Abstract
Men’s poor health behaviors are an increasingly prevalent issue with long-term consequences. This study broadly samples Canadian men to obtain information regarding health behaviors as a predictor of downstream medical comorbidities. A survey of Canadian men included questions regarding demographics, comorbidities, and health behaviors (smoking and alcohol consumption, sleep and exercise behaviors, and dietary habits). Health behaviors were classified as either healthy or unhealthy based upon previous studies and questionnaire thresholds. Multivariate regression was performed to determine predictors for medical comorbidities. The 2,000 participants were aged 19–94 (median 48, interquartile range 34–60). Approximately half (47.4%) were regular smokers, 38.7% overused alcohol, 53.9% reported unhealthy sleep, 48.9% had low levels of exercise, and 61.8% had unhealthy diets. On multivariate analysis, regular smoking predicted heart disease (OR 2.08, p < .01), elevated cholesterol (OR 1.35, p = .02), type 2 diabetes (OR 1.57, p = .02), osteoarthritis (OR 1.43, p = .04), and depression (OR 1.62, p < .01). Alcohol overuse predicted hypertension (OR 1.40, p < .01) and protected against type 2 diabetes (OR 0.61, p < .01). Unhealthy sleep predicted hypertension (OR 1.46, p < .01), erectile dysfunction (OR 1.50, p = .04), and depression (OR 1.87, p < .01). Low levels of exercise predicted hypertension (OR 1.30, p = .03) and elevated cholesterol (OR 1.27, p = .05). Finally, unhealthy diet predicted depression (OR 1.65, p < .01). This study confirms the association of poor health behaviors and comorbidities common to middle-aged and older men. The results emphasize the potential scope of targeted gender-sensitized public awareness campaigns and interventions to reduce common male disease, morbidity, and mortality.
Keywords: epidemiology of men’s health, general health and wellness, health information, public health, health-care issues, health promotion and disease prevention
Introduction
Diseases linked to unhealthy behaviors are amongst the leading causes of male morbidity and mortality, in both North America and worldwide (Danaei et al., 2009; Willett et al., 2006), including cardiovascular disease (9.8%), hypertension (24.2%), obesity (26.5%), diabetes (8.3% with both type 1 and type 2), and cancer (2.45% 10-year prevalence; Health Canada, 2017). Many of these conditions are interrelated and the onset may begin years prior to diagnosis and intervention (Kim, 2015). Up to 80% of men will not visit a physician unless their spouse is actively involved, and therefore delays in diagnosis and management may also contribute to men’s poor health outcomes (Teo, Ling, & Ng, 2018). This has contributed to a lower male 5-year life expectancy compared to females (Teo et al., 2018).
Common behaviors known to predispose to disease include smoking and alcohol overuse, unhealthy sleep habits, unhealthy diet and sedentary lifestyle (Khan, Afaq, & Mukhtar, 2010; Sharma & Majumdar, 2009; Steyn & Damasceno, 2006). Understanding the relationship between unhealthy behaviors and comorbidities is critical to developing public awareness campaigns and interventions targeted to men (Bauer et al., 2016; Christensen, Gronbaek, Pedersen, Graugaard, & Frisch, 2011; Hassapidou et al., 2013). Messaging men is key to initiating behavior change and adaptation toward sustained health promoting lifestyle behaviors (Wakefield, Loken, & Hornik, 2010). Research supports that disease diagnosis can leverage “teachable moments” to garner illness management and instill behavioral changes to advance men’s overall well-being (Lawson & Flocke, 2009; Xiang, 2016).
By characterizing health behaviors among Canadian men, subsequent targeted interventions can be designed, implemented, and formally evaluated (Sodergren, 2013). The objective of our study was to broadly sample men to obtain information regarding health behaviors as a predictor of downstream male medical comorbidities.
Methods
Recruitment
Research ethics approval was obtained from the University of British Columbia. All participants provided written informed consent prior to enrolment in the study. A total of 5,362 Canadian respondents were sourced from an online sample provider (a company that provides specified populations to participate), which have reduced pre-recruitment field times and are more efficient for accessing target samples (Oliffe et al., 2018; Walter, Seibert, Goering, & O’Boyle Jr, 2018), to complete a 15-minute online survey between April 20th and 28th 2017. Incomplete surveys were excluded, as well as those who were female or completed the survey significantly faster than average (<5 minutes; Zhang & Conrad, 2014). Participants were male, aged 19 or older, and able to read French or English. The sample was stratified to reflect an accurate distribution of the Canadian population by both age and location as per the 2016 Canadian Census data.
Survey
The survey consisted of questions enquiring about health behaviors including smoking, alcohol usage, sleeping habits, dietary habits, and exercise. These behaviors were classified as “healthy” or “unhealthy” based on previously validated questionnaires when possible or if literature or guidelines existed for a behavioral threshold as indicated below. However, dietary behaviors were assessed solely based on expert opinion due to the lack of consistent data in the literature.
Participants’ smoking behaviors were categorized as healthy if they never smoked, or unhealthy if they currently smoked or had smoked previously (Husten, 2009; McCarthy, Meza, Jeon, & Moolgavkar, 2012; Statistics Canada, 2005). Alcohol consumption was categorized as healthy if their Audit-C score was equal to or less than 3, and unhealthy if greater than 3 (Caviness et al., 2009; Dawson, Grant, Stinson, & Zhou, 2005). Sleeping habits were classified as healthy if they received 7–9 hours a night, and unhealthy if <7 or >9 hours (Hirshkowitz et al., 2015). Exercise was characterized as healthy if they completed >150 minutes of moderate-to-strenuous exercise in a week, and unhealthy if <150 minutes (CSFE, 2011a, 2011b). Dietary habits were assessed using a modified version of the YouCheck diet score (with a refined sugar component; Pourmalek, Goldenberg, Ho, Skeldon, & Patrick, 2017). These items were based on dietary consumption of food groups associated with greater overall health and reduced morbidity such as increased fruit and vegetable consumption or increased unsaturated fat consumption (Nicoll, Howard, & Henein, 2015; Sabate & Wien, 2015). Unhealthy items were defined as increased consumption of refined sugar, saturated fat, and salt-abundant processed foods associated with increased morbidity and mortality (Clifton & Keogh, 2017; Li et al., 2017; Rust & Ekmekcioglu, 2017). The weekly frequency were recorded and categorized as healthy if their YouCheck diet score was >12, and unhealthy if <12 (Pourmalek et al., 2017).
