Abstract
Three decades of rapid economic development in China have not only benefited millions of Chinese by improving their living standards but have also dramatically increased the number of people who are part of the country's aging population. However, economic growth has not been accompanied by sufficient attention given to important public health issues, including an increase in the incidence of chronic diseases and a decline in physical activity (PA) that comes with an aging population. The rapid growth in China's older population will soon exert an impact on the nation's economy, population health status, and health behaviors, and will increase stress on its healthcare system. This review article provides a broad perspective on the impact of rapid economic development, industrialization, and urbanization on health-related behaviors, with a specific focus on PA among older adults. Specifically, the article offers an overview of the demographic context, significant public health challenges, evidence on PA and exercise interventions, and knowledge gaps and future directions for research.
Keywords: Chronic disease, Exercise, Healthy aging, Older Chinese adults, Physical activity epidemiology, Urban health
1. Introduction
China, with the world's largest population estimated at 1.37 billion people,1 is an emerging global economic power that has undergone unprecedented economic growth over the past 3 decades, with significant expansion in both industrialization and urbanization. The resulting economic prosperity and related developments have increased the length of life and improved the quality of life for millions of people in China,2 but it has also created numerous public health challenges as the population continues to age.2, 3, 4 The unintended consequences of economic development, which has brought with it a rise in the cost of living and a widening in urban–rural income and health inequalities, have had a major impact on the quality of the living environment, the development of non-communicable (chronic) diseases, care arrangements for the elderly, and the healthcare, pension, and welfare systems that serve China's population, especially its most vulnerable subpopulations.2, 3, 4, 5, 6, 7
Research on physical activity (PA) and aging has lagged far behind the economic reforms but is critically needed in order to understand the resulting public health ramifications and challenges. With rapid urbanization and sprawl taking place,5, 8 there have been diminishing opportunities for Chinese citizens to engage in traditional exercise activities, such as walking and bicycling, either for leisure or utilitarian purposes. Three decades of economic growth have resulted in some alarming statistics related to (1) accelerated urbanization due to rural-to-urban migration, which rose from 17.92% in 1978 to an estimated 52.57% by 2012,6 and (2) increased motorization, which saw an increase from 12 vehicles per 1000 people in 2002 to 82 vehicles per 1000 people in 2012.9 One consequence of these changes is that Chinese citizens now have reduced access to public spaces (e.g., sports areas, parks, and open recreational fields) for sporting or leisure activities.10, 11 Another consequence is that the Chinese people are experiencing increasingly deteriorating air quality.12, 13 In fact, about three-eighths of China's population breathes air that would be rated “unhealthy” by the United States' standards, resulting in an estimated 1.6 million deaths each year, or about 4000 people a day.14 These changing realities may well have created barriers to and impeded the promotion of health and PA among older Chinese adults.
Taking into account these significant and unprecedented physical and demographic changes occurring in China and the resulting challenges the country faces in the coming decades, this article has 2 broad purposes, both of which are aimed at stimulating a discussion about health and research on PA among an aging Chinese population. First, the article provides an overview of the older adult population in China (broadly defined as people aged 60 and older) and challenges to their health, and the status of research from selected observational and experimental studies that focus on PA in older Chinese adults. Second, it seeks to identify knowledge gaps in our understanding of PA and aging and provide recommendations on research aimed at narrowing these gaps. Given the growing interest in understanding the impact of economic reforms on aging populations and its implications for promoting PA and healthy aging in China, the article is limited in its scope to the discussion and presentation of research conducted solely in the mainland of China.
2. Aging landscape
Over the past 3 decades, China's population has been on a steady rise, from 981 million in 1980 to 1.37 billion in 2015 (Fig. 1),1 a nearly 40% increase. The increase, however, has been even more pronounced for the older segment of its population. At the end of 2015, the number of Chinese adults aged 60 years and older was approximately 205 million, accounting for about 15% of the country's total population. This percentage will continue to grow in the next few decades,2 and it is projected that by 2050, older adults will account for roughly 33% of China's total population, or an estimated 439 million people.1 Of the 205 million older adults, more than 22.7 million are currently in China's oldest-old category1 (aged 80 and older), and by 2050 this number is expected to grow to 87.3 million, representing the world's largest population of the oldest-old.2 Clearly, as the world transitions to an increasingly aging population,15 older Chinese adults will represent a majority of this global populace.2
Fig. 1.
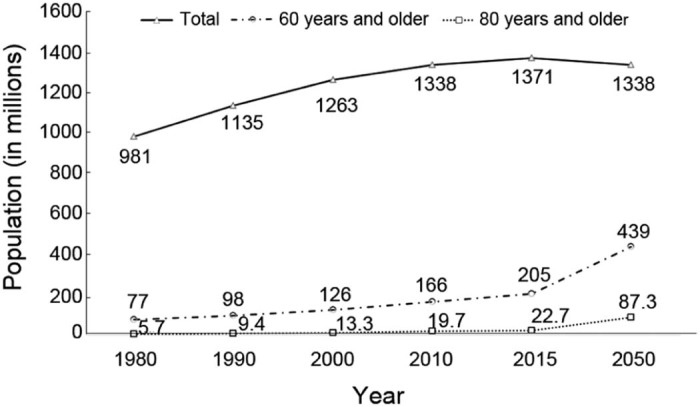
China's population from 1980 to 2050 (estimated).1
The continuing growth of both the general and aging population in China may have been driven by the changing trajectories in life expectancy, fertility, and mortality. Data extracted from the World Bank1, 16 indicate that from 1980 to 2015, life expectancy increased for both women and men, with a longer life expectancy for older women (Fig. 2). The fertility rate (i.e., the number of children born per woman) has also declined (Fig. 3), and the mortality rate (Fig. 4) has remained relatively steady. Thus, the predicted increases in both the number of older adults (including the oldest-old) (Fig. 1) and life expectancy (Fig. 2) in China will have wide-ranging practical implications for the country's public health policies and will create ever-increasing demands on its underprepared and overburdened healthcare system.4, 17, 18
Fig. 2.
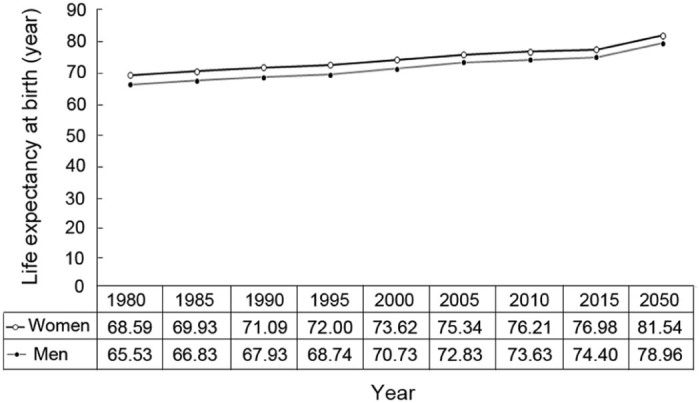
Life expectancy at birth in China from 1980 to 2050 (estimated).1
Fig. 3.
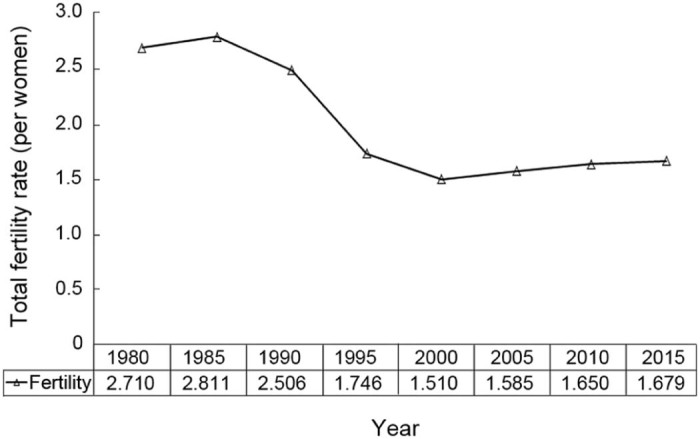
Fertility rate in China from 1980 to 2015 (estimated), births per woman.1
Fig. 4.
