Abstract
Objective:
Cannabis is reported to be the most common illicit substance used among medical students; however, the number of related studies is limited and their results are not systematically reviewed. The aim of our study was to analyze the prevalence of lifetime and current use of cannabis among medical students worldwide.
Methods:
A systematic review and meta-analysis was performed with adherence to the PRISMA guidelines. The electronic databases PubMed, Scopus, and Cochrane library were searched for studies on the prevalence of cannabis use among medical students. Prevalence of lifetime, past-year, and past-month cannabis use was extracted. Pooled prevalence and relative risk for sex were calculated using the random effects model and subgroup analyses were conducted.
Results:
A total of 38 observational (cross-sectional and cohort) studies were included (total number of participants 19 932), and most of them were conducted in Europe, Central and Southern America, and the United States. Overall pooled prevalence of lifetime cannabis use was 31.4% (95% confidence interval [CI]: 23.7%-39.6%), past-year use was 17.2% (95% CI: 10.8%-24.6%), and past-month use was 8.8% (95% CI: 5.6%-12.5%). Men displayed higher rates of cannabis use with a pooled relative risk of 1.55 (95% CI: 1.32-1.81). Heterogeneity was high (I2 > 75%) and there were differences among continents in all outcomes (P < .001).
Conclusions:
In conclusion, 1 in 3 medical students has used cannabis, whereas 8.8% were current users. Significant differences among continents were observed, but common finding was that male students tend to consume cannabis more often than female students.
Keywords: Cannabis, medical students, prevalence
Introduction
Cannabis, both resin (hashish) and herbal (marijuana), is the illicit drug most likely to be used across all age groups.1,2 Medical students are not the exception; cannabis is reported to be the most common illicit substance used, with a reported past-month use of 11.84%.3 Exposure to diverse stressors, burnout, and relatively easy access to drugs set physicians and medical students vulnerable to substance use.4 Substance use may affect students’ current academic performance and also it may contribute to misjudgments and misperceptions of future physicians toward patients with substance use disorders.5 It is reported that students’ attitudes toward substance use behaviors influence their future preventive counseling practices.6 Consequently, the study of lifetime and, especially, current cannabis use among medical students is of great importance.
Interestingly, although cannabis use and its consequences among adults is extensively studied worldwide and detailed analyses are published annually by the responsible offices of the United Nations (UN)1 and the European Union,2 there is a lack of recent studies on cannabis use among medical students. To our knowledge, there is only one published systematic review that examined both legal and illegal substance use by medical students worldwide, where information regarding cannabis use could partly be retrieved.3 Thus, the aim of our article was to systematically review and meta-analyze the literature on the epidemiology of cannabis use among medical students and to present the prevalence of lifetime, past-year, and past-month use by geographical area.
Methods
Search strategy
A systematic review was performed with adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.7 The electronic databases PubMed, Scopus, and Cochrane library were searched from inception through October 31, 2017. The search strategy for PubMed included different combinations of Medical Subject Headings (MeSH) search terms and non-MeSH terms, integrating into the query: (“students, medical” [MeSH Terms] OR (“students” [All Fields] AND “medical” [All Fields]) OR “medical students” [All Fields] OR (“medical” [All Fields] AND “students” [All Fields]) AND (“cannabis” [MeSH Terms] OR “cannabis” [All Fields] OR “hashish” [All Fields] OR “marijuana” [All Fields] OR “illegal drugs” [All Fields] OR “illegal substances” [All Fields] OR “Psychoactive Substances” [All Fields] OR “Psychoactive Drugs” [All Fields]). All of the identified articles were then limited to English language articles to clearly evaluate the results and the methodology of the study, and only full-text articles were included (“Text Availability” filter: Full Text, “Language” filter: English). Similar search strategies were used for the Scopus and Cochrane Library database and duplicates were excluded.
Study selection
The inclusion criteria were as follows: (1) studies that presented the precise number of cannabis prevalence, distinguished from other substances use, to analyze data regarding only the use of cannabis; (2) studies that presented specific data of cannabis use only by medical students and not mixed together with other students’ groups or graduates from medical school (junior doctors, master students, etc); (3) the number of participants who turned in fully completed and acceptable questionnaires had to be written alongside with the initial number of invited participants; and (4) full-text English language articles.
Two investigators (I.K. and I.T.) independently screened all the titles and abstracts, and discrepancies were solved by discussion with a third author (S.S.). The reference lists of relevant articles were also hand-searched. Records that considered as potentially relevant were retrieved in full text and preceded to evaluation. Articles published as editorials, letters, conferences, or meeting abstracts were excluded. The remaining articles were eligible for abstract review.
Data extraction
From each study, data regarding the total number of participants, their year of studies, mean age, prevalence of cannabis use (lifetime, past-year, past-month) alongside with differences among the 2 sexes were extracted. For studies with a cohort of students, followed throughout their medical studies, only percentages from the last, in chronological order, survey were included, to evaluate their most recent use.
