Abstract
Purpose
The aim of this study was to determine if a tablet-based home practice program with weekly telepractice support could enable long-term maintenance of recent treatment gains and foster new language gains in poststroke aphasia.
Method
In a pre–post group study of home practice outcomes, 21 individuals with chronic aphasia were examined before and after a 6-month home practice phase and again at follow-up 4 months later. The main outcome measure studied was change in naming previously treated or untreated, practiced or unpracticed pictures of objects and actions. Individualized home practice programs were created in iBooks Author with semantic, phonemic, and orthographic cueing in pictures, words, and videos in order to facilitate naming of previously treated or untreated pictures.
Results
Home practice was effective for all participants with severity moderating treatment effects, such that individuals with the most severe aphasia made and maintained fewer gains. There was a negative relationship between the amount of training required for iPad proficiency and improvements on practiced and unpracticed pictures and a positive relationship between practice compliance and same improvements.
Conclusion
Unsupervised home practice with weekly video teleconferencing support is effective. This study demonstrates that even individuals with chronic severe aphasia, including those with no prior smart device or even computer experience, can attain independent proficiency to continue practicing and improving their language skills beyond therapy discharge. This could represent a low-cost therapy option for individuals without insurance coverage and/or those for whom mobility is an obstacle to obtaining traditional aphasia therapy.
Aphasia is not a unitary disorder but, at its core, is a disabling impairment in the ability to retrieve words in spite of a preserved idea that fails to be expressed as intended.
Because of the ubiquitous nature of word retrieval impairments in aphasia, many evidence-based treatment programs focus on improving naming. The last two decades have seen an increase in therapeutic translation of basic principles of neuroplasticity (Berthier & Pulvermuller, 2011; Pulvermüller & Berthier, 2008), with positive outcomes often observed in chronic aphasia following short-term intensive naming treatment protocols (e.g., Kurland, Pulvermüller, Silva, Burke, & Andrianopoulos, 2012; Kurland, Stanek, Stokes, Li, & Andrianopoulos, 2016). The success of many of these treatment programs stems from use-dependent plasticity, that is, practice generating target words leads to synaptic strengthening of synchronously fired neuronal circuits in the naming network (Berthier & Pulvermuller, 2011; Kleim & Jones, 2008). Provision of massive doses of treatment is thus a core principle of many short-term intensive treatment protocols, for example, constraint-induced language therapy (Pulvermüller et al., 2001), cued picture naming (Harnish et al., 2014), and semantic/phonological anomia treatment (Fridriksson et al., 2007). Recently, some have called into question the “more is better” framework for treatment intensity (Cherney, Patterson, Raymer, Frymark & Schooling, 2010). It has been suggested, for example, that spaced retrieval practice may be more efficient than massed learning (Middleton et al., 2016) and that better naming outcomes may follow distributed versus intensive therapy schedules in an intensive, comprehensive aphasia program (Dignam et al., 2015). Nonetheless, the bulk of evidence still supports the idea that therapeutic gains are greater and perhaps longer lasting with intensive therapy schedules (Basso & Caporali, 2001; Bhogal, Teasell, & Speechley, 2003; Brady, Kelly, Godwin, Enderby, & Campbell, 2016).
Unfortunately, even when evidence-based treatments demonstrate large effect sizes for primary treatment outcomes in as little as 2 weeks, critical gaps remain in translating experimental programs that take advantage of massive doses of treatment into clinically viable aphasia treatment programs. An obvious problem is that intensive treatment is seldom administered in the real world of “affordable care.” This is particularly true in the United States, whereas in European countries that have single-payer health care systems, intensive therapy may be delivered in inpatient and outpatient rehabilitation hospital settings (e.g., Kirmess & Maher, 2010; Sickert, Anders, Munte, & Sailer, 2014).
One proposed solution, made possible in the last decade by the development and ubiquity of customizable tablet-based application software (apps), comes in the form of aphasia-specific home practice (HP) programs. If the adage “practice makes perfect” applies to neurorehabilitation, then increased opportunities for massed, personalized practice should be of benefit to people with aphasia and the speech-language pathologists (SLPs) who treat them. HP programs offer many advantages to traditional outpatient therapy, including accessibility to those in rural and remote locations, and opportunities for massed practice combined with the portability and autonomy to practice when and where persons with aphasia (PWAs) choose (Kurland, 2014).
Unfortunately, as first seen with the advent of computer-assisted aphasia therapy, the evidence base has taken a back seat to the proliferation of commercially available aphasia-specific apps. Some apps (e.g., Constant Therapy, Tactus Therapy) seem to be routinely utilized in clinical practice, marketed as a tool for increased productivity in therapy, and recommended to outpatients at discharge for unsupervised HP. Although it may be the case that some therapy is better than no therapy, many questions have yet to be answered with regard to aphasia apps' treatment efficacy, for example, whether massed unsupervised practice is effective in maintaining and extending treatment gains and for whom it may be most effective, and whether telepractice can be an effective means of supervising independent home use of apps. Although the literature on both telepractice and aphasia HP programs is sparse, some researchers have begun to investigate these important questions.
Telepractice in Aphasia Treatment
Although video teleconferencing technology has been utilized in group studies to assess PWAs (Hall, Boisvert, & Steele, 2013), the majority of published studies of remote delivery and/or supervision of aphasia treatment are single-subject or small group usability and feasibility studies (e.g., Dechene et al., 2011; Goldberg, Haley, & Jacks, 2012; McGrath, Dowds, & Goldstein, 2008; Rende & Ramsberger, 2011; Simic et al., 2016; Woolf et al., 2016). One very recent group study (n = 20) demonstrated that a functional treatment approach, Promoting Aphasics' Communicative Effectiveness (Davis & Wilcox, 1985), could be delivered via a telerehabilitation platform with positive results (Macoir, Martel Sauvageau, Boissy, Tousignant, & Tousignant, 2017). Likewise, in a quasirandomized controlled feasibility study, Woolf and colleagues found gains in picture naming following remote therapy exceeded those in a control group (Woolf et al., 2016). These studies have all concluded that telepractice is a viable means of service delivery in aphasia that warrants further investigation.
Tablet-Based HP Programs in Aphasia
Tablet-based HP programs are in a relatively nascent but fast-growing stage of development as noted in a recent special issue on iRehab in Aphasia Treatment (Kurland, 2014). Here again, most studies reporting positive results for self-administered home therapy using smart tablets have been single-subject (e.g., Lavoie, Routhier, Legare, & Macoir, 2016; Routhier, Bier, & Macoir, 2016) or small group feasibility studies. For example, a feasibility study of five PWAs demonstrated effectiveness of an iPad-based HP program on maintaining and augmenting recent treatment gains (Kurland, Wilkins, & Stokes, 2014). Similarly, Kiran and colleagues demonstrated feasibility of the Constant Therapy program in four PWAs (Kiran, Des Roches, Balachandran, & Ascenso, 2014).
A relatively new addition to tablet-based HP programs, the so-called “asynchronous telerehabilitation” platform, allows clinicians to individualize tasks for PWAs and remotely monitor therapy progress and update tasks as appropriate (e.g., iAphasia: Choi, Park, & Paik, 2016; eSALT: Hill & Breslin, 2016; Constant Therapy: Des Roches, Balachandran, Ascenso, Tripodis, & Kiran, 2015). Promising results were demonstrated, for example, in a pilot study with eight PWAs assessed pre–post 4 weeks of a pilot study using the web-based iAphasia HP program (Choi et al., 2016).
Similarly, Des Roches and colleagues reported the effectiveness of an iPad-based personalized HP program (Constant Therapy) in supporting improvements in both practiced tasks and generalization to overall language and cognitive skills (Des Roches et al., 2015). Fifty-one survivors of stroke and traumatic brain injury were pseudorandomly enrolled in an experimental group (n = 42) and a control group (n = 9). Whereas both groups attended a 1-hr/week treatment session wherein a clinician assisted participants with the language and cognitive tasks, only the experimental group additionally practiced the therapy at home on iPads. The duration of treatment for both groups was equal (10 weeks), but the dosage was much higher for the experimental group, whose accuracy and latency on treatment tasks and performance on standardized tests improved more than the control group. This study provided evidence that personalized, self-paced language and cognitive HP can be effective. One limitation to the study is that participants had to attend weekly treatment sessions in the clinic over the course of the 10 weeks. Although this made sense in terms of experimental control, it prevents the study from definitively addressing the question of providing remote therapy such as might be optimum for stroke survivors in rural and exurban areas and those who struggle with transportation issues (Brennan, Georgeadis, & Baron, 2002; Mashima & Doarn, 2008), access to limited SLP services (Brady, 2007), and/or a generous enough insurance policy to cover extended reimbursable services (Baron, Hatfield, & Georgeadis, 2005).
The goal of the current study was to examine the effects of a 6-month tablet-based HP program with weekly telepractice check-in that followed a 2-week intensive aphasia treatment program described elsewhere (Kurland et al., 2016). One aim was to investigate whether unsupervised HP with weekly telepractice would make recently treated pictures more resistant to the typical decay that follows treatment gains over time. A second aim was to examine whether PWAs could independently use the HP program to improve accuracy on previously untreated pictures. A third aim was to understand variables that contributed to successful independent use of an HP program in most, but not all, PWAs.
We expected aphasia severity to be an important factor in the outcomes and thus included it in our linear mixed effects (LME) model. We also hypothesized that, generally, naming accuracy would be greatest and maintained longest for treated/practiced pictures, followed by treated/unpracticed and untreated/practiced, with the least change observed on untreated/unpracticed pictures over time. We also expected, based on pilot work, to observe associations between training requirements and performance and between practice compliance and performance during the HP phase, regardless of severity.
Method
Participants
The institutional review board of the University of Massachusetts Amherst approved the study, and signed informed consent was obtained from all participants before commencing assessment and treatment. Twenty-four PWAs were enrolled in and completed a 2-week intensive language therapy protocol (Kurland et al., 2016). Following treatment, participants had the option to continue treatment in a 6-month HP program. Two participants did not complete the HP phase, and one participant did not complete the testing protocols.
For the current study, 21 individuals (eight women, 13 men), with mean age of 66.4 years (SD = 8.4, range 47.3–81) completed this study (see Table 1 for individual demographic and clinical characteristics). All participants were chronically aphasic, and most (n = 18) reported a medical history that included a single unilateral left hemisphere middle cerebral artery stroke. Most participants (n = 19) were premorbidly right-handed according to self-report on the Edinburgh Inventory (Oldfield, 1971). The average time poststroke was 29.3 months (SD = 37.1, range 6–142). Most participants (n = 19) were monolingual English speakers, and all reported the first language was English. Most participants (n = 14) had at least a bachelor's degree, but two did not finish high school. One participant (P20) reported a history of reading difficulty. None of the other participants reported any history of developmental learning disabilities.
