Abstract
Polycystic ovary syndrome (PCOS) is known as the most common hormonal disorder in women at reproductive age. Recent studies have revealed a high prevalence of sleep disorders in PCOS, suggesting that it is an amendable factor for these patients; however, the sleep was not considered in their treatment plan. According to the Iranian traditional medicine (ITM), sleep is an important item in the lifestyle modification of all diseases. The aim of this study is to determine the importance of sleep hygiene in PCOS from the view of ITM and Modern Medicine. In this study, some keywords about “sleep and PCOS” were searched in medical databases and some ITM books. Lifestyle modification is one of the first steps in treatment of patients with PCOS in which the emphasis will be mainly on exercise and diet. Despite proof of the high prevalence of sleep disorders in these patients, modification of sleep is not considered in their lifestyle. ITM as a holistic medicine emphasizes on lifestyle modification under the title of “Settah-e-Zaruria” (In Persian), the six essential schemes for the prevention and treatment of all diseases. Management of sleep is one of these schemes. There are many advices about sleep hygiene in both ITM and modern medicine. It seems that lifestyle modification should be expanded in PCOS patients to include more options, and sleep hygiene should be considered in their lifestyle alongside food and exercise.
Keywords: Iranian traditional medicine, modern medicine, polycystic ovary syndrome, sleep
Introduction
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder among women, affecting 5%–10% of women in the reproductive age.[1] The syndrome is surrounded by controversies over both its diagnosis and treatment.[2,3] PCOS is defined by the Rotterdam criteria, as the existence of any two of the following three: (1) Oligoovulation and/or anovulation; (2) Biochemical or clinical document of hyperandrogenism; and (3) Polycystic ovaries in ultrasound.[4,5] However, according to the National Institute of Health criteria, the simultaneous presence of anovulation and hyperandrogenemia (clinical and/or biochemical) are required for PCOS diagnosis, excluding the reference to ovarian morphology.[4,6]
Women with PCOS are prone to a wide range of metabolic and reproductive disorders.[7,8] The pathogenesis of PCOS is uncertain. Some studies have valued potential contributors including insulin resistance, heredity and genetics factors, abnormal gonadotropin secretion and ovarian factors,[9,10,11] even though lifestyle may be the main factor.[12,13] There are several options for PCOS treatment such as drug administration and some surgical treatments; however, lifestyle modification that includes diet and exercise is the first and most important treatment strategy for these patients. Thus, before initiating any intervention, the lifestyle modification needs to be considered.[6,14,15,16,17]
Complementary and alternative medicine (CAM) is well-defined as a group of different medical and health-care systems, products and practices, that are not a part of conventional medicine.[18] CAM is an increasingly popular choice worldwide.[19] Iranian traditional medicine (ITM) includes the whole knowledge and practices employed in diagnosis, prevention, and treatment of diseases in Persia from ancient times to the present.[20] In ITM, six essential factors, known as “Settah-e-Zaruria” (In Persian), should be improved for prevention and treatment of all diseases and ITM practitioners consider these factors to change the lifestyle of their patients. These factors include weather, food and drinks, rest and movement, sleep and wakefulness, retention and excretion as well as mental status. Imbalances in any of these essential factors will affect human health and cause various diseases.[21] One of these six schemes is sleep management.[22]
Furthermore, sleep disorders are very common in patients with PCOS. These disorders include daytime sleepiness, difficulty falling asleep as well as sleep breathing disorders[3,23,24] that can significantly reduce sleep quality in these patients.[25]
It seems that sleep disorders are an important aspect of PCOS with negative effects on quality of life in these patients. Despite this, sleep management in PCOS patients has not been considered in modern medicine.[26] There are a lot of recommendations about sleep hygiene in modern medicine and ITM, which can be useful in PCOS management. A search was done but no article titled as “sleep hygiene in PCOS” was found. The aim of this study was to determine the importance of sleep hygiene in PCOS from the view of ITM and Modern Medicine. After clarification of this importance, it is recommended that sleep hygiene be considered in lifestyle modification of these patients as the first-line treatment.
Methods
In this review, some keywords including “lifestyle, sleep, sleep hygiene, insomnia, and PCOS (PCOS and polycystic ovarian syndrome)” were searched in the medical databases of PubMed, Google Scholar, Scopus, Irandoc, Magiran, and Scientific Information Database. The searches were limited to studies published in English and Persian languages from 1980 to 2016. We checked all titles and abstracts. Full texts of articles were reviewed in the relevant studies. Articles with their full texts being not available were rejected. In addition, the most important ITM books such as al-Hawi fi al-Tibb by “Rhazes” (9th and 10th centuries), al-Qanun fi al-Tibb by “Avicenna” (10th and 11th centuries), Zakhireye Kharazmshahi and Khofi-e-Alaii by “Jorjani” (11th and 12th centuries), Ghanonche by “Chaghmini” (14th century), Kholasat al-Hekmah by “AqiliKhorasani” (18th century), and so on were also studied. Issues about importance sleep in PCOS were gathered and analyzed by consensus and discussion with two of the review authors.
