Abstract
Introduction
We conducted a systematic review and meta-analysis to estimate the prevalence of overweight and obesity in children (aged 5–12 years) and adolescents (aged 12–19 years) in Asian countries. Study design: Systematic review and meta-analysis.
Material and methods
We comprehensively searched specialised databases for relevant studies conducted in Asian countries between January 1, 1999, and May 30, 2017. Random effects models (using the DerSimonian-Laird method) and generic inverse variance methods were used for quantitative data synthesis. Sensitivity analysis was conducted using the ‘leave-one-out’ method. Heterogeneity was quantitatively assessed using the I2 index. Systematic review registration: CRD42016033061.
Results
Among 22,286 identified citations, 41 studies met the inclusion criteria with n = 71,998 and n = 353,513 for children and adolescents. The pooled prevalence (overall, boys and girls) was 5.8% (n = 4175), 7.0% (n = 2631) and 4.8% (n = 1651) for obesity in children aged 5–11 years; 8.6% (n = 30,402), 10.1% (n = 17,990) and 6.2% (n = 10,874) for obesity in adolescents age 12–19 years. For overweight in children the values for overall, boys and girls were 11.2% (n = 7900), 11.7% (n = 4280) and 10.9% (n = 3698) respectively; and for overweight in adolescents, 14.6% (n = 46,886), 15.9% (27,183), and 13.7% (20,574). These findings were robust in sensitivity analyses. In children and adolescents a higher percentage of boys than girls are obese (children = 7.0 vs. 4.8%, adolescents = 10.1 vs. 6.2%, p < 0.001, respectively). Furthermore, in children and adolescents a higher percentage of boys than girls are overweight (children = 11.7 vs. 10.9%, adolescents = 15.9 vs. 13.7%, p < 0.001, respectively).
Conclusions
In view of the number of children who are overweight or obese, the associated detrimental effects on health, and the cost to health-care systems, implementation of programmes to monitor and prevent unhealthy weight gain in children and adolescents is needed throughout Asian countries.
Keywords: childhood, adolescent, overweight, obesity
Introduction
The worldwide prevalence of overweight and obesity in children and adolescents has increased in recent decades [1]. An estimated 170 million children under 18 years of age were overweight or obese in 2008, and it has been projected that approximately 30% of all children will be affected by these conditions by 2030 [2, 3]. The prevalence of a body mass index (BMI) at or higher than the 95th percentile among children between the ages of 6 and 11 years in the United States increased from 4.2% in 1963–1965 to 15.3% in 1999–2000, before plateauing during the first decade of the 21st century [4, 5]. The overall prevalence of overweight, including obesity, in school children in European countries was estimated at 20.5%: 15.6% for overweight and 4.9% for obesity. The proportion of overweight and obesity was 24.5% in Eastern Asia countries and 11.9% in the Western Asia regions [6]. The World Health Organization (WHO) has estimated that the majority of overweight or obese children live in developing countries, where the rates are increasing faster than in developed countries [7]. A comparative study across developing countries reported that prevalence rates of obesity in adolescents in Asia are highest [8]. Furthermore, there are large within and between countries variations across Asia: 3.5% in rural Bangladesh to over 65% in the Maldives [9], 30% in Iran and Saudi Arabia and approximately 12.5% for Chinese children [10].
Obesity in early life is a precursor to obesity in adulthood [2], and excess weight in adults is associated with many adverse health outcomes including type 2 diabetes, hypertension, dyslipidaemia, cardiovascular diseases and type of cancers [2]. The current increasing prevalence of childhood overweight and obesity will therefore adversely affect the burden of obesity-related diseases and their consequences on families and health systems in the near future [11]. The etiological factors for childhood obesity include genetic, metabolic, and behavioural components [12]. In spite of the demonstrated genetic influence, a strong obesogenic environment is essential for its phenotypic expression of overweight and obesity [11, 13]. However, environmental modulators of the energy intake and expenditure (the imbalance of which leads to overweight and obesity) vary across regions. Studies in the Middle East have reported that among all of the lifestyle factors, overweight and obesity exhibited significant associations with less frequent vigorous physical activity, consumption of breakfast, vegetables and frequent sugar-sweetened beverage consumption [13]. Although there are some profound differences among Asian countries including socio-economic status, diversity of the cultures, races and genetics, the main contributors to the increasing burden of obesity and overweight among children and adolescents in Asia are very similar [13]. Childhood and adolescence is a short-term, but important, window of opportunity for the prevention management and control of obesity and related health consequences. In this regard, reliable data on the burden are a solid foundation of such prevention efforts. Regarding the size and diversity of the population of Asia and its high number of developing countries, the population of children and adolescents in Asia represents a relatively large proportion of the global population of children and adolescents in developing countries.
We performed a systematic review and meta-analysis to determine the prevalence of childhood and adolescent overweight and obesity in Asian countries, with a view to providing accurate data for monitoring future trends.
Material and methods
Literature search
This systematic review is reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Statement [14]. The study protocol was registered with the International Prospective Register of Systematic Reviews, PROSPERO (registration no: CRD42016033061). We aimed to identify prevalence studies in Asian countries published from Jan 1, 1999, to May 30, 2017. A combination of words from the dictionary Medical Subject Heading Terms (MeSH) descriptors, and Boolean operators were used to search PUBMED, EMBASE, Web of Science, SCOPUS and Gray Literature sources with a range of search terms (Tables I and II). An expert librarian helped in designing the search strategy framework and implementing searches. Websites of relevant agencies such as the International Association for the Study of Obesity (IASO), the International Obesity Task Force, the Global School-based Student Health Survey and World Health Organization (WHO) were browsed. Additionally, we performed a manual search for other articles and references of published articles, and sent email requests to corresponding authors for additional data where relevant. To further minimize the effect of any publication bias, a snowball method, characterized by manual checking of references from retrieved articles, was applied. We also searched grey literature databases including the Virtual Library for Public Health and the System for Information on Grey Literature.
Table I.
Full search terms and strategy used for systematically reviewing the articles indexed in PubMed and Scopus
| No. | Concept | Search terms |
|---|---|---|
| 1 | Childhood and adolescence | Child [Text Word] OR Child [MeSH terms] Children [Text Word] OR childhood [Text Word] OR adolescent [MeSH terms] OR adolescent [Text Word] OR adolescent* [Text Word] OR pediatric [Text Word] OR teens [Text Word] OR teen [Text Word] OR Teenage* [Text Word] OR Youth* [Text Word] OR Infan*[Text Word] |
| 2 | Obesity and overweight | “Obesity” [MeSH Terms] OR “Obesity” [All Fields] OR “Obese” [MeSH Terms] OR “Obese” [All Fields] OR “Overweight” [MeSH Terms] OR “Overweight” [All Fields] OR “body-mass index “ [MeSH Terms] OR “body-mass index “ [All Fields] OR “BMI” [All Fields] OR “Weight” [MeSH Terms] OR “Weight” [All Fields] |
| 3 | Prevalence | “Epidemiology” [Subheading] OR “Prevalence” [All Fields] OR “epidemiology” [All Fields] OR “prevalence” [MeSH Terms] OR “Proportion “ [All Fields] OR “Survey” [All Fields] |
| 4 | Asian countries | “Asia” [MeSH Terms] OR (Afghanistan [Text Word]) OR Bahrain [Text Word] OR Bangladesh [Text Word] OR Bhutan [Text Word] OR Brunei [Text Word] OR Cambodia [Text Word] OR China [Text Word] OR Hong Kong [Text Word] OR India [Text Word] OR Indonesia [Text Word] OR Iran [Text Word] OR Iraq [Text Word] OR Israel [Text Word] OR Japan [Text Word] OR Jordan [Text Word] OR Kazakhstan [Text Word] OR Kuwait [Text Word] OR Kyrgyzstan [Text Word] OR Laos [Text Word] OR Lebanon [Text Word] OR Malaysia [Text Word] OR Maldives [Text Word] OR Mongolia [Text Word] OR Myanmar [Text Word] OR Nepal [Text Word] OR North Korea [Text Word] OR Oman [Text Word] OR Pakistan [Text Word] OR Philippines [Text Word] OR Qatar [Text Word] OR Saudi Arabia [Text Word] OR Singapore [Text Word] OR South Korea [Text Word] OR Sri Lanka [Text Word] OR Syria [Text Word] OR Taiwan [Text Word] OR Tajikistan [Text Word] OR Thailand [Text Word] OR Timor-Leste [Text Word] OR Turkmenistan [Text Word] OR United Arab Emirates [Text Word] OR Uzbekistan [Text Word] OR Vietnam [Text Word] OR Yemen [Text Word] |
| 5 | Combination | 1 AND 2 AND 3 AND 4 |
Table II.
Full search terms and strategy used for systematically reviewing the articles published in EMBASE, Web of Science and Open Grey
| No. | Concept | Search terms |
|---|---|---|
| 1 | Childhood and adolescence | Child or youth or childhood or adolescent |
| 2 | Obesity and overweight | Obesity or overweight |
| 3 | Prevalence | Prevalence OR epidemiology |
| 4 | Asian countries | “Asia” OR Afghanistan OR Bahrain OR Bangladesh OR Bhutan OR Brunei OR Cambodia OR China OR Hong Kong OR India OR Indonesia OR Iran OR Iraq OR Israel OR Japan OR Jordan OR Kazakhstan OR Kuwait OR Kyrgyzstan OR Laos OR Lebanon OR Malaysia OR Maldives OR Mongolia OR Myanmar OR Nepal OR North Korea OR Oman OR Pakistan OR Philippines OR Qatar OR Saudi Arabia OR Singapore OR South Korea OR Sri Lanka OR Syria OR Taiwan OR Tajikistan OR Thailand OR Timor-Leste OR Turkmenistan OR United Arab Emirates OR Uzbekistan OR Vietnam OR Yemen |
| 5 | Combination | 1 AND 2 AND 3 AND 4 |
To be included in this systematic review, primary studies had to meet these criteria: 1) population-based cross-sectional or cohort studies reporting the prevalence of overweight and obesity in children and adolescents, 2) studies conducted in Asians after 1999 and published between January 1999 and May 30, 2017, 3) age of the participants ranging between 5 and 19 years, with 5–11 years defining children and 12–19 years defining adolescents, 4) original studies containing a minimum of information necessary to calculate pooled analysis of prevalence (number of subjects, sample size), 5) articles with at least the abstract in English language, 6) obesity and overweight defined using directly measured anthropometries and not based on self-report, 7) participants residing in Asian countries, irrespective of ethnic, socioeconomic, and educational backgrounds. Studies were excluded if: 1) they were done in clinical settings and/or in participants with special medical conditions, 2) they were conducted in Asians living outside Asia, 3) they were based on self-reported weight or height, 4) were narrative reviews, commentaries, opinion pieces, methodological, editorials, letters or any other publications lacking primary data and/or explicit method descriptions, 5) they did not report the prevalence of obesity or overweight separately for children and adolescents. When authors presented the results of the same study in more than one paper, the most recent and most comprehensive paper was included.
