Abstract
STUDY QUESTION
What are the long-term effects of fertility education on knowledge and reproductive outcome?
SUMMARY ANSWER
Participants in the intervention group retained some knowledge after 2 years and the partnered women had a new child more quickly than the comparison group.
WHAT IS KNOWN ALREADY
Fertility education improves knowledge, at least in the short-term. Attitudes toward childbearing and its timing can change after exposure to educational materials.
STUDY DESIGN, SIZE, DURATION
Participants were recruited via an online social research panel. In the original randomized controlled trial (RCT), knowledge of reproductive-aged participants was assessed before (T1) and immediately after (T2) receiving one of three information brochures: fertility (intervention group), healthy pre-pregnancy (focused on intake of folic acid during pregnancy, control group 1), or family policies in Japan (childcare provision, control group 2). The present follow-up study was conducted 2 years later in January 2017 (T3) with the same participants.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Of the T1 participants (n = 1455), 383 men and 360 women (51%) responded to the T3 survey. Fertility knowledge measured with the Japanese version of the Cardiff Fertility Knowledge Scale (CFKS-J) and fertility status (e.g. new births, new medical consultations, and the timing of new birth) was assessed.
MAIN RESULTS AND THE ROLE OF CHANCE
Baseline (T1) characteristics of the T3 participants were well balanced between groups, but T3 participants were older, married, and more educated compared to those lost to follow-up. A repeated-measures analysis of variance showed significant knowledge gains among the intervention group from T1 to T3 (11.2% and 7.0% among men and women, respectively) but no significant change over time for the control groups. There were no differences between groups in the incidence of new births or new medical consultations. However, subgroup analysis showed that timing of new births was accelerated for partnered individuals in the intervention group. Specifically, the proportion of partnered participants at T1 who had a new birth in the first year subsequent to presentation of information was higher in the intervention group versus control group 1 (folic acid): 8.8% versus 1.4% (P = 0.09) among men and 10.6% versus 2.3% (P = 0.03) among women, respectively. The odds ratios (adjusted for age) were 7.8 (95% CI: 0.86–70.7) and 5.2 (95% CI: 1.09–25.0) among men and women, respectively. The timing of births and the proportion of new births during the 2-year follow-up period in the intervention group were similar to that of control group 2 (family policy). The incidence of new medical consultation was higher in the male intervention group (12.0%) than in male control group 2 (family policy, 1.5%, P = 0.04) but similar among women in all groups.
LIMITATIONS REASONS FOR CAUTION
First, the high attrition rate may limit the generalizability of these findings for longer-term acquisition of fertility knowledge, especially when applied to younger people who were more likely to be lost to follow-up. Second, this is a 2-year follow-up study and the results may change in the longer-term. Finally, we relied on self-reported questionnaire data and there is a possibility that some women were unknowingly pregnant at T1 but this risk should be distributed equally in the three groups through randomization.
WIDER IMPLICATIONS OF THE FINDINGS
Effects of one-time education were limited but retained beyond baseline levels. Importantly, education was found to potentially accelerate decision-making about achieving births in partnered subgroups compared to receiving healthy pre-pregnancy information. However, this finding should be confirmed in future stratified RCTs designed to evaluate effects in these subgroups. Follow-up ‘booster’ education sessions might help people retain knowledge and facilitate reproductive decisions for longer. In view of the high attrition rate, especially among young populations, novel educational strategies to retain young people in fertility education cohorts should be explored.
STUDY FUNDING/COMPETING INTEREST(S)
This study was funded by National Center for Child Health and Development, the Daiwa Anglo-Japanese Foundation, Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science. E.M. reports joint research funds from a public interest incorporated foundation ‘1 more Baby Ohendan.’
Keywords: fertility awareness, informed decision-making, delayed childbearing, education, live birth
Introduction
Postponing childbearing is a public health issue for many countries (Lemoine and Ravitsky, 2013; Organisation for Economic Co-operation and Development, 2014). Along with factors such as career, education, relationships and financial security (Mills et al., 2011), overestimation of fertility might contribute in part to delayed parenthood (Bunting and Boivin, 2010). People generally lack accurate knowledge about the duration of the reproductive lifespan, the likelihood of natural conceiving, or the ability of ART to help them conceive (Pedro et al., 2018). Healthcare professionals provide educational initiatives through websites, in the community, at schools and at healthcare facilities to promote informed reproductive decision-making (Daniluk and Koert, 2013; Hammarberg et al., 2017; Hvidman et al., 2015; Boivin et al. 2018).
The few intervention studies available have confirmed knowledge improvement immediately after provision of fertility education (Wojcieszek and Thompson, 2013; Daniluk and Koert, 2015; Maeda et al., 2016; Boivin et al., 2018), however the long-term effects of fertility education remain poorly understood. A 6-month follow-up study after an online education programme among currently childless men and women (Daniluk and Koert, 2015) reported that limited knowledge of fertility items was retained and that beliefs about the ideal timing of parenthood returned to pre-intervention levels. In view of the fact that the reproductive decision-making process generally takes time, long-term effects of education on fertility knowledge and reproductive decision making should be explored.
