Abstract
Objective
To understand the role of county characteristics in the growing divide between rural and urban mortality from 1980 to 2010.
Data Source
Age‐adjusted mortality rates for all U.S. counties from 1980 to 2010 were obtained from the CDC Compressed Mortality File and combined with county characteristics from the U.S. Census Bureau, the Area Health Resources File, and the Inter‐University Consortium for Political and Social research.
Study Design
We used Oaxaca–Blinder decomposition to assess the extent to which rural–urban mortality disparities are explained by observed county characteristics at each decade.
Principal Findings
Decomposition shows that, at each decade, differences in rural/urban characteristics are sufficient to explain differences in mortality. Furthermore, starting in 1990, rural counties have significantly lower predicted mortality than urban counties when given identical county characteristics. We find changes in the effect of characteristics on mortality, not the characteristics themselves, drive the growing mortality divide.
Conclusions
Differences in economic and demographic characteristics between rural and urban counties largely explain the differences in age‐adjusted mortality in any given year. Over time, the role these characteristics play in improving mortality has increased differentially for urban counties. As characteristics continue changing in importance as determinants of health, this divide may continue to widen.
Keywords: Econometrics, determinants of health, population health, socioeconomic causes of health, geographic/spatial factors, small area variations, rural health
Life expectancy in the United States has markedly improved over the past 30 years; the average lifespan has increased from 1980 to 2010 by 3 years for women and 6 years for men (Wang et al. 2012). Researchers often attribute these improvements to a number of factors, including advances in the treatment of heart disease and stroke, reductions in smoking and motor vehicle deaths, increases in educational attainment, and improvements in access to care (Fried 2000; Shrestha 2005; Stewart and David 2014).
Unfortunately, mortality gains are not experienced equally across all populations. Murray et al. (2006) divided the United States into “Eight Americas” using combinations of county characteristics and race and found that gaps in life expectancy between the most and least advantaged of these subpopulations is as much as 15 years. Other studies have echoed the importance of individual‐level characteristics such as determinants of life expectancy, including gender, race, education, and income (Singh and Siahpush 2006; Arias et al. 2010; Olshansky et al. 2012; Wang et al. 2013; Case and Deaton 2015; Chang et al. 2015).
Beyond the role of individual characteristics, mortality has been shown in numerous studies to vary geographically (Murray et al. 2006; Cullen, Cummins, and Fuchs 2012; Rettenmaier and Wang 2013; Dwyer‐Lindgren et al. 2016). In 2014, Singh and Siapush described a growing divide in life expectancy between those living in rural versus urban counties (Singh and Siahpush 2014b). In 1969, there was no significant difference in life expectancy between urban and rural counties. Although both urban and rural counties improved life expectancy overall, by 2009, urban and rural counties had a statistically significant 2‐year gap in overall life expectancy, with urban residents expected to live 78.8 years and rural residents only 76.8 years (Singh and Siahpush 2014b). Evidence suggests that this divide has continued to widen in recent years, with the largest gap seen in potentially preventable causes of death (Garcia 2017). The urban/rural gap is particularly large for “unintentional injury” deaths, including motor vehicle accidents, drug overdose, and suicide (Beck et al. 2017; Ivey‐Stephenson 2017; Mack, Jones, and Ballesteros 2017).
Causes of these urban/rural differences are not well understood. Differences in state‐level characteristics, more so than individual characteristics, have been shown to explain a large portion of state‐level variation in mortality rates (Montez, Zajacova, and Hayward 2016). County‐level characteristics may similarly contribute to variation in outcomes such as care quality (Henning‐Smith et al. 2017), hospital readmission (Herrin et al. 2015), and all‐cause mortality (Singh 2003; Starfield et al. 2005; Ricketts and Holmes 2007; Cullen, Cummins, and Fuchs 2012; Rettenmaier and Wang 2013). County‐level differences in social determinants of health such as education (Olshansky et al. 2012), insurance coverage (Wilper et al. 2009), and employment (Rettenmaier and Wang 2013) use may also influence health outcomes. Many characteristics that are known to be predictive of mortality vary widely between urban counties and rural counties, but it is unclear whether these differences are growing over time or whether they are sufficient to explain the increasing disparity in mortality.
Additionally, the role of the characteristics as predictors of mortality may be changing. Evidence suggests that differences in life expectancy by education and income are widening, whereas differences by race are decreasing over time (Olshansky et al. 2012; Kochanek, Anderson, and Arias 2015; Chetty et al. 2016). While we see changes in both county characteristics and the predictors of mortality over time, the nature of the growth in rural–urban mortality disparities remains unknown. Have rural counties become increasingly disadvantaged relative to urban counterparts, or are predictors of mortality changing in a way that differentially affects rural counties?
This study seeks to decompose the growing rural–urban mortality gap from 1980 to 2010, focusing on county‐level economic, demographic, and regional characteristics. A deeper understanding of the relative role of these factors allows policy solutions that can better address the growing disparity.
Methods
Data
We obtained data reporting age‐adjusted mortality per 100,000 persons for all U.S. counties, each year from 1979 to 2013, using the CDC's National Compressed Mortality Database (CDC WONDER). County‐level mortality data were not available for Alaska until after 1989; therefore, Alaskan counties (n = 20) were excluded from analysis. In addition, the CDC notes a small number of other exceptions for counties that have significantly redefined boundaries or experienced other changes that make estimates inconsistent across years. These counties (14 total) were removed from primary analysis. In sensitivity analysis, both Alaskan counties and CDC exception counties were included without substantive changes to results. To reduce variation in counties with small populations, a weighted 5‐year average mortality was calculated for each county, centered around each decennial year: 1990, 2000, and 2010. As data are only available starting in 1979, a 3‐year average is used for 1980. Counties with very small numbers of deaths in a given year had mortality data censored by the CDC. Counties with a majority of observation years censored (n = 36) were also removed from analysis—these counties were all classified as rural for all or most of the period under study.
We also gathered data on economic, demographic, and structural characteristics that have previously been shown to be predictive of county‐level mortality rates and were available for all years under study (Mansfield et al. 1999; Singh and Miller 2004; Starfield et al. 2005; Murray et al. 2006; Olshansky et al. 2012; Rettenmaier and Wang 2013). We use Social Explorer for data on age distribution, race, and ethnicity characteristics for each county (short form decennial census), as well as percent of the county living in poverty, educational attainment, unemployment (Census 1980; American Community Survey 2010). Poverty rate was measured with both the percent of households with incomes under 100 percent of the Federal Poverty Level (FPL) and under 200 percent of the FPL. Unemployment rate was defined as the percentage of civilians over the age of 16 years who are not currently working but are in search of work. Educational attainment was defined for those 25 years of age or older in three categories: less than high school education, completion of high school or GED, and any post‐high school education. We used the Area Health Resource File (AHRF) to determine the number of non‐Federal physicians per county at each decennial year (Starfield et al. 2005; Area Health Resources Files 2015). Using county population, this was transformed to total physicians per 10,000 for each county. Although we use population size as a weight, we do not include either total population or population density in our demographic variables, as these are defining characteristics of rural counties.
