Abstract
OBJECTIVE
To determine the concordance in the prevalence of hypertension and pharmacological antihypertensive treatment recommendations for U.S. adults with diabetes using definitions from the 2017 American College of Cardiology/American Heart Association (ACC/AHA) blood pressure (BP) guideline and the 2017 American Diabetes Association (ADA) diabetes and hypertension position statement.
RESEARCH DESIGN AND METHODS
We analyzed data for U.S. adults with diabetes in the U.S. National Health and Nutrition Examination Survey (NHANES), 2011–2016 (n = 2,266). Diabetes was defined by treatment with glucose-lowering medication, glycosylated hemoglobin ≥6.5%, fasting serum glucose ≥126 mg/dL, or nonfasting serum glucose ≥200 mg/dL. BP was measured three times and antihypertensive medication use was self-reported.
RESULTS
The prevalence (95% CI) of hypertension among U.S. adults with diabetes was 77.1% (73.9, 80.0) and 66.3% (63.4, 69.1) according to the ACC/AHA and ADA definitions, respectively. Also, 22.9% (20.0, 26.1) did not have hypertension according to either definition, and the concordance in hypertension status was 89.2% (87.2, 91.0). Among U.S. adults with diabetes not taking antihypertensive medication, 52.8% (47.7, 57.8) were not recommended to initiate antihypertensive medication by either the ACC/AHA or the ADA document and 22.4% (19.2, 25.9) were recommended to initiate it by both documents (overall concordance 75.2% [70.4, 79.4]). Among those taking antihypertensive medication, 45.3% (41.3, 49.4) and 50.4% (46.5, 54.2) had BP above the goal in neither and both documents, respectively (overall concordance 95.7% [93.4, 97.2]).
CONCLUSIONS
A high percentage of U.S. adults with diabetes are provided identical antihypertensive treatment recommendations by the ACC/AHA BP guideline and the ADA diabetes and hypertension position statement.
Introduction
Hypertension is one of the most common comorbidities among adults with diabetes. Prior studies have estimated the prevalence of hypertension to be twice as high among adults with diabetes compared with age-matched control subjects without diabetes (1,2). Among adults with diabetes, the presence of hypertension has been associated with a two times higher risk for cardiovascular disease (CVD) events and mortality (3,4).
The 2017 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults provides a comprehensive set of recommendations for the diagnosis and treatment of hypertension among adults, including those with diabetes (5). This guideline defines hypertension in adults, including those with diabetes, as an average systolic blood pressure (SBP) ≥130 mmHg or diastolic blood pressure (DBP) ≥80 mmHg (Table 1). According to this guideline, pharmacological antihypertensive treatment should be initiated in adults with diabetes if they have an average SBP ≥130 mmHg or DBP ≥80 mmHg, and the treatment goal is SBP <130 mmHg and DBP <80 mmHg (5).
Table 1.
BP levels used to define hypertension, to recommend initiation of antihypertensive medication, and as treatment goals for adults with diabetes according to the 2017 ACC/AHA BP guideline and the ADA diabetes and hypertension position statement
| 2017 ACC/AHA | ADA | |
|---|---|---|
| Definition of hypertension† |
||
| SBP, mmHg | ≥130 | ≥140 |
| DBP, mmHg | ≥80 | ≥90 |
| Recommendation for initiation of antihypertensive medication |
||
| SBP, mmHg | ≥130 | ≥140 |
| DBP, mmHg | ≥80 | ≥90 |
| Goal blood pressure (among those taking antihypertensive medication) |
||
| SBP, mmHg | <130 | <140†† |
| DBP, mmHg | <80 | <90†† |
†Participants taking antihypertensive medication were considered to have hypertension regardless of their BP level.
††The ADA position statement recommends patients and clinicians use a shared decision-making process to determine BP goals. Therefore, BP goals may differ from those listed in the table on a patient-by-patient basis. A goal BP of SBP <130 mmHg and DBP <80 mmHg may be appropriate for individuals at high risk of CVD without undue treatment burden. For this analysis, high cardiovascular risk was defined by a 10-year predicted ASCVD risk ≥10% using the Pooled Cohort risk equations or history of CVD.
The American Diabetes Association (ADA) published a position statement on diabetes and hypertension in 2017 that recommends blood pressure (BP) levels different from the ACC/AHA guideline for defining hypertension and for initiating pharmacological antihypertensive treatment (for both, SBP ≥140 mmHg or DBP ≥90 mmHg) (6). The ADA position statement recommends that BP goals should be individualized based on patient priorities and clinician judgment. Treatment goals for those taking antihypertensive medication are SBP <140 mmHg and DBP <90 mmHg, with SBP <130 mmHg and DBP <80 mmHg to be considered for those with high CVD risk as long as these levels can be achieved without undo treatment burden.
The purpose of the current study was to estimate the impact of differences in the definition of hypertension and recommendations for pharmacological antihypertensive treatment initiation and intensification of therapy in U.S. adults with diabetes according to the ACC/AHA guideline and the ADA diabetes and hypertension position statement (5,6). To accomplish these goals, we analyzed data from the U.S. National Health and Nutrition Examination Survey (NHANES).
