Abstract
Limited information is available in Asian populations regarding the association of dietary intake and patterns with age-related functional impairments. Using data from 2 population-based cohort studies in China, the Shanghai Women’s Health Study (1996–2015) and Shanghai Men’s Health Study (2002–2015), we prospectively examined adherence to dietary guidelines, including the Chinese Food Pagoda, the Dietary Approaches to Stop Hypertension, and the Alternative Healthy Eating Index, as well as consumption of specific foods, for their associations with impairment in function, both physical (walking, hearing/vision) and mental (memory, decision-making). Included in the analyses were 30,484 participants who had been followed for an average of 14.4 years and were between the ages of 70 and 86 years at the functional status assessment. Higher dietary-recommendation adherence scores were associated with a lower likelihood of developing functional impairments. The odds ratios ranged from 0.61 (95% confidence interval: 0.54, 0.70) to 0.83 (95% confidence interval: 0.72, 0.95) when extreme quintiles were compared. Higher fish, poultry, vegetable, and fruit intake, moderate red meat intake, and low rice consumption were associated with a reduced probability of having physical or mental impairments. Our findings highlight the importance of a high-quality diet in maintaining functional status among the aged population.
Keywords: diet, elderly, food, function impairments
Aging populations are growing rapidly around the world. By the year 2050, the global population of older adults (aged ≥60 years) is expected to increase from 841 million (2013) to 2 billion, which will comprise 21% of the world’s population (1). Deterioration in various functional capabilities, both physical and mental, arises with aging, which can result in decreased or lost capacity to undertake basic activities. Age-related onset of functional impairments has become a major cause of disability among the elderly population (2). Among the various factors that can contribute to earlier onset of functional impairments, dietary intake has been shown to play an important role. Diets rich in protein, vitamins, polyunsaturated fatty acid (PUFA), or antioxidants can potentially slow down the process or mitigate the impacts of functional impairments. A greater adherence to a Mediterranean diet has been shown to be associated with reduced risk of developing functional impairments (3–5). However, most of the existing research on this topic has been conducted among Western populations, whose dietary patterns are distinct from those of East Asian populations. Also, it remains unclear whether the recommended dietary guidelines in the United States might be associated with functional impairments in the large but understudied East Asian population, especially the Chinese.
We measured compliance with 3 dietary guidelines—the Chinese Food Pagoda (CHFP), modified Dietary Approaches to Stop Hypertension (DASH), and the modified Alternative Healthy Eating Index (AHEI)—and investigated their associations with functional impairments in 2 ongoing Chinese population-based cohort studies. Associations with intake of specific food groups were also assessed.
METHODS
Study population
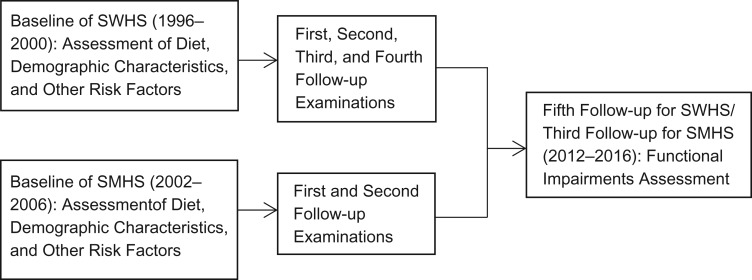
We used data from the Shanghai Women’s Health Study (SWHS) and Shanghai Men’s Health Study (SMHS). Details on the design of these 2 cohort studies have been published elsewhere (6, 7). Briefly, at study enrollment, a total of 74,941 Chinese women (aged 40–70 years old) and 61,480 Chinese men (aged 40–74 years) were recruited during 1996–2000 for SWHS and 2002–2006 for SMHS. Information on usual dietary habits, sociodemographic factors, lifestyle, anthropometrics, and medical history was collected through in-person interviews at baseline surveys. Participants have been followed every 2–4 years to update their health and lifestyle information (follow-up rates: ≥92% for both cohorts) and health status. Through April 2017, there have been a total of 5 follow-up surveys for the SWHS and 3 follow-up surveys for SMHS. The SWHS and SMHS were approved by the ethics review boards of participating institutions, and all participants provided written informed consent.
In the latest follow-up surveys, participants aged 70 years or older (n = 18,602 for SWHS; n = 12,150 for SMHS) were asked about their functional status (independent walking capability, hearing/vision, memory, and independent decision-making ability). Among them, 144 women and 124 men did not provide answers to the related questions. A total of 18,458 women and 12,026 men were included in our final study analysis (Figure 1).
Figure 1.
Timeline for data collection of study variables in Shanghai Women’s Health Study (SWHS), 1996–2016, and Shanghai Men’s Health Study (SMHS), 2002–2016, China.
Dietary assessment
Two virtually identical, comprehensive food-frequency questionnaires (FFQs) were used to assess habitual diet at study baseline for both cohorts. Participants were asked to recall the frequency and average amount of the specific foods they consumed during the past 12 months. The validity and reliability of the FFQs were evaluated by multiple 24-hour dietary recalls recorded twice a month for SWHS and once a month for SMHS, consecutively for 12 months. Food intake assessed by FFQ and the multiple 24-hour dietary recalls correlated well (for SWHS, correlation = 0.41–0.66; for SMHS, correlation = 0.35–0.72), suggesting good validity of assessing major food group intake by FFQ (8, 9).
Based on the dietary intake information, we derived 3 diet adherence scores based on compliance with the CHFP, DASH, or AHEI as described in detail elsewhere (10). In short, the CHFP score was created based on 10 components (grains, vegetables, fruits, dairy products, beans, meat and poultry, fish and shrimp, eggs, fats and oils, and salt) to measure the adherence to 2007 Chinese Dietary Guidelines. The modified DASH score included 7 components (including vegetables, fruits, dairy products, meat, poultry, fish and eggs, nuts, seeds and legumes, fats and oils, and sodium) of the original DASH score. The modified AHEI score was developed from 8 components (vegetables, fruit, nuts and legumes, red or processed meat, eicosapentaenoic acid and docosahexaenoic acid, PUFA, sodium, and alcohol). Information on whole grains, sugar-sweetened beverages, and trans fats were not included in our study due to data unavailability and relatively low intake in our study population (11–13). To score each component of food group intake, we first determined the maximum points based on the recommended intakes for each dietary guideline (45 for CHFP, 70 for modified DASH, and 80 for modified AHEI). The point for minimum intake was set at 0. Then, intermediate intakes between minimum and maximum amounts were graded proportionately. The total score for adherence to each dietary recommendation was obtained by summing all the included component scores.
Outcome assessment
Four questions were used to evaluate impairments in walking capability, hearing/vision, memory, and decision-making ability separately (14). The answers to each question originally included 5 choices that represented different levels of impairments from the least impaired to the most impaired. In consideration of statistical power, we collapsed the outcome variables into 2 or 3 groups in the analyses. Specifically, the outcome assessing independent walking capability was dichotomized into 2 groups: can walk independently without any assistance versus need assistance to walk. Outcomes for hearing/vision, memory, and decision-making ability were defined as having no, minor, or serious impairments in functional status.
Statistical analysis
We evaluated compliance with dietary guidelines by categorizing dietary adherence scores into quintiles based on the distribution of all study participants. Confounding variables adjusted for in the analyses were identified a priori by their association with both dietary intake pattern and functional status. These included total energy intake (kcal), sex, age (continuous), marital status (married/other), occupation (manual, clerical, professional), annual income (low, average, high), education (less than high school, high school, college or above), comorbidity (Charlson Comorbidity Index score (15) ≥1 or 0), alcohol use (continuous), smoking status (previous or current smoker, nonsmoker), exercise (yes/no; “yes” was defined as exercising at least once a week for more than 3 months), body mass index, waist-to-hip ratio, supplement intake (yes/no; included vitamin A, vitamin B, vitamin C, vitamin E, and multivitamins), and ginseng consumption (yes/no) at study baseline. Given the small percentage of missing data (≤3% for all the covariates), covariates with missing values were imputed with the median for continuous variables, or with the most common category for categorical variables. Logistic regression analyses were used to derive the odds ratios and 95% confidence intervals for binary outcomes, with the lowest quintile as the reference group for each dietary recommendation adherence score and food category separately. Multinomial logistic regression analyses were applied when outcomes had more than 2 categories. P values for trend were obtained by modeling the medians of each quintile as a continuous variable to examine the dose-response relationship by using the Wald test. We also evaluated the associations of the consumption of 8 specific food groups (rice, red meat, poultry, fish, vegetables, fruit, soy/soy products, and cooking oil) with functional impairments by categorizing the amount of intake in each food group into sex-specific quintiles. For those food groups that showed significant association with functional impairments, additional analyses were conducted to mutually adjust for other food consumption.
Analyses stratified by sex, education, and comorbidity status were conducted to assess the potential of effect modification. Heterogeneity across strata was assessed by inclusion of interaction terms in the statistical model. All P values were 2-sided and considered significant when they were <0.05. Statistical analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
The average age was 77.7 (range, 70.0 and 86.2) years for men and 78.1 (range, 70 and 88) years for women at the time of functional status assessment. Compared with female participants, male participants were more likely to be currently married, to have held a professional occupation, to have a lower body mass index, and to have higher education and income. Over a quarter of the male participants consumed at least 1 alcoholic drink per day, and over half of them were either ever or current smokers. In contrast, only a small portion of the female participants were habitual alcohol drinkers (2.3%) or smokers (4.3%). About 40% of the men and 18% of the women reported at least 1 chronic disease at study baseline. Over half (62.6% of men and 53% of women) were regular exercisers. The average total energy intake per day was 1,807 (range, 535–5,540) kcal for men and 1,611 (range, 173–5,726) kcal for women, with a large proportion from rice consumption. Soy/soy products were among the major protein sources in our study population (Table 1).
