Abstract
Objective
To evaluate the effectiveness of rapid response teams using early identification of clinical deterioration in reducing the occurrence of in-hospital mortality and cardiorespiratory arrest.
Data sources
The MEDLINE, LILACS, Cochrane Library, Center for Reviews and Dissemination databases were searched.
Study selection
We included studies that evaluated the effectiveness of rapid response teams in adult hospital units, published in English, Portuguese, or Spanish, from 2000 to 2016; systematic reviews, clinical trials, cohort studies, and prepost ecological studies were eligible for inclusion. The quality of studies was independently assessed by two researchers using the Newcastle-Ottawa, modified Jadad, and Assessment of Multiple Systematic Reviews scales.
Data extractions
The results were synthesized and tabulated. When risk measures were reported by the authors of the included studies, we estimated effectiveness as 1-RR or 1-OR. In pre-post studies, we estimated effectiveness as the percent decrease in rates following the intervention.
Results
Overall, 278 studies were identified, 256 of which were excluded after abstract evaluation, and two of which were excluded after full text evaluation. In the meta-analysis of the studies reporting mortality data, we calculated a risk ratio of 0.85 (95%CI 0.76 - 0.94); and for studies reporting cardiac arrest data the estimated risk ratio was 0.65 (95%CI 0.49 - 0.87). Evidence was assessed as low quality due to the high heterogeneity and risk of bias in primary studies.
Conclusion
We conclude that rapid response teams may reduce in-hospital mortality and cardiac arrests, although the quality of evidence for both outcomes is low.
Keywords: Patient care team, Rapid response teams, Mortality, Heart arrest, Quality of health care, Systematic review
INTRODUCTION
The quality of service provided to hospitalized patients deserves greater attention in tertiary hospitals.(1) Several methods of measuring hospital quality are employed to assess services, including accreditation processes.(2-4) One of the strategies suggested in the accreditation process that may improve quality of care and reduce hospital mortality is the implementation of rapid response teams (RRT), also known as emergency medical teams, code team/blue code teams, or cardiac arrest teams.
Rapid response teams are composed of health professionals dedicated exclusively to providing care to hospitalized patients identified as being at high risk for worsening prognoses. Rapid response teams are implemented with the aim of preventing cardiac arrest in patients admitted to hospital wards and, therefore, reducing in-hospital mortality.(5)
Rapid response team implementation was considered a priority intervention in the American "5 Million Lives" campaign.(6) This campaign was implemented in 2004 by the Institute for Healthcare Improvement,(4) with the objective of decreasing the number of deaths in the United States by 5,000,000 in two years. Since this campaign, the implementation of RRTs has been recommended by most accreditation agencies.(6)
A study conducted in three emergency hospitals in Australia showed that approximately 67% of deaths in hospitalized patients occurred in open ward units.(7) It is estimated that patients who have cardiac arrests generally present with symptoms or clinical signs that predict the occurrence six to eight hours before the event.(5) The most common signs of cardiac arrest among 66% of examined patients are desaturation and hypotension, findings that were verified in several studies conducted in hospitals with different conditions and structures.(7-10)
The idea of a RRT originated from trauma teams trained to recognize the signs of early clinical deterioration and rapidly respond to the needs of trauma patients, first introduced in Australia in 1989.(11) Rapid response team composition often differs across hospitals. Some institutions have teams that comprise medical doctors, intensive care nurses, and physiotherapists,(12,13) and in most hospitals, medical doctors serve as the RRT coordinators.(14) Rapid response teams screen and treat inpatients with signs of clinical deterioration.(15) The failure of the detection of this deterioration can reduce the effectiveness of RRTs.(16) Additionally, RRTs were included as the fifth link in the chain of survival described in the Advanced Cardiac Life Support Subcommittee statement.(17,18)
The effectiveness of RRTs remains controversial because the available evidence regarding their impact is inconsistent.(19-23) In a meta-analysis conducted by the Cochrane Collaboration in 2007, the effectiveness of RRTs could not be definitively concluded, mainly due to the number of studies using inappropriate methodology or having a low level of evidence.(23)
The results of another meta-analysis performed in 2010 demonstrated the effectiveness of RRTs, identifying a significant reduction in the number of cardiorespiratory arrests in adults (relative risk - RR = 0.66, 95% confidence intervals - 95%CI 0.54 - 0.80) but a nonsignificant reduction in mortality (RR = 0.96, 95%CI 0.84 - 1.09).(24) The results of the most recent meta-analysis, which was conducted in 2015 and evaluated studies published up to 2013, indicated the presence of statistically significant reductions in mortality (13%) and cardiac arrests (35%).(25) Subsequently, other studies evaluating RRT effectiveness were published,(19,20,26-29) justifying the need for an updated meta-analysis on this subject.