Table 1.
Demographic and clinical characteristics of participants.
| ID | Age (years) | Gender | Premorbid handedness | Time postonset (months) | Etiology (CVA) | Aphasia classification | Aphasia severity block | Presence, absence, severity of AOS | Education (years) | Primary site of lesion |
|---|---|---|---|---|---|---|---|---|---|---|
| P1 | 74.92 | Female | R | 25 | Isch | Anomic | mild/mod | absent | 16 | T-P |
| P2 | 55.00 | Female | R | 7 | Hem | Optic | mild/mod | absent | 16 | T-O |
| P3 | 67.83 | Female | R | 25 | Isch | Anomic | mild/mod | mild/mod | 14 | F-T-P |
| P4 | 67.50 | Male | R | 8 | Isch | Conduction | mild/mod | mild | 17 | T |
| P5 | 62.50 | Male | R | 7 | Hem | Optic | mild/mod | absent | 16 | T-P-O |
| P6 | 64.08 | Male | R | 24 | Isch | Anomic | mild/mod | absent | 16 | n/a |
| P7 | 68.83 | Male | L | 9 | Isch | TCS | mild/mod | absent | 20 | T-P-O |
| P8 | 63.00 | Female | R | 8 | Isch | Anomic | mild/mod | absent | 18 | n/a |
| P9 | 64.50 | Female | R | 12 | Isch | TCMale | mod/sev | mild | 16 | Female |
| P10 | 74.67 | Male | R | 142 | Isch | TCMale | mod/sev | mild/mod | 20 | F-T |
| P11 | 81.00 | Female | R | 16 | Isch | TCS | mod/sev | mild | 12 | n/a |
| P12 | 71.00 | Female | R | 13 | Isch | Anomic | mod/sev | mild | 16 | F-T |
| P13 | 60.83 | Male | R | 7 | Hem | Broca's | mod/sev | mod/marked | 11 | F-T-P |
| P14 | 59.67 | Male | R | 82 | Isch | Wernicke's | mod/sev | mild/mod | 16 | T-P |
| P15 | 47.33 | Male | R | 13 | Hem | Anomic | mod/sev | absent | 16 | T |
| P16 | 70.50 | Female | R | 108 | Hem | Broca's | mod/sev | mod/marked | 12 | F-T-P |
| P17 | 55.33 | Male | R | 23 | Isch | Mixed TC | mod/sev | absent | 14 | F-T-P |
| P18 | 70.00 | Male | R | 6 | Isch | Wernicke's | sev | absent | 12 | T-P |
| P19 | 61.75 | Male | L | 11 | Isch | Global | sev | sev | 18 | F-T |
| P20 | 79.83 | Male | R | 12 | Hem | Broca's | sev | mod/sev | 8 | Female |
| P21 | 74.33 | Male | R | 57 | Isch | Wernicke's | sev | absent | 16 | F-T-P |
Note. CVA = cerebrovascular accident; AOS = apraxia of speech; R = right; L = left; Isch = ischemic; Hem = hemorrhagic; Mixed TC = mixed transcortical aphasia; TCM = transcortical motor aphasia; TCS = transcortical sensory aphasia; mod = moderate; sev = severe; F = frontal; T = temporal; P = parietal; O = occipital; n/a = not available.
Aphasia severity was determined by a combination of Western Aphasia Battery–Revised Aphasia Quotient (WAB-R AQ; Kertesz, 2006), Boston Diagnostic Aphasia Examination (BDAE) Aphasia Severity Rating Scale (Goodglass, Kaplan, & Barresi, 2001), and mean baseline performance on a subset (n = 218) of an object naming task (Snodgrass & Vanderwart, 1980). Participants with mild-to-moderate (mild/mod) aphasia (WAB-R AQ > 75) scored in the range of 2–4 on the BDAE Aphasia Severity Rating Scale with mild/mod word retrieval impairments as demonstrated by their mean baseline object naming scores (group mean = 56% correct, SD = 0.15); participants with moderate-to-severe (mod/sev) aphasia (50 < WAB-R AQ < 75) scored in the range of 1.5–2 on the BDAE Aphasia Severity Rating Scale with mod/sev word retrieval impairments (mean = 44%, SD = 0.22); participants with severe (sev) aphasia (WAB-R AQ < 50) were in the range of 1–1.5 on the BDAE Aphasia Severity Rating Scale with severe word retrieval impairments (mean = 10%, SD = 0.05).
The presence and severity of apraxia of speech (AOS) were determined by an experienced SLP's evaluation of each participant's results on the Apraxia Battery for Adults–Second Edition (Dabul, 2000) and video-recorded speech samples, which were analyzed using the clinical criteria and cardinal signs of AOS published by Darley, Aronson, and Brown (1975), Wambaugh (2006), McNeil, Robin, and Schmidt (2009), and Duffy (2012). Each participant was assigned an overall rating for the presence/absence and severity of AOS based on the outcomes obtained from all test procedures and protocols using the following 5-point scale (0 = normal—no evidence of AOS; 1 = mild AOS; 2 = moderate AOS; 3 = marked AOS; and 4 = severe AOS). The Apraxia Battery for Adults–Second Edition and speech samples for each participant were also scored and analyzed independently by a trained second judge to assess reliability. Discrepancies between the two judges' ratings for severity and/or diagnosis were resolved by reviewing the video recordings and achieving consensus. Interrater reliability on 17.4% of the data revealed what Landis and Koch identify as “substantial” agreement at 0.78 (0.61–0.80; Landis & Koch, 1977).
Procedure
Six-Month HP Program With Weekly Teletherapy
HP stimuli . Treatment stimuli consisted of previously treated (TR; n = 40) and untreated (UNTR; n = 40) sets of black and white line drawings of common objects (Snodgrass & Vanderwart, 1980) and picturable actions (Masterson & Druks, 1998). Half of TR and half of UNTR pictures were practiced (PR) and half were unpracticed (UNPR) during the HP program. For each individual PWA, sets of TR-PR and TR-UNPR objects (OBJ) and actions (ACT) and sets of UNTR-PR and UNTR-UNPR OBJ and ACT were matched on word frequency, length, familiarity, visual complexity, and other variables known to influence word retrieval. They were also approximately matched for posttreatment naming accuracy. Where there was a slight discrepancy, the set with worse performance was assigned to be practiced; otherwise, the sets were randomly assigned to the PR and UNPR condition. Thus, each PWA had a unique set of 10 TR-PR OBJ, 10 TR-PR ACT, 10 UNTR-PR OBJ, and 10 UNTR-PR ACT to be practiced at home, whereas an equal number of OBJ and ACT were TR-UNPR or UNTR-UNPR.
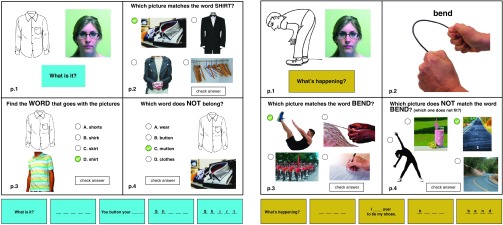
HP iBooks. Following intensive language treatment described elsewhere (Kurland et al., 2016), individualized interactive books were created for each participant using iBooks Author software. Two books of 20 chapters were created for each PWA, one containing OBJ and one containing ACT. Each chapter contained a title page with the name of the OBJ and four interactive pages targeting various levels of semantic, phonologic, and orthographic cueing as described in Kurland et al. (2014). The first page of each OBJ chapter consisted of the picture, along with a series of tasks that participants scrolled through, providing increasing levels of cueing. This exercise could be enlarged to full screen, effectively creating a fifth page. For example, if the target were “shirt,” beginning with the question “What is it?” one scrolled to a screen with a series of five dashes (“- - - - -”), then to a screen with a semantically cued cloze sentence (“You button your - - - - -”), then to an orthographically cued screen (“s h - - -”), and finally to a screen with the word spelled out (“s h i r t”). On the same page, there was a video of a student slowly enunciating the target word, which could be enlarged to full screen. PWAs, particularly those with severe expressive aphasia and/or AOS, were encouraged to repeatedly play the video (rather than guess) unless and until they were confident of their own production of the word. The second page was a picture-to-word matching task (“Which picture matches the word SHIRT?”), with a randomly located color photograph of a representation of the OBJ and three semantically related foils (“jacket,” “sweater,” “hanger”). Page 3 was a word-to-picture matching task that included the line drawing, a different color photograph, and the instruction (“Find the word that goes with the pictures”) along with the randomly located target word and three semantically, orthographically, and/or phonemically related foils (“shorts,” “shirk,” “skirt”). Page 4 was similar to page 3, but with instructions (“Which word does NOT belong?”), with three semantically related foils (“wear,” “button,” “clothes”) and an “odd-man-out” (“mutton”). The odd-man-out could be a phonological neighbor of a semantic associate of the target (as in “mutton”) or an orthographic neighbor of the target (e.g., target: “spider”; foils: “insect,” “legs,” “web”; odd-man-out: “spindle”), or a semantic associate of one of the three foils (e.g., target: “watermelon”; foils: “seeds,” “pink,” “summer”; odd-man-out: “blue”). The last page always signaled completion of the chapter with the OBJ drawing, the word, and a place to check off that exercises were completed. For every interactive task that required a click on an answer, there was a “Check Answer” button, so that PWAs could confirm accuracy or go back and try again (see Figure 1).
Figure 1.
Examples of typical pages from two home practice chapters, one from an Objects Book for the word “shirt” and one from an Actions Book for the word “bend.” Video and audio of the target word were always provided on page 1 of both books. Action books also included video/audio of the target action and word. Bottom row shows the expanded tasks on page 1 of Objects (“What is it?) and Actions (“What's happening?”) books.
Action books were similarly organized with somewhat different content. For example, in lieu of the question “What is it?” in the scrolling tasks on page one, the PWA had to answer the question, “What's happening?” On Page 2, there was a short (5–8 s) video of a student performing the action with a voiceover audio cue at the end (e.g., “bend”). Action words were always printed and spoken in the infinitive. Page 3 was a picture-to-word matching task (“bend,” “twist,” “band,” “break”), and Page 4 included the odd-man-out task with semantically related foils that generally implied the action used in different contexts than the original line drawing. For example, in lieu of a man bending over, there was a woman bent in a yoga pose, a bent straw, and a bend in the road, and the target was a straight road (see Figure 1).
