Supplemental Digital Content is available in the text
Keywords: aspiration, mechanical thrombectomy, retrospective studies, stent-retriever, stroke
Abstract
Background and purpose:
Whether the direct aspiration approach of thrombectomy for recanalization in patients with acute ischemic stroke has a similar efficacy and safety compared to the stent-retriever remains uncertain.
Methods:
We conducted a meta-analysis of 9 studies obtained through PubMed and Embase database searches to determine whether successful recanalization rate, good functional outcome at 3 months (modified Rankin score, mRS≤2), procedure time from groin puncture to maximal revascularization and procedure-related adverse events differed between patients who underwent the direct aspiration and those receiving stent-retriever for recanalization in acute cerebral infarction.
Results:
There was no significant difference between the direct aspiration group and the stent-retriever group in rate of successful recanalization (summary odds ratio [OR], 0.86 [95% confidence interval (CI), 0.45–1.52]; P = .60), but a better functional outcomes in the direct aspiration group at 3 months defined as a mRS score of 0 to 2 (OR, 0.77; 95% CI, 0.66–0.97; P = .03). Furthermore, the direct aspiration patients compared with the stent-retriever patients had a tendency of shorter procedural time (Mean difference [MD], -8.77 [95% CI, from-18.90 to 1.37]; P = .09). Finally, there were less adverse events especially in symptomatic intracerebral hemorrhage (sICH) (OR, 0.56; 95% CI, 0.33–0.98; P = .04) and embolization to a new territory (ENT) (OR, 0.49; 95% CI, 0.28–0.84; P = .01) in the direct aspiration group when compared with the stent-retriever group, although no difference between them in the rate of any ICH (OR, 0.81; 95% CI, 0.41–1.60; P = .54).
Conclusions:
The results support that the direct aspiration technique for those acute ischemic stroke patients may have better functional outcomes, less procedure related-adverse events and a tendency of faster revascularization time as compared to the stent-retriever thrombectomy, with a similar successful recanalization rate. However, major limitations of current evidence (mainly from retrospective and observational studies and a small number of patients population) indicate a need for adequately powered, multicenter randomized controlled trials (RCT) to answer this question.
1. Introduction
Recently, several randomized stroke clinical trials[1–5] demonstrated the superiority of mechanical thrombectomy in patients with acute ischemic stroke from large vessel occlusion when compared with the standard medical therapy alone. Mechanical thrombectomy with stent retrievers is now the standard therapy for selected patients with ischemic stroke. Compared with the stent retrievers approaches, the technique of A Direct Aspiration, First Pass Technique for the Endovascular Treatment of Stroke (ADAPT) for acute ischemic stroke has obtained growing acceptance as it is thought to facilitated a high rate of recanalization, and potentially at lower costs when used either alone or as an adjunct to stent retriever, and promising clinical results.[6–8]
The aspiration approach of thrombectomy is based on using the largest catheter permitted by the vessel, ensuring greater aspiration power for thrombus extraction. In case of failure with the front-line aspiration approach in removing the thrombus, the large-bore aspiration catheter provides the additional benefit of offering access for a stent retriever. The growing acceptance of aspiration approach arises questions regarding the safety and efficacy of aspiration thrombectomy techniques as a first-line therapy. Therefore, we aimed to conduct a meta-analysis of published studies to compare direct aspiration versus stent retriever for efficacy and safety as a front-line endovascular procedure.
2. Methods
2.1. Search strategy and selection criteria
This systematic review and meta-analysis was followed by recommendations from the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guideline.[9] The study was approved by the Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China. Our inclusion criteria were such that only articles in which directly compared the effect of the contact aspiration and stent retriever techniques when used alone for ischemic stroke patients with large vessel occlusion undergoing thrombectomy. We searched titles and abstracts of published journal articles in the Pubmed and Embase (through April 40, 2018) with English restriction using the following string of terms [(aspiration OR ADAPT) AND (stent-retriever OR Solitaire OR Trevo OR Merci) AND (stroke)]. The reference lists of all selected articles were also thoroughly searched to see if there were articles that could be included in the present systematic review and meta-analysis. References generated from these searches were imported into the reference manager Papers 3 for Mac and then removed duplicate references. Titles and abstracts of journal articles included were then systematically screened (by CQ and KS) for studies comparing outcomes of effect between direct aspiration and stent retriever patients used alone. We excluded cases of combined retriever plus local aspiration. A total of 9 studies[10–18] were included in the present study after a full text review of studies identified through the screening process.
