Abstract
Purpose
Despite well-established concerns regarding adverse drug effects, antipsychotics are frequently prescribed for older adults. Our first objective was to identify trends in antipsychotic dispensations to older Nova Scotians. STOPP (Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions) criteria identify antipsychotic use in those with a history of falls as potentially inappropriate. Our second objective was to identify trends, predictors, and adherence with this STOPP criteria by identifying continued antipsychotic dispensations following a fall-related hospitalization.
Methods
A descriptive cross-sectional cohort study of Nova Scotia Seniors’ Pharmacare Program (NSSPP) beneficiaries ≥ 66 years with at least one antipsychotic dispensation annually from April 1, 2009 to March 31, 2014 was completed. As well, unique beneficiaries with at least one antipsychotic dispensation in the four-year period between April 1, 2009 and March 31, 2013 were linked to fall-related hospitalizations recorded in the Canadian Institute for Health Information Discharge Abstract Database. The relationship of age, sex, fiscal year, days supply and length-of-stay were studied to identify predictors of continued antipsychotic dispensation post-discharge. Descriptive statistics and multivariate logistic analysis were performed. Odds ratios for the association of risk factors and adherence to STOPP criteria were calculated.
Findings
We identified that in each year observed, there were 6% of eligible NSSPP beneficiaries that received at least one antipsychotic dispensation. Approximately 70% of antipsychotic dispensations were for second generation agents, primarily quetiapine and risperidone. Of the unique beneficiaries with at least one antipsychotic dispensation in the four-year period between April 1, 2009 and March 31, 2013 who survived a fall-related hospitalization over 75% were dispensed an antipsychotic in the 100 days following hospital discharge. Logistic regression showed no statistically significant association between potentially inappropriate therapy and potential predictors in multivariate analysis.
Implications
In each year from 2009 to 2014, 6% of Nova Scotia Seniors’ Pharmacare beneficiaries were dispensed at least one antipsychotic prescription. Over 75% of the older adults who received an antipsychotic dispensation in the 100 days prior to a fall-related hospitalization, continued the drug class after discharge. This demonstrates that despite the recommendations of quality indicators such as the STOPP criteria, antipsychotics are continued in individuals at a high risk of falling. Future investigations are needed to inform health team, system, and policy interventions to improve concordance with this antipsychotic specific STOPP criterion when appropriate.
Classification: Original Research, Geriatric Therapeutics
Keywords: Antipsychotic drugs, STOPP criteria, Health services for the Aged, Geriatric, Pharmacoepidemiology
Introduction
Optimization of drug use by older adults remains a priority. Recognition of this need has led to creation of explicit measures that suggest optimal medication practices for older adults, including the Beers’ Criteria list1 and Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions (STOPP) criteria.2 Similarly, the Choosing Wisely initiative3 works to promote changes in health care to avoid unnecessary tests, treatments, and procedures for patients. These quality indicators help clinicians and health system managers identify situations where risks from specific medications and procedures may outweigh benefits. Antipsychotic drugs are included among these explicit measures1, 2, 3 as potentially inappropriate medications.
The high use of antipsychotic drugs by older adults is a concern due to their known increased risk of adverse drug events,4, 5, 6, 7, 8 which include akathisia,9 movement disorders,10 confusion,11, 12 pneumonia,13 falls,14 cardiovascular effects (eg, hypertension, dyslipidemia, and obesity),15 hypothyroidism,16, 17, 18 neuroleptic malignant syndrome,19 and death.19, 20 In 2005, the US Food and Drug Administration (FDA) and Health Canada issued black box warnings regarding the increased risk of mortality in older adults with dementia treated with second-generation antipsychotic drugs.4, 21, 22, 23 In response to observational studies that identified this risk, with the use of both typical and atypical antipsychotic drugs,19, 20,23 the FDA extended this black box warning to include all antipsychotic drugs in 2008.22, 24 As a result, antipsychotic agents are only recommended for use in those with a psychotic disorder or symptoms of dementia that have not responded to nonpharmacologic treatment.25, 26, 27, 28, 29, 30 Despite existing quality indicators and limited indications approved by drug regulatory bodies, antipsychotic agents continue to be used off-label.4, 8,31, 32, 33 Many times, off-label antipsychotic drug use occurs where precautions exist due to concomitant health issues (eg, Parkinsonism or history of falls), or where drug interactions exist (eg, augmented anticholinergic burden resulting in dry mouth or blurred vision.4 Sensitivity to antipsychotic agent adverse effects in older adults is potentially related to age-related changes in the brain's response to these agents,34 changes in the blood-brain barrier,35, 36 and/or changes in drug metabolism and elimination.37, 38
We were interested in antipsychotic agent prescribing to older adults in Nova Scotia, Canada. We also wanted to explore concordance with the STOPP criteria that recommends antipsychotic drugs be avoided in those at risk of falls. We conducted a retrospective observational study using Nova Scotia administrative health data to identify annual trends in the dispensation of antipsychotic drugs to older persons (Objective 1). Additionally, with a continuous 4-year cohort, we identified the postdischarge continued dispensation of antipsychotic drugs in older persons who had experienced a fall-related hospitalization (Objective 2).
Methods
Sources of data
Nova Scotia Seniors’ Pharmacare Program Database
The Nova Scotia Seniors’ Pharmacare Program Database (NSSPP) is a provincial drug insurance plan for eligible residents of Nova Scotia, aged 65 years and older qualifying for provincial health coverage (https://novascotia.ca/dhw/pharmacare/seniors-pharmacare.asp). This database was used to identify older adults aged 66 and older for Objectives 1 and 2 in separate data extractions: Objective 1 is based on annual cohorts, whereas Objective 2 has a 4-year single cohort.
Nova Scotians may choose to enroll in this provincially funded drug plan at age 65 years. Opting in requires registration and payment of an annual premium and a copayment, both with an annual maximum (exceptions exist for low-income seniors).39 The NSSPP provides benefits for approximately 66% of this older population.40 Approximately 92% of NSSPP beneficiaries live in the community; 8% live in a variety of care-based settings long-term care facilities). Nova Scotians are excluded from the NSSPP if they receive benefits from a federal government drug insurance program (eg, Veterans Affairs Canada or Non-Insured Health Benefits for First Nations People and Inuit), Nova Scotia Family Pharmacare, or any private plan that covers most medications and supplies. Nova Scotians who qualify for NSSPP but choose to pay for prescriptions themselves are not included in the NSSPP database.
The NSSPP database records prescriptions dispensed in community pharmacies to program beneficiaries who are living in the community or long-term care facilities. Prescription claims data from the NSSPP include demographic details (eg, age and sex) and information on prescriptions dispensed, including the generic and brand name of the medication, strength, quantity, days supplied, and cost. NSSPP data do not contain medications administered in hospitals, on discharge, or in emergency departments.
World Health Organization Anatomical Therapeutic Chemical Classification System codes
Antipsychotic drugs were identified by 2015 World Health Organization Anatomical Therapeutic Chemical Classification System (codes for data extraction for both Objectives 1 and 2 (https://www.whocc.no/atc_ddd_index/) (Appendix 1).
Canadian Institute of Health Information Discharge Abstract Database
The Canadian Institute of Health Information Discharge Abstract Database (DAD) records acute patient discharge information from 33 acute care facilities in Nova Scotia (https://www.cihi.ca/en/discharge-abstract-database-metadata). The DAD was used for Objective 2.
