Abstract
Objective:
Much is known about the associations between negative factors and adjustment to chronic pain. However, less is known about how positive factors [e.g., positive affect (PA), resilience] function in relation to disability and mood in individuals with multiple sclerosis (MS). To better understand how positive factors contribute to function we sought to determine if (1) PA and/or trait resilience moderate the associations between pain intensity and function (pain interference, depressive symptoms), and (2) trait resilience concurrently mediates the association between PA and function in a sample of individuals with MS.
Methods:
455 adults with MS provided data via an ongoing survey.
Results:
Controlling for negative affect, demographic and disease-related variables, cross-sectional path analysis revealed the following: PA and trait resilience did not moderate the associations between pain intensity and pain interference (βPA = 0.01, p = .86; βRESILIENCE = 0.04, p = .33), and pain intensity and depression (βPA = 0.01, p = .79; βRESILIENCE = −0.02, p= .60). However, trait resilience significantly mediated the associations between PA and both criterion variables (abINTERFERENCE = −0.03, p = .03; abDEPRESSION = −0.13, p < .001).
Conclusions:
The findings provide preliminary support for the conclusion that PA is indirectly related to pain interference and depression via resilience, rather than serves as a protective function. The findings are consistent with theoretical models suggesting that increases in PA build personal resources. Research examining the potential benefits of increasing PA and resilience to improve pain outcomes in individuals with MS is warranted.
Keywords: pain, depression, function, emotion, resilience
Chronic pain is a common condition affecting over half of adults with multiple sclerosis (MS; O’Connor, Schwid, Herrmann, Markman, & Dworkin, 2008). Pain can have a significant, negative impact on physical and psychosocial functioning in both the short term, by interfering with daily activities and mood (Day et al., 2016), and the long term, by contributing to increases in disability over time (Molton et al., 2014). Consistent with the pain literature at large, research on coping with pain in MS has focused primarily on the contribution of maladaptive thoughts and behaviors to mood and quality of life (Alschuler, Ehde, & Jensen, 2013). In contrast, there is a paucity of research on the role of positive factors in coping with pain in MS despite the likely meaningful contribution of such factors to pain-related outcomes.
There are both empirical and theoretical reasons to explore the role of positive factors in coping with pain in MS. Empirically, there are numerous studies that suggest positive factors have important effects on pain-related outcomes. In a prior study that included individuals with multiple conditions, including MS, researchers found that positive factors, such as pain acceptance and positive affect, contribute to better mental health over and above the contribution of negative factors like pain catastrophizing (Alschuler, Kratz, & Ehde, 2016). These results are consistent with the more robust literature on the role of positive factors in pain in non-MS populations. Such factors have also been called resilience resources at the trait level and resilience mechanisms at the state level (Sturgeon & Zautra, 2010) in pain resilience models, because they have been found to promote functioning and adjustment to pain (Finan & Garland, 2015; Yeung, Arewasikporn, & Zautra, 2012) and their impact is asserted over and above those associated with negative factors (i.e., sources of vulnerability and vulnerability mechanisms), such as in the case of positive affect (Davis, Zautra, & Smith, 2004). Positive factors have also been shown to be associated with lower incidence of disability risk in other pain populations (Johnson Wright, Zautra, & Going, 2008; Fisher, Snih, Ostir, & Goodwin, 2004).
It is also important to consider whether positive factors may impact negative mood, as individuals with MS and especially those with pain often also experience depressed mood (Alschuler, Jensen, & Ehde, 2013). There is support for a negative association between positive factors and negative mood in individuals with physical disabilities (including MS) and pain (Alschuler, Kratz, & Ehde, 2016), and additional research in MS populations at large (i.e., those not limited to those experiencing pain). For example, greater positive emotion is associated with reduced depressive symptoms in people with MS (Kratz, Ehde, & Bombardier, 2014; Hart, Vella, & Mohr, 2008; Mohr et al., 2005); and high levels of trait resilience - the general ability to respond adaptively to challenges, characterized by relatively swift recovery, maintenance of valued pursuits, and growth (Zautra, Arewasikporn, & Davis, 2010) - is similarly associated with less pain interference (Walsh et al., 2016), reduced depressive symptom severity (Silverman, Molton, Alschuler, Ehde, & Jensen, 2015; Edwards, Alschuler, Ehde, Battalio, & Jensen, 2017), and better quality of life (Terrill et al., 2014) in adults with acquired physical disabilities, including MS. Taken together, these findings indicate that research to determine if the positive relationships of positive affect and trait resilience with better mood and functioning extend specifically to individuals with MS is warranted.
There is also theoretical support for this concept. The broaden-and-build model focuses on the indirect influence of positive emotion on function through the building of psychosocial resources such as trait resilience (Fredrickson, 2001). This theory posits that positive emotions at the state level can facilitate patterns of thought that are flexible, creative, and open to information input, especially in challenging situations in which individuals are compelled to engage in coping (Tugade, Fredrickson, & Feldman Barrett, 2004; Fredrickson, 2001). In the short-term, cognitive broadening allows for flexibility in attending to varying inputs. Repeated states of cognitive broadening over time may lead to a “broadened mindset” that becomes habitual and trait-like. This mindset thus facilitates psychological flexibility and approach-oriented behavior (Tugade & Fredrickson, 2004), two constructs associated with trait resilience (Wilhelm, Geerligs, & Peisah, 2014), eventually increasing an individual’s ability to cope adaptively (Tugade et al, 2004; Conway, Tugade, Catalano, & Fredrickson, 2012).
