Key Teaching Points.
-
•
Reflex syncope is common in the young and typically is benign. We present a case of reflex syncope associated with nonsustained polymorphic ventricular tachycardia.
-
•
In susceptible individuals, autonomic stimuli may trigger significant arrhythmias, other than the anticipated bradyarrhythmias.
-
•
In some individuals with no apparent risk factors, autonomic nervous system miscues may lead to life-threatening arrhythmias, with the potential for progressing to sudden cardiac arrest.
-
•
This case may provide insight into the 50% of individuals who experience a cardiac arrest with no identifiable cause.
Introduction
Syncope is common, occurring in approximately 30%–40% of the population by age 60 years.1 Reflex syncope presents as loss of consciousness and postural tone with spontaneous recovery. The ultimate cause is cerebral hypoperfusion, although the underlying mechanism(s) is not completely understood. The final pathway results in impairments of cerebral perfusion and cardiac output that have vasodepressor, cardioinhibitory, or mixed vasodepressor and cardioinhibitory origins.2 Reflex syncope is most commonly triggered by postural or orthostatic stress, but other well-documented triggers include stereotypical situations such as micturition and defecation syncope. The most informative diagnostic test is an accurate, detailed history, ideally from the patient.1 Confirming typical triggers2 for the syncope is reassuring and implies a benign prognosis. Recurrence is predicted primarily by the frequency of recent syncopal episodes.
There is concern that syncopal events may be a marker of an underlying potentially lethal cardiac condition, so investigations are often extensive in individuals with syncope but invariably yield little information. Moreover, sudden cardiac arrest (SCA) is an uncommon problem in the young. Although so-called warning events are frequent in cohorts of patients who subsequently have a cardiac arrest,3, 4, 5 identifying the 1 in 5000 individuals with syncope who may go on to have SCA is difficult and expensive.
We present an unusual case of seemingly typical reflex syncope, in the form of defecation syncope, in a patient who had a pacemaker in situ. The device recorded polymorphic ventricular tachycardia (PVT) at the time of the syncopal event.
Case report
A 17-year-old girl underwent an epicardial pacemaker implant during infancy for congenital heart block secondary to maternal anti-Ro and anti-La antibodies. The pacemaker had been upgraded to a transvenous dual-chamber pacemaker (Medtronic Adapta, Medtronic PLC, Fridley, MN) 2 years before the episode. At the time of the episode, the pacemaker was programmed to a DDD mode, with an upper tracking rate of 210 bpm and a 3-fold amplitude safety margin in both leads. She would track the atrium and pace the ventricle nearly 100% of the time, except for some low rate atrial pacing at rest. During the 15 years of follow-up, she remained well. Several echocardiograms showed normal function and no evidence of cardiomyopathy. Previous exercise testing was normal. She was known to have rare atrial ectopy, which was asymptomatic and incidentally detected by the device. There was no family history of SCA or suspicious deaths. Her nonpaced QTc was normal (420 ms), with normal QRS morphology and repolarization. In recent years, she had been diagnosed with social anxiety disorder and had started taking sertraline, a selective serotonin reuptake inhibitor.
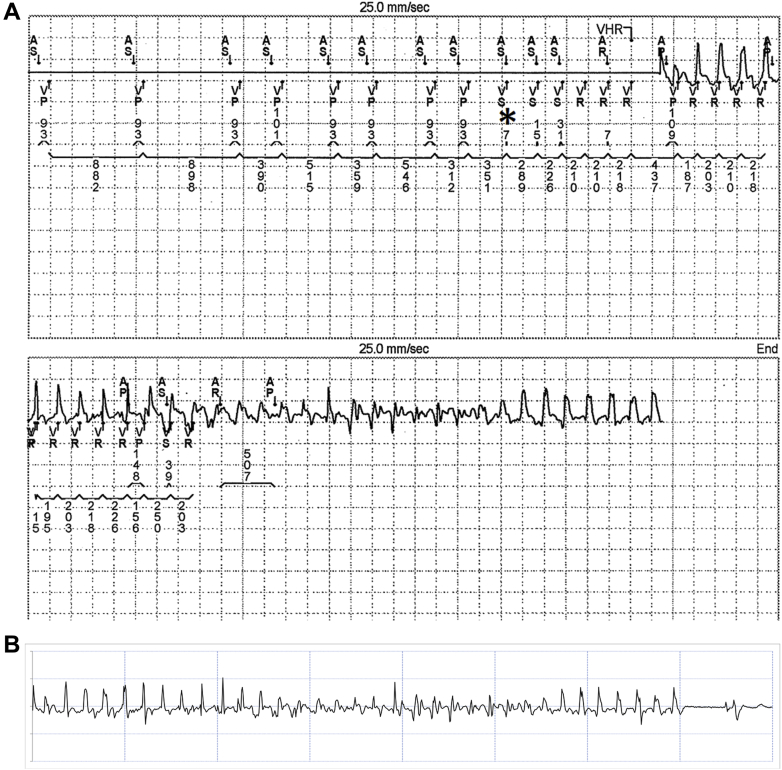