This paper presents a 2-year follow-up of a randomized controlled trial (RCT), which had shown that fertility education improves fertility-related cognitions (knowledge) but increases negative emotions (anxiety) among reproductive-aged people who want (more) children (Maeda et al., 2016). The primary aim of the present follow-up study was to examine the level of knowledge retained over time. We hypothesized that people in the intervention group would retain knowledge better than those in control groups although the level of knowledge would not be fully sustained (Daniluk and Koert, 2015). As a secondary aim, we explored the effects of education on reproductive behaviour. It was expected that people in the intervention group would be more likely to have a child or seek a medical consultation regarding fertility during the follow-up period. Childbearing in Japan is confined almost exclusively to partnered individuals (very few births occur outside of marriage: 2.3%, Ministry of Health, Labour and Welfare, 2015) and therefore the effect of education was also examined according to partnership status.
Materials and Methods
The original study (Maeda et al., 2016) was an RCT that evaluated the effect of online fertility education on subjective anxiety (primary outcome) compared to typical government-provided information about pregnancy and childbirth. The RCT was registered on 13 January 2015 with UMIN Clinical Trials Registry number 000016168. Participants in the original study (the first patient was enroled on 15 January 2015) were randomly allocated to receive one of three information brochures: fertility education (intervention group), need for intake of folic acid during pregnancy (control group 1), and family policies such as parental benefits or parental leave (control group 2). The secondary outcomes were fertility knowledge and childbearing desires, assessed immediately before (T1) and immediately after (T2) exposure to information in January 2015. Full details of the study are published elsewhere (Maeda et al., 2016).
In January 2017 (T3), participants from the RCT were surveyed to ascertain long-term effects of education on fertility knowledge and reproductive behaviour.
Participants
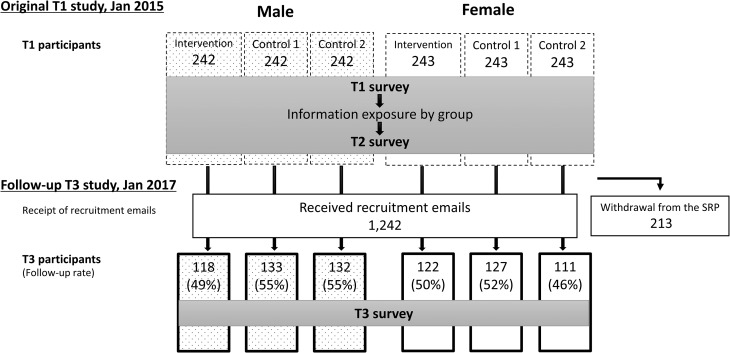
T1 participants (726 men and 729 women) were recruited from an online social research panel obtained via a market research company (Macromill, Tokyo, Japan). At T1, participants were between 20 and 39 years of age and hoping to have (more) children in the future. We excluded from the recruitment pregnant women, men with pregnant partners, and medical and advertising professionals. At T3, all T1 participants, excluding those who withdrew from the social research panel (n = 213), were invited to the T3 survey via an online study link (Fig. 1). Of 1242 people who received recruitment emails, 383 men and 360 women (51% of the T1 sample) responded to the T3 survey. All participants voluntarily agreed to participate in the survey and those who completed the survey were given a coupon worth less than 1 Euro. The ethics committee at Akita University Graduate School of Medicine provided ethical review and approval for the study (no. 1226, October 2014).
Figure 1.
Flow chart of the original randomized controlled trial and follow-up surveys on knowledge and reproductive outcome after online fertility education. Spotted boxes are male participants and clear boxes are female participants. T1, before exposure to an information brochure; T2, immediately after exposure; T3, two years after exposure; SRP, social research panel.
Interventions
Details of the fertility intervention are presented in Maeda et al. (2016). Briefly, the fertility information comprised the definition, prevalence, and causes of infertility, the ages at which female fertility declines, male infertility, fertile period timing and risks for reduce fertility (e.g. sexually transmitted infections, unhealthy weight, smoking and alcohol drinking). The two control brochures were used to control for existing education relevant to reproduction. Control group 1 controlled for information about the intake of folic acid during pregnancy, including effect and appropriate intake (amount, timing). Control group 2 controlled for information about government financial and social support during pregnancy and childbirth. Information was reviewed by reproductive experts and tested for comprehension among a similarly aged cohort.
Measures
The T3 questionnaire consisted of 64 items (four domains) excerpted from the T1 survey. Only those questions relevant to analyses presented in this paper are described here.
