Abstract
To increase teenagers’ nutrition knowledge is an important target and has the potential to improve their dietary habits and lifestyle while reducing incidences of obesity-related non-communicable diseases throughout the whole lifespan. This study protocol presents the general approach and details of an assessment of nutritional knowledge, attitudes toward nutrition, diet quality, lifestyle and body composition that have been used to comprehensively evaluate the cross-behavioral patterns covering dietary and lifestyle behaviors in Polish teenagers. The study was designed in two paths as: a cross-sectional study (covering 1569 students) and an education-based intervention study (464 students) with a 9-month follow-up. We describe a short form of the food frequency questionnaire (SF-FFQ4PolishChildren) used to collect data and details of diet-related and lifestyle-related education program, which was developed and implemented by academic researchers involved in the study. We also describe details of the data development and statistical analysis, including multidimensional methods of clustering variables to identify cross-behavioral patterns covering diet and lifestyle. The results of the study will provide evidence-based support for preventive health care to promote normal growth and development of young population and reduce the risk of diet-related diseases in adulthood, by early shaping of adequate dietary and lifestyle behaviors. In the future, well-tailored education programs addressed to teenagers can be created as an important public health action, based on our results.
Keywords: adolescents, dietary habits, education program, hand grip strength, nutrition knowledge, obesity, physical activity, public health intervention, sedentary lifestyle, three-factor eating questionnaire
1. Introduction
Overweight and obesity are among the most serious public health challenges of the 21st century [1,2,3]. The prevalence of childhood obesity is increasing in most regions of the world, in both developed and developing countries [4,5]. Recent studies suggest that these trends are gradually stabilizing or have already reached a plateau in some countries [6]; however, the problem remains significant [7,8]. According to the World Health Organization (WHO), in Europe in 2009–2010, on average, one in every three children aged six to nine years was overweight or obese, while among children aged 11 and 15 years the prevalence of overweight and obesity was 11–33% and 10–23%, respectively [9]. It is expected that if the current trend continues, there will be 20% or more obese children and adolescents in over 30 countries around the world in 2025 [3]. Among the European countries, Poland has one of the highest rates of prevalence of overweight in children and adolescents; 12–25% of Polish children and young people are overweight with a tendency toward an increase in the prevalence of both overweight and abdominal obesity [5,10,11,12,13].
Being overweight in early childhood has been shown to increase the chance of being obese in later childhood and also leads to adulthood obesity [2,7,11,14]. It is estimated that around 55% of obese children and 70% of obese adolescents will experience adult obesity [15], which increases their risk of obesity-related non-communicable diseases, such as diabetes, cardiovascular disease, various types of cancer, as well as premature mortality [16,17,18,19]. Therefore, prevention and treatment of childhood obesity is of the utmost importance, given the significant health and social consequences both in the short and long terms [20,21].
Obesity has a multi-factorial and multi-level etiology with many factors such genetic, physiological, environmental, and socioeconomic, including gender, family affluence, and education level [12,22,23,24]. Although genetic and biological factors are important, they cannot fully explain the current global childhood obesity trends. Environmental and societal factors associated with food intake and physical activity should be the primary focus for understanding the macro-level impact on obesity [5,9,11,24]. Rapid changes in ways of spending leisure time, a decline in physical activity, the pressure of peers, and the fashion of using electronic devices and almost unlimited access to food create an ”obesogenic” environment with two main factors affecting the positive energy balance and obesity—sedentary lifestyle and unhealthy diet [10,25,26,27,28]. Food marketing also plays a role by increasing children’s exposure to obesogenic foods because children and adolescents are more susceptible to food marketing than adults [29]. The availability of snack vending machines, bars, and kiosks with snack food and soft drinks in schools was also associated with lower fruits and vegetable consumption, higher intake of calories from total and saturated fat, and a higher body mass index (BMI) z-score [30,31].
As childhood obesity has a multi-factorial background, it should be tackled at multiple levels, including individual, household, school, and social [32,33]. Knowledge and beliefs related to health can improve health behaviours, especially when they are part of a targeted intervention, according to the Integrated Theory of Health Behaviour Change [34,35]. Improving nutrition knowledge can be assumed to contribute to the enhancement of dietary habits and food choices in those exposed to education-based intervention [32,33,36].
Since poor dietary habits tend to be carried over from childhood to adulthood [37], childhood and adolescence are periods when good nutritional diet quality is important to establish healthy dietary behaviours. The family environment is a well-known factor influencing the food consumption of children, especially in the early years of life. The influence of peer environment, mass-media, celebrities and schools (due to school nutrition programs) increases rapidly during adolescence [38]. In this period, an awareness of one’s own sexuality and gender differences with regard to diet and health as well as physical abilities arise. The precise indication of the age at which changes start in the perception of oneself as an independent individual and food consumer is difficult, but the age of 10 (12) years old (depending on gender) is considered a breakthrough [39]. Thus, early adolescence may be the last moment for implementing sustained healthy school culture and nutrition education addressed to young people before determining their relatively stable eating habits.
Schools are considered a primary setting for implementing education programs—they have the unique potential of involving a wide population of children and teenagers. A health education curriculum that highlights the importance of nutrition and physical activity can help students adopt and maintain healthy lifestyles regarding eating and physical activity [40,41]. Across the world, there is a wide range of nutrition education initiatives addressed to school children, with the participation of schools, government and health promotion agencies delivering knowledge about diet components [42] and specific education to prevent or manage dietary-related and lifestyle-related diseases.
In Poland, multi-disciplinary programs covering the implementation of multi-component activities are mainly directed at preschool children (e.g., ToyBox-study, Program Eating Healthy, Growing Healthy) [43,44,45]. While programs conducted in schools are focused on single topics, e.g., culinary workshops, nutrition education classes or physical activity education (POL-HEALTH; “Zachowaj Równowagę”), there is a lack of a comprehensive approach with well-documented scientific research [46,47,48]. There have been relatively few comprehensive educational programs in Poland, which have been combined with a scientific assessment of nutrition knowledge, dietary habits and lifestyle. Therefore, our project is aimed at filling the gap, with the potential that our research conducted on Polish teenagers can be interpreted in a wider scope for other European teenagers living in similar conditions.
The aim of the current paper is to describe the design, methodology and approach of the study which was based on “ABC of Healthy Eating” project, and also to present the overall characteristics of the study sample as assessed at baseline, prior to the implementation of a diet-related and lifestyle-related education program.
1.1. Research Objective and Hypothesis
Our study is focused on teenagers aged 11–13 years, taking into account that early adolescence may be the last moment for implementing nutrition-related and lifestyle-related education before determining their relatively stable habits. We hypothesized that education focused on improving teenagers’ dietary and lifestyle behaviours can increase the level of nutrition knowledge and positively influence attitudes toward nutrition, dietary behaviours, lifestyle, and body composition. It was assumed that education should be multi-component and use various forms of education tailored to teenagers’ needs and their perceptions. However, the education effect can decrease over time and the rate of this change depends on the initial level of nutrition knowledge and socio-demographic factors.
There were two aims of the study:
To assess the short- and medium-term effect of nutrition-related and lifestyle-related education program on nutrition knowledge, attitudes toward nutrition, diet quality, lifestyle, and body composition of Polish teenagers in a socio-demographic context.
To determine the association between teenagers’ nutrition knowledge, attitudes toward nutrition, dietary and lifestyle behaviours, body composition, and socio-demographic factors.
1.2. Study Design
Data related to the study were collected as a part of:
A national multicenter “ABC of Healthy Eating” project—the 1st edition in 2015–2016 (“ABC of Healthy Nutrition”) and the 2nd edition in 2016 (“ABC of Kids’ Nutrition”) (Figure S1).
The own research of academic centers involved in the study, carried out in parallel with those two editions of the project.
The study had a wider scope and went beyond the activities carried out under the “ABC of Healthy Eating” project.
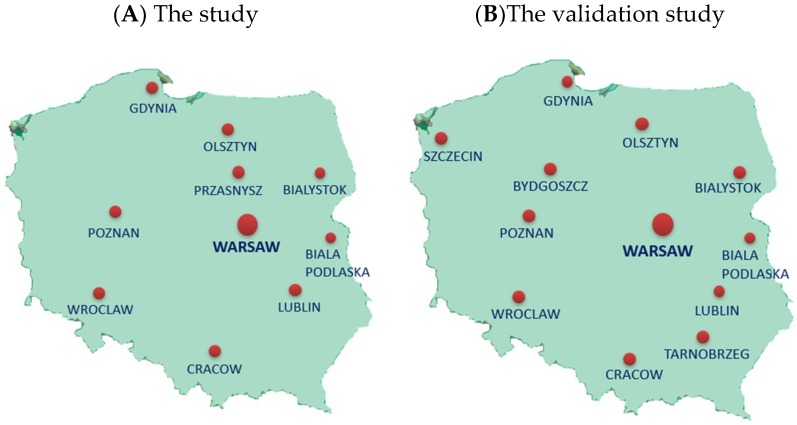
The study was carried out on students of selected elementary schools from urban, sub-urban, and rural areas covering the entire territory of Poland. The schools (not randomly selected) were located a convenient distance from nine Polish universities in ten locations. In 2015–2016, the study was carried out in schools located near following cities: Gdynia, Cracow, Lublin, Olsztyn, Poznan, Przasnysz, Warsaw, Wroclaw, and in 2016, in schools located near: Biala Podlaska, Bialystok, Gdynia, Cracow, Lublin, Olsztyn, Warsaw, and Wroclaw (Figure 1A).
Figure 1.