Participants
Trends in antipsychotic dispensations (Objective 1)
NSSPP claims data were used to determine the annual prevalence, sex, and age categories of NSSPP beneficiaries aged 66 years and older who received at least 1 dispensation of an antipsychotic drug during a fiscal year between April 1, 2009, and March 31, 2014. Each year, the cohort differs as beneficiaries aged, moved, died, or opted in or out of the program.
Antipsychotic dispensations before and following fall-related hospitalization (Objective 2)
Our second objective was to explore concordance with the STOPP criteria that recommends antipsychotic drugs be avoided in older adults at risk of falls.2 NSSPP claims and DAD data were linked to determine unique NSSPP beneficiaries aged 66 years and older with a fall-related hospitalization 100 days following dispensation of an antipsychotic drug between April 1, 2009, and March 31, 2013. These individuals are at a high risk of falls because a previous fall is among the greatest predictors for future falls.41, 42, 43 Although our study period began April 1, 2009, a 100-day window was required at the beginning to identify antipsychotic drug dispensations. Our first fall-related hospitalization was included after May 13, 2009. This design was chosen to provide proximity between the drug supply and the date of the fall, establishing the possible contribution (ie, biologic plausibility) of the antipsychotic drug to the fall-related hospitalization. The choice of a 100-day period reflects the NSSPP usual reimbursement of up to a 100-day drug supply, and would suggest that a patient would still have had access to the antipsychotic drug.
Design
The NSSPP database, the DAD, and Nova Scotia vital statistics for deaths are housed at Dalhousie's Health Data Nova Scotia data repository (https://medicine.dal.ca/departments/department-sites/community-health/research/hdns/health-databases.html). Linkage occurred using unique de-identified and encrypted identifiers based on a patient's Medical Services Insurance number. Following data linkage by Health Data Nova Scotia, person-specific, anonymized, and categorized results were supplied to the study statistician (KM). Length-of-stay and disposition (discharge or death) were identified for the fall-related hospitalizations. As well, surviving patients who received an antipsychotic drug dispensation during the 100 days following discharge from hospital were identified. We did not capture the number of patients with multiple fall-related hospitalizations in each fiscal year; only the first fall-related hospitalization was evaluated.
Statistical analysis
For Objective 1, descriptive statistics were performed to summarize population characteristics (sex and age categories) of NSSPP beneficiaries who received at least 1 antipsychotic drug dispensation in a fiscal year, and the types (atypical vs typical) and generic name of the antipsychotic drug dispensed. We reported counts and frequencies for categorical and continuous variables. Annual trends in antipsychotic drug dispensations were analyzed using the Cochrane-Armitage trend test. Cochran-Armitage tests for trends in binomial proportions across levels of either a single factor or a covariate and can detect trends in data that are not ideal for more traditional statistical tests.44 Logistic regression models were used to model the risk of potentially inappropriate therapy (ie, antipsychotic drugs dispensed to older adults with an increased risk of falls) and covariates identified a priori: year of admission, sex, length of stay, days supply, and age category. All variables were entered into a multivariate model where adjusted odds ratios and 95% CIs were reported. Significance was accepted as a P value < 0.05. All statistical analysis was completed using SAS version 9.3 (SAS Institute Inc, Cary, North Carolina).
This research received ethics approval from the Health Sciences Research Ethics Board, Dalhousie University, Halifax, Nova Scotia (#2014-3302), with subsequent renewals. Approval for the research study, including data linkage, was obtained from the Health Data Nova Scotia Data Access Committee.
Results
Trends in antipsychotic dispensations (Objective 1)
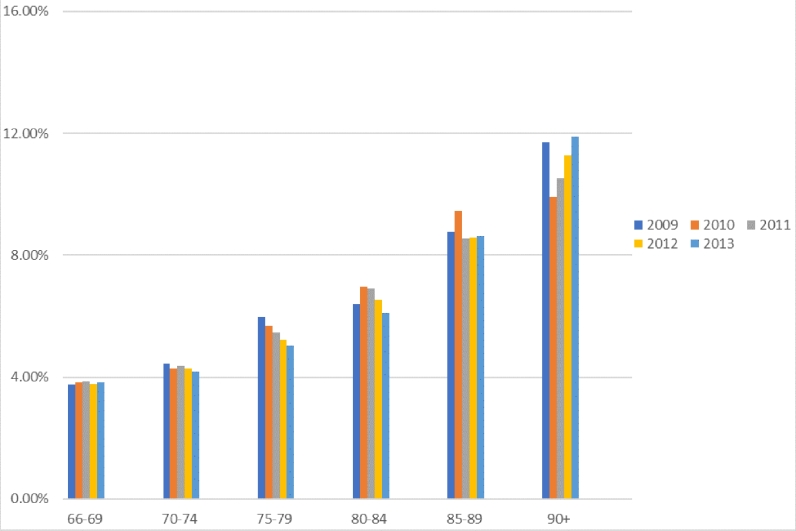
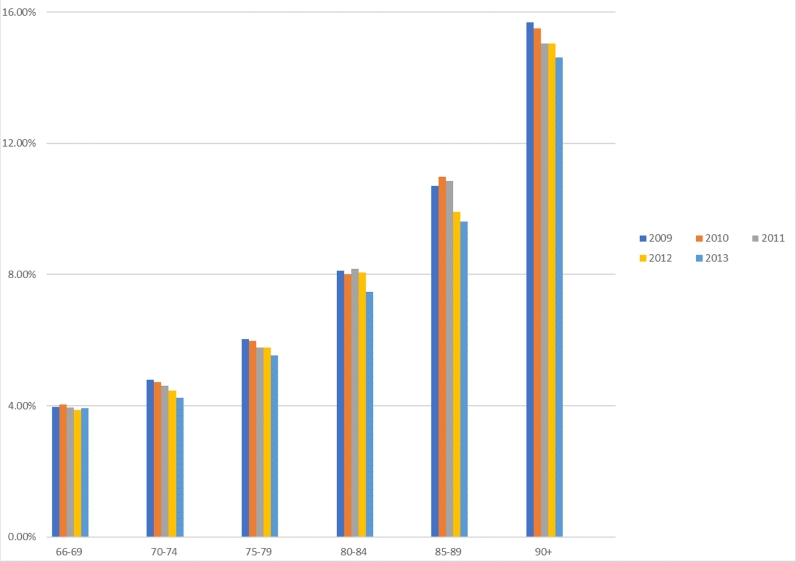
We identified that in each year observed approximately 6% of eligible NSSPP beneficiaries received at least 1 antipsychotic drug dispensation. Of approximately 6000 persons in each year's cohort, the proportion of women varied from 65% (2013) to 67.5% (2009). Figure 1 and Figure 2 show the cohort categorized by age and sex (further details in Appendix 2).
Fig. 1.
Percent of eligible male Nova Scotia Seniors’ Pharmacare Program beneficiaries receiving at least 1 antipsychotic drug dispensation per year, by age category and fiscal year (April 1, 2009–March 31, 2014).
Fig. 2.
Percent of eligible female Nova Scotia Seniors’ Pharmacare Program beneficiaries receiving at least 1 antipsychotic drug dispensation per year, by age category and fiscal year (April 1, 2009–March 31, 2014).
Table 1 shows the antipsychotic dispensations made to our total cohort by generic drug name. Second-generation antipsychotic drugs—risperidone and quetiapine—made up more than 60% of the antipsychotic drug prescriptions dispensed.
