Abstract
Background
In countries with low calcium intake, the WHO recommends integrating calcium supplementation into antenatal care (ANC) to reduce the risk of preeclampsia, a leading cause of maternal mortality. Current WHO guidelines recommend women take 3–4 calcium supplements plus 1 iron-folic acid supplement at separate times daily. There is limited evidence about implementing these guidelines through routine ANC. Through the Micronutrient Initiative-Cornell University Calcium (MICa) trial, we examined the effect of regimen on supplement consumption among ANC clients in western Kenya. A nested process evaluation examined factors that influence calcium supplementation delivery and uptake.
Objectives
This process evaluation assessed ANC providers’, pregnant women's, and family members’ experiences with calcium supplementation, and investigated the feasibility and acceptability of engaging family members to support adherence.
Methods
We conducted semistructured interviews with 7 ANC providers, 32 pregnant women, and 20 adherence partners (family members who provide reminders and support), and 200 observations of ANC consultations. Interviews were transcribed, translated, and analyzed thematically. Observational data were summarized.
Results
ANC providers reported positive feelings about calcium supplementation, the training received, and counseling materials, but reported increased workloads. Women reported that providers counseled them on supplement benefits and managing side effects, offered reminder strategies, and provided supplements and behavior change materials. Women explained that reminder materials and adherence partners improved adherence. Most adherence partners reported providing reminders and other instrumental support to help with pill taking, which women confirmed and appreciated. Some women reported that comorbidities, concerns about being perceived as HIV positive, pill burden, unfavorable organoleptic properties, and lack of food were adherence barriers.
Conclusions
Although integrating calcium into antenatal iron-folic acid supplementation was generally acceptable to ANC providers, pregnant women, and their families, calcium supplementation presents unique challenges that must be considered to successfully implement these guidelines.
This trial was registered at clinicaltrials.gov as NCT02238704.
Keywords: pregnant women, process evaluation, prenatal micronutrient supplementation, behavioral intervention, social support, preeclampsia, male involvement, qualitative methods, maternal nutrition
Introduction
Antenatal calcium supplementation can reduce the risk of preeclampsia, a leading cause of maternal mortality, and is considered a key nutrition-specific intervention to improve maternal and child health in low- and middle-income countries (1). The WHO recommends supplementation with 1.5–2.0 g Ca/d starting at 20 wk of pregnancy for women in countries with low habitual calcium intake (2). The WHO released these guidelines in 2013, but evidence about the acceptability, feasibility, and appropriateness of delivering calcium supplements through antenatal care (ANC) is limited. Antenatal iron and iron-folic acid (IFA) supplementation programs in low- and middle-income countries have historically faced many challenges with implementation and adherence (3), and it is anticipated that the addition of calcium supplementation could exacerbate these challenges (4). Despite these concerns, early evidence suggests that calcium supplementation may be acceptable to pregnant women and feasible to deliver through existing facility- or community-based services (5–7).
In Kenya, national guidelines recommend that women receive IFA as part of ANC (8). However, barriers to antenatal micronutrient supplementation are well documented, and include supply shortages and stockouts; ineffective counseling by ANC providers; and pregnant women forgetting to take supplements, perceiving adverse side effects, and disliking the supplements (9, 10). The Micronutrient Initiative-Cornell University Calcium (MICa) Trial (NCT02238704) was a cluster-randomized noninferiority trial that examined the effect of supplementation regimen on the amount of calcium supplement ingested (5, 11), and included a nested qualitative process evaluation. The objectives of the process evaluation were to assess the delivery of calcium supplementation through routine ANC by examining ANC providers’, pregnant women’s, and family members’ experiences, and to investigate the feasibility and acceptability of engaging family members to support supplementation adherence.
Methods
Overview of the MICa trial
The trial was conducted from September 2014 to June 2015, and has been previously described (5, 11). Briefly, MICa was a parallel, noninferiority, cluster-randomized trial comparing the effect of higher (three 500-mg calcium pills per day) and lower (two 500-mg calcium pills per day) dosage calcium supplement regimens on supplement consumption by pregnant women seeking ANC from government health facilities. Pregnant women (n = 1036; 16–30 weeks of gestation) were recruited from 16 primary care health facilities in Malava subcounty, Kakamega County, Kenya. Facilities were randomized to either a higher- or lower-calcium supplement regimen; all facilities received the same types of supplements. The calcium supplement was a hard pill with 500 mg of elemental calcium as calcium carbonate and 200 IU cholecalciferol. The IFA supplement was a hard pill with 60 mg Fe and 400 μg folic acid. ANC staff were responsible for supplement dispensing and counseling. Based on the assigned regimen, the study team provided health facilities with sufficient supplies of calcium and IFA supplements, 1-d training for ANC providers on calcium and IFA supplements and counseling skills, calcium and IFA counseling cards, and take-home reminder calendars for women (12). An adherence partner strategy was included at all facilities regardless of regimen. An “adherence partner” is someone, typically a family member, whom pregnant women select and ask to provide adherence reminders and support (13). The study team trained all health workers about adherence partners, included information about adherence partners in the counseling cards and calendars, and provided posters with motivating messages for adherence partners that women could take home (12). Adherence partners did not have any direct interaction with the health system or receive any guidance from ANC providers about how to support women. ANC providers gave women the poster to share with their adherence partner and counseled them to ask for adherence support. All training, counseling, and adherence partner materials are freely accessible from the study website (12).
MICa trial findings suggest that incorporating calcium supplementation into ANC is feasible (14), and mean adherence to calcium and IFA was high (>80%) for both regimens (5, 14, 15). Adequate supplies of calcium and IFA supplements and counseling job aids were available during 94%, 98%, and 97% of unannounced facility spot checks, respectively (14). Adherence partners were selected by 90% of trial participants (15).
