Abstract
Background:
Global literature suggests that resilience-based interventions may yield improvements in psychosocial well-being for vulnerable children, but limited data are available regarding the efficacy of such interventions among children affected by parental HIV/AIDS.
Objective:
To evaluate initial efficacy of a multi-level resilience-based intervention among children affected by parental HIV/AIDS in China in improving children’s psychosocial well-being and resilience-related outcomes.
Method:
Seven hundred-ninety children, 6 to 17 years of age, were recruited from rural China. Children were either AIDS orphans or were living with one or two parents infected with HIV/AIDS. Children and primary caregivers were randomly assigned to participate in a 4-arm trial to evaluate the Child-Caregiver-Advocacy Resilience (ChildCARE) intervention. This resilience-based HIV intervention provides programming at three levels (child, caregiver, community). Initial survey data were collected at baseline, 6-months, and 12-months in order to examine efficacy of the child-only and child+caregiver arms in improving children’s resilience.
Results:
Intervention groups displayed improvements in several resilience-related outcomes at 6-and 12-month follow-ups, including self-reported coping, hopefulness, emotional regulation, and self-control. The child-only intervention arm showed some fading of intervention effects by 12-months.
Conclusion:
Preliminary findings suggest that the ChildCARE intervention is efficacious in promoting psychosocial well-being of children affected by parental HIV/AIDS in rural China. Targeting both children and caregivers for psychosocial intervention may be effective in improving children’s resilience. Additional evaluation and modifications, including the inclusion of booster sessions, should be considered to further strengthen the program.
Keywords: Children affected by HIV, Parental HIV/AIDS, resilience, intervention, China
Parental chronic illness or death is a profoundly adverse life event for impacted children and may cause significant stress for both child and family (Luecken & Roubinov, 2012; Nickerson, Bryant, Aderka, Hinton, & Hofmann, 2013). Children of parents with HIV/AIDS are particularly vulnerable to a range of long-lasting and negative physical, psychological, and socioeconomic outcomes (Cluver, Orkin, Boyes, Sherr, Makasi, & Nikelo, 2013; Cluver, Orkin, Gardner, & Boyes, 2011; Sherr et al., 2008). A large body of literature has established that this group frequently faces the experience of stigma, disruptions in caregiving, reduced educational access, and financial hardship (Foster & Williamson, 2000; Guo, Li, & Sherr, 2012). However, despite these adversities, many affected children do not report clinically significant or even elevated levels of mental health problems over time (Chi, Li, Barnett, Zhao, & Zhao, 2013; Li et al., 2009; Pelton & Forehand, 2005). This finding aligns with the nearly fifty years of research on the ability of children to display resilience in the face of stress and hardship (Luthar, 2006; Cicchetti & Curtis, 2006; Masten, 2011).
Resilience is characterized as a dynamic process that allows for positive adaptation despite the experience of adversity (Luthar, Cicchetti, & Becker, 2000; Masten & Narayan, 2012). Studies of children exposed to a range of adversities, including war, disaster, poverty, maltreatment, and parental illness suggest the existence of a set of “resilience factors”, such as positive future orientation, problem-solving skills, trusting relationships, effective school experiences, and a supportive community, that are associated with enhanced physical and psychosocial outcomes (Cicchetti & Toth, 2006a, 2006b; Masten & Narayan, 2012; Rutter, 1985). Resilience occurs when one or more such factors provide protection from the harmful effects of adversity. Thus, resilience typically arises from fundamental and even ordinary human adaptive systems that can be found within individuals, relationships, families, communities, and societies. Though these adaptive systems may be hindered by adversity (e.g., death of family member, natural disaster, etc.), they are theorized to be integral in producing what has been termed the “ordinary magic” of childhood resiliency (Masen, 2001, p. 227; Masten & Narayan, 2012). In contrast to a traditional psychopathology model, unique features of a resilience framework include its focus on socio-ecological strength and its capacity for positive adaptation. A resilience approach is also well suited for intervention development given its focus on the increasing socio-ecological supports within a child’s environment (Li et al., 2015; Lin et al., 2016). This paradigm shift results in a transformative approach to cultivating the resilience of children affected by HIV/AIDS.
Current estimates place the number of individuals affected worldwide by HIV/AIDS at 35 million, with the vast majority residing in low- and middle-income countries (LMICS; World Health Organization [WHO], 2013). Incidence of HIV is highest among young and middle-aged adults, with 35% of new infections occurring among young people, ages 15 to 24 (Centers for Disease Control and Prevention, 2014; WHO, 2013). This places a disproportionate burden on children and young families. Currently, there are 16.6 million children between the ages of 0 and 17 who have been orphaned by AIDS (UN Joint Programme on HIV/AIDS [UNAIDS], 2010). There are also millions of children who have parents living with HIV/AIDS, generally termed children made “vulnerable” by HIV/AIDS (Mishra & Bi gnami-Van Assche, 2008). While substantial work has examined the risks that parental HIV/AIDS poses for a child, emerging research is now investigating the resilience of these children—both why some children thrive despite such adversity and how to develop more resilient children, families, and communities that can adapt to the unique challenges of the epidemic.
A recently proposed framework (Li et al., 2015) delineates the mechanisms of resilience in children’s adaptation to parental HIV/AIDS and identifies protective factors at the individual, family, and community levels (Figure 1). The framework is guided by socio-ecological theories of child development and psychological resilience (Bronfenbrenner, 1979, 1989; Masten, Best, & Garmezy, 1990) and emphasizes malleable individual and contextual factors, with support from family and community theorized to foster development of children’s internal assets (e.g., coping skills, metacognitive skills, etc.).
Figure 1.
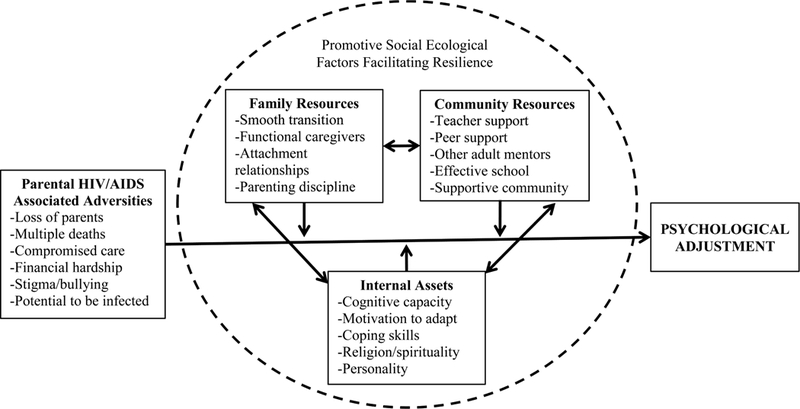
A Conceptual Framework of Psychological Resilience among Children affected by HIV/AIDS. This figure illustrates risk and resilience factors associated with psychological adjustment for children affected by parental HIV/AIDS. Adapted from Li, Chi, Sherr, Cluvery, & Stanton (2015).
Global literature suggests that resilience-based approaches can improve psychosocial well-being of vulnerable children in low- and middle-income countries (de Villiers & van der Berg, 2012; Leventhal et al., 2016). However, intervention research remains limited among children affected by HIV/AIDS, as noted by several recent reviews (Betancourt, Meyers-Ohki, Charrow, & Hanson, 2013; Chi & Li, 2013; King, Silva, Stein, & Patel, 2009; Qiao, Li, & Stanton, 2011). There is also a lack of multi-level conceptual models of HIV intervention. Therefore, based on the conceptual framework and with the support of the US National Institutes of Health, we developed a resilience-based psychosocial intervention that seeks to promote well-being among children affected by parental HIV/AIDS.
