Abstract
BACKGROUND AND OBJECTIVES:
Patients with spina bifida (SB) typically develop serious secondary conditions and undergo surgical procedures related to neurologic disorders, orthopedic abnormalities, bladder and bowel dysfunction, and skin breakdown. In this study, we describe the age distribution of common surgical procedures and health outcomes in patients with SB.
METHODS:
Using serial cross-sectional data from the National Spina Bifida Patient Registry (2009–2013; n = 4664), we examined surgical procedures (gastrointestinal, neurologic, orthopedic, skin, urologic, and other) and health outcomes (fecal continence, urinary continence, skin breakdown, and ambulation status) of patients with SB by age and SB type (myelomeningocele and nonmyelomeningocele).
RESULTS:
All patients who were enrolled had available health outcome data, and 81.5% (n = 3801) of patients had complete surgical procedure data, which totaled 18 891 procedures across their lifetimes. Almost all procedures (91.4%) occurred among participants with myelomeningocele SB. For both types of SB, the distribution of procedures varied by age. The most frequent procedures were neurologic, with approximately half (53%) occurring in patients <1 year of age; orthopedic and urologic procedures followed in frequency but tended to occur at older ages. The health outcomes for patients with myelomeningocele SB revealed lower frequencies of positive health outcomes than those for patients with nonmyelomeningocele SB across all age groups. Overall, the rates of fecal and urinary continence and skin breakdown increased with age whereas the ability to ambulate declined with age.
CONCLUSIONS:
Understanding the surgical procedures and health outcome variations by age and SB type can help clinicians and populations that are affected set expectations regarding the occurrence of these procedures and the outcomes throughout the patients’ life spans.
Chronic conditions often follow predictable patterns when left untreated. Tracking the natural history of these conditions allows the prediction of undesirable health outcomes that could be prevented with opportune treatments.1–4 This prediction and prevention approach applies to many rare conditions in which progression is usually complex, starts early in life, involves numerous organ systems, and includes a host of secondary conditions.
Spina bifida (SB) is a rare congenital abnormality that fulfills these criteria. SB is the result of the failure of a segment of the neural tube to close properly, affecting the development of the spinal cord and column with variable severity.3,5 SB has an estimated birth prevalence of 3.4 cases per 10 000 live births6 and is usually accompanied by multiple secondary conditions, which include neurologic disorders, orthopedic abnormalities, bladder and bowel dysfunction, and skin breakdown. Because of advancements in health care and legislation to protect infants and children, patients with SB now live longer, with most surviving into adulthood.7–10
Despite the advancements, little is known about the course of the disease throughout the life spans of patients with SB. The authors of a recent study reported that ~80% and 90% of patients may have impaired bowel and bladder function, respectively.11 Most research on the surgical histories of patients with SB is outdated, and age has not been taken into consideration.3,8,10,11 Here, we undertook a descriptive analysis of the National Spina Bifida Patient Registry (NSBPR), the largest known database of patients with SB, to examine the age-specific frequency of surgical procedures and health outcomes across the life spans of patients with SB. It is our hope that such an analysis will inform researchers who have noted the lack of age-specific information for the development of standards of care and best practices for patients with SB,12 help health care providers conceptualize a typical sequence of surgical procedures and health outcomes that are experienced by patients with SB and use it as a reference for their own patients, and allow persons with SB and their families to set expectations regarding the future need for common surgical procedures at specific ages.
METHODS
We used serial cross-sectional data from the NSBPR, which is supported by the Centers for Disease Control and Prevention. Data collection started in January 2009 with 10 specialty clinics and was expanded to 19 clinics by September 2013.13 All patients with SB who attend these clinics are eligible to participate. The primary goals for the NSBPR are to characterize the patient population that attends select SB clinics and to assess the effect of care practices on health outcomes.13 Data were obtained from medical records and interviews (conducted at entry into the registry and at subsequent clinic visits no more than annually).13 Each clinic obtained approval to participate in the study from its respective institutional review board.
Surgeries and Outcomes
The medical and surgical histories that were reported by patients were verified through medical record reviews. The success of this verification varied by clinic. SB types include myelomeningocele and nonmyelomeningocele diagnoses: the latter including meningocele, lipomyelomeningocele, and fatty filum. All surgical procedures that were recorded in the NSBPR underwent clinical review and were categorized as gastrointestinal, neurologic, orthopedic, skin, urologic, and other (Table 1). Diagnostic procedures, such as urodynamic studies (also collected by the NSBPR), were not included. All procedures were reported to the NSBPR by using terminology from the Systematized Nomenclature of Medicine. It is important to note that because the NSBPR is retrospective, participating sites were not initially required to document neonatal spinal closure, which is performed in all patients with myelomeningocele SB. Therefore, not all spinal closures were captured in this study and, thus, were not considered in this analysis. Currently, all SB-related surgeries and procedures are recorded by all sites that participate in the NSBPR, beginning at a patient’s birth.
TABLE 1.