Fertility knowledge
T3 participants were asked to complete the Japanese version of the Cardiff Fertility Knowledge Scale (CFKS-J) (Bunting et al., 2013; Maeda et al., 2015). The CFKS-J uses 13 items to measure knowledge about facts, risks and myths of fertility. All items were rated on a three-point scale as true, false, or do not know. A correct answer was assigned one point, and an incorrect or ‘do not know’ answer was assigned zero points. Scores were reported as the percentage of correct answers. Reliability of the CFKS-J was good (internal consistency coefficient α = 0.74), and the scale had a one-factor structure (Maeda et al., 2015).
Marital and fertility status
T3 participants reported their current relationship status (single, having a partner but not married or married), the number of children they had given birth to or fathered, the year of birth of their youngest children, and whether they had sought a medical consultation or treatment regarding fertility (yes/no). We categorized participants as those who had ‘a new birth’ if they reported more children at T3 than at T1 and the birth year of their youngest child was between 2015 and 2017, after the presentation of T1 information. We categorized participants as those who had ‘a new fertility consultation’ if they changed their history of fertility medical consultation from ‘No’ at T1 to ‘Yes’ at T3.
Baseline characteristics
We used T1 information as baseline characteristics, including age, education level, relationship status, fertility status and fertility knowledge score on the CFKS-J.
Statistical analyses
We conducted attrition analyses by gender. To examine the difference between T3 participants and those lost to follow-up, we compared the baseline characteristics at T1. To examine the between-group balance of T3 participants, we compared the response rates and the baseline characteristics between groups. Statistical comparisons were carried out using Student’s t tests, chi-square tests and Wilcoxon-type test for trend according to the type and distribution of the variables.
To determine the knowledge difference between groups and over time (T1, T2 and T3), we performed a mixed factorial between-within (repeated) measures ANOVA using conservative F-tests (Greenhouse–Geisser correction) for the interaction between information group (intervention, control 1, control 2) and time (Time: T1, T2, T3). Simple effects were used as follow-up tests. We computed percentage gain scores for fertility knowledge using the formula: (T2 score-T1 score)/T1 score (T1 → T2 gain score); (T3 score-T2 score)/T2 score (T2 → T3 gain score) and (T3 score-T1 score)/T1 (T1 → T3 gain score). For all, positive and negative gain scores indicated gain and loss (respectively) of fertility knowledge.
To explore differences in reproductive behaviour between groups, we compared marital and fertility status at T3, new births, and new consultations between groups. We conducted subgroup analyses for those who had a partner or a spouse at T1, comparing the incidence of new births and new consultations and the timing of new births (i.e. proportion of those who had a new birth within 12 months, in year 2015) between groups. We used chi-square tests, Fisher’s exact tests, and Wilcoxon-type tests according to the type and distribution of the variables. We conducted logistic regression analyses to assess the relationship between the intervention and the timing of new births, adjusted for age in years.
All analyses were performed using STATA14-MP (StataCorp LP, College Station, TX, USA). A two-sided P-value of < 0.05 was considered statistically significant.
Results
Baseline characteristics and attrition
Supplementary Table SI shows the baseline characteristics of the T3 participants (n = 743) and those lost to follow-up (n = 712). Attrition analyses showed that T3 participants were older, more likely to be married, to have had fertility consultation and [for men only] to be more educated and have had children compared to those lost to follow-up.
There were no significant differences in follow-up rates according to gender or group (Fig. 1). Baseline characteristics (T1) of T3 participants were well balanced between groups except that, among men, the number of children of the intervention group was fewer than that of control group 1 (P = 0.01, Table I), as had been shown in all T1 participants (Maeda et al., 2016).
Table I.
Baseline (T1) characteristics of the T3 participants by group.
| Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 118) | Control 1 (n = 133) | P values | Control 2 (n = 132) | P values | Intervention (n = 122) | Control 1 (n = 127) | P values | Control 2 (n = 111) | P values | |
| Demographics | ||||||||||
| Age in years, mean (SD) | 32.1 (5.2) | 32.1 (5.2) | 0.99a | 32.2 (5.4) | 0.94a | 31.9 (5.0) | 31.0 (5.5) | 0.15a | 31.8 (5.0) | 0.88a |
| University education (n, % yes) | 74 (62.7) | 88 (66.2) | 0.57b | 78 (59.1) | 0.56b | 53 (43.4) | 45 (35.4) | 0.20b | 50 (45.0) | 0.81b |
| Relationship status (n, %) | ||||||||||
| Single | 61 (51.7) | 61 (45.9) | 0.53b | 56 (42.4) | 0.34b | 37 (30.3) | 39 (30.7) | 0.78 b | 35 (31.5) | 0.95b |
| Having partners, not married | 23 (19.5) | 25 (18.8) | 31 (23.5) | 22 (18.0) | 27 (21.3) | 21 (18.9) | ||||
| Married | 34 (28.8) | 47 (35.3) | 45 (34.1) | 63 (51.6) | 61 (48.0) | 55 (49.5) | ||||
| Fertility | ||||||||||
| The number of children (n, %) | ||||||||||
| None | 102 (86.4) | 97 (72.9) | 0.01c | 102 (77.3) | 0.08c | 87 (71.3) | 90 (70.9) | 0.57c | 78 (70.3) | 0.52c |
| One | 12 (10.2) | 25 (18.8) | 22 (16.7) | 30 (24.6) | 27 (21.3) | 24 (21.6) | ||||
| Two or more | 4 (3.4) | 11 (8.3) | 8 (6.1) | 5 (4.1) | 10 (7.9) | 9 (8.1) | ||||
| Prior medical consultation for fertility (n, %) | 7 (5.9) | 11 (8.3) | 0.47b | 9 (6.8) | 0.78b | 16 (13.1) | 17 (13.4) | 0.95b | 13 (11.7) | 0.75b |
P values compare the preceding Control group with the Intervention group (received information brochure on fertility education). Control 1 = received information brochure on healthy pre-pregnancy such as folic acid intake pre-pregnancy. Control 2 = received information brochure on family policy, such as parental benefits or parental leave.
