Abstract
Background and Objectives:
In the past, right hepatectomy via the anterior approach has been regarded as one of the many standard approaches for hepatectomy. However, total laparoscopic right hepatectomy from the anterior approach has been regarded as technically challenging. We report our experience in using the anterior approach in total laparoscopic right hepatectomy for hepatocellular carcinoma (HCC).
Methods:
From June 2013 through December 2015, five consecutive patients underwent total laparoscopic right hepatectomy using the anterior approach, but without the hanging maneuver.
Results:
The mean operative time was 360 (range, 300–480) minutes, and the mean blood loss was 340 (110–600) mL. No patient needed any blood transfusion. There was no conversion to open surgery. Ascites, pleural effusion, and bile leakage occurred in 2, 1, and 1 patients, respectively. No patients expired as a result of the surgery or liver failure. The mean hospital stay was 7 (4–15) days. All patients had R0 resection. After a mean follow-up of 22 (8–33) months, no patients experienced recurrence of disease.
Conclusion:
Total laparoscopic right hepatectomy using the anterior approach is feasible and safe.
Keywords: Anterior approach, Hepatocellular carcinoma, Laparoscopic hepatectomy, Liver neoplasm
INTRODUCTION
Laparoscopic hepatectomy is gaining popularity because of improvements in surgical skill and technology. However, laparoscopic major hepatectomy remains a challenge to liver surgeons. There are great technical hurdles in hemihepatectomy, especially in right hemihepatectomy. Traditionally, surgeons have performed complete mobilization of the right hemiliver before hepatic parenchymal transection. Unfortunately, mobilization of the right hemiliver by the total laparoscopic approach is technically difficult because of its large size and heavy weight. Large and soft hepatocellular carcinomas (HCCs) in the right hemiliver are particularly difficult to handle, as any mobilization increases the risks of tumor rupture, bleeding, or parenchymal tear. In addition, care must be taken to avoid inadvertent injury to the liver, or to the vascular structures during surgery. Therefore, patients with a large liver tumor, particularly a soft HCC, have been considered to be unsuitable for laparoscopic right hemihepatectomy.
To overcome these technical problems, an alternative anterior approach for right hepatectomy has been suggested.1–5 This approach involves prior vascular inflow control, completion of hepatic parenchymal transection, and venous outflow control before complete mobilization of the right liver. The absence of compression and manipulation of the tumor-bearing hemiliver before vascular control has several advantages. This approach avoids squeezing of tumor cells into the systemic circulation and avoids hepatic parenchymal tears. Severe bleeding can still come at the deeper plane of the hepatic parenchymal transection from the right, middle or short hepatic veins, or even from the anterior wall of the inferior vena cava (IVC). Such bleeding is difficult to control without opening up the space in front of the veins before mobilization of the right hemiliver.
This study demonstrated the technical aspects and the short-term outcomes of total laparoscopic right hemihepatectomy for HCC using the anterior approach, but without the hanging maneuver. The protocol was conducted in accordance with the Declaration of Helsinki for research involving human subjects.
METHODS
From June 2013 through December 2015, 5 consecutive patients underwent total laparoscopic right hemihepatectomy via the anterior approach for HCC. The data were collected prospectively but were analyzed retrospectively. Perioperative and short-term outcomes were recorded. All patients gave informed consent for their data to be used for research purposes. The operations were performed by consultant surgeons.
Surgical Procedures
The patient was positioned supine on a split-leg table in a reverse Trendelenburg position. The port sites are shown in Figure 1. Intraoperative ultrasonography (IOUS) was routinely performed to define the number, size, and extent of the liver tumors and the relationship between the liver tumors and the major vascular structures and to mark the hepatic parenchymal transection plane. The right portal pedicle was first dissected from the extra-Glissonian approach by lowering the hilar plate, and it was then slinged with a cotton tape (Figure 2). Hepatic parenchyma transection was performed with a Harmonic scalpel (Ethicon, Cincinnati, Ohio, USA) under low central venous pressure (<5 cm H2O). The hepatic parenchymal transection was started from the anterior surface of the liver to the right side of the liver hilum and then down to the anterior surface of the IVC. The surface of the IVC was properly exposed. Bleeding was controlled with monopolar or bipolar diathermy coagulation or with suture plications with 3-0 Prolene (Ethicon) sutures (Figure 3). Branches of the middle hepatic vein were controlled with clips. (Figures 4, 5) The right portal pedicle was transected with a vascular staple device (Ethicon Endo-Surgery, Cincinnati, Ohio, USA). The short hepatic veins from the IVC were individually controlled with titanium clips, or with suture ligation.(Figure 6). Finally, the right hepatic vein was controlled with a vascular stapling device (Figure 7). After the right hemiliver was completely dissected from the IVC, the related ligaments were divided. The specimen was retrieved in an endobag via a Pfannenstiel incision.