Research Design and Methods
NHANES was designed and conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention (7). Since 1999, it has been conducted in two-year cycles, which can be combined in statistical analyses to provide more stable prevalence estimates. For the current analysis, we pooled data from the 2011–2012, 2013–2014, and 2015–2016 NHANES cycles. For each NHANES cycle, participants were identified through stratified, multistage probability sampling of the noninstitutionalized U.S. population. Among the 16,381 adults aged 20 years or older who completed the study interview and examination, we included 2,651 participants with diabetes (defined below) in our analyses. We excluded 177 participants who did not have three SBP and DBP measurements obtained during their study examination, 3 participants with missing information on self-reported antihypertensive medication use, and 205 participants who were missing data needed to calculate their 10-year predicted atherosclerotic CVD (ASCVD) risk using the Pooled Cohort risk equations (4). After applying these exclusion criteria, we had a final sample size of 2,266 participants with diabetes. The protocols for each NHANES cycle were approved by the National Center for Health Statistics of the Centers for Disease Control and Prevention institutional review board and all participants provided written informed consent. Our analysis of the publicly available NHANES data was considered exempt research by the University of Alabama at Birmingham institutional review board.
Data Collection
The NHANES data were collected using questionnaires and through a study examination conducted at a mobile clinic. Information on age, sex, race/ethnicity, education, cigarette smoking, use of antihypertensive and glucose lowering medication, and a history of myocardial infarction, coronary heart disease, stroke, or heart failure was obtained through self-report. Height and weight were measured during the study visit and used to calculate BMI. A blood specimen was collected and used to measure total and HDL cholesterol, serum creatinine, serum glucose, and glycated hemoglobin. Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (8). Using albumin and creatinine measured from a spot urine sample collected during the study visit, we calculated the albumin-to-creatinine ratio. Chronic kidney disease was defined as an eGFR <60 mL/min/1.73 m2 or albumin-to-creatinine ratio >30 mg/g (9).
BP Measurement
BP was measured three times by a trained physician using a mercury sphygmomanometer, following a standardized protocol. The first measurement was obtained in the seated position after 5 min of quiet rest and the two remaining measurements after 30-s rest intervals between the readings. For each participant, the mean of the three BP measurements was used to estimate SBP and DBP. Quality control included quarterly retraining and certification.
Diabetes
Using blood specimens collected during the NHANES examination, serum glucose was measured by means of a Roche/Hitachi Modular P Chemistry Analyzer or a Roche/Hitachi cobas C Chemistry Analyzer (Roche Diagnostics, Indianapolis, IN) and glycated hemoglobin was measured using a Tosoh G7 Automated HPLC Analyzer or a Tosoh Automated Analyzer HLC-723G8 (Tosoh Medics, Inc., San Francisco, CA). Diabetes was defined by fasting serum glucose ≥126 mg/dL, nonfasting serum glucose ≥200 mg/dL, hemoglobin A1c ≥6.5%, or the self-reported use of glucose-lowering medication (10).
CVD Risk
History of CVD was defined by self-report of a prior diagnosis of myocardial infarction, coronary heart disease, stroke, or heart failure. Among participants without a history of CVD, 10-year ASCVD risk was calculated using the Pooled Cohort risk equations (4). Among participants without a history of CVD who were <60 years old, 30-year predicted ASCVD risk was calculated using an equation developed in the Framingham Offspring Cohort (11). In these equations, ASCVD risk includes the risk for nonfatal myocardial infarction or coronary heart disease death or fatal or nonfatal stroke.
Definitions of Hypertension, Recommendations for Antihypertensive Medication, and BP Treatment Goals
The ACC/AHA guideline and ADA position statement recommendations for the definition of hypertension, initiation of antihypertensive medication, and BP goals in adults with diabetes were as described in the introduction and are displayed in Table 1. Participants taking antihypertensive medication were considered to have hypertension according to both the ACC/AHA guideline and the ADA position statement. The ADA position statement states that a goal SBP and DBP <130 and <80 mmHg, respectively, may be appropriate for individuals at high CVD risk if these levels can be achieved without undue treatment burden. High CVD risk was defined as having a history of CVD or a 10-year predicted ASCVD risk ≥10% using the Pooled Cohort risk equations (5).
Statistical Methods
Using NHANES data extrapolated to the U.S. population, we calculated summary statistics for U.S. adults with diabetes taking and not taking antihypertensive medication, overall and for those with and without high CVD risk separately. We estimated the percentage and number of U.S. adults with diabetes who had hypertension according to the ACC/AHA guideline and the ADA position statement separately. Among those not taking antihypertensive medication, we estimated the percentage and number of U.S. adults with diabetes who would be recommended to initiate antihypertensive medication according to the ACC/AHA guideline and the ADA position statement separately. Among those taking antihypertensive medication, we estimated the percentage and number of U.S. adults with diabetes who had BP above the treatment goal according to the ACC/AHA guideline and the ADA position statement. We calculated the percentage of U.S. adults with diabetes who had concordant and discordant definitions of hypertension and recommendations for initiation of antihypertensive medication and with BP above the treatment goal by the ACC/AHA and ADA documents. As the ADA position statement does not explicitly define high CVD risk, we conducted a sensitivity analysis defining high CVD risk as a history of CVD or a 10-year ASCVD risk ≥20%. Using this definition, we calculated the proportion of U.S. adults with diabetes taking antihypertensive medication that had BP above the treatment goal according to the ADA position statement (SBP ≥140 mmHg or DBP ≥90 mmHg; SBP ≥130 mmHg or DBP ≥80 mmHg for those with high CVD risk) and the ACC/AHA guideline (SBP ≥130 mmHg or DBP ≥80 mmHg).