Although there is no prior research that directly tests the broaden-and-build process in models of pain coping, there is important research that supports aspects of the broaden-and-build model in other populations. For instance, in their study of individuals with pain in the context of physical disability (including MS), researchers found that the use of positive affect and positive pain coping strategies together were specifically associated with better mental health outcomes; though the same relationship was not present for physical health outcomes (Alschuler et al, 2013). In other research, a robust relationship was found between positive affect and resilience (Black & Dorstyn, 2015; Quale & Schanke, 2010), and trait positive emotion was found to play a central role in accounting for the relationships between trait resilience, psychopathology (depression, post-traumatic stress disorder), and pain interference (Walsh et al, 2016) in individuals with acquired disabilities. Furthermore, support for this model has been found in a mixed chronic pain sample in which individuals reporting high trait resilience exhibited maladaptive cognitive styles (i.e., pain catastrophizing) less frequently than those reporting low trait resilience (Ong, Zautra, & Reid, 2010). Finally, highly resilient individuals have been shown to recover more swiftly from daily pain catastrophizing through enhanced positive emotion (Ong et al, 2010), consistent with broaden-and-build model. These studies suggest trait positive affect may indirectly influence adaptation to pain by facilitating trait resilience.
Alternatively, the stress and coping model posits that trait positive affect and trait resilience serve a protective function. In this model, protective factors (e.g., positive affect, resilience) are thought to weaken the relationship between stressor and negative outcome, thus reducing or “buffering” against the negative impact of pain on functioning (Folkman & Moskowitz, 2004). Although the potential buffering effects of positive affect and resilience have not been well studied in MS, significant findings have been found in other chronic health condition populations (Finan & Garland, 2015; Yeung et al., 2012). For example, in a sample of adults with fibromyalgia, osteoarthritis, and rheumatoid arthritis, weaker associations between pain intensity and negative affect were evidenced on weeks when higher than average elevations in positive affect were reported (Zautra, Johnson, & Davis, 2005; Strand et al., 2006). Similar buffering effects have been found in experimental pain studies for women who report high baseline positive affect (Ruiz-Aranda, Salguero, & Fernández-Berrocal, 2010). Trait resilience has been found to buffer against the influence of pain, moderating reports of experimentally-induced pain and stress (Friborg et al., 2006), and buffering against the effects of stress on depression in individuals with spinal cord injury (Catalano, Chan, Wilson, Chiu, & Muller, 2011). Taken together, these studies suggest that high levels of positive affect and trait resilience may protect against the negative influence of pain on pain outcomes.
Having a better understanding of how positive factors affect pain outcomes would add to the growing research literature on pain adaptation and have implications for clinical intervention. If, for example, positive factors function by moderating the influence of pain on pain outcomes, as is proposed in the stress and coping model, there might be implications for whom an intervention is applied (e.g., individuals reporting high levels of pain) and when (e.g., in response to pain flares). If positive factors assert downstream effects on pain outcomes, consistent with the broaden-and-build model, a more general approach to increasing positive factors might be useful.
The present study tested core elements of the broaden-and-build and stress and coping models together in the context of MS and pain by considering how two trait-level positive factors or resilience resources, positive affect and trait resilience, relate to pain interference and depressive symptoms in a sample of adults with MS. We hypothesized both indirect and moderating effects, consistent with both theoretical models. First, consistent with the broaden- and-build model, we hypothesized that positive affect would be indirectly associated with the criterion variables (pain interference and depressive symptoms) through trait resilience, with those reporting high levels of positive affect also reporting greater trait resilience, which in turn would be associated with less pain interference and depression (i.e., significant cross-sectional indirect, or mediating effects). We also anticipated direct, negative associations between positive affect and the criterion variables. Second, consistent with a stress and coping model, we hypothesized that positive affect and trait resilience would function as protective factors, moderating the positive associations between pain intensity and the criterion variables. Specifically, we expected weaker associations between pain intensity and the criterion variables for those reporting high levels of positive affect and trait resilience, relative to those reporting low levels of positive affect and trait resilience (i.e., moderating effects).
Method
Participants and Procedures
This cross-sectional study used data collected from an ongoing longitudinal survey examining aging with a long-term physical disability (see, e.g., Bamer, Cook, & Amtmann, 2012; Molton et al., 2014; Silverman et al., 2015). Participants were recruited from the University of Washington Disability Registry and print and web advertisements. Eligibility criteria for the parent study include: being 18 years of age or older, being able to read and understand English, and having a chronic neurologic condition associated with physical disability, including but not limited to MS. For this study, only participants with a self-reported diagnosis of MS who completed the survey at year 6 (2015–2016) were included (N = 455). Several studies have been conducted using data from the larger parent study, however this study is the first to examine the potential direct, indirect, and moderating effects of positive affect and trait resilience on the pain intensity-pain interference and pain intensity-depression associations in adults with MS.
Surveys are mailed annually to eligible participants with a postage-paid return envelope and consent form. Non-responders receive two reminders to complete the survey at 4 and 6 weeks via a letter and telephone call, respectively. Participants are paid US$25 per survey completed. A total of 1,573 surveys were mailed out during year 6, with 1,466 completed surveys returned. Of these, 455 were participants with MS. The response rate for the present study was 93%.
All returned surveys were checked by research staff for missing data; when found, participants were called up to three times to obtain the missing data. The Human Subjects Division of the University of Washington approved all study procedures.
Measures
Demographic and disease-related characteristics.
Participants were asked to provide demographic data (age, sex, education level, income, race/ethnicity, marital status) and information related to their MS diagnosis (MS type, MS duration).
Negative affect.
A short form of the Positive and Negative Affect Schedule (Mackinnon et al., 1999) was used to assess negative affect. Participants rated the extent to which they experienced five negative emotion adjectives (e.g., “distressed,” “scared”) on a 1 (“Very slightly or not at all”) to 5 (“Extremely”) Likert scale. Internal consistency of the measure was excellent in the current sample (Cronbach’s α = .995).
Pain interference.