Table 1.
Baseline Characteristics According to Sex, Shanghai Women’s Health Study (1996–2015) and Shanghai Men’s Health Study (2002–2015), China
| Characteristic | Men | Women | ||||
|---|---|---|---|---|---|---|
| (n = 12,026) | (n = 18,458) | |||||
| Median | Range | % | Median | Range | % | |
| Age, years | 77.7 | 70.0–86.2 | 78.1 | 70.0–88.0 | ||
| Body mass indexa | 23.9 | 13.9–38.0 | 24.6 | 13.2–49.0 | ||
| Waist-to-hip ratio | 0.90 | 0.66–1.26 | 0.82 | 0.57–1.23 | ||
| Education beyond high school | 59.6 | 33.0 | ||||
| Occupation | ||||||
| Manual | 36.6 | 53.7 | ||||
| Clerical | 18.7 | 16.4 | ||||
| Professional | 44.7 | 30.0 | ||||
| Income | ||||||
| Low | 4.6 | 20.7 | ||||
| Average | 86.3 | 74.6 | ||||
| High | 9.1 | 4.7 | ||||
| Married | 98.8 | 83.3 | ||||
| Alcohol consumption ≥1 cup/day | 28.0 | 2.3 | ||||
| Ever or current smokers | 50.6 | 4.3 | ||||
| Charlson Comorbidity Index score ≥1 | 38.8 | 17.8 | ||||
| Regular leisure-time physical activity | 62.6 | 53.0 | ||||
| Supplement intakeb | 24.6 | 23.2 | ||||
| Ginseng ≥5 times/year | 41.8 | 40.5 | ||||
| Rice intake, g/day | 344.2 | 8.2–883.5 | 312.9 | 13.1–928.6 | ||
| Red meat intake, g/day | 44.6 | 0–1,173.5 | 37.5 | 0–419.5 | ||
| Poultry intake, g/day | 10.9 | 0–261.4 | 7.6 | 0–282.9 | ||
| Fish intake, g/day | 34.6 | 0–472.4 | 32.1 | 0–569.3 | ||
| Vegetable intake, g/day | 303.4 | 8.9–1,842.3 | 249.0 | 5.8–2,469.2 | ||
| Fruit intake, g/day | 137.9 | 0–1,517.9 | 206.4 | 0–2,016.1 | ||
| Soy/soy products intake, g/day | 125.3 | 0–1,113.5 | 104.7 | 0–1,614.2 | ||
| Oil intake, g/day | 34.3 | 0–1,71.7 | 33.3 | 0–175.0 | ||
| Total energy intake, kcal/day | 1,807 | 535–5,540 | 1,611 | 173–5,726 | ||
a Body mass index was calculated as weight (kg)/height (m)2.
b Supplements included vitamin A, vitamin B, vitamin C, vitamin E, and multivitamins.
Greater adherence levels to CHFP, DASH, or AHEI were all significantly associated with reduced probability of developing functional impairments after controlling for potential confounders. For walking capability, the DASH score showed the strongest association, with an odds ratio of 0.76 (95% confidence interval (CI): 0.67, 0.85), when comparing the highest with the lowest quintile. With regard to hearing and vision, the AHEI score showed the strongest association (odds ratio (OR) = 0.71, 95% CI: 0.62, 0.81) when comparing the highest with the lowest quintile. Regarding memory and decision-making, a higher AHEI score also was associated with the lowest probability of having functional impairments, with respective odds ratios being 0.67 (95% CI: 0.58, 0.78) and 0.61 (95% CI: 0.54, 0.70). P values for trend tests were all 0.01 or lower, except for the association between CHFP score and having a minor problem in hearing or vision (Table 2).
Table 2.
Adjusteda Odds Ratios for Functional Impairments According to Quintiles of Adherence to Published Dietary Guidelines (Chinese Food Pagoda, Dietary Approaches to Stop Hypertension, and Alternative Healthy Eating Index), Shanghai Women’s Health Study (1996–2015) and Shanghai Men’s Health Study (2002–2015), China
| Dietary Guideline and Quintile | Median Score | Walking Independently | Hearing and Vision | Memory | Making Decisions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unable | Minor Problem | Serious Problem | Minor Problem | Serious Problem | Sometimes Difficult | Always Difficult | |||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| CHFP | |||||||||||||||
| 1 | 28 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 32 | 0.94 | 0.85, 1.05 | 0.98 | 0.89, 1.07 | 0.92 | 0.81, 1.05 | 0.97 | 0.90, 1.06 | 0.95 | 0.83, 1.08 | 1.05 | 0.95, 1.17 | 0.94 | 0.84, 1.06 |
| 3 | 34 | 0.97 | 0.87, 1.09 | 0.93 | 0.85, 1.01 | 0.91 | 0.80, 1.04 | 0.85 | 0.78, 0.93 | 0.89 | 0.78, 1.02 | 0.91 | 0.82, 1.02 | 0.87 | 0.77, 0.98 |
| 4 | 36 | 0.83 | 0.74, 0.93 | 0.93 | 0.85, 1.02 | 0.81 | 0.71, 0.92 | 0.92 | 0.84, 1.00 | 0.76 | 0.66, 0.88 | 0.94 | 0.84, 1.05 | 0.78 | 0.69, 0.89 |
| 5 | 39 | 0.77 | 0.69, 0.87 | 1.00 | 0.91, 1.10 | 0.83 | 0.72, 0.95 | 0.91 | 0.83, 0.99 | 0.78 | 0.67, 0.90 | 0.91 | 0.81, 1.02 | 0.78 | 0.68, 0.89 |
| P for trend | <0.01 | 0.61 | <0.01 | 0.01 | <0.01 | 0.03 | <0.01 | ||||||||
| DASH | |||||||||||||||
| 1 | 37 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 43 | 0.94 | 0.84, 1.05 | 0.98 | 0.90, 1.08 | 0.99 | 0.87, 1.12 | 0.97 | 0.89, 1.05 | 0.94 | 0.82, 1.07 | 1.01 | 0.91, 1.13 | 0.96 | 0.86, 1.08 |
| 3 | 46 | 0.84 | 0.75, 0.94 | 0.95 | 0.87, 1.04 | 0.93 | 0.82, 1.06 | 0.93 | 0.85, 1.01 | 0.96 | 0.84, 1.10 | 0.93 | 0.83, 1.03 | 0.90 | 0.80, 1.01 |
| 4 | 50 | 0.84 | 0.75, 0.94 | 0.91 | 0.83, 1.00 | 0.81 | 0.71, 0.93 | 0.95 | 0.87, 1.03 | 0.79 | 0.69, 0.92 | 0.91 | 0.82, 1.02 | 0.75 | 0.66, 0.85 |
| 5 | 55 | 0.76 | 0.67, 0.85 | 0.90 | 0.82, 0.99 | 0.74 | 0.65, 0.85 | 0.87 | 0.80, 0.96 | 0.77 | 0.66, 0.89 | 0.88 | 0.78, 0.98 | 0.70 | 0.61, 0.80 |
| P for trend | <0.01 | 0.01 | <0.01 | <0.01 | <0.01 | 0.01 | <0.01 | ||||||||
| AHEI | |||||||||||||||
| 1 | 32 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 38 | 0.93 | 0.83, 1.03 | 0.90 | 0.82, 0.98 | 0.94 | 0.83, 1.07 | 0.97 | 0.89, 1.05 | 0.86 | 0.75, 0.98 | 0.87 | 0.79, 0.97 | 0.87 | 0.78, 0.98 |
| 3 | 43 | 0.87 | 0.78, 0.97 | 0.87 | 0.79, 0.95 | 0.88 | 0.77, 1.00 | 0.91 | 0.84, 0.99 | 0.83 | 0.72, 0.94 | 0.82 | 0.73, 0.91 | 0.76 | 0.67, 0.86 |
| 4 | 47 | 0.84 | 0.75, 0.94 | 0.89 | 0.82, 0.98 | 0.78 | 0.68, 0.89 | 0.83 | 0.77, 0.91 | 0.78 | 0.68, 0.89 | 0.79 | 0.71, 0.89 | 0.74 | 0.65, 0.84 |
| 5 | 53 | 0.77 | 0.68, 0.86 | 0.85 | 0.77, 0.93 | 0.71 | 0.62, 0.81 | 0.85 | 0.78, 0.93 | 0.67 | 0.58, 0.78 | 0.81 | 0.72, 0.90 | 0.61 | 0.54, 0.70 |
| P for trend | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | ||||||||
Abbreviations: AHEI, Alternative Healthy Eating Index; CHFP, Chinese Food Pagoda; CI, confidence interval; DASH, Dietary Approaches to Stop Hypertension; OR, odds ratio.
a Odds ratios were additionally adjusted for total energy intake (Kcal), age (continuous), body mass index, waist-to-hip ratio (categorized into tertiles), marital status (married/other), occupation (manual, clerical, professional), income (low, average, high), exercise (yes/no; “yes” was defined as exercising as least once a week for more than 3 months), comorbidity (yes/no), alcohol (continuous), education (less than high school, high school, college or above), smoking status (previous or current smoker, nonsmoker), sex, supplement intake (yes/no; included vitamin A, vitamin B, vitamin C, vitamin E, and multivitamins), and ginseng consumption (yes/no).