Finally, to understand the contribution of differential migration out of urban/rural counties over this period, we obtained data on county net migration patterns from 1970 to 2010 through the Inter‐University Consortium for Political and Social research (2010). These data incorporate vital statistics on births and deaths to determine the net migration rate for each county, defined as the relative change in population size due to in‐migration or out‐migration from a county over the previous decade.
Rural/Urban Classification
We classified counties using the Office of Management and Budget's (OMB) definition of metropolitan, which defines counties based on population and commuting patterns (Office of Management and Budget 2014). OMB separates counties into three categories; metropolitan, defined as having a “core urban area” with a population of 50,000 or more; micropolitan, defined as having a “core urban area” with a population of 10,000–50,000; and non‐core, which encompasses all remaining counties. Counties defined as metropolitan by OMB were classified as “urban,” while micropolitan or non‐core counties were classified as “rural.” We restricted our primary analysis to those counties that are classified as rural across all four time periods (n = 1,809) and those classified as urban across all four time periods (n = 679). In sensitivity analysis, we included all counties with their contemporaneous classification, regardless of the persistency of their urban/rural status over the study period (adding an additional 612 counties), and found no substantive change in results.
County Characteristics
We present average county characteristics by year and urban/rural status, weighted by population size. T‐tests were used to compare differences in urban and rural counties at each decade as well as changes within urban counties and rural counties across decades.
Cross‐Sectional Decomposition
To determine the extent to which variation in mortality can be explained at each decade by observable characteristics, we performed Oaxaca–Blinder decomposition by rural/urban status (Blinder 1973; Oaxaca 1973). Oaxaca–Blinder decomposition uses stratified (by urban/rural) linear regression to disaggregate mortality differences into differences in observed characteristics (termed “endowments”) and unexplained differences (coefficients). Each model, separately, estimates the relative (marginal) effect of county‐level characteristics (e.g., race, education) on mortality. By applying, for example, urban county characteristics to coefficients estimated using only the rural sub‐sample, we calculate how much of the mortality disparity is explained by differences in characteristics between urban and rural counties. Any remaining differences are attributable, not to changing county characteristics, but to how these counties translate characteristics into improvements in mortality.
Our regression models were specified as follows, for each decade:
For simplicity, we represent all measured characteristics as X RURAL or X URBAN and their coefficients as β RURAL or β URBAN. Thus, in each of our four time periods, we ran separate, identically specified regressions for both urban and rural counties as follows:
Next, counterfactual estimates were generated using the estimated coefficients from the rural county equation and the county characteristics from the urban counties. This value represents the expected mortality rate for a rural county given average urban characteristics.
The difference between the average observed rural mortality () and the counterfactual estimate () represents the “explained” variation in mortality, while the remainder of the difference is due to rural/urban differences in coefficients, or differences in the marginal effect of individual characteristics on mortality, dubbed “unexplained” variation. Mathematically, this can be shown by arranging terms from the difference in observed mortality between the two groups:
We repeated this estimation for each decade to understand the relative contribution at each time period. Because white tests and visual inspection of residuals demonstrated substantial heterogeneity by population size, we use weighted least squares (WLS) where counties are weighted by total population to correct for heteroscedasticity in mortality. Results were analyzed for both absolute difference and percent difference explained by observed characteristics. Characteristics are presented both individually and by category (economic, demographic, and regional characteristics) to assess the relative role of each category of variables on mortality disparities.
We examine two additional specifications to test the robustness of our findings. First, we address the fact that Oaxaca–Blinder decomposition is sensitive to choice of reference group, by estimating differences using an alternative decomposition method, Neumark decomposition (Neumark 1988), which uses coefficients from a pooled urban/rural model, rather than rural coefficients alone, to generate the counterfactual estimates. Additionally, we test the effect of population‐weighting on study conclusions by including both an unweighted model and a model using a feasible generalized least squares approach (Wooldridge 2010).
Characteristic Changes over Time
Decomposition allows us to compare rural and urban counties at each decade and assess the relative contribution of observed characteristics on mortality. However, when analyzed cross‐sectionally, as above, it provides only partial insight into how these characteristics and their importance is changing over time. Consider an increase in explained variation from one decade to another. This type of increase has two plausible explanations: either the explained portion in 1 year is larger because the characteristics are more different ( increased) or it is larger because the coefficients (β RURAL) have increased in absolute value.
To assess independent effects of characteristic changes in urban and rural counties over time, we perform a secondary set of decompositions comparing the explained variation in each decade as a function of county‐level differences over time, using 1980 as the referent group. These regressions were again stratified by urban/rural status, but now use change in county characteristics (e.g., county populations becoming more educated, on average, over time) since 1980, forming three pairwise regressions (1980 vs. 1990, 1980 vs. 2000, 1980 vs. 2010). This analysis asks “what is the contribution of changes in county characteristics to changes in rural or urban mortality rates since 1980?” Models were used to assess whether the expected improvement in mortality attributable to characteristic changes varied significantly between urban and rural counties over time. Coupled with cross‐sectional these analyses allow us to paint a more complete picture of the growing mortality gap between rural and urban counties. All analyses were repeated over 500 bootstrapped samples to generate 95% confidence intervals in the explained and unexplained decomposition.
Results
Table 1 presents the average characteristics for rural and urban counties at each of the four time points, weighted by total population. Urban counties have a larger proportion of non‐white and Hispanic populations than rural counties, including higher proportions of all minority groups except for American Indians. Both urban and rural counties show an aging of the population over time although the percent of the population over 65 is larger in rural counties (2010; 16.1 vs. 13.1 percent, p < .001). Educational attainment also increased for both county types from 1980 to 2010, although the pattern of this increase was different. For urban counties, this manifested as a decrease in both high school dropouts and those with only a high school education while college education increased. For rural counties, there was a decrease in those with less than high school education while both high school and college increased over the 30‐year time frame. Thus, while both experienced a decrease in high school dropouts and an increase in college‐educated individuals, rural counties saw an increase in the percent of the population with high school only education and urban saw a decrease in that percentage over the same time.
Table 1.