Thus, we aimed to conduct a systematic review to examine the available scientific evidence examining the effectiveness of RRT in reducing hospital mortality and cardiac arrests. The outcomes studied were reductions in mortality and cardiac arrest occurrences among adult patients admitted to hospital wards.
METHODS
Data source and study selection
A systematic literature review was performed according to the PRISMA guidelines.(30) The research question was developed using the PICOS strategy (Table 1).
Table 1.
PICOS strategy to literature search
| Population | Adult patients admitted by all causes in hospital open units |
| Intervention | Rapid response team with early clinical deterioration identification systems |
| Comparison | Health services to patients in open units that do not use systems for early identification of clinical deterioration and without flow of triggering medical staff |
| Outcomes | Hospital mortality Cardiac arrest in open unit |
| Study design | Before-after ecological studies, clinical trials, cohort studies and meta-analyses |
A search of the MEDLINE (by PubMed), Cochrane Library, Center for Reviews and Dissemination, and LILACS databases was conducted on February 1, 2016, to identify relevant literature; specific search strategies using the syntax and search engine of each database were used to obtain the highest possible sensitivity (Table 2). A manual search of the references of included studies was also conducted. The search was restricted by language (articles in Portuguese, English or Spanish) and date (articles that had been published since 2000).
Table 2.
Article search strategies in electronic databases
| Databases | List of terms |
|---|---|
| MEDLINE (Pubmed) | #1 ("Hospital Rapid Response Team"[Mesh]) AND
"Hospital Mortality"[Mesh] #2 ("Hospital Rapid Response Team"[Mesh]) AND "Heart Arrest"[Mesh] |
| Cochrane Library | (tw:("rapid response team")) AND (tw:("mortality
hospital")) (tw:("rapid response team")) AND (tw:("cardiac arrest")) |
| Centre for Reviews and Dissemination | "rapid response team" AND “mortality” "rapid response team" AND “cardiac arrest” |
| LILACS | (rapid response team) or "RAPID RESPONSE TEAM"
[Palavras] and (mortality) or "MORTALITY, HOSPITAL"
[Palavras] (rapid response team) or "RAPID RESPONSE TEAM" [Palavras] and "PARADA CARDIO-RESPIRATORIA" [Palavras] |
We included studies that enrolled adults and assessed the effectiveness of RRT relative to no RRT in relation to hospital mortality or cardiac arrest in open hospital units. Only pre-post ecological studies, clinical trials, cohort studies, and meta-analyses that reported quantitative measures of either outcome were included.
Articles were independently selected by two researchers. Articles were initially selected based on the title and abstract. Then, duplicate articles and articles that did not meet the inclusion criteria were excluded. When disagreements occurred, the appraisers jointly reviewed the articles to reach a consensus. The full texts of the selected articles were obtained for comprehensive review. The quality of the articles was evaluated using the following tools: the Newcastle-Ottawa Scale (NOS) for cohort studies,(31) the modified Jadad scale for clinical trials,(32) and the Assessment of Multiple Systematic Reviews (AMSTAR) for systematic reviews.(33)
Two researchers also independently performed quality assessments, classifying the articles as good, medium, or poor quality according to the criteria of each scale. When disagreements occurred during quality evaluation, the evaluators jointly reviewed and discussed each article until a consensus was reached. Articles assessed as being of poor quality were excluded from the study.
We also considered the potential impact of novel research on our confidence in the effect estimates reported by the studies. To do so, the quality of evidence was assessed using the GRADE system. Evidence was classified as high (very unlikely that novel research will affect our confidence in the effect estimates); moderate (novel research may have a major impact on our confidence in the effect estimates); low (very likely that novel research may have a major impact on our confidence in the estimate); and too low (the validity of the effect estimates is uncertain).
Data extraction
Information on the study design, population, outcome measures, results and limitations was extracted from each study.
For all studies, the primary association evaluated and extracted was the effect of RRTs on reducing the outcomes of interest. In cohort and case-control studies, this effect was reported as RR or odds ratio (OR). In pre-post studies, the effect was reported as rates during the periods before and after the intervention.
To allow comparison of the impact measures, we pooled the effectiveness estimates extracted from all studies. For cohort and case-control studies, effectiveness was presented as 1-OR or 1-RR. When possible, the effectiveness of pre-post studies was calculated as the percent decrease of the rates of interest following the intervention using the following formula: (preoccurrence rate - post occurrence rate)/preoccurrence rate x 100.
The results are presented for the comparisons of study design and type of outcome.
Statistical analysis
Meta-analyses of primary study results were performed using the inverse variance method in random effects models to compensate for heterogeneity across studies, and the analyses were conducted using Review Manager 5.3 software.
