Abstract
Inv(3q26) and t(3:3)(q21;q26) are specific to poor-prognosis myeloid malignancies, and result in marked overexpression of EVI1, a zinc-finger transcription factor and myeloid-specific oncoprotein. Despite extensive study, the mechanism by which EVI1 contributes to myeloid malignancy remains unclear. Here we describe a new mouse model that mimics the transcriptional effects of 3q26 rearrangement. We show that EVI1 overexpression causes global distortion of hematopoiesis, with suppression of erythropoiesis and lymphopoiesis, and marked premalignant expansion of myelopoiesis that eventually results in leukemic transformation. We show that myeloid skewing is dependent on DNA binding by EVI1, which upregulates Spi1, encoding master myeloid regulator PU.1. We show that EVI1 binds to the −14 kb upstream regulatory element (−14kbURE) at Spi1; knockdown of Spi1 dampens the myeloid skewing. Furthermore, deletion of the −14kbURE at Spi1 abrogates the effects of EVI1 on hematopoietic stem cells. These findings support a novel mechanism of leukemogenesis through EVI1 overexpression.
Chr3q26 rearrangements cause overexpression of EVI1 and associate with myeloid neoplasms, but the mechanism behind this association is unclear. Here, using a novel mouse model they show that EVI1 causes premalignant myeloid expansion with suppression of other lineages through upregulation of Spi1/PU.1.
Introduction
Chromosomal rearrangements at 3q26 are associated with poor-prognosis acute myeloid leukemia (AML)1, myelodysplastic syndromes (MDS)2, and myeloproliferative neoplasms (MPN)3, and cause activation of MECOM, a gene that encodes multiple zinc-finger (ZF) transcription factor isoforms, including three isoforms of EVI1. These isoforms, generated via alternative splicing, are nuclear factors harboring two ZF domains. Within the hematopoietic system, Evi1 expression is restricted to long-term and short-term hematopoietic stem cells (HSCs), and under normal conditions, is thereafter during hematopoiesis transcriptionally silent4. Activation of the locus, via either chromosomal rearrangement5 or by proviral insertion6,7, results in marked overexpression of the protein isoforms8.
Within hematopoietic tumors, the association between 3q26 rearrangements and myeloid disease is very high: overexpression of EVI1 is virtually never seen in non-myeloid leukemias or lymphomas. The underlying reason for this specific relationship is unknown, but suggest two possibilities: (i) that myeloid cells are particularly susceptible to the transforming effect of EVI1, or (ii) that the overexpression of EVI1 in hematopoietic stem/progenitor cells (HSPCs) drives cells into the myeloid lineage.
While a number of different mechanisms of action for EVI1 have been suggested (reviewed in ref. 9), it is still unclear how it contributes to leukemogenesis. This is in large part due to the lack of model systems that allow studying the mechanism of EVI1-associated leukemogenesis (reviewed in ref. 9). Experimental efforts to overexpress Evi1 in mouse models have yielded mixed results10–14. These disparate results suggest that EVI1-induced disease is difficult to model in the mouse, perhaps due to technical issues; they also suggest that EVI1 by itself is not sufficient to induce neoplastic disease. While Yamazaki et al.14 previously published an EVI1 transgenic model that genetically mimics the 3q26 human leukemias and underlined the significance of GATA2 enhancer, we report the development of the first Evi1-inducible system that allowed us to uncover a mechanism behind EVI1-associated leukemogenesis.
Using this system, Evi1 induction by doxycycline (DOX) causes a massive perturbation of hematopoietic homeostasis, expanding HSCs, suppressing erythropoiesis and lymphopoiesis, and creating a myeloid-skewed phenotype. Our studies provide insight into the molecular mechanism, as they demonstrate that the myeloid skewing is dependent on DNA binding by EVI1; we further show that EVI1 binds to and upregulates Spi1, encoding PU.1, a master regulator of myelopoiesis. Furthermore, the myeloid skewing is dependent on expression of PU.1. These findings support a model wherein EVI1 acts via PU.1 to push hematopoietic HSPCs towards the myeloid lineage, with concomitant suppression of erythropoiesis and lymphopoiesis; this myeloid expansion, eventually progresses to AML.
Results
Establishment of a mouse model for 3q26 translocations
To mimic the effects of rearrangements at 3q26 in AML, we created a tetracycline (Tet)-inducible allele of Evi1 (termed Evi1TO) in the mouse by inserting seven Tet operons within the first exon (Fig. 1a15), allowing for the induction of all three isoforms of Evi18,9. Evi1TO/TO mice are viable and fertile without phenotype indicating that the allele functions normally in the uninduced state. Through genetic crossings, we then introduced the ubiquitously-expressed16–18 reverse-Tet transactivator (rtTA) allele (Rosa26rtTA/rtTA; ref. 19).
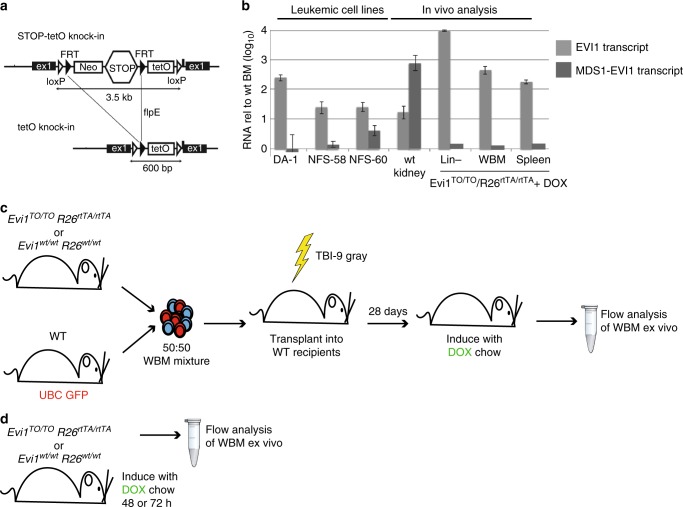
Fig. 1.
Evi1TO mouse model for 3q26-rearranged myeloid malignancies. a Schematic diagram of the Neo-Stop-Tet Operon (NSTO) construct from Tanaka et al.63 that was inserted into the endogenous Evi1 locus by homologous recombination. The construct consists of a neomycin resistance gene and transcriptional Stop cassette flanked by FRT sites, followed by seven Tet operons in succession and a minimal CMV promoter. Following homologous recombination in embryonic stem cells, the Neo-STOP cassette was removed by induction of flpE recombinase. Black triangles represent FRT sites, and white triangles represent loxP sites. b Reverse transcription-quantitative polymerase chain reaction (RT-qPCR) analysis of RNA from cultured leukemic cell lines bearing a provirally-activated EVI1 allele (left-hand columns), or RNA from mouse tissues from wild-type (kidney, an organ with relatively high levels of expression of both Evi1 and Mds1-Evi168), and from DOX-induced Evi1TO, Rosa26rtTA mice. Shown is quantitation of Evi1 and Mds1-Evi1 transcripts. Data is normalized to EVI1 RNA levels in WT bone marrow; log10 scale. c Schematic of competitive transplant long-term induction model. CD45.2 whole bone marrow from either Evi1TO or a WT control with the indicated genotypes was mixed at a 1:1 ratio with WT UBC-GFP-positive bone marrow and transplanted into lethally irradiated recipient mice. Mice were placed on DOX chow at 4 weeks post transplant and analyzed 2, 6, or 10 weeks post induction. Long-term induction experiment was done twice (set A, n = 24, set B, n = 24). Each time point of each set had 8 mice (WT, n = 4, EVI1, n = 4). (Total n = 48). d Schematic of endogenous short-term induction model. Mice were induced with DOX chow for 48 or 72 h and whole bone marrow was harvested for ex vivo analysis
To assess whether Evi1 can be induced in vivo, we tested induction in mice harboring Evi1TO/TO/Rosa26rtTA/rtTA alleles: treatment of these mice with DOX results in dramatic upregulation of the major Evi1 transcript in hematopoietic cells to levels seen in leukemic cells (Fig. 1b); two other mRNA transcripts, encoding shorter isoforms, were also upregulated by DOX (Supplementary Figure 1); however, the longer, MDS1-EVI1 mRNA transcript, (encoding PRDM3, the PR-domain-containing isoform), was not upregulated (Fig. 1b). This accurately models the pattern of MECOM expression commonly seen in human AML with 3q26 rearrangements, in which the EVI1 isoforms are upregulated, but typically not the longer, MDS1-EVI1/PRDM3 isoforms; this particular expression pattern is associated with the poorest prognosis20.
To assess the effect of EVI1 overexpression on hematopoiesis in a context that mimics human myeloid malignancy, in which the oncogene-expressing cells are mixed in with normal hematopoietic cells, we performed competitive transplantations in which the oncogene-expressing bone marrow was mixed 1:1 with WT bone marrow (Fig. 1c); for examination of the short-term effects of EVI1 overexpression, we also fed DOX chow directly to the Evi1TO/TO/Rosa26rtTA/rtTA mice themselves (Fig. 1d).
