Abstract
Background
Previous studies have reported functional and structural abnormalities in the thalamus and the pars triangularis of the inferior frontal gyrus in patients with insomnia disorder. However, no studies have been conducted on the white-matter tracts between these 2 brain regions. We aimed to compare the white-matter integrity and structure of the left thalamus–pars triangularis tracts between patients with insomnia and controls, and to characterize the relationship between white-matter integrity and clinical features in patients with insomnia.
Methods
In total, 22 participants with insomnia disorder and 27 controls underwent overnight polysomnography and brain magnetic resonance imaging, and then completed self-report clinical questionnaires and neurocognitive tests for spatial planning. Structural and diffusion measures such as fractional anisotropy, axial diffusivity, radial diffusivity and trace were analyzed in group comparison and correlation analyses.
Results
The insomnia group showed significantly lower fractional anisotropy (F = 8.647, p = 0.02) and axial diffusivity (F = 5.895, p = 0.038) in the left thalamus–pars triangularis tracts than controls. In patients with insomnia, fractional anisotropy in the tracts was correlated with the results of the Stockings of Cambridge test (r = 0.451, p = 0.034), and radial diffusivity was correlated with Epworth Sleepiness Scale score (r = 0.437, p = 0.042).
Limitations
Limitations included analyses of limited brain regions and the cross-sectional design.
Conclusion
The insomnia group showed decreased integrity in the left thalamus–pars triangularis tracts, and integrity was correlated with cognition and daytime sleepiness. These results may imply that insomnia is characterized by disintegration of the white-matter tract between the left thalamus and inferior frontal gyrus.
Introduction
Insomnia disorder is one of the most prevalent and distressing psychiatric diseases.1 A large-scale epidemiologic study reported that one-third of the community-dwelling population has at least 1 symptom of insomnia.2 Furthermore, 10% of the general population experience insomnia symptoms with daytime consequences, and 6% of people satisfy the diagnostic criteria for primary insomnia.2 Insomnia impairs quality of life, hinders occupational and social functioning, and increases vulnerability to medical illnesses.3 Insomnia has also led to an increase in health care utilization and consequent social burden and economic costs.4 Detailed studies into the pathophysiology of insomnia and its management and care, including diagnosis and treatment, are needed.
For the past decade, the neurobiological mechanism of insomnia has been widely investigated using advanced neuroimaging methodologies. The thalamus is a major region involved in the pathophysiology of insomnia, sleep–wake rhythms, hyperarousal, emotions and restorative autonomic and endocrine processes.5,6 The existence of structural and metabolic alterations in the thalamus or brain circuits involving the thalamus among right-handed patients with insomnia or sleep-deprived individuals has been replicated in neuroimaging studies.7–9 Reduced bilateral thalamic grey-matter volume after sleep deprivation7 and atrophic changes in the thalamus in patients with insomnia8 have been shown. Patients with insomnia had decreased thalamic metabolic differences between non–rapid eye movement (NREM) sleep at night and wakefulness in the morning compared with controls.9
Significant findings in the frontal cortices of patients with insomnia also have been shown consistently. Grey-matter deficits in the bilateral dorsolateral prefrontal regions have been found in patients with insomnia,10 and decreased functional activation has been observed in the left orbitofrontal, left inferior frontal and right middle frontal gyri in right-handed patients with insomnia.11 Recently, the left inferior frontal gyrus has been recognized as an important brain area involved in insomnia, in light of considerable evidence that decline in cognitive functions — such as retrieval of semantic information, controlled selection and divergent thinking — is a symptom of insomnia.12 In addition, a task-related functional magnetic resonance imaging (fMRI) study showed that these associations related to semantic selection and inhibition were significantly stronger in the left inferior frontal region.13 Activity in the left pars triangularis of the inferior frontal gyrus decreased during category and letter fluency tests,14 and the blood oxygen level–dependent signal in the left pars triangularis of the inferior frontal gyrus was more activated following short-term sleep deprivation when divergent thinking ability was needed.15 A meta-analysis including studies comparing activation from rapid eye movement (REM) or NREM sleep to wakefulness found consistently decreased activation in the inferior frontal gyrus during REM sleep, and in the thalamus during NREM sleep.16
Given the structural and functional abnormalities in the thalamus and left inferior frontal gyrus found in insomnia, investigating the neural connectivity between these 2 areas in insomnia is of interest. It has been suggested that thalamofrontal functional connectivity plays an important role in neurobiological models of insomnia.17 The increased activation in the bilateral frontal and thalamic regions observed in good sleepers during a working memory task was not found in right-handed patients with insomnia.18 The topology of intrinsic nodal degree and efficiency of the left pars triangularis of the inferior frontal gyrus were decreased, and the frontostriatal network from the left inferior frontal gyrus was aberrant in right-handed participants with insomnia symptoms in a recent fMRI study.19 However, the majority of prior studies have investigated functional changes in specific cortical or subcortical brain regions by seeking to characterize connected neural circuits, rather than by focusing on white-matter tracts.
Despite the importance of the left inferior frontal gyrus and its connection to the thalamic region in insomnia, there have been no studies using diffusion tensor imaging — which allows visualization of white-matter integrity — to examine these tracts in patients with insomnia. A white-matter tract is a bundle of parallel myelinated axons, and diffusion-weighted MRI (dMRI) can investigate microscopic changes related to myelin, cellular organelles and the movement of water molecules in the white matter.20 The measures used in dMRI are fractional anisotropy (FA), axial diffusivity (AD), radial diffusivity (RD) and trace (TR): FA means the degree of directionality of water diffusion; AD and RD are apparent diffusivity values in parallel and perpendicular directions, respectively; and TR is the sum of diffusivity values in all 3 directions.20 Two previous studies using diffusion tensor imaging have shown reduced FA values in the subcortical brain regions of right-handed patients with insomnia. One study21 found a reduced FA value in the right anterior internal capsule; the other22 found lower FA values in several right subcortical regions, including the internal capsule, the corona radiata, the superior longitudinal fasciculus, the body of the corpus callosum and the thalamus.