Targets and foils were high-quality color photographs downloaded from Internet sites such as Creative Commons, Flickr, and Google Images. Lexical stimuli for the “What is it?” and “What's happening?” routines were produced in Paint. Videos were mostly homemade on an iPad, with video clips edited in iMovie. Although we attempted to select foils that would be semantically, phonologically, and/or orthographically challenging, visual simplicity was always prioritized.
HP training. Participants received variable degrees of training on how to navigate the iPad, the iBooks HP app, the video teleconferencing app (GoToMeeting [GTM]), and a stopwatch app used for keeping track of practice compliance (Clock). With the exception of three PWAs who had prior experience with an iPad, most participants had little exposure to smart devices and required two to three 45-min training sessions (mean = 2.48, SD = 1.03) to get to a basic proficiency level for independent or minimally assisted use of the iPad (see Table 2). Thus for most participants, initial hands-on training in the clinic included a very basic introduction to the device, how to power it on/off, how to find the home screen, how to charge it, how to place it in a stand, how to find the volume button, how to scroll, and so forth. If a participant had difficulty in scrolling with their fingers, they were trained to use a stylus. In all but two cases (P3 and P8, who had their own iPads), participants borrowed lab iPads that had been cleaned up, such that only the relevant apps for the HP program were obvious on the home screen.
Table 2.
Participant prior experience and training required for basic home practice proficiency.
| ID | Prior experience with iPad or other tablet (N = no; Y = yes) | Prior experience with PC or Mac (N = none; L = low; H = high) | No. of sessions of training required for basic iPad proficiency | No. of sessions of training required for basic GTM proficiency |
|---|---|---|---|---|
| P1 | N | N | 3 | 3 |
| P2 | N | L | 2 | 3 |
| P3 | Y | H | 1 | 1 |
| P4 | N | L | 2 | 1 |
| P5 | N | H | 2 | 2 |
| P6 | N | H | 1 | 1 |
| P7 | Y | H | 2 | 1 |
| P8 | Y | L | 2 | 2 |
| P9 | N | L | 2 | 2 |
| P10 | N | L | 3 | 3 |
| P11 | N | N | 5 | 6 |
| P12 | N | L | 3 | 3 |
| P13 | N | L | 2 | 3 |
| P14 | N | L | 3 | 3 |
| P15 | N | H | 2 | 1 |
| P16 | N | N | 2 | 2 |
| P17 | N | H | 2 | 3 |
| P18 | N | L | 3 | na |
| P19 | N | L | 2 | 3 |
| P20 | N | N | 3 | na |
| P21 | N | N | 5 | na |
| Mean | 2.48 | 2.39 | ||
| SD | 1.03 | 1.24 |
Note. GTM = GoToMeeting video teleconferencing app; na = never achieved independent proficiency on GTM.
Once a participant was comfortable with iPad basics, they were introduced to the iBooks app and trained in how to move through the chapters, switch between ACT and OBJ books in the library, and how to practice on their unique word sets. They were encouraged to maximize the number of trials and total amount of practice and to use the video model whenever they were uncertain, so as to minimize incorrect spoken productions. In cases where a participant had difficulty in reading a word, such as might occur in picture/word matching exercises or in reading printed instructions for each task, PWAs were taught to use the text-to-speech function on the iPad. All participants were trained until the SLP was confident that they could perform the tasks independently at home.
PWAs were asked to try to practice for at least 20 min, 5–6 days per week; however, the iBooks app was not able to monitor practice compliance. Instead, participants were trained to locate, start, and stop a digital stopwatch on the iPad home screen before and after practice in order to track daily usage. After each self-initiated practice session, they were asked to copy into a log the numbers that were displayed on the stopwatch. In addition, the SLP who met with each participant for half an hour weekly over GTM would ask them to report how often they had practiced during the previous week.
Once the SLP was confident that participants could practice independently at home, iPads and peripheral devices were delivered to each PWA. The home visit was important because it allowed the SLP to train the participant along with anyone who might be available in the home (spouse, child, etc.) in how to troubleshoot potential technical issues with power, audio signal, Wi-Fi or cellular connectivity, and basic app usage. Moreover, it was essential to ensure that the iPad would pick up a Wi-Fi signal in homes that already had wireless service or that cellular service was available and the signal sufficient for the weekly telepractice meetings. If needed, monthly cellular service was provided free of charge. The initial home visit also allowed the SLP to initiate the onsite training in how to connect weekly with her via GTM.
Telepractice. Participants met with the SLP on their iPad, using GTM, once a week at a regular prescheduled time, usually on a Monday. Telepractice sessions predominantly consisted of informal conversation and a series of clinician-initiated questions that sought to obtain information from each PWA regarding their practice compliance, any technical issues they might be having, and feedback regarding their comfort and confidence in using the device. The session lasted up to 30 min. Once a month, for 6 months during the HP phase, PWAs returned to the clinic for probe testing to track progress on treated and untreated, practiced and unpracticed words. If there was a technical issue with the iPad or connectivity and a monthly probe was imminent, PWAs brought their iPad in for service. On a few occasions, the SLP had to make extra home visits to assess technical issues and/or ensure practice compliance.
Testing
The main outcome measure was percent accuracy on naming sets of treated and untreated, practiced and unpracticed objects and actions. All 80 TR and UNTR pictures were probed along with an additional set of 40 actions and objects that they could name at baseline (CORR). Probes were acquired three times on separate days prior to the start of the HP program (posttreatment/pre-HP), once a month during the HP phase, three times post-HP, and three times following a 4-month period of no HP or other therapy. Pre- and post-HP probes were acquired, on average, once per week over a 3-week period. PWAs named the 120 pictures in alternating blocks of 15 objects, 15 actions, 15 objects, and so forth. Within blocks, pictures alternated between CORR, TR, and UNTR sets, with practice condition quasirandomly ordered (e.g., CORR, TR-PR, UNTR-PR, CORR, TR-UNPR, UNTR-PR, CORR, TR-PR, UNTR-UNPR, etc.).
Other tests administered pre-HP, post-HP, and at follow-up included subtests of the BDAE and the Boston Naming Test (Kaplan, Goodglass, & Weintraub, 2001).
Statistics
We fit an LME model with proportion of accurately named pictures as the response and seven independent variables: (a) severity (mild/mod, mod/sev, sev), (b) word class (ACT, OBJ), (c) treatment condition (TR, UNTR), (d) practice condition (PR, UNPR), (e) phase (posttreatment/pre-HP, HP, post-HP, maintenance/follow-up), (f) a continuous time variable, and (g) PWAs. The LME model deals with the longitudinal design of the study by extending the regular linear regression with an additional PWA variable and modeling the effects of the PWA as normally distributed random variables. The model assumes that there are separate intercepts for each PWA, and the subject-specific intercepts are a random sample from all the intercepts of the population of PWAs. The random intercepts capture the between-subjects heterogeneity and the within-subject correlation as a result of the heterogeneity. The effects of PWAs are called random effects, and those of other variables are called fixed effects. Because of their advantage in dealing with missing values, mixed effects models are often preferred over more traditional approaches such as repeated measures analysis of variance. We included both a continuous time covariate and the discrete time covariate (phase) to decompose the time effect into the between-phases effect and a within-phase continuous time effect.
For model selection, we use the backward elimination of nonsignificant effects, with the full model including the four-way interaction of severity, treatment condition, practice condition, and phase, two-way interaction of severity and word class, and a continuous time effect. Model fitting and inference, and model selection were done through the R lmerTest package (https://CRAN.R-project.org/package=lmerTest). Contrasts between the PR and UNPR conditions were performed using the bootstrap inference for mixed models (https://CRAN.R-project.org/package=lme4).
Exploratory correlational analyses were also performed in order to examine associations between naming gains and factors assumed to support individuals' varying ability to maintain and/or extend the naming gains accrued during the prior treatment period. These variables included amount of training required for participants to reach independence with the equipment and apps and self-reported number of days practiced during the HP phase.
Finally, although a full qualitative analysis of the evolution of errors over time is beyond the scope of this article, a post hoc analysis was performed of change in naming responses, including error types, on a small sample of pre-/post-HP naming probes. Responses to TR and UNTR pictures from the last pre-HP and the first post-HP probes were analyzed and coded as follows: correct, self-corrected, semantic paraphasias, phonemic paraphasias, incorrect, unintelligible, or no response given. The analysis of these data is strictly descriptive.
Results
Mixed Effects Model
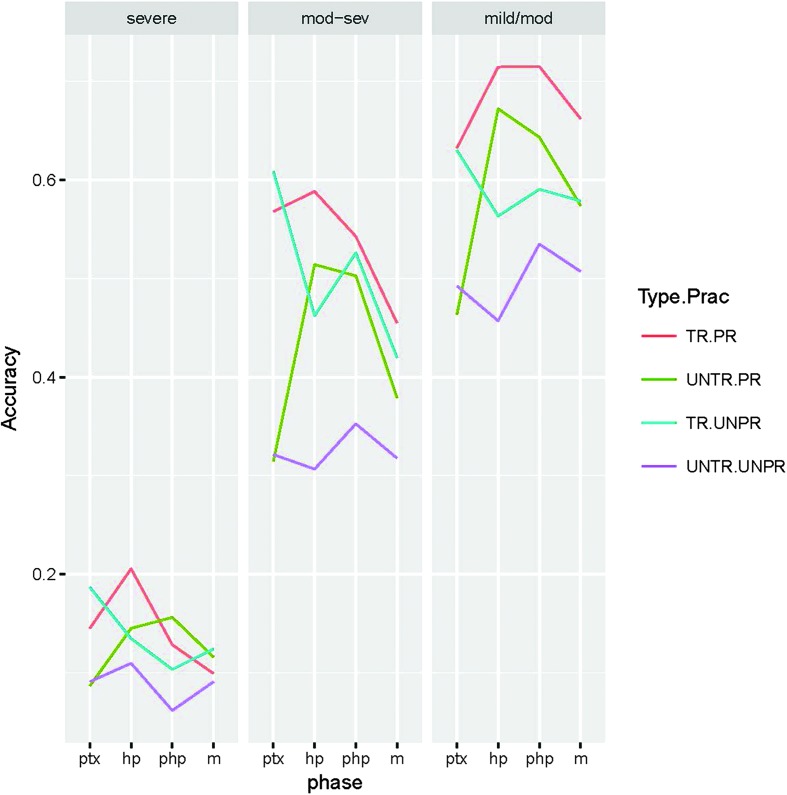
We present in Table 3, Table 4, and Figure 2 the model fitting results based on the LME model. The variables are coded following the rule of effects coding. In effects coding, the coefficient of each variable represents the amount of deviation of the group mean from the grand mean where the group is defined by the first level of the variable. For a two-level variable, the difference between the two group means is therefore two times the coefficient of the variable. The intercept is the grand mean.