Comorbidities were self-reported by participants based on having a formal diagnosis of a medical condition. Participants selected one or more medical conditions from a drop-down menu including heart disease, elevate cholesterol, type 1 and type 2 diabetes, malignancy, cerebrovascular accident (CVA), osteoarthritis, respiratory disease, bowel disease, and erectile dysfunction. Depression was recorded as a separate question and was labeled as present if their PHQ-9 score was >9 (Manea, Gilbody, & McMillan, 2012).
Statistical Methods
Descriptive analysis was performed on the participant population. Multivariate logistic regression was conducted to analyze healthy behaviors which predict various medical comorbidities, adjusting for participant demographic factors. Comorbidities that had low reported numbers in this series (a prevalence of <3%) were excluded from multivariate analysis. A two-sided p value of < .05 was considered significant. Statistical analyses were performed with Stata 14.1.
Results
Demographics
A total of 2,000 men aged 19–94 years were included in the study after both inclusion and exclusion criteria were met. Demographic data are listed in Table 1. The age distribution and geographic distribution is in alignment with the 2016 Canadian Census. Median age was 48 (interquartile range 34–60). Half (n = 1,003, 50%) of the participants were employed, 56% (n = 1,120) of participants had a household income of >$60,000, 50% (n = 998) had some university education, and a significant portion lived with a partner (n = 818, 41%).
Table 1.
Demographics of Survey Population (n = 2,000).
| Demographics and baseline characteristics | Number of participants (n, %) |
|---|---|
| Sex | |
| Male | 2,000 (100) |
| Age | |
| 19–29 | 379 (19.0) |
| 30–54 | 934 (46.7) |
| 55+ | 687 (34.4) |
| Province | |
| British Columbia | 265 (13.3) |
| Alberta | 217 (10.9) |
| Saskatchewan & Manitoba | 131 (6.6) |
| Ontario | 768 (38.4) |
| Quebec | 476 (23.8) |
| Maritime Provinces | 142 (7.1) |
| Territories | 1 (0.1) |
| Visible minority | |
| Yes | 218 (10.9) |
| No | 1782 (89.1) |
| Household income | |
| <$20,000 | 129 (6.5) |
| $20,000 to $39,999 | 336 (16.8) |
| $40,000 to $59,999 | 355 (17.8) |
| $60,000 to $79,999 | 278 (13.9) |
| $80,000 to $99,999 | 222 (11.1) |
| $100,000 to $119,999 | 222 (6.7) |
| $120,000 to 139,999 | 134 (6.7) |
| $140,000+ | 264 (13.2) |
| Highest level of education | |
| Primary school or less | 6 (0.3) |
| Some high school | 48 (2.4) |
| High school graduate | 301 (15.1) |
| Some college/trade school | 225 (11.3) |
| Graduated college/trade school | 422 (21.1) |
| Some university | 175 (8.8) |
| University undergraduate degree | 495 (24.8) |
| University graduate degree | 328 (16.4) |
| Sexual preference | |
| Heterosexual | 1805 (90.3) |
| Homosexual | 118 (5.9) |
| Bisexual | 48 (2.4) |
| Not sure or questioning | 25 (1.3) |
| Other | 4 (0.2) |
| Number of children aged <19 living with participant | |
| None | 1623 (81.2) |
| One | 177 (8.9) |
| Two | 140 (7.0) |
| Three | 42 (2.1) |
| Four+ | 18 (0.9) |
| Living arrangement | |
| Partner | 818 (40.9) |
| Alone | 449 (22.5) |
| Partner & children | 392 (19.6) |
| Parent | 178 (8.9) |
| Non-relatives | 54 (2.7) |
| Children | 49 (2.5) |
| Relatives | 41 (2.1) |
| University or college campus | 14 (0.7) |
| Other | 5 (0.3) |
| Employment | |
| Employed full-time | 1,003 (50.2) |
| Employed part-time | 155 (7.8) |
| Self-employed | 170 (8.5) |
| Looking for employment | 93 (4.7) |
| Unable to work | 63 (3.2) |
| Retired | 453 (22.7) |
| Studying full-time | 108 (5.4) |
| Studying part-time | 47 (2.4) |
| Home caregiver | 14 (0.7) |
| Total number of participants | 2,000 (100) |
Health Behaviors and Comorbidities
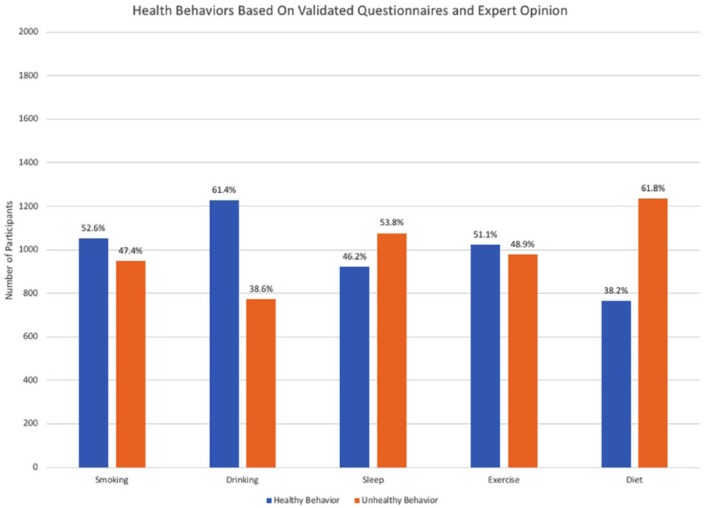
For each of the health behaviors, the distribution of healthy versus unhealthy individuals is described in Figure 1. Approximately half (n = 948, 48%) had unhealthy smoking behavior, 39% (n = 773) had unhealthy drinking behavior, 54% (n = 1,077) had unhealthy sleeping behavior, 49% (n = 977) had unhealthy exercise behavior, and 62% (n = 1,235) had unhealthy eating behaviors.
Figure 1.
Classification of five health behaviors as healthy or unhealthy based on validated questionnaires or expert opinion.