Selecting studies for inclusion
We started with the removal of duplicates; next, two reviewers excluded some papers based on titles and abstracts only. Then eligibility was further assessed via the full text (Figure 1). Disagreements between reviewers were resolved by consensus.
Figure 1.
Overall prevalence of obesity in children
Assessment of the methodological quality of included studies
We assessed the methodological quality of included studies in terms of internal validity, external validity, response rate, and generalizability of study results. We used the ten-item rating system developed by Hoy et al. [15] and modified by Werfalli et al. [16] (Table III) to assess sampling, the sampling frame and size, outcome measures, outcome assessment, response rate, and statistical reporting [15]. Each item was assigned a score of 1 (yes) or 0 (no), and scores were summed across items to generate an overall quality score that ranged from 0 to 10. Each study was rated as having a low, moderate, or high risk of bias depending on the number of questions answered as “yes (low risk)”: studies at low risk of bias had scores higher than 8, moderate a score of 6–8, and high a score of 5 or lower [15]. Risk of selection and attrition biases were assessed according to the Cochrane guidelines, in Review Manager version 5.2. Two reviewers (MM and PR) independently assessed study quality, with disagreements being resolved by consensus.
Table III.
Quality assessment criteria for prevalence studies
| Items | Quality score |
|---|---|
| External validity | |
| 1. Was the study’s target population a close representation of the national population in relation to relevant variables? | (1 point) |
| 2. Was the sampling frame a true or close representation of the target population? | (1 point) |
| 3. Was some form of random selection used to select the sample, OR was a census undertaken? | (1 point) |
| 4. Was the likelihood of non-response bias minimal? | (1 point) |
| Total (4 points) | |
| Internal validity | |
| 1. Were data collected directly from the participants (as opposed to a proxy)? | (1 point) |
| 2. Was an acceptable case definition used in the study? | (1 point) |
| 3. Was the study instrument that measured the parameter of interest shown to have validity and reliability? | (1 point) |
| 4. Was the same mode of data collection used for all participants? (1 point) | (1 point) |
| 5. Was the length of the shortest prevalence period for the parameter of interest appropriate? | (1 point) |
| 6. Were the numerator(s) and denominator(s) for the parameter of interest appropriate? | (1 point) |
| Total (6 points) | |
Data extraction and management
Two reviewers extracted data onto a purpose-designed data extraction form and independently summarized what they considered to be the most important results from each study. These summaries were compared and disagreements resolved by discussion and consultation with a third reviewer. Any further calculations on study data considered necessary were conducted by the first reviewer and checked by the second reviewer. Study characteristics including prevalence of obesity and/or overweight, country where the study was conducted, year of publication, study population, age range, sex (boys, girls, or combined), response rate, study design, criteria for sample selection and sample size, diagnostic criteria, results and notes/comments are presented in Table IV. When a study did not present the mean age of the subjects in each age group we assumed the mid-point of the age interval. When an age group also included subjects older than 19 years (e.g. age group 17–22 years), we computed the mid-point and excluded the data if the mid-point year was higher than 19 years old. Data for age ranges that covered more than one age group were not extracted.
Table IV.
International overweight and obesity classification methods for children and adolescents
| Classification | Indicator | Risk of overweight | Overweight* | Obesity | Age range [years] |
|---|---|---|---|---|---|
| WHO 2007(23) | BMI/age | – | > 1 SD and ≤ 2 SD | > 2 SD | 5–19 |
| IOTF 2000 (97) | BMI/age | – | Age-specific† and sex-specific† BMI cut-off points for overweight and obesity that track with BMI values of 25 at 18 years of age | Age-specific† and sex-specific† BMI cut-off points for overweight and obesity that track with BMI values of 30 at 18 years of age | 2–18 |
| CDC 2000 (98) | BMI/age | – | ≥ p85 < p95 | ≥ p95 | 2–19 |
| NCHS/WHO | BMI/age | – | ≥ p85 < p95 | ≥ p95 | 10–19 |
| 1979 (99) | W/H | – | 2 SD | – | < 10 |
W/H – weight-for-height, SD – standard deviation, IOTF – International Obesity Task Force, CDC – Centers for Disease Control and Prevention, NCHS – National Center for Health Statistics, p85 – 85th percentile, p95 – 95th percentile.
In children younger than 5 years, overweight is currently defined as risk of overweight, and obesity as overweight, according to the WHO 2006 norms and for CDC 2000 reference since 2007.
For children younger than 2 years, the indicator is weight-for-length, referred to here and in the text as weight-for-height.
Diagnosis of obesity and overweight in included studies
In the case of diagnosis of obesity in school-age children and adolescents (5–19 years) the International Obesity Task Force (IOTF) [17] and the WHO 2007 methods [18] were used. Different classification methods used different cut-off points and reference populations. For school-age children and adolescents (5–19 years), the two most widely used classification methods were the IOTF [17] and the WHO 2007 methods [18], both using BMI. WHO criteria were used for overweight and obesity in adults [18].
Data synthesis and analysis
Data extraction and synthesis was based on Cochrane Handbook recommendations [19]. We used a random-effects meta-analysis model to aggregate prevalence estimates across studies while accounting for the between-study variability [20]. Heterogeneity between studies was assessed with Cochran’s χ2 test based on a 10% level of significance cut-off (due to the low power of the test) and the I2 statistic where values of 25%, 50% and 75% reflect low, medium and high heterogeneity, respectively [14]. We explored sources of heterogeneity by comparing obesity and overweight prevalence between subgroups defined by several study level characteristics. In order to evaluate the influence of each study on the overall effect size, sensitivity analysis was conducted using the leave-one-out method, i.e. removing one study each time and repeating the analysis [21–23]. Potential publication bias was explored using visual inspection of Begg’s funnel plot asymmetry, Begg’s rank correlation and Egger’s weighted regression tests. Duval and Tweedie ‘trim and fill’ and ‘fail-safe N’ methods were used to adjust the analysis for the effects of publication bias [24]. Meta-analysis was conducted using Comprehensive Meta-Analysis (CMA) V3 software (Biostat, NJ) [25].
Results
Summary of searches and study selection process
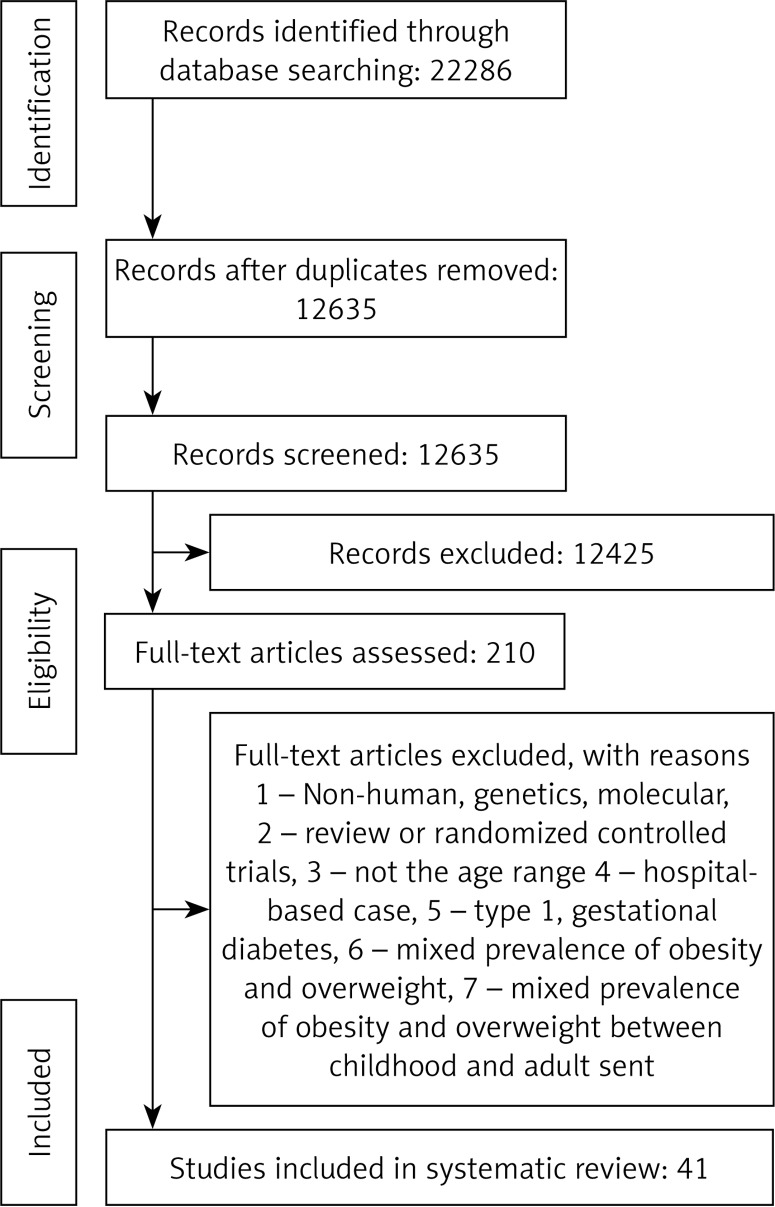
The searches identified 22,286 citations. After screening of titles and abstracts, and removal of duplicates, 12,635 studies were selected for further scrutiny, of which 210 were selected for full-text review. Of these, 47 studies (n = 71,998 and 353,513 for children and adolescents, respectively) met the inclusion criteria and were included in this systematic review (Figure 2).