We calculated summary statistics for U.S. adults with diabetes not taking antihypertensive medication who would not be recommended to initiate antihypertensive medication according to either the ACC/AHA guideline or the ADA position statement and who would be recommended to initiate antihypertensive medication by the ACC/AHA guideline only and by both documents. Also, we calculated summary statistics for U.S. adults with diabetes taking antihypertensive medication without BP above the treatment goal according to either document and with BP above the treatment goal according to the ACC/AHA guideline only and both documents.
Prevalence estimates and differences in prevalence estimates across subgroups were calculated as weighted proportions, and 95% CIs were computed with variance estimates determined using Taylor series linearization. NHANES sampling weights were used in all calculations to obtain U.S. nationally representative prevalence estimates for the overall population and subgroups (e.g., those with diabetes and hypertension) (12). Sampling weights were recalibrated based on the proportion of participants missing data by age, sex, and race/ethnicity within each NHANES cycle. The data analysis took into account the complex survey design of NHANES and was conducted using Stata 14 (Stata Corporation, College Station, TX).
Results
According to data from NHANES 2011–2016, 56.6% (95% CI 53.3, 59.9) of U.S. adults with diabetes were taking antihypertensive medication. Of U.S. adults with diabetes, 57.4% (53.1, 61.6) of those not taking and 80.2% (76.6, 83.4) of those taking antihypertensive medication had high CVD risk. Among U.S. adults with diabetes, those with high CVD risk (history of CVD or 10-year ASCVD risk ≥10%) were on average 15–20 years older and the prevalence of smoking and chronic kidney disease was 10–20% higher when compared with their counterparts without high CVD risk (Supplementary Table 1). Among U.S. adults with diabetes without high CVD risk, the mean 10-year and 30-year predicted CVD risks were 3.8% (3.5, 4.2) and 25.0% (23.4, 26.6), respectively, for those not taking antihypertensive medication and 5.8% (5.3, 6.4) and 37.4% (34.5, 40.3), respectively, for those taking antihypertensive medication.
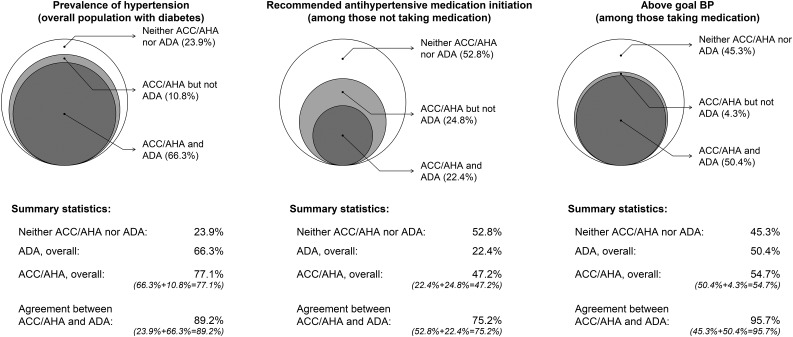
The prevalence of hypertension was 77.1% (95% CI 73.9, 80.0) according to the ACC/AHA guideline and 66.3% (63.4, 69.1) according to the ADA position statement (Fig. 1, left panel, and Supplementary Table 2, top panel). Overall, 10.8% (9.0, 12.8) of U.S. adults with diabetes had hypertension according to the ACC/AHA guideline but not the ADA position statement. Among U.S. adults with diabetes not taking antihypertensive medication, 52.8% (47.7, 57.8), 24.8% (20.6, 29.6) and 22.4% (19.2, 25.9) were recommended antihypertensive medication initiation by neither document, by the 2017 ACC/AHA guideline only, and by both documents, respectively (Fig. 1, middle panel, and Supplementary Table 2, middle panel). Among U.S. adults with diabetes taking antihypertensive medication, 45.3% (41.3, 49.4), 4.3% (2.8, 6.6), and 50.4% (46.5, 54.2) had an average BP that met the goal in both documents, was above the ACC/AHA goal but not the ADA goal, and was above the goals in both documents, respectively (Fig. 1, right panel, and Supplementary Table 2, bottom panel). The overall agreement between the ACC/AHA guideline and the ADA position statement was 89.2% (87.2, 91.0) for the presence of hypertension, 75.2% (70.4, 79.4) for the recommendation to initiate antihypertensive medication, and 95.7% (93.4, 97.2) for having a BP above the recommended treatment goal. The ACC/AHA guideline and the ADA position statement provided concordant antihypertensive medication treatment recommendations for 86.7% (84.4, 88.8) of U.S. adults with diabetes (Supplementary Fig. 1). When defining high CVD risk as a history of CVD or a 10-year ASCVD risk ≥20% for the ADA position statement, the overall agreement between the ACC/AHA guideline and ADA position statement for having BP above the recommended treatment goal was 90.8% (88.1, 93.0) (Supplementary Table 3).