The location of academic centers involved in the study (A) or the validation study (B). A: Universities (cities) involved in the study: Warsaw University of Life Sciences, WULS-SGGW (Warsaw, Przasnysz); Gdynia Maritime University (Gdynia); Medical University in Bialystok (Bialystok); Josef Pilsudski University of Physical Education in Warsaw—The branch in Biala Podlaskiej (Biala Podlaska); University of Agriculture in Krakow (Cracow); University of Life Sciences in Lublin (Lublin); University of Life Sciences in Poznan (Poznan); University of Warmia and Mazury in Olsztyn (Olsztyn); Wroclaw University of Environmental and Life Sciences (Wroclaw). B: Universities (cities) involved in the validation study: Warsaw University of Life Sciences, WULS-SGGW (Warsaw, Tarnobrzeg); Gdynia Maritime University (Gdynia); Medical University in Bialystok (Bialystok); Josef Pilsudski University of Physical Education in Warsaw—The branch in Biala Podlaskiej (Biala Podlaska); University of Agriculture in Krakow (Cracow); University of Life Sciences in Lublin (Lublin); University of Life Sciences in Poznan (Poznan); University of Warmia and Mazury in Olsztyn (Olsztyn); Wroclaw University of Environmental and Life Sciences (Wroclaw); University of Economy (Bydgoszcz); West Pomeranian University of Technology (Szczecin).
In April–May 2015 the research concept and a short form of the food frequency questionnaire (SF-FFQ4PolishChildren) dedicated to school children were developed. The main study was preceded by pilot studies (in May 2015) in which the research procedure and tools were verified in all centers, covering the 200 subjects above. Data collection for the main study started in June 2015. The data were collected and measurements were taken by well-trained researchers. The study started at the same time in all centers involved in the study.
The study was carried out in two paths: as an education-based intervention design and a cross-sectional design. The study is reported according to the guidelines of reporting of observational and intervention studies of public health in nutritional epidemiology [49,50,51].
1.3. The Education-Based Intervention Study
Two groups were established: under intervention (educated group) and without intervention (control group) by accidental allocation of school classes to the educated or control group. In the educated group, a diet-related and lifestyle-related education program lasting three weeks was implemented. The program consisted of 5 topics, each topic included various forms of education from fun to “scientific” cognition (Table 1). Each topic lasted approx. 180 min (4 h of school lessons) and was run by a minimum of 3–4 researchers. The program was developed and implemented by academic researchers involved in the study. School teachers were not involved in the education program, they were only present during educational activities. Apart from the study, students from both educated and control groups took part in regular school activities containing some content related to nutrition and a healthy lifestyle.
Table 1.
Topics and details of the education program.
| Nutrition Topic | |
| Goal | Shaping pro-healthy dietary habits. |
| Scope | Nutrients important in the diet of young people. Health consequences of uncontrolled consumption of energy drinks and dietary supplements. A “Good snack” as an alternative to chips, sticks and sweets. A Pyramid of Healthy Nutrition and Physical Activity [52] and dietary guidelines for teenagers. |
| Methods | Talk; discussion; workshops. |
| Activities | Participants propose three various “healthy” breakfasts to take at school by selecting foods from a levels of the Pyramid of Healthy Nutrition and Physical Activity; Participants prepare an “ideal sandwich”. |
| Tools | Brochure; puzzles; crosswords; website. |
| Dietary topic | |
| Goal | Supporting well-being, physical, and intellectual development through a healthy lifestyle. |
| Scope | General recommendations for a healthy lifestyle (healthy eating and physical activity) at school age. The influence of nutrition and physical activity on physical and intellectual development and healthy well-being. The Student Menu—The brain cannot live only on chocolate—A discussion on the most important nutrients in the diet of young people. |
| Methods | Talk; discussion; workshops. |
| Activities | Using a pedometer to measure the number of calories consumed during the various activities. Determination of time needed to “burn” the calories contained in the selected product. “Nutrition detective”—measuring the amounts of oil, sugar and salt corresponding to fat, sucrose and salt content in various foods (three sets). |
| Tools | Brochure; puzzles; crosswords; website. |
| Sensory-consumer topic | |
| Goal | The world of senses. How to read the food labels? What is important when choosing food? |
| Scope | Recognition of the basic flavors in aqueous solutions. Discovering the different taste sensations in selected foods. “What kind of a consumer am I”—what do I like and why? Qualification of the consumer’s personality. |
| Methods | Talk; discussion; workshops. |
| Activities | Use of sensory memory to identify eight coded odor samples of natural spices, vegetables and fruits. Recognition of selected foods with masked/closed eyes, based on sensory perceptions in the mouth. Preparation of colorful, tasty and healthy snacks from provided foods according to one’s own ideas. |
| Tools | Brochure; recipes of ‘healthy’ snacks; website. |
| Hygiene topic | |
| Goal | Food safety. Hygiene during the preparation and consuming of meals. |
| Scope | The world of microorganisms, pathogens and probiotics. The rules of proper food storage and hygiene during meal preparation and consumption. |
| Methods | Talk; discussion; workshops. |
| Activities | Microscopic observation of selected microorganisms—Lactic acid bacteria (Lactobacillus) as an example of a microorganism with healthy properties, E. coli (Escherichia coli) as an example of a pathogen. Mapping the observed microorganisms’ cells in the prepared templates. Practicing proper hand washing according to instructions. Checking hand cleanness with a test indicator, before and after hand washing. |
| Tools | Brochure; microscope; test indicator of hand washing; puzzles; crosswords; website. |
| Culinary topic | |
| Goal | How to prepare healthy, cheap and tasty meals? |
| Scope | The impact of culinary processes on sensory quality, nutritional value and food safety. The phenomenon of enzymatic browning of fruit and vegetables and ways to prevent this process. |
| Methods | Talk; discussion; workshops. |
| Activities | Culinary experiments—preventing the darkening of fruits and vegetables. Checking the impact of storage temperature on the quality of frozen foods, e.g., vegetables. Preparing low-budget healthy meals and low-sweetened beverages. |
| Tools | A “healthy meals” recipe book; brochure; website. |
The overall content of the intervention-based educational study is presented in Table 2. The data was collected 4 times: (i) before education (at baseline), (ii) 3 weeks from baseline at the end of the education program (in the educated group only), (iii) after 3 months (±2 weeks; 3-month follow-up) to measure the short-term effect of education, (iv) after 9 months (±2 weeks; 9-month follow-up) to measure the medium-term effect of education.
Table 2.
The overall content of the education-based intervention study.
| Timing | Activities | Group | |
|---|---|---|---|
| Educated | Control | ||
| June 2015 Before education (Baseline) |
|
A | A |
|
A | A | |
| June 2015 Education program (lasting 3 weeks) |
|
A | NA |
| June 2015 After education (3 weeks from baseline) |
|
A | NA |
| September 2015 After 3 months from baseline (3-month follow-up) |
|
A | A |
| March 2016 After 9 months from baseline (9-month follow-up) |
|
A | A |
|
A | A | |
SF-FQ4PolishChildren—A short form of food frequency questionnaire; A—applied; NA—not applied.
1.4. The Cross-Sectional Study
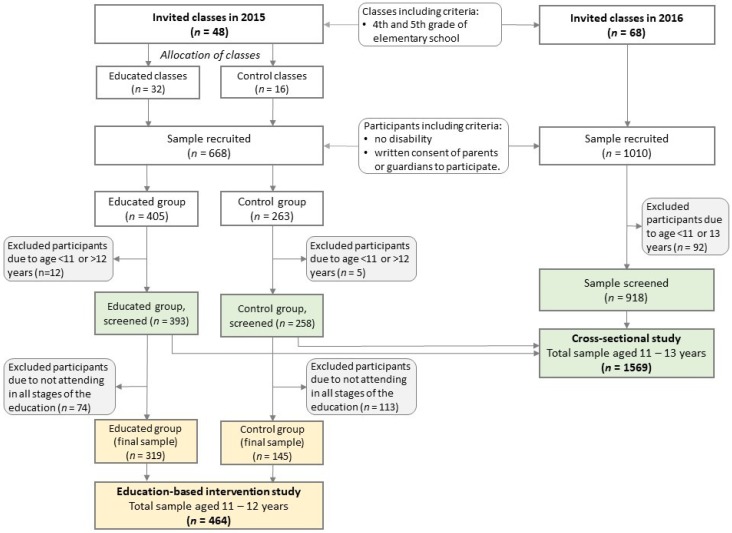
In this study design, pooled data were used (see Figure 2 in Section 2.2) covering the data collected in June 2015 within the intervention-based educational study and June 2016 within the 2nd edition of the project ‘ABC of Kids’ Nutrition’ (Table 3). In this database, all data were collected before education program in those participants who have been subjected to the education, i.e., all participants from educated group in 2015 (at baseline) and all participants in 2016. In the 2nd edition of the project, no effect of education was measured and no control group was established.
Figure 2.
Flow chart of sample collection and study design.
Table 3.
The overall content of the cross-sectional study.
| Timing | Activities | Group | |
|---|---|---|---|
| Educated | Control | ||
| June 2015 Before education |
|
A | A |
|
A | A | |
| June 2016 Before education |
|
A | NA |
|
A | NA | |
A—applied; NA—not applied.
2. Materials and Methods
2.1. Ethical Aspects
The project followed the ethical standards recognized by the Declaration of Helsinki and was approved by the Bioethics Committee of the Faculty of Medical Sciences, University of Warmia and Mazury in Olsztyn on 17 June 2010, Resolution No. 20/2010. The study was explained to the participants before the start (verbally and by leaflets), to the pupils at the school lessons and to the parents or legal guardians during the meetings. Parental or legal guardians’ written informed consent was obtained for the participation of their children. The consent form was distributed for parents or legal guardians during the meetings. All data regarding the study were collected at the time designated for school classes instead of regular school lessons. Participants who refused to participate in the study attended other school activities.
2.2. Participant Selection
A convenient sample selection was applied in both the education-based intervention study and the cross-sectional study. A school class was the smallest unit in the sample selection. All students from a given class were invited to take part in the study. Recruitment was conducted in selected elementary schools (see in Section 1.2). Table 4 presents the criteria of schools and participants’ inclusion or exclusion.
Table 4.
School and participant eligibility criteria.
School inclusion criteria:
|
Participant inclusion criteria—in general:
|
Participant exclusion criteria—for the education-based intervention study:
|
Participant exclusion criteria—for the cross-sectional study:
|
Students from 4th- and 5th-grade classes were invited to attend. The expected ages of the students were 11–12 years in 2015 and 11–13 years in 2016 due to changes in the Polish law concerning the age of starting education by children (obligatory or optional starting from six years). We decided to start recruitment based on school classes because students were subject to the same school education and would be at a similar stage of development. In 2015, 48 classes were invited (educated group/control group: 32/16 classes) and in 2016, 68 classes were invited (Figure 2).
