Abstract
The influence of adverse childhood experiences (ACEs), which often include childhood exposure to maltreatment and household dysfunction, on health risk behaviors during young adulthood has been widely documented. A vulnerability marker for the increased risky behaviors among young ACEs victims such as impulsivity remains to be explored. The present study investigated how different profiles of ACEs influence impulsivity in young adulthood. Respondents were young people (N =336; ages 18–25) who were recruited from the community. Latent class analysis (LCA) was used to identify subpopulations of individuals based on varying exposure to 13 types of ACEs, including childhood maltreatment, household dysfunction, and community violence. Four distinct classes emerged: Low ACEs (56%), Household Dysfunction/Community Violence (14%), Emotional ACEs (14%), and High/Multiple ACEs (16%). Multiple regression analyses found that compared to those in the Low ACEs class, young adults in the Emotional ACEs and High/Multiple ACEs respectively, reported increased levels of negative urgency, controlling for sociodemographic characteristics and other impulsivity traits. This result suggest that childhood exposure to multiple ACEs at high levels is particularly related to impulsive self-control in the context of intense negative emotionality.
Keywords: Adverse childhood experiences (ACEs), Impulsivity, Negative Urgency, Child Maltreatment, Polyvictimization, Latent Class Analysis
Introduction
Exposure to adverse childhood experiences (ACEs), such as child maltreatment and family dysfunction (e.g., domestic violence, incarcerated family members), is highly prevalent. A Center for Disease Control and Prevention (CDC) study, analyzing 26,229 adults in five states, found that the majority of the adults (59.4%) experienced at least one ACEs prior to age 18, whereas 8.7% of participants reported experiencing five or more ACEs (Bynum et al., 2010). Population-based studies, such as the original Adverse Childhood Experiences (ACE) study, have revealed that population attributable health risk associated with ACEs was 54% for adult depression, 65% for alcoholism, 67% for suicide attempts, and 50% for substance use (Chapman et al., 2004; Dube et al., 2003; Felitti et al., 1998).
Since ACEs is a major public health issue, a substantial body of literature has been devoted to identifying consequences of exposure to ACEs. For example, many studies have found that poor self-regulation, such as impulsivity, is one of the developmental sequelae of exposure to ACEs (Beers & De Bellis, 2002; Cicchetti & Curtis, 2005; Narvaez et al., 2012; Pears & Fisher, 2005). Impulsivity is defined as a personality trait related to reacting rapidly or in unplanned ways to behavioral or emotional stimuli without proper regard for negative impacts (Moeller, Barratt, Dougherty, Schmitz, & Swann, 2001). ACEs have been closely related to impulsivity like negative urgency, which is often defined as the propensity to act on impulses, often under the influence of distress (Brodsky et al., 2001; Carrion, Garrett, Menon, Weems, & Reiss, 2008; De Bellis, Hooper, Spratt, & Woolley, 2009; Jovanovic et al., 2013; Lewis, Dozier, Ackerman, & Sepulveda-Kozakowski, 2007; Majer, Nater, Lin, Capuron, & Reeves, 2010; Mueller et al., 2012; Roy, 2005). ACEs victims demonstrate impulsivity, even in the absence of psychiatric disorders, including posttraumatic stress disorder (PTSD) (Brandes et al., 2002; Navalta, Polcari, Webster, Boghossian, Teicher, 2006; Stein, Kennedy, & Twamley, 2002; Twamley, Hami, & Stein, 2004). This suggests that psychiatric symptoms may not exclusively explain the adverse effects of ACEs on impulsive behavioral and emotional reactions (Bücker et al., 2012). Recent neurobiological studies have also confirmed that exposure to ACEs alters stress-response systems (Sinha, 2008, 2009) and impairs neurocognitive functioning, such as inhibitory control and working memory (Gould et al., 2012; Jaffee & Maikovich-Fong, 2011; Nemeroff, 2004), which might render ACEs victims more vulnerable to the development of impulsive personality traits.
Self-regulation processes attained in childhood as a result of person-context transactions are hierarchically incorporated within and among a developing child and have enormous impacts on subsequent development and lifelong health (Cicchetti & Valentino, 2006; Masten & Coatsworth, 1998; Zimmerman, 2000). Indeed, poor self-regulation processes, such as impulsivity, is one of the main components of victimized individuals’ vulnerability to a variety of risky health behaviors, such as substance use, unsafe sexual activity, and unhealthy dietary behaviors (Dick et al., 2010; Kendall-Tackett, 2002; Riggs, Sakuma, & Pentz, 2007). Recent studies exploring the paths between ACEs and substance use among young individuals discovered that impulsive personality traits found among ACEs victims significantly increased an individual’s risk for substance use in young adulthood (Oshri et al., 2017; Wardell, Strang, & Hendershot, 2016). Given the critical role impulsivity plays in lifelong health and well-being, it is important to further understand how exposure to ACEs is associated with impulsivity.
There is well-established evidence in child development research that when children are exposed to ACEs, the majority of children suffer not just one but several types of ACEs (Costello, Erkanli, Fairbank, & Angold, 2002; Finkelhor, Ormrod, & Turner, 2007; Liaw & Brooks-Gunn, 1994; Rutter, 1981; Sameroff, Seifer, Baldwin, & Baldwin, 1993). The National Survey of Children’s Exposure to Violence (NatSCEV) found that one in two children aged 2–17 in a nationally representative sample (N = 4,549) experienced at least two types of ACEs in a single year (Turner, Finkelhor, & Ormrod, 2010). Additionally, the original ACE study (N = 17,337 adults) found that among those participants reporting at least one type of ACEs, nearly two-thirds (62%) reported experiencing more than two different types of ACEs, whereas nearly a quarter (24%) reported experiencing more than four types of ACEs (Anda et al., 2002; Dube et al., 2006; Felitti, 2002). The negative consequences of ACEs on self-regulation processes can be even more pronounced with multiple exposures to different patterns of ACEs (Lynch & Cicchetti, 1998; Sameroff & Rosenblum, 2006). Despite these findings about widespread co-occurrence of ACEs, few studies have examined how different ACEs types might cluster together and how these clusters of ACEs are associated with different impulsivity traits.
Since previous studies of ACEs and impulsivity have often had a unitary view of impulsivity, making distinctions among patterns of ACEs and their relative associations to different impulsivity-related personality traits was challenging. From an intervention perspective, it is important to know which of these ACEs types exert the greatest impact on which personality traits of impulsivity (e.g., non-planning impulsivity versus impulsivity to seek out novel sensations). Furthermore, classifying individuals based on ACEs patterns and examining the associations between the ACEs patterns and different impulsivity-related personality traits might increase our understanding of the developmental effects of ACEs on impulsivity.