RESULTS
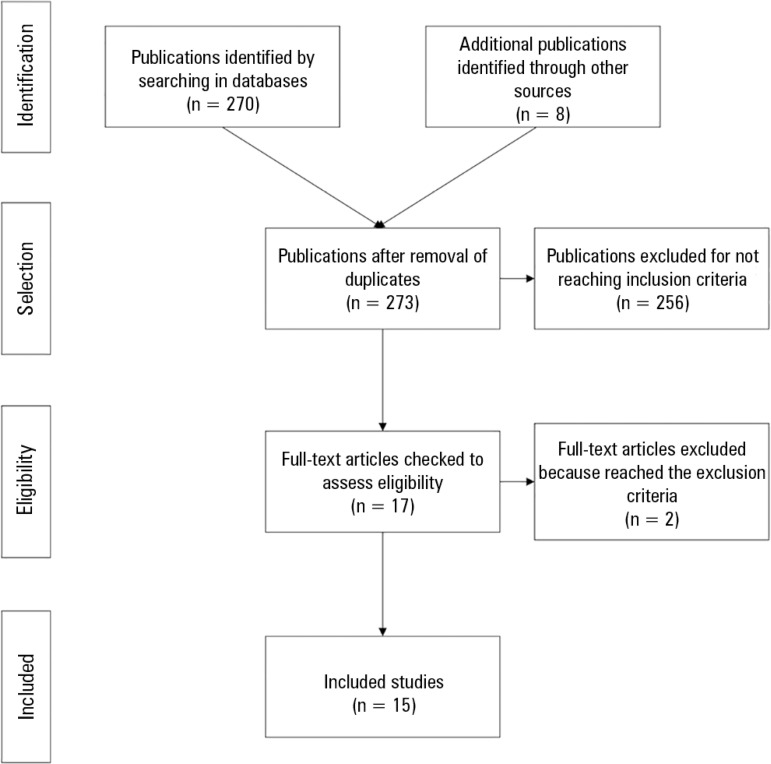
Overall, 278 articles were identified, five of which were duplicates and excluded. We evaluated the titles and abstracts of 273 articles, but 256 of these studies did not meet the inclusion criteria. Thus, 17 full text articles were evaluated, two of which were excluded because they did not meet the required quality standards (Figure 1). Finally, 15 articles published between 2000 and 2016 were included, including 2 clinical trials, 3 meta-analyses and 10 observational studies.
Figure 1.
Diagram of evaluation and selection of articles found.
Table 3 presents the articles included in the review and the results of the initial quality evaluation, including the scores assigned using the NOS(31) for observational studies, modified Jadad scale(32) for clinical trials, and AMSTAR for systematic reviews. Methodological limitations were observed in most studies, but they did not appear to compromise the validity of their results and did not result in exclusion.
Table 3.
Results of paired evaluation on the quality of the observational articles selected
| Article | Checklist | Final conclusion in the scale |
|---|---|---|
| McGaughey et al.(23) | AMSTAR | All items were yes |
| Chan et al.(24) | AMSTAR | No explicit question does not present the record of meta-analysis |
| Maharaj et al.(25) | AMSTAR | All items were yes |
| Salvatierra et al.(26) | Jadad | 8 points (inappropriate concealment) |
| Ludikhuize et al.(29) | NOS | 7 stars (poor comparability) |
| Buist et al.(34) | Jadad | 6 points (inappropriate concealment) |
| DeVita et al.(35) | NOS | 7 stars (poor comparability) |
| Priestley et al.(36) | Jadad | 5 points (inappropriate randomization and concealment) |
| Jones et al.(37) | Jadad | 6 points (inappropriate concealment) |
| Hillman et al.(38) | Jadad | 6 points (inappropriate concealment) |
| Dacey et al.(39) | Jadad | 8 points (inappropriate concealment) |
| Chan et al.(40) | Jadad | 8 points (inappropriate concealment) |
| Konrad et al.(41) | Jadad | 8 points (inappropriate concealment) |
| Beitler et al.(42) | NOS | 7 stars (poor comparability) |
| Gonçales, et al.(43) | Jadad | 8 points (inappropriate concealment) |
The study population assessed, study design employed, outcomes evaluated, effectiveness estimates and their corresponding 95%CI and p-values, and level of evidence classification are described for each study included in this review (Table 4).
Table 4.
