Abstract
Background: Most women will experience uterine fibroids by the age of 50, yet few data exist describing the overall patient experience with fibroids. The objective of this population-based survey was to characterize symptom burden, patient awareness, and treatment decision-making for fibroids, including a comparison among women of varying backgrounds.
Materials and Methods: Women (≥18 years) were recruited via email from GfK KnowledgePanel®, a representative panel of US households, or identified with opt-in consumer panels. The Uterine Fibroid Symptom and Health-Related Quality of Life (UFS-QOL) questionnaire and Aberdeen Menorrhagia Severity Scale (AMSS) were included.
Results: Eligible women were grouped into three cohorts: “at-risk” (symptoms suggestive of fibroids without clinical diagnosis, n = 300), “diagnosed” (n = 871), and fibroid-related “hysterectomy” (n = 272). Cohort and intracohort race/ethnicity and income analyses revealed differences in symptom burden, awareness/perception, and treatment history. Based on UFS-QOL scores, at-risk women reported significantly greater symptom severity and decreased health-related QOL versus diagnosed women; Hispanic women reported greater symptom severity versus white and black women. At-risk women also reported heavy menstrual bleeding and significant impact on work productivity. Among diagnosed women, 71% used pharmacologic therapy for symptom relief, and 30% underwent surgical or procedural treatment. Initial discussions with healthcare providers significantly impacted treatment outcomes; the hysterectomy cohort was most likely to first discuss hysterectomy.
Conclusions: Women with fibroids or symptoms suggestive of fibroids experience significant distress that reduces QOL, particularly racial minorities and women in lower income brackets. Survey results suggest that many women are likely undiagnosed, underscoring the need for improved awareness and education.
Keywords: : uterine fibroids, quality of life, burden, work, race/ethnicity, health disparities
Introduction
Uterine fibroids are the most common benign pelvic tumors in women,1 although prevalence may be underestimated due to asymptomatic women. Prevalence estimates range from 4.5% to 68.6% depending on study population and diagnostic methodology.2 Fibroid risk factors include race, age, family history, time since last birth, premenopausal state, hypertension, and diet.2,3 Based on ultrasonography, the estimated cumulative incidence of fibroids in women ≤50 years is significantly higher for black (>80%) versus white women (∼70%).4
Approximately 25% to 50% of women with fibroids are symptomatic, experiencing heavy menses, reproductive issues, pain, increased urinary frequency, and anemia.3,5,6 There is a general lack of awareness of fibroids among women and their potential health impact.7–9 One survey documented an average of 3.6 years to seek treatment, and 41% saw at least two healthcare providers before diagnosis.10
Uterine fibroid-related symptoms negatively impact physical and social activities, women's health-related quality of life, and work productivity.10–14 Black women experience fibroids at an earlier age, have more severe symptoms,10,15 and increased disease burden15,16; however, less is known about other minorities, including Hispanic women. The overall economic burden of symptomatic fibroids is estimated at $5.9–34.4 billion USD annually in both direct costs (e.g., medications, inpatient/outpatient visits, and surgery) and indirect costs (e.g., lost work time and preterm delivery).17
The objective of this population-based survey was to characterize the overall experience with fibroids across a spectrum of patient demographics, including symptom burden, patient awareness and bleeding perceptions, the treatment journey of diagnosed women, and disparity due to race, ethnicity, and income.
Materials and Methods
Survey overview
The web-based fibroid patient survey was designed and conducted by GfK (New York, NY), with input from physicians. Western Institutional Review Board (Puyallup, WA) reviewed and approved the questionnaire and research design. Female participants over 18 years of age were recruited via email from among members of the GfK KnowledgePanel®, a nationally representative and random panel of US households recruited via address-based sampling methodology. KnowledgePanel includes cell phone only households and captures the 25% of US families (36% of Hispanics) without Internet access. The KnowledgePanel sample was supplemented with high-quality samples from opt-in online panels to maximize the number of completed interviews. Survey responses and personal information were kept confidential. KnowledgePanel members received points for their participation, redeemable for prizes.
Survey questionnaire and selection criteria
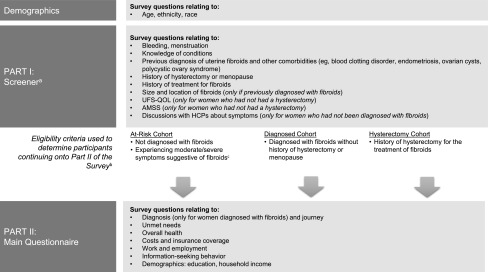
The fibroid patient survey was conducted online between June 30 and September 6, 2016, required approximately 40 minutes to complete, and consisted of multiple choice and free-response questions addressing demographic and health information. The survey contained two parts: the Screener (used to identify eligibility) and the Main Questionnaire (Fig. 1).
