Abstract
Objective
Although numerous studies address the relationships of depression with coping processes directed toward approaching or avoiding stressful experiences, the large majority are cross-sectional in design, assess coping processes at only one timepoint, or solely include prediction of the linear slope of depressive symptoms. In this research, coping processes were investigated as predictors of depressive symptoms, symptom trajectory classes (consistently high, recovery, consistently low), and major depressive episodes (MDEs) over 12 months in the cancer context.
Method
Women (N = 460) within four months of breast cancer diagnosis completed assessments of cancer-related coping processes, depressive symptoms, and MDEs at seven points across one year.
Results
Beyond sociodemographic and medical variables, coping through cancer-related avoidance an average of two months after diagnosis was associated with likelihood of being in the high depressive symptom trajectory class and occurrence of a MDE during the year. Less decline in avoidant coping over time also predicted poor outcomes. In contrast, high initial engagement in approach-oriented coping, as well as increases in coping through emotional expression and acceptance, were associated with lower depressive symptoms across assessments and higher likelihood of being in the recovery or low trajectory class.
Conclusions
Greater engagement in cancer-related avoidant coping was associated with all three indicators of depression, and greater approach-oriented coping was related to more favorable outcomes (except MDE). Sustained or increasing coping through emotional expression or acceptance predicted recovery from initially high depressive symptoms. Approach- and avoidance-oriented coping processes constitute malleable targets for preventive and ameliorative approaches.
Keywords: Depression, Cancer, Coping, Trajectory, Major Depressive Disorder
Across a variety of profoundly stressful experiences, most adults do not evidence severe and enduring psychological compromise. Rather, they demonstrate either sustained psychological health or recovery over time from initial disruption (Bonanno, Westphal, & Mancini, 2011). A sizeable group of affected adults evidences elevated depressive symptoms and MDEs, however, as well as a host of other negative consequences (e.g., Hammen, 2016). A large literature has addressed the role of coping in protection from or exacerbation of depression after stressful experiences. A paucity of research, however, interrogates coping processes and their trajectories over time as predictors of depressive symptoms and disorder in longitudinal designs. Accordingly, the primary goal of this study was to identify predictors of depressive symptoms, distinct depressive symptom trajectory classes, and MDEs across 12 months starting shortly after the onset of the potentially life-threatening diagnosis of breast cancer.
Depression in Adults Diagnosed with Cancer
As demonstrated in prospective research, the diagnosis and treatment of breast cancer (Jones et al., 2015; Suppli et al., 2014) and other cancers (e.g., Lu et al., 2016) prompt elevations in depressive symptoms and MDEs. Assessed with validated interview, the MDE prevalence via meta-analysis is estimated to be 16.3% in cancer patients, with no significant difference in prevalence for adults with breast versus other cancers (Mitchell et al., 2011). In the first findings from the present study (Stanton et al., 2015), 16.6% of 460 women recently diagnosed with breast cancer had a MDE in the next year, twice that of the 8.4% 12-month major depressive disorder prevalence in the US estimated via the same diagnostic interview (Substance Abuse and Mental Health Services Administration, 2013). Most (56%) were first episodes, consistent with population-based cohort studies showing increased risk for new-onset MDEs after cancer diagnosis (Lu et al., 2016; Suppli et al., 2014). In addition, 57% of women had a Center for Epidemiologic Studies Depression Scale (CES-D) score of at least 16, a clinically meaningful threshold (Lewinsohn, Seeley, Roberts, & Allen, 1997; Radloff, 1977), at one or more of seven assessments over the year.
Regarding change in depressive symptoms, CES-D scores on average declined over time. However, latent growth curve analyses estimated distinct trajectories: 38% of women evidenced persistently high depressive symptoms, 20% recovered from initially elevated symptoms, and 43% had consistently low symptoms over 12 months (Stanton et al., 2015). These trajectories converge with patterns of psychological adjustment following a range of major stressors (less reliably, a “delayed” impairment trajectory is observed; Bonanno et al., 2011; Henselmans et al., 2010).
Not only are they painful and impairing in their own right, but elevated depressive symptoms and MDEs in cancer survivors also are linked to poor medical regimen adherence and unhealthy behaviors (DiMatteo, Giordani, Lepper, & Croghan, 2002; Holden, Ramirez, & Gallion, 2014), delayed return to work (Steiner et al., 2008), and higher healthcare use, costs, and depression-associated hospitalizations (Dalton, Laursen, Ross, Mortensen, & Johansen, 2009; Goldstein et al., 2012). Cancer survivors’ suicide risk exceeds that of the general population (Fang et al., 2012). Persistently high depressive symptoms also predict lower survival from serious diseases including cancer, for which plausible biobehavioral mediators exist (Cuijpers et al., 2014). Such grave consequences demand the identification of potentially malleable protective and harmful factors that predict depressive outcomes. In light of the surprisingly small evidence base regarding interventions for depression in adults with breast and other cancers (Fann et al., 2008; Hart et al., 2012; Li et al., 2017), such research is vital to the development of effective and efficient approaches to prevent and treat depression for the projected 20 million people living with a cancer diagnosis by the year 2026 in the United States (Miller et al., 2016). The selection of women recently diagnosed with breast cancer to compose the sample stemmed from that disease being the most commonly diagnosed cancer worldwide (World Health Organization, 2018) and the elevated risk for depression and life disruption in that group, particularly within the first year or more after diagnosis and treatment (e.g., Fann et al., 2008; Fiszer, Dolbeault, Sultan, & Brédart, 2014).
Coping Processes as Contributors to Depression after a Cancer Diagnosis
Defined as cognitive, behavioral, and emotional efforts to manage demands perceived as taxing or exceeding a person’s resources (Lazarus & Folkman, 1984; Stanton, Kirk, Cameron, & Danoff-Burg, 2000), coping processes are classified in a number of ways (Compas et al., 2017; Lazarus & Folkman, 1984; Roth & Cohen, 1986; Skinner, Edge, Altman, & Sherwood, 2003). One central conceptualization involves their approach- and avoidance-oriented functions. These functions align with basic motivational systems in humans and other animals (Davidson, Jackson, & Kalin, 2000), are supported in hierarchical factor analyses of items to assess coping (Tobin, Holroyd, Reynolds, & Wigal, 1989), and are related to psychological and physical health in individuals undergoing major stressors (Compas et al., 2017; Duangdao & Roesch, 2008; Kvillemo & Bränström, 2014; Moskowitz, Hult, Bussolari, & Acree, 2009; Roesch et al., 2005).
Continued investigation of coping domains and their constituent processes is vital because, to date, their relations with important outcomes primarily are examined in cross-sectional studies rather than research that allows stronger causal inference (Kvillemo & Bränström, 2014; Moskowitz et al., 2009); hence, the ability of coping processes to predict subsequent outcomes and their stability or change across time in relation to outcomes require study. Moreover, coping processes constitute potentially malleable targets of intervention to enhance well-being and health (Greer et al., 2018; Low, Stanton, & Bower, 2008). This study addressed the novel and clinically-important question of whether both initial coping efforts and sustained or increasing coping attempts across time could distinguish women who recovered from elevated depressive symptoms from those who did not.