In the education-based intervention study, 668 students (educated/control: 405/263) were initially recruited. Due to age (12/5) or not attending all stages of the study (74/113), 208 participants were excluded from the analyses. Finally, the study included 464 teenagers (319/145) with a baseline age of 11–12 years, including 216 boys (46.6%) and 248 girls (53.4%).
In the cross-sectional study, 1,678 students were initially recruited. Due to age (in 2015/in 2016: 17/92), 109 participants were excluded from analyses. Finally, the study included 1569 teenagers aged 11–13 years, 760 boys (48.4%) and 809 girls (51.6%).
2.3. Questionnaire for Data Collection
Data related to nutrition knowledge, attitudes toward nutrition, diet, lifestyle and socio-demographic factors were collected with 50-item, a short form of food frequency questionnaire (SF-FFQ4PolishChildren) developed by Kowalkowska, Wadolowska, and Hamulka for the “ABC of Healthy Eating” project (Tables S1 and S2).
A validation procedure of the short form of food frequency questionnaire (FFQ) was carried out, regardless of this study, in cooperation with academic researchers from 12 universities covering the entire territory of Poland (data not published, paper in preparation) (Figure 1B). In brief, the internal compatibility of the questionnaire was tested by 630 teenagers, aged 11–15. The questionnaire was completed by teenagers twice (test and retest after 2 weeks). Fleiss’ Kappa for breakfast consumption was 0.54, school meal consumption was 0.53, pro-Healthy Diet Index categories (see in this section below) was 0.44 and the non-Healthy Diet Index categories was 0.35, Family Affluence Scale items were 0.69 to 0.83, nutrition knowledge level was 0.36, screen time categories was 0.46 and physical activity level was 0.52. Compatible classification of subjects (into the same category in test and retest) was for breakfast, 77.3%; school meal, 79.8%; pro-Healthy Diet Index, 75.8%; non-Healthy Diet Index, 92.0%; Family Affluence Scale items, 83.7% to 95.8%; nutrition knowledge level, 72.7%; screen time, 64.8%; total physical activity level, 74.8%. The internal compatibility of the short form of FFQ dedicated for teenagers was considered acceptable to good.
2.4. Nutrition Knowledge
The nutrition knowledge level was determined based on eighteen questions (Q22 to Q39; Table S1). Participants were asked about nutrition based on questions developed by Whati [53] and adapted to Polish conditions and education based on the Polish Food Guide Pyramid [52]. Correct answers were scored with 1 point and wrong or “don’t know” answers and missing data were scored with 0 points. Points were summed up for each respondent. Based on tertile distribution (data from the cross-sectional study), the respondents were divided into three nutritional knowledge levels labeled as follows: the lowest (0–4 points), moderately low (5–7 points), and higher (8–18 points).
2.5. Attitudes toward Nutrition
Based on a three-factor eating questionnaire (TFEQ13), dedicated to children, attitudes toward nutrition were determined. The questionnaire was adapted and validated to the Polish conditions by Dzielska et al. [54]. Originally, TFEQ13 consisted of 13 statements, but a weak understanding of three statements was found during pilot studies. Therefore, we used a shorter version of the questionnaire (TFEQ10) comprising 10 statements (Q12 to Q21; Table S1. According to Dzielska et al. [54], three subscales, in shortened version, were developed: Emotional Eating (Q12, Q14), Uncontrolled Eating (Q13, Q15, Q16, Q17, Q20), and Cognitive Restraint of Eating (Q18, Q19, Q21). The scores of each subscale were calculated as a sum of points assigned to answers given by respondent. Answers were scored as follows (points):
Q12 to Q20: respondents could choose one of four answers: “definitely yes” (3 points), “rather yes” (2 points), “rather not” (1 point), “definitely not” (0 points),
Q21: respondents could choose one of eight points on the graphical scale: 1 or 2 (0 points), 3 or 4 (1 point), 5 or 6 with (2 points), 7 or 8 (3 points).
2.6. Diet Quality
The questionnaire was self-administered by teenagers in the classroom and supervised by well-trained researchers. Explanations were given if necessary. The completion of the questionnaire took the teenagers approx. 40 min.
Respondents were asked to specify their usual frequency consumption within the last 12 months for breakfast and school meal and nine food items such as dairy products (e.g., milk, yogurt, cottage cheese, cheese), fish (e.g., baked, smoked, fried, in vinegar, canned), vegetables (e.g., fresh, boiled, baked, stewed), fruit (fresh or frozen), fruit or mixed fruit-veggie juices, fast foods (e.g., chips, pizza, hamburgers), sweetened carbonated drinks (e.g., cola-type, water with syrup, tea-type with sugar), energy drinks, sweets or confectionery (e.g., cookies, sweets, cake, chocolate bars, chocolate).
Breakfast was considered as consuming solid foods with or without beverages at the first eating episode of a day [55,56]. Drinking only beverages was not considered as breakfast. Respondents could choose one from four categories of breakfast consumption (number of days/week): 0/week, 1–3/week, 4–6/week, and 7/week. Some categories have been combined after distribution analysis. Finally, breakfast consumption was analyzed in three categories as follows: every day (7/week), irregular (4–6/week), and skipping (0–3/week).
The school meal was considered as consuming solid foods with or without beverages at the second eating episode of a day while at school as lunch or a so-called second breakfast (more typical in Poland). Drinking beverages only was not considered as a school meal. Respondents could choose one from four categories of school meal consumption (number of days/week): 0/week, 1–2/week, 3–4/week, and 5/week. Some categories were combined after distribution analysis. Finally, school meal consumption was considered in three categories as follows: every day (5/week), irregular (3–4/week), and skipping (0–2/week).
Breakfast and school meal consumption considered together were analyzed in three categories as follows: every day (breakfast: 7/week; school meal: 5/week), skipping (breakfast: 0–3/week; school meal: 0–2/week), and irregular (other frequencies).
For food frequency consumption, respondents could choose one from the following seven categories (converted into daily frequency, times/day): never or almost never (0 times/day), less than once a week (0.06 times/day), once a week (0.14 times/day), 2–4 times/week (0.43 times/day), 5–6 times/week (0.79 times/day), every day (1 time/day), and several times a day (2 times/day).
Two diet quality scores were used as follows: a pro-Healthy Diet Index (pHDI) and a non-Healthy Diet Index (nHDI). Both diet quality scores were established (a priori approach) on the basis of usual food frequency consumption within the 12 last months. The pHDI included four food items as follows: dairy products, fish, vegetables and fruit; the nHDI included four food items as follows: fast foods, sweetened carbonated drinks, energy drinks and sweets or confectionery. Diet quality scores were calculated by summing up the daily frequencies of four food items (as mentioned above) and expressed in % points (range: 0 to 100). Two various ideas in categorizing diet quality scores (based on data from the cross-sectional study) were applied:
- A posteriori approach—three levels of each diet quality score based on tertile distribution:
- pHDI: bottom tertile (<20.625% points), middle tertile (20.625–32.125% points), upper tertile (≥32.125% points).
- nHDI: bottom tertile (<7.875% points), middle tertile (7.875–16.000% points), upper tertile (≥16.000% points).
A priori approach—three levels of each diet quality score: low (<33.33% points), moderate (33.33–66.66% points), and high (≥66.66% points).
2.7. Lifestyle
Four measures were applied to assess lifestyle: screen time, total physical activity, physical activity at school, and leisure time.
Using the question “How much time do you spend watching TV or in front of a computer on an average day of the week?” (Q48; Table S1), screen time (ST) was assessed. The respondents could choose one of six answers (with assigned scores): <2 h/day (0 points), 2 to <4 h/day (1 point), 4 to <6 h/day (2 points), 6 to <8 h/day (3 points), 8 to <10 h/day (4 points), and ≥10 h/day (5 points). Screen time expressed in points was calculated for each participant. The recommendation of the American Academy of Pediatrics of a maximum of two hours of ST per day for children and youth was used as a reference [57]. Three categories of screen time were established after combining some answers: <2 h/day, 2 to 4 h/day, and ≥4 h/day.
Total physical activity (PA) was assessed using two questions regarding physical activity at school and leisure time (Q49–Q50; Table S1). The respondents could choose one of three answers describing their physical activity at school (low, moderate, vigorous) and leisure time (low, moderate, vigorous). Many examples for each answer were given. Finally, after combining some categories of both questions, the respondents were divided into three total physical activity levels: low, moderate and high, with assigned scores from 0 point to 5 points (Table 5). Total PA expressed in points for each participant was calculated. Vigorous PA at school combined with vigorous PA at leisure time (scored with 5 points) was considered as adherence to the World Health Organization recommendation on physical activity [58]. The WHO recommends that children and adolescents aged 5–17 years have a minimum of 2.5 h/day of moderate-intensity PA. Finally, two categories of total physical activity were considered: with the adherence to WHO recommendation on physical activity or no adherence.
Table 5.
Categorizing and scoring (points) of total physical activity based on physical activity at school and leisure time.
| Physical Activity at School | Physical Activity at Leisure Time | ||
|---|---|---|---|
| Low | Moderate | Vigorous | |
| Low | Low (0) | Low (1) | Moderate (2) |
| Moderate | Low (1) | Moderate (3) | Moderate (4) |
| Vigorous | Moderate (2) | Moderate (4) | High (5) Adherence to WHO recommendation |
Notes: Physical activity at school: low (most of the time in a sitting position, in class or on breaks), moderate (half the time in a sitting position and half the time in motion), vigorous (most of the time on the move or on classes related to high physical exertion). Physical activity at leisure time: low (more time spent sitting, watching TV, in front of a computer, reading, light housework, a short walk to 2 h a week), moderate (walking, cycling, gymnastics, working at home or other light physical activity performed 2–3 h/week), vigorous (cycling, running, working at home or other sports activities requiring physical effort over 3 h/week).