Results and Discussion
The physiology of sleep and its disorders
Sleep is a normal condition of the body which follows a periodic pattern accompanied by a reduction in its physiological role.[27,28] Poor sleep quality leads to excessive daytime sleepiness, memory impairment, neurocognitive dysfunction, fatigue, anxiety, depression, dysglycemia, declined immune function, systemic inflammation, atherosclerosis, and cardiovascular events.[23,29] During the sequence of night, an individual's sleep is divided into nonrapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. REM sleep is also called dreaming sleep since it is associated with dreaming, or paradoxical sleep because the brain waves in the electroencephalogram come to be activated during this state of sleep. NREM sleep is considered to be orthodox sleep or slow wave sleep (SWS), because of falling of physiological and psychological activities.[30,31]
There are eight wide categories of sleep disorders, with their subcategories. The main categories include as follows: Insomnia, hypersomnia, sleep-related breathing disorders, for example, obstructive sleep apnea, parasomnia, circadian rhythm sleep disorders, sleep-related movement disorders, isolated symptoms, and normal variants.[32]
Sleep disorder in polycystic ovary syndrome
Many research studies have revealed that sleep disorders have a significantly higher prevalence in patients with PCOS compared to healthy individuals.[33,34,35] Thus, sleep disturbance could be an important feature of PCOS[26] and assessment of the health status in PCOS should include a concern of sleep quality and the right approach to reduce these disorders and improve the quality of life in these patients.[34,35] However, recent studies suggest that more than 90% of physicians, who manage PCOS women, are rarely trained about the sleep disorders in these patients.[26] Poor sleep in PCOS patients is associated with depression, increased insulin resistance, obesity, cardiovascular diseases, etc.[10,34]
The short duration of nocturnal sleep, less amounts of REM sleep, excessive daytime sleepiness, insomnia, and poor sleep quality are also common in patients with PCOS.[24,31,36] The most common sleep disorder in PCOS patients is obstructive sleep apnea (OSA). OSA is highly prevalent, on the average of 2–3 times,[6] in women with PCOS compared to women without PCOS of the same age and weight.[3,37,38] Apnea is defined as a period of no airflow for at least 5.0 s.[39] Some clinical signs of OSA are daytime sleepiness, snoring, breathing disturbances, interrupted sleep, hypercapnia, hypoxemia, and high sympathetic activity.[40,41] Some adverse effects of this disorder are sleep fragmentation, daytime sleepiness, hypertension, ischemic heart disease, stroke, and metabolic disorders as insulin resistance, glucose intolerance, type II diabetes mellitus, and dyslipidemia.[3,10,36,41] OSA is generally treated with continuous positive airway pressure (CPAP) or mandibular advancement devices that are helpful in lessening sleep disorder in these patients.[42,43]
Neurohormones in sleep pattern of patients with polycystic ovary syndrome
Stress hormones and melatonin are some neurohormones involved in the sleep-wake cycle.[44] Melatonin, synthesized in the pineal gland, plays an important role in the regulation of sleep-wake cycle (circadian rhythm).[45] Melatonin is produced and released rhythmically, during the day-night cycle and is suppressed by light.[46,47] Nocturnal melatonin secretion declines in a shorter duration of night and day sleep leading to lower levels of melatonin.[45,48] Melatonin also plays a vital role in reproductive processes, namely, ovarian function.[49] It may affect gonadal function and secretion of sexual hormones,[45,50] follicular development, oocyte maturation, ovulation, and oocyte quality.[49,51] High levels of melatonin metabolite in urine are accompanied with poor sleep quality and an increase in oxidative stress in untreated PCOS women compared with their treated counterparts.[50] A decrease in melatonin metabolite with the reduction in serum luteinizing hormone, follicle stimulating hormone, dehydroepiandrosterone, and testosterone levels during treatment, was suggestive of a correlation between melatonin and sex steroids in PCOS patients.[25,50]
Recent studies have shown that a reduced sleep duration and poor quality of sleep can affect hypothalamic-pituitary-adrenal (HPA) axis activity.[36,52] The sympathetic system is more active in PCOS patients with poor sleep, especially in people who sleep during the day. Zafari Zangeneh et al., showed that the levels of adrenaline and noradrenaline were higher in PCOS patients compared to non-PCOS women. They also showed that the levels of cortisol in PCOS women who wake up early and women with the proper sleep of about 8 h were significantly lower than other PCOS women.[44] These findings showed that the level of cortisol as an indicator for the HPA axis can be influenced not only by the time of sleep and awakening but also by the duration of nocturnal sleep.[44,53] Appropriate regulatory control of the HPA axis is critical in PCOS patients and leads to a reduction of the adrenal hyperandrogenism, thereby reducing the clinical and laboratory signs in these patients.[54,55] Thus, it seems that modifying sleep patterns in PCOS patients could be used to regulate hormonal balance in the HPA and brain-ovary axis and may have important roles in the management of PCOS.[44,48]