2.2. Data extraction
Two reviewers (CQ and KS) independently reviewed each retrieved article and extracted data. Differences or disagreements between the 2 reviewers were resolved by discussion and consensus with the third reviewer (DST). The primary outcome was the rate of successful recanalization defined angiographically as mTICI2b/3 on the angiogram at the end of procedure. Secondary functional outcome was 90-d modified Rankin scale (mRS) score 0 to 2. Complications extracted included intracerebral hemorrhage on imaging at 24 hours, symptomatic intracerebral hemorrhage (sICH) and embolization to a new territory (ENT). Procedural time was defined as groin puncture to reperfusion time. The outcomes mentioned above were collected from each final study.
2.3. Statistical analysis
A meta-analysis of proportions was conducted for the primary and secondary outcomes of this study. A formal comparison was performed between outcomes for the direct aspiration technique and standard endovascular therapy in terms of clinical and functional outcomes and complications. All analyses were performed using Review Manager (RevMan) for Mac 5.3 (Copenhagen). Dichotomous data from published studies were used to generate odds ratios (ORs) with 95% confidence intervals (CIs), and a meta-analysis was performed with a Mantel–Haenszel fixed/random effects model to calculate a summary OR with 95% CIs. For continuous data, means and standard deviations in each study were collected. If the study did not provide mean and standard deviations, we estimated these parameters from the median and range values by methods described by Hozo et al[19]P values < .05 were considered statistically significant. We assessed primary and secondary outcomes using an OR weighted by inverse variance of the measure in each individual trial. Heterogeneity among the studies included in the meta- analyses was assessed using Cochrane's Q test and I2 statistic. An I2 value ≦50% was considered as low heterogeneity. When I2 > 50% statistics was found, we then chose a random effects model over a fixed effects model because of possible heterogeneity among studies and patient populations. Sensitivity analysis was conducted by sequential exclusion of 1 study at a time to assess for a significant change in the summary OR. Publication bias was assessed with a funnel plot plotting ORs against error/variance. An asymmetrical funnel plot was suggestive of potential publication bias.
3. Results
3.1. Study characteristics
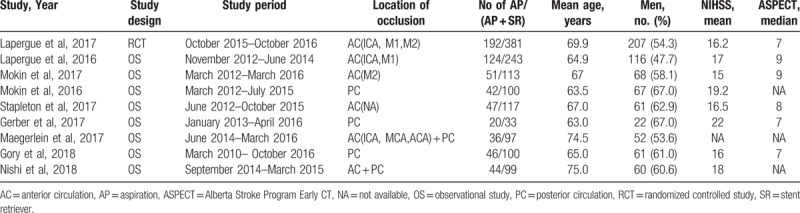
PRISMA flow diagram is presented for study search and selection in the meta-analysis. Our detailed search gathered 359 studies total from PubMed and EMBASE. After excluding studies, article review was performed on 31 studies. A total of 9 studies comprising 1273 patients were included for analysis. Of the 9 studies included, 8 studies were retrospective and observational studies and only one was randomized controlled trial. For each study included in the meta-analysis, the following variables are listed in Table 1: study design, time period, location of occlusion, number of contact aspiration, and the total number of patients undergoing mechanical thrombectomy. Other known predictors of outcome, such as age, baseline NIHSS, or Alberta Stroke Program Early CT score (ASPECT, when available), did not statistically differ between the direct aspiration and stent-retriever groups in all the studies.
Table 1.
Characteristics of the patients in the included studies.
3.2. Successful recanalization and clinical outcomes
The primary outcome of the present review was the rate of successful recanalization defined angiographically as TICI2b/3 at final angiogram. Meta-analysis demonstrated that the pooled proportion of patients with TICI 2b/3 was 78.9% (OR: 0.86, 95% CI: 0.48–1.52, I2 = 73.0%). No significant difference was found between direct aspiration and stent-retriever for favorable recanalization (P = .60; Fig. 1).
Figure 1.