The Child-Caregiver-Advocacy Resilience (ChildCARE) intervention consists of programming at three levels: child, caregiver, and community, and is tailored to the language and culture of individuals affected by HIV/AIDS in rural central China. The child intervention includes 20 hours of facilitator-guided programming delivered in 10 sessions in a peer-group setting and aims to increase resilience by developing several skills, including positive thinking, emotional regulation, coping, and problem solving (see Supplementary Data for session content and full intervention manuals). At the caregiver level, caregivers receive 10 hours of facilitator-guided programming delivered in five sessions that aims to increase positive parenting skills and build the capacity of the caregiver to engage in self-care and seek support. At the community level, trained community advocates (e.g., teachers, village nurses) conduct monthly home visits and organize a series of community-based activities over a period of two years to promote cohesion and strength within local communities and to increase community support for affected families.
Initial evaluation of ChildCARE was undertaken using a community-based 4-arm cluster randomized controlled trial conducted from 2012 to 2016. Seven hundred and ninety children from rural central China aged 6 to 17 were recruited to participate in the trial. Each participating child and one of his or her primary caregivers formed a dyad that was randomly assigned by community cluster to one of four intervention conditions: child-only intervention (n=200 dyads), child+caregiver intervention (n=198 dyads), child+caregiver+community intervention (n=197 dyads), or control (n=195 dyads). Due to resource constraints, the three components of ChildCARE were delivered to children and their caregivers at different time points (see Figure 2 for timeline). This schedule enables comparison of the child-only and control groups at 6 months and comparison of child-only, child+caregiver, and control groups at 12 months, without considering the add-on effects of community-based intervention. Comprehensive outcome data were collected at 6-month intervals throughout the three-year intervention period. The current study analyzes child self-report data at baseline, 6-months, and 12-months to assess the short-term effects of child-only and child+caregiver interventions on resiliency.
Figure 2.
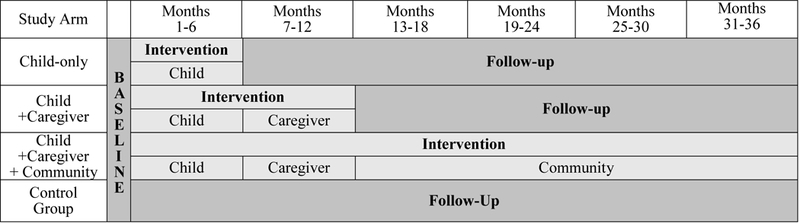
Study timeline. Pilot-testing of the ChildCARE intervention employed community-based 4-arm cluster randomization with intervention components delivered at different time points. The current study reports intervention effects at 6-months (child vs. control) and 12-months, (child vs. child+caregiver vs. control).
Method
Recruitment and Sample Characteristics
Children and caregivers were recruited from five rural villages in Henan province in central China where a large HIV epidemic has existed since the early 1990s, primarily resulting from unhygienic commercial blood and plasma collection practices. We first obtained village-level HIV surveillance data from provincial anti-epidemic stations in order to identify villages with the highest HIV prevalence and then generated a list of families caring for children affected by parental HIV/AIDS in each village with the assistance of local schools and social welfare systems. Children were eligible for the study if they were ages 6 to 17 and had a biological parent with HIV/AIDS (i.e., alive or deceased). Children with known HIV infection were excluded from participation. From a list of eligible participants, random selection was used to invite children/caregivers to participate in the study until the target sample size was achieved (i.e., ~800 dyads). Participating children were clustered based on community location, and these community clusters served as the units of randomization. Clusters were further broken down by children’s schools and grade levels, resulting in the creation of 45 school-based peer groups (mean of 17.5 children per group). Intervention content was delivered to these peer groups and caregivers by facilitators with training in psychology or education. The research protocol was approved by Institutional Review Boards at Henan University, Wayne State University, and the University of South Carolina.
Our sample included 790 Chinese children aged 6 to 17 years, with 94.4% (n=746) aged 8 to 15 years (see Table 1). Girls comprised 48.4% (n=382) of the participant sample, while boys accounted for 51.6% (n=408). The average age of the children was 10.5 years (SD=2.0). Over 97% of the sample was of Han ethnicity, the predominant ethnicity in China. Approximately 12.4% (n=98) of the children were HIV/AIDS orphans (i.e., WHO defines orphan as a child who has lost one or both parents to HIV/AIDS). Of the total sample, 9.3% (n=72) had lost one parent to AIDS (i.e., “single orphan”) and 3.1% ( n=24) had lost both parents to AIDS (i.e., “double orphan”). Approximately 87.7% ( n=680) of children reported that one (72.6%) or both (15.1%) parents were currently living with HIV/AIDS. The average number of siblings was 1.8 (SD=1.2). Children reported low overall levels of parental education, with 59.3% of fathers and 58.2% of mothers having less than a high school education. The most endorsed parental occupations were farmers (46.2% of mothers; 32.9% of fathers) and migrant workers (28.3% of mothers; 42.6% of fathers).
Table 1.
Demographic Characteristics by Intervention Assignment.
| Overall | Control | Intervention1 | Intervention Condition at 12m f/u |
||
|---|---|---|---|---|---|
| Child-Only | Child+Caregiver2 | ||||
| N(%) | 790 (100%) | 195 (24.7%) | 595 (75.3%) | 200 (25.3%) | 395 (50.0%) |
| Boys | 408 (51.6%) | 113 (57.9%) | 295 (49.6%)* | 96 (48.0%) | 199 (50.4%) |
| Mean Age (SD) | 10.51(2.0) | 10.62(2.1) | 10.47(2.0) | 11.24(2.3) | 10.08(1.6)**** |
| Han Ethnicity | 757(99.2%) | 188(98.4%) | 569(99.5%) | 195(99.5%) | 374(99.5%) |
| # of Siblings | 1.77(1.2) | 1.80(0.9) | 1.76(1.2) | 1.72(1.1) | 1.78(1.3) |
| Parental Status | |||||
| Single Infection | 563(72.6%) | 134(73.6%) | 429(72.2%) | 129(64.5%) | 300(76.1%)** |
| Double Infection | 117(15.1%) | 19(10.4%) | 98(16.5%) | 46(23.0%) | 52(13.2%) |
| Single Death | 72(9.3%) | 22(12.1%) | 50(8.4%) | 20(10.0%) | 30(7.6%) |
| Double Death | 24(3.1%) | 7(3.8%) | 17(2.9%) | 5(2.5%) | 12(3.0%) |
| Familial HIV Death & Infection | |||||
| # of deaths in household |
0.5(0.8) | 0.5(0.9) | 0.4(0.7) | 0.4(0.8) | 0.4(0.7) |
| # of infections in household |
1.1(1.0) | 1.1(1.2) | 1.1(1.0) | 1.2(0.9) | 1.0(1.0)* |
| # of deaths among relatives |
0.4(1.1) | 0.5(1.0) | 0.4(1.1) | 0.5(1.0) | 0.4(1.1) |
| # of infections among relatives |
0.8(1.5) | 0.9(1.5) | 0.8(1.5) | 0.9(1.4) | 0.7(1.6) |
| Father Education | |||||
| No Formal Schooling |
19(2.4%) | 2(1.0%) | 17(2.9%) | 6(3.0%) | 11(2.8%) |
| Elementary | 255(32.5%) | 66(34.2%) | 189(32.0%) | 67(33.5%) | 122(31.2%) |
| Middle | 191(24.4%) | 50(25.9%) | 141(23.9%) | 73(36.5%) | 68(17.5%) |
| High School | 61(7.8%) | 16(8.3%) | 45(7.6%) | 10(5.0%) | 35(9.0%) |
| Post-secondary | 51(6.5%) | 12(6.2%) | 39(6.6%) | 8(4.0%) | 31(7.9%) |
| Don’t Know | 207(26.4%) | 47(24.4%) | 160(27.1%) | 36(18.0%) | 124(31.7%)* |
| Mother Education | |||||
| No Formal Schooling |
46(6.0%) | 11(5.8%) | 35(6.0%) | 12(6.1%) | 23(6.0%) |
| Elementary | 249(32.3%) | 64(33.7%) | 185(31.8%) | 71(35.9%) | 114(29.7%) |
| Middle | 154(19.9%) | 116(19.9%) | 38(20.0%) | 55(27.8%) | 61(15.9%) |
| High School | 59(7.6%) | 16(8.4%) | 43(7.4%) | 12(4.1%) | 31(8.1%) |
| Post-secondary | 46(6.0%) | 8(4.2%) | 38(6.5%) | 9(4.5%) | 29(7.6%) |
| Don’t Know | 218(28.2%) | 53(27.9%) | 165(28.4%) | 39(19.7%) | 126(32.8%)** |
Notes.