Table 1.
Individual antipsychotic drugs dispensed to eligible Nova Scotia Seniors’ Pharmacare Program beneficiaries receiving at least 1 antipsychotic dispensation per year, by fiscal year (April 1, 2009–March 31, 2014).*
| Antipsychotic drugs dispensed | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| First generation | |||||
| Chlorpromazine | 137 (2.3) | 130 (2.2) | 120 (2.0) | 116 (1.9) | 109 (1.8) |
| Flupentixol | 28 (0.5) | 30 (0.5) | 37 (0.6) | 35 (0.6) | 38 (0.6) |
| Fluphenazine | 26 (0.4) | 21 (0.4) | 22 (0.4) | 27 (0.5) | 22 (0.4) |
| Haloperidol | 336 (5.7) | 412 (6.8) | 405 (6.7) | 450 (7.5) | 446 (7.4) |
| Levomepromazine or methoprazine | 285 (4.8) | 259 (4.3) | 270 (4.5) | 254 (4.2) | 237 (4.0) |
| Loxapine | 86 (1.5) | 81 (1.3) | 89 (1.5) | 84 (1.4) | 76 (1.3) |
| Periciazine | 8 (0.1) | 6 (0.1) | < 5 | < 5 | < 5 |
| Perphenazine | 229 (3.9) | 218 (3.6) | 192 (3.2) | 177 (2.9) | 163 (2.7) |
| Pimozide | 27 (0.5) | 29 (0.5) | 25 (0.4) | 25 (0.4) | 23 (0.4) |
| Prochlorperazine | 530 (8.9) | 523 (8.7) | 460 (7.6) | 430 (7.1) | 380 (6.3) |
| Tiotixene or Thiothixene | < 5 | < 5 | < 5 | < 5 | < 5 |
| Trifluoperazine | 112 (1.9) | 111 (1.8) | 99 (1.6) | 89 (1.5) | 108 (1.8) |
| Zuclopenthixol | < 5 | < 5 | < 5 | < 5 | 6 |
| Subtotal | ∼1804 (∼30.3) | ∼1820 (∼30.2) | ∼1719 (∼28.5) | ∼1687 (∼28.0) | ∼1608 (∼26.7) |
| Second generation | |||||
| Aripiprazole | < 5 | < 5 | < 5 | 14 (0.2) | 27 (0.5) |
| Clozapine | 7 (0.1) | 11 (0.2) | 14 (0.23) | 15 (0.3) | 19 (0.3) |
| Olanzapine | 443 (7.5) | 453 (7.5) | 458 (7.6) | 459 (7.6) | 447 (7.5) |
| Quetiapine | 1780 (29.9) | 2003 (33.1) | 2212 (36.6) | 2308 (38.2) | 2380 (39.6) |
| Risperidone | 1910 (32.1) | 1753 (29.0) | 1626 (26.9) | 1538 (25.5) | 1519 (25.3) |
| Ziprasidone | < 5 | < 5 | < 5 | < 5 | < 5 |
| Subtotal | ∼4140 (∼69.6) | ∼4220 (∼69.8) | ∼4310 (∼71.3) | 4334 (∼71.8) | ∼4392 (∼73.2) |
| Total | 5946 | 6044 | 6040 | 6029 | 6004 |
Values are presented as n (%).
Antipsychotic drug dispensations before and following fall-related hospitalization (Objective 2)
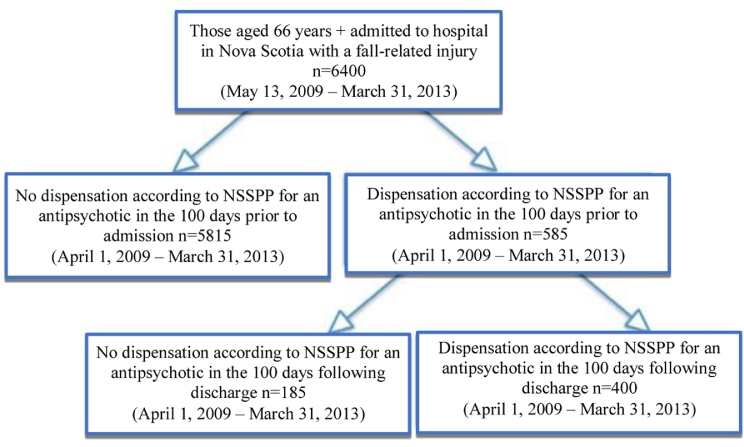
There were 585 eligible NSSPP beneficiaries who received at least 1 antipsychotic drug dispensation during the 100 days before a fall-related hospital admission between May 13, 2009, and March 31, 2013 (Figure 3). Of these, 62 (10.6%) died in hospital. Of 523 surviving beneficiaries, the majority— 400 (76.5%)—had an antipsychotic drug dispensation within 100 days of discharge. The age and sex breakdown of the NSSPP beneficiaries who survived a fall-related hospitalization that was preceded by at least 1 antipsychotic drug dispensation in the 100 days prior is shown in Table 2. Table 3 shows the distribution of individual antipsychotic drugs dispensed before and after a fall-related hospitalization.
Fig. 3.
Cohort for Objective 2 (post discharge continued dispensation of antipsychotic drugs in older persons who had experienced a fall-related hospitalization). NSSPP = Nova Scotia Seniors’ Pharmacare Program. *Only data from NSSPP; older adults may have received prescriptions from other sources such as private insurance.
Table 2.
Age category and sex of eligible Nova Scotia Seniors’ Pharmacare Program beneficiaries who experienced a fall-related hospitalization, after dispensation of an antipsychotic drug during the 100 days before the fall (April 1, 2009–March 31, 2013).*
| Sex | Age group, y† |
Total | |||||
|---|---|---|---|---|---|---|---|
| 66-69 | 70-74 | 75-79 | 80-84 | 85-89 | 90+ | ||
| Female | 32 (64.0) | 42 (63.6) | 59 (67.1) | 81 (72.3) | 98 (85.2) | 86 (93.5) | 398 |
| Male | 18 (36.0) | 24 (36.4) | 29 (32.9) | 31 (27.7) | 17 (14.8) | 6 (6.5) | 125 |
| Total | 50 | 66 | 88 | 112 | 115 | 92 | 523 |
Cochran-Armitage trend test P < 0.0001.
Values are presented as n (%).
Table 3.
Individual antipsychotic drugs dispensed to eligible Nova Scotia Seniors’ Pharmacare Program beneficiaries before a fall-related hospitalization and following discharge (April 1, 2009–March 31, 2013).*
| Antipsychotic drug dispensed | During 100 d before fall-related hospitalization | During 100 d following discharge |
|---|---|---|
| First generation | ||
| Chlorpromazine | 6 (1.2) | 6 (1.5) |
| Haloperidol | 23 (4.4) | 14 (3.5) |
| Levomepromazine or methoprazine | 12 (2.3) | 9 (2.3) |
| Loxapine | 8 (1.5) | 8 (2.0) |
| Perphenazine | 12 (2.3) | 8 (2.0) |
| Prochlorperazine | 13 (2.5) | <5 |
| Subtotal | 74 (14.2) | 45 (11.3) |
| Second generation | ||
| Olanzapine | 29 (5.5) | 28 (7) |
| Quetiapine | 238 (45.5) | 195 (48.8) |
| Risperidone | 172 (32.9) | 119 (29.8) |
| Subtotal | 439 (83.9) | 342 (85.6) |
| Flupentixol, pimozide, clozapine, Fluphenazine, periciazine, trifluperazine and prochloperazine after fall† |
10 (1.9) | 13 (3.3) |
| Total | 523 | 400 |
Values are presented as n (%).