We evaluated all 4 measures of dMRI to find more specific axonal alteration and pathology in the white matter of the left thalamus–pars triangularis tracts. Our aims were to investigate whether the integrity of white-matter tracts in the left thalamus–pars triangularis of the inferior frontal gyrus differed between patients with insomnia and controls, to identify any structural differences in these tracts between patients with insomnia and controls, and to measure the correlation between dMRI measures and clinical variables in patients with insomnia.
Methods
Participants
We recruited patients with insomnia disorder and controls from the sleep clinic of Gil Medical Center, Incheon, South Korea. Recruitment was accomplished using a notice posted on the bulletin board of Gil Medical Center, an online advertisement and physician-initiated referrals or requests. All participants were screened by telephone interview and using screening scales on a website built for this study. After initial screening, board-certified psychiatrists with a specialty in sleep medicine interviewed participants to assess their eligibility for the study based on the Structured Clinical Interview for the DSM-5.23
The inclusion criteria for patients with insomnia were as follows: aged 18–60 years and right-handed; negative pregnancy test for women; history of illness lasting at least 1 year and meeting the diagnostic criteria for insomnia disorder as stated in the DSM-524; a total score of ≥ 8 on the Korean version of the Pittsburgh Sleep Quality Index (PSQI) at screening25; and no psychiatric medications or hypnotics and no cognitive behavioural therapy for insomnia in the previous 2 weeks.
Controls were included according to the following criteria: aged 18–60 years and right-handed; no symptoms or history of psychiatric disorders or sleep disorders, including insomnia; a total score ≤ 4 on the PSQI at screening; and no lifetime history of taking psychotropic medications or hypnotics.
Participants who had comorbid psychiatric or neurologic disorders other than insomnia disorder were excluded from the study. The detailed exclusion criteria for both groups are presented in Appendix 1, Supplementary Methods, available at jpn.ca/170195-a1.
A total of 155 participants (76 patients with insomnia and 79 controls) who passed initial telephone screening were recruited to the study. Then, 54 insomnia patients and 52 controls were excluded based on the following criteria: not appropriate for the study based on the screening scale (insomnia = 33; controls = 30); deemed ineligible after face-to-face interview (insomnia = 4; controls = 5); metal in the body (insomnia = 7; controls = 6); abnormal polysomnography findings (insomnia = 3; controls = 2); withdrew informed consent or did not attend the clinic on the scanning day (insomnia = 6; controls = 8); or had a newly found structural brain abnormality following MRI (insomnia = 1; controls = 1). After we applied the above exclusion criteria, 22 patients with insomnia and 27 controls completed the full research protocol. We obtained written informed consent from all participants before they were included in the study. The study was approved by the Institutional Review Board of Gil Medical Center.
Clinical measurement
All participants were asked to complete the Korean versions of the PSQI, the Epworth Sleepiness Scale,26 the Berlin Questionnaire, 27 the Beck Depression Inventory28 and the Beck Anxiety Inventory29 at screening. They also completed the Korean versions of the PSQI, the Insomnia Severity Index,30 the Epworth Sleepiness Scale, the Beck Depression Inventory and the Beck Anxiety Inventory on the scanning date. To adjust for the effect of depression severity on diffusion measures, we summed the non-sleep items from the Beck Depression Inventory 21-item scale (excluding item 16, which is classified as a sleep-related item). We used the Stockings of Cambridge subset of the Cambridge Neuropsychological Test Automated Battery to assess spatial planning as an index of neurocognitive functioning.31
Polysomnography
Overnight polysomnography was performed using the Embletta X100 system (Embla) to exclude participants with occult sleep disorders other than insomnia. Manual scoring was performed according to the manual of the American Academy of Sleep Medicine (AASM) 2.0.2., with RemLogic 3.4.0 (Embla Systems) as the scoring platform.
MRI acquisition and processing
We acquired MRI scans using a 3.0 T MR scanner (Magnetom Verio, Siemens) with a 12-element matrix head coil. We acquired high-resolution transaxial T1-weighted structural images using 3D magnetization-prepared rapid gradient-echo (3D-MPRAGE). The parameters are presented in Appendix 1, Supplementary Methods. The structural images were inspected for structural abnormalities by board-certified neuroradiologists before image processing. Motion and eddy current effects were corrected using affine registration of 62 volumes in 2 sets to the b0 baseline volume in the first set by FLIRT (version 6.0, FMRIB Software).32,33 Using unscented Kalman filter (UKF)–based 2-tensor tractography,34 we conducted whole-brain tractography (number of tensors = 2; seeds per voxel = 10; step length = 0.3; seed FA limit = 0.18; record length = 1.7).