Intervention group includes both child-only and child+caregiver groups;
Significance level in this column denotes the overall difference among control, child-only intervention, and child+caregiver intervention.
p <.05
p <.01
p <.001
p <.0001
Data Collection
As children’s self-report data are the only outcome measures reported in the current study, only procedures relevant for these measures are described here. See work by Chi and colleagues (2015) as well as Wei, Li, Harrison, Zhao, and Zhao (2016) for further description of recruitment and other outcome measures collected at baseline (e.g., caregiver-reported data, teacher-reported data). For the current study, children completed self-report questionnaires at baseline, 6-months, and 12-months that included demographic and psychosocial scales. The questionnaire was self-administrated individually or in small groups in the presence of two interviewers. Around 2% of the sample were too young to read or had reading difficulties; for these children, interviewers read survey items aloud and recorded children’s oral responses in a private room. If a private room was not available, the interviewer read the survey items to the child and asked the child to indicate his or her response directly on the questionnaire. Children received small, age-appropriate gifts at completion of each data collection period as tokens of appreciation.
Study Measures
Measures that had not previously been used with Chinese samples were forward and back translated by a team of researchers fluent in both Mandarin and English, following a standard protocol (Li et al., 2009).
Demographic characteristics.
Children provided information about their age, gender, ethnicity, parents’ education and occupations, orphan status, and presence of additional HIV-infected individuals in the household.
Resilience.
Children’s resilience was measured with the Connor-Davidson Resilience Scale (CD-RISC), a 25-item rating scale that assesses ability to cope with stress and adapt in the face of adversity (Connor & Davidson, 2003). The scale has been translated into Chinese and used in previous resilience studies of Chinese children (Yu & Zhang, 2007; Yu et al., 2011). Items on the CD-RISC are rated on a 5-point scale (i.e., 0 to 4), with higher scores reflecting greater resilience. Participants responded to questions such as “I tend to bounce back after illness or hardship” and “I can handle unpleasant feelings”. Cronbach’s α for the CD-RISC ranged from 0.88 to 0.90 in the three waves of survey data.
Positive coping.
A subscale was adapted from the Children’s Coping Strategies Checklist (Ayers, Sandier, West, & Roosa, 1996) to assess children’s positive and active coping strategies. Children were asked to describe the extent to which various coping statements described their actions (e.g., “I will tell myself the problem will be solved very soon”). They responded to 12 items on a 4-point Likert scale (1=strongly disagree to 4=strongly agree). Cronbach’s α for the scale was 0.75 at baseline, 0.81 at 6-months, and 0.82 at 12-months.
Support seeking.
A subscale from the Children’s Coping Strategies Checklist (Ayers, Sandier, West, & Roosa, 1996) was also adapted to assess children’s competence in seeking support from others. Children were asked to rate their support-seeking actions by responding to9 four items (e.g., “I will ask my teacher for help”) using the same 4-point Likert scale (1=strongly disagree to 4=strongly agree). Cronbach’s α in the three waves of survey ranged from 0.61 to 0.81.
Posttraumatic growth.
Children’s experience of positive change in the aftermath of adversity was assessed using a version of the Posttraumatic Growth Inventory for Children-Revised (PTGI-C-R; Cryder, Kilmer, Tedeschi, & Calhoun, 2006; Kilmer et al., 2009). The PTGI-C-R was previously modified and validated with a sample of Chinese children (Yu et al., 2010). Children responded to eight items on a 4-point scale (0=never to 3=often) to indicate their experience of positive effects in the aftermath of trauma (e.g., “I appreciate each day more than I used to”; “I can now handle problems better than I used to”). Cronbach’s α ranged from 0.77 to 0.86 in the three waves of the current study.
Hopefulness.
Children reported their expectations and hopefulness about their future by responding to a brief hopefulness scale utilized in prior studies with Chinese children (Li et al., 2009). Children responded to four items to indicate how likely they were to reach future milestones such as graduating from high school or securing a job. Children provided responses using a 4-point Likert scale (1=will not happen to 4=will definitely happen). Cronbach’s α of the hopefulness scale ranged from 0.73 to 0.78 in the three waves of data collection.
Perceived control over future.
Children’s perceived control of future events was measured with a brief scale that was initially adapted from the Perceived Control over the Future Scale (Whitaker, Miller, & Clark, 2000) and later modified and validated with Chinese children (Li et al., 2009). Children were asked to indicate their agreement with seven statements (e.g., “What happens to me in the future mostly depends on me”; “My future is what I make of it”) using a 4-point Likert scale (1=strongly disagree to 4=strongly agree). Cronbach’s α in the three waves of data collection were 0.72 (baseline), 0.77 (6-months), and 0.82 (12-months).
Self-esteem.
Children’s global self-esteem was measured with a 16-item scale modeled after a previously developed personality questionnaire (Gosling, Rentfrow, Swann, 2003). Children provided information about self-worth and self-image by indicating their agreement with a variety of statements (e.g., “I believe I am a person of worth”, “I have a number of good qualities”) using a 4-point response option (1=stro ngly disagree to 4=strongly agree). This scale demonstrated good internal consistency in the current study (Cronbach’s α =0.93 for baseline, 0.94 at 6-months, and 0.95 at 12-months).
Positive emotion.
To measure positive emotion, children were asked to complete a modified version of the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988). From the initial PANAS, a 10-item short form was developed and found to be reliable and valid for use with respondents from a wide range of cultural backgrounds (Thompson, 2007). Children indicated the extent to which they felt a particular positive emotion (e.g., enthusiastic, proud, energized) within that past six months using a 5-point scale (1=not at all to 5=very much). Cronbach’s α in three waves ranged from 0.70 to 0.77.
Emotion regulation.
The six-item Emotional Regulation subscale of the Social Competence Scale (Conduct Problem Prevention Research Group, 1995; Corrigan, 2002, 2003) was used to assess children’s ability to regulate emotions. The subscale was slightly modified to address cultural differences in emotional constructs. Children rated their competence in adjusting emotions when necessary (e.g., “I can control tempe r when I have a disagreement with my friends”) using a 4-point scale (1=does not suit me at all to 4=suits me totally). Cronbach’s α in the three waves ranged from 0.63 to 0.76.
