Abstract
Limitation of access to lethal methods used for suicide—so-called means restriction—is an important population strategy for suicide prevention. Many empirical studies have shown that such means restriction is effective. Although some individuals might seek other methods, many do not; when they do, the means chosen are less lethal and are associated with fewer deaths than when more dangerous ones are available. We examine how the spread of information about suicide methods through formal and informal media potentially affects the choices that people make when attempting to kill themselves. We also discuss the challenges associated with implementation of means restriction and whether numbers of deaths by suicide are reduced.
Introduction
For more than a century, writers and researchers have considered suicide from two opposite perspectives, invoking broad cultural and societal factors as causes or focusing on uniquely individual characteristics and experiences to explain why people kill themselves. Public health approaches to suicide prevention, however, have to integrate these viewpoints and to develop strategies that will benefit most lives in an effective and measurable way.
Suicide is a well recognised public health challenge. WHO estimates that the global suicide rate is about 16 per 100 000 individuals per year, which is a 45% increase in the past 45 years.1 Depending on the nation cited by WHO, suicide is one of the top three leading causes of death in people aged 10–24 years or 15–44 years, and often is an especially large burden late in life, when suicide rates are highest in many countries.2 Therefore, suicide causes the loss of many potential years of life and has substantial economic and emotional costs, disrupting families, communities, and society, broadly ramifying sadness and loss.3
Many countries have initiated suicide prevention programmes,4,5 which use public health strategies that focus on individuals in known high-risk groups and promote population-oriented strategies to broadly reduce risk, in keeping with Rose’s theorem (many people at low risk might give rise to more cases than would a small number at high risk).6 Suicide is not a disease caused by well defined pathological mechanisms, and the occurrence of suicidal behaviour is usually an outcome of complex interactions of socio-environmental, behavioural, and psychiatric factors.6 Identified risk factors, such as severe depression or other mental illnesses, do not have sufficient specificity (ie, high rates of false positives) to guide effective preventive actions.7
One important population strategy to reduce suicides has been modification of the environment to decrease general access to suicide means. This approach (so- called means restriction) is reported to be one of the intervention measures with strongest empirical support.8,9 Several factors apparently underpin the effectiveness of this approach. Many suicidal people cannot be accessed with interventions or restrictions at the time of their greatest risk; indeed, they often seek to avoid detection. The probability of individuals attempting suicide decreases when they are precluded from implementing a preferred method10—ie, suicide attempts are often method-specific. Moreover, if a highly lethal method is not available and some individuals do not defer their attempt, they frequently use less lethal, more common ones (eg, drug overdose). From the perspectives of public health and injury prevention, the choice of a method that is less lethal than are others can be advantageous if the attempt proves to be non-fatal.
The case fatality of suicide methods varies greatly (appendix).11–14 The potentially fatal moments of suicidal crises are often brief. Strongly felt ambivalence is common, with competing wishes to die and to live.9 The sudden, unplanned (or briefly planned) nature of many suicides implies that individuals tend to use the method most readily accessible to them. When a lethal method is unavailable at the moment of potential action, suicide attempts might be delayed so that (in some cases at least) suicidal impulses will pass without fatal effects.15 Even when individuals have planned, poor access to the most lethal means can be a substantial impediment.
Although means restriction is considered a generic preventive intervention, few investigators have assessed the relative strength of supporting evidence for different methods. Moreover, the potential effect of decreased access to various methods on overall suicide rates in different countries or regions has not been established. We review the empirical evidence for means restriction from the past decade (figure) and assess its effectiveness and its relation to the dissemination of information about different methods of suicide through various media outlets. We put special emphasis on the difficulties encountered when attempts to measure potential substitution effects are made. Additionally, we draw attention to the potential of socially enacted means restriction (ie, not absolute restriction) as a public health intervention for commonly available products.
Figure:
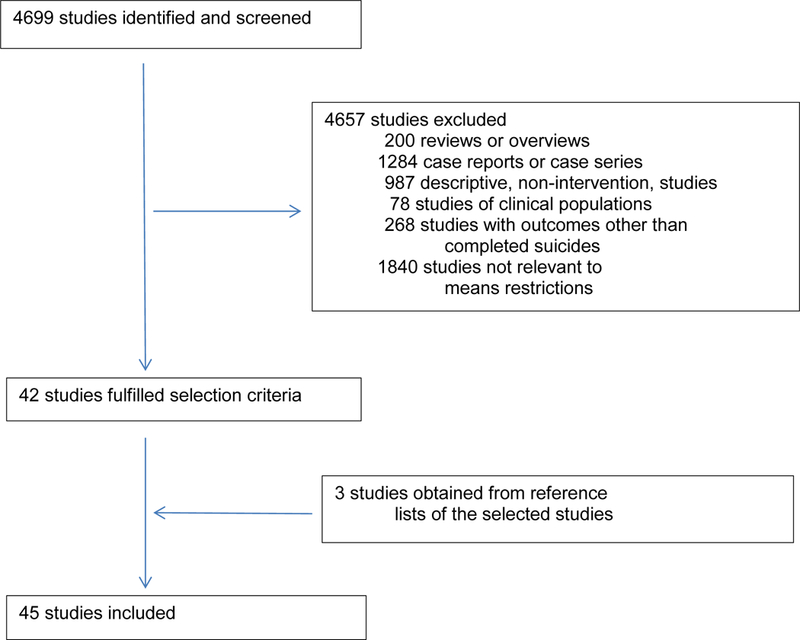
Selection process of studies cited
Theory of means restriction
Suicide is a rare event and high-risk factors are common (eg, depression, other mental disorders). A recurring challenge in suicide prevention is how to accurately identify vulnerable individuals in populations at risk. A prevention strategy that targets the population as a whole, such as means restriction, has many advantages, especially when implemented through so-called distal measures— eg, removal of carbon monoxide from domestic gas or withdrawal of highly lethal pesticides from the market.
