Abstract
Pulmonary rehabilitation (PR) reduces the number and duration of hospital admissions and readmissions, and improves health-related quality of life in patients with COPD. Despite clinical guideline recommendations, under-referral and limited uptake to PR contribute to poor treatment access. We reviewed published literature on the effectiveness of interventions to improve referral to and uptake of PR in patients with COPD when compared to standard care, alternative interventions, or no intervention. The review followed recognized methods. Search terms included “pulmonary rehabilitation” AND “referral” OR “uptake” applied to MEDLINE, EMBASE, CINAHL, PsycINFO, ASSIA, BNI, Web of Science, and Cochrane Library up to January 2018. Titles, abstracts, and full papers were reviewed independently and quality appraised. The protocol was registered (PROSPERO # 2016:CRD42016043762). We screened 5,328 references. Fourteen papers met the inclusion criteria. Ten assessed referral and five assessed uptake (46,146 patients, 409 clinicians, 82 hospital departments, 122 general practices). One was a systematic review which assessed uptake. Designs, interventions, and scope of studies were diverse, often part of multifaceted evidence-based management of COPD. Examples included computer-based prompts at practice nurse review, patient information, clinician education, and financial incentives. Four studies reported statistically significant improvements in referral (range 3.5%–36%). Two studies reported statistically significant increases in uptake (range 18%–21.5%). Most studies had methodological and reporting limitations. Meta-analysis was not conducted due to heterogeneity of study designs. This review demonstrates the range of approaches aimed at increasing referral and uptake to PR but identifies limited evidence of effectiveness due to the heterogeneity and limitations of study designs. Research using robust methods with clear descriptions of intervention, setting, and target population is required to optimize access to PR across a range of settings.
Keywords: health services research, service improvement, access to healthcare, evidence-based practice, long-term condition, supervised exercise
Introduction
COPD presents a considerable health challenge. It is estimated that worldwide 328 million people have COPD and 65 million people live with moderate to severe COPD.1 In 2015, COPD accounted for 5% of all deaths globally,2 and in the UK, ~1.2 million people and 4.5% of all people aged over 40 years live with the condition.3 COPD is likely to be underdiagnosed and prevalence in the UK may be rising.3 It compromises individuals’ quality of life and impacts healthcare costs, mostly relating to hospital admissions. In 2012, it was estimated to cost the UK National Health Service £800 million per annum.4 Pulmonary rehabilitation (PR), providing supervised exercise and education, improves COPD symptoms leading to improvements in exercise capacity and quality of life.5 PR reduces the number and duration of respiratory hospital admissions experienced by individuals,6 the number of readmissions,6,7 and can foster self-management skills.8 It is a cost-effective treatment.9
Despite a clear evidence base and guidelines recommending PR,10,11 it is grossly underutilized in practice worldwide.12 In England and Wales, for example, the National COPD Audit Programme for 2013/14 estimated the prevalence of COPD patients eligible for PR to be 446,000; however, only 68,000 were referred (15% of normative need) of whom only 69% attended an initial assessment (10% of normative need).13 Utilization may be impacted by availability, referral, and uptake but even where places are available they may not be utilized. In the East of England in 2014/15, the number of available PR places represented only 53.8% of the proposed target, but just 73% of these places were taken up.14 There is an urgent need to improve referral and uptake to PR both in the UK6,13 and globally12 but there is no best practice guidance for doing so.
We set out to conduct a systematic review of published studies on the effectiveness of interventions to increase rates of referral and uptake from primary care or outpatient departments to exercise-based PR programs in patients with COPD compared to standard care, alternative interventions, or no intervention.
Methods
Recognized systematic review methods15 were adapted to conduct the review. The review protocol was registered on PROSPERO (2016:CRD42016043762)16 and reported according to PRISMA guidelines.17
Eligibility
Studies were required to report at least one of the main outcomes of interest: rates of referral to or uptake of exercise-based PR programs in patients with COPD. We defined PR programs as including “multicomponent, multidisciplinary interventions, which are tailored to the individual patient’s needs. The rehabilitation process should incorporate a program of physical training, disease education, and nutritional, psychological, and behavioral intervention.”18 Uptake was defined as having attended a first appointment with a PR provider including initial assessment.
We included all studies that used established quantitative or mixed methods of data collection, eg, trials, surveys, direct observations, action research, interviews, focus groups or questionnaires, systematic reviews, and meta-analyses. Interventions could be contrasted with standard care, alternative interventions, or have no comparator or control.
We included studies of i) healthcare professionals who referred COPD patients to PR in primary, secondary, or community care settings; ii) adult patients (≥18 years) with a diagnosis of COPD in any setting, who had received a referral to PR (whether taken up or not); and iii) informal adult carers (≥18 years) of these patients, defined as spouse or partner, family members, friends, or significant others, who provided physical, practical, transportation, or emotional help to someone with COPD. We excluded professional carers. We also excluded studies that featured mixed participant groups where subgroups with COPD were not described or where studies were conducted in various settings and data from inpatient and outpatient services could not be separated.
Published studies were included. Conference abstracts and opinion papers were not considered for analysis. No language restrictions were applied.
Data sources and search strategy
We searched the following databases: MEDLINE and EMBASE (via OVID), CINAHL and PsycINFO (via Ebsco-Host), ASSIA and BNI (via ProQuest), Web of Science, and Cochrane Library to the end of January 2018. A search strategy was developed on MEDLINE (see Supplementary material) and adapted for other databases. The strategy included “quantitative” OR “mix* method*.” Filters for randomized controlled trials (RCTs) and systematic reviews were adapted from Scottish Intercollegiate Guidelines Network search filters.19 We also searched “related article” searches in PubMed for all studies included in the review and scanned reference lists of all included studies and key references, searching for relevant papers citing the included papers in the Institute for Scientific Information Web of Science (Science Citation Index and Social Sciences Citation Index). An interim report of this work, searching literature up to June 2016 and without specific search criteria for quantitative and mixed methods studies, was presented at the British Thoracic Society in 2016.20
Study selection and data extraction
Search results were screened on titles and abstracts and then on full text by two independent reviewers (FE and IW), gaining consensus on inclusion with input from a referee (JF) if required.
A data extraction form was piloted and two reviewers (FE and IW) independently extracted data from eligible papers. Data included study setting, sample size, recruitment method, study design, study objectives, participant/patient characteristics, methods of data collection, data analysis, recorded outcomes, limitations, and conflict of interests. We planned to tabulate data and carry out a meta-analysis using Review Manager ([RevMan], Version 5.3; The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, 2014) statistical software according to our prespecified protocol if this was appropriate.
Quality assessment
The same reviewers independently appraised study quality to assess the risk of bias in individual studies using the Cochrane Collaboration’s tool for assessing risk of bias in RCTs,21 the ACROBAT-NRSI (A Cochrane Risk Of Bias Assessment Tool for Non-Randomized Studies of Interventions),22 and AMSTAR (A MeaSurement Tool to Assess systematic Reviews)23 depending on the type of study.