FIG. 1.
Overview of Survey and Questions. aScreening questions also included consent to participate and determined qualification to participate in the remainder of the study. bParticipants who did not meet eligibility criteria did not see questions included in Part II of the survey. cBased on responses to the UFS-QOL and select questions from the AMSS portion of the Screener (Part I), severe or moderate uterine fibroids were defined as at least a moderate or higher score on both transformed UFS-QOL measures (Symptom Severity ≥36.5 and HRQOL Total Score ≤72.5) and the AMSS (≥40.5) or a severe score on at least one of the following metrics: UFS-QOL Symptom Severity ≥56.5, UFS-QOL HRQOL Total Score ≤50.5, or AMSS ≥72.5. AMSS, Aberdeen Menorrhagia Severity Scale; HCP, healthcare provider; UFS-QOL, Uterine Fibroid Symptom and Health-Related Quality of Life.
The Screener assessed fibroid and hysterectomy history, as well as symptoms suggestive of fibroids in women without a clinical diagnosis via general health-related questions and two standardized disease-specific instruments: the Uterine Fibroid Symptom and Health-Related Quality of Life (UFS-QOL) questionnaire18 (1-month recall version19) and select questions from the Aberdeen Menorrhagia Severity Scale (AMSS) for heavy menstrual bleeding.20 Women who had a hysterectomy or had gone through menopause were not administered the UFS-QOL and AMSS. The UFS-QOL—a validated 37-item questionnaire to assess fibroid-specific symptom severity and health-related quality of life—is considered a sensitive measure of disease severity and treatment effect.18 The UFS-QOL includes a Symptom Severity score (range: 0–100; higher scores indicate greater symptom severity) and a health-related quality of life (HRQOL) Total Score (range: 0–100; higher scores indicating better HRQOL; consisting of six subscales: Concern, Activities, Energy/Mood, Control, Self-Consciousness, and Sexual Function). The AMSS is a validated 15-item questionnaire to assess the severity of bleeding that occurs during menses and between cycles (higher scores indicate greater severity).20 To limit survey duration, 9 of the 15 original AMSS questions were assessed in the Screener (nonvalidated); the maximum raw score (29) was converted to a maximum score of 100, with higher scores indicating greater bleeding severity. Severe or moderate fibroids were defined based on a combination of the UFS-QOL and AMSS bleeding scales using literature benchmarks18,20 (Fig. 1).
Following completion of the Screener, eligible participants were grouped into three analysis cohorts based on self-reported information: women who experienced symptoms suggestive of uterine fibroids without a clinical diagnosis (“at-risk cohort”), women diagnosed with fibroids (“diagnosed cohort”), and women with hysterectomy due to fibroids (“hysterectomy cohort”); eligibility for inclusion is detailed in Figure 1. Only eligible participants received the Main Questionnaire; those who did not qualify did not proceed with the survey.
The Main Questionnaire included questions related to menstrual symptoms and fibroids (i.e., diagnosis and treatment journey, hysterectomy journey, at-risk journey, and unmet needs), as well as overall health. Participants answered additional questions on HRQOL (e.g., 36-Item Short Form Survey [SF-36]; each subscale is scored from 0 to 100, with higher scores indicating better quality of life21), work-related impairment (Work Productivity and Activity Impairment Questionnaire22; 4 percentage scores were calculated as described by Reilly Associates,23 with higher scores indicating greater impairment and less productivity), healthcare provider relationship, costs and insurance coverage, and information-seeking behavior.
Statistical analyses
Raw data were adjusted based on the US Census Bureau's American Community Survey 5-year estimates (2010–2014)24 to more accurately reflect the composition of US adult women; sample weights were adjusted based on participant demographics: age, race, ethnicity, education, income, Internet at home, census region, and residence. Predefined population quotas were included to ensure a balanced sample (i.e., age, race, ethnicity, and fibroid severity) across the three cohorts and to ensure robust base sizes for analysis. Unless otherwise noted, all results are reported as weighted values. Mean transformed symptom severity scores and HRQOL are reported with standard deviation as the measure of dispersion. Subanalyses included results by race and ethnicity (white, black, and Hispanic) and annual income (<$24K, $24–59K, and ≥$60K).
All statistical analyses were carried out at the 0.10 significance level using overlap formulae, which is a methodology developed by Kish to account for overlapping samples and the resulting reduced number of independent observations (Section 12.4, Correlations for Overlap25); data reported in this study as significant reflect a p-value <0.10.