Since person-centered approaches, such as latent class analysis (LCA), allow for identifying unobserved groups of individuals with similar characteristics of ACEs exposure, researchers are better able to empirically identify only those patterns of ACEs exposure that occur most frequently in a given sample and classify individuals into classes (i.e., groups). Specific classes contain individuals that are similar to each other in ACEs patterns and different from individuals in other classes. While previous ACEs studies have used different types of ACEs in classifying ACEs patterns, making it difficult to compare findings to each other, the utility of LCA for classifying patterns of s exposure among young people has already been demonstrated. For example, Ford et al. (2013) identified three latent classes of ACEs exposure patterns in a sample of 1,595 youths (ages 10–16) in juvenile detention facilities: (1) low adversity; (2) relative moderate adversity; and (3) poly-victims. Another adult LCA study of a nationally representative sample of 34,653 adults, identified five classes of ACEs exposure that were based on the nine types of ACEs exposure, primarily family violence and caregiver maladjustment (e.g., parental incarceration substance use) (Roos et al., 2016). These classes included: (1) low adversity; (2) caregiver substance use and neglect; (3) physical and emotional maltreatment; (4) multiple exposure to maltreatment and caregiver substance use; and (5) caregiver maladjustment. These studies also found that compared to the low adversity class, polyvictimized classes had increased risk for adverse outcomes, including mental illness and incarceration.
The present study investigated whether discrete classes of individuals who endorse similar patterns of ACEs exposure can be identified in a community sample of young adults. We then examined how these patterns of ACEs might be related to four distinct facets of impulsivity, including urgency, lack of premeditation, lack of perseverance, and sensation seeking. For more stringent evaluation of the relationship between ACEs patterns and impulsivity, our study included 13 different types of ACEs exposure compared to 10 used in previous studies, including six types of child abuse and neglect, five types of household dysfunction (e.g., mental illness, incarcerated family members), and two types of community violence. Furthermore, in order to evaluate the utility of our classification of ACEs, we examined whether the present group assignment based on ACEs patterns was associated with psychological symptoms and alcohol problems, both well-known health outcomes of ACEs.
Method
Participants and procedure
Participants were recruited through community advertisements targeting young adults, ages 18–25 in a Northeastern metropolitan area of the United States. Flyers were distributed in public areas around the community, including shared bulletin boards, two- and four-year college campuses, and local businesses. Individuals who responded were given a phone screening and determined eligible if their ages were between 18 and 25 and self-reported current physical health status as either good or excellent. Respondents with poor health were excluded in our study because medical disorders could affect brain and cognitive development, which in turn could influence impulsive personality development. Trained interviewers administered hour-long, structured, in-person interviews to eligible participants, and data were collected from a sample of 335 interviewees with an average age of 21.7(SD=2.1).Over half(58.2%)wereWhiteand51.5% were female. All respondents provided written informed consent upon completion of a thorough review of study requirements with a trained interviewer. university Institutional Review Board comprehensively reviewed and approved all study procedures.
Measures
ACEs.
Multiple measures were used to replicate original ACE study items (i.e., five household dysfunctions and five maltreatment types), and to examine additional ACEs not included (i.e., gang violence, property crime, and caregiver verbal offense). The Childhood Trauma Questionnaire (CTQ; 25 items) was used to measure types of maltreatment, including emotional, physical and sexual abuse, and emotional and physical neglect (Bernstein & Fink, 1998). CTQ internal consistencies (measured using Cronbach’s α) ranged from .71 for neglect to .89 for emotional abuse. project-developed binary item assessed the witnessing of past domestic violence, “watched domestic violence in your family?” Additionally, household alcohol abuse and drug abuse were separately examined using two items adapted from the 6-item Children of Alcoholics Screening Test (Hodgins, Maticka-Tyndale, el-Guebaly, & West, 1993): “Have you ever thought that one of your parents had drinking” or “drug problems?” Household mental health was measured using four items developed for the present study. Respondents were coded “yes” on mental illness if they identified a biological father or mother with depression or any other mental illnesses. Furthermore, family member incarceration was assessed using two items: “Did your parents/caregivers go to prison?” and “Did other household member go to prison?”. Respondents were coded “yes” on household incarceration after endorsing at least one incarceration item. The Verbal Aggression Scale (VAS; 15 items) was used to examine verbal offense. Included items (e.g., swear, insult, threaten, humiliate) measured the frequency of parental verbal aggression (Tomoda et al., 2011). An established cutoff score was used to identify participants exposed to a substantial degree of verbal offense (Polcari, Rabi, Bolger, & Teicher, 2014). Finally, property victimization was assessed using two items, “has anyone ever attempted to rob you” or “actually robbed you?” Gang violence exposure was explored using two items (i.e., witnessed gang violence or a drive-by shooting). Participants were coded “yes” on property victimization and gang violence, respectively, after endorsing at least one item for each construct.
Impulsivity.
We measured impulsivity using the Urgency, Premeditation, Perseverance, and Sensation Seeking (UPPS) Impulsive Behavior scale (Whiteside & Lynam, 2001). The UPPS (45 items) defines impulsivity through the following four unique characteristics, each represented by its own subscale: negative urgency (e.g., when I feel bad, I will often do things I later regret in order to make myself feel better now), lack of premeditation (e.g., I am one of those people who blurt out things without thinking), lack of perseverance (e.g., I tend to give up easily), and sensation seeking (e.g., I quite enjoy taking risks). Scores were computed for each impulsivity trait; higher UPPS scale scores indicate a more impulsive personality. The UPPS scale has demonstrated adequate reliability and validity (Magid & Colder, 2007; Whiteside & Lynam, 2001; Whiteside, Lynam, Miller, & Reynolds, 2005). For the current sample, estimates of internal consistency reliability for the four scales ranged from .71 to 92.
Covariates.