In the competitive transplantation model, to allow each donor origin to be traced by flow cytometry, the WT competitor was marked with UBC-GFP, while Evi1TO/TO/Rosa26rtTA/rtTA cells were of CD45.2/GFP-negative origin; transplants were performed into lethally irradiated CD45.1/GFP-negative recipients. For a control cohort, we transplanted Evi1WT/WT/Rosa26WT/WT CD45.2/GFP-negative bone marrow cells instead of the Evi1TO/TO/Rosa26rtTA/rtTA cells together with GFP-positive WT cells (Fig. 1c). We documented that the stem cell and progenitor populations from the bone marrow of Evi1TO/TO/Rosa26rtTA/rtTA donors did not differ from that of the control just prior to transplantation (Supplementary Figure 2A). Recipients were analyzed for the engraftment of donors’ BM 4 weeks post transplantation and prior to EVI1 induction, which showed that the two donors (GFP-positive and GFP-negative) were no different, both in control recipients and those receiving Evi1TO/TO/Rosa26rtTA/rtTA cells (Supplementary Figure 2B, left). After confirming successful engraftments, recipients were placed on DOX chow to induce Evi1. After 10 weeks, we analyzed cells in peripheral blood and bone marrow. The mice appeared healthy, and CBCs revealed no cytopenias (not shown). We performed flow analysis of marrow and blood, identifying Evi1TO/TO/Rosa26rtTA/rtTA cells by lack of GFP, and engraftment ratio was determined, which revealed a significant (more than twofold) expansion of the EVI1-overexpressing compartment (Supplementary Figure 2B, right).
EVI1 overexpression suppresses erythropoiesis
Analysis of the erythroid lineage in competitively transplanted mice at 2, 6, and 10 weeks post induction showed a deficiency in the ability of the EVI1-overexpressing cells to effectively contribute to erythropoiesis (Fig. 2a–c). At the 6 and 10 weeks post-induction time points, the number of EVI1-overexpressing Ter119-positive nucleated erythroid cells within the bone marrow was significantly lower than the number of GFP-negative WT cells in control transplant recipients (Fig. 2a). In the peripheral blood of chimeric mice harboring Evi1TO/TO, Rosa26rtTA/rtTA cells, EVI1-overexpressing reticulocyte, and erythrocyte numbers were significantly lower than control at every time point (Fig. 2b, c). During the same time period, there was no difference in platelets (Fig. 2d), or megakaryocytes between EVI1-overexpressing and wild-type GFP cells.
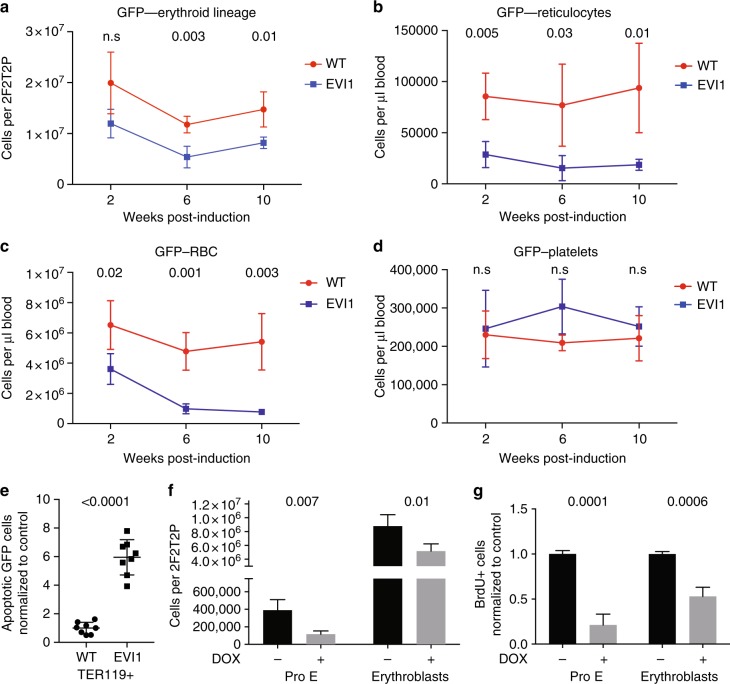
Fig. 2.
EVI1 overexpression suppresses erythropoiesis. a Quantification of erythroid (TER119+) cells overexpressing EVI1 (GFP−) in bone marrow of competitively transplanted recipients harvested 2, 6, or 10 after DOX induction. (WT n = 4 mice, EVI1 n = 4 mice at each time point, total n = 24). b–d Numbers of donor-derived reticulocytes (GFP−, Ter119+, CD71+), erythrocytes (GFP−,Ter119+, CD71−), and platelets (GFP−, low SSC/FSC, CD41+) as indicated at 2, 6, and 10 weeks post induction per microliter of peripheral blood of mice competitively transplanted with DOX-induced Evi1TO, Rosa26rtTA mice or WT cells. (WT n = 4 mice, EVI1 n = 4 mice at each time point, total n = 24). e Quantification of apoptotic (annexin-v+ 7AAD−) erythroid (TER119+) cells overexpressing EVI1 (GFP−) or WT WBM of competitively transplanted recipients, expressed relative to WT GFP− cells from the control transplant, harvested 10 weeks after DOX induction. Each dot represents an individual recipient mouse. (WT = 8 mice, EVI1 = 8 mice). f, g Quantification of total (f) and BrdU-positive (g) proerythroblasts (TER119+low cKit+), and erythroblasts (TER119+ CD71+) in WBM of Evi1TO/TO Rosa26rtTA/rtTA mice harvested 48 h with or without DOX induction. (WT n = 4, EVI1 n = 4). For all panels, error bars represent standard deviation; p values calculated with Student’s t-test
To understand the etiology of the lower numbers of erythroid cells in the EVI1-overexpressing compartment, we quantitated apoptosis and proliferation in erythroid progenitors using flow cytometry; these studies revealed a sixfold increase in apoptosis within the erythroblasts relative to WT cells (Fig. 2e), and a marked drop in the number of, and proliferation of, both proerythroblasts and erythroblasts relative to WT (Fig. 2f, g).
In summary, EVI1 overexpression has a dramatic effect on erythropoiesis and this is mediated by both an increase in apoptosis and a decrease in proliferation.
EVI1 overexpression suppresses lymphopoiesis
We examined the bone marrow at 2–10 weeks post induction for changes in T and B cells; we noted significantly lower numbers of EVI1-overexpressing B-cell lineage cells within the bone marrow at 6 and 10 weeks time points (Fig. 3a). While the number of Evi1TO/TO/Rosa26rtTA/rtTA T cells in the bone marrow was not significantly different from the WT control, examination of blood for lymphocytes showed a marked diminution in both T and B cells from the EVI1-overexpressing compartment: at 10 weeks post induction, EVI1 overexpression caused a decrease in peripheral T cells from ≈1800 cells per μl to ≈750 cells per μl, and nearly eliminated the peripheral B cells completely (Fig. 3b). This was associated with a two to threefold increase in the number of apoptotic bone marrow T and B cells (Fig. 3c).
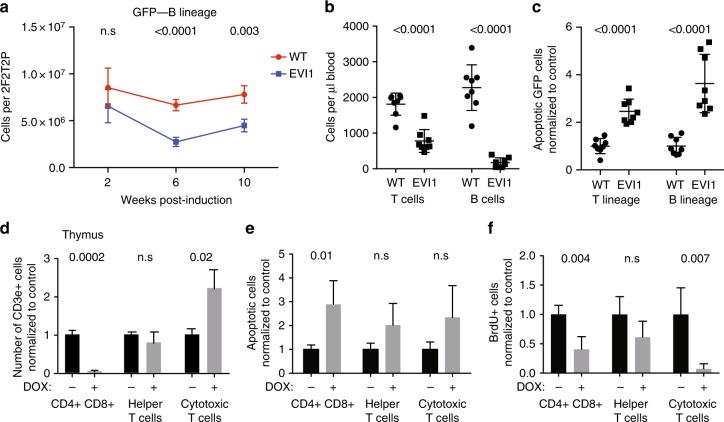
Fig. 3.