Means restriction entails a community or societal action that (ideally) does not depend on an individual’s intention or volition. Applied to the population as a whole, it typically affects people whose suicide risk is otherwise undetected and who do not seek therapeutic assistance to prevent their crisis or for life-saving interventions when necessary. Removal or restriction of access to a lethal method changes the context of a potential suicide by precluding potentially fatal actions or forcing the use of a less lethal method. Because means restriction is broadly applied, detection of its individual- level effect is often impossible; it is best measured by aggregate findings of method-specific community rates of suicide and related self-harm injuries.
As a public health measure, means restriction has a long history; removal of the pump handle in Broad Street, London, UK, by John Snow was an early example and a historic landmark in public health practice.16 Similar approaches have been widely applied in criminology, with the label of opportunity-reduction theory (or so-called situational crime prevention).17 Instead of a focus on individual criminals, an opportunity-reduction approach introduces discreet managerial and environmental changes to reduce the opportunities for crime. Suicide can be affected or forestalled by alteration of environments or access.17 To be successful, this type of strategy depends on committed societal leadership and sustained political will. This approach fits with the notion of context changes to make individuals’ default decisions healthy. The principle of this type of intervention is that individuals would have to expend substantial effort not to benefit.18
Although means restriction can be broadly applied, related approaches exist for individuals. Clinicians can work with high-risk patients and their kin to remove potentially lethal methods from the immediate environment. By contrast with universal approaches, this strategy necessitates care providers’ vigilance and cooperative participation by people close to the suicidal individual. Such safety planning is not means specific, but is tailored to individuals and situations.
Suicide rate, method availability, and lethality
International variations in common suicide methods suggest that these patterns are linked closely to differences in the availability and lethality of specific approaches.19 Suicides by pesticide poisoning (case fatality up to 75%) have been common in many Asian and Latin American countries where there are large agrarian populations,20 whereas many individuals killing themselves in cities and city states jump from high places (70% lethality).21,22 Indeed, jumping has accounted for more than 50% of suicides in Hong Kong and 80% of those in Singapore in the past 20 years.21
Thomas and colleagues23 described the large increase in suicides in the UK, first in men and later in women, after carbon monoxide gas from coalmines became widely available in the first half of the 20th century. Gas rose to become the primary national method of suicide. The replacement of coal gas with natural gas from North Sea wells between the late 1950s and early 1970s led to a gradual reduction in the carbon monoxide content of domestic gas, which in turn was followed by a steady and prominent decrease in fatal gassing and the overall suicide rate in the UK.23,24 This decline in the overall rate was directly caused by the reduction in suicide with domestic gas. Thomas and colleagues23 showed that the number of fatal gas poisonings in the UK rose in the early 1980s, but it later fell after the introduction of catalytic converters into car exhaust systems.25–29
The increased use of pesticides during the second half of the 20th century was associated with an increase in suicides in many agrarian societies.30 Prevention strategies have sought to substitute less lethal, newer generation compounds,31–33 and to install double-lock boxes34 to remove access to potentially lethal but commonly available chemicals. Enforcement of gun-control policies lowers numbers of firearm suicides.35–52
An individual’s choice of method is not only dependent on ready access to a specific means of suicide, but also on its socio-cultural acceptability.53 Local norms and traditions, moral attitudes towards suicide, knowledge about past suicides, and personal experience and accessibility all potentially shape a person’s suicidal actions. In turn, means restriction should shape contextual factors, promoting healthy decisions.
Means substitution after restriction
A common concern about means restriction has been that individuals will simply switch to other methods of suicide—ie, so-called means substitution. Such concern could be a result of distressed individuals being considered by clinicians as equally at risk of suicide by any method when they are assessed as being very suicidal. However, studies5 have shown that restriction of one method of suicide does not inevitably lead to a compensating rise in the use of others (as shown in the UK in the 1970s), just as the emergence of a new method (eg, domestic gas in the UK in the first half of the 20th century, or the burning of charcoal in confined spaces to generate toxic amounts of carbon monoxide in Hong Kong in the late 1990s) does not result in a substantial decline in the use of long-available means.