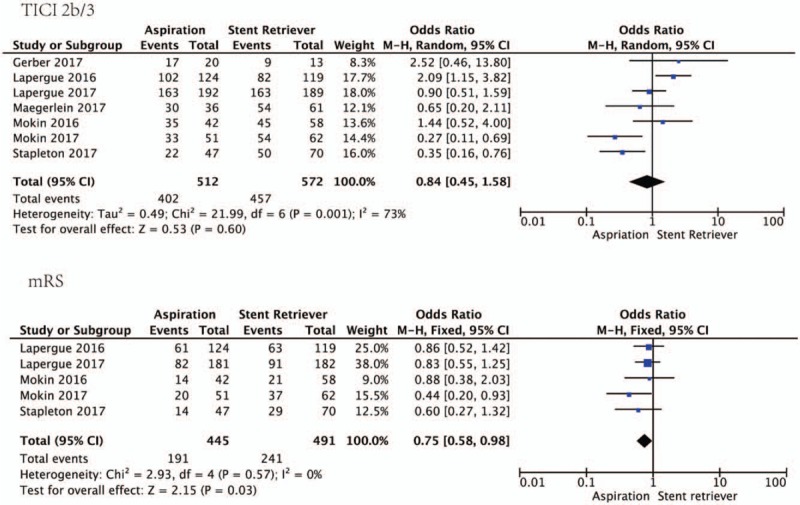
Forest plots of successful recanalization and clinical outcomes between direct aspiration and stent-retriever. Upper panel, successful recanalization (TICI 2b/3); Lower panel, good clinical outcome (90-day mRS of 0–2).
The secondary outcome measure of this study was favorable outcome, defined by mRS score of 0 to 2 at 90 days of follow-up. Figure 1 showed the pooled odds of 0.77 (0.60–0.97) for good outcome of mRS (0–2). We found the proportion of good functional outcome in the direct aspiration group is higher than that in the stent retriever group (P = .03; Fig. 1).
3.3. Procedure-related adverse events
A total of 228 intracerebral hemorrhages (ICH) occurred, with no evidence of a difference between the direct aspiration group (36.7%, n = 294) and the stent retriever group (37.4%, n = 321) (P = .54; Fig. 2). The proportion of patients with symptomatic intracerebral hemorrhage (sICH) in the direct aspiration group was 4.8% (n = 441) compared to the stent retriever group with 8.3% (n = 492). Figure 2 showed the pooled odds for sICH of 0.56 (0.33–0.98). In addition, embolization to a new territory (ENT) caused by mechanical thrombectomy occurred in 9.7% (n = 435) in the stent retriever group, whereas only 5.1% (n = 414) in the direct aspiration group. Although no significant differences between these 2 mechanical thromobectomy in any ICH have been found yet, there was lower rate about sICH and ENT in the direct aspiration group compared with the stent retriever group (P = .04 in sICH and P = .01 in ENT; Fig. 2).
Figure 2.
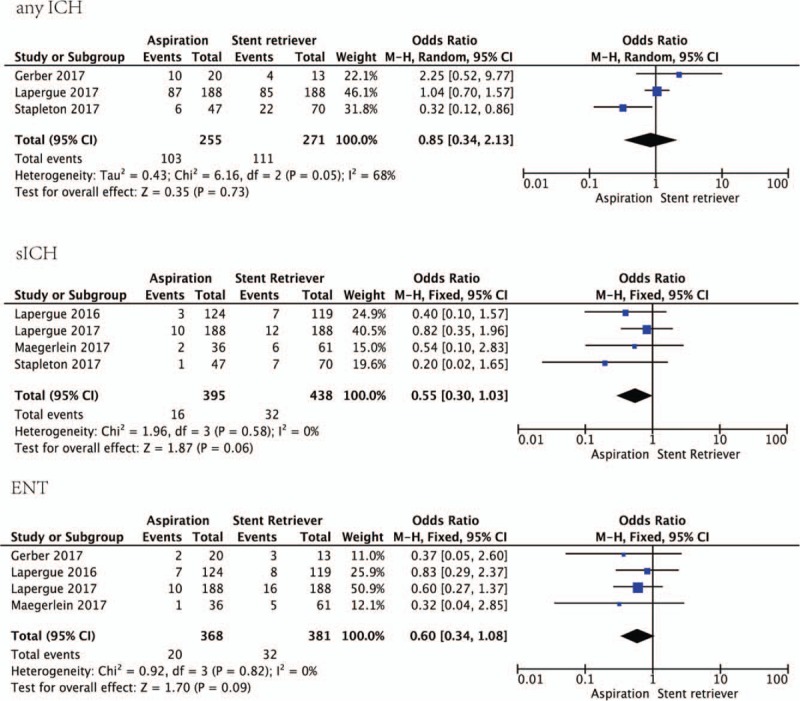
Forest plots of procedure-related adverse events including any ICH, sICH, and ENT between direct aspiration and stent-retriever. Upper panel, any SCH; middle panel, sICH; lower panel, ENT. ENT = embolization to a new territory, ICH = intracerebral haemorrhage, sICH = symptomatic intracerebral haemorrhage.