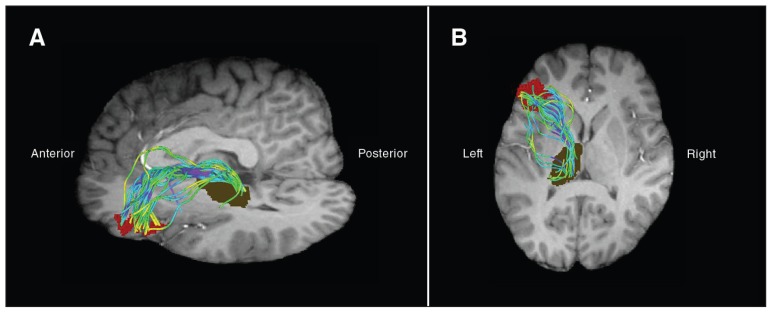
The T1-weighted structural images were parcellated into discrete regions of interest (ROIs) using the Desikan–Killiany atlas in FreeSurfer version 5.3.35 Registration of a T1 image to the b0 baseline image of the dMRI was performed using a nonlinear registration method, part of the Advanced Normalization Tools.36,37 We transformed FreeSurfer-parcellated labels into dMRI using the same registration transformation. We selected transformed, parcellated grey matter/white matter ROIs of 2 structures (the thalamus and the pars triangularis) on the left side. We combined the grey matter and white matter ROIs into 1 ROI for the pars triangularis. We extracted the left thalamus–pars triangularis tracts (i.e., the tracts connecting the left thalamus ROI and the left pars triangularis ROI) using white-matter query language (e.g., Fig. 1).38
Fig. 1.
Example of the tracts between the left thalamus and the left pars triangularis. The olive-coloured region of interest indicates grey matter and white matter of the thalamus. The red region of interest indicates grey matter and white matter of the left pars triangularis. (A) Sagittal view. (B) Axial view.
We calculated FA,39 AD (λ1),40 RD ([λ2 + λ3]/2) and TR (λ1 + λ2 + λ3) according to previous studies.41 We extracted the means for the diffusion measures (FA, AD, RD and TR) and volumes for the left thalamus–pars triangularis tracts. We calculated the mean volume, surface area, grey-matter volume and thickness of the left pars triangularis and the mean volume of the left thalamus.
Statistical analysis
We compared the demographic data, clinical data, structural MRI measures (volume surface area, grey-matter thickness and grey-matter volume by the selected ROIs) and dMRI measures (FA, AD, RD and TR) of the 2 groups using the Student t test (for equal variance) or the Welch t test (for unequal variance) and a χ2 test or Fisher exact test (for categorical variables). We considered individual variation of intracranial volume and used the adjusted ROI volume in analyzing differences in ROI volumes between the 2 groups. In group comparisons of structural and diffusion measures, data that were 1.5 × the interquartile range below Q1 (lower quartile) or above Q3 (upper quartile) were removed from the analyses.42 We performed analysis of covariance of diffusion measures, in which age and sex were regarded as covariates. We used Pearson r correlation to evaluate associations among the clinical and polysomnography variables and the diffusion measures. Statistical analysis was performed at a 2-sided significance level of p < 0.05 using SPSS for Windows version 20.0 (SPSS). To correct for multiple comparisons, we used the Benjamini–Hochberg procedure, with a false discovery rate43 of q < 0.05.
Results
Demographics, clinical characteristics and polysomnographic data
Demographic and clinical characteristics of patients with insomnia and controls are presented in Table 1. The control and insomnia groups did not differ significantly with respect to age (33.4 ± 7.2 v. 37.5 ± 10.5 yr; t = 1.618, p = 0.11) or proportion of women (59.3% v. 54.5%; χ2 = 0.110, p = 0.74). The mean duration of insomnia was 5.3 ± 5.9 years. Patients with insomnia had significantly more severe PSQI total scores (p < 0.001), Insomnia Severity Index scores (p < 0.001), Beck Depression Inventory scores (p < 0.001) and problems solved in the minimum number of moves in Stockings of Cambridge (p = 0.017) than controls. Polysomnography results showed that patients with insomnia had significantly lower total sleep time (p < 0.001) and sleep efficiency (p < 0.001), and a higher total arousal index (p < 0.001) than controls.
Table 1.
Demographic, clinical and polysomnographic information from participants
| Group; mean ± SD* | Statistical tests† | ||||
|---|---|---|---|---|---|
|
|
|
||||
| Variables | Control (n = 27) | Insomnia disorder (n = 22) | t or χ2 | df | p value |
| Age, yr | 33.4 ± 7.2 | 37.5 ± 10.5 | t = 1.618 | 47 | 0.11 |