aTwo-tailed t test.
bChi-square test.
cWilcoxon-type test for trend.
T1: time immediately before exposure to information in original RCT in January 2015. At T3, in January 2017, participants from original RCT were surveyed to determine 2-year effects of education on fertility knowledge and reproductive behaviour.
Effect of the intervention on T3 status
Fertility knowledge
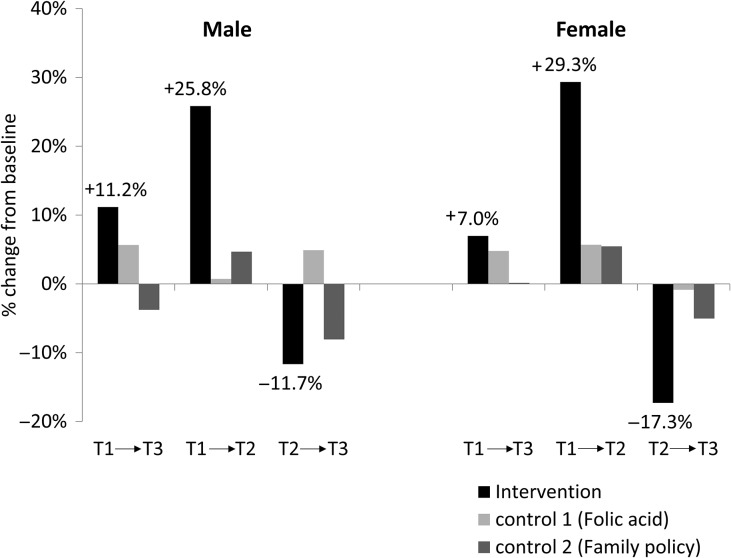
A repeated-measures ANOVA of the percentage of correct scores on the CFKS-J showed a significant interaction between exposure and time, both among men (F(4, 380) = 4.73, P = 0.002) and women (F(4, 357) = 8.87, P < 0.001, Supplementary Fig. S1). Simple effects of time (within-group comparisons) showed that in the intervention group, the T3 score was significantly higher than the T1 score and lower than the T2 score. Among men, significant change across time showed a knowledge gain from T1 to T2 (+25.8%), a knowledge loss from T2 to T3 (−11.7%) with an overall knowledge gain from T1 to T3 of +11.2% (Fig. 2). Among women, the significant change across time showed an average knowledge gain from T1 to T2 (+29.3%), a knowledge loss from T2 to T3 (−17.3%) with an overall average knowledge gain from T1 to T3 of +7.0%. In the control groups, simple effects of time among men or women were not significant, indicating no change over time.
Figure 2.
Percentage change from each baseline score on the Japanese version of the Cardiff Fertility Knowledge Scale by group. T1, before exposure to an information brochure; T2, immediately after exposure; T3, 2 years after exposure.
Marital and fertility status
As shown in Table II, overall the T3 groups did not differ in relationship status, the proportion of those who had sought a medical consultation, or the incidence of new births or new fertility medical consultations. The number of children among men was fewer in the intervention group than in control groups (as per baseline).
Table II.
Marital and fertility status of the T3 participants at T3.
| Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 118) | Control 1 (n = 133) | P values | Control 2 (n = 132) | P values | Intervention (n = 122) | Control 1 (n = 127) | P values | Control 2 (n = 111) | P values | |
| Relationship status (n, %) | ||||||||||
| Single | 51 (43.2) | 60 (45.1) | 0.64a | 57 (43.2) | 0.50a | 34 (27.9) | 31 (24.4) | 0.23a | 36 (32.4) | 0.75a |
| Having partners, not married | 25 (21.2) | 22 (16.5) | 21 (15.9) | 16 (13.1) | 27 (21.3) | 14 (12.6) | ||||
| Married | 42 (35.6) | 51 (38.3) | 54 (40.9) | 72 (59.0) | 69 (54.3) | 61 (55.0) | ||||
| The number of children (n, %) | ||||||||||
| None | 95 (80.5) | 93 (69.9) | 0.04b | 93 (70.5) | 0.07b | 77 (63.1) | 81 (63.8) | 0.90b | 71 (64.0) | 0.74b |
| One | 15 (12.7) | 22 (16.5) | 24 (18.2) | 28 (23.0) | 29 (22.8) | 20 (18.0) | ||||
| Two or more | 8 (6.8) | 18 (13.5) | 15 (11.4) | 17 (13.9) | 17 (13.4) | 20 (18.0) | ||||
| New births (n, %) | 12 (10.2) | 10 (7.5) | 0.46a | 15 (11.4) | 0.76a | 23 (18.9) | 17 (13.4) | 0.24a | 19 (17.1) | 0.73a |
| Prior fertility consultation (n, %) | 13 (11.0) | 16 (12.0) | 0.80a | 10 (7.6) | 0.35a | 23 (18.9) | 24 (18.9) | 0.99a | 20 (18.0) | 0.87a |
| New consultations (n, %)e | 6 (5.4) | 5 (4.1) | 0.76d | 1 (0.8) | 0.06d | 7 (6.6) | 7 (6.4) | 1.00d | 7 (7.1) | 1.00d |
| Subgroup analyses among partnered individuals | ||||||||||
| New births (n, %)f | 11 (19.3) | 10 (13.9) | 0.41a | 15 (19.7) | 0.95a | 23 (27.1) | 16 (18.2) | 0.16a | 19 (25.0) | 0.77a |
| New births in 2015 (n, %)f | 5 (8.8) | 1 (1.4) | 0.09d | 4 (5.3) | 0.50d | 9 (10.6) | 2 (2.3) | 0.03d | 8 (10.5) | 1.00d |
| New consultations (n, %)g | 6 (12.0) | 5 (8.2) | 0.54d | 1 (1.5) | 0.04d | 6 (8.7) | 7 (9.7) | 1.00d | 7 (10.9) | 0.77d |
P values compare the preceding Control group with the Intervention group. Control 1 = folic acid intake pre-pregnancy. Control 2 = family policy.
aChi-square test.
bWilcoxon-type test for trend.
cTwo-tailed t test.
dFisher’s exact test.
eAmong those who had no prior fertility consultation at T1. Men: n = 111 (intervention), n = 122 (control 1), n = 123 (control 2). Women: n = 106 (intervention), n = 110 (control 1), n = 98 (control 2).
fSample sizes for partnered or married men are n = 57 (intervention), n = 72 (control 1), n = 76 (control 2). Sample sizes for women are n = 85 (intervention), n = 88 (control 1), n = 76 (control 2).
gSample sizes for partnered or married men who had no prior fertility consultation at T1 are n = 50 (intervention), n = 61 (control 1), n = 67 (control 2). Sample sizes for women are n = 69 (intervention), n = 72 (control 1), n = 64 (control 2).
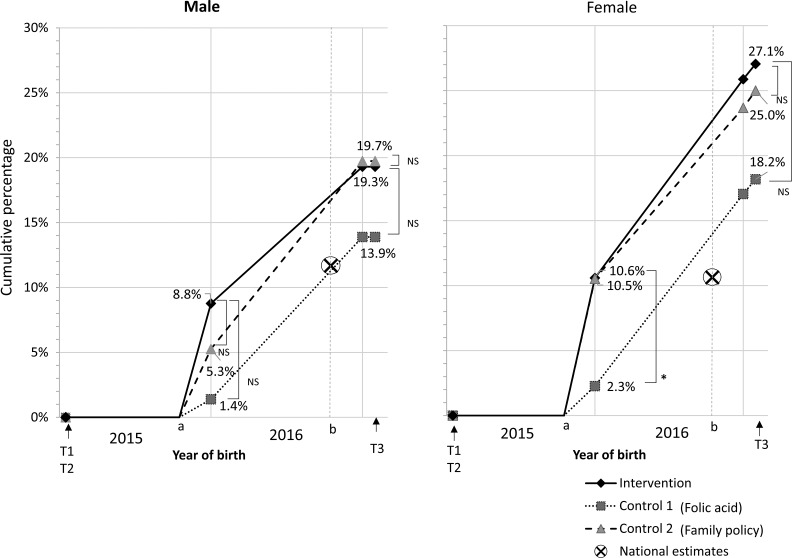
We examined the effect of information on reproductive outcomes of partnered individuals. Of 454 participants who had a partner (married or unmarried) at T1, 94 participants (20.7%) had a new child during the 2-year follow-up period, whereas only two of 289 participants without a partner (0.7%) had a new child (Table II). Figure 3 shows cumulative new births among those who had a partner at T1. The proportions of those who had a new birth in the intervention group and in control group 2 (family policy) were similar throughout the follow-up period. However, the proportion of partnered participants who had a new birth within a year was higher in the intervention group than in folic acid control group 1:8.8% versus 1.4% (P = 0.09) among men and 10.6% versus 2.3% (P = 0.03) among women (Table II). Compared to folic acid control group 1, the odds ratios for the intervention of having a new birth within a year were 7.8 (95% CI: 0.86–70.7) among men and 5.2 (95% CI: 1.09–25.0) among women after adjusting for age.