EVI1 overexpression suppresses lymphopoiesis. a Quantification of B lymphocytes (B220+) cells overexpressing EVI1 (GFP−) and WT control (GFP−) in WBM of competitively transplanted recipients harvested 2, 6, or 10 after DOX induction. (WT n = 4 mice, EVI1 n = 4 mice at each time point, total n = 24). b Circulating donor-derived T cells (GFP−, CD3e+, CD11b−) and B cells (GFP−, CD19+, CD11b−) in competitively transplanted mice at 10 weeks post induction. Each time point (WT n = 8 mice, EVI1 n = 8 mice). c Quantification of apoptotic (annexin-V+, 7AAD−) T lymphocytes (CD3e+) and B lymphocytes (B220+) overexpressing EVI1 (GFP−) compared to WT (GFP−) in WBM of competitively transplanted recipients harvested 10 weeks after DOX induction. Each dot represents an individual recipient mouse. (WT n = 8 mice, EVI1 n = 8 mice). d Quantification of CD4/CD8 double-positive cells (CD3e+, CD4+, CD8a+), helper T cells (CD3e+, CD4+, CD8a−), and cytotoxic T cells (CD3e+, CD4-, CD8a+) in thymus of Evi1TO/TO Rosa26rtTA/rtTA mice harvested 48 h with or without DOX induction. (WT n = 4, EVI1 n = 4). e Quantification of apoptotic (annexin-v+ 7AAD−) CD4/CD8 double-positive cells (CD3e+, CD4+, CD8a+), helper T cells (CD3e+, CD4+, CD8a−), and cytotoxic T cells (CD3e+, CD4−, CD8a+) in thymi of Evi1TO/TO Rosa26rtTA/rtTA mice harvested 48 h with or without DOX induction. (WT n = 4, EVI1 n = 4). f Quantification of BrdU+ CD4/CD8 double-positive cells (CD3e+, CD4+, CD8a+), helper T cells (CD3e+, CD4+, CD8a−), and cytotoxic T cells (CD3e+, CD4−, CD8a+) in thymi of Evi1TO/TO Rosa26rtTA/rtTA mice harvested 48 h with or without DOX induction. (WT n = 4, EVI1 n = 4). For all panels, error bars represent standard deviation; p values calculated with Student’s t-test
We found that the number of T cells in the marrow was low, which is to be expected: T cells are derived from HSCs in the bone marrow, but at an early stage, migrate from the bone marrow to the thymus, where they complete their development. To better assess the effect of EVI1 overexpression on T cells, we enumerated T cells in the thymus at the double (CD4/CD8)-positive stage, and at the CD4 or CD8 single-positive stage. This revealed a marked diminution of double-positive cells relative to control but little change in CD4-positive T cells (Fig. 3d). Interestingly, there was an increase in CD8-positive T cells (Fig. 3d). To further assess these changes, we assessed apoptosis and proliferation (Fig. 3e, f) and found increased apoptosis only in the double-positive compartment, but decreased proliferation in both the double-positive and CD8 single-positive population.
EVI1 overexpression expands myelopoiesis
At 2 weeks post induction, EVI1-overexpressing and control bone marrows showed the same number of myeloid cells (GFP-negative, CD11b-positive (Fig. 4a) or Ly6G/C-positive (Fig. 4b)). However, at 6 and 10 weeks post induction, there was marked expansion of the EVI1-overexpressing myeloid compartment, from ≈7.5e6 cells/2F2T2P to ≈30e6 cells/2F2T2P for CD11b+ cells, and from ≈12e6 cells/2F2T2P to ≈36e6 cells/2F2T2P for LY6G/C+ cells (Fig. 4a). We also quantified HSCs and myeloid progenitors using flow cytometry at 10 weeks post induction; The expansion of lineage-negative, c-Kit+, Sca-1+ (LSK cells; approximately twofold) was not significant (p > 0.05), but both CMPs and granulocyte-monocyte progenitors (GMPs) were significantly increased (Fig. 4c). By performing colony-forming assay, we found that myeloid colony-forming cells were over 2.5-fold increased relative to controls (Fig. 4d). By flow-based analysis, monocytes/macrophages and granulocytes within the marrow were increased (Fig. 4e). However, blood monocytes were unchanged, and granulocytes were increased but not as significantly as in the marrow. Analysis of annexin-V revealed no increase in apoptosis of the marrow myeloid cells (Fig. 4f). We also assessed the composition of the LSK compartment in the marrows, which contain HSCs and multipotent progenitors (MPPs) using the surface marker phenotype described and detailed by Cabezas-Wallscheid et al.21 (Supplementary Figure 2C, Supplementary Table 1). We found that Evi1 expression expands HSCs, multipotent MPP2s, and the myeloid-biased MPP3 populations, while reducing the erythroid-biased MPP4 populations; no change in MPP1 was seen (Supplementary Figure 2D).
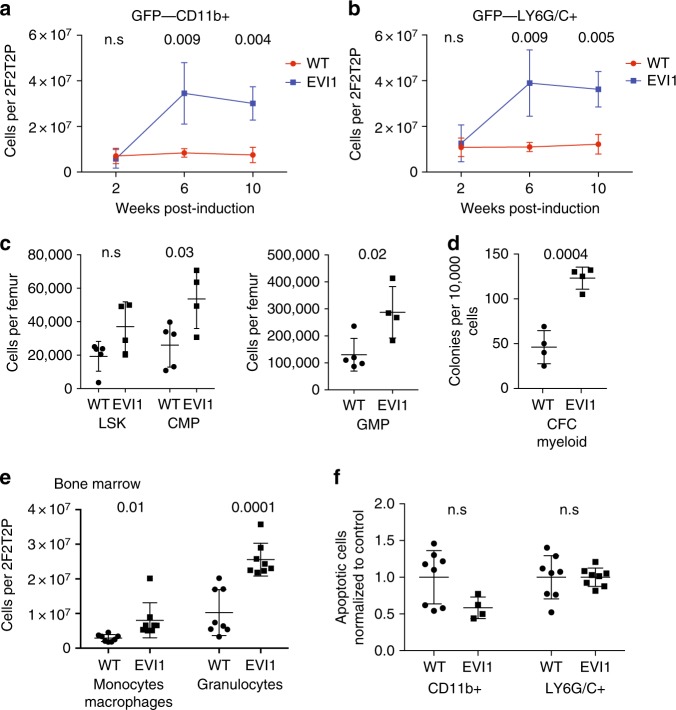
Fig. 4.
EVI1 overexpression expands myelopoiesis. a Quantification of GFP−, CD11b+ myelocytes, either overexpressing EVI1 or WT as indicated in WBM of competitively transplanted recipients, harvested 2, 6, or 10 weeks after DOX induction. (WT n = 4 mice, EVI1 n = 4 mice at each time point, total n = 24). b Quantification of GFP− LY6G/C+ myelocytes, either overexpressing EVI1 or WT in WBM of competitively transplanted recipients harvested 2, 6, or 10 weeks after DOX induction. (WT n = 4 mice, EVI1 n = 4 mice at each time point, total n = 24). c Flow cytometry analysis of progenitor populations from recipient mice after 10 weeks of DOX treatment. Data represents mean number of cells per femur for individual mice. (WT n = 5, Evi1+ n = 4). d Relative numbers of GFP− CFC-myeloid (G−, M and GM-CFC) in bone marrow of competitively transplanted mice 10 weeks post induction, comparing the Evi1TO/TO Rosa26rtTA/rtTA:WT to WT:WT transplants as indicated. (WT n = 8, EVI1 n = 8). e Quantification of GFP− monocyte/macrophage (nucleated, CD11b+, Gr1−) or GFP− granulocytes (nucleated, CD11b+, Gr1+) as determined by imaging flow cytometry in bone marrow of competitively transplanted mice, comparing Evi1TO/TO Rosa26rtTA/rtTA donor cells to WT donor cells, 10 weeks post induction. (WT n = 8, EVI1 n = 8). f Quantification of GFP− apoptotic (annexin-V+ 7AAD−) CD11b+ myelocytes (left) and LY6G/C+ myelocytes (right), comparing WT to EVI1-overexpressing cells in WBM of competitively transplanted recipients harvested 10 weeks after DOX induction. Each dot represents an individual recipient mouse. (WT n = 8, EVI1 n = 8). For all panels, error bars represent standard deviation; p values calculated with Student’s t-test
In summary, these data indicate that Evi1 overexpression induces myeloid expansion via a proliferative and a survival advantage; increased maturation/differentiation from uncommitted progenitors at a higher rate may also play a role.
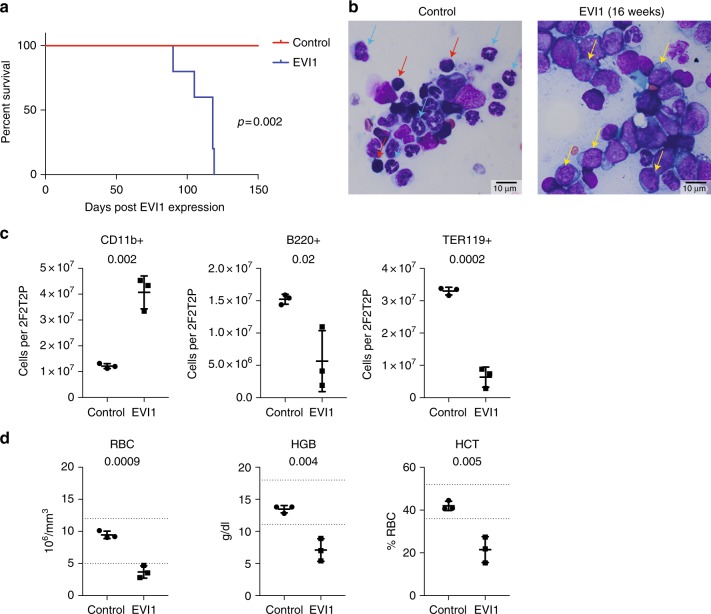
EVI1 overexpression results in AML
To determine if chronic overexpression of EVI1 might result in leukemia, we aged a cohort of five mice, competitively transplanted with a 1:1 mix of WT bone marrow cells:Evi1TO/TO/Rosa26rtTA/rtTA cells, chronically on DOX chow to maintain high-level expression of EVI1. All five mice succumbed, becoming moribund at 90–119 days of DOX treatment (median = 118 days; Fig. 5a; p = 0.002; Fig. 5a); flow and morphological analysis revealed AML in all mice analyzed, with the bone marrow replete with blast forms (Fig. 5b), which, by immunophenotyping by flow cytometry, were positive for Mac1 (CD11b) (Fig. 5c). The peripheral blood revealed severe anemia (Fig. 5d).