Sleep hygiene in modern medicine
Sleep hygiene is known as the set of behavioral and environmental advice that are planned for encouraging healthy sleeping and were developed to treat sleep disorders. In sleep hygiene education, patients receive healthy sleep habits and are refreshed to apply a set of recommendations to recover their sleep.[23,56]
The most common sleep hygiene recommendations are:
Avoid caffeine consumption
Caffeine administration close to bedtime disrupts sleep.[29,56,57,58]
Some studies show that consumption of caffeine approximately 30 min before bedtime, causes sleep disturbances, increased sleep onset latency (SOL), decreased total sleep time (TST), and sleep efficiency.[59]
Avoid smoking
The use of nicotine is associated with decreased TST, increased SOL, more repeated early-morning awakening and suppression of SWS and REM sleeps. Thus, avoiding the nicotine use leads to better sleep.[29,56,60]
Avoid alcohol use
Alcohol consumption just before bedtime is accompanied with a decrease in SWS and an increase in SOL during the first portion of the night.[29,56,61] However, when the alcohol is metabolized in the first few hours of sleep, sleep becomes lighter with more arousals.[56]
Exercise regularly
Regular exercise is a usual sleep hygiene recommendation, but intensive exercise should be avoided within 2 h of bedtime.[29,62,63]
Manage stress
Psychosocial stress is accompanied with impaired sleep and increased presleep arousal.[64] Some techniques like relaxation have provided some initial support for stress management as an operative recommendation to overcome sleep disorders.[65]
Reduce noise
Nighttime noise raises arousals and leads to lighter sleep by suppressing SWS and REM sleeps.[23,56,66] Specific noise reduction have been shown to improve sleep in some patients.[67]
Sleep timing regularity
Sleep hygiene recommendations often advise regular bed and wake-times, which are considered to increase the synchrony between circadian rhythms, physiological sleep drive, and the nocturnal sleep period.[62] An irregular sleep-wake pattern leads to shortening of sleep period and as a result daytime sleepiness.[29,56,58,63]
Avoid daytime napping
Daytime napping has been posited to disturb the sleep drive, and sleep hygiene recommendations often include the advice to avoid naps of longer than 30 min a day.[23,56,62,63]
Avoiding bedtime technology use
The studies demonstrate a negative correlation between use of technology and sleep, so one of the most common sleep hygiene recommendations is limiting technology use close to bedtime. Some of these activities are watching television, use of cell phones, surfing the net, listening to electronic music devices, and playing video games.[58,63,68,69]
Other recommendations in sleep hygiene are: Not going to bed thirsty or hungry, having a light snack close to bedtime, sleeping in a comfortable bedroom with regulable-temperature to cool it,[23,56,70,71] and comfortable mattress,[29,70,71] taking a warm to hot bath 2 h before bedtime, setting a list of problem-solving tasks to be done the next day, using the bedroom only for sleep,[70] avoiding excessive time in bed,[29] and avoiding thinking about particular matters at bedtime or in bed.[56]
Sleep hygiene in Iranian traditional medicine
Avicenna (980–1037AD) was the author of more than 250 books on different outlets of science such as medicine. His most important work is: al-Qanun fi al-Tibb (The Canon of Medicine).[72] One chapter of this textbook is devoted to “sleep and wakefulness.”[22] In view of Ibn Sina, normal sleep has specific and vital functions, such as revitalizing, restoring strength, eliminating the fatigue produced by wakefulness, strengthening the vital energy, relaxing the mental aspect, improving food digestion, and helping to improve the function of other organs.[21,73,74,75] According to Rhazes (865–925), good and normal sleep not only reduces weakness and anxiety but also restores thought and refreshes the mind making an individual so cheerful.[76] Hence, improvement of sleep is important by attention upon the sleep hygiene principles according to the ITM. On the other hand, since a variety of conditions such as age, sex, season, geographic region, and different physical activities can alter sleep qualities, it is suggested that sleep and wakefulness could be recommended in various quantities and qualities for people.[73,74,75,77]