Results
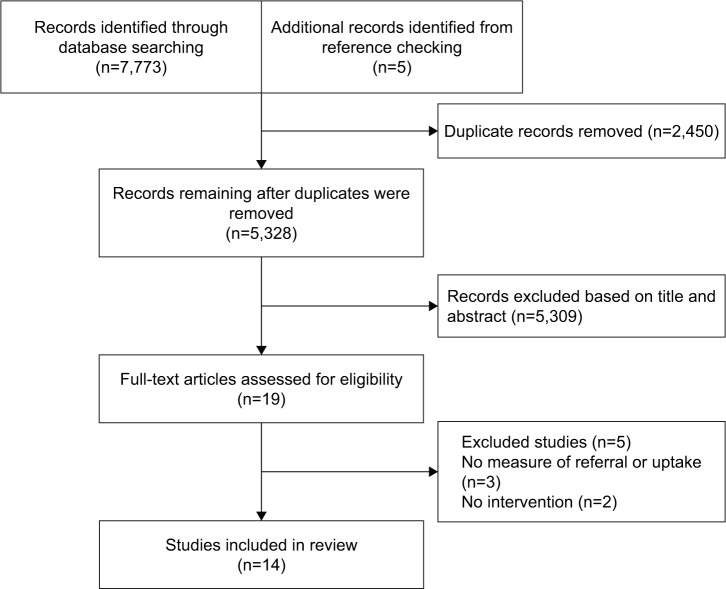
Searches identified 5,328 potentially relevant articles of which 14 met our inclusion criteria (Figure 1). All were in English language. Six studies were conducted in the UK,24–29 four in Denmark,30–33 two in Australia,34,35 and one in USA.36 One was a systematic review.36 Study characteristics and findings are summarized in Table 1.
Figure 1.
Study flow diagram.
Table 1.
Study characteristics
| Study and setting | Sample size | Demographicsa | Source of participants | Study design | Intervention | Comparator group | Outcome measures | Findings relevant to this review |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| <a>Studies measuring referral | ||||||||
| Angus et al;24 primary care, urban, semirural, and rural, UK | 16 General practices; 18 practice nurses; 293 patients | Age: mean 69.7 (SD 10.1) Male: 55.6% |
COPD registers | Descriptive observational study | Computer-guided review, based on NICE guidance, by practice nurses during routine COPD review | None | Change to primary diagnosis. Percentage of patients recommended for inhaler prescription, smoking cessation support, oxygen assessment, PR referral | 24% (47/191) of patients with confirmed COPD diagnosis were referred to PR |
| Deprez et al;36 primary care, rural, USA | 18 General practices (>25 primary care physicians and mid-level providers); 1,210 patient records | Not reported | Samples of records from each participating practice | Before and after audit of patient charts | 1) Team-based model. Three collaborative learning sessions to educate and empower clinical staff with ideas to implement and sustain practice changes 2) On-site visits, email, and telephone support from faculty 3) Change tools: COPD flow sheet, COPD registry, patient self-management worksheet 4) Feedback from patient focus groups |
None | Percentage of patients with documented spirometry results, COPD stage, annual influenza vaccine, pneumonia vaccine, diet, exercise counseling, PR referral. Percentage of visits with documented smoking status, self-management goals, respirator education, smoking cessation counseling (smokers only) | 5% Increase in PR referral (7%–12%, 16 practices) (P=0.048)* |
| Hopkinson et al;27 respiratory ward, acute hospital, London, UK | 1 Respiratory ward; 94 patients | Age: mean 74.6 (11.2) Male: 64% |
Patients on ward from October 2009 to September 2010 | Before and after study of process indicators | 1) Ward-based staff education 2) Discharge care bundle with referral for PR assessment 3) Patient offered phone call 48–72 hours postdischarge to check if they were improving, if not then community input expedited 4) PDSA cycles to refine the process 5) Prize draw for staff completing checklist 6) Ward staff attended hospital PR sessions 7) PR patient information leaflet |
Usual care (historical) | Compliance with smoking cessation advice. PR referral. Self-management plan administered. Inhaler technique reviewed. Follow-up arrangements documented |
54.4% Increase in PR referral (13.6%–68%) |
| Hull et al;28 primary care trust, inner London, UK | 36 General practices | Not reported | COPD management data routinely collected from participant practices | Longitudinal audit, borough- wide quality improvement project | 1) Eight networks of 4–5 general practices 2) Financially incentivized KPIs 3) Care package based on NICE guidance 4) IT infrastructure to monitor networks and KPIs 5) Support from community respiratory team 6) Network boards to review practice performance against targets, supported by clinical leads 7) Quarterly community COPD multidisciplinary team meeting 8) Rapid email/phone advice from respiratory consultant |
COPD management data from two neighboring PCTs. UK-wide QOF for national performance comparison | Number of COPD cases on network registers. Completed care plans. Referral to community-based PR. Flu immunization. Smoking prevalence. Stop smoking attempts. Rates of emergency hospital admission for COPD | 25% Increase in PR referral (45%–70%, between 2010 and 2013). No comparative data reported |
| Lange et al;30 primary care, Denmark | 186 GPs; 4,943 patients | 1st audit: Age: mean 70.7 (8.7) Male: 44.2% Current smoker: 42.3% FEV1 %: 56.4 (23.3) |
20 Consecutive patients visiting each GP over two 4-month periods 1 year apart | Before and after audit of GP patient notes | Educational program: individual meeting with consultant from sponsoring company focused on GOLD guidelines; regional meetings with 30 GPs and staff, pulmonary specialist, and GP from steering committee to discuss the guidelines; symposium for all GPs and staff, plenary sessions, workshops, practical issues | None | Proportion of patients having spirometry testing (primary parameter). Secondary parameters: compliance with inhaler technique, smoking cessation advice (current smokers), referral to COPD rehabilitation, physical exercise advice, dietary instruction, influenza vaccination, inhaled corticosteroids in mild and severe COPD | 3.5% Increase in referral for COPD rehabilitation (16.7%–20.2%) (P<0.01)* |
| Lange et al;31 outpatient clinics, Denmark | 1,868 Patients; 22 hospitals with outpatient departments | 1st audit: Age: mean 69.2 (10.7) Male: 45% Current smoker: 29.2% FEV1 %: 43.6 (17.7) |
30–50 Consecutive patients from each department over two 3-month periods 1 year apart | Before and after audit of hospital records | 1) Educational program: regional meeting; local meeting at department level with workshops on evidence-based diagnosis and treatment of COPD, rationale for COPD assessment, documentation tools 2) A nurse from each department completed an advanced diploma course on COPD |
None | Care quality indicators recorded: height, weight, BMI, smoking status, pack-years, FEV1 % predicted, FVC % predicted, pulse oximetry, smoking cessation advice (current smokers), PR referral, nutritional advice if relevant, inhaler technique checked | 6.4% Increase in PR referral (56.3%–62.7%) (P=0.006). Not significant in weighted analysis due to considerable variation between hospitals, 95% CI (-2%; 22%) |
| Roberts et al;29 primary care, North East London, UK | 20 General practices (10 intervention, 10 control); 1,235 patients (640 intervention, 595 control) | Not reported | Patients on practice lists with COPD diagnosis | Quasi- experimental, pragmatic nonrandomized controlled study | 1) Patient-held scorecard containing six care quality indicators comparing patient’s care to the standard. Sent to patient with letter advising patient to discuss scorecard at the next COPD review 2) Telephone helpline for patients |
Usual care | Compliance with care quality indicators: diagnosis confirmed by postbronchodilator spirometry, annual review performed, self-management plan received, PR referral for patients with MRC score ≥3, patients quit smoking | 7.4% Increase in PR referral for intervention group (1.2%–8.6%) compared to 1.3% increase for control group (0.9%–2.2%). Difference between groups of 6.1% (P=0.03)* |
| Tøttenborg et al;32 hospital outpatients, Denmark | 56 Hospitals; 32,018 patients | Reported by year (2008–2011); 2008 outpatients: Age: median 70.1 Male: 45% Current smoker: 32.6% FEV1%: median 41 |