Fig. 5.
EVI1 overexpression results in AML with intermediate latency. a Kaplan–Meier curve showing survival of CD45.1 mice that were transplanted with WT:Evi1TO/TO, R26RrtTA/rtTA at a 1:1 ratio with and without DOX induction. Mice were harvested when morbidity presented (survival range = 90–119 days, median = 118 days, n = 5) b Representative Wright-Giemsa-stained bone marrow brush smears from CD45.1 mice that were transplanted with WT:Evi1TO/TO, R26RrtTA/rtTA at a 1:1 ratio without (left) or with (right) DOX induction at the day of harvest. Mice were harvested when morbidity presented. Blue arrows, maturing myeloid forms (metamyelocytes and bands); red arrows, erythroblasts; yellow arrows, leukemic blasts (scale bars: 10 μm). c Quantification of CD11b+ cells (left), B220+ cells (middle), or TER119+ cells (right) using flow cytometry analysis on WBM of CD45.1 mice that were transplanted with WT:Evi1TO/TO, R26RrtTA/rtTA at a 1:1 ratio with and without DOX induction at the day of harvest. Mice were harvested when morbidity presented (n = 3). d Quantification of red blood cells (RBC), hemoglobin (HGB), and hematocrit (HCT) using complete blood count assay performed on PB from CD45.1 mice that were transplanted with WT:Evi1TO/TO, R26RrtTA/rtTA at a 1:1 ratio with and without DOX induction at the day of harvest. Mice were harvested when morbidity presented (n = 3). For all panels, error bars represent standard deviation; p values calculated with Student’s t-test
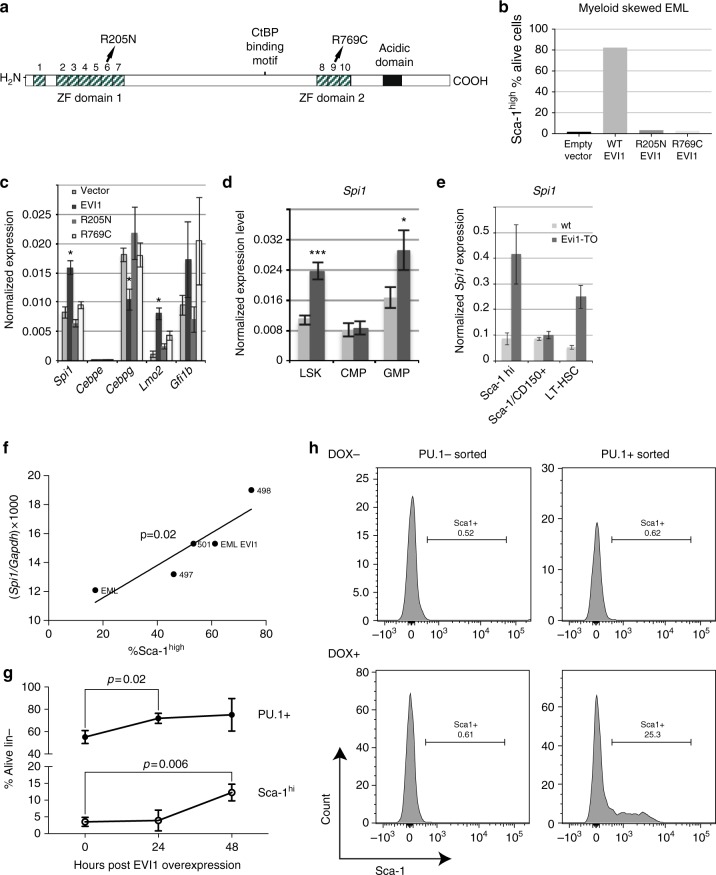
EVI1 myeloid-biased phenotype depends on DNA binding by EVI1
The data shown above indicate that Evi1 overexpression results in suppression of erythroid and lymphoid cells, and expansion of myeloid cells. Since EVI1 harbors two DNA-binding zinc-finger domains (Supplementary Figure 1G; refs. 22,23) and can modulate the transcription of target genes via binding in cis (e.g., refs. 15,24), we wished to determine if the myeloid skewing phenotype induced by EVI1 was dependent on its binding to DNA using two EVI1 mutants (Fig. 6a): EVI1-R205N, which lacks DNA binding via ZF domain18 and EVI1-R769C, which lacks DNA binding via ZF225. However, rather than testing these in our mouse model that would have entailed the development of two new mouse strains, instead we utilized EML cells26, a hematopoietic progenitor cell line that does not express Evi1. Previous analysis of EML cells27,28 indicated that Sca-1 provides an excellent marker for the lineage proclivity of these progenitor cells, with Sca-1lo cells showing high GATA-1 expression and being poised for erythroid differentiation, and Sca-1hi cells expressing high PU.1 expression and being poised for myeloid differentiation27,28. To determine if Sca-1 upregulation depended on the action of EVI1 on downstream targets, we tested the two EVI1 DNA-binding mutants (Fig. 6a, EVI1-R205N and EVI1-R769C) in EML cells for their ability to upregulate Sca-1. Both of these mutations abrogated the upregulation of Sca-1 (Fig. 6b), indicating that the myeloid skewing phenotype requires both ZF1 and ZF2 domains and that the action of EVI1 on downstream target genes is an essential mechanistic link. To investigate this further, we assessed the expression of five key hematopoietic regulators in vector-transduced EMLs, compared to EVI1-expressing EMLs, as well as those expressing ZF mutants, specifically focusing on the Sca-1hi population (Fig. 6c). These regulators were Spi1, encoding PU.1, a major regulator of the lineage choice between erythroid and myeloid cells29,30; Cebpe, encoding C/EBP-ε, essential for terminal myeloid maturation31; Cebpg, encoding CEBP-γ, essential for NK cell development32 and which interacts with CEBP-α, a major regulator of myelopoiesis33; Lmo2, encoding a transcriptional regulator and facilitator of DNA replication34 that is essential for adult hematopoiesis35; and Gfi1b, which is required for erythropoiesis and thrombopoiesis36. We found significant changes in three of these: Spi1 (up twofold), Cebpg (down 50%), and Lmo2 (up 10-fold). For Spi1, Cebpg, and Lmo2, EVI1-induced changes in expression were dependent on DNA binding, since point mutations in ZF1 or ZF2 abrogated the effect (Fig. 6c).
Fig. 6.
EVI1-induced myeloid skewing: downstream effectors include PU.1. a Schematic of EVI1 protein domains, documenting the two zinc-finger domains and the location of the two arginine mutations that disrupt ZF1 and ZF2. b Flow cytometric quantitation of Sca-1hi myeloid-skewed population in EML cells transduced with the indicated retroviral construct, designated on x axis. c RT-qPCR analysis of RNA from sorted Sca-1hi EML cells transduced with the indicated constructs. Gene names are indicated on the x axis. All qPCR reactions performed in triplicate; displayed values represent the average. Errors bars represent standard deviation between qPCR reactions. *p < 0.005. d RT-qPCR data (normalized to Gapdh) showing expression of Spi1 in progenitor populations from Evi1TO/TOR26rtTA/rtTA CD45.2 donor compartments at 10 weeks of induction. e RT-qPCR data (normalized to Gapdh) for Spi1 expression in sorted bone marrow progenitor populations from either WT mice or Evi1TO, R26rtTA mice (as indicated) treated with DOX for 72 hrs. f Scatterplot comparing Spi1 mRNA expression (y axis) to percent Sca-1hi cells (x axis) for five EML cell populations: unmanipulated EMLs (“EML”); EVI1-overexpressing EMLs (“EML EVI1”), and three derivatives of the latter, transduced with either a Spi1-specific shRNA (497, 501) or a control shRNA (498). The p value is calculated using linear regression analysis. g Flow cytometric analysis for Sca-1 and PU.1 (GFP+; top, percent positive) and Sca-1 (bottom; percent positive) on lineage-subpopulation within WBM harvested from Evi1TO/TO, Rosa26rtTA/rtTA, Spi1GFP/GFP mice at 0, 24, or 48 h after DOX induction (0 h n = 3, 24 h n = 3, 48 h n = 3). h Flow cytometric analysis for Sca-1 in Lin-Sca-1-cKit-PU.1GFP-sorted (left two histograms), or Lin-Sca-1-cKit-PU.1GFP+sorted (right two histograms), uninduced (top) or induced with 1 μg/ml DOX (bottom) for 72 h. Error bars represent standard deviation; p values for all except F were calculated using Student’s t-test
EVI1 myeloid-biased phenotype is dependent on Spi1
The transcription factor PU.1 is a master regulator of early myelopoiesis, with highest levels being expressed in CD11b-positive myeloid cells, including macrophages, monocytes, and immature granulocytes, and lower levels in B lymphocytes, while erythroid cells lack expression37. We posited that activation of Spi1 by EVI1 could help explain the expansion of the myeloid compartment in EVI1-overexpressing bone marrow. Thus, we decided to study the link between EVI1, Spi1/PU.1, and myeloid skewing.