The four-item Pain Interference short form from the Patient Reported Outcomes Measurement Information System-29 (PROMIS-29) Health Profile (Amtmann et al., 2010; Cella et al., 2010) was used to assess pain interference. Participants rated the level of pain interference in daily activities (e.g., “To what extent did pain interfere with work around home?”) in the past 7 days using a 1 (“Not at all) to 5 (“Very much”) Likert scale. Like all PROMIS measures, the items were scored on a t-score metric (M= 50 and SD = 10 in the normative sample). The PROMIS Pain Interference item bank has been validated for use in adults with MS (Bamer et al., 2012; Cook, Bamer, Amtmann, Molton, & Jensen, 2012). The internal consistency of the measure was excellent (Cronbach’s α = .90).
Depressive symptoms.
The 6-item PROMIS Profile-43 short form (Pilkonis et al, 2011; Teresi et al., 2009) was used to assess depressive symptoms. Sample items include: “I felt hopeless,” “I felt depressed”). Participants rated how often they experienced each depressive symptom in the past 7 days on a 1 (“Never”) to 5 (“Always”) Likert scale. As with the pain interference items, a depression score was computed on a t-score metric. The PROMIS Depression item bank has been validated for use in MS samples (Bamer et al., 2012; Amtmann et al., 2014). However, the internal consistency of the measure in the current sample was poor (Cronbach’s α = .58).
Pain intensity.
Participants were asked to rate average pain intensity in the past week on a single-item, 0 (‘No pain”) to 10 (“Pain as bad as you can imagine”) numerical rating scale (NRS). A great deal of research supports the reliability and validity of the NRS as a measure of pain intensity in various pain populations (Jensen & Karoly, 2011), including MS (Dworkin et al., 2005).
Positive affect.
A short form of the Positive and Negative Affect Schedule (Mackinnon et al, 1999) was also used to measure positive affect. Five positive emotion adjectives (e.g., “enthusiastic,” “determined”) were presented. Participants were asked to rate the extent to which they experienced these emotions in the past week on a 1 (“Very slightly or not at all”) to 5 (“Extremely”) scale. The internal consistency of the measure was excellent (Cronbach’s α = .96) in the current sample.
Trait resilience.
The 10-item short form Connor Davidson Resilience Scale was used to measure trait resilience (Campbell-Sills & Stein, 2007). This scale measures the degree to which respondents are able to adapt to challenges (e.g., “I am able to adapt when changes occur “ “I am able to handle unpleasant or painful feelings like sadness, fear, and anger”). Respondents were asked to rate how true each trait resilience descriptor was for them in the past month on a 0 (“Not true at all”) to 4 (“True nearly all the time”) scale. This measure has been validated for use in individuals with physical disabilities including in individuals with MS (Terrill et al, 2014). The internal consistency of the scale was excellent (Cronbach’s α = .96) in the current sample.
Data Analysis
We first computed descriptive statistics (mean, standard deviations, percentages, skewness, kurtosis) for the demographic, pain, and disease-related variables to describe the sample (see Table 1) and examine assumptions for planned data analyses, all of which were met.
Table 1.
Demographic and Disease-Related Sample Characteristics (N = 455)
| Sample Characteristics | n (%) | M (SD) |
|---|---|---|
| Age (years) | 61.0 (10.1) | |
| < 45 | 25 (5.5) | |
| 45–64 | 273 (60.0) | |
| ≥ 65 | 157 (34.5) | |
| Race | ||
| White | 403 (88.6) | |
| Black | 25 (5.5) | |
| American Indian | 2 (0.4) | |
| Asian | 1 (0.2) | |
| More than 1 race | 21 (4.6) | |
| Sex | ||
| Female | 375 (82.4) | |
| Male | 80 (17.6) | |
| Education | ||
| High school or less | 43 (9.4) | |
| Tech or some college | 147 (17.2) | |
| College degree or higher | 264 (58.0) | |
| Annual household income | ||
| < $25,000 | 77 (16.9) | |
| $25,000-$55,000 | 113 (24.8) | |
| $56,000-$85,000 | 70 (15.4) | |
| ≥ $86,000 | 115 (25.3) | |
| Marital status | ||
| Married/civil union | 284 (62.5) | |
| Living with significant other | 16 (3.5) | |
| Divorced/separated | 94 (20.6) | |
| Widowed | 35 (7.7) | |
| Never married | 25 (5.5) | |
| MS type | ||
| Relapsing-remitting | 271 (59.6) | |
| Secondary progressive | 101 (22.2) | |
| Primary progressive | 29 (6.4) | |
| Progressive-relapsing | 12 (2.6) | |
| Disease duration (years) | 21.2 (9.6) | |
| Average paina (range: 0–10) | 2.94 (2.52) | |
| No pain | 97 (21.3) | |
| Mild pain | 132 (29.0) | |
| Moderate pain | 146 (32.1) | |
| Severe pain | 79 (17.4) |
Note:
Cut-off scores for pain intensity adapted from Alschuler, Jensen, & Ehde, 2012 where mild: 1–2, moderate: 3–5, and severe: 6–10.
Data from all participants in the sample were included in the analyses, including those who did not report pain. We then performed a series of t-tests and correlation analyses to identify potential confounding variables associated with the criterion variables that should be controlled in the primary analyses. We used path analysis with the TYPE = GENERAL command in Mplus 7.6 (Muthén & Muthén, 1998) to model both theoretical models (i.e., broaden-and-build, stress and coping) simultaneously, and evaluate the hypothesized direct, indirect (cross-sectional mediation), and moderation effects. Using path analysis allowed us to estimate the strength of the association between two variables while controlling for shared variance among all variables in the model, thus allowing for a “purer” estimate of the association. Path analysis also allowed us estimate all hypothesized direct, indirect, and moderation effects simultaneously. Model fit was evaluated using the following criteria representing good fit: Standardized Root Mean Square Residual (SRMR) ≤ .08, The Root Mean Square Error of Approximation (RMSEA) ≤ .05, and Bender’s Comparative Fit Index (CFI) ≥ .95; and acceptable fit: RMSEA ≤ .08 and CFI ≥ .90 (Hu & Bentler, 1998). Potential confounding variables were entered individually into the model. Both linear and quadratic relationships between age and depressive symptoms were also entered, as there is evidence that depressive symptoms peak in middle age and decrease over time thereafter (i.e., inverted U-shaped; Alschuler et al, 2013; Molton et al., 2014). We also included negative affect as a covariate to help distinguish between effects attributed to both positive and negative affect. Nonsignificant variables were eliminated; significant covariates were retained in the final models. Indirect effects were tested by using the product of coefficients (ab; Sobel, 1982), where the a path refers to the relationship between the independent variable (positive affect) and the mediator (resilience), the b path refers to the relationship between the mediator and criterion variable (pain interference, depression). We planned to use post hoc simple slopes analysis (Aiken & West, 1991) to interpret any significant moderation effects that emerged.