The occurrence of substitution varies between regions and is associated with individual characteristics such as age and sex (appendix).25,46 The effectiveness of means restriction differs between the sexes; women seem to be more responsive than are men, and method substitution is more common in men than in women (appendix).46 Where means restriction has been implemented in Asia—typically of pesticide and charcoal—substitution has been reported rarely.31,33,54,55 The cause of this apparent difference is unknown; characteristics of the populations affected or the restricted methods might play a part.
At the population level, means restriction proves most effective when the method is common and highly lethal, accounting for a substantial percentage of deaths.15,18 Common methods that have been restricted, such as domestic gas and pesticides, are available in the home. The likelihood that a specific method will lead to death is related to both its lethal properties and its accessibility. When reduction of access to a highly lethal method is possible, people who do attempt suicide with less dangerous means have an increased chance of survival. If the overall population rate of suicide is to be substantially reduced by means restriction, the fatality rate of alternative methods should be lower than that of the restricted method of suicide (appendix).15
The role of the media
Nowadays, publicly available media—whether in print, on television, or on the internet—might affect the creation or alteration of suicide methods, and hence affect suicide rates. The deaths of celebrities have been publicised.56 Perhaps most importantly, this type of rapid dissemination most often involves members of the public dying in extraordinary circumstances.57 For example, the media introduced and quickly disseminated reports on the burning of charcoal in a confined space in Hong Kong and Taiwan, which then rapidly increased and spread to other Asian regions in the late 1990s.23 An ethnographical investigation in Hong Kong58 established that people chose charcoal burning because they were reminded of the method by newspaper reports. An interview-based study in Taiwan59 showed that 87% of individuals who attempted suicide with charcoal burning reported that the media pointed them towards this method. Suicides by charcoal burning have been recorded in the UK.60 Whether charcoal burning would have spread so quickly had initial graphic reports, pictures, and diagrams not been presented in Hong Kong tabloids in 1998 is unknown. Therefore, in addition to sensationalising suicide, the media can provide precise instructions about how a method can be implemented, further complicating prevention initiatives.
New online social media can be used to disseminate information within minutes or hours, rather than slow diffusion of models or methods that was the norm previously, such as when domestic gas was introduced.61 As yet, little research has tested whether all forms of today’s media can be used to positively affect vulnerable individuals or populations in a way that promotes good mental health or adaptive help seeking at times of distress.62
Examples of means restriction
Implementation of means restriction can be viewed as a continuum, ranging from complete elimination or removal of a potentially fatal substance or compound (eg, changes in the composition of domestic cooking gas), through impeding or interfering with access (eg, barriers to jumping and packaging changes), to promotion of educational and social interventions to enhance safety (eg, education of clinicians to encourage families to remove potentially lethal means from the home). We believe that removal of an agent would have the greatest effects on broadly measured suicide rates, whereas social-educational interventions would be least potent, especially because they necessitate concerted and sustained actions by many individuals.
Legislation to restrict the quantities of paracetamol and other analgesics (eg, aspirin) sold was enacted in the UK in 1998. Early data suggested that mortality and morbidity associated with paracetamol overdose declined as a result,63,64 with little evidence for substitution to other kinds of analgesics, such as ibuprofen (a compound that is safer than is paracetamol).64 Subsequent studies65 have cast doubt on these early findings. Implementation of such legislation does not depend on specific actions of individuals, but is done during manufacture and with widely applied sales regulations. Further research is needed to establish whether people attempting suicide hoard their paracetamol supplies until they have sufficiently lethal amounts, and whether they have the patience to open blister packs to obtain enough pills. Such findings would point to carefully planned suicides and would potentially suggest that other prevention measures are needed.
In 2010, Yip and colleagues55 described the results of a controlled community experiment in Hong Kong, in which they moved bags of charcoal from easy self-service access on store counters to locked storage, so that customers had to ask store attendants for assistance. This measure did not prohibit purchases, but sales became a source of attention and slightly more time consuming than they had been previously. Compared with a district with a similar population size (500 000 inhabitants), area, and socioeconomic status that had no change in method of shelving, a measurable and significant decline in suicides was reported.55
Unlike repackaging of paracetamol, agreement of the managers of supermarket chains and day-to-day implementation by store employees was necessary to move the bags of charcoal. Such a high level of cooperation could pose substantial challenges, and many community members might resent or resist such constraints.