Assessment of quality
The quality of the selected articles was assessed using the Grading of Recommendations Assessment, Development and Evaluation system.8 The grading scheme classifies quality of evidence as high (A), moderate (B), or low (C)
Data synthesis
The narrative description was accompanied by the pooled prevalence (lifetime, past year, and past month) of cannabis use and the pooled relative risk for sex, worldwide and stratified by continent. The 95% confidence intervals (CIs) of prevalence estimates were calculated using the Wilson methods.9 Prevalence data were transformed using the Freeman-Tukey double arcsine transformation, to stabilize the variance and avoid overestimation of prevalence extremities.10 The relative risk and the accompanied 95% CIs were calculated to estimate the risk of sex for cannabis use. The random effects model was used to incorporate heterogeneity. The DerSimonian-Laird estimator for tau-squared was used, as well as the inverse variance method was used to calculate the pooled prevalence and the Mantel-Haenszel method to calculate the pooled relative risk. Heterogeneity was assessed with I2, considering as high heterogeneity when I2 was equal to or greater than 75%. Subgroup analyses were conducted for continents, publication year, and sample size for overall studies and stratified by continent. Subgroup differences were assessed by the χ2-statistic. Significance was predefined at α level .05 and for subgroup analyses at .01 to reduce false-positive results due to multiple hypotheses testing. The statistical analysis was performed using the package meta version 4.9-011 on R version 3.3.2.12
Results
Study characteristics
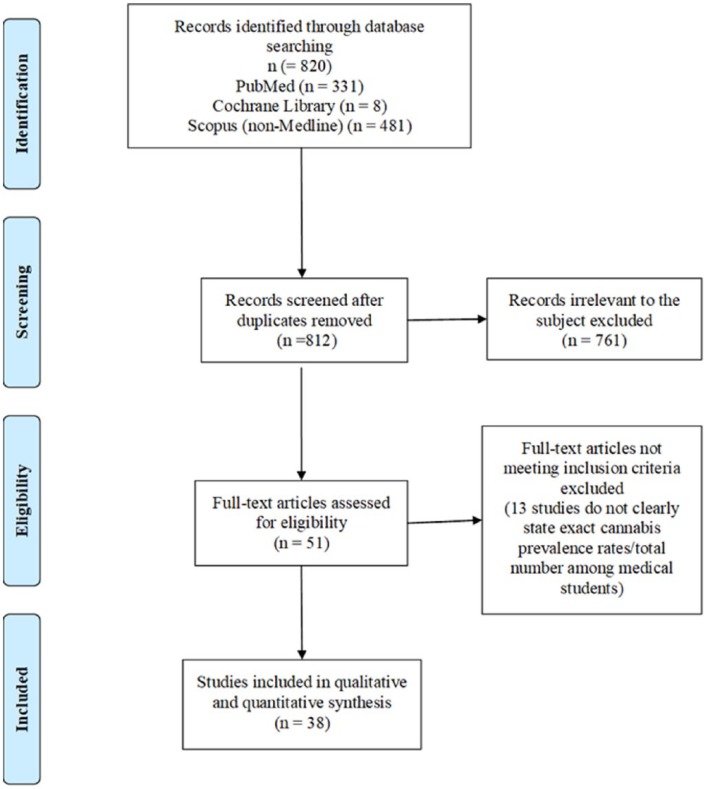
The initial total number of studies after implementing the aforementioned filters was 331 from PubMed, 481 from Scopus, and 8 from the Cochrane Database. The screening of the titles and abstracts identified 51 potentially relevant articles that were retrieved in full-text format. A total of 13 full-text articles were excluded because they did not meet the inclusion criteria. Thus, after complete review, 38 studies were included in the systematic review (Figure 1). From them, 11 referring to Europe: 6 the United Kingdom,13–18 2 Spain,19,20 1 Croatia,21 1 France,22 and 1 Serbia23; 13 to the United States24–36; 8 to the Central and Southern America: 7 Brazil37–43 and 1 Honduras44; 4 to Asia: 2 India,45,46 1 Iran,47 and 1 Nepal48; as well as 2 to Africa, Nigeria49,50 (Table 1). No study was identified for Oceania.
Figure 1.
PRISMA flowchart.
Table 1.
Studies of cannabis use among medical students worldwide.