Results of clinical trials, before-after ecological and cohort studies included in the systematic review
| Studies | Study design/population | Outcome | Results | Study limitations | Effectiveness (%) |
Quality of evidence |
|---|---|---|---|---|---|---|
| McGaughey et al.(23) | Systematic review Studies published between 1996 and June 2006 Outcome: mortality Intervention: Introduction of early warning scores by RRT |
Mortality | Reduction in mortality | Only two studies were examined; did not conduct economic analyses | Reduction in mortality | Moderate |
| Chan et al.(24) | Systematic review and meta-analysis Studies published between 01 January 1950 and 31 November 2008 Outcome: mortality and cardiopulmonary arrest Intervention: Introduction of RRT |
Mortality Cardiac arrest |
RR 0.96 (95%CI 0.84 - 1.09) RR 0.66 (95%CI 0.54 - 0.80) |
Did not analyze data at the individual level; academic centers were used in most studies reviewed | 4% (95%CI -9 - 16) 0.34 (95%CI 0.20 - 0.46) |
Moderate |
| Maharaj et al.(25) | Systematic review and meta-analysis Studies published between 01 January 1990 and 31 November 2013 Outcome: mortality and cardiopulmonary arrest Intervention: Introduction of RRT |
Mortality Cardiac arrest |
RR 0.87 (95%CI 0.81 - 0.95) (p < 0.001) RR 0.65 (95%CI 0.61 - 0.70) (p < 0.001) |
Did not analyze data at the individual level | 13% (95%CI 5 - 19) 35% (95%CI 30 - 39) |
Moderate |
| Salvatierra et al.(26) | Before-after study Adult patients Intervention: Introduction of medical emergency teams in 10 hospitals in Washington over 31 months, 235344 patients Control: 235718 patients before intervention |
Mortality | RR 0.76 (95%CI 0.72 - 0.80) |
Used historical controls | 24% (95%CI 20 - 28) | Low |
| Ludikhuize et al.(29) | Before-after study Adult patients Intervention: The implementation of RRS was divided into two phases. First, the MEWS (Modified Early Warning Score) and the SBAR communication tools were administered; then after 7 months, RRTs were implemented in 12 Dutch hospitals, 29560 admissions Control: 28298 admissions |
Mortality Cardiac arrest |
OR 0.80 (95%CI 0.64 - 1.00) OR 0.60 (95%CI 0.39 - 0.93) |
Used historical controls | 20% (95%CI 0 - 36) 40% (95%CI 7 - 61) |
Low |
| Buist et al.(34) | Before-after study Adult patients in American hospitals with 300 beds Intervention: Introduction of rapid response teams Controls: historical, 19317 admissions |
Cardiac arrest | OR 0.5 (95%CI 0.35 - 0.73) |
Used historical controls | 50% (95%CI 27 - 65) | Low |
| DeVita et al.(35) | Retrospective analysis of outcomes Adult patients in American hospitals with 622 beds Intervention: Introduction of objective criteria medical emergency team activation |
Cardiac arrest | 6.5 to 5.4/1000 | Observational study; retrospective analysis with confounders that were difficult to control for | 16% | Moderate |
| Priestley et al.(36) | Clinical trial randomized by wards 16 wards in an 800-bed general hospital in England Outcome: mortality Intervention: Introduction of critical care service in wards |
Mortality | OR 0.52 (95%CI 0.32 - 0.85) |
Few hospitals participated; Hawthorne effect; contamination of controls; problems with data collection | 48% (95%CI 15 - 68) | Moderate |
| Jones et al.(37) | Before-after study, analysis of three periods Adult patients in an Australian hospital with 400 beds Intervention: Introduction of medical emergency teams Controls: historical, 16246 admissions |
Cardiac arrest | OR 0.47 (95%CI 0.35 - 0.62) |
Used historical controls; not randomized or blinded; only one hospital was evaluated; cardiac arrest reduction mechanism was not revealed | 53% (95%CI 38 - 65) | Low |
| Hillman et al.(38) | Randomized trial Adult patients in 23 Australian hospitals Outcome: cardiopulmonary arrest and unexpected death Intervention: introduction of medical emergency teams Control: No introduction of medical emergency team |
Mortality Cardiac arrest |
OR 1.03 (95%CI 0.84 - 1.28) OR 0.94 (95%CI 0.79 - 1.13) |
Variations found between hospitals were higher than was anticipated by the researchers | -3% (95%CI -28 - 16) 6% (95%CI -13 - 21) |
Moderate |