2.8. Body Composition
The measurements of body weight (kg), height (cm), waist circumference (WC, cm), and hand grip strength (HGS, kg) were taken with a precision of 0.1 kg, 0.1 cm, 0.1 cm, or 0.5 kg, respectively, (between 8 and 12 a.m.) according to the ISAK International Standards for Anthropometric Assessment guidelines [59]. Professional equipment and measuring tape were used, the same type across all the research centers. Table 6 presents the details relating to procedures for body composition measurements. Body mass index (BMI, kg/m2) and waist-to-height ratio (WHtR) were calculated. Body mass index was categorized according to age-sex-specific BMI cut-offs for teenagers [60]. A BMI ≥25 kg/m2 was used as the overweight measure (general adiposity) and WHtR ≥0.5 as the central obesity measure (central adiposity) [61]. Z-scores of WC, BMI, and WHtR as well as HGS were calculated to achieve mean equal 0 and standard deviation (SD) equal 1. Z-scores were categorized as follows: <−1, −1 to 1 and >1 SD.
Table 6.
Procedures for body composition measurements.
| Parameter (Units) | Procedure, Accuracy, and Equipment |
|---|---|
| Height (H) (cm) |
|
| Body weight (BW) (kg) |
|
| Waist circumference (WC) (cm) |
|
| Hand grip strength (HGS) (kg) |
|
2.9. Socio-Demographic Data
Respondents were divided into two categories of residence (rural or urban), based on question Q43 (Table S1. The socioeconomic status was determined by using the Family Affluence Scale (FAS). The FAS was a measure of material affluence derived from the characteristics of the household. The scale was developed for the Health Behavior of School-aged Children (HBSC) cross-national study including 44 countries. We used a scale composed of four questions described by the Polish HBSC study team [62]. For each answer, points were assigned (Table S1). Some of the answers were scored with the same number of points.
Q44: “Does your family own a car, van or truck?” Answers: no (0 points); yes, one (1 point); yes, two or more (2 points).
Q45: “During the past year, how many times did you travel away on holiday with your family?” (necessary examples were given) Answers: not at all (0 points); once (1 point); twice (2 points); more than twice (2 points).
Q46: “Do you have your own bedroom for yourself?” Answers: no (0 points); yes (1 point).
Q47: “How many computers, laptops or tablets do your family own?” Answers: none (0 points); one (1 point); two (2 points); more than two (2 points).
The points were summed up for each respondent (range: 0 to 7). Based on quartile distribution, the respondents were divided into three FAS categories labeled as: low (0–4 points; <25th quartiles), moderate (5–6 points) and high (7 points; ≥75th quartiles).
2.10. Sample Size Calculation
Two calculations of minimum sample size were made separately for two study designs.
For the education-based intervention study, the minimum sample size was calculated in regards to nutrition knowledge as a key measure of the study. The calculation was based on the expected increase in nutrition knowledge score after the 9-month follow-up and the expected difference between the educated and control groups. With 5% significance level and 80% power, the sample size required approximately 304 respondents (assuming 2/1 ratio for educated/control group, i.e., 200/104 respondents and an equal number of respondents in each research center) at the end of the study, to detect a 50% difference between the educated group (increase by 30%) and the control group (increase by 15%) in the increase of nutrition knowledge score, including a 50% drop out rate (at the end of the study) and recoding error or missing data of 10%.
For the cross-sectional study, the minimum sample size was calculated in regards to consuming breakfast, which we chose as a key dietary habit and overweight occurrence. The calculation was based on the expected proportion of respondents not consuming breakfast every day (25%) and the difference in overweight occurrence between respondents consuming and not consuming breakfast every day (20% vs. 30%, respectively). With a 5% significance level and 80% power, the minimum sample size required is approximately 904 respondents (assuming a 75/25 ratio for respondents consuming and not consuming breakfast every day, i.e., 678/226 and an equal number of respondents in each research center) to detect a difference between groups in overweight occurrence, including recoding error or missing data of 10%.
2.11. Statistical Analysis
Categorical variables are presented as a sample percentage (%), and continuous variables as means with 95% confidence interval (95% confidence interval (CI)) or medians with inter-quartile range for variables with normal or non-normal distribution, respectively. The normality of variables distribution was verified with Kolmogorov-Smirnov test before the statistical analysis. Table 7 presents the general characteristics of the sample across all key variables under study.
Table 7.
Sample characteristics by study design (% or means (95% confidence interval)).
| Parameters | Education-Based Intervention Study (At Baseline) | Cross-Sectional Study | ||||
|---|---|---|---|---|---|---|
| Total Sample | Boys | Girls | Total Sample | Boys | Girls | |
| Sample size | 464 | 216 | 248 | 1569 | 760 | 809 |
| Sample percentage | 100.0 | 46.6 | 53.4 | 100.0 | 48.4 | 51.6 |
| Age (years) | 11.9 (11.9, 12.0) | 11.9 (11.9, 12.0) | 11.9 (11.9, 11.9) | 11.9 (11.9, 12.0) | 11.9 (11.9, 12.0) | 11.9 (11.9, 12.0) |
| Age (categories) | ||||||
| 11 years | 7.1 | 5.1 | 8.9 | 16.6 | 15.3 | 17.9 |
| 12 years | 92.9 | 94.9 | 91.1 | 73.6 | 75.9 | 71.3 |
| 13 years | 0.0 | 0.0 | 0.0 | 9.8 | 8.8 | 10.8 |
| Residence | ||||||
| rural | 34.9 | 36.1 | 33.9 | 40.3 | 40.3 | 40.3 |
| urban | 65.1 | 63.9 | 66.1 | 59.7 | 59.7 | 59.7 |
| Family Affluence Scale (points) | 5.3 (5.1, 5.5) | 5.2 (4.9, 5.4) | 5.4 (5.2, 5.6) | 5.4 (5.3, 5.4) | 5.3 (5.2, 5.4) | 5.4 (5.3, 5.5) |
| Nutrition knowledge | ||||||
| Nutrition knowledge score (points) | 6.0 (5.7, 6.2) | 5.5 (5.2, 5.9) | 6.3 (6.0, 6.7) | 6.1 (5.9, 6.2) | 5.7 (5.5, 5.9) | 6.5 (6.3, 6.6) |
| Nutrition knowledge (categories) | ||||||
| the lowest | 30.6 | 35.6 | 26.2 | 30.9 | 35.7 | 26.3 |
| moderately low | 41.4 | 42.1 | 40.7 | 39.3 | 40.1 | 38.6 |
| higher | 28.0 | 22.2 | 33.1 | 29.8 | 24.2 | 35.1 |
| Attitudes toward nutrition | ||||||
| Emotional Eating (points) | 1.3 (1.2, 1.5) | 1.3 (1.1, 1.5) | 1.4 (1.2, 1.5) | 1.3 (1.3, 1.4) | 1.3 (1.2, 1.3) | 1.4 (1.3, 1.5) |
| Uncontrolled Eating (points) | 5.3 (5.0, 5.5) | 5.5 (5.1, 5.9) | 5.1 (4.8, 5.4) | 5.3 (5.2, 5.4) | 5.3 (5.1, 5.5) | 5.3 (5.1, 5.5) |
| Cognitive Restraint of Eating (points) | 4.2 (4.0, 4.4) | 4.0 (3.7, 4.3) | 4.3 (4.1, 4.6) | 4.3 (4.2, 4.4) | 4.3 (4.1, 4.4) | 4.4 (4.2, 4.5) |
| Diet quality | ||||||
| Every day consumption of | ||||||
| breakfast | 71.0 | 70.7 | 71.3 | 70.0 | 72.7 | 67.4 |
| school meal | 67.5 | 59.8 | 74.2 | 69.0 | 64.7 | 72.9 |
| pHDI (% points) | 27.7 (26.4, 29.0) | 24.4 (22.8, 26.1) | 30.5 (28.6, 32.4) | 28.4 (27.7, 29.1) | 27.4 (26.3, 28.4) | 29.4 (28.4, 30.4) |
| pHDI (categories) | ||||||
| low | 71.0 | 81.8 | 61.7 | 69.2 | 72.9 | 65.8 |
| moderate | 28.6 | 17.8 | 37.9 | 29.8 | 25.9 | 33.5 |
| high | 0.4 | 0.5 | 0.4 | 1.0 | 1.2 | 0.7 |
| nHDI (% points) | 14.3 (13.3, 15.3) | 15.1 (13.8, 16.4) | 13.6 (12.2, 15.1) | 14.1 (13.5, 14.7) | 15.0 (14.1, 15.9) | 13.3 (12.5, 14.0) |
| nHDI (categories) | ||||||
| low | 93.9 | 94.0 | 92.7 | 93.8 | 93.8 | 93.8 |
| moderate | 6.7 | 6.0 | 7.3 | 5.9 | 5.5 | 6.2 |
| high | 0.0 | 0.0 | 0.0 | 0.3 | 0.7 | 0.0 |
| Lifestyle | ||||||
| Screen time (points) | 0.84 (0.74, 0.94) | 0.91 (0.76, 1.06) | 0.78 (0.65, 0.91) | 0.86 (0.81, 0.92) | 0.98 (0.89, 1.06) | 0.76 (0.69, 0.82) |
| Screen time (categories) | ||||||
| <2 h/day | 46.5 | 41.1 | 51.2 | 46.3 | 42.1 | 50.3 |
| 2 to 4 h/day | 34.7 | 40.7 | 29.4 | 34.4 | 35.2 | 33.6 |
| ≥4 h/day | 18.8 | 18.2 | 19.4 | 19.3 | 22.7 | 16.1 |
| Total physical activity (points) | 3.65 (3.53, 3.78) | 3.66 (3.48, 3.85) | 3.65 (3.49, 3.81) | 3.68 (3.61, 3.74) | 3.73 (3.63, 3.82) | 3.63 (3.54, 3.71) |
| Total physical activity (categories) | ||||||
| low | 12.3 | 13.4 | 11.3 | 9.8 | 10.0 | 9.5 |
| moderate | 54.6 | 49.5 | 59.1 | 58.9 | 53.3 | 58.9 |
| high | 33.0 | 37.0 | 29.6 | 31.3 | 36.7 | 26.3 |
| Body composition | ||||||
| Waist circumference (cm) | 64.4 (63.5, 65.3) | 65.7 (64.3, 67.0) | 63.3 (62.2, 64.5) | 66.1 (65.6, 66.5) | 67.8 (67.1, 68.6) | 64.4 (63.8, 65.0) |
| z-Waist circumference >1 SD | 13.5 | 18.5 | 9.2 | 15.1 | 20.1 | 10.4 |
| WHtR | 0.42 (0.42, 0.43) | 0.43 (0.42, 0.44) | 0.42 (0.41, 0.42) | 0.43 (0.43, 0.43) | 0.44 (0.44, 0.45) | 0.42 (0.42, 0.42) |
| Central obesity a | 10.0 | 11.4 | 8.8 | 12.2 | 15.9 | 8.7 |
| BMI (kg/m2) | 19.6 (19.2, 19.9) | 19.7 (19.1, 20.2) | 19.5 (19.0, 20.0) | 19.4 (19.2, 19.6) | 19.5 (19.2, 19.7) | 19.3 (19.1, 19.6) |
| BMI category b | ||||||
| underweight | 10.2 | 9.0 | 11.3 | 9.8 | 8.4 | 11.1 |
| normal weight | 63.4 | 62.3 | 64.4 | 65.6 | 64.8 | 66.2 |
| overweight | 26.4 | 28.8 | 24.3 | 24.7 | 26.8 | 22.7 |
| Hand grip strength c (kg) | 20.1 (19.5, 20.8) | 20.7 (19.8, 21.6) | 19.6 (18.7, 20.5) | 20.8 (20.4, 21.1) | 21.4 (20.9, 21.8) | 20.2 (19.7, 20.6) |
| z-Hand grip strength c >1 SD | 10.0 | 11.9 | 8.3 | 12.5 | 14.6 | 10.4 |
Sample size may vary in variables due to missing data. pHDI: pro-Healthy Diet Index. nHDI: non-Healthy Diet Index. a Central obesity identified as waist-to-height ratio ≥0.5 according to Ashwell et al. [61]. b Body mass index (BMI) categorized according to age-sex-specific cut-offs for teenagers [60]: underweight BMI <18.5 kg/m2; normal weight BMI = 18.5 to 24.9 kg/m2; overweight BMI ≥25 kg/m2. c Hand grip strength for dominant hand.
