Abstract
Autosomal Dominant Polycystic Kidney Disease (ADPKD) is a genetic disorder caused by loss-of-function mutations in PKD1 or PKD2. Increased glycolysis is a prominent feature of the disease, but how it impacts on other metabolic pathways is unknown. Here, we present an analysis of mouse Pkd1 mutant cells and kidneys to investigate the metabolic reprogramming of this pathology. We show that loss of Pkd1 leads to profound metabolic changes that affect glycolysis, mitochondrial metabolism, and fatty acid synthesis (FAS). We find that Pkd1-mutant cells preferentially use glutamine to fuel the TCA cycle and to sustain FAS. Interfering with either glutamine uptake or FAS retards cell growth and survival. We also find that glutamine is diverted to asparagine via asparagine synthetase (ASNS). Transcriptional profiling of PKD1-mutant human kidneys confirmed these alterations. We find that silencing of Asns is lethal in Pkd1-mutant cells when combined with glucose deprivation, suggesting therapeutic approaches for ADPKD.
Christine Podrini et al. present a comprehensive analysis of Pkd1 mutant mouse cells and kidneys, providing new insight into autosomal dominant polycystic kidney disease (ADPKD). They find that Pkd1 loss leads to profound metabolic changes, including asparagine synthase-driven glutamine anaplerosis.
Introduction
Autosomal dominant Polycystic Kidney Disease (ADPKD) is a monogenic disorder, caused by loss-of-function mutations in either the PKD1 (in ∼85% of cases) or PKD2 (in the remaining ∼15%) genes1–3. The two proteins encoded by these genes, Polycystin-1 (PC-1) and Polycystin-2 (PC-2), are assembled into a functional complex at primary cilia, whose activity is defective in the disease. Additionally, PC-1 can be cleaved at several proteolytic sites4 resulting in products that can translocate either into the nucleus5, or into mitochondria6 or be localized at mitochondrial-associated membrane contacts7,8. Cysts are epithelial outpouches of clonal origin increasing in number and size along the life of affected individuals. Inheriting one mutant allele is not sufficient for cysts to arise, requiring a second event causing the function of the polycystins to drop below a critical threshold of activity2. Loss of heterozygosity has been reported in a subset of cysts suggesting that this might be one of the mechanisms9.
Together with the deregulation of several signalling cascades, ADPKD exhibits metabolic alterations10–12. Among these, defective glucose metabolism was shown to be a feature of the disease11,12 in a process resembling the Warburg effect observed in cancer. This finding prompted investigators to hypothesize that metabolic reprogramming might be a general feature of the disease13,14. Indeed, increased aerobic glycolysis, impaired beta-oxidation, reduced mitochondrial activity were reported in cellular and animal models lacking the Pkd1 gene6–8,11,15–19, while altered glutamine usage was reported in a non-orthologous animal model of recessive polycystic kidney disease20. Likewise, inhibitors of glutamine usage proved effective in retarding disease progression in some, but not in other, models of the disease21,22. However, an overview of these metabolic alterations and their interconnections is still lacking. Metabolic profiling was carried out in non-orthologous models of the disease (i.e. cystogenesis caused by mutations in other genes)23,24, while a single study has attempted at profiling metabolites in the kidneys of a Pkd1 orthologous mouse model15 reporting only a minimal metabolic change in murine kidneys derived from a ubiquitous, inducible inactivation of the Pkd1 gene.
Here, we present a comprehensive metabolomics characterization of cells and renal tissues from a mouse model carrying the kidney-specific inactivation of the Pkd1 gene. Our data indicate a broad metabolic rewiring that involves several pathways including central carbon metabolism and glutamine utilization. Finally, we show that glutamine metabolism is interlinked with asparagine synthesis in ADPKD and we identify the Asparagine Synthase (Asns) gene as an essential component of the process. Of note, targeting this enzyme by siRNA becomes lethal to ADPKD when associated with inhibition of glycolysis. Our data provide evidence of a broad and coordinated metabolic reprogramming in ADPKD, suggesting potential therapeutic strategies.
Results
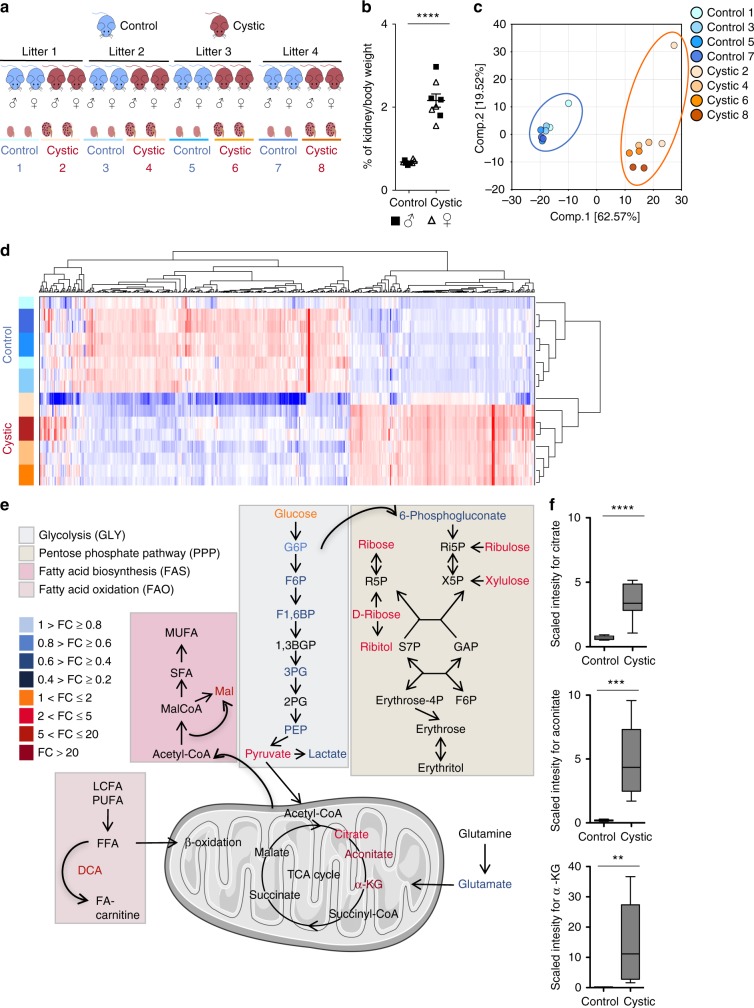
Metabolomic profiling shows multiple changes in Pkd1-mutants
To gather a comprehensive picture of the metabolic derangements observed in ADPKD mouse models, we applied non-targeted global metabolomics25 to an orthologous mouse model of ADPKD carrying inactivation of the Pkd1 gene exclusively in the kidney as to avoid confounding effects derived from extra-renal inactivation. To this end we employed KspCre;Pkd1flox/− kidneys carrying inactivation of the Pkd1 gene in the distal tubules and collecting ducts of the kidney. To minimize phenotype variability in the experimental design we used a pure C57BL/6N background (i.e. >10 backcrosses) and performed the study upon precise timing of the day of birth of the animals (see methods). Furthermore, samples were collected at P4, when the kidneys are already cystic, but not yet functionally or structurally severely compromised (Supplementary Fig. 1a, b). Importantly, neither infiltration nor fibrosis could be detected at this time (Supplementary Fig. 1a). To further strengthen the outcome, we designed the study so that kidneys were collected from 4 litters containing each 2 cystic (KspCre;Pkd1flox/−) and 2 control littermates (KspCre;Pkd1flox/+ or Pkd1flox/+, used interchangeably) of each gender (8 males and 8 females in total) (Fig. 1a) to maximize the possibility to use intra-litter controls. Kidney-over-body weight ratios of Pkd1-mutant mice were significantly different from controls (P < 0.0001), but very similar in males and females at this neonatal stage (P4), possibly because sexual maturation is not yet achieved (Fig. 1b). Furthermore, no increase in Epo or Vegf transcription could be detected, thus excluding the possibility of these kidneys being hypoxic (Supplementary Fig. 1c). Application of Liquid Chromatography–Mass Spectrometry (LC-MS) resulted in the detection of 550 metabolites. A Principal Component Analysis (PCA) showed a clear separation between the cystic and control samples indicating a negligible influence of inter-gender and inter-litter differences in these samples (Fig. 1c). In line with this, hierarchical clustering analysis showed separation of the cystic and control samples (Fig. 1d). Paired t-test analysis was applied to take into account the intra-litter samples, resulting in the identification of 488 metabolites that significantly changed (adjusted P < 0.05), and 384 significantly different metabolites when considering both P-value and fold change (adjusted P < 0.05, absolute fold change >2) between cystic and control samples. A volcano plot of the data shows that 213 of these metabolites are downregulated, while 171 are upregulated, and that the main alterations are related to amino acids, carbohydrates, and lipids (Supplementary Fig. 1d and Supplementary Data 1).
Fig. 1.
Global metabolomic profiling reveals defective TCA cycle in polycystic kidneys. a Study design of the experiment performed on kidneys from Ksp-cre;Pkd1flox/− at P4. 4 litters each containing 2 cystic (red) Ksp-cre;Pkd1flox/− and 2 control littermates Ksp-Cre;Pkd1flox/+ or Pkd1flox/+ (blue, used interchangeably) were collected. Samples were processed for analysis by Ultrahigh Performance Liquid Chromatography–Tandem Mass Spectrometry. b Dot plot view showing percentage of kidney/body weight in the cystic and control kidneys. c PCA applied to the identified metabolites, shows a good separation between cystic versus control kidneys. d Hierarchical clustering analysis shows good clustering between the groups of cystic and control kidneys samples. e Significant metabolites were colour-coded according to the pathway classification. Scheme of the Glycolysis (GLY), Pentose Phosphate Pathway (PPP), Tricarboxylic acid (TCA) cycle, Fatty acid biosynthesis (FAS), Fatty acids oxidation (FAO) in cystic versus control kidneys. Colour corresponds to the fold changes between cystic and control kidneys, orange-red are metabolites more abundant in cystic compared to the control kidneys, whereas blue labelled ones correspond to the less abundant metabolites in cystic kidneys compared to controls. The figure contains modified elements from Servier Medical Art (http://smart.servier.com/). All abbreviations are in Supplementary Table 2. f Box and whiskers view of the levels of TCA intermediates citrate, aconitate, and α-KG were assessed by LC-MS, they were significantly more abundant in cystic compared to the control kidneys. n = 8 independent biological replicates. Dot blots are shown as mean and error bars as SEM; Box and whiskers show median and 2.5-97.5 percentiles, n.s. not significant (P ≥ 0.05), *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001, t-test for b, e, and f
A number of different metabolic pathways were found significantly altered (adjusted P < 0.05, absolute fold change > 2) (Supplementary Fig. 1e). Among these, striking differences were observed in metabolic pathways involved in bioenergetics, including glycolysis (GLY), pentose phosphate pathway (PPP), the tricarboxylic acid (TCA) cycle, fatty acid oxidation (FAO), and fatty acid biosynthesis (FAS) (Fig. 1e). The metabolites that appeared to be mostly accumulated in the cystic kidneys were citrate (P < 0.0001), aconitate (P = 0.0003), and α-ketoglutarate (α-KG) (P = 0.0079) (Fig. 1f). In line with this, KEGG-Pathways Based Enrichment Analysis showed that the TCA cycle is among the pathways affected with a statistically significant Enrichment Score (ES) (P ≤ 0.05) (Supplementary Fig. 1e).