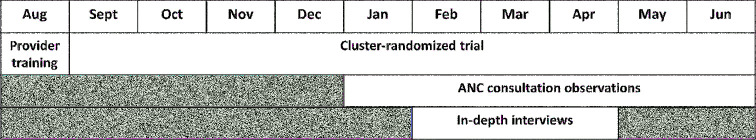
Process evaluation
This process evaluation included in-depth interviews with ANC providers from trial-affiliated health facilities, MICa trial participants, and their adherence partners, plus structured observations of ANC visits (Figure 1). We purposively recruited a subsample of trial participants for the in-depth interviews. Women were sampled to reflect diversity in the type of facility at which they accessed ANC (i.e., health centers, small dispensaries with 1–2 staff), assigned regimen, calcium supplement adherence levels (high, low), and having an adherence partner. Adherence partners of women participating in the process evaluation were invited to participate in independent interviews. Everyone invited agreed to participate. For the structured observations, the study team sought to observe 9–15 consultations at each facility, divided evenly between women's first, second, and third ANC visits.
FIGURE 1.
Process evaluation timeline. ANC, antenatal care.
Data collection
In February–April 2015, a PhD-level qualitative researcher (VW) and graduate student (HO) conducted semistructured interviews with ANC providers, women, and adherence partners using separate semistructured interview guides (Supplemental Material). Interviews were conducted in Kiswahili, Luhya, or English based on participant preference, and lasted between 45 and 75 min. To reduce social desirability bias, the 2 interviewers had not participated in data collection for the larger trial and conducted the interviews separately from trial data collection. The interviewers interviewed ANC providers in a private room at the health facilities, and women and adherence partners individually at home. The interviewers assured participants that the study team was interested in their experiences with supplementation, both negative and positive. All interviews were audio recorded, transcribed, and translated into English.
Trained data collectors used an observation checklist adapted from Phillips et al. (16) to conduct ANC consultation observations at 16 facilities. Observers identified trial participants whose consultations were consistent with the sampling guidelines. Observers obtained consent from all health care providers and clients to stay in the room during consultations, but did not describe what was being observed. They observed sequential consultations until reaching the required number.
Analysis
We analyzed interview transcripts thematically, based on the constant comparative method (17). The qualitative analysis team comprised 5 members. To foster coding consistency across the team, all analysts identified and coded each ANC provider transcript using principles of grounded theory (17). Key themes were discussed during frequent peer debriefings and summarized in a matrix. Because of the larger number of women’s and adherence partners’ interviews, the team used Atlas.ti version 7 (Scientific Software Development GmbH, Berlin, Germany) to analyze women's and adherence partners’ interview transcripts. For the women's interviews, all analysts independently read and coded the same 2 transcripts. The team then reviewed the codes as a group and collaboratively created a codebook. To ensure coding consistency, we agreed on code names, definitions, and inclusion and exclusion criteria (18, 19). Through the debriefings and code book development, we determined that the level of agreement when coding was quite high across the analysis team, and no longer necessitated all team members reading each transcript. All transcripts were then coded with the use of Atlas.ti version 7 with ≥2 analysts independently coding each transcript. The analysts met frequently to discuss emergent codes and any discrepancies, iteratively revising the codebook. Any discrepancies in coding that occurred were deliberated until reaching consensus. Major themes and findings were discussed during peer debriefings. The analysis team followed the same approach for the adherence partner transcripts. Observation data were managed in Excel (Microsoft, Redmond, WA) and summarized for each category of ANC consultation (i.e., first, second, or third visit).
In-depth interview participants provided written informed consent before enrollment. The Institutional Review Board at Cornell University and Kenyatta National Hospital and University of Nairobi Ethics and Research Review Committee approved this study.
Results
Participants
We interviewed 7 ANC providers (4 women, 3 men) from 4 health centers and 3 dispensaries. Their median years of professional experience was 3 (range 2–21). The characteristics of the 32 women in the sample are summarized in Table 1. We also interviewed 20 adherence partners, including 13 husbands, 4 mothers-in-law, 2 mothers, and 1 grandmother. We observed 200 ANC consultations; 68% were conducted by female ANC providers.
TABLE 1.
Women participants’ demographic characteristics
| Characteristic | (n = 32) |
|---|---|
| Age, mean (range) | 25.4 (17–40) |
| Ethnicity, n (%) | |
| Luhya | 28 (87.5) |
| Luo | 2 (6.3) |
| Other | 2 (6.3) |
| Education, n (%) | |
| Some primary | 4 (12.5) |
| Completed primary | 20 (62.5) |
| Some secondary | 6 (18.8) |
| Completed secondary or higher | 2 (6.3) |
| Married or cohabitating, n (%) | 29 (90.6) |
| Number of children, mean (range) | 2.1 (0–10) |
| Primigravid, n (%) | 8 (25) |
| Had an adherence partner, n (%) | 20 (62.5) |
ANC providers
ANC providers were generally positive when asked about their experiences with calcium supplementation, but they identified a few ways to improve the delivery of calcium supplementation through ANC.
Training
Although all ANC providers reported that the training they received was sufficient to implement the program, more than half wanted additional information about calcium supplementation and more detailed information to better answer women's questions (Table 2).
TABLE 2.