Table 3.
Significant fixed effects in the linear mixed effects model.
| Fixed effect | β | SE | p |
|---|---|---|---|
| (Intercept) | 0.396 | 0.039 | < .001 |
| Severity, sev | −0.284 | 0.062 | < .001 |
| Phase, HP | 0.019 | 0.005 | < .001 |
| Phase, post-HP | 0.017 | 0.007 | .011 |
| Practice condition, PR | 0.03 | 0.004 | < .001 |
| Treatment condition, TR | 0.045 | 0.004 | < .001 |
| Word class, ACT | 0.009 | 0.003 | .007 |
| Word class, ACT × Severity, sev | −0.021 | 0.005 | < .001 |
| Word class, ACT × Severity, mod/sev | −0.019 | 0.004 | < .001 |
| Phase, pre-HP × Practice condition, PR | −0.04 | 0.006 | < .001 |
| Phase, HP × Practice condition, PR | 0.037 | 0.005 | < .001 |
| Severity, sev × Phase, post-HP | −0.029 | 0.01 | .005 |
| Severity, sev × Practice condition, PR | −0.019 | 0.005 | .001 |
| Phase, pre-HP × Treatment condition, TR | 0.038 | 0.006 | < .001 |
| Phase, post-HP × Treatment condition, TR | −0.016 | 0.007 | .02 |
| Practice condition, PR × Treatment condition, TR | −0.008 | 0.004 | .019 |
| Severity, sev × Treatment condition, TR | −0.028 | 0.005 | < .001 |
| Severity, mod/sev × Treatment condition, TR | 0.027 | 0.005 | < .001 |
| Severity, sev × Phase, HP × Practice condition, PR | −0.022 | 0.008 | .006 |
| Severity, mod/sev × Phase, pre-HP × Treatment condition, TR | 0.024 | 0.008 | .003 |
| Severity, sev × Phase, HP × Practice condition, PR × Treatment condition, TR | 0.017 | 0.008 | .028 |
Note. The intercept represents the overall mean accuracy, and the coefficient of a variable represents the effect of the variable as the amount of deviation from the overall mean. ACT = action pictures; sev = severe; HP = home practice phase; PR = practiced pictures; TR = treated pictures; mod/sev = moderate-to-severe.
Table 4.
Estimated change of the percent difference between practiced and unpracticed pictures over time.
| Pre-HP treatment condition | Between phases | PWA severity | deltaDiff | Lower | Upper |
|---|---|---|---|---|---|
| Treated pictures | HP–pre-HP | ||||
| sev | 0.113* | 0.006 | 0.217 | ||
| mod/sev | 0.167* | 0.1 | 0.237 | ||
| mild/mod | 0.149* | 0.071 | 0.226 | ||
| Post-HP–pre-HP | |||||
| sev | 0.067 | −0.063 | 0.187 | ||
| mod/sev | 0.057 | −0.04 | 0.155 | ||
| mild/mod | 0.123* | 0.03 | 0.213 | ||
| Maint–pre-HP | |||||
| sev | 0.017 | −0.101 | 0.14 | ||
| mod/sev | 0.076 | −0.001 | 0.152 | ||
| mild/mod | 0.081 | −0.007 | 0.167 | ||
| Untreated pictures | HP–pre-HP | ||||
| sev | 0.04 | −0.058 | 0.145 | ||
| mod/sev | 0.214* | 0.141 | 0.278 | ||
| mild/mod | 0.244* | 0.174 | 0.314 | ||
| Post-HP–pre-HP | |||||
| sev | 0.099 | −0.023 | 0.223 | ||
| mod/sev | 0.157* | 0.065 | 0.252 | ||
| mild/mod | 0.138* | 0.043 | 0.231 | ||
| Maint–pre-HP | |||||
| sev | 0.029 | −0.098 | 0.143 | ||
| mod/sev | 0.068 | −0.015 | 0.146 | ||
| mild/mod | 0.096* | 0.014 | 0.179 |
Note. Estimated change of the percent difference between practiced and unpracticed pictures over time and the corresponding confidence interval based on the linear mixed effects model. deltaDiff is the estimated change of the difference in naming accuracy. deltaDiff is significantly different from zero (*) if its (lower/upper) confidence interval does not contain zero. HP = home practice; pre-HP = same as posttreatment; PWA = person with aphasia; mod = moderate; sev = severe; Maint = maintenance/follow-up testing.
Figure 2.
Estimated naming accuracy for object pictures for different training (TR) and practice (PR) conditions by aphasia severity. Type.Prac = condition of training and practice; UNTR = untrained; UNPR = unpracticed; mod = moderate; sev = severe; ptx = posttreatment; hp = home practice; php = post-home practice; m = maintenance.
In accordance with expectations, there was a main effect of aphasia severity, such that more severe participants had smaller naming gains. Starting from the intercept that represents overall average naming accuracy (β = .396, SE = .039, p < .001), participants with severe aphasia named fewer pictures (β = −.284, SE = .062, p < .001). In other words, participants with severe aphasia named 28.4% fewer pictures correctly than the grand mean. Accuracy of participants with mod/sev aphasia was at the level of the grand mean (the deviation was not significant), and accuracy of those with mild/mod aphasia was 28.4% greater. Participants demonstrated elevated accuracy during HP and post-HP phases by 1.9% and 1.7%, respectively. The average accuracy in the posttreatment phase was not significantly different from the grand mean, and it was 3.6% (= 1.9% + 1.7%) less than the grand mean in the follow-up testing phase. PR and TR pictures were named more accurately by 3% and 4.5%, respectively.
On average, participants performed better on ACT words (0.9% better than the grand mean of 39.6% and 1.8% [= 2 × 0.9%] better than on OBJ words). It is worth noting, however, that when we removed two participants with optic aphasia (P2 and P5) from the model in a post hoc analysis, we found nearly no changes in other variables except for the word class variable. With P2 and P5 removed, participants performed better on OBJ words (0.9% better).
The following summarizes some of the important significant interactions shown in Table 3. Word class and severity of aphasia interacted significantly, such that participants with severe or mod/sev aphasia had greater difficulty in naming ACT words. Phase interacted separately with word class, practice condition, severity, and treatment condition. On average, PR pictures were named more accurately than UNPR pictures with a 6% difference. The difference was narrowed in the pre-HP phase, in which UNPR pictures were estimated to be named more accurately. As expected, the difference was widened in the HP phase. On average, TR pictures were named more accurately than UNTR pictures, with a 9% difference. Given that half of TR and half of UNTR pictures were selected for HP, as expected, the difference was widened in the pre-HP (posttreatment) phase and then narrowed in the post-HP phase.
Severity of aphasia interacted negatively with practice condition and treatment condition, such that persons with severe aphasia did not show as large differences in accuracy between naming TR and UNTR or PR and UNPR pictures. The three-way interaction among severity (sev), phase (HP), and practice condition (PR) indicates that, compared to the expected wider difference between naming PR and UNPR pictures in the HP phase, the difference for participants with severe aphasia was expected to be narrower. Finally, the continuous time effect was insignificant, indicating that naming accuracy only changed between phases and did not change significantly within a phase.
Table 4 shows the estimated change (delta) of the percent difference in naming accuracies with TR/PR versus TR/UNPR and UNTR/PR versus UNTR/UNPR pictures over time. For example, all PWAs, regardless of severity, were estimated to make significant gains naming TR/PR versus TR/UNPR pictures from posttreatment (pre-HP) to HP, with, on average, 11% gain for those with severe, 17% gain for those with mod/sev, and 15% gain for those with mild/mod. Although the estimated change continued to demonstrate a positive trend over time, the differences were only significant for the mild/mod group and only through post-HP. For UNTR pictures, naming gains for UNTR/PR versus UNTR/UNPR were also evident but not statistically significant for those with severe aphasia over time. For example, a 4% gain was estimated from pre-HP to HP (severe), whereas significant gains were estimated for mod/sev (21%) and mild/mod (24%) over this same time period. The delta difference continued to be significant for these two groups from pre-HP to post-HP (16% mod/sev, 14% mild/mod) and remained significant for the mild/mod group from pre-HP to 4 months post-HP (10%).
Variables Supporting Independent HP Success
Successful independent use of the HP program was seen in most, but not all, of the participants. One aim of this study was to gain a better understanding of the variables that contributed to success. As noted above in LME results, we found every term to interact significantly with severity. Thus, perhaps unsurprisingly, severity is a key variable underlying successful use of HP to maintain and extend treatment gains, effects that were observed to be particularly strong in persons with less severe aphasia.
To address other variables that may have contributed to HP success, we performed some exploratory correlational analyses on associations between number of training sessions required to reach basic iPad proficiency and HP success as well as between practice compliance and HP success. The SLP kept track of practice compliance through interviews conducted during weekly video teleconference meetings on GTM. These remote meetings also allowed the SLP to ascertain which participants were achieving independent use of both the iBooks HP programs and the GTM app and to schedule extra home visits as needed. Most PWAs attended most of the 24 scheduled GTM remote meetings, on average missing 4 (X = 4.14, SD = 2.89), and required very few extra home visits after the first home visit to set up equipment. On average, participants practiced daily 83% of the time (SD = 23%), and the majority was able to attain independence in using the iPad and connecting on GTM or independence with an assist to connect to weekly meetings (see Table 5).
Table 5.
Participant practice compliance and ultimate HP proficiency.
| ID | No. of GTMs missed | No. of extra home visits | % weeks where client practiced 5 days | HP program proficiency | GTM proficiency |
|---|---|---|---|---|---|
| P1 | 2 | 6 | 0.80 | Ind w assist | Ind w assist |
| P2 | 4 | 1 | 0.96 | Ind | Ind |
| P3 | 7 | 1 | 1.00 | Ind | Ind |
| P4 | 0 | 0 | 1.00 | Ind | Ind |
| P5 | 1 | 0 | 0.17 | Ind | Ind |
| P6 | 3 | 0 | 0.96 | Ind | Ind |
| P7 | 3 | 0 | 0.79 | Ind | Ind |
| P8 | 4 | 0 | 0.47 | Ind | Ind |
| P9 | 6 | 0 | 0.60 | Ind | Ind |
| P10 | 4 | 0 | 0.81 | Ind | Ind w assist |
| P11 | 1 | 7 | 0.93 | Ind | Ind w assist |
| P12 | 2 | 2 | 1.00 | Ind | Ind |
| P13 | 4 | 0 | 0.79 | Ind | Ind |
| P14 | 3 | 3 | 1.00 | Ind | Ind |
| P15 | 1 | 0 | 1.00 | Ind | Ind |
| P16 | 5 | 1 | 1.00 | Ind | Ind |
| P17 | 3 | 1 | 1.00 | Ind | Ind |
| P18 | 9 | 3 | 1.00 | Ind | Dep |
| P19 | 10 | 0 | 0.54 | Ind | Ind w assist |
| P20 | 10 | 0 | 0.56 | Dep | Dep |
| P21 | 5 | 5 | 1.00 | Dep | Dep |
| Mean | 4.14 | 1.43 | 0.83 | ||
| SD | 2.89 | 2.16 | 0.23 |
Note. GTM = GoToMeeting; HP = home practice; Ind = independent; Dep = dependent; Ind w assist = independent with assistance.