| Dacey et al.(39) | Before-after study Adult patients in American hospitals with 350 beds Intervention: Introduction of rapid response teams Controls: historical |
Mortality Cardiac arrest |
2.82 to 2.35/100 hospitalizations (p < 0.001) 7.6 to 3.0/1000 hospitalizations (p < 0.001) |
Not randomized; Hawthorne effect | 16% (p < 0.001) 60% (p < 0.001) |
Low |
| Chan et al.(40) | Prospective cohort Adult patients in an American hospital with 404 beds Intervention: Introduction of rapid response teams Controls: historical, 24193 admissions |
Mortality | OR 0.95 (95%CI 0.81 - 1.11) |
Used historical controls, but adjusted for temporal trends; weak statistical power to identify differences in mortality | 5% (95%CI -11 - 19) | Low |
| Konrad et al.(41) | Before-after study Adult patients Intervention: Introduction of medical emergency teams, 73825 patients Control: 203892 patients before intervention |
Mortality Cardiac arrest |
OR 0.90 (95%CI 0.84 - 0.97) OR 0.74 (95%CI 0.55 - 0.98) |
Used historical controls; delays in the team drive were not evaluated | 10% (95%CI 3 - 16) 26% (95%CI 2 - 45) |
Low |
| Beitler et al.(42) | Prospective cohort Adult patients in American hospitals with 809 beds Intervention: Introduction of rapid response teams Controls: historical, 77021 patients |
Mortality Cardiac arrest |
RR 0.82 (95%CI 0.69 - 0.98) RR 0.49 (95%CI 0.39 - 0.61) |
Used historical controls, but adjusted for temporal trends | 18% (95%CI 2 - 31) 51% (95%CI 39 - 61) |
Low |
| Gonçales et al.(43) | Before-after study Adult patients in Brazilian hospitals with 477 beds Intervention: Introduction of medical emergency teams Control: patients attended over the 19 months before intervention |
Mortality Cardiac arrest |
14.34/1000 after intervention 16.27 before (p <
0.001) 1.69/1000 hospitalizations 3.54 before (p < 0.001) |
Used historical controls; delays in the team drive were not evaluated | 11% (p < 0.001) 52% (p < 0.001) |
Low |
RR - relative risk; 95%CI - confidence intervals; RRT - rapid response teams; MEWS - Modified Early Warning Score; SBAR - situation, background, assessment, recommendation.
A total of 12 studies evaluated mortality. Nine of these studies yielded results indicating that RRTs are associated with a significant reduction in mortality, with estimates varying from 10 - 48%.(25,26,29,34,36,41-43) The three remaining studies did not find RRTs to be effective in achieving reduced mortality.(24,38,40) Of the three meta-analyses included, two reported no significant reduction in mortality.(24,38) However, the most recent meta-analysis conducted in 2015 indicated a statistically significant reduction (Table 4).
Eleven studies considered the occurrence of cardiopulmonary arrests. Nine of these studies, including two meta-analyses, presented results indicating that RRTs are associated with a significant reduction in cardiopulmonary arrest occurrence, with ORs ranging between 0.47 and 0.74.(25,29,35-37,39,41-43) The remaining two studies did not find RRTs to be effective in reducing cardiopulmonary arrest (Table 4).(35,38)
The most recent meta-analysis, which was conducted in 2015 and included studies published until 2013, reported the following pooled measures of RRT effectiveness: 13% for mortality (95%CI 5 - 19) and 35% for cardiopulmonary arrest (95% CI 30 - 39). Two studies that were conducted in 2014 and 2015 and not included in that meta-analysis also reported a significant reduction in mortality, with an RR of 0.76(26) and OR of 0.80.(29) In Brazil, RRTs have been found to be associated with significant reductions in the occurrence of mortality (11%) and cardiac arrest (52%) (Table 4).(43)
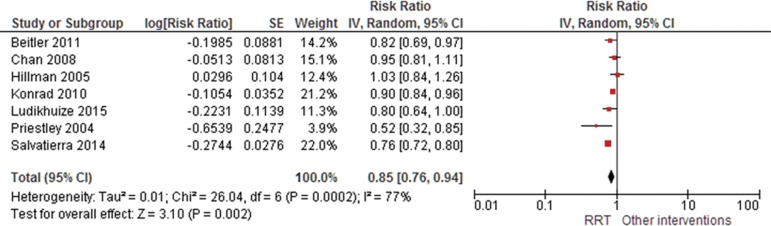
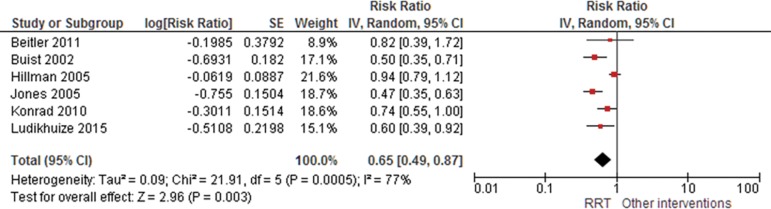
The results of the meta-analysis of studies reporting mortality suggested that RRTs demonstrated a protective effect, with a risk ratio of 0.85 (95%CI 0.76 - 0.94); similar results were identified for the occurrence of cardiac arrest (RR 0.65; 95%CI 0.49 - 0.87). Significant heterogeneity was observed (Figures 2 and 3). Evidence was assessed as low quality by the GRADE system due to high heterogeneity and risk of bias in primary studies.
Figure 2.