Illustrative quotes from antenatal care providers about calcium supplementation
| Themes | Illustrative quotes |
|---|---|
| Training was sufficient, but more depth was desired | We never went so deep into it. But, we got the essence, we got that this is calcium, it is there to do this and this for the mother… but if there was time, we could have gone deeper… but the training we got, we are using it and we are performing. —Health center nurse, #03-06 |
| Perceived improvements in women's health as a result of calcium supplements | I know it is essential to give women the supplements because… before this program was introduced these women had difficulties during pregnancy… When we started giving out this calcium, those problems with pregnancy reduced… women are taking it positively because they find someone to encourage them at home and remind them to take these supplements. The way that we counsel them, they usually find it essential for them to take these pills because they know the benefits. —Dispensary nurse, #11-31 |
| Observed increased attendance at antenatal care | I have liked [calcium] because initially when you give pregnant women health education, it really spreads and everybody is eager. Whenever they come, they will even remind you, “What about the calcium and IFA?” Compared to places where they are not giving calcium, they prefer coming here because they say they understand there is a new pill. —Health center nurse, #17-48 |
| Experienced increased workload | [The addition of calcium] has led to more work on our side. You see, I have to do the counseling and the dispensing… but there is nothing you can do about the workload because we [providers] are few. —Health center nurse, #15-43 |
| Comorbidities made adherence challenging | We are giving them anti-malaria medicine, IFA, and now calcium… for some, it is like you are overloading them. Even some will tell you, “Doctor, there are so many medicines.” Others say they don't like swallowing tablets. After counseling, they come to see the benefits and will take them, but she will tell you she doesn't like taking all these medicines. —Health center nurse, #03-06 |
| Suggestions to improve supplementation programs | What I have heard from almost all my clients, in fact all of them, is that these tablets are too many to take. At least, if it could have been 1, it would be OK. If there was a way they could make 1 tablet taken once, however big or small, at least it will be a combination. There wouldn't be a lot tablets being carried all over. —Dispensary nurse, #04-13 |
| Opinions about adherence partner strategy | It is also good when you have somebody who is encouraging you to take it; at least you feel you have somebody who is caring for you, who is concerned. —Health center nurse, #17-46 |
Delivery
All ANC providers reported positive feelings about the addition of calcium supplementation (Table 2). They said that women liked the calcium pills and appreciated the information they received. The results of the observations suggest that ANC providers counseled participants with a high level of fidelity (Table 3).
TABLE 3.
Observations of providers counseling clients during first, second, and third ANC visits1
| Information ANC providers shared | First visit (n = 73), n (%) | Second visit (n = 63), n (%) | Third visit (n = 64), n (%) |
|---|---|---|---|
| Purpose of calcium pills | |||
| Reduce risk of preeclampsia or high blood pressure | 73 (100%) | 55 (87.3%) | 54 (84.4%) |
| Protect the health of women and infant/protect against health problems | 73 (100%) | 58 (92.1%) | 49 (76.6%) |
| Prevent fits that can lead to death of mother and infant | 63 (86.3%) | 23 (36.5%) | 26 (40.6%) |
| Purpose of iron-folic acid pills | |||
| Reduce risk of anemia or weak blood | 73 (100%) | 54 (85.7%) | 48 (75.0%) |
| Protect the health of women and infant/protect against health problems | 72 (98.6%) | 58 (92.1%) | 45 (70.3%) |
| Prevent feeling tired, dizzy, weak or give strength/energy | 69 (94.5%) | 44 (69.8%) | 20 (31.3%) |
| Reduce risk of bleeding during delivery | 45 (61.6%) | 4 (6.35%) | 6 (9.38%) |
| How to take supplements | |||
| What times of day to take supplements | 73 (100%) | 60 (95.2%) | 60 (93.8%) |
| Take calcium with food | 66 (90.4%) | 58 (92.1%) | 56 (87.5%) |
| How many iron-folic acid pills to take each day | 72 (98.6%) | 59 (93.7%) | 54 (84.4%) |
| Strategies to cope with side effects | |||
| Side effects are not harmful and usually go away if you keep taking the tablets | 61 (83.6%) | 33 (52.4%) | 11 (17.2%) |
| Talk to a health care provider if side effects continue | 60 (82.2%) | 32 (50.8%) | 18 (28.1%) |
| Taking tablets with food can help | 59 (80.8%) | 39 (61.9%) | 14 (21.9%) |
| Specific side effects | |||
| Black stools | 59 (80.8%) | 23 (36.5%) | 2 (3.1%) |
| Diarrhea | 58 (79.5%) | 15 (23.9%) | 3 (4.7%) |
| Nausea | 45 (61.6%) | 17 (27.0%) | 7 (10.9%) |
| Constipation | 33 (45.2%) | 12 (19.1%) | 2 (3.1%) |
| Counseling cards and take-home materials | |||
| Gave a reminder calendar | 72 (98.6%) | 60 (95.2%) | 64 (100%) |
| Gave adherence partner poster | 68 (93.2%) | 55 (87.3%) | 64 (100%) |
| Used counseling cards to suggest asking someone to support adherence | 61 (83.6%) | 8 (12.7%) | 4 (6.3%) |
| Used counseling cards to discuss calcium and iron-folic acid supplements | 61 (83.6%) | 8 (12.7%) | 2 (3.1%) |
Some regimen and counseling information is less relevant at the second and third ANC visits. ANC, antenatal care.
Providers felt that women were motivated to adhere to calcium and IFA supplementation because of the health benefits for themselves and their infant. Most providers reported observing improvements in women's health since the calcium supplementation program began. Several ANC providers associated the availability of calcium with increased numbers of pregnant women seeking care, and mentioned that women knew that the supplements were available and it motivated them to come for ANC.
When asked about difficulties they experienced implementing the program, almost all ANC providers mentioned increased workload as their main challenge. ANC providers also discussed the challenge of counseling women with comorbidities (e.g., HIV, malaria) and the associated high daily pill burden. Additional counseling challenges included concerns about information overload, women with side effects, and women worrying about being perceived as HIV positive. No ANC providers mentioned supply challenges.
ANC providers said they used the counseling materials often, and that they were easy to use, facilitated counseling, saved time, and women liked them. One provider felt that the images of recommended food items were excessive because some women interpreted the images to mean they needed to eat all of the foods, rather than a diverse diet in pregnancy as was intended.