Results
Participant Description
Descriptive information about the sample (N= 455) can be found in Table 1. The mean age of the sample was 61 years (range: 27–90). The participants were primarily female (82%), White (89%), and highly educated, with 58% having a college degree or higher. The majority of the participants (60%) indicated they had the relapsing-remitting MS subtype, and the mean disease duration of the sample was 21.2 years (range: 4–61). In the overall sample, 79% of the participants reported some level of pain, and the average level of pain intensity reported was mild (2.94 out of 10, SD= 2.52). Mean scores on the PROMIS pain interference scale (M= 55.12, SD= 10.06) were markedly higher and those on the PROMIS depression scale (M= 51.00, SD= 9.31) were somewhat higher than those in the normative population (see Table 2 for additional descriptive statistics).
Table 2.
Descriptive information for and correlations among study variables (N = 455).
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Pain interference | |||||
| 2. Depressive symptoms | 0.42 | ||||
| 3. Pain intensity | 0.78 | 0.19 | |||
| 4. Positive affect | −0.24 | −0.34 | −0.20 | ||
| 5. Resilience | −0.33 | −0.59 | −0.29 | 0.47 | |
| M | 55.12 | 51.00 | 2.94 | 14.79 | 28.82 |
| SD | 10.06 | 9.31 | 2.52 | 4.05 | 7.25 |
| Range | 41.6 – 75.6 | 38.4 – 80.3 | 0–10 | 4–24 | 3–40 |
| Skewness | 0.05 | 0.35 | 0.62 | −0.19 | −0.42 |
| Kurtosis | −0.85 | −0.08 | −0.52 | −0.46 | −0.10 |
Note. All correlations significant at p < .001.
Overall Model Fit
The model demonstrated good fit, χ2(10) = 15.22, p= .12, RMSEA = .034, CFI = .994, SRMR = .037. The model accounted for 61% of the variance in pain interference, 50% of the variance in depressive symptoms, 39% of the variance in resilience, and 3% of the variance in positive affect.
Broaden-and-Build Model
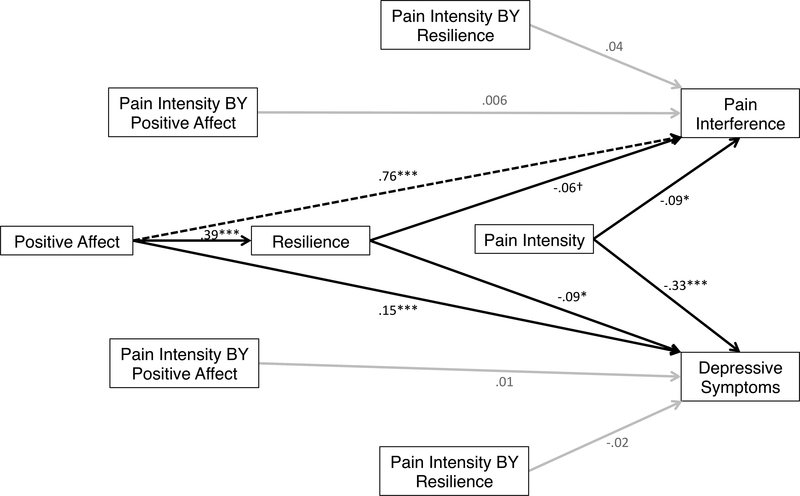
All direct effects were in the hypothesized directions (see Figure 1 for standardized parameter estimates). Positive affect and trait resilience were positively associated (a path); trait resilience was negatively associated with pain interference (b1 path) and depressive symptoms (b2 path); and positive affect was negatively associated with depressive symptoms (c3 path), but not pain interference (c2 path), though there was a negative trend.
Figure 1.
Path analysis model showing standardized parameter estimates of hypothesized pathways. Black arrows denote significant paths, black dashed arrows denote marginal paths, gray paths denote nonsignificant paths. †p<.10, *p<.05, **p<.01, ***p<. 001
The hypothesized cross-sectional indirect effects were also significant. Trait resilience significantly mediated the cross-sectional associations between pain intensity and the criterion variables (ab1 pain interference = −0.03 , p = .03; ab2 depression = −0.13 , p< .001).
Stress and Coping Model
As expected, pain intensity was positively associated with pain interference and depressive symptoms (see Figure 1 for standardized parameter estimates). However, and inconsistent with the hypotheses based on a stress and coping model, there were no significant interaction effects that suggested moderation for either criterion variable. That is, positive affect and trait resilience did not moderate the association between pain intensity and pain interference (βPOSITIVE AFFECT = 0.006, p = .86; βRESILIENCE = 0.04, p = .33), nor did they moderate the association between pain intensity and depressive symptoms (βPOSITIVE AFFECT = 0.01, p= .79; βRESILIENCE = −0.02, p= .60).
Discussion
The purpose of this study was to evaluate the potential role of positive factors in the context of coping with MS. Using the broaden-and-build model and a stress and coping model as the theoretical foundation, we sought to better understand how two trait-level positive factors associated with pain adaptation—positive affect and resilience—relate to pain interference and depressive symptoms in people with MS. Results yielded preliminary support for the broaden- and-build model, but did not support the stress and coping model.