Figure 1.
Percentage of U.S. adults with diabetes who have hypertension (left panel), who are recommended to initiate antihypertensive medication (middle panel), and with above-goal BP among those taking antihypertensive medication (right panel). Estimates from NHANES 2011–2016 data using definitions from the 2017 ACC/AHA BP guideline and the ADA diabetes and hypertension position statement. Supplementary Table 1 contains the 95% CIs for the percentages presented in this figure.
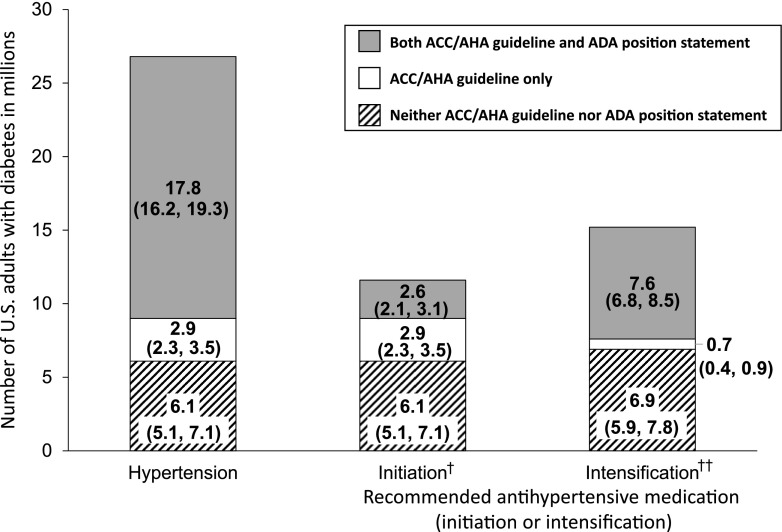
Based on both the ACC/AHA guideline and ADA position statement, 17.8 (95% CI 16.2, 19.3) million U.S. adults with diabetes had hypertension (Fig. 2, left bar). An additional 2.9 (2.3, 3.5) million U.S. adults had hypertension based on the ACC/AHA guideline only. Among U.S. adults with diabetes not taking antihypertensive medication, 2.6 (2.1, 3.1) million were recommended to initiate antihypertensive medication by both the ACC/AHA guideline and the ADA position statement with an additional 2.9 (2.3, 3.5) million recommended to initiate antihypertensive medication by the ACC/AHA guideline only (Fig. 2, middle bar). Among U.S. adults with diabetes taking antihypertensive medication, 7.6 (6.8, 8.5) million had a BP above the goal in both documents, with an additional 700,000 (400,000, 900,000) having a BP above the goal recommended in the ACC/AHA guideline only (Fig. 2, right bar).
Figure 2.
Number of U.S. adults with diabetes who have hypertension (left bar), who are recommended to initiate antihypertensive medication among those not taking it (middle bar), and with above-goal BP among those taking antihypertensive medication (right bar) according to the 2017 ACC/AHA BP guideline and the ADA diabetes and hypertension position statement. Numbers in the figure are point estimates in millions with 95% CIs in parentheses.†Recommended antihypertensive medication initiation among those not taking antihypertensive medication. ††Recommended antihypertensive medication intensification due to above-goal BP (see Table 1 for the definitions of above-goal BP) among those taking antihypertensive medication.
Among U.S. adults with diabetes not taking antihypertensive medication, the mean 10-year CVD risk was 10.7% (95% CI 9.4, 12.0) for those not recommended treatment initiation by either the ACC/AHA guideline or the ADA position statement, 14.6% (11.5, 17.6) for those recommended treatment initiation by the ACC/AHA guideline but not the ADA position statement, and 23.2% (19.5, 27.0) among those recommended treatment initiation by the ACC/AHA guideline and the ADA position statement (Table 2). The mean 30-year CVD risk exceeded 25% in each of these groups. Among U.S. adults with diabetes taking antihypertensive medication, the mean 10-year CVD risk was 10.6% (9.4, 12.0), 6.5% (CI 5.6, 7.3), and 33.8% (32.1, 35.5) among those with above-goal BP according to neither document, the ACC/AHA guideline only, and both documents, respectively (Supplementary Table 4). The 30-year CVD risk exceeded 40% in each group.
Table 2.