Grouped because each were dispensed <5 times during the study period.
No significant predictors for the continuation of antipsychotic drugs following discharge were found. Both univariate and multivariate regression were performed to evaluate the potential predictive value of the fiscal year of admission, sex, length of stay in hospital, and age as predictors of discontinuation of the antipsychotic drug for NSSPP beneficiaries after experiencing a fall-related hospitalization within 100 days of an antipsychotic drug dispensation (Appendix 3).
Discussion
Results from our analysis of annual trends in antipsychotic drug dispensations (Objective 1) showed that each year for 5 years from April 1, 2009, through March 31, 2014, approximately 6% of NSSPP beneficiaries were dispensed at least 1 antipsychotic drug prescription. The rate of dispensation did not vary significantly over the 5 years. Women and older adults were more likely to receive antipsychotic drug dispensations.
A study of community-dwelling adults aged 65 years and older living in the Canadian province of Manitoba showed lower antipsychotic dispensations than we found in our population; 1.35% and 0.59% received second and first-generation antipsychotic drugs, respectively.45 Our data showed that 60% of antipsychotic drug dispensations were for risperidone and olanzapine and that approximately one-third were for first-generation antipsychotic drugs. Although our results are similar in the distribution between first- and second-generation antipsychotic drug dispensations, time frame, and design, the Manitoba study included residents of all ages and was also able to report separately for patients living in nursing homes versus the community.
In studies of older adults in Canada; Japan; Taiwan; Denmark; Finland; France; Germany; Lithuania; Italy; the Netherlands; Norway; Spain; Sweden; Australia; New Zealand; Colombia; and the United States rates of antipsychotic drug prescribing varied widely. Antipsychotic drug use was as low as 0.32% in Colombia and as high as 15% for Taiwanese older adults.45, 46, 47, 48, 49, 50, 51, 52, 53 Some of the studies were in earlier time periods than our investigation; that is, before widespread knowledge of the risks of antipsychotic agents, especially for those with dementia.
The US Medical Expenditure Panel Survey of 2004-2005 (USMEPS) provides a useful description of the characteristics of antipsychotic drug users and a breakdown of the drugs used.46 Based on the self-reported data samples (all age groups), the study estimated that approximately 1.3% of the US population uses antipsychotic drugs, and within this population risperidone (26%), quetiapine (25%), and olanzapine (20%) were the antipsychotic drugs used most frequently. The higher rates of quetiapine dispensations in our study (40% in 2013) may be related to the age of the surveyed individuals (only 13% were older than age 65 years in the USMEPS study), the older survey dates, and possibly to off-label potentially inappropriate use of quetiapine in our cohort for insomnia.8, 54 Although the 10-year-old USMEPS study gave a much clearer description of the socioeconomic status and the race/ethnicity of its participants, it did not focus specifically on an older population and employed survey data subject to recall bias.
Kales et al,55 using time-series methodology, found that in community-dwelling US veterans aged 65 years and older with dementia, quetiapine dispensation increased from 0.35% to 6.09% of all antipsychotic drug prescribing between 1999 and 2005. The greatest increase was before FDA post-black box warning period (2003-2005). There was very little decline in quetiapine use after the FDA black box warning in 2006-2007.55 The authors hypothesized that the period of increase from 1999 to 2005 was related to Veteran's Affairs recommendation to use risperidone and quetiapine (vs other antipsychotics) for behavioral and psychological symptoms of dementia due to a lack of difference in efficacy, a lack of safety warnings for quetiapine, and cost savings.55 They also note that quetiapine may have been prescribed in low doses as a sedative and hypnotic.55 The leveling off of use, they proposed, was related to reluctance to prescribe or to alter seemingly successful therapy after the warnings were released. The strength of this study lies in its longitudinal design; however, it reflects the antipsychotic prescribing in a veteran population, consisting of mainly male patients with dementia diagnoses. Multiple warnings regarding mortality risk in persons with dementia taking antipsychotic drugs had been released before our first year of analysis (ie, 2009). As well, the most commonly used drugs (risperidone and quetiapine) were multisource drugs by the time of our study and were available as both generic and brand-name medications. Thus, we were unable to study the effect of the FDA and Health Canada warnings21, 22, 24 or introduction of multisource drugs. In contrast to Kales et al,55 our mixed-sex population that included both patients with and without a diagnosis of dementia, captured between 2009 and 2014 showed that quetiapine dispensations increased from representing 30% in 2009 of all antipsychotic drug dispensations to 40% in 2014.
In our study, antipsychotic drug dispensations exceeded expectations despite recommendations from guidelines to limit antipsychotic drug prescribing to appropriate indications.2,25, 26, 27, 28, 29, 30 The Canadian Foundation for Healthcare Improvement describes expected antipsychotic use in nursing homes to be between 5% and 15%.56 In our study, with a cohort in which the majority of patients were community-living, we found that there was an annual rate of 6% of older adults receiving at least 1 antipsychotic drug dispensation. We are especially concerned about the issue of off-label antipsychotic drug prescribing quantified by Equale et al,54 who found that 43.8% of all antipsychotic agents (and 66.7% of quetiapine) were prescribed off-label. We were unable to establish evidence of off-label antipsychotic drug use due lack of access to medical information such as diagnosis.
Results from the linked antipsychotic dispensation and fall-related hospitalization data (Objective 2) demonstrate that 585 of NSSPP beneficiaries who were dispensed an antipsychotic drug experienced a fall-related hospitalization. Seventy-seven percent of survivors of a fall-related hospitalization (following the dispensation of an antipsychotic drug in the 100 days prior) received an antipsychotic in the 100 days postdischarge. This finding is distinctly discordant with the STOPP criteria that state that antipsychotic drugs are potentially inappropriate for older adults at risk of falling.2 Those who have had a previous fall are at an increased risk of a future fall41–43 and attempts should be made to decrease antipsychotic drug use in this population.
There were more fall-related hospitalizations in women in our study population. In a report of older adult fallers in the Eastern Health region of Newfoundland,57 the rate of women's fall-related hospitalization was twice that of men. The authors suggest that increased fall-related hospitalization in women may be partially explained by osteoporosis increasing women's potential for more serious injury. It is unclear if, in our cohort, antipsychotic drugs were overlooked as a contributor to falls or whether they were deemed crucial for patient management.
In 2014, approximately one-third of older adults in the United States reported falling.53 One in 5 falls required medical attention, and fractures that occurred in 6% to 10% of falls result in hospitalization and may lead to functional decline, loss of independence, social withdrawal, fear, activity avoidance, and death.58, 59, 60, 67 One of the fall prevention strategies is managing medications that are implicated as contributors to falls.58 Antipsychotic drug use increases the risk of falls.14, 59 Explicit criteria1, 2 and systematic reviews60, 61 advocate for a trial reduction in antipsychotic drug use and cessation if possible after a fall. The implementation of integrated care models in Nova Scotia whereby community and hospital pharmacy services collaborate with other health care professionals to adjust therapy and monitor for future adverse drug events would be useful.