A multi-dimensional statistical analysis will be applied to derive dietary-lifestyle patterns (DLPs). We will aim to cluster dietary and lifestyle variables in teenagers in order to identify specific sets of dietary habits existing in combination with lifestyle behaviors (cross-behavioral patterns covering diet and lifestyle). We intend to apply two methods as alternative procedures: Cluster Analysis (CA) and Principal Component Analysis (PCA) [63]. In both analyses, the input variables will be 14 variables (all standardized before) including:
Eleven dietary, i.e., frequency consumption of breakfast, school meal and nine food items such as dairy products, fish, vegetables, fruit, fruit or vegetable juices, fast foods, sweetened drinks, energy drinks, sweets (in times/day).
Three lifestyles, i.e., screen time, physical activity at school, physical activity at leisure time (in scores).
A k-means clustering algorithm will be used in CA, and subjects will be grouped into clusters based on the Euclidean distances. The analysis will be conducted several times in order to identify the optimal number of clusters. After selecting clusters, the correctness of cluster identification will be verified by comparing the dietary and lifestyle components of DLPs between clusters with one-way analysis of variance (ANOVA).
A varimax rotation will be used in PCA. The following three criteria will be considered in order to identify the number of PCA-derived patterns: (i) the eigenvalues from the correlation matrix of the standardized variables >1.0, (ii) the break-point identified in the scree plot of the eigenvalues and (iii) the total variance explained. Rotated factor loadings >|0.30| will be considered as significantly contributing to each DLP, interpreted as follows: the higher factor loadings, the stronger association between dietary and lifestyle components of DLPs, and the DLP. For each subject, a DLP score reflecting subject’s adherence to the DLP will be calculated as a sum of the product of the input variables and its factor loadings. In each PCA-derived pattern, subjects will be divided into tertiles based on the DLP scores.
For continuous variables, changes in nutrition knowledge score, Emotional Eating score, Uncontrolled Eating score, Cognitive Restraint of Eating score, pHDI, nHDI, screen time, total physical activity, z-BMI, z-WHtR, z-Waist circumference and z-HGS (all expressed in scores or points or SDs) after 3- or 9-month follow-up in respect to baseline will be verified with ANOVA or Mann-Whitney test, for variables with normal or non-normal distribution, respectively.
For categorical variables, logistic regression modeling will be applied. The odds ratios (ORs) and 95% CIs will be calculated. The significance of ORs will be verified with Wald’s statistics. Crude model and models with an adjustment for confounders will be created.
The following categories of modeled variables in the logistic regression analysis will be included: nutrition knowledge score (low, moderate low, higher), breakfast consumption (skipping, irregular, every day), school meal consumption (skipping, irregular, every school day), food frequency consumption (≤1/week, several times a week, every day), pHDI (tertiles: bottom, middle, upper), nHDI (tertiles: bottom, middle, upper), screen time (<2, 2 to 4, ≥4 h/day), physical activity at school (low, moderate, vigorous), physical activity at leisure time (low, moderate, vigorous), total physical activity (low, moderate, high), CA-derived the DLPs (clusters), PCA-derived the DLPs (tertiles: bottom, middle, upper), BMI (underweight, normal weight, overweight), WHtR (lack of central obesity, central obesity) or z-BMI, z-WHtR, z-Waist circumference, z-HGS (categories for z-scores: <−1, −1 to 1, >1 SD).
The following confounders in the logistic regression analysis will be included: gender, age (years), residence (rural, urban), FAS (points), nutrition knowledge score (points), Emotional Eating score (points), Uncontrolled Eating score (points), Cognitive Restraint of Eating score (points), pHDI (% points), nHDI (% points), screen time (points), and total physical activity (points). For each analysis, the set of confounders will be selected according to the modeled research question.
We will consider assessing four main applications of the logistic regression modeling:
For the education-based intervention study: (i) a chance to fall in the modeled category after 3- or 9-month follow-up in respect to baseline as reference, (ii) the chance to fall in the modeled category in the educated group in respect to the control group as reference,
For the cross-sectional study: (iii) adherence to chosen DLP by nutrition knowledge, attitudes toward nutrition and sociodemographic factors in respect to referent DLP, (iv) the chance to fall in the modeled category of body composition in respect to normal body composition category as reference.
All tests will be two-tailed, p-values <0.05 will be considered as significant. Analyses will be performed using Statistica software (version 12.0 PL; StatSoft Inc., Tulsa, OK, USA; StatSoft, Krakow, Poland).
3. Discussion
This study protocol presents a general approach and details of assessment of nutrition knowledge, attitudes toward nutrition, diet quality, lifestyle, and body composition that were used to comprehensively evaluate the cross-behavioral patterns covering dietary and lifestyle behaviors in teenagers. The protocol also presents a scope of nationwide nutrition education activities taken in Polish teenagers as a part of public health interventions.
Reducing childhood obesity is not a straightforward task. There are many factors that influence this phenomenon, making it hard to create intervention programs that have a significant impact on obesity reduction. Schools are considered a primary setting for implementing education programs—they have the unique potential to involve a wide population of children and adolescents. However, there are many variables influencing the effectiveness of school-based programs, including school staff who need to be well-trained and familiarized with the program’s aims, procedures, and tools. The creation of education programs by highly-specialized researchers and scientific support for educators at the first stage of implementation of such programs can increase their effectiveness [43,64].
As mentioned before, in Poland a multi-disciplinary approach covering the implementation of multi-component programs are directed mainly to preschool children while relatively few comprehensive educational programs have been combined with scientific assessment of nutrition knowledge, dietary habits, and lifestyle which have targeted teenagers [44,45]. Such programs, focused on reduction of body mass through changing lifestyle and diet have been widely introduced in United States, Australia, China, Brazil, Turkey, and many European countries, e.g., Spain, France, Belgium, Great Britain, Ireland, Germany, Netherlands, Greece, and Norway. Their recapitulation has been presented in several meta-analysis [21,41,65]. There is convincing evidence from this analysis that school-based prevention interventions can lead to an improvement in dietary behaviors by increasing the consumption of healthy foods and decreasing the consumption of unhealthy foods, as well as by changing lifestyle patterns to be more physically active and less sedentary. However, recently published systematic reviews have shown that school-based intervention programs have been at least mildly effective in reducing BMI in children [64,65,66]. It was explained that these new studies tended to have longer observation periods and be more comprehensive, including more factors under study and confounders. Furthermore, more pronounced results were reported in older than younger school children.
Scientific research shows that linking nutrition knowledge to dietary patterns or diet quality scores would then seem most effective for assessing the relationship between dietary intake and health outcomes. It seems that investing in high-quality research to measure nutrition knowledge is a far-sighted approach, as the burden of diet-related diseases continues to rise worldwide [38,42]. To our knowledge, current intervention and cross-sectional studies should lead to evidence-based initiatives in the field of nutrition education and public health policy. The effectiveness of a public health campaign should be optimized to reduce the prevalence of obesity-related non-communicable diseases, especially in children and adolescents as a vulnerable group.
We anticipate that the results of our comprehensive and multi-factorial statistical analysis will be of great importance. Currently, considering breakfast consumption as a key dietary characteristic along with total physical activity as the key lifestyle characteristic and overweight as the key health outcome, we can discuss these variables based on initial cross-sectional results (in students 11–13 years old). We estimated that 29% of students did not consume breakfast every day. A higher or wider range of the percentage of Polish adolescents (9 to <19 years) not consuming breakfast every day (28–52%) was previously reported [67,68,69,70]. Across Europe, generally more children and adolescents from central (e.g., Slovenia 51–52%) or southern (e.g., Greece 46–48%) than northern countries (e.g., Finland 20%) did not consume breakfast every day [71,72,73]. We found a higher percentage of students (33%) who reached the WHO recommendation on physical activity [58] in comparison with the latest reports (24.2% of Polish children 11–15 years old) [10]. In a further analysis, we will analyze whether this is a positive trend, for example, resulting from the fashion for a healthy lifestyle, or if there are mixed lifestyle behaviors combining greater physical activity with a longer time spent sitting [74]. Overweight was found in 26% of students under study, and this percentage was above the range previously reported in Polish children and young people (12–25%) [5,10]. Thus, our initial findings support previous studies, which have reported that more and more Polish children are overweight or obese.