All patients aged ≥30 seen at hospital outpatient clinic from January 2008 to December 2011 | Before and after audit. Nationwide, population- based quality improvement initiative | Continuous mandatory monitoring of quality of hospital-based COPD care via Danish Clinical Register of COPD. Focus on six care quality indicators. Patient data prospectively registered as part of clinical routine | None | Fulfillment of care quality indicators for each year: lung function (FEV1 % predicted), BMI, MRC dyspnea score, smoking status, smoking cessation (current smokers), PR offer where MRC score ≥3 | 36% Increase in PR referral (55%–91%) (RR 2.78, 95% CI, 2.65; 2.90)* |
| Ulrik et al;33 primary care, Denmark | 124 GPs; 3,058 patients | 1st audit: Age: mean 68 (range 35–95) Male: 44% |
20 Consecutive patients visiting each GP during two 4-month periods 1 year apart | Before and after audit surveys | Educational program for GPs and staff: individual meeting with consultant from sponsoring company focused on GOLD guidelines; meetings with GPs and staff with steering committee, pulmonologist, and a GP to discuss GOLD guidelines; regional symposiums for GPs and staff; individual meeting with consultant from a sponsoring company focusing on GP’s data | None | Proportion of patients with spirometric data (primary parameter). Secondary parameters: BMI, dietary instruction given, instruction for inhaler technique, smoking cessation advice, monitoring of MRC dyspnea score, referral to COPD rehabilitation | 4% Increase in referral to COPD rehabilitation (12% vs 16%) (NS) |
| <a>Studies measuring referral and uptake | ||||||||
| Foster et al;25 primary care, Stoke on Trent, UK | 8 Primary care practices; 126 patients | Current smoker: 34.9% | Patients on COPD registers eligible for PR | Before and after audit of practice data. Survey of practitioners and patients | Participatory action research: clinician questionnaire to assess knowledge and attitudes about PR and ideas for increasing referrals; briefing note based on questionnaire feedback and literature review with suggestions for standardizing PR knowledge and increasing referral (in- house education, practice protocols, “pop-ups,” and memory aids to prompt discussion about PR) | None | Audit data: COPD register size, number of patients eligible for PR, number of eligible patients coded for conversation about PR, outcome of conversation about PR (referred, referral declined, completed, not completed). Cross-sectional survey of patients eligible for PR: PR referral accepted, reasons for declining referral, whether a conversation about PR had taken place |
Patients with PR code and PR referral ranged from 27% to 100% across 6/8 practices; proportion coded as attending PR ranged from 0% to 25% (data collected at one time point only). 25.7% (126/490) of patients returned the survey: 66% (84/126) had discussed PR with a clinician, of which 70.2% (59/84) had accepted PR referral |
| <a>Studies measuring uptake | ||||||||
| Graves et al;26 setting unclear, North Bristol, UK | 600 Patients (400 inter- vention, 200 noninter- vention) | Intervention group who opted in (n=235): | Patients invited to PR program | Observational study | GOIS (1.5 hours) prior to assessment for PR; run by physiotherapist and clinical psychologist; discussion of patient case study, self- management, PR information, alternatives to PR | Rates of attendance at GOIS. Attendance at PR assessment. Starting PR. PR drop out. PR graduation | 16.3% Fewer patients in the intervention group attended pre-course assessment compared to usual care (58.7% vs 75%) (P<0.001)* | |
| Harris et al;34 secondary and outpatient, Adelaide, Australia | 3 Respiratory outpatient clinics; 249 patients (125 intervention, 124 control) | Intervention group: Age: mean 73.6 Male: 55% Current smoker: 18% |
Patients with moderate to severe COPD identified through inpatient admission for COPD and at respiratory outpatient clinics | Controlled before and after | Patient manual summarizing Cochrane evidence on COPD treatments, related topics, and suggested questions to ask the doctor | Usual care including single sheet information pamphlet about COPD | Main outcomes: PR enrollment, rates of influenza vaccination, bone density testing. Secondary outcomes: COPD mastery, COPD knowledge, communication with usual doctor, satisfaction with disease-related information, anxiety | 18% Increase in PR enrollment for the most socioeconomically disadvantaged patients in the intervention group compared to 0% in the control group (P=0.05)*. 12% Increase for the least socioeconomically disadvantaged patients in the intervention group compared to 7% in the control group (NS) |
| Jones et al;37 no restriction on setting | 0 | N/a | N/a | Systematic review | Review of RCTs of interventions to improve patient uptake and/or completion of PR in COPD | Any concurrent control group referred to and/or enrolled on to PR but not receiving an intervention aimed to improve uptake and/or completion | Uptake of PR: received baseline assessment and/or enrolled on to PR. Completion of PR: received discharge assessment; total number of sessions attended | No studies of uptake identified |
| Zwar et al;35 community, Sydney, Australia | 44 General practices; 56 GPs; 451 patients (234 intervention, 217 control) | Intervention group: Age: mean 65.8 (10.3) Male: 47% Current smoker: 31.6% |
Patients in participant practices with COPD diagnosis | Cluster RCT | Individualized care plan based on clinical practice guidelines delivered by nurses in patient’s home over 6 months. Partnership model of working between nurses and GPs | GPs provided with a copy of COPD guidelines. Patients received usual care |
Primary outcome: health- related quality of life. Secondary outcomes: overall quality of life, lung function, smoking status, immunization status, attendance at PR, patient knowledge of COPD |
21.5% Difference in the number attending PR in the intervention group compared to the control group (31.1% vs 9.6%) (OR 5.16 (2.40–11.10)) (P=0.002)* |
Notes:
Studies varied in their reporting of patient characteristics. Here, we present age, sex, smoking status, and lung function where reported. Some studies also reported other patient characteristics.
Statistically significant at P<0.05.
Abbreviations: BMI, body mass index; FEV, forced expiratory volume; GOIS, group opt-in session; GP, general practitioner; IT, information technology; KPI, key performance indicator; MRC score, score on Medical Research Council Dyspnea Scale; NICE, National Institute for Clinical Excellence (UK); NS, not significant; PCT, primary care trust; PDSA, plan, do study, act; PR, pulmonary rehabilitation; QOF, Quality and Outcomes Framework; RCT, randomized controlled trial.
Ten studies included rates of referral to PR as an outcome24,25,27–33,36 of which eight24,27,29–33,36 reported the number of patients or patient records studied, in total 44,720. This total included five large audits capturing data from 43,098 patient records (range 1,211–32,018).30–33,36 Five studies assessed rates of uptake to PR of which three reported the number of patients studied, in total 1,426 (range 126–600).26,34,35 One study reported only percentages.25 A systematic review by Jones et al37 found no eligible studies of uptake.
Populations and settings
Descriptions of patient populations were limited. Age and sex were most commonly reported and no studies reported ethnicity. Age and sex were reported by six studies that measured referral24,27,30–33 and three that measured uptake.26,34,35 The number and/or roles of clinicians involved were reported by seven studies that measured referral24,25,28,30,31,33,36 and two that measured uptake.25,35 Overall, patients were older (mean age ≥69 years) and 44%–64% of the samples were males.