| Study | Country | Participants Gender: M/F |
Study year | Age | Gender of users (M/F) | Lifetime use, % | Past-year use, % | Past-month use, % | Quality (grade) |
|---|---|---|---|---|---|---|---|---|---|
| Αfrica | |||||||||
| Ihezue49 | Nigeria | 728 M/F: 607/121 |
2nd-6th | 22.6 ± 2.36 | M/F: 22/1 | ns | ns | 3.1%, n = 23 | C |
| James et al. 201350 | Nigeria | 200 M/F: 109/91 |
5th | 24.1 ± 2.45 | ns | 10.5%, n = 21 | ns | 5%, n = 10 | C |
| Asia | |||||||||
| Ali and Vankar45 | India | 215 ns |
1st, 2nd, 6th | 19.7 | M/F: 2/0 | 0.93%, n = 2 | ns | 0 | C |
| Jodati et al47 | Iran | 173 M/F: 173/0 |
ns | 21.3 | ns | ns | 5.7%, n = 10 | ns | C |
| Rai et al46 | India | 2135 M/F: 1512/623 |
1st-6th | 20.5 | M/F: 129/12 | 6.0%, n = 141 | ns | 1.4%, n = 32 | C |
| Budhathoki et al48 | Nepal | 510 M/F: 324/186 |
3rd | 22.5 | M/F: 62/5 | 13.1%, n = 67 | ns | ns | C |
| Central and Southern America | |||||||||
| Lambert Passos et al37 | Brazil | 1054 M/F: 499/553 |
1st-6th | 21.1 ± 3.9 | M/F: 124/94 | 20.9%, n = 218 | ns | 5.5%, n = 59 | C |
| Di Pietro et al38 | Brazil | 456 M/F: 247/209 |
1st-6th | 21.12 ± 2.4 | ns | ns | ns | 15%, n = 68 | C |
| Boniatti et al40 | Brazil | 183 M/F: 84/99 |
1st-6th | 22.5 ± 2.4 | M/F: 31/26 | 31.1%, n = 57 | 13.6%, n = 25 | 7.6%, n = 14 | C |
| Buchanan and Pillon44 | Honduras | 260 M/F: 115/145 |
4th-5th | 22.5 | ns | ns | 3.8%, n = 10 | 1.9%, n = 5 | C |
| Carvalho et al41 | Brazil | 465 M/F: 265/200 |
1st-6th | 21.5 | ns | 14.4%, n = 67 | 4.5%, n = 21 | ns | C |
| Da Silveira et al39 | Brazil | 456 M/F: 247/209 |
1st-6th | 21 | M/F: 63/12 | ns | 16.4%, n = 75 | ns | C |
| De Oliveira et al42 | Brazil | 209 M/F: 111/98 |
6th | 22 | M/F: 34/17 | 24.3%, n = 51 | 14.3%, n = 30 | 10.5%, n = 22 | C |
| Petroianu et al43 | Brazil | 332 M/F: 160/172 |
1st-6th | 23 | M/F: 37/16 | ns | 16%, n = 53 | ns | C |
| Europe | |||||||||
| McKay et al13 | United Kingdom | 749 ns |
1st-4th | 20 | M/F: 80/20 | 13.4%, n = 100 | ns | 3.6%, n = 27 | C |
| Laporte et al19 | Spain | 808 M/F: 515/293 |
1st-6th | ns | M/F: 45/19 | 7.9%, n = 64 | ns | 3.8%, n = 31 | C |
| Rodriguez et al. 198620 | Spain | 2308 M/F: 1112/1196 |
ns | ns | M/F: 285/193 | 20.7%, n = 478 | ns | ns | C |
| Ashton and Kamali14 | United Kingdom | 186 M/F: 76/109 | ns | 20.4 ± 1.8 | M/F: 26/30 | 30.3%, n = 56 | ns | ns | C |
| Webb et al15 | United Kingdom | 750 M/F: 333/417 |
2nd | ns | M/F: 180/165 | 46%, n = 345 | ns | 10%, n = 75 | C |
| Newbury-Birch et al16 | United Kingdom | 194 M/F: 64/130 |
1st | 18.8 ± 2.1 | M/F:32/54 | 44.3%, n = 86 | ns | 19%, n = 37 | C |
| Pickard et al17 | United Kingdom | 136 M/F: 46/90 |
2nd | ns | M/F: 11/30 | 30.1%, n = 41 | ns | ns | C |
| Newbury-Birch et al18 | United Kingdom | 110 M/F: 33/77 |
6th | ns | M/F: 22/50 | 65.5%, n = 72 | ns | 23.6%, n = 26 | C |
| Trkulja et al21 | Croatia | 775 M/F: 290/485 |
1st-6th | 18-24 | M/F: 129/144 | 61.5%, n = 273 | ns | ns | C |
| Gignon et al22 | France | 171 ns |
2nd-6th | 22.1 ± 1.7 | ns | ns | 77%, n = 131 | 33%, n = 56 | C |
| Vujcic et al23 | Serbia | 418 M/F: 156/262 |
4th | 22.46 ± 1.12 | M/F: 63/83 | 34.9%, n = 146 | ns | ns | C |
| USA | |||||||||
| Solursh et al24 | USA | 234 ns |
3rd-Final | ns | ns | 20.5%, n = 48 | 16.6%, n = 39 | 11.9%, n = 28 | C |
| Lipp et al25 | USA | 1063 ns |
ns | ns | ns | 52%, n = 550 | ns | 30.9%, n = 328 | C |
| Rochford et al26 | USA | 134 ns |
1st | 22 | ns | 72%, n = 96 | ns | ns | C |
| Kory and Crandall27 | USA | 463 M/F: 421/42 |
1st-Final | 23.6 | ns | 70%, n = 302 | ns | 27.4%, n = 127 | C |
| McAuliffe et al28 | USA | 381 M/F: 225/156 |
1st-Final | 25 | ns | 18.9%, n = 72 | 5.77%, n = 22 | 3.1%, n = 12 | C |
| Conard et al29 | USA | 589 M/F: 383/206 |
4th | 27.6 | ns | 74%, n = 436 | 31.9%, n = 188 | 16.9%, n = 100 | C |
| Schwartz et al. 199030 | USA | 263 M/F: 170/93 |
2nd-3rd | ns | ns | 48.3%, n = 127 | 19%, n = 50 | 5.3%, n = 14 | C |
| Croen et al31 | USA | 139 M/F: 79/60 |
3rd | <22 | ns | ns | 21.6%, n = 30 | ns | C |
| Choi et al32 | USA | 301 M/F: 109/192 |
1st-Final | ns | ns | ns | ns | 1.3%, n = 4 | C |
| Zhou et al33 | USA | 431 M/F: 217/214 |
1st-Final | 25 | ns | 31.5%, n = 136 | 12.2%, n = 53 | 9%, n = 39 | C |
| Chan et al34 | USA | 236 M/F: 119/115 |
1st-Final | 25-29 | ns | 33.3%, n = 127 | ns | ns | C |
| Merlo et al35 | USA | 862 M/F: 369/491 |
1st-Final | ns | M/F: 190/224 | 46.8%, n = 414 | ns | 4.1%, n = 36 | C |
| Ayala et al36 | USA | 855 M/F: 304/534 |
1st-Final | 25.6 ± 3.30 | ns | ns | 26.2%, n = 224 | 11.7% n = 100 | C |
When available, age is displayed with average and its standard deviation. M, male; F, female; ns, data not stated).