To confirm the upregulation of Spi1 by EVI1 overexpression in HSPCs in vivo, we assessed changes in Spi1 gene expression following EVI1 induction with DOX in our Evi1TO/Rosa26rtTA mice. We found that EVI1 upregulates Spi1 expression in HSCs and progenitors (LSK) and in GMPs (Fig. 6d) suggesting that EVI1 increases the expression of the key myeloid gene Spi1 in early hematopoietic and myeloid progenitor cells. We then analyzed Spi1 expression in sub-compartments within the LSKs: we observed strong upregulation of Spi1 within the lineage-negative/Sca-1hi compartment, as well as in long-term HSCs (LT-HSCs; Fig. 6e).
Our data in the EML cell system (Fig. 6b) implies that EVI1 upregulates PU.1, leading to increase in myeloid poised Sca-1hi cells. This predicts that knockdown of PU.1 in EVI1-transduced cells would lead to decreased percentage of Sca-1 high cells. We introduced Spi1-specific shRNA constructs specific into EML-EVI1 cells, and quantitated both Sca-1 and Spi1; the results show a strong positive correlation between Sca-1 expression and Spi1 expression: the higher the level of PU.1, the greater the percentage of Sca-1hi cells (Fig. 6f). These data indicate that EVI1-mediated upregulation of Sca-1, and hence myeloid skewing, depends on Spi1/PU.1.
PU.1 is necessary for EVI1-mediated upregulation of Sca-1
To better understand the relationship between EVI1, PU.1, and Sca-1, we turned to an in vivo system in which PU.1 expression can be followed at the single cell level: we utilized a Spi1gfp allele, in which GFP is driven by the endogenous Spi1 promoter37. We crossed our Evi1TO and Rosa26rtTA alleles with the Spi1gfp allele and assessed whether DOX-induced upregulation of Evi1 expression would lead to increased Spi1/PU.1 and Sca-1 expression within the bone marrow.
Bone marrow from DOX-induced Evi1TO/Rosa26rtTA/Spi1gfp mice was isolated at 24 h, and 48 h post induction and analyzed for GFP and Sca-1 expression. We found a significant upregulation of GFP, from 55 to 70% of cells by 24 h (p = 0.02) (Fig. 6g). This was followed by a marked increase in Sca-1 expression at 48 h (Fig. 6g, bottom panel).
We wondered whether EVI1 overexpression within early erythroid cells could induce Sca-1 expression. From previous studies37, maturing erythroid cells are negative for PU.1. To test this, we isolated lin-negative, c-Kit-negative, Sca-1-negative bone marrow cells from Evi1TO/Rosa26rtTA/Spi1gfp mice, and separated GFP-negative erythroid progenitors from GFP-positive progenitors. Each population was cultured in vitro and induced with DOX to determine the effects of EVI1 on both PU.1 and Sca-1 expression. Remarkably, Sca-1 induction was confined specifically to the GFP-positive population, indicating that PU.1 is required together with EVI1 to induce Sca-1 expression (Fig. 6h). Interestingly, we did not observe induction of GFP expression in either compartment with DOX treatment.
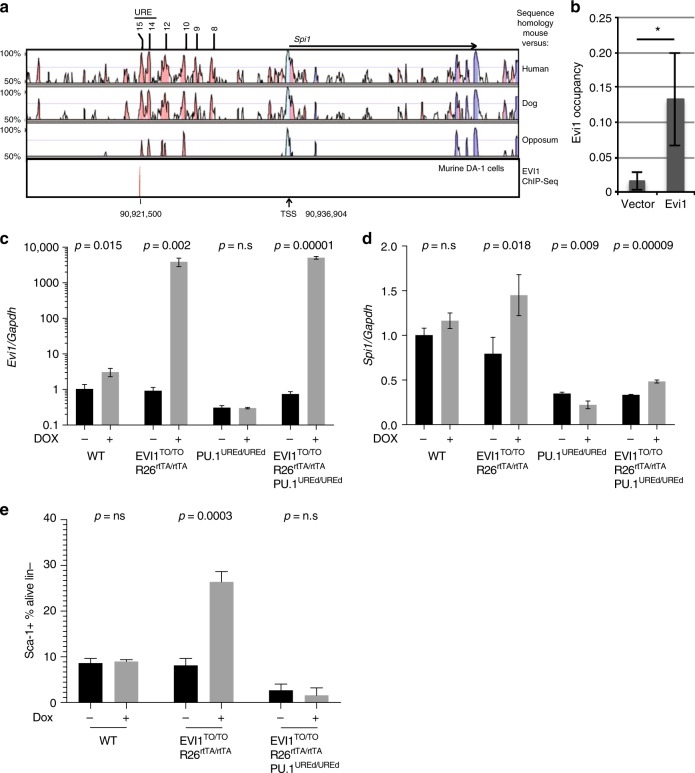
EVI1 binds to −14 kb Spi1 upstream regulatory element
Our data indicate a role for both ZF1 and ZF2 of EVI1 in myeloid skewing and in the upregulation of key myeloid regulator, Spi1. To further examine the role of EVI1 in transcriptional regulation of Spi1, we performed Chromatin Immunoprecipitation Sequencing (ChIP-Seq) on DA.1 cells, an EVI1-overexpressing AML. These data (reported in toto previously38), identified a binding site at −15.45 kb from the Spi1 transcription start site (Fig. 7a), within a previously described regulatory element termed the −14 kb upstream regulatory element (−14kbURE)39. We confirmed this binding using ChIP-PCR (Fig. 7b).
Fig. 7.
EVI1 binds to the −14kbURE of Spi1 and requires this element for Sca-1 upregulation. a Region of mouse genome encompassing the transcription start site (TSS) of Spi1 together with 25 kb of upstream DNA. Top three bands show peaks of sequence homology between mouse and human, dog, and opossum, as indicated, while the bottom band displays our ChIP-Seq for EVI1 occupancy in the murine myeloid leukemia cell line, DA-1, at −15.45 kb from the Spi1 transcription start site. Also indicated is the location of the −15 to −14 kb upstream regulatory element, referred to in the text as −14kbURE. b ChIP-qPCR data showing EVI1 occupancy at the Spi1–15.45 binding site in EML cells transduced with WT EVI1 or vector control. c, d RT-qPCR for Evi1 (c) or Spi1 (d) on Lin− bone marrow cells, with or without in vivo DOX treatment for 72 h from four genotypes of mice, harboring either Evi1TO/TO Rosa26rtTA/rtTA or Spi-1UREd/UREd genotypes, as indicated. e Quantification of Sca-1+cells of WBM from mice with genotypes as indicated either with or without DOX treatment for 72 h (n = 3). For all panels, error bars represent standard deviation; p values calculated with Student’s t-test
Sca-1 upregulation depends on EVI1 binding to −14 kb Spi1 URE
To test the role of the −14kbURE in EVI1-mediated upregulation of Spi1/PU.1 and Sca-1, we combined the Evi1TO/Rosa26rtTA alleles with the Spi1–14UREdel (ref. 40; a deletion that encompasses the −15.45 kb EVI1-binding element), with the expectation that in mice lacking the −14kbURE, EVI1 would not be able to bind to the Spi1 promoter, which would abrogate EVI1-mediated upregulation of PU.1; this would allow us to assess the requirement for PU.1 in EVI1-mediated upregulation of Sca-1. We generated Evi1TO/Rosa26rtTA/Spi1–14UREdel and Evi1TO/Rosa26rtTA mice, and then treated these (as well as WT and Spi1–14UREdel control mice) with DOX (or not) for 72 h; bone marrow was analyzed for upregulation of EVI1, Spi1/PU.1, and Sca-1. As expected, administration of DOX resulted in upregulation of EVI1 in both groups harboring the Evi1TO and Rosa26rtTA alleles; there was no induction in WT or Spi1–14UREdel mice (Fig. 7c). DOX treatment resulted in an 83% increase in Spi1/PU.1 expression in Evi1TO/Rosa26rtTA mice, but no change in WT or Spi1–14UREdel mice; however, baseline levels of Spi1/PU.1 transcripts were lower in the latter (Fig. 7d; ref. 40). In Evi1TO/Rosa26rtTA/Spi1–14UREdel mice, we did observe a DOX-induced increase in Spi1/PU.1 transcripts of 45% despite the deletion of the −14kbURE; while this is less than the increase seen in Evi1TO/Rosa26rtTA mice, the increase of 45% was still significant (p < 0.001), indicating that EVI1-responsive elements exist outside of the −14kbURE.