The Brief Symptom Inventory 18 (BSI-18; 18 items) was used to assess psychological symptoms. The BSI-18 measures the presence of three characteristics of distress within the last seven days (i.e., somatization, depression, and anxiety). Higher BSI scores indicate the presence of more psychological symptoms (Derogatis, 1993). Internal consistency of the BSI-18 for the current sample was .92 (measured using Cronbach’s α). Alcohol use was measured using The Alcohol Use Disorders Identification Test (AUDIT; 10 items), which was developed to screen participants for hazardous and harmful patterns of alcohol consumption (Saunders, Aasland, Babor, Fuente, & Grant, 1993). Seven items examined past experiences of alcohol-related problems (e.g., “Have you or someone else been injured as a result of your drinking?”), while three items assessed frequency of alcohol consumption (e.g., “How often do you have a drink containing alcohol?”). A total score was calculated by summing the endorsed items. The AUDIT has been widely used in addiction research and has good psychometric properties (Aertgeerts et al., 2000; Reinert & Allen, 2007; Selin, 2003). The AUDIT’s internal consistency for the current sample was .75.
Demographic variables.
Demographic information, including age, gender, race/ethnicity, and family income was gathered using a self-reported structured questionnaire.
Data Analysis
ACEs classes were identified through the exploratory approach of latent class analysis (LCA) using Mplus version 7.3 (Muthén & Muthén, 2016). Using the 13 ACEs items, the 1-class model was tested first; then, the number of classes was systematically increased until the best fitting model was identified. Parameters were estimated using the maximum likelihood estimation with robust standard errors (Little & Rubin, 1987). The best-fitting model was determined by examining the following model fit statistics: Akaike information criteria (AIC) (Akaike, 1974), Bayesian information criterion (BIC) (Schwarz, 1978), adjusted BIC, Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (LMRT) (Lo, Mendell, & Rubin, 2001), and Bootstrapped Likelihood-Ratio Test (BLRT) (Arminger, Stein, & Wittenberg, 1999). For AIC and BIC, smaller values indicate better model fit. LMRT and BLRT statistics evaluate the fit of a target model (e.g., 4 class model) to a comparison model that is one class less than (e.g., 3 class model) the target, and the p-values associated with these statistics indicate whether the target solution (p < .05) or comparison model (p > .05) provides a better fit to the data. In addition to model fit statistics, we considered the theoretical meaningfulness of the classes (Nylund, Asparouhov, & Muth´en, 2007) and proportion of participants represented in the classes (Hipp & Bauer, 2006).
After determining the best fitting model, the association between a set of demographic covariates and class membership was assessed using the modified three-step Mplus procedures (R3STEP auxiliary command) recommended by Asparouhov and Muthén (2014) and Härtwig, Crayen, Heuser, and Eid (2014) to ensure that the effects of the covariates on the classes were minimally biased. This approach takes into account measurement error associated with the most likely class membership, while preserving the stability of class formation. As an additional check of the validity of the LCA solutions, one-way analysis of variance (ANOVA) was used to identify mean differences in psychological and alcohol use outcomes among the four classes. Bonferroni corrections for multiple comparisons were used since multiple testing increases the probability of declaring false significance (Shaffer, 1995). Given the high entropy of the best-fitting model, most likely class membership was used as an observed variable to explore class differences (Clark & Muthén, 2009). Finally, we conducted a series of regression models to examine the relationship between class on four traits of impulsivity, while accounting for the effects of demographics and family income. For these models, participants’ most likely class memberships were transformed into dummy variables, which were then entered into the regression models alongside the covariates (Clark & Muthen, 2009).
Results
As shown in Table 1, results of the LCA determined that the 4-class solution described the optimal number of ACE typologies, with significant LMR (p= .03) and BLR (p<.001) tests. The 4-class solution exhibited high entropy (85%), and the average posterior class membership probability scores were excellent across groups (.88 – .95; Table 2). Figure 1 shows the four ACE typologies and item-response probabilities for the 13 childhood ACEs for each class. he most prevalent class (Class 1) was labeled Low ACEs (56% of sample). Participants in this class had low probabilities (.005 – .22) of all ACEs. The remaining 149 participants were rather equally distributed across the other three classes. Class 2 (14% of sample) was labeled Home Dysfunction/Community Violence ACEs. This group had the highest probability of endorsing exposure to household alcohol abuse (.71) and property crime (.65), and was differentiated from Classes 3 and 4 by low probabilities of direct physical victimization and neglect, and exposure to verbal aggression. Class 3, Emotional ACEs (14% of sample), was distinguished by moderate probabilities of exposure to emotional victimization and by low probabilities of exposure to family-focused adversities. Lastly, individuals in Class 4 had the highest probabilities of endorsing 11 out of the 13 ACEs, and was labeled High Multiple ACEs (16% of sample). Specifically, this group was characterized by moderate to high probabilities of direct childhood victimization, including emotional abuse (.94), and physical abuse (.77) and neglect (.74) as well as moderate probabilities (.40 – .64) of exposure to family- (i.e., household alcohol and drug abuse, IPV, incarceration, verbal aggression) and community-focused adversities (i.e., property crime, gang violence).
Table 1.
Fit statistics for the unconditional latent class analyses for 1–5 classes
| ClassNo. of FreeLog- Parameters likelihood |
AIC | BIC | N-adj BIC |
Entropy | LMRT |BLRT p-value |
No. classes with n<5% study sample |
||
|---|---|---|---|---|---|---|---|---|
| 1 | 13 | −2246.21 | 4518.41 | 4567.99 | 4526.76 | N.A. | N.A. | |
| 2 | 27 | −1913.11 | 3880.26 | 3983.20 | 3897.55 | 0.88 | 0|0 | 0 |
| 3 | 41 | −1868.24 | 3818.48 | 3974.86 | 3844.80 | 0.88 | .02|0 | 0 |
| 4 | 55 | −1837.00 | 3800.01 | 4040.29 | 3840.30 | 0.85 | .03|0 | 0 |
| 5 | 69 | −1805.31 | 3748.62 | 4011.79 | 3792.92 | 0.88 | .05|.05 | 1 |
Note: Final solutions are in bold. AIC= Akaike information criterion; BIC= Bayesian information criterion; N-adj = sample size adjusted; LMRT= Lo-Mendell-Rubin test; BLRT =Bootstrap Likelihood Ratio Test.
Table 2.
Average latent class probabilities for most likely latent class membership (row) by latent class (column).
| Class 1 | Class 2 | Class 3 | Class 4 | |
|---|---|---|---|---|
| Class 1: Low ACEs | 94% | 4% | 2% | 0% |
| Class 2: Home Dysfunction/Community Violence | 8% | 87% | 1% | 4% |
| Class 3: Emotional ACEs | 5% | 2% | 88% | 5% |
| Class 4: High Multiple ACEs | 0% | 3% | 2% | 95% |
Fig. 1.