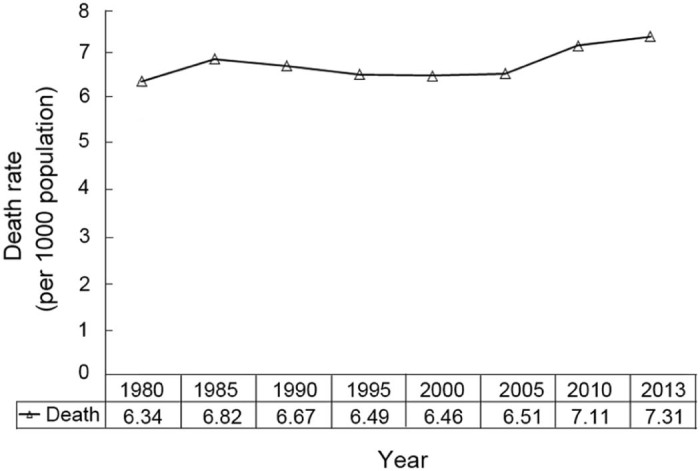
Mortality rate in China from 1980 to 2013 (estimated).1
3. Public health challenges
The challenges to public health related to the aging population will come primarily from the increasing occurrence of chronic and degenerative diseases, which are the major causes of death and disability in China and worldwide.2, 4, 7, 19 Epidemiological studies have shown that, among older Chinese adults, there has been an increase in the prevalence of obesity20 and diabetes,21 an increase in smoking rates among men,22 a decline in cognitive health and an increase in dementia,23 deteriorating physical and mental health, and increased rates in chronic diseases and disabilities,4, 24, 25, 26 particularly among women and rural residents.25 Data from 2010 surveys show that about 64.0% of urban and rural older Chinese adults were living with chronic diseases, with a higher percentage occurring among those living in urban areas (72.3%) than in rural areas (57.5%).18 Estimates in 2012 of mortality from communicable and non-communicable diseases and injuries27 indicate that more than 90% of deaths in older Chinese adults were attributable to chronic diseases (Fig. 5). Leading causes of deaths included disease conditions such as cardiovascular diseases, diabetes mellitus, chronic obstructive pulmonary diseases, and lung cancer.4 There is no question that there will be an increased need and demand for elderly care in the future, and health service costs will undoubtedly rise as a result.4, 18, 24
Fig. 5.
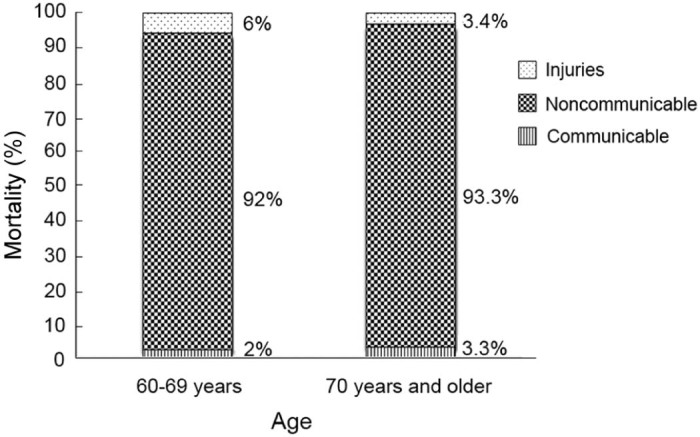
Mortality from communicable diseases, noncommunicable (chronic) diseases, and injuries in 2012 (estimated)27
Continuing industrialization and urbanization, along with increases in motorization, have also brought about rising levels of ambient urban air pollution that will inevitably have a negative impact on health and outdoor PA.5, 12, 13, 14 The current situation has made it undesirable for many Chinese to engage in sustained outdoor PAs and is not expected to improve over time even with the adoption in 2012 of the Ambient Air Quality Standards.28 From the perspective of promoting active lifestyles, air pollution creates a significant barrier and health risk in that it discourages community-based and culturally inherited outdoor PAs, such as Tai Ji Quan, walking, jogging, dancing, and bicycling.12 This situation will result in poor lifestyle characteristics (e.g., reduced PA, increased fat intake) for economically disadvantaged older adults, which will in turn increase their risk for developing chronic diseases.
PA levels have long been studied in the fields of public health and PA epidemiology because they are physiologically and psychologically linked to many chronic diseases and are relevant to public health in terms of healthy aging.29, 30, 31, 32 In China, there is a long history and tradition of using PA to ward off diseases and promote health.33, 34 Until recently, epidemiological studies conducted to better understand PA and its relation to health have been both limited and fragmented. The following section provides an overview of PA patterns and the relationship between PA and health outcomes among older Chinese adults. This is followed by a description of some intervention studies that have targeted the effects of chronic diseases common among this population (see also Lü et al.35 and Zhu et al.36 for extended reviews in these areas).
4. PA
To date, only a few epidemiological studies have examined patterns and correlates of PA among older Chinese adults, and these studies have primarily been cross-sectional in design and descriptive in nature. In general, the results have been inconsistent across study regions and residential settings. Furthermore, differences in survey methodologies and measurements make comparisons across studies difficult.
4.1. PA patterns
In an early study involving a representative sample of Chinese adults aged 35 to 75 years (n = 14,933),37 researchers examined the prevalence of overall, work-related, and leisure-time PA using data during 2000–2001 collected from the International Collaborative Study of Cardiovascular Disease in Asia. PA was defined as 30 or more minutes of daily moderate or vigorous activity. The results on overall PA patterns showed a clear decline with increasing age; those who were 65 years and older had the lowest percentage of being physically active (45%). There was also a notable difference in overall PA and work-related PA depending on residential setting. A lower percentage of older adults living in urban areas were physically active (9.8% for overall PA, 1.0% for work-related PA) compared to older adults living in rural areas (52.7% and 42.0%, respectively).
In contrast to the rural–urban difference found in the previously cited study,37 a cross-sectional survey of PA in Guangdong Province showed an opposite pattern.38 As part of a large study, it included a total of 407 adults between 65 and 69 years old. It was found that about 83% of the older adults living in urban areas reported engaging in daily moderate-to-vigorous intensity PA (including occupational, transport, and recreational activities) compared to about 61% of the older adults living in rural areas.
Two independent urban studies in Shanghai that involved middle-aged and older adult men39 (n = 61,582) in 2002–2006and women40 (n = 75,221) in 1997–2000 (aged 40–70 years) reported higher percentages of older adults (aged 65–70 years) participating in sports or exercise activities (63% of men and 56% of women) compared to their 5 younger cohorts (40–44 = 19%, 45–49 = 20%, 50–54 = 26%, 55–59 = 37%, 60–64 = 52% in the men's study; 40–44 = 18%, 45–49 = 26%, 50–54 = 38%, 55–59 = 48%, 60–64 = 53% in the women's study). In the men's study, older males (aged 65–70 years) engaged in more daily activities compared to younger males (aged 40–44 years), whereas in the women's study, older females participated in more transportation- and housework-related activities than did younger women. In an examination of domain-specific PAs, a study conducted between 2004 and 2008 covering 10 geographical areas (inclusive of urban and rural) showed that older adults (60 years and over) were more likely to engage in higher levels of household and recreational activities but in lower levels of occupational activities than their younger counterparts.41
The findings of high levels of PA in the Guangdong study and the 2 Shanghai studies did not match the findings in other studies and surveys. In a survey conducted in 2010, researchers examined leisure-time PA and physical inactivity in a sample of adults aged 60 years and older (n = 15,193) living in northern China.42 Regular PA was defined as engaging in activities at a moderate level of intensity at least 30 min/day for at least 3 days/week. The results of the study showed that a large percentage of older adults (85.4%) did not engage in leisure-time PA. Only 12% of older adults reported regularly participating in PA. There was also a difference in the prevalence of PA based on gender and residential settings, with a slightly higher percentage of PA reported by men than women (12.9% vs. 11.2%, respectively) and a much higher percentage reported by those living in urban areas than those in rural areas (23.8% vs. 6.3%, respectively). The findings, along with those reported by Xu et al.38 related to higher levels of PA in urban areas, contradicts the findings of Muntner et al.37 Furthermore, this study showed that older adults with higher levels of education and higher family incomes tended to be more physically active than those with lower levels of education and family incomes.42
Selected data from 2 large-scale national PA surveys, one conducted in 200743 and the other in 2014,44 are presented in Fig. 6. Each survey targeted various age cohorts (≥19 years old and ≥20 years old, respectively) and used a multistage random stratified cluster sampling strategy involving approximately 80,000 households in the 2007 study and 50,000 households in the 2014 study. The households surveyed were located in 2249 communities in the 2007 study and 1269 communities in the 2014 study across 31 Chinese provinces.