Figure 2.
PRISMA Flow chart for the studies selection
Methodological quality of included studies
From all the studies, 30 of them were considered as having a “low risk of bias” while the rest of them had a “moderate risk of bias”. Six surveys did not report how subjects were selected; 26 studies mentioned random selection as a selection technique while 12 surveys reported a non-random sampling method. Nineteen studies stated the response rates, which ranged from 71.1% to 100% (median: 85.5%).
Characteristics of included studies
The characteristics of the included studies are summarized in Table V. Of the 44 countries of the Asian continent, 15 were represented in this systematic review: five studies from India [26–30], eight from Iran [31–38], seven from Saudi Arabia [13, 39–43], three from Kuwait [44–46], four from Taiwan [47–50], four from China [51–54], two from the United Arab Emirates [55, 56], four from Jordan [57–60], two from Bahrain [61, 62], two from Japan [63, 64] and one from Singapore [65], Thailand [66], Malaysia [67], Israel [68], Pakistan [69] and Turkey [70]. Two studies conducted in Israel and Thailand [66, 68] had national coverage while the remainder were subnational. Different diagnosis criteria for obesity and overweight were applied across studies including the CDC criteria in 7 studies [31, 33, 35, 37, 38, 41, 57], IOTF criteria in 11 studies [29, 42, 45, 50, 52, 58, 63–65, 71, 72], NCHC criteria in 2 studies [44, 46], WHO criteria in 16 studies [28, 32, 36, 39, 42, 49, 54, 56, 59, 62, 66–69, 73, 74], NHANES criteria in 1 study [55], Cole criteria in 6 studies [27, 30, 43, 53, 60, 75] and the Chinese index in 1 study [51], Table IV. These studies were published between 1994 and 2015. Participants in two studies were only female, while the proportion of men in other studies ranged from 34% [66] to 100% [43]. Participants’ age ranged from 2 years [54] to 25 years [67].
Table V.
National prevalence of overweight and obesity in children and adolescents from cross-sectional surveys in Asian countries
| First author surname, date of publication | Sample design | Date of fieldwork | Sample size (% male) | Age range | Classification method | Urban or rural | Prevalence of overweight | Prevalence of obesity | Combined prevalence of overweight and obesity | Response rate |
|---|---|---|---|---|---|---|---|---|---|---|
| Baker, 2010 [3] | Cluster random | May 2007. | 1355 (44.4%) | 13 to 16 years | Based on CDC | Both (urban 29.2% and rural 70.8%) | 15.7% | 8.7% | 24.4% | 98.9% |
| Aggarwal, 2008 [10] | Random | Not known | 1000 (50%) | 12 to 18 years | WHO | Urban | 15% (male) 10.2% (female) |
3.4% (male) 3.4% (female) |
18.4% 13.6% |
Not known |
| Ahmed, 2013 [12] | Random | January 2008 to June 2009 | 501 (50.8%) | 6 to 10 years | Based on WHO | Urban | 8% | 12% | 20% | 99.4% |
| Akbulut, 2013 [13] | Random | Not known | 1348 (50.4%) | 10 to 14 years | Based on Cole et al. | Urban | 57% | 15% | 72% | 79% to 90% |
| Al Alwan, 2013 [14] | Multistage cluster random | January to June 2006 | 1212 (42.2%) | 6 to 16 years | Based on WHO | Urban | 21.1% | 12.7% | 33.8% | 97.5% |
| AlHazza, 2014 [24] | A random multistage stratified cluster-sampling | 2009–2010 | 2908 (48.1%) | 14 to 19 years | Based on IOTF | Urban | 40.3% | 38.1% | 78.4% | Not known |
| AlHazza, 2007 [25] | Random | April to May 2006 | 224 (48.6%) | 4 to 6 years | Based on CDC | Urban | 20.6% | 10.8% | 31.4% | 75% |
| Huda, 2003 [26] | Not known | October 1998 to April 1999 | 898 (females) | 11–18 years | Based on NHANES | Urban | 14% | 9% | 23% | Not known |
| Al Isa, 2004 [27] | Multistage stratified random | October 1999 to April 2000 | 14659 (49.1%) | 10 to 14 years | Based on NCHS | Urban | 61.8% | 27.8% | 89.6% | Not known |
| Al Sendi, 2003 [30] | Multistage stratified random | September to November 2000 | 506 (49.2%) | 12 to 17 years | Based on WHO, Must et al. and Cole et al. | Urban | 11.9% (WHO), 32% (Must et al.), and 39.8% (Cole et al.) | 56.7% (WHO), 36.7% (Must et al.), and 32.8% (Cole et al.) | 68.6% (WHO), 68.7% (Must et al.), and 72.6% (Cole et al.) | 93.7% |
| Amin, 2008 [31] | Multistage stratified random | Not known | 1139 (100%) | 10 to 14 years | Based on Cole et al. | Urban/rural | 14.2% | 9.7% | 23.9% | 88.8% |
| Ayatollahi, 2006 [32] | Random | 2002–2003 | 2397 (52.8%) | 6.5 to 11.5 years | Based on CDC | Urban | 10.6% | 9.4% | 20% | 91.5% |
| Dayan, 2005 [37] | Not known | Not known | 76 732 (57.8%) | 17 years | Not known | Urban | 23.8% | 7.4% | 31.2% | Not known |
| Chen, 2008 [52] | Random | Not known | 883 (51%) | 12 to 16 years | Not known | Urban and rural | 38.4% | 12.3% | 50.7% | Not known |
| Chen, 2012 [53] | Random | 2007 and 2010 | 5091 2839 |
≤ 9 to ≥ 13 years | Based on WHO | Urban | 32.5% (2007)32% (2010) | 18.3% (2007)15.9% (2010) | 50.8 (2007)47.9 (2010) | 86.5%75.5% |
| Chu, 2007 [62] | Stratified, multistaged, and clustered | 2001 | 2405 (53.6%) | 6 to 13 years | Based on Nutrition and Health Survey in Taiwan (WHO) |
Urban | 15.5% (male) 14.4% (female) |
14.7% (male) 9.1% (female) |
30.2% (male) 23.5% (female) |
Not known |
| El Bayoumy, 2009 [80] | Random | January to July 2006 | 5402 (49.18%) | 10 to 14 years | Based on NCHS | Urban | 30.7% | 14.6% | 45.3% | Not known |
| Fu, 2003 [85] | Random | Not known | 623 (51.5%) | 6 to 11 years | Based on IOTF and PWH | Urban | Not known | 6.9% (IOTF) and (PWH) 16.4% | Not known | Not known |
| Hamaideh, 2010 [99] | Cluster random | Not known | 824 (51.4%) | 14 to 17 years | Based on IOTF | Urban and rural | 19.1% | 6.3% | 25.4% | 84% |
| Jagadesan, 2014 [114] | Not known | Not known | 18 955 (56.2%) | 6 to 17 years | Based on IOTF and Khadilkar’s criteria | Urban | 13.5% (IOFT) and 19.9% (Khadilkar’s criteria) | 3.4% (IOFT) and 9.4% (Khadilkar’s criteria) | Not known | 95.3% |
| Khader, 2009 [126] | Cluster random | March to May 2006 | 2131 (49.3%) | 6 to 12 years | Based on Cole et al. | Urban and rural | 19.4% | 5.6% | 25% | 94.2% |
| Xinhua, 2010 [135] | Cluster | March to June 2005 | 6288 (52.5%) | 6 to 9 years | Based on IOTF | Urban | 10.1% | 3.5% | 13.6% | 100% |