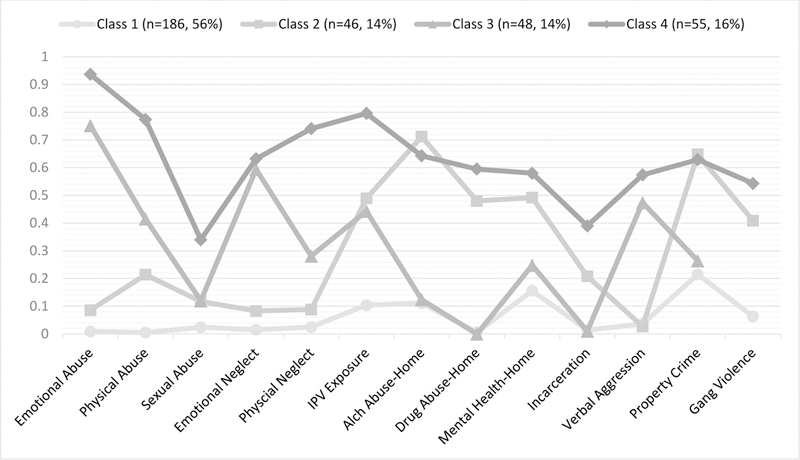
Item-response probabilities for 13 childhood ACEs across the four classes. Note: Class 1 = Low ACEs; Class 2 = Home Dysfunction/Community Violence; Class 3=Emotional ACEs; Class 4= High Multiple ACEs.
Several demographic factors were shown to influence the likelihood of membership in the different ACE classes. When comparing the victimized classes to the Low ACEs class, higher household income was associated with a decreased likelihood of membership in all three victimization classes (Class 2 odd ratio (OR) = .58; Class 3 OR= .47; Class 4 OR= .61). However, SES did not influence the likelihood of membership in the High Multiple ACEs class when the Household Dysfunction/Community Violence ACEs or Emotional ACEs classes were used as the reference group. Furthermore, participant age and gender were also associated with class membership. As participant age increased, the likelihood of membership in the High Multiple ACEs group increased (OR = 1.32; confidence interval (CI; 1.10–1.60). Finally, compared to the Low ACEs classes, participants in the High Multiple ACEs class were more likely to be female (OR = 1.88). Racial minority status was not significantly associated with class membership in any of the models.
The utility of our classification of ACEs was demonstrated in that class assignment based on ACEs patterns was associated with psychological symptoms and problematic alcohol use. The one-way ANOVAs for psychological symptoms (F (3, 331) = 17.66, p < .001) and problematic alcohol use (F (3, 295) = 12.01, p < .001) were statistically significant. he High Multiple ACEs class had the highest mean scores across outcomes. Post-hoc comparisons identified several significant mean differences among the classes. Specifically, the mean psychological symptoms score for the High Multiple ACEs class (58.4) was significantly higher than the Low (47.7) and Home Dysfunction/Community Violence ACEs (51.2) classes, but not the Emotional ACEs (53.8) class. Post-hoc comparisons revealed that the Emotional ACEs class, on average, had significantly higher levels of psychological symptoms than the Low ACEs class. In addition, post-hoc comparisons revealed that the mean problematic alcohol use score for the High Multiple ACEs (17.3) class was significantly higher than the mean scores for the Low (7.58) and Emotional ACEs (7.64) classes, but not the Home Dysfunction/Community Violence ACEs (11.6) class.
Finally, we examined the associations between ACE classes and different impulsivity traits using a series of linear regression models (Table 3). These models were estimated by entering the class variable and covariates simultaneously for each impulsivity variable. Class membership was dummy coded to compare young adults in the four ACEs classes. First, we conducted regression analyses using Low ACEs as the reference group. Then, Home Dysfunction/Community Violence ACEs, and Emotional ACEs were respectively entered as the reference groups to examine potential differences among ACEs classes. Compared to Low ACEs, both High Multiple ACEs (β=.27, p<.001) and Emotional ACEs (β=.11, p<.05) were significantly associated with higher levels of negative urgency, after controlling for demographics, family income, and other impulsivity dimensions. Since the present study considered impulsivity as a multi-dimensional construct that can overlap in each individual, other impulsivity dimensions were adjusted in our analyses. High Multiple ACEs was also associated with higher levels of negative urgency than those of Emotional ACEs and Home Dysfunction/Community Violence ACEs, respectively. Furthermore, compared to young adults with xposure to Emotional ACEs, those in the Home Dysfunction/Community Violence ACEs had higher levels of sensation seeking (β=.14, p<.05), after adjusting for demographics, family income, and other impulsivity dimensions. No significant associations were found for class membership and premeditation or perseverance.
Table 3.
Regression analyses indicating the relationship between ACEs classes and young adult outcomes.
| Negative urgency |
Premeditation |
Perseverance |
Sensation-seeking |
|
|---|---|---|---|---|
| β (SE) | β (SE) | β (SE) | OR (CI) | |
| Age | −0.02 (0.27) | 0.05 (0.25) | 0.00 (0.21) | −0.15 (0.36)* |
| Gender (female) | 0.04 (0.96) | 0.07 (0.86) | −0.07 (0.72) | −0.29 (1.23)*** |
| Racial minority | −0.07 (0.97) | −0.15 (0.86)** | 0.07 (0.73) | 0.04 (1.30) |
| Family SES | 0.01 (0.60) | 0.09 (0.54) | 0.01 (0.45) | 0.04 (0.80) |
| Educational level | −0.06 (0.50) | −0.07 (0.45) | 0.01 (0.38) | 0.11 (0.67) |
| Negative urgency | --- | 0.15 (0.05)* | 0.39 (0.04)*** | 0.15 (0.07)* |
| Premeditation | 0.14 (0.06)* | --- | 0.37 (0.04)*** | 0.21 (0.08)** |
| Perseverance | 0.39 (0.07)*** | 0.39 (0.06)*** | --- | −0.15 (0.10)* |
| Sensation-seeking | 0.12 (0.04)* | 0.17(004)*** | 0.12 (0.03)* | --- |
| ACEs Classes | ||||
| House/Community ACEs | 0.04 (1.38)a | 0.02(1.24) | −0.03 (1.04) | 0.04 (1.85)a |
| Emotional ACEs | 0.11 (1.37)*, b | 0.06 (1.24) | 0.02 (1.04) | −0.10 (1.84)a |
| High/Multiple ACEs | 0.27 (1.39)*** ab | 0.06 (1.24) | −0.10 (1.09) | 0.01 (1.93) |
p < 0.05;
p < 0.01;
p < 0.001.