Fig. 6.
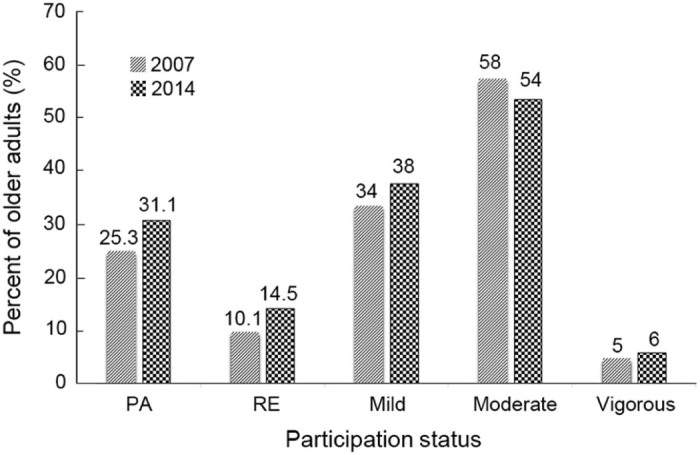
Percentage of physical activity (PA) participation, regular exercise (RE), and exercise intensity among older Chinese adults (60 years and over) in 200743 and 2014.44
The overall percentage of older Chinese adults (aged 60 years and older) who were physically active (i.e., participated in PA, recreation, and sports) was 25.3% in 2007 and 31.1% in 2014, representing a 5.8% increase in the 7-year span. The percentages of those who reported being physically active in both the 2007 and 2014 surveys were, however, lower than the percentages reported in the previously cited 1997 survey (38.6% for people aged 66–75 years; 30.7% for those aged 76 years and older).33 The percentage of those who reported engaging in regular PA, which was defined as participating at least 3 times a week in moderate-intensity activities that lasted 30 min or longer, increased by 4.4% between 2007 (10.1%) and 2014 (14.5%). Older-age adults (70 years and older) were, however, consistently shown to have lower levels of regular PA (8.5% in 2007; 10.8% in 2014) compared to those between 60 and 69 years old (11.7% in 2007; 18.2% in 2014), indicating that the younger age cohort may represent the most physically active group among the older adult population.
Consistent with an earlier survey study,42 the data from the 2007 survey showed a higher level of PA reported among urban residents (18.4%) compared to rural residents (3.5%). No urban–rural comparison data were publicly available in the 2014 survey. Also, across the 2 national surveys,43, 44 common PAs included outdoor walking, gym exercises, traditional Chinese sports, and leisure activities. Walking for fitness was listed as the most popular activity (>90%) in the 60 years and older age cohort. As expected, most of reported activities were done outdoors in locations such as public parks, streets, or community open spaces. In terms of exercise intensity, moderate intensity (i.e., a moderate amount of effort that noticeably accelerates the heart rate) was the most prevalent intensity at which activities were performed. There was no noticeable change in the level of exercise intensity reported by older adults across the time span of the 2 surveys.
4.2. PA and health
Although limited in number, epidemiological studies conducted in the Mainland of China yielded results consistent with those from studies conducted in Western countries showing that PA is related to various health outcomes among older Chinese adults. For example, in a cross-sectional survey study of 1015 older adults (60 years and older) living in the northern city of Jinzhou in Liaoning province, physical inactivity, which was found among 65% of the sample, was identified as one of the major factors associated with poor health-related quality of life.45 In another large-scale study involving older Chinese veterans (n = 9676; median age = 82 years old) living in 18 Chinese cities, PA, even when performed at low intensity, was found to be inversely related to symptoms of depression.46 PA has also been shown to be a protective factor for reducing health risks. For example, in a study of middle-aged and older adults (n = 28,946; mean age = 63 years old), moderate-to-vigorous activity was found to be associated with lower diabetes risk, especially among abdominally obese individuals.47 Another study that involved older adults (n = 9245; mean age = 71 years old) living in rural areas in southern China showed that older adults who reported weekly PA of moderate-to-vigorous intensity had a reduced likelihood of suffering major chronic diseases.25
4.3. PA and social and built environments
There has been surprisingly little research focusing on the ways that social, built, and physical environmental factors might have affected patterns of PA as a result of economic reforms in China. These factors include urban sprawl (including the establishment of urban farms in large or mega cities),8, 48, 49 poor environmental quality in urban areas,13, 14 food safety issues,50 and rapid but uncoordinated rural-to-urban development and migration patterns.5, 51, 52, 53 In the absence of vigorous research studies, it is unclear to what degree social factors (e.g., community cohesiveness), the built environment (e.g., neighborhood walkability, accessibility, safety, open space), and physical environmental characteristics (e.g., terrain, air pollution) are related to the health of older Chinese adults.
To date, only a handful of studies have examined the relationship between neighborhood-level social and built environmental characteristics and various forms of PA in China.54, 55, 56, 57, 58 Two such studies were conducted in Shanghai: one included older adults as part of the study population57 and the other specifically focused on older adults.58 In the study involving individuals between the ages of 15 and 75 years,57 researchers examined the association between self-reported community walking activity and perceptions of neighborhood environments. One of the findings related to older adults was that those who perceived that their neighborhoods had easy access to local services were more likely to engage in walking for transportation purposes. Relationships were also found between other characteristics of neighborhoods (e.g., aesthetics, traffic, crime) and walking for either recreational or transportation purposes.
In the other cross-sectional study cited above, researchers examined whether perceptions of social and built environmental factors were related to self-reported leisure-time PA among older adults sampled from 47 neighborhoods.58 Through multilevel analysis, the study showed that older adults who perceived their neighborhoods to have high social cohesion and who engaged in frequent neighborhood-based social activities tended to report higher levels (at least 150 min weekly) of leisure-time PA. Those who perceived that their neighborhoods had good walkability also reported higher levels of leisure-time PA. These findings suggest that it is important to provide opportunities for social activities and to create conditions conducive to walkability in order to increase the likelihood that older Chinese adults will engage in leisure-time PAs.
5. PA interventions
Compared to the number of studies conducted in North America and Europe, relatively few studies in China have evaluated exercise-based interventions specifically developed or tailored to address common health-risk lifestyle behaviors (e.g., physical inactivity) and chronic diseases (e.g., stroke, heart disease, diabetes) in older adult populations. The following section provides a brief overview of some published Chinese intervention studies that used either a quasi-experimental design or a true experimental design (i.e., a randomized controlled trial (RCT)).
5.1. Cognitive function
A few studies (see Lü et al.35 for a review) have demonstrated the health benefits of exercise on brain and cognitive performance in either healthy older adults59, 60, 61 or those with cognitive impairment.62, 63, 64, 65 One early RCT examined the effects of 3 types of interventions—Tai Ji Quan, walking, and social interaction—on brain volume and cognition.59 The study used a population-based sample of cognitively intact, community-dwelling older adults (aged 60–79 years) in Shanghai. A 40-week exposure to the interventions yielded results indicating that Tai Ji Quan was more effective than walking or social interaction in eliciting brain growth (i.e., growth in the volume of white and gray matter in relation to the total intracranial volume) and improving cognitive abilities (executive function).
Changes in brain neural activity and cognitive performance were also observed in a series of reports from a 6-week intervention study that examined the effects of a multimodal intervention, which included cognitive training, exercise, and counseling, on brain functional plasticity in healthy older adults. Specifically, the multicomponent intervention was able to (a) influence resting-state functional connectivity between the prefrontal cortex and medial temporal lobe of the brain, (b) modify regional intensity by enhancing the amplitude of low-frequency fluctuations in the middle frontal gyrus, superior frontal gyrus, and anterior cerebellum lobe, and (c) alter the local functional homogeneity of brain activity in the superior and middle temporal gyri and the posterior lobe of the cerebellum.60, 66, 67 A more recent experiment shows that a 12-week-long exercise program of Tai Ji Quan or Ba Duan Jin (a form of Qigong exercise34) resulted in increased functional connectivity between the bilateral hippocampus (a key region in memory function) and the medial prefrontal cortex (involved in the consolidation of memory).68 These intervention-induced changes in brain activity were found to correlate with cognitive performance outcomes (e.g., executive function, memory, and attention).60, 66, 68
Four studies targeting at-risk populations have examined the effects of exercise on older adults with cognitive impairment.62, 63, 64, 65 Three RCTs explored whether an exercise intervention involving the use of a combined jogging and shadowboxing exercise,62 momentum-based dumbbell training,63 or handball training64 would be effective in improving cognitive function among older adults with mild cognitive impairment. Findings from these studies generally indicated positive results in terms of the effects of exercise on improving global cognitive function. Another RCT evaluated the effect of moderate-intensity aerobic exercise on elderly people with mild Alzheimer's disease.65 The results from this 3-month intervention showed that, compared to those assigned to the control group, participants in the exercise group significantly improved in global cognitive function.