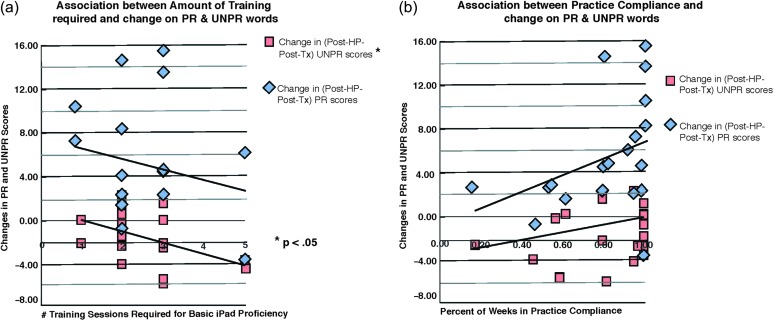
There was a significant relationship between number of training sessions required to achieve basic iPad proficiency and losses on UNPR words, r(21) = −.466, p < .05, during the HP program. In general, greater number of training sessions to reach independent proficiency was associated with fewer gains accurately naming PR and more losses naming UNPR words. Practice compliance was generally associated with better gains accurately naming PR words and fewer losses naming UNPR words (see Figure 3).
Figure 3.
Correlations between (a) number of training sessions required and (b) practice compliance, and change in number of correctly named practiced (PR) and unpracticed (UNPR) pictures. * = significant correlation (p < .05). HP = home practice; Tx = treatment.
A Post Hoc Exploration of Evolving Errors
A post hoc examination of changes in response types to naming TR and UNTR pictures on a small sample of pre- and post-HP probes revealed, on average, small changes in the evolution of error types in most PWAs. Some individuals, however, demonstrated interesting patterns of change, for example, most of P3's naming gains came from sharply decreased “no responses” and “unintelligible” responses. P5 made fewer semantic paraphasias and “no responses,” but some of these were replaced with incorrect responses. P7 replaced incorrect responses and semantic paraphasias with correct responses. P14 replaced “no responses” and “unintelligible” responses with correct responses (see Table 6).
Table 6.
Evolution of responses, including errors, on naming treated and untreated pictures from pre- to post-HP.
| ID | Correct | Self-corrected | Semantic paraphasia | Phonemic paraphasia | Incorrect | No response | Unintelligible response |
|---|---|---|---|---|---|---|---|
| P1 pre-HP | 58 | 5 | 6 | 0 | 4 | 7 | 0 |
| P1 post-HP | 61 | 2 | 8 | 0 | 1 | 8 | 0 |
| P2 pre-HP | 47 | 2 | 6 | 0 | 0 | 25 | 0 |
| P2 post-HP | 53 | 2 | 5 | 0 | 0 | 20 | 0 |
| P3 pre-HP | 50 | 2 | 9 | 1 | 1 | 13 | 4 |
| P3 post-HP | 67 | 1 | 8 | 0 | 0 | 3 | 1 |
| P4 pre-HP | 56 | 6 | 6 | 2 | 2 | 8 | 0 |
| P4 post-HP | 67 | 1 | 7 | 1 | 1 | 3 | 0 |
| P5 pre-HP | 25 | 4 | 9 | 0 | 17 | 24 | 1 |
| P5 post-HP | 25 | 2 | 4 | 0 | 34 | 13 | 2 |
| P6 pre-HP | 65 | 0 | 3 | 1 | 4 | 6 | 1 |
| P6 post-HP | 66 | 0 | 7 | 0 | 7 | 0 | 0 |
| P7 pre-HP | 38 | 2 | 13 | 0 | 8 | 19 | 0 |
| P7 post-HP | 53 | 0 | 6 | 0 | 4 | 17 | 0 |
| P8 pre-HP | 39 | 0 | 11 | 0 | 6 | 24 | 0 |
| P8 post-HP | 24 | 0 | 10 | 0 | 4 | 42 | 0 |
| P9 pre-HP | 53 | 2 | 8 | 0 | 7 | 10 | 0 |
| P9 post-HP | 58 | 2 | 8 | 0 | 3 | 9 | 0 |
| P10 pre-HP | 31 | 0 | 5 | 0 | 1 | 42 | 1 |
| P10 post-HP | 29 | 0 | 9 | 1 | 0 | 41 | 0 |
| P11 pre-HP | 42 | 1 | 9 | 3 | 6 | 15 | 4 |
| P11 post-HP | 46 | 0 | 14 | 1 | 3 | 13 | 3 |
| P12 pre-HP | 36 | 0 | 17 | 0 | 6 | 21 | 0 |
| P12 post-HP | 51 | 1 | 8 | 1 | 8 | 8 | 3 |
| P13 pre-HP | 51 | 1 | 15 | 2 | 0 | 8 | 3 |
| P13 post-HP | 50 | 0 | 6 | 6 | 9 | 6 | 3 |
| P14 pre-HP | 14 | 5 | 9 | 1 | 15 | 20 | 16 |
| P14 post-HP | 34 | 1 | 9 | 0 | 15 | 8 | 13 |
| P15 pre-HP | 18 | 1 | 5 | 0 | 2 | 52 | 2 |
| P15 post-HP | 19 | 0 | 5 | 0 | 3 | 53 | 0 |
| P16 pre-HP | 51 | 3 | 9 | 3 | 0 | 12 | 2 |
| P16 post-HP | 47 | 3 | 14 | 1 | 6 | 7 | 2 |
| P17 pre-HP | 22 | 0 | 0 | 0 | 1 | 56 | 1 |
| P17 post-HP | 19 | 0 | 9 | 0 | 4 | 48 | 0 |
| P18 pre-HP | 9 | 0 | 7 | 0 | 60 | 1 | 3 |
| P18 post-HP | 13 | 0 | 6 | 0 | 43 | 6 | 12 |
| P19 pre-HP | 3 | 0 | 7 | 0 | 10 | 48 | 12 |
| P19 post-HP | 5 | 1 | 9 | 0 | 3 | 53 | 9 |
| P20 pre-HP | 13 | 1 | 1 | 1 | 3 | 29 | 32 |
| P20 post-HP | 17 | 4 | 1 | 0 | 6 | 39 | 13 |
| P21 pre-HP | 14 | 0 | 9 | 0 | 5 | 48 | 4 |
| P21 post-HP | 2 | 0 | 3 | 0 | 1 | 73 | 1 |
Note. HP = home practice.
Discussion
In a pre–post group study of HP outcomes, a 6-month unsupervised HP program with weekly teletherapy support was studied in 21 individuals with chronic aphasia. HP consisted of multimodal practice recognizing, matching, and naming pictures of actions and objects, half of which had been recently treated during an intensive 2-week language therapy program. Tablet-based exercises were created to provide semantic, phonemic, and orthographic visual and auditory cues using words, pictures, and videos that aimed to facilitate spreading activation for practiced items, thus taking advantage of use-dependent neuroplasticity. Picture-naming performance during HP, immediately post-HP, and at follow-up testing 4 months post-HP was compared to performance pre-HP.
HP Supports Maintenance of Posttreatment Language Gains
Clinicians and PWAs are painfully aware that treatment gains in aphasia can be fleeting. Many studies do not provide follow-up testing, and when they do, it is not surprising to see that improvements are generally not as durable as one would hope, particularly the longer the follow-up period with no intervening therapy. It has been suggested that learning beyond criterion or “overlearning” contributes to maintenance of newly acquired skills in neurotypical adults (Monfils, Plautz, & Kleim, 2005). Likewise, extended practice may be responsible for the maintenance of treatment effects in aphasia (Kurland et al., 2008; McNeil et al., 1998; Wambaugh, Martinez, McNeil, & Rogers, 1999).
Our first research question thus focused on whether HP would maintain and/or enhance gains that were made in picture naming during the prior 2-week intensive treatment period, that is, would HP maintain and improve naming of recently treated (TR) pictures. It was expected that treated and practiced (TR/PR) pictures would be the most resistant to posttreatment decay. Indeed, this effect was robust, that is, all groups, regardless of severity, made gains in naming TR/PR pictures during the 6-month HP phase. Only in the mild/mod group were the TR/PR gains observed to be long lasting and estimated to exceed improvements observed immediately posttreatment. In the groups with mod/sev and severe aphasia, it was estimated to return to lower than posttreatment levels, although treatment gains from the prior treatment period were not entirely vulnerable to decay. In summary, although practice could not be said to “make perfect,” it did provide a level of protection from the deterioration in performance typically observed in the weeks and months following the end of aphasia treatment, more so for persons with mild/mod aphasia.
Independent Unsupervised Practice Also Improves Naming of Untreated Pictures
Our second research question investigated whether PWAs could use the HP program to improve naming accuracy on previously UNTR pictures. Given the recent, albeit scant, literature demonstrating positive effects of unsupervised tablet-based home therapy (e.g., Kurland et al., 2014; Lavoie et al., 2016), we hypothesized positive outcomes on the UNTR/PR pictures. As expected, regardless of severity, HP had a robust positive effect on UNTR/PR pictures across participants. A main effect for phase demonstrated that, regardless of prior TR condition, PWAs improved during the HP phase.
Although participants performed significantly worse on UNTR than TR pictures following the 2-week intensive treatment that preceded the HP phase, UNTR/PR pictures were estimated to improve sharply during HP, regardless of severity. In participants with mild/mod and severe aphasia, the estimated gains in naming UNTR/PR pictures was on a par with that of TR pictures posttreatment. The positive effect of unsupervised practice on UNTR/PR pictures was maintained at 4 months post-HP across participants, regardless of severity, at levels higher than pre-HP. Thus, the typical vulnerability to decay that was observed in persons with mod/sev and severe aphasia when they ceased practicing TR/PR pictures was less pronounced in the UNTR/PR condition.
Who Benefits From HP With Teletherapy?
Our third research question aimed to gain a better understanding of variables contributing to successful independent use of the HP program in most, but not all, participants. We predicted that severity would have a deleterious effect on maintaining treatment effects and on new learning. We also sought to examine the relationships that might exist between prior experience, need for extended training with a smart device, degree of practice compliance, and ultimate independence and successful use of the device during HP.