On the day of the syncopal event, she awoke uneventfully and went through her usual morning routine, including drinking a cup of coffee. She then went to the bathroom to defecate. After the bowel movement, she felt dizzy and her vision was going black. She tried to get up but collapsed to the floor. She hit her head on the counter but did not sustain a significant injury. By the time the patient’s mother arrived upstairs to the bathroom, the patient was standing up, but she was somewhat dizzy and confused. She gradually improved but remained light-headed and tired all day, although she was able to go out on a planned shopping trip. In view of the event and concern about a possible role of her pacemaker, she presented to our emergency department. Her vital signs and physical assessment were normal. Our service was called because of the presence of the pacemaker. Device interrogation showed normal function but detection of a brief run of PVT that coincided with the time of the syncopal event (Figure 1). The patient reported that she had been pushing herself quite hard lately, which was confirmed by her family. She was in her senior year and in the International Baccalaureate program. She was applying for admission to universities and was training for a half-marathon, running approximately 40 km/wk. Her echocardiogram continued to show normal function. The patient was admitted to the hospital for an upgrade of her pacemaker to an implantable defibrillator. This procedure was performed uneventfully, and the patient has been clinically well, with no therapies or recurrent syncopal episodes. Follow-up echocardiography and stress testing have been normal, showing no induced arrhythmia. A commercial 57 arrhythmia gene panel was negative.
Figure 1.
A: Interrogation strip from pacemaker showing an atrial sensed, ventricular paced rhythm with abrupt onset of polymorphic ventricular tachycardia (PVT) (asterisk marks first ventricular sensed event). The atrial rate is irregular, representing premature atrial complexes. The atrial sensed events following the asterisk likely represent far-field sensing of ventricular tachycardia by the atrial lead. B: Device-stored electrogram showing PVT with spontaneous termination after approximately 7 seconds.
Given the association of the patient’s syncopal episode with the autonomic maneuver, she was referred for autonomic function testing with noninvasive beat-to-beat blood pressure and electrocardiographic monitoring (Lead II: Finometer Pro, Finapres Medical Systems, Amsterdam, The Netherlands) acquired through LabChart (Powerlab 16/30, AD Instruments, Colorado Springs, CO). Her supine heart rate variability (autoregressive spectral analysis) was reduced in the very low (1798 ms2), low (672 ms2), and high (107 ms2) frequency ranges, but with a normal low frequency to high frequency ratio (6.3). This indicates reduced sympathetic and parasympathetic regulation of cardiac function; however, the balance between these 2 systems remains preserved. Cardiac vagal control was impaired. Cross-spectral analyses of systolic pressure and R-R interval data revealed normal baroreflex delay (2.2 seconds) but low sensitivity (3.8 ms/mm Hg). Heart rate responses to deep breathing (6 breaths/min) were small (±16 bpm).6 The QT variability index (determined using LabView 2009, National Instruments, Colorado Springs, CO) was -0.325, which is less negative than age-matched normal data7 and reflects increased susceptibility to ventricular arrhythmia. Heart rate and blood pressure responses to the Valsalva maneuver were within the normal ranges, but the blood pressure recovery time, a marker of adrenergic baroreflex sensitivity, was long (3.7 seconds), confirming impaired sympathetic baroreflex control. Finally, an active stand from the supine position revealed a borderline abnormal initial blood pressure decrease (−38/−19 mm Hg, compared to the clinical criteria for initial orthostatic hypotension of −40/−20 mm Hg), which was associated with light-headedness and accompanied by an excessive heart rate response (+50 bpm).8 The blood pressure decline recovered well within 3 minutes of standing, but the heart rate remained elevated (+40 bpm).
