Abstract
Background / Aims
The advent of mobile old age psychiatry intervention teams supports policies maintaining older adults in their habitual living environments, even those who are very old and suffering from acute cognitive and psychiatric impairments. Analyzing sociodemographic data, clinical and health characteristics, reasons for crisis-oriented psychiatric consultations, and other therapeutic suggestions for supporting home- or nursing home-dwelling older adult patients suffering from an onset of a psychiatric crisis.
Methods
Reviews of the medical records and discharge letters of home- or nursing home-dwelling older adults who had undergone a consultation with the Lausanne region's Mobile Old Age Psychiatry Teams (MOAPTs), between May 2016 and December 2017.
Results
Of 570 older adult patients referred for consultation with MOAPTs, 333 had medical records and discharge letters eligible for retrospective analysis (59%). The majority of these older adult patients were women aged over 80 years suffering from dementia, mood disorders with and without a risk of suicide, and delirium. Challenging behaviors related to different stages of cognitive impairment were the most important clinical reason for crisis consultations. Nonpharmacological and pharmacological treatments were delivered concurrently in 68% of crisis consultations.
Conclusion
Appropriate responses by dual nurse-psychiatrist teams using crisis-oriented nonpharmacological and pharmacological interventions decreased hospitalization.
Keywords: Liaison psychiatry, Crisis-oriented psychiatric interventions, Nurse, Geriatric psychiatrist, Dementia, Challenging behavior, Mood disorders, Pharmacological treatment, Nonpharmacological treatment
Introduction
The population aged 65 years and above is expected to grow by 56% worldwide between 2015 and 2030, with the fastest growth in urban areas [1]. There is no doubt demographic transition towards more aged societies increases the need for both informal and professional support and services for older adults (OAs) with multiple chronic conditions [2]. A significant proportion of those vulnerable OAs are at high risk of acute mental health problems, as they grow older. Epidemiological studies among OAs have revealed that the aging process is associated with more numerous psychiatric problems in the community and a huge need for care [3, 4, 5, 6]. In Switzerland, approximately one fifth of home-dwelling OAs and more than half of nursing home patients suffer from a moderate or severe mental disorder that expresses a challenging behavior caused by different stressors, geriatric syndromes, and pathological aging processes [7]. Acute psychiatric crises are common among OAs with cognitive and psychiatric impairment. However, diagnosis and treatment can pose significant challenges because of the high incidence of medical and neurological comorbidities, atypical symptomatology, psychosocial problems, polypharmacy and/or the adverse effects of medication, and a lack of knowledge about nonpharmacological and pharmacological treatments [8].
We developed the following description for psychiatric crises among home- and nursing home-dwelling OAs: “The appearance of new symptoms or the worsening of existing psychiatric clinical signs and symptoms based on healthcare professionals' unusual observations and perceptions (subjective feelings, appearance of the first signs and symptoms of a mental imbalance) and objectivized (using instruments and scales) in relation to the older adult's usual state of homeostasis.” The most common psychiatric emergencies in this population are delirium, depression with suicidality, substance abuse, and dementia accompanied by disturbing behavior (e.g., agitation or aggression) as a clinical manifestation of the behavioral and psychological symptoms of dementia (BPSD) [9]. Challenging behavior is considered as “culturally abnormal behavior of such an intensity, frequency or duration that the physical safety of the person or others is likely to be placed in serious jeopardy, or behavior which is likely to seriously limit use of, or result in the person being denied access to, ordinary community facilities” [10].
The systematic review of Reilly et al. [11] found some evidence that rapid psychiatric interventions among home-dwelling OAs with BPSP were useful for improving certain outcomes, both for the person and their informal and formal caregivers. They suggested that admissions and readmissions to emergency departments and acute care hospitals, in addition to overall healthcare costs, were reduced in the medium term and could delay institutionalization in nursing homes.
The canton of Vaud's Public Health Service, in collaboration with Lausanne University Hospital's Service of Old Age Psychiatry, has developed a community-based pathway for managing psychiatric crisis situations in the place of residence of home- and nursing home-dwelling OAs. The Mobile Old Age Psychiatry Teams (MOAPTs) began to prescribe nonpharmacological and pharmacological treatment approaches and, when necessary, hospitalization to manage acute psychiatric disorders, to referring physicians and nursing staff. Sampson et al. [12] showed that 42% of individuals aged over 70 who experienced an unplanned admission to an acute care hospital had dementia; this rose to 48% among those aged over 80. A systematic review of crisis intervention teams for OAs with mental health problems concluded that they were likely to reduce the number of acute care admissions [13]. The present work will explore the following questions. Why were home- and nursing home-dwelling OA patients referred to an MOAPT consultation? What kinds of nonpharmacological and pharmacological therapeutic approaches were suggested to the referring physicians? What proportion of the OAs consulted were hospitalized? Was there a relationship between hospitalization and the sociodemographic characteristics and health statuses of home- and nursing home-dwelling OA patients?