On the island of Cheung Chau in the Islands District of Hong Kong, deaths from poisoning by charcoal burning in holiday houses increased from three to four per year to the high of 14 in 2002.54 Most suicides were of visitors. The community reported negative effects on the island in terms of resort business and general wellbeing after a series of suicides.54 Island residents and businesses developed a self-help organisation to restrict access to holiday flats for distressed or suicidal individuals; owners refused to rent to people on their own. Store employees were alert to visitors who wished to purchase charcoal and beer but no food. The police cycled around the island to identify anyone deemed to be at risk of suicide and irregularities in the community. Of 40 000 residents, the number of suicides on the island declined to two in 2005, without any substantial increase on nearby islands.54 These findings emphasise that means restriction must be embedded into other efforts to modify environments, such as the restriction of access to rental units. Cohesive community action was the central part of this initiative; means restriction—like other elements of the Cheung Chau programme—was a result of concerted and widespread commitment.
The social dilemma
Application of universal measures for means restriction might be considered intrusive by many members of the community. Moreover, the benefits for most people will be small or non-existent. Thus, use of widely applied prevention measures could be met with substantial resistance, even though data support large population effects. Many community members express common misunderstandings that, despite data showing powerful population- level effects, a seriously suicidal person will inevitably find a way to die and that all methods have roughly equal case fatalities. In many community discussions about means restriction—whether control of access to bags of charcoal safety doors on subway platforms, or bridge barriers54,55,66–73—many participants believe that removal of access to one method of suicide would force people to use another.
On the basis of the data for relocation of bags of charcoal in supermarket chains in Hong Kong,55 prevention strategies should gain support from senior managers of affected companies, as well as having supporting scientific data. With appropriate media coverage and endorsement by community leaders, means restriction could gain greater acceptance and less resistance from the public than it does presently. The fundamental premise of means restriction is based on the assertion that it is both a community-level intervention and a community-supported initiative.
We suggest that policy makers and advocates consider several a priori criteria when assessing the potential benefits of means restraint. First, the method in consideration should contribute substantially to the mortality from suicide in the region because of its high lethality. Second, the method should be suitable for elimination or constraint, ideally with broadly applicable policy actions rather than day-to-day implementation by individuals, either alone or collectively. Third, they should assess whether a method is socially important or recognised (eg, suicides from iconic sites or bridges), when the preventive intervention would be noticed by many people, even though the overall contribution to regional rates might be marginal. Fourth, they should be able to monitor the implementation and effects of an intervention.
Limitations
Glasgow’s 2011 report74 emphasised that bridge barriers—however effective they might be at individual sites—do not lower regional suicide rates when people jumping from those bridges contributed little to the rates before the barriers were put in place. Although placement of such barriers might not lower regional rates—even when it prevents deaths at specific sites—the action conveys a powerful public message, expressing important community values and serving to promote help-seeking. Such committed political will to save lives could be one potential way to counteract media-driven contagion, because it affords opportunities for widespread discussion and collective community action.
Constraint or elimination of access to commonly used suicide methods of low lethality (eg, fairly non-toxic prescription or over-the-counter drugs) would have a negligible effect on rates and also might inadvertently force individuals attempting suicide in the future to use more lethal methods.75 When high-lethality methods have been constrained, some substitution with low- lethality means has been reported.76 Such findings do not indicate what exactly would happen if low-lethality methods were eliminated.75 For methods of intermediate lethality, such as charcoal burning, the potential gains from constraints that cannot entirely eliminate access should be assessed carefully (appendix).
Hanging, jumping from heights (particularly from individuals’ own apartments or houses), and fatal shooting with firearms in countries with relatively nonrestrictive gun laws such as the USA cannot be readily restricted. However, safety planning for firearm storage is potentially a form of means restriction when effectively applied as part of routine procedures. Similarly to the decision to place bags of charcoal behind shop counters, such changes need committed leadership, corporate cooperation, and consistent individual action to attain sustained, widespread implementation. In clinical practice, physicians and other health professionals should speak with family members about the removal of potentially lethal methods from the reach of vulnerable kin. This type of intervention necessitates an alert clinical provider, a vigilant family, and a cooperative patient, but too often one or several of these components could be absent.
Conclusion
Restriction of access to a specific suicide method can have a widespread effect when the method is highly lethal and common, and the means restriction is supported by the community. Newly emerging methods might have large effects as they spread through communities, and in the internet era, the results can be sudden and pronounced. Once a method of suicide has become common, it is especially difficult to eradicate. If faced with similar emerging methods in the future, policy makers should seek support from formal media outlets to restrain spread and lessen the effects, although informal media now makes such interventions even more challenging than previously.
It is beyond the scope of this report to define elements necessary for promotion of the type of collaborative community discussions that address the balance between the imperative of constraining potentially lethal methods of suicide and the wishes of most community members who are not at risk and might be inconvenienced. But just such discussions are necessary if further, meaningfully broad-based interventions are to be implemented. Although we have expressed concerns about the media’s potential to serve as a powerful vector for spreading contagion, these venues of information dissemination can effectively pass on scientific knowledge and protective guidance. As with discussions about means restriction, broad community participation and dynamic social leadership are necessary.