Figure 1.
Port sites.
Figure 2.
Dissection of the right portal pedicle via the extra-Glissonian approach.
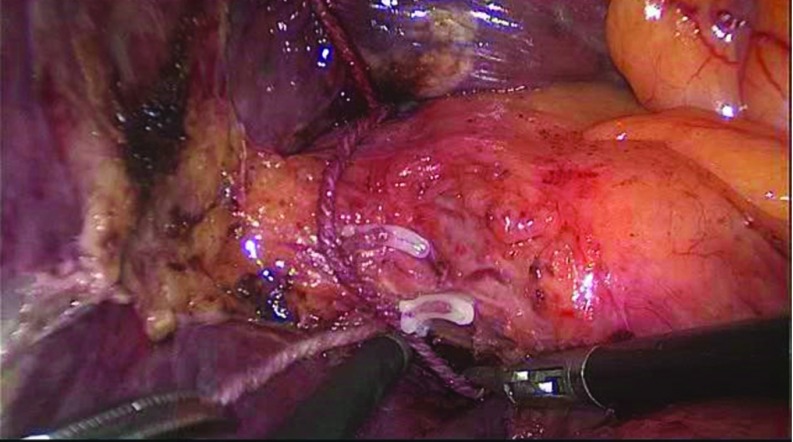
Figure 3.
Control of parenchymal bleeding with bipolar diathermy coagulation.
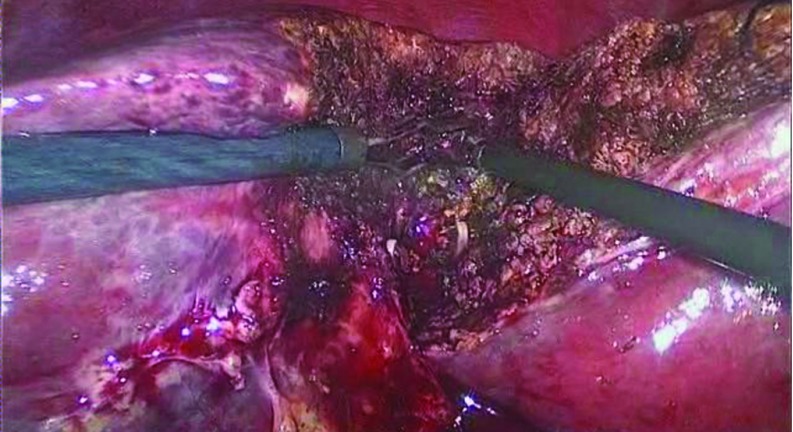
Figure 4.
Control of the segment 5 branch of the middle hepatic vein.
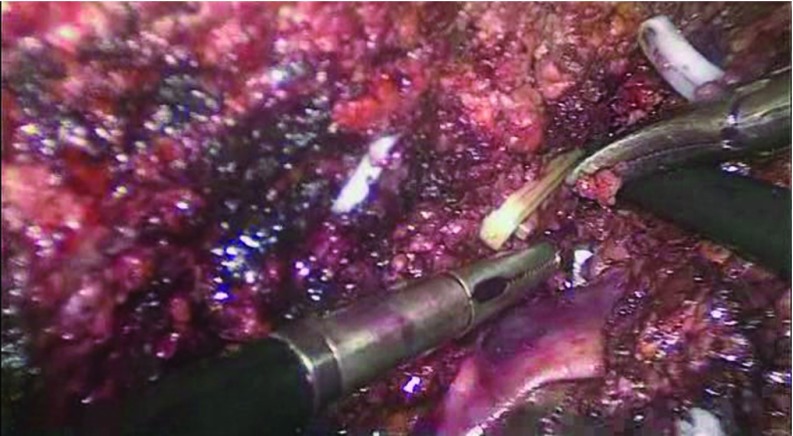
Figure 5.
Control of the segment 8 branch of the middle hepatic vein.