Materials and Methods
Design
The study used a systematic retrospective sampling of data retrieved from eligible patients' medical records and discharge letters based on the methodology of Vassar and Holzman [14].
Population and Selection Criteria
We included all OA patients living at home or in a nursing home who were referred for a crisis-oriented consultation by their family practitioner or a specialized physician in the Lausanne region. The observation period ran from April 2016 to December 2017. Patients' medical records and discharge letters were eligible for inclusion if patients were at least 65 years old and accepting nonpharmacological and pharmacological treatments regimens.
Interventions
Following referrals by a family practitioner or a specialized physician, a team composed of a psychiatric nurse and a geriatric psychiatrist provided psychiatric consultations for home- or nursing home-dwelling OA patients with acute mental health problems. Interventions were based on the principle that as soon as signs and symptoms become manifest, it is best to treat patients' psychiatric disorders in their own living environment in order not to disrupt the patient's family or community ties, and to mobilize the family and every means of community healthcare support available. Nonpharmacological and pharmacological psychiatric interventions were chosen based on best practices documented in systematic reviews and the evidence-based recommendations of Kales et al. [15], Tible et al. [16], and Cohn-Mansfield [17]. Recommendations to prefer nonpharmacological interventions to pharmacological ones were based on the literature [15, 18, 19]. Nonpharmacological interventions also aimed to orient and organize care with and for the patient and the caregivers in order to prevent admission to a psychiatric hospital or shorten the time spent there. Pharmacological interventions were suggested, if needed, using antidementia drugs, antidepressants, antipsychotics, mood stabilizers, and benzodiazepines [16, 20]. It was not the crisis-oriented psychiatric intervention's aim to make hospitalization unnecessary [8].
Clinical Determinants
We developed a new tool for documenting the subjective and objective psychiatric signs and symptoms based on literature review in the absence of an existing tool demonstrating onset, signs, and symptoms of acute psychiatric crises among home- and nursing home-dwelling OA patients [16, 21, 22, 23]. The tool is filled in by the requesting healthcare providers (family practitioner, specialist physician, and/or nursing staff) and attached to the form requesting a crisis-oriented intervention.
Mental Assessment Instruments
Where appropriate and indicated, the intervention teams documented the mental and physiological statuses of older adult patients using the following French language-validated physical and mental assessment tools.
Data Collection Procedure
Data were extracted from the eligible patients' medical records and discharge letters according to procedural guidelines. Data were entered into the database and checked for plausibility and completeness. All data from patient discharge letters were retrieved, from February to June 2018, using a standardized extraction sheet. Sample size respected best practices, using variables that were available in at least 10 patients' medical records [24]. The data retrieved included: year of consultation, sociodemographic characteristics, place of domicile/consultation, reasons for the crisis-oriented consultation, primary diagnosis, number of somatic and psychiatric comorbidities, and number of consultations, nonpharmacological and pharmacological interventions, and hospitalizations.
Statistical Analysis
Descriptive statistics were analyzed to describe the sociodemographic, clinical, and health characteristics of the older adult patients. Means, medians, and standard deviations were calculated where appropriate. The χ2 test or Fisher's exact test were calculated to explore differences between categorical data (sociodemographic and clinical characteristics, year of consultation, and place of residence). Parametric and nonparametric statistics were considered to explore associations between sociodemographic and clinical characteristics, proposed therapeutic approaches, consultation frequency, and orientation (Spearman's rank correlation). Results were considered statistically significant when p < 0.05. Statistical analyses were performed using the IBM Statistical Package for the Social Sciences – SPSS 25.0 [25].
Results
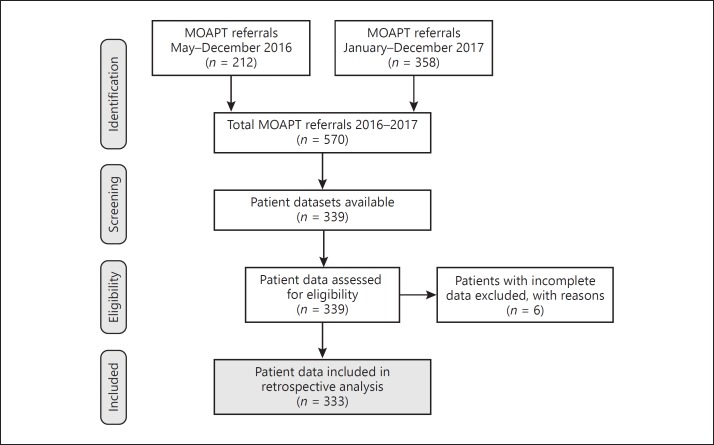
Of the total sample of 570 patients referred to the Lausanne's region MOAPTs, 333 medical records and discharge letters (58%) met the eligibility criteria for analysis using the standardized extraction sheet (Fig. 1). Of the 333 patient datasets examined for eligibility, 97 were from 2016 and 236 were from 2017. The difference is explainable because the MOAPTs were only launched in May 1, 2016 (Fig. 1).
Fig. 1.
Flowchart with the selection procedure using patient medical records and discharge letters for retrospective analysis.