These data indicate that the loss of Pkd1 in the mouse kidney leads to profound metabolic changes, broader than what previously appreciated.
We then used a set of Pkd1+/+ and Pkd1−/− Mouse Embryonic Fibroblasts (MEFs)26 to further investigate the metabolic changes in Pkd1-mutant cells. A metabolomic profiling revealed that Pkd1+/+ and Pkd1−/− MEFs are well separated by PCA with many metabolites being significantly different between the two genotypes (adjusted P < 0.05) (Supplementary Fig. 2a, b) and that metabolic pathways such as glycolysis, PPP, FAS, and FAO were impaired (Supplementary Figure 2c and Supplementary Data 2). Likewise, targeted metabolomics profiling revealed an accumulation of the TCA cycle intermediates citrate, α-KG, succinate, and malate in Pkd1−/− cells as compared to controls (Supplementary Fig. 2c, d). These results show that the response to Pkd1 loss is strikingly similar between Pkd1-mutant MEFs and kidneys, supporting the validity of our cellular model for further mechanistic investigations.
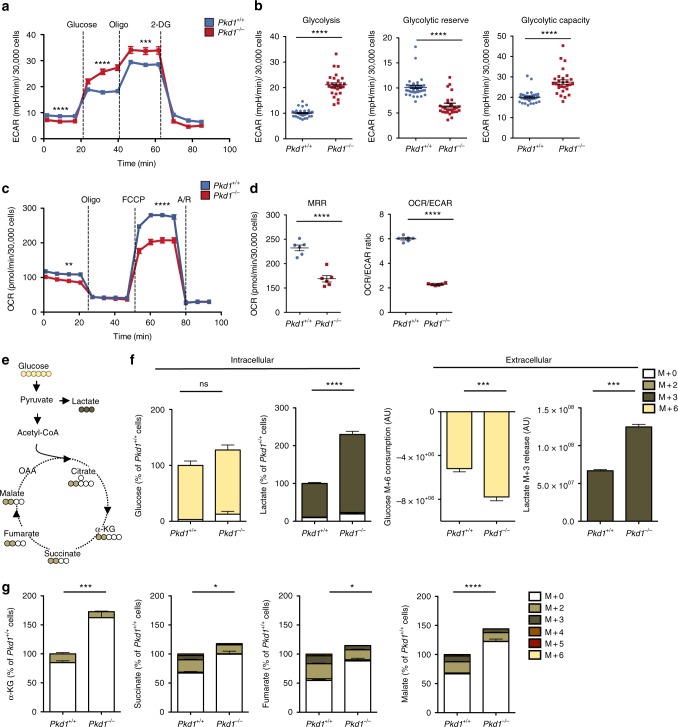
We first assessed whether the TCA cycle alterations could be associated with a defective cellular respiration in Pkd1−/− cells as recently reported7,15. Consistent with this hypothesis, extracellular flux analysis of Pkd1−/− MEFs showed enhanced glycolysis (P < 0.0001) (Fig. 2a, b) and defective respiration (Oxygen Consumption Rate, OCR) (P < 0.0001) (Fig. 2c, d) as compared to Pkd1+/+. Similar results on OCR were generated using primary Pkd1−/− MEFs (Supplementary Fig. 3a) and murine Inner Medullary Collecting Duct Cells (mIMCD cells) where the Pkd1 gene was silenced (P < 0.0001) (Supplementary Fig. 3b)27.
Fig. 2.
Impaired respiration and usage of glucose in the TCA cycle in Pkd1−/− cells. a, b Representative analysis of ECAR outputs of Pkd1−/− compared to Pkd1+/+ cells subject to glycolysis tests in response to glucose, oligomycin and 2-DG, b dot plots showing means with 28 to 39 replicate wells per group for glycolysis, glycolytic capaticity, and glycolytic reserve. Glycolysis was calculated on the 6th measurement time (after substraction of 3rd measurement); the glycolytic reserve was measured on the 9th measurement time (after substraction of 6th measurement); the glycolytic capacity was calculated on the 9th measurement time (after substraction of the 3rd measurement). c, d Representative analysis of OCR measurement in Pkd1+/+ and Pkd1−/− cells in basal conditions and after sequential addition of oligomycin, FCCP and antimycin/rotenone (A/R). d Dot plots showing means with 6 replicate wells per group for: MRR calculated from the 10th measurement (after subtraction of the 13th measurement); OCR/ECAR ratio from basal measurement, 2nd time point. a–d Representative of three independent experiments. e The scheme illustrates the fate of glucose C atoms in glycolysis and Krebs cycle intermediates. Cells were incubated in glucose-free DMEM supplemented with 25 mM 13C6-glucose for 24 h. The uniformly labelled glucose (M + 6 yellow) leads to formation of M + 3 lactate (dark brown) or M + 2 TCA cycle intermediates after its first round (M + 2 light brown). f Percentage of isotopologue distribution of intracellular and extracellular glucose and lactate shows that glucose (M + 6) is more consumed and more converted into lactate (M + 3) in Pkd1−/− cells in comparison to control cells (see Methods for calculations). g Percentage of isotopologue distribution of intracellular intermediates of the TCA: total α-KG, succinate, fumarate, and malate shows that the molecules coming from glucose (M + 2) are decreased in Pkd1−/− MEFs compared to the control cells. Graphs (f, g) are means in percentages relative to control cells of six technical replicates from one experiment. Mean ± SEM were indicated, statistical significance is provided for total pool. n.s. not significant (P ≥ 0.05), *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001, t-test
Glucose entry into the TCA cycle is reduced in Pkd1−/− cells
We then further investigate to what extent the loss of Pkd1 affects central carbon metabolism. To track the contribution of glucose, one of the major carbon sources for the cells, to the TCA cycle in the Pkd1−/− cells, we incubated cells with uniformly labelled 13C-glucose and followed the incorporation of 13C in downstream metabolites (Fig. 2e). Relative to control cells, Pkd1−/− cells took up more glucose (P = 0.0002) and converted it into lactate (P = 0.0001), which is released into the culture medium (Fig. 2f and Supplementary Fig. 3c) in line with our previous findings11,12. Not surprisingly, the results showed that lactate almost entirely derives from glucose (Fig. 2f and Supplementary Fig. 3c). The data also confirmed that total α-KG is significantly increased (P = 0.0002). Importantly, the data showed that the glucose-derived isotopologues of succinate (M + 2) (P = 0.0025), fumarate (M + 2) (P = 0.0001), and malate (M + 2) (P = 0.0023) were all significantly decreased in Pkd1−/− MEFs, indicating a reduced contribution of glucose to the TCA cycle (Fig. 2g).
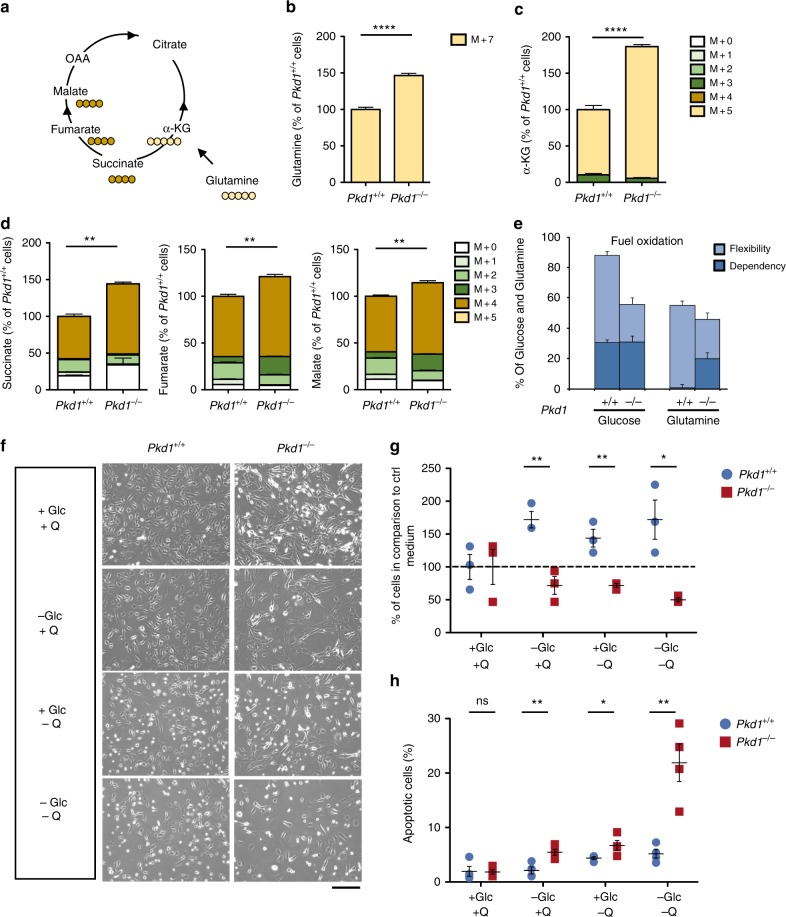
Rewiring of glutamine metabolism in Pkd1−/− cells
We next assessed the utilization of glutamine, another key carbon source for the cells. To this end, we incubated cells with 13C5-15N2-glutamine and the fate of glutamine-derived carbons and nitrogen was assessed by LC-MS (Fig. 3a). Pkd1−/− cells exhibited increased glutamine uptake, compared to the controls (P < 0.0001) (Fig. 3b), and glutamine-derived (M + 5) α-KG (P < 0.0001) (Fig. 3c). In addition, Pkd1−/− cells diverted glutamine towards the TCA cycle, as demonstrated by the increased levels of glutamine-derived succinate (M + 4) (P < 0.0001), fumarate (M + 4) (P < 0.0001), and malate (M + 4) (P < 0.0001) in Pkd1−/− as compared with Pkd1+/+ cells (Fig. 3d). Next, we measured the dependency and flexibility of Pkd1−/− cells relative to their controls (using the XF Mito Fuel Flex test, see Methods). This assay measures the OCR of Pkd1+/+ and Pkd1−/− cells in the presence of glucose and glutamine followed by their blockade using specific inhibitors of the two metabolic pathways (2-Deoxy-d-glucose and BPTES, respectively). Data showed that Pkd1−/− cells are dependent on glutamine for their OCR production (P = 0.0007), while the glucose-driven OCR is overall reduced (P < 0.0001) (Fig. 3e). These data suggest that cells lacking Pkd1 increased their utilization of glutamine to fuel the TCA cycle and maintain their OCR, most likely as a compensatory mechanism due to the reduced funnelling of glucose into mitochondria. Based on these findings, we hypothesized that cells lacking functional Pkd1 would become addicted to glutamine in addition to glucose. Indeed, starvation from either glutamine or glucose reduced cell numbers (P = 0.0068 and P = 0.0057, respectively) (Fig. 3f, g) and increased cell death in Pkd1−/− cells (P = 0.047 and P = 0.0077, respectively) (Fig. 3h) relative to the controls. Importantly, starvation from both carbon sources had a synergistic effect both on cell number (P = 0.015) and on apoptosis (P = 0.0032) (Fig. 3h).