No one measure, however effective, can sufficiently address the many factors that contribute to regional or national suicide rates. A frank and open discussion of a community’s abiding values, legislative or policy changes, continuing community education, consultation about the challenges posed by suicide and its antecedents, and effective clinical management of individual cases are all necessary for prevention programmes.
Supplementary Material
Search strategy and selection criteria.
We searched PubMed, PsycINFO, ISI Web of Knowledge, and The Cochrane Library, with the terms “suicide” in combination with each method (ie, “jumping”, “hanging”, “charcoal burning”, “carbon monoxide poisoning”, “drowning”, “pesticide*”, “fi rearm*” and “medicine*” or “drug overdose”) and “restriction”, “availability”, “access”, or “means”. We included reports of epidemiological studies showing change in suicides or suicide rates after method restriction published between January, 2001, and January, 2012. Review articles, case reports, or studies based on clinical populations or those that had non-fatal outcomes (eg, suicidal behaviour or ideation) were excluded. The reference lists of identifi ed reports were also examined for relevant references.
Acknowledgments
PSFY was supported by a GRF grant of the University of Hong Kong (HKU 784210M). EC was partly supported by the National Institutes of Health (grant number D43TW009101). Y-YC was supported by the National Science Council, Taiwan (grant number 99–2314-B-532–004-) and the National Health Research Institute, Taiwan (grant number NHRI-EX100–10024PC). We thank the research team of the Centre for Suicide Research and Prevention (University of Hong Kong, Hong Kong SAR, China) for their diligent efforts to implement suicide prevention programmes in Hong Kong.
Footnotes
Conflicts of interest
We declare that we have no conflicts of interest.
Contributor Information
Prof Paul S F Yip, Department of Social Work and Social Administration, University of Hong Kong, Hong Kong SAR, China; Center for Suicide Research and Prevention, University of Hong Kong, Hong Kong SAR, China.
Saman Yousuf, Department of Social Work and Social Administration, University of Hong Kong, Hong Kong SAR, China.
Shu-Sen Chang, Center for Suicide Research and Prevention, University of Hong Kong, Hong Kong SAR, China.
Prof Eric Caine, Center for the Study and Prevention of Suicide, Department of Psychiatry, University of Rochester, Rochester, NY, USA; VA Center of Excellence for Suicide Prevention, Canandaigua, NY, USA.
Kevin Chien-Chang Wu, Department of Social Medicine, National Taiwan University College of Medicine, Taipei, Taiwan; Department of Psychiatry, National Taiwan University Hospital, Taipei, Taiwan.
Ying-Yeh Chen, Taipei City Psychiatric Centre, Taipei City Hospital, Taipei, Taiwan; Institute of Public Health and Department of Public Health, National Yang-Ming University, Taipei,Taiwan.
References
- 1.WHO. Suicide prevention (SUPRE). 2011. http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/ (accessed Feb 16, 2012).
- 2.Shah A The relationship between suicide rates and age: an analysis of multinational data from the World Health Organization. Int Psychogeriatr 2007; 19: 1141–52. [DOI] [PubMed] [Google Scholar]
- 3.Law CK, Yip PSF, Chen YY. The economic and potential years of life lost from suicide in Taiwan, 1997–2007. Crisis 2011; 32: 152–59. [DOI] [PubMed] [Google Scholar]
- 4.Hadlaczky G, Wasserman D, Hoven CW, Mandell DJ, Wasserman C. Suicide prevention strategies: case studies from across the globe In: O’Connor RC, Platt S, Gordon J, eds. International handbook of suicide prevention—research, policy and practice. Chichester, UK: Wiley-Blackwell, 2011: 475–86. [Google Scholar]
- 5.Chen YY, Wu KC, Yousuf S, Yip PSF. Suicide in Asia: opportunities and challenges. Epidemiol Rev 2012; 34: 129–44. [DOI] [PubMed] [Google Scholar]
- 6.Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing to prevent it? Am J Public Health 2004; 94: 37–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oquendo MA, Currier D, Mann JJ. Prospective studies of suicidal behavior in major depressive and bipolar disorders: what is the evidence for predictive risk factors? Acta Psychiatr Scand 2006; 114: 151–58. [DOI] [PubMed] [Google Scholar]
- 8.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA 2005; 294: 2064–74. [DOI] [PubMed] [Google Scholar]