Sociodemographic Characteristics
Women composed the majority of the sample (233; 70%), with an overall average age of 83.9 years (SD = 8.2), and most OAs were living in their own homes (55%). No significant differences were found between the year of consultation and age, sex, place of consultation, and the place of residence/consultation (p = 0.141) (Table 1). However, a significant difference was found between the age average and the place of residence/consultation (p = 0.004; at home = 82.6 years; nursing home = 84.1 years; clinics = 77.0 years).
Table 1.
Baseline sociodemographic characteristics for 2016 and 2017
| Baseline variable | 2016 (n = 97) | 2017 (n = 236) | p valuea |
|---|---|---|---|
| Age, years | 0.146 | ||
| Mean ± SD | 83.9±6.7 | 82.5±8.8 | |
| Min–Max | 66–100 | 65–101 | |
| Sex, n (%) | 0.116 | ||
| Female | 74 (76) | 159 (67) | |
| Male | 23 (24) | 77 (33) | |
| Place of consultation, n (%) | 0.382 | ||
| Nursing home | 40 (41) | 96 (41) | |
| At home | 55 (57) | 127 (54) | |
| Clinics | 2 (2) | 13 (5) |
χ2 test.
Health Status and Comorbidities
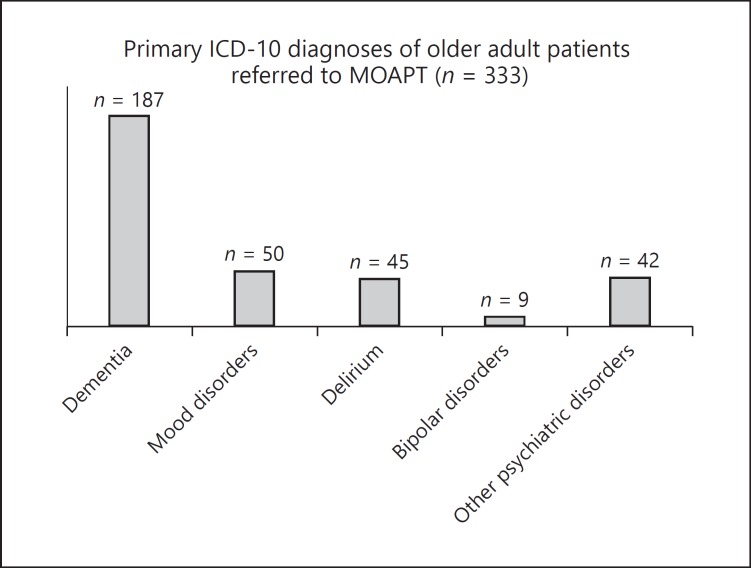
Based on the ICD-10, the majority of the OA patients were suffering from dementia (n = 187; 57%), followed by mood disorders (n = 50; 15%) with or without suicidal clinical signs and symptoms, delirium alone or superimposed on dementia (n = 45; 13%), bipolar disorders (n = 9; 3%), and other psychiatric disorders (n = 42; 13%) (Fig. 2). Other psychiatric disorders included alcohol and drug addiction, schizophrenia, general anxiety, and personality disorders. No significant differences were found between primary diagnoses and sex (p = 0.870), place of residence/consultation (p = 0.05), and year of intervention (p = 0.118).
Fig. 2.
Diagnoses of the home- and nursing home-dwelling patients referred to an MOAPT (n = 333).
An average of 7–8 comorbidities was documented in their medical records or discharge letters (mean = 7.6; SD = 4.5). There was no difference in the average number of comorbidities found between patients consulted in 2016 and 2017 (p = 0.089), men and women (p = 0.726), and home- and nursing home-dwelling OA patients (p = 0.376). In 7% (n = 23) of patient data, no comorbidities were documented.
Reason for Crisis-Oriented Consultation
Almost 9 out of 10 of the MOAPT consultations occurred following manifestations of challenging behaviors (or behavioral and psychological symptoms of dementia: BPSD) (n = 286; 86%) versus about 1 in 10 for nonchallenging acute psychiatric disorders and assessments (n = 47; 14%). Among those patients displaying challenging behavior, 190 exhibited disruptive behavior in the form of agitation, verbal and/or physical aggression, and resistance to care (66%), 29 presented symptoms of mood disorders and apathy with or without suicidal behavior (10%), and 20 presented with full-blown delirium (7%). Bearing in mind that most clinical manifestations are multidimensional and multifactorial, our analyses considered the dominant clinical features/symptoms. Of the remaining 47 OA patients with a nonchallenging behavior, 29 (62%) referrals to the MOAPT were for cognitive assessments of mental impairment among home-dwelling OAs, with and without a request for pharmacological treatment adaptation, 12 (26%) were for psychiatric assessments for different reasons (26%), and 6 were requests for an MOAPT to resolve conflicts between OA patients and family members and/or healthcare providers. No difference was observed between the places of residence/consultation (homes, nursing homes, and clinics; p = 0.627).