Fig. 3.
Metabolic rearrangement in bioenergetics pathways and glutaminolysis rewiring in Pkd1-/- cells. a The scheme illustrates the fate of glutamine C atoms in Krebs cycle intermediates (Oxidative). Cells were incubated in glutamine-free DMEM supplemented with 4 mM 13C5–15N2 glutamine for 24 h. b Quantification of the intracellular labelled 13C5–15N2 glutamine (M+7) showing that Pkd1−/− cells have a higher uptake compared to the controls. c Isotopologue distribution of intracellular α-KG shows that pools containing five 13C (M + 5), coming from labelled glutamine, were all significantly higher in Pkd1−/− as compared with Pkd1+/+ cells. d Isotopologue distribution of intracellular succinate, fumarate, and malate shows that pools containing four 13C (M + 4), coming from labelled glutamine, were all significantly higher in Pkd1−/− as compared with Pkd1+/+ cells. Graphs are means in percentages relative to control cells of six technical replicates from one experiment. statistical significance is provided for total pool. e Representative graph showing the results in percentage of the XFMitoFuel Flex Test analysis measuring OCR in response to either glucose or glutamine from at least seven technical replicates per well of two independent experiments. Data show a reduced oxidation of glucose in Pkd1−/− cells and an increased dependency on glutamine compared to wild-type cells. f Cells were grown under starvation from either glucose or glutamine or both in 10% serum for 24 and 48 h after an overnight 0.5% serum. Representative images showing the cellular morphology of Pkd1−/− compared to Pkd1+/+cells in starved and non-starved conditions. g Viability of Pkd1+/+ and Pkd1−/− cells, expressed as percentage cell count compared to time 0, after 24 h of incubation in starvation from glucose, glutamine, or both. h Percentage of apoptotic cells assayed by TUNEL assay, showing significant higher percentage of apototic cells in starvation. Graphs (f–h) are representative of at least three independent experiments, data are means from at least three technical replicates. Mean ± SEM were indicated, n.s. not significant (P ≥ 0.05), *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001. t-test (b, c, and d) and (g and h, comparison between each condition)
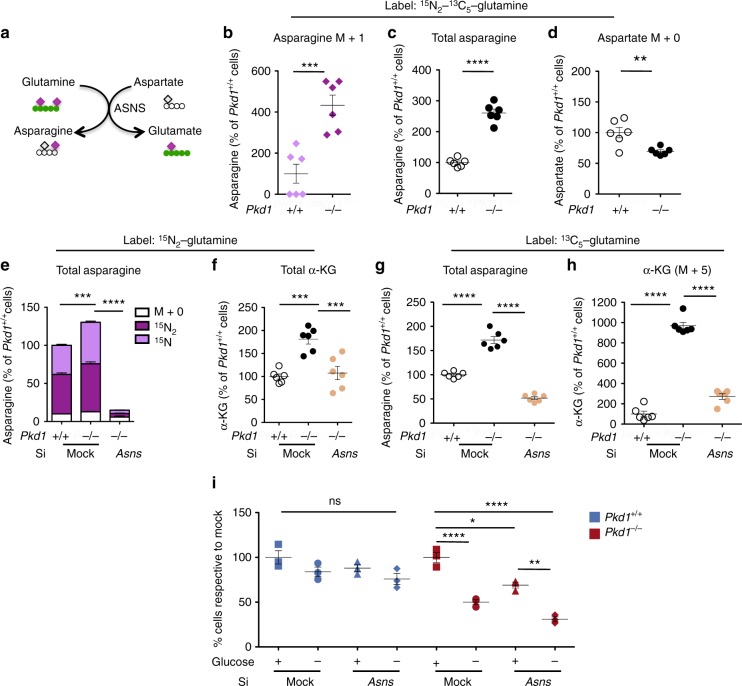
Following the fate of the 15N2-labelled glutamine we noticed that there was a significant increase (P = 0.0006) of 15N-asparagine in the Pkd1−/− cells suggesting an increased activity of asparagine synthase (Fig. 4a, b) and a concomitant increase of the overall levels of labelled asparagine derived from glutamine (P < 0.0001) (Fig. 4c), while aspartate was decreased in the same cells (P = 0.0060) (Fig. 4d). We therefore hypothesized that Pkd1−/− cells exhibit increase asparagine synthesis from glutamine. Of note, quantitative RT-PCR revealed that asparagine synthase, the enzyme that generates asparagine from aspartate (Fig. 4a), was significantly upregulated in cells (P = 0.03) and murine kidneys (P = 0.0095) (Supplementary Fig. 4a). Furthermore, analysis of microarrays from murine and human samples confirmed a significant upregulation of this enzyme in both systems (P = 0.01 and P < 0.0001, respectively) (Supplementary Fig. 4a). Of interest, quantitative RT-PCR revealed no difference in the expression levels of the two enzymes Gls and Glud1 (Supplementary Fig. 4b). To evaluate the relevance of asparagine biosynthesis, we silenced Asns in both Pkd1+/+ and in Pkd1−/− cells (Fig. 4e–h and Supplementary Fig. 4c). As expected, the silencing of Asns reduced the intracellular levels of total asparagine in Pkd1−/− cells (P < 0.0001)(Fig. 4e, g and Supplementary Fig. 4c). Furthermore, metabolic tracing with 15N2-glutamine showed that silencing of Asns indeed reduced the levels of labelled asparagine as expected (Fig. 4e) and importantly the total levels of α-KG (P =0.0001) (Fig. 4f). Furthermore, metabolic tracing with 13C5-glutamine showed a significant reduction in the glutamine-derived α-KG (M + 5) (P < 0.0001) showing that Asns plays a central role in glutamine fuelling of the TCA cycle in Pkd1−/− cells (Fig. 4h). Importantly, the downregulation of Asns also resulted in reduced cell numbers in Pkd1−/− cells (P < 0.05), but not in controls (Fig. 4i). Furthermore, when siAsns:Pkd1−/− cells were subject to glucose starvation we noticed a further decrease in cell numbers compared to controls treated in the same conditions (P < 0.0001) (Fig. 4i). We conclude that Pkd1−/− cells depend on Asns for survival and when they are glucose deprived, downregulation of this enzyme further enhances their dependency.
Fig. 4.
Glutamine usage is interlinked with asparagine synthase (ASNS) in ADPKD. a Schematic overview of the conversion of glutamine into glutamate by transamidating aspartate into asparagine by ASNS. b Labelled 15N-asparagine is significantly increased in the Pkd1 mutant MEFs, c total levels of asparagine are increased compared to the control cells and d decreasing levels of aspartate (M + 0), expressed as percentage relative to controls. e Isotopologue distribution of intracellular asparagine showing that the pool coming from glutamine (15N1 and 15N2) is significantly decreased in siAsns compared to the mock Pkd1−/− and control cells. f Total α-KG was significantly decreased in siAsns compared to the mock Pkd1−/− and control cells in the 15N2 glutamine labelling. g Total asparagine was significantly decreased in siAsns compared to the mock Pkd1−/− cells. h α-KG (M + 5) in the 13C5-glutamine labelling was significantly decreased in siAsns compared to the mock Pkd1−/− and control cells. Data are means from six technical replicates from one experiment. i Representative graph showing the percentage of cell count compared to the respective mock controls. Silencing Asns, deprivation of glucose or both treatments in Pkd1+/+ resulted in no significant difference, whilsts each condition resulted in a significant reduction in cell number with an additive effect of Asns silencing with glucose starvation in Pkd1−/− cells. Data are means from three technical replicates from two independent experiments. Mean ± SEM were indicated, n.s. not significant (P ≥ 0.05), *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001, t-test for b, c, and e. ANOVA followed by Bonferroni for e, f, g, h, and i
Thus, our data show that increased glutaminolysis, interlinked with asparagine metabolism is an important feature of ADPKD and targeting Asns in conjunction with glycolysis might offer a novel therapeutic opportunity.