Indicators of Depression in the Present Study
In this study, a first indicator of depression was a continuous score on a validated measure of depressive symptoms, as is most commonly used. Second, depressive symptom trajectory classes aided in modeling the substantial heterogeneity apparent over time that is otherwise masked when a single slope is used. Trajectory classes also allow interrogation of predictors that distinguish individuals most at risk for chronically elevated symptoms both from those who recover and those who remain unperturbed. To date, research has identified predictors of membership in a chronically-impaired versus a never-impaired trajectory following stressful experiences such as breast cancer, but few predictors have been detected that distinguish the group who recovers from initial impairment (Foster et al., 2016; Henselmans et al., 2010). Characterizing contributors to the distinct trajectories could promote identification of processes that can be harnessed in interventions to catalyze recovery from depressive symptoms or prevent symptom elevations, thereby promoting efficient deployment of scarce resources. Diagnostic interview-detected MDE was a third indicator. In adults undergoing serious disease or other major stressors, MDEs occur less frequently than do questionnaire-assessed elevated depressive symptoms, but involve more debilitating consequences (e.g., Krebber et al., 2014).
Questions and Hypotheses
The available literature (e.g., Kvillemo & Bränström, 2014; Roesch et al., 2005) supported the hypotheses that participants who engaged in relatively high levels of approach-oriented coping would not evidence depression or would recover from initially elevated symptoms. Coping intended to avoid the stressor was posited to predict less favorable outcomes. The questions of whether specific coping strategies would yield similar relations with outcomes and whether findings would vary for the three indicators of depression also were examined.
Coping processes were expected to predict outcomes over and above covariates selected a priori or based on statistically significant relationships with outcomes in this sample. (Regarding relevant papers from this data set, note that Stanton et al. [2015] did not include coping processes as predictors, and Marroquín, Czamanski-Cohen, Weihs, and Stanton [2016] examined other predictors of the continuous 12-month depressive symptoms outcome only). Covariates included sociodemographic factors (age; Latina versus non-Latina; marital status [married/living as married versus not]; income; employment [employed, retired, unemployed]; subjective socioeconomic status; recruitment site [AZ or CA]) and medical variables (cancer stage; assessment interval [1–7] at which surgery, chemotherapy, and radiation ended; number of physical comorbidities; time-varying treatment variables [i.e., receipt of chemotherapy, radiation therapy, surgery, endocrine therapy, depression therapy at each assessment]).
METHOD
Participants
Women (N = 460) recently diagnosed with breast cancer took part in the My Year After cancer (MYA) study (Stanton et al., 2015). Eligibility criteria were: diagnosis of a new or initially recurrent invasive breast cancer; enrollment in the study within four months after cancer diagnosis; and ability to complete assessments in English. Any standard oncologic treatment was allowed (i.e., surgery, chemotherapy, radiotherapy, endocrine therapy [medication to block estrogen and progesterone, which promotes growth of breast cancers that have receptors for those hormones]), and any additional medication was permitted. Exclusion criteria were: diagnosis of current or past bipolar disorder, schizophrenia, or schizoaffective disorder; current cognitive disorder (e.g., dementia); current suicidality; younger than 21 years; and insufficient English literacy.
Procedures
After approval by the relevant institutional review boards, women were recruited from three oncology clinics in the greater Los Angeles area and one clinic at the University of Arizona Cancer Center. Research or clinic staff introduced consecutive (within scheduling constraints) and potentially eligible patients to the study, and research personnel explained the study further at that time or via telephone (with verbal consent for contact).
After giving written informed consent, participants completed an initial in-person assessment within four months of breast cancer diagnosis, assessments via telephone every six weeks through six months after study entry, an in-person assessment at nine months, and a telephone assessment at 12 months. Women received $60 compensation for in-person assessments and $30 for phone assessments. Retention was high, with 81% of the sample maintained through 12 months (n = 9 deaths; for details, see Stanton et al., 2015).
The in-person study entry and 9-month assessments were completed in the treating oncology center or women’s homes. Trained post-baccalaureate research staff conducted the sessions. Participants completed the relevant measures (and other measures not included in this report) via interview or laptop computer. In addition, every six weeks for six months after study entry and at 12 months, women completed measures via phone with the research staff.
Measures
Demographic and medical variables
At study entry, participants reported age, marital status, race/ethnicity, education, employment, income, subjective social status (Chen, Covinsky, Stijacic Cenzer, Adler, & Williams, 2012), and diagnosed physical comorbidities (Groll, To, Bombardier, & Wright, 2005). Medical record review provided cancer stage, date of diagnosis, and whether diagnosis was primary or recurrent, as supplemented by self-report when the record was unavailable (n = 39). Other self-reported variables (confirmed through medical records) at each assessment were: surgery, chemotherapy, radiotherapy, endocrine therapy, Herceptin (a biological treatment used for some breast cancers), and oncologic treatment duration (the 1–7 assessment point at which primary oncologic treatments were completed). Time-varying treatment factors were used for the continuous depressive symptom indicator and dichotomous treatment variables (e.g., ever received chemotherapy) for analyses of trajectory classes and MDEs. At each assessment, receipt of psychological or pharmacologic treatment for depression was assessed and coded for minimal adequacy from evidence-based guidelines of receiving ≥ two months of an appropriate medication or ≥ 8 visits with a mental health professional averaging ≥ 30 minutes each (Wang et al., 2005).
Breast cancer-related coping processes
Anchored to participants’ experience of breast cancer and assessed at all except the final assessment, coping items were rated on a 4-point scale from 1 = “I usually don’t do this at all”; 2 = “I do this a little bit”; 3 = “I do this a medium amount”; 4 = “I usually do this a lot”; items are averaged so that subscale scores potentially range from 1 to 4. Approach-oriented coping was assessed with 16 items from four COPE (Carver, Scheier, & Weintraub, 1989) subscales (Problem-Focused Coping, Acceptance, Seeking Social Support, Positive Reinterpretation) and the Emotional Approach Coping scales’ eight items in two subscales (Emotion Expression, Emotional Processing; (Stanton et al., 2000). Sample items include: “I think hard about what steps to take” (Problem-Focused), “I accept the reality of the fact that it happened” (Acceptance), “I try to get advice from someone about what to do” (Social Support), “I look for something good in what is happening” (Positive Reinterpretation), “I try to understand my feelings” (Emotional Processing), and “I take time to express my emotions” (Emotional Expression). Internal consistency estimates of reliability (Cronbach’s α) across the study ranged from 0.91–0.94 for the approach-oriented composite and 0.80–0.88 for problem-focused coping, 0.69–0.83 for acceptance (5/6 Cronbach’s α > 0.70), 0.77–0.83 for seeking social support, 0.78–0.83 for positive reinterpretation, 0.88–0.90 for emotional expression, and 0.75–0.80 for emotional processing.
Avoidance-oriented coping was assessed with three COPE subscales: Mental Disengagement (e.g., “I turn to work or other substitute activities to take my mind off things”), Behavioral Disengagement (“I admit to myself that I can’t deal with it, and quit trying”), and Denial (“I pretend that it hasn’t really happened”). Because 14 of 18 Cronbach’s α were < 0.70 for the separate subscales (range = 0.47–0.76), the 12-item avoidance-oriented coping composite was used (5/6 Cronbach’s α > 0.70; range = 0.68–0.74).
Depression
Completed at each assessment, the frequently used 20-item CES-D (Radloff, 1977) had Cronbach’s α ranging from 0.91 to 0.93 over seven assessments. Continuous CES-D score and the symptom trajectory classes previously identified (Stanton et al., 2015) were analyzed. At all assessments, supervised research staff administered relevant modules of the computer-guided Composite International Diagnostic Interview (CIDI; Kessler & Ustun, 2004) to assess MDEs, which were collapsed into a single binary variable: experience of a MDE over 12 months (yes/no). Two authors examined individual CIDI data to ensure that any episode did not reflect only the neurovegetative symptoms that can accompany cancer treatments.