3.4. Procedural time
The average time from groin puncture to maximal revascularization after mechanical thrombectomy was compared in the direct aspiration alone group and in the stent -retriever group. Although no significant difference between the 2 groups with regard to the procedural time, there was a tendency of shorter time in the direct aspiration alone group compared with the stent-retriever group (95% CI: from −18.90 to −1.37, I2 = 84.0%; P = .09; Fig. 3).
Figure 3.
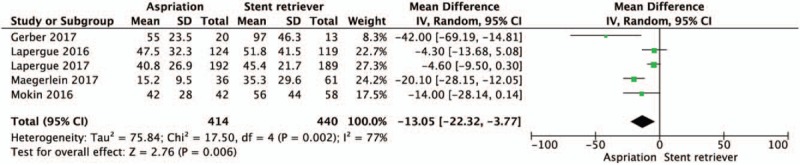
Forest plots of the average time from groin puncture to maximal revascularization after mechanical thrombectomy between direct aspiration and stent-retriever.
3.5. Study heterogeneity
I2 values were <50% for the following outcomes: mRS ≤2 at 90 days (I2 = 0%), symptomatic ICH (I2 = 0%), and embolization to a new territory (I2 = 0%). I2 values were >50% (indicating moderate or substantial heterogeneity) for the following outcomes: the rate of successful recanalization (TICI2b/3) (I2 = 73%), any ICH (I2 = 53%), and procedure time from groin puncture to revascularization (I2 = 84%). Publication bias was assessed using funnel plot analysis. Considerable risk of publication bias existed in these studies (Figure I in the online-only Data Supplement), mainly in procedural time.
4. Discussion
In the present systematic review and meta-analysis, we found that the use of first-pass aspiration approach or ADAPT achieved less adverse events especially in sICH and ENT compared to front-line stent retriever strategy and a tendency of faster procedural time from groin puncture to favorable revascularization. Although the rate of successful revascularization (TICI2b/3) in the ADAPT group did not differ from those in the stent retriever group, the favorable clinical outcomes (mRS as 0–2) in the ADAPT cohort was higher. This outcome should be interpreted with caution given that most of studies included were comparative observational studies.
It has been shown that clinical efficiency of mechanical thrombectomy is time dependent that indicated successful reperfusion is correlated with favorable outcomes in those ischemic stroke patients due to large vessel occlusion.[2,20,21] Although the stent retriever technology is considered as the gold standard for thrombectomy, the rate of revascularization failure still remains suboptimal. Hence, alternative strategies are of interest in the research and development, which may offer more rapid, cheaper, and better recanalization rates and finally favorable outcomes. One such alternative technique is the use of the aspiration alone strategy as first pass. The direct aspiration technology of thrombectomy or ADAPT is a recent endovascular treatment for ischemic stroke with large vessel occlusion that has been gaining popularity due to the rapidity of the technique and the potential for cost savings in comparison to the gold standard thrombectomy methods such as stent retrievers. However, few studies have directly compared the efficacy and safety of direct aspiration versus stent-retriever for recanalization in acute cerebral infarction.