Statistical Analyses
First, demographic and other key study variables were compared between intervention and control groups at the baseline using t tests for continuous variables and χ2-tests for categorical variables. An intent-to-treat approach was used to examine intervention effects on primary outcomes. Thus, analyses included all children who were randomized into either the child-only group (n=200), the two groups that had received the child+caregiver components at 12-month follow-up (i.e., child+caregiver and child+caregiver+community groups; n=390), or the control group (n=195). Missing data at the follow-up assessments (e.g., at 12 months: 13.5% child; 10.3% child+caregiver; 18.7% control) were accounted for in the mixed-effects models using maximum likelihood estimation.
Second, to assess the impact of the child-only and child+caregiver interventions, we ran a series of random effect difference score models to compare mean change over time across treatment arms from baseline to 6- and 12-month follow-ups, respectively. Following recommendations in the literature (Rogosa, 1988; Rogosa, Brandt, & Zimowski, 1982; Rogosa & Willet, 1985), we employed random-effects difference score models due to the significant baseline differences in a number of outcome variables across treatment arms, thus violating an assumption of other standard multivariate models such as ANCOVA.
We controlled for baseline differences (child age and number of HIV/AIDS-infected individuals in the household) in all analyses. School identifiers and child groups were modeled as random effects to dis-attenuate standard errors and account for the hierarchical nature of the data structure (i.e., repeated measures nested within children and child groups nested within school). Restricted maximum likelihood (REML) was invoked for model estimation, effectively estimating mean and variance parameters as well as handling missing data on outcome variables. The p-values for multiple comparisons were adjusted by the Tukey-Kramer method. All analyses were generated using SAS® software (Version 9.4; SAS Institute, 2013), employing the PROC MIXED analysis framework.
Results
Sample Characteristics and Attrition Analysis
Descriptive statistics are presented in Table 1. Average age differed significantly among the three groups at baseline, F(2,787)=24.08, p<.0001. In addition, children in the child+caregiver group reported significantly less HIV infections in the household than other groups, F(2,763)=3.50, p<.05. At 12-month follow-up, 86.9% of the sample (n=680) completed assessments.
Baseline Differences in Outcome Measures
Mean comparisons of outcome variables at baseline are presented in Table 2. There were significant differences in a number of baseline measures with the control group displaying higher resilience, F(2,779)=11.71, p<.0001, posttraumatic growth, F(2,775)=5.81, p<.01, hopefulness toward future, F(2,772)=5.35, p<.01, and perceived control over the future, F(2,773)=8.35, p<.001. These baseline imbalances led to the choice of difference score models as our primary analytic approach; difference score models provide a natural estimate of change that allows for examination of whether existing differences between groups persist across time. Using difference score modeling, the null hypothesis is that baseline differences remain constant and there would thus be no mean change across measurement occasions. This contrasts to an ANCOVA model that assumes baseline equivalence and evaluates mean differences at posttest controlling for baseline measurement and other applicable covariates. With ANCOVA modeling, the null hypothesis considers naturally occurring regression to the mean and assumes no posttest mean differences.
Table 2.
Comparison of Outcome Measures by Intervention Assignment at Baseline.
| Outcomes | Control group (n=195) |
Intervention group overall (n=595) |
F (Control vs Intervention overall) |
Intervention groups |
F (Control vs Child-only vs Child+Caregiver) |
|
|---|---|---|---|---|---|---|
| Child-only (n=200) |
Child+Caregiver (n=395) |
|||||
| Resilience | 2.20(0.61) | 1.96(0.62) | 21.89**** | 2.00(0.66) | 1.93(0.59) | 11.71**** |
| Positive coping | 2.86(0.49) | 2.76(0.51) | 4.77* | 2.77(0.50) | 2.76(0.51) | 2.41 |
| Support-seeking | 2.60(0.71) | 2.55(0.69) | <1 | 2.55(0.66) | 2.55(0.71) | <1.00 |
| Post-traumatic Growth |
2.84(0.61) | 2.75(0.61) | 3.24 | 2.65(0.63) | 2.80(0.60) | 5.83** |
| Hope | 2.95(0.70) | 2.77(0.67) | 9.54** | 2.82(0.64) | 2.75(0.69) | 5.35** |
| Control | 2.88(0.64) | 2.71(0.65) | 9.97** | 2.81(0.64) | 2.66(0.65) | 8.35**** |
| Self-esteem | 2.98(0.52) | 2.92(0.54) | 2.10 | 2.92(0.53) | 2.91(0.54) | 1.05 |
| Positive emotion | 2.98(0.67) | 2.89(0.67) | 2.58 | 2.86(0.70) | 2.91(.66) | 1.65 |
| Emotion regulation |
2.80(0.58) | 2.71(0.56) | 3.88* | 2.73(0.51) | 2.70(0.58) | 2.18 |
Note.
p <.05;
p <.01;
p <.001;
p<.0001
Rogosa and colleagues (1988, 1982, 1985) have clarified the utility of examining difference scores to evaluate pretest-posttest change in the presence of baseline imbalances across groups, particularly with moderate or small correlations across measurement occasions that allow for observable differences in growth. Specifically, given a pretest-posttest correlation of r=.60 and baseline measurement reliability of α=.60, the reliability of the difference score across measurement occasions is α=.86 (Rogosa, 1988). Importantly, this estimate only improves with decreases in pretest-posttest correlation and increases in reliability of component measurements. For the current analyses, correlations across time points for variables that displayed significant baseline imbalance (p<.05) ranged from r=.11 to r=.34, providing a high level of confidence that difference score modeling is adequately able to control for baseline difference and detect change over time.
Intervention Effects: Child-only Intervention
Intervention effects at the 6-month follow-up appear in Table 3. By then, all children assigned to all intervention conditions (n=595) had received the child-only intervention. Results from the mixed-effect difference score models indicate that mean change from baseline to 6-months in the child-only intervention significantly differed from the mean change in the control group for resilience (p<.01; Cohen’s d=0.89), support-seeking (p<.05; Cohen’s d=0.82) and positive emotion (p<.05; Cohen’s d=0.69). Please see Table 3 for parameter estimates, standard errors, and exact p-values, with the child-only intervention displaying greater increases in these outcome variables. Additionally, marginally significant differences (i.e., p<.10) in mean change were observed across child-only and control treatment arms for self-esteem and positive coping (Cohen’s d=0.55 and Cohen’s d=0.52, respectively), with the child-only intervention again showing greater increases.
Table 3.
Random Effect Models assessing Results of the Child-only Intervention at 6-month follow-up.
| Variable | Estimate | Standard Error | p-value |
|---|---|---|---|
| Resilience | 0.2158 | 0.0741 | 0.0057** |
| Positive coping | 0.1237 | 0.0725 | 0.0949+ |
| Support seeking | 0.2015 | 0.0748 | 0.0101* |
| Post-traumatic growth | 0.1362 | 0.0897 | 0.1361 |
| Hope | 0.1441 | 0.0903 | 0.1180 |
| Control | 0.1398 | 0.0912 | 0.1323 |
| Self-esteem | 0.1564 | 0.0868 | 0.0786+ |
| Positive emotion | 0.2276 | 0.1005 | 0.0286* |
| Emotional regulation | 0.1286 | 0.0838 | 0.1323 |
Note. Effects represent contrasts of change scores from baseline to 6-month follow-up scores between child-only intervention and control group.
denotes significance at p<.10.
denotes significance at p<.05.
denotes significance at p<.01.
Intervention effects at 12-month follow-up are presented in Table 4. The child-only intervention displayed significantly more posttraumatic growth than the control group (p<.05). While there was a positive trend in other outcome measures, the changes, in comparison to the control group, did not reach statistical significance.
Table 4.