Figure 6.
Exposure of short hepatic veins.
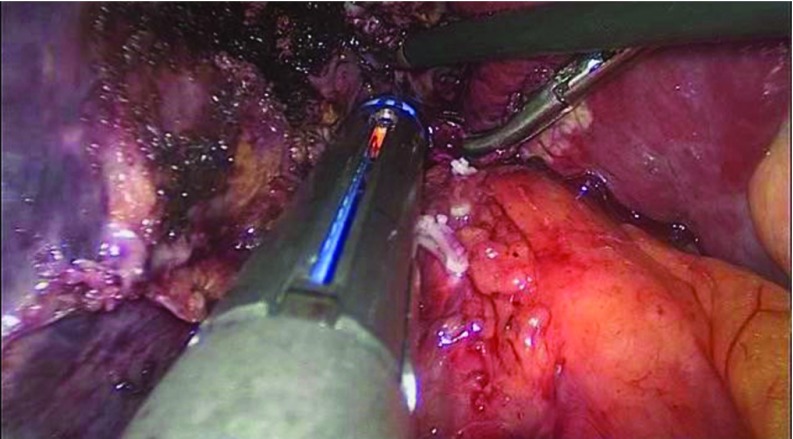
Figure 7.
Control of right hepatic vein with an Endostapler.
RESULTS
During the study period, there were 5 male patients, with a mean age of 49.6 (range, 32–62) years. All were hepatitis B carriers, and 2 had cirrhosis. The mean tumor size was 4.3 (3–6) cm. Two patients had satellite tumor nodules. The mean bilirubin, albumin, and international normalized ratio (INR) were 18.4 (12.4–36.2) μmol/L, 40.9 (37.3–44.9) g/L, and 0.932 (0.87–1.06), respectively.
The mean operative time was 360 (300–480) min, and the mean blood loss was 340 (110–600) mL. No blood transfusion or conversion to open surgery was needed. Postoperative ascites, pleural effusion, and bile leakage occurred in 2, 1, and 1 patients, respectively. No liver failure and no operative morality occurred. The mean hospital stay was 7 (4–15) days. All patients had an R0 resection. The mean surgical resection margin was 2.4 (1–4.5) cm. After a mean follow-up of 22 (8–33) months, all patients had no disease recurrence.
DISCUSSION
The development of minimally invasive surgery in the past 3 decades has had a major impact on clinical practice. Laparoscopic hemihepatectomy becomes possible with new developments in surgical skills and technology that allow easy and secure bleeding control during hepatic parenchymal transection. The advantages of laparoscopic over open hemihepatectomy include earlier recovery, shorter hospital stay, less immunosuppression and better cosmetic outcomes.6,7 Because the abdominal wall and its collateral venous drainage are better preserved, there is less postoperative ascites in cirrhotic patients with portal hypertension.8–13 The Second International Consensus Conference on Laparoscopic Liver Resections (Morioka, Japan, 2014) evaluated the status of laparoscopic hepatectomy and gave recommendations for its development.14 The jury concluded that laparoscopic minor hepatectomy was then the standard approach, but it was still in an assessment stage with adoption by an increasing proportion of surgeons. Laparoscopic major hepatectomy is an innovative procedure that is still in an exploration or learning stage without well-defined risks. Therefore, laparoscopic major hepatectomies should be introduced cautiously into clinical practice.