| Sex, female, no. (%) | 16 (59.3) | 12 (54.5) | χ2 = 0.110 | 1 | 0.74 |
| Duration of insomnia disorder, yr | ― | 5.3 ± 5.9 | |||
| Pittsburgh Sleep Quality Index | |||||
| Total score | 2.4 ± 1.3 | 12.3 ± 3.4 | t = 12.925 | 25.680 | < 0.001 |
| Total sleep time, min | 437.0 ± 44.9 | 254.6 ± 98.0 | t = −8.074 | 28.131 | < 0.001 |
| Sleep efficiency, % | 95.2 ± 4.5 | 62.0 ± 21.2 | t = −7.228 | 22.517 | < 0.001 |
| Insomnia Severity Index score | 1.4 ± 1.8 | 18.2 ± 5.4 | t = 13.998 | 24.996 | < 0.001 |
| Epworth Sleepiness Scale score | 3.82 ± 2.9 | 6.96 ± 3.8 | t = −3.265 | 47 | 0.002 |
| Dysfunctional Beliefs and Attitutes About Sleep score | 57.3 ± 20.2 | 97.0 ± 22.5 | t = 6.489 | 47 | < 0.001 |
| Beck Depression Inventory (non-sleep score)‡ | 2.0 ± 2.1 | 8.7 ± 4.4 | t = −6.485 | 26.534 | < 0.001 |
| Neuropsychological data of CANTAB | |||||
| SOC, mean initial thinking time (5 moves), s | 5064.48 ± 3448.58 | 5632.02 ± 5989.57 | t = −0.416 | 47 | 0.68 |
| SOC, mean subsequent thinking time (5 moves), s | 1367.21 ± 2432.04 | 2634.85 ± 4485.00 | t = −1.261 | 47 | 0.21 |
| SOC, problems solved in minimal moves | 7.7 ± 1.2 | 6.6 ± 1.8 | t = 2.499 | 34.663 | 0.017 |
| Polysomnographic data | |||||
| Total sleep time, min | 390.9 ± 58.9 | 323.8 ± 60.2 | t = −3.935 | 47 | < 0.001 |
| Sleep latency, min | 5.4 ± 3.8 | 16.9 ± 14.1 | t = 3.750 | 23.474 | 0.001 |
| Sleep efficiency, % | 94.5 ± 3.2 | 80.3 ± 9.3 | t = −6.874 | 25.043 | < 0.001 |
| Wake after sleep onset, min | 18.4 ± 14.3 | 64.6 ± 43.4 | t = 4.779 | 24.708 | < 0.001 |
| Apnea–Hypopnea Index, n per h | 2.4 ± 1.6 | 2.8 ± 1.7 | t = 0.872 | 47 | 0.39 |
| Total arousal index, n per h | 5.3 ± 1.5 | 10.0 ± 4.3 | t = 4.921 | 25.402 | < 0.001 |
| Stage N1 | 4.4 ± 2.8 | 15.5 ± 4.8 | t = 10.077 | 47 | < 0.001 |
| Stage N2 | 52.1 ± 9.1 | 49.5 ± 7.7 | t = −1.068 | 47 | 0.29 |
| Stage N3 | 18.4 ± 6.6 | 12.2 ± 6.6 | t = −3.260 | 47 | 0.002 |
| Stage R | 25.1 ± 4.9 | 22.9 ± 4.1 | t = −1.719 | 47 | 0.092 |
CANTAB = Cambridge Neuropsychological Test Automated Battery; SD = standard deviation; SOC = Stockings of Cambridge from the Cambridge Neuropsychological Test Automated Battery.
Unless otherwise specified.
Statistical tests were performed using the Student t test (for equal variance) or Welch t test (for unequal variance).
Beck Depression Inventory (non-sleep score): excluding the sleep item (16) from the total Beck Depression Inventory 21-item score.
Diffusion-weighted MRI measures of the left thalamus–pars triangularis tracts
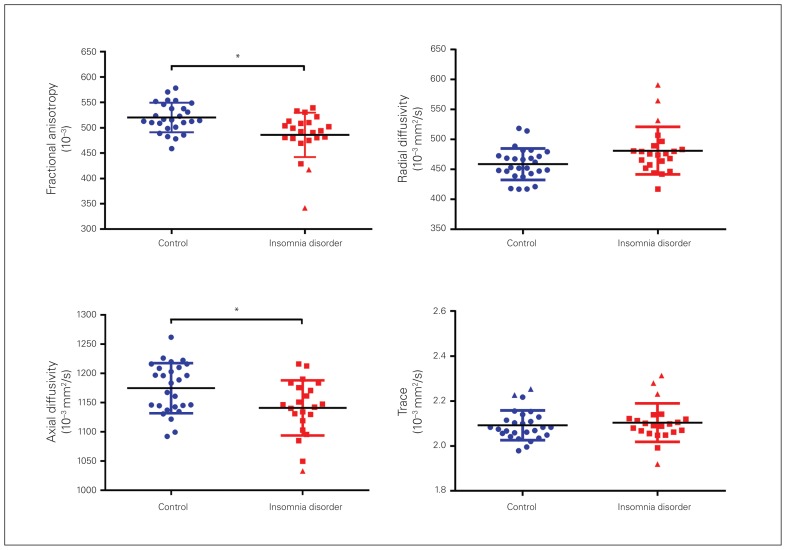
Patients with insomnia had significantly lower FA (F1,43 = 8.647; p = 0.02) and AD (F1,44 = 5.895; p = 0.038) of the left thalamus–pars triangularis tracts than controls after adjustment for age and sex (Table 2, Fig. 2). The statistical significance of group differences in diffusion measures did not change after controlling for Beck Depression Inventory non-sleep score (Appendix 1, Table S1).
Table 2.
Group differences in diffusion measures of the tracts connecting the left thalamus and the left pars triangularis*
| Group; mean ± SD | Statistical tests† | Statistical tests‡ | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Variables | Control (n = 27) | Insomnia disorder (n = 22) | t | df | pFDR | F | df | pFDR |
| Fractional anisotropy (10−3) | 520.32 ± 29.00 | 485.95 ± 43.76 | 2.913 | 45 | 0.022 | 8.647 | 1,43 | 0.02 |
| Radial diffusivity (10−3 mm2/s) | 458.58 ± 26.33 | 481.20 ± 39.63 | −1.337 | 44 | 0.25 | 0.897 | 1,42 | 0.47 |
| Axial diffusivity (10−3 mm2/s) | 1174.59 ± 42.90 | 1140.90 ± 47.29 | 2.316 | 46 | 0.05 | 5.895 | 1,44 | 0.038 |
| Trace (10−3 mm2/s) | 2.09 ± 0.67 | 2.10 ± 0.86 | −0.345 | 41 | 0.73 | 0.056 | 1,39 | 0.81 |
FDR = false discovery rate; SD = standard deviation.
Diffusion measures 1.5 × interquartile range below Q1 (lower quartile) or above Q3 (upper quartile) were removed in all analyses.
Group differences in each diffusion measure using Student’s t-test.
Adjusted for age and sex; analysis of covariance was performed to reveal group differences in each diffusion measure.
Fig. 2.