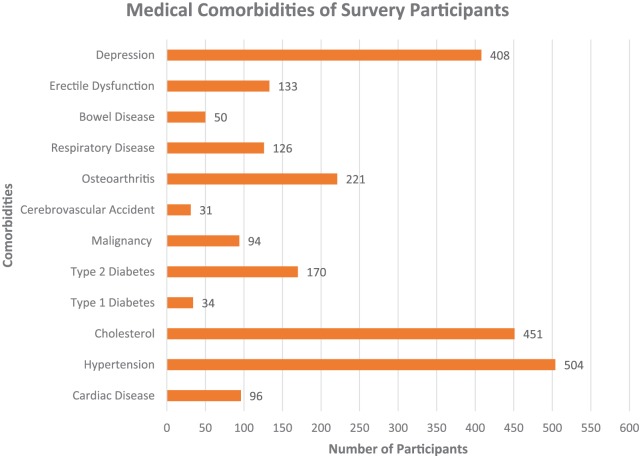
Participant comorbidities are described in Figure 2. The majority of participants were healthy, with hypertension (n = 504, 25.2%), elevated cholesterol (n = 451, 22.6%), and depression (n = 408, 20.4%) being the most common comorbidities. Less than 5% had a malignancy of some type. Fewest participants (<3%) had CVA, bowel disease, or type 1 diabetes. On average, respondents had 1.3 medical comorbidities.
Figure 2.
Commodities self-reported by participants as formal medical diagnoses.
Further breakdown of each comorbidity by unhealthy behavior is outlined in Table 2. For the unhealthy smoking group, hypertension (n = 287, 30.3%), high cholesterol (n = 268, 28.3%), and depression (n = 222, 23.4%) were found to be the most common medical comorbidities (n = 287, 30.3%). For the unhealthy drinking group, depression (n = 175, 22.6%) was the most commonly associated comorbidity. Among men with unhealthy sleep, unhealthy exercise, and unhealthy diet, hypertension (n = 287, 26.6%; n = 290, 29.7%; and n = 304, 24.6%, respectively) was the most common medical condition.
Table 2.
Number of Participants with Unhealthy Behaviors per Respective Medical Comorbidities.
| Number of men with unhealthy behaviors |
|||||
|---|---|---|---|---|---|
| Comorbidity | Smoking (n, %) (n = 948) |
Drinking (n, %) (n = 773) |
Sleep (n, %) (n = 1,077) |
Exercise (n, %) (n = 977) |
Diet (n, %) (n = 1,235) |
| Cardiac disease | 67 (7.1%) | 32 (4.1%) | 52 (4.8%) | 53 (5.4%) | 52 (4.2%) |
| Hypertension | 287 (30.3%) | 220 (2.8%) | 287 (26.6%) | 290 (29.7%) | 304 (24.6%) |
| Cholesterol | 268 (28.3%) | 176 (2.3%) | 241 (22.4%) | 258 (26.4%) | 267 (21.6%) |
| Type 1 diabetes | 16 (1.7%) | 10 (1.3%) | 19 (1.8%) | 20 (2.0%) | 20 (1.6%) |
| Type 2 diabetes | 112 (11.8%) | 50 (6.5%) | 96 (8.9%) | 105 (10.7%) | 104 (8.4%) |
| Malignancy | 63 (6.6%) | 36 (4.7%) | 44 (4.1%) | 47 (4.8%) | 57 (4.6%) |
| Cerebrovascular accident | 26 (2.7%) | 12 (1.6%) | 19 (1.8%) | 19 (1.9%) | 12 (1.0%) |
| Osteoarthritis | 141 (14.9%) | 85 (11.0%) | 124 (11.5%) | 130 (13.3%) | 128 (10.4%) |
| Respiratory disease | 78 (8.2%) | 50 (6.5%) | 71 (6.6%) | 61 (6.2%) | 82 (6.6%) |
| Bowel disease | 29 (3.1%) | 22 (2.8%) | 34 (3.2%) | 29 (3.0%) | 36 (2.9%) |
| Erectile dysfunction | 86 (9.1%) | 59 (7.6%) | 76 (7.1%) | 85 (8.7%) | 80 (6.5%) |
| Depression | 222 (23.4%) | 175 (22.6%) | 268 (24.9%) | 202 (20.7%) | 303 (24.5%) |
Multivariate Analysis
Multivariate analysis is illustrated in Table 3. Type 1 diabetes, bowel disease, and CVA were not included in the multivariate analysis (<3% prevalence). Overall unhealthy smoking predicted heart disease (OR 2.08, p < .01), elevated cholesterol (OR 1.35, p = .02), type 2 diabetes (OR 1.57, p = .02), osteoarthritis (OR 1.43, p = .04), and depression (OR 1.62, p < .01). Unhealthy drinking behavior predicted hypertension (OR 1.40, p < .01) and protected against type 2 diabetes (OR 0.61, p < .01). Unhealthy sleep predicted hypertension (OR 1.46, p < .01), erectile dysfunction (OR 1.50, p = .04), and depression (OR 1.87, p < .01). Unhealthy exercise predicted hypertension (OR 1.30, p = .03) and elevated cholesterol (OR 1.27, p = .05). Finally, unhealthy eating predicted depression (OR 1.65, p < .01).
Table 3.