Comparison of Outcome Measures by Intervention Assignment at 12-month follow-up.
| Child-only vs Child+Caregiver | Child-only vs Control | Child+Caregiver vs Control | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Estimate | Standard Error |
p-value | Estimate | Standard Error |
p-value | Estimate | Standard Error |
p-value |
| Resilience | −0.0435 | 0.1040 | 0.6781 | 0.1890 | 0.1154 | 0.1089 | 0.2325 | 0.0973 | 0.0215* |
| Positive Coping |
−0.0799 | 0.0743 | 0.2884 | 0.1350 | 0.0849 | 0.1195 | 0.2149 | 0.0729 | 0.0052** |
| Support seeking |
0.1051 | 0.0817 | 0.2052 | 0.1564 | 0.0964 | 0.1122 | 0.0513 | 0.0843 | 0.5460 |
| Post- traumatic growth |
0.0683 | 0.1056 | 0.5215 | 0.2451 | 0.1190 | 0.0457* | 0.1769 | 0.1014 | 0.0884+ |
| Hope | −0.1756 | 0.1108 | 0.1207 | 0.1093 | 0.1242 | 0.3839 | 0.2849 | 0.1057 | 0.0101* |
| Control | −0.1333 | 0.1120 | 0.2406 | 0.1873 | 0.1251 | 0.1418 | 0.3206 | 0.1062 | 0.0043** |
| Self- Esteem |
−0.0526 | 0.1006 | 0.6039 | 0.1161 | 0.1106 | 0.2999 | 0.1687 | 0.0928 | 0.0762+ |
| Positive Emotion |
−0.0513 | 0.1191 | 0.6688 | 0.1616 | 0.1324 | 0.2290 | 0.2130 | 0.1118 | 0.0637+ |
| Emotional Regulation |
−0.0694 | 0.1004 | 0.4933 | 0.1597 | 0.1116 | 0.1598 | 0.2290 | 0.0942 | 0.0194* |
Note. Effects represent contrast in change scores from baseline to 12-month follow-up among Child-only intervention, Child+Caregiver intervention, and Control groups.
denotes significance at p<.10.
denotes significance at p<.05.
denotes significance at p<.01.
Intervention Effects: Child+Caregiver Intervention
After the 6-month follow-up, the caregiver intervention was delivered, enabling comparison at 12-months between child-only, child+caregiver, and control groups. The child+caregiver intervention displayed significant differences in mean change from baseline to 12-month follow-up when compared with the control group, with significant improvements in resilience (p<.05; r=.38), positive coping (p<.01; r=.37), hope (p<.05; r=.41), control (p<.01; r=.46), and emotional regulation (p<.05; r=.38; see Table 4). Additionally, marginally significant differences (i.e., p<.10) in mean change were observed between the child+caregiver and control arms for self-esteem (r=.30), and positive emotion (r=.31). There was no significant difference in mean changes between the child+caregiver intervention group and child-only intervention group at 12-month follow-up.
Discussion
Initial evaluation of ChildCARE suggests that a multilevel intervention targeting both children and caregivers may be effective in building resilience for children affected by parental HIV/AIDS. The use of a 4-arm, randomized controlled trial design and a time-lagged delivery of intervention components enabled comparisons of a child-only intervention with a child+caregiver intervention. Children who participated in the 10-session peer program reported significantly greater resilience skills after six months than those who did not. They also reported greater capacity for seeking support from others as well as more positive emotions than HIV-affected children who did not participate in the intervention.
Parental HIV infection creates profound impacts on a child’s psychosocial well-being, and unsurprisingly, many impacted children display impaired psychopathologies, with previous reviews having identified increased rates of depression, increased externalization of problems, poorer social competence, and poorer sense of control for affected children (Chi & Li, 2013; Wild, 2001). Current findings suggest that a resilience-based program tailored to the unique needs of this group may—at least initially—yield ps ychosocial benefits that help to buffer these risks. The observed increases in resilience, support seeking, and positive emotion may stem from the 20 hours of psychoeducation and skill building that is involved in the intervention, with lessons addressing topics including positive thinking, adapting to change, and managing emotions.
In addition, intervention content was delivered within peer groups comprised of other children who also have experienced parental HIV/AIDS. Improvements in resilience, support seeking, and positive emotions may have resulted from the supportive environment that is created when children befriend others who identify and empathize with their experiences. This is consistent with previous literature that has examined the importance of the peer context for HIV-affected children (Cluver & Orkin, 2009; Du, Li, Chi, Zhao, & Zhao, 2015). Peer support groups have been found to be effective in producing positive psychological outcomes for children and adolescents infected with HIV/AIDS (e.g., Funch-Brentano et al., 2005; Kumakech, Cantor-Graae, Maling, & Bajunirwe, 2009), and similar mechanisms may be at work for peer groups composed of children affected by parental HIV/AIDS. There is also evidence to suggest that strengthening psychological well-being for this vulnerable group may be one way to combat the pervasive stigma that is often felt by HIV-infected and HIV–affected populations (Miller et al., 2016).
At 12-month follow-up, children who had participated in the peer intervention differed from those who had not in their reports of posttraumatic growth. Participating children reported more positive growth, a greater capacity to handle difficulties, and an increased appreciation for life. This link between peer support and posttraumatic growth has been found previously among Chinese children affected by HIV/AIDS (Mo, Lau, Yu, & Gu, 2014), and may reflect the power of social support and connectedness to bring about feelings of positive growth despite the hardships of parental HIV/AIDS.
However, improvements in other markers of resilience were not sustained at 12-month follow-up for children in the child-only intervention. The fade-out of some resilience effects for the child-only intervention warrants potential modifications to this arm of the program. ChildCARE was designed to include multiple intervention components, and a “stripped down” version that includes only child intervention may not be as robust as the multi-component intervention. If the child intervention is provided alone without caregiver and community components, it may be necessary to add booster sessions at regular intervals to serve as reminders of curriculum content and to provide refresher practice sessions for coping skills. Within the context of the HIV literature, booster or maintenance sessions have been found to be effective in sustaining healthy behaviors following HIV prevention counseling (Metcalf et al., 2005), and such booster sessions that could be conducted either in vivo or through mHealth venues (e.g., texting, mobile apps) that are garnering a growing evidence base in LMICs (Hall, Fottrell, Wilkinson, & Byass, 2014).
In addition to the child-only intervention, the current study also evaluated the effects of adding a caregiver training to the intervention. Children whose caregivers took part in a five session (i.e., 10 hour) positive parenting training showed significantly greater resilience at 12-months when compared to the control condition in several domains. The child and caregiver combination yielded significant improvements in children’s self-reported resilience, coping skills, hopefulness for the future, control over their lives, and ability to regulate emotions when compared to the control group. These findings lend support to recent calls to develop multi-level approaches to HIV-related behavior and care (Albarracín, Rothman, Di Clemente, & del Rio, 2010; Kaufman, Cornish, Zimmerman, & Johnson, 2014). Although multi-level interventions present numerous challenges to researchers and implementers alike (e.g., time-consuming, difficult to replicate and disseminate), the incorporation of multi-level factors that go beyond the individual and include peers, caregivers, and/or community members in interventions will push HIV social and behavioral science forward. Recent theoretical approaches that seek to address multi-level influences, such as the Network-Individual-Resource Model (Johnson et al., 2010), highlight the complex and influential interactions that occur between individuals and their wider networks and the capacity of these networks to shape behaviors, including the giving and receiving of psychosocial support.