Group differences in diffusion measures of the tracts connecting the left thalamus and the left pars triangularis. Blue dots represent controls, and red rectangles represent patients with insomnia disorder. Blue bars (controls) and red bars (insomnia disorder) represent the mean ± standard deviation. Blue and red triangles denote outliers. Significant group differences in diffusion measures of the left thalamus–pars triangularis white-matter tracts were found in fractional anisotropy and axial diffusivity values. Data that were 1.5 × interquartile range below Q1 (lower quartile) or above Q3 (upper quartile) were removed from the analyses. *Significant group differences (p < 0.05).
Structural measures of the left thalamus and pars triangularis tracts
We compared the structural variables of the left thalamus and pars triangularis between the 2 groups (Table 3). The pars triangularis of patients with insomnia had significantly lower volume (F1,45 = 5.782; p = 0.048), adjusted volume (F1,45 = 14.322; p = 0.003; intracranial volume adjusted) and surface area (F1,45 = 6.911; p = 0.041) than those of controls after adjustment for age and sex.
Table 3.
Group differences in the structural variables of the left thalamus and the pars triangularis*
| Group; mean ± SD | Statistical tests† | Statistical tests‡ | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| Variables | Control (n = 27) | Insomnia disorder (n = 22) | t | df | pFDR | F | df | pFDR |
| Pars triangularis | ||||||||
| Volume, mm3 | 3107.10 ± 512.07 | 2802.36 ± 37.62 | 2.209 | 47 | 0.05 | 5.782 | 1,45 | 0.048 |
| Adjusted volume§ | 0.00239 ± 0.00048 | 0.00202 ± 0.00031 | 3.236 | 45.001 | 0.014 | 14.322 | 1,45 | 0.003 |
| Surface area, mm2 | 1322.78 ± 189.98 | 1189.45 ± 169.25 | 2.564 | 47 | 0.044 | 6.911 | 1,45 | 0.041 |
| Grey matter thickness, mm | 2.46 ± 0.15 | 2.46 ± 0.17 | 0.105 | 47 | 0.92 | 0.368 | 1,45 | 0.55 |
| Grey matter volume, mm3 | 3725.22 ± 592.80 | 3349.82 ± 460.49 | 2.431 | 47 | 0.044 | 4.406 | 1,45 | 0.06 |
| Thalamus | ||||||||
| Volume, mm3 | 8699.79 ± 1129.52 | 8402.70 ± 1101.21 | 0.926 | 47 | 0.42 | 1.099 | 1,45 | 0.35 |
| Adjusted volume§ | 0.00665 ± 0.00093 | 0.00605 ± 0.00061 | 2.158 | 45 | 0.05 | 4.62 | 1,43 | 0.058 |
FDR = false discovery rate; SD = standard deviation.
Structural measures 1.5 × interquartile range below Q1 (lower quartile) or above Q3 (upper quartile) were removed in all analyses.
Group differences in each diffusion measure using a Student’s t-test (for equal variance) or Welch’s t-test (for unequal variance).
Adjusted for age and sex; analysis of covariance was performed to reveal group differences in structural variables.
Adjusted volume was defined as each region of interest volume divided by intracranial volume.
Correlation between the clinical data and dMRI measures
In patients with insomnia, the Epworth Sleepiness Scale score was significantly correlated with RD (r = 0.437, p = 0.042) and the number of problems solved in minimal moves in the Stockings of Cambridge test was significantly correlated with the FA value of the left thalamus–pars triangularis tracts (r = 0.451, p = 0.034). We found no correlation between dMRI measures and PSQI (Table 4).
Table 4.
Correlations between clinical or polysomnographic data and diffusion measures connecting the left thalamus and the left pars triangularis in patients with insomnia
| Fractional anisotropy | Radial diffusivity | Axial diffusivity | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Variables | r | p | r | p | r | p |
| Insomnia duration, yr | −0.218 | 0.33 | 0.142 | 0.53 | −0.217 | 0.33 |
| Epworth Sleepiness Scale score | −0.318 | 0.15 | 0.437 | 0.042 | 0.017 | 0.94 |
| Insomnia Severity Index score | 0.254 | 0.25 | −0.183 | 0.41 | 0.210 | 0.35 |
| Dysfunctional Beliefs and Attitudes About Sleep score | 0.186 | 0.41 | −0.238 | 0.29 | −0.067 | 0.77 |
| Pittsburgh Sleep Quality Index score | 0.279 | 0.21 | −0.261 | 0.24 | 0.167 | 0.46 |
| Beck Depression Inventory (non-sleep score)* | 0.018 | 0.94 | −0.037 | 0.87 | −0.028 | 0.90 |
| Neuropsychological test data | ||||||
| SOC, problems solved in minimal moves | 0.451 | 0.034 | −0.348 | 0.11 | 0.355 | 0.11 |
| Polysomnographic data | ||||||
| Total sleep time, min | −0.046 | 0.84 | −0.056 | 0.80 | −0.115 | 0.61 |
| Sleep efficiency, % | −0.237 | 0.29 | 0.280 | 0.21 | −0.006 | 0.98 |
SOC = Stockings of Cambridge from the Cambridge Neuropsychological Test Automated Battery.
Statistical analyses were performed using Pearson’s r correlation.
Beck Depression Inventory (non-sleep score): excluding the sleep item (16) from the total Beck Depression Inventory 21-item score.
Discussion
In this study, we found that patients with insomnia had disrupted white-matter integrity (lower FA and lower AD) in the left thalamus–pars triangularis tracts and lower structural values (volumes and surface areas) in the left pars triangularis of the inferior frontal gyrus compared with controls.