Pkd1 loss leads to increased de novo fatty acid biosynthesis
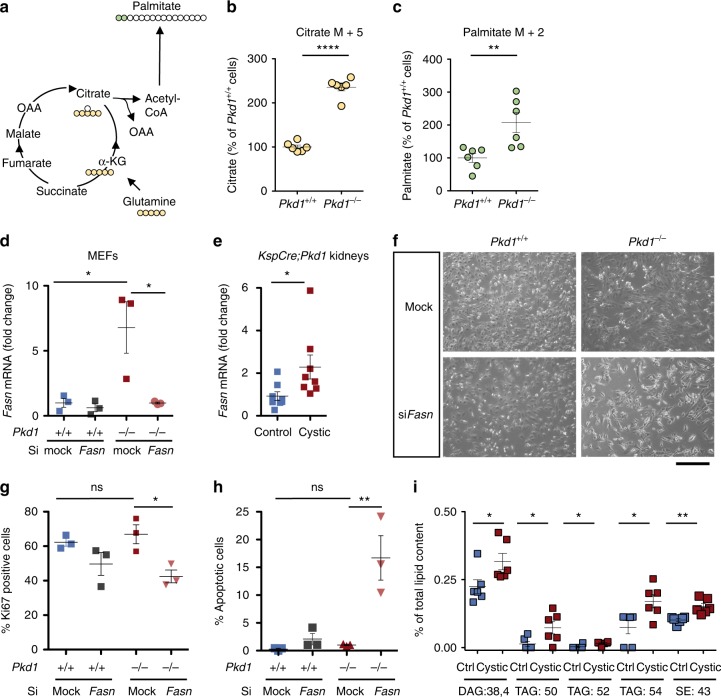
Of interest, the experiments of glutamine tracing also revealed that glutamine is used in an anaplerotic manner by Pkd1−/− cells. Indeed, the increased level of citrate (M + 5) in the 13C5–15N2 glutamine labelling experiment (P < 0.0001) (Fig. 5a, b) suggested that glutamine undergoes reductive carboxylation in Pkd1−/− cells. Given that reductive carboxylation has been linked with synthesis of lipogenic acetyl-CoA, we examined the labelling of palmitate, a fatty acid generated via de novo fatty acid biosynthesis. Consistent with this hypothesis, we noticed an increased labelling of glutamine-derived palmitate (M + 2) (Fig. 5c) in Pkd1−/− cells compared to controls (P = 0.0094), although higher isotopologues could not be detected in this assay. Next, we tested whether Pkd1−/− cells showed increased expression of fatty acids synthase (Fasn), a key enzyme involved in FAS. We found that Fasn is highly expressed in Pkd1−/− cells (P = 0.044) and kidneys of KspCre;Pkd1flox/− animals (P = 0.038) (Fig. 5d, e). Furthermore, its silencing reduced cell proliferation (P < 0.05) and enhanced cell apoptosis (P < 0.05) in Pkd1−/− cells (Fig. 5f–h). In further support of an alteration in lipid metabolism, lipidomics profiling revealed a significant increase in diacylglycerols (DAG) (P = 0.03), triacyglycerols (TAG) (P = 0.03), and sterol esters (P = 0.002) in cystic kidneys compared to controls (Fig. 5i and Supplementary Data 3).
Fig. 5.
Glutaminolysis and fatty acids synthase dependence of Pkd1−/− cells. a The scheme illustrates the fate of glutamine C atoms in TCA cycle intermediates and fatty acid biosynthesis. b Quantification of intracellular citrate (M + 5) labelled by glutamine was significantly higher in Pkd1−/− as compared with Pkd1+/+ cells. c Incorporation of glutamine carbons into intracellular palmitate (M + 2) was significantly higher in Pkd1−/− as compared with Pkd1+/+ cells. Data are means from six technical replicates from one experiment. d Dot plots showing means fold change, SEM, mRNA levels of Fasn in Pkd1−/− compared to mock Pkd1+/+ cells and SiFasnPkd1−/− compared to mock Pkd1−/− normalized to Hprt. Three technical replicates of at least 3 independent experiments. e Dot plots showing means fold change, SEM, mRNA Fasn levels measured in control compared to cystic kidneys normalized to Hprt. n = 8, two technical replicates of at least two independent experiments. f Representative images showing cellular morphology of siFasn in Pkd1+/+ and Pkd1−/− and mock controls. g Representative graph of percentage Ki67-positive cells for mock and SiFasn for Pkd1+/+ and Pkd1−/− cells after 48 h of transient silencing. Data from three technical replicates of at least two independent experiments. h Representative graphs showing percentage of apoptotic cells after 48 h of transfection, data from three technical replicates from three independent experiments. i Lipidomic profiling of cystic versus control kidneys showed altered percentage of diacylglycerol (DAG:38.4), three different species of triacylglycerol (TAG:50, TAG:52 TAG:54) and sterol esters (SE:43) from total lipid content, n = 6. Scale bar is 100 μm. Mean ± SEM were indicated, n.s. not significant (p ≥ 0.05), *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001. t-test for b, c, ANOVA followed by Bonferroni for d, e, g, and h ANOVA for i
Overall, enhanced de novo fatty acids biosynthesis is a feature of ADPKD observed both in cells and in murine tissues and this process is necessary for Pkd1−/− cells to proliferate and survive.
A mathematical model reveals energetic pathways coordination
To gather a broader understanding of the metabolic changes observed, and to predict whether the different pathways are causally linked, we performed an in silico study. To this end we applied a recently described algorithm to predict changes in metabolic fluxes and metabolites across two conditions in a genome-scale metabolic model including 785 metabolites linked by 2589 enzymatic reactions (Differential Flux Balance Analysis, DFA)28. After removing all liver-specific functions, we used DFA to simulate in silico an increase in glucose uptake by imposing a constrain of enhanced glucose input driven by two transporters (TCDB:2.A.21.3.6 and TCDB:2.A.1.1.29, see Methods and Supplementary Data 4). We used as input the amount of increase in glucose uptake (1.6 fold) observed in the tracing experiments of Pkd1−/− MEFs as compared to Pkd1+/+ controls (Fig. 2f). Next, we analysed the complete list of metabolites ranked according to their predicted change. This list was used as the input to KEGG-Pathways Based Enrichment Analysis, resulting in 31 pathways significantly enriched for altered metabolites (FDR ≤ 0.01). The most significant were glycolysis, TCA cycle, PPP, OXPHOS, and FAS (FDR ≤ 0.01) (Supplementary Fig. 5a). Importantly, this method allows to assign a direction to all the metabolic fluxes and to further predict additional alterations. Besides the metabolic pathways above we noticed a remarkable increase in glutamine uptake in the model system (DAp = 0.5) (Fig. 6a, b and Supplementary Data 5), consistent with our glutamine labelling experiments. Further to this, the in silico simulations suggested that CPT1 and CPT2 metabolic fluxes might be reduced as a consequence of increased FAS. Indeed, qRT-PCR analysis showed that Cpt1a was significantly reduced in cells (P = 0.01) and kidneys lacking functional Pkd1 (P = 0.009) (Supplementary Fig. 5b), further validating the predictions originated by the algorithm and in line with previous findings15,16.
Fig. 6.
Global metabolic changes from in silico simulation and transcriptional profiling in polycystic kidney disease. a Analysis of metabolic rearrangement in bioenergetic pathways resulting from in silico simulations. The Differential Abundance (DA) score captures the average, gross changes of all metabolic fluxes in a pathway. A score of −1 indicates that all the simulated metabolic fluxes in the pathway decrease, while a score of 1 indicates that all in silico fluxes increase upon comparing the simulations of increased of glucose uptake with the computations of wild-type conditions. b Representation of the results of metabolic changes in the DFA in silico simulations upon increased glucose uptake. Data show that equilibrium is reached when upregulation of GLY, PPP, glutaminolysis, and FAS is achieved, while a reduction of OXPHOS and FAO. The figure contains modified elements from Servier Medical Art (http://smart.servier.com/). c Identification of genes differentially expressed in Pkd1V/V kidneys versus controls in GLY, PPP, TCA/OXPHOS, FAS, and FAO. D-val represents the output of SAM algorithm launched with the parameter delta set to 1.0. All genes in the panel were differentially expressed between Pkd1V/V animal model and wild-type model at P10 with a FDR equal to 0.1. Upregulated genes are shown in red, while downregulated ones are reported in blue. d Identification of genes differentially expressed in GLY, PPP, TCA/OXPHOS, FAS, and FAO in human PKD1 microarrays data sets. D-val represents the output of SAM algorithm launched with the parameter delta set to 2.4. All genes in the panel were differentially expressed between cystic (small, medium, and large cysts) versus control tissues (minimal cystic and normal renal cortical tissues) with a FDR equal to zero. n = 4 for Pkd1V/V animal model, n = 8 (normal and minimal cyst) and n = 13 for large, medium, small cyst for human PKD1 microarrays
The analysis of the in silico fluxes generated by the model revealed that most of the alterations in the discussed metabolic pathways is coordinated and likely causally linked, to the point that a single change in the increased uptake of glucose recapitulates a broad alteration in the other metabolic pathways (Fig. 6b).
Analysis of ADPKD kidneys transcriptional profiles
We next reasoned that if these changes are indeed coordinated, they should occur in a synchronous fashion in the cystic kidneys. To address this point we first used a qPCR-based transcriptional profiling (qPCR arrays QiagenTM) applied to a KspCre;Pkd1flox/− kidneys analysed at the same time point in which metabolomics was performed (P4). Although the qPCR-based arrays provided a rather limited number of targets, the data showed a trend of alterations to key enzymes involved in GLY, PPP, FAS, and FAO, despite only a few displaying significant changes between the cystic and the control samples (P in the range 0.0002–0.03), (Supplementary Fig. 5c and Supplementary Data 6, 7).
To assess more comprehensively the expression of metabolic enzymes, we performed a microarray analysis on kidneys collected at P10 derived from a hypomorphic Pkd1 mutant mouse (Pkd1V/V), which results in a milder polycystic kidney disease phenotype29. First, data were analysed by PCA and hierarchical clustering analysis, showing a very good separation of the samples in both assays (Supplementary Fig. 5d, e and Supplementary Data 8). Next, microarrays data have been analysed by means of the Significant Analysis of Microarrays (SAM) algorithm to identify differentially expressed genes30 followed by analysis of the full list of genes (Supplementary Data 9) involved in GLY, PPP, and FAS. These genes are mostly upregulated, while the genes involved in OXPHOS and FAO are markedly downregulated (FDR = 0.1) (Fig. 6c). Next, to validate our findings in human samples, we applied again the SAM algorithm30 to a previously published dataset of microarrays derived from the cystic kidneys of patients carrying PKD1 mutations. Data were next screened for the complete list of genes involved in bioenergetics (Methods section) (Fig. 6d)31. The results showed that the metabolic alterations described in cellular and animal models of ADPKD (Figs. 1–3) and recapitulated by the mathematical model (Fig. 6a, b) and by the murine microarrays (Fig. 6c) are all perturbed in ADPKD1 kidneys including GLY, PPP, oxidative TCA cycle (TCA/OXPHOS), FAS, and FAO. Importantly, in human samples as well GLY, PPP, and FAS appear to be mostly upregulated, even if some isoforms of the enzymes are downregulated (FDR = 0). In contrast, both the OXPHOS and FAO enzymes are markedly downregulated (FDR = 0) (Fig. 6d).