The goal of the study was to directly compare the contact aspiration and stent retriever techniques when used alone. Revascularization rate was chosen as the primary outcome because it is a major early indicator of treatment success. Favorable recanalization has been correlated with good clinical outcome defined as mRS of 0 to 2,[22,23] and has been used as a primary outcome in other stroke trials to compare the efficacy of different thrombectomy devices; eg, SWIFT[24] and TREVO2.[25] Successful revascularization was specifically defined as an mTICI score of 2b or 3 in this study because this outcome has been reported to be a predictor of clinical outcome.[23,26,27] We found that there was no significant difference in the rate of successful recanalization (TICI2b/3) between the 2 groups; in addition, a better favorable clinical outcome (mRS as 0–2) was found in the aspiration group compared with the stent retriever group. The results of the present study are similar to that of Lapergue et al,[11] which was the first randomized clinical trial that directly compared the effect of contact aspiration and stent retriever techniques when used alone on revascularization in patients with acute ischemic stroke. In their study of 381 patients who underwent mechanical thrombectomy, they compared 192 contact aspiration cases and 189 cases of stent retriever, and reported 84.9% cases TICI 2b/3 with aspiration, compared to 86.2% with stent retriever. Similarly, among those patients with mRS assessments at 3 months, no significant difference was found in the proportion who were functionally independent, but a tendency of better clinical efficacy outcome in the stent retriever group (50.0%) compared with that in the contact aspiration group (45.3%). As such, the authors concluded that first-line thrombectomy with contact aspiration compared with stent retriever did not result in an increased successful revascularization rate and a better clinical efficacy outcomes for large vessel intracranial occlusions.[11] Our results are partly inconsistent with a recent published study of meta-analysis in which reported higher rates of complete revascularization in ADAPT but similar clinical outcomes compared to the stent retriever.[28] Only those literatures directly compare the contact aspiration and stent retriever techniques when used alone were included in our present study.
In our meta-analysis, average procedural times from groin puncture to favorable revascularization were 8.77 minutes shorter for direct aspiration when used alone than the stent-retriever technique, which might be attributed to the lower number of maneuvers during the process of contact aspiration. Procedure-related adverse events, especially symptomatic intracranial hemorrhage and embolization to a new vascular territory, the most frequent events during thrombectomy, are also mentioned in the present meta-analysis. Here we found that a significant difference and smaller frequency of these adverse events in the direct aspiration group compared to that in the stent retriever group. It is consistent with results of other recent studies.[10,29,30] A retrospective study comparing aspiration and stent retriever techniques reported a lower rate of symptomatic hemorrhages for contact aspiration compared with stent retriever (2.9% for contact aspiration and 5.4% for stent retriever),[10] and retrospective studies have reported low rates of 2% embolization in a new territory and no incidence of symptomatic intracranial hemorrhage when using contact aspiration.[29,30] Longer procedure time has been suggested to be an independent risk factor for symptomatic intracranial hemorrhage.[31] In the present study, the lower rate of sICH in the direct aspiration compared to the stent-retriever may be explained by the tendency of shorter procedural time in the contact aspiration group. In addition, the higher number of maneuvers that were performed in the stent retriever group also increase the risk of sICH and embolization in a new territory during procedure. Theoretically, it is reasonable because use of a stent retriever requires that it be passed through the clot and therefore might result in a higher rate of distal emboli, which was confirmed in an in vitro study,[32] but there were no significant differences between groups in the frequency of embolization to a new vascular territory.[11]
4.1. Limitations
This study has several limitations. The present findings are mainly derived from observational analyses and only one RCT, which are subject to well-known limitations. Firstly, most studies included were retrospective in nature with limited follow-up, which may overestimate the effect size of outcomes and limit interpretation of pooled data. Secondly, it is the potential for confounding by measured or unmeasured variables, which cannot be ruled out, even after adjustment for baseline between-group differences. Thirdly, it concerns the potential evaluation bias in clinical outcomes in the absence of blinded evaluation. In addition, the studies included used a variety of devices (i.e., guide catheters, aspiration catheters, different stent retrievers), contributing to heterogeneity. Finally, there is always inherent risk in meta-analysis of bias within the component studies that cannot be completely addressed. Long-term follow-up and direct comparative studies in the future are required to determine whether the contact aspiration approach can be a suitable alternative to golden standard stent-retriever technique for acute ischemic stroke.