Study designs
Study designs were heterogeneous and most were observational. Of the referral studies, two captured referral data at one time point only,24,25 six reported before and after longitudinal data,28,30–33,36 one reported before and after results using a historical comparison group,27 and one conducted a pragmatic non-RCT.29 Of the uptake studies, one captured uptake data at one time point only,25 one reported before and after results using a historical comparison group,26 one used a controlled before and after design,34 and there was one cluster RCT.35 The systematic review by Jones et al37 searched for RCTs evaluating uptake and identified none.
Interventions
Most studies measured referral or uptake to PR in the context of multifaceted evidence-based management of COPD. Only one study focused specifically on referral25 and one on uptake.26 Interventions ranged from clinician education to system-wide change.
Studies measuring referral in primary care included a computer-guided COPD review,24 educational programs for healthcare providers (HCPs),30,33 collaborative team-based education and empowerment,36 an action research study which generated a range of interventions including education and memory aids,25 general practice networks with specialist support and financial incentives,28 and a patient-held scorecard comparing the patient’s own care against care quality indicators.29 Secondary care interventions included education for HCPs,31 education for HCPs plus a discharge bundle,27 and quality monitoring through a clinical register.32 Studies measuring uptake included a group opt-in session for patients prior to PR assessment,26 a patient-held manual summarizing evidence on COPD treatments with questions to ask the physician,34 individualized care planning supported by partnership working between general practitioners (GPs) and nurses,34 and the action research study by Foster et al.25
Referral was reported at the level of individual patients,24 practice/department,25,29,36 and system level or GP network.28–33 Uptake was reported at individual patient levels.26,34,35
Table 1 illustrates the range of characteristics of the studies. Primary care was the most common setting. Most interventions targeted clinicians. Patients were targeted in two studies measuring referral27,29 and three measuring uptake.26,34,35 Two interventions were at the level of healthcare systems, both measuring referral.28,32 Education and learning support were the most common features of interventions that targeted clinicians.25,27,30,31,33,36 Regarding design, three out of four studies measuring uptake had a comparison group design26,34,35 compared to three out of 10 measuring referral.27–29 All studies of interventions that included elements aimed at patients had a comparison group design.26,27,29,34,35
Outcomes
Referral to PR was the main outcome in eight out of 10 studies24,25,27–29,31,32,36 and uptake was the main outcome in three out of four studies.25,26,34 There was limited detail about procedures for data collection. Most referral outcomes were measured by audits of patient records.25,28–33,36 Graves et al,26 Harris et al,34 and Zwar et al35 measured uptake for individual patients though terms such as “enrollment”34 and “attendance”25 were not defined. Foster et al25 asked patients about their decision to attend PR in a survey.
Conflicts of interest
Potential conflicts of interest were noted in four studies where the authors developed and owned the computer software being assessed24 and where consultants from funding organizations were involved in intervention delivery and quality control.30,31,33
Assessment of methodological quality of included studies
All studies had areas of high risk of bias. In the RCT by Zwar et al,35 this related to the unavoidable lack of blinding of participants (Table 2). The risk of attrition bias was unclear. Furthermore, 52 out of 234 patients allocated to the intervention group did not receive the intervention. No reasons were given for this and the risk of bias is unclear in this regard (Other bias in Table 2). All remaining studies were considered to have a high risk of bias due to a critical risk of confounding that was associated with the study designs (Table 3). The systematic review by Jones et al37 was of high methodological quality (Table 4).
Table 2.
Risk of bias assessment (Cochrane RCT) for randomized studies
| Study | Random sequence generation (selection bias) | Allocation concealment (selection bias) | Blinding of participants and personnel (performance bias) | Incomplete outcome data (attrition bias) | Blinding of outcome assessment (detection bias) | Selective reporting (reporting bias) | Other bias |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Zwar et al35 | Low | Low | High | Unclear | Low | Low | Unclear |
Abbreviation: RCT, randomized controlled trial.
Table 3.
Cochrane Risk of Bias Assessment Tool for nonrandomized studies of interventions (ACROBAT-NRSI)
| Study | Bias due to confounding | Bias in selection of participants into the study | Bias in measurement of interventions | Bias due to departures from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of the reported results |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Angus et al24 | Critical | Serious | Serious | Serious | Serious | Moderate | Moderate |
| Deprez et al36 | Critical | Serious | Low | No information | Moderate | Moderate | Low |
| Foster et al25 | Critical | Serious | Serious | Serious | Serious | Moderate | Moderate |
| Graves et al26 | Critical | Low | Low | Serious | Low | Moderate | Moderate |
| Harris et al34 | Critical | Serious | Low | Moderate | Moderate | Moderate | Moderate |
| Hopkinson et al27 | Critical | Serious | Low | Serious | Low | Moderate | Moderate |
| Hull et al28 | Critical | Moderate | Serious | Moderate | Low | Moderate | Moderate |
| Lange et al30 | Critical | Serious | Low | Moderate | Moderate | Moderate | Moderate |
| Lange et al31 | Critical | Serious | Low | Moderate | Moderate | Moderate | Moderate |
| Roberts et al29 | Critical | Serious | Low | Moderate | Moderate | Moderate | Moderate |
| Tøttenborg et al32 | Critical | Low | Low | Moderate | Moderate | Moderate | Moderate |
| Ulrik et al33 | Critical | Serious | Low | Moderate | Moderate | Moderate | Moderate |
Table 4.
Quality assessment of Jones et al37 against the AMSTAR (A MeaSurement Tool to Assess systematic Reviews) measurement tool”
| Was an “a priori” design provided? | Yes |
| Was there duplicate study selection and data extraction? | Yes |
| Was a comprehensive literature search performed? | Yes |
| Was the status of publication (ie, gray literature) used as an inclusion criterion? | Yes |
| Was a list of studies (included and excluded) provided? | Yes |
| Were the characteristics of the included studies provided? | Yes |
| Was the scientific quality of the included studies assessed and documented? | Yes |
| Was the scientific quality of the included studies used appropriately in formulating conclusions? | Yes |
| Were the methods used to combine the findings of studies appropriate? | N/a |
| Was the likelihood of publication bias assessed? | Yes |
| Was the conflict of interest stated? | Yes |
Study findings
Due to study heterogeneity, we considered it inappropriate to summarize results using a meta-analysis. The reported outcomes can only be understood in the context of each study and are not readily comparable across studies. Furthermore, when considering the study outcomes in light of the various characteristics shown in Table 5 there were no discernible patterns to link study characteristics and outcomes.
Table 5.