List of Surgical Procedures in Patients With SB, Grouped Into 6 Categories; From the NSBPR, 2009–2013
| Category | Procedure |
|---|---|
| Gastrointestinal | Cecostomy tube |
| Colostomy | |
| Creation of antegrade continence enema stoma | |
| Gastrostomy tube procedures | |
| Ileostomy | |
| Repair of anal sphincter | |
| Neurologic | Chiari decompression |
| Creation of syrinx shunt | |
| Endoscopic third ventriculostomy | |
| Laminectomy | |
| Meningocele repair | |
| Repair of SB (spinal closure) | |
| Shunt insertion | |
| Shunt revision | |
| Spinal syrinx revision | |
| Tethered cord release | |
| Orthopedic | Correction of ankle or foot deformity |
| Correction of congenital foot deformity | |
| Correction of equinus contracture | |
| Correction of scoliosis | |
| Osteotomy for correction of bony deformity | |
| Osteotomy of femur | |
| Pelvic osteotomy | |
| Reduction of hip dislocation | |
| Release of contracture of hip joint | |
| Release of contracture of knee joint | |
| Spinal fusion for kyphosis | |
| Skin | Debridement of wound of skin |
| Flap graft | |
| Incision and drainage of abscess | |
| Reduction of callus | |
| Revision of scar of skin | |
| Skin flap operation | |
| Skin grafting | |
| Urologic | Antireflux procedure |
| Appendicovesicostomy | |
| Augmentation of bladder | |
| Bladder neck procedure | |
| Cystectomy, dome of bladder | |
| Nephrectomy | |
| Revision of urinary diversion | |
| Stone procedure | |
| Transurethral cystoscopy | |
| Transurethral fulguration of bladder | |
| Urinary bladder reconstruction | |
| Vesicostomy | |
| Vesicostomy closure | |
| Other | Circumcision |
| Myringotomy and insertion of tympanostomy tube | |
| Repair of inguinal hernia | |
| Testis procedure | |
| Tonsillectomy and adenoidectomy | |
| Tracheostomy |
Our data collection is serial cross-sectional. We collect data from an expanding pool of patients as they are recruited and as they attend annual clinic visits afterward. The most recent data are from the last clinic visit, and data over time are from current and past annual visits. Not all patients visit the clinics every year. The 4 disease-related outcomes of interest for this study (fecal continence, urinary continence, skin breakdown, and ambulation) were obtained from interviews or medical records at the last clinic visit recorded. Fecal and urinary continence were analyzed for patients with multiple visits beginning at 5 years of age. Fecal continence was defined as no involuntary stool leakage, with or without interventions, during the day. Urinary continence was defined as being dry, with or without interventions, during the day. The occurrence of skin breakdown was determined by asking if the patient had a skin breakdown in the last 12 months or since the last SB clinic visit. Following Hoffer et al,14 ambulation status was categorized into 4 possible outcomes: community ambulator (walks indoors and outdoors for most activities and may need crutches or braces), household ambulator (walks only indoors with the help of apparatuses and may use a wheelchair for some activities), therapeutic ambulator (walks only during therapy sessions), and nonambulator (exclusively uses a wheelchair for most activities).
Sample and Analysis
Between January 2009 and September 2013, 4664 patients were enrolled in the NSBPR. Fifteen of the 19 clinics recruited at least 70% of their patients with SB to participate. All patients who were enrolled had outcome data available, and 3801 patients had complete surgical procedure data available. To examine age distributions, we divided the samples into 20 age groups of 1 year each (0–19 years of age) and 2 multiyear age groups (20–24 years of age and ≥25 years of age). Within each age group, we calculated the percentage of patients who reported a given procedure or outcome by SB diagnosis. For ambulation status, we analyzed only patients with myelomeningocele SB (the group with the nonmyelomeningocele type of SB was populated by mostly community ambulators).
We also calculated the percentage of patients who underwent each surgical procedure category by age and SB type and reported these data in 2 ways: (1) the percentage of patients who underwent a surgical procedure in each category within each age group and (2) the distribution of surgical procedures within each category across all age groups. In this second case, patients were counted just once per procedure category and age group. For example, a patient who underwent both shunt insertion and revision surgeries before 1 year of age was counted once in the neurologic category for that age group. Analyses were completed by using SAS software.15
RESULTS
General
Of the 4664 participants, 3801 had complete surgical histories. There were 391 participants who had no surgical procedures on record, and 472 had undated or misdated surgeries. Over 83% of participants had myelomeningocele SB, and almost half were <10 years of age (Table 2). Neurologic surgeries were the most common; more than half of all patients underwent neurologic surgeries (in addition to the necessary initial spinal closure in patients with myelomeningocele SB). Negative outcomes were less common in patients with nonmyelomeningocele SB than in patients with myelomeningocele SB.
TABLE 2.