Consistent with the broaden-and-build model, trait resilience was found to partially mediate the cross-sectional associations between positive affect and the criterion variables (pain interference and depressive symptoms). Consistent with our hypotheses, the relationships between (1) high levels of positive affect and greater trait resilience, and (2) greater trait resilience and better pain outcomes, replicate those found in the literature outside of pain (Kratz et al., 2014; Hart et al., 2008, Walsh et al., 2016; Black & Dorstyn, 2015). The present study’s findings support the existence of similar associations in people with MS. We also found significant cross-sectional mediating effects that were consistent with our hypotheses. Trait resilience mediated the associations between positive affect and pain interference, and positive affect and depressive symptom severity. These findings may have clinical utility for rehabilitation professionals. Assuming that the direction of relationships among study variables is accurate, one could imagine that individuals who present as anhedonic (i.e., low in positive emotions) or have a history of difficulty dealing with stressful circumstances (i.e., low trait resilience), might be at risk for poor pain outcomes. Early identification of at-risk individuals could result in more immediate intervention before symptoms worsen.
We did not find support for the stress and coping model, as the relationships between pain intensity and the criterion variables were not moderated by positive affect or trait resilience. The lack of support for moderation effects indicates a lack of support for a stress and coping model in which positive affect and/or resilience weaken the relationship between pain intensity and function. It is possible that positive affect and trait resilience are not sufficient in buffering the effects of pain intensity on pain interference and depression, or that potential bidirectional effects may be obscuring buffering effects. On the other hand, the presence of cross-sectional mediation effects suggests that a broaden-and-build model in which positive emotion affects pain-related function through resources (i.e., trait resilience) may better describe how positive emotion relates to the relationship between pain intensity and function. While there are a number of studies that have found strong associations between measures of resilience and pain outcomes (e.g., Alschuler et al, 2016) there are some that have found weak or no associations at all (e.g., Newton-John, Mason, & Hunter, 2014). These differences may be due to differences in conceptualization and measurement of trait resilience or other factors. Further study of the potentially complex relationships between trait resilience, other positive factors, and pain outcomes is needed, as are additional tests of the broaden-and-build and stress and coping models.
Importantly, the present study supports the development of clinical interventions that attend to the role of positive factors in improving pain outcomes in individuals with MS. In non-MS populations, there have been promising trials targeting positive factors such as positive affect and resilience in psychosocial interventions to reduce pain and psychosocial distress. Preliminary research on novel interventions that utilize positive activities (e.g., gratitude exercises, positive reappraisal, using strengths) to enhance positive factors such as positive affect, hope, and optimism have been found to reduce pain (Müller et al., 2016; Bartley, 2017; Hassett, 2017). Within MS, there have been non-pain-focused studies that focus on building resilience that have demonstrated the ability to modify positive factors (Alschuler, Arewasikporn, Nelson, Molton, & Ehde, 2018; Pakenham, Mawdsley, Brown, & Burton, 2018). In addition to reducing pain and depression, positive activity interventions have also been shown to increase well-being (Bolier et al, 2013; Sin & Lyubomirsky, 2009). Helping individuals with MS find ways to live the “good life” is a concern that often comes up in rehabilitation psychology work (Dunn & Brody, 2008). The use of the positive activity interventions could potentially help meet this need. Given the findings of the present study and others (e.g., Alschuler et al, 2016; Black & Dorstyn, 2015), there is support for the development of interventions targeting positive factors to improve pain and mood outcomes in individuals with MS, including through the modification of prior work to attend to specific, MS-related conditions such as chronic pain.
The current study’s focus on resilience is of particular relevance for the field of rehabilitation psychology, as one of the central goals of the field is to help individuals overcome day-to-day obstacles such as pain, associated with disability and more broadly facilitate adjustment to disability. The focus on positive factors is consistent with calls for rehabilitation professionals to use a strengths-based approach to facilitate positive functioning when working with individuals with disabilities (Wright, 1983; Dunn & Brody, 2008).
Limitations
The conclusions of this study are limited by the cross-sectional nature of the data. For instance, the cross-sectional mediational analyses related to the broaden-and-build model are absent the preferred temporal precedence that would be present in longitudinal studies. Similarly, when assessing the buffering effect posited by the stress and coping model, it would have been preferable to identify a causal relationship between pain intensity and pain outcome. Although we hypothesized a particular sequence of effects that has been established with methods that have stronger support for causality (e.g., laboratory and intervention studies; see Finan & Garland, 2015), we acknowledge that reasonable arguments exist for reverse causal effects or bidirectional associations. For example, depression might precede pain intensity (Gatchel, Peng, Peters, Fuchs, & Turk, 2007), rather than pain intensity preceding depression. It is also possible that the direct and indirect effect estimates may be overestimated, as evidence of increased Type I error in cross-sectional mediation has been found in some studies (Sheikh, Abelsen, & Olsen, 2016). We could not model growth processes associated with broaden-and-build theory, which posits increases in positive emotion causes subsequent increases in personal resources (i.e., resilience). Thus, although by testing these two models together we find preliminary empirical support for the broaden-and-build model in understanding pain adaptation, future studies would benefit from using research designs that examine change and potential causality over time (e.g., lagged effects analysis in time series or longitudinal data, or manipulation of pain, positive affect, or resilience in laboratory paradigms).
Another intriguing option for future longitudinal research would be to utilize ecological momentary assessment (EMA) of pain and affect to assess real-time states and thus better examine state-level relationships. Studies using EMA to explore common MS symptoms such as pain, fatigue, and depressed mood have found that symptoms can vary considerably within individuals and throughout the course of the day (Kratz, Murphy, & Braley, 2017). Given that positive affect and other variables examined in this study may also vary considerably within individuals and across time, EMA methods may help elucidate what might be complex relationships. For example, EMA could allow one to examine how morning positive affect affects end of day function, and whether midday resilience mediates this relationship.