Figure 3.
Cumulative childbirths among participants who had been married or had a partner at T1. Significance of Fisher’s exact tests between groups was indicated by *(P < 0.05) and NS (not significant). aDepicted on the assumption that births were given later than 9 months after T1 (start point a). b12 months after start point a. × represents the national estimates, calculated from the national birth rates among those who have a spouse or a partner in their thirties: 0.12 and 0.11 per year among men and women, respectively. T1, before exposure to an information brochure; T2, immediately after exposure; T3, 2 years after exposure.
In terms of fertility consultations, among 670 participants without prior fertility consultation at T1, the proportion of those who had a new consultation was 32/383 (8.4%) among participants with a partner at T1 and 1/287 (0.3%) among participants without a partner. Subgroup analyses for partnered individuals showed the incidence of new medical consultation was higher in the male intervention group (12.0%) than in male control group 2 (family policy, 1.5%, P = 0.04) but no difference in incidence of new births (Table II). There was no difference between the intervention and control group 1 (folic acid) on incidence of new consultations. Similarly, there was no difference for women in the incidence of new consultations (between 8% and 10% for all groups).
Discussion
Single session, fertility education delivered online was associated with a modest knowledge gain (about 7–11%) at 2-year follow-up and accelerated the timing of new births among men and women with partners, compared to control information on pre-pregnancy health. The results suggest, for the first time, that fertility awareness could modify future reproductive outcomes. However, findings need to be interpreted with caution because people potentially less ready to conceive were lost to follow-up (i.e. younger, single, lower education, childless). Future campaigns could improve knowledge by integrating booster education sessions and addressing the needs of people without a partner.
The level of fertility knowledge in the intervention group was shown to improve by more than 10 points on the CFKS-J at T2, immediately after education (Maeda et al., 2016). In the present 2-year follow-up, we showed knowledge then dropped significantly but still remained four points higher than baseline levels (Supplementary Fig. S1). These results are consistent with previous findings that, regardless of educational strategy (i.e. web-based, printed, or tailored), knowledge retention reliably improves immediately after provision of information (Wojcieszek and Thompson, 2013; Garcia et al., 2016; Boivin et al., 2018) with reversion to near pre-interventional levels (Daniluk and Koert, 2015). The finding that some knowledge is retained suggests that follow-up ‘booster’ sessions of fertility education (Tolan et al., 2009; Hong et al., 2013) might be necessary to maintain high fertility knowledge over time.
Fertility education might potentially affect the timing of having children among people who already have partners or spouses. Men and women showed similar results, although the difference was marginally significant among men. Partnered participants who received fertility information were more than five times more likely to give birth within a year than those exposed to information on folic acid. The fertility information comprised information about fecundity and fecundability, infertility and risk factors for reduced fertility, any of which could have had the motivating effect. Although ultimately the incidence of new births for the 2-year follow-up period was not different between groups, advancing the timing could have implications for reduced age-related pregnancy health risks for those who want children (Gilbert et al., 1999; Yang et al., 2007) providing public health benefits (Lemoine and Ravitsky, 2013). Similarly, (among men) fertility knowledge increased attendance for fertility medical consultations. Although consults did not lead to more births in the follow-up period, having consults does again suggest a potential impact of fertility information on fertility decision-making compared to control (although only family policy). The fact that women did not show a similar effect might be because the intervention made men’s knowledge level similar to what women had already attained at baseline; this level of knowledge (~50% correct on CFKS) could be the minimum knowledge requirements for understanding when to seek medical help.
Interpretation of the effects of control information should be discussed because these were associated with different outcomes. We believe this is the first evidence for differential effects of fertility-related information. Family policy appeared to be more related to the timing of births whereas pre-pregnancy health more related to fertility medical consultations. The incidence rate of new births in the intervention group and control group 2 (family policies) was similar, and about 26% (Fig. 3). This incidence was higher than that of control group 1 (folic acid, about 18%) and of the national estimate (for partnered individuals in their 30 s, Ministry of Health, Labour and Welfare, 2015; National Institute of Population and Social Security Research, 2016). Family policy information included child and parental leave allowances and maternity benefits, and these have been shown to have a small positive impact on fertility and the timing of birth (Björklund, 2006; Gauthier, 2007). The folic acid information focused on informing women about the need to consume sufficient folic acid prior to pregnancy for avoidance of neural tube defects. Folic acid messaging is not associated with high uptake in Europe (Fulford et al., 2014) and one reason why is that it could induce too much fear about having children in women of reproductive-age, as seen with other health messaging (Job, 1988). One could speculate that fear could have the paradoxical effect of increasing worry and thereby medical consultations about fertility. These differential effects make clear that future RCTs should include multiple outcomes to types of control information to capture the diverse impacts of fertility and control information because these may influence the reproductive trajectory differently.