| Liou, 2010 [136] | Three-stage stratified cluster | 2006 and 2007 | 8640 (51.7%) | 13 to 16 years | Based on IOTF | Urban | 16.1% | 7.2% | 23.3% | 86.3 |
| Ma, 2011 [138] | Random | 2008 to 2009 | 8 653 (51.9%) | 2 to 7 years | Based on WHO, IOTF and CDC | Urban | 10.9% (WHO), 10.9% (IOTF) and 11.2% (CDC) | 13.8% (WHO), 6.08% (IOTF) and 11.7% (CDC) | 24.7% (WHO), 17.7% (IOTF) and 22.9% (CDC) | 89.4% |
| Maddah, 2010 [139] | Random | October 2006 to March 2007 | 2577 (female) | 12 to 17 years | Based on IOTF | Urban | 18.6% | 5.9% | 24.5% | 98.7% |
| Nakano, 2010 [150] | Not known | 2001 to 2007 | 16245 (51.8%) | 6 to 14 years | Based on IOTF | Urban | 30% –14% | 6% – 11% | 36% – 25% | 71.1% |
| Ramachandran, 2002 [159] | Not known | Not known | 4700 (50.7%) | 13 to 18 years | Not known | Urban | 33.6% | 6.5% | 40.1% | Not known |
| Sun, 2009 [168] | Not known | June to July 2010 | 5753 (49.4%) | 12 to 13 years | Based on IOTF | Urban | 16.4% | Not known | Not known | 91.6% |
| Tabesh, 2014 [169] | Random | 2012–2013 | 5811 (49.9%) | 7 to 11 years | Based on WHO | Urban | 21.4% | 5.5% | 26.8% | Not known |
| Taheri, 2013 [170] | Cluster | November to February 2012 | 1541 (44.7%) | 6 to 11 years | Based on CDC | Urban | 9.6% | 9.2% | 18.8% | 93.5% |
| Zaal, 2011 [181] | Random | Not known | 661 (49%) | 12 to 17 years | Based on WHO | Urban | 15.7% | 21.3% | 37% | Not known |
| Bose, 2007 [195] | Cross-sectional | January to March 2002 | 431 | 6 to 9 years | Not known | Not known | 17.63% | 5.10% | Not known | Not known |
| Gopalakrishnan, 2012 [199] | Cross sectional | Not known | 290 (45.2%) | 19 to 25 years | Not known | Not known | Male; 13.7% Female; 15.7% Total; 14.8% |
Male; 9.2%; Female 1.2%; Total 5.2% |
Not known | Not known |
| Ibrahim, 2007 [201] | Random | From March 2006 to September 2006 | 1695 (49.6%) | 3 to 6 years | Based on data provided at the website of Jordanian Ministry of Education for the academic year 2005/2006 | Urban and semi-urban | Male; 3.8% Female; 7.2% |
Male 20.8%; Female 19.1% |
Not known | Not known |
| Maddah, 2006 [206] | Cross-sectional | December 2004 and April 2005 |
1054 | 14 to 17 years | Based on IOTF | Urban | 21.9% | 5.3% | Not known | Not known |
| Montazerifar, 2009 [209] | Cross-sectional | 2005–2006 | 752 | 14 to 18 years | Based on IOTF, NHANES I and CDC | Urban | 8.6% (CDC) 8.8% (IOTF) 8.4% (NHANES I) |
1.5% (CDC) 1.5% (IOTF) 1.5% (NHANES I) |
Not known | Not known |
| Pwint, 2013 [213] | Cross-sectional | May 2006 to November 2008 | 3009 (52.2%) | 6 to 72 months | Based on IOTF, CDC and NHGP | Urban | 8.1% (CDC) 7.6% (IOTF) 7.5% (NHGP) |
7.1% (CDC) 3.9% (IOTF) 5.3% (NHGP) |
Not known | 72.3% |
| Ghada, 2009 | Random | 2009 | 698 (50.0%) | 4 to 6 years (male) 2 to 4 years (female) |
WHO | Both | 8.4% (male) 12.3% (female) |
7.2% (male) 8.4% (female) |
15.6% (male) 20.7% (female) |
Not known |
| Zekavat, 2014 | Random | 2009 | 1158 (50.6%) | 7 to 13 years | CDC | Urban | 9.9% (male) 10.0% (female) |
5.1% (male) 4.9% (female) |
15% (male) 14.9% (female) |
Not known |
| Cao, 2012 | Sampling | 2012 | 88974 (49.6%) | 12 to 17 years | Chinese index | Urban | 14.6% (male) 8.6% (female) |
7% (male) 2.9% (female) |
21.6% (male) 11.5% (female) |
Not known |
| Al-Almaie, 2005 | Random | 2001 | 1766 (38.2%) | 14 to 18 years | IOTF | Urban | 10.2% (male) 17.2% (female) |
19.3% (male) 11.8% (female) |
29.5% (male) 29% (female) |
Not known |
| Hajian Tilaki, 2008 | Population-based cross-sectional | 2006 | 1000 (45.0%) | 7 to 12 years | CDC | Urban | 12.5% (male) 12.2% (female) |
8.8% (male) 3.8% (female) |
21.3% (male) 16% (female) |
|
| Al-Rukban, 2003 | Cross-sectional study | 2001–2002 | 894 (100%) | 12 to 20 years | WHO | Urban | 13.8% | 20.5% | 34.3% | |
| Goyal, 2010 | Random | 11328 (50%) | 12 to 18 years | WHO | Urban and Rural | 14.3% (male) 9.2% (female) |
2.9% (male) 1.5% (female) |
17.2% (male) 10.7% (female) |
||
| Alenazi, 2015 | Cross-sectional study | 2012 | 523 (100%) | 15.5 to 17.5 years | CDC | Urban | 17.2% | 30.4% | 47.6% | |
| Allafi, 2013 | Cross-sectional study | 2009 | 906 (51.0%) | 14 to 19 years | IOTF-WHO | Urban | 25.1% (male) 25.3% (female) |
25.5% (male) 21.3% (female) |
50.6% (male) 46.6% (female) |
|
| Seubsman, 2010 | A National Cohort Study | 2005 | 29065 (34%) | 15 to 25 years | WHO | Urban | 10.4% (male) 5.9% (female) |
Prevalence by age, sex, region, and type of residence
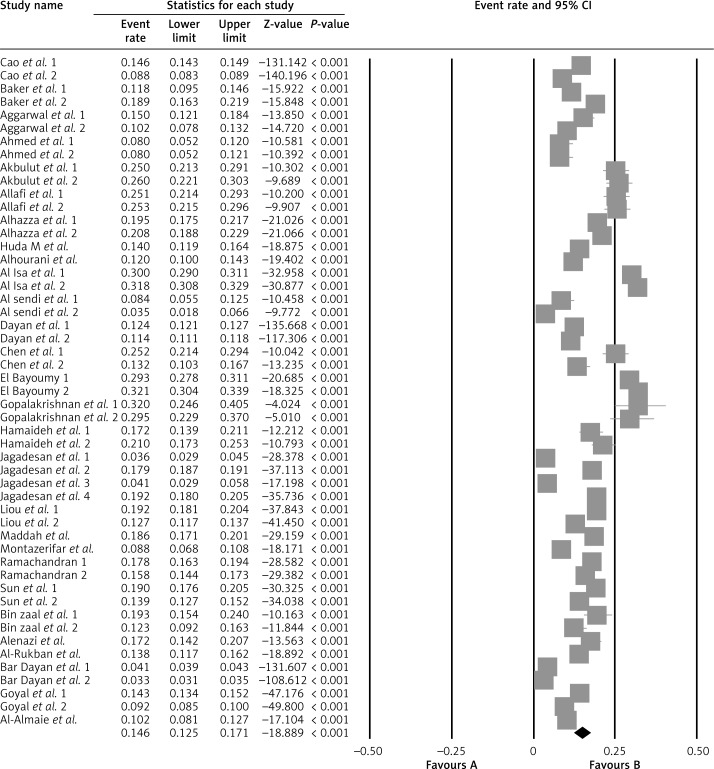
Overall prevalence of obesity
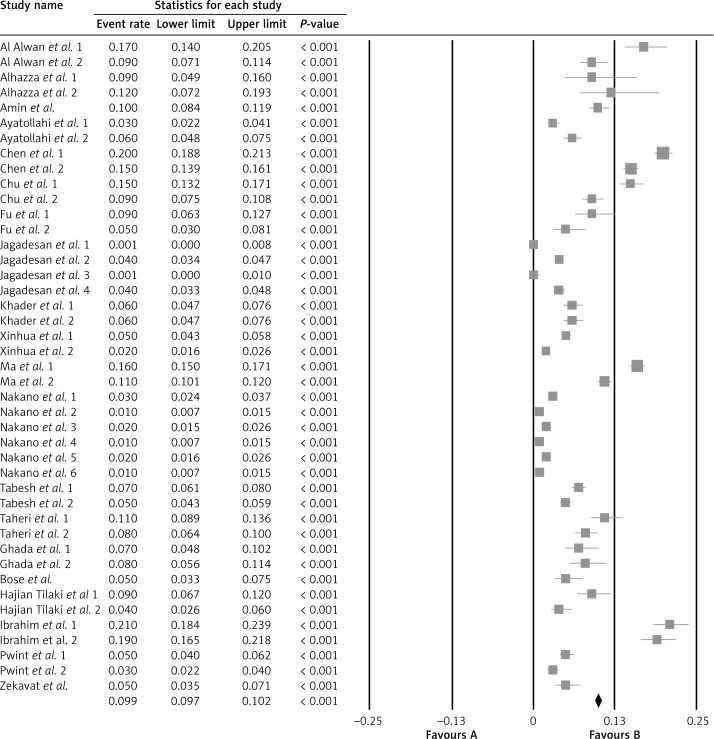
The overall prevalence of obesity was 5.8% (n = 4175) (95% CI: 4.6–7.3; 43 studies, heterogeneity p = 0.214; I2 = 6.3%) in children (Figure 1) and 8.6% (n = 30,402) (95% CI: 7.2–10.2; 47 studies, heterogeneity p = 0.318; I2 = 4.1%) in adolescents (Figure 3). The prevalence of obesity in children by diagnostic criteria was 6.7% (95% CI: 6.1–7.5; 7 studies, heterogeneity p = 0.091; I2 = 4.2%) for CDC, 3.1% (95% CI: 2.8–3.3; 14 studies, heterogeneity p = 0.122; I2 = 6.9%) for IOTF, 12.1% (95% CI: 11.0–12.9; 14 studies, heterogeneity p = 0.213; I2 1.3%) for WHO and 12.8% (95% CI: 12.3–13.4; 8 studies, heterogeneity p = 0.203; I2 = 4.6%) for Cole criteria; p < 0.001 for the difference in the prevalence of obesity across criteria in children.
Figure 3.
Overall prevalence of obesity in adolescents
The prevalence of obesity in adolescents by diagnostic criteria was 15.3% (95% CI: 13.7–17.1; 4 studies, heterogeneity p = 0.412; I2 = 6.3%) for CDC, 8.9% (95% CI: 8.4–9.3; 10 studies, heterogeneity p = 0.124; I2 = 2.1%) for IOTF, 14.1% (95% CI: 13.7–14.6; 4 studies, heterogeneity p = 0.532; I2 = 9.6%) for NCHC, 8.8% (95% CI: 8.7–8.9; 23 studies, heterogeneity p = 0.421; I2 = 8.3%) for WHO, 9.0% (95% CI: 7.3–11.1; 1 study, heterogeneity p = 0.100; I2 = 0.0%) for NHANES, 4.4% (95% CI: 3.9–5.0; 3 studies, heterogeneity p = 0.632; I2 = 1.2%) for Cole and 5.4% (95% CI: 5.2–5.6; 2 studies, heterogeneity p = 0.100; I2 = 0.0%) for the Chinese index; p < 0.001 for the difference in the prevalence of obesity across criteria in adolescents.