An additional limitation, beyond the cross-sectional nature of the data, is that the sample was disproportionately female, and therefore the findings may not generalize to male adults with MS. Similarly, the findings likely do not capture the experience of young, newly diagnosed people with MS-related pain given that the average age of onset is 30 years (Milo & Miller, 2014) and only 3% of our sample was under the age of 40. We also did not examine other variables that may influence the study variables, such as fatigue, sleep, medication use, and other symptoms. Nevertheless, it is still possible to gather meaningful information about the potential role of positive affect and resilience in pain, mood, and function from the present study.
Conclusions
This study supports the possibility that our understanding of adaptation to pain in people with MS may be improved by examining positive constructs such as positive affect and resilience. We found that positive affect may be indirectly related to pain interference and depression via resilience, but may not serve a significant buffering (protective) function. The findings are consistent with theoretical models suggesting that increases in positive affect build personal resources. Longitudinal research testing the broaden-and-build theory as applied to pain is warranted, as are other studies examining the potential benefits of increasing positive affect and resilience in individuals with MS and chronic pain.
Impact.
Although risk factors for poor quality of life, such as pain catastrophizing, are often examined in samples of adults with MS, research on positive factors is scarce.
This study is the first to examine relationships between positive affect, resilience, and pain measures by simultaneously evaluating two models of positive coping.
Contrary to some previous research, no support was found for a stress and coping model hypothesizing buffering/moderating effects of positive affect and resilience on the associations between pain intensity and pain-related measures.
This study is the first to test and demonstrate preliminary support for the broaden-and-build model of coping with pain in a sample of individuals with MS.
Additional research to examine the potential for positive factors to enhance the efficacy of psychosocial interventions for pain in MS is warranted.
Acknowledgments
The contents of this publication were developed under a grant from National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90RT5023–01-00, NIDIRR grant number H133B080024) and the National Multiple Sclerosis Society (MB0026). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
References
- Aiken LS, & West SG (1991). Multiple Regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Alschuler KN, Arewasikporn A, Nelson IK, Molton IR, & Ehde DM (2018). Promoting resilience in individuals aging with multiple sclerosis: Results from a pilot randomized controlled trial. Rehabilitation Psychology, 63(3),338–348. doi: 10.1037/rep0000223 [DOI] [PubMed] [Google Scholar]
- Alschuler KN, Ehde DM, & Jensen MP (2013). The co-occurrence of pain and depression in adults with multiple sclerosis. Rehabilitation Psycholology, 58(2), 217–221. doi: 10.1037/a0032008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alschuler KN, Jensen MP, & Ehde DM (2012). Defining mild, moderate, and severe pain in persons with multiple sclerosis. Pain Medicine, 13(10), 1358–1365. doi: 10.1111/j.1526-4637.2012.01471.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alschuler KN, Jensen MP, Sullivan-Singh SJ, Borson S, Smith AE, & Molton IR (2013). The association of age, pain, and fatigue with physical functioning and depressive symptoms in persons with spinal cord injury. Journal of Spinal Cord Medicine, 36(5), 483–491. doi: 10.1179/2045772312Y.0000000072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alschuler KN, Kratz AL, & Ehde DM (2016). Resilience and vulnerability in individuals with chronic pain and physical disability. Rehabilitation Psychology, 61(1), 7–18. doi: 10.1037/rep0000055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amtmann D, Cook KF, Jensen MP, Chen WH, Choi SW, Revicki DA,.. Lai JS (2010). Development of a PROMIS item bank to measure pain interference. Pain, 150(1), 173–182. doi: 10.1016/j.pain.2010.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amtmann D, Kim J, Chung H, Bamer AM, Askew RL, Wu S, . . . Johnson KL (2014). Comparing CESD-10, PHQ-9, and PROMIS depression instruments in individuals with multiple sclerosis. Rehabilitation Psychology, 59(2), 220–229. doi: 10.1037/a0035919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamer AM, Cook KF, & Amtmann D (2012). Reliability and validity of pain, fatigue, depression, and social roles participation PRO measures in populations of individuals aging with a disability. Quality of Life Research, 20(Suppl 1), 66. doi: 10.1007/s11136-011-0097 [DOI] [Google Scholar]
- Bartley E (2017, July). Harnessing power of resilience: Mechanisms and approaches that promote adaptive functioning in chronic pain. In Sibille KT (Chair), Living well with less chronic pain: Shifting the lens from pathology to resilience. Symposium conducted at the meeting of the Fifth World Congress on Positive Psychology, Montreal, Quebec. [Google Scholar]
- Black R, & Dorstyn D (2015). A biopsychosocial model of resilience for multiple sclerosis. Journal of Health Psychology, 20(11), 1434–1444. doi: 10.1177/1359105313512879 [DOI] [PubMed] [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, & Bohlmeijer E (2013). Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health, 13, 119. doi: 10.1186/1471-2458-13-119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, & Stein MB (2007). Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. doi: 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Catalano D, Chan F, Wilson L, Chiu CY, & Muller VR (2011). The buffering effect of resilience on depression among individuals with spinal cord injury: A structural equation model. Rehabilitation Psychology, 56(3), 200–211. doi: 10.1037/a0024571 [DOI] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, . . . Hays R (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. doi: 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway AM, Tugade MM, Catalano LI, & Fredrickson BL (2012). The broaden-and-build theory of positive emotions: Form, function, and mechanisms In David S, Boniwell I, & Ayers AC (Eds.), Oxford Handbook of Happiness (pp. 17–34). Oxford, UK: Oxford University Press. [Google Scholar]