Laparoscopic major hepatectomy has presented great technical hurdles to liver surgeons, and that explains why it has not been popular. There are several technical difficulties, particularly in right hemihepatectomy. First, laparoscopic mobilization of the right hemiliver is difficult because of its large volume and heavy weight. Large and soft liver tumors, especially HCCs, in the right hemiliver are particularly dangerous. Any mobilization and manipulation before vascular control of the right hemiliver increase the risks of tumor rupture and tumor cell dissemination through the blood stream. Caution should also be exercised to avoid injury of the liver and vascular structures during surgery. The short-term outcomes of laparoscopic major hepatectomies have been reported by experienced surgeons. Dagher et al15 reported 1184 laparoscopic major hepatectomies carried out from 1996 through 2014 in 18 world centers. The most common indication was colorectal liver metastases (37.0%). Seven centers used the hand-assisted or the hybrid approach selectively, mostly at the initial starting stages. Seven centers used the routine vascular inflow control technique. The open conversion rate was 10%, the mean operative time was 291 min, and the mean blood loss was 327 mL. The R0 resection rate was 96.5%. Hwang et al16 reported data from 265 laparoscopic major hepatectomies coming from 12 surgical centers from 2001 through 2011 in Korea.16 The most common indications were primary hepatolithiasis (n = 131) and HCC (n = 62). The most commonly performed liver surgery was left hemihepatectomy (n = 165), followed by right hemihepatectomy (n = 53). The total laparoscopic approach was used in 190 patients, including the robotic approach in 19. The hand-assisted approach and the hybrid approach were used in 3 and 55 patients, respectively. The mean operative time and blood loss were 399.3 min and 836.0 mL, respectively. The intraoperative blood transfusion rate was 24.5%. Open conversion was necessary in 17 patients (6.4%). Postoperative complications and in-hospital mortality occurred in 53 (20%) and 2 (0.75%) patients, respectively. The mean postoperative hospital stay was 12.3 d. R0 resection was achieved in 120 patients with liver tumors, but R1 resection occurred in 8 patients. The mean resection margin was 14.6 mm.
Traditionally, most liver surgeons have preferred complete mobilization of the right hemiliver before hepatic parenchymal transection in the open approach, so that the subsequent transection plane can be opened, and the bleeding points during transection are easier to control. However, mobilization of a large, bulky right hemiliver bearing a large tumor is difficult, particularly with the laparoscopic approach. An alternative approach is to use the anterior approach for right hemihepatectomy. The open technique has been well reported.1–3 The open anterior approach involves vascular inflow control, completion of hepatic parenchymal transection, and then venous outflow control before mobilization and ligament detachment of the right hemiliver. The absence of liver rotation and manipulation before vascular control has several potential advantages. It avoids squeezing any tumor cells into the systemic circulation and any inadvertent injuries to the liver remnant. The total laparoscopic anterior approach also avoids the difficulties encountered in mobilizing a heavy and bulky right hemiliver. The laparoscopic anterior approach for right hemihepatectomy has been reported to be safe and feasible in case reports and small cohort series.17–21 In a large series, Soubrane et al18 reported the results of 30 patients who underwent laparoscopic right hemihepatectomy using the anterior approach. The median operating duration was 360 (210–510) min, the median blood loss was 100 (50–700) mL, and the transfusion rate was 7%. Five patients (16.6%) needed open conversion, including 2 patients in whom the hybrid approach was used. The postoperative morbidity and mortality rates were 23% and 0%, respectively. The median hospital stay was 8 d. The R0 resection rate was 87%. Our current reported outcomes are comparable to those results. A shortcoming of our study was the small sample size.
CONCLUSION
Total laparoscopic right hepatectomy using the anterior approach was feasible and safe in selected patients. A larger case series with a longer follow-up is needed, to determine the proper role of laparoscopic major resection in liver surgery.
Contributor Information
Huan Wei Chen, Department of Liver Surgery, The First People's Hospital of Foshan, Guang Dong, The People's Republic of China..
Fei Wen Deng, Department of Liver Surgery, The First People's Hospital of Foshan, Guang Dong, The People's Republic of China..
Feng Jie Wang, Department of Liver Surgery, The First People's Hospital of Foshan, Guang Dong, The People's Republic of China..
Jie Yuan Li, Department of Liver Surgery, The First People's Hospital of Foshan, Guang Dong, The People's Republic of China..
Eric C. H. Lai, Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, The People's Republic of China..
Wan Yee Lau, Department of Liver Surgery, The First People's Hospital of Foshan, Guang Dong, The People's Republic of China.; Faculty of Surgery, The Chinese Univirsity of Hong Kong, Hong Kong SAR, The People's Republic of China.