Characteristics of U.S. adults with diabetes not taking antihypertensive medication by recommendation for initiation of antihypertensive medication according to the ACC/AHA BP guideline and the ADA diabetes and hypertension position statement
| Recommended antihypertensive medication initiation by: |
|||
|---|---|---|---|
| Neither ACC/AHA BP guideline or ADA position statement† (n = 510) | ACC/AHA BP guideline but not ADA position statement†† (n = 231) | ACC/AHA BP guideline and ADA position statement††† (n = 213) | |
| Age, years | 53.6 (51.9, 55.3) | 53.8 (50.9, 56.8) | 59.2 (57.3, 61.1) |
| Male, % | 53.2 (48.6, 57.8) | 60.2 (53.1, 66.9) | 61.1 (50.2, 71.0) |
| Race/ethnicity, % | |||
| Non-Hispanic white | 51.1 (43.1, 59.1) | 58.7 (48.4, 68.3) | 58.1 (47.6, 67.9) |
| Non-Hispanic black | 12.0 (8.6, 16.4) | 12.8 (8.3, 19.3) | 15.6 (10.5, 22.5) |
| Non-Hispanic Asian | 8.6 (6.4, 11.4) | 7.0 (4.6, 10.6) | 8.9 (5.7, 13.7) |
| Hispanic | 22.7 (17.4, 29.1) | 21.0 (14.2, 29.9) | 16.2 (11.0, 23.3) |
| Less than HS education, % | 26.0 (21.3, 31.4) | 21.8 (15.7, 29.4) | 25.5 (19.0, 33.4) |
| Current smoking, % | 20.8 (17.4, 24.7) | 18.8 (13.0, 26.4) | 18.3 (12.5, 26.0) |
| BMI, kg/m2 | 32.4 (31.5, 33.2) | 32.4 (30.9, 33.9) | 33.0 (31.1, 35.0) |
| SBP, mmHg | 115.8 (114.7, 116.9) | 130.6 (129.4, 131.8) | 151.4 (148.1, 154.7) |
| DBP, mmHg | 67.0 (66.0, 67.9) | 75.8 (73.9, 77.6) | 78.3 (75.8, 80.8) |
| Total cholesterol, mg/dL | 186 (180, 192) | 200.6 (193.0, 208.3) | 194.1 (185.8, 202.3) |
| HDL cholesterol, mg/dL | 45.6 (43.7, 47.5) | 46.6 (44.2, 48.9) | 45.2 (42.4, 47.9) |
| eGFR <60 mL/min/1.73 m2, % | 8.6 (6.6, 11.1) | 8.0 (4.5, 13.7) | 18.0 (11.0, 27.9) |
| ACR >30 mg/g, % | 11.8 (8.9, 15.4) | 27.4 (19.3, 37.2) | 40.5 (30.9, 50.9) |
| Chronic kidney disease, % | 18.4 (14.7, 22.8) | 32.6 (23.3, 43.6) | 48.8 (41.1, 56.5) |
| Mean 10-year CVD risk,‡ % | 10.7 (9.4, 12.0) | 14.6 (11.5, 17.6) | 23.2 (19.5, 27.0) |
| 10-year ASCVD risk ≥10%, % | 44.1 (38.2, 50.2) | 52.3 (42.2, 62.2) | 76.4 (67.3, 83.6) |
| History of CVD, % | 15.2 (11.1, 20.5) | 13.1 (8.4, 19.9) | 13.1 (8.2, 20.2) |
| High CVD risk,* % | 49.1 (43.0, 55.2) | 56.9 (47.0, 66.2) | 77.7 (69.1, 84.4) |
| Mean 30-year ASCVD risk,‡‡ % | 28.4 (25.5, 31.3) | 36.6 (32.2, 41.0) | 50.0 (44.5, 55.4) |
Data are prevalence or mean (95% CI). ACR, albumin-to-creatinine ratio; HS, high school.
†The group not recommended to initiate antihypertensive medication according to either the ACC/AHA guideline or the ADA position statement had SBP <130 mmHg and DBP <80 mmHg.
††The group recommended to initiate antihypertensive medication according to the ACC/AHA guideline but not the ADA position statement had SBP 130–139 mmHg with DBP <90 mmHg or DBP 80–89 mmHg with SBP <140 mmHg.
†††The group recommended to initiate antihypertensive medication according to both the ACC/AHA guideline and the ADA position statement had SBP ≥140 mmHg or DBP ≥90 mmHg.
‡Mean 10-year ASCVD risk was calculated among participants without a history of CVD.
*High CVD risk was defined as a history of CVD or a 10-year predicted ASCVD risk ≥10%.
‡‡Mean 30-year ASCVD risk was calculated among participants 20–59 years of age without a history of CVD.
Conclusions
In this study of U.S. adults with diabetes, we compared the prevalence of hypertension and recommendations for pharmacological antihypertensive treatment in the 2017 ACC/AHA BP guideline (5) with the 2017 ADA diabetes and hypertension position statement (6). The results demonstrate a high level of agreement between these documents with a few small differences. Consistent with the use of lower SBP and DBP thresholds, the prevalence of hypertension was 10.8% higher, representing an estimated 2.9 million U.S. adults with diabetes, according to the ACC/AHA guideline compared with the ADA position statement. Among U.S. adults with diabetes not taking antihypertensive medication, 75.2% had an identical recommendation for initiation of antihypertensive drug therapy according to the ACC/AHA guideline and the ADA position statement. The majority of those who were recommended to initiate pharmacological antihypertensive therapy according to the ACC/AHA guideline but not the ADA position statement had high CVD risk. Among U.S. adults with diabetes taking antihypertensive medication, there was almost complete agreement with respect to meeting goal BP levels in the ACC/AHA guideline and the ADA position statement.