Adjusted R2: Negative urgency (.34); Premeditation (.29); Perseverance (.34); Sensation-seeking (.14) Note: All regression analyses were controlled for demographics, family income, and other impulsivity traits. Statistics sharing a common superscript in ACEs classes note significantly different effect sizes for post-hoc analyses where Household Dysfunction/Community ACEs and Emotional ACEs were used as the reference group.
Discussion
The goal of the current study was to contribute to the emerging literature on multiple exposures to Es by identifying latent classes of ACEs and examining the associations between ACEs classes and four impulsivity-related personality traits in a community sample of young adults. Four classes of ACEs were identified, including Low ACEs, Home Dysfunction/Community Violence ACEs, Emotional ACEs, and High Multiple ACEs. We found that participants in the High Multiple ACEs class demonstrated the highest levels of psychological symptoms and problematic drinking behaviors. Furthermore, compared to Low ACEs, both Emotional ACEs and High Multiple ACEs, respectively, were significantly associated with increased levels of negative urgency, controlling for sociodemographic characteristics and other impulsivity traits, such as sensation seeking and (lack of) premeditation and perseverance.
We found that individuals in the High Multiple ACEs class had significantly higher levels of negative urgency than those in the Low ACEs class. Our findings suggest that among four personality traits of impulsivity, childhood exposure to high levels of multiple life stressors particularly relates to impulsive behavioral control in the context of intense negative emotional arousal. This is consistent with previous studies demonstrating that negative urgency is among the various impulsivity dimensions most closely linked to childhood adversity (Oshri et al., 2017; Wardell et al., 2016). The trait of negative urgency is characterized by both negative emotionality and impulsiveness within the NEO Personality Inventory-Revised (NEO PI-R) dimension of Neuroticism (Costa & McCrae, 1992). Individuals with a personality trait of negative urgency are likely to interpret ordinary situations as threatening and often fail to respond properly to stressors, which are frequently cited developmental sequelae of cumulative exposure to severe ACEs (Cyders & Smith, 2007; Jaffee, Caspi, Moffitt, Polo-Tomas, & Taylor, 2007; Pollak, Cicchetti, Hornung, & Reed, 2000; Shields & Cicchetti, 1998).
There are several theoretical models predicting that exposure to multiple and severe ACEs leads to individual adaptations that decrease emotional self-regulation and increase the probability of developing the personality trait of negative urgency. For example, according to the cumulative stressors model, victimized children, even those with considerable individual resilience, tend to display impulsive behaviors under conditions of multiple exposures to severe types of ACEs (Rutter, 1981; Sameroff & Rosenblum, 2006; Thibodeau, Cicchetti, & Rogosch, 2015). The stress-vulnerability model also posits that early exposure to severe and multiple ACEs exerts overwhelming demands on neural processes and alters individual stress-response systems (Daughters, Richards, Gorka, & Sinha, 2009; Fox, Hong, Siedlarz, & Sinha, 2008; Sinha, 2008, 2009). Because regaining homeostasis is difficult to achieve due to the altered stress-response systems, additional exposure to ACEs induces morphological and functional modifications in brain regions including the limbic system and prefrontal cortex that affect emotion regulation and impulse control (Andersen & Teicher, 2009; De Bellis & Zisk, 2014; Prasad, Kramer, & Ewing-Cobbs, 2005; Teicher et al., 2003). Thus, exposure to high and multiple ACEs and related alterations in the brain may instigate behavioral difficulties in handling stressful situations and modulating emotions, which is a textbook definition of negative urgency (Whiteside & Lynam, 2001). While numerous studies have found that CEs are associated with behavioral self-control and ability to delay gratification (Brodsky et al., 2001; De Bellis et al., 2009; Lewis et al., 2007; Mueller et al., 2012; Roy, 2005), the current study found that exposure to multiple childhood adversities is particularly related to a personality trait of negative urgency. Future studies are warranted to clarify the neurocognitive mechanisms by which cumulative exposure to ACEs influences the development of negative urgency.
We also found that young adults whose ACEs were predominantly emotional victimization, such as emotional abuse and neglect, reported a higher level of negative urgency. The finding that emotionally victimized children are particularly vulnerable to develop emotion-driven impulsivity is consistent with research linking childhood emotional abuse with negative emotionality and deficits in emotional regulation (Cyders & Smith, 2008; Kim & Cicchetti, 2010; Maughan & Cicchetti, 2002). For emotionally victimized children who often live in hostile and threatening caretaking environments, many forms of positive emotion regulation are difficult to learn. As a result of compromised emotional self-regulation, young adults with a history of emotional victimization are prone to develop a tendency to act rashly to regulate negative emotions (Trickett, Mennen, Kim, & Sang, 2009). Few studies have examined the associations between ACEs classes and specific facets of impulsivity. The present study offers initial evidence that individuals who largely experienced emotional victimization in childhood are likely to demonstrate negative urgency. Several studies have found that among various impulsivity traits, negative urgency is the strongest predictor of mental health and substance use problems in young adulthood (Anestis, Selby, & Joiner, 2007; Cyders & Smith, 2007; Martens, Pedersen, mith, Stewart, & O’Brien, 2011; Simons, Dvorak, Batien, & Wray, 2010). Since negative urgency has been consistently linked to adverse health and behavioral outcomes, our findings highlight the importance of assessing negative emotionality and negative urgency among young adults with a history of emotional victimization. Furthermore, the cumulative effects of childhood emotional victimization and negative urgency on the health and life prospects of young adults need to be examined in future studies. Currently, minimal understanding of such cumulative effects limits the success of prevention and intervention efforts for this highly vulnerable population.