Data Analysis
Analyses were conducted to assess coping processes as predictors of three outcomes: growth curve models of the continuous CES-D score, depressive symptom trajectory class, and MDE occurrence. Analyses included the covariates described previously. Prior to the analyses, growth models with random intercepts and linear slopes were fit for each coping measure, and the intercepts (with time centered at 2.1 months after diagnosis) and linear slopes for each participant were estimated for use as predictors in models for trajectory classes and MDEs.
The continuous depressive symptom outcome was analyzed with multilevel structural equation modeling. The longitudinal CES-D scores were modelled using random intercept, linear, and quadratic slope terms. Time-varying coping was entered as a predictor of CES-D level as well as in interaction with linear and quadratic time trends. Interaction terms that did not reach statistical significance (α = .05) were dropped sequentially. Separate models were estimated for the two coping composites and each coping subscale. A multivariate model including both composites was also fit to examine their unique effects. In all cases, coping was allowed to predict the CES-D intercept as well as the linear and quadratic slopes over time.
Depressive symptom trajectory classes were determined previously (Stanton et al., 2015). Four trajectory classes were apparent in growth mixture models: High, characterized by unremittingly elevated depressive symptoms (38% of 460 participants); Recovery, indicating by initially elevated depressive symptoms that improved over time (20%); and Low, indicating by consistently low depressive symptoms over time and empirically formed by two classes: low (32%) and very low (11%) depressive symptoms (which yielded nearly identical findings in preliminary analyses). Participants’ estimated coping intercept and slope were tested as predictors of symptom trajectory classes using multinomial logistic regression. Coping composites and subscales were assessed in separate models. The covariates were the same as for the multilevel structural equation models for the continuous outcome except that treatment variables were treated as time-invariant: ever received chemotherapy, radiation, surgery, and endocrine therapy.
MDE occurrence was modelled using binary logistic regression. Women’s estimated coping intercept and slope were tested as predictors, with each coping composite and subscale in a separate model. Covariates were the same as for the model of depressive symptom trajectory classes.
Full information maximum likelihood was used to address missing data in all models. The robust maximum likelihood estimator was used to provide model fit, confidence intervals, and statistical inference robust to non-normality. Data were analyzed with R v. 3.3.1 and Mplus v. 7.3 via MplusAutomation v. 0.6–4 (Hallquist & Wiley, in press). Statistical significance was set at α < .05.
Results
Sample Characteristics
The sample is characterized in detail in a previous publication (Stanton et al., 2015). Women were 56.4 years old on average (SD = 12.6 years), married or living as married (67.0%) and predominantly non-Latina white (67.6%) or Latina (19.3%). The sample had relatively high socioeconomic status, with 54.9% being college graduates, 52.1% employed, and 49.2% with a $75,000+ yearly household income. Women entered the study an average of 2.1 (SD = 0.81) months after diagnosis; 94.3% had primary non-metastatic breast cancer (breast cancer that had not spread beyond the breast and armpit lymph nodes), typically Stage 1 (44.4%) or Stage 2 (38.8%). Regarding treatments, 90.6% of women had surgery, 64.1% were prescribed endocrine therapy, 53.0% had chemotherapy, and 37.2% had radiation therapy.
Table 1 displays descriptive statistics for coping processes. Women reported relatively high levels of approach-oriented coping (M = 3.03–3.20; > “a medium amount”) and low avoidance-oriented coping (M = 1.42–1.63; < “a little bit”). Average trajectories of coping are shown in Figure 1. In general, engagement in coping processes declined significantly (p < .001) over time. The two exceptions were coping through emotional expression, which evidenced no change (p = .24), and coping through acceptance, which increased significantly (p < .001). Approach- and avoidance-oriented coping composites were not significantly correlated at study entry (r = −0.08, p = .09). All approach-oriented coping subscales were significantly and positively correlated (Supplementary Table S1).
Table 1.
Descriptive Statistics for Depressive Symptoms and Coping Processes over Time (n = 383–452)
| Measure | Week 0 | Week 6 | Week 12 | Week 18 | Week 24 | Week 36 |
|---|---|---|---|---|---|---|
| Depressive Symptoms | 12.82 (10.64) | 12.35 (10.73) | 11.65 (10.94) | 9.97 (9.44) | 10.10 (10.16) | 8.04 (9.26) |
|
| ||||||
| Approach Composite | 3.20 (0.52) | 3.14 (0.51) | 3.11 (0.54) | 3.05 (0.59) | 3.01 (0.61) | 3.03 (0.58) |
| Avoidance Composite | 1.58 (0.39) | 1.61 (0.37) | 1.63 (0.39) | 1.56 (0.38) | 1.56 (0.39) | 1.42 (0.38) |
|
| ||||||
| Problem Focused | 3.12 (0.75) | 2.97 (0.79) | 2.86 (0.83) | 2.78 (0.90) | 2.72 (0.92) | 2.67 (0.91) |
| Acceptance | 3.52 (0.54) | 3.59 (0.48) | 3.63 (0.52) | 3.63 (0.51) | 3.63 (0.53) | 3.70 (0.51) |
| Social Support | 3.23 (0.67) | 3.09 (0.70) | 2.99 (0.71) | 2.90 (0.78) | 2.79 (0.82) | 2.78 (0.79) |
| Positive Reinterpret | 3.32 (0.74) | 3.22 (0.71) | 3.19 (0.72) | 3.09 (0.78) | 3.06 (0.81) | 3.13 (0.79) |
| Emotional Expression | 2.94 (0.80) | 2.99 (0.76) | 2.95 (0.79) | 2.93 (0.81) | 2.89 (0.82) | 2.94 (0.80) |
| Emotional Processing | 3.06 (0.69) | 3.01 (0.67) | 3.00 (0.71) | 2.97 (0.73) | 2.94 (0.73) | 2.94 (0.73) |
Note. Results are means and standard deviations in parentheses.
Figure 1.
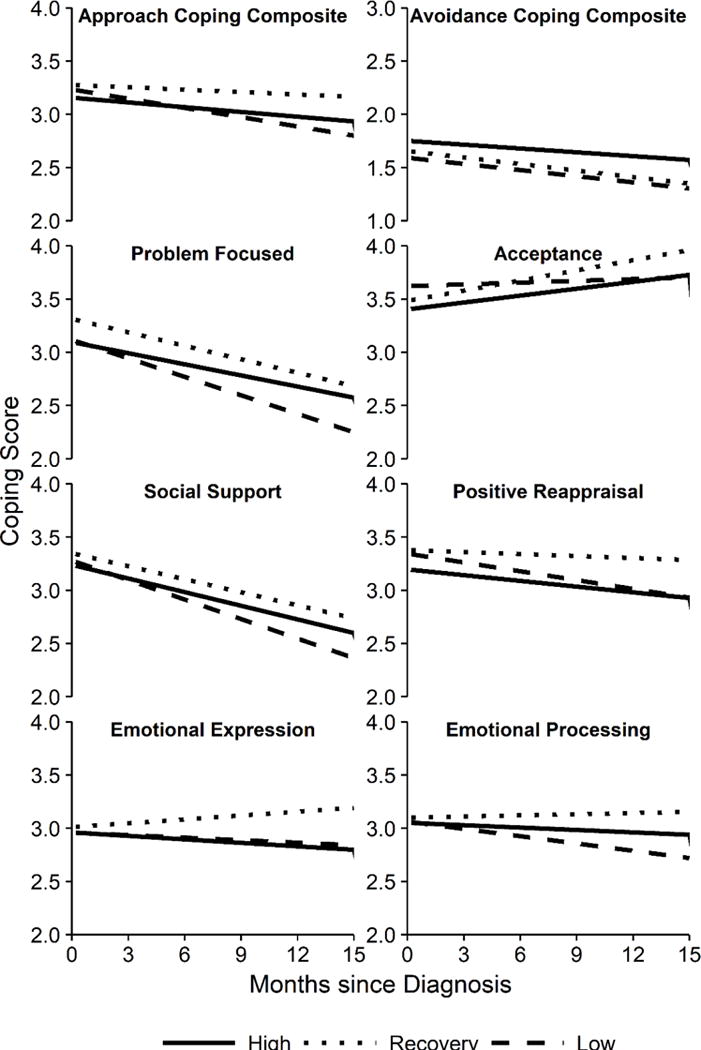
Estimated average coping trajectories by latent CES-D depressive symptom trajectory class.