Our results indicate that white matter in the left thalamus–pars triangularis tracts showed decreased integrity in patients with insomnia, a novel finding. The differences in the diffusion measures of these white-matter tracts between patients with insomnia and controls show the low connectivity of these tracts in insomnia. Because dMRI measures reflect microstructural changes such as demyelination of the axons, diffusivity modulated by myelin, axonal degeneration and ongoing pathology, 20 the decreased connectivity of the left thalamus–pars triangularis tracts can result in functional failure in the adaptive interplay between activation and inhibition in the ascending reticular formation between the thalamus and inferior frontal gyrus.10,44 Many studies with functional imaging have suggested decreased connectivity in the thalamofrontal regions in patients with insomnia, and this may be associated with decreased white-matter connectivity in these tracts.16,45 Nofzinger and colleagues9 found higher glucose metabolism in the subcortical regions (including the bilateral thalamus) during NREM sleep, and relatively lower glucose metabolism in the bilateral prefrontal cortex, thalamus and ascending reticular activating system during the waking state in patients with insomnia. They assumed that the increased glucose metabolism was owing to a hyperarousal mechanism, the failure of “transition from waking to sleep” and decreased activation in the waking state resulting from chronic insomnia.9 The hyperarousal system is engaged mainly in the bottom–up process by which the wake drive is activated by the brainstem, transmitted through the thalamus and usually manifested in the frontal cortex, which is involved in behavioural activation and inhibition.44 Our study found low white-matter integrity in these regions in patients with insomnia. Although we cannot draw a causal relationship between insomnia and altered white-matter tracts, our result may imply that insomnia is characterized by this altered thalamofrontal connectivity.
Cognitive problems in patients with insomnia or sleep-deprived individuals may be associated with low structural connectivity and structural abnormalities in the left thalamus–pars triangularis tracts. It has been suggested that the neural networks of the cognitive system relate to decreased functional connectivity between the thalamus and inferior frontal gyrus in right-handed sleep-deprived individuals15,46 or patients with insomnia.10,14,18 Sleep-deprived adults showed reduced functional connectivity between the left inferior frontal gyrus and parahippocampal area in MRI scans during a selective attentional task.46 Patients with insomnia and sleep-deprived participants showed hypoactivation or decreased volume in several frontal cortical areas and the thalamus in relation to executive dysfunction.10,14,15,18,46 In addition, the laterality to the left dominant hemisphere of this altered connectivity has been shown in neuroimaging studies.14,15,46 These studies can explain the major role of the left inferior frontal gyrus in the functional mechanisms of the sleep–wake cycle, which is associated with frontal cognitive function. Our study also showed that the number of problems solved in minimal moves in the Stockings of Cambridge test was significantly lower in the insomnia group and was correlated with the FA value of the left thalamus–pars triangularis tracts in patients with insomnia. The Stockings of Cambridge test is known to effectively reflect executive function in the domains of spatial planning and problem-solving strategies.31 Hence, the cognitive theory of insomnia and the thalamofrontal connectivity that have been continuously suggested in previous studies are shown in our study, with visibly poor integrity of the white-matter tracts in patients with insomnia.
Scores on the Epworth Sleepiness Scale, which reflects daytime sleepiness, showed significant correlations with the RD value of the left thalamus–pars triangularis. In previous grey-matter structural studies, decreased volumes in the orbitofrontal cortex among the right-handed, healthy participants were found to correlate with daytime sleepiness and play a role in the influence of sleep loss on vigilance.47 As well, the thalamus is a central region for consciousness, and the thalamocortical network enables integrative communication for the transmission of signals regarding consciousness.6 In the context of these previous findings, the present results linking daytime sleepiness to the white-matter tract between the left thalamus and the inferior frontal gyrus may constitute neural support for the clinical findings of sleepiness, inattention and loss of vigilance. However, in the insomnia group in our study, none of the other clinical or polysomnographic results was correlated with diffusion tensor imaging parameters. In previous studies, grey-matter deficits in the left or right prefrontal cortices were correlated with sleep latency,10 and hippocampal atrophy was correlated with PSQI scores and arousal indices in patients with insomnia.8 In diffusion tensor imaging studies, FA in the right thalamus was correlated with disease duration and PSQI scores,22 and FA in the internal capsule was correlated with Insomnia Severity Index scores in right-handed people with insomnia.21 These inconsistencies might be attributable to small sample sizes in this study field and different characteristics of the insomnia groups in different studies. Another possible explanation is that each neural network system is accountable for different sleep and wake manifestations. The left thalamus–pars triangularis tracts are largely responsible for the cognitive network in the insomnia model and might be associated with cognitive function, inattention or daytime sleepiness. On the other hand, the emotion-regulating system of the insomnia model, which incorporates limbic structures such as the hippocampus, the amygdala, the anterior cingulate cortex and the corpus callosum in the right hemisphere, may correlate with subjective sleep perception measures such as the PSQI and the Insomnia Severity Index.21,22 Further studies are needed to address the functional differences of individual white-matter tracts related to specific phenotypes involving sleep and insomnia.
Strengths and limitations
The present study had several methodological strengths. We extracted fibre tracts using a UKF-based 2-tensor tractography algorithm. Other tractography methods estimate local fibre orientation as a single direction, but UKF-based 2-tensor tractography models the signal as a mixture of 2 tensors,34 allowing recovery of the branching and crossing fibres, which cannot be extracted by traditional tractography. Moreover, UKF-based 2-tensor tractography takes into account the correlation of diffusion and spatial regularization.34 The current estimate is guided by the previous estimate at each step of tracing the fibre, allowing it to account for the correlation in diffusion of water along the fibre path.