Specific food analyses showed that higher rice intake and lower poultry, fish, vegetable, and fruit intake were significantly associated with higher likelihood of having functional impairments regardless of whether the consumption data were analyzed continuously or categorically. The odds ratios for impaired walking capability, when comparing the highest with the lowest quintile intake of rice, poultry, fish, and fruit were 1.21 (95% CI: 1.02, 1.43), 0.83 (95% CI: 0.74, 0.94), 0.74 (95% CI: 0.66, 0.84), and 0.74 (95% CI: 0.66, 0.84), respectively. The odds ratios for impaired hearing or vision, comparing the highest with the lowest quintile of poultry, fish, vegetable, and fruit intake, were 0.85 (95% CI: 0.74, 0.97), 0.79 (95% CI: 0.69, 0.91), 0.84 (95% CI: 0.73, 0.96), and 0.70 (95% CI: 0.61, 0.81), respectively. Rice, poultry, fish, vegetable, and fruit intake were significantly associated with impairments in memory as well as decision-making ability. Fish consumption showed the strongest inverse association with impaired memory (OR = 0.68, 95% CI: 0.58, 0.79) and decision-making (OR = 0.65, 95% CI: 0.57, 0.74). Fruit intake was inversely associated with impaired decision-making ability (OR = 0.65, 95% CI: 0.57, 0.74). High red meat intake (fourth quintile: 44.7–64.3 grams/day for women, 52.9–75.8 grams/day for men) was associated with a lower likelihood of impairments in walking (OR = 0.86, 95% CI: 0.77, 0.97), memory (OR = 0.86, 95% CI: 0.75, 0.99), and decision-making (OR = 0.82, 95% CI: 0.72, 0.93). Soy/soy product consumption and cooking-oil use were not significantly associated with functional impairments (Table 3).
Table 3.
Adjusteda Odds Ratios Relating Quintiles of Intake for Each Food Group to Functional Impairments Among Elderly Persons, Shanghai Women’s Health Study (1996–2015) and Shanghai Men’s Health Study (2002–2015), China
| Food Group and Quintile | Median Intake, g/day | Walking Independently | Hearing and Vision | Memory | Making Decisions | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unable | Minor Problem | Serious Problem | Minor Problem | Serious Problem | Sometimes Difficult | Always Difficult | ||||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| Men | Women | |||||||||||||||
| Rice | ||||||||||||||||
| 1 | 253 | 222 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 301 | 275 | 0.87 | 0.78, 0.98 | 0.94 | 0.86, 1.03 | 0.85 | 0.74, 0.97 | 1.03 | 0.94, 1.12 | 0.96 | 0.83, 1.11 | 0.94 | 0.84, 1.06 | 1.03 | 0.91, 1.17 |
| 3 | 344 | 313 | 0.99 | 0.88, 1.12 | 0.98 | 0.89, 1.08 | 0.90 | 0.79, 1.04 | 1.04 | 0.95, 1.14 | 0.92 | 0.79, 1.07 | 1.07 | 0.95, 1.20 | 1.05 | 0.91, 1.20 |
| 4 | 402 | 351 | 1.00 | 0.87, 1.14 | 1.07 | 0.97, 1.19 | 1.06 | 0.91, 1.23 | 1.09 | 0.98, 1.21 | 1.10 | 0.93, 1.29 | 1.21 | 1.06, 1.38 | 1.19 | 1.02, 1.38 |
| 5 | 500 | 430 | 1.21 | 1.02, 1.43 | 1.03 | 0.91, 1.17 | 1.09 | 0.90, 1.31 | 1.21 | 1.07, 1.37 | 1.27 | 1.04, 1.55 | 1.45 | 1.23, 1.71 | 1.55 | 1.29, 1.86 |
| P for trend | 0.02 | 0.19 | 0.09 | <0.01 | 0.02 | <0.01 | <0.01 | |||||||||
| Red meat | ||||||||||||||||
| 1 | 16 | 12 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 31 | 25 | 0.98 | 0.88, 1.09 | 1.07 | 0.98, 1.17 | 1.12 | 0.99, 1.27 | 0.96 | 0.88, 1.16 | 1.00 | 0.88, 1.14 | 0.91 | 0.82, 1.01 | 0.98 | 0.87, 1.10 |
| 3 | 45 | 38 | 0.95 | 0.85, 1.06 | 1.04 | 0.95, 1.14 | 1.00 | 0.87, 1.14 | 0.92 | 0.85, 1.01 | 0.90 | 0.79, 1.04 | 0.94 | 0.84, 1.05 | 0.87 | 0.77, 0.98 |
| 4 | 62 | 53 | 0.86 | 0.77, 0.97 | 1.00 | 0.91, 1.10 | 1.04 | 0.92, 1.19 | 0.87 | 0.80, 0.95 | 0.86 | 0.75, 0.99 | 0.82 | 0.73, 0.92 | 0.82 | 0.72, 0.93 |
| 5 | 97 | 84 | 1.03 | 0.91, 1.17 | 0.99 | 0.90, 1.09 | 1.01 | 0.88, 1.16 | 0.95 | 0.86, 1.04 | 0.95 | 0.81, 1.10 | 0.87 | 0.77, 0.98 | 0.92 | 0.80, 1.05 |
| P for trend | 0.99 | 0.42 | 0.71 | 0.17 | 0.26 | 0.02 | 0.05 | |||||||||
| Poultry | ||||||||||||||||
| 1 | 2 | 1 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 6 | 4 | 0.88 | 0.79, 0.98 | 1.07 | 0.98, 1.18 | 1.07 | 0.94, 1.22 | 0.96 | 0.89, 1.05 | 0.89 | 0.78, 1.02 | 0.96 | 0.86, 1.07 | 0.87 | 0.77, 0.97 |
| 3 | 11 | 8 | 0.91 | 0.81, 1.01 | 1.02 | 0.93, 1.12 | 1.05 | 0.92, 1.19 | 0.90 | 0.83, 0.98 | 0.84 | 0.74, 0.96 | 0.88 | 0.79, 0.98 | 0.82 | 0.73, 0.93 |
| 4 | 19 | 14 | 0.84 | 0.75, 0.94 | 0.99 | 0.90, 1.08 | 0.89 | 0.78, 1.02 | 0.89 | 0.82, 0.97 | 0.83 | 0.72, 0.95 | 0.84 | 0.75, 0.94 | 0.77 | 0.68, 0.87 |
| 5 | 35 | 29 | 0.83 | 0.74, 0.94 | 0.96 | 0.87, 1.05 | 0.85 | 0.74, 0.97 | 0.87 | 0.80, 0.95 | 0.78 | 0.68, 0.91 | 0.81 | 0.72, 0.91 | 0.75 | 0.66, 0.85 |
| P for trend | <0.01 | 0.06 | 0.05 | <0.01 | <0.01 | <0.01 | <0.01 | |||||||||
| Fish | ||||||||||||||||
| 1 | 10 | 8 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 22 | 20 | 0.86 | 0.77, 0.95 | 0.98 | 0.90, 1.08 | 0.85 | 0.75, 0.96 | 0.97 | 0.90, 1.06 | 0.87 | 0.76, 0.99 | 0.95 | 0.86, 1.05 | 0.88 | 0.79, 0.99 |
| 3 | 35 | 32 | 0.81 | 0.73, 0.91 | 1.04 | 0.95, 1.14 | 0.94 | 0.83, 1.07 | 0.96 | 0.88, 1.04 | 0.88 | 0.77, 1.00 | 0.89 | 0.80, 0.99 | 0.87 | 0.77, 0.98 |
| 4 | 54 | 51 | 0.79 | 0.71, 0.89 | 1.05 | 0.96, 1.16 | 0.91 | 0.80, 1.04 | 0.91 | 0.83, 0.99 | 0.79 | 0.68, 0.90 | 0.81 | 0.72, 0.90 | 0.75 | 0.66, 0.85 |
| 5 | 97 | 94 | 0.74 | 0.66, 0.84 | 0.97 | 0.88, 1.07 | 0.79 | 0.69, 0.91 | 0.87 | 0.79, 0.95 | 0.68 | 0.58, 0.79 | 0.78 | 0.69, 0.88 | 0.65 | 0.57, 0.74 |
| P for trend | <0.01 | 0.54 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | |||||||||
| Vegetables | ||||||||||||||||
| 1 | 140 | 113 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 226 | 183 | 0.90 | 0.81, 1.01 | 1.05 | 0.96, 1.15 | 0.98 | 0.86, 1.11 | 0.93 | 0.85, 1.01 | 0.96 | 0.84, 1.10 | 0.86 | 0.77, 0.96 | 0.93 | 0.83, 1.05 |
| 3 | 303 | 249 | 0.93 | 0.83, 1.03 | 1.02 | 0.93, 1.11 | 0.95 | 0.84, 1.08 | 0.98 | 0.90, 1.07 | 0.95 | 0.83, 1.09 | 0.86 | 0.77, 0.96 | 0.83 | 0.73, 0.93 |
| 4 | 396 | 334 | 0.89 | 0.80, 1.00 | 1.02 | 0.93, 1.12 | 0.96 | 0.84, 1.09 | 0.97 | 0.89, 1.06 | 0.96 | 0.83, 1.10 | 0.88 | 0.78, 0.98 | 0.79 | 0.69, 0.89 |
| 5 | 577 | 494 | 0.95 | 0.84, 1.07 | 0.97 | 0.88, 1.07 | 0.84 | 0.73, 0.96 | 0.90 | 0.82, 0.98 | 0.82 | 0.71, 0.96 | 0.81 | 0.72, 0.91 | 0.71 | 0.62, 0.81 |
| P for trend | 0.46 | 0.29 | 0.01 | 0.06 | 0.02 | <0.01 | <0.01 | |||||||||
| Fruit | ||||||||||||||||
| 1 | 23 | 48 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 83 | 128 | 0.86 | 0.77, 0.95 | 0.98 | 0.90, 1.08 | 0.98 | 0.86, 1.11 | 0.86 | 0.79, 0.94 | 0.84 | 0.74, 0.96 | 0.86 | 0.77, 0.96 | 0.91 | 0.81, 1.02 |
| 3 | 138 | 206 | 0.72 | 0.65, 0.81 | 0.97 | 0.88, 1.07 | 0.87 | 0.76, 0.99 | 0.91 | 0.84, 1.00 | 0.79 | 0.69, 0.91 | 0.88 | 0.79, 0.98 | 0.76 | 0.67, 0.86 |