In view of ITM, normal sleep must have some characteristics such as:
Sleep quality
Time
Night is the best time to sleep. Sleeping during the day is disturbed due to light and noise. Hence it is unable to help the body function better.[74,80] Thus from the perspective of ITM, sleeping during the day which can cause nightmares is not recommended.[78,81] However in the summer because of the short hours of sleep through the night, sleeping for up to an hour a day is recommended.[78] In ITM, it is recommended that the person sleeps early in the evening and wakes up early in the morning.[74,75]
Relationship with food
Sleeping in a state of hunger or full stomach is harmful and should be avoided. It is recommended to have a gap of about 3 h between food consumption and sleep. Consumption of some foods such as milk and lettuce close to bedtime elevates sleep quality, whereas some foods such as cabbage and coriander disturbs the sleep.[75,78] Sleeping soon after mealtime causes impaired digestion and produces bloat as well as sleep disorders. Ideally, an accepted sleep should be after waste disposal, this means that sleep should be after urination and defecation.[74,75]
Duration
Sleep should have a normal duration. It is recommended to have 6–8 h of sleep in the night depending on the individual. Excessive wakefulness disrupts the work of different body organs, especially brain activity; it harms digestive power, and causes gastrointestinal disturbances. Loss of energy is another complication of poor sleep.[74,75,78,79] On the other hand, excessive sleep has some complications such as weight gain and obesity.[75,78,79]
Position
Sleep should not be in the supine or prone positions. The best position of the start of sleep is on the right side and then rolls to the left side.[78,82] Lying on your back causes nightmares and postnasal drip.[78]
Bedroom
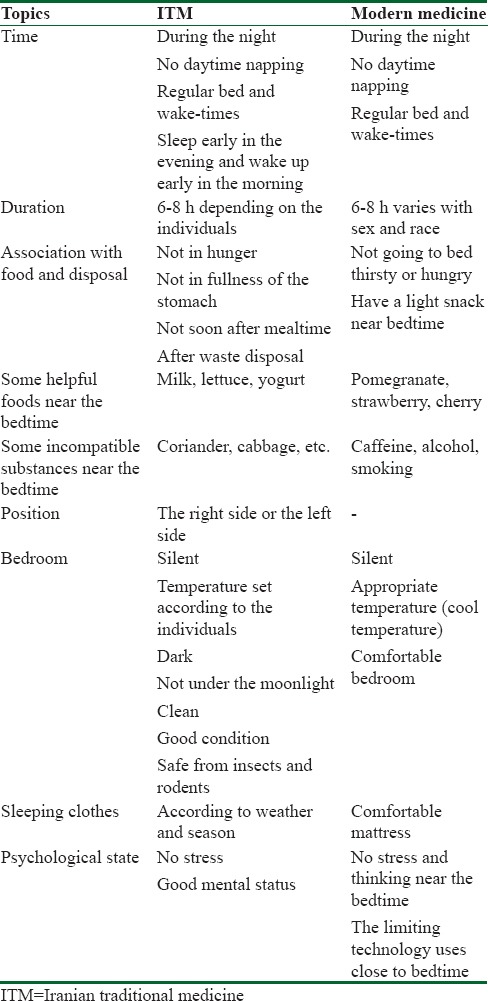
The bedroom must be dark and silent during sleeping time.[78,83] Bedroom temperature should be set according to the individual. The bedroom should be clean and in good condition and safe from insects and rodents. Sleeping clothes should be chosen according to the weather and season. Sleeping clothes must be comfortable, soft, loose, and appropriate for the season.[83] During warm weather, linen should be used and in the cold weather silk and cotton is preferred. Sleep should not be under the moonlight or sunlight.[75] Table 1 shows the sleep hygiene rules in ITM and modern medicine.
Table 1.
Sleep hygiene in iranian traditional medicine and modern medicine
Conclusions
The purpose of this study was to evaluate the importance of sleep in lifestyle modification of PCOS. High prevalence of sleep disorders has been reported in PCOS patients.[33,34,35] Sleep disorders are treatable in the general population, although more studies are needed to manage these disorders in PCOS patients. Lifestyle modification is suggested as the first-line treatment in the management of PCOS in females, in which nutrition and physical exercise are the main attentions.[27,84,85,86,87,88] Many studies have proven high incidence of sleep disorders in patients with PCOS,[33,34] but they are mostly just a report of these disorders, and the sleep has not been considered in the lifestyle of these patients.[26]
According to the research conducted on the neurohormones and their relationship with circadian rhythm, it seems that the balance of these hormones and their circadian changes is associated with the quality and quantity of sleep.[44] Thus sleep modification can be effective in neurohormonal regulation and management of PCOS.
Poor sleep quality is associated with an increased risk of obesity and insulin resistance[89] which plays a key role in PCOS.[1,90] Accordingly, sleep modification is regarded as one of the most important items of lifestyle modification in PCOS patients.[21,74,75,78,91] There are many commands regarding sleep hygiene in ITM and modern medicine. According to ITM, sleep management is an important item in lifestyle modification of all diseases including the PCOS. Hence, it seems that sleep regulation can help achieve good results in the treatment of PCOS patients, and sleep management could be considered in their lifestyle modification besides food and exercise in modern medicine. It is recommended that future clinical studies be done on sleep modification in PCOS patients and its effects on hormonal levels, oocyte maturation and ovulation. Furthermore, evaluation of the effects of PCOS treatment on the sleep quality of patients will be useful.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgments
This article is drawn from Maryam Bahman's PhD degree thesis no 166 and research project no 151 from the School of Traditional Medicine, Shahid Beheshti University of Medical Sciences. The authors gratefully acknowledge the help of the Dr. Rasool Choopani and Dr. Saeed Zarein-dolab.