We asked ANC providers for suggestions about ways to improve calcium supplementation delivery and uptake. Many suggested additional strategies to inform women and the community about calcium and IFA, such as radio spots and community health workers. Several suggested reducing the calcium regimen or creating a combined calcium and IFA supplement to address pill burden. All ANC providers were in favor of the adherence partner concept, saying it helped women remember to take the pills, served as a source of encouragement, and involved the husband in the pregnancy.
Women's adherence to supplementation
Most women reported positive experiences with calcium and IFA supplements and the counseling and materials they received (Table 4). Several women identified the counseling as their reason for taking the calcium and IFA supplements. They felt ANC providers were knowledgeable about calcium and IFA supplementation, explained information thoroughly, counseled them about what to do if they experienced side effects, and answered their questions. However, when we asked women whether they had questions about either supplement, half asked about taking calcium supplements outside of pregnancy. They wondered whether they should stop taking them after delivery, and whether others, including children, could take them.
TABLE 4.
Illustrative quotes from women about their experiences with calcium and iron-folic acid supplementation
| Theme | Illustrative quote |
|---|---|
| Valued the counseling from providers | They talked with us in a good, gentle way. If you didn't understand something they would repeat the explanation until you understood it well. —20-y-old primigravida, #17-011 |
| Motivated by perceived benefits | Here we don't have good food that has all the required nutrients for good health. When you take those medicines, they kind of bring about a balance. —23-y-old multigravida, #17-001 |
| Visual cues supported adherence | On this poster, I can see the pills, there is a person who is helping you take your pills… To me, I feel [the poster] is helpful because it is a reminder that I should continue taking my pills and when it is hanging there, when I sit there I remember that I need to take my pills. —19-y-old multigravida, #04-064 |
| Neighbors discouraged pill taking | She told me that if I take those pills, I will be bedridden and never be able to wake up again. She told me that I will be very tired, and I will not be able to do any work and who will do it for me. I should just leave [the supplements] alone. I told her that I am going to try them and see for myself. —30-y-old multigravida, #04-049 |
| Concerns about being perceived as HIV positive | I was given [the poster] and hung it here, but removed it when I heard people saying I have HIV… I tried telling them that this is just a picture and when I look at it I remember to take my pills but they insisted and told me to remove it otherwise people will think I have the disease. —25-y-old multigravida, #14-057 |
| Taking pills with food helped with adherence | What helped me was that when I eat and then take them I would feel good, but if I take them before having a meal, then I would feel so nauseated and then become very weak… But once I eat and then take them, all would be well. —20-y-old primigravida, #17-011 |
| Food insecurity was a barrier to adherence | It is a must that you have to eat before taking that medicine and so you start worrying about how you will take your medicine and you have not eaten. That is the one thing that really makes it difficult for me. —19-y-old multigravida, #04-064 |
| Taking supplements reduced pica | When I started taking those tablets, my urge to eat soil disappeared and I developed an appetite for food. —25-y-old multigravida, #03-004 |
Women listed several factors that motivated their adherence to calcium and IFA supplementation. Most mentioned anticipated and experienced benefits, including feeling strong, having more energy, increased appetite, compensating for inadequate diets, and overall well-being. Almost all listed reminders from family members, the calendar, and the adherence partner poster as facilitators.
Although women generally felt positively about calcium and IFA supplementation, several highlighted factors that made adherence challenging. A few women reported being discouraged from taking calcium supplements by neighbors or others in their community who said supplements could harm them or their fetus. Most women reported other pregnant women and peers giving this advice, whereas others referred to “people” in the community. However, all of the women who reported this continued to take their supplements. A few women reported that other people thought they were HIV positive when they saw their calcium pills or the poster, but this also did not influence their adherence. More than half of the participants reported experiencing side effects (e.g., dizziness, vomiting, stomach pains) when they first started to take calcium and IFA supplements, but they said they continued to take the supplements in spite of this, and the side effects stopped with time. Several women complained about the organoleptic properties (e.g., taste, smell, size) of both supplements, but said this did not influence their adherence. We asked for suggestions about how the supplements could be improved. Several women suggested making the calcium supplements smaller and coating both supplements to make them more palatable.
Women talked about the relation between food and calcium adherence. Meals served as a reminder to take calcium pills and helped reduce side effects. However, almost half of the participants reported that food availability was an issue. A few women reported that the calcium and IFA supplements caused them to stop eating soil, which they had previously craved.
Women's experiences with calcium and IFA supplementation presented here did not vary by calcium regimen, and they were similar among women with high and low calcium adherence. However, some challenges were far more common among women with low calcium adherence (Table 5). Being away from home was a common barrier reported by women with low calcium adherence. This included women who traveled out of town or were away from home during the day. A few women attributed their low calcium adherence to forgetting because of their busy schedules. Several reported that illness or taking other medications led them to stop taking their calcium and IFA supplements, either permanently or for long periods. Only 1 participant reported running out of IFA supplements; none reported running out of calcium supplements.
TABLE 5.
Illustrative quotes about barriers to calcium and iron-folic acid supplementation from women with low adherence
| Theme | Illustrative quote |
|---|---|
| Traveling | I only forgot once… only those 2 weeks when I went home [to parents’ house] for my father's funeral and it was because I was in a hurry and only remembered when I had reached home. —23-y-old multigravida, #11-035 |
| Being out of the house during the day | Maybe before I go to church I remember to take them, but we usually go very early and then come back by 2:00 pm. That is how I got defeated. —25-y-old multigravida, #03-004 |
| Being busy | I wake up and start with my chores, by 10:00 am you have forgotten that you were supposed to take any pills. —29-y-old multigravida, #11-052 |
| Taking other pills for comorbidities | When I went for treatment, I was given some drugs and when I looked at these ones, I felt they are too many for me to take at one go. I took those ones for healing purposes, since it was just for a short period and then I continued with IFA and calcium. —22-y-old primigravida, #03-032 |
Participants with adherence partners
Almost all of the participants who had adherence partners appreciated the experience (Table 6). Women reported that adherence partners provided reminders, and helped provide or prepare food. Several women reported improved relationships with their adherence partners, and increased involvement with their pregnancy. A few women reported their spouses initially served as their adherence partner, but with time their spouses were no longer available to remind them, mainly because of long work hours or travel. Women who reported never having an adherence partner described their husbands or other family members as not being available to help, or felt they did not need help.