County Characteristics by Rural/Urban Status (1980–2010)
| Mean (SD) | 1980 | 1990 | 2000 | 2010 | ||||
|---|---|---|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | |
| n | 1,781 | 656 | 1,781 | 656 | 1,781 | 656 | 1,781 | 656 |
| Age‐adjusted mortality rate | 1027.00 (101.98) | 1020.67 (83.52) | 957.56 (108.27) | 937.35 (90.42) | 923.55 (121.48) | 857.23 (93.58) | 849.01 (131.9) | 730.25 (99.09) |
| Percent white | 88.80 (15.80) | 82.10 (13.10) | 87.80 (16.10) | 78.70 (14.60) | 85.20 (16.60) | 72.70 (16.00) | 83.90 (16.50) | 69.70 (15.60) |
| Percent black | 8.20 (14.60) | 12.30 (11.50) | 8.26 (14.60) | 12.70 (11.90) | 8.40 (14.70) | 13.10 (12.30) | 8.27 (14.40) | 13.60 (12.20) |
| Percent AI/AN | 1.39 (5.99) | 0.40 (0.61) | 1.81 (6.92) | 0.51 (0.77) | 2.01 (7.28) | 0.60 (0.77) | 2.14 (7.33) | 0.67 (0.83) |
| Percent Asian | 0.40 (3.08) | 1.64 (2.21) | 0.60 (3.24) | 3.35 (3.89) | 0.66 (2.32) | 4.49 (4.84) | 0.87 (2.32) | 5.88 (5.82) |
| Percent other | 1.23 (3.47) | 3.57 (4.75) | 1.55 (4.35) | 4.75 (6.13) | 3.73 (5.25) | 9.10 (8.06) | 4.82 (4.96) | 10.20 (7.24) |
| Percent hispanic | 3.11 (9.40) | 7.38 (10.40) | 3.79 (10.60) | 10.30 (12.90) | 5.65 (11.80) | 14.30 (15.10) | 7.75 (12.90) | 18.40 (16.40) |
| Percent foreign born | 1.68 (2.17) | 7.44 (6.54) | 1.75 (2.76) | 9.50 (9.10) | 2.87 (3.86) | 13.10 (10.70) | 3.80 (4.28) | 15.10 (10.50) |
| Net migration ratio | 0.06 (0.15) | 0.04 (0.20) | (0.03) (0.11) | 0.06 (0.15) | 0.05 (0.11) | 0.05 (0.13) | 0.02 (0.08) | 0.05 (0.12) |
| MDs per capita | 8.01 (5.01) | 21.20 (13.20) | 9.30 (6.10) | 24.60 (15.10) | 11.30 (8.14) | 29.30 (17.60) | 11.20 (9.30) | 30.60 (19.00) |
| Percent <HS education | 41.90 (11.40) | 31.00 (7.93) | 31.70 (9.90) | 22.90 (6.79) | 23.80 (8.52) | 18.60 (6.64) | 16.00 (6.73) | 13.30 (5.52) |
| Percent HS only | 35.20 (7.38) | 34.60 (4.90) | 35.10 (6.20) | 28.70 (5.73) | 35.90 (6.18) | 26.70 (6.25) | 36.10 (6.33) | 26.00 (6.00) |
| Percent any college | 22.90 (7.62) | 34.40 (8.64) | 33.20 (9.20) | 48.40 (9.30) | 40.30 (9.70) | 54.60 (8.95) | 47.90 (9.40) | 60.70 (8.16) |
| Percent unemployed | 7.52 (3.17) | 6.43 (2.27) | 7.37 (3.00) | 6.28 (2.00) | 6.40 (2.64) | 5.82 (2.10) | 9.30 (3.50) | 9.30 (2.35) |
| Percent under 100% FPL | 16.30 (7.24) | 11.30 (4.74) | 17.70 (7.83) | 12.00 (5.42) | 15.20 (6.50) | 11.80 (5.20) | 18.50 (6.26) | 15.10 (5.15) |
| Percent 100–200% FPL | 25.30 (4.68) | 17.50 (4.42) | 24.60 (4.14) | 16.10 (4.49) | 22.30 (4.01) | 16.00 (4.40) | 22.90 (3.91) | 18.10 (4.09) |
| Percent under 18 | 29.50 (3.35) | 27.80 (3.14) | 26.80 (3.25) | 25.30 (3.10) | 25.30 (3.04) | 25.80 (2.86) | 23.20 (3.12) | 24.30 (2.95) |
| Percent over 65 | 13.50 (3.34) | 10.70 (3.12) | 15.20 (3.46) | 12.00 (3.40) | 15.00 (3.21) | 11.80 (3.20) | 16.10 (3.35) | 12.30 (2.88) |
| Northeast (proportion) | 0.10 | 0.27 | 0.11 | 0.25 | 0.10 | 0.23 | 0.10 | 0.21 |
| West (proportion) | 0.11 | 0.21 | 0.12 | 0.23 | 0.13 | 0.24 | 0.14 | 0.25 |
| South (proportion) | 0.42 | 0.28 | 0.42 | 0.29 | 0.42 | 0.31 | 0.43 | 0.33 |
| Midwest (proportion) | 0.36 | 0.29 | 0.35 | 0.25 | 0.34 | 0.23 | 0.33 | 0.22 |
AI/AN, American Indian/Alaskan Native; HS, high school; FPL, Federal Poverty Level.
Estimates weighted by population size.
Economic characteristics showed less of a directional change over time. Unemployment was higher for rural in counties in all years (urban vs. rural, p < .001), excepting 2010 where there was no difference between county types (urban vs. rural, p = 0.51). Higher percentages of the population in rural counties were living below 200 percent of FPL than in urban counties at all time points. Rural poverty rates do not vary much over time, whereas urban counties had an increase in the number of persons under 200 percent of FPL from 1980 to 2010.
The gap in age‐adjusted mortality was small in 1980 (2.36 deaths/100,000 population) but grew each decade. By 2010, there were an additional 65.8 deaths per 100,000 population in rural counties compared to urban counties.
Cross‐Sectional Decomposition
On decomposing the mortality difference between urban and rural counties, we find that differences in rural/urban characteristics more than explain the difference in mortality at each decade. That is, rural counties appear to have even better expected outcomes than urban counties when given identical characteristics. Figure 1 demonstrates this difference, showing the change in both observed and predicted mortality over time. At each decade, the counterfactual rural county with urban characteristics has lower mortality than the observed rural and the observed urban counties.
Figure 1.