5.2. Osteoarthritis
In an RCT conducted by Zhu et al.,69 the researchers examined whether a specially tailored Tai Ji Quan exercise routine would improve gait and physical function outcomes among older Chinese women with clinically diagnosed knee osteoarthritis. Compared to those assigned to an educational control group, participants in the Tai Ji Quan group showed significant improvement in gait velocity, step length, range of motion, and physical function at the end of the 24-week intervention. The study findings were congruent with findings from trials conducted in the West, and it is notable that Zhu et al.'s study69 represents the first intervention trial conducted in China that used a specifically designed Tai Ji Quan intervention.
5.3. Strength, balance, and physical function/mobility
Tai Ji Quan has been extensively studied as a modality for older adults to improve various physical outcomes.34 Two Chinese RCTs, with training durations of 12 weeks70 and 16 weeks,71 respectively, yielded results showing that Tai Ji Quan training improved strength, balance, joint proprioception, range of motion, and gait outcomes among healthy community-dwelling older adults in Shanghai. Likewise, a non-RCT Tai Ji Quan study showed improved reaction time, balance, postural control, and flexibility in older male adults.72
5.4. Falls prevention
In a large-scale, community-level RCT, Xia et al.73 evaluated the effectiveness of a multifaceted intervention (including components such as guidance on exercise, healthcare consultation, in-home hazard assessment, community-wide education, and assessment of fall risk factors) designed to reduce the incidence of falls among urban, community-dwelling older adults. At the end of Year 1 of the intervention, the study showed that, compared to those assigned to the control communities, older adults in the intervention communities had a significant reduction (about 64%) in their incidence of falls.
5.5. Diabetes and hypertension
In a study that examined the effect of a traditional Qigong exercise—Ba Duan Jin—on cognitive function among older adults with type 2 diabetes, it was reported that older adults who participated in the 12-month Ba Duan Jin intervention significantly improved their cognitive function compared to those assigned to a usual-care condition.74 A community-based study conducted in Tianjin examined the effectiveness of a lifestyle intervention that targeted older adults (mean age = 60 years old) with diabetes and hypertension.75 As part of intervention, participants engaged in moderate-intensity PA (defined as any activity involving between 3 and 6 metabolic equivalents and lasting at least 6 min). At the end of the 3-month intervention, participants in the intervention group significantly increased their total energy expenditure by 54.6 kcal/day and decreased their total dietary intake by 328.5 kcal/day compared to the control group. In addition, compared to the control group the intervention group improved on a number of biomarkers, including blood pressure, postprandial glucose, and hemoglobin A1c. These results indicate that a community-based lifestyle management intervention was able to produce short-term beneficial changes in activity, diet, and clinical outcomes among older adults with mild diabetes and hypertension.
6. Research gaps and needs
In the US and Europe, the health benefits of engaging in regular moderate and vigorous PAs and muscle-strengthening activities are now well established. The evidence has led to the development of worldwide PA guidelines for general populations, including older adults.76, 77, 78 These guidelines, which are based predominantly on populations from developed countries, are of great public health importance in reducing physical inactivity and preventing diseases, but the extent to which they are generalizable and applicable to Chinese populations remains unclear. Given the vast differences between China's cultural history and that of other countries, and the unprecedented changes the country has experienced in urban growth and forms, lifestyle trends, and PA behaviors, the guidelines may well be inadequate or inapplicable.
This review and others appearing in this issue34, 35, 36 indicate that epidemiological studies of PA that exclusively focus on older Chinese adult populations have been significantly limited in scope and volume. Those studies that do exist are largely fragmented, and many of them suffer from weaknesses in design and methodologies. China's rapid economic development has already generated significant economic and health disparities for the aging population, yet there is a significant lack of knowledge regarding its negative impact on various health-related outcomes in older adults. Areas where additional knowledge and research are needed include:
-
•
Overall trends and patterns in various types of PA among older adult populations and subpopulations (e.g., “young old”, “old”, and “oldest-old” groups);
-
•
Relationships between PA and disease and all-cause mortality;
-
•
Determinants of and health risks associated with physical inactivity;
-
•
Development of guidelines specifically designed for Chinese populations recommending the amount, types, and intensity of PA needed to improve health;
-
•
Various correlates and/or determinants of social, physical, and built environmental factors that either facilitate or impede neighborhood-based PA;
-
•
Effects of urbanization and continual rural–urban migration on PA among older adults, especially among “empty nesters” who experience depression and loneliness;7
-
•
Influence of cultural, ethnic, and health-related differences on the acceptability and effectiveness of PA;
-
•
Evidence of the efficacy/effectiveness and benefits of community-based exercise interventions targeting salient chronic disease conditions in older adults;
-
•
Effectiveness of exercise-based interventions in practice settings (e.g., clinics/hospitals, communities) and living settings (rural areas vs. urban areas);
-
•
Appropriate approaches to design, method, and implementation in PA epidemiology research on the aging Chinese population.
These research and knowledge gaps create significant barriers to addressing urgent public health needs and promoting PA among older Chinese adults. To narrow these gaps, a strategic research agenda should be developed, which aims at understanding the benefits of PA in promoting healthy lifestyles, ameliorating chronic health conditions, improving quality of life, and prolonging life independence among older adults. The following subsections describe some of the epidemiological and experimental research that is needed to advance the field of PA epidemiology and aging in China.
6.1. Tracking PA prevalence and trends
There is a need to establish a national PA and health risk tracking (surveillance) system for China that allows for the systematic study of PA epidemiology to better understand the prevalence of and trends and patterns in PA in the population, as well as the relationship between PA and health and disease. Like the behavioral risk factor surveillance system used in the US,79 it would allow for identification of patterns and trends regarding the mode (walking, Tai Ji Quan, dancing); domain (leisure-time, transportation, household); and frequency, duration, and intensity of activity participation.80 Information collected from such a system would help us understand not only general PA patterns across groups (e.g., by age and socioeconomic status) and settings (i.e., urban, suburban, rural) but also their relationships to health factors. This information could be used to develop guidelines that inform policymakers, physical educators, healthcare providers, and the public on the amount, types, and intensity of PA needed to achieve health benefits, as well as recommend community-based interventions that are useful in promoting healthy aging.
Many of the studies on PA and aging in China conducted to date have used cross-sectional designs and self-report assessments of PA. Research needs to go beyond cross-sectional survey studies by adopting longitudinal or prospective designs. Such an approach would allow PA trajectories to be examined over a period of time in order to establish the time-sequence in which PA occurs and to identify personal, social, and built environmental characteristics that are related to various patterns of change in PA. This information is especially important for addressing public health issues that accompany continued growth in urbanization and motorization and that are related to increases in lifestyle risk factors (smoking, obesity/overweight, physical inactivity) associated with an aging population.2
Valid assessment of PA is essential in research on this topic because it can provide information on population trends and patterns of PA or inactivity, as well as gauge the efficacy or effectiveness of exercise, PA, and interventions used to increase PA. The use of self-reported PA questionnaires in population studies threatens their validity because this type of measure introduces the potential for error and recall bias. Although objective measuring devices for movement activity (e.g., global positioning systems, pedometers, accelerometers) cost more to use than self-report measures, they increase data validity and can be used to better quantify the association between PA and health outcomes, dose-response associations, longitudinal trends, and the effects of public health interventions intended to increase a population's level of PA.
6.2. Understanding correlates and determinants of PA across settings and at various contextual levels
Creating a friendly and active community living environment for older Chinese adults aging in place should be a high priority for the Chinese government.2 Despite the significant transformations in urban forms, research has lagged behind these changes in terms of determining the impact of social, physical, and built environments on PA among older adults. Although a few studies have examined younger populations in the Mainland of China81 and populations living outside the Mainland of China (e.g., in Taiwan, China,82 and Hong Kong, China83, 84), little empirical evidence has been gathered from studies using mainland populations of community-living older adults. There is enormous potential for Chinese researchers to fill the knowledge gap in this area.