TABLE 6.
Illustrative quotes from women about their experiences with adherence partners
| Theme | Illustrative quote |
|---|---|
| Adherence partners provided food | When I told her that if I take the medicine before eating I feel weak, she would ask me if I had eaten before I take the medicine. If I hadn't eaten anything, she would bring me something to eat. —31-y-old multigravida, #03-033 |
| Relationships with adherence partners improved | We sit together and chat away and when it is time for medicine she [mother-in-law] reminds me. Before we never used to sit together and talk. She used to go away at lunchtime, but these days she makes sure she is around so that I can take my medicine. —17-y-old primigravida, #03-052 |
| Not all adherence partners provided support | I thought it [having an adherence partner] was a good idea and since I am usually with my husband, I chose him. But, it reached a point whereby he was coming home late and would even find us asleep… so I got tired with him and I decided to encourage myself and try to remember to take the medicine. —29-y-old multigravida, #04-006 |
Women without adherence partners described aspects of their experience with calcium and IFA supplementation that were distinct from those with adherence partners. Several women without adherence partners mentioned being encouraged by family members to take their supplements, but most reported receiving daily reminders from their young children, and not from their spouse or female family members. Women without adherence partners who identified not having food as a barrier to adherence did not talk about receiving help with food in the same way as did women with adherence partners.
Adherence partners
All adherence partners described their role as reminding women to take their supplements; several also talked about providing healthy foods, helping with chores, and reducing stress (Table 7). Several adherence partners said that being an adherence partner was consistent with their responsibility as a spouse, mother, or mother-in-law. Adherence partners also helped women manage side effects and provided food. Almost all adherence partners said they were assisting the woman because they wanted her to have a safe delivery and, for a few, a healthy child.
TABLE 7.
Adherence partners’ experiences supporting antenatal micronutrient supplementation
| Theme | Illustrative quote |
|---|---|
| Adherence partners provide instrumental, emotional, and informational support | I take care of all the things and any sort of work around the house, including fetching water. For the last 4 months she has never stepped in the river… I also have to leave her food to prepare; at least she can do that without much strain… I vowed that whether in joy or pain, hardships and happiness, I have to be there for her. Any husband is supposed to look after his pregnant wife in all ways possible. —Husband, #04-001 |
| When she is pregnant, I am supposed to keep her from being stressed all the time because the baby in the womb will also be affected. —Husband, #03-005 | |
| I have to make sure that she eats something and does not stay without any food; I have to try to find some so that she can eat and then take her pills after the meal. —Mother, #15-004 | |
| Support adherence for the woman's health | When your wife is healthy, you feel proud… if she has a safe delivery and the baby is healthy, it is to your benefit. Also, when you are helping and reminding her to take her pills it improves your relationship and brings you closer. It builds your marriage together. —Husband, #03-004 |
| Adherence support was consistent with their role | I am happy because when a girl comes to your homestead and she is pregnant you need to support her so that even when she goes to her home, her people can see that she is healthier than when she left their home. —Mother-in-law, #15-040 |
| A few husbands closely monitored adherence, which women had mixed feelings about | She used to be weak but now that she is taking the pills, she is better… In the beginning when she would cook food and bring it to the table, I would ask her, “Where is the book [calendar]?” She would give me the book and I would tell her to take the medicine. Now it has become easy. Even if I'm not around she takes her pills. —Husband, #03-034 |
| In the morning he looks at the calendar and asks me if I have taken my pills and then I tell him I have just taken it now, and if I have forgotten he will look for [the pills] and bring them to me… Him reminding me has really helped me take the pills as directed. —24-y-old multigravida, #03-034 | |
| Sometimes if you are not feeling well or are tired and maybe somebody is persisting, you don't feel good, at times you tell him to get off your case, and he persists. When somebody keeps persisting, I don't like it. —37-y-old multigravida, #15-006 |
A few husbands talked about closely monitoring supplement adherence; women talked about this monitoring differently. One woman found her husband's monitoring to be positive; another viewed it negatively (Table 7).
Discussion
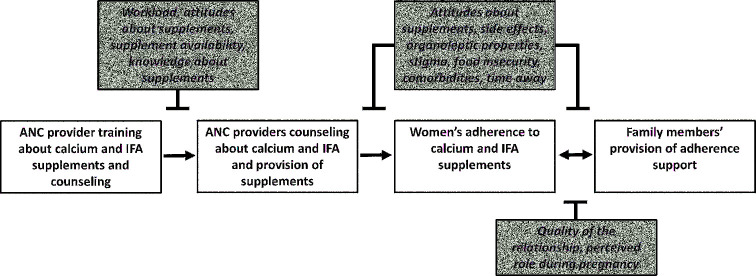
ANC providers, pregnant women, and adherence partners identified several factors that facilitate and impede the implementation of calcium supplementation delivered alongside IFA through ANC (Figure 2). We found that in western Kenya calcium supplementation was acceptable to providers, women, and their families, but there are modifiable factors that can be addressed to improve implementation.
FIGURE 2.