Cross-sectional Demographic and Clinical Profile of Patients With SB and Distribution of Surgical Procedures and Health Outcomes; From the NSBPR, 2009–2013 (n = 3801 Patients With Complete Surgical Procedure Data)
| Variable | Overall, n (%) | Myelomeningocele, n (%) | Nonmyelomeningocele, n (%) |
|---|---|---|---|
| Age distribution, y | |||
| <5 | 1165 (30.7) | 931 (29.5) | 234 (36.5) |
| 5–9 | 780 (20.5) | 623 (19.7) | 157 (24.5) |
| 10–14 | 709 (18.7) | 599 (19.0) | 110 (17.1) |
| 15–19 | 603 (15.9) | 511 (16.2) | 92 (14.3) |
| 20–24 | 221 (5.8) | 194 (6.1) | 27 (4.1) |
| ≥25 | 323 (8.5) | 301 (9.5) | 22 (3.4) |
| Total | 3801 (100) | 3159 (83.1) | 642 (16.9) |
| Sex | |||
| Female | 1992 (52.4) | 1640 (51.9) | 352 (54.8) |
| Male | 1809 (47.6) | 1519 (48.1) | 290 (45.2) |
| Total | 3801 (100) | 3159 (83.1) | 642 (16.9) |
| Race and/or ethnicity | |||
| Non-Hispanic white | 2492 (65.6) | 2107 (66.7) | 385 (60.0) |
| Non-Hispanic African American | 295 (7.8) | 265 (8.4) | 30 (4.7) |
| Hispanic or Latino | 758 (19.9) | 613 (19.4) | 145 (22.6) |
| Other | 245 (6.5) | 163 (5.2) | 82 (12.8) |
| Refused or unknown | 11 (0.3) | 11 (0.4) | 0 (0.0) |
| Total | 3801 (100) | 3159 (83.1) | 642 (16.9) |
| Type and No. surgical procedures reported in all visits | |||
| Neurologic | 11 133 (58.9) | 10 269 (59.5) | 864 (53.1) |
| Orthopedic | 2936 (15.5) | 2666 (15.4) | 270 (16.6) |
| Urologic | 1823 (9.7) | 1651 (9.6) | 172 (10.6) |
| Gastrointestinal | 1076 (5.7) | 942 (5.5) | 134 (8.2) |
| Skin | 989 (5.2) | 890 (5.2) | 99 (6.1) |
| Other | 934 (4.9) | 847 (4.9) | 87 (5.4) |
| Total | 18 891 (100) | 17 265 (91.4) | 1626 (8.6) |
| Prevalence of key outcomesa status reported at last visit | |||
| Fecal incontinence | 1453 (59.4) | 1091 (63.0) | 362 (43.0) |
| Urinary incontinence | 1482 (58.6) | 1106 (62.5) | 376 (40.8) |
| Skin breakdown | 754 (16.2) | 692 (18.3) | 62 (7.0) |
| Non ambulator | 1204 (28.5) | 1171 (34.3) | 33 (4.1) |
We report negative outcomes in this section of the table to facilitate risk comparisons.
Surgical Procedures
The 3801 participants with a complete surgical history had experienced 18 891 surgical procedures (an average of 4.97 per patient). Of those procedures, 17 265 (91.4%) occurred among patients with myelomeningocele SB (Table 2). Tables 3 and 4 reveal detailed age distributions of surgical procedures by category and SB type. Given a procedure, these tables indicate the probability that such procedure would occur at a specific age. Overall, the frequency of these procedures declined drastically from childhood to young adulthood. Approximately 53% of the neurologic procedures occurred before 1 year of age in both types of SB. Most neurologic procedures at this age were spinal closure, shunt insertion, and shunt revision (91.3% combined). For the other surgical categories, a similar cumulative proportion is reached at ages between 2 and 10 years. In all categories, ≥88% of surgeries have been performed in patients with either type of SB by the time they have reached 18 years of age.
TABLE 3.
Frequency Distribution and Cumulative Frequency of 6 Categories of Surgical Procedures Among Patients With Myelomeningocele SB, by Age; From the NSBR, 2009–2013 (Total = 17 265 Procedures)
| Age, y | Gastrointestinal, n = 942 Procedures |
Neurologic, n = 10 269 Procedures |
Orthopedic, n = 2666 Procedures |
Skin, n = 890 Procedures | Urologic, n = 1651 Procedures | Other, n = 847 Procedures | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
|
| <1 | 9.7 | 10 | 53.1 | 53 | 10.2 | 10 | 17.8 | 18 | 4.4 | 4 | 29.3 | 29 |
| 1 | 2.2 | 12 | 5.0 | 58 | 10.0 | 20 | 1.4 | 19 | 3.9 | 8 | 16.8 | 46 |
| 2 | 1.7 | 14 | 3.9 | 62 | 8.7 | 29 | 1.9 | 21 | 3.2 | 12 | 10.5 | 57 |
| 3 | 2.6 | 16 | 3.4 | 65 | 8.3 | 37 | 2.8 | 24 | 3.6 | 15 | 7.1 | 64 |
| 4 | 5.8 | 22 | 3.1 | 69 | 8.1 | 45 | 3.8 | 28 | 6.1 | 21 | 7.8 | 72 |
| 5 | 6.5 | 29 | 2.8 | 71 | 6.6 | 52 | 4.3 | 32 | 7.0 | 28 | 5.3 | 77 |
| 6 | 8.5 | 37 | 2.6 | 74 | 7.4 | 59 | 2.9 | 35 | 8.5 | 37 | 4.4 | 81 |
| 7 | 6.1 | 43 | 2.3 | 76 | 6.0 | 65 | 2.4 | 37 | 7.1 | 44 | 3.5 | 85 |
| 8 | 6.5 | 50 | 2.5 | 79 | 5.1 | 70 | 3.4 | 41 | 6.4 | 50 | 3.7 | 88 |
| 9 | 5.9 | 56 | 2.0 | 81 | 4.8 | 75 | 4.3 | 45 | 6.1 | 56 | 1.8 | 90 |
| 10 | 6.2 | 62 | 2.0 | 83 | 5.1 | 80 | 5.1 | 50 | 5.8 | 62 | 2.0 | 92 |
| 11 | 5.4 | 67 | 2.1 | 85 | 4.8 | 85 | 5.6 | 56 | 5.2 | 67 | 1.1 | 93 |
| 12 | 6.1 | 73 | 2.6 | 87 | 4.1 | 89 | 8.1 | 64 | 6.5 | 74 | 1.1 | 94 |
| 13 | 3.8 | 77 | 2.2 | 90 | 3.1 | 92 | 4.5 | 68 | 5.8 | 80 | 1.5 | 96 |
| 14 | 3.2 | 80 | 1.8 | 91 | 2.2 | 95 | 6.4 | 75 | 2.7 | 82 | 1.2 | 97 |
| 15 | 3.2 | 83 | 1.5 | 93 | 1.8 | 96 | 4.2 | 79 | 3.0 | 85 | 0.7 | 98 |
| 16 | 2.8 | 86 | 0.9 | 94 | 1.3 | 98 | 2.7 | 82 | 2.7 | 88 | 0.7 | 99 |
| 17 | 3.4 | 90 | 0.9 | 95 | 0.6 | 98 | 4.4 | 86 | 3.3 | 91 | 0.7 | 99 |
| 18 | 1.7 | 91 | 0.6 | 95 | 0.6 | 99 | 2.4 | 88 | 1.9 | 93 | 0.5 | 100 |
| 19 | 1.9 | 93 | 0.8 | 96 | 0.5 | 99 | 2.4 | 91 | 1.2 | 94 | 0.1 | 100 |
| 20–24 | 3.9 | 97 | 1.9 | 98 | 0.8 | 100 | 3.9 | 95 | 3.7 | 98 | 0.1 | 100 |
| >25 | 3.1 | 100 | 2.0 | 100 | 0.3 | 100 | 5.6 | 100 | 1.9 | 100 | 0.2 | 100 |
See a complete list of the surgical procedures by category in Table 1.