5. Conclusions
Among patients with acute ischemic stroke and large vessel occlusion undergoing mechanical thrombectomy, first-line direct aspiration versus stent retriever when used alone did not result in a higher successful revascularization rate at the end of the procedure; however, aspiration technique has been shown to better functional outcomes at 3 months, less procedure-related adverse events and a tendency of shorter revascularization time compared to front-line stent retriever strategy. More randomized clinical trials are required in the near future to confirm the benefit of the first-line direct aspiration strategy compared to standard endovascular therapy for acute ischemic stroke.
Author contributions
Conceptualization: Qiang Zhang, Dai-Shi Tian.
Data curation: Chuan Qin, Ke Shang.
Formal analysis: Chuan Qin, Ke Shang, Sha-Bei Xu.
Funding acquisition: Sha-Bei Xu, Dai-Shi Tian.
Investigation: Chuan Qin, Ke Shang, Sha-Bei Xu, Qiang Zhang.
Methodology: Sha-Bei Xu.
Project administration: Wei Wang, Qiang Zhang, Dai-Shi Tian.
Supervision: Wei Wang, Qiang Zhang, Dai-Shi Tian.
Writing – original draft: Chuan Qin, Ke Shang.
Writing – review & editing: Sha-Bei Xu, Qiang Zhang, Dai-Shi Tian.
Supplementary Material
Footnotes
Abbreviations: ADAPT = A Direct Aspiration, First Pass Technique for the Endovascular Treatment of Stroke, ASPECT = Alberta Stroke Program Early CT score, CI = confidence interval, ENT = embolization to a new territory, ICH = intracerebral hemorrhage, MD = mean difference, mRS = modified Rankin score, OR = odds ratio, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analysis, RCT = randomized controlled trials, RevMan = Review Manager, sICH = symptomatic intracerebral hemorrhage.
Disclosures: This work was supported by National Natural Science Foundation of China (81873743, 81571132 to DST), the Fundamental Research Funds for the Central Universities (2017KFYXJJ107 to DST, 2017KFYXJJ124 to CQ), and Clinical Research Physician Program of Tongji Medical College, HUST (SBX).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–30. [DOI] [PubMed] [Google Scholar]
- [2].Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11–20. [DOI] [PubMed] [Google Scholar]
- [3].Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015;372:2285–95. [DOI] [PubMed] [Google Scholar]
- [4].Campbell BCV, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009–18. [DOI] [PubMed] [Google Scholar]
- [5].Jovin TG, Chamorro Á, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015;372:2296–306. [DOI] [PubMed] [Google Scholar]
- [6].Jankowitz B, Grandhi R, Horev A, et al. Primary manual aspiration thrombectomy (MAT) for acute ischemic stroke: safety, feasibility and outcomes in 112 consecutive patients. J Neurointerv Surg 2015;7:27–31. [DOI] [PubMed] [Google Scholar]
- [7].Jankowitz B, Aghaebrahim A, Zirra A, et al. Manual aspiration thrombectomy: adjunctive endovascular recanalization technique in acute stroke interventions. Stroke 2012;43:1408–11. [DOI] [PubMed] [Google Scholar]
- [8].Comai A, Haglmuller T, Ferro F, et al. Sequential endovascular thrombectomy approach (SETA) to acute ischemic stroke: preliminary single-centre results and cost analysis. Radiol Med 2015;120:655–61. [DOI] [PubMed] [Google Scholar]
- [9].BMJ Publishing Group, Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-analyses: The PRISMA Statement. BMJ (Clinical research ed.) 2009;b2535-5. [PMC free article] [PubMed] [Google Scholar]
- [10].Lapergue B, Blanc R, Guedin P, et al. A Direct Aspiration, First Pass Technique (ADAPT) versus stent retrievers for acute stroke therapy: an observational comparative study. AJNR Am J Neuroradiol 2016;37:1860–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lapergue B, Blanc R, Gory B, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel Occlusion: The ASTER randomized clinical trial. JAMA 2017;318:443–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Mokin M, Sonig A, Sivakanthan S, et al. Clinical and procedural predictors of outcomes from the endovascular treatment of posterior circulation strokes. Stroke 2016;47:782–8. [DOI] [PubMed] [Google Scholar]