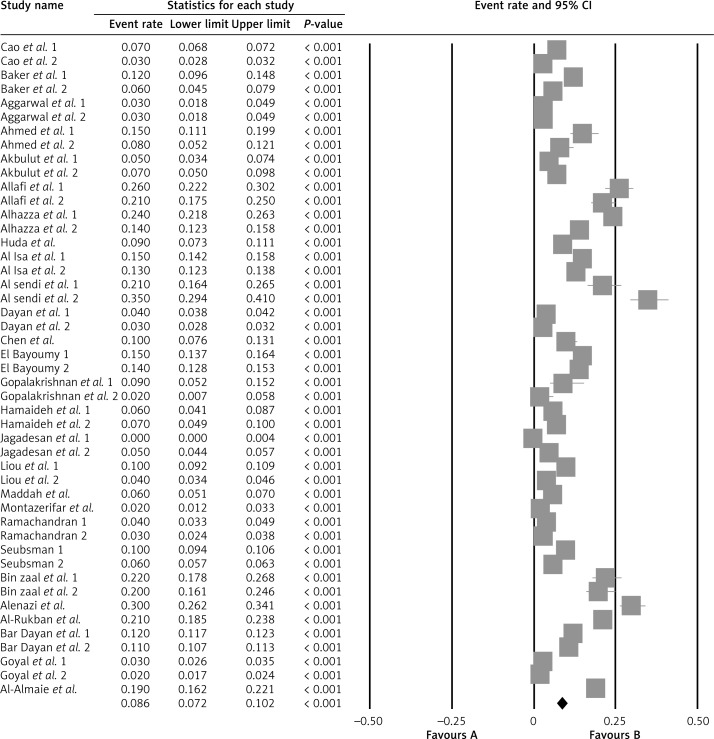
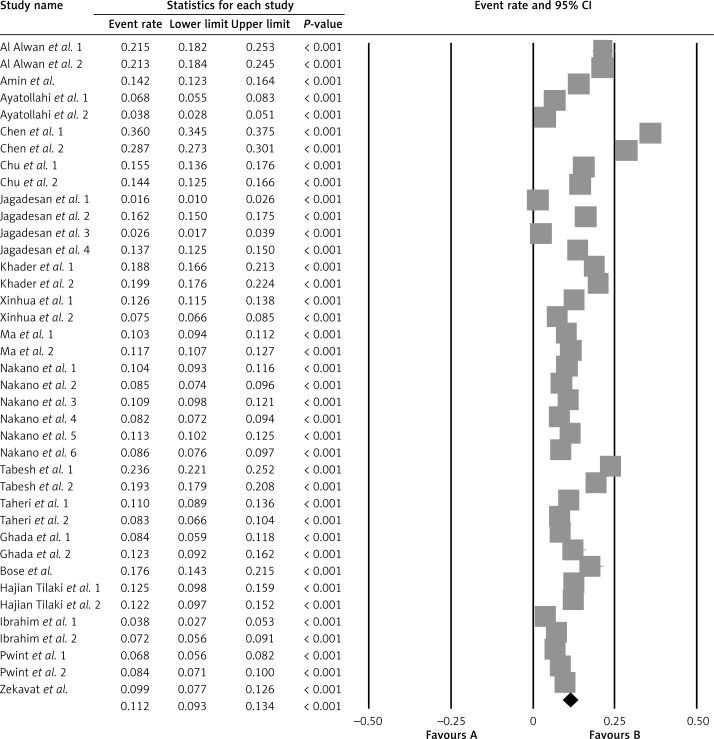
Overall prevalence of overweight
The overall prevalence of overweight was 11.2% (n = 7902) (95% CI: 9.3–13.4; 39 studies, heterogeneity p = 0.183; I2 = 6.4%) in children (Figure 4) and 14.6% (n = 46,886) (95% CI: 12.5–17.1; 51 studies, heterogeneity p = 0.128; I2 = 9.7%) in adolescents (Figure 5). The prevalence of overweight in children by diagnostic criteria was 8.8% (95% CI: 8.1–9.6; 7 studies, heterogeneity p = 0.421; I2 = 4.6%) for CDC, 10.8% (95% CI: 10.5–11.2; 12 studies, heterogeneity p = 0.692; I2 = 4.1%) for IOTF, 15.5% (95% CI: 15.0–16.0; 12 studies, heterogeneity p = 0.158; I2 = 3.1%) for WHO and 23.7% (95% CI: 23.0–24.3; 8 studies, heterogeneity p = 0.782; I2 = 9.6%) for Cole criteria; p < 0.001 for the difference in the prevalence of obesity across criteria in children.
Figure 4.
Overall prevalence of overweight in children
Figure 5.
Overall prevalence of overweight in adolescents
The prevalence of overweight in adolescents by diagnostic criteria was 14.6% (95% CI: 13.3–16.0; 4 studies, heterogeneity p = 0.084; I2 = 6.5%) for CDC, 17.0% (95% CI: 16.5–17.4; 14 studies, heterogeneity p = 0.142; I2 = 4.2%) for IOTF, 30.9% (95% CI: 30.2–31.5; 4 studies, heterogeneity p = 0.823; I2 = 4.2%) for NCHC, 9.8% (95% CI: 9.7–10.0; 22 studies, heterogeneity p = 0.961; I2 = 2.8%) for WHO and 17.4% (95% CI: 16.4–18.4; 4 studies, heterogeneity p = 0.635; I2 = 1.4%) for Cole criteria; p < 0.001 for the difference in the prevalence of obesity across criteria in adolescents.
Prevalence of obesity and overweight by sex
The overall prevalence of obesity in children by gender was 7.0% (n = 2631) (95% CI: 5.0–9.6; 21 studies, heterogeneity p = 0.262; I2 = 6.9%) in boys and 4.8% (n = 1561) (95% CI: 3.4–6.8; 21 studies, heterogeneity p = 0.102; I2 = 2.1%) in girls; p < 0.001 for the difference by gender. The overall prevalence of obesity in adolescents by gender was 10.1% (n = 17,989) (95% CI: 8.0–12.6; 24 studies, heterogeneity p = 0.832; I2 = 1.4%) in boys and 6.2% (n = 10,872) (95% CI: 4.6–8.2; 25 studies, heterogeneity p = 0.209; I2 = 9.2%) in girls; p < 0.001 for the difference by gender.
The overall prevalence of overweight in children by gender was 11.7% (n = 4296) (95% CI: 8.8–15.3; 19 studies, heterogeneity p = 0.965; I2 = 7.1%) in boys and 10.9% (n = 3694) (95% CI: 8.4–14.1; 19 studies, heterogeneity p = 0.101; I2 = 3.4%) in girls; p < 0.001 for the difference by gender. The overall prevalence of overweight in adolescents by gender was 15.9% (n = 27,183) (95% CI: 12.8–19.7; 24 studies, heterogeneity p = 0.321; I2 = 8.9%) in boys and 13.7% (n = 20,574) (95% CI: 10.6–17.6; 26 studies, heterogeneity p = 0.215; I2 = 3.3%) in girls; p < 0.001 for the difference by gender.
Prevalence of obesity and overweight by region
Childhood obesity prevalence in urban boys and girls was 6.6% (95% CI: 4.3–9.9; heterogeneity p = 0.425; I2 = 6.2%) and 4.6% (95% CI: 3.1–6.7; heterogeneity p = 0.329; I2 = 8.3%), and for overweight it was 12.6% (95% CI: 8.9–17.6; heterogeneity p = 0.211; I2 = 2.1%) and 10.8% (95% CI: 7.8–14.8; heterogeneity p = 0.159; I2 = 1.4%) respectively.
The prevalence of obesity in urban adolescent boys and girls was 10.3% (95% CI: 7.7–13.7; heterogeneity p = 0.825; I2 = 2.1%) and 6.6% (95% CI: 4.8–9.0; heterogeneity p = 0.742; I2 = 6.3%) and for overweight it was 17.1% (95% CI: 14.3–20.1; heterogeneity p = 0.269; I2 = 1.3%) and 14.8% (95% CI: 11.7–18.6; heterogeneity p = 0.867; I2 = 8.6%) respectively.
Sensitivity analysis
In leave-one-out sensitivity analyses, the pooled effect estimates remained similar across all studies and within specific subgroups (Table VI). This stability confirmed that the significant difference between the studied groups is the overall effect from all included studies.
Table VI.