TABLE 4.
Frequency Distribution and Cumulative Frequency of 6 Categories of Surgical Procedures Among Patients With Nonmyelomeningocele SB, by Age; From the NSBPR, 2009–2013 (Total = 1626 Procedures)
| Age, y | Gastrointestinal, n = 134 Procedures |
Neurologic, n = 864 Procedures |
Orthopedic, n = 270 Procedures |
Skin, n = 99 Procedures | Urologic, n = 172 Procedures | Other, n = 87 Procedures | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
Frequency, % | Cumulative Frequency, % |
|
| <1 | 40.3 | 40 | 52.8 | 53 | 6.3 | 6 | 25.3 | 25 | 13.4 | 13 | 20.7 | 21 |
| 1 | 7.5 | 48 | 8.2 | 61 | 5.2 | 12 | 1.0 | 26 | 5.8 | 19 | 13.8 | 35 |
| 2 | 0.8 | 49 | 4.1 | 65 | 5.9 | 17 | 1.0 | 27 | 8.1 | 27 | 10.3 | 45 |
| 3 | 5.2 | 54 | 2.7 | 68 | 7.8 | 25 | 5.1 | 32 | 4.1 | 31 | 11.5 | 56 |
| 4 | 4.5 | 58 | 3.0 | 71 | 8.2 | 33 | 4.0 | 36 | 8.1 | 40 | 9.2 | 66 |
| 5 | 3.7 | 62 | 2.8 | 74 | 7.0 | 40 | 2.0 | 38 | 11.6 | 51 | 6.9 | 72 |
| 6 | 4.5 | 67 | 2.3 | 76 | 3.7 | 44 | 3.0 | 41 | 6.4 | 58 | 3.5 | 76 |
| 7 | 3.0 | 70 | 3.6 | 80 | 4.8 | 49 | 2.0 | 43 | 5.2 | 63 | 6.9 | 83 |
| 8 | 5.2 | 75 | 1.6 | 81 | 5.2 | 54 | 0.0 | 43 | 7.6 | 70 | 4.6 | 87 |
| 9 | 3.7 | 78 | 3.6 | 85 | 5.2 | 59 | 2.0 | 45 | 2.3 | 73 | 1.2 | 89 |
| 10 | 6.0 | 84 | 2.8 | 88 | 4.8 | 64 | 4.0 | 49 | 2.9 | 76 | 3.5 | 92 |
| 11 | 0.8 | 85 | 2.4 | 90 | 8.2 | 72 | 6.1 | 56 | 2.3 | 78 | 1.2 | 93 |
| 12 | 2.2 | 87 | 1.3 | 91 | 8.2 | 81 | 6.1 | 62 | 4.7 | 83 | 2.3 | 96 |
| 13 | 1.5 | 89 | 1.3 | 93 | 5.6 | 86 | 4.0 | 66 | 2.3 | 85 | 0.0 | 96 |
| 14 | 0.0 | 89 | 1.0 | 94 | 3.3 | 89 | 5.1 | 71 | 1.1 | 86 | 1.2 | 97 |
| 15 | 2.2 | 91 | 0.7 | 94 | 1.9 | 91 | 6.1 | 77 | 8.7 | 95 | 2.3 | 99 |
| 16 | 0.0 | 91 | 1.5 | 96 | 1.5 | 93 | 6.1 | 83 | 1.2 | 96 | 0.0 | 99 |
| 17 | 0.8 | 92 | 1.5 | 97 | 2.2 | 95 | 5.1 | 88 | 1.7 | 98 | 0.0 | 99 |
| 18 | 0.8 | 93 | 0.5 | 98 | 0.0 | 95 | 9.1 | 97 | 1.2 | 99 | 0.0 | 99 |
| 19 | 0.0 | 93 | 0.6 | 98 | 3.0 | 98 | 1.0 | 98 | 0.0 | 99 | 1.2 | 100 |
| 20–24 | 5.2 | 98 | 0.5 | 99 | 1.9 | 100 | 2.0 | 100 | 1.2 | 100 | 0.0 | 100 |
| >25 | 2.2 | 100 | 1.4 | 100 | 0.4 | 100 | 0.0 | 100 | 0.0 | 100 | 0.0 | 100 |
See a complete list of the surgical procedures by category in Table 1.
Tables 5 and 6 reveal age-specific distributions of participants of the NSBPR across categories of surgical procedures. Given a specific age, these tables indicate the probability that patients would undergo any of the 6 types of procedure at that age. Approximately 78% and 62% of patients <1 year of age with a myelomeningocele and a nonmyelomeningocele type of SB, respectively, underwent at least 1 surgical procedure; most of these patients underwent neurologic procedures (76.6% and 59.2%, respectively). Further examination revealed that among patients with myelomeningocele SB, 65.1% reported shunt insertion, and 42.4% reported shunt revision.