Forest plot of the effectiveness of rapid response teams in mortality prevention.
Figure 3.
Forest plot of the effectiveness of rapid response teams in cardiac arrest prevention.
DISCUSSION
This systematic review found that the implementation of RRT can be issued as a B level recommendation because most studies have shown that teams effectively reduce in-hospital mortality and the occurrence of cardiac arrest in adults in open hospital units. Findings from the meta-analysis suggests that RRTs are associated with a 15% reduction in mortality.
Although the evidence supports only a B level of recommendation, it is important to consider ethical issues that may derail the provision of results with the highest level of evidence. The ethics of conducting studies to evaluate the effectiveness of RRTs may be questionable, as one group of patients receives the intervention, while the other is deprived of it. This complicates the use of control groups, the randomized allocation of the intervention, and the blinding of subjects to their received intervention. However, since it is a controversial issue, a clinical trial may be performed.
In an assessment of the optimal epidemiological design for evaluating health service quality, observational cohorts were identified as one of the best possible approaches available.(44) This is why many studies utilized a pre-post design, at times using historical controls, which reduced the strength of the provided evidence. Thus, we believe that the evidence presented in this study may be the optimal way to assess the effectiveness of RRTs.
Nine of the fifteen evaluated studies found a significant reduction in mortality following the implementation of RRT, including a study and a meta-analysis that were recently published in 2015.(25,26,29,36,39,41-43) For cardiorespiratory arrest, nine of the eleven studies reporting this outcome also indicated satisfactory results, showing a statistically significant reduction in cardiorespiratory arrest when hospitals implemented RRTs.(25,29,34,37,39,41-43)
The heterogeneity of the results is due in part to the different settings in which each study was performed, as well as to the different designs that each study used and the number of patients evaluated. Furthermore, the composition of teams in each study and the manner detecting clinical deterioration were not strictly the same, although sufficiently comparable.
Some previous studies have reported on the implementation of RRTs in Brazil.(5,43,45,46) A large private tertiary hospital in São Paulo that instituted an RRT in 2005 evaluated the impact of this implementation. That study demonstrated that RRT implementation was associated with a significant reduction in the rates of cardiorespiratory arrest (from 3.54 to 1.69 per 1,000 discharges) and in-hospital mortality (16.27 to 14.34 deaths per 1,000 discharges).(43) No official data are available regarding the number of Brazilian hospitals in which RRTs are currently implemented.
Other health technology assessment databases were searched for recommendations on the use of RRT, including the databases of the National Institute for Clinical Excellence and Health, National Institute for Health Research Health Technology Assessment Programme, Canadian Agency for Drugs and Technologies in Health, and Agencias y Unidades de Evaluación de Tecnologías Sanitarias, but no recommendations were identified regarding the use of RRTs. Therefore, health technology assessment agencies have not yet established recommendations on the use of RRTs in the countries in which they are located, perhaps because of the lack of evidence provided thus far.
One of this study's limitations was the heterogeneous nature of the hospitals in which RRT have been assessed. Many if the included studies used historical controls, the implications of which have been previously mentioned and discussed. In addition, randomized controlled intervention trials and blinded assessments of the effectiveness of the intervention were not identified. Finally, gray literature was not searched, and language was restricted.
CONCLUSION
We conclude that rapid response teams may reduce in-hospital mortality and cardiac arrest, although the quality of evidence for both outcomes is low.
Footnotes
Conflicts of interest: None.
Responsible editor: Alexandre Biasi Cavalcanti
Funding:
This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), as founders of the Specialization Course in Evaluation of Health Technologies Institute of Technology Assessment in Health (IATS).