Interventions are required to improve the quality of the prescribing of antipsychotic drugs in older adults at the patient, caregiver, prescriber, health care facility, and system levels. Some jurisdictions have been successful and others unsuccessful62 with interventions to improve prescribing of antipsychotic agents. The following examples highlight some of the successes and failures. Between 2011 and 2014 in Sweden with the assistance of a pay-for-performance model for physicians, the number of antipsychotic drugs being prescribed with no clear indication in older adults aged 75 years and older was reduced by 12%.63 Alternatively, a Canadian academic detailing study initiated in 2014 and based in Ontario Nursing Homes has published preliminary results showing insignificant changes in prescribing of antipsychotic drugs.64 Improvements in processes may improve results as this study continues. In 2013, a Winnipeg long-term-care facility piloted a program to reduce antipsychotic drug prescribing to patients with dementia. Based on the success of their model and early results (27% of 70 dementia patients were de-prescribed antipsychotic drugs over a 6-month period with no negative influence on behavior), in 2014, the Canadian Foundation for Healthcare Improvement (www.cfhi-fcass.ca) became involved in assisting this project achieving a pan-Canadian scope. Currently, the Reducing Antipsychotic Medication Use in Long Term Care collaboration includes 56 facilities from Atlantic Canada to British Columbia. Between 2014 and 2016, Tasmanian long-term-care facility researchers engaged in an educational/audit and feedback intervention with the objective of reducing both antipsychotic drug and benzodiazepine prescribing. By the 6-month evaluation, the prevalence of residents regularly prescribed antipsychotic agents was reduced by 13% (from 21.6%).65
This study represents, to our knowledge, the first time that the continuation of an antipsychotic drug following a fall-related hospitalization has been assessed in Canada. Two previous Canadian studies (Winnipeg and Toronto) have examined the relationship between antipsychotic agents and fall risk at a population level but these studies failed to evaluate prescribing after the fall-related event.66, 67 The study completed in nursing home residents in Winnipeg, Canada, used a case-control design to evaluate the risk of falls associated with use of atypical antipsychotic drugs and demonstrated that more than 150 mg/d quetiapine (odds ratio = 3.6; 95% CI, 1.3–10.2) or 2 mg/d risperidone (odds ratio = 3.1; 95% C, 1.2–7.9) was associated with an increased risk of falling. Olanzapine did not show an increased risk of falling at any dose.66 A population-based cohort study in Ontario, Canada, suggested that a new outpatient prescription for an atypical antipsychotic medication was associated with a 52% increased risk of a serious fall and a 50% increased risk of a nonvertebral osteoporotic fracture67 compared with those who did not initiate atypical antipsychotic therapy.
Strengths and limitations
The choice of retrospective cross-sectional design for our observational study was cost-efficient and allowed us to use person-specific de-identified data at a provincial level. By linking the 2 comprehensive longitudinal databases (NSSPP and DAD databases), we were able to assess the continuation of antipsychotic drug dispensation following a fall-related hospitalization and implement a population wide subnational antipsychotic drug prescribing indicator.
Our heterogeneous population includes both rural and urban and both community and long-term care dwelling adults older than age 66 years with varying levels of socioeconomic status. We have accessed the antipsychotic drug dispensation records of older adults usually excluded from clinical trials. Participants were not excluded because of any diagnosis or care status.
Although the study only captures two-thirds of Nova Scotian older adults and may not be generalizable to all older Nova Scotians, a more comprehensive database (https://novascotia.ca/dhw/ehealth/dis/) available during the summer of 2018 offers the ability to establish the antipsychotic dispensations of all Nova Scotians.
We were unable to incorporate specific patient variables including indications for antipsychotic drug use, comorbidity, cognition, socioeconomic status, multiple morbidities, and severity of illness.70 Patient variables that may have influenced fall risk such as visual impairment and living arrangements (eg, community, residential care facilities, or nursing home) were not available. Our databases did not offer data on genomic analysis or individual drug levels or pharmacokinetic variation. Two of our age categories reflect uneven year ranges, which may make it more challenging to draw conclusions or make comparisons to other age groups.
Our study was based on prescription dispensation data. We used World Health Organization Anatomical Therapeutic Chemical Classification System codes to access our drug data and not drug identification numbers; therefore, we did not record if generic or brand-name drugs were supplied. Because we did not have access to dosage data, we were unable to determine whether antipsychotic drug use was being tapered following the fall-related hospitalizations.
We were unable to detect whether prescription drugs were dispensed but not consumed by patients or whether patients were adherent to prescribed directions. We did not determine treatment adherence using such approaches as refill data. We were unable to determine whether participants were independent for medication management, were sharing medications, or had supported medication management and what the influence of this support would be on medication adherence. We were unable to collect data about medication sharing that may occur in populations of older adults.68, 69 In a previous study that examined the influence of patient hospitalization on adherence determined by administrative data, it was noted that the effect was small at a population level because 70% of patients were never hospitalized and 17% were hospitalized ≤7 days.70 Antipsychotic drugs dispensed during the 100 days before hospitalization may not have been consumed at the time of the fall. Concomitant drug use (both prescription and over the counter), single prescription versus chronic drug use, and nonoral antipsychotic agent use were not included in our research study. Because we did not follow individual patients over time and we did not have access to data relating to switches in antipsychotic medications.
Our fall injury information was restricted to fall-related hospitalizations. Falls that resulted in either no primary care visit or resulted in a visit to a physician's office or walk-in clinic have not been recorded. We did not examine data by characteristics of the prescriber or health care institution where they patients were hospitalized for a fall.
We did not complete a longitudinal analysis but instead made comparisons of repeated cross-sectional analyses. Future work could involve longitudinal data analysis using such approaches as marginal models or generalized estimating equations to better capture the changes in prescription drug use and disease processes over time.
Conclusions
In each of the five fiscal years of our study, approximately 6% of our cohort of Nova Scotian older adults were dispensed at least one antipsychotic with approximately 60% of prescriptions being for a second-generation antipsychotic. Women were dispensed more antipsychotics than men at all ages and had increasing antipsychotic dispensation with increasing age. In our cohort of beneficiaries experiencing a fall-related hospitalization following antipsychotic dispensation in the 100 days prior to the fall, 76.5% had an antipsychotic dispensation within 100 days of hospital discharge. There were no risk factors identified to predict continuation of an antipsychotic after a fall-related hospitalization. Future work should focus on interventions such as validated screening criteria incorporated into computer-assisted order-entry or health care surveillance systems such as medication review to facilitate a significant, manageable and sustainable improvement in falls prevention and patient care. Our study demonstrates that prescribing quality can be assessed on a population level and we look forward to continued evaluation of prescribing in our province, nationally and internationally.
Acknowledgements
K. Matheson completed the statistical analysis. S. Trenaman and B. J. Hill-Taylor drafted the manuscript. D. Gardner provided clinical expertise and manuscript review. I. Sketris developed the project and reviewed the manuscript.
Conflicts of Interest
This work was supported by the Drug Evaluation Alliance of Nova Scotia. The Drug Evaluation Alliance of Nova Scotia provided partial salary support for S. Trenaman and B. J. Hill-Taylor.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.curtheres.2018.08.002.
Appendix 1
Antipsychotic drugs (N05A) dispensed to adults aged 66 years and older enrolled in the Nova Scotia Seniors’ Pharmacare Program between April 1, 2009, and March 31, 2014, included aripiprazole, chlorpromazine, clozapine, flupentixol, fluphenazine, haloperidol, levomepromazine or methoprazine, loxapine, olanzapine, periciazine, perphenazine, pimozide, prochlorperazine, quetiapine, risperidone, tiotixene or thiothixene, trifluoperazine, ziprasidone, and zuclopenthixol. Note that lithium is not included in this list.