TABLE 5.
Age-Specific Frequency Distribution of Patients With SB Across 6 Categories of Surgical Procedures: Patients With Myelomeningocele SB; From the NSBPR, 2009–2013
| Age, y (n)a | Gastrointestinal, % | Neurologic, % | Orthopedic, % | Skin, % | Urologic, % | Other, % | None, % |
|---|---|---|---|---|---|---|---|
| <1 (3159) | 2.8 | 76.6b | 6.8 | 3.7 | 2.1 | 6.3 | 22.5 |
| 1 (2999) | 0.6 | 11.1 | 7.2 | 0.3 | 1.8 | 3.9 | 78.7 |
| 2 (2862) | 0.5 | 8.8 | 6.3 | 0.3 | 1.4 | 2.7 | 82.7 |
| 3 (2736) | 0.9 | 7.9 | 6.0 | 0.6 | 1.8 | 2.0 | 83.2 |
| 4 (2593) | 1.9 | 8.3 | 6.7 | 0.9 | 2.8 | 2.3 | 80.7 |
| 5 (2440) | 2.3 | 7.1 | 5.5 | 0.7 | 3.2 | 1.5 | 83.4 |
| 6 (2299) | 3.1 | 7.3 | 6.5 | 0.8 | 3.8 | 1.5 | 81.4 |
| 7 (2157) | 2.4 | 6.6 | 5.8 | 0.7 | 3.7 | 1.2 | 83.0 |
| 8 (2020) | 2.9 | 8.0 | 5.1 | 1.0 | 3.6 | 1.3 | 82.7 |
| 9 (1884) | 2.8 | 7.1 | 5.6 | 1.3 | 3.8 | 0.8 | 82.6 |
| 10 (1768) | 3.1 | 7.6 | 5.8 | 1.4 | 3.7 | 0.8 | 81.2 |
| 11 (1637) | 2.8 | 8.6 | 6.0 | 1.9 | 4.3 | 0.6 | 81.1 |
| 12 (1516) | 3.6 | 9.0 | 5.9 | 2.4 | 4.8 | 0.5 | 79.2 |
| 13 (1406) | 2.2 | 8.8 | 4.7 | 1.9 | 5.1 | 0.9 | 80.9 |
| 14 (1299) | 2.0 | 8.2 | 3.6 | 2.5 | 2.6 | 0.8 | 83.5 |
| 15 (1189) | 2.3 | 7.4 | 3.1 | 2.3 | 3.3 | 0.5 | 83.5 |
| 16 (1027) | 2.0 | 6.0 | 2.9 | 1.7 | 3.6 | 0.6 | 85.7 |
| 17 (899) | 2.7 | 5.2 | 1.7 | 2.3 | 4.3 | 0.7 | 85.5 |
| 18 (779) | 1.9 | 5.0 | 1.9 | 2.3 | 3.2 | 0.5 | 86.9 |
| 19 (680) | 2.2 | 6.2 | 1.5 | 2.1 | 2.7 | 0.2 | 88.5 |
| 20–24 (576) | 4.9 | 13.0 | 2.8 | 4.5 | 6.8 | 0.2 | 74.5 |
| ≥25 (317) | 7.3 | 23.3 | 1.9 | 6.9 | 5.1 | 0.6 | 62.8 |
See a complete list of the surgical procedures by category in Table 1. Percentages may not add to 100% because patients could have had >1 type of procedure at a given age.
n equals the number of patients in the respective age category. Patients might appear multiple times across age categories because they might have had multiple visits to the registry at different ages during the study period.
This number is expected to be 100% for this category of patients but, until recently, reporting the initial spinal closure was not mandatory for member clinics (see text for explanation).
TABLE 6.
Age-Specific Frequency Distribution of Patients With SB Across 6 Categories of Surgical Procedures: Patients With Nonmyelomeningocele SB; From the NSBPR, 2009–2013
| Age, y (n)a | Gastrointestinal, % | Neurologic, % | Orthopedic, % | Skin, % | Urologic, % | Other, % | None, % |
|---|---|---|---|---|---|---|---|
| <1 (642) | 5.9 | 59.2 | 2.2 | 3.3 | 2.8 | 2.5 | 37.7 |
| 1 (619) | 1.3 | 10.3 | 1.9 | 0.2 | 1.5 | 1.6 | 85.1 |
| 2 (587) | 0.2 | 5.5 | 2.6 | 0.2 | 2.0 | 1.4 | 89.3 |
| 3 (542) | 1.3 | 3.7 | 3.0 | 0.6 | 1.3 | 1.7 | 89.7 |
| 4 (496) | 1.2 | 5.0 | 3.2 | 0.6 | 1.8 | 1.4 | 87.9 |
| 5 (447) | 0.9 | 5.2 | 3.6 | 0.5 | 3.8 | 1.3 | 86.1 |
| 6 (416) | 1.4 | 4.3 | 2.4 | 0.7 | 1.4 | 0.7 | 90.1 |
| 7 (391) | 1.0 | 7.4 | 3.1 | 0.5 | 1.5 | 1.5 | 86.7 |
| 8 (350) | 2.0 | 3.7 | 3.7 | 0.0 | 2.6 | 1.1 | 87.7 |
| 9 (320) | 1.3 | 6.9 | 3.8 | 0.6 | 1.3 | 0.3 | 87.5 |
| 10 (290) | 2.1 | 6.6 | 3.1 | 1.0 | 1.0 | 1.0 | 87.9 |
| 11 (254) | 0.4 | 7.5 | 5.1 | 2.0 | 1.6 | 0.4 | 85.8 |
| 12 (226) | 1.3 | 4.4 | 7.5 | 1.8 | 2.7 | 0.9 | 83.2 |
| 13 (199) | 1.0 | 5.5 | 6.0 | 1.5 | 2.0 | 0.0 | 85.4 |
| 14 (181) | 0.0 | 5.0 | 5.0 | 1.1 | 1.1 | 0.6 | 87.3 |
| 15 (166) | 1.8 | 3.6 | 3.0 | 1.8 | 6.6 | 1.2 | 85.5 |
| 16 (149) | 0.0 | 7.4 | 2.7 | 3.4 | 0.7 | 0.0 | 86.6 |
| 17 (125) | 0.8 | 10.4 | 4.8 | 3.2 | 1.6 | 0.0 | 81.6 |
| 18 (100) | 1.0 | 4.0 | 0.0 | 8.0 | 2.0 | 0.0 | 85.0 |
| 19 (75) | 0.0 | 6.7 | 8.0 | 1.3 | 0.0 | 1.3 | 82.7 |
| 20–24 (61) | 4.9 | 6.6 | 8.2 | 1.6 | 3.3 | 0.0 | 82.0 |
| ≥25 (24) | 8.3 | 41.7 | 4.2 | 0.0 | 0.0 | 0.0 | 50.0 |
See a complete list of the surgical procedures by category in Table 1. Percentages may not add to 100% because patients could have had >1 type of procedure at a given age.