Interventions
The sample of 333 OA patients underwent 883 interventions during the investigation period, ranging from 1 to 17 per person. A mean of 2.7 interventions per person was recorded in both years (SD = 2.6; median 2.0). No significant differences were observed between men and women (p = 0.218), place of intervention/consultation (p = 0.615), and challenging behavior versus nonchallenging behavior (p = 0.261). However, one significant difference was the higher average number of interventions in 2016 than in 2017 (3.6 vs. 2.3; p ≤ 0.001). A moderate negative correlation was found between challenging behavior and the number of interventions, with a higher number of interventions among home- and nursing home-dwelling OAs with challenging behavior (r = −0.158; p ≤ 0.001).
Nonpharmacological and/or Pharmacological Prescriptions and Hospitalizations
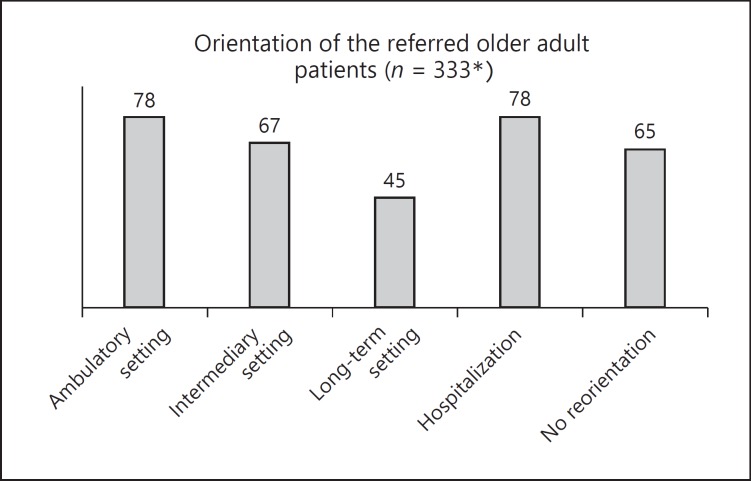
Reinforcing medical and nursing care and behavioral therapy were the nonpharmacological interventions most frequently suggested by the MOAPTs; environmental and social contact interventions were proposed less often (Table 2). One fifth of the subjects (n = 65; 20%) did not need reorientation and remained in their place of consultation/residence (home, nursing home). A consequent proportion was prescribed hospitalization (n = 76; 22%), 78 OA patients (23%) were prescribed regular visits to an ambulatory setting (day hospital, community health care centers); 45 were prescribed long-term institutional settings (13%; nursing homes), 67 were prescribed intermediary settings (20%; temporary rehabilitation units), and 2 patients died (Fig. 3).
Table 2.
Nonpharmacological and pharmacological approaches prescribed by MOAPTs
| Therapeutic approaches | CHC/patient's home | Nursing homes | Clinics | Total | p value | Challenging behavior | Nonchallenging behavior | p value |
|---|---|---|---|---|---|---|---|---|
| Nonpharmacological optionsa | ||||||||
| Sensorial interventions | 4 | 2 | 0 | 7 | 7 | 0 | ||
| Structured activities | 27 | 15 | 2 | 44 | 41 | 3 | ||
| Physical activities | 0 | 2 | 0 | 0 | <0.000* | 2 | 0 | 0.235 |
| Social contacts | 3 | 2 | 0 | 5 | 2 | 3 | ||
| Environmental interventions | 1 | 5 | 0 | 6 | 6 | 0 | ||
| Behavioral therapy | 22 | 49 | 5 | 76 | 66 | 10 | ||
| Reinforced medical and nursing care | 68 | 14 | 3 | 85 | 72 | 13 | ||
| Psychotherapeutic therapy | 27 | 15 | 1 | 43 | 39 | 4 | ||
| None | 30 | 30 | 4 | 64 | 50 | 14 | ||
| Pharmacological optionsb | ||||||||
| Antidementia drug | 1 | 0 | 0 | 1 | 1 | 0 | ||
| Introduction/adaptation antidepressants | 15 | 9 | 1 | 25 | 21 | 4 | ||
| Introduction/adaptation antipsychotics | 108 | 91 | 10 | 189 | 0.525 | 191 | 16 | 0.004* |
| Introduction/adaptation mood stabilizers | 4 | 2 | 1 | 7 | 7 | 0 | ||
| Introduction/adaptation benzodiazepines | 0 | 2 | 0 | 2 | 2 | 0 | ||
| No prescription proposed | 54 | 32 | 3 | 89 | 64 | 23 | ||
| Combined options | ||||||||
| Nonpharmacological approaches | 30 | 11 | 1 | 42 | 31 | 11 | ||
| Pharmacological treatment | 7 | 11 | 2 | 20 | 0.184 | 18 | 2 | 0.006* |
| Nonpharmacological and pharmacological proposition | 122 | 94 | 10 | 226 | 205 | 21 | ||
| No prescriptionc | 23 | 20 | 2 | 45 | 32 | 13 | ||
Fig. 3.
Orientation of MOAPT patients. * Two patients died during the intervention period.