Discussion
The patient’s history is consistent with typical reflex syncope. Defecation is recognized as a relatively common trigger for reflex syncope, with events occurring during or immediately after the bowel movement.9 Defecation syncope is thought to be triggered by a Valsalva-like maneuver, although the condition is not always associated with straining.2 In 7 patients (mean age 62 years) with defecation syncope, sympathetic dysfunction was the predominant abnormality, although the patients also had parasympathetic dysfunction.9 This is compatible with our patient, in whom autonomic function testing revealed labile blood pressure, with orthostatic tachycardia and abnormal vagal and sympathetic baroreflex function. Unusually, in the present case, the event was associated with arrhythmia.
Ventricular arrhythmias have only rarely been associated with reflex syncope. In a report of 1374 tilt tests, there were no reports of PVT or ventricular fibrillation (VF) either during or immediately after tilt-induced syncope.10 This is in keeping with the many studies demonstrating the antifibrillatory effect of vagal stimulation, which tends to accompany reflex syncope.11 However, this may be an oversimplification. For example, episodes of arrhythmia in patients with Brugada syndrome most often occur during times of increased vagal tone, such as sleep and rest.12
Kataoka and colleagues13 reported a 25-year-old woman who experienced 3 suspected episodes of vasovagal syncope without prodrome. During tilt-table testing, she developed nonsustained ventricular tachycardia upon returning to the supine position. Another episode was triggered by failed venepuncture and was accompanied by nonsustained PVT and VF. For each episode, the syncope was preceded by ventricular ectopy, which seemed to be of right ventricular outflow tract origin. Ablation of the origin of her arrhythmia was curative of her syncope. The substrate for arrhythmia was likely modulated by the autonomic nervous system, with fairly typical triggers. Shenthar and colleagues14 reported the case of a 55-year-old man who experienced nonsustained VF during a head-up tilt test. Syncope occurred 5 minutes after administration of sublingual nitroglycerin and was associated with a 9-second sinus pause. VF began as the patient was being lowered to the supine position, and sinus rhythm returned after brief cardiac massage. Lepiece and colleagues15 reported a 62-year-old man who collapsed while giving a talk. He was initially asystolic. Cardiopulmonary resuscitation was administered, and cardiac activity soon resumed as a junctional escape rhythm. He then went into VF, which required defibrillation. Cardiac workup revealed no structural or functional cardiac abnormalities, and the event was considered vasovagal syncope leading to cardiac arrest. In the preceding reports, a prolonged period of bradycardia and/or hypotension may have been the trigger for PVT and VF. The previously reported patients also were older and more likely to have the substrate for an arrhythmia. In our patient, there was no possibility for asystole given the patient had a pacemaker, although hypotension was present based on the history. Certainly her blood pressure was labile based on autonomic function testing. We are limited by the lack of blood pressure data during the event and cannot prove that the episode was reflex mediated. However, the timing of the PVT in relation to the reflex syncope event likely is not coincidental. Although it can be argued that underlying heart block or the patient’s pacemaker lead could be a substrate for an arrhythmia, the triggering event seems to have been the autonomic activity during defecation, and the patient did demonstrate impaired cardiovascular autonomic function during laboratory testing.
The Canadian-led Cardiac Arrest Survivors with Preserved Ejection Fraction Registry (CASPER) is a registry of previously healthy individuals, both adult and pediatric, who experienced a SCA or sudden unexpected death (SUD).3 Approximately 50% of the cases in CASPER remain unexplained despite systematic evaluation. Within CASPER, 35% of the SCA survivors experienced syncopal episodes before their arrest. Patient and witness reports of sudden cardiac events often sound typical of reflex syncope but result in SCA or SUD. Drezner and colleagues4 reported 63 of their 87 young (mean age 16 years) SCA respondents experienced at least 1 cardiovascular symptom before arrest, with 30% experiencing presyncope and 18% experiencing syncope. Marijon and colleagues5 studied 839 SCA victims and found 51% experienced symptoms in the preceding month.
To our knowledge, ours is the first case of reflex syncope associated with PVT in an adolescent. We propose this case as a proof of concept that the profound cardiovascular autonomic changes that are associated with apparently benign reflex syncope in a young person may, in susceptible individuals, precipitate PVT and VF, with the potential of progressing to SCA. The high incidence of normal investigations of SCA in the young may be partially explained by this unusual case.
Conclusion
We present the case of a 17-year-old girl with concomitant complete heart block and anxiety disorder whose pacemaker recorded PVT at the time of a seemingly typical episode of reflex syncope immediately after defecation. This rare occurrence may represent a mechanism for SCA and SUD in the young for which no other etiology has been identified.