n equals the number of patients in the respective age category. Patients might appear multiple times across age categories because they might have had multiple visits to the registry at different ages during the study period.
Within most surgical categories, and particularly for patients with myelomeningocele SB, the proportion of patients who underwent surgery varied with age. For example, the average proportion of participants who underwent orthopedic surgery ranged from ~7% (between birth and 5 years of age) to 2% (≥18 years of age). Also, the proportion of patients who underwent skin procedures was typically <1% at early ages, with the exception of the first year of age, but reached ~7% at ≥25 years of age. Other than the neurologic procedures, such variation with age was not present in patients with nonmyelomeningocele SB. Overall, regardless of the type of SB, 75% to 90% of patients in each age category <24 years of age did not undergo any of the surgical procedures that were examined here after the first year of life. In contrast, only 50% to 63% of patients ≥25 years of age did not undergo any of these surgeries, and neurologic procedures had the highest frequencies in this age group for both types of SB: 23.3% for myelomeningocele SB and 41.7% for nonmyelomeningocele SB.
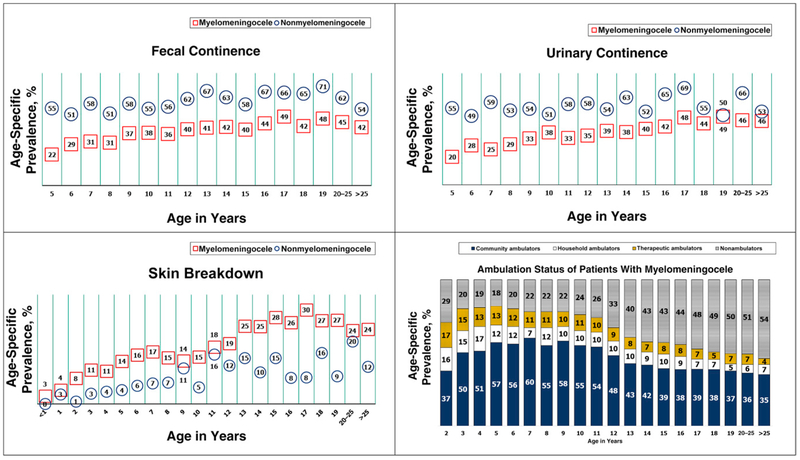
Outcomes
The age-specific distributions of the 4 outcomes (fecal continence, urinary continence, skin breakdown, and ambulation) are shown in Fig 1. In the first 3 of these outcomes, the results are segregated by SB type. For ambulation, the results are presented only for the group with the myelomeningocele SB diagnosis because the group with the nonmyelomeningocele type of SB showed little variation with age (80%–90% of them were ambulating after 2 years of age; data not shown). The age-specific prevalence of fecal continence ranged from 51% to 71% among patients with nonmyelomeningocele SB and from 22% to 49% among patients with myelomeningocele SB. For both types of SB, patients ≤10 years of age had a lower rate of fecal continence than older patients. The results for urinary continence paralleled those observed for fecal continence, with a peak in the late teenage years. On the other hand, the age-specific frequency of skin breakdown ranged from 3% to 30% among patients with myelomeningocele SB and from 0% to 20% among patients with nonmyelomeningocele SB. Overall, the prevalence of skin breakdown increased with age, particularly in patients with myelomeningocele SB after 12 years of age. Of note, <30% of participants with myelomeningocele reported skin breakdown in the previous 12 months. This prevalence peak was reached at 17 years of age.
FIGURE 1.
Age-specific prevalence of 4 major outcomes according to the type of diagnosis in patients participating in the NSBPR, 2009–2013.
Ambulation status was found to vary markedly with age for patients with myelomeningocele SB. The frequency of community ambulators peaked at 60% at 7 years of age then steadily declined to 35% at ≥25 years of age. The decline is sharper between 11 and 15 years of age (from 54% to 39%). The frequency of nonambulators is lowest at 5 years of age (18%) and highest at ≥25 years of age (54%). Among patients with the nonmyelomeningocele type of SB, 80% to 90% of them retained their community ambulation status at all ages (data not shown).