References
- 1.Raja-Khan N, Stener-Victorin E, Wu X, Legro RS. The physiological basis of complementary and alternative medicines for polycystic ovary syndrome. Am J Physiol Endocrinol Metab. 2011;301:E1–10. doi: 10.1152/ajpendo.00667.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hung JH, Hu LY, Tsai SJ, Yang AC, Huang MW, Chen PM, et al. Risk of psychiatric disorders following polycystic ovary syndrome: A nationwide population-based cohort study. PLoS One. 2014;9:e97041. doi: 10.1371/journal.pone.0097041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tasali E, Chapotot F, Leproult R, Whitmore H, Ehrmann DA. Treatment of obstructive sleep apnea improves cardiometabolic function in young obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011;96:365–74. doi: 10.1210/jc.2010-1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Chatterjee B, Suri J, Suri JC, Mittal P, Adhikari T. Impact of sleep-disordered breathing on metabolic dysfunctions in patients with polycystic ovary syndrome. Sleep Med. 2014;15:1547–53. doi: 10.1016/j.sleep.2014.06.023. [DOI] [PubMed] [Google Scholar]
- 6.Conway G, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Franks S, Gambineri A, et al. The polycystic ovary syndrome: A position statement from the European Society of Endocrinology. Eur J Endocrinol. 2014;171:1–29. doi: 10.1530/EJE-14-0253. [DOI] [PubMed] [Google Scholar]
- 7.Huang G, Coviello A. Clinical update on screening, diagnosis and management of metabolic disorders and cardiovascular risk factors associated with polycystic ovary syndrome. Curr Opin Endocrinol Diabetes Obes. 2012;19:512–9. doi: 10.1097/MED.0b013e32835a000e. [DOI] [PubMed] [Google Scholar]
- 8.Amjadi F, Aflatoonian R, Javanmard SH, Saifi B, Ashrafi M, Mehdizadeh M, et al. Apolipoprotein A1 as a novel anti-implantation biomarker in polycystic ovary syndrome: A case-control study. J Res Med Sci. 2015;20:1039–45. doi: 10.4103/1735-1995.172813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sam S, Dunaif A. Polycystic ovary syndrome: Syndrome XX? Trends Endocrinol Metab. 2003;14:365–70. doi: 10.1016/j.tem.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Vgontzas AN, Bixler EO, Chrousos GP. Metabolic disturbances in obesity versus sleep apnoea: The importance of visceral obesity and insulin resistance. J Intern Med. 2003;254:32–44. doi: 10.1046/j.1365-2796.2003.01177.x. [DOI] [PubMed] [Google Scholar]
- 11.Rajaeieh G, Marasi M, Shahshahan Z, Hassanbeigi F, Safavi SM. The relationship between intake of dairy products and polycystic ovary syndrome in women who referred to Isfahan University of Medical Science Clinics in 2013. Int J Prev Med. 2014;5:687–94. [PMC free article] [PubMed] [Google Scholar]
- 12.Setji TL, Brown AJ. Polycystic ovary syndrome: Update on diagnosis and treatment. Am J Med. 2014;127:912–9. doi: 10.1016/j.amjmed.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 13.Kang X, Jia L, Shen X. Manifestation of hyperandrogenism in the continuous light exposure-induced PCOS rat model. Biomed Res Int 2015. 2015:943694. doi: 10.1155/2015/943694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Consensus on infertility treatment related to polycystic ovary syndrome. Hum Reprod. 2008;23:462–77. doi: 10.1093/humrep/dem426. [DOI] [PubMed] [Google Scholar]
- 15.Babu A, Fogelfeld L. Metabolic syndrome and prediabetes. Dis Mon. 2006;52:55–144. doi: 10.1016/j.disamonth.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 16.Moran LJ, Ko H, Misso M, Marsh K, Noakes M, Talbot M, et al. Dietary composition in the treatment of polycystic ovary syndrome: A systematic review to inform evidence-based guidelines. J Acad Nutr Diet. 2013;113:520–45. doi: 10.1016/j.jand.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 17.Shoaei T, Heidari-Beni M, Tehrani HG, Feizi A, Esmaillzadeh A, Askari G, et al. Effects of probiotic supplementation on pancreatic β-cell function and C-reactive protein in women with polycystic ovary syndrome: A randomized double-blind placebo-controlled clinical trial. Int J Prev Med. 2015;6:27. doi: 10.4103/2008-7802.153866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sood A, Narayanan S, Wahner-Roedler DL, Knudsen K, Sood R, Loehrer LL, et al. Use of complementary and alternative medicine treatments by patients with obstructive sleep apnea hypopnea syndrome. J Clin Sleep Med. 2007;3:575–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Feyzabadi Z, Jafari F, Kamali SH, Ashayeri H, Badiee Aval S, Esfahani MM, et al. Efficacy of viola odorata in treatment of chronic insomnia. Iran Red Crescent Med J. 2014;16:e17511. doi: 10.5812/ircmj.17511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rezaeizadeh H, Alizadeh M, Naseri M, Ardakani MS. The traditional Iranian medicine point of view on health and disease. Iran J Public Health. 2009;38:169–72. [Google Scholar]