The demographics of the selected studies, individual study quality, as well as the prevalence of cannabis use among medical students are listed in Table 1. The median publication year was 2004 (ranging from 1971 to 2017) and the median sample size was 400 (ranging from 110 to 2308). The total number of participants in the studies included in our review was 19 932. Specifically, the studies included 6605 participants from Europe, 5951 from the United States, 3415 from Central and Southern America (92% came from Brazil), 3033 from Asia, and 928 participants from Africa (all of them from Nigeria). Because of the observational nature of the investigations, there were no studies that received a grade higher than C (Table 1).
Prevalence of cannabis use
Lifetime cannabis use
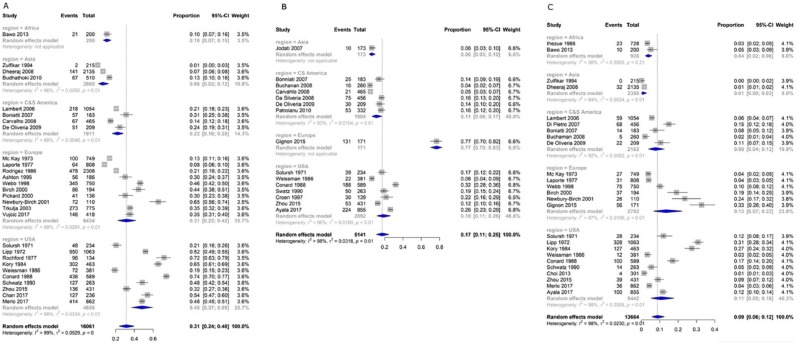
The pooled prevalence of lifetime cannabis use among medical students worldwide was 31.4% (number of studies k = 28, number of participants N = 16 061, prevalence = 31.4% [95% CI: 23.7%-39.6%], I2 = 99.2%; Figure 2A). There were differences among continents (, P < .001), with the lowest prevalence in Asia (k = 3, N = 2860, 6% [1.77%-12.44%]) and the highest in the United States (k = 10, N = 4656, 48.05% [36.72%-59.48%]). Publication year and sample size did not moderate lifetime prevalence of cannabis use, except for studies from Asia. Studies from Asia published after 2000 and having sample size larger than 400 reported higher prevalence (k = 2, N = 2645, 9.52% [4.09%-16.87%] versus an earlier and smaller study; k = 1, N = 215, 0.93% [0.01%-2.78%]; , P = .0015; see subgroup analyses in eAppendix 1).
Figure 2.
Forest plot of (A) lifetime, (B) past-year, and (C) past-month cannabis use among medical students, stratified by continent. “Events” refer to the number of cannabis users, and “Total” refers to the sample size of each study. Black squares represent the point estimate of prevalence of each study. The area of the square is proportional to the percent weight of the study, which contributes to the pooled prevalence (calculated using the inverse variance method). Horizontal lines show 95% confidence intervals. The diamond shows the pooled results and its width the 95% confidence interval. Between-study heterogeneity is represented by I2. The vertical dashed line indicates the overall pooled prevalence.
Past-year cannabis use
Pooled prevalence of past-year cannabis use around the world was estimated to be 17.2% (k = 15, N = 5141, 17.2% [10.8%-24.6%], I2 = 97.7%; Figure 2B). Again, there were subgroup differences regarding the continent (, P < .001). There was no study reporting past-year use in Africa and only 1 study in Europe; this single European study reported surprisingly a very high past-year prevalence of 76.6%. Excluding this study from Europe,22 the overall pooled prevalence was 13.9% (95% CI: 9.4%-19.2%, I2 = 96%). Regarding the other continents, prevalence ranged between 5.8% in Asia (k = 1, N = 173, 5.8% [2.72%-9.82%])47 and 18.3% in the United States (k = 7, N = 2892, 18.3% [11.48%-26.32%], I2 = 96.2%). Subgroup analyses suggested that publication year and sample sizes did not moderate prevalence of past-year cannabis use (see subgroup analyses in eAppendix 2).