Through parent training, caregivers of children affected by parental HIV may learn more effective strategies for resolving conflict, communicating effectively, and meeting the unique emotional and developmental needs of this group. The caregivers themselves may also see improved psychosocial functioning as a result of participation, and future studies should evaluate whether ChildCARE yields better psychological health, improved feelings of support, and reduced stress among caregivers. This is critical, as caring for a child affected by HIV/AIDS can pose significant psychological, financial, and social burdens, and caregivers of HIV-affected children in China have been found to be at increased risk for depression (Lv et al., 2010). The impact of caregiving for HIV-affected children warrants greater attention, and future studies are needed to determine how to expand and improve parenting training for these caregivers.
Children enrolled in the intervention faced challenges that extended beyond HIV/AIDS. They were rural and largely from poorly educated farming or migrant families. Despite these challenges, we saw high rates of families maintain involvement in the intervention over a 12-month period, suggesting that ChildCARE may be a feasible, culturally acceptable intervention for children and caregivers impacted by HIV in LMICs. This is particularly notable given that this appears to be the first implemented resilience-based intervention for children affected by HIV/AIDS in China.
Limitations
There are several limitations to the current study. First, we employed community-based cluster randomization to reduce risk of contamination between intervention and control groups. However, the use of clusters resulted in baseline un-equivalence on several baseline variables. We therefore employed difference modeling as our primary analytic approach, which should increase confidence in the findings. Future studies though may wish to recruit a more homogeneous sample across clusters.
Secondly, two aspects of our sample may limit generalizability of findings to other HIV-affected children: geographic location and HIV infection source. While findings may be potentially relevant for other LMICs, they may not replicate within high-income nations. Future efforts to tailor ChildCARE to cultural and societal norms as well as the socioeconomic and educational characteristics of the target audience will be necessary. In addition, the HIV epidemic in central China is distinct as it originated from unhygienic blood and plasma collection, and this was the likely infection route for parents of our sample. Thus, the psychosocial impacts of HIV may be unique for our sample, including aspects of HIV-related stigma. It is possible that families and children affected by the central China HIV epidemic may feel less stigmatized because of a “shared” communi ty burden of the disease and because most did not acquire HIV through a highly-stigmatized manner (e.g., sexual behavior, IV drug use). On the other hand, villages and local communities with high prevalence of HIV/AIDS may experience compounding effects of pervasive morbidity and mortality (e.g., widespread economic impact, lack of caregivers for young and old) that may worsen individual outcomes. Previous studies have found that despite the unique nature of infection (i.e., unhygienic blood and plasma collection practices), children impacted by parental HIV/AIDS in central China do typically report high levels of perceived public stigma and more psychological problems than peers whose families are unaffected (Lin et al., 2010; Zhao, Li, Zhao, Zhang, & Stanton, 2012).
A final area of limitation involves our measures. Some scales, most notably our measures of social support and emotional regulation, displayed relatively low reliability at baseline (0.061 and 0.63 respectively). Brief measures often have low internal reliability as α is dependent upon the magnitude of correlations among items, as well as the number of items (Streiner & Norman, 1989). Future studies may wish to expand the measures used to assess various resiliency factors. In addition, our intervention outcomes were measured via self-report, which is susceptible to some validity threats including social desirability bias. Finally, some measures had not been previously validated in China, and this could represent a threat to construct validity. Future studies should continue to develop psychosocial resilience measures validated for use in a Chinese population, and efforts to include parent and teacher behavioral ratings would strengthen confidence in findings.
Future Directions
The past decade has seen increased calls for the development of psychosocial interventions to improve well-being among children impacted by parental HIV/AIDS (Richter et al., 2009; Chandan & Richter, 2009), as well as a shift toward a resilience-based approach to understanding how vulnerable children cope with and adapt to adversity. While the current study contributes to this emerging global literature, future studies are needed to examine whether its initial efficacy is maintained over longer periods of time and to evaluate whether the addition of a community-based intervention (i.e., the third component of ChildCARE) provides additional benefits. Future efforts should explore whether changes in content or delivery (e.g., booster sessions) could strengthen and prolong effects, as well as evaluate mediating and moderating variables to provide a fuller picture of the intervention’s mechanisms. Nonetheless, ChildCARE represents a promising first step in developing resilience-based psychosocial programming for children, families, and communities impacted by HIV/AIDS in China. The observed improvements in a number of important aspects of well-being provide hope that building “ordinary magic” (Masten, 2001, p. 227) within and around the most vulnerable children is a task that can be accomplished.
Supplementary Material
Research Highlights:
Children affected by HIV face numerous threats to their psychosocial well-being.
Resilience-based interventions offer promise for vulnerable youth.
We created ChildCARE—a multi-level psychosocial HIV intervention for children.
ChildCARE yielded improvements in resilience for children affected by HIV in China.
Acknowledgement:
The authors also want to thank Bonita Stanton (Seton Hall University), Danhua Lin (Beijing Normal University), Cheuk Chi Tam (Virginia Commonwealth University), Shaobing Su (Tufts University), Chao Cai (University of South Carolina), and other team members for their contribution to study design, intervention curriculum development, data collection, and data analysis.
Disclosure: The study described in this report was supported by NIH Research Grants # R01MH076488 and R01NR013466 by the National Institute of Mental Health and the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institute of Nursing Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Albarracin D, Rothman AJ, Di Clemente R, & del Rio C (2010). Wanted: A theoretical roadmap to research and practice across individual, interpersonal, and structural levels of analysis. AIDS and Behavior, 14(S2), 185–188. doi: 10.1007/s10461-010-9805-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers TS, Sandier IN, West SG, & Roosa MW (1996). A dispositional and situational assessment of children’s coping: Testing alternative models of coping. Journal of Personality, 64(4), 923–958. doi: 10.1111/j.1467-6494.1996.tb00949.x [DOI] [PubMed] [Google Scholar]
- Betancourt TS, Meyers-Ohki SE, Charrow A, & Hansen N (2013). Annual Research Review: Mental health and resilience in HIV/AIDS-affected children—A review of the literature and recommendations for future research. Journal of child psychology and psychiatry, 54(4), 423–44. doi: 10.1111/j.1469-7610.2012.02613.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U (1979). The ecology of human development: Experiments by nature and design Cambridge, MA: Harvard University Press; Bronfenbrenner U. (1989). Ecological systems theory. Annals of Child Devleopment, 6, 187–249. [Google Scholar]