Multivariate Analysis for Comorbidities Predicting Health Behaviors.**
| Health behaviors [OR (95% CI) & p value] |
|||||
|---|---|---|---|---|---|
| Comorbidity | Smoking | Drinking | Sleep | Exercise | Diet |
| Cardiac disease |
2.08 [1.26, 3.41]
p < .01 |
0.63 [0.40, 1.01] p = .06 |
1.15 [0.74, 1.80] p = .53 |
1.01 [0.64, 1.59] p = .96 |
0.82 [0.53, 1.29] p = .40 |
| Hypertension | 1.14 [0.89, 1.45] p = .29 |
1.40 [1.10, 1.77]
p < .01 |
1.46 [1.16, 1.84]
p < .01 |
1.30 [1.03, 1.64]
p = .03 |
1.14 [0.90, 1.45] p = .27 |
| Cholesterol |
1.35 [1.05, 1.73]
p = .02 |
0.99 [0.78, 1.27] p = .96 |
1.16 [0.92, 1.47] p = .22 |
1.27 [1.00, 1.62]
p = .05 |
1.00 [0.79, 1.27] p = 1.00 |
| Type 2 diabetes |
1.57 [1.08, 2.27]
p = .02 |
0.61 [0.42, 0.88]
p < .01 |
1.22 [0.86, 1.73] p = .26 |
1.37 [0.96, 1.95] p = .08 |
1.05 [0.74, 1.49] p = .80 |
| Malignancy | 1.61 [0.97, 2.67] p = .06 |
0.82 [0.51, 1.32] p = .41 |
1.03 [0.65, 1.64] p = .89 |
0.74 [0.47, 1.18] p = .21 |
1.44 [0.90, 2.31] p = .13 |
| Osteoarthritis |
1.43 [1.02, 2.00]
p = .04 |
1.01 [0.73, 1.40] p = .95 |
1.25 [0.91, 1.71] p = .18 |
1.10 [0.80, 1.52] p = .55 |
0.93 [0.68, 1.29] p = .68 |
| Respiratory disease | 1.39 [0.92, 2.10] p = .12 |
0.94 [0.64, 1.40] p = .77 |
1.25 [0.85, 1.83] p = .26 |
0.76 [0.51, 1.12] p = .17 |
1.20 [0.80, 1.79] p = .38 |
| Erectile dysfunction | 1.35 [0.89, 2.06] p = .16 |
1.34 [0.90, 2.98] p = .15 |
1.50 [1.02, 2.23]
p = .04 |
1.46 [0.98, 2.17] p = .07 |
1.10 [0.74, 1.64] p = .65 |
| Depression |
1.62 [1.25, 2.09]
p < .01 |
1.26 [0.98, 1.63] p = .07 |
1.87 [1.45, 2.40]
p < .01 |
1.13 [0.87, 1.45] p = .36 |
1.65 [1.27, 2.16]
p < .01 |
Note. *adjusted for age, ethnicity, employment, sexual orientation, geographic location, living conditions, education, and income. **Type 1 Diabetes, Bowel Disease, and Cerebrovascular Accident Were Excluded (<3% Prevalence).
Bold values highlights the significant associations as p values are also listed.
Interpretation
By affirming relationships between men’s unhealthy behaviors and medical comorbidities among a representative sample of Canadian men, this study identifies important opportunities to thoughtfully consider strategies for gender-sensitized interventions and public health messaging.
Looking at the common medical comorbidities described in the study analysis, cardiovascular disease including heart disease and elevated cholesterol was predicted by smoking behavior. Smoking is a well-known risk factor and preventable cause of cardiovascular disease (Gepner et al., 2011). Male smoking rates in Canada are rising (Statistics Canada, 2016) and this demands attention to the design and formal evaluation of targeted smoking cessation interventions. While some headway has been made with online interventions in this regard (Bottorff et al., 2016, 2017), there remains challenges in pre-empting the significant impact of cardiovascular disease on men’s lives (including work) and the lives of significant others (Bottorff, Oliffe, Sarbit, Kelly, & Cloherty, 2015).
Additionally, the comorbidity of elevated cholesterol was predicted by unhealthy exercise in this study. Numerous studies have demonstrated the strong protective effect of exercise on cholesterol levels independent of any medication, including beneficial effects on low density lipoproteins, high density lipoproteins, and triglyceride levels (Huffman et al., 2012; Mann, Beedie, & Jimenez, 2014; Wang & Xu, 2017).
Another comorbidity, hypertension was predicted by unhealthy sleeping behavior, alcohol consumption, and low exercise levels. It would be expected that hypertension was predicted by unhealthy exercise as aerobic exercise has significant favorable impacts on blood pressure (Wen & Wang, 2017). While exercise has been espoused as a health promotion practice that appeals to many men, a recent review by Bottorff, Oliffe, et al. (2015) revealed few programs that were explicitly designed for men, and/or formally evaluated (Bottorff, Seaton, et al., 2015; Caperchione et al., 2017). Numerous research teams (Faraut et al., 2012; Palagini et al., 2013; Wang et al., 2015) have examined the effect of sleep on hypertension, and while there are conflicting reports, many large studies have highlighted that reduced sleep having a significant impact on hypertension, most of which are unrelated to other conditions such as obstructive sleep apnea (Calhoun & Harding, 2010). Alcohol consumption has also been demonstrated to have a significant impact on hypertension; however, the mechanisms are not completely understood (Husain, Ansari, & Ferder, 2014).
Diabetes mellitus as a comorbidity was predicted by smoking, but alcohol consumption was protective for the development of type 2 diabetes. Smoking has been described as inducing type 2 diabetes through its impacts on insulin resistance and inflammation (Chang, 2012). Other studies have demonstrated results in keeping with the study findings that alcohol consumption may have a protective role and reduce the incidence of diabetes (Rasouli et al., 2013). Conversely, theories have been proposed suggesting excessive alcohol consumption causes insulin resistance and pancreatic beta-cell dysfunction, predisposing one to diabetes (Kim & Kim, 2012). This controversy suggests that interventions that prescribe manageable change such as “Don’t Change Much” may provide avenues for sustainable adjustments, employing harm reduction rather than necessitating a focus on abstinence (Krueger, Goldenberg, Koot, & Andres, 2017). Interestingly, diet in this study was not predictive but this may be due to heterogeneity of dietary recommendations for diabetic prevention and the study capturing diabetic patients who may have already made dietary modifications for control and further prevention of worsening disease as part of first line management (Asif, 2014; Povey & Clark-Carter, 2007). While numerous studies have shown that diet can be used as a preventative measure for diabetes, it is important to acknowledge that these effects are related more to attempting to reduce adiposity, decrease insulin resistance, and decrease glycemic index (Ley, Hamdy, Mohan, & Hu, 2014).
Malignancy as a comorbidity had no predictive behaviors as seen in this model. The etiology of malignancy continues to be studied many of which may have a genetic component (Pomerantz & Freedman, 2011). The low volume of malignancies in this patient population and lack of stratification into type of malignancy may explain the lack of associations seen. That said, longstanding empirical evidence reveals smoking, alcohol overuse, unhealthy diet, and low exercise levels are deeply implicated as epigenetic factors in some male malignancies (Alegria-Torres, Baccarelli, & Bollati, 2011; Hardy & Tollefsbol, 2011; Lee & Pausova, 2013; Varela-Rey, Woodhoo, Martinez-Chantar, Mato, & Lu, 2013). Moreover, perhaps cause-effect messages linking specific men’s behaviors with disease outcomes might be abandoned here with a strength-based focus suggesting healthy lifestyles can protect, or delay, progression of malignancies.