Past-month cannabis use
A total of 25 studies reported past-month use of cannabis, with an estimated prevalence of 8.8% (k = 25, N = 13 664, 8.8% [5.6%-12.5%], I2 = 98.1%) worldwide (Figure 2C). Differences among continents were noticed (, P < .001), ranging from 0.6% in Asia (k = 2, N = 2350, 0.6% [0%-2.8%], I2 = 84.1%) to 10.6% in the United States (k = 10, N = 5442, 10.6% [5.13%-17.74%], I2 = 98.3%) and 13.4% in Europe (k = 6, N = 2782, 13.4% [6.54%-22.17%], I2 = 97.1%). Again, leaving out the recent study in France, which reported high past-month and past-year prevalence,22 the remaining overall pooled prevalence was similar, 8.1% (95% CI: 5.1%-11.7%) and 10.3% (95% CI: 5.1%-17.1%) in Europe. Subgroup analyses did not suggest any moderating effect except for Europe. Studies from Europe published after 2000 reported higher prevalence (k = 2, N = 281, 28.46% [20.04%-37.69%] versus earlier studies; k = 4, N = 2501, 7.98% [3.56%-13.91%]; , P < .001), as well as studies with sample size smaller than 400 participants (k = 3, N = 475, 24.94% [17.02%-33.8%] versus larger studies; k = 3, N = 2307, 5.5% [2.34%-9.87%]; , P < .001; see subgroup analyses in eAppendix 3).
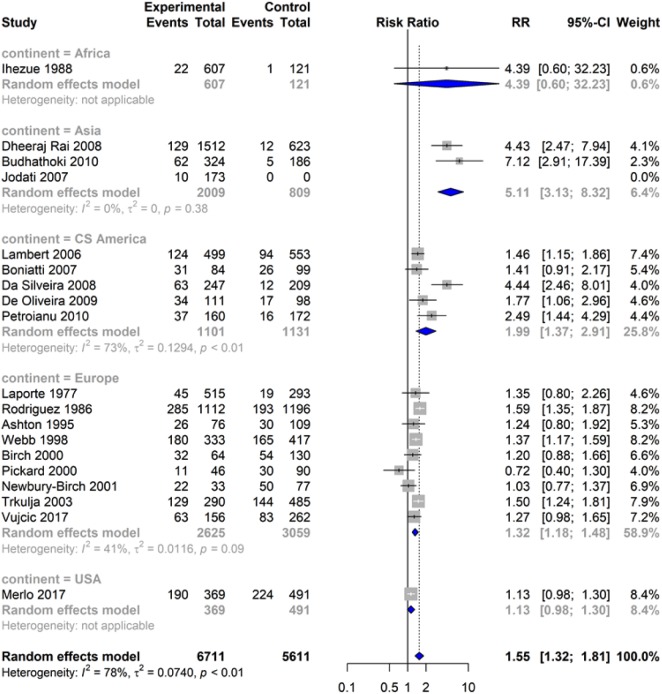
Pooled relative risk for sex
Male medical students in comparison with female seem to be in higher risk for cannabis use, with an overall pooled relative risk of 1.55 (k = 15, N = 12 149, 1.55 [1.32-1.81], I2 = 78.2%; Figure 3). There were differences among continents (, P < .001), with higher risk for men demonstrated in Asia (k = 2, N = 2818, risk ratio [RR] = 5.11 [3.13-8.32], I2 = 0%) and Central and Southern America (k = 5, N = 2232, RR = 1.99 [1.37-2.91], I2 = 72.9%). Only 1 study in the United States reported cannabis use stratified by sex but no association was identified (k = 1, N = 860, RR = 1.13 [0.98-1.30]).35 Regarding Europe, men were in higher risk with a relative risk of 1.32 (k = 9, N = 5684, RR = 1.32 [1.18-1.48], I2 = 41.5%). Subgroup analyses suggested that publication year and sample sizes did not moderate the relative risk, except for Europe. Studies from Europe with sample size larger than 400 participants seem to have higher relative risk (k = 5, N = 5059, RR = 1.45 [1.32-1.58], I2 = 0.0 versus smaller studies; k = 4, N = 625, RR = 1.08 [0.90-1.30], I2 = 0.0; , P = .0053; see subgroup analyses in eAppendix 4).
Figure 3.
Forest plot of pooled relative risk for sex of medical students for cannabis use by continent. Male medical students are referred as the experimental group and female students as the control group. The “Events” refer to the number of cannabis users, and “Total” refers the total number of males or females of the study. Black squares represent the relative risk of each study. The area of the square is proportional to weight of the study, which contributes to the pooled relative risk (calculated using the Mantel-Haenszel method). Horizontal lines show 95% confidence intervals. The diamond shows the pooled results and its width the 95% confidence interval. Between-study heterogeneity is represented by I2. The vertical dashed line indicates the overall pooled relative risk.
Discussion
This is a first attempt to systematically review the published literature to examine lifetime and recent cannabis use among medical students’ population. It is impressive that although cannabis use and its consequences for the adult population is extensively studied worldwide and detailed analyses are published annually by the responsible offices of the UN1 and the European Union,2 recent studies on the prevalence of cannabis use among medical students are lacking: only 8 studies were published worldwide within the past 5 years, whereas most of the studies (k = 14) are more than 20 years old. This might explain some discrepancies found in our results compared with published data of the general population for some areas.