These data taken together show that a general metabolic reprogramming of bioenergetic pathways is a hallmark of ADPKD and that likely most alterations are highly coordinated and occur simultaneously, opening unique opportunities for targeting them all with a few interventions.
Discussion
In this study we performed a thorough analysis of the metabolic derangements observed in ADPKD using studies that range from global profiling in orthologous animal models to in silico flux analysis, in vitro carbon and nitrogen tracing, and finally validation in murine and human microarray data sets. The main conclusion of our studies is that a global metabolic reprogramming occurs in ADPKD, involving several pathways. Of all pathways involved, rewiring of central carbon metabolism is the most prominent and includes interlinked alterations of increased GLY, PPP, and FAS along with decreased OXPHOS and FAO. Of interest, we found that glutaminolysis is enhanced as a compensatory mechanism and used for both energy yielding purposes as well as for anabolic needs. Finally, we found that the usage of glutamine in ADPKD is interlinked with the asparagine metabolism and it involves upregulation of Asns. This is particularly intriguing because we found that targeting Asns is lethal in ADPKD cells, particularly when associated with glucose deprivation, thus opening new therapeutic perspectives for a combination therapy in this disease.
Based on previous studies it appeared that minimal changes in a few individual metabolic pathways might occur in ADPKD. Here we show instead that the metabolic alteration in ADPKD tissues is rather robust and occurs in multiple pathways. In addition to GLY and FAO, we find here alterations in the PPP, in FAO, in glutaminolysis and in OXPHOS. Furthermore, we show here that not only multiple metabolic pathways are occurring simultaneously, but that they are interconnected and likely causally linked.
A previous study has performed profiling of metabolites in an orthologous model of ADPKD, reporting only minimal changes in a few metabolites in Pkd1-mutant kidneys. The authors used a Pkd1 orthologous mouse model carrying an inducible ubiquitous Cre15. Inactivation was induced after weaning, leading to a slowly progressive disease model with great variability in the renal phenotype15. This may explain why the metabolomics profiling data failed to separate in PCA based on the genotype. In the current study, we have used a kidney-specific Cre line to inactivate the Pkd1 gene exclusively in the distal tubules and in collecting ducts (cadherin16-Cre, KspCre). This animal model develops a rapidly progressive phenotype with manifestation in the neonatal life. The different time points at which samples were analysed might in part explain the discrepancies with previous work15. More importantly, the animal model used in the current study shows reduced variability in the renal phenotype allowing for a good separation of the sample by PCA analysis and hierarchical clustering. Our data on the reduced FAO agree with those previously reported15, but we propose here that a much broader metabolic derangement than previously appreciated is present in ADPKD.
Importantly, we analysed renal samples at the cystic stage. Therefore, we cannot exclude that the metabolic alterations are secondary to cyst expansion. Relevant to this is the fact that recent investigations have unveiled an important correlation between chronic kidney disease (CKD) and metabolic changes32. Here we have excluded that at the time of analysis (P4) the animals are reaching CKD. Indeed, we observed a minimal initial increase in circulating urea, but absence of prominent inflammatory infiltrate or fibrosis. In addition, most of the metabolic alterations can be observed in isolated cells. Likewise, we have excluded that a prominent hypoxic state is present in the kidneys at the stages analysed. All these pieces of evidence suggest that the observed metabolic derangements are not secondary to CKD or hypoxia. However, based on the current knowledge we cannot exclude that, as disease progresses, additional alterations such as hypoxia and/or CKD can further contribute to disease worsening through additional metabolic stress.
In a recent elegant study, Hajarnis et al. has shown that the reduced FAO is secondary to the upregulation of microRNA-17, which in turn downregulates the expression levels of Pparα, ultimately reducing FAO16. Of interest, the authors were able to rescue the phenotype of Pkd1 mutant mice by using fenofibrate, a natural compound acting as an agonist of Pparα and achieving enhancement of β-oxidation and OXPHOS16,33. Notably, the authors showed that the oncogene Myc is the main driver of miRNA17 expression16. It is important to note here that Myc is indeed considered a master regulator of metabolism in several types of cancer, with glycolysis and glutaminolysis both being regulated by this oncogene34.
In the current study we have used both LC-MS and GC-MS studies to perform metabolic profiling. While this type of analysis is informative, it also has the limitation that it provides a static snapshot of the metabolites detected, without a precise information on whether a given metabolic pathway is upregulated or downregulated. Indeed, we found decreased levels of most glycolytic intermediates in the static analysis of KspCre;Pkd1flox/−, including lactate. This is likely due to a rapid degradation or excretion of lactate in vivo. Indeed, by metabolic tracing with 13C6-glucose we previously showed detection of a large increase in lactate production in vivo11,12 when kidneys are collected after 40 minutes.
Metabolic tracing is a much more powerful tool to study the dynamic regulation of metabolic pathways. Our current studies show that Pkd1−/− cells uptake large amounts of glucose used in the glycolytic pathway to generate lactate and that only minimal amounts of glucose are funnelled into the TCA cycle in mitochondria. Furthermore, we found that an increased uptake of glutamine is occurring in Pkd1−/− cells as compared to the controls and it is oxidized into the TCA cycle, likely compensating for the reduced usage of glucose. Since the overall respiration of the cells is diminished, the likely explanation is that glutamine is used by these cells to preserve the mitochondrial membrane potential and avoid undergoing apoptosis. Indeed, in a previous study we demonstrated that the mitochondrial membrane potential was not majorly affected in the mutant cells11, despite the negligible contribution of glucose to mitochondria-generated ATP11. Our data are in disagreement with previous work reporting lack of enhanced glycolysis, and presence of defective mitochondrial membrane potential in Pkd1−/− cells6. While differences in the cell type employed, in the immortalization procedure or in the culture conditions might account for part of the discrepancies, this cannot be the sole explanation for the controversial results. The glycolysis measurements in the previous studies are affected by wild-type cells being highly glycolytic, suggesting a minimal mitochondrial activity in the control cells and possibly limiting the capability to detect any increase in mutant cells15. Further studies will be required to reconcile the findings in the various different cell types analysed.
In the current study, we show that in addition to being oxidized in the TCA, glutamine is also used reductively in the Pkd1−/− cells to generate citrate, which is transported into the cytosol and converted to acetyl-CoA, an essential substrate for fatty acids biosynthesis. The last process is upregulated in ADPKD likely to generate the membranes required for the proliferation of these cells. Indeed, silencing of Fasn greatly impacts cell proliferation and survival. Thus, our studies demonstrate a critical role for glutamine as a compensatory mechanism for the reduced usage of glucose in polycystic kidney disease. Our data provide the mechanistic explanation for two recent studies demonstrating that targeting glutaminolysis via the inhibition of the enzyme glutaminase (GLS) retards the progression of the disease. However, this effect was observed in some, but not in other animals carrying mutations in Pkd121,22. Our study here provides a potential explanation for this discrepant observation. In our analyses we did not detect changes in the expression levels of GLS. This is in line with the results of Soomro et al., that showed no differences in vitro in the response of polycystic kidney disease or normal cells to inhibitors of GLS22. It should be noted, however, that despite this lack of increased expression we would expect that interfering with this enzyme should reduce glutamine uptake at least in vivo, because GLS is certainly the most commonly used enzyme to convert glutamine to glutamate in most tissues under physiological conditions. Indeed, treatment with the GLS inhibitors CB-839 resulted in a certain degree of reduction of cyst burden in two models of Pkd1 mutants21,22, while it failed to improve the phenotype in a third one22. However, we have shown here that the utilization of glutamine in ADPKD is interlinked with the synthesis of asparagine via asparagine synthetase, ASNS, a transamidase that converts aspartate into asparagine while deaminating glutamine to form glutamate35. A recent study has shown that this reaction is used in physiological conditions by endothelial cells to utilize glutamine as a carbon source36. Our study shows that a similar mechanism is likely employed in ADPKD to consume glutamine. Indeed, silencing of Asns resulted in a complete rescue of the accumulation of α-KG, specifically by reducing the glutamine contribution to α-KG generation. Based on this, we propose that inhibiting ASNS would be a much more specific way to reduce glutamine usage in polycystic kidney disease, opening an important opportunity for a more targeted approach in ADPKD treatment. In line with this, we have found that silencing Asns impacts the growth of Pkd1−/− cells and this is more prominent when cells are also deprived from glucose. The data indicates that indeed glutamine usage compensates for the lack of glucose utilization in the TCA cycle by the Pkd1−/− cells and that targeting both processes at once is more effective than either one alone. In line with this, the starvation from both glucose and glutamine drastically enhances cell death in cells lacking Pkd1. Thus, inhibitors of Asns along with the glycolytic inhibitor 2-deoxy-d-glucose11,12 might offer a good therapeutic strategy in ADPKD and further studies should be devoted to test this possibility.
Ultimately, it should be noted that our results do not show the precise mechanism through which PC-1 regulates cellular and mitochondrial metabolism. Recent studies have reported a possible role for PC-1 in regulation of mitochondrial function either through regulation of mitochondrial Ca2+ uptake in mitochondrial-associated membranes7 or by direct translocation of a short fragment of the protein into the matrix of mitochondria6. Future efforts should be devoted to the understanding of the origin of the metabolic alterations in ADPKD, including the role of the Polycystins in regulation of mitochondrial function.
In conclusion, we report here the first broad overview of the metabolic derangement observed in ADPKD. Importantly, the altered pathways that we report in the current study expand our view on the potential use of inhibitors able to tackle the metabolic alterations to retard disease progression. The highly coordinated alterations observed offer a unique opportunity for targeting the process at multiple levels to block at once the capability of ADPKD cells to produce energy and to synthesize the building blocks needed for proliferation and survival.
Methods
Generation of Pkd1flox/−: Ksp-Cre mice
Pkd1flox/−: Ksp-Cre is a mouse model for ADPKD that develops massive enlarged kidney cysts within few days after birth and was generated by crossing Pkd1flox/flox and Pkd1+/−:Ksp-Cre mice37,38. The age of the pups was accurately assessed by daily control of birth combined with the follow up of the variation of coat colours as described by Jackson Laboratories (https://www.jax.org). All mice used in these experiments were in a pure C57/BL6N genetic background (i.e. >10 backcrosses) and were maintained in specific pathogen free colonies handled by a service company provided at the San Raffaele Scientific Institute (Charles River). Mice received a sterilized (vacuum packed and irradiated) chow diet [25/18 CR, 5 % w/w crude fat (predominantly from soya products), soya oil 0.5% (14% kcal from fats, energy density of 2.64 kcal/g)]. All mice had ad libitum access to water and food. All experiments involving animals were performed under a protocol approved by an institutional ethical committee and, subsequently, by the Italian Ministry of Health (IACUC number: 736).