High attrition rate is another important finding of this study. Those lost to follow-up could have been less ready to have a child because they were younger, unmarried, more likely to have fewer (or no) children, and less likely to have consulted for a fertility problem than the follow-up cohort. Fertility education targets young people who have long reproductive lifespans ahead of them (Daniluk and Koert, 2013; Hammarberg et al., 2017; Boivin et al., 2018), but engaging this group with fertility information and the decision to have a child itself could require more engaged forms of educating (e.g. face to face, Stern et al., 2013; or at fertility planning clinics, Hvidman et al., 2015). Attrition implies a critical challenge to evaluating effects of information via online surveys and implementation of education that needs to be addressed in future research.
Less than 1% of the single participants had a child in the 2 years after the original study, even though all the T1 participants had hoped to have children in the future. The lack of an appropriate partner has been reported to be a main reason for people to delay childbearing in modern societies (Mills et al., 2011). In Japan, more than 20% of women and 30% of men in their early 30 s are estimated to be without a partner or a spouse, even though about half want a partner (National Institute of Population and Social Security Research, 2016). Local governments have launched many initiatives to promote marriage (e.g. matchmaking parties or seminars) (Cabinet Office, 2018), but reactions to these initiatives have been mixed. Along with fertility health education, it would be necessary to explore ways to help young people to meet their family building needs in view of societal changes (Zegers-Hochschild et al., 2017).
This study has some limitations. First, the high attrition rate decreased the statistical power and limited the generalizability of our findings, especially when applied to younger people who were more likely to be lost to follow-up. Second, this is a 2-year follow-up study. There is a possibility that the results may change in the longer run. Finally, we relied on self-reported questionnaire data and could not access additional medical information, such as date of pregnancy or date of consultation. It was assumed that all children born between 2015 and 2017 were conceived after T1 because we excluded women and partners of women who were pregnant at T1 from the recruitment. There is a possibility that some women were unknowingly pregnant at T1 but this risk should be distributed equally in the three groups through randomization. Nevertheless, this first RCT exploring the long-term effect of fertility education provided important findings, which should be pursued and confirmed in future research.
In conclusion, people exposed to an online fertility brochure lost most of the newly acquired knowledge but retained some after 2 years. Although one-time education did not affect the 2-year incidence of new childbirths or new medical consultations for fertility, it accelerated births among partnered individuals: partnered women in the intervention group were five times more likely to have a new child in the first year after exposure than those exposed to folic acid information. Further interventional studies using other strategies (e.g. tailored education, interactive web education) and other control materials should confirm the association between education and behaviour to develop effective educational strategies.
Supplementary Material
Acknowledgements
The authors thank Dr Fumiaki Nakamura (Bayer Yakuhin, Ltd.) for his expert advice and statistical help with this study. This study was presented at the 34th Annual Meeting of the European Society of Human Reproduction and Embryology (ESHRE), Barcelona, 1–4 July 2018.
Authors’ roles
E.M. contributed to the conception and design of the study, the acquisition of data and analysis and interpretation of data; drafted all versions of the article; and approved the final version for publication. J.B. contributed to the conception and design of the study, the analysis and interpretation of data, all revisions, and the final approval for publication. S.T. and K.M. contributed to the analysis and interpretation of data, all revisions and the final approval for publication. H.S. contributed to the conception and design of the study, all revisions and the final approval for publication.
Funding
This study was funded by National Center for Child Health and Development (Seiiku Medical Study Grant 28-7), the Daiwa Anglo-Japanese Foundation (Small Grant 9770-10492), Pfizer Health Research Foundation (Grant Number 29-25), and the Japan Society for the Promotion of Science: KAKENHI (Grant Number 16H06647).
Conflict of interest
E.M. reports a joint research fund from a public interest incorporated foundation ‘1 more Baby Ohendan.’