Results
Survey respondents and prevalence
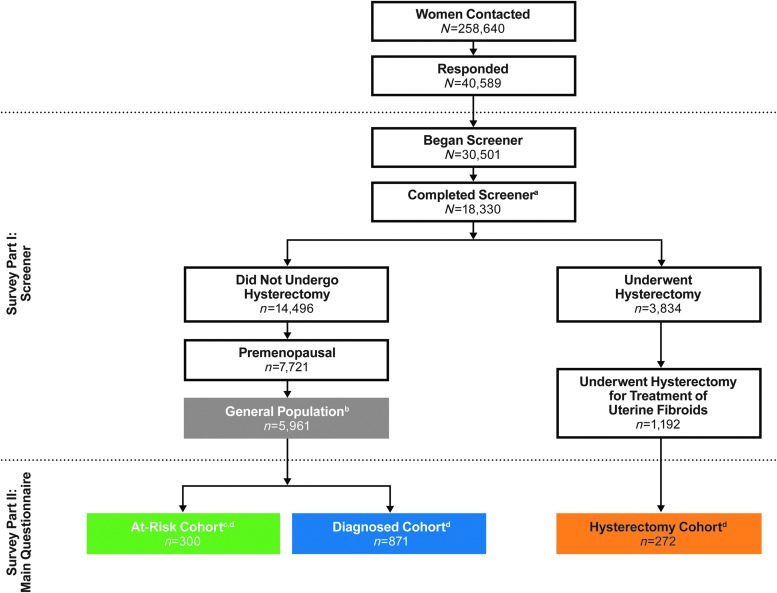
An overview of respondent disposition is provided in Figure 2. Of the 258,640 women contacted, 40,589 responded and 30,501 began the Screener. A total of 18,330 women completed the Screener. Of these women, approximately 9% had been diagnosed with uterine fibroids, and, of these, 42% received hysterectomy for treatment, and 58% had not undergone hysterectomy. An additional 3% of women who were premenopausal, had not undergone a hysterectomy, and were undiagnosed with fibroids experienced moderate-to-severe symptoms as measured by the UFS-QOL and AMSS.
FIG. 2.
Respondent Disposition. aCompleted the Screener portion asked of all women (UFS-QOL and AMSS not asked of women with hysterectomy). bGeneral population represents women who completed the entire Screener, had not undergone a hysterectomy, and were premenopausal. cWomen who experienced symptoms suggestive of uterine fibroids without a clinical diagnosis. dCompleted the Main Questionnaire, were eligible for inclusion, and were selected for analysis based on predefined population quotas included to ensure a sample representative of the US population.
In total, 1,443 women completed the survey and were eligible for inclusion in this analysis. Analysis groups were the at-risk cohort (n = 300), the diagnosed cohort (n = 871), and the hysterectomy cohort (n = 272; Fig. 2).
Demographics and baseline clinical characteristics are shown in Supplementary Table S1 (Supplementary Data are available online at www.liebertpub.com/jwh). Compared with the diagnosed and hysterectomy cohorts, the at-risk cohort was significantly younger and had significantly lower income and education levels. The at-risk cohort also had a significantly higher percentage of Hispanic women compared with the hysterectomy cohort. The hysterectomy cohort was significantly older and had a higher percentage of white women than both the at-risk and diagnosed cohorts. The most common comorbidities (≥30% in any cohort) were depression, high blood pressure, anxiety, high cholesterol, and ovarian cysts (Supplementary Table S1). Depression and anxiety occurred more frequently in the at-risk cohort compared with the diagnosed and hysterectomy cohorts, whereas cysts, high blood pressure, and high cholesterol were significantly lower in the at-risk cohort versus the hysterectomy cohort.
Burden of uterine fibroids
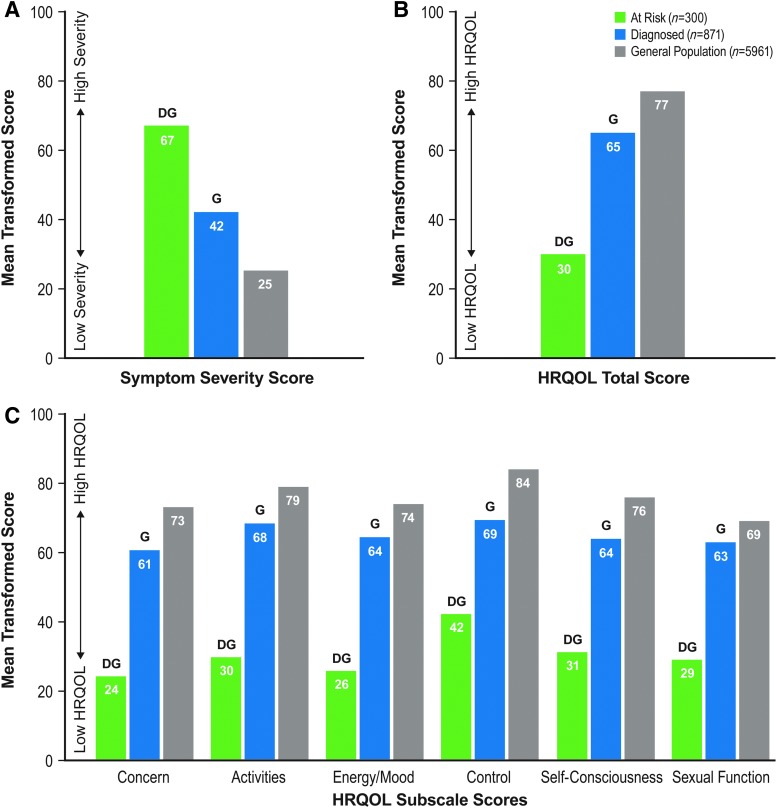
The severity of fibroid symptoms or symptoms suggestive of uterine fibroids, as measured by the UFS-QOL Symptom Severity subscale (Fig. 3; Supplementary Table S2), was significantly higher in the at-risk cohort compared with the diagnosed cohort and a general population who did not undergo hysterectomy (mean ± SD: 67 ± 18 vs. 42 ± 28 and 25 ± 22; Fig. 3). Similar trends by cohort were observed for the UFS-QOL HRQOL Total Score and HRQOL subscale scores, with at-risk women being significantly more impacted versus the diagnosed cohort and general population (Fig. 3).