Concerning Europe, our results suggest that the lifetime prevalence among medical students was 31.4% and the past month was 13.4%, whereas the past-year use could not be estimated as only 1 study with a small sample size reported related information.22 Unfortunately, official data for the young adult population in Europe (aged 15-24) presented by the European Drug Report 2017 concern only past year use, which was 17.7% for 2017, with men outnumbering women by a factor of 2.2 To the same report, cannabis is the illicit drug most likely to be used among European adults (aged 15-64) with a lifetime prevalence of 26.3%, whereas around 1% of European adults estimated to be daily or near-daily cannabis users. However, levels of use differ considerably between European countries ranging from the lowest 3.3% to the highest 22% concerning national estimates of past-year use.2
Of interest was our finding that the lifetime prevalence among US medical students was 48.1%, meaning that 1 in 2 medical students in the United States has experienced, even once, in lifetime the use of cannabis. This percentage on lifetime prevalence is hard to compare because the nationwide studies provide data only for past-year and past-month use. However, according to the UN Office on Drugs and Crime, cannabis use has been rising over the past decade in the Americas, most pronounced in the United States, with an overall increase of 43% in the number of past-year cannabis users and of 54% in the number of past-month users. Regarding Asia and Africa, the UN analysis noticed that cannabis use among the general adult population in Africa and in Asia is perceived to have continued to increase relatively rapidly in the past 5 years.1 However, precise data are missing not only for the medical students but also for the general population due to the lack of systematic research.
To our results, male students tend to consume cannabis almost 2-fold more often than female students because pooled relative risk worldwide was 1.55 and higher risk for men was demonstrated in Asia, Central and Southern America, as well as Europe. This is in accordance with the findings of a previously published narrative review where a male:female usage ratio of 2:1 among medical students was reported.3 It is known that use of all drugs is generally higher among men and the recent European report found that among 88 million adult users in Europe, use of cannabis was more frequently reported by men (53.8 million) than women (34.1 million). Furthermore, an estimated 18.7 million young adults (aged 15-34) used drugs in the past year, with twice as many men as women.2
The major strength of this review was the number of studies included (k = 38) and the total number of participants (N = 19 932). However, there were some limitations. Many of the included studies had sample sizes smaller than 400 and they were published before 2000, which may have had an impact on the exact prevalence of cannabis use. As in previous meta-analyses of prevalence of cannabis use among other population groups,51,52 considerable heterogeneity between studies was detected. A meta-analysis of prevalence of cannabis use in Iranian students had considerable heterogeneity (I2 > 94%), despite the inclusion of studies with a more homogeneous population.52 Another meta-analysis on prevalence of cannabis use in patients with first episode psychosis found also considerable heterogeneity between studies (I2 = 92.1%).51 It is suggested that prevalence of cannabis use could vary considerably at local level, even within geographical regions, reflecting diverge and changing patterns of cannabis cost and availability, as well as of attitudes toward cannabis use and awareness of the potential harms of cannabis use.51 Methodologic differences among studies (such as different sampling of participants or questionnaires used) are also suggested as possible sources of heterogeneity.52 As a result, the pooled worldwide and within-continents results of our study should be interpreted with some caution. In addition, subgroup analyses had small statistical power and for some outcomes, they could not be conducted due to paucity of available data.
In conclusion, our results suggest a worldwide pooled lifetime prevalence of 31.4%, meaning that about 1 in 3 medical students has used cannabis one or more times during their life, whereas 8.8% of the students reported current use. However, significant differences were observed among continents, whereas Africa and Asia were underrepresented. Considering the future role of medical students toward patients’ substance abuse behaviors, these numbers are not negligible. Further international studies among medical students are needed to strengthen the research on the epidemiology of cannabis use and to study their motivations and attitudes toward this risky behavior.
Supplemental Material
Supplemental material, rev_supplementary_xyz9610434e3d4a for Prevalence of Cannabis Use Among Medical Students: A Systematic Review and Meta-analysis by Georgios Papazisis, Spyridon Siafis, Ioannis Tsakiridis, Ioannis Koulas, Themistoklis Dagklis and Dimitrios Kouvelas in Substance Abuse: Research and Treatment
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: GP: Study concept, design and supervision, critical revision of the manuscript. SS: Drafting of the manuscript, statistical analysis, interpretation of data. IT: Drafting of the manuscript, data and statistical analysis. IK: Study design,acquisition and analysis of data. TD: Drafting of the manuscript, data interpretation. DK: Critical revision of the manuscript, study supervision.