| 4 | 203 | 296 | 0.81 | 0.73, 0.91 | 0.88 | 0.80, 0.97 | 0.76 | 0.67, 0.87 | 0.88 | 0.80, 0.96 | 0.78 | 0.67, 0.90 | 0.86 | 0.77, 0.96 | 0.71 | 0.62, 0.80 |
| 5 | 313 | 445 | 0.74 | 0.66, 0.84 | 0.81 | 0.73, 0.89 | 0.70 | 0.61, 0.81 | 0.81 | 0.74, 0.88 | 0.79 | 0.69, 0.92 | 0.80 | 0.71, 0.90 | 0.65 | 0.57, 0.74 |
| P for trend | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | |||||||||
| Soy/soy products | ||||||||||||||||
| 1 | 40 | 29 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 81 | 63 | 0.99 | 0.88, 1.11 | 1.06 | 0.97, 1.16 | 1.07 | 0.94, 1.22 | 0.98 | 0.90, 1.07 | 0.96 | 0.83, 1.10 | 0.92 | 0.82, 1.03 | 0.90 | 0.80, 1.02 |
| 3 | 125 | 105 | 1.04 | 0.93, 1.16 | 1.09 | 1.00, 1.19 | 1.11 | 0.97, 1.26 | 1.00 | 0.92, 1.09 | 0.99 | 0.86, 1.14 | 0.98 | 0.87, 1.09 | 0.97 | 0.86, 1.10 |
| 4 | 196 | 188 | 1.07 | 0.95, 1.20 | 1.06 | 0.97, 1.16 | 1.01 | 0.89, 1.15 | 0.97 | 0.89, 1.06 | 0.95 | 0.83, 1.09 | 0.92 | 0.83, 1.03 | 0.97 | 0.85, 1.09 |
| 5 | 342 | 332 | 1.05 | 0.93, 1.17 | 1.02 | 0.93, 1.12 | 1.08 | 0.95, 1.23 | 0.98 | 0.90, 1.07 | 0.91 | 0.80, 1.05 | 0.95 | 0.85, 1.07 | 0.90 | 0.80, 1.02 |
| P for trend | 0.30 | 0.79 | 0.67 | 0.66 | 0.20 | 0.65 | 0.27 | |||||||||
| Cooking oil | ||||||||||||||||
| 1 | 550 | 625 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 830 | 833 | 0.97 | 0.86, 1.09 | 1.09 | 1.00, 1.19 | 1.19 | 1.04, 1.36 | 1.04 | 0.95, 1.13 | 1.08 | 0.93, 1.26 | 0.98 | 0.87, 1.10 | 1.00 | 0.88, 1.14 |
| 3 | 1,030 | 1,000 | 1.11 | 0.99, 1.25 | 1.07 | 0.98, 1.17 | 1.11 | 0.97, 1.26 | 1.07 | 0.98, 1.17 | 1.13 | 0.97, 1.31 | 1.05 | 0.94, 1.18 | 1.06 | 0.93, 1.21 |
| 4 | 1,275 | 1,250 | 1.05 | 0.93, 1.18 | 1.00 | 0.92, 1.10 | 1.13 | 0.99, 1.30 | 1.07 | 0.98, 1.17 | 1.18 | 1.02, 1.37 | 1.06 | 0.95, 1.19 | 1.09 | 0.96, 1.25 |
| 5 | 1,683 | 1,667 | 1.07 | 0.95, 1.20 | 1.04 | 0.95, 1.14 | 1.10 | 0.96, 1.26 | 1.07 | 0.98, 1.17 | 1.16 | 1.00, 1.35 | 1.09 | 0.97 1.22 | 0.97 | 0.85, 1.10 |
| P for trend | 0.17 | 0.94 | 0.53 | 0.14 | 0.05 | 0.07 | 0.67 | |||||||||
Abbreviations: CI, confidence interval; OR, odds ratio.
a Odds ratios were additionally adjusted for total energy intake (Kcal), age (continuous), body mass index, waist-to-hip ratio (categorized into tertiles), marital status (married/other), occupation (manual, clerical, professional), income (low, average, high), exercise (yes/no; “yes” was defined as exercising as least once a week for more than 3 months), comorbidity (yes/no), alcohol (continuous), education (less than high school, high school, college or above), smoking status (previous or current smoker, nonsmoker), sex, supplement intake (yes/no; included vitamin A, vitamin B, vitamin C, vitamin E, and multivitamins), and ginseng consumption (yes/no).
After mutual adjustment for food group intake, higher rice intake was positively associated with having some difficulty in making decisions. The odds ratio comparing the highest versus the lowest quintile of rice intake was 1.22 (95% CI: 1.01, 1.47). A significant inverse dose-response trend was observed between poultry intake and hearing/vision impairment (P for trend = 0.01), but point estimates comparing quintiles were not statistically significant. Higher poultry intake was associated with having less difficulty in making decisions (OR = 0.84, 95% CI: 0.74, 0.97). Higher fish consumption was inversely associated with impaired walking capability (OR = 0.79, 95% CI: 0.69, 0.89), memory decline (OR = 0.73, 95% CI: 0.62, 0.86), and having difficulty in making decisions (OR = 0.75, 95% CI: 0.65, 0.87). A significant inverse dose-response trend was observed between vegetable intake and having difficulty in decision-making (P for trend = 0.02). Fruit intake showed an inverse association for all 4 functional impairments under study; the odds ratio was 0.77 (95% CI: 0.68, 0.87) for impairment in walking, 0.70 (95% CI: 0.61, 0.81) for hearing and vision deficiency, 0.85 (95% CI: 0.73, 1.00) for memory decline, and 0.73 (95% CI: 0.63, 0.84) for impairment in decision-making (Table 4). Sensitivity analyses showed that excluding red meat intake in the mutually adjustment model did not make an appreciable difference for the observed significant associations.
Table 4.
Mutually Adjusteda Odds Ratios Relating Quintiles of Intake for Each Food Group to Functional Impairments Among Elderly Persons, Shanghai Women’s Health Study (1996–2015) and Shanghai Men’s Health Study (2002–2015), China
| Food Group and Quintile | Median Intake, g/day | Walking Independently | Hearing and Vision | Memory | Making Decisions | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unable | Minor Problem | Serious Problem | Minor Problem | Serious Problem | Sometimes Difficult | Always Difficult | ||||||||||
| Men | Women | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Rice | ||||||||||||||||
| 1 | 253 | 222 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 301 | 275 | 0.84 | 0.75, 0.95 | 0.90 | 0.82, 0.99 | 0.78 | 0.68, 0.89 | 0.99 | 0.91, 1.08 | 0.90 | 0.78, 1.05 | 0.91 | 0.81, 1.02 | 0.93 | 0.82, 1.06 |
| 3 | 344 | 313 | 0.92 | 0.81, 1.05 | 0.93 | 0.84, 1.03 | 0.79 | 0.68, 0.92 | 0.98 | 0.89, 1.08 | 0.83 | 0.71, 0.97 | 1.00 | 0.88, 1.14 | 0.89 | 0.77, 1.02 |
| 4 | 402 | 351 | 0.90 | 0.78, 1.04 | 0.99 | 0.88, 1.11 | 0.87 | 0.74, 1.03 | 1.01 | 0.90, 1.13 | 0.94 | 0.79, 1.12 | 1.10 | 0.95, 1.26 | 0.93 | 0.79, 1.09 |
| 5 | 500 | 430 | 0.99 | 0.82, 1.20 | 0.89 | 0.77, 1.04 | 0.77 | 0.62, 0.96 | 1.05 | 0.91, 1.21 | 0.96 | 0.76, 1.21 | 1.22 | 1.01, 1.47 | 1.00 | 0.81, 1.24 |
| P for trend | 0.79 | 0.51 | 0.11 | 0.48 | 0.61 | 0.03 | 0.84 | |||||||||
| Poultry | ||||||||||||||||
| 1 | 2 | 1 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 6 | 4 | 0.91 | 0.82, 1.02 | 1.08 | 0.98, 1.18 | 1.09 | 0.96, 1.24 | 0.97 | 0.90, 1.06 | 0.92 | 0.80, 1.05 | 0.98 | 0.88, 1.09 | 0.89 | 0.79, 1.00 |
| 3 | 11 | 8 | 0.96 | 0.86, 1.07 | 1.02 | 0.93, 1.12 | 1.06 | 0.93, 1.21 | 0.91 | 0.84, 1.00 | 0.88 | 0.76, 1.01 | 0.91 | 0.82, 1.02 | 0.86 | 0.76, 0.97 |
| 4 | 19 | 14 | 0.91 | 0.81, 1.02 | 0.98 | 0.90, 1.08 | 0.92 | 0.80, 1.05 | 0.92 | 0.84, 1.00 | 0.88 | 0.76, 1.01 | 0.89 | 0.80, 1.00 | 0.83 | 0.73, 0.94 |
| 5 | 35 | 29 | 0.91 | 0.80, 1.03 | 0.95 | 0.87, 1.05 | 0.88 | 0.76, 1.01 | 0.91 | 0.83, 1.00 | 0.86 | 0.74, 1.00 | 0.89 | 0.79, 1.00 | 0.84 | 0.74, 0.97 |
| P for trend | 0.08 | 0.09 | 0.01 | 0.06 | 0.06 | 0.02 | 0.02 | |||||||||
| Fish | ||||||||||||||||
| 1 | 10 | 8 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 22 | 20 | 0.89 | 0.80, 0.99 | 0.99 | 0.90, 1.09 | 0.86 | 0.76, 0.98 | 1.00 | 0.92, 1.08 | 0.90 | 0.79, 1.02 | 0.99 | 0.89, 1.10 | 0.93 | 0.83, 1.05 |
| 3 | 35 | 32 | 0.86 | 0.77, 0.96 | 1.06 | 0.96, 1.16 | 0.98 | 0.86, 1.12 | 1.00 | 0.91, 1.09 | 0.92 | 0.80, 1.06 | 0.95 | 0.85, 1.06 | 0.94 | 0.83, 1.07 |