References
- 1.Sanatani S., Chau V., Fournier A., Dixon A., Blondin R., Sheldon R.S. Canadian Cardiovascular Society and Canadian Pediatric Cardiology Association position statement on the approach to syncope in the pediatric patient. Can J Cardiol. 2017;33:189–198. doi: 10.1016/j.cjca.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Adkisson W.O., Benditt D.G. Pathophysiology of reflex syncope: a review. J Cardiovasc Electrophysiol. 2017;28:1088–1097. doi: 10.1111/jce.13266. [DOI] [PubMed] [Google Scholar]
- 3.Krahn A.D., Healey J.S., Chauhan V. Systematic assessment of patients with unexplained cardiac arrest: Cardiac Arrest Survivors With Preserved Ejection Fraction Registry (CASPER) Circulation. 2009;120:278–285. doi: 10.1161/CIRCULATIONAHA.109.853143. [DOI] [PubMed] [Google Scholar]
- 4.Drezner J.A., Fudge J., Harmon K.G., Berger S., Campbell R.M., Vetter V.L. Warning symptoms and family history in children and young adults with sudden cardiac arrest. J Am Board Fam Med. 2012;25:408–415. doi: 10.3122/jabfm.2012.04.110225. [DOI] [PubMed] [Google Scholar]
- 5.Marijon E., Uy-Evanado A., Dumas F., Karam N., Reinier K., Teodorescu C., Narayanan K., Gunson K., Jui J., Jouven X., Chugh S.S. Warning symptoms are associated with survival from sudden cardiac arrest. Ann Intern Med. 2016;164:23–29. doi: 10.7326/M14-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Low P.A., Denq J.C., Opfer-Gehrking T.L., Dyck P.J., O'Brien P.C., Slezak J.M. Effect of age and gender on sudomotor and cardiovagal function and blood pressure response to tilt in normal subjects. Muscle Nerve. 1997;20:1561–1568. doi: 10.1002/(sici)1097-4598(199712)20:12<1561::aid-mus11>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 7.Baumert M., Porta A., Vos M.A., Malik M., Couderc J.P., Laguna P., Piccirillo G., Smith G.L., Tereshchenko L.G., Volders P.G. QT interval variability in body surface ECG: measurement, physiological basis, and clinical value: position statement and consensus guidance endorsed by the European Heart Rhythm Association jointly with the ESC Working Group on Cardiac Cellular Electrophysiology. Europace. 2016;18:925–944. doi: 10.1093/europace/euv405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freeman R., Wieling W., Axelrod F.B. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci. 2011;161:46–48. doi: 10.1016/j.autneu.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 9.Allan L., Johns E., Doshi M., Anne Kenny R., Newton J.L. Abnormalities of sympathetic and parasympathetic autonomic function in subjects with defaecation syncope. Europace. 2004;6:192–198. doi: 10.1016/j.eupc.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Li W., Wang C., Wu L.J., Hu C.Y., Xu Y., Li M.X., Lin P., Luo H.Y., Xie Z.W. [Arrhythmia after a positive head-up tilt table test] Zhonghua Xin Xue Guan Bing Za Zhi. 2010;38:805–808. [PubMed] [Google Scholar]
- 11.Ng G.A. Neuro-cardiac interaction in malignant ventricular arrhythmia and sudden cardiac death. Auton Neurosci. 2016;199:66–79. doi: 10.1016/j.autneu.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Franciosi S., Perry F.K.G., Roston T.M., Armstrong K.R., Claydon V.E., Sanatani S. The role of the autonomic nervous system in arrhythmias and sudden cardiac death. Auton Neurosci. 2017;205:1–11. doi: 10.1016/j.autneu.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Kataoka M., Takatsuki S., Tanimoto K., Akaishi M., Ogawa S., Mitamura H. A case of vagally mediated idiopathic ventricular fibrillation. Nat Clin Pract Cardiovasc Med. 2008;5:111–115. doi: 10.1038/ncpcardio1082. [DOI] [PubMed] [Google Scholar]
- 14.Shenthar J., Pujar D., Aravind Prabhu M., Sadashivappa Surhynne P. Ventricular fibrillation a rare complication during head-up tilt test. HeartRhythm Case Rep. 2015;1:363–365. doi: 10.1016/j.hrcr.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lepiece C., Dormal F., Blommaert D. Vasovagal syncope initiating ventricular fibrillation in a healthy subject. Acta Cardiol. 2013;68:635–638. doi: 10.1080/ac.68.6.8000012. [DOI] [PubMed] [Google Scholar]