- Centers for Disease Control and Prevention. (2014). HIV surveillance report, 2014, volume 26 Atlanta: US Department of Health and Human Services; Retrieved from http://www.cdc.gov/hiv/library/reports/surveillance/ [Google Scholar]
- Chandan U & Richter L (2009). Strengthening families through early intervention in high HIV prevalence countries. AIDS Care, 21(s1), 76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi P & Li X (2013). Impact of parental HIV/AIDS on children’s psychological well-being: A systematic review of global literature. AIDS Behavior, 17(7), 2554–2574. doi: 10.1007/s10461-012-0290-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi P, Li X, Barnett D, Zhao J, & Zhao G (2013). Do children orphaned by AIDS experience distress over time? A latent growth curve analysis of depressive symptoms. Psychology, Health & Medicine, 19(4), 420–432. doi: 10.1080/13548506.2013.841965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi P, Li X, Chi Tam C, Du H, Zhao G, & Zhao J (2015). Parenting mediates the impact of caregivers’ distress on children’s well-being i n families affected by HIV/AIDS. AIDS Behavior, 19, 2130–2139. doi: 10.1007/s10461-015-1104-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, & Curtis WJ (2006). The developing brain and neural plasticity: Implications for normality, psychopathology, and resilience. In Cicchetti D & Cohen DJ (Eds.), Developmental psychopathology: Developmental neuroscience (Vol. 2, 2nd ed., pp. 1– 64). Hoboken, NJ: Wiley. [Google Scholar]
- Cicchetti D, & Toth SL (2006a). A developmental psychopathology perspective on preventive interventions with high risk children and families. In Renninger A and Sigel I (Eds.), Handbook of child psychology (6th ed., p. 497–547). New York: Wiley. [Google Scholar]
- Cicchetti D., & Toth SL (Eds.). (2006b). Translational Research in Developmental Psychopathology. [Special Issue]. Development and Psychopathology, 18(3), 619–933. [DOI] [PubMed] [Google Scholar]
- Cluver LD & Orkin M (2009). Cumulative risk and AIDS-orphanhood: Interactions of stigma, bullying and poverty on child mental health in South Africa. Social Science & Medicine, 69(8), 1186–1193. doi: 10.1016/j.socscimed.2009.07.033 [DOI] [PubMed] [Google Scholar]
- Cluver L, Orkin M, Gardner F, & Boyes M (2011). Persisting mental health problems among AIDS-orphaned children in South Africa. Journal of Child Psychology and Psychiatry, 53(4), 363–370. doi: 10.1111/j.1469-7610.2011.02459.x [DOI] [PubMed] [Google Scholar]
- Cluver L, Orkin M, Boyes ME, Sherr L, Makasi D, & Nikelo J (2013). Pathways from parental AIDS to child psychological, educational, and sexual risk: Developing an empirically-based interactive theoretical model. Social Science & Medicine, 87, 185–193. 10.1016/j.socscimed.2013.03.028 [DOI] [PubMed] [Google Scholar]
- Conduct Problem Prevention Research Group. (1995). Psychometric properties of the social competence scale: Teacher and parent ratings. Fast Track Project technical report University Park, PA: Pennsylvania State University. [Google Scholar]
- Connor KM, & Davidson JR (2003). Development of a new resilience scale: The Connor‐ Davidson resilience scale (CD‐RISC). Depression and anxiety, 18, 76–82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Corrigan A (2002). Social Competence Scale – Pare nt Version, Grade 1/Year 2 (Fast Track Project Technical Report) Available from the fast Track Project Web site, http://www.fasttrackproject.org/
- Corrigan A (2003). Social Competence Scale – Pare nt Version, Grade 2/Year 3 (Fast Track Project Technical Report) Available from the fast Track Project Web site, http://www.fasttrackproject.org/
- Cryder CH, Kilmer RP, Tedeschi RG, & Calhoun LG (2006). An exploratory study of posttraumatic growth in children following a natural disaster. American Journal of Orthopsychiatry, 76(1), 65–69. doi: 10.1037/0002-9432.76.1.65 [DOI] [PubMed] [Google Scholar]
- de Villiers M & van den Berg H (2012). The implementation and evaluation of a resiliency programme for children. South African Journal of Psychology, 42(1), 93–102. [Google Scholar]
- Du H, Li X, Chi P, Zhao J, & Zhao G (2015). Relational self-esteem, psychological well-being, and social support in children affected by HIV. Journal of Health Psychology, 20(12), 1568–1578. doi. 2014:10.1177/1359105313517276 [DOI] [PubMed] [Google Scholar]
- Foster G, & Williamson J (2000). A review of current literature on the impact of HIV/AIDS on children in sub-Saharan Africa. AIDS 2000, 14, S275–S284. [PubMed] [Google Scholar]
- Funch-Brentano I, Dalban C, Veber F, Quartier P, Hefez S, Costagliola D, & Blanch S (2005). Evaluation of a peer support group therapy for HIV-infected adolescents. AIDS, 19(14), 1501–1508. [DOI] [PubMed] [Google Scholar]
- Gosling SD, Rentfrow PJ, & Swann WB (2003). A very brief measure of the big-five personality domains. Journal of Research in Personality, 37, 504–528. doi: 10.1016/S0092-6566(03)00046-1 [DOI] [Google Scholar]
- Guo Y, Li X, & Sherr L (2012). The impact of HIV/AIDS on children’s educational outcome: A critical review of global literature. AIDS Care, 24, 993–1012. 10.1080/09540121.2012.668170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall CS, Fottrell E, Wilkinson S, & Byass P (2014). Assessing the impact of mhealth interventions in low- and middle-income countries— what has been shown to work? Global Health Action, 7, 25606. doi: 10.3402/gha.v7.25606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BT, Redding CA, DiClemente RJ, Mustanski BS, Dodge B, Sheeran P, … Fishbein M. (2010). A network-individual-resource model for HIV prevention. AIDS and Behavior, 14(S2), 204–221. doi: 10.1007/s10461-010-9803-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman M, Cornish F, Zimmerman RS, & Johnson BT (2014). Health behavior change models for HIV prevention and AIDS care: Practical recommendations for a multi-level approach. Journal of Acquired Immune Deficiency Syndromes, 66(S3), S250–S258. doi: 10.1097/QAI.0000000000000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer RP, Gil-Rivas V, Tedeschi RG, Cann A, Calhoun LG, Buchanan T, & Taku K (2009). Use of the revised posttraumatic growth inventory for children. Journal of Traumatic Stress, 22(3), 248–253. doi: 10.1002/jts.20410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King E, Silva DM, Stein A, & Patel V (2009). Interventions for improving the psychosocial well‐being of children affected by HIV and AIDS. The Cochrane Library doi: 10.1002/14651858.CD006733.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumakech E, Cantor-Graae E, Maling S, & Bajunirwe F (2009). Peer-group support intervention improves the psychosocial well-being of AIDS orphans: Cluster randomized trial. Social Science & Medicine, 68(6), 1038–1043. 10.1016/j.socscimed.2008.10.033 [DOI] [PubMed] [Google Scholar]
- Leventhal KS, DeMaria LM, Gillham JE, Andrew G, Peabody J, & Leventhal SM (2016). A psychosocial resilience curriculum provides the “missing piece” to boost adolescent physical health: A randomized controlled trial of Girls First in India. Social Science & Medicine, 161, 37–46. 10.1016/j.socscimed.2016.05.004 [DOI] [PubMed] [Google Scholar]
- Li X, Barnett D, Fang X, Lin X, Zhao G, Zhao J, … Stanton B. (2009). Lifetime incidences of traumatic events and mental health among children affected by HIV/AIDS in rural China. Journal of Clinical Child & Adolescent Psychology, 38(5), 731–744. doi: 10.1080/15374410903103601 [DOI] [PubMed] [Google Scholar]