Regarding Sca-1 expression: as expected, DOX treatment of Evi1TO/Rosa26rtTA mice resulted in a more than threefold increase in Sca-1-expressing lineage-negative bone marrow cells (from 8 to 29%), while in Evi1TO/Rosa26rtTA/Spi1–14UREdel mice, induction of EVI1 resulted in no change in Sca-1 expression (both <5% Sca-1+; Fig. 7e, Supplementary Figure 3). These data indicate that EVI1-induced upregulation of Sca-1 is dependent on upregulation of Spi1/PU.1 by EVI1 via the −14kbURE.
Discussion
Overexpression of EVI1 is associated with poor-prognosis AML with a median overall survival of 12 months41. Despite much investigation, the mechanisms by which EVI1 contributes to leukemia have remained obscure. One key observation is that EVI1 is associated specifically with myeloid malignancies42–44. Our findings here offer an insight into this curious association: EVI1 acts through the activation of PU.1 to promote myeloid expansion and interfere with erythropoiesis and lymphopoiesis. Our data indicate that EVI1 overexpression does not by itself cause immediate malignant transformation of hematopoietic cells, but regulates the functional output of the hematopoietic system. Importantly, our analysis also indicates that EVI1 overexpression does not preclude terminal differentiation of the myeloid cells: the EVI1-overexpressing myeloid cells are well-represented in the peripheral blood, and by morphology, these appear normal, consistent with previous findings45.
This model mimics human myeloid malignancies bearing rearrangements at 3q26 for the following reasons: (1) the native, unmutated gene, with all of the alternatively spliced isoforms, is upregulated (Supplementary Figure 1H); (2) the levels of EVI1 expression are similar to activated MECOM alleles (Fig. 1b); (3) because we induce EVI1 in the transplanted setting, only hematopoietic cells overexpress EVI1; (4) the overexpressing cells are mixed in with normal cells, as is the case in incipient human myeloid malignancies. While we have not documented EVI1 overexpression in specific lineages within the hematopoietic system in our mouse model, it is known that DOX induction of target genes harboring the tetracycline operons via the rtTA transactivator occurs in multiple compartments within the marrow, and, in general, gene activation in the marrow with this system is quite strong16–18. Thus, it is very likely that in our system, EVI1 overexpression occurs in both the HSC compartment, as well as more mature and differentiated derivatives. In humans with 3q26 rearrangements, a super-enhancer from the 3q21/GATA2 locus relocates to be in proximity to MECOM46, resulting in high expression of EVI15; whereas the EVI1 is exclusively active in long-term and short-term HSCs4, the GATA2 gene is active both in HSCs and in more mature cells, including erythroid lineage cells47. It is known that 3q26 translocations in myeloid malignancies occur in early MPPs48, and leukemia-associated translocations have been found in erythroid cells and lymphoid cells49. Thus, it is very likely that in humans, the 3q26-rearranged chromosome is present and expressed as stem/progenitor cells mature to the MPP stage.
While binding of EVI1 to PU.1 has been noted previously50, the relationship between EVI1 and Spi1/PU.1 transcriptional regulation has not been investigated previously. Here, we document binding of EVI1 to a previously characterized regulatory element, the −14kbURE, together with EVI1-induced upregulation of PU.1. Strikingly, knocking down PU.1 abrogated myeloid skewing associated with EVI1 overexpression, revealing that PU.1 is necessary for EVI1-induced myeloid expansion. The mechanism by which EVI1 and PU.1 interfere with erythropoiesis likely includes antagonism of GATA1 function; PU.1 has been shown to have this activity51,52, and EVI1 is known to bind to GATA1’s DNA motif22, so it is possible that EVI1 itself, in addition to PU.1, impedes GATA1 function in developing erythroid cells.
The most striking transcriptional response induced by EVI1 is upregulation of Sca-1, which is known to have an important role in the granulocytic response to bacteria via TLR4, the receptor for lipopolysaccharides (LPS)53,54; PU.1 is known to play an important role in this53. Our data presented here indicate that upregulation of Sca-1 occurs via PU.1 action (Figs. 6, 7). The key findings of our work—that EVI1 overexpression causes lymphoid and erythroid suppression while expanding the myeloid compartment—bears a striking similarity to what is seen during emergency granulopoiesis55. Infection with a number of pathogenic organisms results in a shift away from erythropoiesis and lymphopoiesis and towards myelopoiesis56–60. The similarities between the effects of EVI1 on the hematopoietic system and the marrow’s response to infection suggest either that EVI1 is acting through molecular mimicry, or that it plays a role in the bacterial response. While EVI1 is normally only expressed in the long- and short-term HSCs4, recent findings indicate that it is also induced by LPS (E.A., A.S.P., unpublished findings; ref. 61); and a recently described mutation in EVI1 is susceptible to bacterial infections62.
In summary, our findings offer an insight into mechanisms of leukemogenesis, whereby a single nuclear oncoprotein can induce clinically significant suppression of erythropoiesis and lymphopoiesis, while promoting a shift in differentiation that results in a preleukemic expansion of myeloid cells. These findings help to explain the singular association between EVI1 and myeloid malignancies.
Methods
Mice
The Evi1TO allele was generated by insertion of the NSTO cassette63 via homologous recombination in ES cells using standard techniques64. PU.1gfp reporter mice37 and the Spi-1UREd mice40 have been described. UBC-GFP mice were obtained from Jackson Labs. All procedures involving mice were approved by the institutional animal care and use committees of all participating institutions.
Harvesting bone marrow
Bone marrow was harvested by one of two methods: (1) flushing the leg long bones the marrow space with flow cytometry (FACS) buffer (PBS, 2% fetal bovine serum (FBS)) using a 1 ml syringe and 25-gauge needle or (2) grinding femurs, tibia, and pelvis bones (2F2T2P) in FACS buffer using a mortar and pestle65.
Flow cytometry and imaging flow cytometry
Marrow harvest, analysis, and transplantations and other procedures were performed as described4,15,65,66. Imaging flow was done on ImageStreamX with IDEAS 6.0 (Amnis). Accuri C6, FACSCalibur, LSR II, and FACScan instruments (BD Biosciences) were used for flow cytometric analysis and cell sorting. Supplementary Table 2 has cell-surface marker phenotypes. Cells were stained with antibodies targeted against the appropriate hematopoietic marker for 30 min on ice in the dark using manufacturer’s recommended antibody dilutions. Cells were then rinsed once with PBS and resuspended in 1× PBS, 2% FBS before analysis. Antibodies used for flow cytometic analysis and cell sorting are listed in Supplementary Table 3. Collection of all flow cytometry data were done using BD FACSDIVA software. Analyses of all flow cytometry data were done using FlowJo version 10 software (TreeStar).
Proliferation and apoptosis
Mice were injected with 2 mg of BrdU 60 min before harvest; incorporation levels were assessed using kit (Cat#552598; BD Biosciences). Apoptosis rates were determined by flow with anti-annexinV (BD Biosciences).
Cell lines and cell culture
EML cells were provided by Shickwann Tsai and were cultured as described26. Methylcellulose colony-forming assays for myeloid progenitors (M, G, and GM-CSF combined) were carried out by plating 10,000 bone marrow cells as previously described67. Other cell culture techniques were adapted from previously published protocols4,66.
Genetic analysis
RT-qPCR, ChIP, and genomic PCR were performed as described4,38,66. The corresponding primers are listed in Supplementary Table 4.
Statistical analysis
Data were analyzed using Prism (GraphPad); significance was determined using Student’s t-test (α = 0.05).
Electronic supplementary material
Acknowledgements
This work was funded by National Institutes of Health (NIH) grants: (R01CA175761, and R01CA120313 to ASP), (F31HL143994 to EA); New York State Stem Cell Science awards: (C026423 and C029547 to YZ); funds from the Clinical and Translational Science Institute (CTSA award number UL1 TR002001 from the National Center for Advancing Translational Sciences of the National Institutes of Health) and the Wilmot Cancer Institute at the University of Rochester.We thank Seana C. Catherman, Xiaohui Cui, Stacey Duemel, Ahmed Faisal, Katherine H. Fegan, AnneD. Koniski, Lizz Lamere, Mark Lamere, and Huy Nguyen for their technical assistance.We thank Kenji Tanaka for the pNSTO plasmid and Mineo Kurakawa for the pMys-Evi1 vector; LeightonGrimes for providinthe Spi1GFP mice; Dan Tenen for providing the Spi1-4UREd mice. We thank ShickwannTsai for providing the EML cell line.
Author contributions
E.A, M.P.W, K.E.M, A.L, B.J.F. and Y.Z. performed the experiments and created the figures; A.S.P, J.P, and L.M.C. designed the experiments; A.S.P, E.A, K.E.M, M.P.W, and J.P. contributed to the writing of the manuscript.
Data availability
The authors declare that the data supporting the findings of this study are available within the paper and its supplementary information files. All other relevant data supporting the findings of this study are available from the corresponding author on reasonable request. ChIP-seq data are available in Figshare Repository with the identifier 10.6084/m9.figshare.7043468.