Appendix 2
Percent of eligible Nova Scotia Seniors’ Pharmacare Program beneficiaries receiving at least 1 antipsychotic drug dispensation per year, by sex, age category, and fiscal year (April 1, 2009–March 31, 2014).
| Age | 2009 |
2010 |
2011 |
2012 |
2013 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Females | Males | Females | Males | Females | Males | Females | Males | Females | Males | |
| 66-69 | 3.96 | 3.75 | 4.04 | 3.84 | 3.94 | 3.85 | 3.88 | 3.77 | 3.92 | 3.83 |
| 70-74 | 4.80 | 4.45 | 4.73 | 4.29 | 4.60 | 4.37 | 4.46 | 4.30 | 4.25 | 4.18 |
| 75-79 | 6.03 | 5.96 | 5.98 | 5.66 | 5.78 | 5.46 | 5.78 | 5.23 | 5.53 | 5.05 |
| 80-84 | 8.12 | 6.40 | 8.01 | 6.96 | 8.18 | 6.90 | 8.06 | 6.54 | 7.48 | 6.11 |
| 85-89 | 10.70 | 8.75 | 10.99 | 9.45 | 10.86 | 8.55 | 9.90 | 8.57 | 9.61 | 8.63 |
| 90+ | 15.68 | 11.70 | 15.51 | 9.91 | 15.05 | 10.53 | 15.04 | 11.28 | 14.62 | 11.90 |
Appendix 3
Multivariate model estimates for risk of receiving inappropriate therapy within 100 days after a fall with risk factors in eligible Nova Scotia Seniors’ Pharmacare Program beneficiaries receiving at least 1 antipsychotic drug dispensation per year, by sex, age category, and fiscal year (April 1, 2009–March 31, 2013).*
| Variable | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Fiscal year of admission | 0.994 | 0.821–1.203 | 0.9470 |
| Gender (female vs male) | 1.541 | 0.945–2.512 | 0.0829 |
| Length of stay per 30-d increase | 0.958 | 0.8591–1.068 | 0.4421 |
| Days supply | |||
| 30 to <60 vs <30 | 1.208 | 0.779–1.875 | 0.7731 |
| 60 to <90 vs <30 | 1.073 | 0.418–2.755 | |
| 90+ vs <30 | 1.483 | 0.567–3.877 | |
| Age class, y | |||
| 70-74 vs 66-69 | 0.964 | 0.964–2.297 | 0.0881 |
| 75-79 vs 66-69 | 1.369 | 0.580–3.226 | |
| 80-84 vs 66-69 | 1.445 | 0.631–3.308 | |
| 85-89 vs 66-69 | 0.710 | 0.324–1.557 | |
| 90+ vs 66-69 | 0.600 | 0.266–1.352 |
Modeled as the odds of receiving inappropriate therapy within 100 days after a fall.
Appendix D. Supplementary materials
References
- 1.American Geriatrics Society 2015 Beers Criteria Update Expert Panel American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015 Nov;63(11):2227–2246. doi: 10.1111/jgs.13702. [DOI] [PubMed] [Google Scholar]
- 2.O'Mahony D, O'Sullivan D, Byrne S, O'Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015 Mar;44(2):213–218. doi: 10.1093/ageing/afu145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wisely Choosing. Promoting conversations between patients and clinicians [Internet]. 510 Walnut Street, Suite 1700 Philadelphia, PA 19106; 2018 [cited 26 April 2018]. Available from http://www.choosingwisely.org/.\
- 4.Brett J. Concerns about quetiapine. Aust Prescr. 2015 Jun;38(3):95–97. doi: 10.18773/austprescr.2015.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Briesacher BA, Tjia J, Field T, Peterson D, Gurwitz JH. Antipsychotic use among nursing home residents. JAMA. 2013 Feb 6;309(5):440–442. doi: 10.1001/jama.2012.211266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curkovic M, Dodig-Curkovic K, Eric AP, Kralik K, Pivac N. Psychotropic medications in older adults: a review. Psychiatr Danub. 2016 Mar;28(1):13–24. [PubMed] [Google Scholar]
- 7.El-Saifi N, Moyle W, Jones C, Tuffaha H. Quetiapine safety in older adults: a systematic literature review. J Clin Pharm Ther. 2016 Feb;41(1):7–18. doi: 10.1111/jcpt.12357. [DOI] [PubMed] [Google Scholar]
- 8.Pringsheim T, Gardner DM. Dispensed prescriptions for quetiapine and other second-generation antipsychotics in Canada from 2005 to 2012: a descriptive study. CMAJ Open. 2014 Oct 1;2(4):E225–E232. doi: 10.9778/cmajo.20140009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forcen FE, Matsoukas K, Alici Y. Antipsychotic-induced akathisia in delirium: A systematic review. Palliat Support Care. 2016 Feb;14(1):77–84. doi: 10.1017/S1478951515000784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stegmayer K, Walther S, van Harten P. Tardive Dyskinesia Associated with Atypical Antipsychotics: Prevalence, Mechanisms and Management Strategies. CNS Drugs. 2018 Feb;32(2):135–147. doi: 10.1007/s40263-018-0494-8. [DOI] [PubMed] [Google Scholar]
- 11.Tsai MC, Chang PT, Yang CH, Liu ME. The delirium related to oral paliperidone in dementia: a case report. J Clin Psychopharmacol. 2016 Apr;36(2):184–185. doi: 10.1097/JCP.0000000000000472. [DOI] [PubMed] [Google Scholar]
- 12.Vigen CL, Mack WJ, Keefe RS, Sano M, Sultzer DL, Stroup TS. Cognitive effects of atypical antipsychotic medications in patients with Alzheimer's disease: outcomes from CATIE-AD. Am J Psychiatry. 2011 Aug;168(8):831–839. doi: 10.1176/appi.ajp.2011.08121844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nose M, Recla E, Trifiro G, Barbui C. Antipsychotic drug exposure and risk of pneumonia: a systematic review and meta-analysis of observational studies. Pharmacoepidemiol Drug Saf. 2015 Aug;24(8):812–820. doi: 10.1002/pds.3804. [DOI] [PubMed] [Google Scholar]
- 14.Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009 Nov 23;169(21):1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 15.Silva AASD, Ribeiro MVMR, Sousa-Rodrigues CF, Barbosa FT. Association between antipsychotics and cardiovascular adverse events: A systematic review. Rev Assoc Med Bras. 1992 doi: 10.1590/1806-9282.63.03.261. 2017 Mar;63(3):261-267. [DOI] [PubMed] [Google Scholar]
- 16.Liappas J, Paparrigopoulos T, Mourikis I, Soldatos C. Hypothyroidism induced by quetiapine: a case report. J Clin Psychopharmacol. 2006 Apr;26(2):208–209. doi: 10.1097/01.jcp.0000203227.56494.ff. [DOI] [PubMed] [Google Scholar]
- 17.Ramaswamy S, Siddiqui Z, Saharan S, Gabel TL, Bhatia SC. Quetiapine-induced hypothyroidism. J Psychiatry Neurosci. 2005 Jan;30(1):57. [PMC free article] [PubMed] [Google Scholar]
- 18.Poutanen O, Iso-Koivisto E, Tyolajarvi M, Leinonen E. Quetiapine-associated hypothyroidism in young female patients: a report of three cases. Pharmacopsychiatry. 2010 Aug;43(6):237–239. doi: 10.1055/s-0030-1261880. [DOI] [PubMed] [Google Scholar]
- 19.Tse L, Barr AM, Scarapicchia V, Vila-Rodriguez F. Neuroleptic Malignant Syndrome: A Review from a Clinically Oriented Perspective. Curr Neuropharmacol. 2015;13(3):395–406. doi: 10.2174/1570159X13999150424113345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ballard C, Isaacson S, Mills R, Williams H, Corbett A, Coate B. Impact of Current Antipsychotic Medications on Comparative Mortality and Adverse Events in People With Parkinson Disease Psychosis. J Am Med Dir Assoc. 2015 Oct 1;16(10) doi: 10.1016/j.jamda.2015.06.021. 898.e1,898.e7. [DOI] [PubMed] [Google Scholar]
- 21.Health Canada Endorsed Important Safety Information on Atypical Antipsychotic Drugs and Dementia [Internet]. Available from http://www.healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2005/14307a-eng.php?_ga=2.179544032.597193171.1502215244-1788363691.1485272228.