The comorbidity of osteoarthritis in this study was predicted by smoking. This is supported by some studies in the literature which have demonstrated a detrimental effect of smoking (Amin et al., 2007). It has been suggested that this harmful effect may be due to the impact of smoking on joint cartilage, including increased oxidant stress, increased tissue hypoxia, and inhibition of cell proliferation, which can result in accelerated cartilage loss (Felson & Zhang, 2015). However, this is controversial as other studies have also described a protective effect of smoking (Felson & Zhang, 2015) and some have suggested no association at all (Dube et al., 2016). In the absence of definitive correlation and in keep with smoking as a risk factor for many other conditions, this is certainly a reasonable target for messaging along with the strategy of remaining as active as possible, as exercise may help prevent osteoarthritis (Hunter & Eckstein, 2009).
In this study, no behavioral predictors of the respiratory disease comorbidity. This could be explained by the generalization of respiratory pathology which may be cofounded with respiratory diseases of childhood rather than acquired respiratory disease due to health behaviors.
Erectile dysfunction as a comorbidity is an indicator of general health and strong predictor of cardiovascular comorbidity (Salonia et al., 2013), and was predicted by unhealthy sleep in this study. Research has illustrated a relationship between sleep disorders and specifically obstructive sleep apnea and erectile dysfunction; evidence suggests that patients presenting with erectile dysfunction, especially those who are treatment refractory, should be assessed for sleep disorders (Jankowski, Seftel, & Strohl, 2008; Kalejaiye et al., 2017).
Depression as a comorbidity was predicted by smoking, unhealthy sleep, and unhealthy eating. Smoking has been described as an independent predictor of depression in some patient populations including those with coronary artery disease (Stafford, Berk, & Jackson, 2013). Overall, the literature demonstrates conflicting evidence for the direction of the association between smoking and depression and indicates the need for further work to determine the true casual direction of this relationship (Fluharty, Taylor, Grabski, & Munafo, 2017). Similarly, while sleep deprivation and chronic fatigue have been highlighted as risk factors for the development of depressive symptoms and illness, there also does exist a bi-directional association (Al-Abri, 2015). In addition to depression, sleep disturbance also has an impact on other psychiatric illness such as anxiety, and therefore sleep patterns warrant screening in individuals with psychiatric illness (Krystal, 2012; Luca, Luca, & Calandra, 2013). Finally, unhealthy diet has been linked to depressive illness, including diets low in carbohydrates, altered protein diets which affect dopamine availability from amino acid breakdown, diets with low omega-3 fatty acids as well as those in vitamins and minerals (O’Neil et al., 2014; Rao, Asha, Ramesh, & Rao, 2008). Nutritional psychiatry has actually developed as a field that warrants more research and studies to understand the complex nature of diet and mental illness as well as the relationship between the gut microbiome and mental illness (Evrensel & Ceylan, 2015; Jacka, 2017).
Limitations to this study include the cross-sectional study design and recall bias associated with survey-based studies. This may lead to misclassification of data. The analysis also implies association between two factors and therefore causation cannot necessarily be implied. Despite a fairly robust sample size, some disease entities are rare and are likely underpowered to show an adequate association, and therefore type 1 diabetes, bowel disease, and CVA were excluded from analysis as their prevalence was <3%. A subset of patients also may have already made behavioral lifestyle changes after acquiring a disease or new diagnosis, and since the study is cross-sectional, behavior data prior to this time point may not be captured, and therefore these individuals still remain candidates for intervention. Some of the unhealthy behavior data may also be a result of testosterone deficiency but this cannot be evaluated in this type of survey. Finally, the reported dietary data does not rely on any validated method as there is a lack of any true consensus in the literature for a standardized dietary questionnaire (Shim, Oh, & Kim, 2014).
Conclusion
This study emphasizes that unhealthy behaviors are associated with comorbidities among men and provides evidence to affirm health-care providers’ efforts for promoting lifestyle change. The study findings have demonstrated that common behaviors such as smoking are associated with cardiac disease, type 2 diabetes, elevated cholesterol, osteoarthritis, and depression, and alcohol consumption is associated with hypertension and type 2 diabetes. Unhealthy sleep is associated with hypertension, erectile dysfunction, and depression, and unhealthy exercise is associated with hypertension, elevated cholesterol, and erectile dysfunction. Unhealthy diets are associated with depression.
With increasing morbidity and mortality among men with lifestyle-related comorbidities, interest exists to investigate and influence the intricacies of lifestyle. Ultimately these data can guide health-care providers to identify predictors of disease earlier on, and employ timely targeted screening and preventative health-care interventions and strategies.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Canadian Men’s Health Foundation. Public Health Agency of Canada; American Urologic Association, New York Section E. Darracott Vaughan MD Research Scholar Award (RF).