Prior to the 2017 ACC/AHA guideline, hypertension in the U.S. was defined by an average SBP ≥140 mmHg or DBP ≥90 mmHg for adults with and without diabetes (13,14). The lower BP thresholds used to define hypertension in the ACC/AHA guideline are supported by observational data on the association between higher SBP and DBP and increased risk for CVD and kidney disease as well as randomized controlled trials of lifestyle modification and treatment with antihypertensive medication to lower BP and prevent CVD (5). The ADA position statement retained SBP ≥140 mmHg and DBP ≥90 mmHg to define hypertension (6). Two authors of the ADA position statement argued that the prevalence of hypertension is already high among adults with diabetes and would not increase substantially by applying lower BP thresholds (15). The current study provides data to support this statement. The prevalence of hypertension was high when defined using BP thresholds in both the ACC/AHA guideline and the ADA position statement, and only 10.8% of U.S. adults with diabetes—an estimated 2.9 million adults—would be classified differently when using the ACC/AHA guideline versus the ADA position statement definition of hypertension.
The recommendation in the ACC/AHA guideline to use CVD risk to guide the decision to initiate antihypertensive medication was based, in part, on data showing that the absolute benefit of antihypertensive medication on CVD risk reduction is larger among individuals with higher CVD risk (16). As a matter of practical convenience for clinicians, all adults with diabetes and hypertension are grouped with other adults who have high CVD risk in the ACC/AHA guideline. Not all U.S. adults with diabetes had a high 10-year predicted ASCVD risk in the current study. However, the Pooled Cohort risk equations do not include heart failure as an outcome, likely leading to an underestimation of predicted CVD risk (4). The risk for heart failure is high among adults with diabetes, and BP control reduces this risk. Future risk prediction models used to guide antihypertensive medication initiation should consider including heart failure as an outcome. Also, many younger adults with diabetes have a high CVD risk over a longer time horizon (11). Personal characteristics of those who were discordant between the ACC/AHA guideline and ADA position statement were more similar to those not recommended antihypertensive medication initiation by either the ACC/AHA guideline or the ADA position statement than to those recommended initiation of antihypertensive medication by both. However, the mean 10-year and 30-year ASCVD risks among the discordant individuals were higher than among those not recommended antihypertensive medication initiation by either the ACC/AHA guideline or the ADA position statement. Additionally, initiating antihypertensive medication at lower BP levels may have advantages. Prior studies have reported that maintaining lower BP levels across the life course may have CVD risk reduction benefits (17).
The basis for the 2017 ACC/AHA guideline recommendation to achieve a target SBP <130 mmHg among adults with diabetes includes the results of several randomized clinical trials and meta-analyses of these trials. In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, randomization to an SBP goal of 120 mmHg vs. 140 mmHg was not associated with a statistically significant risk reduction for the primary CVD outcome, but it did lead to a reduced stroke event rate (18). Several post hoc analyses of ACCORD have supported an SBP goal lower than 140 mmHg for adults with diabetes (19–23). Another large randomized controlled trial conducted among adults with diabetes, the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE), demonstrated lower CVD event rates with randomization to antihypertensive medication versus placebo among participants with SBP <140 mmHg at baseline (24). Results from a post hoc analysis of the Systolic Blood Pressure Intervention Trial (SPRINT) suggest that the CVD risk reduction benefits of an intensive versus standard SBP goal (<120 mmHg vs. <140 mmHg) do not differ by levels of fasting serum glucose (25). In addition, a meta-analysis of randomized controlled trials with participants who had diabetes demonstrated statistically significant reductions in stroke, retinopathy, and albuminuria with initiation of antihypertensive medication at SBP <140 mmHg and when an SBP <130 mmHg was achieved (26).
The decision to initiate and intensify antihypertensive medication should take into consideration both the benefits of treatment and potential harm. Some patients experience side effects from antihypertensive medication, including electrolyte abnormalities and a reduction in eGFR (27). The latter is usually small and may be due to a hemodynamic treatment effect. In SPRINT, there was no difference in the incidence of serious adverse effects between the participants randomized to the intensive and standard treatment groups (28). The clinical implications of serious adverse events that were more common in the intensively treated participants are uncertain, but investigation of those hospitalized for acute kidney injury indicated most had a single instance of stage 1 acute kidney injury that resolved in more than 90% of cases within 1 year of follow-up (29). In ADVANCE, there was no evidence that rates of treatment discontinuation due to side effects were higher among participants with baseline SBP between 120 and 139 mmHg than among their counterparts with baseline SBP between 140 and 159 mmHg (30). Randomization to a goal SBP <120 mmHg in the ACCORD-BP trial was associated with a 3-year cumulative incidence of chronic kidney disease (defined as a >30% decrease in eGFR to <60 mL/min/1.73 m2) of 10.0% vs. 4.1% for their counterparts randomized to a goal SBP <140 mmHg (31). Studies are needed to determine the long-term outcomes associated with developing chronic kidney disease following intensive antihypertensive treatment and whether they outweigh the CVD risk reduction benefit. Kidney function should be monitored among adults receiving antihypertensive medication with increased vigilance when treating individuals to lower BP levels.
At the population level, the ACC/AHA guideline and ADA position statement have more similarities than differences. However, at the individual level, some patients with diabetes will have fundamental changes in their care depending on which advice is followed. The decision to initiate and intensify antihypertensive medication should always be individualized, based on discussions between patients and their clinicians. Both the ACC/AHA BP guideline and ADA position statement acknowledge the need to individualize treatment decisions to align with patients’ interests.