As expected and perhaps unsurprisingly, aphasia severity influenced outcomes and interacted significantly with other variables. Whereas the model estimated significant improvements in all participants regardless of severity, the estimated change in the difference in proportion of accurately produced TR/PR versus TR/UNPR pictures from pre-HP to the HP phase was higher for individuals with mild/mod (15%) and mod/sev (17%) than severe aphasia (11%). Following the 6-month HP program, the estimated change was no longer significant in mod/sev (6%) and severe groups (7%), whereas it remained significantly different in the participants with mild/mod aphasia (12%). By 4 months post-HP, however, the estimated change was no longer significant in any group, although the model still estimated positive differences between practiced and unpracticed TR picture naming for those with mild/mod (8%), mod/sev (8%), and severe aphasia (2%).
With regard to our second question, whether PWAs could use the HP program to improve naming accuracy on previously untreated pictures, aphasia severity again influenced the outcomes. Only those with mild/mod and mod/sev aphasia showed significantly improved naming on UNTR pictures from pre-HP to HP (24% and 21%, respectively). Following the HP phase, the estimated percent improvements dropped but remained significant in these two groups (14% and 16%, respectively). By 4 months post-HP, only the participants with mild/mod aphasia maintained significant gains on UNTR pictures (10%).
Other factors influencing outcomes included participant familiarity with smart devices and how long it took to train them for the HP program. Prior to the HP phase, all but three of the participants had no prior experience using an iPad or other tablet device. Of these 18 novices to smart technology, nine had low and five had no prior experience even using a PC or Mac computer. Given the generally low prior exposure to computers and smart devices, it is not surprising that it took on average two to three sessions to train basic iBooks/iPad proficiency and two to three sessions to train basic proficiency to connect to and use the weekly video teleconferencing app (GTM). The number of required training sessions correlated negatively with change scores on PR and UNPR picture naming.
One caveat is a relationship between training and aphasia severity. Coincidentally, all of the participants with smart tablet experience and most (4/5) with a high level of PC or Mac prestroke experience were in the mild/mod severity group. Also, three participants with no prior tablet exposure and low or no prior PC or Mac experience never attained independence with the GTM app, and two of them never achieved independent use of the iBooks app. These three were in the severe aphasia group, and the failure to achieve independence was likely not coincidental but rather related to issues with auditory comprehension, memory, and/or executive function. Their baseline auditory comprehension percentile scores (BDAE; Goodglass et al., 2001) were among the lowest in the study. Likewise, baseline testing placed these three PWAs among the four lowest scoring participants of the study in the memory domain of the Cognitive Linguistic Quick Test (Helm-Estabrooks, 2001). The two who never achieved independence using the app were also among the three lowest scoring participants in the Cognitive Linguistic Quick Test executive function domain. As more and more investigators begin to examine the effects of brain damage associated with aphasia on more general cognitive domains such as attention, memory, and executive function (e.g., Dignam et al., 2017; Heuer, Ivanova, & Hallowell, 2017; Minkina, Rosenberg, Kalinyak-Fliszar, & Martin, 2017; Sandberg, 2017), a clearer picture may emerge regarding the limits and potential for independent use of smart technology in aphasia rehabilitation.
We also examined the influence of practice compliance on HP outcomes. Self-reported practice compliance, that is, percentage of weeks in which participants reported having practiced at least 20 min a day for 5 days in the prior week, correlated positively with changes in post-HP picture naming. The correlation was, as expected, stronger for PR than UNPR pictures. In the case of practice compliance, there did not seem to be a confound with severity. Although two of the persons with severe aphasia were among the least compliant (54% and 56%), one person with mod/sev and two persons with mild/mod aphasia also reported low compliance (17%–60%).
In a preliminary study of the first five participants to complete the HP program, we observed that motivation to use the technology and adequate training were more important factors than age, aphasia type or severity, or prior experience with computers (Kurland et al., 2014). This observation mostly stands with the larger cohort, although the current study found severity to interact negatively with almost all other variables, including treatment phase and treatment and practice condition of pictures. This is not to suggest, however, that PWAs in the severe group did not benefit from or experience satisfaction with the HP program. Quite the contrary and despite only modest gains in naming, satisfaction was very high in three of the four persons with severe aphasia, all of whom subsequently purchased iPads and continue to seek out aphasia-friendly apps for HP.
Comparison With Other Studies
There are not a lot of studies in the literature with which to compare, apples-to-apples, the results of our HP program with weekly telepractice check-in. Examination of the effectiveness of telepractice, whether for testing, treating, or maintaining skills in aphasia, is still in a nascent stage. Most studies do share a promising outlook for the future of telepractice, and in this regard, the current study is in agreement. We did not utilize telepractice for treatment, per se, but rather as a tool for checking in and obtaining feedback on participants' independent progress, verifying practice compliance, and encouraging them to continue practicing. Although we did not test the question of whether this weekly remote check-in was valuable or even necessary, our clinical intuition suggested that it was in fact quite important to the participants.
This is a question that should be addressed in future research. The owners/developers of Constant Therapy, the “go to” tablet-based app many clinicians recommend on discharging their patients, for example, have the means to test this empirical question and hopefully will do so in the future. Their findings comparing traditional in-clinic therapy with remote unsupervised therapy with a weekly visit to the clinic found HP to be effective (Des Roches et al., 2015). It remains to be seen, however, how effective it is when participants are not also treated once a week face-to-face in the clinic.
Although there is still a limited literature on tablet-based HP, with or without remote or onsite clinical monitoring or supervision, the current study adds to a small but growing set of investigations that generally agree on a promising future for this technology in neurorehabilitation. Studies over the last few years all suggest that HP is feasible and, quite often, effective. In their recent systematic review of the effectiveness of aphasia treatments delivered via technology, Lavoie and colleagues found 23 studies, including three using smart tablets (Lavoie, Macoir, & Bier, 2017). They concluded that technology is an efficient approach in treatment of poststroke anomia.
There is little doubt of the enormous potential of mobile health technology. The convenience afforded by enabling PWAs to practice when and where they choose, without having to travel to a clinic, may represent a paradigm shift in accessibility to therapeutic services in chronic aphasia. Future studies should address how effective aphasia apps are in the absence of supervision, a scenario that is likely to become more and more common as rising costs of health care collide with shrinking availability of affordable insurance for many stroke survivors.
Limitations of the iPad/iBooks App
A few characteristics of the iBooks app had a limiting effect on our ability to monitor participant progress and collect data regarding participant accuracy, reaction time, and so forth. Thus, unlike some of the recently developed asynchronous telerehabilitation platforms (e.g., Choi et al., 2016; Des Roches et al., 2015; Hill & Breslin, 2016), the practice books created in iBooks Author did not allow for intrinsic remote monitoring of progress or updating of task difficulty as participants improved. The iBooks were easy to assemble and individually tailored to participants' lists of treated and untreated pictures and, importantly for our participants with moderate to severe aphasia, easy to learn how to use. However, one result of the “static” nature of the tasks was that some participants ultimately got bored with practicing. Also, not having the ability to automatically track participant usage meant that we had to rely on self-report of practice compliance. Even though all participants were capable of copying the numbers off of the stopwatch app, they did not always reliably turn the stopwatch on and off. Future studies of the benefits of HP should take advantage of technological advances in mobile health technology to include the latest software in speech recognition and a web-based platform that can allow for remote monitoring, video/audio collection of speech samples, reaction time, practice time, and remote adjustment of task difficulty.
Study Limitations
In addition to intrinsic limitations of the HP app, the study design could be improved. A recurring comment from participants, particularly those who grew bored of the tasks, was that the HP phase was too long. Examination of longitudinal graphs of individual progress suggests that 3 months may have sufficed for many participants. As noted above, the programs were “static,” and this contributed to some participants' boredom and low practice compliance. Future studies, in addition to shortening the practice period, should build in means for expanding the tasks to include more functional and naturalistic applications. This could be achieved most efficiently during teletherapy sessions.
The current study was part of a clinical trial examining the benefits of HP with weekly telepractice check-in to maintain and augment treatment gains during a prior 2-week intensive language treatment program. As such, we were obliged to deliver, to the extent possible, the same treatment to all participants, regardless of aphasia severity and/or comorbid AOS. This limitation effectively prevented us from taking full advantage of the iPad-based home HP program to specifically target AOS in aphasic participants, half of whom presented with AOS. Moreover, given the collinearity of aphasia severity and presence/severity of AOS in the current sample, it was not possible to tease out the influence of AOS on treatment outcomes. Future studies should be carefully designed to tease out the effects of severity of aphasia and AOS. Moreover, tablet-based HP programs have the advantage of enabling PWAs to practice intensively, with correct video/audio models, whenever and wherever they choose. The jury is still out on the influence of practice intensity or schedules of practice, feedback frequency, timing, and other variables that comprise principles of motor learning from nonspeech motor skills and how they translate to rehabilitation of AOS (Maas et al., 2008). Nonetheless, tablet-based HP programs have enormous potential to empirically address these questions and close the gap in developing effective treatment techniques for what has been referred to as a “difficult treatment problem” (Davis, Farias, & Baynes, 2009).
Another limitation is that the study lacked a means for assessing the effect of the weekly telepractice check-ins. As noted, most participants reported satisfaction with the HP phase. On the other hand, it was not necessary to ask them about the weekly telepractice meetings, which they always seemed excited about. With a few exceptions, the track record for showing up, on time, for these meetings was remarkably good. Given these participants' overwhelmingly abysmal prior experience with smart technology, this fact was, itself, a statement of their satisfaction with the weekly videoconference meetings. Future studies should attempt to measure the necessity and/or sufficiency of the telepractice aspect, as well as expand on the functionality of the telepractice sessions to include, for example, inclusion of target words in naturalistic conversation and other tasks that could potentially promote carryover of treatment gains to functional communication.
Separate studies should also investigate the many potential intrinsic benefits available via iPad-based rehabilitation. Van de Sandt-Koenderman (2011) observed that technological approaches to aphasia rehabilitation tend to favor either a disorder-oriented approach or a functional treatment approach. Whereas computer-assisted aphasia treatment programs have largely focused on restoring linguistic skills and AAC devices have focused on compensating for linguistic deficits, tablet-based apps have the potential to include but also surpass impairment-based treatment approaches. Indeed, part of the profound promise of iPad or other tablet-based home therapy is that so many apps could potentially contribute toward participation-oriented approaches to aphasia rehabilitation. Portable access to the Internet lends itself toward social networking. Harnessing this technology in the hands of people with aphasia, who could potentially take advantage of many built-in features such as text-to-speech and other accessibility settings, has enormous potential to aid in overcoming the social isolation often experienced in poststroke aphasia. Separate controlled studies of the benefits of including online group meetings, e-mail or text assignments, or other social networking tools should be explored.