Untargeted metabolomic analysis of kidneys and MEFs
The untargeted metabolomics in kidneys (Fig. 1) and MEFs (Supplementary Fig. 2) were carried out at Metabolon®. Briefly, samples were subjected to preparation and analysis as per the description of the supplier Metabolon®: to methanol extraction, split into aliquots for analysis by ultrahigh performance liquid chromatography/mass spectrometry (UPLC/MS). Thermo Scientific Q-Exactive high resolution/accurate mass spectrometer interfaced with a heated electrospray ionization (HESI-II) source and Orbitrap mass analyzer operated at 35,000 mass resolution. The sample extract was dried then reconstituted in solvents compatible to each of the four methods. Each reconstitution solvent contained a series of standards at fixed concentrations to ensure injection and chromatographic consistency. One aliquot was analysed using acidic positive ion conditions, chromatographically optimized for more hydrophilic compounds. In this method, the extract was gradient eluted from a C18 column (Waters UPLC BEH C18-2.1 × 100 mm, 1.7 µm) using water and methanol, containing 0.05% perfluoropentanoic acid (PFPA) and 0.1% formic acid. Another aliquot was analysed using acidic positive ion conditions, however it was chromatographically optimized for more hydrophobic compounds. In this method, the extract was gradient eluted from the same afore mentioned C18 column using methanol, acetonitrile, water, 0.05% PFPA, and 0.01% formic acid and was operated at an overall higher organic content. A third aliquot was analysed using basic negative ion optimized conditions using a separate dedicated C18 column. The basic extracts were gradient eluted from the column using methanol and water, however with 6.5 mM Ammonium Bicarbonate at pH 8. The fourth aliquot was analysed via negative ionization following elution from a HILIC column (Waters UPLC BEH Amide 2.1×150 mm, 1.7 µm) using a gradient consisting of water and acetonitrile with 10 mM Ammonium Formate, pH 10.8. The mass-spectrophotometric analysis alternated between MS and data-dependent MSn scans using dynamic exclusion. The scan range varied slighted between methods but covered 70–1000 m/z. Metabolite concentrations were determined by automated ion detection, manual visual curation and were analysed in-line using software developed by Metabolon®39.
Lipid extraction for untargeted mass spectrometry profiling
Mass spectrometry-based lipid analysis was performed at Lipotype GmbH (Dresden, Germany) as previously described and lipids were extracted using a two-step chloroform/methanol procedure40. Briefly, samples were treated as per the description of the company Lypotype GmbH: samples were spiked with internal lipid standard mixture containing: cardiolipin16:1/15:0/15:0/15:0 (CL), ceramide 18:1;2/17:0 (Cer), diacylglycerol 17:0/17:0 (DAG), hexosylceramide18:1;2/12:0 (HexCer), lyso-phosphatidate 17:0 (LPA), lyso-phosphatidylcholine 12:0 (LPC), lysophosphatidylethanolamine 17:1 (LPE), lyso-phosphatidylglycerol 17:1 (LPG), lyso-phosphatidylinositol 17:1 (LPI), lyso-phosphatidylserine 17:1 (LPS), phosphatidate 17:0/17:0 (PA), phosphatidylcholine 17:0/17:0 (PC), phosphatidylethanolamine 17:0/17:0 (PE), phosphatidylglycerol 17:0/17:0 (PG), phosphatidylinositol 16:0/16:0 (PI), phosphatidylserine 17:0/17:0 (PS), cholesterol ester 20:0 (CE), sphingomyelin 18:1;2/12:0;0 (SM), triacylglycerol 17:0/17:0/17:0 (TAG), and cholesterol D6 (Chol). After extraction, the organic phase was transferred to an infusion plate and dried in a speed vacuum concentrator. First step dry extract was re-suspended in 7.5 mM ammonium acetate in chloroform/methanol/propanol (1:2:4,V:V:V) and second step dry extract in 33% ethanol solution of methylamine in chloroform/methanol (0.003:5:1; V:V:V). All liquid handling steps were performed using Hamilton Robotics STARlet robotic platform with the Anti Droplet Control feature for organic solvents pipetting.
Targeted metabolomics and stable isotope tracer analysis
Immortalized Pkd1+/+ and Pkd1−/− MEFs26 and siAsns Pkd1−/− were plated at 150,000 cells/well onto a 6-well plate (n = 6) and cultured in standard conditions. 24 h before sampling for 13C-labelling experiments, MEFs were washed twice with PBS and supplemented with media (DMEM (Gibco) supplemented with 10% dialysed foetal bovine serum (Gibco), 1% Penicillin Streptomycin (Pen/Strep, Gibco), Sodium Bicarbonate (3.7 g/l; Sigma Aldrich) containing either uniformly labelled 13C6-glucose (25 mM) (Cortecnet), 13C5-15N2-glutamine (4 mM) (Cortecnet), 15N2-Glutamine (Cambridge Isotope Laboratories), or 13C5-Glutamine (Cambridge Isotope Laboratories). Metabolites were extracted from cell pellets (intracellular) with 1 ml of extraction solution (methanol for highly pure liquid chromatography (Sigma Aldrich): acetonitrile gradient grade for liquid chromatography (Merck): ultrapure water (Sigma Aldrich), 50:30:20 with 100 ng ml−1 of HEPES (Sigma Aldrich) per million cells. The cell culture medium (extracellular) extracts were prepared by adding 750 µl of extraction solution to 50 µl of centrifuged cell culture medium. Samples were incubated at 4 °C for 15 min at 700 r.p.m., before centrifugation at 13,000 r.p.m. The supernatant was transferred into autosampler vials and stored at −80 °C prior to analysis by LC-MS.
LC-MS analysis was performed using a Q Exactive Orbitrap mass spectrometer coupled to a Dionex U3000 UHPLC system (Thermo Fisher Scientific). The liquid chromatography system was fitted with a Sequant ZIC-pHILIC column (150×2.1 mm) and guard column (20×2.1 mm) from Merck Millipore and temperature maintained at 45 °C. The mobile phase was composed of 20 mM ammonium carbonate and 0.1% ammonium hydroxide in water, and acetonitrile. The flow rate was set at 200 µl min−1 with the gradient described previously41. To expand on the range of metabolites covered in the analysis, the sample extracts were then run on a ZIC-HILIC column (150 mm × 4.6 mm) fitted with a guard column (20 mm × 2.1 mm) (both Merck Millipore). The aqueous mobile phase solvent used was 0.1% formic acid in water, and the organic mobile phase was 0.1% formic acid in acetonitrile. The flow rate was set at 300 μl min−1 and the column oven set to 30 °C, as described previously41. The mass spectrometer was operated in full MS mode with polarity switching, and samples were randomized in order to avoid bias due to machine drift and processed blindly. The acquired spectra were analysed using XCalibur Qual Browser and XCalibur Quan Browser software (Thermo Fisher Scientific).
Mass isotopologue distribution of metabolites was determined by integration of the corresponding peaks, and correction for natural abundance was performed using the PollyTM IsoCorrect tool from the cloud-based platform Elucidata (https://polly.elucidata.io).
Consumption and release of metabolites was assessed by subtracting each metabolite total pool in the fresh medium (incubated in the absence of cells) from the pool found in the spent medium samples. The resulting value was then adjusted to the amount of protein generated during the incubation of the cells with the labelled substrate. For this purpose, cells were seeded in parallel plates and protein content was determined by the Bradford method at 0 and 24 h post medium change. Percentage of intracellular pool from each isotopologue was calculated respective of the control (for each metabolite).
Glycolysis and mitochondrial respiration assays
Cells were plated at a density of 20,000 or 30,000 cells per well in a 96-wells Seahorse cell culture microplates and incubated in a 5% CO2 incubator at 37 °C overnight. The following day, 1 h before the test, culture media was replaced with pH-adjusted (pH = 7.4 ± 0.1) bicarbonate-free DMEM (Agilent) with 10 mM glucose (Sigma Aldrich), 1 mM sodium pyruvate (Gibco), and 2 mM l-glutamine (Gibco) for Mito Flex Test (Agilent) and Mito Stress Test or with 2 mM l-glutamine only for Glycolysis Stress Test (Agilent). The plate was then incubated at 37 °C for 1 h in a non-CO2 incubator. For the Mito Fuel Flex test and Mito Stress Test, OCR were measured using the Seahorse XF Mito Fuel Flex Test Kit XF and Mito Stress Test Kit (Agilent). Extracellular Acidification Rate (ECAR) was measured using XF Glycolysis Stress Test Kit (Agilent) on an XFe96 Analyzer (Agilent) following the manufacturer’s instructions. Cell numbers were normalized using CyQuant (Thermo Fisher).
RNA extraction and microarray
Kidneys were removed from wild-type (n = 4) and Pkd1V/V (n = 4) mice at P10 and homogenized in PBS buffer using mini handheld homogenizer. The homogenate was centrifuged and supernatant was discarded. Total RNAs were extracted from the pellet using an RNeasy mini kit (Qiagen) and the quality of total RNA samples was verified by a 260/280 ratio in NanoDrop and agarose gel electrophoresis. Further sample processing for microarray analysis was performed by the Genomics Core of Cleveland Clinic’s Lerner Research Institute, following the facility’s protocols, and hybridized to Illumina’s MouseRef-8 v2.0 BeadChip expression arrays.
Real-time PCR analysis
RNA was isolated from plated cells or snap-frozen kidneys using the RNAspin Mini kit (GE Healthcare). Total RNA was isolated using the RNA-Isol lysis reagent according to the manufacturer’s instructions. For reverse transcription of RNA, Oligo(dT)15 primers (Promega) and ImProm-II Reverse Transcriptase (Promega) were used. Quantitative real-time PCR analysis was performed on duplicate using SYBR Green I master mix (Roche) on LightCycler 480 Instrument (Roche). For primers sequence see supplementary methods, Supplementary Table 1.