No significant differences were found between men and women (p = 0.424), challenging or nonchallenging behaviors (p = 0.902), and the primary diagnosis (p = 0.188). One significant difference was observed in the orientation given to nursing home residents and home-dwelling OAs (p ≤ 0.001), and another one was between patients with and without dementia (p = 0.026). MOAPTs suggested that more than half of OA patients introduce/adapt antipsychotropic medication, and a fraction received advice to reinforce or introduce/adapt antidepressants. Almost one third of the crisis-oriented consultations resulted in no medication being prescribed (Table 2). Of the analyzed sample, 226 (68%) OA patients were prescribed a dual nonpharmacological and pharmacological treatment approach, 42 (13%) were prescribed solely nonpharmacological approaches, 20 (6%) were prescribed solely pharmacological treatments, and 45 (13%) received neither pharmacological nor nonpharmacological treatment and were immediately hospitalized. No statistical differences were found between patients' homes, nursing homes, and clinics with regard to what patients were proposed therapeutically (p = 0.184). However, a significant difference was observed between challenging behavior and nonchallenging behavior (p = 0.006), with higher proportions of nonpharmacological and pharmacological therapeutic approaches for OAs with challenging behavior. OAs suffering from dementia, delirium, and mood disorders received more combined approaches than those with other primary psychiatric diagnoses (p = 0.018). A moderate positive correlation was found between the orientation suggested for home- or nursing home-dwelling OAs and their place of residence/consultation (r = 0.271; p ≤ 0.001)
Of the 76 hospitalizations in the acute Service Old Age Psychiatry (SUPAA), 47 were home dwelling, 27 lived in nursing homes, and 2 came from clinics. No difference was found between those with challenging and nonchallenging behavior (p = 0.837). However, home- and nursing home-dwelling OA patients with dementia were significantly more frequently hospitalized than those with other psychiatric diagnoses (p ≤ 0.001). Hospitalization was prescribed for 25 men (33%) and 51 women (67%), with no significant difference between home- and nursing home-dwelling OAs (p = 0.135).
Discussion
To the best of our knowledge, this retrospective study was the first to examine a selected number of clinical interventions delivered by dual nurse-psychiatrist teams taking care of home- and nursing home-dwelling OAs suffering from an onset of psychiatric disorders. Cognitively impaired female OAs aged 80 years or more were shown to be a vulnerable subgroup for onset of psychiatric crises, with their challenging behavior being an important reason for requesting interventions by MOAPTs, as was their risk of being admitted to hospital. An onset of a psychiatric crisis is expressed in the form of disruptive behavior, such as agitation or verbal and physical aggression, which critically destabilizes informal and formal caregivers and requires the assistance of a specialized old age psychiatry team formed by a nurse and a psychiatrist. This is not surprising and indeed was reported previously in publications by Toot et al. [26] and Ebbing [27] as the most important reason for asking for medical and social support for cognitively impaired OAs in different types of accommodation. Moreover, clinical manifestations of disruptive behaviors underscore the need for rapid, multiprofessional, patient-centered interventions which involve calming the psychiatric distress of cognitively impaired OAs and supporting their informal caregivers, as confirmed by Zwijsen et al. [28] in their study among home-dwelling OAs suffering from BPSD. Our findings showed that home- and nursing home-dwelling OA patients suffering from dementia were highly at risk of an onset of a psychiatric crisis, such as agitation and aggressive behavior, and this for different somatic and psychiatric reasons. This has been confirmed by multiple authors exploring BPSD in the community and nursing homes [29, 30]. Our findings showed that BPSD were almost universally present in the home- and nursing home-dwelling OA patients with challenging behavior who were referred for MOAPT interventions. Indeed, the majority had multiple symptoms, and these were frequently the reason for requesting those interventions. However, our findings also demonstrated the problem of defining exactly which situations or events constitute psychiatric crises, and how they become crises because of individual perceptions or reactions to an event or stimulus, rather than because of the event itself. During the mental imbalance of a crisis, an OA is more susceptible to overstimulation by others than during periods of stable functioning [31, 32]. Crisis interventions can also have particular connotations due to the deliberate use of a crisis to effect change, and interventions can be great opportunities to expose unsustainable care situations [33]. This is of particular importance in dementia care situations, where the crisis may be experienced by multiple different individuals and where the emphasis is not on unresolved conflicts but rather on the issues affecting caregiving systems [34].
An important part of the intervention requests was made to assess cognitive impairment and/or cognitive discernment (nonchallenging behavior) among home-dwelling OAs. This underpins the hypothesis that healthcare providers have a diverse understanding of the meaning and definition of psychiatric crises among home-dwelling OAs. Furthermore, it may also reveal that other healthcare services are functioning suboptimally and that the immediate availability of a dual nurse-psychiatrist team corresponds better with community-based care needs, as already suggested by Jeste et al. [35]. This position was underlined by Toot et al. [26], who revealed the various definitions of crisis interventions used by home crisis intervention teams. Psychiatric crisis intervention aims to reduce inappropriate hospital admissions and maximize the ability of healthcare service users to live independently in their homes. To do this, the nurse-psychiatrist MOATP delivered a certain number of interventions. Our findings showed extremely heterogeneous results with regard to the number of interventions among home- and nursing home-dwelling OAs, with moderate associations between those with and without challenging behavior. However, we found no other research exploring the effectiveness of the number of interventions needed to prevent hospitalization among home- or nursing home-dwelling OAs during an onset of a psychiatric disorder. Further research will be necessary to discover whether or how the relationship between the reason for crisis interventions and their number can prevent hospitalization.