3.1. Strengths and Limitations in General
The main limitation of the study is the use of a questionnaire to collect dietary and lifestyle data. The questionnaire contained a short list of food items and simple questions related to sedentary and active behaviors. However, there is evidence of many advantages of using brief tools, for example, high reproducibility of simple questions, the possibility to rank respondents into categories of habitual food consumption and identify dietary patterns, the possibility to assess compliance with dietary or lifestyle recommendations as well as low-cost, quick and easy administration [75].
The strengths of the study, regarding this questionnaire, are the validation procedure carried out on a large sample of Polish teenagers (630 subjects 11–15 years old). Second, the questionnaire was filled out by teenagers to reduce possible bias, which could be introduced by parents [76]. Future studies should consider the use of a long form of FFQ and/or applying other methods of dietary and lifestyle assessment to fully describe the teenagers’ dietary behaviors and measure physical activity (e.g., use of accelerometry) instead of self-reported data on lifestyle [77,78,79]. However, to date, there is no validated long form of FFQ, which has been developed for Polish children or adolescents.
To measure adiposity, we applied simple obesity measures (BMI, WHtR) with some interpretative limitations but proper for comprehensive assessment of high adiposity levels [60,61,80,81]. In many large epidemiological studies, both measures are widely used. Furthermore, it is easy to interpret results and compare with others due to well-established procedures and strong documented cut-offs developed for children and adolescents [60,61,80]. A fat-free mass was not directly measured, we applied hand grip strength as an indirect measure of muscle mass. There are no cut-offs for the hand grip strength of teenagers, including Polish individuals, so we used z-score of hand grip strength to assess the differences between groups. Future studies should consider the use of more advanced methods of body composition measurement.
To measure socioeconomic status and attitudes toward nutrition, we applied scales dedicated to children (the Family Affluence Scale, FAS, and three-factor eating questionnaire, TFEQ, respectively), both previously validated and used in the Polish population [54,62]. Although we have slightly changed FAS and shortened TFEQ, both new versions have been tested in pilot and validation studies.
Data collection and all measurements were taken by well-trained researchers with the same type of equipment in all scientific centers to minimize inter-center differences. The main study was preceded by a pilot study that was carried out in all centers (covering above 200 subjects).
3.2. Strengths and Limitations of the Education-Based Intervention Study
The sample was relatively large (over 460), taking into account that complete dietary and weight status data were obtained at all stages of the study. We applied a very rigorous selection of the sample, each participant had to take part in lectures and workshops within all five topics of education program lasting three weeks—students absent at least one school day for the lectures or workshops were excluded. Next, we used appropriate statistical methods to interpret the differences between the educated and control groups in regards to changes from the baseline to a 3- or 9-month follow-up.
The main limitation is a lack of random subjects to be allocated into the educated and control groups. Unfortunately, we were unable to apply the random approach for several reasons. First, for organizational reasons, we wanted to choose schools located at a convenient distance from the academic centers (up to 50 km). Second (surprisingly), many schoolmasters did not permit their school to participate in the study. Third, many of the schools had previously participated in other nutrition-health education programs, so they could not be included in our study. There was an element of randomness in our study because assigning classes to the educated or control group was accidental and the schools represented a wide social spectrum.
3.3. Strengths and Limitations of the Cross-Sectional Study
The main strength of the study was the clustering of dietary and lifestyle variables and identifying sets of dietary habits existing in teenagers in combination with lifestyle behaviors (DLPs). To date, few studies have been aimed at identifying cross-behavioral patterns covering both dietary and lifestyle variables. Although there is limited data available for teenagers from some developed countries [74,76,82,83,84,85,86], there is the gap for Eastern or Central Europe, including Poland.
The main limitation is the sample itself, which was not randomly selected, although it is relatively large (above 1500), has a narrow age range (11–13 years) and covers the entire territory of Poland—widely reflecting the social diversity of Poles (Figure 1A) and providing a good basis for generalizations.
4. Conclusions
The study will be able to assess the effectiveness of a nutrition-related and lifestyle-related education program in the medium-term perspective. The weaknesses and strengths of such education programs in respect to teenagers, as a target group, could be identified. Based on the results, in future, well-tailored education programs addressed to teenagers can be created. We think that our results can be interpreted in a wider scope, at least for European teenagers living in similar conditions.
The findings may contribute to identifying teenage subpopulations at risk for excessive body weight and adiposity as well as poor muscling and determine predictors related to diet, lifestyle, nutrition knowledge, attitudes toward nutrition and socio-demographic factors which influence improper body composition and increase obesity risk.
The study provides evidence-based support for preventive health care to promote normal growth and development of the young population and reduce the risk of diet-related diseases in adulthood by the early shaping of adequate dietary and lifestyle behaviors. The results of the study can be implemented as an important public health action.
Acknowledgments
Thanks are expressed to the participants for their contributions to the study and the academic researchers from: Warsaw University of Life Sciences (WULS-SGGW), Gdynia Maritime University, Faculty of Health Sciences, Medical University in Bialystok, Faculty of Physical Education and Sport in Biala Podlaska of the Josef Pilsudski University of Physical Education in Warsaw, University of Agriculture in Krakow, University of Life Sciences in Lublin, University of Life Sciences in Poznan, University of Warmia and Mazury in Olsztyn, Wroclaw University of Environmental and Life Sciences.
Supplementary Materials
The following are available online at http://www.mdpi.com/2072-6643/10/10/1439/s1, Figure S1: Planned results of the implementation of the national multicenter project ‘ABC of Healthy Eating’, Table S1: The short form of the Food Frequency Questionnaire for Polish Children (SF-FFQ4PolishChildren)—translation into English, Table S2: The short form of the Food Frequency Questionnaire for Polish Children (SF-FFQ4PolishChildren)—Polish language version.
Author Contributions
J.H., L.W., M.H., J.K., and. K.G. were responsible for the conception and design of the main study. J.H., M.H. and K.G. were involved in the funding acquisition in respect to the project and managing of the project. J.K. and L.W. were responsible for development of design of statistical analysis and results interpretation for the study. J.K. was responsible for the data cleaning and statistical analysis for the main study. J.H. and L.W. were responsible for writing the manuscript. M.H. was responsible for visualization. K.G. was responsible for revising the manuscript critically for important intellectual content. The manuscript has been revised by all co-authors.
Funding
The study was financially supported by Carrefour Foundation (Agreement ABC No.1/2014; Agreement ABC No. 2/2016) and each scientific centre from sources of the Polish Ministry of Sciences and Higher Education.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., Mullany E.C., Biryukov S., Abbafati C., Abera S.F., et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lobstein T., Jackson-Leach R. Planning for the worst: Estimates of obesity and comorbidities in school-age children in 2025. Pediatr. Obes. 2016;11:321–325. doi: 10.1111/ijpo.12185. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Global Nutrition Monitoring Framework: Operational guidance for tracking progress in meeting targets for 2025. [(accessed on 20 July 2018)];2017 Geneva, Switzerland. Available online: http://apps.who.int/iris/bitstream/handle/10665/259904/9789241513609-eng.pdf;jsessionid=004DBB115D5F666C3EE9F022BFD99D86?sequence=1.
- 4.Ogden C.L., Carroll M.D., Kit B.K., Flegal K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suder A., Gomula A., Koziel S. Central overweight and obesity in Polish schoolchildren aged 7–18 years: Secular changes of waist circumference between 1966 and 2012. Eur. J. Pediatr. 2017;176:909–916. doi: 10.1007/s00431-017-2938-4. [DOI] [PubMed] [Google Scholar]
- 6.Olds T., Maher C., Zumin S., Péneau S., Lioret S., Castetbon K., Bellisle F., de Wilde J., Hohepa M., Maddison R., et al. Evidence that the prevalence of childhood overweight is plateauing: Data from nine countries. Int. J. Pediatr. Obes. 2011;6:342–360. doi: 10.3109/17477166.2011.605895. [DOI] [PubMed] [Google Scholar]
- 7.Sahoo K., Sahoo B., Choudhury A.K., Sofi N.Y., Kumar R., Bhadoria A.S. Childhood obesity: Causes and consequences. J. Family Med. Prim. Care. 2015;4:187–192. doi: 10.4103/2249-4863.154628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Onis M., Blössner M., Borghi E. Prevalence and trends of stunting among pre-school children, 1990–2020. Public Health Nutr. 2012;15:142–148. doi: 10.1017/S1368980011001315. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization European Food and Nutrition Action Plan 2015–2020, REGIONAL COMMITTEE FOR EUROPE 64th SESSION. [(accessed on 28 July 2018)];2014 Copenhagen, Denmark. Available online: http://www.euro.who.int/__data/assets/pdf_file/0008/253727/64wd14e_FoodNutAP_140426.pdf.