Coping Processes as Predictors of the Continuous Depressive Symptoms Outcome
In this analysis, time-varying coping scores were matched to the time-varying depressive symptom scores. Table 2 contains final models. Within assessments, for every one unit higher approach-oriented coping, women reported an average 2.46 points lower depressive symptom scores. Each approach-oriented coping process (except problem-focused coping) predicted significantly lower depressive symptoms within assessments. For every one unit higher avoidance-oriented coping, women reported an average 5.66 points higher depressive symptom scores within assessments. Neither the approach-oriented nor the avoidance-oriented composites significantly interacted with the linear or quadratic time trends, but higher coping through positive reinterpretation significantly interacted with the linear slope such that greater positive reinterpretation was associated with a more slowly declining slope of depressive symptoms. Results were essentially unchanged when both coping composites were included in one analysis.
Table 2.
Multilevel Models for Coping Processes and Continuous Depressive Symptoms
| Coping Predictor | Intercept | Linear Slope |
|---|---|---|
| Approach Coping Composite | −2.46*** [−3.45, −1.47] | n.s. |
| Avoidance Coping Composite | 5.66*** [4.26, 7.05] | n.s. |
|
| ||
| Problem Focused | −0.54 [−1.09, 0.02] | n.s. |
| Acceptance | −2.19*** [−3.16, −1.22] | n.s. |
| Social Support | −0.76* [−1.39, −0.12] | n.s. |
| Positive Reinterpretation | −3.01*** [−4.16, −1.87] | 0.14* [0.00, 0.28] |
| Emotional Expression | −1.38*** [−1.96, −0.79] | n.s. |
| Emotional Processing | −1.18** [−1.87, −0.50] | n.s. |
Note. Estimates are unstandardized regression coefficients. 95% confidence intervals are in brackets. Each coping measure was tested in a separate model. Coping was tested as a predictor of the intercept, linear, and quadratic slopes of depressive symptoms, and higher-order terms (quadratic and linear slope) were dropped if not statistically significant. No quadratic slope was statistically significant. Final models are reported here. Bold values indicate effects that were significant in a multivariate model that simultaneously included approach- and avoidance-oriented coping composites. All models adjusted for: age, Latina versus nonLatina, marital status (married/living as married versus not), income, employment (employed, retired, unemployed), subjective socioeconomic status, cancer stage, assessment interval (1–7) at which major oncologic treatments (surgery, chemotherapy, radiation) ended, number of comorbidities, recruitment site (California, Arizona), and time-varying chemotherapy, radiation therapy, surgery, and aromatase inhibitors or endocrine antagonists.
p < .05.
p < .01.
p < .001.
Coping Processes as Predictors of Depressive Symptom Trajectory Classes
The first three columns of Table 3 contain odds ratios representing effects of the coping trajectories (i.e., estimates of the intercept and linear slope of each coping measure) on membership in depressive symptom trajectory classes (High, Recovery, Low). The fourth column contains odds ratios representing effects on MDE likelihood. Table 4 displays the predicted change in probability of membership in each depressive symptom trajectory class when moving from one standard deviation below to one standard deviation above the mean on the intercept and slope for each coping variable.
Table 3.
Odds Ratios for Associations of Coping Intercepts and Slopes with Depressive Symptom Trajectory Classes and Major Depressive Episodes
| Coping Predictor | Low vs. High | Recovery vs. High | Low vs. Recovery | MDE vs. No MDE |
|---|---|---|---|---|
| Approach Composite | ||||
| Intercept | 2.02* [1.08, 3.78] | 3.03** [1.40, 6.55] | 0.67 [0.31, 1.46] | 0.77 [0.38, 1.55] |
| Slope | 0.33* [0.12, 0.91] | 2.32 [0.56, 9.71] | 0.14** [0.03, 0.56] | 1.76 [0.58, 5.40] |
| Avoidance Composite | ||||
| Intercept | 0.07*** [0.02, 0.23] | 0.17** [0.05, 0.56] | 0.39 [0.10, 1.55] | 4.17** [1.44, 12.07] |
| Slopea | 0.41* [0.18, 0.93] | 0.46 [0.18, 1.17] | 0.89 [0.34, 2.31] | 2.26* [1.02, 5.01] |
|
| ||||
| Problem Focused | ||||
| Intercept | 1.39 [0.87, 2.21] | 2.67** [1.44, 4.95] | 0.52* [0.29, 0.93] | 0.78 [0.45, 1.34] |
| Slope | 0.55* [0.31, 0.96] | 0.80 [0.38, 1.67] | 0.69 [0.33, 1.43] | 1.69 [0.88, 3.25] |
| Acceptance | ||||
| Intercept | 3.66** [1.36, 9.81] | 7.73** [2.12, 28.13] | 0.47 [0.12, 1.83] | 0.46 [0.19, 1.12] |
| Slope | 0.33 [0.08, 1.38] | 9.87* [1.25, 77.94] | 0.03*** [0.00, 0.27] | 1.35 [0.35, 5.26] |
| Social Support | ||||
| Intercept | 1.27 [0.77, 2.09] | 1.94* [1.07, 3.53] | 0.65 [0.37, 1.16] | 1.04 [0.58, 1.85] |
| Slope | 0.58 [0.30, 1.14] | 1.17 [0.50, 2.73] | 0.50 [0.22, 1.14] | 1.61 [0.68, 3.80] |
| Positive Reinterpretation | ||||
| Intercept | 2.20*** [1.35, 3.57] | 2.67** [1.45, 4.92] | 0.82 [0.44, 1.55] | 0.75 [0.43, 1.33] |
| Slope | 0.62 [0.27, 1.39] | 1.93 [0.62, 6.00] | 0.32* [0.11, 0.97] | 0.78 [0.31, 1.94] |
| Emotional Expression | ||||
| Intercept | 1.19 [0.81, 1.77] | 1.73* [1.06, 2.82] | 0.69 [0.43, 1.12] | 0.97 [0.62, 1.52] |
| Slope | 1.12 [0.48, 2.59] | 3.77* [1.29, 11.05] | 0.30* [0.10, 0.88] | 0.95 [0.36, 2.49] |
| Emotional Processing | ||||
| Intercept | 1.17 [0.72, 1.88] | 1.47 [0.81, 2.65] | 0.79 [0.44, 1.43] | 1.04 [0.59, 1.82] |
| Slope | 0.39* [0.16, 0.93] | 2.16 [0.68, 6.82] | 0.18** [0.06, 0.57] | 1.29 [0.54, 3.10] |
Note. Estimates are odds ratios for the latent CES-D depressive symptom trajectory classes and major depressive episodes. 95% confidence intervals are in brackets. Odds ratios and confidence intervals are reported for each coping measure tested in a separate model. Bold values indicate effects that were significant in a multivariate model that simultaneously included the approach and avoidance composites intercepts and slopes. MDE = major depressive episode. The depressive symptom trajectory classes were estimated in a single, multinomial logistic regression model. The MDE model was estimated separately as a binary logistic regression model. All models adjusted for: age, Latina versus nonLatina, marital status (married/living as married versus not), income, employment (employed, retired, unemployed), subjective socioeconomic status, cancer stage, assessment interval (1–7) at which major oncologic treatments (surgery, chemotherapy, radiation) ended, number of comorbidities, recruitment site (California, Arizona), ever received chemotherapy, ever received radiation therapy, ever received surgery, and ever received aromatase inhibitors or endocrine antagonists.