| 4 | 54 | 51 | 0.84 | 0.75, 0.95 | 1.08 | 0.98, 1.19 | 0.96 | 0.84, 1.10 | 0.95 | 0.87, 1.04 | 0.84 | 0.72, 0.97 | 0.88 | 0.78, 0.99 | 0.84 | 0.74, 0.96 |
| 5 | 97 | 94 | 0.79 | 0.69, 0.89 | 1.00 | 0.91, 1.11 | 0.85 | 0.74, 0.99 | 0.92 | 0.84, 1.01 | 0.73 | 0.62, 0.86 | 0.88 | 0.78, 1.00 | 0.75 | 0.65, 0.87 |
| P for trend | <0.01 | 0.80 | 0.10 | 0.04 | <0.01 | 0.01 | <0.01 | |||||||||
| Vegetables | ||||||||||||||||
| 1 | 140 | 113 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 226 | 183 | 0.96 | 0.86, 1.08 | 1.06 | 0.97, 1.16 | 1.01 | 0.89, 1.15 | 0.95 | 0.87, 1.03 | 1.01 | 0.88, 1.16 | 0.90 | 0.80, 1.00 | 0.99 | 0.88, 1.11 |
| 3 | 303 | 249 | 1.01 | 0.90, 1.13 | 1.04 | 0.94, 1.14 | 1.01 | 0.88, 1.15 | 1.01 | 0.94, 1.11 | 1.03 | 0.89, 1.18 | 0.92 | 0.82, 1.02 | 0.91 | 0.80, 1.03 |
| 4 | 396 | 334 | 0.99 | 0.88, 1.12 | 1.06 | 0.96, 1.17 | 1.04 | 0.91, 1.19 | 1.03 | 0.94, 1.12 | 1.05 | 0.91, 1.22 | 0.96 | 0.85, 1.07 | 0.90 | 0.79, 1.02 |
| 5 | 577 | 577 | 1.07 | 0.94, 1.22 | 1.03 | 0.93, 1.14 | 0.93 | 0.80, 1.08 | 0.97 | 0.88, 1.07 | 0.91 | 0.78, 1.08 | 0.91 | 0.80, 1.04 | 0.83 | 0.79, 1.02 |
| P for trend | 0.31 | 0.84 | 0.37 | 0.91 | 0.41 | 0.34 | 0.02 | |||||||||
| Fruit | ||||||||||||||||
| 1 | 23 | 48 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| 2 | 83 | 128 | 0.88 | 0.79, 0.97 | 0.97 | 0.89, 1.07 | 0.98 | 0.86, 1.11 | 0.87 | 0.80, 0.95 | 0.86 | 0.75, 0.98 | 0.89 | 0.80, 0.99 | 0.94 | 0.84, 1.05 |
| 3 | 138 | 206 | 0.75 | 0.67, 0.84 | 0.95 | 0.87, 1.05 | 0.87 | 0.76, 0.99 | 0.93 | 0.86, 1.02 | 0.83 | 0.72, 0.95 | 0.93 | 0.83, 1.04 | 0.81 | 0.72, 0.92 |
| 4 | 203 | 296 | 0.85 | 0.75, 0.95 | 0.86 | 0.78, 0.95 | 0.77 | 0.67, 0.88 | 0.90 | 0.82, 0.99 | 0.82 | 0.71, 0.95 | 0.93 | 0.83, 1.05 | 0.78 | 0.68, 0.89 |
| 5 | 313 | 445 | 0.77 | 0.68, 0.87 | 0.79 | 0.71, 0.87 | 0.70 | 0.61, 0.81 | 0.84 | 0.76, 0.92 | 0.85 | 0.73, 1.00 | 0.90 | 0.79, 1.02 | 0.73 | 0.63, 0.84 |
| P for trend | <0.01 | <0.01 | <0.01 | <0.01 | 0.03 | 0.19 | <0.01 | |||||||||
Abbreviations: CI, confidence interval; OR, odds ratio.
a Odds ratios were additionally adjusted for total energy intake (Kcal), age (continuous), body mass index, waist-to-hip ratio (categorized into tertiles), marital status (married/other), occupation (manual, clerical, professional), income (low, average, high), exercise (yes/no; “yes” was defined as exercising as least once a week for more than 3 months), comorbidity (yes/no), alcohol (continuous), education (less than high school, high school, college or above), smoking status (previous or current smoker, nonsmoker), sex, supplement intake (yes/no; included vitamin A, vitamin B, vitamin C, vitamin E, and multivitamins), and ginseng consumption (yes/no).
Additional analyses stratified by education, comorbidity, and sex were conducted. Mutually adjusted odds ratios comparing the highest with the lowest quintile of each food group intake are presented in Table 5. Educational level modified several associations: rice intake with walking ability, poultry consumption with memory and decision-making, and fruit intake with hearing/vision, memory, and decision-making. Higher consumption of poultry showed significant inverse associations with impairments in memory and decision-making only among the population with less than a high-school education. The estimated association between fruit intake and serious impairments in hearing/vision was stronger among those with at least a high-school education. Estimated odds ratios stratified by comorbidity status showed heterogeneity only for the association of rice with walking capability and decision-making, but none of the odds ratios in these strata were statistically significant. We did not find that sex modified the associations under study (data not shown).
Table 5.
Adjusteda Odds Ratios Comparing the Highest to the Lowest Quintile of Intake for Each Food Group in Relation to Functional Impairments Among Elderly Persons, Stratified by Education and Comorbidity, Shanghai Women’s Health Study (1996–2015) and Shanghai Men’s Health Study (2002–2015), China
| Food Group and Stratum | Walking Independently | Hearing and Vision | Memory | Making Decision | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unable | Minor Problem | Serious Problem | Minor Problem | Serious Problem | Sometimes Difficult | Always Difficult | ||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Rice | ||||||||||||||
| Less than high school | 0.98 | 0.93, 1.04 | 1.02 | 0.97, 1.07 | 0.97 | 0.91, 1.03 | 0.98 | 0.94, 1.02 | 0.99 | 0.93, 1.05 | 1.04 | 0.99, 1.10 | 0.97 | 0.92, 1.03 |
| High school or more | 1.01 | 0.93, 1.09 | 0.98 | 0.93, 1.03 | 0.99 | 0.91, 1.07 | 1.06 | 1.01, 1.12 | 0.99 | 0.90, 1.09 | 1.06 | 0.98, 1.14 | 1.03 | 0.95, 1.13 |
| P for interaction | 0.01 | 0.81 | 0.63 | 0.35 | 0.87 | 0.41 | 0.31 | |||||||
| Poultry | ||||||||||||||
| Less than high school | 0.97 | 0.94, 1.00 | 1.00 | 0.97, 1.03 | 0.97 | 0.93, 1.01 | 0.97 | 0.95, 1.00 | 0.95 | 0.91, 0.99 | 0.95 | 0.92, 0.98 | 0.94 | 0.91, 0.98 |
| High school or more | 0.99 | 0.94, 1.04 | 0.97 | 0.94, 1.00 | 0.95 | 0.90, 1.00 | 0.98 | 0.95, 1.02 | 0.99 | 0.93, 1.05 | 1.00 | 0.96, 1.05 | 0.99 | 0.94, 1.05 |
| P for interaction | 0.33 | 0.69 | 0.97 | <0.01 | 0.25 | <0.01 | 0.02 | |||||||
| Fish | ||||||||||||||
| Less than high school | 0.94 | 0.91, 0.98 | 1.01 | 0.98, 1.04 | 0.96 | 0.92, 1.01 | 0.99 | 0.96, 1.01 | 0.94 | 0.90, 0.98 | 0.96 | 0.92, 0.99 | 0.96 | 0.92, 0.99 |
| High school or more | 0.94 | 0.89, 0.99 | 1.02 | 0.99, 1.06 | 1.01 | 0.95, 1.06 | 0.97 | 0.94, 1.00 | 0.93 | 0.87, 0.99 | 0.98 | 0.93, 1.03 | 0.89 | 0.84, 0.94 |
| P for interaction | 0.24 | 0.63 | 0.52 | 0.05 | 0.55 | 0.48 | 0.38 | |||||||
| Vegetables | ||||||||||||||
| Less than high school | 1.01 | 0.98, 1.05 | 1.02 | 0.99, 1.06 | 1.00 | 0.95, 1.04 | 1.00 | 0.97, 1.02 | 1.00 | 0.95, 1.04 | 0.99 | 0.96, 1.03 | 0.95 | 0.91, 0.99 |
| High school or more | 1.03 | 0.97, 1.08 | 0.99 | 0.96, 1.02 | 0.99 | 0.93, 1.05 | 1.01 | 0.98, 1.05 | 0.97 | 0.91, 1.04 | 0.98 | 0.93, 1.04 | 0.97 | 0.91, 1.03 |
| P for interaction | 0.97 | 0.98 | 0.61 | 0.14 | 0.77 | 0.84 | 0.30 | |||||||
| Fruit | ||||||||||||||
| Less than high school | 0.95 | 0.91, 0.98 | 0.95 | 0.92, 0.98 | 0.93 | 0.89, 0.97 | 0.96 | 0.93, 0.99 | 0.95 | 0.91, 0.99 | 0.98 | 0.95, 1.02 | 0.90 | 0.86, 0.93 |
| High school or more | 0.92 | 0.87, 0.97 | 0.94 | 0.91, 0.97 | 0.88 | 0.83, 0.93 | 0.98 | 0.95, 1.02 | 0.99 | 0.93, 1.06 | 0.97 | 0.92, 1.02 | 0.97 | 0.92, 1.03 |
| P for interaction | 0.45 | 0.07 | 0.04 | 0.02 | 0.50 | 0.02 | 0.72 | |||||||
| Rice | ||||||||||||||
| No comorbidity | 1.01 | 0.96, 1.06 | 0.99 | 0.95, 1.03 | 0.97 | 0.92, 1.03 | 1.01 | 0.97, 1.05 | 0.98 | 0.92, 1.04 | 1.06 | 1.01, 1.12 | 0.98 | 0.93, 1.04 |