- 10.Mazur J., editor. Zdrowie i Zachowania Zdrowotne Młodzieży Szkolnej w Polsce na tle Wybranych Uwarunkowań Socjodemograficznych. Wyniki. Badań HBSC 2014 [Health and Health Behaviour of School Children in Poland against the Background of Selected Sociodemographic Conditions. HBSC 2014 Results] IMiD; Warsaw, Poland: 2015. [Google Scholar]
- 11.Chobot A., Górowska-Kowolik K., Sokołowska M., Jarosz-Chobot P. Obesity and diabetes-Not only a simple link between two epidemics. Diabetes Metab. Res. Rev. 2018;21:e3042. doi: 10.1002/dmrr.3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kowalkowska J., Wadolowska L., Wuenstel J.W., Słowińska M.A., Niedźwiedzka E. Socioeconomic status and overweight prevalence in polish adolescents: The impact of single factors and a complex index of socioeconomic status in respect to age and sex. Iran J. Public Health. 2014;43:913–925. [PMC free article] [PubMed] [Google Scholar]
- 13.Wadolowska L., Kowalkowska J., Czarnocinska J., Jezewska-Zychowicz M., Babicz-Zielinska E. Comparing dietary patterns derived by two methods and their associations with obesity in Polish girls aged 13–21 years: The cross-sectional GEBaHealth study. Perspect. Public Health. 2017;137:182–189. doi: 10.1177/1757913916679859. [DOI] [PubMed] [Google Scholar]
- 14.Faienza M.F., Wang D.Q., Frühbeck G., Garruti G., Portincasa P. The dangerous link between childhood and adulthood predictors of obesity and metabolic syndrome. Intern. Emerg Med. 2016;11:175–182. doi: 10.1007/s11739-015-1382-6. [DOI] [PubMed] [Google Scholar]
- 15.Simmonds M., Llewellyn A., Owen C.G., Woolacott N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016;17:95–107. doi: 10.1111/obr.12334. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization Prevention of Cardiovascular Disease. [(accessed on 2 August 2018)];2007 Geneva, Switzerland. Available online: http://www.who.int/cardiovascular_diseases/guidelines/en/
- 17.Vucenik I., Stains J.P. Obesity and cancer risk: Evidence, mechanisms, and recommendations. Ann. N.Y. Acad. Sci. 2012;1271:37–43. doi: 10.1111/j.1749-6632.2012.06750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Llewellyn A., Simmonds M., Owen C.G., Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes. Rev. 2016;17:56–67. doi: 10.1111/obr.12316. [DOI] [PubMed] [Google Scholar]
- 19.Li L., Pérez A., Wu L.T., Ranjit N., Brown H.S., Kelder S.H. Cardiometabolic Risk Factors among Severely Obese Children and Adolescents in the United States, 1999–2012. Child Obes. 2016;12:12–19. doi: 10.1089/chi.2015.0136. [DOI] [PubMed] [Google Scholar]
- 20.Estrada E., Eneli I., Hampl S., Mietus-Snyder M., Mirza N., Rhodes E., Sweeney B., Tinajero-Deck L., Woolford S.J., Pont S.J., Children’s Hospital Association Children’s Hospital Association consensus statements for comorbidities of childhood obesity. Child Obes. 2014;10:304–317. doi: 10.1089/chi.2013.0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sbruzzi G., Eibel B., Barbiero S.M., Petkowicz R.O., Ribeiro R.A., Cesa C.C., Martins C.C., Marobin R., Schaan C.W., Souza W.B., et al. Educational interventions in childhood obesity: A systematic review with meta-analysis of randomized clinical trials. Prev. Med. 2013;56:254–264. doi: 10.1016/j.ypmed.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 22.Chaput J.P., Pérusse L., Després J.P., Tremblay A., Bouchard C. Findings from the quebec family study on the etiology of obesity: Genetics and environmental highlights. Curr. Obes. Rep. 2014;3:54–66. doi: 10.1007/s13679-013-0086-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Serra-Majem L., Bautista-Castaño I. Etiology of obesity: Two ‘key issues’ and other emerging factors. Nutr. Hosp. 2013;28(Suppl. 5):32–43. doi: 10.3305/nh.2013.28.sup5.6916. [DOI] [PubMed] [Google Scholar]
- 24.Wadolowska L., Kowalkowska J., Lonnie M., Czarnocinska J., Jezewska-Zychowicz M., Babicz-Zielinska E. Associations between physical activity patterns and dietary patterns in a representative sample of Polish girls aged 13–21 years: A cross-sectional study (GEBaHealth Project) BMC Public Health. 2016;16:698. doi: 10.1186/s12889-016-3367-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Popkin M.P., Adair L.S., Ng S.W. The Global Nutrition Transition: The pandemic of obesity in developing countries. Nutr. Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu H., Wen L.M., Rissel C. Associations of parental influences with physical activity and screen time among young children: A systematic review. J. Obes. 2015;2015:546925. doi: 10.1155/2015/546925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Hecke L., Loyen A., Verloigne M., van der Ploeg H.P., Lakerveld J., Brug J., De Bourdeaudhuij I., Ekelund U., Donnelly A., Hendriksen I., et al. Variation in population levels of physical activity in European children and adolescents according to cross-European studies: A systematic literature review within DEDIPAC. Int. J. Behav. Nutr. Phys. Act. 2016;28:13–70. doi: 10.1186/s12966-016-0396-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dumith S.C., Gigante D.P., Domingues M.R., Kohl H.W. Physical activity change during adolescence: A systematic review and a pooled analysis. Int. J. Epidemiol. 2011;40:685–698. doi: 10.1093/ije/dyq272. [DOI] [PubMed] [Google Scholar]
- 29.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kubik M.Y., Lytle L.A., Hannan P.J., Perry C.L., Story M. The association of the school food environment with dietary behaviors of young adolescents. Am. J. Public Health. 2003;93:1168–1173. doi: 10.2105/AJPH.93.7.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fox M.K., Dodd A.H., Wilson A., Gleason P.M. Association between school food environment and practices and body mass index of US public school children. J. Am. Diet Assoc. 2009;109(Suppl. 2):108–117. doi: 10.1016/j.jada.2008.10.065. [DOI] [PubMed] [Google Scholar]
- 32.Singh R. Childhood obesity: An epidemic in waiting? Int. J. Med. Public Health. 2013;3:2–7. doi: 10.4103/2230-8598.109298. [DOI] [Google Scholar]
- 33.Trude A.C.B., Kharmats A.Y., Jones-Smith J.C., Gittelsohn J. Exposure to a multi-level multi-component childhood obesity prevention community-randomized controlled trial: Patterns, determinants, and implications. Trials. 2018;19:287. doi: 10.1186/s13063-018-2663-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ryan P. Integrated theory of health behavior change: Background and intervention development. Clin. Nurse Spec. 2009;23:161–172. doi: 10.1097/NUR.0b013e3181a42373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jezewska-Zychowicz M., Wadolowska L., Kowalkowska J., Lonnie M., Czarnocinska J., Babicz-Zielinska E. Perceived Health and Nutrition Concerns as Predictors of Dietary Patterns among Polish Females Aged 13–21 Years (GEBaHealth Project) Nutrients. 2017;9:613. doi: 10.3390/nu9060613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alkaed D., Ibrahim N., Ismail F., Barake R. Validity and Reliability of a Nutrition Knowledge Questionnaire in an Adult Student Population. J. Nutr. Educ. Behav. 2018;50:718–723. doi: 10.1016/j.jneb.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 37.Birch L., Jennifer S., Savage J.S., Ventura A. Influences on the development of children’s eating behaviours: From infancy to adolescence. Can. J. Diet Pract. Res. 2007;68:S51–S56. [PMC free article] [PubMed] [Google Scholar]
- 38.Spronk I., Kullen C., Burdon C., O’Connor H. Relationship between nutrition knowledge and dietary intake. Br. J. Nutr. 2014;111:1713–1726. doi: 10.1017/S0007114514000087. [DOI] [PubMed] [Google Scholar]
- 39.Baxter S.D. Cognitive processes in children’s dietary recalls: Insight from methodological studies. Eur. J. Clin. Nutr. 2009;63(Suppl. 1):19–32. doi: 10.1038/ejcn.2008.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Story M., Kaphingst K.M., French S. The role of schools in obesity prevention. Future Child. 2006;16:109–142. doi: 10.1353/foc.2006.0007. [DOI] [PubMed] [Google Scholar]
- 41.Hung L.S., Tidwell D.K., Hall M.E., Lee M.L., Briley C.A., Hunt B.P. A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutr. Res. 2015;35:229–240. doi: 10.1016/j.nutres.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 42.Worsley A. Nutrition knowledge and food consumption: Can nutrition knowledge change food behaviour? Asia Pac. J Clin. Nutr. 2002;11:S579–S585. doi: 10.1046/j.1440-6047.11.supp3.7.x. [DOI] [PubMed] [Google Scholar]
- 43.Manios Y., Grammatikaki E., Androutsos O., Chinapaw M.J., Gibson E.L., Buijs G., Iotova V., Socha P., Annemans L., Wildgruber A., et al. A systematic approach for the development of a kindergarten-based intervention for the prevention of obesity in preschool age children: The ToyBox-study. Obes. Rev. 2012;13:3–12. doi: 10.1111/j.1467-789X.2011.00974.x. [DOI] [PubMed] [Google Scholar]
- 44.Manios Y., Androutsos O., Katsarou C., Iotova V., Socha P., Geyer C., Moreno L., Koletzko B., De Bourdeaudhuij I., on behalf of the ToyBox-study group Designing and implementing a kindergarten-based, family-involved intervention to prevent obesity in early childhood: The ToyBox-study. Obes. Rev. 2014;15:5–13. doi: 10.1111/obr.12175. [DOI] [PubMed] [Google Scholar]
- 45.Myszkowska-Ryciak J., Harton A. Eating Healthy, Growing Healthy: Impact of a Multi-Strategy Nutrition Education on the Assortments of Beverages Served in Preschools, Poland. Int. J. Environ. Res. Public Health. 2018;15:1355. doi: 10.3390/ijerph15071355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization Cancer Control: Knowledge into Action. [(accessed on 2 August 2018)];2007 Geneva, Switzerland. Available online: http://www.who.int/cancer/modules/en/
- 47.World Health Organization Framework for Care and Control of Tuberculosis and Diabetes. [(accessed on 27 July 2018)];2011 Geneva. Available online: https://www.worlddiabetesfoundation.org/files/collaborative-framework-care-and-control-tuberculosis-and-diabetes. [PubMed]
- 48. [(accessed on 11 September 2018)]; Available online: http://www.zachowajrownowage.pl/pl/o-projekcie/
- 49.Hoffmann T.C., Glasziou P.P., Boutron I., Milne R., Perera R., Moher D., Altman D.G., Barbour V., Macdonald H., Johnston M., et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;7:348. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 50.Hörnell A., Berg C., Forsum E., Larsson C., Sonestedt E., Åkesson A., Lachat C., Hawwash D., Kolsteren P., Byrnes G., et al. Perspective: An Extension of the STROBE Statement for Observational Studies in Nutritional Epidemiology (STROBE-nut): Explanation and Elaboration. Adv. Nutr. 2017;8:652–678. doi: 10.3945/an.117.015941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reporting Guidelines for Main Study Types. [(accessed on 23 July 2018)]; Available online: http://www.equator-network.org.