- Li X, Chi P, Sherr L, Cluver L, & Stanton B (2015). Psychological resilience among children affected by parental HIV/AIDS: A conceptual framework. Health Psychology and Behavioral Medicine, 3(1), 217–235. doi: 10.1080/21642850.2015.1068698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X, Zhao G, Li X, Stanton B, Zhang L, Hong Y, … Fang X. (2010). Perceived HIV stigma among children in a high HIV-prevalence area in central China: Beyond the parental HIV-related illness and death. AIDS Care, 22(5), 545–555. doi: 10.1080/09540120903253999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X, Fang X, Chi P, Heath MA, Li X, & Chen W (2016). Social ecological factors associated with future orientation of children affected by parental HIV infection and AIDS. Journal of Health Psychology, 21(7), 1404–1414. doi: 10.1177/1359105314554817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luecken LJ & Roubinov DS (2012). Pathways to lifespand health following childhood parental death. Social and Personality Psychology Compass, 6(3), 243–257. doi: 10.1111/j.1751-9004.2011.00422.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, & Becker B (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child Development, 71(3), 543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS (2006). Resilience in development: A synthesis of research across five decades. In Cicchetti D & Cohen DJ (Eds.), Developmental psychopathology: Vol. 3. Risk, disorder, and adaptation (2nd ed., pp. 739–795). New York: Wiley. [Google Scholar]
- Lv Y, Zhao Q, Li X, Stanton B, Fang X, Lin X …Zhao J. (2010). Depression symptoms among caregivers of children in HIV-affected families in rural China. AIDS Care, 22(6), 669–676. 10.1080/09540120903334633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS (2001). Ordinary magic. American Psychologist, 56(3), 227–238. [DOI] [PubMed] [Google Scholar]
- Masten AS, Best KM, & Garmezy N (1990). Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology, 2(4), 435–444. [Google Scholar]
- Masten AS (2011). Resilience in children threatened by extreme adversity: Frameworks for research, practice, and translational synergy. Development and Psychopathology, 23, 493–506. doi: 10.1017/S0954579411000198 [DOI] [PubMed] [Google Scholar]
- Masten AS, & Narayan AJ (2012). Child development in the context of disaster, war, and terrorism: Pathways of risk and resilience. Psychology doi: 10.1146/annurev-psych-120710-100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metcalf CA, Malotte CK, Douglas JM, Paul S, Dillon BA, Cross H, …Peterman TA. (2005). Efficacy of a booster counseling session 6 months after HIV testing and counseling: A randomized, controlled trial (RESPECT-2). Sexually Transmitted Diseases, 32(2), 123–129. [DOI] [PubMed] [Google Scholar]
- Miller CT, Solomon SE, Varni SE, Hodge JJ, Knapp FA, & Bunn JY (2016). A transactional approach to relationships over time between perceived HIV stigma and the psychological and physical well-being of people with HIV. Social Science & Medicine, 162, 97–105. 10.1016/j.socscimed.2016.06.025 [DOI] [PubMed] [Google Scholar]
- Mishra V & Bignami-Van Assche S (2008). Orphans and vulnerable children in high HIV-prevalence countries in sub-Saharan Africa. DHS Analytical Studies No. 15 Calverton, Maryland, USA: Macro International Inc. [Google Scholar]
- Mo PK, Lau JT, Yu X, & Gu J (2014). The role of social support on resilience, posttraumatic growth, hopelessness, and depression among children of HIV-infected parents in mainland China. AIDS Care, 26(12), 1526–1533. 10.1080/09540121.2014.923810 [DOI] [PubMed] [Google Scholar]
- Nickerson A, Bryant RA, Aderka IM, Hinton DE, & Hofmann SG (2013). The impacts of parental loss and adverse parenting on mental health: Findings from the National Comorbidity Survey-Replication. Psychological Trauma: Theory, Research, Practice, & Policy, 5(2), 119–127. 10.1037/a0025695 [DOI] [Google Scholar]
- Pelton J & Forehand R (2005). Orphans of the AIDS epidemic: An examination of clinical level problems of children. Journal of the American Academy of Child & Adolescent Psychiatry, 44(6), 585–591. [DOI] [PubMed] [Google Scholar]
- Qiao S, Li X, & Stanton B (2011). Disclosure of parental HIV infection to children: A systematic review of global literature. AIDS Behavior, 17(1), 369–389. doi: 10.1007/s10461-011-0069-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter LM, Sherr L, Adato M, Belsey M, Chandan U, Desmond C, et al. (2009). Strengthening families to support children affected by HIV and AIDS. AIDS Care, 21(s1), 3–12. 10.1080/09540120902923121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogosa D (1988). Myths about Longitudinal Research. In Schaie KW, Campbell RT, Meredith W, Rawlings SC (Eds.), Methodological issues in aging research, pp. 171–209. Springer, New York. [Google Scholar]
- Rogosa D, Brandt D & Zimowski M (1982). A growth curve approach to the measure of change. Psychological Bulletin, 92, 726–748. [Google Scholar]
- Rogosa D & Willett JB (1985). Understanding correlates of change by modeling individual differences in growth. Psychometrika, 50, 203–228. [Google Scholar]
- Rutter M (1985). Resilience in the face of adversity: Protective factors and resistance to psychiatric disorder. British Journal of Psychiatry, 147, 598–611. [DOI] [PubMed] [Google Scholar]
- Institute SAS. (2013). SAS user’s guide, version 9. 4 Cary, NC: SAS Institute, Inc. [Google Scholar]
- Sherr L, Varrall R, Mueller J, JLICA Workgroup 1 Members, Richter L., Wakhweya A., … Desmond C. (2008). A systematic review on the meaning of the concept of ‘AIDS Orphan’: Confusion over definitions and implications for care. AIDS Care, 20(5), 527–536. doi: 10.1080/09540120701867248 [DOI] [PubMed] [Google Scholar]
- Streiner DL & Norman GR (1989). Health measurement scales: A practical guide to their development and use New York: Oxford Medical Publications. [Google Scholar]
- Thompson ER (2007). Development and validation of an internationally reliable short-form of the positive and negative affect schedule (PANAS). Journal of Cross-Cultural Psychology, 38(2), 22–242. [Google Scholar]
- UNAIDS. (2010). Global Report: UNAIDS Report on the Global AIDS Epidemic: 2010 Retrieved on June 18, 2016 from http://www.refworld.org/docid/4cfca9c62.html.
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wei W, Li X, & Harrison S (2016). The relationships of HIV stigma, emotional status, and emotional regulation among HIV-affected children in rural China. AIDS Care, 28(S2), 161–167. doi: 10.1080/09540121.2016.1178974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild L (2001). The psychosocial adjustment of children orphaned byAIDS. Southern African Journal of Child and Adolescent Mental Health, 13(1):3–22. [Google Scholar]
- Whitaker DJ, Miller KS, & Clark LF (2000). Reconceptualizing adolescent sexual behavior: Beyond did they or didn’t they? Perspectives on Sexual and Reproductive Health, 32(3), 107–111. doi: 10.1363/3211100 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2013). Global update on HIV treatment 2013: Results, impact and opportunities. Geneva, Switzerland: World Health Organization. Retrieved from: http://apps.who.int/iris/bitstream/10665/85326/1/9789241505734_eng.pdf?ua=1 [Google Scholar]
- Yu X & Zhang J (2007). Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Social Behavior and Personality: An International Journal, 35(1), 19–30. [Google Scholar]
- Yu X, Lau JT, Zhang J, Mak WW, Choi KC, Lui WW, Zhang J, & Chan EY (2010). Posttraumatic growth and reduced suicidal ideation among adolescents at month 1 after the Sichuan earthquake. Journal of Affective Disorders, 123(1–3), 327–331. 10.1016/j.jad.2009.09.019 [DOI] [PubMed] [Google Scholar]
- Yu X, Lau JT, Mak WW, Zhang J, Lui WW, & Zhang J (2011). Factor structure and psychometric properties of the Conner-Davidson Resilience Scale among Chinese adolescents. Comprehensive Psychiatry, 52(2), 218–224. 10.1016/j.comppsych.2010.05.010 [DOI] [PubMed] [Google Scholar]
- Zhao G, Li X, Fang X, Zhao J, Yang H, & Stanton B (2007). Care arrangements, grief and psychological problems among children orphaned by AIDS in China. AIDS Care, 19(9), 1075–1082. 10.1080/09540120701335220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao G, Li X, Zhao J, Zhang L, & Stanton B (2012). Relative importance of various measures of HIV-related stigma in predicting psychological outcomes among children affected by HIV. Community Mental Health Journal, 48, 275–283. doi: 10.1007/x10597-011-9424-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