| ≥1 comorbidity | 0.97 | 0.90, 1.04 | 1.04 | 0.97, 1.11 | 0.98 | 0.89, 1.07 | 1.01 | 0.95, 1.08 | 1.03 | 0.93, 1.13 | 1.01 | 0.94, 1.10 | 1.01 | 0.93, 1.10 |
| P for interaction | <0.01 | 0.40 | 0.44 | 0.10 | 0.06 | 0.06 | <0.01 | |||||||
| Poultry | ||||||||||||||
| No comorbidity | 0.98 | 0.95, 1.02 | 0.99 | 0.96, 1.01 | 0.96 | 0.92, 0.99 | 0.96 | 0.94, 0.99 | 0.97 | 0.93, 1.01 | 0.97 | 0.94, 1.00 | 0.95 | 0.92, 0.99 |
| ≥1 comorbidity | 0.96 | 0.92, 1.01 | 0.97 | 0.93, 1.02 | 0.97 | 0.91, 1.02 | 1.01 | 0.97, 1.05 | 0.95 | 0.89, 1.01 | 0.96 | 0.91, 1.01 | 0.97 | 0.92, 1.02 |
| P for interaction | 0.48 | 0.84 | 0.62 | 0.49 | 0.46 | 0.26 | 0.21 | |||||||
| Fish | ||||||||||||||
| No comorbidity | 0.94 | 0.91, 0.97 | 1.01 | 0.98, 1.04 | 0.98 | 0.94, 1.02 | 0.99 | 0.96, 1.01 | 0.93 | 0.89, 0.97 | 0.96 | 0.93, 0.99 | 0.93 | 0.89, 0.97 |
| ≥1 comorbidity | 0.95 | 0.90, 1.00 | 1.03 | 0.98, 1.07 | 1.00 | 0.94, 1.06 | 0.96 | 0.92, 1.00 | 0.94 | 0.88, 1.00 | 0.96 | 0.91, 1.01 | 0.95 | 0.89, 1.00 |
| P for interaction | 0.77 | 0.62 | 0.85 | 0.57 | 0.66 | 0.62 | 0.34 | |||||||
| Vegetables | ||||||||||||||
| No comorbidity | 1.01 | 0.97, 1.05 | 1.01 | 0.98, 1.03 | 0.98 | 0.94, 1.02 | 1.00 | 0.98, 1.03 | 0.99 | 0.95, 1.04 | 0.99 | 0.96, 1.03 | 0.95 | 0.91, 0.99 |
| ≥1 comorbidity | 1.02 | 0.97, 1.07 | 1.01 | 0.97, 1.06 | 1.01 | 0.95, 1.08 | 1.00 | 0.96, 1.04 | 0.98 | 0.92, 1.05 | 0.98 | 0.92, 1.03 | 0.96 | 0.91, 1.02 |
| P for interact | 0.77 | 0.64 | 0.98 | 0.48 | 0.48 | 0.62 | 0.56 | |||||||
| Fruit | ||||||||||||||
| No comorbidity | 0.95 | 0.92, 0.99 | 0.94 | 0.91, 0.96 | 0.91 | 0.88, 0.95 | 0.96 | 0.93, 0.98 | 0.96 | 0.92, 1.00 | 0.97 | 0.94, 1.00 | 0.91 | 0.87, 0.95 |
| ≥1 comorbidity | 0.93 | 0.89, 0.98 | 0.96 | 0.92, 1.01 | 0.92 | 0.87, 0.97 | 1.00 | 0.96, 1.04 | 0.97 | 0.91, 1.03 | 1.00 | 0.95, 1.06 | 0.95 | 0.90, 1.00 |
| P for interaction | 0.33 | 0.96 | 0.88 | 0.42 | 0.69 | 0.14 | 0.79 | |||||||
Abbreviations: CI, confidence interval; OR, odds ratio.
a Odds ratios were additionally adjusted for total energy intake (Kcal), age (continuous), body mass index, waist-to-hip ratio (categorized into tertiles), marital status (married/other), occupation (manual, clerical, professional), income (low, average, high), exercise (yes/no; “yes” was defined as exercising as least once a week for more than 3 months), comorbidity (yes/no), alcohol (continuous), education (less than high school, high school, college or above), smoking status (previous or current smoker, nonsmoker), sex, supplement intake (yes/no; included vitamin A, vitamin B, vitamin C, vitamin E, and multivitamins), and ginseng consumption (yes/no).
Comorbidity status modified the association between DASH score and having difficulty in decision-making; the significant inverse association only existed among participants with no comorbidity (OR = 0.74, 95% CI: 0.62, 0.89). Sex also modulated the associations of CHFP and DASH scores with decision-making. The estimated inverse associations were significant only among women. The association between AHEI score and walking capability showed significant heterogeneity between men and women, with men showing a stronger association with a higher AHEI score, when compared with women (Table 6). No significant effect modification by educational level was seen (data not shown).
Table 6.
Adjusteda Odds Ratios Comparing the Highest to the Lowest Scoring Quintile of Adherence to Published Dietary Guidelines (Chinese Food Pagoda, Dietary Approaches to Stop Hypertension, and Alternative Healthy Eating Index) in Relation to Functional Impairments Among Elderly Persons, Stratified by Comorbidity and Sex, Shanghai Women’s Health Study (1996–2015) and Shanghai Men’s Health Study (2002–2015), China
| Dietary Guideline and Stratum | Walking Independently | Hearing and Vision | Memory | Making Decisions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unable | Minor Problem | Serious Problem | Minor Problem | Serious Problem | Sometimes Difficult | Always Difficult | ||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| CHFP | ||||||||||||||
| No comorbidity | 0.81 | 0.70, 0.94 | 0.98 | 0.88, 1.09 | 0.80 | 0.68, 0.94 | 0.93 | 0.84, 1.03 | 0.78 | 0.65, 0.93 | 0.93 | 0.84, 1.03 | 0.78 | 0.65, 0.93 |
| ≥1 comorbidity | 0.72 | 0.59, 0.89 | 1.09 | 0.90, 1.32 | 0.92 | 0.71, 1.18 | 0.86 | 0.72, 1.02 | 0.80 | 0.61, 1.04 | 0.86 | 0.72, 1.02 | 0.80 | 0.61, 1.04 |
| P for interaction | 0.89 | 0.96 | 0.61 | 0.09 | 0.08 | >0.99 | 0.10 | |||||||
| DASH | ||||||||||||||
| No comorbidity | 0.77 | 0.66, 0.89 | 0.88 | 0.79, 0.98 | 0.72 | 0.61, 0.84 | 0.87 | 0.78, 0.96 | 0.74 | 0.62, 0.89 | 0.87 | 0.78, 0.96 | 0.74 | 0.62, 0.89 |
| ≥1 comorbidity | 0.76 | 0.61, 0.93 | 0.98 | 0.81, 1.18 | 0.84 | 0.64, 1.08 | 0.91 | 0.76, 1.08 | 0.85 | 0.66, 1.11 | 0.91 | 0.76, 1.08 | 0.85 | 0.66, 1.11 |
| P for interaction | 0.71 | 0.30 | 0.09 | 0.85 | 0.35 | 0.31 | 0.02 | |||||||
| AHEI | ||||||||||||||
| No comorbidity | 0.77 | 0.67, 0.89 | 0.82 | 0.73, 0.91 | 0.64 | 0.55, 0.75 | 0.83 | 0.75, 0.92 | 0.70 | 0.59, 0.83 | 0.83 | 0.75, 0.92 | 0.70 | 0.59, 0.83 |
| ≥1 comorbidity | 0.74 | 0.60, 0.92 | 0.96 | 0.79, 1.17 | 0.93 | 0.71, 1.21 | 0.93 | 0.78, 1.11 | 0.63 | 0.48, 0.84 | 0.93 | 0.78, 1.11 | 0.63 | 0.48, 0.84 |
| P for interaction | 0.98 | 0.09 | 0.16 | 0.46 | 0.46 | 0.75 | 0.44 | |||||||
| CHFP | ||||||||||||||
| Men | 0.70 | 0.57, 0.86 | 1.08 | 0.94, 1.25 | 0.89 | 0.72, 1.10 | 0.91 | 0.79, 1.04 | 0.85 | 0.66, 1.09 | 0.91 | 0.79, 1.04 | 0.85 | 0.66, 1.09 |
| Women | 0.82 | 0.71, 0.96 | 0.94 | 0.83, 1.07 | 0.79 | 0.66, 0.94 | 0.91 | 0.81, 1.02 | 0.74 | 0.62, 0.89 | 0.91 | 0.81, 1.02 | 0.74 | 0.62, 0.89 |
| P for interaction | 0.13 | 0.31 | 0.39 | 0.33 | 0.13 | 0.59 | 0.01 | |||||||
| DASH | ||||||||||||||
| Men | 0.74 | 0.60, 0.91 | 1.00 | 0.87, 1.15 | 0.79 | 0.64, 0.98 | 0.88 | 0.77, 1.02 | 0.82 | 0.64, 1.05 | 0.88 | 0.77, 1.02 | 0.82 | 0.64, 1.05 |
| Women | 0.76 | 0.66, 0.89 | 0.83 | 0.73, 0.93 | 0.70 | 0.59, 0.84 | 0.87 | 0.78, 0.98 | 0.74 | 0.62, 0.90 | 0.87 | 0.78, 0.98 | 0.74 | 0.62, 0.90 |
| P for interaction | 0.98 | 0.46 | 0.67 | 0.30 | 0.12 | 0.74 | 0.01 | |||||||
| AHEI | ||||||||||||||
| Men | 0.66 | 0.53, 0.81 | 0.87 | 0.76, 1.01 | 0.78 | 0.63, 0.96 | 0.85 | 0.74, 0.99 | 0.65 | 0.50, 0.84 | 0.85 | 0.74, 0.99 | 0.65 | 0.50, 0.84 |
| Women | 0.82 | 0.71, 0.94 | 0.83 | 0.73, 0.94 | 0.66 | 0.56, 0.79 | 0.86 | 0.77, 0.96 | 0.69 | 0.58, 0.83 | 0.86 | 0.77, 0.96 | 0.69 | 0.58, 0.83 |
| P for interaction | <0.01 | 0.92 | 0.32 | 0.82 | 0.65 | 0.44 | 0.14 | |||||||
Abbreviations: AHEI, Alternative Healthy Eating Index; CHFP, Chinese Food Pagoda; CI, confidence interval; DASH, Dietary Approaches to Stop Hypertension; OR, odds ratio.