- 52.Piramida Zdrowego Zywienia i Aktywnosci Fizycznej. [(accessed on 23 July 2018)]; Available online: http://www.izz.waw.pl/pl/zasady-prawidowego-ywienia.
- 53.Whati L.H., Senekal M., Steyn N.P., Nel J.H., Lombard C., Norris S. Development of a reliable and valid nutritional knowledge questionnaire for urban South African adolescents. Nutrition. 2005;21:76–85. doi: 10.1016/j.nut.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 54.Dzielska A., Mazur J., Małkowska-Szkutnik A., Kołoło H. Adaptation of the Three-Factor Eating Questionnaire (TFEQ-13) for school-aged adolescents in a population study. Probl. Hig. Epidemiol. 2009;90:362–369. [Google Scholar]
- 55.Rampersaud G.C., Pereira M.A., Girard B.L., Adams J., Metzl J.D. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J. Am. Diet. Assoc. 2005;105:743–760. doi: 10.1016/j.jada.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 56.Pereira M.A., Erickson E., McKee P., Schrankler K., Raatz S.K., Lytle L.A., Pellegrini A.D. Breakfast frequency and quality may affect glycemia and appetite in adults and children. J. Nutr. 2011;141:163–168. doi: 10.3945/jn.109.114405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.AAP Council on communications and media Media Use in School-Aged Children and Adolescents. Pediatrics. 2016;138:e20162592. doi: 10.1542/peds.2016-2592. [DOI] [PubMed] [Google Scholar]
- 58.World Health Organization Global Recommendations on Physical Activity for Health. [(accessed on 29 July 2018)];2010 Geneva, Switzerland. Available online: http://www.who.int/dietphysicalactivity/factsheet_recommendations/en/ [PubMed]
- 59.ISAK International Standards for Anthropometric Assessment. Potchefstroom, South Africa: International Society for the Advancement of Kinanthropometry. [(accessed on 17 July 2018)];2001 Available online: http://www.ceap.br/material/MAT17032011184632.pdf.
- 60.Cole T.J., Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012;7:284–294. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 61.Ashwell M., Gunn P., Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012;13:275–286. doi: 10.1111/j.1467-789X.2011.00952.x. [DOI] [PubMed] [Google Scholar]
- 62.Mazur J. Family Affluence Scale—validation study and suggested modification. Hygeia Pub. Health. 2013;48:211–217. [Google Scholar]
- 63.Armitage P., Berry G., Matthews J.N.S. Statistical Methods in Medical Research. 4th ed. Blackwell Science; Oxford, UK: 2008. [Google Scholar]
- 64.Centeio E.E., McCaughtry N., Moore E.W.G., Kulik N., Garn A., Martin J., Shen B., Somers C.L., Fahlman M. Building healthy communities: A comprehensive school health program to prevent obesity in elementary schools. Prev. Med. 2018;111:210–215. doi: 10.1016/j.ypmed.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 65.Sobol-Goldberg S., Rabinowitz J., Gross R. School-based obesity prevention programs: A meta-analysis of randomized controlled trials. Obesity. 2013;21:2422–2428. doi: 10.1002/oby.20515. [DOI] [PubMed] [Google Scholar]
- 66.Lycett K., Miller A., Knox A., Dunn S., Kerr J.A., Sung V., Wake M. ‘Nudge’ interventions for improving children’s dietary behaviors in the home: A. systematic review. Obes. Med. 2017;7:21–33. doi: 10.1016/j.obmed.2017.06.001. [DOI] [Google Scholar]
- 67.Zielińska M., Hamułka J., Gajda K. Family influences on breakfast frequency and quality among primary school pupils in Warsaw and its surrounding areas. Rocz. Panstw. Zakl. Hig. 2015;66:143–149. [PubMed] [Google Scholar]
- 68.Inchley J., Currie D., Young T., Samdal O., Torsheim T., Augustson L., Mathison F., Aleman-Diaz A., Molcho M., Weber M., et al. WHO Regional Office for Europe; Copenhagen, Denmark: 2016. [(accessed on 9 September 2018)]. Growing up unequal: Gender and socioeconomic differences in young people’s health and wellbeing. Health Behaviour in School-aged Children (HBSC) study: International report from the 2013/2014 survey. Available online: http://www.euro.who.int/en/hbsc-report-2016. [Google Scholar]
- 69.Wunstel J.W., Kowalkowska J., Wadolowska L., Slowinska M.A., Niedzwiedzka E., Kurp L. Habitual eating breakfast consumption. Dev. Period Med. 2015;19:193–201. [PubMed] [Google Scholar]
- 70.Kollataj W., Sygit K., Sygit M., Karwat I.D., Kollataj B. Eating habits of children and adolescents from rural regions depending on gender, education, and economic status of parents. Ann. Agric. Environ. Med. 2011;18:393–397. [PubMed] [Google Scholar]
- 71.Zakrzewski J.K., Gillison F.B., Cumming S., Church T.S., Katzmarzyk P.T., Broyles S.T., Champagne C.M., Chaput J.P., Denstel K.D., Fogelholm M., et al. Associations between breakfast frequency and adiposity indicators in children from 12 countries. Int. J. Obes. 2015;5(Suppl. 2):80–88. doi: 10.1038/ijosup.2015.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Brug J., van Stralen M.M., te Velde S.J., Chinapaw M.J.M., De Bourdeaudhuij I., Lien N., Bere E., Maskini V., Singh A.S., Maes L. Differences in weight status and energy-balance related behaviors among schoolchildren across europe: The energy-project. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0034742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hallstrom L., Vereecken C.A., Labayen I., Ruiz J.R., Le Donne C., Garcia M.C., Gilbert C.C., Martínez S.G., Grammatikaki E., Huybrechts I. Breakfast habits among European adolescents and their association with sociodemographic factors: The HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study. Public Health Nutr. 2012;15:1879–1889. doi: 10.1017/S1368980012000341. [DOI] [PubMed] [Google Scholar]
- 74.Gubbels J.S., Kremers S.P., Stafleu A., Goldbohm A., Vries N.K., Thijs C. Clustering of energy balance-related behaviors in 5-year-old children: Lifestyle patterns and their longitudinal association with weight status development in early childhood. Int. J. Behav. Nutr. 2012;9:77. doi: 10.1186/1479-5868-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Food and Agriculture Organization Dietary Assessment: A Resource Guide to Method Selection and Application in Low Resource Settings. [(accessed on 17 July 2018)];2018 Rome. Available online: http://www.fao.org/3/i9940en/I9940EN.
- 76.Gubbels J.S., van Assema P., Kremers S.P.J. Physical activity, sedentary behavior, and dietary patterns among children. Curr. Nutr. Rep. 2013;2:105–112. doi: 10.1007/s13668-013-0042-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ferrari P., Friedenreich C., Matthews C.E. The role of measurement error in estimating levels of physical activity. Am. J. Epidemiol. 2007;166:832–840. doi: 10.1093/aje/kwm148. [DOI] [PubMed] [Google Scholar]
- 78.Saunders T.J., Prince S.A., Tremblay M.S. Clustering of children’s activity behaviour: The use of self-report versus direct measures. Int. J. Behav. Nutr. Phys. Act. 2011;8 doi: 10.1186/1479-5868-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Verbestel V., De Henauw S., Bammann K., Barba G., Hadjigeorgiou C., Eiben G., Konstabel K., Kovács E., Pitsiladis Y., Reisch L., et al. Are context-specific measures of parental-reported physical activity and sedentary behaviour associated with accelerometer data in 2–9-year-old European children? Public Health Nutr. 2015;18:860–868. doi: 10.1017/S136898001400086X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Martin-Calvo N., Moreno-Galarraga L., Martinez-Gonzalez M.A. Association between body mass index, waist-to-height ratio and adiposity in children: A systematic review and meta-analysis. Nutrients. 2016;8:512. doi: 10.3390/nu8080512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ashwell M., Gibson S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open. 2016;6:e010159. doi: 10.1136/bmjopen-2015-010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Leech R.M., McNaughton S.A., Timperio A. Clustering of diet, physical activity and sedentary behaviour among Australian children: Cross-sectional and longitudinal associations with overweight and obesity. Int. Obes. 2015;39:1079–1085. doi: 10.1038/ijo.2015.66. [DOI] [PubMed] [Google Scholar]
- 83.Pérez-Rodrigo C., Gil A., González-Gross M., Ortega R.M., Serra-Majem L., Varela-Moreiras G., Aranceta-Bartrina J. Clustering of Dietary Patterns, Lifestyles, and Overweight among Spanish Children and Adolescents in the ANIBES Study. Nutrients. 2016;8:11. doi: 10.3390/nu8010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mandic S., Bengoechea E.G., Coppell K.J., Spence J.C. Clustering of (Un) Healthy Behaviors in Adolescents from Dunedin, New Zealand. Am. J. Health Behav. 2017;41:266–275. doi: 10.5993/AJHB.41.3.6. [DOI] [PubMed] [Google Scholar]
- 85.Nuutinen T., Lehto E., Ray C., Roos E., Villberg J., Tynjälä J. Clustering of energy balance-related behaviours, sleep, and overweight among Finnish adolescents. Int. J. Public Health. 2017;62:929–938. doi: 10.1007/s00038-017-0991-4. [DOI] [PubMed] [Google Scholar]
- 86.Laxer R.E., Brownson R.C., Dubin J.A., Cooke M., Chaurasia A., Leatherdale S.T. Clustering of risk-related modifiable behaviours and their association with overweight and obesity among a large sample of youth in the COMPASS study. BMC Public Health. 2017;17:102. doi: 10.1186/s12889-017-4034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.