Transient knockdown of Fasn and Asns
For transient knockdown of siFasn and siAsns 20 nM (Ambion) pre-designed mRNA with the target sequences: FASN 5′-GGGAUCAUAAAGAUAACUUtt-3′ and 5′-AAGUUAUCUUUAUGAUCCCtc ASNS 5′-GGCCCUUGUUUAAAGCCAUtt-3′ and 5′-AUGGUUUAAACAAGGGCCtg-3’ along with control scrambled siRNA (siCONTROL, Dharmacon), were used following the manufacturer’s instructions and transfection control. For siRNA transfection cells were seeded into a 6-well plate, 100,000/well in 10% FBS (Gibco) in DMEM (Gibco) without antibiotics. The transfections were performed two times over 2 days at a final concentration of 30 nM using Lipofectamine 3000® following the manufacturer’s protocol. Total RNA was prepared from the cells 72 h after the first transfection and qRT-PCR was performed.
Apoptosis cell assay
Cell death detection kit (TUNEL, Promega) was performed according to the manufacturer instructions after transient knockdown of siFasn or after 48 h of starvation experiments (glutamine, glucose starvation). The protocols and quantifications were previously optimized11.
Growth curve of MEFs in glucose and glutamine starvation
Immortalized Pkd1+/+ and Pkd1−/− MEFs were plated at a density of 150,000 cells/well in DMEM (Gibco) supplemented with 0.5% FBS (Gibco) and 1% Pen/Strep (Gibco). After 16 h, medium was changed to control medium (DMEM, Gibco), supplemented with 10% FBS (Gibco), 1% Pen/Strep (Gibco), sodium pyruvate (1 mM; Gibco), sodium bicarbonate (44 mM; Sigma Aldrich), 25 mM glucose (Sigma Aldrich), and 4 mM glutamine (Gibco); glucose starvation medium (DMEM supplemented with 1 mM Sodium pyruvate, 44 mM sodium bicarbonate, 10% FBS, 1% Pen/Strep and 4 mM glutamine); glutamine starvation medium (DMEM supplemented with 10% FBS, 1% Pen/Strep, 1 mM sodium pyruvate, 44 mM sodium bicarbonate, and 25 mM glucose) or glucose and glutamine starvation medium (DMEM supplemented with 10% FBS and 1% Pen/Strep, 1 mM sodium pyruvate, 44 mM sodium bicarbonate). After 24 and 48 h, cells were trypsinized and counted with an automated cell counter (Countess cell counter, Invitrogen). Pictures from each sample at both time points were taken with a white field microscope, using a ×10 objective.
Analysis using the KEGG-pathways based enrichment analysis
Analysis of the untargeted metabolomics studies was performed by implementing a KEGG-Pathways Based Enrichment Analysis (PBEA) system based on a similar concept than the Gene Set Enrichment Analysis (GSEA)42 which tests whether compounds involved in predefined pathways occur towards the top or bottom of the ranked query list. The method identifies altered pathways of the Kyoto Encyclopaedia of Genes and Genomes (KEGG)43 using metabolite data. An enrichment score and a statistical significance (P-value) have been computed for each pathway having at least one metabolite captured in the list of metabolites ranked, in descending order, according to a specific metric. Particularly, a fold change was used to rank the metabolites deriving from non-targeted global metabolomics, while the Differential Flux balance Analysis algorithm was used to rank the compounds resulting from the in silico simulations. In order to avoid ambiguous identification and to obtain reliable results only metabolites having a KEGG-identifier have been considered. The list of ranked metabolites named as L, and S for the set of compounds of a particular pathway. Analysis is performed to test whether the elements of S are randomly distributed through L or primarily found at the top or bottom of the list. The enrichment score reflects the degree to which S is over-represented at the extremes of L, and it is computed by walking down L, increasing a running-sum statistic when a metabolite in S is found and decreasing it when a compound not in S is encountered. The obtained score corresponds to a weighted Kolmogorov-Smirnov-like statistic43 and represents the maximum deviation from zero associated with a random walk. The P-value associated with an enrichment score has been computed as the fraction of 1000 random permutations of the elements of L that are at least as extreme as the original enrichment score, that has been derived from non-permuted elements. A Matlab® implementation of the method is available upon request.
Differential abundance score
For a particular pathway P, the Differential Abundance (DAp) score is defined as:
where ur is the delta of in silico flux of reaction r computed by DFA. This score captures the tendency for a pathway to be upregulated or downregulated and varies from −1 to 1. A score of −1 indicates that all the metabolic fluxes associated with reactions in pathway P decreased respect to wild-type, while a score of 1 indicates that all fluxes increased when comparing with the wild-type simulation.
In silico modelling and simulation of increased glycolysis
For the in silico studies the Genome-Scale Metabolic Model described in Pagliarini et al. was applied28. The model comprises 785 metabolites and 2589 enzymatic and transport reactions in eight compartments. In order to have more physiological results, the following additional constrains have been imposed: citrate cannot move from cytosol to mitochondria; pyruvate cannot move from mitochondria to cytosol; cytosolic enzyme LDH can only convert pyruvate to lactate and not vice versa. Then, Differential Flux balance Analysis was applied28 to simulate either the wild-type condition or an increase of glucose entering the cytosol (GLY). DFA is based on solving a linear optimization problem across 442 metabolic objectives for both the wild-type model and the perturbed model. For the current study, the liver-specific metabolic functions were removed. The average flux carried by each reaction across the different metabolic objectives for each of the two models is computed. For each reaction, the difference of the average flux in the wild-type model minus its value in the modified model are then considered. These differential fluxes are then used to rank the reactions from the ones that change the most in the modified model to the ones that change the least or do not change at all. Metabolites are then ranked according to the sum of the absolute values of the differential fluxes. In order to simulate an increase of the glucose uptake the results of the 13C-glucose labelled experiments showing an increase of 1.6 fold change in the uptake of glucose has been used. Therefore, the fluxes through the reactions Glucose(s) + Na + (s) − > Glucose(c) + Na + (c) (TCDB:2.A.21.3.6) and Glucose(s) < = > Glucose(c) (TCDB:2.A.1.1.29) has been forced, to be equal or greater than a specific threshold set to the their average value obtained in the wild-type simulations increased of 60%.
Analysis of murine and human microarray data
In order to infer differentially expressed genes in microarrays data from Pkd1V/V animal model at P10, a Matlab® implementation the SAM algorithm with delta = 1.0 was applied.
For human microarrays, data from Song et al.31 have been considered. First, affymetrix probe sets have been collapsed to one gene level by using the maximum expression value of the probe set in each gene. Then, the SAM algorithm has been applied, with delta = 2.4, to identify differentially expressed genes between transcripts in renal cysts of different sizes, and minimal cystic tissue plus normal renal cortical samples. The Matlab® implementation of SAM can be found in (https://it.mathworks.com/matlabcentral/fileexchange/42346-significance-analysis-of-microarrays–sam–using-matlab). In both microarrays analysis, after the computation of all the differentially expressed genes, those belonging to glycolysis, pentose phosphate pathway, TCA cycle/OXPHOS, fatty acid synthesis, and fatty acid oxidation were identified (Supplementary Data 9).
Statistical analysis
For statistical analysis the Prism 5, GraphPad Software, and Matlab® were used using statistical analysis tool. t-test was used for all analysis of two groups. ANOVA statistical analysis followed by Bonferroni’s multiple comparison test was performed in all analysis where more than two groups were present. The P-values for each condition are indicated in the legends.
Images creation
Figures 1e, 6b, and Suppl Fig. 2C contain modified images from Servier Medical Art, licensed under a Creative Common Attribution 3.0 Generic License. http://smart.servier.com/. All other images were generated by the authors.
Electronic supplementary material
Acknowledgements
We are grateful to other members of the Boletta lab for helpful discussions. This work was funded by the PKD Foundation (grant #187G14a/b to A.B., grant #211G16a to F.Q.), the Italian association for PKD (Associazione Italiana Rene Policistico—AIRP, to A.B. and M.C.) by the Italian Ministry of Health (RF-2011-02351840 to A.B., GR-2016-02364851 to C.P. and R.P.), the European Community (COFUND-INVEST, GA-2010-267264 to C.P.), and the Umberto Veronesi Foundation (Post-Doctoral fellowship to R.P.) and the National Institutes of Health (R01DK111611 to F.Q.) and the Baltimore PKD Research and Clinical Core Center (P30DKO90868 from NIDDK). The support of Fondazione Pierfranco e Luisa Mariani, Milan (to V.T.), is gratefully acknowledged. We are deeply grateful to Dr. S. Bramani for her continuous support.
Author contributions
C.P., I.R., and R.P. designed the studies, performed experiments and analysis, wrote the manuscript; R.P. generated all in silico analysis and transcriptional profiles data analysis; A.S.H.C. designed, performed and analysed studies of metabolic tracing; M.C. performed experiments on murine models; I.D.M. performed analysis with the SeaHorse; H.K. performed collection and analysis of Pkd1v/v kidneys for microarrays analysis; G.D. performed experiments with the SeaHorse; V.T. supervised studies with the SeaHorse technology; F.Q. supervised the murine microarrays studies on Pkd1v/v kidneys; D.d.B. supervised the in silico work; C.F. supervised the work on metabolic tracing, discussed data on metabolic profiling, and wrote the manuscript; A.B. supervised all the work and collaborations, analysed data, discussed the results, and wrote the manuscript.
Data availability
All data are provided within the manuscript. Raw data and elaboration for figures preparation are contained in Supplementary data 10. The raw data of metabolic tracing experiments ara available in Supplementary Data 11 and deposited into the MetaboLights database (reference number MTBLS677). Raw data of microarrays from Pkd1v/v mice are available at GEO (GSE121563).
Competing interests
A.B., I.R., and M.C. are co-inventors on a pending patent for the use of glycolysis inhibitors in polycystic kidney disease (European patent application N. 13733319.1; US Patent application N. 14/413,280). A.B., I.R., and C.P. are also co-inventors on a pending patent for the use of multiple metabolic interventions in polycystic kidney disease (European patent application, undisclosed number-under secrecy). The remaining authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Christine Podrini, Isaline Rowe, Roberto Pagliarini.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s42003-018-0200-x.