Due to low variability, results for the avoidance composite slope are presented for a 0.1 unit change, rather than the typical 1.0 unit change used for all others.
p < .05.
p < .01.
p < .001.
Table 4.
Estimated Change in Percentage of Participants in Depressive Symptom Trajectory Classes as a Function of Level and Change in Coping Processes
| Coping Predictor | Coping Intercept | Coping Slope | ||||
|---|---|---|---|---|---|---|
| Low | Recovery | High | Low | Recovery | High | |
| Approach Coping Composite | 1.5% | 2.7% | −4.1% | −6.6% | 4.8% | 1.8% |
| Avoidance Coping Composite | −9.4% | −0.9% | 10.3% | −2.7% | −1.0% | 3.7% |
| Problem-Focused Coping | 0.1% | 2.8% | −2.7% | −2.5% | 0.2% | 2.2% |
| Acceptance | 2.5% | 5.2% | −7.7% | −9.0% | 10.1% | −1.2% |
| Social Support | 0.0% | 1.9% | −1.9% | −2.8% | 1.5% | 1.3% |
| Positive Reinterpretation | 2.1% | 2.1% | −4.2% | −3.3% | 3.0% | 0.3% |
| Emotional Expression | −0.1% | 1.6% | −1.5% | −1.7% | 4.3% | −2.6% |
| Emotional Processing | 0.0% | 1.2% | −1.2% | −5.7% | 4.5% | 1.2% |
Note. Table shows the predicted change in percent of women in each depressive symptom trajectory class (Low, Recovery, High) when moving from 1 SD below the mean to 1 SD above the mean on the intercept (left side) and slope (right side) for each coping variable. Covariates were held at their mean for continuous variables, median for ordered discrete variables, and mode for unordered discrete variables.
Coping process predictors of Low versus High depressive symptom trajectory classes
Women who at study entry (i.e., intercept) engaged in more approach-oriented coping, particularly acceptance and positive reinterpretation, as well as less avoidance-oriented coping, had significantly higher odds of membership in the Low, as opposed to High, class. Women whose approach-oriented coping, and specifically problem-focused coping and emotional processing, as well as avoidant coping, decreased more steeply over time (i.e., more negative linear slope) had significantly higher odds of being in the Low (versus High) class.
Coping process predictors of Recovery versus High depressive symptom trajectory classes
Participants who at study entry used more approach-oriented coping, and specifically problem-focused coping, acceptance, social support, emotional expression, and positive reinterpretation, had significantly higher odds of membership in the Recovery versus High class. Conversely, women who engaged in more avoidant coping had lower odds of membership in the Recovery class. Greater increases over time in coping through acceptance and through emotional expression also were associated with higher odds of being in the Recovery class versus remaining in the High class.
Coping process predictors of Recovery versus Low depressive symptom trajectory classes
Women who used more (as opposed to less) problem-focused coping at study entry had significantly higher odds of being in the Recovery compared to the Low class. Women with more positive slopes of approach-oriented coping and specifically acceptance, emotional expression and processing, and positive reinterpretation, had significantly higher odds of being in the Recovery class, compared to the Low class.
Coping Processes Predicting Occurrence of Major Depressive Episodes
The final column of Table 3 contains the relations between coping trajectories (estimates of the intercept and linear slope of each coping measure) and MDEs. Neither the intercept nor slope of the approach-oriented coping composite or any subscale was related significantly to the odds of having a MDE. However, both a higher intercept and a more positive linear slope of avoidance-oriented coping were associated with greater odds of MDE occurrence.
Discussion
In this study of 460 women diagnosed on average two months previously with breast cancer, coping processes predicted all three indicators of depression over the subsequent 12 months. As hypothesized, women who coped through more actively approaching the cancer experience generally had more favorable outcomes, whereas engagement in avoidance-oriented coping predicted higher risk for depression. These findings, which are consistent with evidence from a meta-analysis on coping with breast cancer (Kvillemo & Bränström, 2014), held over and above the contribution of an array of sociodemographic and medical covariates.
The most consistent evidence accrued for the hazards of coping through cognitive and behavioral avoidance. Specifically, breast cancer patients who engaged in more (versus less) avoidance-oriented coping at study entry were more likely to evidence: 1) higher depressive symptoms overall; 2) greater odds of being in the High (versus Recovery or Low) symptom trajectory class; and 3) greater odds of meeting diagnostic criteria for MDE during the following year. Importantly, women with a more positive (versus more negative) avoidant coping slope had greater odds of having high and sustained depressive symptoms (versus being in the Low class) or an MDE over 12 months. The prospective link of avoidance with MDE converges with theory and evidence that adults prone to psychological disorders, including depression, often evaluate their frequent, strong negative emotions as aversive and unacceptable, and attempt to regulate them through avoidance. In turn, avoidance amplifies negative affect and disrupts coping and other processes that lend emotions, cognitions, and behaviors initiated during stressful experiences their functional value (e.g., informing and pursuing goal-congruent behaviors; e.g., Barlow, Bullis, Comer, & Ametaj, 2013; Wegner, Schneider, Carter, & White, 1987).
Findings also point to the generally salutary, albeit more nuanced, role of approach-oriented coping in improving depressive symptoms and trajectories (but not MDE). As hypothesized, relatively high engagement in approach-oriented processes was associated with significantly lower depressive symptoms across assessments, as well as higher odds of membership in the Recovery and Low as opposed to High symptom trajectory classes. Findings regarding the specific indicators of approach-oriented coping and their change over time were more complex. Cancer-related coping through active acceptance and emotional expression were the most potent predictors of outcomes, in that both significantly predicted lower CES-D scores across assessments as well as odds of membership in the Recovery symptom trajectory class (and for acceptance, the Low symptom class) versus the High class. Addressing the research question on the importance of stable or increasing attempts to cope over time, the only coping processes that did not on average decline significantly over time (i.e., emotional expression) or that increased significantly (i.e., acceptance) were also the ones that predicted higher odds of recovering from initially high depressive symptoms. Perseverance in these two processes appears useful, particularly as one undergoes and emerges from a cascade of largely uncontrollable stressful experiences such as cancer diagnosis and treatment. The significant decline in all other coping processes is understandable; theoretically, individuals reduce their coping efforts when they are no longer needed (Lazarus & Folkman, 1984).
When engaged shortly after cancer diagnosis, the other approach-oriented coping processes—positive reinterpretation, emotional processing, problem-focused coping, and seeking social support—also appeared to promote recovery. The relation of higher positive reinterpretation with lower depressive symptoms declined significantly across time. Furthermore, women with more decline in problem-focused coping and emotional processing had lower odds of being in the High (versus Low) depressive symptom trajectory class. These findings likely speak to the importance of timing of the coping effort and degree of correspondence to the stressor’s demands. Perhaps problem-focused coping and emotional processing efforts declined when women had used them efficiently soon after cancer diagnosis.