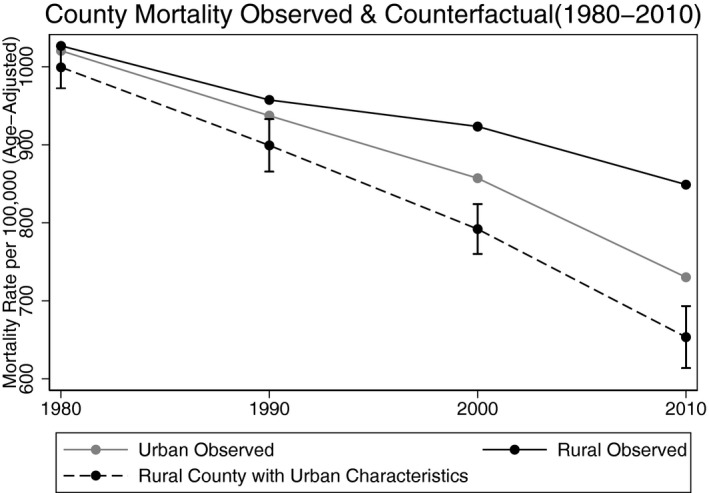
- Notes. Dashed line represents predicted age‐adjusted mortality rate for a county with coefficients from urban regression estimates and average rural characteristics at each decade. Bars represented 95% confidence intervals generated through 500 bootstrapped replications of the prediction.
A detailed set of results from the two‐step decomposition procedure is presented in Table S1 for the year 2010. Table 2 summarizes the results across all decades, presenting the “explained” mortality differences between rural and urban countries (i.e., the difference between the counterfactual mortality and the observed rural county rates). Larger numbers represent larger explained differences.
Table 2.
“Explained” Mortality Gap (Rural/Urban), by Year
| 1980 | 1990 | 2000 | 2010 | |
|---|---|---|---|---|
| Demographics | ||||
| Racial composition | −9.2 (−28.7, 10.3) | −10.4 (−41.9, 21.0) | −27.4 (−64.6, 9.7) | −0.2 (−31.8, 31.4) |
| Percent hispanic | 5.3 (−1.1, 11.6) | 10.8** (4.1, 17.4) | 41.5*** (24.2, 58.9) | 29.4*** (16.2, 42.7) |
| Percent foreign born | 12.1 (−5.4, 29.6) | 21.8 (−5.3, 48.8) | 52.0*** (26.9, 77.0) | 115.49*** (76.8, 154.0) |
| Age distribution | −16.0** (−25.2, −6.7) | −13.7** (−22.0, −5.5) | −15.4*** (−20.7, −10.1) | −17.7*** (−24.0, −11.4) |
| Net migration rate | −0.1 (−0.9, 0.6) | 0.01 (−3.6, 3.7) | 0.3 (−1.1, 1.7) | 5.1* (1.0, 9.2) |
| Region | −6.9* (−12.2, −1.6) | −3.4 (−7.8, 1.0) | 6.8* (1.7, 11.9) | 7.2* (0.5, 13.8) |
| Economic | ||||
| Education | 54.1*** (40.6, 67.7) | 58.9*** (47.1, 70.6) | 59.6*** (47.55, 71.6) | 36.9*** (24.3, 49.5) |
| Unemployment rate | 6.3*** (3.7, 9.0) | 9.9*** (6.2, 13.6) | 3.4* (0.7, 6.0) | −0.2 (−1.5, 1.1) |
| Poverty rate | −6.9 (−14.9, 1.2) | 0.7 (−10.6, 12.1) | 19.0*** (9.0, 29.0) | 23.1*** (14.3, 32.0) |
| MDs per capita | −11.2 (−28.1, 5.6) | −16.3* (−31.7, −0.9) | −8.2 (−21.3, 4.8) | −3.5 (−16.2, 9.2) |
| Total mortality difference explained | 27.5* | 58.2** | 131.5*** | 195.6*** |
| (Age‐adjusted deaths/100,000) | (3.0, 52.0) | (24.3, 92.1) | (95.0, 168.1) | (156.6, 234.6) |
Brackets represent 95% confidence intervals Values are reported as the difference between the observed age‐adjusted rural mortality rate and the estimated counterfactual (country characteristics) mortality rate (per 100,000).
* p < .05; ** p < .01; ***p < .001.
FPL, Federal Poverty Level.
Over time, increasing portions of the mortality difference can be explained by demographic differences between urban and rural counties, especially in the proportion of the population that identifies as Hispanic and the number of foreign‐born residents in a county. In 1980, the percent of the population born outside the United States explained 10.2 [95% CI: −9.7 to 29.1] deaths/100,000 and 2010, differences in foreign‐born population explains 105.9 [67.1 to 144.8] deaths/100,000. The negative result for racial composition suggests that we would expect rural counties to experience lower mortality due to having a smaller representation of minority racial groups relative to urban counties although this difference is not significant for any year. The mortality difference explained by age distribution is also negative at each decade, suggesting that the percent of the population over 65 or under 18 is predictive of lower mortality. As our outcome is age‐adjusted, this is likely a proxy for the marketshare of Medicare in the community or other social support programs available for younger and older age groups (Ricketts et al. 2007).
Differences in educational attainment between rural and urban counties explain a large portion of mortality differences in each decade, but this effect does not change substantively over time. A rural county with urban educational attainment would be expected to see 47.7 [34.1–61.0] fewer deaths/100,000 in 1980 and 39.7 [26.1–53.2] fewer deaths/100,000 in 2010. Differences in the average poverty rate change direction over time. Rural counties with a reduction in poverty rate to the average rate seen in urban counties would be expected to have 16.7 [8.7 to 24.8] more deaths/100,000. However, poverty rate is not significant in 1990 or 2000 and by 2010 is a positive and significant explainer of the mortality gap (rural counties with urban poverty rates would be expected to have 16.1 [4.0, 28.3] fewer deaths/100,000).
Figure 2 demonstrates the portion of the explained difference attributable to each group of variables by showing the predicted mortality for an urban county if changing its (A) demographics, (B) economic characteristics, or (C) geographic distribution to that of an average rural county at each decade. When considered together, economic characteristics explain a large but relatively constant portion of the mortality differences over time (from 39.2 [25.4–52.9] in 1980 to 59.1 [40.5–77.8] deaths/100,000 in 2010). Demographics, by comparison, explain less of the overall difference, but grow in importance over time (from 4.7 [−25.8 to 34.7] in 1980 to 137.8 [86.0–189.6] deaths/100,000 in 2010). Differences attributable to regional differences (e.g., North, Midwest) also grow significantly over this time period (from −7.3 [−1.2 to 13.3] in 1980 to 7.0 [0.5–12.6] deaths/100,000 in 2010) but remain small relative to other characteristics.
Figure 2.