Since the majority of intervention requests concern home- and nursing home-dwelling OAs with challenging behavior, it is not surprising that a significant proportion of treatment prescriptions suggested combining nonpharmacological and pharmacological approaches. Although many authors recommend nonpharmacological best practice approaches for challenging behavior [15, 36], our findings showed that nonpharmacological and pharmacological approaches were prescribed simultaneously to calm onset of a psychiatric crisis disorder. Our findings also stressed the importance of considering the distress caused to OA patients by changes in their living environment and of maintaining a vision of separate nonpharmacological and pharmacological interventions.
A substantial proportion of the requests for a crisis intervention did not result in any nonpharmacological or pharmacological prescription by the MOAPT. This would certainly differ depending on whether one is a family member living permanently with a person with cognitive impairment or a nurse practitioner or physician visiting a home- or nursing home-dwelling OA in psychiatric crisis once or twice a week. Referral for a potential psychiatric crisis may also be prompted by greater awareness of dementia/cognitive impairment or changes in an OA's personality, behavior, social or economic situation, the initial impact of which may be internalized by those involved without any immediate need of nonpharmacological or pharmacological prescriptions. Recently published recommendations of good practices for dealing with challenging behavior and BPSD support this therapeutic approach [16, 37, 38, 39]. They suggest, as expressed by Kumfor et al. [40], that a biographical understanding of the OA is important to understanding and working with a crisis interpreted within the context of that person's life. Dealing with a psychiatric crisis should thus not only consider the diagnosis, prognosis, and the changes in behavior, personality, or relationships that caused it but also the perceptions of those involved. These, in turn, are contingent on a multitude of other factors, including personality, relationship history and quality, attitudes, coping strategies, and values [41]. Crisis recognition by persons not experiencing this mental distress suggests that crises can be understood intersubjectively and that a degree of consensus can develop in which one individual can anticipate the actions and responses of another. An individual undergoing the changes associated with dementia/cognitive impairment may be considered by informal and formal caregivers to be in crisis, as might the person caring for that individual. An individual whose OA partner has become forgetful but has no diagnosed syndrome, although the individual feels a sense of despair and display symptoms of anxiety, may not evoke the same degree of sympathy and support as a formal caregiver of someone diagnosed with dementia. Normative concepts of behavior may lead to eligibility criteria being used to limit access to services that can alleviate crises, thereby unwittingly leading to a maladaptive response [42, 43].
Although a substantial proportion of the referred home- and nursing home-dwelling OAs were still hospitalized in our acute hospital's Service of Old Age Psychiatry, the proportion of OAs living in nursing homes and the duration of hospitalizations showed a tendency towards a decrease compared with previous periods. More research is needed to explore the effectiveness of nurse-psychiatrist MOAPTs and their impact on hospitalization rates and the circumstances of hospitalization.
Statement of Ethics
The Internal Review Board of Lausanne University Hospital's Service of Old Age Psychiatry approved this project. It also fulfils the provisions of the Declaration of Helsinki.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was received.
Author Contributions
E.G.P. and K.E. are the guarantors, and all the authors contributed to drafting the original research. All authors contributed to the development of the selection criteria, data extraction, and analysis.
References
- 1.Affairs UNDoEaS: World Population Aging 2015. In: UNO. Edited by UNDESA, vol. Report No.: ST/ESA/SER.A/390 Geneva; 2015.
