAS programming, BCH); Sarah Steltz (quality control, BCH); Dale Hamel (executive vice president, FSU); Linda Vaden-Goad (vice president of academic affairs and provost, FSU); Beth Winthrop (product development director for wellness, Sodexo); Beth Olson (dietitian for on-site service solutions, Sodexo); Ann Zaleta (recipe/menu contractor, Sodexo); David Garufi, Renae Gauvin, and Carolyn Holland (food production and meal service, Sodexo); Darline Hughes, Eric Johnson, and Denise Stultz (executive chefs, Sodexo); Ernest F Houle (superintendent-director, AV); Kristopher Luoto (director of business operations, AV); Jon Thering (executive chef, AV); and Kelsey Viera (sous chef, AV). The authors’ responsibilities were as follows—JMWW, LB, DSL, and CBE: calculated different macronutrient diets; RGE: was the food service director and conceptualized the (FS)2 kitchen; LB and LS: managed and coordinated day-to-day implementation of the intervention; PRL: was the SAS programmer; MS: coordinated participant support; CD: coordinated remote participant monitoring; LS-S: provided participant support and reviewed production sheets; DW: was the food service director at AV; JMWW: was the associate study director; PKL and GLK: were the study directors; DSL and CBE: were the principal investigators and were responsible for the overall study design and implementation; JMWW and CBE: wrote the first draft of the manuscript; and all authors: contributed to writing the manuscript and read and approved the final manuscript.
Notes
Supported by grants from the Nutrition Science Initiative (made possible by gifts from the Laura and John Arnold Foundation and Robert Lloyd Corkin Charitable Foundation), New Balance Foundation, Many Voices Foundation, and Blue Cross Blue Shield. DSL was supported by a midcareer mentoring award from the National Institute of Diabetes and Digestive and Kidney Diseases (K24DK082730).
Author disclosures: JMWW, LB, LS, PRL, MS, CD, LS-S, DW, PKL, GLK, and CBE, no conflicts of interest. RGE is the director of dining services for Sodexo, Inc., a global for-profit provider of sustainable, integrated facilities management and food service operations; DSL has received royalties for books on obesity and nutrition. The funding organizations played no role in the design and conduct of the study; preparation of the manuscript; and decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Abbreviations used:
- AV
Assabet Valley Regional Technical High School
- BCH
Boston Children's Hospital
- (FS)2
Framingham State Food Study
- FSU
Framingham State University
- QRC
Quick Response Code
References
- 1. Stevens J, Taber DR, Murray DM, Ward DS. Advances and controversies in the design of obesity prevention trials. Obesity (Silver Spring) 2007;15:2163–70. [DOI] [PubMed] [Google Scholar]
- 2. Hebert JR, Frongillo EA, Adams SA, Turner-McGrievy GM, Hurley TG, Miller DR, Ockene IS. Perspective: randomized controlled trials are not a panacea for diet-related research. Adv Nutr 2016;7:423–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thorpe KE, Zwarenstein M, Oxman AD, Treweek S, Furberg CD, Altman DG, Tunis S, Bergel E, Harvey I, Magid DJ et al. , A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J Clin Epidemiol 2009;62:464–75. [DOI] [PubMed] [Google Scholar]
- 4. Hall KD, Guo J. Obesity energetics: body weight regulation and the effects of diet composition. Gastroenterology 2017;152:1718–27, e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA 2005;293:43–53. [DOI] [PubMed] [Google Scholar]
- 6. Alhassan S, Kim S, Bersamin A, King AC, Gardner CD. Dietary adherence and weight loss success among overweight women: results from the A to Z weight loss study. Int J Obes (Lond) 2008;32:985–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne CM, Bishop LM, Laranjo N et al. , Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009;360:859–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ebbeling CB, Klein GL, Luoto PK, Wong JMW, Bielak L, Eddy RG, Steltz SK, Devlin C, Sandman M, Hron B et al. , A randomized study of dietary composition during weight-loss maintenance: rationale, study design, intervention, and assessment. Contemp Clin Trials 2017;65:76–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moncher FJ, Prinz RJ. Treatment fidelity in outcome studies. Clin Psychol Rev 1991;11:247–66. [Google Scholar]
- 10. Ebbeling CB, Swain JF, Feldman HA, Wong WW, Hachey DL, Garcia-Lago E, Ludwig DS. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA 2012;307:2627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Institute of Medicine Dietary Reference Intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington (DC): National Academies Press; 2002. [DOI] [PubMed] [Google Scholar]
- 12. Rosal MC, Ebbeling CB, Lofgren I, Ockene JK, Ockene IS, Hebert JR. Facilitating dietary change: the patient-centered counseling model. J Am Diet Assoc 2001;101:332–41. [DOI] [PubMed] [Google Scholar]
- 13. Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER 3rd, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM et al. , Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 2005;294:2455–64. [DOI] [PubMed] [Google Scholar]
- 14. Sacks FM, Carey VJ, Anderson CA, Miller ER 3rd, Copeland T, Charleston J, Harshfield BJ, Laranjo N, McCarron P, Swain J et al. , Effects of high vs low glycemic index of dietary carbohydrate on cardiovascular disease risk factors and insulin sensitivity: the OmniCarb randomized clinical trial. JAMA 2014;312:2531–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Colorado Clinical and Translational Sciences Institute, University of Colorado Denver Nutrition services pricing [Internet]. [cited 2018 Feb 26]. Available from: http://www.ucdenver.edu/research/CCTSI/programs-services/ctrc/Pages/Nutrition-Pricing.aspx. [Google Scholar]
- 16. Institute for Translational Medicine, University of Chicago Clinical Research Center (CRC) service rates [Internet]. [cited 2018 Feb 26]. Available from: https://itm.uchicago.edu/wp-content/uploads/2016/02/CRC-Rates-June-2014-May-2015_updated5.pdf. [Google Scholar]
- 17. Nutrition Obesity Research Center, University of Michigan Core services: human phenotyping: Nutrition Assessment Laboratory [Internet]. [cited 2018 Feb 26]. Available from: http://mmoc.med.umich.edu/CoreHP_NAL.php. [Google Scholar]
- 18. Center for Clinical Investigation, Brigham and Women's Hospital CCI Research Operations Service Support (CROSS) core FY16 rates [Internet]. [cited 2018 Jun 4]. Available from: https://www.brighamandwomens.org/assets/BWH/research/pdfs/fy16-cci-cross-core-rates.pdf. [Google Scholar]
- 19. Botero D, Ebbeling CB, Blumberg JB, Ribaya-Mercado JD, Creager MA, Swain JF, Feldman HA, Ludwig DS. Acute effects of dietary glycemic index on antioxidant capacity in a nutrient-controlled feeding study. Obesity (Silver Spring) 2009;17:1664–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hall KD, Chen KY, Guo J, Lam YY, Leibel RL, Mayer LE, Reitman ML, Rosenbaum M, Smith SR, Walsh BT et al. , Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am J Clin Nutr 2016;104:324–33. [DOI] [PMC free article] [PubMed] [Google Scholar]