Limitations of the study deserve mention. First, coping processes and depressive symptoms were self-reported, and the three avoidance subscales were of inadequate internal consistency, leading to analysis of an avoidance-oriented coping composite. Modest floor (avoidance) and ceiling (approach) effects were noted on coping strategies; critically, most women were not at the floor or ceiling. The generally low use of avoidance and high use of approach-oriented coping may have served to weaken the relations of coping with depression. However, these were generally psychometrically sound measures with demonstrated predictive utility, and MDEs were assessed through structured interview. That the three indicators of depression had similar predictors also increases confidence in the findings.
Second, causality is not definitive in this longitudinal design. The causal priority of avoidance, however, is suggested by the finding that initial engagement in avoidant coping successfully distinguished the depressive symptom trajectory classes and predicted MDE occurrence, both of which were based on assessments over the ensuing 12 months. In addition, the pernicious role of intentional avoidance in psychological and physical health is supported by considerable longitudinal and experimental research (Cronkite et al., 2013; Nash et al., 2015; Price et al., 2013; Roesch et al., 2005; Wegner et al., 1987), except under particular conditions such as use of focused distraction during an acute or uncontrollable stressor (e.g., Suls & Fletcher, 1985). Similarly, approach-oriented coping strategies predicted recovery from depressive symptoms. These processes can be induced experimentally, with ensuing positive psychological and physical health-related consequences (Greer et al,. 2018; Low et al., 2008; Pennebaker & Smyth, 2016).
Third, although the sample was relatively large and somewhat geographically diverse, generalization of findings to men, people undergoing other stressful experiences, and specific under-represented groups requires study. It is notable that Latinas comprised 19% of the sample; preliminary analyses provided no evidence that ethnicity interacted significantly with coping to predict depression (data not shown; also see Moreno et al., 2016). Finally, personality attributes and other factors contribute to coping attempts and psychosocial outcomes (e.g., Carver & Connor-Smith, 2010). Evidence is accruing for additional significant predictors of trajectories of psychological and physical health during the experience of cancer and other stressors, which constitutes a productive focus of future research (Burton, Galatzer-Levy, & Bonanno, 2015; Ciere et al., 2017; Danhauer et al., 2015; Donovan, Gonzalez, Small, Andrykowski, & Jacobsen, 2014; Foster et al., 2016; Linden, MacKenzie, Rnic, Marshall, & Vodermaier, 2015; McGinty, Small, Laronga, & Jacobsen, 2016; Nash et al., 2015; Pérez et al., 2016).
With regard to clinical implications, the present findings are heartening in that processes amenable to change—such as coping through avoidance, acceptance, and emotional expression—predict depressive outcomes in women with breast cancer. In addition, malleable predictors—not only of having consistently low depressive symptoms but also of recovering effectively from initially elevated symptoms—can be identified. As such, they pave the way for development and refinement of approaches to prevent and ameliorate depression. Although interventions designed to counter avoidance and promote approach-oriented strategies are available (e.g., Andersen et al., 2004; Antoni et al., 2006; Barlow et al., 2013, 2017; Foa & Kozak, 1986; Hayes, Luoma, Bond, Masuda, & Lillis, 2006), change in those strategies as potentially powerful “active ingredients” (i.e., therapeutic targets) in intervention efficacy is understudied, both with regard to psychological disorders (Barlow et al., 2013) and adjustment to stressful experiences including cancer (Moyer et al., 2013; Stanton et al., 2013). Within the hundreds of interventions tested to improve cancer survivors’ quality of life (Faller et al., 2013), evidence that avoidance and approach-oriented processes can be altered effectively to influence outcomes in adults diagnosed with cancer is accruing in trials of in-person interventions spanning seven to 20 hours (Antoni et al., 2006; Manne et al., 2008; Penedo et al., 2004; Rost, Wilson, Buchanan, Hildebrandt, & Mutch, 2012). The current findings suggest specific coping processes that might be efficiently and productively targeted to treat or prevent depression.
In light of the projected 37% rise (2012–2022) in the U.S. population living for at least five years with a cancer diagnosis (de Moor et al., 2013), evidence-supported, efficient, and disseminable approaches to promote the group’s emotional and physical well-being are vitally needed. Moreover, accumulating evidence indicates that effective transdiagnostic change processes involve: 1) overcoming avoidance and increasing distress tolerance; 2) promoting specific approach-oriented cognitions, emotions, and behaviors; and 3) modifying cognitive appraisals (Barlow et al., 2017; Greer et al., 2017). Pending additional empirical scrutiny, such approaches promise to aid adults contending with cancer and other serious diseases, undergoing profound and on-going stressors, and at risk for or experiencing psychological disorders.
Supplementary Material
Public Health Significance.
This prospective, longitudinal study identified potentially malleable coping processes that contribute to depressive symptoms and episodes in women recently diagnosed with breast cancer. Interventions targeted toward reducing cancer-related avoidance and fostering acceptance and emotional expression, among other approach-oriented coping strategies, could hold promise for preventing and lessening the burden of depression in this group and perhaps others undergoing life-threatening diseases.
Acknowledgments
We are thankful to the women who participated in the My Year After Breast Cancer study, the referring oncologists, and the research staff.
Sponsors: Supported by 1R01 CA133081 (Stanton & Weihs, co-PIs), Breast Cancer Research Foundation BCRF-17-151 (Stanton), NCI P30CA023074 University of Arizona Cancer Center Support Grant (Weihs, PI: Kraft), Jonsson Comprehensive Cancer Center support grant, NIH/NCI P30 CA 16042 (Crespi, PI: Gasson).