Competing interests
The authors declare no competing interests. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Edward Ayoub, Michael P. Wilson.
These authors jointly supervised this work: Yi Zhang, Archibald S. Perkins.
Contributor Information
Yi Zhang, Email: yi_zhang@urmc.rochester.edu.
Archibald S. Perkins, Email: archibald_perkins@urmc.rochester.edu
Electronic supplementary material
Supplementary Information accompanies this paper at 10.1038/s41467-018-06208-y.
References
- 1.Bitter M, Neilly M, LeBeau M, Pearson M, Rowley J. Rearrangements of chromosome 3 involving bands 3q21 and 3q26 are associated with normal or elevated platelet counts in acute non-lymphocytic leukemia. Blood. 1985;66:1362–1370. [PubMed] [Google Scholar]
- 2.Haase D, et al. New insights into the prognostic impact of the karyotype in MDS and correlation with subtypes: evidence from a core dataset of 2124 patients. Blood. 2007;110:4385. doi: 10.1182/blood-2007-03-082404. [DOI] [PubMed] [Google Scholar]
- 3.Hu Z, et al. 3q26.2/EVI1 rearrangement is associated with poor prognosis in classical Philadelphia chromosome-negative myeloproliferative neoplasms. Mod. Pathol. 2017;30:940–951. doi: 10.1038/modpathol.2017.19. [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y, et al. PR domain–containing Mds1-Evi1 is critical for long-term hematopoietic stem cell function. Blood. 2011;118:3853–3861. doi: 10.1182/blood-2011-02-334680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suzukawa K, et al. Identification of a breakpoint cluster region 3′ of the ribophorin I gene at 3q21 associated with the transcriptional activation of the EVI1 gene in acute myelogenous leukemias with inv(3)(q21q26) Blood. 1994;84:2681–2688. [PubMed] [Google Scholar]
- 6.Morishita K, et al. Retroviral activation of a novel gene encoding a zinc finger protein in IL3-dependent myeloid leukemia cell lines. Cell. 1988;54:831–840. doi: 10.1016/S0092-8674(88)91175-0. [DOI] [PubMed] [Google Scholar]
- 7.Mucenski ML, Gilbert DJ, Taylor BA, Jenkins NA, Copeland NG. Common sites of viral integration in lymphomas arising in AKXD recombinant inbred mouse strains. Oncogene Res. 1987;2:33–48. [PubMed] [Google Scholar]
- 8.Yatsula B, et al. Identification of binding sites of EVI1 in mammalian cells. J. Biol. Chem. 2005;280:30712–30722. doi: 10.1074/jbc.M504293200. [DOI] [PubMed] [Google Scholar]
- 9.Glass C, Wilson M, Gonzalez R, Zhang Y, Perkins AS. The role of EVI1 in myeloid malignancies. Blood. Cells Mol. Dis. 2014;53:67–76. doi: 10.1016/j.bcmd.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Louz D, et al. Erythroid defects and increased retrovirally-induced tumor formation in Evi1 transgenic mice. Leukemia. 2000;14:1876–1884. doi: 10.1038/sj.leu.2401887. [DOI] [PubMed] [Google Scholar]
- 11.Buonamici S, et al. EVI1 induces myelodysplastic syndrome in mice. J. Clin. Invest. 2004;114:713–719. doi: 10.1172/JCI21716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoshimi A, et al. Evi1 represses PTEN expression and activates PI3K/AKT/mTOR via interactions with polycomb proteins. Blood. 2011;117:3617–3628. doi: 10.1182/blood-2009-12-261602. [DOI] [PubMed] [Google Scholar]
- 13.Cuenco G, Ren R. Both AML1 and EVI1 oncogenic components are required for the cooperation of AML1/MDS1/EVI1 with BCR/ABL in the induction of acute myelogenous leukemia in mice. Oncogene. 2004;23:569–579. doi: 10.1038/sj.onc.1207143. [DOI] [PubMed] [Google Scholar]
- 14.Yamazaki H, et al. A remote GATA2 hematopoietic enhancer drives leukemogenesis in inv(3)(q21;q26) by activating EVI1 expression. Cancer Cell. 2014;25:415–427. doi: 10.1016/j.ccr.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson M, et al. EVI1 interferes with myeloid maturation via transcriptional repression of Cepba, via binding to two far downstream regulatory elements. J. Biol. Chem. 2016;291:13591–13607. doi: 10.1074/jbc.M115.708156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kharas MG, et al. Musashi-2 regulates normal hematopoiesis and promotes aggressive myeloid leukemia. Nat. Med. 2010;16:903–908. doi: 10.1038/nm.2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beard C, Hochedlinger K, Plath K, Wutz A, Jaenisch R. Efficient method to generate single-copy transgenic mice by site-specific integration in embryonic stem cells. Genesis. 2006;44:23–28. doi: 10.1002/gene.20180. [DOI] [PubMed] [Google Scholar]
- 18.Giel-Moloney M, Krause DS, Chen G, Van Etten RA, Leiter AB. Ubiquitous and uniform in vivo fluorescence in ROSA26-EGFP BAC transgenic mice. Genes. 2007;45:83–89. doi: 10.1002/dvg.20269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hochedlinger K, Yamada Y, Beard C, Jaenisch R. Ectopic expression of Oct-4 blocks progenitor-cell differentiation and causes dysplasia in epithelial tissues. Cell. 2005;121:465–477. doi: 10.1016/j.cell.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 20.Barjesteh van Waalwijk van Doorn-Khosrovani S, et al. High EVI1 expression predicts poor survival in acute myeloid leukemia: a study of 319 de novo AML patients. Blood. 2003;101:837–845. doi: 10.1182/blood-2002-05-1459. [DOI] [PubMed] [Google Scholar]
- 21.Cabezas-Wallscheid N, et al. Identification of regulatory networks in HSCs and their immediate progeny via integrated proteome, transcriptome, and DNA methylome analysis. Cell Stem Cell. 2014;4:507–522. doi: 10.1016/j.stem.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 22.Perkins AS, Fishel R, Jenkins NA, Copeland NG. Evi-1, a murine zinc finger proto-oncogene, encodes a sequence-specific DNA-binding protein. Mol. Cell. Biol. 1991;11:2665–2674. doi: 10.1128/MCB.11.5.2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Funabiki T, Kreider BL, Ihle JN. The carboxyl domain of zinc fingers of the Evi-1 myeloid transforming gene binds a consensus sequence GAAGATGAG. Oncogene. 1994;9:1575–1581. [PubMed] [Google Scholar]
- 24.Shimabe M, et al. Pbx1 is a downstream target of Evi-1 in hematopoietic stem/progenitors and leukemic cells. Oncogene. 2009;28:4364–4374. doi: 10.1038/onc.2009.288. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, et al. Targeting a DNA binding motif of the EVI1 protein by a pyrrole-imidazole polyamide. Biochemistry. 2011;50:10431–10441. doi: 10.1021/bi200962u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsai S, Bartelmez S, Sitnicka E, Collins S. Lymphohematopoietic progenitors immortalized by a retroviral vector harboring a dominant-negative retinoic acid receptor can recapitulate lymphoid, myeloid, and erythroid development. Genes Dev. 1994;8:2831–2841. doi: 10.1101/gad.8.23.2831. [DOI] [PubMed] [Google Scholar]
- 27.Chang H, Hemberg M, Barhona M, Ingber D, Huang S. Transcriptome-wide noise controls lineage choice in mammalian progenitor cells. Nature. 2008;453:544. doi: 10.1038/nature06965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pina C, et al. Inferring rules of lineage commitment in haematopoiesis. Nat. Cell Biol. 2012;14:287–294. doi: 10.1038/ncb2442. [DOI] [PubMed] [Google Scholar]
- 29.Iwasaki H, et al. Distinctive and indispensable roles of PU.1 in maintenance of hematopoietic stem cells and their differentiation. Blood. 2005;106:1590. doi: 10.1182/blood-2005-03-0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arinobu Y, et al. Reciprocal activation of GATA-1 and PU.1 marks initial specification of hematopoietic stem cells into myeloerythroid and myelolymphoid lineages. Cell Stem Cell. 2007;1:416–427. doi: 10.1016/j.stem.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 31.Yamanaka R, et al. Impaired granulopoiesis, myelodysplasia, and early lethality in CCAAT/enhancer binding protein epsilon-deficient mice. Proc. Natl Acad. Sci. USA. 1997;94:13187–13192. doi: 10.1073/pnas.94.24.13187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaisho T, et al. Impairment of natural killer cytotoxic activity and interferon gamma production in CCAAT/enhancer binding protein gamma-deficient mice. J. Exp. Med. 1999;190:1573–1582. doi: 10.1084/jem.190.11.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parkin SE, Baer M, Copeland TD, Schwartz RC, Johnson PF. Regulation of CCAAT/enhancer-binding protein (C/EBP) activator proteins by heterodimerization with C/EBPgamma (Ig/EBP) J. Biol. Chem. 2002;277:23563–23572. doi: 10.1074/jbc.M202184200. [DOI] [PubMed] [Google Scholar]