References
- Al-Abri M. A. (2015). Sleep deprivation and depression: A bi-directional association. Sultan Qaboos University Medical Journal, 15(1), e4–e6. [PMC free article] [PubMed] [Google Scholar]
- Alegria-Torres J. A., Baccarelli A., Bollati V. (2011). Epigenetics and lifestyle. Epigenomics, 3(3), 267–277. doi: 10.2217/epi.11.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amin S., Niu J., Guermazi A., Grigoryan M., Hunter D. J., Clancy M., … Felson D. T. (2007). Cigarette smoking and the risk for cartilage loss and knee pain in men with knee osteoarthritis. Annals of the Rheumatic Disease, 66(1), 18–22. doi: 10.1136/ard.2006.056697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asif M. (2014). The prevention and control the type-2 diabetes by changing lifestyle and dietary pattern. Journal of Education and Health Promotion, 3, 1. doi: 10.4103/2277-9531.127541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer I. E., Galvez J. F., Hamilton J. E., Balanza-Martinez V., Zunta-Soares G. B., Soares J. C., Meyer T. D. (2016). Lifestyle interventions targeting dietary habits and exercise in bipolar disorder: A systematic review. Journal of Psychiatric Research, 74, 1–7. doi: 10.1016/j.jpsychires.2015.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottorff J. L., Oliffe J. L., Sarbit G., Caperchione C., Clark M., Anand A., Howay K. (2017). Assessing the feasibility, acceptability and potential effectiveness of an integrated approach to smoking cessation for new and expectant fathers: The Dads in Gear study protocol. Contemporary Clinical Trials, 54, 77–83. doi: 10.1016/j.cct.2017.01.002 [DOI] [PubMed] [Google Scholar]
- Bottorff J. L., Oliffe J. L., Sarbit G., Kelly M. T., Cloherty A. (2015). Men’s responses to online smoking cessation resources for new fathers: The influence of masculinities. Journal of Medical Internet Research Protocols, 4(2), e54. doi: 10.2196/resprot.4079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottorff J. L., Oliffe J. L., Sarbit G., Sharp P., Caperchione C. M., Currie L. M., … Stolp S. (2016). Evaluation of quitnow men: An online, men-centered smoking cessation intervention. Journal of Medical Internet Research, 18(4), e83. doi: 10.2196/jmir.5076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottorff J. L., Seaton C. L., Johnson S. T., Caperchione C. M., Oliffe J. L., More K., … Tillotson S. M. (2015). An updated review of interventions that include promotion of physical activity for adult men. Sports Medicine, 45(6), 775–800. doi: 10.1007/s40279-014-0286-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calhoun D. A., Harding S. M. (2010). Sleep and hypertension. Chest, 138(2), 434–443. doi: 10.1378/chest.09-2954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Canada. (2017). How healthy are Canadians? A trend analysis of the health of Canadians from a healthy living and chronic disease perspective (pp. 1–46). Public Health Agency of Canada. Retrieved from https://www.canada.ca/en/public-health/services/publications/healthy-living/how-healthy-canadians.html
- Statistics Canada. (2005). Canadian Tobacco Use Monitoring Survey (CTUMS) 2005 Cycle 1 Questionnaire. Retrieved from http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=22693&dis=1
- Statistics Canada. (2016). Smokers, by sex, provinces and territories. Table 13-10-0096-10. Retrieved from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009610
- Caperchione C. M., Bottorff J. L., Oliffe J. L., Johnson S. T., Hunt K., Sharp P., … Goldenberg S. L. (2017). The HAT TRICK programme for improving physical activity, healthy eating and connectedness among overweight, inactive men: Study protocol of a pragmatic feasibility trial. British Medical Journal Open, 7(9), e016940. doi: 10.1136/bmjopen-2017-016940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caviness C. M., Hatgis C., Anderson B. J., Rosengard C., Kiene S. M., Friedmann P. D., Stein M. D. (2009). Three brief alcohol screens for detecting hazardous drinking in incarcerated women. Journal of Studies on Alcohol and Drugs, 70(1), 50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang S. A. (2012). Smoking and type 2 diabetes mellitus. Diabetes and Metabolism Journal, 36(6), 399–403. doi: 10.4093/dmj.2012.36.6.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen B. S., Gronbaek M., Pedersen B. V., Graugaard C., Frisch M. (2011). Associations of unhealthy lifestyle factors with sexual inactivity and sexual dysfunctions in Denmark. Journal of Sexual Medicine, 8(7), 1903–1916. doi: 10.1111/j.1743-6109.2011.02291.x [DOI] [PubMed] [Google Scholar]
- Clifton P. M., Keogh J. B. (2017). A systematic review of the effect of dietary saturated and polyunsaturated fat on heart disease. Nutrition, Metabolism and Cardiovascular Diseases, 27(12), 1060–1080. doi: 10.1016/j.numecd.017.10.0102 [DOI] [PubMed] [Google Scholar]
- CSFE P. (2011. a). Canadian Physical Activity Guidelines for Adults 18–64 years. [Google Scholar]
- CSFE P. (2011. b). Canadian Physical Activity Guidelines For Adults 65 years & Older. [Google Scholar]
- Danaei G., Ding E. L., Mozaffarian D., Taylor B., Rehm J., Murray C. J., Ezzati M. (2009). The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Medicine, 6(4), e1000058. doi: 10.1371/journal.pmed.1000058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D. A., Grant B. F., Stinson F. S., Zhou Y. (2005). Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcoholism: Clinical And Experimental Research, 29(5), 844–854. [DOI] [PubMed] [Google Scholar]
- Dube C. E., Liu S. H., Driban J. B., McAlindon T. E., Eaton C. B., Lapane K. L. (2016). The relationship between smoking and knee osteoarthritis in the osteoarthritis initiative. Osteoarthritis Cartilage, 24(3), 465–472. doi: 10.1016/j.joca.2015.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evrensel A., Ceylan M. E. (2015). The gut-brain axis: The missing link in depression. Clinical Psychopharmacology and Neuroscience, 13(3), 239–244. doi: 10.9758/cpn.2015.13.3.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraut B., Touchette E., Gamble H., Royant-Parola S., Safar M. E., Varsat B., Leger D. (2012). Short sleep duration and increased risk of hypertension: A primary care medicine investigation. Journal of Hypertension, 30(7), 1354–1363. doi: 10.1097/HJH.0b013e32835465e5 [DOI] [PubMed] [Google Scholar]