From a public health perspective, it is important to understand and delineate specific social and environmental correlates (factors associated with activity) and/or determinants (those with a causal relationship) of PA,85, 86 including factors associated with popular activities such as walking or cycling,87 so that interventions can be developed that target level-specific factors contributing to increased PA in older adults. Ecological-based theories88, 89 suggest that PA is influenced by multiple impeding and facilitating factors at various levels,87, 90, 91 including individuals (e.g., health status, intention, self-efficacy, attitudes), neighborhood social structures (e.g., social support, social capital, cohesion and engagement, neighborhood socioeconomic status), and characteristics of the built environment in the context of Chinese urban design53 where PA, including walking, occurs (e.g., the prevalence of parks and green spaces, shopping areas, walkability, accessibility, aesthetics, safety from traffic and crime).90, 91, 92, 93 Such a conceptual perspective is intrinsically multilevel; that is, factors that influence PA need to be viewed as simultaneously operating at the individual level and at the community/organizational level, as well as across levels of a hierarchy (e.g., cross-level interaction effects between variables at different levels). These factors could be further applied at the micro and macro levels across settings (i.e., rural, suburban, and urban), thus yielding even more useful information for the design of multilevel health-promotion interventions.
Surveys have shown that PAs among older Chinese adults primarily take place in outdoor settings in immediate living environments (e.g., parks, streets, and neighborhoods),43, 44 which makes the community context a unique setting in which to study and promote PA in this population.90 However, little attention has been paid to the impact of environmental modifications brought about by urbanization on older adults' PA behaviors. For example, we know little about the association between community-built environmental features and levels of PA, including walking, among older Chinese adults. Examples of these features include parks and open spaces (and the exercise equipment at these locations), street connectivity and density of intersections, and access to public transportation, grocery stores, and sidewalks. Both qualitative and quantitative studies are needed in order to understand how these features can help create friendly and livable community environments that are conducive to walking and biking and that maximize the opportunities for outdoor PA by older adults with varying physical abilities and with various medical or health conditions.
Walking is one of most purposeful activities reported by older adults.43, 44 However, with China's increased urbanization and resulting urban density, along with its rapid expansion of road infrastructure for motorization, the country is slowly drifting away from its traditional pedestrian- and bicycle-oriented forms of transportation,48 which means that residents of many neighborhoods now predominantly use motor vehicles or public transportation (e.g., rail transit, buses).49 If this trend continues, non-motorized active transportation behaviors94 will likely be discouraged or made extremely difficult. Therefore, research is needed to determine the extent to which the change from traditional to contemporary urban forms influences the degree to which older Chinese adults use either walking or cycling as a type of PA for sport, recreational, or utilitarian purposes.
Given the continually worsening situation involving air quality, research is urgently needed to determine the demarcation point at which the level of ambient air pollution increases or attenuates health risks in relation to walking or biking for either leisure or utilitarian purposes.12 Studies using the geographic information system (GIS) and remote sensing technologies are needed to identify seasonal and time-sensitive geographic locations (i.e., hot-spots) where high levels of air pollution may exacerbate negative health consequences when walking or biking. This information can subsequently be used to inform public health efforts to improve living environmental conditions and encourage healthy engagement in outdoor PA.
Research is also needed to examine how changes and transitions brought about by rapid urbanization and rural-to-urban migration may have impacted or modified PA behaviors among older adults with different chronic disease conditions, especially among those living in rural areas where high mortality95, 96 and inequalities in health and healthcare resources2, 4 have been reported. This research should focus on examining environmental influences on PA among older adults with chronic conditions as they relate to living environments (e.g., senior living facilities vs. community-based neighborhoods, rural vs. urban settings). This is an important research area of high public health significance because it can help us understand the relationship between living environments and levels of PA, thus assisting us in determining how healthcare resources should be prioritized and how interventions might be tailored for older adults living in different settings.
6.3. Developing and evaluating interventions
In recent years, the overall number of exercise-based intervention studies in China has increased significantly. Nevertheless, the number of well-designed and carefully conducted RCTs that address important public health issues remains low. These issues include (1) the prevalence of chronic diseases,4, 7, 97 (2) falls and fall-related injuries,98 (3) poor lifestyle behaviors including physical inactivity,2 and (4) the health benefits of PA in older adults. As a result, very few rigorously tested exercise interventions have been identified that can be appropriately used and widely disseminated in efforts to reduce health risks and improve the health of China's aging population.
To prevent and reduce chronic disease and improve the quality of life of older Chinese adults, there is an urgent need to develop exercise interventions and rigorously evaluate them through well-designed RCTs. Such interventions are needed to establish a coordinated public health approach encompassing 3 levels: (1) preserving health and preventing physical inactivity among disease-susceptible older adults (primary prevention), (2) restoring health and reducing the severity of disease through prompt intervention (secondary prevention), and (3) minimizing disease-related suffering, limiting the degree of disability, and promoting PA in people with chronic diseases (tertiary prevention).99
Efficacy (or explanatory) trials of exercise interventions are often carried out under tightly controlled or optimal conditions with carefully selected populations. This means that the interventions may be less effective when implemented in real-world settings. Therefore, a pragmatic approach is needed to make these efficacy-based interventions work in community and clinical practice. Two recent studies serve as positive examples: a community-based trial that examined a multifaceted fall-prevention intervention for older Chinese adults73 and a study examining a community-based individualized lifestyle intervention for older adults with diabetes and hypertension.75 Results from these types of trials are more likely to be generalizable to their intended populations.
There is an equally important need to evaluate the cost-effectiveness of evidence-based interventions. Cost information is imperative from a policy-making standpoint. Policymakers and healthcare planners and providers must have accurate cost information in order to choose programs that have been shown to be clearly beneficial. Accurate cost-effectiveness information can reduce the demand for expensive medical care for treatment of chronic diseases and improve the quality of life among vulnerable older adults.
6.4. Enhancing scientific rigor in research design and methodologies
A large majority of the published studies from China suffer from poor research designs and methodologies, including issues related to the use of non-experimental designs, low response rates, improper use of the unit or level of analysis, lack of proper control for confounders, small sample sizes, unpowered or underpowered studies stemming from a lack of pilot work, multiple outcomes that are not specified a priori, and multiple statistical testing. Rigorously designed studies are needed to enhance the internal and external validity and generalizability of the study findings and to provide a high standard of evidence that can be used in developing public health policies and initiatives and in making clinical decisions.100
More population-based cohort studies are needed in order to understand the patterns and correlates of PA in older Chinese adults. In particular, longitudinal designs with repeated measures of PA outcomes over time are needed. Additionally, time-varying factors (e.g., perceived health, body weight), which can change value over the course of the observation period, and invariant factors (e.g., gender, education), which remain constant over the course of observation, should be used as covariates to examine change in PA. Given the multilevel influences of individual- and community-level variables, a multilevel analytic framework is needed to take into account within- and between-level changes in PA.
Intervention studies that use RCT designs101 are strongly recommended in evaluating the efficacy and effectiveness of an exercise intervention. These studies should seek to answer questions of high public health importance (e.g., whether the intervention is effective in reducing the health burdens brought on by high-priority diseases, such as stroke, ischemic heart disease, and respiratory diseases).6 They should also (1) have specifically targeted populations (e.g., sedentary older adults or those with chronic disease conditions for which the intervention can have a meaningful impact), (2) have carefully considered outcome measures that are well defined, reliable, and valid (e.g., that can be assessed with objective measures), (3) be fully randomized (at either the individual or group level), (4) be sufficiently powered, and (5) have planned analyses, with intent to treat, on pre-planned primary and/or secondary outcomes. Studies that test the sustainability of the intervention over the long term are also needed.
6.5. Multidisciplinary research
To gain a more complete understanding of the multiple influences that affect PA levels in older adults, a multidisciplinary research approach is encouraged. Exercise and PA researchers, public health practitioners, health education/epidemiology experts, health economics specialists, civic planning/urban design/transportation professionals, and GIS technologists need to work together to identify economic, biological, demographic, physical, built–environmental, and social–psychological factors that either facilitate or hinder PA among older Chinese adults. Fostering multidisciplinary research will enhance knowledge in the field and lead to the integration of theory and practice in the field of exercise and PA. The end result will offer improvement in the identification of effective interventions for preventing chronic disease and lessening health risks, better implementation policies and strategies, improvements in health and healthcare at the population level, and reductions in healthcare costs.