Sensitivity analysis across all studies
| Variables | Result of the leave-one-out sensitivity analyses |
|---|---|
| Total obesity in children | 5.8% (95% CI: 4.6–7.3) |
| Total obesity in adolescents | 8.6% (95% CI: 7.2–10.2) |
| Obesity in children: | |
| CDC | 6.7% (95% CI: 6.1–7.5) |
| WHO | 3.1% (95% CI: 2.8–3.3) |
| Cole | 12.8% (95% CI: 12.3–13.4) |
| Obesity in adolescents: | |
| CDC | 15.3% (95% CI: 13.7–17.1) |
| IOTF | 8.9% (95% CI: 8.4–9.3) |
| NCHC | 14.1% (95% CI: 13.7–14.6) |
| WHO | 8.8% (95% CI: 8.7–8.9) |
| NHANES | 9.0% (95% CI: 7.3–11.1) |
| Cole | 4.4% (95% CI: 3.9–5.0) |
| Chinese index | 5.4% (95% CI: 5.2–5.6) |
| Total overweight in children | 11.2% (95% CI: 9.3–13.4) |
| Total overweight in adolescents | 14.6% (95% CI: 12.5–17.1) |
| Overweight in children: | |
| CDC | 10.8% (95% CI: 10.5–11.2) |
| WHO | 15.5% (95% CI: 15.0–16.0) |
| Cole | 23.7% (95% CI: 23.0–24.3) |
| Overweight in adolescents: | |
| CDC | 14.6% (95% CI: 13.3–16.0) |
| IOTF | 17.0% (95% CI: 16.5–17.4) |
| NCHC | 30.9% (95% CI: 30.2–31.5) |
| WHO | 9.8% (95% CI: 9.7–10.0) |
| Cole | 17.4% (95% CI: 16.4–18.4) |
Publication bias
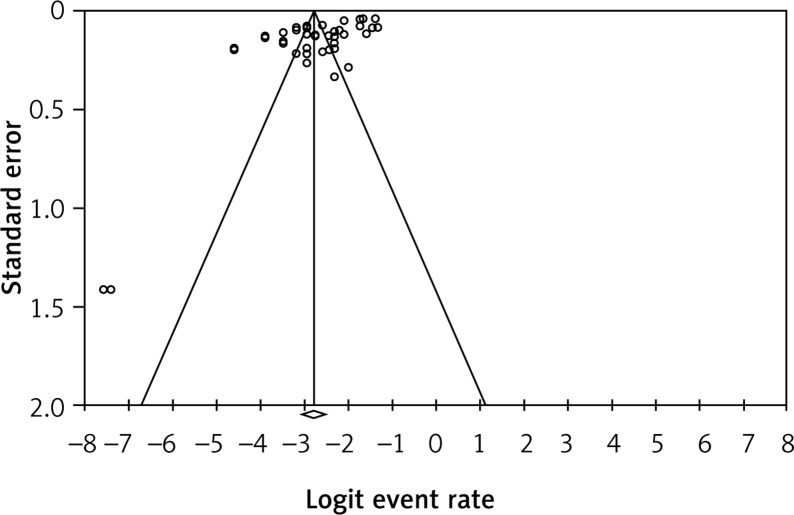
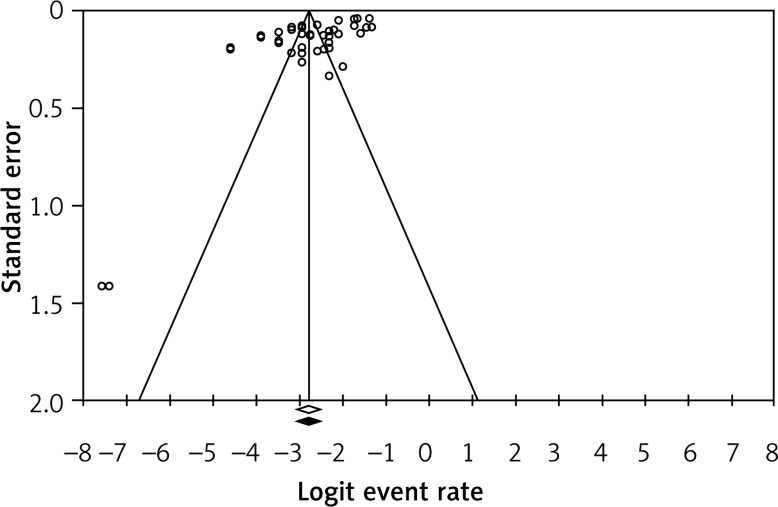
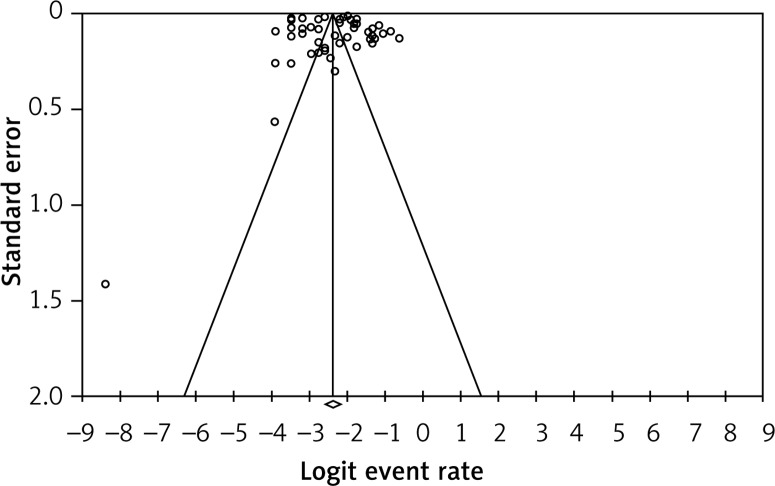
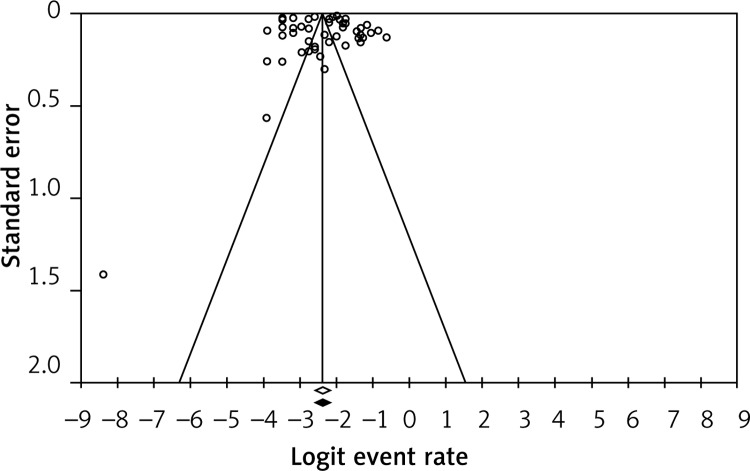
Visual inspection of funnel plot symmetry suggested no potential publication bias for the overall prevalence of obesity in children and adolescents (Figures 6 and 7). The presence of publication bias was also not suggested by Begg’s rank correlation test (Kendall’s τ with continuity correction = –0.17, z = 1.61, p = 0.107 in children and –0.13, z = 1.30, p = 0.192 in adolescents). After adjustment of effect sizes for potential publication bias using the ‘trim and fill’ correction, no potentially missing studies were imputed in the funnel plot (Figures 8 and 9). The ‘fail-safe N’ test showed that 7525 studies (in children) and 8070 studies (in adolescents) would be needed to bring the result to a non-significant (p > 0.05) value.
Figure 6.
Funnel plots for publication bias for the overall prevalence of obesity in children. Open circles represent observed published studies; open diamond represents observed effect size
Figure 7.
Funnel plots for publication bias for the overall prevalence of obesity in adolescents. Open circles represent observed published studies; open diamond represents observed effect size
Figure 8.
Trim and fill method to impute potentially missing studies (prevalence of obesity in children). No potentially missing study was imputed in the funnel plot. Open circles represent observed published studies; open diamond represents observed effect size; closed diamond represents imputed effect size
Figure 9.
Trim and fill method to impute potentially missing studies (prevalence of obesity in adolescents). No potentially missing study was imputed in the funnel plot. Open circles represent observed published studies; open diamond represents observed effect size; closed diamond represents imputed effect size
Discussion
This study has systematically evaluated the scientific literature to provide robust estimates for obesity and overweight prevalence by age group, sex and setting in children and adolescents in Asian countries. The overall prevalence of obesity was 5.8% in Asian children and 8.6% in adolescents. Equivalents for overweight were 11.2% in children and 14.6% in adolescents. The overall prevalence by gender was 7.0% and 4.8% in boys and girls for obesity in children, and 11.7% and 10.9% in boys and girls respectively for overweight in children. Furthermore, according to our findings, childhood obesity prevalence in urban boys and girls was 6.6% and 4.6% and for overweight it was 12.6 and 10.8% respectively, and the prevalence of obesity in urban adolescent boys and girls was 10.3% and 6.6%, while for overweight it was 17.1% and 14.8% respectively.
In line with our findings, some systematic reviews have reported on growing prevalence of obesity and overweight among children and adolescents. The Global Burden of Disease Study estimated that the prevalence of obesity/overweight in children and adolescents in developing countries was 12.9% for boys and 13.4% for girls in 2013 [76]. A meta-analysis concluded that the prevalence of obesity in children and adolescents aged 2 to 19 years in the United States in 2011–2014 was 17.0%, while the prevalence of extreme obesity was 5.8% [77]. The combined prevalence of overweight and obesity in European children below the age of 10 ranged from > 40% in southern Europe to < 10% in northern Europe [78]. These findings confirm the high prevalence of overweight and obesity in children and adolescents worldwide. In another study in which worldwide trends in mean BMI in children and adolescents were estimated, they reported that the rising trends in children’s and adolescents’ BMI have plateaued in many high-income countries, albeit at high levels, but have accelerated in parts of Asia [79].
Different definitions have been used for childhood and adolescent obesity; thus, it is difficult to make meaningful comparisons across countries and studies. According to the cut-off point references when used to compare the obesity status in this meta-analysis, we found that compared with the CDC criteria, the IOTF, WHO and Cole definitions tend to underestimate the prevalence of obesity and overestimate the prevalence of overweight among Asian children and adolescents.
The WHO reported that childhood overweight and obesity could be the results of the changing life style including consuming high energy-dense diets that are high in fat content and carbohydrate but low in vitamins and minerals, and doing less physical activity because of the sedentary lifestyles [80]. Asian investigations have reported epidemiologic transition along with a notable nutrition transition in the Asian child and adolescent population, and suggested that urbanization in most parts of Asia is associated with increased sedentary behaviour and lack of physical activity [28, 81], due to a lack of play areas, both in the community and in schools, as well as increasing time spent watching television and playing computer games [82, 83]. Additionally, due to more recent widespread availability of fast food shops in Asian countries, increasing consumption of junk foods has also contributed to dietary changes [83]. Furthermore, it has been reported that socioeconomic status (SES) influences the prevalence of childhood overweight and obesity [84]. National studies have confirmed a diet with higher energy-dense, animal-based foods in childhood with a high SES, and desire in city children to have a lower intake of fruit and vegetables [85]. It has been reported that urban families spend more time watching television, have less sleep and digital playing. Moreover, compared to rural area, subjects in urban areas have easier access to cars, which could be a contributing factor [86].
In our study the prevalence of obesity and overweight differed by sex. We found that girls had a lower prevalence of obesity than boys, and this ratio in adolescents was higher in boys compared to girls. It could be due to differences in body fat composition or physical activity, or the fact that girls care more about their appearance and pay higher attention to their body image than boys [87]. Boys and girls differ in several factors such as body composition, hormone biology and susceptibility to certain social, patterns of weight gain, ethnic, genetic, and environmental factors, which can explain gender differences [88].
The alarmingly high rate of overweight/obesity in Asian children and adolescents warrants immediate intervention: raising awareness among children, adolescents and their families about the health consequences of obesity and its related diseases including diabetes and cardiovascular diseases, teaching community members to encourage lifestyle changes including in diet and physical activity, national and international monitoring programmes in order to decrease the rate of overweight and obesity in the community in order to avoid an obesity epidemic in the future generation.
The comparisons of overweight and obesity prevalence need to be interpreted with caution due to the differences in survey sampling methods, sample sizes, age range of subjects, quality of data in terms of height and weight measurement. Moreover, like most meta-analyses, we pooled together studies conducted under different circumstances in different parts of Asian countries among different population groups. In addition, a specific limitation of our meta-analysis is related to the difficulty of combining studies that used four different diagnostic criteria to assess overweight/obesity. This is directly related to the lack of consensus about the diagnostic criteria for overweight/obesity. In order to evaluate the sources of bias in the review, we performed subgroup analyses. Important strengths of the present study include the use of meta-analytic techniques to derive the pooled estimates, and the application of sensitivity analyses to confirm the robustness of our findings.