Summary of intervention characteristics
| Clinician-focused intervention elements
|
Patient-focused intervention elements
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Comparator group | Study of wider COPD care | System level intervention | Primary care setting | Guideline support tools and methods | Decision support | Protocol guidance | Education and learning | Expert support | Clinician collaborative working | Individual financial incentive | Patient information | Personal support for patients | |
|
| |||||||||||||
| Angus et al24 (R) | ♦ | ♦ | ♦ | ♦ | |||||||||
| Deprez et al36 (R)* | ♦ | ♦ | ♦ | ♦ | |||||||||
| Hull et al28 (R) | ♦ | ♦ | ♦ | ♦ | ♦ | ♦ | ♦ | ♦ | |||||
| Lange et al30 (R)* | ♦ | ♦ | ♦ | ||||||||||
| Lange et al31 (R) | ♦ | ♦ | |||||||||||
| Hopkinson et al27 (R) | ♦ | ♦ | ♦ | ♦ | ♦ | ♦ | ♦ | ♦ | |||||
| Roberts et al29 (R)* | ♦ | ♦ | ♦ | ♦ | ♦ | ||||||||
| Tøttenborg et al32 (R)* | ♦ | ♦ | |||||||||||
| Ulrik et al33 (R) | ♦ | ♦ | ♦ | ♦ | |||||||||
| Foster et al25 (R) (U) | ♦ | ♦ | ♦ | ♦ | ♦ | ||||||||
| Graves et al26 (U) | ♦ | ♦ | |||||||||||
| Harris et al34 (U)* | ♦ | ♦ | ♦ | ||||||||||
| Zwar et al35 (U)* | ♦ | ♦ | ♦ | ♦ | ♦ | ||||||||
Notes:
Study reported statistically significant increase in referral or uptake (P<0.05). R, study including referral measure; U, study including uptake measure.
Referral to PR
Four studies reported statistically significant increases in PR referral. In primary care, Roberts et al29 reported an increase for the intervention group following use of a patient-held quality scorecard, which was 6.1% (P=0.03) greater than that for the control group. Following a collaborative model of education and change implementation, mean referral to PR across 16 general practices increased by 5% (from 7% to 12%) (P=0.048),36 and a 3.5% increase in referrals (from 16.7% to 20.2%) (P<0.01) followed an education program in primary care.30 Tøttenborg et al32 reported a 36% increase in referrals (from 55% to 91%) (relative risk 2.78, 95% CI, 2.65; 2.90) across hospital outpatient departments during mandatory monitoring of quality indicators.
Positive but statistically nonsignificant results followed an educational program in primary care33 and an education program across outpatient departments.31 Two studies reported increases based on descriptive data following use of a COPD discharge care bundle in a hospital ward27 and a quality improvement intervention across primary care.28 A computer-guided COPD review24 and an action research study25 did not collect comparative data.
Uptake of PR
Two studies reported statistically significant increases in uptake. Harris et al34 evaluated a patient manual summarizing evidence on COPD treatments and reported an increase of 18% in PR enrollment among participants in the most socioeconomically disadvantaged stratum compared to no increase in the matched control group (P=0.05). Zwar et al35 reported a 21.5% difference in the number of intervention group patients attending PR (P=0.002) compared to controls where the intervention group had received an individualized care plan supported by partnership working between nurses and GPs.
One study did not collect comparative data25 and a statistically significant decrease in uptake followed a group opt-in patient information session compared to usual care (58.7% vs 75%, P<0.001).26
Discussion
Our carefully conducted systematic review identified a heterogeneous group of studies. Most reported some positive results but only six out of 14 demonstrated statistically significant improvements. Statistically significant increases in referral followed educational sessions for clinicians in primary care,30 collaborative learning sessions for HCPs,36 use of a patient-held COPD care scorecard in primary care,29 and continuous monitoring of care quality indicators in hospital settings.32 Statistically significant increases in uptake followed use of a patient-held summary of COPD research evidence in secondary care34 and a nurse/GP partnership model of care.35 Significantly fewer patients who attended a group opt-in information session subsequently attended PR assessment compared to patients for whom no opt-in session was offered, although subsequent completion rates improved among those who attended.26 Only three studies focused specifically on referral25 or uptake26,37 and we are unable to accurately evaluate the impact of a targeted approach to increase referral or uptake to PR.
The potential for generalizability from the studies is limited by four factors. Firstly, most study designs carried areas of high risk of bias. Secondly, some interventions were not well defined. For example, in two studies the terms “enrollment”34 and “attendance”35 were not explained and it was not possible to distinguish between attendance at pre-course assessment and the first PR class, which are separate stages in the PR pathway. Thirdly, there was limited reporting of patient and clinician populations which may be potentially nonrepresentative. Fourthly, the studies were conducted in high income countries and there were no interventions in low-to-middle income countries where over 90% of deaths globally from COPD occur.2
Two of the studies performed spirometry and confirmed a COPD diagnosis in 57.8%35 and 81%24 of patients. Jones et al37 included only participants with a diagnosis of COPD confirmed by spirometry in their systematic review and identified no studies of uptake. Evidence shows that patients on COPD registers do not always have a confirmed diagnosis with proportions varying from 73%38 to 90%.39 The question remains as to whether this is problematic for drawing conclusions from intervention studies. If studies do not confirm a COPD diagnosis it is possible that the COPD population is overestimated and that effect sizes are therefore over or underestimated. However, Zwar et al35 provided a pragmatic argument for including patients with a clinical diagnosis of COPD that did not require confirmation by spirometry, indicating that this reflects practice in primary care, where diagnosis is often made and treatment initiated on clinical grounds.
Strengths and limitations
Strengths of this review are the use of recognized systematic methods and a search without language or date restriction, which reduced the risk of bias in conducting the review. A limitation is that it was not possible to verify the content of the reported PR programs to ensure that they matched the definition adopted for this review.18 Due to heterogeneity among the studies and poor quality assessments relative to evidence-based medicine quality criteria it is not possible to provide clear evidence-based recommendations for practice. The scope of this review, inclusive of different study designs, provides a novel and broad insight into the extent and type of evidence in the field and can provide a useful stimulus for intervention developers and researchers.
Comparison with other studies
Our review supplements that of Jones et al37 by including a broad range of study designs and not requiring spirometry-confirmed diagnosis. A Cochrane review of referral, uptake, and adherence to PR has been registered recently and will add knowledge to this field.40
Whilst we cannot draw clear conclusions from our review about the efficacy of the interventions to increase referral and uptake to PR, these studies do address some of the known barriers and facilitators to referral and uptake.
Referral is impacted by accessibility of PR programs, HCPs’ knowledge of who and how to refer, the administrative burden of making a referral, successful previous referral of other patients, the influence of the referring doctor (either positive or negative), and by patients knowing what PR involves and how it will help their health.41 Interventions in this review supported clinicians through education and guidance to improve their knowledge of referral and PR,24,25,27,28,30,31,33,36 use of reminders and prompts,24,25 and the inclusion of PR referral in a discharge care bundle.27 Education and learning support were the most common features of interventions directly targeting clinicians though it is unclear whether the education programs addressed the nature of the conversation between the HCP and the patient about PR referral or supported clinician skills in this regard. None of the interventions addressed accessibility of PR programs and it can only be assumed that sufficient capacity was available.