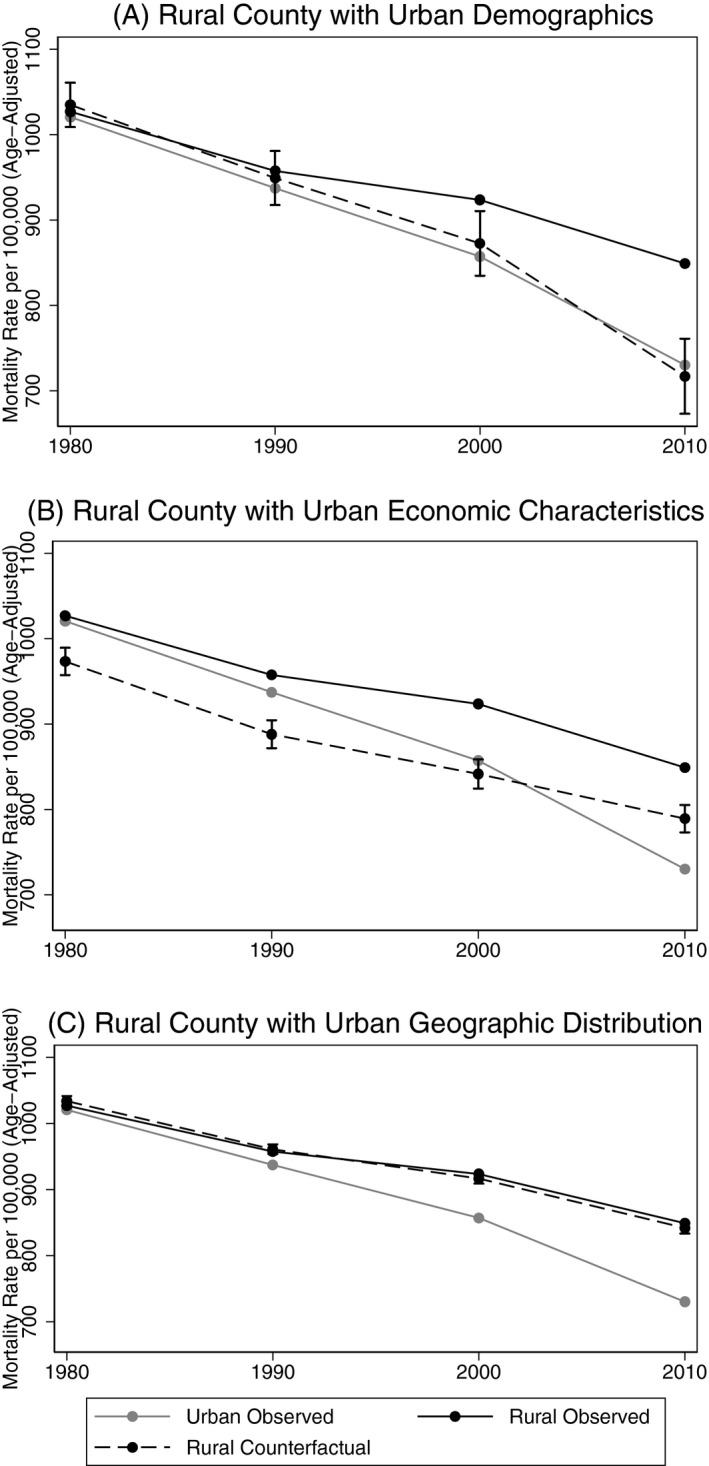
- Notes. Dashed line represents predicted age‐adjusted mortality rate for a county with coefficients from urban regression estimates and characteristics replaced with those of a rural county within each category. Demographic characteristics include racial and ethnic composition, foreign‐born population, and net migration rate. Economic characteristics include education, poverty, and unemployment. Geographic distribution is percent of counties in each census region. Bars represented 95% confidence intervals generated through 500 bootstrapped replications of the prediction.
To assess the effect of comparison group, findings were replicated using Neumark decomposition (Table S3). Using pooled coefficients, we find the magnitude of explained variation is smaller, but trends over time remain the same. This method similarly shows mortality differences are sufficiently explained by characteristics at each decade, with rural and urban counties predicted to have equivalent mortality rates given identical characteristics. Finally, we replicated model results using both an unweighted approach and an FGLS approach. Both the absolute rural/urban gap and the number of deaths explained were sensitive to weighting approach; however, the relative difference (percent of the gap explained by characteristic difference) remained at or above 100 percent after 1990 in all strategies, suggesting conclusions are robust to different weighting strategies.
Change in Mortality Decomposition
Next, we assess how changes in county characteristics explain changes in the mortality rate for urban and rural counties over time. During the 30‐year period under study, urban mortality rates improved by 233.1 deaths/100,000 persons and rural mortality rates improved by 173.6 deaths/100,000 persons. For urban counties, 59.2 [22.6–95.9] deaths/100,000 persons are explained by changes in county characteristics over this time period, which is about 25 percent of the total improvement. For rural counties, the absolute difference explained through characteristic changes is much greater: 81.6 [56.9–106.3] deaths/100,000 persons, or about 47 percent of the total improvement. That is, for rural counties, characteristics explain significantly more of the gains in life expectancy, relative to urban counties.
Figure 3 shows the predicted mortality for urban and rural counties if only county characteristics had changed during this period while coefficients remained constant. Over time, characteristic improvements are insufficient to explain the full reduction in observed mortality for either urban or rural counties. Additionally, the predicted mortality for urban and rural counties is not significantly different from each other when only characteristic changes are considered. This finding places the cross‐sectional result into important context. Taken together, these findings suggest that the widening urban/rural mortality gap is not due to a widening gap in the characteristics themselves, but rather to a strengthening over time of the relationship between these characteristics and mortality.
Figure 3.
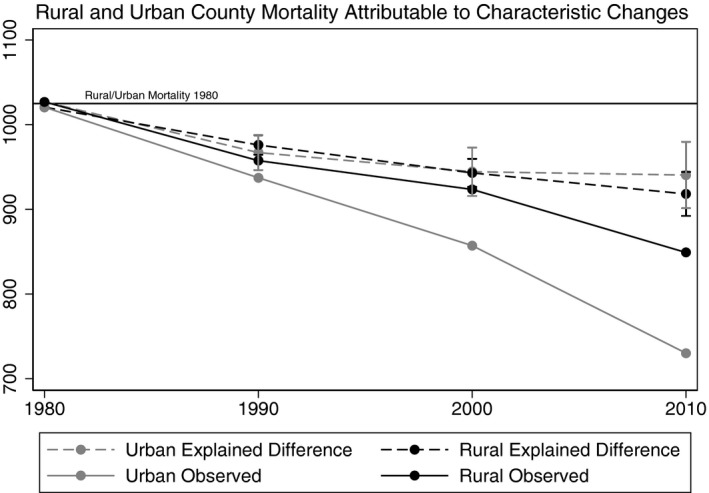
- Notes. Dashed lines represent separate urban/rural predictions where county characteristics change in each decade and regression coefficients remain at 1980 values. Bars represented 95% confidence intervals generated through 500 bootstrapped replications.