FIG. 3.
UFS-QOL Symptom Severity Score (A), HRQOL Total Score (B), and HRQOL Subscale Scores (C). Letters denote statistical difference at 90% confidence between cohorts, where G indicates a significant difference versus the general population and D indicates a significant difference versus diagnosed cohort. The n values reflect the unweighted base; mean values are based on the weighted base. General population represents women who completed the entire Screener, had not undergone a hysterectomy, and were premenopausal (Fig. 2). HRQOL, health-related quality of life; UFS-QOL, Uterine Fibroid Symptom and Health-related Quality of Life.
When evaluating symptom impact based on race, ethnicity, or income, Hispanic women had significantly higher Symptom Severity scores compared with white and black women (at risk: 72 ± 17 vs. 65 ± 16 and 65 ± 18; diagnosed: 49 ± 30 vs. 38 ± 28 and 41 ± 27). Within the diagnosed cohort, women making <$60,000 (both <$24,000 and between $24,000 and $59,000) had significantly higher Symptom Severity scores compared with women making >$60,000 (51 ± 28 and 45 ± 29 vs. 38 ± 27, respectively).
Based on responses to the AMSS, at-risk women were severely impacted by heavy bleeding, with significantly higher AMSS scores compared with the diagnosed cohort and general population (mean ± SD AMSS scores of 41 ± 12 compared with 27 ± 14 and 25 ± 22, respectively). Most of the at-risk women were passing blood clots (84%), were at least moderately affected by heavy periods (82%), and required more than 1 form of protection at the same time (73%; Supplementary Table S3).
The SF-36, which was asked of all women in the three cohorts, demonstrated that at-risk women reported a significantly lower quality of life in each of the eight HRQOL subscales compared with both the diagnosed and the hysterectomy cohorts (Supplementary Fig. S1). Women suffering from fibroids or fibroid-like symptoms (diagnosed and at-risk cohorts, respectively) reported a lower overall quality of life versus the hysterectomy cohort, with significant impact on health and ability to carry out daily activities (Supplementary Table S4).
Over half of the women in this survey were employed and working for pay (at-risk cohort, 49%; diagnosed 66%; and hysterectomy 65%). For these employed respondents, the negative impact of symptoms on presenteeism, overall work impairment, and activity impairment was highest for the at-risk cohort and lowest for the diagnosed cohort (Supplementary Table S5; no statistical analyses were performed). Given the smaller number of employed respondents, subanalyses by race, ethnicity, and income did not yield any clear trends.
Cost and/or insurance coverage for the at-risk group significantly affected their ability to visit a doctor (35% responded it had “an effect” or “significant effect” versus 22% and 20% for the diagnosed and hysterectomy cohort, respectively) and ability to access medications for women's health needs (34% vs. 21% and 17%, respectively).
Awareness and perceptions
Roughly half of at-risk women (49%) had previously heard of uterine fibroids. Within the at-risk cohort, 47% of white and Hispanic women had heard of fibroids compared with 60% of black women; differences were not significant. Women making over $60,000 were significantly more likely to have heard of fibroids compared with women making <$24,000 or between $24,000 and $59,000 (60% vs. 43% and 44%, respectively).