Young adults in the Home Dysfunction/Community Violence ACEs class showed higher levels of sensation seeking than those in the Emotional ACEs class. There were, however, no significant group differences in sensation seeking among other ACEs classes. Unfortunately, limited literature is available to explicate the relatively strong effects of Home Dysfunction/Community Violence ACEs on sensation seeking compared to Emotional ACEs. In the present study, young people in the Emotional ACEs class reported high levels of direct emotional victimization by caregivers while reporting low levels of exposure to household dysfunction and community violence. In contrast, individuals in the Home Dysfunction/Community Violence ACEs class were predominantly exposed to household alcohol abuse and witnessing gang violence and property crime. A recent study suggested that direct victimization confers risk for negative outcomes, but household dysfunction, alone, does not (Roos et al., 2016). We, however, found that compared to direct emotional victimization, exposure to household dysfunction and community violence relates to increased levels of sensation seeking. Repeated exposure to community-based ACEs such as gang violence can be an overwhelming sensory experience and lead to sensory overstimulation. Thus, childhood exposure to chronic and severe community violence may reduce individuals’ sensory arousal levels and increase sensation seeking in young adulthood (Lieberman, Chu, Van Horn, & Harris, 2011; Van Goozen, Fairchild, Snoek, & Harold, 2007). None of the identified ACEs groups in our study is limited to community-violence-only, making it difficult to explore potential differences in sensation seeking between exposures to community violence and emotional victimization. Future studies should extend the current findings to examine whether direct emotional victimization and community violence may confer different risks for sensation seeking.
Limitations
Reflective self-reports of ACEs taking place prior to age 18 are subject to recall and social desirability bias. Additionally, due to the present study’s cross-sectional nature, the temporal relationship between ACEs classes and personality traits of impulsivity during young adulthood cannot be established. Thus, while the study is robust to the inclusion of many controls, such as demographic information and other facets of impulsivity, a causal link is not attached to the findings. Respondents with poor health were excluded in our study because medical disorders could affect brain and cognitive development, which might in turn influence impulsive personality development. This might have eliminated some respondents who have exposure to ACEs and medical disorders. Finally, exclusively examining the environmental contexts of child development such as ACEs will explain only a small proportion of variance in personality development. The effects of childhood adversity cannot be fully appreciated without dedicating attention to the individual and family process factors that contribute to the development of impulsivity.
Acknowledgments
This research was supported by grants from NIDA DA030884 (Shin) and the AMBRF/The Foundation for Alcohol Research (Shin). The Foundation had no role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aertgeerts B, Buntinx F, Bande Knops J, Vanderrneulen C, Roelants M, Ansoms S, & Fevery J (2000). The value of CAGE, CUGE, and AUDIT in screening for alcohol abuse and dependence among college freshmen. Alcoholism: Clinical and Experimental Research, 24(1), 53–57 [PubMed] [Google Scholar]
- Akaike H (1974). A new look at the statistical model identification. IEEE transactions on automatic control, 19(6), 716–723. [Google Scholar]
- Alkan Härtwig E, Crayen C, Heuser I, & Eid M (2014). It’s in the mix: psychological distress differs between combinations of alexithymic facets. Frontiers in psychology, 5, 1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda R, Whitfield C, Felitti V, Chapman D, Edwards V, Dube S, & Williamson D (2002). Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatric Services, 53(8), 1001–1009. [DOI] [PubMed] [Google Scholar]
- Andersen SL, & Teicher MH (2009). Desperately driven and no brakes: Developmental stress exposure and subsequent risk for substance abuse. Neuroscience & Biobehavioral Reviews, 33(4), 516–524. PMCID: PMC2688959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestis MD, Selby EA, & Joiner TE (2007). The role of urgency in maladaptive behaviors. Behaviour Research and Therapy, 45(12), 3018–3029. [DOI] [PubMed] [Google Scholar]
- Arminger G, Stein P, & Wittenberg J (1999). Mixtures of conditional mean-and covariance-structure models. Psychometrika, 64(4), 475–494. [Google Scholar]
- Beers SR, & De Bellis MD (2002). Neuropsychological function in children with maltreatment-related Posttraumatic Sress Disorder. American Journal of Psychiatry, 159(3), 483–486. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, & Fink L (1998). Childhood Trauma Questionnaire: A retrospective self-report San Antonio, TX: Harcourt Brace, Psychological Corporation. [Google Scholar]
- Brandes D, Ben-Schachar G, Gilboa A, Bonne O, Freedman S, & Shalev AY (2002). PTSD symptoms and cognitive performance in recent trauma survivors. Psychiatry Research, 110(3), 231–238 [DOI] [PubMed] [Google Scholar]
- Brodsky BS, Oquendo M, Ellis SP, Haas GL, Malone KM, & Mann JJ (2001). The relationship of childhood abuse to impulsivity and suicidal behavior in adults with major depression. The American journal of psychiatry, 158(11), 1871. [DOI] [PubMed] [Google Scholar]
- Bücker J, Kapczinski F, Post R, Ceresér KM, Szobot C, Yatham LN, … Kauer-Sant’Anna M (2012). Cognitive impairment in school-aged children with early trauma. Comprehensive Psychiatry, 53(6), 758–764. [DOI] [PubMed] [Google Scholar]
- Bynum L, Griffin T, Riding D, Wynkoop K, Anda R, Edwards V, … Croft J (2010). Adverse childhood experiences reported by adults-five states, 2009. Morbidity and Mortality Weekly Report, 59(49), 1609–1613 [PubMed] [Google Scholar]
- Carrion VG, Garrett A, Menon V, Weems CF, & Reiss AL (2008). Posttraumatic stress symptoms and brain function during a response‐ inhibition task: an fMRI study in youth. Depression and Anxiety, 25(6), 514–526. [DOI] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, & Anda RF (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82(2), 217–225. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Curtis WJ (2005). An event-related potential study of the processing of affective facial experessions in young chldren who experienced maltreatment during the first year of life. Development and Psychopathology, 17(3), 641–677. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Valentino K (2006). An ecological transactional perspective on child maltreatment: Failure of the average expectable environment and its influence upon child development. In Cicchetti D & Cohen DJ (Eds.), Developmental Psychopathology: Risk, Disorder, and Adaptation (2nd ed.) (2nd ed., Vol. 3, pp. 129–201). New York: Wiley. [Google Scholar]
- Clark SL, & Muthén B (2009). Relating latent class analysis results to variables not included in the analysis from http://statmodel2.com/download/relatinglca.pdf