- Felson D. T., Zhang Y. (2015). Smoking and osteoarthritis: A review of the evidence and its implications. Osteoarthritis Cartilage, 23(3), 331–333. doi: 10.1016/j.joca.2014.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fluharty M., Taylor A. E., Grabski M., Munafo M. R. (2017). The association of cigarette smoking with depression and anxiety: A Systematic Review. Nicotine & Tobacco Research, 19(1), 3–13. doi: 10.1093/ntr/ntw140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gepner A. D., Piper M. E., Johnson H. M., Fiore M. C., Baker T. B., Stein J. H. (2011). Effects of smoking and smoking cessation on lipids and lipoproteins: Outcomes from a randomized clinical trial. American Heart Journal, 161(1), 145–151. doi: 10.1016/j.ahj.2010.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy T. M., Tollefsbol T. O. (2011). Epigenetic diet: Impact on the epigenome and cancer. Epigenomics, 3(4), 503–518. doi: 10.2217/epi.11.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassapidou M., Papadopoulou S. K., Vlahavas G., Kapantais E., Kaklamanou D., Pagkalos I., … Tzotzas T. (2013). Association of physical activity and sedentary lifestyle patterns with obesity and cardiometabolic comorbidities in Greek adults: Data from the National Epidemiological Survey. Hormones (Athens), 12(2), 265–274. [DOI] [PubMed] [Google Scholar]
- Hirshkowitz M., Whiton K., Albert S. M., Alessi C., Bruni O., DonCarlos L., … Ware J. C. (2015). National sleep foundation’s updated sleep duration recommendations: Final report. Sleep Health, 1(4), 233–243. doi: 10.1016/j.sleh.2015.10.004 [DOI] [PubMed] [Google Scholar]
- Huffman K. M., Hawk V. H., Henes S. T., Ocampo C. I., Orenduff M. C., Slentz C. A., … Bales C. W. (2012). Exercise effects on lipids in persons with varying dietary patterns-does diet matter if they exercise? Responses in studies of a targeted risk reduction intervention through defined exercise I. American Heart Journal, 164(1), 117–124. doi: 10.1016/j.ahj.2012.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter D. J., Eckstein F. (2009). Exercise and osteoarthritis. Journal of Anatomy, 214(2), 197–207. doi: 10.1111/j.1469-7580.2008.01013.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husain K., Ansari R. A., Ferder L. (2014). Alcohol-induced hypertension: Mechanism and prevention. World Journal of Cardiology, 6(5), 245–252. doi: 10.4330/wjc.v6.i5.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husten C. G. (2009). How should we define light or intermittent smoking? Does it matter? Nicotine & Tobacco Research, 11(2), 111–121. doi: 10.1093/ntr/ntp010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacka F. N. (2017). Nutritional psychiatry: Where to next? EBioMedicine, 17, 24–29. doi: 10.1016/j.ebiom.2017.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankowski J. T., Seftel A. D., Strohl K. P. (2008). Erectile dysfunction and sleep related disorders. Journal of Urology, 179(3), 837–841. doi: 10.1016/j.juro.2007.10.024 [DOI] [PubMed] [Google Scholar]
- Kalejaiye O., Raheem A. A., Moubasher A., Capece M., McNeillis S., Muneer A., … Ralph D. J. (2017). Sleep disorders in patients with erectile dysfunction. British Journal of Urology International, 120(6), 855–860. doi: 10.1111/bju.13961 [DOI] [PubMed] [Google Scholar]
- Khan N., Afaq F., Mukhtar H. (2010). Lifestyle as risk factor for cancer: Evidence from human studies. Cancer Letters, 293(2), 133–143. doi: 10.1016/j.canlet.2009.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. J., Kim D. J. (2012). Alcoholism and diabetes mellitus. Diabetes & Metabolism, 36(2), 108–115. doi: 10.4093/dmj.2012.36.2.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. W. (2015). Men’s health: What should we know? World Journal of Men’s Health, 33(2), 45–49. doi: 10.5534/wjmh.2015.33.2.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger H., Goldenberg S. L., Koot J., Andres E. (2017). Don’t change much. American Journal of Men’s Health, 11(2), 275–283. doi: 10.1177/1557988316671567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krystal A. D. (2012). Psychiatric disorders and sleep. Neurology Clinics, 30(4), 1389–1413. doi: 10.1016/j.ncl.2012.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson P. J., Flocke S. A. (2009). Teachable moments for health behavior change: A concept analysis. Patient Education and Counseling, 76(1), 25–30. doi: 10.1016/j.pec.2008.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K. W., Pausova Z. (2013). Cigarette smoking and DNA methylation. Frontier in Genetics, 4, 132. doi: 10.3389/fgene.2013.00132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ley S. H., Hamdy O., Mohan V., Hu F. B. (2014). Prevention and management of type 2 diabetes: Dietary components and nutritional strategies. Lancet, 383(9933), 1999–2007. doi: 10.1016/S0140-6736(14)60613-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li N., Petrick J. L., Steck S. E., Bradshaw P. T., McClain K. M., Niehoff N. M., … Gammon M. D. (2017). A pooled analysis of dietary sugar/carbohydrate intake and esophageal and gastric cardia adenocarcinoma incidence and survival in the USA. International Journal of Epidemiology, 46(6), 1836–1846. doi: 10.1093/ije/dyx203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luca A., Luca M., Calandra C. (2013). Sleep disorders and depression: Brief review of the literature, case report, and nonpharmacologic interventions for depression. Clinical Interventions in Aging, 8, 1033–1039. doi:s10.2147/CIA.S47230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manea L., Gilbody S., McMillan D. (2012). Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. Canadian Medical Association Journal, 184(3), E191–E196. doi: 10.1503/cmaj.110829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann S., Beedie C., Jimenez A. (2014). Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: Review, synthesis and recommendations. Sports Medicine, 44(2), 211–221. doi: 10.1007/s40279-013-0110-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy W. J., Meza R., Jeon J., Moolgavkar S. H. (2012). Chapter 6: Lung cancer in never smokers: Epidemiology and risk prediction models. Risk Analysis, 32(Suppl 1), S69–S84. doi: 10.1111/j.1539-6924.2012.01768.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicoll R., Howard J. M., Henein M. Y. (2015). A review of the effect of diet on cardiovascular calcification. International Journal of Molecular Sciences, 16(4), 8861–8883. doi: 10.3390/ijms16048861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliffe J. L., Rice S., Kelly M. T., Ogrodniczuk J. S., Broom A., Robert S., Black N. (2018). A Mixed-Methods Study Of The Health-Related Masculine Values Among Young Canadian Men. Psychology of Men & Masculinity. Advance online publication. doi:10.1037/men0000157 [Google Scholar]