Women in the general population felt that a normal menstrual period involved a mean of 5.0 (SD = 1.3) days of bleeding, roughly in line with what women in the diagnosed and hysterectomy cohort believed (5.0 ± 1.2 and 4.6 ± 1.6 days, respectively); however, women in the at-risk cohort reported a significantly longer duration for a normal menstrual period (5.3 ± 1.9 days) compared with both diagnosed and hysterectomy cohorts. Subanalyses of bleeding expectations by race, ethnicity, and income revealed some additional significant differences. For example, white women and women making under $24,000 in the at-risk cohort anticipate on average 5.6 ± 2.6 and 5.4 ± 1.8 days, respectively, of bleeding as normal, significantly longer than the general population (5.0 days). Within the diagnosed cohort, no differences between races or ethnicities were reported (data not shown). Women in the diagnosed cohort who made >$60,000 believed fewer days were normal compared to women making <$24,000 and women making between $24,000 and $60,000 (4.8 ± 1.1 versus 5.2 ± 1.2 and 5.1 ± 1.3 days, respectively). Of women in the hysterectomy cohort, white women felt that 4.8 days of bleeding was normal, significantly longer than black women in the hysterectomy cohort (4.1 ± 1.4 days). In addition, women in the hysterectomy cohort making <$60,000 thought 4.7 ± 2.0 bleeding days was normal, significantly more than women in the middle-income bracket (4.2 ± 1.9 days).
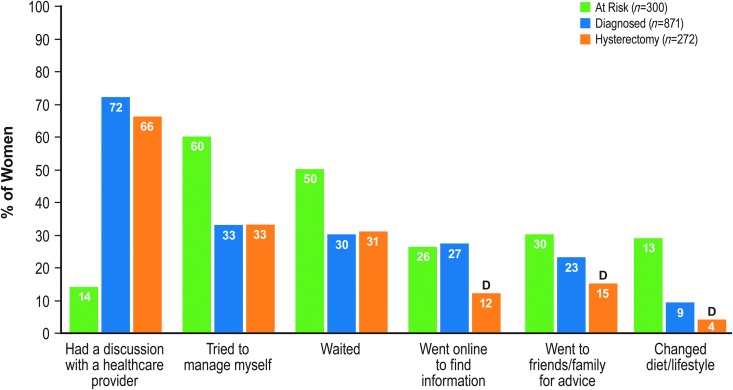
Mean ± SD age of symptom onset for women in the diagnosed cohort was 29.7 ± 9.6 years, while average age for women in the hysterectomy cohort was 32.7 ± 8.4 years. White women in both the diagnosed and hysterectomy cohorts had a significantly later age of symptom onset compared with black women (diagnosed: 31.1 ± 10.0 vs. 28.9 ± 8.5 years; hysterectomy: 33.5 ± 8.5 vs. 30.8 ± 8.8 years). Women in the at-risk cohort reported experiencing symptoms for 8.5 ± 7.7 years. Following symptom onset, most at-risk women (60%) tried to manage symptoms themselves or waited to see if symptoms went away (50%) (Fig. 4). Black women in this cohort were significantly less likely to visit a healthcare provider than white women (6% vs. 18%). Most women in the diagnosed and hysterectomy cohorts, however, spoke with a healthcare provider when symptoms first appeared (72% and 66%, respectively; Fig. 4). No race, ethnic, or income disparities were seen among women in either the diagnosed or hysterectomy cohorts (data not shown).
FIG. 4.
Action at Onset of Symptoms. The letter D denotes statistical difference at 90% confidence between the hysterectomy and diagnosed cohorts. Significance was not tested against the at-risk cohort since questions varied slightly. For the diagnosed and hysterectomy cohorts, phrasing was “what were the first things you did [when] uterine fibroid symptoms first appeared/first diagnosed with uterine fibroids,” whereas the at-risk cohort was asked about when “symptoms first appeared.” The n values reflect the unweighted base; percentages are based on the weighted base.
Treatment
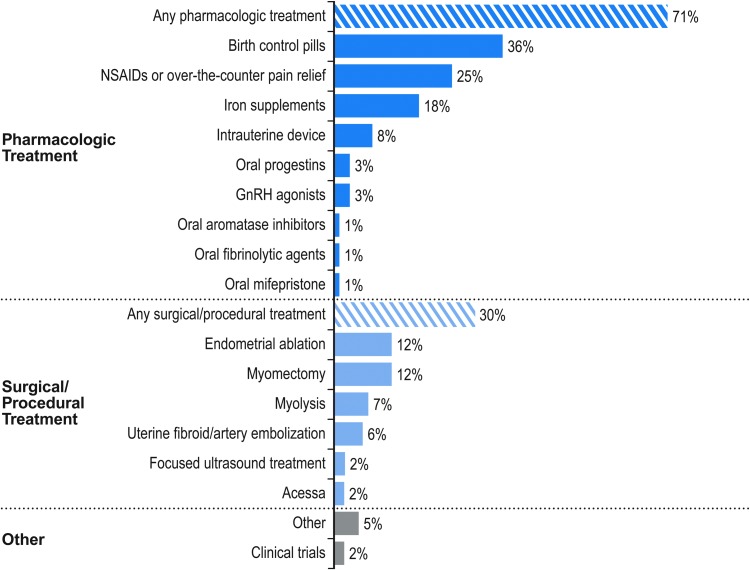
Most women diagnosed with fibroids who have not undergone a hysterectomy have sought treatment (73% overall; Fig. 5 by treatment type). Among diagnosed women, 71% have tried some form of pharmacologic therapy, including prescription treatments, over-the-counter pain relief, iron supplements, and hormonal contraceptives. In addition, 30% have undergone some form of surgery or procedure, with most electing endometrial ablation or myomectomy. Among all women who went to a healthcare provider for symptoms related to their fibroids, those who had undergone a hysterectomy were significantly more likely to discuss hysterectomy as a treatment option at first discussion compared with diagnosed women (60% vs. 16%, respectively), while those who had not undergone hysterectomy were more likely to discuss birth control pills (43% vs. 28%, respectively; Supplementary Fig. S2).