References:
- 1. Lau WY. A review on the operative techniques in liver resection. Chin Med J (Engl). 1997;110:567–570. [PubMed] [Google Scholar]
- 2. Liu CL, Fan ST, Cheung ST, Lo CM, Ng IO, Wong J. Anterior approach versus conventional approach right hepatic resection for large hepatocellular carcinoma: a prospective randomized controlled study. Ann Surg. 2006;244:194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wu TJ, Wang F, Lin YS, Chan KM, Yu MC, Lee WC. Right hepatectomy by the anterior method with liver hanging versus conventional approach for large hepatocellular carcinomas. Br J Surg. 2010;97:1070–1078. [DOI] [PubMed] [Google Scholar]
- 4. Chen HW, Lai EC, Wang FJ, et al. Anterior approach for right hepatectomy using the 5-steps stapling technique: a preliminary study. Int J Surg. 2016;16:19–23. [DOI] [PubMed] [Google Scholar]
- 5. Li L, Wang HQ, Wang Q, Yang J, Yang JY. Anterior vs conventional approach hepatectomy for large liver cancer: a meta-analysis. World J Gastroenterol. 2014;20:17235–17243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jackson NR, Hauch A, Hu T, Buell JF, Slakey DP, Kandil E. The safety and efficacy of approaches to liver resection: a meta-analysis. JSLS. 2015;19(1):e2014.00186. 10.4293/JSLS.2014.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Slakey DP, Simms E, Drew B, Yazdi F, Roberts B. Complications of liver resection: laparoscopic versus open procedures. JSLS. 2013;17:46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lai EC, Tang CN, Yang GP, Li MK. Multimodality laparoscopic liver resection for hepatic malignancy: from conventional total laparoscopic approach to robot-assisted laparoscopic approach. Int J Surg. 2011;9:324–328. [DOI] [PubMed] [Google Scholar]
- 9. Lai EC, Tang CN, Yang GP, Li MK. Minimally invasive surgical treatment of hepatocellular carcinoma: long-term outcome. World J Surg. 2009;33:2150–2154. [DOI] [PubMed] [Google Scholar]
- 10. Lai EC, Tang CN, Ha JP, Li MK. Laparoscopic liver resection for hepatocellular carcinoma: ten-year experience in a single center. Arch Surg. 2009;144:143–147. [DOI] [PubMed] [Google Scholar]
- 11. Singhal A, Huang Y, Kohli V. Laparoscopic liver resection for benign and malignant liver tumors. Hepatobiliary Pancreat Dis Int. 2011;10:38–42. [DOI] [PubMed] [Google Scholar]
- 12. Chen H, Wang F, Deng F, Zhen Z, Lai EC, Lau WY. Laparoscopic right hemihepatic vascular inflow occlusion by lowering of the hilar plate. J Laparoendosc Adv Surg Tech A. 2014;24:833–836. [DOI] [PubMed] [Google Scholar]
- 13. Chen YJ, Zhen ZJ, Chen HW, et al. Laparoscopic liver resection under hemihepatic vascular inflow occlusion using the lowering of hilar plate approach. Hepatobiliary Pancreat Dis Int. 2014;13:508–512. [DOI] [PubMed] [Google Scholar]
- 14. Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261:619–629. [DOI] [PubMed] [Google Scholar]
- 15. Dagher I, Gayet B, Tzanis D, et al. International experience for laparoscopic major liver resection. J Hepatobiliary Pancreat Sci. 2014;21:732–736. [DOI] [PubMed] [Google Scholar]
- 16. Hwang DW, Han HS, Yoon YS, et al. Laparoscopic major liver resection in Korea: a multicenter study. J Hepatobiliary Pancreat Sci. 2013;20:125–130. [DOI] [PubMed] [Google Scholar]
- 17. Takahashi M, Wakabayashi G, Nitta H, et al. Pure laparoscopic right hepatectomy by anterior approach with hanging maneuver for large intrahepatic cholangiocarcinoma. Surg Endosc. 2013;27:4732–4733. [DOI] [PubMed] [Google Scholar]
- 18. Soubrane O, Schwarz L, Cauchy F, et al. A conceptual technique for laparoscopic right hepatectomy based on facts and oncologic principles: the caudal approach. Ann Surg. 2015;261:1226–1231. [DOI] [PubMed] [Google Scholar]
- 19. Kim JH, Ryu DH, Jang LC, Choi JW. Lateral approach liver hanging maneuver in laparoscopic anatomical liver resections. Surg Endosc. 2016;30:3611–3617. [DOI] [PubMed] [Google Scholar]
- 20. Ratti F, Cipriani F, Catena M, Paganelli M, Aldrighetti L. Approach to hepatocaval confluence during laparoscopic right hepatectomy: three variations on a theme. Surg Endosc. 2016;30:5015. [DOI] [PubMed] [Google Scholar]
- 21. Chen HW, Deng FW. Pure laparoscopic right hemihepatectomy via anterior approach. Surg Endosc. 2016;30:5621. [DOI] [PubMed] [Google Scholar]