Barriers to patient uptake include transport and location,42–44 inconvenient timing,42,44 disruption to routine/other priorities,41–43 influence of the referring doctor,42 lack of explanation of benefits,44 lack of perceived benefit,41,42,44 believing oneself to be too disabled44 or that one’s conditions is not serious enough,41,44 negative past experience with PR or exercise,44 and burden of COPD and other health conditions.41 Reasons for attending include a trusted, enthusiastic doctor who explained the benefits, perceived increased severity of the condition, perceiving that PR would help increase control and independence and improve health, and perceived social benefits.44 Positive reinforcement of PR by HCPs during the referral process is important.41 The study by Zwar et al,35 in which attendance at PR increased, provided individualized care plans and nurse support in patients’ homes, a model which could accommodate a personalized discussion over time about the benefits of PR to the patient and presumably establish a trusting relationship. However, Zwar et al35 noted that although more patients in the intervention group attended PR this was still less than a third of the group. Interestingly, the information session provided in the study by Graves et al,26 which informed patients about the benefits of PR, was associated with reduced attendance at assessment but did improve attendance of those who started PR. Whilst perhaps not providing motivational support for patients who were unsure about attending, it could nevertheless improve service efficiency and highlights the importance of considering the whole PR pathway. The manual of COPD evidence-based treatments provided by Harris et al34 was helpful for more socioeconomically disadvantaged patients and may have facilitated a constructive clinician–patient interaction for this group. The authors also noted that more patients in this group reported actually using the manual, which would clearly influence any impact assessment. This highlights the need for good understanding of how interventions work as well as whether they work. Practical factors such as transport, travel, and timing were not addressed by the interventions.
Strategies to improve referral and uptake have also been studied in cardiac rehabilitation (CR) with some success. A systematic review of interventions to promote uptake and adherence in CR reported improvements in eight out of 10 studies of uptake but, as in our review, the authors could not make clear practice recommendations due to heterogeneity and risk of bias in the studies.45 Another systematic review of interventions around referral and uptake to CR found 11 studies of referral and 13 studies of enrollment in the US, Canada, and the UK.46 The highest rates of referral (up to 85%) were found in studies that implemented automatic referral orders (eg, from healthcare records or data) whereas the highest rates of enrollment (up to 86%) were achieved with a combination of automatic and liaison methods, including discussion with an HCP. Enrollment and uptake to CR can also be improved by referral and structured follow-up by nurses or therapists and early outpatient education.45,47,48 Whether findings from CR might be translated to PR is worthy of further research. The rehabilitation pathway differs for CR because referrals typically occur at the time of hospitalization for an acute event or procedure, whereas in the UK, for example, most PR referrals occur in primary care at the time of stable disease.13
Implications for practice and research
There is a call to provide recommendations to increase the delivery of PR worldwide to validate novel techniques for doing so, and to enhance evidence-based policy.12 While more evidence is needed to establish the efficacy and effectiveness of different approaches, the studies reviewed here provide a useful platform for further work. The variety of interventions they represent, from one-off information sessions to system-wide improvement projects, reflects the complex nature of COPD care management and the potential value of a range of evidence building approaches.
Firstly, there is an urgent need for high quality study designs to determine the efficacy, effectiveness, and causal mechanisms of interventions. There is a lack of evidence from RCTs and we identified only one ongoing RCT to test a method not previously evaluated: a video to increase PR uptake following hospitalized exacerbations of COPD.49 Whilst RCTs are the gold standard for establishing a generalizable evidence base, they may not be the only relevant evaluation design in this field. There is a need to recognize contextual factors and the diversity of PR delivery and settings across the world.50 In this regard, quality improvement approaches are well suited to learn what works in a local context, particularly where rapid testing of novel interventions is needed. In contrast to research methods which aim to generate new knowledge, the aim of these approaches is to achieve positive and practical change in an identified service through focus on a well-defined problem.51 These methods are accessible to service providers in “real-world” settings. Two studies reviewed here, Hull et al28 and Hopkinson et al,27 utilized quality improvement methods. In addition, for the researcher, realist approaches that seek to identify what works, in which circumstances, and for whom could help to recognize and accommodate contextual complexity within the evaluation design and provide more transferable learning about the impact of contextual factors.52 Such methods have value in real-world settings where multiple variables cannot be controlled.
Secondly, there is a need to improve reporting of study populations as a factor to enhance external validity. Results from Harris et al34 suggest differential effects across subgroups of patients and this is worthy of further investigation. None of the studies in this review reported the ethnicity of patients. In an area of East London in the UK members of some Black and minority ethnic populations have lower rates of referral to PR compared to White patients53 and there is a need to understand more about how to support PR access in ethnically diverse communities. There may also be specific issues in resource poor countries54 which are not represented among the studies in this review.
Thirdly, in their study of a group opt-in session prior to assessment, Graves et al26 reported that, despite no impact on uptake, fewer intervention patients who started PR dropped out for reasons other than illness and significantly more graduated. This indicates the importance of considering the whole PR pathway. Following the patient through the entirety of their PR journey will lead to a greater understanding of how to improve service efficiency. Only two studies in this review intervened at the system level28,32 and there is scope for more research in this area. More studies measured referral than uptake and more patients were included in referral studies than in uptake studies, suggesting a differential focus on these two stages.
Fourthly, interventions may benefit from theory-based design. Cox et al41 used the Theoretical Domains Framework to analyze factors affecting referral and participation in PR and we have highlighted above how some of the reviewed studies addressed these factors, although it was not possible to asses this accurately without access to more detailed intervention descriptions. However, we believe that the work by Cox et al41 provides a useful theoretical framework for intervention designers. Interventions could focus on specific constructs that have been shown to have relevance and then assess the impact on those constructs to generate a theoretically informed understanding of what works and why.
Conclusion
This review demonstrates the broad range of approaches aimed at increasing referral and uptake to PR across primary and secondary care. Some positive results have been demonstrated but there is limited generalizable evidence because interventions and methods are heterogeneous and descriptions of populations are limited. Further theory-based testing of promising interventions using robust methods in various populations and settings is required to draw clear conclusions about how to optimize access to PR across a range of settings.
Supplementary material
MEDLINE search strategy
(((pulmonary rehabilitation.ti,ab.) or (((emphysema or copd or chronic obstructive pulmonary disease or chronic bronchitis or chronic asthma).ti,ab. or exp Pulmonary Disease, Chronic Obstructive/or exp Bronchitis, Chronic/or exp Asthma/or exp Emphysema/) and ((exercis* or rehab* or physiotherap* or “physical therap*”).ti,ab. or exp Exercise Therapy/or exp Exercise/or exp rehabilitation/or exp Physical Therapy Modalities/))) and ((refer* 1 or referring or referred or referral* or assess*).ti,ab. Or exp “Referral and Consultation”/) And ((rate* or number* or audit* or percentage or barrier* or facilitat* or frequen* or infrequent* or rare* or common* or uncommon or standard* or influenc* or reluctant* or barrier* or obstacle or (meet* adj3 criter*)).ti,ab. Or exp practice patterns, physicians/or exp guideline adherence or exp data collection/))
((pulmonary rehabilitation.ti,ab.) or (((emphysema or copd or chronic obstructive pulmonary disease or chronic bronchitis).ti,ab. or exp Pulmonary Disease, Chronic Obstructive/or exp Bronchitis, Chronic/or exp Emphysema/) and ((exercis* or rehab* or physiotherap* or “physical therap*”).ti,ab. or exp Exercise Therapy/or exp Exercise/or exp rehabilitation/or exp Physical Therapy Modalities/))) and ((uptake or up-take or (up adj3 take*) or non-attend* or nonattend* or attend* or engag* or (treat* adj3 refus*) or decline* or concordan* or complian* or barrier* or obstacle* or adher* or accept*).ti,ab. Or exp treatment refusal/or exp patient compliance/or exp patient acceptance of healthcare/)
or 2
((((Meta-Analysis as Topic/or Meta-Analysis/or exp Review Literature as Topic/) or ((meta analy$) or (metaanaly$) or ((systematic adj (review$1 or overview$1)))).tw. or (Cochrane or embase or psychlit or psyclit or psychinfo or psycinfo or cinahl or cinhal or (science citation index) or bids or cancerlit or reference list$ or bibliograph$ or hand-search$ or (relevant journals) or (manual search$)).ab. or ((selection criteria or data extraction).ab. and review/)) NOT (Comment/or Letter/or Editorial/)) Or (((Randomized Controlled Trials as Topic/or randomized controlled trial/or Random Allocation/or Double Blind Method/or Single Blind Method/or clinical trial/or exp Clinical Trials as topic/or PLACEBOS/) or ((clinical trial, phase i) or (clinical trial, phase ii) or (clinical trial, phase iii) or (clinical trial, phase iv) or (controlled clinical trial) or (randomized controlled trial) or (multicenter study) or (clinical trial)).pt or ((clinical adj trial$) or ((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)) or (placebo$) or (randomly allocated) or (allocated adj2 random$)).tw) NOT (case report.tw or letter/or historical article/))) or (quantitative or (mix* adj method*)).mp.