7. Conclusion
With China continuing on its path toward stabilizing economic reform and expanding urbanization, there is a significant lack of epidemiological studies related to PA among the population of older Chinese adults. Insufficient attention has been given to the development and evaluation of PAs and exercise interventions that will meet the public health needs of this fast-growing population group. These unmet needs and challenges call for an accelerated effort in the fields of PA epidemiology and aging. Such an effort will promote epidemiological studies that address the health benefits of PA and will ultimately inform policy initiatives and preventive strategies aimed at reducing the disease burden and promoting healthy aging in China.
Competing interests
The author declares no competing finacial interest.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.The World Bank Population estimates and projections. 2016. http://datatopics.worldbank.org/hnp/popestimates Available at: accessed 15.04.2016.
- 2.World Health Organization China country assessment report on ageing and health. 2015. http://apps.who.int/iris/bitstream/10665/194271/1/9789241509312_eng.pdf Available at: accessed 09.06.2016.
- 3.Dong P.T., Zhai D.H. Active aging is becoming a major strategic plan of Central Committee of CPC. In: Wu Y.S., Dang J.W., editors. China report of the development on aging cause. Social Sciences Academic Press; Beijing: 2013. pp. 1–24. in Chinese. [Google Scholar]
- 4.The World Bank Toward a healthy and harmonious life in China: stemming the rising tide of non-communicable diseases. 2011. http://www.worldbank.org/content/dam/Worldbank/document/NCD_report_en.pdf Available at: accessed 01.06.2016.
- 5.Gong P., Liang S., Carlton E.J., Jiang Q.W., Wu J.Y., Wang L. Urbanisation and health in China. Lancet. 2012;379:843–852. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mu X.Y., Yu F., Zhai D.H. The new type urbanization ought to include the friendly environment of the elderly. In: Wu Y.S., Dang J.W., editors. China report of the development on aging cause. Social Sciences Academic Press; Beijing: 2013. pp. 168–191. in Chinese. [Google Scholar]
- 7.Fang E.F., Scheibye-Knudsen M., Jahn H.J., Li J., Ling L., Guo H. A research agenda for aging in China in the 21st century. Ageing Res Rev. 2015;24:197–205. doi: 10.1016/j.arr.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye L., Wu A.M. Urbanization, land development, and land financing: evidence from Chinese cities. J Urban Aff. 2014;36:354–368. [Google Scholar]
- 9.United States Department of Energy Vehicles per thousand people: U.S. vs. other world regions. 2014. http://energy.gov/eere/vehicles/fact-841-october-6-2014-vehicles-thousand-people-us-vs-other-world-regions Available at: accessed 09.06.2016.
- 10.Wolch J.R., Byrne J., Newell J.P. Urban green space, public health, and environmental justice: the challenge of making cities ‘just green enough’. Landsc Urban Plan. 2014;125:234–244. [Google Scholar]
- 11.Yin H., Xu J. 2009. Measuring the accessibility of parks: a case study in Shanghai, China. Fuzzy systems and knowledge discovery, 2009 – FSKD'09. Sixth International Conference on IEEE; Tianjin, China. August 14–16. [Google Scholar]
- 12.Li F., Liu Y., Lü J., Liang L., Harmer P. Ambient air pollution in China poses a multifaceted health threat to outdoor physical activity. J Epidemiol Community Health. 2015;69:201–204. doi: 10.1136/jech-2014-203892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lü J., Liang L., Feng Y., Li R., Liu Y. Air pollution exposure and physical activity in China: current knowledge, public health implications, and future research needs. Int J Environ Res Public Health. 2015;12:14887–14897. doi: 10.3390/ijerph121114887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rohde R.A., Muller R.A. Air pollution in China: mapping of concentrations and sources. PLoS One. 2015;10 doi: 10.1371/journal.pone.0135749. e0135749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Department of Economic and Social Affairs Population Division, United Nations World population ageing. http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf Available at: accessed 09.06.2016.
- 16.The Work Bank Death rate, crude (per 1,000 people) 2016. http://data.worldbank.org/indicator/SP.DYN.CDRT.IN Available at: accessed 09.06.2016.
- 17.Smith J.P., Strauss J., Zhao Y. Healthy aging in China. J Econ Ageing. 2014;4:37–43. doi: 10.1016/j.jeoa.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu X.L., Luo X.H. Healthy aging as the core concept of the medical and health services for the elderly. In: Wu Y.S., Dang J.W., editors. China report of the development on aging cause. Social Sciences Academic Press; Beijing: 2013. pp. 94–116. in Chinese. [Google Scholar]
- 19.Department of Health and Human Services, World Health Organization Global health and aging. https://www.nia.nih.gov/research/publication/global-health-and-aging/preface Available at: accessed 09.06.2016.
- 20.Mi Y.J., Zhang B., Wang H.J., Yan J., Han W., Zhao J. Prevalence and secular trends in obesity among Chinese adults, 1991–2011. Am J Prev Med. 2015;49:661–669. doi: 10.1016/j.amepre.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu Y., Wang L., He J., Bi Y., Li M., Wang T. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–958. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 22.Lei X.Y., Sun X.T., Strauss J., Zhao Y.H., Yang G.H., Hu P. Health outcomes and socio-economic status among the mid-aged and elderly in China: evidence from the CHARLS national baseline data. J Econ Ageing. 2014;3:29–43. doi: 10.1016/j.jeoa.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan K.Y., Wang W., Wu J.J., Liu L., Theodoratou E., Car J. Epidemiology of Alzheimer's disease and other forms of dementia in China, 1990–2010: a systematic review and analysis. Lancet. 2013;381:2016–2023. doi: 10.1016/S0140-6736(13)60221-4. [DOI] [PubMed] [Google Scholar]
- 24.Fu F., Guo Y., Kowal P., Jiang Y., Yu M., Li X. Prevalence of major chronic conditions among older Chinese adults: the Study on Global AGEing and Adult Health (SAGE) Wave 1. PLoS One. 2013;8 doi: 10.1371/journal.pone.0074176. e74176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang X., Yang H., Wang H.H., Qiu Y., Lai X., Zhou Z. The association between physical activity, mental status, and social and family support with five major non-communicable chronic diseases among elderly people: a cross-sectional study of a rural population in Southern China. Int J Environ Res Public Health. 2015;12:13209–13223. doi: 10.3390/ijerph121013209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bao C., Mayila M., Ye Z., Wang J., Jin M., He W. Forecasting and analyzing the disease burden of aged population in China, based on the 2010 Global Burden of Disease Study. Int J Environ Res Public Health. 2015;12:7172–7184. doi: 10.3390/ijerph120707172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization (WHO) Global burden of disease. Estimates from 2000–2012. Cause-specific mortality. 2014. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html Available at: accessed 09.06.2016.
- 28.Ministry of Enviromental Protection of China Ambient Air Quality Standards. GB 3095–2012. 2012. http://kjs.mep.gov.cn/hjbhbz/bzwb/dqhjbh/dqhjzlbz/201203/W020120410330232398521.pdf Available at: accessed 09.06.2016; in Chinese.