- 21.Choopani R, Emtiazy M. The concept of lifestyle factors, based on the teaching of avicenna (Ibn Sina) Int J Prev Med. 2015;6:30. doi: 10.4103/2008-7802.154772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soltani SS, Minaii B, Besharat M. Sleep and wakefulness correction in different seasons from avicenna's perspective. Iran Red Crescent Med J. 2013;15:276–7. doi: 10.5812/ircmj.7677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gellis LA, Lichstein KL. Sleep hygiene practices of good and poor sleepers in the united states: An internet-based study. Behav Ther. 2009;40:1–9. doi: 10.1016/j.beth.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 24.de Sousa G, Schlüter B, Menke T, Trowitzsch E, Andler W, Reinehr T, et al. A comparison of polysomnographic variables between adolescents with polycystic ovarian syndrome with and without the metabolic syndrome. Metab Syndr Relat Disord. 2011;9:191–6. doi: 10.1089/met.2010.0081. [DOI] [PubMed] [Google Scholar]
- 25.Shreeve N, Cagampang F, Sadek K, Tolhurst M, Houldey A, Hill CM, et al. Poor sleep in PCOS; Is melatonin the culprit? Hum Reprod. 2013;28:1348–53. doi: 10.1093/humrep/det013. [DOI] [PubMed] [Google Scholar]
- 26.Tasali E, Van Cauter E, Ehrmann DA. Polycystic ovary syndrome and obstructive sleep apnea. Sleep Med Clin. 2008;3:37–46. doi: 10.1016/j.jsmc.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stachenfeld NS, Yeckel CW, Taylor HS. Greater exercise sweating in obese women with polycystic ovary syndrome compared with obese controls. Med Sci Sports Exerc. 2010;42:1660–8. doi: 10.1249/MSS.0b013e3181d8cf68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kimura T, Ho IK, Yamamoto I. Uridine receptor: Discovery and its involvement in sleep mechanism. Sleep. 2001;24:251–60. doi: 10.1093/sleep/24.3.251. [DOI] [PubMed] [Google Scholar]
- 29.Tamanna S, Geraci SA. Major sleep disorders among women: (Women's health series) South Med J. 2013;106:470–8. doi: 10.1097/SMJ.0b013e3182a15af5. [DOI] [PubMed] [Google Scholar]
- 30.Sadock BJ, Sadock VA. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2010. Kaplan and Sadock's Pocket Handbook of Clinical Psychiatry; p. 278. [Google Scholar]
- 31.Liu X, Forbes EE, Ryan ND, Rofey D, Hannon TS, Dahl RE, et al. Rapid eye movement sleep in relation to overweight in children and adolescents. Arch Gen Psychiatry. 2008;65:924–32. doi: 10.1001/archpsyc.65.8.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lazaratou H, Soldatou A, Dikeos D. Medical comorbidity of sleep disorders in children and adolescents. Curr Opin Psychiatry. 2012;25:391–7. doi: 10.1097/YCO.0b013e3283556c7a. [DOI] [PubMed] [Google Scholar]
- 33.El-Sharkawy AA, Abdelmotaleb GS, Aly MK, Kabel AM. Effect of metformin on sleep disorders in adolescent girls with polycystic ovarian syndrome. J Pediatr Adolesc Gynecol. 2014;27:347–52. doi: 10.1016/j.jpag.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Naqvi SH, Moore A, Bevilacqua K, Lathief S, Williams J, Naqvi N, et al. Predictors of depression in women with polycystic ovary syndrome. Arch Womens Ment Health. 2015;18:95–101. doi: 10.1007/s00737-014-0458-z. [DOI] [PubMed] [Google Scholar]
- 35.Moran LJ, March WA, Whitrow MJ, Giles LC, Davies MJ, Moore VM, et al. Sleep disturbances in a community-based sample of women with polycystic ovary syndrome. Hum Reprod. 2015;30:466–72. doi: 10.1093/humrep/deu318. [DOI] [PubMed] [Google Scholar]
- 36.Vgontzas AN, Bixler EO, Chrousos GP. Obesity-related sleepiness and fatigue: The role of the stress system and cytokines. Ann N Y Acad Sci. 2006;1083:329–44. doi: 10.1196/annals.1367.023. [DOI] [PubMed] [Google Scholar]
- 37.Fogel RB, Malhotra A, Pillar G, Pittman SD, Dunaif A, White DP, et al. Increased prevalence of obstructive sleep apnea syndrome in obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2001;86:1175–80. doi: 10.1210/jcem.86.3.7316. [DOI] [PubMed] [Google Scholar]
- 38.Gopal M, Duntley S, Uhles M, Attarian H. The role of obesity in the increased prevalence of obstructive sleep apnea syndrome in patients with polycystic ovarian syndrome. Sleep Med. 2002;3:401–4. doi: 10.1016/s1389-9457(02)00033-3. [DOI] [PubMed] [Google Scholar]
- 39.Zhou XS, Rowley JA, Demirovic F, Diamond MP, Badr MS. Effect of testosterone on the apneic threshold in women during NREM sleep. J Appl Physiol (1985) 2003;94:101–7. doi: 10.1152/japplphysiol.00264.2002. [DOI] [PubMed] [Google Scholar]
- 40.Epstein LJ, Kristo D, Strollo PJ, Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–76. [PMC free article] [PubMed] [Google Scholar]
- 41.Nitsche K, Ehrmann DA. Obstructive sleep apnea and metabolic dysfunction in polycystic ovary syndrome. Best Pract Res Clin Endocrinol Metab. 2010;24:717–30. doi: 10.1016/j.beem.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Giles TL, Lasserson TJ, Smith BJ, White J, Wright J, Cates CJ, et al. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;1:CD001106. doi: 10.1002/14651858.CD001106.pub2. DOI: 10.1002/14651858.CD001106.pub2. [DOI] [PubMed] [Google Scholar]