Conceptual framework: barriers and facilitators to calcium and IFA supplementation. White boxes indicate research questions guiding the process evaluation; shaded boxes indicate study findings about barriers and facilitators. ANC, antenatal care; IFA, iron-folic acid.
Provider training and counseling
Although ANC providers had positive views of calcium supplementation, they identified 2 issues of concern. First, an increase in their workloads, in terms of both counseling clients and dispensing supplements. Based on ANC providers’ suggestions, task-shifting approaches could be considered for improving the delivery of calcium supplementation. Community health workers have counselled women and dispensed supplements in micronutrient supplementation programs (3, 20) and specifically for calcium supplementation (6, 7). Second, providers desired additional training about calcium supplementation. In this setting, a 1-d training appeared to be adequate for providers to deliver calcium supplements and counsel women on their regimen and managing side effects with high fidelity at their first ANC consultation. Adding topics could enhance the quality of counseling and women's adherence, as well as meet providers’ expressed needs. Based on provider feedback and women's questions, topics could include counseling about food and diet; advising women about supplementation postpartum; and providing strategies to help women who were busy or away from home, taking pills for other morbidities, or concerned about being perceived as HIV positive. ANC providers, women, and adherence partners all valued the job aids and behavior change materials provided as part of the trial. Providing context-specific materials based on formative research can strengthen the impact of antenatal calcium supplementation programs.
Adherence
Through our formative research when counseling and supplements were delivered at home by study staff, we identified several adherence facilitators and barriers (21). Although this trial differed in that ANC providers rather than study staff delivered supplements and counseling at health facilities, several of our findings were similar. Women identified feeling better and reminder strategies (i.e., calendar, poster, adherence partners) as adherence facilitators, and traveling, being away from home, being busy, experiencing side effects, and negative organoleptic properties as barriers (21). In this study, the most salient adherence motivator women reported was the counseling they received from ANC providers. Benefits of high-quality counseling have been identified in other micronutrient supplementation studies (22). This is notable, because many women reported receiving inadequate IFA counseling in our formative research (10).
The importance of food was prominent in this context and should be considered in training providers and developing counseling materials. Women reported that taking supplements with food helped manage side effects, and mealtimes triggered calcium pill taking. However, in this food-insecure environment, not having food readily available emerged as an issue. Food insecurity was a barrier to calcium adherence in our previous research in Kenya (15, 21) and has been reported as such in Bangladesh (7). The 3-pill calcium regimen lends itself to taking supplements at mealtimes, but only if women eat 3 meals/d. Providers can counsel women to take calcium supplements with food, and our observation data showed that they did so consistently. At the same time, ANC providers should assure women that pills can be taken without food. Counseling materials should emphasize the role calcium and IFA play in helping to supplement women's diets, particularly for women who view their diets as inadequate, which is common in this setting (10). Our observations found that women were consistently counseled about the calcium and IFA regimens, and there is no indication from our analysis that the multiple calcium pill regimen resulted in women consuming additional IFA.
Family support
Family members influence antenatal micronutrient supplement adherence (10, 22, 23). Recognizing this influence, we included the adherence partner strategy in the MICa trial. Engaging family members, particularly male partners, to support maternal health is promoted widely (24). Although our previous research suggested that adherence partners were acceptable to most women (13), we had not previously examined adherence partners’ perspectives.
Adherence partners reported providing instrumental, informational, and emotional support to pregnant women, which women confirmed. The support provided was both specific to supplement adherence (e.g., reminders, food) and related to health and well-being in pregnancy more broadly (e.g., helping with chores). Adherence partners were motivated to support adherence because they believed supplementation was important for women's health in pregnancy, and providing adherence support was consistent with how many husbands and other family members perceived their role. Other maternal and child nutrition studies in Kenya have found that family members want nutrition information, and are willing to support maternal and child nutrition practices (25–27).
In general, women who had adherence partners appreciated the support they received. A limited number of women reported that their adherence partner stopped providing support and 1 reported that the reminders from her husband were excessive. Challenges with adherence support waning over time (28) and overbearing monitoring (29) have been reported in other contexts. Encouraging women to select adherence partners who are supportive in other aspects of their lives should limit the risk of overbearing monitoring. Alternatively, programs can engage men directly and discuss how best to provide adherence support and reminders. Although adherence partners were acceptable and helpful to most women in this process evaluation, the strategy will not be appropriate for all women. It requires that women have a supportive person in their daily life, and women who do not will need other adherence strategies and support.
Another finding of note in relation to family support is that receiving a poster from a provider during ANC was sufficient for most women to have a conversation with a family member about supplementation in pregnancy and ask for adherence support. Male attendance at ANC is positively associated with maternal health outcomes (30), but is not widespread in Kenya (31). The adherence partner strategy was a successful approach for encouraging supplement adherence support without directly engaging family members. Although a poster cannot address larger issues around gender norms, and gender transformative programming is needed to engage family members in maternal health, adherence partners are a low-cost, simple strategy that can be included in ANC.
Limitations
This study had several limitations with respect to the generalizability of the findings. Supply shortages and stockouts are a challenge with antenatal micronutrient supplementation in Kenya (9, 10) and globally (3, 22, 32), and negatively affect provider and client behavior and inhibit the effectiveness of supplementation programs. Owing to the study team managing supplement procurement and the supply chain (5), our findings may not be relevant to contexts with widespread supply issues. Facility-based calcium supplementation programs will depend upon women seeking ANC early in pregnancy and frequently (6, 7, 22). This study only included participants who sought ANC early enough to be included in the larger study, potentially creating a less representative sample. However, almost all pregnant women in Kakamega County attend ANC ≥1 time (33), although typically late in pregnancy. All participants were part of a trial promoting IFA and calcium adherence and social desirability bias may have affected the credibility of their responses. Although ANC providers were not told what we were observing exactly, it is likely that the presence of the research team sensitized them to paying particular attention to issues and counseling points related to calcium supplementation.