References
- Björklund A. Does family policy affect fertility? J Popul Econ 2006;19:3–24. [Google Scholar]
- Boivin J, Koert E, Harris T, O’Shea L, Perryman A, Parker K, Harrison C. An experimental evaluation of the benefits and costs of providing fertility information to adolescents and emerging adults. Hum Reprod 2018;33:1247–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunting L, Boivin J. Development and preliminary validation of the fertility status awareness tool: FertiSTAT. Hum Reprod 2010;25:1722–1733. [DOI] [PubMed] [Google Scholar]
- Bunting L, Tsibulsky I, Boivin J. Fertility knowledge and beliefs about fertility treatment: findings from the International Fertility Decision-making Study. Hum Reprod 2013;28:385–397. [DOI] [PubMed] [Google Scholar]
- Cabinet Office , Government of Japan. Marriage support in prefectures. 2018. http://www8.cao.go.jp/shoushi/shoushika/kekkon_ouen_pref.html
- Daniluk JC, Koert E. The other side of the fertility coin: a comparison of childless men’s and women’s knowledge of fertility and assisted reproductive technology. Fertil Steril 2013;99:839–846. [DOI] [PubMed] [Google Scholar]
- Daniluk JC, Koert E. Fertility awareness online: the efficacy of a fertility education website in increasing knowledge and changing fertility beliefs. Hum Reprod 2015;30:353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulford B, Macklon N, Boivin J. Mental models of pregnancy may explain low adherence to folic acid supplementation guidelines: a cross-sectional international survey. Eur J Obstet Gynecol Reprod Biol 2014;176:99–103. [DOI] [PubMed] [Google Scholar]
- Garcia D, Vassena R, Prat A, Vernaeve V. Increasing fertility knowledge and awareness by tailored education: a randomized controlled trial. Reprod Biomed Online 2016;32:113–120. [DOI] [PubMed] [Google Scholar]
- Gauthier AH. The impact of family policies on fertility in industrialized countries: a review of the literature. Popul Res Policy Rev 2007;26:323–346. [Google Scholar]
- Gilbert WM, Nesbitt TS, Danielsen B. Childbearing beyond age 40: pregnancy outcome in 24,032 cases. Obstet Gynecol 1999;93:9–14. [DOI] [PubMed] [Google Scholar]
- Hammarberg K, Norman RJ, Robertson S, McLachlan R, Michelmore J, Johnson L. Development of a health promotion programme to improve awareness of factors that affect fertility, and evaluation of its reach in the first 5 years. Reprod Biomed Soc Online 2017;4:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong O, Chin DL, Fiola LA, Kazanis AS. The effect of a booster intervention to promote hearing protection behavior in operating engineers. Am J Ind Med 2013;56:258–266. [DOI] [PubMed] [Google Scholar]
- Hvidman HW, Petersen KB, Larsen EC, Macklon KT, Pinborg A, Nyboe Andersen A. Individual fertility assessment and pro-fertility counselling; should this be offered to women and men of reproductive age? Hum Reprod 2015;30:9–15. [DOI] [PubMed] [Google Scholar]
- Job SRF. Effective and ineffective use of fear in health promotion campaigns. Am J Public Health 1988;78:163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemoine ME, Ravitsky V. Toward a public health approach to infertility: the ethical dimensions of infertility prevention. Public Health Ethics 2013;6:287–301. [Google Scholar]
- Maeda E, Nakamura F, Kobayashi Y, Boivin J, Sugimori H, Murata K, Saito H. Effects of fertility education on knowledge, desires and anxiety among the reproductive-aged population: findings from a randomized controlled trial. Hum Reprod 2016;31:2051–2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda E, Sugimori H, Nakamura F, Kobayashi Y, Green J, Suka M, Okamoto M, Boivin J, Saito H. A cross sectional study on fertility knowledge in Japan, measured with the Japanese version of Cardiff Fertility Knowledge Scale (CFKS-J). Reprod Health 2015;12:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills M, Rindfuss RR, McDonald P, te Velde E. Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update 2011;17:848–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health, Labour and Welfare Vital Statistics 2015.
- National Institute of Population and Social Security Research The 15th Japanese National Fertility Survey. 2016. http://www.ipss.go.jp/ps-doukou/e/doukou15/Nfs15_gaiyoEng.html.
- Organisation for Economic Co-operation and Development (OECD) OECD Family Database 2010, Indicator SF2.1, ‘Fertility Rates’ http://www.oecd.org/els/social/family/database 2014.
- Pedro J, Brandão T, Schmidt L, Costa ME, Martins MV. What do people know about fertility? A systematic review on fertility awareness and its associated factors. Ups J Med Sci 2018;123:71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern J, Larsson M, Kristiansson P, Tydén T. Introducing reproductive life plan-based information in contraceptive counselling: an RCT. Hum Reprod 2013;28:2450–2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolan PH, Gorman-Smith D, Henry D, Schoeny M. The benefits of booster interventions: evidence from a family-focused prevention program. Prev Sci 2009;10:287–297. [DOI] [PubMed] [Google Scholar]
- Wojcieszek AM, Thompson R. Conceiving of change: a brief intervention increases young adults’ knowledge of fertility and the effectiveness of in vitro fertilization. Fertil Steril 2013;100:523–529. [DOI] [PubMed] [Google Scholar]
- Yang Q, Wen SW, Leader A, Chen XK, Lipson J, Walker M. Paternal age and birth defects: how strong is the association? Hum Reprod 2007;22:696–701. [DOI] [PubMed] [Google Scholar]
- Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, Rienzi L, Sunde A, Schmidt L, Cooke ID et al. The International Glossary on Infertility and Fertility Care, 2017. Hum Reprod 2017;32:1786–1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.