DISCUSSION
Our analysis revealed that the distributions of surgical procedures and selected health outcomes in persons with SB varied considerably by age and type of SB. Neurologic procedures to repair spinal cord lesions and to address hydrocephalus exceeded all other surgical procedures combined by more than threefold. Neurologic, gastrointestinal, orthopedic, and other surgeries appeared to decline with age more so than surgeries in urologic and skin categories. The minority of those who required surgeries at ≥18 years of age likely had long-lasting manifestations of the condition or some age-related complications. Liptak et al16 reported that older adults with SB had fewer primary care visits than younger adults with SB. However, this difference may be more attributable to failures in transition from childhood care to adult care than to successful interventions early in life.17 The relatively large proportion of orthopedic procedures that occur in the first year of life is likely due to congenital deformities that require correction. This proportion remained high until ~6 years of age, particularly among patients with myelomeningocele SB. At this age, the reliability of muscle strength measures peaks after increasing steadily from birth.18 These measures are key for the surgical management of patients with orthopedic conditions. The skin procedures that occur before 1 year of age are likely skin flaps and skin grafts associated with spinal closure. Subsequent skin procedures likely addressed skin breakdown, a consequence of both the friction and pressure related to the use of orthotics to assist with ambulation and positioning and the constant pressure on insensate skin areas due to immobility, particularly with increasing body size. Urologic procedures occurred more frequently at 4 to 6 years of age, coinciding with participants reaching school age, when incontinence becomes more of a concern.13 Urologic and gastrointestinal procedures that were performed on adolescents and adults may be due to the natural history of SB-related dysfunction, complications from previous surgical procedures, age-related problems (eg, calculus disease), or personal choice for later surgical procedures for continence.
We found that the proportion of participants who underwent neurologic procedures was relatively high among patients with myelomeningocele SB after 20 years of age. This is likely the combined result of several factors, such as a small number of participants, some of them affected by more severe manifestations of SB (adults with mild manifestations of SB are less likely to be in a clinic-based registry) or shunt malfunction. Finally, we noted that >80% of participants reported having undergone no additional surgical procedures after the first year of life except for participants in the last age category, which spanned ages 25 to 83 years.
Our results clearly revealed that at all ages, positive health outcomes were more frequent among participants with nonmyelomeningocele SB than among patients with myelomeningocele SB. This result was expected because patients with nonmyelomeningocele SB tend to experience fewer secondary complications, fewer functional impairments, and tend to undergo fewer surgeries than patients with myelomeningocele SB.11 In both types of SB, fecal and urinary continence increased with age, indicating that surgical procedures and interventions that are performed on these patients are likely having a positive impact on these 2 outcomes. Regarding ambulation and skin breakdown, our findings were consistent with previous reports that revealed that patients with myelomeningocele SB were more likely to develop skin breakdown during their teenage years than during the other ages19 and were more likely to decrease ambulation as they aged.20
A major limitation of this study was the incomplete capture of data on initial spinal closure surgery among participants with myelomeningocele SB in the NSBPR. This limitation affects the accuracy of the estimation of an important category of surgical procedures (neurologic); however, even without the capture of data on initial spinal closure, neurologic procedures predominated in the first year of life. Another limitation was the reporting of surgical procedures in broad categories, which makes it impossible to note how many single types of procedures of the same category each patient had and assess the impact of multiple related surgeries on a single patient. Regarding data collection, with the combined use of a serial cross-sectional design (1 initial interview and several interviews during annual clinic visits) with retrospective data collection (medical record abstraction), the number of surgical procedures may have been underestimated if the recall of medical histories was inaccurate and the pertinent medical records were missing. In addition, the longitudinal collection of data was not homogeneous (ie, some patients had data collected multiple times whereas others may have had data collected from a single time point). Furthermore, not all clinics were involved in the registry for the entire duration of the study. This was particularly problematic for the continence status because it may have changed with time. Regarding representativeness of the data, we have not confirmed that the population of patients with SB from the selected NSBPR clinics is comparable with the population of those who do not attend these SB clinics; thus, the results of this article are only applicable to patients who have attended specific SB clinics in the United States. Additionally, selection bias could have been an issue because we are not certain that patients who were enrolled in the NSBPR are comparable with those who were not enrolled, although most clinics enrolled a high percentage of their eligible patients, and in a previous analysis of patients who were enrolled in the NSBPR, selection bias was not detected.21 Survival bias could have also been an issue, but we did not have enough mortality data to examine it. Finally, this was a descriptive study. It did not include multivariate analyses to test for trends and group differences or to predict surgical procedures and outcomes at specific ages; however, this study suggests that age is an important factor in models to predict outcomes and surgical procedures in this population, particularly in those with myelomeningocele SB.
CONCLUSIONS
Using cross-sectional data from the NSBPR, we described the age-specific occurrence of key surgical procedures and 4 health outcomes in a large population of patients with SB who attended specialty clinics in the United States. This thorough description may contribute to the planning of care across the life spans of persons with SB by informing health care providers and families of patterns of surgeries and outcomes over time. Our findings may provide insight into the ages at which the frequency of surgical procedures and prevalence of outcomes increase or decrease. We noted that the prevalence of fecal and urinary continence tends to increase with age, likely as the result of opportune surgical and behavioral interventions. On the other hand, as patients with SB age, the increasing prevalence of skin breakdowns must be addressed because this is a preventable outcome. A next step could be to develop statistical models to predict outcomes and surgical procedures at specific ages in persons with SB.
WHAT’S KNOWN ON THIS SUBJECT:
Patients who are born with spina bifida undergo a series of surgical procedures that are focused on preventing serious health outcomes during the patients’ lifetimes.