FIG. 5.
Treatment Usage Among Women in the Diagnosed Cohort (n = 871). The n value reflects the unweighted base; percentages are based on the weighted base. GnRH, gonadotropin-releasing hormone; NSAID, nonsteroidal anti-inflammatory drug.
Among women who discussed their fibroids with a healthcare provider, 20% of women in the diagnosed cohort and 15% of women in the hysterectomy cohort had been prescribed a pharmacologic treatment at their first discussion; the majority were prescribed birth control pills (69% and 59%, respectively; Supplementary Fig. S3). With respect to first discussion, no significant racial/ethnic or income disparities were noted among women who underwent a hysterectomy (data not shown). In contrast, women in the diagnosed cohort compared with the hysterectomy cohort were significantly more likely to have discussed pharmacologic treatments such as birth control pills (43% vs. 28%, respectively) or over-the-counter pain relief (19% vs. 13%, respectively) at first discussion. White and black women in the diagnosed cohort were significantly more likely to have first discussed a hysterectomy compared with Hispanic women (17% and 21% vs. 8%), while Hispanic women were significantly more likely to have discussed birth control pills (51%) than white women (39%).
The mean age of women who underwent a hysterectomy to treat fibroids was 41 years, regardless of race, ethnicity, or income level (mean range: 40–42 years). Approximately 11% of women had a hysterectomy before age 35. The leading reasons for opting for hysterectomy were recommendations from a healthcare provider (58%) and significant pain (55%) and distress (47%) due to symptoms. One in three women who had undergone a hysterectomy said that they would have been somewhat interested to extremely interested in a uterus-preserving option with roughly half desiring to maintain the ability to have children (Supplementary Fig. S4). Black women (40%) were significantly more likely to express interest in uterus-preserving options than white women (26%). Among women who reported interest in a uterus-preserving option, black women were significantly more likely to respond that they still wanted the option to have children compared with white women (69% vs. 21%, respectively).
Overall, women in all three cohorts cited relief from heavy bleeding as the most important aspect of fibroid treatment (other options included reduction of fibroid size, regain energy/relief, preserve fertility, stop all bleeding within 1 week, and relief from pelvic tightness or pressure). Women in the diagnosed cohort also reported a high desire for treatment to reduce fibroid size, while at-risk women reported a high desire to regain energy and experience relief from fatigue.
Discussion
In this survey, approximately 9% of women had a fibroid diagnosis, which is slightly higher than a 2009 international Internet-based survey in which 6.9% of U.S. women self-reported a fibroid diagnosis.13 When using American Community Survey 5-year estimates24 to extrapolate the 9% rate to the US population, approximately 11 million women are currently diagnosed with fibroids. Of those diagnosed without a hysterectomy, 71% tried some form of pharmacologic treatment, which extrapolates to approximately 2.7 million women. An additional 3% of undiagnosed women experienced moderate-to-severe symptoms suggestive of fibroids, adding 3.7 million women also potentially affected. Therefore, fibroid prevalence is likely higher than currently reported.
Women diagnosed with fibroids who did not undergo hysterectomy are heavily burdened by their symptoms, including reduced quality of life. While nearly three-quarters of the diagnosed cohort received pharmacologic treatment, these women reported lower mean scores on seven of eight SF-36 subscales compared to the hysterectomy cohort. Although treatment selection (pharmacologic and/or surgical) depends on patient perception of symptom severity and impact on quality of life, the most commonly prescribed treatments reported in this study are consistent with pharmacologic therapies reported in prior studies.26 Women with severe quality of life burden likely seek permanent treatment through hysterectomy. Given the HRQOL gap between the diagnosed and hysterectomy cohorts, an unmet need persists in fibroid therapy.