A recent analysis using NHANES 2005–2014 data reported the prevalence of hypertension among U.S. adults with diabetes according to the 2017 ACC/AHA guideline and the ADA position statement (32). In that study, approximately 10% of U.S. adults with diabetes were recommended to initiate antihypertensive medication by the ACC/AHA guideline but not the ADA position statement. Although the results in the current study are consistent with those previously reported, we extend those findings in several important ways. For example, the proportion of U.S. adults with diabetes taking antihypertensive medication for whom treatment intensification is recommended by the ACC/AHA guideline and ADA position statement and the overall agreement in the definition of hypertension and the recommendations for initiation and intensification of antihypertensive medication between the ACC/AHA guideline and ADA position statement were not reported in the previous analysis. Also, we used more contemporary data (NHANES 2011–2016 vs. NHANES 2005–2014) and had a larger sample size than the previous study (n = 2,266 vs. n = 1,824).
The current study has several strengths. NHANES is designed to provide nationally representative estimates. Therefore, there is a high degree of generalizability of the current findings. Data collection in NHANES is rigorous and conducted following standardized protocols. Despite these strengths, the results should be interpreted in the context of known and potential limitations. BP was measured at a single visit using a mercury sphygmomanometer. Both the ACC/AHA BP guideline and the ADA position statement recommend making the diagnosis of hypertension based on two or more BP measurements at two or more visits. As some NHANES participants may not have had high BP if measurements were obtained at a follow-up visit, the prevalence of hypertension, as defined by both the ACC/AHA BP guideline and the ADA position statement, may be lower than reported. In addition, mercury sphygmomanometers are rarely used in clinical practice in the U.S. A history of CVD was determined using self-report and is subject to recall errors. Finally, data were not available on whether SBP <130 mmHg and DBP <80 mmHg could be achieved without undo treatment burden. Therefore, we may have overestimated the percentage of U.S. adults with diabetes for whom this BP goal is recommended by the ADA position statement. This would result in lower agreement than we report for above-goal BP.
In conclusion, the current study demonstrates a high degree of concordance between the 2017 ACC/AHA BP guideline and the 2017 ADA position statement on diabetes and hypertension. Using either document, the majority of U.S. adults with diabetes have hypertension. A substantial proportion of U.S. adults with diabetes not taking antihypertensive medication are recommended to initiate treatment by both documents, with additional individuals being candidates for antihypertensive medication treatment by the ACC/AHA guideline only. U.S. adults with diabetes for whom initiation of antihypertensive medication is recommended by the ACC/AHA guideline but not the ADA position statement have high CVD risk. Finally, almost all U.S. adults with diabetes taking antihypertensive medication have identical recommendations to intensify or not intensity drug treatment to achieve SBP <130 mmHg and DBP <80 mmHg according to both the ACC/AHA guideline and the ADA position statement. These data demonstrate the high prevalence of hypertension among U.S. adults with diabetes and the need to increase the appropriate use of antihypertensive medication to reduce CVD in this high-risk population.
Supplementary Material
Article Information
Funding. P.M. receives research support from the American Heart Association through grant 15SFRN2390002. P.K.W. receives research support from the National Institutes of Health through grant P20GM109036 (Tulane Center of Biomedical and Research Excellence for Clinical and Translational Research in Cardiometabolic Diseases). M.W. receives support from the National Health and Medical Research Council of Australia. R.M.C. receives research support from the National Institutes of Health through grants R01-HL128189 and P01-HL074940.
Duality of Interest. P.K.W. was chair, R.M.C. was vice-chair, and P.M. was a member of the writing group for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. P.M. was a member of the writing group for the 2017 ADA position statement on diabetes and hypertension. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. P.M., P.K.W., and R.M.C. conceived the hypotheses for the current manuscript. P.M. conducted the statistical analysis. M.W. provided guidance on the statistical analysis and all authors were involved in the interpretation of the results and provided guidance for the presentation of results. P.M. and R.M.C. drafted the manuscript. P.K.W. and M.W. reviewed draft versions of the manuscript and provided substantive input to all sections of the manuscript. P.M. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc18-1307/-/DC1.