In conclusion, from our findings it was revealed that in regard of the number of children who are overweight or obese, relevant health authorities should review the obesity preventive strategies and, using public health interventions, reduce the rate of obesity throughout Asian countries.
Acknowledgments
The study protocol was registered with the International Prospective Register of Systematic Reviews, PROSPERO (registration no: CRD42016033061).
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Rivera JA, de Cossio TG, Pedraza LS, Aburto TC, Sanchez TG, Martorell R. Childhood and adolescent overweight and obesity in Latin America: a systematic review. Lancet Diabetes Endocrinol. 2014;2:321–32. doi: 10.1016/S2213-8587(13)70173-6. [DOI] [PubMed] [Google Scholar]
- 2.Mistry SK, Puthussery S. Risk factors of overweight and obesity in childhood and adolescence in South Asian countries: a systematic review of the evidence. Public Health. 2015;129:200–9. doi: 10.1016/j.puhe.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–14. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham SA, Kramer MR, Narayan KMV. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370:403–11. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lakshman R, Elks CE, Ong KK. Childhood obesity. Circulation. 2012;126:1770–9. doi: 10.1161/CIRCULATIONAHA.111.047738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olaya B, Moneta MV, Pez O, et al. Country-level and individual correlates of overweight and obesity among primary school children: a cross-sectional study in seven European countries. BMC Public Health. 2015;15:1–12. doi: 10.1186/s12889-015-1809-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO . Commission on Ending Childhood Obesity: Facts and figures on childhood obesity. 2014. [Google Scholar]
- 8.Caleyachetty R, Echouffo-Tcheugui JB, Tait CA, Schilsky S, Forrester T, Kengne AP. Prevalence of behavioural risk factors for cardiovascular disease in adolescents in low-income and middle-income countries: an individual participant data meta-analysis. Lancet Diabetes Endocrinol. 2015;3:535–44. doi: 10.1016/S2213-8587(15)00076-5. [DOI] [PubMed] [Google Scholar]
- 9.Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Hills AP. Prevalence, trends and associated socio-economic factors of obesity in South Asia. Obesity Facts. 2013;6:405–14. doi: 10.1159/000355598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lobstein T, Jackson-Leach R, Moodie ML, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385:2510–20. doi: 10.1016/S0140-6736(14)61746-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Afshin A, Forouzanfar MH, Reitsma MB, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramachandran A, Snehalatha C. Rising burden of obesity in Asia. J Obesity. 2010;2010 doi: 10.1155/2010/868573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Hazzaa HM, Abahussain NA, Al-Sobayel HI, Qahwaji DM, Alsulaiman NA, Musaiger AO. Prevalence of overweight, obesity, and abdominal obesity among urban Saudi adolescents: gender and regional variations. J Health Popul Nutr. 2014;32:634–45. [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Wiley Online Library; 2008. [Google Scholar]
- 15.Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–9. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Werfalli M, Musekiwa A, Engel ME, Ross I, Kengne AP, Levitt NS. The prevalence of type 2 diabetes mellitus among older people in Africa: a systematic review study protocol. BMJ Open. 2014;4:e004747. doi: 10.1136/bmjopen-2013-004747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cole T, Bellizzi M, Flegal K, Dietz W. Establishing a standard definition of child overweight and obesity worldwide: international survey. BMJ. 2000;320:1420–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins J, Green S. Cochrane Handbook for Systematic Reviews, version 5.0. The Cochrane Collaboration; 2009. [Google Scholar]
- 20.Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Son F. Methods for meta-analysis in medical research. West Sussex: John Wiley & Sons; 2000. [Google Scholar]
- 21.Ferretti G, Bacchetti T, Sahebkar A. Effect of statin therapy on paraoxonase-1 status: a systematic review and meta-analysis of 25 clinical trials. Progress Lipid Research. 2015;60:50–73. doi: 10.1016/j.plipres.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Sahebkar A. Are curcuminoids effective C-reactive protein-lowering agents in clinical practice? Evidence from a meta-analysis. Phytother Res. 2014;28:633–42. doi: 10.1002/ptr.5045. [DOI] [PubMed] [Google Scholar]
- 23.Sahebkar A, Serban MC, Mikhailidis DP, et al. Head-to-head comparison of statins versus fibrates in reducing plasma fibrinogen concentrations: a systematic review and meta-analysis. Pharmacol Res. 2016;103:236–52. doi: 10.1016/j.phrs.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 24.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 25.Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive Metaanalysis (Vers. 2) Englewood Cliffs, NJ: Biostat. Inc; 2005. [Google Scholar]
- 26.Agarwal RK. Childhood obesity: emerging challenge. Indian Pediatr. 2008;45:443–4. [PubMed] [Google Scholar]
- 27.Bose K, Bisai S, Mukhopadhyay A, Bhadra M. Overweight and obesity among affluent Bengalee schoolgirls of Lake Town, Kolkata, India. Matern Child Nutr. 2007;3:141–5. doi: 10.1111/j.1740-8709.2007.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goyal RK, Shah VN, Saboo BD, et al. Prevalence of overweight and obesity in Indian adolescent school going children: its relationship with socioeconomic status and associated lifestyle factors. J Assoc Phys India. 2010;58:151–8. [PubMed] [Google Scholar]
- 29.Jagadesan S, Harish R, Miranda P, Unnikrishnan R, Anjana RM, Mohan V. Prevalence of overweight and obesity among school children and adolescents in Chennai. Indian Pediatr. 2014;51:544–9. doi: 10.1007/s13312-014-0444-6. [DOI] [PubMed] [Google Scholar]
- 30.Ramachandran A, Snehalatha C, Vinitha R, et al. Prevalence of overweight in urban Indian adolescent school children. Diabetes Res Clin Pract. 2002;57:185–90. doi: 10.1016/s0168-8227(02)00056-6. [DOI] [PubMed] [Google Scholar]
- 31.Ayatollahi SMT, Mostajabi F. National prevalence of obesity – prevalence of obesity among schoolchildren in Iran. Obes Rev. 2007;8:289–91. doi: 10.1111/j.1467-789X.2006.00299.x. [DOI] [PubMed] [Google Scholar]
- 32.Behzadnia S, Vahidshahi K, Hosseini SH, Anvari S, Ehteshami S. Obesity and related factors in 7-12 year-old elementary school students during 2009-2010 in Sari, Iran. Medicinski Glasnik. 2012;9:86–90. [PubMed] [Google Scholar]
- 33.Hajian-Tilaki KO, Heidari B. Prevalence of obesity, central obesity and the associated factors in urban population aged 20-70 years, in the north of Iran: a population-based study and regression approach. Obes Rev. 2007;8:3–10. doi: 10.1111/j.1467-789X.2006.00235.x. [DOI] [PubMed] [Google Scholar]
- 34.Maddah M. Overweight among rural girls in Iran: a terrifying prospects of cardiometabolic disorders. Int J Cardiol. 2009;132:442–4. doi: 10.1016/j.ijcard.2007.08.083. [DOI] [PubMed] [Google Scholar]
- 35.Montazerifar F, Karajibani M, Rakhshani F, Hashemi M. Prevalence of underweight, overweight and obesity among high-school girls in Sistan va Baluchistan. East Mediterr Health J. 2009;15:1293–300. [PubMed] [Google Scholar]
- 36.Tabesh H, Hosseiny SM, Kompani F, et al. Prevalence and trend of overweight and obesity among schoolchildren in Ahvaz, Southwest of Iran. Global J Health Sci. 2014;6:35–41. doi: 10.5539/gjhs.v6n2p35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taheri F, Kazemi T, Chahkandi T, Namakin K, Zardast M, Bijari B. Prevalence of overweight, obesity and central obesity among elementary school children in Birjand, east of Iran, 2012. J Res Health Sci. 2013;13:157–61. [PubMed] [Google Scholar]
- 38.Zekavat OR, Makarem AR, Shayan Z, Shojaee M, Karami MY. Obesity and overweight among primary school children in Iran. Minerva Pediatr. 2014;66:579–84. [PubMed] [Google Scholar]
- 39.Al Alwan I, Al Fattani A, Longford N. The effect of parental socioeconomic class on children’s body mass indices. J Clin Res Pediatr Endocrinol. 2013;5:110–5. doi: 10.4274/Jcrpe.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Al-Almaie S. Knowledge of healthy diets among adolescents in eastern Saudi Arabia. Ann Saudi Med. 2005;25:294–8. doi: 10.5144/0256-4947.2005.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alenazi SA, Koura HM, Zaki SM, Mohamed AH. Prevalence of obesity among male adolescents in Arar Saudi Arabia: future risk of cardiovascular disease. Indian J Com Med. 2015;40:182–7. doi: 10.4103/0970-0218.158864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Al-Rukban MO. Obesity among Saudi male adolescents in Riyadh, Saudi Arabia. Saudi Med J. 2003;24:27–33. [PubMed] [Google Scholar]
- 43.Amin TT, Al-Sultan AI, Ali A. Overweight and obesity and their relation to dietary habits and socio-demographic characteristics among male primary school children in Al-Hassa, Kingdom of Saudi Arabia. Eur J Nutr. 2008;47:310–8. doi: 10.1007/s00394-008-0727-6. [DOI] [PubMed] [Google Scholar]
- 44.Al-Isa AN. Body mass index, overweight and obesity among Kuwaiti intermediate school adolescents aged 10-14 years. Eur J Clin Nutr. 2004;58:1273–7. doi: 10.1038/sj.ejcn.1601961. [DOI] [PubMed] [Google Scholar]