- 43.Phillips CL, Grunstein RR, Darendeliler MA, Mihailidou AS, Srinivasan VK, Yee BJ, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: A randomized controlled trial. Am J Respir Crit Care Med. 2013;187:879–87. doi: 10.1164/rccm.201212-2223OC. [DOI] [PubMed] [Google Scholar]
- 44.Zafari Zangeneh F, Naghizadeh MM, Abdollahi A, Bagheri M. Synchrony between ovarian function and sleep in polycystic ovary syndrome patients. Open J Obstet Gynecol. 2014;4:725–31. [Google Scholar]
- 45.Kakizaki M, Kuriyama S, Sone T, Ohmori-Matsuda K, Hozawa A, Nakaya N, et al. Sleep duration and the risk of breast cancer: The ohsaki cohort study. Br J Cancer. 2008;99:1502–5. doi: 10.1038/sj.bjc.6604684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Macchi MM, Bruce JN. Human pineal physiology and functional significance of melatonin. Front Neuroendocrinol. 2004;25:177–95. doi: 10.1016/j.yfrne.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 47.Kohyama J. Neurochemical and neuropharmacological aspects of circadian disruptions: An introduction to asynchronization. Curr Neuropharmacol. 2011;9:330–41. doi: 10.2174/157015911795596522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zangeneh FZ, Naghizadeh MM, Abdollahi A, Bagheri M. Evaluation of Neurohormones in sleep pattern of patients with polycystic ovary syndrome. Iran J Obstet Gynecol Infertil. 1393;17:10–20. [Google Scholar]
- 49.Tamura H, Nakamura Y, Korkmaz A, Manchester LC, Tan DX, Sugino N, et al. Melatonin and the ovary: Physiological and pathophysiological implications. Fertil Steril. 2009;92:328–43. doi: 10.1016/j.fertnstert.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 50.Luboshitzky R, Herer P, Shen-Orr Z. Urinary 6-sulfatoxymelatonin excretion in hyperandrogenic women: The effect of cyproterone acetate-ethinyl estradiol treatment. Exp Clin Endocrinol Diabetes. 2004;112:102–7. doi: 10.1055/s-2004-815765. [DOI] [PubMed] [Google Scholar]
- 51.Reiter RJ, Tan DX, Maldonado MD. Melatonin as an antioxidant: Physiology versus pharmacology. J Pineal Res. 2005;39:215–6. doi: 10.1111/j.1600-079X.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- 52.Minkel J, Moreta M, Muto J, Htaik O, Jones C, Basner M, et al. Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychol. 2014;33:1430–4. doi: 10.1037/a0034219. [DOI] [PubMed] [Google Scholar]
- 53.Federenko I, Wüst S, Hellhammer DH, Dechoux R, Kumsta R, Kirschbaum C, et al. Free cortisol awakening responses are influenced by awakening time. Psychoneuroendocrinology. 2004;29:174–84. doi: 10.1016/s0306-4530(03)00021-0. [DOI] [PubMed] [Google Scholar]
- 54.Gambineri A, Forlani G, Munarini A, Tomassoni F, Cognigni GE, Ciampaglia W, et al. Increased clearance of cortisol by 5beta-reductase in a subgroup of women with adrenal hyperandrogenism in polycystic ovary syndrome. J Endocrinol Invest. 2009;32:210–8. doi: 10.1007/BF03346454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Invitti C, De Martin M, Delitala G, Veldhuis JD, Cavagnini F. Altered morning and nighttime pulsatile corticotropin and cortisol release in polycystic ovary syndrome. Metabolism. 1998;47:143–8. doi: 10.1016/s0026-0495(98)90210-4. [DOI] [PubMed] [Google Scholar]
- 56.Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med Rev. 2015;22:23–36. doi: 10.1016/j.smrv.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nicholson AN, Stone BM. Heterocyclic amphetamine derivatives and caffeine on sleep in man. Br J Clin Pharmacol. 1980;9:195–203. doi: 10.1111/j.1365-2125.1980.tb05833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li S, Zhu S, Jin X, Yan C, Wu S, Jiang F, et al. Risk factors associated with short sleep duration among Chinese school-aged children. Sleep Med. 2010;11:907–16. doi: 10.1016/j.sleep.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 59.Roehrs T, Roth T. Caffeine: Sleep and daytime sleepiness. Sleep Med Rev. 2008;12:153–62. doi: 10.1016/j.smrv.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 60.Jaehne A, Loessl B, Bárkai Z, Riemann D, Hornyak M. Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep Med Rev. 2009;13:363–77. doi: 10.1016/j.smrv.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 61.Stein MD, Friedmann PD. Disturbed sleep and its relationship to alcohol use. Subst Abus. 2005;26:1–13. doi: 10.1300/j465v26n01_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. 2003;7:215–25. doi: 10.1053/smrv.2001.0246. [DOI] [PubMed] [Google Scholar]
- 63.Malone SK. Early to bed, early to rise?: An exploration of adolescent sleep hygiene practices. J Sch Nurs. 2011;27:348–54. doi: 10.1177/1059840511410434. [DOI] [PubMed] [Google Scholar]
- 64.Hauri PJ. Consulting about insomnia: A method and some preliminary data. Sleep. 1993;16:344–50. doi: 10.1093/sleep/16.4.344. [DOI] [PubMed] [Google Scholar]