ORCID iDs: Georgios Papazisis  https://orcid.org/0000-0003-1641-9095
https://orcid.org/0000-0003-1641-9095
Ioannis Tsakiridis  https://orcid.org/0000-0003-4337-7871
https://orcid.org/0000-0003-4337-7871
References
- 1. United Nations Office on Drugs Crime. World Drug Report 2017. Herndon, VA: United Nations Publications; 2017. [Google Scholar]
- 2. EMCDDA. European Drug Report 2017: Trends and Developments. Lisbon, Portugal: European Monitoring Centre for Drugs and Drug Addiction (EMCDDA); 2017. [Google Scholar]
- 3. Roncero C, Egido A, Rodriguez-Cintas L, Perez-Pazos J, Collazos F, Casas M. Substance use among medical students: a literature review 1988-2013. Actas Esp Psiquiatr. 2015;43:109–121. [PubMed] [Google Scholar]
- 4. Dumitrascu CI, Mannes PZ, Gamble LJ, Selzer JA. Substance use among physicians and medical students. Med Student Res J. 2014;3:26–35. [Google Scholar]
- 5. Boland M, Fitzpatrick P, Scallan E, et al. Trends in medical student use of tobacco, alcohol and drugs in an Irish university, 1973-2002. Drug Alcohol Depend. 2006;85:123–128. [DOI] [PubMed] [Google Scholar]
- 6. Roncero C, Rodriguez-Cintas L, Egido A, et al. The influence of medical student gender and drug use on the detection of addiction in patients. J Addict Dis. 2014;33:277–288. [DOI] [PubMed] [Google Scholar]
- 7. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Statist Med. 1998;17:857–872. [DOI] [PubMed] [Google Scholar]
- 10. Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T.Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67:974–978. [DOI] [PubMed] [Google Scholar]
- 11. Schwarzer G. meta: an R package for meta-analysis. R News. 2007;7:40–45. [Google Scholar]
- 12. R: A Language and Environment for Statistical Computing [computer program], Version 3.5, 2017. [Google Scholar]
- 13. McKay AJ, Hawthorne VM, McCartney HN. Drug taking among medical students at Glasgow university. Br Med J. 1973;1:540–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ashton CH, Kamali F. Personality, lifestyles, alcohol and drug consumption in a sample of British medical students. Med Educ. 1995;29:187–192. [DOI] [PubMed] [Google Scholar]
- 15. Webb E, Ashton CH, Kelly P, Kamah F. An update on British medical students’ lifestyles. Med Educ. 1998;32:325–331. [DOI] [PubMed] [Google Scholar]
- 16. Newbury-Birch D, White M, Kamali F. Factors influencing alcohol and illicit drug use amongst medical students. Drug Alcohol Depend. 2000;59:125–130. [DOI] [PubMed] [Google Scholar]
- 17. Pickard M, Bates L, Dorian M, Greig H, Saint D. Alcohol and drug use in second-year medical students at the University of Leeds. Med Educ. 2000;34:148–150. [DOI] [PubMed] [Google Scholar]
- 18. Newbury-Birch D, Walshaw D, Kamali F. Drink and drugs: from medical students to doctors. Drug Alcohol Depend. 2001;64:265–270. [DOI] [PubMed] [Google Scholar]
- 19. Laporte JR, Cami J, Gutierrez R, Laporte J. Caffeine, tobacco, alcohol and drug consumption among medical students in Barcelona. Eur J Clin Pharmacol. 1977;11:449–453. [DOI] [PubMed] [Google Scholar]
- 20. Rodriguez ME, Cami J. Substance use among medical students in Barcelona (Spain). A comparison with previous surveys. Drug alcohol Depend. 1986;18(3):311–318. [DOI] [PubMed] [Google Scholar]
- 21. Trkulja V, Zivcec Z, Cuk M, Lackovic Z. Use of psychoactive substances among Zagreb University medical students: follow-up study. Croatian Med J. 2003;44:50–58. [PubMed] [Google Scholar]
- 22. Gignon M, Havet E, Ammirati C, et al. Alcohol, cigarette, and illegal substance consumption among medical students: a cross-sectional survey. Workplace Health Saf. 2015;63:54–63. [DOI] [PubMed] [Google Scholar]
- 23. Vujcic I, Pavlovic A, Dubljanin E, Maksimovic J, Nikolic A, Sipetic-Grujicic S. Attitudes toward medical cannabis legalization among Serbian medical students. Subst Use Misuse. 2017;52:1225–1231. [DOI] [PubMed] [Google Scholar]
- 24. Solursh LP, Weinstock SJ, Saunders CS, Ungerleider JT. Attitudes of medical students toward cannabis. JAMA. 1971;217:1371–1372. [PubMed] [Google Scholar]
- 25. Lipp M, Tinklenberg J, Benson S, Melges F, Taintor Z, Peterson M. Medical student use of marijuana, alcohol, and cigarettes: a study of four schools. Int J Addict. 1972;7:141–152. [DOI] [PubMed] [Google Scholar]
- 26. Rochford J, Grant I, LaVigne G. Medical students and drugs: further neuropsychological and use pattern considerations. Int J Addict. 1977;12:1057–1065. [DOI] [PubMed] [Google Scholar]
- 27. Kory WP, Crandall LA. Nonmedical drug use patterns among medical students. Int J Addict. 1984;19:871–884. [DOI] [PubMed] [Google Scholar]
- 28. McAuliffe WE, Rohman M, Santangelo S, et al. Psychoactive drug use among practicing physicians and medical students. N Engl J Med. 1986;315:805–810. [DOI] [PubMed] [Google Scholar]
- 29. Conard S, Hughes P, Baldwin DC, Achenbach KE, Sheehan DV. Substance use by fourth-year students at 13 U.S. medical schools. J Med Educ. 1988;63:747–758. [DOI] [PubMed] [Google Scholar]
- 30. Schwartz RH, Lewis DC, Hoffmann NG, Kyriazi N. Cocaine and marijuana use by medical students before and during medical school. Arch Intern Med. 1990;150:883–886. [PubMed] [Google Scholar]