- 22.FDA. Requests Boxed Warnings on Older Class of Antipsychotic Drugs [Internet] 2013. Available from http://wayback.archive-it.org/7993/20161022204622/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116912.htm
- 23.Wang PS, Schneeweiss S, Avorn J, Fischer MA, Mogun H, Solomon DH. Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med. 2005 Dec 1;353(22):2335–2341. doi: 10.1056/NEJMoa052827. [DOI] [PubMed] [Google Scholar]
- 24.Schneeweiss S, Setoguchi S, Brookhart A, Dormuth C, Wang PS. Risk of death associated with the use of conventional versus atypical antipsychotic drugs among elderly patients. CMAJ. 2007 Feb 27;176(5):627–632. doi: 10.1503/cmaj.061250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dyer SM, Harrison SL, Laver K, Whitehead C, Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2017 Nov;16:1–15. doi: 10.1017/S1041610217002344. [DOI] [PubMed] [Google Scholar]
- 26.Schroeck JL, Ford J, Conway EL, Kurtzhalts KE, Gee ME, Vollmer KA. Review of Safety and Efficacy of Sleep Medicines in Older Adults. Clin Ther. 2016 Nov;38(11):2340–2372. doi: 10.1016/j.clinthera.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 27.Alberta Health Services. Clinical Indications for Prescribing Antipsychotic Medication. 2016. Available from https://www.albertahealthservices.ca/assets/about/scn/ahs-scn-srs-aua-prescribing-antipsychotic.pdf.
- 28.Society Alzheimer's. Drugs for behavioral and psychological symptoms. United against Dementia. 2018 [Google Scholar]; Available from https://www.alzheimers.org.uk/sites/default/files/pdf/factsheet_drugs_used_to_relieve_behavioural_and_psychological_symptoms_in_dementia.pdf.
- 29.Prime Minister's challenge on dementia 2020. 2015. Available from https://www.gov.uk/government/publications/prime-ministers-challenge-on-dementia-2020.
- 30.Alexopoulos GS, Streim J, Carpenter D, Docherty JP. Expert Consensus Panel for Using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry. 2004;65 Suppl 2:5,99. [PubMed] [Google Scholar]
- 31.Skoldunger A, Fastbom J, Wimo A, Fratiglioni L, Johnell K. Impact of Inappropriate Drug Use on Hospitalizations, Mortality, and Costs in Older Persons and Persons with Dementia: Findings from the SNAC Study. Drugs Aging. 2015 Aug;32(8):671–678. doi: 10.1007/s40266-015-0287-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Painter JT, Owen R, Henderson KL, Bauer MS, Mittal D, Hudson TJ. Analysis of the Appropriateness of Off-Label Antipsychotic Use for Mental Health Indications in a Veteran Population. Pharmacotherapy. 2017 Apr;37(4):438–446. doi: 10.1002/phar.1910. [DOI] [PubMed] [Google Scholar]
- 33.Connolly A, Taylor D. Factors associated with non evidence-based prescribing of antipsychotics. Ther Adv Psychopharmacol. 2014 Dec;4(6):247–256. doi: 10.1177/2045125314540298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leon C, Gerretsen P, Uchida H, Suzuki T, Rajji T, Mamo DC. Sensitivity to antipsychotic drugs in older adults. Curr Psychiatry Rep. 2010 Feb;12(1):28–33. doi: 10.1007/s11920-009-0080-3. [DOI] [PubMed] [Google Scholar]
- 35.Reeves S, McLachlan E, Bertrand J, Antonio FD, Brownings S, Nair A. Therapeutic window of dopamine D2/3 receptor occupancy to treat psychosis in Alzheimer's disease. Brain. 2017 Apr 1;140(4):1117–1127. doi: 10.1093/brain/aww359. [DOI] [PubMed] [Google Scholar]
- 36.Shah GN, Mooradian AD. Age-related changes in the blood-brain barrier. Exp Gerontol. 1997 Jul-Oct;32(4-5):501–519. doi: 10.1016/s0531-5565(96)00158-1. [DOI] [PubMed] [Google Scholar]
- 37.Aichhorn W, Weiss U, Marksteiner J. Influence of age and gender on risperidone plasma concentrations. J Psychopharmacol. 2005;19:395. doi: 10.1177/0269881105053306. [DOI] [PubMed] [Google Scholar]
- 38.Gareri P, Segura-Garcia C, Manfredi VG, Bruni A, Ciambrone P, Cerminara G. Use of atypical antipsychotics in the elderly: a clinical review. Clin Interv Aging. 2014 Aug;9:1363–1373. doi: 10.2147/CIA.S63942. 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seniors’ Pharmacare Program [Internet]. Available from http://novascotia.ca/dhw/pharmacare/seniors-pharmacare.asp.
- 40.Medical Services Insurance Annual Statistical Tables 12 Months Ending March 31, 2016. 2016.