References
- Andersen BL, Farrar WB, Golden-Kreutz DM, Glaser R, Emery CF, Crespin TR, Carson WE. Psychological, behavioral, and immune changes after a psychological intervention: A clinical trial. Journal of Clinical Oncology. 2004;22:3570–3580. doi: 10.1200/JCO.2004.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoni MH, Lechner SC, Kazi A, Wimberly SR, Sifre T, Urcuyo KR, Carver CS. How stress management improves quality of life after treatment for breast cancer. Journal of Consulting and Clinical Psychology. 2006;74:1143–1152. doi: 10.1037/0022-006X.74.6.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow D, Bullis J, Comer J, Ametaj A. Evidence-based psychological treatments: An update and a way forward. Annual Review of Clinical Psychology. 2013;9:1–27. doi: 10.1146/annurev-clinpsy-050212-185629. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, Cassiello-Robbins C. The Unified Protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry. 2017;74:875–884. doi: 10.1001/jamapsychiatry.2017.2164.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annual Review of Clinical Psychology. 2011;7:511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- Burton CL, Galatzer-Levy IR, Bonanno GA. Treatment type and demographic characteristics as predictors for cancer adjustment: Prospective trajectories of depressive symptoms in a population sample. Health Psychology. 2015;34:602–609. doi: 10.1037/hea0000145. [DOI] [PubMed] [Google Scholar]
- Carver CS, Connor-Smith J. Personality and coping. Annual Review of Psychology. 2010;61:679–704. doi: 10.1146/annurev.psych.093008.100352. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Chen B, Covinsky KE, Stijacic Cenzer I, Adler N, Williams BA. Subjective social status and functional decline in older adults. Journal of General Internal Medicine. 2012;27:693–699. doi: 10.1007/s11606-011-1963-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciere Y, Janse M, Almansa J, Visser A, Sanderman R, Sprangers MAG, Fleer J. Distinct trajectories of positive and negative affect after colorectal cancer diagnosis. Health Psychology. 2017;36:521–528. doi: 10.1037/hea0000485. [DOI] [PubMed] [Google Scholar]
- Compas BE, Jaser SS, Bettis AH, Watson KH, Gruhn MA, Dunbar JP, Thigpen JC. Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychological Bulletin. 2017;143:939–991. doi: 10.1037/bul0000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronkite RC, Woodhead EL, Finlay A, Timko C, Unger Hu K, Moos RH. Life stressors and resources and the 23-year course of depression. Journal of Affective Disorders. 2013;150:370–377. doi: 10.1016/j.jad.2013.04.022. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. American Journal of Psychiatry. 2014;171:453–462. doi: 10.1176/appi.ajp.2013.13030325. [DOI] [PubMed] [Google Scholar]
- Dalton SO, Laursen TM, Ross L, Mortensen PB, Johansen C. Risk for hospitalization with depression after a cancer diagnosis: A nationwide, population-based study of cancer patients in Denmark from 1973 to 2003. Journal of Clinical Oncology. 2009;27:1440–1445. doi: 10.1200/JCO.2008.20.5526. [DOI] [PubMed] [Google Scholar]
- Danhauer SC, Russell G, Case LD, Sohl SJ, Tedeschi RG, Addington EL, Avis NE. Trajectories of posttraumatic growth and associated characteristics in women with breast cancer. Annals of Behavioral Medicine. 2015;49:650–659. doi: 10.1007/s12160-015-9696-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, Jackson DC, Kalin NH. Emotion, plasticity, context, and regulation: Perspectives from affective neuroscience. Psychological Bulletin. 2000;126:890–909. doi: 10.1037/0033-2909.126.6.890. [DOI] [PubMed] [Google Scholar]
- de Moor JS, Mariotto AB, Parry C, Alfano CM, Padgett L, Kent EE, Rowland JH. Cancer survivors in the United States: Prevalence across the survivorship trajectory and implications for care. Cancer Epidemiology Biomarkers & Prevention. 2013;22:561–570. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: A meta-analysis. Medical Care. 2002;40:794–811. doi: 10.1097/01.MLR.0000024612.61915.2D. [DOI] [PubMed] [Google Scholar]
- Donovan KA, Gonzalez BD, Small BJ, Andrykowski MA, Jacobsen PB. Depressive symptom trajectories during and after adjuvant treatment for breast cancer. Annals of Behavioral Medicine. 2014;47:292–302. doi: 10.1007/s12160-013-9550-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duangdao KM, Roesch SC. Coping with diabetes in adulthood: A meta-analysis. Journal of Behavioral Medicine. 2008;31:291–300. doi: 10.1007/s10865-008-9155-6. [DOI] [PubMed] [Google Scholar]
- Faller H, Schuler M, Richard M, Heckl U, Weis J, Küffner R. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: Systematic review and meta-analysis. Journal of Clinical Oncology. 2013;31:782–793. doi: 10.1200/JCO.2011.40.8922. [DOI] [PubMed] [Google Scholar]
- Fang F, Fall K, Mittleman MA, Sparen P, Ye W, Adami HO, Valdimarsdottir U. Suicide and cardiovascular death after a cancer diagnosis. New England Journal of Medicine. 2012;366:1310–1318. doi: 10.1056/NEJMoa1110307. [DOI] [PubMed] [Google Scholar]
- Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Gralow J. Major depression after breast cancer: A review of epidemiology and treatment. General Hospital Psychiatry. 2008;30:112–126. doi: 10.1016/j.genhosppsych.2007.10.008. [DOI] [PubMed] [Google Scholar]
- Fiszer C, Dolbeault S, Sultan S, Brédart A. Prevalence, intensity, and predictors of the supportive care needs of women diagnosed with breast cancer: A systematic review. Psycho-Oncology. 2014;23:361–374. doi: 10.1002/pon.3432. [DOI] [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Foster C, Haviland J, Winter J, Grimmett C, Chivers Seymour K, Batehup L, Members of the Study Advisory Committee Pre-surgery depression and confidence to manage problems predict recovery trajectories of health and wellbeing in the first two years following colorectal cancer: Results from the CREW cohort study. PloS One. 2016;11(5):e0155434. doi: 10.1371/journal.pone.0155434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein D, Bennett BK, Webber K, Boyle F, de Souza PL, Wilcken NR, Lloyd AR. Cancer-related fatigue in women with breast cancer: Outcomes of a 5-year prospective cohort study. Journal of Clinical Oncology. 2012;30:1805–1812. doi: 10.1200/JCO.2011.34.6148. [DOI] [PubMed] [Google Scholar]
- Greer JA, Jacobs JM, El-Jawahri A, Nipp RD, Gallagher ER, Pirl WF, Temel JS. Role of patient coping strategies in understanding the effects of early palliative care on quality of life and mood. Journal of Clinical Oncology. 2018;36:53–60. doi: 10.1200/JCO.2017.73.7221.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groll DL, To T, Bombardier C, Wright JG. The development of a comorbidity index with physical function as the outcome. Journal of Clinical Epidemiology. 2005;58:595–602. doi: 10.1016/j.jclinepi.2004.10.018. [DOI] [PubMed] [Google Scholar]
- Hallquist M, Wiley JF. MplusAutomation: An R package for facilitating large-scale latent variable analyses in Mplus. Structural Equation Modeling: A Multidisciplinary Journal. 2018;25:621–638. doi: 10.1080/10705511.2017.1402334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Depression and stressful environments: Identifying gaps in conceptualization and measurement. Anxiety, Stress, & Coping. 2016;29:335–351. doi: 10.1080/10615806.2015.1134788. [DOI] [PubMed] [Google Scholar]
- Hart SL, Hoyt MA, Diefenbach M, Anderson DR, Kilbourn KM, Craft LL, Stanton AL. Meta-analysis of efficacy of interventions for elevated depressive symptoms in adults diagnosed with cancer. Journal of the National Cancer Institute. 2012;104:990–1004. doi: 10.1093/jnci/djs256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Henselmans I, Helgeson VS, Seltman H, de Vries J, Sanderman R, Ranchor AV. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychology. 2010;29:160–168. doi: 10.1037/a0017806. [DOI] [PubMed] [Google Scholar]
- Holden AE, Ramirez AG, Gallion K. Depressive symptoms in Latina breast cancer survivors: A barrier to cancer screening. Health Psychology. 2014;33:242–248. doi: 10.1037/a0032685. [DOI] [PubMed] [Google Scholar]