- 31. Croen LG, Woesner M, Herman M, Reichgott M. A longitudinal study of substance use and abuse in a single class of medical students. Acad Med. 1997;72:376–381. [DOI] [PubMed] [Google Scholar]
- 32. Choi D, Tolova V, Socha E, Samenow CP. Substance use and attitudes on professional conduct among medical students: a single-institution study. Acad Psychiatry. 2013;37:191–195. [DOI] [PubMed] [Google Scholar]
- 33. Zhou S, Van Devanter N, Fenstermaker M, Cawkwell P, Sherman S, Weitzman M. A study of the use, knowledge, and beliefs about cigarettes and alternative tobacco products among students at one U.S. medical school. Acad Med. 2015;90:1713–1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chan MH, Knoepke CE, Cole ML, McKinnon J, Matlock DD. Colorado medical students’ attitudes and beliefs about Marijuana. J Gen Intern Med. 2017;32:458–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Merlo LJ, Curran JS, Watson R. Gender differences in substance use and psychiatric distress among medical students: a comprehensive statewide evaluation. Subst Abuse. 2017;38:401–406. [DOI] [PubMed] [Google Scholar]
- 36. Ayala EE, Roseman D, Winseman JS, Mason HRC. Prevalence, perceptions, and consequences of substance use in medical students. Med Educ Online. 2017;22:1392824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lambert Passos SR, Alvarenga Americano do Brasil PE, Borges dos Santos MA, Costa de Aquino MT. Prevalence of psychoactive drug use among medical students in Rio de Janeiro. Soc Psychiatry Psychiatr Epidemiol. 2006;41:989–996. [DOI] [PubMed] [Google Scholar]
- 38. Di Pietro MC, Doering-Silveira EB, Oliveira MP, Rosa-Oliveira LQ, Da Silveira DX. Factors associated with the use of solvents and cannabis by medical students. Addict Behav. 2007;32:1740–1744. [DOI] [PubMed] [Google Scholar]
- 39. Da Silveira DX, Rosa-Oliveira L, Di Pietro M, Niel M, Doering-Silveira E, Jorge MR. Evolutional pattern of drug use by medical students. Addict Behav. 2008;33:490–495. [DOI] [PubMed] [Google Scholar]
- 40. Boniatti MM, Zubaran C, Panarotto D, et al. The use of psychoactive substances among medical students in southern Brazil. Drug Alcohol Rev. 2007;26:279–285. [DOI] [PubMed] [Google Scholar]
- 41. Carvalho KA, Sant’Anna MJ, Coates V, Omar HA. Medical students: abuse of psychoactive substances and sexuality aspects. Int J Adoles Med Health. 2008;20:321–328. [DOI] [PubMed] [Google Scholar]
- 42. De Oliveira LG, Barroso LP, Wagner GA, et al. Drug consumption among medical students in São Paulo, Brazil: influences of gender and academic year. Rev Bras Psiquiatr. 2009;31:227–239. [DOI] [PubMed] [Google Scholar]
- 43. Petroianu A, Reis DC, Cunha BD, Souza DM. Prevalence of alcohol, tobacco and psychotropic drug use among medical students at the Universidade Federal de Minas Gerais. Rev Assoc Med Bras. 2010;56:568–571. [DOI] [PubMed] [Google Scholar]
- 44. Buchanan JC, Pillon SC. Drug consumption by medical students in Tegucigalpa, Honduras. Rev Lat Am Enfermagem. 2008;16 Spec No:595–600. [DOI] [PubMed] [Google Scholar]
- 45. Ali RV, Vankar GK. Psychoactive substance use among medical students. Ind J Psychiatry. 1994;36:138–140. [PMC free article] [PubMed] [Google Scholar]
- 46. Rai D, Gaete J, Girotra S, Pal HR, Araya R. Substance use among medical students: time to reignite the debate? Natl Med J India. 2008;21:75–78. [PubMed] [Google Scholar]
- 47. Jodati AR, Shakurie SK, Nazari M, Raufie MB. Students’ attitudes and practices towards drug and alcohol use at Tabriz University of Medical Sciences. East Mediterr Health J. 2007;13:967–971. [PubMed] [Google Scholar]
- 48. Budhathoki N, Shrestha MK, Acharya N, Manandhar A. Substance use among third year medical students of Nepal. J Nepal Health Res Counc. 2010;8:15–18. [PubMed] [Google Scholar]
- 49. Ihezue UH. Drug abuse among medical students at a Nigerian university: part 1. Prevalence and pattern of use. J Nat Med Assoc. 1988;80:81–85. [PMC free article] [PubMed] [Google Scholar]
- 50. James BO, Omoaregba JO. Nigerian medical students’ opinions about individuals who use and abuse psychoactive substances. Subst Abuse. 2013;7:109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Myles H, Myles N, Large M. Cannabis use in first episode psychosis: meta-analysis of prevalence, and the time course of initiation and continued use. Aust N Z J Psychiatry. 2016;50:208–219. [DOI] [PubMed] [Google Scholar]
- 52. Nazarzadeh M, Bidel Z, Mosavi Jarahi A, et al. Prevalence of Cannabis lifetime use in Iranian high school and college students: a systematic review, meta-analyses, and meta-regression. Am J Mens Health. 2015;9:397–409. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, rev_supplementary_xyz9610434e3d4a for Prevalence of Cannabis Use Among Medical Students: A Systematic Review and Meta-analysis by Georgios Papazisis, Spyridon Siafis, Ioannis Tsakiridis, Ioannis Koulas, Themistoklis Dagklis and Dimitrios Kouvelas in Substance Abuse: Research and Treatment