- 9.Daigle MS. Suicide prevention through means restriction: assessing the risk of substitution. A critical review and synthesis. Accid Anal Prev 2005; 37: 625–32. [DOI] [PubMed] [Google Scholar]
- 10.Clarke R, Lester D. Suicide: closing the exits. New York, NY: Springer Verlag, 1989. [Google Scholar]
- 11.Spicer RS, Miller TR. Suicide acts in 8 states: incidence and case fatality rates by demographics and method. Am J Public Health 2000; 90: 1885–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elnour AA, Harrison J. Lethality of suicide methods. Inj Prev 2008; 14: 39–5. [DOI] [PubMed] [Google Scholar]
- 13.Chen VC, Cheng AT, Tan HK, et al. A community-based study of case fatality proportion among those who carry out suicide acts. Soc Psychiatry Psychiatr Epidemiol 2009; 44: 1005–11. [DOI] [PubMed] [Google Scholar]
- 14.Yip PSF, Caine ED, Kwok RC, Chen YY. A decompositional analysis of the relative contribution of age, sex and methods of suicide to the changing patterns of suicide in Taipei City, 2004–2006. Inj Prev 2011; published online Oct 25. DOI: 10.1136/injuryprev-2011-040177 [DOI] [PubMed] [Google Scholar]
- 15.Hawton K Restricting access to methods of suicide: rationale and evaluation of this approach to suicide prevention. Crisis 2007; 28 (suppl 1): 4–9. [DOI] [PubMed] [Google Scholar]
- 16.Johnson S The ghost map: the story of London’s most terrifying epidemic—and how it changed science, cities and the modern world. London: Riverhead Books, 2006. [Google Scholar]
- 17.Clarke RV. Introduction. In: Clarke RV, ed. Situational crime prevention: successful case studies. Monsey, NY: Criminal Justice Press, 1997: 1–43. [Google Scholar]
- 18.Chen YY, Wu KC-C, Yip PSF. Suicide prevention through restricting access to suicide means and hotspots In: O’Connor RC, Platt S, Gordon J, eds. International handbook of suicide prevention: research, policy and practice. Chichester: John Wiley & Sons, 2011: 545–60. [Google Scholar]
- 19.Ajdacic-Gross V, Weiss MG, Ring M, et al. Methods of suicide: international suicide patterns derived from the WHO mortality database. Bull World Health Organ 2008; 86: 726–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health 2007; 7: 357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen YY, Yip PSF. Prevention of suicide by jumping: experiences from Taipei City (Taiwan), Hong Kong and Singapore In: Wasserman D, Wasserman C, eds. Oxford textbook of suicidology and suicide prevention. Oxford: Oxford University Press, 2009: 569–72. [Google Scholar]
- 22.Chen YY, Gunnell D, Lu TH. Descriptive epidemiological study of sites of suicide jumps in Taipei, Taiwan. Inj Prev 2009; 15:41—44. [DOI] [PubMed] [Google Scholar]
- 23.Thomas K, Chang SS, Gunnell D. Suicide epidemics: the impact of newly emerging methods on overall suicide rates—a time trends study. BMC Public Health 2011; 11: 314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kreitman N The coal gas story: United Kingdom suicide rates, 1960–71. Br J Prev Soc Med 1976; 30: 86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amos T, Appleby L, Kiernan K. Changes in rates of suicide by car exhaust asphyxiation in England and Wales. Psychol Med 2001; 31: 935–39. [DOI] [PubMed] [Google Scholar]
- 26.Nordentoft M, Qin P, Helweg-Larsen K, Juel K. Restrictions in means for suicide: an effective tool in preventing suicide: the Danish experience. Suicide Life Threat Behav 2007; 37: 688–97. [DOI] [PubMed] [Google Scholar]
- 27.Studdert DM, Gurrin LC, Jatkar U, Pirkis J. Relationship between vehicle emissions laws and incidence of suicide by motor vehicle exhaust gas in Australia, 2001–06: an ecological analysis. PLoS Med 2010; 7: e1000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mott JA, Wolfe MI, Alverson CJ, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA 2002; 288: 988–95. [DOI] [PubMed] [Google Scholar]
- 29.Skilling GD, Sclare PD, Watt SJ, Fielding S. The effect of catalytic converter legislation on suicide rates in Grampian and Scotland 1980–2003. Scott Med J 2008; 53: 3–6. [DOI] [PubMed] [Google Scholar]
- 30.Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: a continuing tragedy in developing countries. Int J Epidemiol 2003; 32: 902–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gunnell D, Fernando R, Hewagama M, Priyangika WD, Konradsen F, Eddleston M. The impact of pesticide regulations on suicide in Sri Lanka. Int J Epidemiol 2007; 36: 1235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roberts DM, Karunarathna A, Buckley NA, Manuweera G, Sheriff MH, Eddleston M. Influence of pesticide regulation on acute poisoning deaths in Sri Lanka. Bull World Health Organ 2003; 81: 789–98. [PMC free article] [PubMed] [Google Scholar]