a Odds ratios were additionally adjusted for total energy intake (Kcal), age (continuous), body mass index, waist-to-hip ratio (categorized into tertiles), marital status (married/other), occupation (manual, clerical, professional), income (low, average, high), exercise (yes/no; “yes” was defined as exercising as least once a week for more than 3 months), comorbidity (yes/no), alcohol (continuous), education (less than high school, high school, college or above), smoking status (previous or current smoker, nonsmoker), sex, supplement intake (yes/no; included vitamin A, vitamin B, vitamin C, vitamin E, and multivitamins), and ginseng consumption (yes/no).
DISCUSSION
In this large-scale population-based study of Chinese men and women aged 70–88 years, we found that greater adherence to dietary guidelines (CHFP, DASH, and AHEI), reflecting an overall higher diet quality, was associated with a lower probability of having physical or mental impairments. Magnitudes of reduction in functional impairments ranged from 17% to 39% when extreme quintiles were compared. Higher poultry, fish, vegetable, and fruit intake were shown to be associated with a lower likelihood of having functional impairments when a wide range of potential confounders, caloric intake, and consumptions of these foods were mutually adjusted. Additionally, socioeconomic status, measured by educational level, modified some of the associations between food group intake and functional impairments. Comorbidity and sex modulated the associations between adherence to dietary guidelines and functional impairments.
Our findings are generally consistent with previous reports on this topic. Prospective cohort studies have linked greater adherence to a Mediterranean-style diet with reduced risk of frailty and cognitive impairment (16–18). In a population-based study from Australia, greater adherence to the Healthy Eating Index for Australians was found to be associated with a reduced likelihood of developing concurrent vision and hearing loss (19). In a 13-year follow-up study of elderly French women, it was found that recent cognitive decline was associated with lower intakes of poultry, fish, animal fats, and soluble dietary fiber, and that frailty was associated with a lower intake of vegetables (20). In the Women’s Health Initiative observational study, higher protein consumption was associated with a dose-responsive lower risk of incident frailty in older women (21). Results from the Taiwan Longitudinal Study of Aging suggested that a diet that includes low consumption of fish and fruits may adversely affect cognitive function in older Taiwanese (22).
Several potential explanations have been proposed for the identified associations between dietary food groups and functional impairments. Animal source proteins are complete proteins and are a source of higher biological-value proteins than plant proteins (23–25). Higher intake of such protein can help overcome the age-related blunting capacity of protein synthesizing, absorption, and utilization to meet nutritional demands (26, 27). Studies have shown a link between lower dietary protein and lean body mass loss (28, 29). Low muscle mass is known to be associated with both physical and cognitive impairment (30–34). Moreover, research has shown that omega-3 PUFA-enriched foods (such as fish) play an important role in supporting human cognitive processes (35) and can regulate genes for maintaining synaptic function and plasticity in animals (36). A deficiency of omega-3 PUFA has also been shown to be related to higher likelihood of cognitive decline (37–39).
The association of vegetables and fruits with physical and mental functional capacities may be attributed to beneficial antioxidants and vitamins rich in these foods. Both are significantly associated with decreased risk of chronic diseases (40) and oxidative damage (41), as well as maintenance of immune system responses (42). The inverse association between fruit intake and sensory impairments could probably be mediated by reduction of inflammation, oxidative stress, or improving endothelial dysfunction among older adults (43–47). For the majority of the observed significant associations, fruit intake remained associated with functional impairment after mutual adjustment for other food groups, whereas vegetable intake did not. A potential explanation for this is that fruits are consumed raw while vegetables are often cooked in our study population. Some beneficial nutrients, such as antioxidative vitamin C, may get lost during the cooking process. In addition, vegetable intake in our study population is in general high, and variation is not as large as with fruit intake. Furthermore, our FFQs have a higher validity to capture information on fruit intake (for the SWHS, correlation = 0.55; for the SMHS, correlation = 0.72) versus vegetable intake (for the SWHS, correlation = 0.41; for the SMHS, correlation = 0.42). The latter two may reduce the statistical power to detect an association between vegetable intake and functional impairment. Research from other populations is needed to confirm our speculation.
Rice is the most common energy source among the Chinese, particularly elderly Chinese, accounting for approximately 70% of total caloric intake in our study population. Higher rice intake was significantly associated with multiple areas of functional decline when consumption of other foods was not controlled for. However, after adjusting for other foods, most of the rice associations were no longer significant. These results indicate that higher rice intake may become detrimental only when its consumption replaces the intake of other, more nutritious foods. Our study also found that higher poultry consumption showed a stronger protective association for those with a lower educational level. The possible explanation for this could be that participants with lower socioeconomic status generally are not able to afford to consume much high-quality protein from other foods or are more likely to face other detrimental exposures that we did not capture in this study.
Regarding dietary adherence scores, AHEI showed the strongest association, especially for cognitive impairment. This lends further support to the important role of PUFA in maintaining cognitive function among the elderly, given the fact that AHEI is the only index that gives weights to eicosapentaenoic acid, docosahexaenoic acid, and PUFA consumption as independent components. Although the CHFP index also showed inverse associations with functional impairments, the estimated associations were generally not as strong as for the DASH or AHEI score. This might be explained by the main difference between CHFP and the other 2 indices: the recommendation of minimum grains consumption. For our study population, the majority of grains consumed were white rice, which has been shown to be detrimental in the food group analysis.
To our knowledge, our study is the largest longitudinal study to comprehensively assess the association between dietary patterns and physical/mental functioning among an elderly East Asian population. We have also included in our analyses a wide range of potential confounders to minimize confounding bias. Nevertheless, when interpreting our results, several limitations must be taken into account. First, we are relying on just 4 questions in the survey to capture the information on functional impairments. The item used to assess walking capability was from a validated measure of self-reported physical function, the RAND SF-36 scale (48). The other 3 questions were adopted from publications with unknown validation status. Second, the functional assessment was conducted only during the latest follow-up survey, meaning that we cannot completely rule out the possibility of reverse causation between our exposure and outcomes. However, this possibility is less likely because of the long interval between dietary assessment and the functional status assessment (average interval = 13.0 years, standard deviation = 2.7 years). Third, the results in Table 3 should be interpreted with some caution because multiple comparisons were not considered for the estimated odds ratio. When a Bonferroni-corrected P value threshold of 0.006 (0.05/8) was applied, the trend tests remained statistically significant for the associations of rice intake with cognitive function, poultry with walking ability and cognitive function, vegetables with decision-making, and fish and fruit with all 4 outcomes. Finally, hearing and vision were measured simultaneously in a single question, so that inferences cannot be made for each of them separately. Therefore, well-designed studies would be needed to validate our findings.
In conclusion, our study indicates that dietary intake plays an important role in the development of both physical and mental functional impairments among elderly Chinese. Greater compliance with either Chinese or US dietary recommendations; higher consumption of fish, poultry, vegetables and fruit; and moderate consumption of red meat may delay the onset or development of these aging-related impairments.
ACKNOWLEDGMENTS
Author affiliations: Vanderbilt Epidemiology Center, Division of Epidemiology, Department of Medicine, Vanderbilt-Ingram Cancer Center, Vanderbilt University Medical Center, Nashville, TN (Jingjing Zhu, Hui Cai, Wei Zheng, Xiao-Ou Shu); State Key Laboratory of Oncogenes and Related Genes, Shanghai Cancer Institute, Renji Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China (Yong-Bing Xiang, Honglan Li, Yu-Tang Gao); and Department of Epidemiology, Shanghai Cancer Institute, Renji Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China (Yong-Bing Xiang, Honglan Li, Yu-Tang Gao).
This work was supported by the US National Institutes of Health (grants UM1 CA182910 and UM1 CA173640).
We thank Nancy Kennedy for her assistance in editing and preparing the manuscript.
Conflict of interest: none declared.