- [13].Mokin M, Primiani CT, Ren Z, et al. Endovascular treatment of middle cerebral artery M2 occlusion strokes: clinical and procedural predictors of outcomes. Neurosurgery 2017;81:795–802. [DOI] [PubMed] [Google Scholar]
- [14].Maegerlein C, Prothmann S, Lucia KE, et al. Intraprocedural thrombus fragmentation during interventional stroke treatment: a comparison of direct thrombus aspiration and stent retriever thrombectomy. Cardiovasc Intervent Radiol 2017;40:987–93. [DOI] [PubMed] [Google Scholar]
- [15].Stapleton CJ, Leslie-Mazwi TM, Torok CM, et al. A direct aspiration first-pass technique vs stent retriever thrombectomy in emergent large vessel intracranial occlusions. J Neurosurg 2017;128:1–8. [DOI] [PubMed] [Google Scholar]
- [16].Gerber JC, Daubner D, Kaiser D, et al. Efficacy and safety of direct aspiration first pass technique versus stent-retriever thrombectomy in acute basilar artery occlusion-a retrospective single center experience. Neuroradiology 2017;59:297–304. [DOI] [PubMed] [Google Scholar]
- [17].Gory B, Mazighi M, Blanc R, et al. Mechanical thrombectomy in basilar artery occlusion: influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg 2018;1–0. [DOI] [PubMed] [Google Scholar]
- [18].Nishi H, Ishii A, Nakahara I, et al. Different learning curves between stent retrieval and a direct aspiration first-pass technique for acute ischemic stroke. J Neurosurg 2018;1–8. [DOI] [PubMed] [Google Scholar]
- [19].Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Khatri P, Yeatts SD, Mazighi M, et al. Time to angiographic reperfusion and clinical outcome after acute ischaemic stroke: an analysis of data from the Interventional Management of Stroke (IMS III) phase 3 trial. Lancet Neurol 2014;13:567–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zaidi SF, Shawver J, Espinosa Morales A, et al. Stroke care: initial data from a county-based bypass protocol for patients with acute stroke. J Neurointerv Surg 2017;9:631–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J 2013;368:914–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Dargazanli C, Consoli A, Barral M, et al. Impact of modified TICI 3 versus modified TICI 2b reperfusion score to predict good outcome following endovascular therapy. AJNR Am J 2017;38:90–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Saver JL, Jahan R, Levy EI, et al. SOLITAIRE™ with the intention for thrombectomy (SWIFT) trial: design of a randomized, controlled, multicenter study comparing the SOLITAIRE™ Flow Restoration device and the MERCI Retriever in acute ischaemic stroke. Int J Stroke 2014;9:658–68. [DOI] [PubMed] [Google Scholar]
- [25].Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet 2012;380:1231–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kleine JF, Wunderlich S, Zimmer C, et al. Time to redefine success? TICI 3 versus TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. J Neurointerv Surg 2017;9:117–21. [DOI] [PubMed] [Google Scholar]
- [27].Suh SH, Cloft HJ, Fugate JE, et al. Clarifying differences among thrombolysis in cerebral infarction scale variants: is the artery half open or half closed? Stroke 2013;44:1166–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Phan K, Dmytriw AA, Teng I, et al. A Direct aspiration first pass technique vs standard endovascular therapy for acute stroke: a systematic review and meta-analysis. Neurosurgery 2017;83:19–28. [DOI] [PubMed] [Google Scholar]
- [29].Kowoll A, Weber A, Mpotsaris A, et al. Direct aspiration first pass technique for the treatment of acute ischemic stroke: initial experience at a European stroke center. J Neurointerv Surg 2016;8:230–4. [DOI] [PubMed] [Google Scholar]
- [30].Turk AS, Frei D, Fiorella D, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg 2014;6:260–4. [DOI] [PubMed] [Google Scholar]
- [31].Kass-Hout T, Kass-Hout O, Sun C-HJ, et al. Longer procedural times are independently associated with symptomatic intracranial hemorrhage in patients with large vessel occlusion stroke undergoing thrombectomy. J Neurointerv Surg 2016;8:1217–20. [DOI] [PubMed] [Google Scholar]
- [32].Mokin M, Setlur Nagesh SV, Ionita CN, et al. Comparison of modern stroke thrombectomy approaches using an in vitro cerebrovascular occlusion model. AJNR Am J Neuroradiol 2015;36:547–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