A final limitation of the study involves a common complaint in aphasia research, that is, that existing instruments for capturing functional changes that result from therapy do not always reflect the same degree of positive change observed in primary outcome measures. Evidence from the UNTR/UNPR pictures suggests that, for most participants, the gains did not generalize beyond the treated and practiced sets. Analysis of post-HP secondary outcomes also suggested minimal change, on average, in measures of auditory comprehension, sentence repetition, and word retrieval in discourse, although there were demonstrations of individual variability that included some PWAs making impressive gains in some or all of these measures. Moreover, some of the changes in the primary outcome measure were small, particularly in persons with severe aphasia and AOS.
Nonetheless, some of the most satisfying results were obtained in anecdotal evidence, mostly provided by significant others, sometimes accompanying functional outcomes questionnaires, sometimes unsolicited. Examples include the following: “…at our last doctor's visit, she specifically commented on how much [his] speech has improved” (wife of P6); [he] seemed to really enjoy the experience…when I'm not around he is starting to initiate conversations and make himself understood” (wife of P10); “…[he] is definitely talking better. He puts more words together” (wife of P13); “…Home program helped her—hard in beginning, wonderful at end—she looked forward to it every day” (husband of P16); “…we have noticed a huge change in not only [his] speech, but in his self-confidence as well” (wife of P17); “…his daughter told me that she can understand his speech on the phone much better than even a few months ago” (significant other of P20); “…[he] has gained confidence in his speech with people outside of the family” (wife of P21). These and so many other comments, though difficult to quantify, nonetheless attest to the beneficial effects of the HP program, regardless of aphasia severity.
Can “Practice Make Perfect” in Aphasia Home Therapy?
The notion that more practice would obtain better outcomes gets to the core of the “more is better” argument for HP in aphasia. In neurotypical adults, there is an extensive literature examining the neurobiology of memory, learning, and priming that would suggest, at least in the realm of motor, visuomotor, and visuospatial tasks, that practice does in fact lead to neuroplastic changes that manifest behaviorally in higher accuracy and faster reaction times (e.g., Karni et al., 1995; Poldrack, Desmond, Glover, & Gabrieli, 1998; Sakai et al., 1998). Although studies of the effects of practice on language tasks are less common, researchers have demonstrated similar brain–behavior changes both at the item and task level after brief practice on tasks such as verb generation (Raichle et al., 1994) and, more recently, picture naming (Basso et al., 2013; Kurland, Liu, & Stokes, 2018 ; MacDonald et al., 2015).
Whether and to what extent we can expect unsupervised HP in aphasia to take advantage of the same or similar mechanisms underlying functional reorganization in neurotypical adults is as yet unknown. “Practice makes perfect” is an imperfect truism, even without consideration of learning in the environment of a damaged brain. A more fitting maxim in the setting of poststroke aphasia may be “practice makes better.” Certainly, it is clear from the observed and estimated results that during the HP phase, in particular, the practiced items were named more accurately. The evidence is also irrefutable that ceasing practice over a period of months, both at the level of particular items and more generally the task, is deleterious to maintaining progress naming objects and actions in aphasia. Unfortunately, this vulnerability to decay is even more pronounced as a function of aphasia severity.
This pattern of diminishing returns over time has prompted some to suggest a “use it or lose it” kind of learning mechanism in aphasia. Framing it in a more positive light, neurorehabilitation seeks to “overcome learned nonuse” (Berthier & Pulvermuller, 2011; Taub et al., 1994). Although we may think of learned nonuse as manifesting on a behavioral level, there is also evidence to suggest that it begins at a cellular level, that is, effortful learning has been shown to save new neurons created during adult hippocampal neurogenesis from dying (Shors, Anderson, Curlik, & Nokia, 2012). In persons who have already suffered from cerebrovascular necrotic cell death, it is fitting that HP might contribute to the prevention of apoptotic cell death in adult persistent neurogenesis.
Acknowledgments
This work was supported by funding from the National Institute on Deafness and Other Communication Disorders of the National Institutes of Health (Grant R01DC011526 to Jacquie Kurland). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to thank Kylee Osowski, Alisson Reber, Kristen Stem, and Abigail Wilkins for their assistance in creating the iBooks, Mary Andrianopoulos for her evaluation of AOS, Nicole Kurland for her assistance with graphics, and the individuals with aphasia and their families for participating in this study.
Funding Statement
This work was supported by funding from the National Institute on Deafness and Other Communication Disorders of the National Institutes of Health (Grant R01DC011526 to Jacquie Kurland).
References
- Baron C., Hatfield B., & Georgeadis A. (2005). Management of communication disorders using family member input, group treatment, and telerehabilitation. Topics in Stroke Rehabilitation, 12(2), 49–56. [DOI] [PubMed] [Google Scholar]
- Basso A., & Caporali A. (2001). Aphasia therapy or the importance of being earnest. Aphasiology, 15(4), 307–332. [Google Scholar]
- Basso G., Magon S., Reggiani F., Capasso R., Monittola G., Yang F. J., & Miceli G. (2013). Distinguishable neurofunctional effects of task practice and item practice in picture naming: A BOLD fMRI study in healthy subjects. Brain and Language, 126(3), 302–313. [DOI] [PubMed] [Google Scholar]
- Berthier M. L., & Pulvermuller F. (2011). Neuroscience insights improve neurorehabilitation of poststroke aphasia. Nature Reviews Neurology, 7, 86–97. [DOI] [PubMed] [Google Scholar]
- Bhogal S. K., Teasell R., & Speechley M. (2003). Intensity of aphasia therapy, impact on recovery. Stroke, 34(4), 987–993. [DOI] [PubMed] [Google Scholar]
- Brady A. (2007). Moving toward the future: Providing speech-language pathology services via telehealth. Home Healthcare Nurse, 25(4), 240–244. [DOI] [PubMed] [Google Scholar]
- Brady M. C., Kelly H., Godwin J., Enderby P., & Campbell P. (2016). Speech and language therapy for aphasia following stroke. Cochrane Database of Systematic Reviews, 1469–1493. https://doi.org/10.1002/14651858.CD000425.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan D., Georgeadis A., & Baron C. (2002). Telerehabilitation tools for the provision of remote speech-language treatment. Topics in Stroke Rehabilitation, 8(4), 71–78. [DOI] [PubMed] [Google Scholar]
- Cherney L. R., Patterson J. P., Raymer A. M., Frymark T., & Schooling T. (2010, October). Updated evidence-based systematic review: Effects of intensity of treatment and constraint-induced language therapy for individuals with stroke-induced aphasia. ASHA's National Center for Evidence-Based Practice in Communication Disorders, October 2010. [DOI] [PubMed] [Google Scholar]
- Choi Y. H., Park H. K., & Paik N. J. (2016). A telerehabilitation approach for chronic aphasia following stroke. Telemedicine Journal and e-Health, 22(5), 434–440. [DOI] [PubMed] [Google Scholar]
- Dabul B. (2000). Apraxia Battery for Adults–Second Edition (ABA-2). Austin, TX: PRO-ED. [Google Scholar]
- Darley F. L., Aronson A. E., & Brown J. R. (1975). Motor speech disorders (3rd ed.). Philadelphia, PA: Saunders. [Google Scholar]
- Davis A., & Wilcox M. (1985). Adult aphasia rehabilitation: Applied pragmatics. San Diego, CA: Singular. [Google Scholar]
- Davis C., Farias D., & Baynes K. (2009). Implicit phoneme manipulation for the treatment of apraxia of speech and co-occurring aphasia. Aphasiology, 23, 503–528. [Google Scholar]
- Dechene L., Tousignant M., Boissy P., Macoir J., Heroux S., Hamel M., … Pagé C. (2011). Simulated in-home teletreatment for anomia. International Journal of Telerehabilitation, 3(2), 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Roches C. A., Balachandran I., Ascenso E. M., Tripodis Y., & Kiran S. (2015). Effectiveness of an impairment-based individualized rehabilitation program using an iPad-based software platform. Frontiers in Human Neuroscience, 8, 1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dignam J., Copland D., McKinnon E., Burfein P., O'Brien K., Farrell A., & Rodriguez A. D. (2015). Intensive versus distributed aphasia therapy: A nonrandomized, parallel-group, dosage-controlled study. Stroke, 46, 2206–2211. [DOI] [PubMed] [Google Scholar]
- Dignam J., Copland D., O'Brien K., Burfein P., Khan A., & Rodriguez A. D. (2017). Influence of cognitive ability on therapy outcomes for anomia in adults with chronic poststroke aphasia. Journal of Speech, Language, and Hearing Research, 60(2), 406–421. [DOI] [PubMed] [Google Scholar]
- Duffy J. R. (2012). Motor speech disorders, substrates, differential diagnosis, and management (3rd ed.). St. Louis, MO: Elsevier Mosby. [Google Scholar]
- Fridriksson J., Moser D., Bonilha L., Morrow-Odom K. L., Shaw H., Fridriksson A., … Rorden C. (2007). Neural correlates of phonological and semantic-based anomia treatment in aphasia. Neuropsychologia, 45(8), 1812–1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg S., Haley K. L., & Jacks A. (2012). Script training and generalization for people with aphasia. American Journal of Speech-Language Pathology, 21(3), 222–238. [DOI] [PubMed] [Google Scholar]
- Goodglass H., Kaplan E., & Barresi B. (2001). The assessment of aphasia and related disorders (3rd ed.). Austin, TX: Pro-Ed. [Google Scholar]
- Hall N., Boisvert M., & Steele R. (2013). Telepractice in the assessment and treatment of individuals with aphasia: A systematic review. International Journal of Telerehabilitation, 5(1), 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnish S. M., Morgan J., Lundine J. P., Bauer A., Singletary F., Benjamin M. L., … Crosson B. (2014). Dosing of a cued picture-naming treatment for anomia. American Journal of Speech-Language Pathology, 23(2), S285–S299. [DOI] [PubMed] [Google Scholar]
- Helm-Estabrooks N. (2001). Cognitive Linguistic Quick Test. San Antonio, TX: Pearson. [Google Scholar]