- 2.Moreau A. Perspectives de population 2015–2040, Vaud et ses régions. Lausanne: Département des finances et des relations extérieures. 2016 [Google Scholar]
- 3.Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016 May;387((10033)):2145–54. doi: 10.1016/S0140-6736(15)00516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maurice J. WHO puts healthy ageing on the front burner. Lancet. 2016 Jan;387((10014)):109–10. doi: 10.1016/S0140-6736(15)01365-3. [DOI] [PubMed] [Google Scholar]
- 5.Dening T, Barapatre C. Mental health and the ageing population. J Br Menopause Soc. 2004 Jun;10((2)):49–53. doi: 10.1258/136218004774202346. [DOI] [PubMed] [Google Scholar]
- 6.Karlin B, D Fuller J. 62; 2007. Meeting the mental health needs of older adults, vol. [PubMed] [Google Scholar]
- 7.Weber R, Abel B, Ackermann G, Biedermann A, Burgi F, Kessler C, et al. Promotion Santé Suisse, Rapport 5. Berne, Lausanne: Promotion Santé Suisse; 2016. Santé et qualité de vie des personnes âgées. Bases pour les programmes d'action cantonaux; p. p. 143. [Google Scholar]
- 8.Wheeler C, Lloyd-Evans B, Churchard A, Fitzgerald C, Fullarton K, Mosse L, et al. Implementation of the Crisis Resolution Team model in adult mental health settings: a systematic review. BMC Psychiatry. 2015 Apr;15((1)):74. doi: 10.1186/s12888-015-0441-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abrams RC, Boné B, Reid MC, Adelman RD, Breckman R, Goralewicz R, et al. Psychiatric assessment and screening for the elderly in primary care: design, implementation, and preliminary results. J Geriatr. 2015;2015:792043. doi: 10.1155/2015/792043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emerson E, Einfeld LS. Challenging behaviour. Cambridge: Cambridge University Press; 2011. https://doi.org/10.1017/CBO9780511861178 [Google Scholar]
- 11.Reilly S, Miranda-Castillo C, Malouf R, Hoe J, Toot S, Challis D, Orrell M. Case management approaches to home support for people with dementia. Cochrane Database of Syst Rev. 2015 Jan 5;1 doi: 10.1002/14651858.CD008345.pub2. CD008345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry. 2009 Jul;195((1)):61–6. doi: 10.1192/bjp.bp.108.055335. [DOI] [PubMed] [Google Scholar]
- 13.Toot S, Devine M, Orrell M, Toot S, Devine M, Orrell M. The effectiveness of crisis resolution/home treatment teams for older people with mental health problems: a systematic review and scoping exercise. Int J Geriatr Psychiatry. 2011 Dec;26((12)):1221–30. doi: 10.1002/gps.2686. [DOI] [PubMed] [Google Scholar]
- 14.Vassar M, Holzmann M. The retrospective chart review: important methodological considerations. J Educ Eval Health Prof. 2013 Nov;10:12. doi: 10.3352/jeehp.2013.10.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kales HC, Gitlin LN, Lyketsos CG, Detroit Expert Panel on Assessment and Management of Neuropsychiatric Symptoms of Dementia Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel. J Am Geriatr Soc. 2014 Apr;62((4)):762–9. doi: 10.1111/jgs.12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tible OP, Riese F, Savaskan E, von Gunten A. Best practice in the management of behavioural and psychological symptoms of dementia. Ther Adv Neurol Disorder. 2017 Aug;10((8)):297–309. doi: 10.1177/1756285617712979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen-Mansfield J. Nonpharmacologic treatment of behavioral disorders in dementia. Curr Treat Options Neurol. 2013 Dec;15((6)):765–85. doi: 10.1007/s11940-013-0257-2. [DOI] [PubMed] [Google Scholar]
- 18.Gerlach LB, Kales HC. Managing Behavioral and Psychological Symptoms of Dementia. Psychiatr Clin North Am. 2018 Mar;41((1)):127–39. doi: 10.1016/j.psc.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 19.Maust DT, Kales HC. Medicating Distress. JAMA Intern Med. 2017 Jan;177((1)):42–3. doi: 10.1001/jamainternmed.2016.7528. [DOI] [PubMed] [Google Scholar]
- 20.Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ. 2015 Mar;350:h369. doi: 10.1136/bmj.h369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cerejeira J, Lagarto L, Mukaetova-Ladinska EB. Behavioral and psychological symptoms of dementia. Front Neurol. 2012 May;3:73. doi: 10.3389/fneur.2012.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen-Mansfield J, Thein K, Marx MS, Dakheel-Ali M, Jensen B. Sources of Discomfort in Persons with Dementia: Scale and Initial Results. Behav Neurol. 2015;2015:732832. doi: 10.1155/2015/732832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cummings JL. The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology. 1997 May;48((5 Suppl 6)):S10–6. doi: 10.1212/wnl.48.5_suppl_6.10s. [DOI] [PubMed] [Google Scholar]
- 24.Shaughnessy AF. Clinical Epidemiology: A Basic Science for Clinical Medicine. BMJ. 2007;335((7623)):777–777. [Google Scholar]
- 25.SPSS . Statistical Package for Social Sciences 22.0 - IBM. Somer (NY): IBM Corporation; 2011. [Google Scholar]