- 45.Allafi A, Al-Haifi AR, Al-Fayez MA, et al. Physical activity, sedentary behaviours and dietary habits among Kuwaiti adolescents: gender differences. Public Health Nutr. 2014;17:2045–52. doi: 10.1017/S1368980013002218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.El-Bayoumy I, Shady I, Lotfy H. Prevalence of obesity among adolescents (10 to 14 years) in Kuwait. Asia Pac J Publ Health. 2009;21:153–9. doi: 10.1177/1010539509331786. [DOI] [PubMed] [Google Scholar]
- 47.Chen CM. Overview of obesity in Mainland China. Obes Rev. 2008;9(Suppl 1):14–21. doi: 10.1111/j.1467-789X.2007.00433.x. [DOI] [PubMed] [Google Scholar]
- 48.Chen F, Wang Y, Shan X, et al. Association between childhood obesity and metabolic syndrome: evidence from a large sample of chinese children and adolescents. PloS One. 2012;7:e47380. doi: 10.1371/journal.pone.0047380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chu NF, Pan WH. Prevalence of obesity and its comorbidities among schoolchildren in Taiwan. Asia Pac J Clin Nutr. 2007;16:601–7. [PubMed] [Google Scholar]
- 50.Liou YM, Liou TH, Chang LC. Obesity among adolescents: sedentary leisure time and sleeping as determinants. J Adv Nurs. 2010;66:1246–56. doi: 10.1111/j.1365-2648.2010.05293.x. [DOI] [PubMed] [Google Scholar]
- 51.Cao ZQ, Zhu L, Zhang T, Wu L, Wang Y. Blood pressure and obesity among adolescents: a school-based population study in China. Am J Hyper. 2012;25:576–82. doi: 10.1038/ajh.2012.5. [DOI] [PubMed] [Google Scholar]
- 52.Fu WPC, Lee HC, Ng CJ, et al. Screening for childhood obesity: international vs population-specific definitions. Which is more appropriate? Int J Obes. 2003;27:1121–6. doi: 10.1038/sj.ijo.0802385. [DOI] [PubMed] [Google Scholar]
- 53.Li X, Liao B, Liu J, et al. Prevalence and risk factors for childhood obesity in Changsha and Shenzhen in China. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2010;35:11–6. doi: 10.3969/j.issn.1672-7347.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 54.Ma YN, Chen T, Wang D, Liu MM, He QC, Dong GH. Prevalence of overweight and obesity among preschool children from six cities of northeast China. Arch Med Res. 2011;42:633–40. doi: 10.1016/j.arcmed.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 55.Al-Hourani HM, Henry CJK, Lightowler HJ. Prevalence of overweight among adolescent females in the United Arab Emirates. Am J Hum Biol. 2003;15:758–64. doi: 10.1002/ajhb.10212. [DOI] [PubMed] [Google Scholar]
- 56.bin Zaal AA, Musaiger AO, D’Souza R. Dietary habits associated with obesity among adolescents in Dubai, United Arab Emirates. Nutr Hospital. 2009;24:437–44. [PubMed] [Google Scholar]
- 57.Abu Baker NN, Daradkeh SM. Prevalence of overweight and obesity among adolescents in Irbid governorate, Jordan. East Mediterr Health J. 2010;16:657–62. [PubMed] [Google Scholar]
- 58.Hamaideh SH, Al-Khateeb RY, Al-Rawashdeh AB. Overweight and obesity and their correlates among Jordanian adolescents. J Nurs Scholarship. 2010;42:387–94. doi: 10.1111/j.1547-5069.2010.01367.x. [DOI] [PubMed] [Google Scholar]
- 59.Ibrahim AI, Hawamdeh ZM, Al-Smadi JT, Ammari BA. Prevalence of overweight and obesity in urban and semi-urban Jordanian children aged 3-6 years. Child Care Health Develop. 2008;34:464–9. doi: 10.1111/j.1365-2214.2008.00821.x. [DOI] [PubMed] [Google Scholar]
- 60.Khader Y, Irshaidat O, Khasawneh M, Amarin Z, Alomari M, Batieha A. Overweight and obesity among school children in Jordan: prevalence and associated factors. Matern Child Health J. 2009;13:424–31. doi: 10.1007/s10995-008-0362-0. [DOI] [PubMed] [Google Scholar]
- 61.Al-Raees GY, Al-Amer MA, Musaiger AO, D’Souza R. Prevalence of overweight and obesity among children aged 2-5 years in BahraIn: a comparison between two reference standards. Int J Pediatr Obes. 2009;4:414–6. doi: 10.3109/17477160902763325. [DOI] [PubMed] [Google Scholar]
- 62.Al-Sendi AM, Shetty P, Musaiger AO. Prevalence of overweight and obesity among Bahraini adolescents: a comparison between three different sets of criteria. Eur J Clin Nutr. 2003;57:471–4. doi: 10.1038/sj.ejcn.1601560. [DOI] [PubMed] [Google Scholar]
- 63.Nakano T, Sei M, Ewis AA, Munakata H, Onishi C, Nakahori Y. Tracking overweight and obesity in Japanese children; a six years longitudinal study. J Med Investig. 2010;57:114–23. doi: 10.2152/jmi.57.114. [DOI] [PubMed] [Google Scholar]
- 64.Sun Y, Sekine M, Kagamimori S. Lifestyle and overweight among Japanese adolescents: the Toyama Birth Cohort Study. J Epidemiol. 2009;19:303–10. doi: 10.2188/jea.JE20080095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pwint MK, Lee YS, Wong TY, Saw SM. Prevalence of overweight and obesity in Chinese preschoolers in Singapore. Ann Acad Med Singapore. 2013;42:66–72. [PubMed] [Google Scholar]
- 66.Seubsman SA, Lim LLY, Banwell C, et al. Socioeconomic status, sex, and obesity in a large national cohort of 15-87-year-old open university students in Thailand. J Epidemiol. 2010;20:13–20. doi: 10.2188/jea.JE20090014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gopalakrishnan S, Ganeshkumar P, Prakash MVS, Christopher, Amalraj V. Prevalence of overweight/obesity among the medical students, Malaysia. Med J Malaysia. 2012;67:442–4. [PubMed] [Google Scholar]
- 68.Bar Dayan Y, Elishkevits K, Grotto I, et al. The prevalence of obesity and associated morbidity among 17-year-old Israeli conscripts. Public Health. 2005;119:385–9. doi: 10.1016/j.puhe.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 69.Ahmed J, Laghari A, Naseer M, Mehraj V. Prevalence of and factors associated with obesity among Pakistani schoolchildren: a school-based, cross-sectional study. East Mediterr Health J. 2013;19:242–7. [PubMed] [Google Scholar]
- 70.Akbulut G, Yildirim M, Sanlier N, et al. Comparison of energy balance-related behaviours and measures of body composition between Turkish adolescents in Turkey and Turkish immigrant adolescents in the Netherlands. Public Health Nutr. 2014;17:2692–9. doi: 10.1017/S1368980013003388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Al-Almaie SM. Prevalence of obesity and overweight among Saudi adolescents in Eastern-Saudi Arabia. Saudi Med J. 2005;26:607–11. [PubMed] [Google Scholar]
- 72.Maddah M, Nikooyeh B. Obesity among Iranian adolescent girls: location of residence and parental obesity. J Health Popul Nutr. 2010;28:61–6. doi: 10.3329/jhpn.v28i1.4524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Aggarwal T, Bhatia RC, Singh D, Sobti PC. Prevalence of obesity and overweight in affluent adolescents from Ludhiana, Punjab. Indian Pediatr. 2008;45:500–2. [PubMed] [Google Scholar]
- 74.Al-Raees GY, Al-Amer MA, Musaiger AO, D’Souza R. Prevalence of overweight and obesity among children aged 2-5 years in BahraIn: a comparison between two reference standards. Int J Pediatr Obes. 2009;4:414–6. doi: 10.3109/17477160902763325. [DOI] [PubMed] [Google Scholar]
- 75.Li AM, Au CT, Ng C, Lam HS, Ho CKW, Wing YK. A 4-year prospective follow-up study of childhood OSA and its association with BP. Chest. 2014;145:1255–63. doi: 10.1378/chest.13-1333. [DOI] [PubMed] [Google Scholar]
- 76.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the united states, 1988-1994 through 2013-2014. JAMA. 2016;315:2292–9. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ahrens W, Pigeot I, Pohlabeln H, et al. Prevalence of overweight and obesity in European children below the age of 10. Int J Obes. 2014;38(Suppl 2):S99–107. doi: 10.1038/ijo.2014.140. [DOI] [PubMed] [Google Scholar]
- 79.Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–42. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Organization WH. Obesity and overweight. Fact sheet No. 311. September 2006. Online document at: www.who.int/mediacentre/factsheets/fs311/en/index.html Accessed September. 2010;13. [Google Scholar]
- 81.Kotian MS, Kumar SG, Kotian SS. Prevalence and determinants of overweight and obesity among adolescent school children of South Karnataka, India. Indian J Community Med. 2010;35:176–8. doi: 10.4103/0970-0218.62587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Goyal JP, Kumar N, Parmar I, Shah VB, Patel B. Determinants of overweight and obesity in affluent adolescent in Surat city, South Gujarat region, India. Indian J Community Med. 2011;36:296–300. doi: 10.4103/0970-0218.91418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vohra R, Bhardwaj P, Srivastava JP, Srivastava S, Vohra A. Overweight and obesity among school-going children of Lucknow city. J Family Community Med. 2011;18:59–62. doi: 10.4103/2230-8229.83369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bovet P, Chiolero A, Shamlaye C, Paccaud F. Prevalence of overweight in the Seychelles: 15 year trends and association with socio-economic status. Obesity Rev. 2008;9:511–7. doi: 10.1111/j.1467-789X.2008.00513.x. [DOI] [PubMed] [Google Scholar]
- 85.Zhang X, van der Lans I, Dagevos H. Impacts of fast food and the food retail environment on overweight and obesity in China: a multilevel latent class cluster approach. Public Health Nutr. 2012;15:88–96. doi: 10.1017/S1368980011002047. [DOI] [PubMed] [Google Scholar]
- 86.Cheng TO. Fast food, automobiles, television and obesity epidemic in Chinese children. Int J Cardiol. 2005;98:173–4. doi: 10.1016/j.ijcard.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 87.Kelishadi R, Marashinia F, Heshmat R, et al. First report on body image and weight control in a nationally representative sample of a pediatric population in the Middle East and North Africa: the CASPIAN-III study. Arch Med Sci. 2013;9:210–7. doi: 10.5114/aoms.2013.34558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wisniewski AB, Chernausek SD. Gender in childhood obesity: family environment, hormones, and genes. Gender Med. 2009;6:76–85. doi: 10.1016/j.genm.2008.12.001. [DOI] [PubMed] [Google Scholar]