Discussion
We find that the growing urban/rural mortality gap can be more than explained by differences in county demographics, economics, and geographic distribution at each decade from 1980 to 2010. Although mortality differences explained by these characteristics increases over time, we do not find evidence to support that this is driven by increasingly disparate county characteristics. Rather, we find that the relative importance of individual characteristics (i.e., what an extra unit of education means for improvements in mortality) far outstrips any increasing disparity in the characteristics themselves over time.
The contribution of these two factors can be seen more clearly by way of example. The share of a county population born outside the United States is, by 2010, the largest source of explained variation. Foreign‐born population increases in both urban and rural counties over time although more so in urban counties. Yet the growing urban/rural divide in foreign‐born population does not sufficiently explain that it is increasing importance to mortality. Started differently, if the only change since 1980 had been to change the proportion of foreign‐born resident as a proportion of the total rural and urban county population, we could explain only 20.3 deaths/100,000 by 2010 instead of the 105.9 deaths/100,000 that we explain using our cross‐sectional model. The remaining 85.6 deaths are a product of a dramatic increase in the association between foreign‐born population and mortality rate. A 1 percentage point growth in foreign‐born population for a rural county reduces expected mortality by 1.8 deaths/100,000 in 1980 but by 9.4 deaths/100,000 by 2010. We observe this relationship across most of the determinants used in the models. Overall, while urban and rural counties do become more disparate in characteristics over time, the effect of each unit of difference is increasing more strongly.
We find support for this finding in other studies which show that life expectancy differences by income, education, and area deprivation are widening over time (Singh 2003; Singh and Siahpush 2006; Olshansky et al. 2012; Hayward, Hummer, and Sasson 2015; Chetty et al. 2016). That these trends may differentially affect rural counties is not surprising. However, as both characteristics and coefficients change together over time, it is helpful to consider the joint effect of these changes, captured by the portion of explained variation in our cross‐sectional decomposition.
On comparing the sources of explained difference over time, we find that economic characteristics represent a large but relatively constant portion of the explained differences while demographic characteristics, most notably the importance of foreign‐born and Hispanic populations, appears to be increasing over time. The increasing benefit for foreign‐born relative to native‐born Americans has been attributed to several factors, including shifting demographics of the immigrant population toward Hispanics and Asians, and increasingly low rates of obesity and smoking relative to U.S. populations (Singh and Hiatt 2006). At a county‐level, increases in foreign‐born populations may also reflect differences in economic or social conditions within the county not otherwise captured by the model. Both foreign‐born and native‐born Hispanics have been shown to have longer life expectancy than non‐Hispanic White, a trend that is increasing as causes of mortality shift for these populations (Case and Deaton 2015). We also find that regional characteristics, while comparatively small, do increase significantly as a source of explained difference. This is particularly notable because regional distribution has very little characteristic change over this time period, which means this change is almost entirely driven by shifting relationships between region and mortality. Specifically, mortality rates are lowest for counties in the Northeast, which has the largest urban population and highest in the largely rural Midwest. This increasing regional effect may be due to differences in health behaviors or diverging of state‐level policy; however, further exploration of this disparity is needed.
After 1990, characteristic differences more than explain the observed mortality gap in a given year. This means that for these years we would predict that given identical characteristics, a rural county would have a lower age‐adjusted mortality rate than an urban county. This suggests that while rural counties are increasingly disadvantaged, they also have important strengths which may allow them to derive a higher mortality reduction from a given characteristic improvement than a corresponding urban county. Previous work has explored the role of social networks and found evidence that stronger social ties in rural communities may play a role in helping protect communities faced with economic hardships (Holt‐Lunstad, Smith, and Layton 2010; Yang, Jensen, and Haran 2011). Public health strategies that utilize or enhance these ties may therefore be better able to address the growing disadvantage faced by rural communities.
We interpret these results in light of several limitations. Other factors that may be important predictors of mortality could not be considered in this analysis due to lack of reliable, county‐level data over the full study period. Better measures of social capital, access to care (e.g., hospitals beds/capita, uninsurance rates), and health behavior differences (e.g., binge drinking, drug use, exercise) between rural and urban counties may provide insight into the role of these characteristics in observed mortality disparities. Particularly as unintentional injury rises (including alcohol and drug‐related deaths) as a cause of death in rural counties (Singh and Siahpush 2014a), it may be particularly important to understand the role that these behaviors play in the widening mortality gap. The mortality gap has continued to widen in recent years (Garcia 2017). We are unable to meaningfully extend our analysis, as our outcome uses a multi‐year average of county mortality rate and CDC mortality data currently only extend to 2015.
Additionally, due to changes in how metropolitan counties were defined by the Office of Management and Budget, our primary analysis included only counties that were rural across all time periods or urban across all time periods. While we included all counties in sensitivity analysis and found similar overall conclusions, we do not explore the experience of counties transitioning from rural to urban (or vice versa) over this time period, which may reflect a very different set of challenges to those faced by counties not undergoing such a change.
Disparities in rural and urban mortality have increased over time. Decomposing these differences to understand the relative contribution of characteristic versus coefficient changes over a 30‐year time frame suggests that differences in observable characteristics can explain this gap in every decade, but that patterns of these differences change and reasons behind these changes are only partially changes in the characteristics themselves. Economic differences describe a large portion of the mortality gap across all years while demographic characteristics grow more important over time.
Despite increasing challenges faced by rural counties, we find evidence that rural communities are also “protected” from otherwise unfavorable characteristics. At the very least, rural counties appear to “do more with less” relative to their urban counterparts. Further exploring the unexplained sources of protection experienced by rural counties may provide insight into strategies that could help improve mortality rates across these populations. In particular, interventions building on stronger social ties within rural communities may be effective at overcoming the economic and demographic disadvantages faced by these populations. Similarly, understanding how predictors of mortality have changed differentially in rural counties over time could help identify potential areas for intervention. Furthermore, it is important for policy makers and community leaders to recognize the ways in which rural counties experience both disadvantage and advantage compared to urban counties, and to consider issues of resource allocation and public health policy accordingly.