Conclusion
Our study provides evidence of the acceptability of antenatal calcium supplementation delivered through ANC and the feasibility of using ANC to recommend adherence partners, a low-cost strategy to engage family members to support supplement adherence. It also demonstrates the insights gained from small-scale research efforts that examine the experiences of program beneficiaries and those who influence them, in our case, family members and ANC providers. Based on the barriers and facilitators identified, ensuring a consistent supply of supplements, high-quality counseling from ANC providers, reminder materials for women to take home, and family support are recommended for the successful integration of calcium supplementation into ANC.
Supplementary Material
Acknowledgments
We gratefully acknowledge Willis Opondo and Brian Kitiavi for conducting the ANC observations, and study team members Rose Chesoli, Felix Makasanda, Hillary Opoma, and Erina Oundo; and Erick Mwanga (Malava Sub-County Health Management Team) and Jacqueline Kung'u (Nutrition International) for their contributions to this study. Carolyne Egesa transcribed and translated the interviews. Discussions with Jeff Sobal (Cornell University) influenced study design for the in-depth interviews; conversations with David Pelletier and Erica Phillips (Cornell University) informed the design of the ANC observations and checklist; and discussions with Kiersten Israel-Ballard (PATH) about infant feeding buddies influenced the adherence partner strategy. The authors’ contributions were as follows—SLM, KLD, RJS, MOO, GMC, and GHP: designed the qualitative study; MOO, KLD, and RJS: designed the observation study; MOO: oversaw the recruitment of study participants and conducted the ANC observations; VW and HO: conducted the in-depth interviews; SLM, TL, KS, HT, AW, VW, and HO: conducted the qualitative data analysis; MOO and TL: analyzed the observation data; SLM: wrote the initial draft of the manuscript and had primary responsibility for final content; and all authors: participated in interpretation of the findings, edited subsequent drafts, and read and approved the final manuscript.
Notes
Supported by Global Affairs Canada through a grant given to Nutrition International (formerly the Micronutrient Initiative) (to KLD) and by the Sackler Institute for Nutrition Science at the New York Academy of Sciences (to RJS).
Author disclosures: SLM, VW, HO, TL, KS, HT, AW, GHP, MOO, GMC, RJS, and KLD, no conflicts of interest.
Supplemental Material is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/.
Abbreviations used:
- ANC
antenatal care
- IFA
iron-folic acid
- MICa
Micronutrient Initiative-Cornell University Calcium trial
References
- 1. Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, Webb P, Lartey A, Black RE, The Lancet Nutrition Interventions Review Group, and the Maternal and Child Nutrition Study Group. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 2013;382:452–77. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization (WHO). Guideline: calcium supplementation in pregnant women [Internet]. Geneva, Switzerland: WHO; 2013. Available from: http://apps.who.int/iris/bitstream/10665/85120/1/9789241505376_eng.pdf. [PubMed] [Google Scholar]
- 3. Sanghvi TG, Harvey PWJ, Wainwright E. Maternal iron-folic acid supplementation programs: evidence of impact and implementation. Food Nutr Bull 2010;31:S100–7. [DOI] [PubMed] [Google Scholar]
- 4. Omotayo MO, Dickin KL, O'Brien KO, Neufeld LM, De Regil LM, Stoltzfus RJ. Calcium supplementation to prevent preeclampsia: translating guidelines into practice in low-income countries. Adv Nutr 2016;7:275–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Omotayo MO, Dickin KL, Pelletier DL, Mwanga EO, Kung'u JK, Stoltzfus RJ. A simplified regimen compared with WHO guidelines decreases antenatal calcium supplement intake for prevention of preeclampsia in a cluster-randomized noninferiority trial in rural Kenya. J Nutr 2017;147:1986–91. [DOI] [PubMed] [Google Scholar]
- 6. Thapa K, Sanghvi H, Rawlins B, Karki YB, Regmi K, Aryal S, Aryal Y, Murakami P, Bhattarai J, Suhowatsky S. Coverage, compliance, acceptability and feasibility of a program to prevent pre-eclampsia and eclampsia through calcium supplementation for pregnant women: an operations research study in one district of Nepal. BMC Pregnancy Childbirth 2016;16:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nguyen PH, Sanghvi T, Kim SS, Tran LM, Afsana K, Mahmud Z, Aktar B, Menon P. Factors influencing maternal nutrition practices in a large scale maternal, newborn and child health program in Bangladesh. PLoS One 2017;12:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kenya Ministry of Health. National policy guideline on combined iron and folic acid (IFA) supplementation for pregnant mothers in Kenya [Internet]. 2013. [cited 2018 Feb 28]. Available from: http://www.nutritionhealth.or.ke/wp-content/uploads/Downloads/IFA%20SIGNED%20IFA%20POLICY.pdf. [Google Scholar]
- 9. Maina-Gathigi L, Omolo J, Wanzala P, Lindan C, Makokha A. Utilization of folic acid and iron supplementation services by pregnant women attending an antenatal clinic at a regional referral hospital in Kenya. Matern Child Health J 2013;17:1236–42. [DOI] [PubMed] [Google Scholar]