Women who underwent hysterectomy for fibroids reported suffering with symptoms for years before diagnosis and often quickly decided to undergo hysterectomy. These data also demonstrate that initial healthcare provider recommendations matched treatment course, highlighting the impact of these initial discussions. Interestingly, the decision to pursue hysterectomy did not appear to strongly correlate with age or parity status. Furthermore, consistent with previous survey results,15 black women were more interested in uterine-preserving options. Preserving the ability to have children, relieving symptoms (specifically heavy bleeding), and regaining energy represent significant unmet needs for fibroid treatment.
Fibroid burden may also extend to undiagnosed women experiencing symptoms suggestive of fibroids. These at-risk women reported bleeding more than what they considered normal and rated their quality of life as severely impacted, yet few had consulted a healthcare provider. These results underscore previous studies showing that women often delay medical help despite high symptom burden.7,8,14 Based on self-reported averages of 8.5 years of symptoms, women in the at-risk cohort began experiencing fibroid-like symptoms around age 25. In addition, these women reported more severe symptom impact compared with women in the other two cohorts. Hispanic women, underrepresented in fibroid surveys, comprised nearly one-third of this at-risk cohort and reported significantly higher Symptom Severity scores compared with white and black women. It should be noted, however, that at-risk women were identified based on UFS-QOL and AMSS scores (e.g., higher symptom severity, lower quality of life, and heavy bleeding) and may have other diseases (e.g., ovulatory dysfunction and adenomyosis) that obscure fibroid symptom identification. Awareness is also low in this at-risk population, with only about half of women having heard of fibroids. Women of racial/ethnic minorities and in lower income brackets are less likely to be aware versus white women, which may be compounded by inadequate access to care.
Comparisons based upon race or ethnicity are difficult to characterize, in part, due to lack of comparative data within racially/ethnically diverse populations in the literature and uniform under-representation or characterization of minority women in clinical studies. One systematic review showed that three-quarters of fibroid-related studies did not report race, and in the remaining studies, representation of black women was lower than expected based on US census data.27 Our results are strengthened by the unique inclusion of relatively high numbers of black and Hispanic women, demonstrating that symptom severity and distress may differ between groups.
Subjective retrospective data may be impacted by response bias, as the survey explored sensitive topics and requested recollection of possibly distant medical information. The survey is also unable to capture cases of asymptomatic fibroids that are likely undiagnosed. Unfinished surveys could have led to less robust sampling, and nonresponder bias could have impacted survey results. Finally, diagnosed and at-risk cohorts were included in the general population; because the patient cohorts were not mutually exclusive, this could have led to more conservative results in this general population comparator group.
Conclusions
Women with fibroids or symptoms suggestive of fibroids experience significant distress that negatively affects quality of life, particularly impacting racial/ethnic minorities and women in lower income brackets. Survey results further suggest that a substantial number of women are likely undiagnosed, underscoring the need for improved awareness and education.
The patient perspective amassed from this survey provides clear patient-care recommendations. Given evidence suggesting fibroids are likely underdiagnosed, routine patient–provider discussions should include signs and symptoms of fibroids. Healthcare providers should focus on lower income and minority populations as they are less aware of fibroids, more likely to self-treat, and may carry greater symptom burden compared with higher income or white women. Overall, our results underscore the need for improved uterine fibroid awareness and education.
Supplementary Material
Acknowledgments
Writing and editorial assistance was provided by Jacqueline Benjamin, PhD, and Krystina Neuman, PhD, of Prescott Medical Communications Group (Chicago, IL) and was funded by Allergan plc. This study was conducted by GfK, with financial support from Allergan plc. All authors contributed to the editing of the article and approved the final submitted version of the article without compensation.
Author Disclosure Statement
Erica Marsh is a consultant for Allergan plc and AbbVie. Ayman Al-Hendy is a consultant for Allergan plc, Bayer, Repros, and AbbVie. Dale Kappus was an employee of GfK at time of study. Dale Kappus is currently employed by Time Inc. in a noneditorial capacity—she coauthored the article in a personal capacity, any opinions are her own, and Time Inc. is not in any way affiliated. Alex Galitsky is an employee of GfK. Elizabeth A. Stewart received grant funding from the National Institutes of Health. Dr. Stewart has also served as a consultant/on advisory boards for AbbVie, Allergan, Astellas Pharma, Bayer Healthcare, Glaxo Smith Kline, Gynesonics, Myovant, and Welltwigs. Majid Kerolous is an employee of Allergan plc.