- 29.Lee I.-M., Blair S., Manson J., Paffenbarger R.S. Oxford University Press; New York, NY: 2009. Epidemiological methods in physical activity. [Google Scholar]
- 30.Spirduso W.W. 2nd ed. Human Kinetics; Champaign, IL: 2005. Physical dimensions of aging. [Google Scholar]
- 31.Bouchard C., Blair S.N., Haskell W.L. Human Kinetics; Champaign, IL: 2007. Physical activity and health. [Google Scholar]
- 32.Dishman R.K., Heath G.W., Lee I.M. Human Kinetics; Champaign, IL: 2013. Physical activity epidemiology. [Google Scholar]
- 33.Hong Y.L., Lu Y.Z. Physical activity and health among older adults in China. J Aging Phys Act. 1999;7:247–250. [Google Scholar]
- 34.Guo Y., Shi H., Yu D., Qiu P. Health benefits of traditional Chinese sports and physical activity for older adults: a systematic review of evidence. J Sport Health Sci. 2016;5:270–280. doi: 10.1016/j.jshs.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lü J., Fu W., Liu Y. Physical activity and cognitive function among older adults in China: a systematic review. J Sport Health Sci. 2016;5:287–296. doi: 10.1016/j.jshs.2016.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhu W., Chi A., Sun Y. Physical activity among older Chinese adults living in urban and rural areas: a review. J Sport Health Sci. 2016;5:281–286. doi: 10.1016/j.jshs.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muntner P., Gu D., Wildman R.P., Chen J., Qan W., Whelton P.K. Prevalence of physical activity among Chinese adults: results from the International Collaborative Study of Cardiovascular Disease in Asia. Am J Public Health. 2005;95:1631–1636. doi: 10.2105/AJPH.2004.044743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu Y.J., Ma W.J., Xu X.J., Cai Q.M., Song X.L., Ni S.P. Patterns in influencing factors of physical activity among residents in Guangdong Province. South Chin J Prev Med. 2009;35:5. in Chinese. [Google Scholar]
- 39.Lee S.A., Xu W.H., Zheng W., Li H., Yang G., Xiang Y.B. Physical activity patterns and their correlates among Chinese men in Shanghai. Med Sci Sports Exerc. 2007;39:1700–1707. doi: 10.1249/mss.0b013e3181238a52. [DOI] [PubMed] [Google Scholar]
- 40.Jurj A.L., Wen W., Gao Y.T., Matthews C.E., Yang G., Li H.L. Patterns and correlates of physical activity: a cross-sectional study in urban Chinese women. BMC Public Health. 2007;7:213. doi: 10.1186/1471-2458-7-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Du H., Li L., Whitlock G., Bennett D., Guo Y., Bian Z. Patterns and socio-demographic correlates of domain-specific physical activities and their associations with adiposity in the China Kadoorie Biobank study. BMC Public Health. 2014;14:826. doi: 10.1186/1471-2458-14-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang M., Chen X., Wang Z., Wang L., Jiang Y. Leisure-time physical exercise and sedentary behavior among Chinese elderly, in 2010. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35:242–245. in Chinese. [PubMed] [Google Scholar]
- 43.General Administration of Sport of China Physical activity survey of urban and rural areas in China in 2007. 2008. http://www.gov.cn/test/2012-04/19/content_2117453.htm Available at: accessed 05.05.2016; in Chinese.
- 44.General Administration of Sport of China Survey report of exercise activities for the general public in 2014. 2015. http://www.sport.gov.cn/n16/n1077/n1422/7300210.html?from=singlemessage&isappinstalled=0 Available at: accessed 05.05.2016; in Chinese.
- 45.Dai H., Jia G., Liu K. Health-related quality of life and related factors among elderly people in Jinzhou, China: a cross-sectional study. Public Health. 2015;129:667–673. doi: 10.1016/j.puhe.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 46.Du W.J., Tan J.P., Yi F., Zou Y.M., Gao Y., Zhao Y.M. Physical activity as a protective factor against depressive symptoms in older Chinese veterans in the community: result from a national cross-sectional study. Neuropsychiatr Dis Treat. 2015;11:803–813. doi: 10.2147/NDT.S80295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Qin L., Corpeleijin E.C., Jiang C., Thomas G.N., Schooling C.M., Zhang W. Physical activity, adiposity, and diabetes risk in middle-aged and older Chinese population: the Guangzhou Biobank Cohort Study. Diabetes Care. 2010;33:2342–2348. doi: 10.2337/dc10-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pan H.X., Shen Q., Zhang M. Influence of urban form on travel behavior in four neighborhoods of Shanghai. Urban Stud. 2009;46:275–294. [Google Scholar]
- 49.Lin H., Sun G., Li R. The influence of built environment on walking behavior: measurement issues, theoretical considerations, modeling methodologies and Chinese empirical studies. In: Kwan M.P., Richardson D., Wang D., Zhou C., editors. Space-time integration in geography and GIScience. Springer Science + Business Media B.V.; Dordrecht: 2015. pp. 53–75. [Google Scholar]
- 50.Alcom T., Quyang Y. China's invisible burden of foodborne illness. Lancet. 2012;379:789–790. doi: 10.1016/s0140-6736(12)60330-4. [DOI] [PubMed] [Google Scholar]
- 51.Wang Y.F., Yiu Y.S., Li Y.H., Li T.T. The spatial-temporal patterns of urban-rural development transformation in China since 1990. Habitat Int. 2016;53:178–187. [Google Scholar]
- 52.He C.F., Chen T.M., Mao X.Y., Zhou Y. Economic transition, urbanization and population redistribution in China. Habitat Int. 2016;51:39–47. [Google Scholar]
- 53.Kuang W.H., Liu J.Y., Dong J.W., Chi W.F., Zhang C. The rapid and massive urban and industrial land expansions in China between 1990 and 2010: a CLUD-based analysis of their trajectories, patterns, and drivers. Landsc Urban Plan. 2016;145:21–33. [Google Scholar]
- 54.Alfonzo M., Guo Z., Lin L., Day K. Walking, obesity and urban design in Chinese neighborhoods. Prev Med. 2014;69(Suppl. 1):S79–85. doi: 10.1016/j.ypmed.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 55.Zhou R., Li Y., Umezaki M., Ding Y., Jiang H., Comber A. Association between physical activity and neighborhood environment among middle-aged adults in Shanghai. J Environ Public Health. 2013;2013:239595. doi: 10.1155/2013/239595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Su M., Tan Y.Y., Liu Q.M., Ren Y.J., Kawachi I., Li L.M. Association between perceived urban built environment attributes and leisure-time physical activity among adults in Hangzhou, China. Prev Med. 2014;66:60–64. doi: 10.1016/j.ypmed.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 57.Jia Y., Usagawa T., Fu H. The association between walking and perceived environment in Chinese community residents: a cross-sectional study. PLoS One. 2014;9 doi: 10.1371/journal.pone.0090078. e90078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gao J., Fu H., Li J., Jia Y. Association between social and built environments and leisure-time physical activity among Chinese older adults—a multilevel analysis. BMC Public Health. 2015;15:1317. doi: 10.1186/s12889-015-2684-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mortimer J.A., Ding D., Borenstein A.R., DeCarli C., Guo Q., Wu Y. Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented Chinese elders. J Alzheimers Dis. 2012;30:757–766. doi: 10.3233/JAD-2012-120079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li R., Zhu X., Yin S., Niu Y., Zheng Z., Huang X. Multimodal intervention in older adults improves resting-state functional connectivity between the medial prefrontal cortex and medial temporal lobe. Front Aging Neurosci. 2014;6:39. doi: 10.3389/fnagi.2014.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sun J., Kanagawa K., Sasaki J., Ooki S., Xu H., Wang L. Tai chi improves cognitive and physical function in the elderly: a randomized controlled trial. J Phys Ther Sci. 2015;27:1467–1471. doi: 10.1589/jpts.27.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hu J.P., Guo Y.H., Wang F., Zhao X.P., Zhang Q.H., Song Q.H. Exercise improves cognitive function in aging patients. Int J Clin Exp Med. 2014;7:3144–3149. [PMC free article] [PubMed] [Google Scholar]
- 63.Lü J., Sun M., Liang L., Feng Y., Pan X., Liu Y. Effects of momentum-based dumbbell training on cognitive function in older adults with mild cognitive impairment: a pilot randomized controlled trial. Clin Interv Aging. 2015;6:9–16. doi: 10.2147/CIA.S96042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wei X.H., Ji L.L. Effect of handball training on cognitive ability in elderly with mild cognitive impairment. Neurosci Lett. 2014;566:98–101. doi: 10.1016/j.neulet.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 65.Yang S.Y., Shan C.L., Qing H., Wang W., Zhu Y., Yin M.M. The effects of aerobic exercise on cognitive function of Alzheimer's disease patients. CNS Neurol Disord Drug Targets. 2015;14:1292–1297. doi: 10.2174/1871527315666151111123319. [DOI] [PubMed] [Google Scholar]
- 66.Yin S., Zhu X., Li R., Niu Y., Wang B., Zheng Z. Intervention-induced enhancement in intrinsic brain activity in healthy older adults. Sci Rep. 2014;4:7309. doi: 10.1038/srep07309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zheng Z., Zhu X., Yin S., Wang B., Niu Y., Huang X. Combined cognitive-psychological-physical intervention induces reorganization of intrinsic functional brain architecture in older adults. Neural Plast. 2015;2015:713104. doi: 10.1155/2015/713104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tao J., Liu J., Egorova N., Chen X., Sun S., Sue X. Increased hippocampus-medical prefrontal cortex resting-state frontal connectivity and memory function after Tai Chi Chuan practice in elder adults. Front Aging Neurosci. 2016;8:25. doi: 10.3389/fnagi.2016.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhu Q., Huang L., Wu X., Wang L., Zhang Y., Fang M. Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis: a randomized controlled trial. J Sport Health Sci. 2016;5:297–303. doi: 10.1016/j.jshs.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhuang J., Huang L., Wu Y., Zhang Y. The effectiveness of a combined exercise intervention on physical fitness factors related to falls in community-dwelling older adults. Clin Interv Aging. 2014;9:131–140. doi: 10.2147/CIA.S56682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu J., Wang X.Q., Zheng J.J., Pan Y.J., Hua Y.H., Zhao S.M. Effects of Tai Chi versus proprioception exercise program on neuromuscular function of the ankle in elderly people: a randomized controlled trial. Evid Based Complement Alternat Med. 2012;2012:265486. doi: 10.1155/2012/265486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yu D.H., Yang H.X. The effect of Tai Chi intervention on balance in older males. J Sport Health Sci. 2012;1:57–60. [Google Scholar]
- 73.Xia Q.H., Jiang Y., Niu C.J., Tang C.X., Xia Z.L. Effectiveness of a community-based multifaceted fall-prevention intervention in active and independent older Chinese adults. Inj Prev. 2009;15:248–251. doi: 10.1136/ip.2008.020420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhu H., Zhang N., Ji C. Influence of Baduanjin on mild cognitive impairment in elderly diabetic patients. Chin J Pract Nurs. 2009;31:1202–1204. [Google Scholar]
- 75.Yu R., Yan L.L., Wang H., Ke L., Yang Z., Gong E. Effectiveness of a community-based individualized lifestyle intervention among older adults with diabetes and hypertension, Tianjin, China, 2008–2009. Prev Chronic Dis. 2014;11:E84. doi: 10.5888/pcd11.120333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion Physical activity guidelines for Americans. 2016. http://health.gov/paguidelines/guidelines/ Available at: accessed 27.03.2016.