- O’Neil A., Quirk S. E., Housden S., Brennan S. L., Williams L. J., Pasco J. A., … Jacka F. N. (2014). Relationship between diet and mental health in children and adolescents: A systematic review. American Journal of Public Health, 104(10), e31–e42. doi: 10.2105/AJPH.2014.302110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palagini L., Bruno R. M., Gemignani A., Baglioni C., Ghiadoni L., Riemann D. (2013). Sleep loss and hypertension: A systematic review. Current Pharmaceutical Design, 19(13), 2409–2419. [DOI] [PubMed] [Google Scholar]
- Pomerantz M. M., Freedman M. L. (2011). The genetics of cancer risk. Cancer Journal, 17(6), 416–422. doi: 10.1097/PPO.0b013e31823e5387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourmalek F., Goldenberg S. L., Ho K., Skeldon S. C., Patrick D. M. (2017). Development and case-control validation of the Canadian Men’s Health Foundation’s self risk-assessment tool: “You check”. Journal of Men’s Health, 13, e9–e18. [Google Scholar]
- Povey R. C., Clark-Carter D. (2007). Diabetes and healthy eating: A systematic review of the literature. Diabetes Education, 33(6), 931–959; discussion 960–931. doi: 10.1177/0145721707308408 [DOI] [PubMed] [Google Scholar]
- Rao T. S., Asha M. R., Ramesh B. N., Rao K. S. (2008). Understanding nutrition, depression and mental illnesses. Indian Journal of Psychiatry, 50(2), 77–82. doi: 10.4103/0019-5545.42391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasouli B., Ahlbom A., Andersson T., Grill V., Midthjell K., Olsson L., Carlsson S. (2013). Alcohol consumption is associated with reduced risk of type 2 diabetes and autoimmune diabetes in adults: Results from the Nord-Trondelag health study. Diabetic Medicine, 30(1), 56–64. doi: 10.1111/j.1464-5491.2012.03713.x [DOI] [PubMed] [Google Scholar]
- Rust P., Ekmekcioglu C. (2017). Impact of salt intake on the pathogenesis and treatment of hypertension. Advances in Experimental Medicine and Biology, 956, 61–84. doi: 10.1007/5584_2016_147 [DOI] [PubMed] [Google Scholar]
- Sabate J., Wien M. (2015). A perspective on vegetarian dietary patterns and risk of metabolic syndrome. British Journal of Nutrition, 113(Suppl 2), S136–S143. doi: 10.1017/S0007114514004139 [DOI] [PubMed] [Google Scholar]
- Salonia A., Capogrosso P., Clementi M. C., Castagna G., Damiano R., Montorsi F. (2013). Is erectile dysfunction a reliable indicator of general health status in men? Arab Journal of Urology, 11(3), 203–211. doi: 10.1016/j.aju.2013.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma M., Majumdar P. K. (2009). Occupational lifestyle diseases: An emerging issue. Indian Journal of Occupational and Environmental Medicine, 13(3), 109–112. doi: 10.4103/0019-5278.58912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim J. S., Oh K., Kim H. C. (2014). Dietary assessment methods in epidemiologic studies. Epidemiology and Health, 36, e2014009. doi: 10.4178/epih/e2014009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sodergren M. (2013). Lifestyle predictors of healthy ageing in men. Maturitas, 75(2), 113–117. doi: 10.1016/j.maturitas.2013.02.011 [DOI] [PubMed] [Google Scholar]
- Stafford L., Berk M., Jackson H. J. (2013). Tobacco smoking predicts depression and poorer quality of life in heart disease. BMC Cardiovascular Disorders, 13, 35. doi: 10.1186/1471-2261-13-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steyn K., Damasceno A. (2006). Lifestyle and related risk factors for chronic diseases. In Jamison D. T., Feachem R. G., Makgoba M. W., Bos E. R., Baingana F. K., Hofman K. J., Rogo K. O. (Eds.), Disease and mortality in Sub-Saharan Africa. Washington, DC: World Bank. [PubMed] [Google Scholar]
- Teo C. H., Ling C. J., Ng C. J. (2018). Improving health screening uptake in men: A systematic review and meta-analysis. American Journal of Preventative Medicine, 54(1), 133–143. doi: 10.1016/j.amepre.2017.08.028 [DOI] [PubMed] [Google Scholar]
- Varela-Rey M., Woodhoo A., Martinez-Chantar M. L., Mato J. M., Lu S. C. (2013). Alcohol, DNA methylation, and cancer. Alcohol Research, 35(1), 25–35. [PMC free article] [PubMed] [Google Scholar]
- Wakefield M. A., Loken B., Hornik R. C. (2010). Use of mass media campaigns to change health behaviour. Lancet, 376(9748), 1261–1271. doi: 10.1016/S0140-6736(10)60809-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter S. L., Seibert S. E., Goering D., O’Boyle E. H. Jr. (2018). A tale of two sample sources: Do results from online panel data and conventional data converge? Journal of Business and Psychology. Advance online publication. doi: 10.1007/s10869-018-9552-y [DOI] [Google Scholar]
- Wang Y., Mei H., Jiang Y. R., Sun W. Q., Song Y. J., Liu S. J., Jiang F. (2015). Relationship between duration of sleep and hypertension in adults: A meta-analysis. Journal of Clinical Sleep Medicine, 11(9), 1047–1056. doi: 10.5664/jcsm.5024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Xu D. (2017). Effects of aerobic exercise on lipids and lipoproteins. Lipids in Health and Disease, 16(1), 132. doi: 10.1186/s12944-017-0515-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H., Wang L. (2017). Reducing effect of aerobic exercise on blood pressure of essential hypertensive patients: A meta-analysis. Medicine (Baltimore), 96(11), e6150. doi: 10.1097/MD.0000000000006150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett W. C., Koplan J. P., Nugent R., Dusenbury C., Puska P., Gaziano T. A. (2006). Prevention of chronic disease by means of diet and lifestyle changes. In Jamison D. T., Breman J. G., Measham A. R., Alleyne G., Claeson M., Evans D. B., Jha P., Mills A., Musgrove P. (Eds.), Disease control priorities in developing countries. Washington, DC: World Bank. [PubMed] [Google Scholar]
- Xiang X. (2016). Chronic disease diagnosis as a teachable moment for health behavior changes among middle-aged and older adults. Journal of Aging and Health, 28(6), 995–1015. doi: 10.1177/0898264315614573 [DOI] [PubMed] [Google Scholar]
- Zhang C., Conrad F. (2014). Speeding in web surveys: The tendency to answer very fast and its association with straightlining. Survey Research Methods, 8(2), 127–135. [Google Scholar]