- 41.Dewan N, MacDermid JC, Grewal R, Beattie K. Risk factors predicting subsequent falls and osteoporotic fractures at 4 years after distal radius fracture-a prospective cohort study. Arch Osteoporos. 2018 Mar;13(1) doi: 10.1007/s11657-018-0445-5. 2032,018-0445-5. [DOI] [PubMed] [Google Scholar]
- 42.Boonen S, Dequeker J, Pelemans W. Risk factors for falls as a cause of hip fracture in the elderly. Acta Clin Belg. 1993;48(3):190–194. doi: 10.1080/17843286.1993.11718306. [DOI] [PubMed] [Google Scholar]
- 43.Nagai K, Yamada M, Komatsu M, Tamaki A, Kanai M, Miyamoto T. Near falls predict substantial falls in older adults: A prospective cohort study. Geriatr Gerontol Int. 2017 Oct;17(10):1477–1480. doi: 10.1111/ggi.12898. [DOI] [PubMed] [Google Scholar]
- 44.Agresti A. 2nd ed. New Jersey: John Wiley & Sons; Hoboken: 1990. Categorical data analysis. [Google Scholar]
- 45.Alessi-Severini S, Dahl M, Schultz J, Metge C, Raymond C. Prescribing of psychotropic medications to the elderly population of a Canadian province: a retrospective study using administrative databases. Peer J. 2013 Sep;1:e168. doi: 10.7717/peerj.168. 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang CC, Farley JF. Patterns and predictors of antipsychotic medication use among the U.S. population: findings from the Medical Expenditure Panel Survey. Res Social Adm Pharm. 2013 May-Jun;9(3):263–275. doi: 10.1016/j.sapharm.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 47.Meng X, D'Arcy C, Tempier R. Trends in psychotropic use in Saskatchewan from 1983 to 2007. Can J Psychiatry. 2013 Jul;58(7):426–431. doi: 10.1177/070674371305800708. [DOI] [PubMed] [Google Scholar]
- 48.Beck CA, Williams JV, Wang JL, Kassam A, El-Guebaly N, Currie SR. Psychotropic medication use in Canada. Can J Psychiatry. 2005 Sep;50(10):605–613. doi: 10.1177/070674370505001006. [DOI] [PubMed] [Google Scholar]
- 49.Yang M, Barner JC, Lawson KA, Rascati KL, Wilson JP, Crismon ML. Antipsychotic medication utilization trends among Texas veterans: 1997-2002. Ann Pharmacother. 2008 Sep;42(9):1229–1238. doi: 10.1345/aph.1L155. [DOI] [PubMed] [Google Scholar]
- 50.Trifiro G, Sini G, Sturkenboom MC, Vanacore N, Mazzaglia G, Caputi AP. Prescribing pattern of antipsychotic drugs in the Italian general population 2000-2005: a focus on elderly with dementia. Int Clin Psychopharmacol. 2010 Jan;25(1):22–28. doi: 10.1097/YIC.0b013e3283334f08. [DOI] [PubMed] [Google Scholar]
- 51.Ravera S, Visser ST, de Gier JJ, de Jong-van den Berg LT. Prevalence, cumulative incidence, monotherapy and combination therapy, and treatment duration of frequently prescribed psychoactive medications in the Netherlands: retrospective database analysis for the years 2000 to 2005. Clin Ther. 2010 Dec;32(14):2457–2466. doi: 10.1016/j.clinthera.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 52.Marras C, Kopp A, Qiu F, Lang AE, Sykora K, Shulman KI. Antipsychotic use in older adults with Parkinson's disease. Mov Disord. 2007 Feb 15;22(3):319–323. doi: 10.1002/mds.21192. [DOI] [PubMed] [Google Scholar]
- 53.Halfdanarson O, Zoega H, Aagaard L, Bernardo M, Brandt L, Fuste AC. International trends in antipsychotic use: A study in 16 countries, 2005-2014. Eur Neuropsychopharmacol. 2017 Oct;27(10):1064–1076. doi: 10.1016/j.euroneuro.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 54.Eguale T, Buckeridge DL, Winslade NE, Benedetti A, Hanley JA, Tamblyn R. Drug, patient, and physician characteristics associated with off-label prescribing in primary care. Arch Intern Med. 2012 May 28;172(10):781–788. doi: 10.1001/archinternmed.2012.340. [DOI] [PubMed] [Google Scholar]
- 55.Kales HC, Zivin K, Kim HM, Valenstein M, Chiang C, Ignacio RV. Trends in antipsychotic use in dementia 1999-2007. Arch Gen Psychiatry. 2011 Feb;68(2):190–197. doi: 10.1001/archgenpsychiatry.2010.200. [DOI] [PubMed] [Google Scholar]
- 56.New National Results: Taking seniors off antipsychotics shows dramatic improvement in care [Internet]. Available from http://www.cfhi-fcass.ca/SearchResultsNews/2016/05/16/new-national-results-taking-seniors-off-antipsychotics-shows-dramatic-improvement-in-care.
- 57.Health Status Report: Seniors' Health. Newsletter. Newfoundland, Canada: Eastern Health; 2016. Report No.: 11. Available from http://www.easternhealth.ca/OurCommunity.aspx?d=1&id=2217&p=379.
- 58.Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged >/=65 Years - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016 Sep 23;65(37):993-998. [DOI] [PubMed]
- 59.Hill KD, Wee R. Psychotropic drug-induced falls in older people: a review of interventions aimed at reducing the problem. Drugs Aging. 2012 Jan 1;29(1):15–30. doi: 10.2165/11598420-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 60.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012 Sep doi: 10.1002/14651858.CD007146.pub3. 12;(9):CD007146. doi(9):CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.van der Cammen TJ, Rajkumar C, Onder G, Sterke CS, Petrovic M. Drug cessation in complex older adults: time for action. Age Ageing. 2014 Jan;43(1):20–25. doi: 10.1093/ageing/aft166. [DOI] [PubMed] [Google Scholar]
- 62.Ralph SJ, Espinet AJ. Use of antipsychotics and benzodiazepines for dementia: Time for action? What will be required before global de-prescribing? Dementia (London). 2017 Jan 1:1471301217746769. [DOI] [PubMed]
- 63.Fastbom J, Johnell K. National indicators for quality of drug therapy in older persons: the Swedish experience from the first 10 years. Drugs Aging. 2015 Mar;32(3):189–199. doi: 10.1007/s40266-015-0242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Desveaux L, Saragosa M, Rogers J, Bevan L, Loshak H, Moser A. Improving the appropriateness of antipsychotic prescribing in nursing homes: a mixed-methods process evaluation of an academic detailing intervention. Implement Sci. 2017 May;12(1) doi: 10.1186/s13012-017-0602-z. 2671,017-0602-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Westbury JL, Gee P, Ling T, Brown DT, Franks KH, Bindoff I, Bindoff A, Peterson GM. RedUSe: reducing antipsychotic and benzodiazepine prescribing in residential aged care facilities. Med J Aust. 2018 May 21;208(9):398–403. doi: 10.5694/mja17.00857. Epub 2018 May 14. [DOI] [PubMed] [Google Scholar]
- 66.Bozat-Emre S, Doupe M, Kozyrskyj AL, Grymonpre R, Mahmud SM. Atypical antipsychotic drug use and falls among nursing home residents in Winnipeg. Int J Geriatr Psychiatry. 2015 Aug;30(8):842–850. doi: 10.1002/gps.4223. [DOI] [PubMed] [Google Scholar]
- 67.Fraser LA, Liu K, Naylor KL, Hwang YJ, Dixon SN, Shariff SZ. Falls and fractures with atypical antipsychotic medication use: a population-based cohort study. JAMA Intern Med. 2015 Mar;175(3):450–452. doi: 10.1001/jamainternmed.2014.6930. [DOI] [PubMed] [Google Scholar]
- 68.Beyene KA, Sheridan J, Aspden T. Prescription medication sharing: a systematic review of the literature. Am J Public Health. 2014 Apr;104(4):e15–e26. doi: 10.2105/AJPH.2013.301823. Epub 2014 Feb 13. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Beyene K, Aspden T, McNeill R, Sheridan J. Modifiable risk factors for prescription medicine sharing behaviours. Res Social Adm Pharm. 2018 Apr doi: 10.1016/j.sapharm.2018.04.005. 6. pii: S1551-7411(17)30874-4[Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 70.Morningstar BA, Sketris IS, Kephart GC, Sclar DA. Variation in pharmacy prescription refill adherence measures by type of oral antihyperglycaemic drug therapy in seniors in Nova Scotia, Canada. J Clin Pharm Ther. 2002 Jun;27(3):213–220. doi: 10.1046/j.1365-2710.2002.00411.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.