- Costa PT, & McCrae RR (1992). Neo Personality Inventory-Revised (NEO PI-R)
- Costello E, Erkanli A, Fairbank J, & Angold A (2002). The prevalence of potentially traumatic events in childhood and adolescence. Journal of Traumatic Stress, 15(2), 99–112. [DOI] [PubMed] [Google Scholar]
- Cyders MA, & Smith GT (2007). Mood-based rash action and its components: Positive and negative urgency. Personality and Individual Differences, 43(4), 839–850. [Google Scholar]
- Cyders MA, & Smith GT (2008). Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin, 134(6), 807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB,Richards JM,Gorka SM, & Sinha R(2009).HPAaxisresponse to psychological stress and treatment retention in residential substance abuse treatment: a prospective study. Drug & Alcohol Dependence, 105(3), 202–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD, Hooper SR, Spratt EG, & Woolley DP (2009). Neuropsychological findings in childhood neglect and their relationships to pediatric PTSD. Journal of the International Neuropsychological Society, 15(6), 868–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD, & Zisk A (2014). The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am, 23(2), 185–222, vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR (1993). BSI Brief Symptom Inventory. Administration, scoring, and procedures manual (4 ed.). Minneapolis: National Computer Systems. [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O’Malley SS, & Sher K (2010). Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology, 15(2), 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, & Anda RF (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics, 111(3), 564–572. [DOI] [PubMed] [Google Scholar]
- Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, & Anda RF (2006). Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of Adolescent Health, 38(4), 1–44. [DOI] [PubMed] [Google Scholar]
- Felitti VJ (2002). The relation between adverse childhood experiences and adult health: Turning gold into lead: Kaiser Permanente’s Department of Preventive Medicine and Centers for Disease Control [DOI] [PMC free article] [PubMed]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998).Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. Am J Prev Med, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, & Turner HA (2007). Poly-victimization: a neglected component in child victimization. Child Abuse Negl, 31(1), 7–26. [DOI] [PubMed] [Google Scholar]
- Fox HC, Hong KI, Siedlarz K, & Sinha R (2008). Enhanced sensitivity to stress and drug/alcohol craving in abstinent cocaine-dependent individuals compared to social drinkers. Neuropsychopharmacology, 33(4), 796–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould F, Clarke J, Heim C, Harvey PD, Majer M, & Nemeroff CB (2012). The effects of child abuse and neglect on cognitive functioning in adulthood. Journal of Psychiatric Research, 46(4), 500–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipp JR, & Bauer DJ (2006). Local solutions in the estimation of growth mixture models. Psychological Methods, 11(1), 36. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Maticka-Tyndale E, el-Guebaly N, & West M (1993). The CAST-6: Development of a short-form of the Children of Alcoholics Screening Test. Addictive Behaviors, 18(3), 337–345. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Polo-Tomas M, & Taylor A (2007). Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: a cumulative stressors model. Child Abuse & Neglect, 31(3), 231–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffee SR, & Maikovich-Fong AK (2011). Effects of chronic maltreatment and maltreatment timing on children’s behavior and cognitive abilities. Journal of Child Psychology and Psychiatry, 52(2), 184–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovanovic T, Ely T,Fani N,Glover EM, Gutman D, Tone EB, … Ressler KJ (2013). Reduced neural activation during an inhibition task is associated with impaired fear inhibition in a traumatized civilian sample. Cortex, 49(7), 1884–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall-Tackett K (2002). The health effects of childhood abuse: four pathways by which abuse can influence health. Child Abuse Negl, 26(6–7), 715–729. [DOI] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, 51(6), 706–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis EE, Dozier M, Ackerman J, & Sepulveda-Kozakowski S (2007). The effect of placement instability on adopted children’s inhibitory control abilities and oppositional behavior. Dev Psychol, 43(6), 1415–1427. [DOI] [PubMed] [Google Scholar]
- Liaw F. r., & Brooks-Gunn J (1994). Cumulative familial risks and low-birthweight children’s cognitive and behavioral development. J Clin Child Psychol, 23(4), 360–272. [Google Scholar]
- Lieberman AF, Chu A, Van Horn P, & Harris WW (2011). Trauma in early childhood: Empirical evidence and clinical implications. Development and Psychopathology, 23(2), 397–410. [DOI] [PubMed] [Google Scholar]
- Little R, & Rubin D (1987). Statistical analysis with missing data New York: Wiley. [Google Scholar]
- Lo Y, Mendell N, & Rubin D (2001). Testing the number of components in a normal mixture. Biometrika, 88, 767–778. [Google Scholar]
- Lynch M, & Cicchetti D (1998). An ecological-transactional analysis of children and contexts: The longitudinal interplay among child maltreatment, community violence, and children’s symptomatology. Development and Psychopathology, 10, 235–257. [DOI] [PubMed] [Google Scholar]
- Magid V, & Colder CR (2007). The UPPS Impulsive Behavior Scale: Factor structure and associations with college drinking. Personality and Individual Differences, 43(7), 1927–1937. [Google Scholar]
- Majer M, Nater U, Lin J-M, Capuron L, & Reeves W (2010). Association of childhood trauma with cognitive function in healthy adults: a pilot study. BMC Neurology, 10(1), 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Pedersen ER, Smith AE, Stewart SH, & O’Brien K (2011). Predictors of alcohol-related outcomes in college athletes: The roles of trait urgency and drinking motives. Addictive Behaviors, 36, 456–464. [DOI] [PubMed] [Google Scholar]
- Masten AS, & Coatsworth JD (1998). The development of competence in favorable and unfavorable environments: Lessons from research on successful children. American Psychologist, 53, 205–220. [DOI] [PubMed] [Google Scholar]
- Maughan A, & Cicchetti D (2002). Impact on child maltreatment and inter adult violence on children’s emotion regulation abilities and socioemotional adjustment. Child Development, 73(5), 1525–1542. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, & Swann AC (2001). Psychiatric aspects of impulsivity. American Journal of Psychiatry, 158(11), 1783–1793. [DOI] [PubMed] [Google Scholar]
- Mueller SC, Hardin MG, Korelitz K, Daniele T, Bemis J, Dozier M, … Ernst M (2012). Incentive effect on inhibitory control in adolescents with early-life stress: an antisaccade study. Child Abuse & Neglect, 36(3), 217–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, & Muthén B (2016). Mplus User’s Guide Los Angeles: Author. [Google Scholar]