- 65.Lichstein KL, Riedel BW, Wilson NM, Lester KW, Aguillard RN. Relaxation and sleep compression for late-life insomnia: A placebo-controlled trial. J Consult Clin Psychol. 2001;69:227–39. doi: 10.1037//0022-006x.69.2.227. [DOI] [PubMed] [Google Scholar]
- 66.Zaharna M, Guilleminault C. Sleep, noise and health: Review. Noise Health. 2010;12:64–9. doi: 10.4103/1463-1741.63205. [DOI] [PubMed] [Google Scholar]
- 67.Xie H, Kang J, Mills GH. Clinical review: The impact of noise on patients' sleep and the effectiveness of noise reduction strategies in Intensive Care Units. Crit Care. 2009;13:208. doi: 10.1186/cc7154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smaldone A, Honig JC, Byrne MW. Sleepless in america: Inadequate sleep and relationships to health and well-being of our nation's children. Pediatrics. 2007;119(Suppl 1):S29–37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- 69.Van den Bulck J. Adolescent use of mobile phones for calling and for sending text messages after lights out: Results from a prospective cohort study with a one-year follow-up. Sleep. 2007;30:1220–3. doi: 10.1093/sleep/30.9.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Friedman L, Benson K, Noda A, Zarcone V, Wicks DA, O’Connell K, et al. An actigraphic comparison of sleep restriction and sleep hygiene treatments for insomnia in older adults. J Geriatr Psychiatry Neurol. 2000;13:17–27. doi: 10.1177/089198870001300103. [DOI] [PubMed] [Google Scholar]
- 71.Schoicket SL, Bertelson AD, Lacks P. Is sleep hygiene a sufficient treatment for sleep-maintenance insomnia? Behav Ther. 1988;19:183–90. [Google Scholar]
- 72.Hojjati A, Vahdani A. Health care accreditation: The past, present, and future in the Middle East. Iran Red Crescent Med J 2010. 2010:80–1. [Google Scholar]
- 73.Razi MZ. al-Hawi fi al-Tibb (Liber continents).Beirut: Daral Kotob Al-ilmiyah. 1422:40–1. [Google Scholar]
- 74.Jorjani E. Treasure of Kharazmshah (Zakhireye Kharazmshahi) Vol. 1391. Qom: Moasseseh Ehyae Teb Tabiee; pp. 474–7. [Google Scholar]
- 75.Ibn Sina AA. (Avicenna). al-Qanun fi al-Tibb (The Canon of Medicine) Beirut: Dar Ehia Al-Tourath Al-Arabi; 2005. pp. 223–4. [Google Scholar]
- 76.Razi MZ. al-Morshed av al-Fosool. Vol. 1384. Tehran: Publication of Tehran University of Medical Sciences; p. 40. [Google Scholar]
- 77.Soltani SS. Iranian Traditional Medicine Aspect in Principle of Sleep and Wakefulness. Shahid Beheshti University; 2012. pp. 90–1. [Google Scholar]
- 78.Aqilikhorasani M. Kholasat al-Hekmah. Qom: Ismaielian; 2006. pp. 467–73. [Google Scholar]
- 79.Chaghmini MM. Ghanonche. Tehran, Iran: Almaei Publications; 2013. pp. 340–1. [Google Scholar]
- 80.Razi B. Kholasat al-Tajareb. Vol. 1382. Tehran: Iran University of Medical Sciences; p. 97. [Google Scholar]
- 81.Jorjani E. Alaii's secret (Khofi-e-Alaii) Vol. 1369. Tehran: Ettelaat; pp. 41–3. [Google Scholar]
- 82.Feyzabadi Z, Jafari F, Feizabadi PS, Ashayeri H, Esfahani MM, Badiee Aval S, et al. Insomnia in iranian traditional medicine. Iran Red Crescent Med J. 2014;16:e15981. doi: 10.5812/ircmj.15981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gilani MK. Naseri's Health care (Hefz al-Sehat Naseri) Tehran: Almaee Press; 2009. p. 140. [Google Scholar]
- 84.Harwood K, Vuguin P, DiMartino-Nardi J. Current approaches to the diagnosis and treatment of polycystic ovarian syndrome in youth. Horm Res. 2007;68:209–17. doi: 10.1159/000101538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhao L. Comprehensive treatment of polycystic ovarian syndrome and related infertility. J Assoc Tradit Chin Med Acupunct UK. 2012;19:12–6. [Google Scholar]
- 86.Bates GW, Legro RS. Longterm management of polycystic ovarian syndrome (PCOS) Mol Cell Endocrinol. 2013;373:91–7. doi: 10.1016/j.mce.2012.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tymchuk CN, Tessler SB, Barnard RJ. Changes in sex hormone-binding globulin, insulin, and serum lipids in postmenopausal women on a low-fat, high-fiber diet combined with exercise. Nutr Cancer. 2000;38:158–62. doi: 10.1207/S15327914NC382_3. [DOI] [PubMed] [Google Scholar]
- 88.Miri M, Karimi Jashni H, Alipour F. Effect of exercise intensity on weight changes and sexual hormones (androstenedione and free testosterone) in female rats with estradiol valerate-induced PCOS. J Ovarian Res. 2014;7:37. doi: 10.1186/1757-2215-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Koren D, Dumin M, Gozal D. Role of sleep quality in the metabolic syndrome. Diabetes Metab Syndr Obes. 2016;9:281–310. doi: 10.2147/DMSO.S95120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jelodar G, Karami E. Effect of hydroalcoholic extract of Vitex Agnus-castus fruit on ovarian histology in rat with induced Polycystic Ovary Syndrome (PCOS) J Babol Univ Med Sci. 2013;13:96–102. [Google Scholar]
- 91.Zarshenas MM, Khademian S, Moein M. Diabetes and related remedies in medieval persian medicine. Indian J Endocrinol Metab. 2014;18:142–9. doi: 10.4103/2230-8210.129103. [DOI] [PMC free article] [PubMed] [Google Scholar]