- 34.Sincennes MC, et al. The LMO2 oncogene regulates DNA replication in hematopoietic cells. Proc. Natl Acad. Sci. USA. 2016;113:1393. doi: 10.1073/pnas.1515071113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamada Y, et al. The T cell leukemia LIM protein Lmo2 is necessary for adult mouse hematopoiesis. Proc. Natl Acad. Sci. USA. 1998;95:3890–3895. doi: 10.1073/pnas.95.7.3890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Foudi A, et al. Distinct, strict requirements for Gfi-1b in adult bone marrow red cell and platelet generation. J. Exp. Med. 2014;211:909. doi: 10.1084/jem.20131065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nutt SL, Metcalf D, D’Amico A, Polli M, Wu L. Dynamic regulation of PU.1 expression in multipotent hematopoietic progenitors. J. Exp. Med. 2005;201:221–231. doi: 10.1084/jem.20041535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Glass C, et al. Global identification of EVI1 target genes in acute myeloid leukemia. PLoS ONE. 2013;8:e67134. doi: 10.1371/journal.pone.0067134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li Y, et al. Regulation of the PU.1 gene by distal elements. Blood. 2001;98:2958. doi: 10.1182/blood.V98.10.2958. [DOI] [PubMed] [Google Scholar]
- 40.Rosenbauer F, et al. Acute myeloid leukemia induced by graded reduction of a lineage-specific transcription factor, PU.1. Nat. Genet. 2004;36:624–630. doi: 10.1038/ng1361. [DOI] [PubMed] [Google Scholar]
- 41.Lugthart S, et al. High EVI1 levels predict adverse outcome in acute myeloid leukemia: prevalence of EVI1 overexpression and chromosome 3q26 abnormalities underestimated. Blood. 2008;111:4329–4337. doi: 10.1182/blood-2007-10-119230. [DOI] [PubMed] [Google Scholar]
- 42.Cui W, Sun J, Cotta CV, Medeiros LJ, Lin P. Myelodysplastic syndrome with inv(3)(q21q26.2) or t(3;3)(q21;q26.2) has a high risk for progression to acute myeloid leukemia. Am. J. Clin. Pathol. 2011;136:282–288. doi: 10.1309/AJCP48AJDCKTHUXC. [DOI] [PubMed] [Google Scholar]
- 43.Secker-Walker LM, Mehta A, Bain B. Abnormalities of 3q21 and 3q26 in myeloid malignancy: a United Kingdom Cancer Cytogenetic Group study. Br. J. Haematol. 1995;91:490–501. doi: 10.1111/j.1365-2141.1995.tb05329.x. [DOI] [PubMed] [Google Scholar]
- 44.Wang W, et al. Clinical and prognostic significance of 3q26.2 and other chromosome 3 abnormalities in CML in the era of tyrosine kinase inhibitors. Blood. 2015;126:1699–1706. doi: 10.1182/blood-2015-05-646489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Metais JY, Dunbar CE. The MDS1-EVI1 gene complex as a retrovirus integration site: impact on behavior of hematopoietic cells and implications for gene therapy. Mol. Ther. 2008;16:439–449. doi: 10.1038/sj.mt.6300372. [DOI] [PubMed] [Google Scholar]
- 46.Groschel S, et al. A single oncogenic enhancer rearrangement causes concomitant EVI1 and GATA2 deregulation in leukemia. Cell. 2014;157:369–381. doi: 10.1016/j.cell.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 47.Walsh JC, et al. Cooperative and antagonistic interplay between PU.1 and GATA-2 in the specification of myeloid cell fates. Immunity. 2002;17:665–676. doi: 10.1016/S1074-7613(02)00452-1. [DOI] [PubMed] [Google Scholar]
- 48.Shi G, Weh HJ, Duhrsen U, Zeller W, Hossfeld D. Chromosomal abnormality inv(3)(q21q26) associated with multilineage hematopoietic progenitor cells in hematopoietic malignancies. Cancer Genet. Cytogenet. 1997;96:58–63. doi: 10.1016/S0165-4608(96)00293-2. [DOI] [PubMed] [Google Scholar]
- 49.Crescenzi B, et al. NUP98/11p15 translocations affect CD34+ cells in myeloid and T lymphoid leukemias. Leuk. Res. 2015;39:769–772. doi: 10.1016/j.leukres.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 50.Laricchia-Robbio L, Premanand K, Rinaldi CR, Nucifora G. EVI1 Impairs myelopoiesis by deregulation of PU.1 function. Cancer Res. 2009;69:1633–1642. doi: 10.1158/0008-5472.CAN-08-2562. [DOI] [PubMed] [Google Scholar]
- 51.Zhang P, et al. Negative cross-talk between hematopoietic regulators: GATA proteins repress PU.1. Proc. Natl Acad. Sci. USA. 1999;96:8705–8710. doi: 10.1073/pnas.96.15.8705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang P, et al. PU.1 inhibits GATA-1 function and erythroid differentiation by blocking GATA-1 DNA binding. Blood. 2000;96:2641. [PubMed] [Google Scholar]
- 53.Shi X, et al. Toll-Like receptor 4/stem cell antigen 1 signaling promotes hematopoietic precursor cell commitment to granulocyte development during the granulopoietic response to Escherichia coli bacteremia. Infect. Immun. 2013;81:2197–2205. doi: 10.1128/IAI.01280-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Melvan JN, et al. Alcohol impairs the myeloid proliferative response to bacteremia in mice by inhibiting the stem cell antigen-1/ERK pathway. J. Immunol. 2012;188:1961–1969. doi: 10.4049/jimmunol.1102395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Manz MG, Boettcher S. Emergency granulopoiesis. Nat. Rev. Immunol. 2014;14:302–314. doi: 10.1038/nri3660. [DOI] [PubMed] [Google Scholar]
- 56.Stein B. The anemia of inflammation. J. Clin. Rheumatol. 2012;18:437–442. doi: 10.1097/RHU.0b013e318278f553. [DOI] [PubMed] [Google Scholar]
- 57.Zaretsky AG, Engiles JB, Hunter CA. Infection-induced changes in hematopoiesis. J. Immunol. 2014;192:27. doi: 10.4049/jimmunol.1302061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ueda Y, Kondo M, Kelsoe G. Inflammation and the reciprocal production of granulocytes and lymphocytes in bone marrow. J. Exp. Med. 2005;201:1771. doi: 10.1084/jem.20041419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nagaoka H, Gonzalez-Aseguinolaza G, Tsuji M, Nussenzweig MC. Immunization and infection change the number of recombination activating gene (Rag)-expressing B cells in the periphery by altering immature lymphocyte production. J. Exp. Med. 2000;191:2113. doi: 10.1084/jem.191.12.2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu, A. et al. Hematopoietic stem cell expansion and common lymphoid progenitor depletion requires hematopoietic-derived, cell-autonomous TLR4 in a model of chronic endotoxin. J. immunol.195, 2524–2528 (2015). [DOI] [PMC free article] [PubMed]
- 61.Xu X, et al. EVI1 acts as an inducible negative-feedback regulator of NF-kappaB by inhibiting p65 acetylation. J. Immunol. 2012;188:6371–6380. doi: 10.4049/jimmunol.1103527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Parkinson, N. et al. Mutation at the Evi1 locus in Junbo mice causes susceptibility to otitis media. PLoS Genet.3, 1556–1564 (2006). [DOI] [PMC free article] [PubMed]
- 63.Tanaka K, et al. Flexible accelerated STOP tetracycline operator-knockin (FAST): a versatile and efficient new gene modulating system. Biol. Psych. 2010;67:770–773. doi: 10.1016/j.biopsych.2009.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Copeland N, Jenkins N, Court D. Recombineering: a powerful new tool for mouse functional genomics. Nat. Rev. Genet. 2001;2:769–779. doi: 10.1038/35093556. [DOI] [PubMed] [Google Scholar]
- 65.Balderman SR, et al. Targeting of the bone marrow microenvironment improves outcome in a murine model of myelodysplastic syndrome. Blood. 2016;127:616. doi: 10.1182/blood-2015-06-653113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang Y, et al. Essential role of PR-domain protein MDS1-EVI1 in MLL-AF9 leukemia. Blood. 2013;122:2888–2892. doi: 10.1182/blood-2012-08-453662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Palis J, Koniski A. Analysis of hematopoietic progenitors in the mouse embryo. Methods Mol. Med. 2005;105:289–302. doi: 10.1385/1-59259-826-9:289. [DOI] [PubMed] [Google Scholar]
- 68.Perkins AS, Mercer JA, Jenkins NA, Copeland NG. Patterns of Evi-1 expression in embryonic and adult tissues suggest that Evi-1 plays an important role in mouse development. Development. 1991;111:479–487. doi: 10.1242/dev.111.2.479. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors declare that the data supporting the findings of this study are available within the paper and its supplementary information files. All other relevant data supporting the findings of this study are available from the corresponding author on reasonable request. ChIP-seq data are available in Figshare Repository with the identifier 10.6084/m9.figshare.7043468.