WHAT THIS STUDY ADDS:
In this study, we provide the distribution of 6 types of surgical procedures and 4 health outcomes over a wide range of ages in a large group of patients with spina bifida.
Acknowledgments
FUNDING: The National Spina Bifida Patient Registry is funded by the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
ABBREVIATIONS
- NSBPR
National Spina Bifida Patient Registry
- SB
spina bifida
Footnotes
Ms Alabi designed the study, performed the data analyses, wrote the first completed draft of the manuscript, and integrated suggestions from coauthors into the subsequent drafts; Ms Thibadeau provided expert consultation on the structure and data content of the National Spina Bifida Patient Registry and critically reviewed subsequent versions of the manuscript; Dr Wiener provided expert consultation on urologic procedures and health outcomes in general and critically reviewed subsequent versions of the manuscript; Dr Conklin provided expert consultation on orthopedic procedures and health outcomes in general and critically reviewed subsequent versions of the manuscript; Dr Dias provided expert consultation on neurologic procedures and health outcomes in general and critically reviewed subsequent versions of the manuscript; Dr Sawin provided expert consultation on the overall array of surgical procedures and health outcomes and critically reviewed subsequent versions of the manuscript; Dr Valdez conceptualized the study, supervised the work, directed the analyses of the data, and contributed to editing and critically reviewing all versions and sections of the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2018-1985.
REFERENCES
- 1.Hampel C, Wienhold D, Benken N, Eggersmann C, Thüroff JW. Prevalence and natural history of female incontinence. Eur Urol. 1997;32(suppl 2):3–12 [PubMed] [Google Scholar]
- 2.Laurence KM, Coates S. The natural history of hydrocephalus. Detailed analysis of 182 unoperated cases. Arch Dis Child. 1962;37:345–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laurence KM. The natural history of spina bifida cystica: detailed analysis of 407 cases. Arch Dis Child. 1964;39:41–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pound CR, Partin AW, Eisenberger MA, Chan DW, Pearson JD, Walsh PC. Natural history of progression after PSA elevation following radical prostatectomy. JAMA. 1999;281 (17):1591–1597 [DOI] [PubMed] [Google Scholar]
- 5.Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg. 2001;34(3):114–120 [DOI] [PubMed] [Google Scholar]
- 6.Parker SE, Mai CT, Canfield MA, et al. ; National Birth Defects Prevention Network. Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol. 2010;88(12):1008–1016 [DOI] [PubMed] [Google Scholar]
- 7.Liptak GS, El Samra A. Optimizing health care for children with spina bifida. Dev Disabil Res Rev. 2010;16(1):66–75 [DOI] [PubMed] [Google Scholar]
- 8.Wilson CB, Llewellyn RC. The surgical management of meningoceles and meningomyeloceles. J Pediatr. 1962;61:595–602 [DOI] [PubMed] [Google Scholar]
- 9.Shin M, Kucik JE, Siffel C, et al. Improved survival among children with spina bifida in the United States. J Pediatr. 2012;161(6):1132–1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharrard WJ. The mechanism of paralytic deformity in spina bifida. Dev Med Child Neurol. 1962;4: 310–313 [DOI] [PubMed] [Google Scholar]
- 11.Sawin KJ, Liu T, Ward E, et al. ; NSBPR Coordinating Committee. The National Spina Bifida Patient Registry: profile of a large cohort of participants from the first 10 clinics. J Pediatr. 2015;166(2):444–450.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webb TS. Optimizing health care for adults with spina bifida. Dev Disabil Res Rev. 2010;16(1):76–81 [DOI] [PubMed] [Google Scholar]
- 13.Thibadeau JK, Ward EA, Soe MM, et al. Testing the feasibility of a National Spina Bifida Patient Registry. Birth Defects Res A Clin Mol Teratol. 2013;97(1):36–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hotter MM, Feiwell E, Perry R, Perry J, Bonnett C. Functional ambulation in patients with myelomeningocele. J Bone Joint Surg Am. 1973;55(1):137–148 [PubMed] [Google Scholar]
- 15.SAS Institute, Inc. SAS 9.3. Cary, NC: SAS Institute, Inc; 2010 [Google Scholar]
- 16.Liptak GS, Robinson LM, Davidson PW, et al. Life course health and healthcare utilization among adults with spina bifida. Dev Med Child Neurol. 2016;58(7):714–720 [DOI] [PubMed] [Google Scholar]
- 17.Dicianno BE, Kurowski BG, Yang JM, et al. Rehabilitation and medical management of the adult with spina bifida. Am J Phys Med Rehabil. 2008;87(12) :1027–1050 [DOI] [PubMed] [Google Scholar]
- 18.McDonald CM, Jaffe KM, Shurtleff DB. Assessment of muscle strength in children with meningomyelocele: accuracy and stability of measurements over time. Arch Phys Med Rehabil. 1986;67(12):855–861 [PubMed] [Google Scholar]
- 19.Kim S, Ward E, Dicianno BE, et al. ; National Spina Bifida Patient Registry. Factors associated with pressure ulcers in individuals with spina bifida. Arch Phys Med Rehabil. 2015;96(8):1435–1441.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schechter MS, Liu T, Soe M, Swanson M, Ward E, Thibadeau J. Sociodemographic attributes and spina bifida outcomes. Pediatrics. 2015;135 (4). Available at: www.pediatrics.org/cgi/content/full/135/4/e957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu T, Ouyang L, Thibadeau J, et al. Longitudinal study of bladder continence in patients with spina bifida in the National Spina Bifida Patient Registry. J Urol. 2018;199(3):837–843 [DOI] [PMC free article] [PubMed] [Google Scholar]