3 and 4
Acknowledgments
Delivery of this work was supported by the Cambridge Biomedical Research Centre.
Footnotes
Author contributions
JF, FE, IW, and CD conceived and designed the review. IK provided expert support and conducted the literature search. FE and IW reviewed the titles and abstracts, selected the papers, and extracted and analyzed the data. All authors were involved in drafting and revision of the manuscript for important intellectual content and approved the final version to be published. All authors agree to be accountable for aspects of the work. JF is the guarantor of the paper.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21(1):14–23. doi: 10.1111/resp.12660. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation [Accessed April 19, 2018]. [updated 2018]. Available from: http://www.who.int/respiratory/copd/burden/en/
- 3.British Lung Foundation Chronic obstructive pulmonary disease (COPD) statistics. [Accessed April 19, 2018]. Available from: http://statistics.blf.org.uk/copd.
- 4.Medical Directorate NHS, Commissioning Toolkit COPD. 2012. [Accessed September 25, 2018]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/212876/chronic-obstructive-pulmonary-disease-COPD-commissioning-toolkit.pdf.
- 5.Mccarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease (Review) Cochrane Database Syst Rev. 2015;2:CD003793. doi: 10.1002/14651858.CD003793.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steiner M, McMillan V, Lowe D. Pulmonary rehabilitation: beyond breathing better. National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme: outcomes from the clinical audit of pulmonary rehabilitation services in England 2015. London: RCP; 2017. [Google Scholar]
- 7.Seymour JM, Moore L, Jolley CJ, et al. Outpatient pulmonary rehabilitation following acute exacerbations of COPD. Thorax. 2010;65(5):423–428. doi: 10.1136/thx.2009.124164. [DOI] [PubMed] [Google Scholar]
- 8.Singh SJ, Zuwallack RL, Garvey C, Spruit MA. American Thoracic Society/European Respiratory Society Task Force on Pulmonary Rehabilitation. Learn from the past and create the future: the 2013 ATS/ERS statement on pulmonary rehabilitation. Eur Respir J. 2013;42(5):1169–1174. doi: 10.1183/09031936.00207912. [DOI] [PubMed] [Google Scholar]
- 9.Griffiths TL, Phillips CJ, Davies S, Burr ML, Campbell IA. Cost effectiveness of an outpatient multidisciplinary pulmonary rehabilitation programme. Thorax. 2001;56(10):779–784. doi: 10.1136/thorax.56.10.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax. 2013;68(Suppl 2):1–30. doi: 10.1136/thoraxjnl-2013-203808. [DOI] [PubMed] [Google Scholar]
- 11.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e15. doi: 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 12.Vogiatzis I, Rochester CL, Spruit MA, Troosters T, Clini EM. American Thoracic Society/European Respiratory Society Task Force on Policy in Pulmonary Rehabilitation. Increasing implementation and delivery of pulmonary rehabilitation: key messages from the new ATS/ERS policy statement. Eur Respir J. 2016;47(5):1336–1341. doi: 10.1183/13993003.02151-2015. [DOI] [PubMed] [Google Scholar]
- 13.Steiner M, Holzhauer-Barrie J, Lowe D, et al. National organisational audit report. London: RCP; 2015. Pulmonary rehabilitation: time to breathe better. National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme: resources and organisation of pulmonary rehabilitation services in England and Wales 2015. [Google Scholar]
- 14.Jongepier L, Barlow R. Pulmonary rehabilitation (PR) capacity, uptake and completion rate in the East of England. Eur Respir J. 2016;48(Suppl 60):3584. [Google Scholar]
- 15.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 [updated March 2011] London: The Cochrane Collaboration; 2011. [Accessed April 24, 2018]. Available from: http://handbook.cochrane.org. [Google Scholar]
- 16.Early F, Wellwood I, Kuhn I, Deaton C, Fuld J. A systematic review of literature on interventions to increase referral to and uptake of pulmonary rehabilitation programmes in people with chronic obstructive pulmonary disease (COPD) 2016. [Accessed April 24, 2018]. (PROSPERO 2016 CRD42016043762). Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42016043762. [DOI] [PMC free article] [PubMed]
- 17.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Institute for Health and Clinical Excellence Chronic obstructive pulmonary disease in over 16s: diagnosis and management. 2010. [Accessed April 24, 2018]. (Clinical guideline CG101). Available from: http://www.nice.org.uk/guidance/cg101.