- Narvaez JCM, Magalhães PVS, Trindade EK, Vieira DC, Kauer-Sant’Anna M, Gama CS, … Kapczinski F (2012). Childhood trauma, impulsivity, and executive functioning in crack cocaine users. Comprehensive Psychiatry, 53(3), 238–244, [DOI] [PubMed] [Google Scholar]
- Navalta CP, Polcari A, Webster DM, Boghossian A, & Teicher MH (2006). Effects of childhood sexual abuse on neuropsychological and cognitive function in college women. The Journal of Neuropsychiatry & Clinical Neurosciences, 18(1), 43–53. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB (2004). Neurobiological consequences of childhood trauma. J Clin Psychiatry, 65 Suppl 1, 18–28. [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muth´en BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14(4), 535–569. [Google Scholar]
- Oshri A, Kogan SM, Kwon JA, Wickrama KAS, Vanderbroek L, Palmer AA, & MacKillop J (2017). Impulsivity as a mechanism linking child abuse and neglect with substance use in adolescence and adulthood. Dev Psychopathol, 1–19. [DOI] [PubMed] [Google Scholar]
- Pears KC, & Fisher P (2005). Developmental, cognitive, and neuropsychological functioning in preschool-aged foster children: Associations with prior maltreatment and placement history. Journal of Developmental & Behavioral Pediatrics, 26, 112–122. [DOI] [PubMed] [Google Scholar]
- Polcari A, Rabi K, Bolger E, & Teicher MH (2014). Parental verbal affection and verbal aggression in childhood differentially influence psychiatric symptoms and wellbeing in young adulthood. Child Abuse & Neglect, 38(1), 91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD, Cicchetti D, Hornung K, & Reed A (2000). Recognizing emotion in faces: developmental effects of child abuse and neglect. Dev Psychol, 36(5), 679. [DOI] [PubMed] [Google Scholar]
- Prasad MR, Kramer LA, & Ewing-Cobbs L (2005). Cognitive and neuroimaging findings in physically abused preschoolers. Archives of disease in childhood, 90(1), 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinert DF, & Allen JP (2007). The alcohol use disorders identification test: An update of research findings. Alcoholism: Clinical and Experimental Research, 31(2), 185–199. [DOI] [PubMed] [Google Scholar]
- Riggs NR, Sakuma KL, & Pentz MA (2007). Preventing risk for obesity by promoting self-regulation and decision-making skills: pilot results from the PATHWAYS to health program (PATHWAYS). Evaluation Review, 31(3), 287–310. [DOI] [PubMed] [Google Scholar]
- Roos LE, Afifi TO, Martin CG, Pietrzak RH, Tsai J, & Sareen J (2016). Linking typologies of childhood adversity to adult incarceration: Findings from a nationally representative sample. American Journal of Orthopsychiatry, 86(5), 584. [DOI] [PubMed] [Google Scholar]
- Roy A (2005). Childhood trauma and impulsivity. Possible relevance to suicidal behavior. Archives of Suicide Research, 9(2), 147. [DOI] [PubMed] [Google Scholar]
- Rutter M (1981). Stress, coping and development: Some issues and some questions. Journal of Child Psychology and Psychiatry, 22(4), 323–356. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, & Rosenblum KL (2006). Psychosocial constraints on the development of resilience. Ann N Y Acad Sci, 1094, 116–124. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, & Baldwin C(1993).Stability of intelligence from preschool to adolescence: the influence of social and family risk factors. Child Dev, 64(1), 80–97. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. The annals of statistics, 6(2), 461–464. [Google Scholar]
- Selin KH (2003). Test retest reliability of the lcohol Use Disorder Identification Test in a general population sample. Alcoholism: Clinical and Experimental Research, 27(9), 1428–1435. [DOI] [PubMed] [Google Scholar]
- Shaffer JP (1995). Multiple hypothesis testing. Annu Rev Psychol, 46(1), 561–584. [Google Scholar]
- Shields A, & Cicchetti D (1998). Reactive aggression among maltreated children: The contributions of attention and emotion dysregulation. J Clin Child Psychol, 27(4), 381–395. [DOI] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Batien BD, & Wray TB (2010). Event-level associations between affect, alcohol intoxication, and acute dependence symptoms: Effects of urgency, self-control, and drinking experience. Addictive Behaviors, 35(12), 1045–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R (2008). Chronic stress, drug use, and vulnerability to addiction. Annals of the New York Academy of Sciences, 1141, 105–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R (2009). Stress and addiction: a dynamic interplay of genes, environment, and drug intake. Biological Psychiatry, 66(2), 100–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, Kennedy CM, & Twamley EW (2002). Neuropsychological function in female victims of intimate partner violence with and without posttraumatic stress disorder. Biological Psychiatry, 52(11), 1079–1088 [DOI] [PubMed] [Google Scholar]
- Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, & Kim DM (2003). The neurobiological consequences of early stress and childhood maltreatment. Neurosci Biobehav Rev, 27(1–2), 33–44. [DOI] [PubMed] [Google Scholar]
- Thibodeau EL, Cicchetti D, & Rogosch FA (2015). Child maltreatment, impulsivity, and antisocial behavior in African American children: Moderation effects from a cumulative dopaminergic gene index. Development and Psychopathology, 27(4pt2), 1621–1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomoda A, Sheu YS, Rabi K, Suzuki H, Navalta P, Polcari A, & Teicher MH (2011). Exposure to parental verbal abuse is associated with increased gray matter volume in superior temporal gyrus. NeuroImage, 54 Suppl 1, S280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trickett PK, Mennen FE, Kim K, & Sang J (2009). Emotional abuse in a sample of multiply maltreated, urban young adolescents: Issues of definition and identification. Child Abuse & Neglect, 33(1), 27–35. Epub 2009 Jan 2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, & Ormrod R (2010). Poly-victimization in a national sample of children and youth. Am J Prev Med, 38(3), 323–330. [DOI] [PubMed] [Google Scholar]
- Twamley EW, Hami S, & Stein MB(2004). Neuropsychological function in college students with and without posttraumatic stress disorder. Psychiatry Research, 126(3), 265–274. [DOI] [PubMed] [Google Scholar]
- Van Goozen SH, Fairchild G, Snoek H, & Harold GT (2007). The evidence for a neurobiological model of childhood antisocial behavior. Psychological Bulletin, 133(1), 149. [DOI] [PubMed] [Google Scholar]
- Wardell JD, Strang NM, & Hendershot CS (2016). Negative urgency mediates the relationship between childhood maltreatment and problems with alcohol and cannabis in late adolescence. Addictive Behaviors, 56, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669–689. [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, & Reynolds SK (2005). Validation of the UPPS impulsive behaviour scale: A four factor model of impulsivity. European Journal of Personality, 19(7), 559–574. [Google Scholar]
- Zimmerman BJ (2000). Attaining self-regulation: social cognitive perspective. In Boekaerts M, Pintrich PR, & Zeidner M (Eds.), Handbook of self-regulation (pp. 13–39). San Diego: Academic Press. [Google Scholar]