- 10. Martin SL, Seim GL, Wawire S, Chapleau GM, Young SL, Dickin KL. Translating formative research findings into a behaviour change strategy to promote antenatal calcium and iron and folic acid supplementation in western Kenya. Matern Child Nutr 2017;13:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Omotayo MO, Dickin KL, Chapleau GM, Martin SL, Chang C, Mwanga EO, Kung'u JK, Stoltzfus RJ. Cluster-randomized non-inferiority trial to compare supplement consumption and adherence to different dosing regimens for antenatal calcium and iron-folic acid supplementation to prevent preeclampsia and anaemia: rationale and design of the Micronutrient Initiative study. J Public Health Res 2015;4:171–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. CENTIR Research Group. MICa prenatal supplementation [Internet]. [cited 2018 Jan 1]. Available from: http://blogs.cornell.edu/centirgroup/research-projects/mica/. [Google Scholar]
- 13. Martin SL, Omotayo MO, Chapleau GM, Stoltzfus RJ, Birhanu Z, Ortolano SE, Pelto GH, Dickin KL. Adherence partners are an acceptable behaviour change strategy to support calcium and iron-folic acid supplementation among pregnant women in Ethiopia and Kenya. Matern Child Nutr 2017;13:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Omotayo MO, Dickin KL, Pelletier DL, Martin SL, Kung'u JK, Stoltzfus RJ. Feasibility of integrating calcium and iron-folate supplementation to prevent preeclampsia and anemia in pregnancy in primary healthcare facilities in Kenya. Matern Child Nutr 2017;13:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Martin SL, Omotayo MO, Pelto GH, Chapleau GM, Stoltzfus RJ, Dickin KL. Adherence-specific social support enhances adherence to calcium supplementation regimens among pregnant women. J Nutr 2017;147:686–96. [DOI] [PubMed] [Google Scholar]
- 16. Phillips E, Stoltzfus RJ, Michaud L, Pierre GLF, Vermeylen F, Pelletier D. Do mobile clinics provide high-quality antenatal care? A comparison of care delivery, knowledge outcomes and perception of quality of care between fixed and mobile clinics in central Haiti. BMC Pregnancy Childbirth 2017;17:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Strauss AL, Corbin JM. Basics of qualitative research. Thousand Oaks, CA: Sage; 1990. [Google Scholar]
- 18. DeCuir-Gunby JT, Marshall PL, McCulloch AW. Developing and using a codebook for the analysis of interview data: an example from a professional development research project. Field Methods 2010;23:136–55. [Google Scholar]
- 19. Macqueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Cult Anthropol Methods 1996;10:31–6. [Google Scholar]
- 20. Berti C, Gaffey MF, Bhutta ZA, Cetin I. Multiple-micronutrient supplementation: evidence from large-scale prenatal programmes on coverage, compliance and impact. Matern Child Nutr 2017:e12531 doi: 10.1111/mcn.12531. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Omotayo MO, Ortolano SE, Martin SL, Stoltzfus RJ, Mwanga E, Dickin KL. With adaptation, the WHO guidelines on calcium supplementation for prevention of pre-eclampsia are adopted by pregnant women. Matern Child Nutr 2017;14(2):e12521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Siekmans K, Roche M, Kung'u JK, Desrochers RE, De-Regil LM. Barriers and enablers for iron folic acid (IFA) supplementation in pregnant women. Matern Child Nutr 2017:e12532 doi: 10.1111/mcn.12532. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nagata JM. Social determinants of iron supplementation among women of reproductive age: a systematic review of qualitative data. Matern Child Nutr 2011;8:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. World Health Organization (WHO). WHO recommendations on antenatal care for a positive pregnancy experience [Internet]. Geneva, Switzerland: WHO; 2016[cited 2018 Jan 1]. Available from: http://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf?ua=1. [PubMed] [Google Scholar]
- 25. Martin SL, Muhomah T, Thuita F, Bingham A, Mukuria AG. What motivates maternal and child nutrition peer educators? Experiences of fathers and grandmothers in western Kenya. Soc Sci Med 2015;143:45–53. [DOI] [PubMed] [Google Scholar]
- 26. Thuita FM, Martin SL, Ndegwa K, Bingham A, Mukuria AG. Engaging fathers and grandmothers to improve maternal and child dietary practices: planning a community-based study in western Kenya. Afr J Food Agric Nutr Dev 2015;15:10386–405. [Google Scholar]
- 27. DeLorme AL, Gavenus ER, Salmen CR, Benard GO, Mattah B, Bukusi E, Fiorella KJ. Nourishing networks: a social-ecological analysis of a network intervention for improving household nutrition in western Kenya. Soc Sci Med 2018;197:95–103. [DOI] [PubMed] [Google Scholar]
- 28. Taiwo BO, Idoko JA, Welty LJ, Otoh I, Job G, Iyaji PG, Agbaji O, Agaba PA, Murphy RL. Assessing the viorologic and adherence benefits of patient-selected HIV treatment partners in a resource-limited setting. J Acquir Immune Defic Syndr 2010;54:85–92. [DOI] [PubMed] [Google Scholar]
- 29. Shaw A, Golding L, Girard AW. Alternative approaches to decreasing maternal anemia: identifying the need for social marketing strategies to promote iron-folic acid supplementation in the Peruvian highlands. Int J Nonprofit Volunt Sect Mark 2012;17:325–33. [Google Scholar]
- 30. Yargawa J, Leonardi-Bee J. Male involvement and maternal health outcomes: systematic review and meta-analysis. J Epidemiol Community Health 2015;69:604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brubaker K, Nelson BD, McPherson H, Ahn R, Oguttu M, Burke TF. Qualitative study of the role of men in maternal health in resource-limited communities in western Kenya. Int J Gynecol Obstet 2016;135:245–9. [DOI] [PubMed] [Google Scholar]
- 32. Galloway R, Dusch E, Elder L, Achadi E, Grajeda R, Hurtado E, Favin M, Kanani S, Marsaban J, Meda N, et al. Women's perceptions of iron deficiency and anemia prevention and control in eight developing countries. Soc Sci Med 2002;55:529–44. [DOI] [PubMed] [Google Scholar]
- 33. Kenya National Bureau of Statistics (KNBS). Kenya demographic and health survey 2014 [Internet]. Nairobi, Kenya: KNBS; 2015[cited 2018 Jan 1]. Available from: https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.