- 33.Vijayakumar L, Satheesh-Babu R. Does ‘no pesticide’ reduce suicides? Int J Soc Psychiatry 2009; 55: 401–06. [Google Scholar]
- 34.Konradsen F, Pieris R, Weerasinghe M, van der Hoek W, Eddleston M, Dawson AH. Community uptake of safe storage boxes to reduce self-poisoning from pesticides in rural Sri Lanka. BMC Public Health 2007; 7: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beautrais AL, Fergusson DM, Horwood LJ. Firearms legislation and reductions in firearm-related suicide deaths in New Zealand. Aust N Z J Psychiatry 2006; 40: 253–59. [DOI] [PubMed] [Google Scholar]
- 36.Bridges FS. Gun control law (Bill C-17), suicide, and homicide in Canada. Psychol Rep 2004; 94: 819–26. [DOI] [PubMed] [Google Scholar]
- 37.Caron J Gun control and suicide: possible impact of Canadian legislation to ensure safe storage of firearms. Arch Suicide Res 2004; 8: 361–74. [DOI] [PubMed] [Google Scholar]
- 38.Caron J, Julien M, Huang JH. Changes in suicide methods in Quebec between 1987 and 2000: the possible impact of bill C-17 requiring safe storage of firearms. Suicide Life Threat Behav 2008; 38: 195–208. [DOI] [PubMed] [Google Scholar]
- 39.Chapman S, Alpers P, Agho K, Jones M. Australia’s 1996 gun law reforms: faster falls in firearm deaths, firearm suicides, and a decade without mass shootings. Inj Prev 2006; 12: 365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cheung AH, Dewa CS. Current trends in youth suicide and firearms regulations. Can J Public Health 2005; 96: 131–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Conner KR, Zhong Y. State firearm laws and rates of suicide in men and women. Am J Prev Med 2003; 25: 320–24. [DOI] [PubMed] [Google Scholar]
- 42.De Leo D, Dwyer J, Firman D, Neulinger K. Trends in hanging and firearm suicide rates in Australia: substitution of method? Suicide Life Threat Behav 2003; 33: 151–64. [DOI] [PubMed] [Google Scholar]
- 43.Marinho de Souza F, Macinko J, Alencar AP, Malta DC, de Morais Neto OL. Reductions in firearm-related mortality and hospitalizations in Brazil after gun control. Health Aff 2007, 26: 575–84. [DOI] [PubMed] [Google Scholar]
- 44.Gagne M, Robitaille Y, Hamel D, St-Laurent D. Firearms regulation and declining rates of male suicide in Quebec. Inj Prev 2010; 16: 247–53. [DOI] [PubMed] [Google Scholar]
- 45.Kapusta ND, Etzersdorfer E, Krall C, Sonneck G. Firearm legislation reform in the European Union: impact on firearm availability, firearm suicide and homicide rates in Austria. Br J Psychiatry 2007; 191: 253–57 [DOI] [PubMed] [Google Scholar]
- 46.Klieve H, Barnes M, De Leo D. Controlling firearms use in Australia: has the 1996 gun law reform produced the decrease in rates of suicide with this method? Soc Psychiatry Psychiatr Epidemiol 2009; 44: 285–92. [DOI] [PubMed] [Google Scholar]
- 47.Lee WS, Suardi S. The Australian firearms buyback and its effect on gun deaths. Contemp Econ Policy 2010; 28: 65–79. [Google Scholar]
- 48.Lubin G, Werbeloff N, Halperin D, Shmushkevitch M, Weiser M, Knobler HY. Decrease in suicide rates after a change of policy reducing access to firearms in adolescents: a naturalistic epidemiological study. Suicide Life Threat Behav 2010; 40: 421–24. [DOI] [PubMed] [Google Scholar]
- 49.Ozanne-Smith J, Ashby K, Newstead S, Stathakis VZ, Clapperton A. Firearm related deaths: the impact of regulatory reform. Inj Prev 2004; 10: 280–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rodriguez Andres A, Hempstead K. Gun control and suicide: the impact of state firearm regulations in the United States, 1995–2004. Health Policy 2011; 101: 95–103. [DOI] [PubMed] [Google Scholar]
- 51.Rosengart M, Cummings P, Nathens A, Heagerty P, Maier R, Rivara F. An evaluation of state firearm regulations and homicide and suicide death rates. Inj Prev 2005; 11: 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Webster DW, Vernick JS, Zeoli AM, Manganello JA. Association between youth-focused firearm laws and youth suicides. JAMA 2004; 292: 594–601. [DOI] [PubMed] [Google Scholar]
- 53.Cantor CH, Baume PJ. Access to methods of suicide: what impact? Aust N Z J Psychiatry 1998; 32: 8–14. [DOI] [PubMed] [Google Scholar]