- 77.Department of Health Physical activity guidelines for older adults. 2011. https://www.gov.uk/government/publications/uk-physical-activity-guidelines Available at: accessed 09.06.2016.
- 78.World Health Organization Physical activity and older adults—Recommended levels of physical activity for adults aged 65 and above. 2010. http://www.who.int/dietphysicalactivity/factsheet_olderadults/en/ Available at: accessed 09.06.2016.
- 79.Centers for Disease Control and Prevention Behavioral risk factor surveillance system. 2011. http://www.cdc.gov/brfss/ Available at: accessed 20.04.2016.
- 80.Kohl H.W., Kimsey C.D. Physical activity surveillance. In: Lee I.M., Blair S., Manson J., Paffenbarger R.S., editors. Epidemiologic methods in physical activity studies. Oxford University Press; New York, NY: 2009. p. 1166. [Google Scholar]
- 81.Ng S.W., Howard A.G., Wang H.J., Su C., Zhang B. The physical activity transition among adults in China: 1991–2011. Obes Rev. 2014;15:27–36. doi: 10.1111/obr.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huang S.J., Hung W.C., Sharpe P.A., Wai J.P. Neighborhood environment and physical activity among urban and rural schoolchildren in Taiwan. Health Place. 2010;16:470–476. doi: 10.1016/j.healthplace.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 83.Cerin E., Lee K.Y., Barnett A., Sit C.H., Cheung M.C., Chan W.M. Objectively-measured neighborhood environments and leisure-time physical activity in Chinese urban elders. Prev Med. 2013;56:86–89. doi: 10.1016/j.ypmed.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 84.Barnett A., Cerin E., Ching C.S., Johnson J.M., Lee R.S. Neighborhood environment, sitting time and motorised transport in older adults: a cross-sectional study in Hong Kong. BMJ Open. 2015;5:e007557. doi: 10.1136/bmjopen-2014-007557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bauman A., Bull F.C. Environmental correlates of physical activity and walking in adults and children: a review of reviewers. 2007. https://www.nice.org.uk/guidance/ph8/evidence/environmental-correlates-of-physical-activity-review2 Available at: accessed 30.01.2016.
- 86.Bauman A.E., Reis R.S., Sallis J.F., Wells J.C., Loos R.J., Martin B.W. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 87.Wang Y., Chau C.K., Ng W.Y., Leung T.M. A review on the effects of physical built environment attributes on enhancing walking and cycling activity levels within residential neighborhoods. Cities. 2016;50:1–15. [Google Scholar]
- 88.King A.C., Stokols D., Talen E., Brassington G.S., Killingsworth R. Theoretic approaches to the promotion of physical activity forging a transdisciplinary paradigm. Am J Prev Med. 2002;23:15–25. doi: 10.1016/s0749-3797(02)00470-1. [DOI] [PubMed] [Google Scholar]
- 89.Sallis J.F., Owen N. Ecological models of healthy behavior. In: Glanz K., Lewis F.M., Rimer B.K., editors. Health behavior and health education: theory, research and practice. Jossey-Bass; San Francisco, CA: 2002. pp. 462–484. [Google Scholar]
- 90.Li F., Fisher K.J., Bauman A., Ory M.G., Chodzko-Zajko W., Harmer P. Neighborhood influences on in middle-aged and older adults: a multilevel perspective. J Aging Phys Act. 2005;13:87–114. doi: 10.1123/japa.13.1.87. [DOI] [PubMed] [Google Scholar]
- 91.Li F. Influences of social and built environment on physical activity in middle-aged and older adults. In: Meyer A.L., Gullotta T.P., editors. Physical activity across the lifespan: prevention and treatment for health and well-being. Springer; New York, NY: 2012. pp. 65–80. [Google Scholar]
- 92.Carr K., Weir P.L., Azar D., Azar N.R. Universal design: a step toward successful aging. J Aging Res. 2013;2013:324624. doi: 10.1155/2013/324624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Haselwandter E.M., Corcoran M.P., Folta S.C., Hyatt R., Fenton M., Nelson M.E. The built environment, physical activity, and aging in the United States: a state of the science review. J Aging Phys Act. 2015;23:323–329. doi: 10.1123/japa.2013-0151. [DOI] [PubMed] [Google Scholar]
- 94.Sallis J.F., Frank L.D., Saelens B.E., Krafe M.K. Active transportation and physical activity: opportunities for collaboration on transportation and public health research. Transport Res A- Pol. 2004;38:249–268. [Google Scholar]
- 95.Zimmer Z., Kaneda T., Spess L. An examination of urban versus rural mortality in China using community and individual data. J Gerotol B Psychol Sci Sco Sci. 2007;62:349–357. doi: 10.1093/geronb/62.5.s349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li Q., Guo J., Cao X.Q., Yuan X., Ro K.Q., Zheng Z. Trend of non-communicable disease mortality for three common conditions in the elderly population from 2002 to 2010: a population-based study in China. Chronic Dis Translat Med. 2015;1:152–157. doi: 10.1016/j.cdtm.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tang S., Ehiri J., Long Q. China's biggest, most neglected health challenge: non-communicable diseases. Infect Dis Poverty. 2013;2:7. doi: 10.1186/2049-9957-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jiang J., Long J., Ling W., Huang G., Guo X., Su L. Incidence of fall-related injury among older people in mainland China. Arch Gerontol Geriatr. 2015;61:131–139. doi: 10.1016/j.archger.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 99.McKenzie J.F., Smeltzer J.L. Allyn and Bacon; Needham Heights, MA: 1997. Planning, implementing, and evaluating health promotion programs: a primer. [Google Scholar]
- 100.Bauman A., Phongsavan P. How can we increase physical activity level? In: Lee I.M., Blair S., Manson J., Paffenbarger R.S., editors. Epidemiologic methods in physical activity studies. Oxford University Press; New York, NY: 2009. pp. 302–316. [Google Scholar]
- 101.Friedman L.M., Furberg C.D., DeMets D.L. Springer; New York, NY: 1998. Fundamentals of clinical trials. [Google Scholar]