Abbreviations
- AHEI
Alternative Healthy Eating Index
- CHFP
Chinese Food Pagoda
- CI
confidence interval
- DASH
Dietary Approaches to Stop Hypertension
- FFQ
food frequency questionnaire
- OR
odds ratio
- PUFA
polyunsaturated fatty acids
- SMHS
Shanghai Men’s Health Study
- SWHS
Shanghai Women’s Health Study
REFERENCES
- 1. United Nations, Department of Economic and Social Affairs, Population Division World Population Ageing 2013 New York, NY: United Nations; 2013. (Report no.: ST/ESA/SER.A/348). [Google Scholar]
- 2. Beard JR, Officer A, de Carvalho IA, et al. . The world report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Talegawkar SA, Bandinelli S, Bandeen-Roche K, et al. . A higher adherence to a Mediterranean-style diet is inversely associated with the development of frailty in community-dwelling elderly men and women. J Nutr. 2012;142(12):2161–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tsivgoulis G, Judd S, Letter AJ, et al. . Adherence to a Mediterranean diet and risk of incident cognitive impairment. Neurology. 2013;80(18):1684–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Féart C, Samieri C, Rondeau V, et al. . Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA. 2009;302(6):638–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zheng W, Chow WH, Yang G, et al. . The Shanghai Women’s Health Study: rationale, study design, and baseline characteristics. Am J Epidemiol. 2005;162(11):1123–1131. [DOI] [PubMed] [Google Scholar]
- 7. Shu XO, Li H, Yang G, et al. . Cohort profile: the Shanghai Men’s Health Study. Int J Epidemiol. 2015;44(3):810–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shu XO, Yang G, Jin F, et al. . Validity and reproducibility of the food frequency questionnaire used in the Shanghai Women’s Health Study. Eur J Clin Nutr. 2004;58:17–23. [DOI] [PubMed] [Google Scholar]
- 9. Villegas R, Yang G, Liu D, et al. . Validity and reproducibility of the food-frequency questionnaire used in the Shanghai Men’s Health Study. Br J Nutr. 2007;97(5):993–1000. [DOI] [PubMed] [Google Scholar]
- 10. Yu D, Zhang X, Xiang YB, et al. . Adherence to dietary guidelines and mortality: a report from prospective cohort studies of 134,000 Chinese adults in urban Shanghai. Am J Clin Nutr. 2014;100(2):693–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yu D, Shu XO, Li H, et al. . Dietary carbohydrates, refined grains, glycemic load, and risk of coronary heart disease in Chinese adults. Am J Epidemiol. 2013;178(10):1542–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li D, Yu D, Zhao L. Trend of sugar-sweetened beverage consumption and intake of added sugar in China nine provinces among adults [in Chinese]. Wei Sheng Yan Jiu. 2014;43(1):70–72. [PubMed] [Google Scholar]
- 13. Liu AD, Li JW, Liu ZP, et al. . Trans fatty acid levels in foods and intakes among population aged 3 years and above in Beijing and Guangzhou Cities, China. Biomed Environ Sci. 2015;28(7):477–485. [DOI] [PubMed] [Google Scholar]
- 14. Zhu J, Xiang YB, Cai H, et al. . Associations of obesity and weight change with physical and mental impairments in elderly Chinese people. Maturitas. 2018;108:77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Charlson ME, Pompei P, Ales KL, et al. . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 16. Lourida I, Soni M, Thompson-Coon J, et al. . Mediterranean diet, cognitive function, and dementia: a systematic review. Epidemiology. 2013;24(4):479–489. [DOI] [PubMed] [Google Scholar]
- 17. León-Muñoz LM, Guallar-Castillón P, López-García E, et al. . Mediterranean diet and risk of frailty in community-dwelling older adults. J Am Med Dir Assoc. 2014;15(12):899–903. [DOI] [PubMed] [Google Scholar]
- 18. Talegawkar SA, Bandinelli S, Bandeen-Roche K, et al. . A higher adherence to a Mediterranean-style diet is inversely associated with the development of frailty in community-dwelling elderly men and women. J Nutr. 2012;142(12):2161–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gopinath B, Schneider J, Flood VM, et al. . Association between diet quality with concurrent vision and hearing impairment in older adults. J Nutr Health Aging. 2014;18(3):251–256. [DOI] [PubMed] [Google Scholar]
- 20. Vercambre MN, Boutron-Ruault MC, Ritchie K, et al. . Long-term association of food and nutrient intakes with cognitive and functional decline: a 13-year follow-up study of elderly French women. Br J Nutr. 2009;102(3):419–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Beasley JM, LaCroix AZ, Neuhouser ML, et al. . Protein intake and incident frailty in the Women’s Health Initiative observational study. J Am Geriatr Soc. 2010;58(6):1063–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tsai HJ. Dietary patterns and cognitive decline in Taiwanese aged 65 years and older. Int J Geriatr Psychiatry. 2015;30(5):523–530. [DOI] [PubMed] [Google Scholar]
- 23. Young VR, Fajardo L, Murray E, et al. . Protein requirements of man: comparative nitrogen balance response within the submaintenance-to-maintenance range of intakes of wheat and beef proteins. J Nutr. 1975;105(5):534–542. [DOI] [PubMed] [Google Scholar]
- 24. Millward DJ, Fereday A, Gibson NR, et al. . Efficiency of utilization of wheat and milk protein in healthy adults and apparent lysine requirements determined by a single-meal [1-13C]leucine balance protocol. Am J Clin Nutr. 2002;76(6):1326–1334. [DOI] [PubMed] [Google Scholar]
- 25. Inoue G, Fujita Y, Niiyama Y. Studies on protein requirements of young men fed egg protein and rice protein with excess and maintenance energy intakes. J Nutr. 1973;103(12):1673–1687. [DOI] [PubMed] [Google Scholar]
- 26. Weiser MJ, Butt CM, Mohajeri MH. Docosahexaenoic acid and cognition throughout the lifespan. Nutrients. 2016;8(2):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Baum JI, Kim IY, Wolfe RR. Protein consumption and the elderly: what is the optimal level of intake? Nutrients. 2016;8(6):359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Beasley JM, LaCroix AZ, Neuhouser ML, et al. . Protein intake and incident frailty in the Women’s Health Initiative observational study. J Am Geriatr Soc. 2010;58(6):1063–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bartali B, Frongillo EA, Stipanuk MH, et al. . Protein intake and muscle strength in older persons: does inflammation matter? J Am Geriatr Soc. 2012;60(3):480–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. . Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fielding RA, Vellas B, Evans WJ, et al. . Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Boyle PA, Buchman AS, Wilson RS, et al. . Association of muscle strength with the risk of Alzheimer disease and the rate of cognitive decline in community-dwelling older persons. Arch Neurol. 2009;66(11):1339–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hsu YH, Liang CK, Chou MY, et al. . Association of cognitive impairment, depressive symptoms and sarcopenia among healthy older men in the veterans retirement community in southern Taiwan: a cross-sectional study. Geriatr Gerontol Int. 2014;14(suppl 1):102–108. [DOI] [PubMed] [Google Scholar]
- 34. Nourhashémi F, Andrieu S, Gillette-Guyonnet S, et al. . Is there a relationship between fat-free soft tissue mass and low cognitive function? Results from a study of 7,105 women. J Am Geriatr Soc. 2002;50(11):1796–1801. [DOI] [PubMed] [Google Scholar]
- 35. McCann JC, Ames BN. Is docosahexaenoic acid, an N-3 long-chain polyunsaturated fatty acid, required for development of normal brain function? An overview of evidence from cognitive and behavioral tests in humans and animals. Am J Clin Nutr. 2005;82(2):281–295. [DOI] [PubMed] [Google Scholar]
- 36. Wu A, Ying Z, Gomez-Pinilla F. Omega-3 fatty acids supplementation restores mechanisms that maintain brain homeostasis in traumatic brain injury. J Neurotrauma. 2007;24(10):1587–1595. [DOI] [PubMed] [Google Scholar]
- 37. Samieri C, Féart C, Proust-Lima C, et al. . Omega-3 fatty acids and cognitive decline: modulation by ApoEε4 allele and depression. Neurobiol Aging. 2011;32(12):2317.e13–e22. [DOI] [PubMed] [Google Scholar]
- 38. Vercambre MN, Boutron-Ruault MC, Ritchie K, et al. . Long-term association of food and nutrient intakes with cognitive and functional decline: a 13-year follow-up study of elderly French women. Br J Nutr. 2009;102(3):419–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Eskelinen MH, Ngandu T, Helkala EL, et al. . Fat intake at midlife and cognitive impairment later in life: a population-based CAIDE study. Int J Geriatr Psychiatry. 2008;23(7):741–747. [DOI] [PubMed] [Google Scholar]
- 40. Fairfield KM, Fletcher RH. Vitamins for chronic disease prevention in adults: scientific review. JAMA. 2002;287(23):3116–3126. [DOI] [PubMed] [Google Scholar]
- 41. Ames BN, Shigenaga MK, Hagen TM. Oxidants, antioxidants, and the degenerative diseases of aging. Proc Natl Acad Sci U S A. 1993;90(17):7915–7922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. High KP. Micronutrient supplementation and immune function in the elderly. Clin Infect Dis. 1999;28(4):717–722. [DOI] [PubMed] [Google Scholar]
- 43. Kim JY, Yang YJ, Yang YK, et al. . Diet quality scores and oxidative stress in Korean adults. Eur J Clin Nutr. 2011;65(12):1271–1278. [DOI] [PubMed] [Google Scholar]
- 44. Fung TT, McCullough ML, Newby PK, et al. . Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82(1):163–173. [DOI] [PubMed] [Google Scholar]
- 45. Jarrett SG, Boulton ME. Consequences of oxidative stress in age-related macular degeneration. Mol Aspects Med. 2012;33(4):399–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Seidman MD, Ahmad N, Joshi D, et al. . Age-related hearing loss and its association with reactive oxygen species and mitochondrial DNA damage. Acta Otolaryngol Suppl. 2004;(suppl 552):16–24. [DOI] [PubMed] [Google Scholar]
- 47. Lip PL, Blann AD, Hope-Ross M, et al. . Age-related macular degeneration is associated with increased vascular endothelial growth factor, hemorheology and endothelial dysfunction. Ophthalmology. 2001;108(4):705–710. [DOI] [PubMed] [Google Scholar]
- 48. Ware JE., Jr. SF-36 health survey update. Spine (Phila Pa 1976). 2000;25(24):3130–3139. [DOI] [PubMed] [Google Scholar]