- Cook KF, Bamer AM, Amtmann D, Molton IR, & Jensen MP (2012). Six patient-reported outcome measurement information system short form measures have negligible age- or diagnosis-related differential item functioning in individuals with disabilities. Archives of Physical Medicine and Rehabilitation, 93(7), 1289–1291. doi: 10.1016/j.apmr.2011.11.022 [DOI] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, & Smith BW (2004). Chronic pain, stress, and the dynamics of affective differentiation. Journal of Personality, 72(6), 1133–1159. doi: 10.1111/j.1467-6494.2004.00293.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day MA, Ehde DM, Ward LC, Hartoonian N, Alschuler KN, Turner AP, . . . Jensen MP (2016). An empirical investigation of a biopsychosocial model of pain in multiple sclerosis. Clinical Journal of Pain, 32(2), 155–163. doi: 10.1097/AJP.0000000000000240 [DOI] [PubMed] [Google Scholar]
- Dunn DS, & Brody C (2008). Defining the good life following acquired physical disability. Rehabilitation Psychology, 53(4), 413–425. doi: 10.1037/a0013749 [DOI] [Google Scholar]
- Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, . . . Witter J (2005). Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain, 113(1–2), 9–19. doi: 10.1016/j.pain.2004.09.012 [DOI] [PubMed] [Google Scholar]
- Edwards KA, Alschuler KN, Ehde DM, Battalio SL, & Jensen MP (2017). Changes in resilience predict function in adults with physical disabilities: A longitudinal study. Archives of Physical Medicine and Rehabilitation, 98(2), 329–336. doi: 10.1016/j.apmr.2016.09.123 [DOI] [PubMed] [Google Scholar]
- Finan PH, & Garland EL (2015). The role of positive affect in pain and its treatment. Clinical Journal of Pain, 31(2), 177–187. doi: 10.1097/AJP.0000000000000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher MN, Snih SA, Ostir GV, & Goodwin JS (2004). Positive affect and disability among older Mexican Americans with arthritis. Arthritis Care and Research, 51(1), 34–39. doi: 10.1002/art.20079 [DOI] [PubMed] [Google Scholar]
- Folkman S, & Moskowitz JT (2004). Coping: Pitfalls and promise. Annual Review of Psychology, 55, 745–774. doi: 10.1146/annurev.psych.55.090902.141456 [DOI] [PubMed] [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden- and-build theory of positive emotions. American Psychologist, 56(3), 218–226. doi: 10.1037/0003-066X.56.3.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M, Aslaksen PM, & Flaten MA (2006). Resilience as a moderator of pain and stress. Journal of Psychosomatic Research, 61(2), 213–219. doi: 10.1016/jjpsychores.2005.12.007 [DOI] [PubMed] [Google Scholar]
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, & Turk DC (2007). The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin, 133(4), 581–624. doi: 10.1037/0033-2909.133.4.581 [DOI] [PubMed] [Google Scholar]
- Hart SL, Vella L, & Mohr DC (2008). Relationships among depressive symptoms, benefit-finding, optimism, and positive affect in multiple sclerosis patients after psychotherapy for depression. Health Psychology, 27(2), 230–238. doi: 10.1037/0278-6133.27.2.230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassett AL (2017). Positive affect as a predictor of outcome and a target for intervention in chronic pain. In Sibille KT (Chair), Living well with less chronic pain: Shifting the lens from pathology to resilience. Symposium conducted at the meeting of the Fifth World Congress on Positive Psychology, Montreal, Quebec. [Google Scholar]
- Hu L, & Bentler PM (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424–453. doi: 10.1037/1082-989X.3.4.424 [DOI] [Google Scholar]
- Jensen MP, & Karoly P (2011). Self-report scales and procedures for assessing pain in adults In Turk DC & Melzack R (Eds.), Handbook of pain assessment (3rd ed., pp. 19–44). New York, NY: The Guilford Press. [Google Scholar]
- Johnson Wright LM, Zautra AJ, & Going S (2008). Adaptation to early knee osteoarthritis: The role of risk, resilience, and disease severity on pain and physical functioning. Annals of Behavioral Medicine, 36(1), 70–80. doi: 10.1007/s12160-008-9048-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kratz AL, Ehde DM, & Bombardier CH (2014). Affective mediators of a physical activity intervention for depression in multiple sclerosis. Rehabilitation Psychology, 59(1), 57–67. doi: 10.1037/a0035287 [DOI] [PubMed] [Google Scholar]
- Kratz AL, Murphy SL, & Braley TJ (2017). Ecological momentary assessment of pain, fatigue, depressive, and cognitive symptoms reveals significant daily variability in multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 98(11), 2142–2150. doi: 10.1016/j.apmr.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon A, Jorm AF, Christensen H, Korten AE, Jacomb PA, & Rodgers B (1999). A short form of the Positive and Negative Affect Schedule: Evaluation of factorial validity and invariance across demographic variables in a community sample. Personality and Individual Differences, 27(3), 405–416. doi: 10.1016/S0191-8869(98)00251-7 [DOI] [Google Scholar]
- Milo R, & Miller A (2014). Revised diagnostic criteria of multiple sclerosis. Autoimmunity Reviews, 13(4–5), 518–524. doi: 10.1016/j.autrev.2014.01.012 [DOI] [PubMed] [Google Scholar]
- Mohr DC, Hart SL, Julian L, Catledge C, Honos-Webb L, Vella L, & Tasch ET (2005). Telephone-administered psychotherapy for depression. Archives of General Psychiatry, 62(9), 1007–1014. doi: 10.1037/0022-006X.68.2.356 [DOI] [PubMed] [Google Scholar]
- Molton IR, Cook KF, Smith AE, Amtmann D, Chen WH, & Jensen ΜP (2014). Prevalence and impact of pain in adults aging with a physical disability: Comparison to a US general population sample. Clinical Journal of Pain, 30(4), 307–315. doi: 10.1097/AJP.0b013e31829e9bca [DOI] [PubMed] [Google Scholar]