- 26.Toot S, Hoe J, Ledgerd R, Burnell K, Devine M, Orrell M. Causes of crises and appropriate interventions: the views of people with dementia, carers and healthcare professionals. Aging Ment Health. 2013;17((3)):328–35. doi: 10.1080/13607863.2012.732037. [DOI] [PubMed] [Google Scholar]
- 27.Ebbing K. Symptômes comportementaux et psychologiques dans les démences: quelles alternatives à la pharmacothérapie? Rev Med Suisse. 2016 Apr;12((515)):786–9. [PubMed] [Google Scholar]
- 28.Zwijsen SA, Gerritsen DL, Eefsting JA, Hertogh CM, Pot AM, Smalbrugge M. The development of the Grip on Challenging Behaviour dementia care programme. Int J Palliat Nurs. 2014 Jan;20((1)):15–21. doi: 10.12968/ijpn.2014.20.1.15. [DOI] [PubMed] [Google Scholar]
- 29.Tropea J, LoGiudice D, Kelly L. People with dementia in the emergency department: Behavioural symptoms and use of restraint. Emergency Medicine Australasia. 2017 Oct;29((5)):605–6. doi: 10.1111/1742-6723.12838. [DOI] [PubMed] [Google Scholar]
- 30.Zhao QF, Tan L, Wang HF, Jiang T, Tan MS, Tan L, et al. The Prevalence of Neuropsychiatric Symptoms in Alzheimer's Disease: Systematic Review and Meta-analysis. J Affect Disord. 2015 doi: 10.1016/j.jad.2015.09.069. [DOI] [PubMed] [Google Scholar]
- 31.Black BS, Johnston D, Rabins PV, Morrison A, Lyketsos C, Samus QM. Unmet needs of community-residing persons with dementia and their informal caregivers: findings from the maximizing independence at home study. J Am Geriatr Soc. 2013 Dec;61((12)):2087–95. doi: 10.1111/jgs.12549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peeters JM, Van Beek AP, Meerveld JH, Spreeuwenberg PM, Francke AL. Informal caregivers of persons with dementia, their use of and needs for specific professional support: a survey of the National Dementia Programme. BMC Nurs. 2010 Jun;9((1)):9. doi: 10.1186/1472-6955-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alvira MC, Risco E, Cabrera E, Farré M, Rahm Hallberg I, Bleijlevens MH, et al. RightTimePlaceCare Consortium The association between positive-negative reactions of informal caregivers of people with dementia and health outcomes in eight European countries: a cross-sectional study. J Adv Nurs. 2015 Jun;71((6)):1417–34. doi: 10.1111/jan.12528. [DOI] [PubMed] [Google Scholar]
- 34.Parker J. Crisis intervention: A practice model for people who have dementia and their Carers. Practice. 2007;19((2)):115–26. [Google Scholar]
- 35.Jeste DV, Alexopoulos GS, Bartels SJ, Cummings JL, Gallo JJ, Gottlieb GL, et al. Consensus statement on the upcoming crisis in geriatric mental health: research agenda for the next 2 decades. Arch Gen Psychiatry. 1999 Sep;56((9)):848–53. doi: 10.1001/archpsyc.56.9.848. [DOI] [PubMed] [Google Scholar]
- 36.Maust DT, Kales HC. Bringing Precision Medicine to the Management of BPSD. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2017;25((5)):469–470. doi: 10.1016/j.jagp.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 37.Barry HE, Cooper JA, Ryan C, Passmore AP, Robinson AL, Molloy GJ, et al. Potentially Inappropriate Prescribing Among People with Dementia in Primary Care: A Retrospective Cross-Sectional Study Using the Enhanced Prescribing Database. J Alzheimers Dis. 2016 Apr;52((4)):1503–13. doi: 10.3233/JAD-151177. [DOI] [PubMed] [Google Scholar]
- 38.Eichler T, Thyrian JR, Hertel J, Richter S, Wucherer D, Michalowsky B, et al. Unmet Needs of Community-Dwelling Primary Care Patients with Dementia in Germany: prevalence and Correlates. J Alzheimers Dis. 2016;51((3)):847–55. doi: 10.3233/JAD-150935. [DOI] [PubMed] [Google Scholar]
- 39.Miranda-Castillo C, Woods B, Orrell M. The needs of people with dementia living at home from user, caregiver and professional perspectives: a cross-sectional survey. BMC Health Serv Res. 2013 Feb;13((1)):43. doi: 10.1186/1472-6963-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kumfor F, Teo D, Miller L, Lah S, Mioshi E, Hodges JR, et al. Examining the Relationship Between Autobiographical Memory Impairment and Carer Burden in Dementia Syndromes. J Alzheimers Dis. 2016;51((1)):237–48. doi: 10.3233/JAD-150740. [DOI] [PubMed] [Google Scholar]
- 41.Polenick CA, Sherman CW, Birditt KS, Zarit SH, Kales HC. Purpose in Life Among Family Care Partners Managing Dementia: Links to Caregiving Gains. Gerontologist. 2018 Jun; doi: 10.1093/geront/gny063. https://doi.org/10.1093/geront/gny063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Palm R, Jünger S, Reuther S, Schwab CG, Dichter MN, Holle B, et al. People with dementia in nursing home research: a methodological review of the definition and identification of the study population. BMC Geriatr. 2016 Apr;16((1)):78. doi: 10.1186/s12877-016-0249-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Palm R, Köhler K, Bartholomeyczik S, Holle B, Assessing the application of non-pharmacological interventions for people with dementia in German nursing homes feasibility and content validity of the dementia care questionnaire (DemCare-Q) BMC Res Notes. 2014 Dec;7((1)):950. doi: 10.1186/1756-0500-7-950. [DOI] [PMC free article] [PubMed] [Google Scholar]