References
- 1.Kannel WB, Wilson PW, Zhang TJ. The epidemiology of impaired glucose tolerance and hypertension. Am Heart J 1991;121:1268–1273 [DOI] [PubMed] [Google Scholar]
- 2.Tarnow L, Rossing P, Gall MA, Nielsen FS, Parving HH. Prevalence of arterial hypertension in diabetic patients before and after the JNC-V. Diabetes Care 1994;17:1247–1251 [DOI] [PubMed] [Google Scholar]
- 3.Adler AI, Stratton IM, Neil HAW, et al. . Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al.; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2935–2959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whelton PK, Carey RM, Aronow WS, et al. doi: 10.1161/HYP.0000000000000065. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in Hypertension 2018;71:e140–e144]. Hypertension 2018;71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 6.de Boer IH, Bangalore S, Benetos A, et al. . Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care 2017;40:1273–1284 [DOI] [PubMed] [Google Scholar]
- 7.National Center for Health Statistics. National Health and Nutrition Examination Survey [Internet], 2018. Available from https://www.cdc.gov/nchs/nhanes/index.htm. Accessed 1 June 2018
- 8.Levey AS, Stevens LA, Schmid CH, et al.; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) . A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stevens PE, Levin A; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members . Evaluation and management of chronic kidney disease: synopsis of the Kidney Disease: Improving Global Outcomes 2012 clinical practice guideline. Ann Intern Med 2013;158:825–830 [DOI] [PubMed] [Google Scholar]
- 10.Inzucchi SE, Bergenstal RM, Buse JB, et al. . Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015;38:140–149 [DOI] [PubMed] [Google Scholar]
- 11.Pencina MJ, D’Agostino RB Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: the Framingham Heart Study. Circulation 2009;119:3078–3084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. NHANES tutorials [Internet]. Available from https://www.cdc.gov/nchs/nhanes/tutorials/default.aspx. Accessed 1 June 2018
- 13.American Diabetes Association 9. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018;41(Suppl. 1):S86–S104 [DOI] [PubMed] [Google Scholar]
- 14.Chobanian AV, Bakris GL, Black HR, et al.; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 15.de Boer IH, Bakris G, Cannon CP. Individualizing blood pressure targets for people with diabetes and hypertension: Comparing the ADA and the ACC/AHA recommendations. JAMA 2018;319:1319–1320 [DOI] [PubMed] [Google Scholar]
- 16.Blood Pressure Lowering Treatment Trialists’ Collaboration Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet 2014;384:591–598 [DOI] [PubMed] [Google Scholar]
- 17.Allen NB, Siddique J, Wilkins JT, et al. . Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA 2014;311:490–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cushman WC, Evans GW, Byington RP, et al.; ACCORD Study Group . Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Margolis KL, O’Connor PJ, Morgan TM, et al. . Outcomes of combined cardiovascular risk factor management strategies in type 2 diabetes: the ACCORD randomized trial. Diabetes Care 2014;37:1721–1728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buckley LF, Dixon DL, Wohlford GF IV, Wijesinghe DS, Baker WL, Van Tassell BW. Intensive versus standard blood pressure control in SPRINT-eligible participants of ACCORD-BP. Diabetes Care 2017;40:1733–1738 [DOI] [PubMed] [Google Scholar]
- 21.Huang C, Dhruva SS, Coppi AC, et al. . Systolic blood pressure response in SPRINT (Systolic Blood Pressure Intervention Trial) and ACCORD (Action to Control Cardiovascular Risk in Diabetes): a possible explanation for discordant trial results. J Am Heart Assoc 2017;6:e007509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buckley LF, Dixon DL, Wohlford GF IV, Wijesinghe DS, Baker WL, Van Tassell BW. Effect of intensive blood pressure control in patients with type 2 diabetes mellitus over 9 years of follow-up: a subgroup analysis of high-risk ACCORDION trial participants. Diabetes Obes Metab 2018;20:1499–1502 [DOI] [PubMed] [Google Scholar]
- 23.Brouwer TF, Vehmeijer JT, Kalkman DN, et al. . Intensive blood pressure lowering in patients with and patients without type 2 diabetes: a pooled analysis from two randomized trials. Diabetes Care 2018;41:1142–1148 [DOI] [PubMed] [Google Scholar]
- 24.Patel A, MacMahon S, Chalmers J, et al.; ADVANCE Collaborative Group . Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet 2007;370:829–840 [DOI] [PubMed] [Google Scholar]
- 25.Bress AP, King JB, Kreider KE, et al.; SPRINT Research Group . Effect of intensive versus standard blood pressure treatment according to baseline prediabetes status: a post hoc analysis of a randomized trial. Diabetes Care 2018;40:1401–1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA 2015;313:603–615 [DOI] [PubMed] [Google Scholar]
- 27.Cheung AK, Rahman M, Reboussin DM, et al.; SPRINT Research Group . Effects of intensive BP control in CKD. J Am Soc Nephrol 2017;28:2812–2823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wright JT Jr, Williamson JD, Whelton PK, et al.; SPRINT Research Group . A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rocco MV, Sink KM, Lovato LC, et al.; SPRINT Research Group . Effects of intensive blood pressure treatment on acute kidney injury events in the Systolic Blood Pressure Intervention Trial (SPRINT). Am J Kidney Dis 2018;71:352–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Atkins ER, Hirakawa Y, Salam A, et al. . Side effects and tolerability of combination blood pressure lowering according to blood pressure levels: an analysis of the PROGRESS and ADVANCE trials. J Hypertens 2017;35:1318–1325 [DOI] [PubMed] [Google Scholar]
- 31.Beddhu S, Greene T, Boucher R, et al. . Intensive systolic blood pressure control and incident chronic kidney disease in people with and without diabetes mellitus: secondary analyses of two randomised controlled trials. Lancet Diabetes Endocrinol 2018;6:555–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shin D, Bohra C, Kongpakpaisarn K. Impact of the discordance between the American College of Cardiology/American Heart Association and American Diabetes Association recommendations on hypertension in patients with diabetes mellitus in the United States. Hypertension 2018;72:256–259 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.