- Müller R, Gertz KJ, Molton IR, Terrill AL, Bombardier CH, Ehde DM, & Jensen ΜP (2016). Effects of a tailored positive psychology intervention on well-being and pain in individuals with chronic pain and a physical disability: A feasibility trial. Clinical Journal of Pain, 32(1), 32–44. doi: 10.1097/AJP.0000000000000225 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998). Mplus user’s guide (Seventh ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- O’Connor AB, Schwid SR, Herrmann DN, Markman JD, & Dworkin RH (2008). Pain associated with multiple sclerosis: Systematic review and proposed classification. Pain, 137(1), 96–111. doi: 10.1016/j.pain.2007.08.024 [DOI] [PubMed] [Google Scholar]
- Ong AD, Zautra AJ, & Reid MC (2010). Psychological resilience predicts decreases in pain catastrophizing through positive emotions. Psychology and Aging, 25(3), 516–523. doi: 10.1037/a0019384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakenham KI, Mawdsley M, Brown FL, & Burton NW (2018). Pilot evaluation of a resilience training program for people with multiple sclerosis. Rehabilitation Psychology, 63(1), 29–42. doi: 10.1037/rep0000167 [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, & PROMIS CG (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18(3), 263–283. doi: 10.1177/10731911111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton-John TR, Mason C, & Hunter M (2014). The role of resilience in adjustment and coping with chronic pain. Rehabilitation Psychology, 59(3), 360–365. doi: 10.1037/a0037023 [DOI] [PubMed] [Google Scholar]
- Quale AJ, & Schanke AK (2010). Resilience in the face of coping with a severe physical injury: A study of trajectories of adjustment in a rehabilitation setting. Rehabilitation Psychology, 55(1), 12–22. doi: 10.1037/a0018415 [DOI] [PubMed] [Google Scholar]
- Ruiz-Aranda D, Salguero JM, & Fernández-Berrocal P (2010). Emotional regulation and acute pain perception in women. Journal of Pain, 11(6), 564–569. doi: 10.1016/j.jpain.2009.09.011 [DOI] [PubMed] [Google Scholar]
- Sheikh MA, Abelsen B, & Olsen JA (2016). Differential recall bias, intermediate confounding, and mediation analysis in life course epidemiology: An analytic framework with empirical example. Frontiers in Psychology, 7, 1828. doi: 10.3389/fpsyg.2016.01828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman AM, Molton IR, Alschuler KN, Ehde DM, & Jensen MP (2015). Resilience predicts functional outcomes in people aging with disability: A longitudinal investigation. Archives of Physical Medicine and Rehabilitation, 96(7), 1262–1268. doi: 10.1016/j.apmr.2015.02.023 [DOI] [PubMed] [Google Scholar]
- Sin NL, & Lyubomirsky S (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467–487. doi: 10.1002/jclp.20593 [DOI] [PubMed] [Google Scholar]
- Sobel ME (1982). Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology, 13, 290–312. doi: 10.2307/270723 [DOI] [Google Scholar]
- Strand EB, Zautra AJ, Thoresen M, Ødegård S, Uhlig T, & Finset A (2006). Positive affect as a factor of resilience in the pain-negative affect relationship in patients with rheumatoid arthritis. Journal of Psychosomatic Research, 60(5), 477–484. doi: 10.1016/j.jpsychores.2005.08.010 [DOI] [PubMed] [Google Scholar]
- Sturgeon JA, & Zautra AJ (2010). Resilience: A new paradigm for adaptation to chronic pain. Current Pain and Headache Reports, 14(2), 105–112. doi: 10.1007/s11916-010-0095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teresi JA, Ocepek-Welikson K, Kleinman M, Eimicke JP, Crane PK, Jones RN, . . . Cella D (2009). Analysis of differential item functioning in the depression item bank from the Patient Reported Outcome Measurement Information System (PROMIS): An item response theory approach. Psychology Science Quarterly, 51(2), 148–180. [PMC free article] [PubMed] [Google Scholar]
- Terrill AL, Molton IR, Ehde DM, Amtmann D, Bombardier CH, Smith AE, & Jensen MP (2014). Resilience, age, and perceived symptoms in persons with long-term physical disabilities. Journal of Health Psychology, 1–10. doi: 10.1177/1359105314532973 [DOI] [PubMed] [Google Scholar]
- Tugade MM, & Fredrickson BL (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol, 86(2), 320–333. doi: 10.1037/0022-3514.86.2.320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tugade MM, Fredrickson BL, & Feldman Barrett L (2004). Psychological resilience and positive emotional granularity: Examining the benefits of positive emotions on coping and health. Journal of Personality, 72(6), 1161–1190. doi: 10.1111/j.1467-6494.2004.00294.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh MV, Armstrong TW, Poritz J, Elliott TR, Jackson WT, & Ryan T (2016). Resilience, pain interference, and upper limb loss: Testing the mediating effects of positive emotion and activity restriction on distress. Archives of Physical Medicine and Rehabilitation, 97(5), 781–787. doi: 10.1016/j.apmr.2016.01.016 [DOI] [PubMed] [Google Scholar]
- Wilhelm K, Geerligs L, & Peisah C (2014). Successful transition to later life: Strategies used by baby boomers. Australasian Journal on Ageing, 33(2), 81–85. doi: 10.1111/ajag.12025 [DOI] [PubMed] [Google Scholar]
- Wright BA (1983). Physical disability, a psychosocial approach (2nd ed.). HarperCollins Publishers; Retrieved May 17, 2017 from http://oxfordhandbooks.com/view/10.1093/oxfordhb/9780195398786.001.0001/oxfordhb-9780195398786-e-015 [Google Scholar]
- Yeung EW, Arewasikporn A, & Zautra AJ (2012). Resilience and chronic pain. Journal of Social and Clinical Psychology, 31(6), 593–617. doi: 10.1521/jscp.2012.31.6.593 [DOI] [Google Scholar]
- Zautra AJ, Arewasikporn A, & Davis MC (2010). Resilience: Promoting well-being through recovery, sustainability, and growth. Research in Human Development, 7(3), 221–238. [Google Scholar]
- Zautra AJ, Johnson LM, & Davis MC (2005). Positive affect as a source of resilience for women in chronic pain. Journal of Consulting and Clinical Psychology, 73(2), 212–220. doi: 10.1037/0022-006X.73.2.212 [DOI] [PMC free article] [PubMed] [Google Scholar]