We find that large portions of the mortality difference are explained by unequal distribution in social determinants of health, including education and poverty, rather than differential use of these resources by urban and rural counties. This suggests that policy makers should consider economic policies hand‐in‐hand with health policy to address inequities in health outcomes. Consideration of both direct and indirect pathways through which economic inequity may influence health outcomes is crucial for identifying potential areas for intervention (Adler and Newman 2002). However, recent policy and budget proposals curtail rural‐specific programs and resources, including the Medicare Rural Hospital Flexibility Program and funding for the State Office of Rural Health (Lee 2017) and evidence suggests that proposed decreases in the Medicaid program would disproportionately affect rural communities (Wagnerman et al. 2017). As the rural/urban mortality gap continues to grow, an understanding of the causes is necessary, but not sufficient, to narrow this gap. It will take purposive creativity, investment, support, and innovation—all of which require a policy environment that recognizes the unique challenges and underappreciated assets of rural communities.
Supporting information
Appendix SA1: Author Matrix.
Table S1. Example Decomposition Results (2010).
Table S2. Regression Results by Year and Urban/Rural Status.
Table S3. Decomposition Results, Comparison of Model Specification.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Partial support for this study was provided by the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services (HHS) under cooperative agreement # U1GRH03714. The information, conclusions and opinions expressed in this brief are those of the authors and no endorsement by FORHP, HRSA, HHS, or The University of North Carolina is intended or should be inferred.
Disclosure: None.
Disclaimer: None.
References
- Adler, N. E. , and Newman K.. 2002. “Socioeconomic Disparities in Health: Pathways and Policies.” Health Affairs 21: 60–75. [DOI] [PubMed] [Google Scholar]
- American Community Survey . 2010. United States Department of Commerce. Bureau of the Census. 2014 American Community Survey (5‐Year Estimates), Social Explorer [distributor], accessed on March 22, 2017.
- Area Health Resources Files . 2015. Bureau of Health Professions. Area Health Resources Files. Rockville, MD: Health Resources and Services Administration. [Google Scholar]
- Arias, E. , Eschbach K., Schauman W. S., Backlund E. L., and Sorlie P. D.. 2010. “The Hispanic Mortality Advantage and Ethnic Misclassification on US Death Certificates.” American Journal of Public Health 100 (suppl 1): S171–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, L. F. , Downs J., Stevens M. R., and Sauber‐Schatz E. K.. 2017. “Rural and Urban Differences in Passenger‐Vehicle–Occupant Deaths and Seat Belt Use Among Adults—United States, 2014“. MMWR Surveillance Summary 66(No. SS‐17): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blinder, A. S. 1973. “Wage Discrimination: Reduced Form and Structural Estimates.” Journal of Human Resources 8: 436–55. [Google Scholar]
- Case, A. , and Deaton A.. 2015. “Rising Morbidity and Mortality in Midlife Among White Non‐Hispanic Americans in the 21st Century.” Proceedings of the National Academy of Sciences of the United States of America 112 (49): 15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census . 1980. –2010. United States Department of Commerce. Bureau of the Census. 1980–2010 Decennial Census, Summary Files 1 and 3, Social Explorer [distributor], accessed on March 22, 2017.
- Chang, M. H. , Molla M. T., Truman B. I., Athar H., Moonesinghe R., and Yoon P. W.. 2015. “Differences in Healthy Life Expectancy for the US Population by Sex, Race/Ethnicity and Geographic Region: 2008.” Journal of Public Health (Oxf) 37 (3): 470–9. [DOI] [PubMed] [Google Scholar]
- Chetty, R. , Stepner M., Abraham S., Lin S., Scuderi B., Turner N., Bergeron A., and Cutler D.. 2016. “The Association Between Income and Life Expectancy in the United States, 2001–2014.” Journal of the American Medical Association 315 (16): 1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- “Compressed Mortality File–CDC WONDER Online.” Center for Disease Control and Prevention. National Center for Health Statistics.
- Cullen, M. R. , Cummins C., and Fuchs V. R.. 2012. “Geographic and Racial Variation in Premature Mortality in the U.S.: Analyzing the Disparities.” PLoS ONE 7 (4): e32930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer‐Lindgren, L. , Bertozzi‐Villa A., Stubbs R. W., Morozoff C., Kutz M. J., Huynh C., Barber R. M., Shackelford K. A., Mackenbach J. P., van Lenthe F. J., Flaxman A. D., Naghavi M., Mokdad A. H., and Murray C. J. L.. 2016. “US County‐Level Trends in Mortality Rates for Major Causes of Death, 1980–2014.” Journal of the American Medical Association 316 (22): 2385–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried, L. P. 2000. “Epidemiology of Aging.” Epidemiologic Reviews 22 (1): 95–106. [DOI] [PubMed] [Google Scholar]
- Garcia, M. C. 2017. “Reducing Potentially Excess Deaths from the Five Leading Causes of Death in the Rural United States.” MMWR Surveillance Summaries 66: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward, M. D. , Hummer R. A., and Sasson I.. 2015. “Trends and Group Differences in the Association between Educational Attainment and U.S. Adult Mortality: Implications for Understanding Education's Causal Influence.” Social Science and Medicine 127: 8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henning‐Smith, C. , Kozhimannil K., Casey M., Prasad S., and Moscovice I.. 2017. “Rural‐Urban Differences in Medicare Quality Outcomes and the Impact of Risk Adjustment.” Medical Care 55 (9): 823–9. [DOI] [PubMed] [Google Scholar]
- Herrin, J. , St Andre J., Kenward K., Joshi M. S., Audet A. M. J., and Hines S. C.. 2015. “Community Factors and Hospital Readmission Rates.” Health Services Research 50 (1): 20–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt‐Lunstad, J. , Smith T. B., and Layton J. B.. 2010. “Social Relationships and Mortality Risk: A Meta‐analytic Review.” PLoS Medicine 7 (7): e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inter‐university Consortium for Political and Social Research . 2010. County‐Specific Net Migration Estimates, 1970‐2010 [United States]. Ann Arbor, MI: Inter‐university Consortium for Political and Social Research. [Google Scholar]
- Ivey‐Stephenson, A. Z. 2017. “Suicide Trends Among and Within Urbanization Levels by Sex, Race/ethnicity, Age Group, and Mechanism of Death—United States, 2001–2015.” MMWR Surveillance Summaries 66: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek, K. D. , Anderson R. N., and Arias E.. 2015. “Leading Causes of Death Contributing to Decrease in Life Expectancy Gap between Black and White Populations: United States, 1999–2013.” NCHS Data Brief 218: 1–8. [PubMed] [Google Scholar]
- Lee, M. 2017. “Trump Budget Targets Rural Hospitals, Minority Health Professional Education” Modern Healthcare [accessed on February 21, 2018]. Available at http://www.modernhealthcare.com/article/20170523/NEWS/170529966 [Google Scholar]
- Mack, K. A. , Jones C. M., and Ballesteros M. F.. 2017. “Illicit Drug Use, Illicit Drug Use Disorders, and Drug Overdose Deaths in Metropolitan and Nonmetropolitan Areas—United States.” American Journal of Transplantation 17 (12): 3241–52. [DOI] [PubMed] [Google Scholar]
- Mansfield, C. J. , Wilson J. L., Kobrinski E. J., and Mitchell J.. 1999. “Premature Mortality in the United States: The Roles of Geographic Area, Socioeconomic Status, Household Type, and Availability of Medical Care.” American Journal of Public Health 89 (6): 893–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez, J. K. , Zajacova A., and Hayward M. D.. 2016. “Explaining Inequalities in Women's Mortality between U.S. States.” SSM Population Health 2: 561–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, C. J. , Kulkarni S. C., Michaud C., Tomijima N., Bulzacchelli M. T., Iandiorio T. J., and Ezzati M.. 2006. “Eight Americas: Investigating Mortality Disparities Across Races, Counties, and Race‐counties in the United States.” PLoS Medicine 3 (9): e260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark, D. 1988. “Employers’ Discriminatory Behavior and the Estimation of Wage Discrimination.” The Journal of Human Resources 23 (3): 279–95. [Google Scholar]
- Oaxaca, R. 1973. “Male‐female Wage Differentials in Urban Labor Markets.” International Economic Reviews 14 (3): 693–709. [Google Scholar]
- Office of Management and Budget . 2014. 2010 Standards of Delineating Metropolitan and Micropolitan Statistical Areas; Notice.