- 54.Wong PW, Liu PM, Chan WS, et al. An integrative suicide prevention program for visitor charcoal burning suicide and suicide pact. Suicide Life Threat Behav 2009; 39: 82–90. [DOI] [PubMed] [Google Scholar]
- 55.Yip PSF, Law CK, Fu KW, Law YW, Wong PW, Xu Y. Restricting the means of suicide by charcoal burning. Br J Psychiatry 2010, 196: 241–2. [DOI] [PubMed] [Google Scholar]
- 56.Chen YY, Liao SF, Ten PR, et al. The impact of of media reporting of the suicide of a singer on suicide rates in Taiwan . Soc Psychiatry Psychiatr Epidemiol 2012; 47: 215–21. [DOI] [PubMed] [Google Scholar]
- 57.Chen YY, Chen F, Yip PSF. The impact of media reporting of suicide on actual suicides in Taiwan, 2002–2005. J Epidemiol Community Health 2010; 65: 934–0. [DOI] [PubMed] [Google Scholar]
- 58.Chan KP, Yip PS, Au J, Lee DT. Charcoal-burning suicide in post-transition Hong Kong. Br J Psychiatry 2005; 186: 67–73. [DOI] [PubMed] [Google Scholar]
- 59.Tsai CW, Gunnell D, Chou YH, Kuo CJ, Lee MB, Chen YY. Why do people choose charcoal burning as a method of suicide? An interview based study of survivors in Taiwan. J Affect Disord 2011; 131: 402–07 [DOI] [PubMed] [Google Scholar]
- 60.The Age Company. UK records first online suicide pact. Sept 30, 2005. http://www.theage.com.au/news/world/uk-records-first-online-suicide-pact/2005/09/30/Í127804638937html (accessed Feb 16, 2012). [Google Scholar]
- 61.Pirkis J, Nordentoft M. Media influences on suicide and attempted suicide In: O’Connor RC, Platt S, Gordon J, eds. International handbook of suicide prevention: research, policy and practice. Chichester: John Wiley & Sons, 2011: 531–44. [Google Scholar]
- 62.Niederkrotenthaler T, Voracek M, Herberth A, et al. Role of media reports in completed and prevented suicide: Werther v Papageno effects. Br J Psychiatry 2010; 197: 234–43. [DOI] [PubMed] [Google Scholar]
- 63.Hawton K, Townsend E, Deeks J, et al. Effects of legislation restricting pack sizes of paracetamol and salicylate on self poisoning in the United Kingdom: before and after study. BMJ 2001; 322: 1203–07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hawton K, Simkin S, Deeks J, et al. UK legislation on analgesic packs: before and after study of long term effect on poisonings. BMJ 2004; 329: 1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bateman DN. Limiting paracetamol pack size: has it worked in the UK? Clin Toxicol 2009; 47: 536–41. [DOI] [PubMed] [Google Scholar]
- 66.Beautrais AL. Effectiveness of barriers at suicide jumping sites: a case study. Aust N Z J Psychiatry 2001; 35: 557–62. [DOI] [PubMed] [Google Scholar]
- 67.Beautrais AL, Gibb SJ, Fergusson DM, Horwood LJ, Larkin GL. Removing bridge barriers stimulates suicides: an unfortunate natural experiment. Aust N Z J Psychiatry 2009; 43: 495–97 [DOI] [PubMed] [Google Scholar]
- 68.Bennewith O, Nowers M, Gunnell D. Effect of barriers on the Clifton suspension bridge, England, on local patterns of suicide: implications for prevention. Br J Psychiatry 2007; 190: 266–67. [DOI] [PubMed] [Google Scholar]
- 69.Law CK, Yip PSF, Chan WS, Fu KW, Wong PW, Law YW. Evaluating the effectiveness of barrier installation for preventing railway suicides in Hong Kong. J Affect Disord 2009; 114: 254–62. [DOI] [PubMed] [Google Scholar]
- 70.Pelletier AR. Preventing suicide by jumping: the effect of a bridge safety fence. Inj Prev 2007; 13: 57–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Reisch T, Michel K. Securing a suicide hot spot: effects of a safety net at the Bern Muenster Terrace. Suicide Life Threat Behav 2005; 35: 460–67 [DOI] [PubMed] [Google Scholar]
- 72.Sinyor M, Levitt AJ. Effect of a barrier at Bloor Street Viaduct on suicide rates in Toronto: natural experiment. BMJ 2010; 341: c2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Skegg K, Herbison P. Effect of restricting access to a suicide jumping site. Aust N Z J Psychiatry 2009; 43: 498–502. [DOI] [PubMed] [Google Scholar]
- 74.Glasgow G Do local landmark bridges increase the suicide rate? An alternative test of the likely effect of means restriction at suicide-jumping sites. Soc Sci Med 2011; 72: 884–89. [DOI] [PubMed] [Google Scholar]
- 75.Gunnell D, Miller M. Strategies to prevent suicide. BMJ 2010, 341: c3054. [DOI] [PubMed] [Google Scholar]
- 76.de Silva VA, Senanayake S, Dias P, Hanwella R. From pesticides to medicinal drugs: time series analyses of methods of self-harm in Sri Lanka. Bull World Health Organ 2012; 90: 40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