REFERENCES
- 1.Keeler EB, Rubenstein LV, Kahn KL, Draper D, Harrison ER, McGinty MJ, et al. Hospital characteristics and quality of care. JAMA. 1992;268(13):1709–1714. [PubMed] [Google Scholar]
- 2.Lindenauer PK, Remus D, Roman S, Rothberg MB, Benjamin EM, Ma A, et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007;356(5):486–496. doi: 10.1056/NEJMsa064964. [DOI] [PubMed] [Google Scholar]
- 3.Schmaltz SP, Williams SC, Chassin MR, Loeb JM, Wachter RM. Hospital performance trends on national quality measures and the association with Joint Commission accreditation. J Hosp Med. 2011;6(8):454–461. doi: 10.1002/jhm.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manzo BF, Brito MJ, Corrêa AR. Implicações do processo de Acreditação Hospitalar no cotidiano de profissionais de saúde. Rev Esc Enferm USP. 2012;46(2):388–394. doi: 10.1590/s0080-62342012000200017. [DOI] [PubMed] [Google Scholar]
- 5.Mezzaroba AL, Tanita MT, Festti J, Carrilho CM, Cardoso LT, Grion CM. Avaliação de 5 anos de atuação de um time de resposta rápida liderado por médico intensivista em hospital universitário. Rev Bras Ter Intensiva. 2016;28(3):278–284. doi: 10.5935/0103-507X.20160045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCannon CJ, Hackbarth AD, Griffin FA. Miles to go: an introduction to the 5 Million Lives Campaign. Jt Comm J Qual Pat Saf. 2007;33(8):477–484. doi: 10.1016/s1553-7250(07)33051-1. [DOI] [PubMed] [Google Scholar]
- 7.Hillman KM, Bristow PJ, Chey T, Daffurn K, Jacques T, Norman SL, et al. Antecedents to hospital deaths. Intern Med J. 2001;31(6):343–348. doi: 10.1046/j.1445-5994.2001.00077.x. [DOI] [PubMed] [Google Scholar]
- 8.Churpek MM, Yuen TC, Edelson DP. Predicting clinical deterioration in the hospital: the impact of outcome selection. Resuscitation. 2013;84(5):564–568. doi: 10.1016/j.resuscitation.2012.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98(6):1388–1392. doi: 10.1378/chest.98.6.1388. [DOI] [PubMed] [Google Scholar]
- 10.Franklin C, Mathew J. Developing strategies to prevent inhospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244–247. [PubMed] [Google Scholar]
- 11.Deane SA, Gaudry PL, Pearson I, Ledwidge DG, Read C. Implementation of a trauma team. Aust N Z J Surg. 1989;59(5):373–378. doi: 10.1111/j.1445-2197.1989.tb01589.x. [DOI] [PubMed] [Google Scholar]
- 12.Mailey J, Digiovine B, Baillod D, Gnam G, Jordan J, Rubinfeld I. Reducing hospital standardized mortality rate with early interventions. J Trauma Nurs. 2006;13(4):178–182. doi: 10.1097/00043860-200610000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Offner PJ, Heit J, Roberts R. Implementation of a rapid response team decreases cardiac arrest outside of the intensive care unit. J Trauma. 2007;62(5):1223–1227. doi: 10.1097/TA.0b013e31804d4968. discussion 1227-8. [DOI] [PubMed] [Google Scholar]
- 14.Braithwaite RS, DeVita MA, Mahidhara R, Simmons RL, Stuart S, Foraida M, Medical Emergency Response Improvement Team Use of medical emergency team (MET) responses to detect medical errors. Qual Saf Health Care. 2004;13(4):255–259. doi: 10.1136/qshc.2003.009324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones D, George C, Hart GK, Bellomo R, Martin J. Introduction of medical emergency teams in Australia and New Zealand: a multi-centre study. Crit Care. 2008;12(2):R46–R46. doi: 10.1186/cc6857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barbosa V, Gomes E, Vaz S, Azevedo G, Fernandes G, Ferreira A, et al. Falha na ativação da equipe de emergência intra-hospitalar: causas e consequências. Rev Bras Ter Intensiva. 2016;28(4):420–426. doi: 10.5935/0103-507X.20160075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, et al. Part 7: Adult advanced cardiovascular life support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18) Suppl 2:S444–S464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 18.Kronick SL, Kurz MC, Lin S, Edelson DP, Berg RA, Billi JE, et al. Part 4: Systems of Care and Continuous Quality Improvement: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18) Suppl 2:S397–S413. doi: 10.1161/CIR.0000000000000258. [DOI] [PubMed] [Google Scholar]
- 19.Rashid MF, Imran M, Javeri Y, Rajani M, Samad S, Singh O. Evaluation of rapid response team implementation in medical emergencies: A gallant evidence based medicine initiative in developing countries for serious adverse events. Int J Crit Illn Inj Sci. 2014;4(1):3–9. doi: 10.4103/2229-5151.128005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Segon A, Ahmad S, Segon Y, Kumar V, Friedman H, Ali M. Effect of a rapid response team on patient outcomes in a community-based teaching hospital. J Grad Med Educ. 2014;6(1):61–64. doi: 10.4300/JGME-D-13-00165.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ANZICS-CORE MET dose investigators Mortality of rapid response team patients in Australia: a multicentre study. Crit Care Resusc. 2013;15(4):273–278. [PubMed] [Google Scholar]