- Jones SM, LaCroix AZ, Li W, Zaslavsky O, Wassertheil-Smoller S, Weitlauf J, Danhauer SC. Depression and quality of life before and after breast cancer diagnosis in older women from the Women’s Health Initiative. Journal of Cancer Survivorship. 2015;9:620–629. doi: 10.1007/s11764-015-0438-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebber AMH, Buffart LM, Kleijn G, Riepma IC, de Bree R, Leemans CR, Verdonck-de Leeuw IM. Prevalence of depression in cancer patients: A meta-analysis of diagnostic interviews and self-report instruments. Psycho-Oncology. 2014;23:121–130. doi: 10.1002/pon.3409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvillemo P, Bränström R. Coping with breast cancer: A meta-analysis. PloS One. 2014;9(11):e112733. doi: 10.1371/journal.pone.0112733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging. 1997;12:277–287. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- Li M, Kennedy EB, Byrne N, Gérin-Lajoie C, Katz MR, Keshavarz H, Green E. Systematic review and meta-analysis of collaborative care interventions for depression in patients with cancer. Psycho-Oncology. 2017;26:573–587. doi: 10.1002/pon.4286. [DOI] [PubMed] [Google Scholar]
- Linden W, MacKenzie R, Rnic K, Marshall C, Vodermaier A. Emotional adjustment over 1 year post-diagnosis in patients with cancer: Understanding and predicting adjustment trajectories. Supportive Care in Cancer. 2015;23:1391–1399. doi: 10.1007/s00520-014-2492-9. [DOI] [PubMed] [Google Scholar]
- Low CA, Stanton AL, Bower JE. Effects of acceptance-oriented versus evaluative emotional processing on heart rate recovery and habituation. Emotion. 2008;8:419–424. doi: 10.1037/1528-3542.8.3.419. [DOI] [PubMed] [Google Scholar]
- Lu D, Andersson TL, Fall K, Hultman CM, Czene K, Valdimarsdóttir U, Fang F. Clinical diagnosis of mental disorders immediately before and after cancer diagnosis: A nationwide matched cohort study in Sweden. JAMA Oncology. 2016;2:1188–1196. doi: 10.1001/jamaoncol.2016.0483. [DOI] [PubMed] [Google Scholar]
- Manne S, Winkel G, Rubin S, Edelson M, Rosenblum N, Bergman C, Rocereto T. Mediators of a coping and communication-enhancing intervention and a supportive counseling intervention among women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology. 2008;76:1034–1045. doi: 10.1037/a0014071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marroquín B, Czamanski-Cohen J, Weihs KL, Stanton AL. Implicit loneliness, emotion regulation, and depressive symptoms in breast cancer survivors. Journal of Behavioral Medicine. 2016;39:832–844. doi: 10.1007/s10865-016-9751-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty HL, Small BJ, Laronga C, Jacobsen PB. Predictors and patterns of fear of cancer recurrence in breast cancer survivors. Health Psychology. 2016;35:1–9. doi: 10.1037/hea0000238. [DOI] [PubMed] [Google Scholar]
- Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Jemal A. Cancer treatment and survivorship statistics, 2016. CA: A Cancer Journal for Clinicians. 2016;66:271–289. doi: 10.3322/caac.21349. [DOI] [PubMed] [Google Scholar]
- Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncology. 2011;12:160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- Moreno PI, Bauer MR, Yanez B, Jorge A, Maggard-Gibbons M, Stanton AL. Dispositional emotional expressivity, cancer-specific coping, and distress in socioeconomically-disadvantaged Latinas. Health Psychology. 2016;35:584–593. doi: 10.1037/hea0000319. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT, Hult JR, Bussolari C, Acree M. What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychological Bulletin. 2009;135:121–141. doi: 10.1037/a0014210. [DOI] [PubMed] [Google Scholar]
- Moyer A, Goldenberg M, Hall MA, Knapp-Oliver SK, Sohl SJ, Schneider S. Mediators of change in psychosocial interventions for cancer patients: A systematic review. Behavioral Medicine. 2012;38:90–114. doi: 10.1080/08964289.2012.695412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash WP, Boasso AM, Steenkamp MM, Larson JL, Lubin RE, Litz BT. Posttraumatic stress in deployed Marines: Prospective trajectories of early adaptation. Journal of Abnormal Psychology. 2015;124:155–171. doi: 10.1037/abn0000020. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR, Molton I, Gonzalex JS, Kinsinger D, Roos BA, Antoni MH. Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer. 2004;100:192–200. doi: 10.1002/cncr.11894. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW, Smyth J. Opening up by writing it down: The healing power of expressive writing. 3rd. New York, NY: Guilford; 2016. [Google Scholar]
- Pérez S, Conchado A, Andreu Y, Galdón MJ, Cardeña E, Ibáñez E, Durá E. Acute stress trajectories 1 year after a breast cancer diagnosis. Supportive Care in Cancer. 2016;24:1671–1678. doi: 10.1007/s00520-015-2960-x. [DOI] [PubMed] [Google Scholar]
- Price MA, Bell ML, Sommeijer DW, Friedlander M, Stockler MR, Defazio A, Butow PN. Physical symptoms, coping styles and quality of life in recurrent ovarian cancer: A prospective population-based study over the last year of life. Gynecologic Oncology. 2013;130:162–168. doi: 10.1016/j.ygyno.2013.03.031. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Roesch SC, Adams L, Hines A, Palmores A, Vyas P, Tran C, Vaughn AA. Coping with prostate cancer: A meta-analytic review. Journal of Behavioral Medicine. 2005;28:281–293. doi: 10.1007/s10865-005-4664-z. [DOI] [PubMed] [Google Scholar]
- Rost AD, Wilson K, Buchanan E, Hildebrandt MJ, Mutch D. Improving psychological adjustment among late-stage ovarian cancer patients: Examining the role of avoidance in treatment. Cognitive and Behavioral Practice. 2012;19:508–517. [Google Scholar]
- Roth S, Cohen LJ. Approach, avoidance, and coping with stress. American Psychologist. 1986;41:813–819. doi: 10.1037//0003-066x.41.7.813. [DOI] [PubMed] [Google Scholar]
- Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychological Bulletin. 2003;129:216–269. doi: 10.1037/0033-2909.129.2.216. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Kirk SB, Cameron CL, Danoff-Burg S. Coping through emotional approach: Scale construction and validation. Journal of Personality and Social Psychology. 2000;78:1150–1169. doi: 10.1037/0022-3514.78.6.1150. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Luecken LJ, MacKinnon DP, Thompson EH. Mechanisms in psychosocial interventions for adults living with cancer: Opportunity for integration of theory, research, and practice. Journal of Consulting and Clinical Psychology. 2013;81:318–335. doi: 10.1037/a0028833. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Wiley JF, Krull JL, Crespi CM, Hammen C, Allen JB, Weihs KL. Depressive episodes, symptoms, and trajectories in women recently diagnosed with breast cancer. Breast Cancer Research and Treatment. 2015;154(1):105–115. doi: 10.1007/s10549-015-3563-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiner JF, Cavender TA, Nowels CT, Beaty BL, Bradley CJ, Fairclough DL, Main DS. The impact of physical and psychosocial factors on work characteristics after cancer. Psycho-Oncology. 2008;17:138–147. doi: 10.1002/pon.1204. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-47, HHS Publication No (SMA) 13-4805. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. Results from the 2012 National Survey on Drug Use and Health: Mental health findings. https://www.samhsa.gov/data/sites/default/files/NSDUHmhfr2012/NSDUHmhfr2012.pdf Accessed September 25, 2017. [Google Scholar]
- Suls J, Fletcher B. The relative efficacy of avoidant and nonavoidant coping strategies: A meta-analysis. Health Psychology. 1985;4:249–288. doi: 10.1037//0278-6133.4.3.249. [DOI] [PubMed] [Google Scholar]
- Suppli NP, Johansen C, Christensen J, Kessing LV, Kroman N, Dalton SO. Increased risk for depression after breast cancer: A nationwide population-based cohort study of associated factors in Denmark, 1998–2011. Journal of Clinical Oncology. 2014;32:3831–3839. doi: 10.1200/JCO.2013.54.0419. [DOI] [PubMed] [Google Scholar]
- Tobin DL, Holroyd KA, Reynolds RV, Wigal JK. The hierarchical factor structure of the Coping Strategies Inventory. Cognitive Therapy and Research. 1989;13:343–361. [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Schneider DJ, Carter SR, White TL. Paradoxical effects of thought suppression. Journal of Personality and Social Psychology. 1987;53:5–13. doi: 10.1037//0022-3514.53.1.5. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Cancer fact sheet. 2018 http://www.who.int/mediacentre/factsheets/fs297/en/ Accessed March 15, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