There were also limitations to the present study. First, this preliminary study evaluated only a small proportion of ROIs — the left thalamus and the left pars triangularis of the inferior frontal gyrus — to ascertain the white-matter connectivity in these tracts. Our hypothesis was motivated by previous reports and imaging studies implicating the left thalamus–pars triangularis tracts in the cognitive and arousal system of patients with insomnia. Future studies will need to include additional white-matter tracts to fully characterize the association between brain networks and the sleep–wake system. Second, the causality of the association between white-matter abnormalities and primary insomnia is still unknown because of the cross-sectional design. A further longitudinal study is needed to ascertain the direction of the relationship. Third, the small sample size of the insomnia group might have resulted in less significant correlation between diffusion measures and clinical measures. A larger sample is needed to verify the correlations between sleep and diffusion measures in patients with insomnia. Fourth, hormonal effects of the menstrual cycle on sleep in female participants were not considered in our study for practical reasons, such as MRI scheduling. Fifth, polysomnography was performed only for a single night, so we could not exclude the first-night effect.
Conclusion
To the best of our knowledge, our finding of decreased integrity of the left thalamus–pars triangularis white-matter tracts of patients with insomnia compared with controls using diffusion tensor imaging is a novel one. We also showed a significant correlation between the integrity of these tracts and both spatial planning function and degree of sleepiness in the insomnia group. These findings suggest that low integrity in these tracts might be related to the pathophysiology and cognitive function of insomnia. Studies with larger samples, comprehensive neuropsychological testing and longitudinal study design will be needed to find the role of the thalamus–pars triangularis tracts and the neural mechanism of insomnia disorder. Further studies are also needed to investigate other white-matter tracts in association with self-reported and polysomnographic sleep measures in patients with insomnia. These efforts will help identify the neurobiological evidence of insomnia and reveal clues regarding the treatment of insomnia.
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (NRF-2017R1D1A1B03032431). It was also supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI17C2665).
Footnotes
Competing interests: None declared.
Contributors: J. Lee and S.-G. Kang designed the study. J. Kang and S.-G. Kang acquired the data, which all authors analyzed. J. Kang and S. Joo wrote the article, which all authors reviewed. All authors approved the final version to be published and can certify that no other individuals not listed as authors have made substantial contributions to the paper.
References
- 1.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 2.Ohayon MM, Reynolds CF. Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD) Sleep Med. 2009;10:952–60. doi: 10.1016/j.sleep.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Léger D, Guilleminault C, Bader G, et al. Medical and socio-professional impact of insomnia. Sleep. 2002;25:625–9. [PubMed] [Google Scholar]
- 4.Rosekind MR, Gregory KB. Insomnia risks and costs: health, safety, and quality of life. Am J Manag Care. 2010;16:617–26. [PubMed] [Google Scholar]
- 5.Lugaresi E. The thalamus and insomnia. Neurology. 1992;42(Suppl 6):28–33. [PubMed] [Google Scholar]
- 6.Min B-K. A thalamic reticular networking model of consciousness. Theor Biol Med Model. 2010;7:10. doi: 10.1186/1742-4682-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu C, Kong XZ, Liu X, et al. Long-term total sleep deprivation reduces thalamic gray matter volume in healthy men. Neuroreport. 2014;25:320–3. doi: 10.1097/WNR.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 8.Koo DL, Shin J-H, Lim J-S, et al. Changes in subcortical shape and cognitive function in patients with chronic insomnia. Sleep Med. 2017;35:23–6. doi: 10.1016/j.sleep.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Nofzinger EA, Buysse DJ, Germain A, et al. Functional neuroimaging evidence for hyperarousal in insomnia. Am J Psychiatry. 2004;161:2126–8. doi: 10.1176/appi.ajp.161.11.2126. [DOI] [PubMed] [Google Scholar]
- 10.Joo EY, Noh HJ, Kim J-S, et al. Brain gray matter deficits in patients with chronic primary insomnia. Sleep. 2013;36:999–1007. doi: 10.5665/sleep.2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li C, Ma X, Dong M, et al. Abnormal spontaneous regional brain activity in primary insomnia: a resting-state functional magnetic resonance imaging study. Neuropsychiatr Dis Treat. 2016;12:1371–8. doi: 10.2147/NDT.S109633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fortier-Brochu É, Morin CM. Cognitive impairment in individuals with insomnia: clinical significance and correlates. Sleep. 2014;37:1787–98. doi: 10.5665/sleep.4172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fink A, Grabner RH, Benedek M, et al. The creative brain: investigation of brain activity during creative problem solving by means of EEG and fMRI. Hum Brain Mapp. 2009;30:734–48. doi: 10.1002/hbm.20538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Altena E, Van Der Werf YD, Sanz-Arigita EJ, et al. Prefrontal hypoactivation and recovery in insomnia. Sleep. 2008;31:1271–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Vartanian O, Bouak F, Caldwell J, et al. The effects of a single night of sleep deprivation on fluency and prefrontal cortex function during divergent thinking. Front Hum Neurosci. 2014;8:214. doi: 10.3389/fnhum.2014.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jakobson AJ, Laird AR, Maller JJ, et al. Brain activity in sleep compared to wakefulness: a meta-analysis. J Behav Brain Sci. 2012;2:249. [Google Scholar]