- 22.Howell MD, Ngo L, Folcarelli P, Yang J, Mottley L, Marcantonio ER, et al. Sustained effectiveness of a primary-team-based rapid response system. Crit Care Med. 2012;40(9):2562–2568. doi: 10.1097/CCM.0b013e318259007b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGaughey J, Alderdice F, Fowler R, Kapila A, Mayhew A, Moutray M. Outreach and Early Warning Systems (EWS) for the prevention of intensive care admission and death of critically ill adult patients on general hospital wards. Cochrane Database Syst Rev. 2007;(3):CD005529–CD005529. doi: 10.1002/14651858.CD005529.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010;170(1):18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- 25.Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015;19:254–254. doi: 10.1186/s13054-015-0973-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salvatierra G, Bindler RC, Corbett C, Roll J, Daratha KB. Rapid response team implementation and in-hospital mortality. Crit Care Med. 2014;42(9):2001–2006. doi: 10.1097/CCM.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 27.Moriarty JP, Schiebel NE, Johnson MG, Jensen JB, Caples SM, Morlan BW, et al. Evaluating implementation of a rapid response team: considering alternative outcome measures. Int J Qual Health Care. 2014;26(1):49–57. doi: 10.1093/intqhc/mzt091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee YJ, Park JJ, Yoon YE, Kim JW, Park JS, Kim T, et al. Successful implementation of a rapid response system in the Department of Internal Medicine. Korean J Crit Care Med. 2014;29(2):77–82. [Google Scholar]
- 29.Ludikhuize J, Brunsveld-Reinders AH, Dijkgraaf MG, Smorenburg SM, de Rooij SE, Adams R, de Maaijer PF, Fikkers BG, Tangkau P, de Jonge E, Cost and Outcomes of Medical Emergency Teams Study Group Outcomes Associated With the Nationwide Introduction of Rapid Response Systems in The Netherlands. Crit Care Med. 2015;43(12):2544–2551. doi: 10.1097/CCM.0000000000001272. [DOI] [PubMed] [Google Scholar]
- 30.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 31.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 32.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 33.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10–10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324(7334):387–389. doi: 10.1136/bmj.324.7334.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL, Medical Emergency Response Improvement Team Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care. 2004;13(4):251–254. doi: 10.1136/qshc.2003.006585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Priestley G, Watson W, Rashidian A, Mozley C, Russell D, Wilson J, et al. Introducing Critical Care Outreach: a ward-randomised trial of phased introduction in a general hospital. Intensive Care Med. 2004;30(7):1398–1404. doi: 10.1007/s00134-004-2268-7. [DOI] [PubMed] [Google Scholar]
- 37.Jones D, Bellomo R, Bates S, Warrillow S, Goldsmith D, Hart G, et al. Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care. 2005;9(6):R808–R815. doi: 10.1186/cc3906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, Finfer S, Flabouris A, MERIT study investigators Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005;365(9477):2091–2097. doi: 10.1016/S0140-6736(05)66733-5. Erratum in Lancet. 2005;366(9492):1164. [DOI] [PubMed] [Google Scholar]
- 39.Dacey MJ, Mirza ER, Wilcox V, Doherty M, Mello J, Boyer A, et al. The effect of a rapid response team on major clinical outcome measures in a community hospital. Crit Care Med. 2007;35(9):2076–2082. doi: 10.1097/01.ccm.0000281518.17482.ee. [DOI] [PubMed] [Google Scholar]
- 40.Chan PS, Khalid A, Longmore LS, Berg RA, Kosiborod M, Spertus JA. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506–2513. doi: 10.1001/jama.2008.715. [DOI] [PubMed] [Google Scholar]
- 41.Konrad D, Jäderling G, Bell M, Granath F, Ekbom A, Martling CR. Reducing in-hospital cardiac arrests and hospital mortality by introducing a medical emergency team. Intensive Care Med. 2010;36(1):100–106. doi: 10.1007/s00134-009-1634-x. [DOI] [PubMed] [Google Scholar]
- 42.Beitler JR, Link N, Bails DB, Hurdle K, Chong DH. Reduction in hospital-wide mortality after implementation of a rapid response team: a long-term cohort study. Crit Care. 2011;15(6):R269–R269. doi: 10.1186/cc10547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gonçales PD, Polessi JA, Bass LM, Santos GP, Yokota PK, Laselva CR, et al. Redução de paradas cardiorrespiratórias por times de resposta rápida. Einstein (São Paulo) 2012;10(4):442–448. doi: 10.1590/s1679-45082012000400009. [DOI] [PubMed] [Google Scholar]
- 44.Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ. 1996;312(7040):1215–1218. doi: 10.1136/bmj.312.7040.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Taguti PS, Dotti AZ, Araujo KP, Pariz OS, Dias GF, Kauss IA, et al. Atuação do time de resposta rápida em hospital universitário no atendimento de código amarelo. Rev Bras Ter Intensiva. 2013;25(2):99–105. doi: 10.5935/0103-507X.20130020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Veiga VC. Atuação do time de resposta rápida nos indicadores de melhoria da qualidade assistencial. Campinas: Faculdade de Ciências Médicas, Universidade Estadual de Campinas; 2013. [tese] [Google Scholar]