References
- 1.Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007;369:1287–1301. doi: 10.1016/S0140-6736(07)60601-1. [DOI] [PubMed] [Google Scholar]
- 2.Harris PC, Torres VE. Genetic mechanisms and signaling pathways in autosomal dominant polycystic kidney disease. J. Clin. Invest. 2014;124:2315–2324. doi: 10.1172/JCI72272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ong AC, Harris PC. A polycystin-centric view of cyst formation and disease: the polycystins revisited. Kidney Int. 2015;88:699–710. doi: 10.1038/ki.2015.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qian F, et al. Cleavage of polycystin-1 requires the receptor for egg jelly domain and is disrupted by human autosomal-dominant polycystic kidney disease 1-associated mutations. Proc. Natl Acad. Sci. USA. 2002;99:16981–16986. doi: 10.1073/pnas.252484899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chauvet V, et al. Mechanical stimuli induce cleavage and nuclear translocation of the polycystin-1 C terminus. J. Clin. Invest. 2004;114:1433–1443. doi: 10.1172/JCI21753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin CC, et al. A cleavage product of Polycystin-1 is a mitochondrial matrix protein that affects mitochondria morphology and function when heterologously expressed. Sci. Rep. 2018;8:2743. doi: 10.1038/s41598-018-20856-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Padovano V, et al. The polycystins are modulated by cellular oxygen-sensing pathways and regulate mitochondrial function. Mol. Biol. Cell. 2017;28:261–269. doi: 10.1091/mbc.e16-08-0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Padovano Valeria, Podrini Christine, Boletta Alessandra, Caplan Michael J. Metabolism and mitochondria in polycystic kidney disease research and therapy. Nature Reviews Nephrology. 2018;14(11):678–687. doi: 10.1038/s41581-018-0051-1. [DOI] [PubMed] [Google Scholar]
- 9.Qian F, Watnick TJ, Onuchic LF, Germino GG. The molecular basis of focal cyst formation in human autosomal dominant polycystic kidney disease type I. Cell. 1996;87:979–987. doi: 10.1016/S0092-8674(00)81793-6. [DOI] [PubMed] [Google Scholar]
- 10.Menezes LF, et al. Network analysis of a Pkd1-mouse model of autosomal dominant polycystic kidney disease identifies HNF4alpha as a disease modifier. PLoS Genet. 2012;8:e1003053. doi: 10.1371/journal.pgen.1003053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rowe I, et al. Defective glucose metabolism in polycystic kidney disease identifies a new therapeutic strategy. Nat. Med. 2013;19:488–493. doi: 10.1038/nm.3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiaravalli M., Rowe I., Mannella V., Quilici G., Canu T., Bianchi V., Gurgone A., Antunes S., DAdamo P., Esposito A., Musco G., Boletta A. 2-Deoxy-D-Glucose Ameliorates PKD Progression. Journal of the American Society of Nephrology. 2015;27(7):1958–1969. doi: 10.1681/ASN.2015030231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Priolo C, Henske EP. Metabolic reprogramming in polycystic kidney disease. Nat. Med. 2013;19:407–409. doi: 10.1038/nm.3140. [DOI] [PubMed] [Google Scholar]
- 14.Seeger-Nukpezah T, Geynisman DM, Nikonova AS, Benzing T, Golemis EA. The hallmarks of cancer: relevance to the pathogenesis of polycystic kidney disease. Nat. Rev. Nephrol. 2015;11:515–534. doi: 10.1038/nrneph.2015.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Menezes LF, Lin CC, Zhou F, Germino GG. Fatty acid oxidation is impaired in an orthologous mouse model of autosomal dominant polycystic kidney disease. EBioMedicine. 2016;5:183–192. doi: 10.1016/j.ebiom.2016.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hajarnis S, et al. microRNA-17 family promotes polycystic kidney disease progression through modulation of mitochondrial metabolism. Nat. Commun. 2017;8:14395. doi: 10.1038/ncomms14395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riwanto Meliana, Kapoor Sarika, Rodriguez Daniel, Edenhofer Ilka, Segerer Stephan, Wüthrich Rudolf P. Inhibition of Aerobic Glycolysis Attenuates Disease Progression in Polycystic Kidney Disease. PLOS ONE. 2016;11(1):e0146654. doi: 10.1371/journal.pone.0146654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li X, et al. A tumor necrosis factor-alpha-mediated pathway promoting autosomal dominant polycystic kidney disease. Nat. Med. 2008;14:863–868. doi: 10.1038/nm1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Warner G., Hein K. Z., Nin V., Edwards M., Chini C. C. S., Hopp K., Harris P. C., Torres V. E., Chini E. N. Food Restriction Ameliorates the Development of Polycystic Kidney Disease. Journal of the American Society of Nephrology. 2015;27(5):1437–1447. doi: 10.1681/ASN.2015020132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hwang VJ, et al. The cpk model of recessive PKD shows glutamine dependence associated with the production of the oncometabolite 2-hydroxyglutarate. Am. J. Physiol. Ren. Physiol. 2015;309:F492–498. doi: 10.1152/ajprenal.00238.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flowers EM, et al. Lkb1 deficiency confers glutamine dependency in polycystic kidney disease. Nat. Commun. 2018;9:814. doi: 10.1038/s41467-018-03036-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soomro Irfana, Sun Ying, Li Zhai, Diggs Lonnette, Hatzivassiliou Georgia, Thomas Ajit G, Rais Rana, Slusher Barbara S, Somlo Stefan, Skolnik Edward Y. Glutamine metabolism via glutaminase 1 in autosomal-dominant polycystic kidney disease. Nephrology Dialysis Transplantation. 2018;33(8):1343–1353. doi: 10.1093/ndt/gfx349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor SL, et al. A metabolomics approach using juvenile cystic mice to identify urinary biomarkers and altered pathways in polycystic kidney disease. Am. J. Physiol. Ren. Physiol. 2010;298:F909–F922. doi: 10.1152/ajprenal.00722.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Natoli TA, et al. Inhibition of glucosylceramide accumulation results in effective blockade of polycystic kidney disease in mouse models. Nat. Med. 2010;16:788–U787. doi: 10.1038/nm.2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naz S, Vallejo M, Garcia A, Barbas C. Method validation strategies involved in non-targeted metabolomics. J. Chromatogr. A. 2014;1353:99–105. doi: 10.1016/j.chroma.2014.04.071. [DOI] [PubMed] [Google Scholar]
- 26.Distefano G, et al. Polycystin-1 regulates extracellular signal-regulated kinase-dependent phosphorylation of tuberin to control cell size through mTOR and its downstream effectors S6K and 4EBP1. Mol. Cell Biol. 2009;29:2359–2371. doi: 10.1128/MCB.01259-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Castelli M, et al. Polycystin-1 binds Par3/aPKC and controls convergent extension during renal tubular morphogenesis. Nat. Commun. 2013;4:2658. doi: 10.1038/ncomms3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pagliarini R, et al. In silico modeling of liver metabolism in a human disease reveals a key enzyme for histidine and histamine homeostasis. Cell Rep. 2016;15:2292–2300. doi: 10.1016/j.celrep.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yu S, et al. Essential role of cleavage of Polycystin-1 at G protein-coupled receptor proteolytic site for kidney tubular structure. Proc. Natl Acad. Sci. USA. 2007;104:18688–18693. doi: 10.1073/pnas.0708217104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tusher VG, Tibshirani R, Chu G. Significance analysis of microarrays applied to the ionizing radiation response. Proc. Natl Acad. Sci. USA. 2001;98:5116–5121. doi: 10.1073/pnas.091062498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Song X, et al. Systems biology of autosomal dominant polycystic kidney disease (ADPKD): computational identification of gene expression pathways and integrated regulatory networks. Hum. Mol. Genet. 2009;18:2328–2343. doi: 10.1093/hmg/ddp165. [DOI] [PubMed] [Google Scholar]
- 32.Kang HM, et al. Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development. Nat. Med. 2015;21:37–46. doi: 10.1038/nm.3762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lakhia R, et al. PPARalpha agonist fenofibrate enhances fatty acid beta-oxidation and attenuates polycystic kidney and liver disease in mice. Am. J. Physiol. Ren. Physiol. 2018;314:F122–F131. doi: 10.1152/ajprenal.00352.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dejure FR, Eilers M. MYC and tumor metabolism: chicken and egg. EMBO J. 2017;36:3409–3420. doi: 10.15252/embj.201796438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lomelino CL, Andring JT, McKenna R, Kilberg MS. Asparagine synthetase: function, structure, and role in disease. J. Biol. Chem. 2017;292:19952–19958. doi: 10.1074/jbc.R117.819060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huang Hongling, Vandekeere Saar, Kalucka Joanna, Bierhansl Laura, Zecchin Annalisa, Brüning Ulrike, Visnagri Asjad, Yuldasheva Nadira, Goveia Jermaine, Cruys Bert, Brepoels Katleen, Wyns Sabine, Rayport Stephen, Ghesquière Bart, Vinckier Stefan, Schoonjans Luc, Cubbon Richard, Dewerchin Mieke, Eelen Guy, Carmeliet Peter. Role of glutamine and interlinked asparagine metabolism in vessel formation. The EMBO Journal. 2017;36(16):2334–2352. doi: 10.15252/embj.201695518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wodarczyk C, et al. A novel mouse model reveals that polycystin-1 deficiency in ependyma and choroid plexus results in dysfunctional cilia and hydrocephalus. PLoS ONE. 2009;4:e7137. doi: 10.1371/journal.pone.0007137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shao X, Somlo S, Igarashi P. Epithelial-specific Cre/lox recombination in the developing kidney and genitourinary tract. J. Am. Soc. Nephrol. 2002;13:1837–1846. doi: 10.1097/01.ASN.0000016444.90348.50. [DOI] [PubMed] [Google Scholar]
- 39.Dehaven CD, Evans AM, Dai H, Lawton KA. Organization of GC/MS and LC/MS metabolomics data into chemical libraries. J. Chemin. 2010;2:9. doi: 10.1186/1758-2946-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sampaio JL, et al. Membrane lipidome of an epithelial cell line. Proc. Natl Acad. Sci. USA. 2011;108:1903–1907. doi: 10.1073/pnas.1019267108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mackay GM, Zheng L, van den Broek NJ, Gottlieb E. Analysis of cell metabolism using LC-MS and isotope tracers. Methods Enzymol. 2015;561:171–196. doi: 10.1016/bs.mie.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 42.Subramanian A, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA. 2005;102:15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are provided within the manuscript. Raw data and elaboration for figures preparation are contained in Supplementary data 10. The raw data of metabolic tracing experiments ara available in Supplementary Data 11 and deposited into the MetaboLights database (reference number MTBLS677). Raw data of microarrays from Pkd1v/v mice are available at GEO (GSE121563).