- Olshansky, S. J. , Antonucci T., Berkman L., Binstock R. H., Boersch‐Supan A., Cacioppo J. T., Carnes B. A., Carstensen L. L., Fried L. P., Goldman D. P., Jackson J., Kohli M., Rother J., Zheng Y., and Rowe J.. 2012. “Differences in Life Expectancy Due to Race and Educational Differences are Widening, and Many May not Catch Up.” Health Affairs 31 (8): 1803–13. [DOI] [PubMed] [Google Scholar]
- Rettenmaier, A. J. , and Wang Z.. 2013. “What Determines Health: A Causal Analysis Using County Level Data.” European Journal of Health Economics 14 (5): 821–34. [DOI] [PubMed] [Google Scholar]
- Ricketts, T. C. , and Holmes G. M.. 2007. “Mortality and Physician Supply: Does Region Hold the Key to the Paradox?” Health Services Research 42 (6 Pt 1): 2233–51 discussion 94–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricketts, T. C. , Goldsmith L. J., Holmes G. M., Randolph R. M., Lee R., Taylor D. H., and Ostermann J.. 2007. “Designating Places and Populations as Medically Underserved: A Proposal for a New Approach.”Journal of Health Care for the Poor and Underserved 18: 567–89. [DOI] [PubMed] [Google Scholar]
- Shrestha, L. B. 2005. “Life expectancy in the United States.” Congressional Information Service, Library of Congress.
- Singh, G. K. 2003. “Area Deprivation and Widening Inequalities in US mortality, 1969–1998.” American Journal of Public Health 93 (7): 1137–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, G. K. , and Hiatt R. A.. 2006. “Trends and Disparities in Socioeconomic and Behavioural Characteristics, Life Expectancy, and Cause‐Specific Mortality of Native‐born and Foreign‐born Populations in the United States, 1979–2003.” International Journal of Epidemiology 35 (4): 903–19. [DOI] [PubMed] [Google Scholar]
- Singh, G. K. , and Miller B. A.. 2004. “Health, Life Expectancy, and Mortality Patterns Among Immigrant Populations in the United States.” Canadian Journal of Public Health. Revue Canadienne de Santé Publique 95 (3): I14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, G. K. , and Siahpush M.. 2006. “Widening Socioeconomic Inequalities in US Life Expectancy, 1980–2000.” International Journal of Epidemiology 35 (4): 969–79. [DOI] [PubMed] [Google Scholar]
- Siahpush M.. 2014a. “Widening Rural‐Urban Disparities in All‐cause Mortality and Mortality from Major Causes of Death in the USA, 1969–2009.” Journal of Urban Health 91 (2): 272–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M.. 2014b. “Widening Rural‐urban Disparities in Life Expectancy, U.S., 1969–2009.” American Journal of Preventive Medicine 46 (2): e19–29. [DOI] [PubMed] [Google Scholar]
- Starfield, B. , Shi L., Grover A., and Macinko J.. 2005. “The Effects of Specialist Supply on Populations’ Health: Assessing the Evidence.” Health Affairs Suppl Web Exclusives 10: W5‐97–W5‐107. [DOI] [PubMed] [Google Scholar]
- Stewart, S. T. C. , and David M.. 2014. “The Contribution of Behavior Change and Public Health to Improved US Population Health.” Washington, DC: National Bureau of Economic Research No. w20631. [Google Scholar]
- Wagnerman, K. , Alker J., Hope C., Jordan P., Gonzalez D., Scaffidi S., Corcoran A., Farkas A., Findings K., Hoadley J., and Holmes M.. 2017. “Medicaid in Small Towns and Rural America: A Lifeline for Children, Families, and Communities” Sheps Center for Health Services Research [accessed on February 21, 2018]. Available at http://www.shepscenter.unc
- Wang, H. , Dwyer‐Lindgren L., Lofgren K. T., Rajaratnam J. K., Marcus J. R., Levin‐Rector A., Levitz C. E., Lopez A. D., and Murray C. J.. 2012. “Age‐specific and Sex‐specific Mortality in 187 Countries, 1970–2010: A Systematic Analysis for the Global Burden of Disease Study 2010.” Lancet 380 (9859): 2071–94. [DOI] [PubMed] [Google Scholar]
- Wang, H. , Schumacher A. E., Levitz C. E., Mokdad A. H., and Murray C. J.. 2013. “Left behind: Widening Disparities for Males and Females in US County Life Expectancy, 1985–2010.” Popul Health Metrices 11 (1): 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilper, A. P. , Woolhandler S., Lasser K. E., McCormick D., Bor D. H., and Himmelstein D. U.. 2009. “Health Insurance and Mortality in US Adults.” American Journal of Public Health 99 (12): 2289–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldridge, J. M. 2010. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press. [Google Scholar]
- Yang, T. C. , Jensen L., and Haran M.. 2011. “Social Capital and Human Mortality: Explaining the Rural Paradox with County‐level Mortality Data.” Rural Sociology 76 (3): 347–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. Example Decomposition Results (2010).
Table S2. Regression Results by Year and Urban/Rural Status.
Table S3. Decomposition Results, Comparison of Model Specification.