- Heuer S., Ivanova M. V., & Hallowell B. (2017). More than the verbal stimulus matters: Visual attention in language assessment for people with aphasia using multiple-choice image displays. Journal of Speech, Language, and Hearing Research, 60(5), 1348–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill A. J., & Breslin H. M. (2016). Refining an asynchronous telerehabilitation platform for speech-language pathology: Engaging end-users in the process. Frontiers in Human Neuroscience, 10, 640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan E., Goodglass H., & Weintraub S. (2001). Boston Naming Test–Second Edition. Philadelphia, PA: Lea & Febiger. [Google Scholar]
- Karni A., Meyer G., Jezzard P., Adams M. M., Turner R., & Ungerleider L. G. (1995). Functional MRI evidence for adult motor cortex plasticity during motor skill learning. Nature, 377(6545), 155–158. [DOI] [PubMed] [Google Scholar]
- Kertesz A. (2006). Western Aphasia Battery–Revised. San Antonio, TX: Pearson. [Google Scholar]
- Kiran S., Des Roches C., Balachandran I., & Ascenso E. (2014). Development of an impairment-based individualized treatment workflow using an iPad-based software platform. Seminars in Speech and Language, 35(1), 38–50. [DOI] [PubMed] [Google Scholar]
- Kirmess M., & Maher L. M. (2010). Constraint induced language therapy in early aphasia rehabilitation. Aphasiology, 24(6–8), 725–736. [Google Scholar]
- Kleim J. A., & Jones T. A. (2008). Principles of experience-dependent neural plasticity: Implications for rehabilitation after brain damage. Journal of Speech, Language, and Hearing Research, 51, S225–S239. [DOI] [PubMed] [Google Scholar]
- Kurland J. (2014). iRehab in aphasia treatment. Seminars in Speech and Language, 35, 3–4. [DOI] [PubMed] [Google Scholar]
- Kurland J., Cortes C. R., Wilke M., Sperling A. J., Lott S., Tagamets M. A., … Friedman R. B. (2008). Neural mechanisms underlying learning and maintenance of learning following semantic mediation treatment in a case of phonologic alexia. Brain Imaging and Behavior, 2, 147–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurland J., Liu A., & Stokes P. (2018). Practice effects in healthy older adults: Implications for treatment-induced neuroplasticity in aphasia. Neuropsychologia, 109, 116–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurland J., Pulvermüller F., Silva N., Burke K., & Andrianopoulos M. (2012). Constrained versus unconstrained intensive language therapy in two individuals with chronic, moderate-to-severe aphasia and apraxia of speech: Behavioral and fMRI outcomes. American Journal of Speech-Language Pathology, 21(2), S65–S87. [DOI] [PubMed] [Google Scholar]
- Kurland J., Stanek E. J. III, Stokes P., Li M., & Andrianopoulos M. (2016). Intensive language action therapy in chronic aphasia: A randomized clinical trial examining guidance by constraint. American Journal of Speech-Language Pathology, 25(4S), S798–S812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurland J., Wilkins A. R., & Stokes P. (2014). iPractice: Piloting the effectiveness of a tablet-based home practice program in aphasia treatment. Seminars in Speech and Language, 35, 51–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis J. R., & Koch G. G (1977). The measurement of observer agreement for categorical data. Biometrics, 33, 159–174. [PubMed] [Google Scholar]
- Lavoie M., Macoir J., & Bier N. (2017). Effectiveness of technologies in the treatment of post-stroke anomia: A systematic review. Journal of Communication Disorders, 65, 43–53. [DOI] [PubMed] [Google Scholar]
- Lavoie M., Routhier S., Legare A., & Macoir J. (2016). Treatment of verb anomia in aphasia: Efficacy of self-administered therapy using a smart tablet. Neurocase, 22(1), 109–118. [DOI] [PubMed] [Google Scholar]
- Maas E., Robin D. A., Ausermann Hula S. N., Wulf G., Ballard K. J., & Schmidt R. A. (2008). Principles of motor learning in treatment of motor speech disorders. American Journal of Speech-Language Pathology, 17, 277–298. [DOI] [PubMed] [Google Scholar]
- MacDonald A. D., Heath S., McMahon K. L., Nickels L., Angwin A. J., van Hees S., … Copland D. A. (2015). Neuroimaging the short- and long-term effects of repeated picture naming in healthy older adults. Neuropsychologia, 75, 170–178. [DOI] [PubMed] [Google Scholar]
- Macoir J., Martel Sauvageau V., Boissy P., Tousignant M., & Tousignant M. (2017). In-home synchronous telespeech therapy to improve functional communication in chronic poststroke aphasia: Results from a quasi-experimental study. Telemedicine Journal and e-Health, 23(8), 630–639. [DOI] [PubMed] [Google Scholar]
- Mashima P. A., & Doarn C. R. (2008). Overview of telehealth activities in speech-language pathology. Telemedicine Journal and e-Health, 14(10), 1101–1117. [DOI] [PubMed] [Google Scholar]
- Masterson J., & Druks J. (1998). Description of a set of 164 nouns and 102 verbs matched for printed word frequency, familiarity and age-of-acquisition. Journal of Neurolinguistics, 11(4), 331–354. [Google Scholar]
- McGrath N., Dowds M. M. Jr., & Goldstein R. (2008). Clinical supervision of a client with traumatic brain injury in a host home placement using video teleconferencing: A case study. The Journal of Head Trauma Rehabilitation, 23(6), 388–393. [DOI] [PubMed] [Google Scholar]
- McNeil M. R., Doyle P. J., Spencer K., Goda J., Flores D., & Small S. L. (1998). Effects of training multiple form classes on acquisition, generalization, and maintenance of word retrieval in a single subject. Aphasiology, 12, 57–585. [Google Scholar]
- McNeil M. R., Robin D. A., & Schmidt R. A. (2009). Apraxia of speech: Definition and differential diagnosis. In McNeil M. R. (Ed.), Clinical management of sensorimotor speech disorders (2nd ed., pp. 331–354). New York, NY: Thieme. [Google Scholar]
- Middleton E. L., Schwartz M. F., Rawson K. A., Traut H., & Verkuilen J. (2016). Towards a theory of learning for naming rehabilitation: Retrieval practice and spacing effects. Journal of Speech, Language, and Hearing Research, 59, 1111–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkina I., Rosenberg S., Kalinyak-Fliszar M., & Martin N. (2017). Short-term memory and aphasia: From theory to treatment. Seminars in Speech and Language, 38(1), 17–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monfils M. H., Plautz E. J., & Kleim J. A. (2005). In search of the motor engram: Motor map plasticity as a mechanism for encoding motor experience. The Neuroscientist, 11, 471–483. [DOI] [PubMed] [Google Scholar]
- Oldfield R. C. (1971). The assessment and analysis of handedness: The Edinburgh Inventory. Neuropsychologia, 9(1), 97–113. [DOI] [PubMed] [Google Scholar]
- Poldrack R. A., Desmond J. E., Glover G. H., & Gabrieli J. D. (1998). The neural basis of visual skill learning: An fMRI study of mirror reading. Cerebral Cortex, 8(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Pulvermüller F., & Berthier M. L. (2008). Aphasia therapy on a neuroscience basis. Aphasiology, 22(6), 563–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulvermüller F., Neininger B., Elbert T., Mohr B., Rockstroh B., Koebbel P., & Taub E. (2001). Constraint-induced therapy of chronic aphasia after stroke. Stroke, 32(7), 1621–1626. [DOI] [PubMed] [Google Scholar]
- Raichle M. E., Fiez J. A., Videen T. O., MacLeod A. M., Pardo J. V., Fox P. T., & Petersen S. E. (1994). Practice-related changes in human brain functional anatomy during non-motor learning. Cerebral Cortex, 4(1), 8–26. [DOI] [PubMed] [Google Scholar]
- Rende B., & Ramsberger G. (2011). Telepractice experiences in a university training clinic. Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders, 21, 120–129. [Google Scholar]
- Routhier S., Bier N., & Macoir J. (2016). Smart tablet for smart self-administered treatment of verbal anomia: Two single case studies in aphasia. Aphasiology, 30(2–3), 269–289. [Google Scholar]
- Sakai K., Hikosaka O., Miyauchi S., Takino R., Sasaki Y., & Putz B. (1998). Transition of brain activation from frontal to parietal areas in visuomotor sequence learning. The Journal of Neuroscience, 18(5), 1827–1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg C. W. (2017). Hypo-connectivity of resting-state networks in persons with aphasia compared with healthy age-matched adults. Frontiers in Human Neuroscience, 11, 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shors T. J., Anderson M. L., Curlik D. M., & Nokia M. S. (2012). Use it or lose it: How neurogenesis keeps the brain fit for learning. Behavioural Brain Research, 227(2), 450–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sickert A., Anders L. C., Munte T. F., & Sailer M. (2014). Constraint-induced aphasia therapy following sub-acute stroke: A single-blind, randomised clinical trial of a modified therapy schedule. Journal of Neurology, Neurosurgery, and Psychiatry, 85(1), 51–55. [DOI] [PubMed] [Google Scholar]
- Simic T., Leonard C., Laird L., Cupit J., Hobler F., & Rochon E. (2016). A usability study of Internet-based therapy for naming deficits in aphasia. American Journal of Speech-Language Pathology, 25(4), 642–653. [DOI] [PubMed] [Google Scholar]
- Snodgrass J. G., & Vanderwart M. (1980). A standardized set of 260 pictures: Norms for name agreement, image agreement, familiarity, and visual complexity. Journal of Experimental Psychology: Human Learning and Memory, 6(2), 174–215. [DOI] [PubMed] [Google Scholar]
- Taub E., Crago J. E., Burdio L. D., Groomes T. E., Cook E. W. III, DeLuca S. C., & Miller N. E. (1994). An operant approach to rehabilitation medicine: Overcoming learned nonuse by shaping. Journal of the Experimental Analysis of Behavior, 61, 281–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Sandt-Koenderman W. M. E. (2011). Aphasia rehabilitation and the role of computer technology: Can we keep up with modern times? International Journal of Speech-Language Pathology, 13, 21–27. [DOI] [PubMed] [Google Scholar]
- Wambaugh J. L. (2006). Treatment guidelines for apraxia of speech: Lessons for future research. Journal of Medical Speech-Language Pathology, 14, 317. [Google Scholar]
- Wambaugh J. L., Martinez A. L., McNeil M. R., & Rogers M. A. (1999). Sound production treatment for apraxia of speech: Overgeneralization and maintenance effects. Aphasiology, 13, 821–837. [Google Scholar]
- Woolf C., Caute A., Haigh Z., Galliers J., Wilson S., Kessie A., … Marshall J. (2016). A comparison of remote therapy, face to face therapy and an attention control intervention for people with aphasia: A quasi-randomised controlled feasibility study. Clinical Rehabilitation, 30(4), 359–373. [DOI] [PubMed] [Google Scholar]