- 19.Strings attached: Strings attached: CADTH database search filters [Internet] Ottawa: CADTH; 2016. [Accessed September 25, 2018]. Available from: https://www.cadth.ca/resources/finding-evidence/strings-attached-cadths-database-search-filters. [Google Scholar]
- 20.Early F, Wellwood I, Kuhn I, et al. P212 Interventions to increase referral to and uptake of pulmonary rehabilitation programmes for people with chronic obstructive pulmonary disease (COPD): a systematic review. Thorax. 2016;71(Suppl 3):A200–A201. doi: 10.2147/COPD.S172239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sterne JAC, Higgins JPT, Reeves BC on behalf of the development group for ACROBAT-NRSI A Cochrane Risk Of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI), Version 1.0.0. Sep 24, 2014. [Accessed September 25, 2018]. Available from: http://www.bristol.ac.uk/population-health-sciences/centres/cresyda/barr/riskofbias/robins-i/acrobat-nrsi/
- 23.Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7(1):10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Angus RM, Thompson EB, Davies L, et al. Feasibility and impact of a computer-guided consultation on guideline-based management of COPD in general practice. Prim Care Respir J. 2012;21(4):425–430. doi: 10.4104/pcrj.2012.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foster F, Piggott R, Riley L, Beech R. Working with primary care clinicians and patients to introduce strategies for increasing referrals for pulmonary rehabilitation. Prim Health Care Res Dev. 2016;17(3):226–237. doi: 10.1017/S1463423615000286. [DOI] [PubMed] [Google Scholar]
- 26.Graves J, Sandrey V, Graves T, Smith DL. Effectiveness of a group opt-in session on uptake and graduation rates for pulmonary rehabilitation. Chron Respir Dis. 2010;7(3):159–164. doi: 10.1177/1479972310379537. [DOI] [PubMed] [Google Scholar]
- 27.Hopkinson NS, Englebretsen C, Cooley N, et al. Designing and implementing a COPD discharge care bundle. Thorax. 2012;67(1):90–92. doi: 10.1136/thoraxjnl-2011-200233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hull S, Mathur R, Lloyd-Owen S, Round T, Robson J. Improving outcomes for people with COPD by developing networks of general practices: evaluation of a quality improvement project in east London. NPJ Prim Care Respir Med. 2014;24(1):14082. doi: 10.1038/npjpcrm.2014.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roberts CM, Gungor G, Parker M, Craig J, Mountford J. Impact of a patient-specific co-designed COPD care scorecard on COPD care quality: a quasi-experimental study. NPJ Prim Care Respir Med. 2015;25(1):15017. doi: 10.1038/npjpcrm.2015.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lange P, Rasmussen FV, Borgeskov H, et al. The quality of COPD care in general practice in Denmark: the KVASIMODO study. Prim Care Respir J. 2007;16(3):174–181. doi: 10.3132/pcrj.2007.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lange P, Andersen KK, Munch E, et al. Quality of COPD care in hospital outpatient clinics in Denmark: the KOLIBRI study. Respir Med. 2009;103(11):1657–1662. doi: 10.1016/j.rmed.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 32.Tøttenborg SS, Thomsen RW, Nielsen H, Johnsen SP, Frausing Hansen E, Lange P. Improving quality of care among COPD outpatients in Denmark 2008–2011. Clin Respir J. 2013;7(4):319–327. doi: 10.1111/crj.12009. [DOI] [PubMed] [Google Scholar]
- 33.Ulrik CS, Hansen EF, Jensen MS, et al. Management of COPD in general practice in Denmark – participating in an educational program substantially improves adherence to guidelines. Int J COPD. 2010;5:73–79. doi: 10.2147/copd.s9102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harris M, Smith BJ, Veale AJ, Esterman A, Frith PA, Selim P. Providing reviews of evidence to COPD patients: controlled prospective 12-month trial. Chron Respir Dis. 2009;6(3):165–173. doi: 10.1177/1479972309106577. [DOI] [PubMed] [Google Scholar]
- 35.Zwar NA, Hermiz O, Comino E, et al. Care of patients with a diagnosis of chronic obstructive pulmonary disease: a cluster randomised controlled trial. Med J Aust. 2012;197(7):394–398. doi: 10.5694/mja12.10813. [DOI] [PubMed] [Google Scholar]
- 36.Deprez R, Kinner A, Millard P, Baggott L, Mellett J, Loo JL. Improving quality of care for patients with chronic obstructive pulmonary disease. Popul Health Manag. 2009;12(4):209–215. doi: 10.1089/pop.2008.0043. [DOI] [PubMed] [Google Scholar]
- 37.Jones AW, Taylor A, Gowler H, O’Kelly N, Ghosh S, Bridle C. Systematic review of interventions to improve patient uptake and completion of pulmonary rehabilitation in COPD. ERJ Open Res. 2017;3(1):00089–2016. doi: 10.1183/23120541.00089-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jones RCM, Dickson-Spillmann M, Mather MJC, Marks D, Shackell BS. Accuracy of diagnostic registers and management of chronic obstructive pulmonary disease: the Devon primary care audit. Respir Res. 2008;9(1):62. doi: 10.1186/1465-9921-9-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baxter N, Holzhauer-Barrie J, McMillan V, Saleem Khan M, Skipper E, Roberts CMI. Time to take a breath. National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme: clinical audit of COPD in primary care in Wales 2014–2015 National clinical audit report. London: RCP; 2016. [Google Scholar]
- 40.Young J, Jordan RE, Adab P, Enocson A, Jolly K. Interventions to promote referral, uptake and adherence to pulmonary rehabilitation for people with chronic obstructive pulmonary disease (COPD) (protocol) Cochrane Database Syst Rev. 2017;10:CD012813. [Google Scholar]
- 41.Cox NS, Oliveira CC, Lahham A, Holland AE. Pulmonary rehabilitation referral and participation are commonly influenced by environment, knowledge, and beliefs about consequences: a systematic review using the Theoretical Domains Framework. J Physiother. 2017;63(2):84–93. doi: 10.1016/j.jphys.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 42.Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8(2):89–99. doi: 10.1177/1479972310393756. [DOI] [PubMed] [Google Scholar]
- 43.Mathar H, Fastholm P, Hansen IR, Larsen NS. Why do patients with COPD decline rehabilitation. Scand J Caring Sci. 2016;30(3):432–441. doi: 10.1111/scs.12268. [DOI] [PubMed] [Google Scholar]
- 44.Sohanpal R, Steed L, Mars T, Taylor SJC. Understanding patient participation behaviour in studies of COPD support programmes such as pulmonary rehabilitation and self-management: a qualitative synthesis with application of theory. NPJ Prim Care Respir Med. 2015;25(1):15054. doi: 10.1038/npjpcrm.2015.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karmali KN, Davies P, Taylor F, Beswick A, Martin N, Ebrahim S. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev. 2014;6:CD007131. doi: 10.1002/14651858.CD007131.pub3. [DOI] [PubMed] [Google Scholar]
- 46.Gravely-Witte S, Leung YW, Nariani R, et al. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nat Rev Cardiol. 2010;7(2):87–96. doi: 10.1038/nrcardio.2009.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clark AM, King-Shier KM, Duncan A, et al. Factors influencing referral to cardiac rehabilitation and secondary prevention programs: a systematic review. Eur J Prev Cardiol. 2013;20(4):692–700. doi: 10.1177/2047487312447846. [DOI] [PubMed] [Google Scholar]
- 48.Grace SL, Angevaare KL, Reid RD, et al. Effectiveness of inpatient and outpatient strategies in increasing referral and utilization of cardiac rehabilitation: a prospective, multi-site study. Implement Sci. 2012;7(1):120. doi: 10.1186/1748-5908-7-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jones S. Video to increase rehabilitation uptake following hospitalised exacerbations of COPD: a randomised controlled trial. ISRCTN. 2015. [Accessed October 02, 2018]. Available from: http://www.isrctn.com/ISRCTN13165073.
- 50.Spruit MA, Pitta F, Garvey C, et al. Differences in content and organisational aspects of pulmonary rehabilitation programmes. Eur Respir J. 2014;43(5):1326–1337. doi: 10.1183/09031936.00145613. [DOI] [PubMed] [Google Scholar]
- 51.Portela MC, Pronovost PJ, Woodcock T, Carter P, Dixon-Woods M. How to study improvement interventions: a brief overview of possible study types. BMJ Qual Saf. 2015;24(5):325–336. doi: 10.1136/bmjqs-2014-003620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pawson R, Tilley N. Realistic Evaluation. London: Sage; 2013. [Google Scholar]
- 53.Martin A, Badrick E, Mathur R, Hull S. Effect of ethnicity on the prevalence, severity, and management of COPD in general practice. Br J Gen Pract. 2012;62(595):e76–e81. doi: 10.3399/bjgp12X625120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Desalu OO, Onyedum CC, Adeoti AO, et al. Guideline-based COPD management in a resource-limited setting – physicians’ understanding, adherence and barriers: a cross-sectional survey of internal and family medicine hospital-based physicians in Nigeria. Prim Care Respir J. 2013;22(1):79–85. doi: 10.4104/pcrj.2013.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]