- 17.Buysse DJ, Germain A, Hall M, et al. A neurobiological model of insomnia. Drug Discov Today Dis Models. 2011;8:129–37. doi: 10.1016/j.ddmod.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drummond SPA, Walker M, Almklov E, et al. Neural correlates of working memory performance in primary insomnia. Sleep. 2013;36:1307–16. doi: 10.5665/sleep.2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu F-M, Liu C-H, Lu S-L, et al. Disrupted topology of frontostriatal circuits is linked to the severity of insomnia. Front Neurosci. 2017;11:214. doi: 10.3389/fnins.2017.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beaulieu C. The basis of anisotropic water diffusion in the nervous system — a technical review. NMR Biomed. 2002;15:435–55. doi: 10.1002/nbm.782. [DOI] [PubMed] [Google Scholar]
- 21.Spiegelhalder K, Regen W, Prem M, et al. Reduced anterior internal capsule white matter integrity in primary insomnia. Hum Brain Mapp. 2014;35:3431–8. doi: 10.1002/hbm.22412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li S, Tian J, Bauer A, et al. Reduced integrity of right lateralized white matter in patients with primary insomnia: a diffusion-tensor imaging study. Radiology. 2016;280:520–8. doi: 10.1148/radiol.2016152038. [DOI] [PubMed] [Google Scholar]
- 23.First M, Williams J, Karg R, et al. Structured clinical interview for DSM-5 disorders, clinician version (SCID-5-CV) Arlington (VA): APA; 2015. [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington (DC): APA; 2013. [Google Scholar]
- 25.Sohn SI, Kim DH, Lee MY, et al. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012;16:803–12. doi: 10.1007/s11325-011-0579-9. [DOI] [PubMed] [Google Scholar]
- 26.Cho YW, Lee JH, Son HK, et al. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath. 2011;15:377–84. doi: 10.1007/s11325-010-0343-6. [DOI] [PubMed] [Google Scholar]
- 27.Kang K, Park KS, Kim JE, et al. Usefulness of the Berlin Questionnaire to identify patients at high risk for obstructive sleep apnea: a population-based door-to-door study. Sleep Breath. 2013;17:803–10. doi: 10.1007/s11325-012-0767-2. [DOI] [PubMed] [Google Scholar]
- 28.Hahn HM, Yeom TH, Shin YW, et al. A standardization study of Beck Depression Inventory in Korea. J Korean Neuropsychiatr Assoc. 1986;25:487–500. [Google Scholar]
- 29.Han-Kyeong L, Eun-Ho L, Soon-Taeg H, et al. Psychometric properties of the Beck Anxiety Inventory in the community-dwelling sample of Korean adults. Korean J Clin Psychol. 2016;35:822–30. [Google Scholar]
- 30.Cho YW, Song ML, Morin CM. Validation of a Korean version of the Insomnia Severity Index. J Clin Neurol. 2014;10:210–5. doi: 10.3988/jcn.2014.10.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robbins TW, James M, Owen AM, et al. Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia. 1994;5:266–81. doi: 10.1159/000106735. [DOI] [PubMed] [Google Scholar]
- 32.Jenkinson M, Bannister P, Brady M, et al. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage. 2002;17:825–41. doi: 10.1016/s1053-8119(02)91132-8. [DOI] [PubMed] [Google Scholar]
- 33.Jenkinson M, Smith S. A global optimisation method for robust affine registration of brain images. Med Image Anal. 2001;5:143–56. doi: 10.1016/s1361-8415(01)00036-6. [DOI] [PubMed] [Google Scholar]
- 34.Rathi Y, Kubicki M, Bouix S, et al. Statistical analysis of fiber bundles using multi-tensor tractography: application to first-episode schizophrenia. Magn Reson Imaging. 2011;29:507–15. doi: 10.1016/j.mri.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fischl B, Salat DH, Busa E, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33:341–55. doi: 10.1016/s0896-6273(02)00569-x. [DOI] [PubMed] [Google Scholar]
- 36.Avants BB, Tustison NJ, Song G, et al. A reproducible evaluation of ANTs similarity metric performance in brain image registration. Neuroimage. 2011;54:2033–44. doi: 10.1016/j.neuroimage.2010.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Avants BB, Yushkevich P, Pluta J, et al. The optimal template effect in hippocampus studies of diseased populations. Neuroimage. 2010;49:2457–66. doi: 10.1016/j.neuroimage.2009.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wassermann D, Makris N, Rathi Y, et al. The white matter query language: a novel approach for describing human white matter anatomy. Brain Struct Funct. 2016;221:4705–21. doi: 10.1007/s00429-015-1179-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Papadakis NG, Xing D, Houston GC, et al. A study of rotationally invariant and symmetric indices of diffusion anisotropy. Magn Reson Imaging. 1999;17:881–92. doi: 10.1016/s0730-725x(99)00029-6. [DOI] [PubMed] [Google Scholar]
- 40.Alexander AL, Lee JE, Lazar M, et al. Diffusion tensor imaging of the brain. Neurotherapeutics. 2007;4:316–29. doi: 10.1016/j.nurt.2007.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Basser PJ, Jones DK. Diffusion-tensor MRI: theory, experimental design and data analysis — a technical review. NMR Biomed. 2002;15:456–67. doi: 10.1002/nbm.783. [DOI] [PubMed] [Google Scholar]
- 42.Tukey J. Addison-Wesley series in behavioral science: quantitative methods. Reading: Addison-Wesley; 1977. [Google Scholar]
- 43.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57:289–300. [Google Scholar]
- 44.Kay DB, Buysse DJ. Hyperarousal and beyond: new insights to the pathophysiology of insomnia disorder through functional neuroimaging studies. Brain Sci. 2017;7:23. doi: 10.3390/brainsci7030023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kay DB, Karim HT, Soehner AM, et al. Sleep-wake differences in relative regional cerebral metabolic rate for glucose among patients with insomnia compared with good sleepers. Sleep. 2016;39:1779–94. doi: 10.5665/sleep.6154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lim J, Tan JC, Parimal S, et al. Sleep deprivation impairs object-selective attention: a view from the ventral visual cortex. PLoS One. 2010;5:e9087. doi: 10.1371/journal.pone.0009087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Killgore WD, Schwab ZJ, Kipman M, et al. Voxel-based morphometric gray matter correlates of daytime sleepiness. Neurosci Lett. 2012;518:10–3. doi: 10.1016/j.neulet.2012.04.029. [DOI] [PubMed] [Google Scholar]