References
- 1.Drayer SM, Catherino WH. Prevalence, morbidity, and current medical management of uterine leiomyomas. Int J Gynaecol Obstet 2015;131:117–122 [DOI] [PubMed] [Google Scholar]
- 2.Stewart EA, Cookson C, Gandolfo RA, Schulze-Rath R. Epidemiology of uterine fibroids: A systematic review. BJOG 2017;124:1501–1512 [DOI] [PubMed] [Google Scholar]
- 3.Stewart EA, Laughlin-Tommaso SK, Catherino WH, Lalitkumar S, Gupta D, Vollenhoven B. Uterine fibroids. Nat Rev Dis Primers 2016;2:16043. [DOI] [PubMed] [Google Scholar]
- 4.Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: Ultrasound evidence. Am J Obstet Gynecol 2003;188:100–107 [DOI] [PubMed] [Google Scholar]
- 5.Bartels CB, Cayton KC, Chuong FS, et al. An evidence-based approach to the medical management of fibroids: A systematic review. Clin Obstet Gynecol 2016;59:30–52 [DOI] [PubMed] [Google Scholar]
- 6.Khan AT, Shehmar M, Gupta JK. Uterine fibroids: Current perspectives. Int J Womens Health 2014;6:95–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghant MS, Sengoba KS, Vogelzang R, Lawson AK, Marsh EE. An altered perception of normal: Understanding causes for treatment delay in women with symptomatic uterine fibroids. J Womens Health (Larchmt) 2016;25:846–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marsh EE, Brocks ME, Ghant MS, Recht HS, Simon M. Prevalence and knowledge of heavy menstrual bleeding among African American women. Int J Gynaecol Obstet 2014;125:56–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ekpo GE, Ghant MS, Woodley LM, Recht HS, McKnight T, Marsh EE. Knowledge of uterine fibroid symptoms and presentation among African-American women: A pilot study. J Reprod Med 2014;59:448–454 [PubMed] [Google Scholar]
- 10.Borah BJ, Nicholson WK, Bradley L, Stewart EA. The impact of uterine leiomyomas: A national survey of affected women. Am J Obstet Gynecol 2013;209:319.e311–e319.e320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghant MS, Sengoba KS, Recht H, Cameron KA, Lawson AK, Marsh EE. Beyond the physical: A qualitative assessment of the burden of symptomatic uterine fibroids on women's emotional and psychosocial health. J Psychosom Res 2015;78:499–503 [DOI] [PubMed] [Google Scholar]
- 12.Laberge PY, Vilos GA, Vilos AG, Janiszewski PM. Burden of symptomatic uterine fibroids in Canadian women: A cohort study. Curr Med Res Opin 2016;32:165–175 [DOI] [PubMed] [Google Scholar]
- 13.Zimmermann A, Bernuit D, Gerlinger C, Schaefers M, Geppert K. Prevalence, symptoms and management of uterine fibroids: An international internet-based survey of 21,746 women. BMC Womens Health 2012;12:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Downes E, Sikirica V, Gilabert-Estelles J, et al. The burden of uterine fibroids in five European countries. Eur J Obstet Gynecol Reprod Biol 2010;152:96–102 [DOI] [PubMed] [Google Scholar]
- 15.Stewart EA, Nicholson WK, Bradley L, Borah BJ. The burden of uterine fibroids for African-American women: Results of a national survey. J Womens Health (Larchmt) 2013;22:807–816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sengoba KS, Ghant MS, Okeigwe I, Mendoza G, Marsh EE. Racial/Ethnic Differences in Women's Experiences with Symptomatic Uterine Fibroids: A Qualitative Assessment. J Racial Ethn Health Disparities 2017;4:178–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cardozo ER, Clark AD, Banks NK, Henne MB, Stegmann BJ, Segars JH. The estimated annual cost of uterine leiomyomata in the United States. Am J Obstet Gynecol 2012;206:211.e211–e219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spies JB, Coyne K, Guaou Guaou N, Boyle D, Skyrnarz-Murphy K, Gonzalves SM. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol 2002;99:290–300 [DOI] [PubMed] [Google Scholar]
- 19.Coyne KS, Soliman AM, Margolis MK, Thompson CL, Chwalisz K. Validation of the 4 week recall version of the Uterine Fibroid Symptom and Health-related Quality of Life (UFS-QOL) Questionnaire. Curr Med Res Opin 2017;33:193–200 [DOI] [PubMed] [Google Scholar]
- 20.Ruta DA, Garratt AM, Chadha YC, Flett GM, Hall MH, Russell IT. Assessment of patients with menorrhagia: How valid is a structured clinical history as a measure of health status? Qual Life Res 1995;4:33–40 [DOI] [PubMed] [Google Scholar]
- 21.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–483 [PubMed] [Google Scholar]
- 22.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics 1993;4:353–365 [DOI] [PubMed] [Google Scholar]
- 23.Reilly Associates. WPAI:SHP Scoring. Available at: www.reillyassociates.net/WPAI_Scoring.html Accessed January29, 2018
- 24.U.S. Census Bureau. 2010–2014 American Community Survey 5-year estimates. Available at: https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2014/5-year.html Accessed January29, 2018
- 25.Kish L. Survey sampling. J. Wiley; 1965. Accessible at: https://books.google.com/books?id=xiZmAAAAIAAJ&source=gbs_book_other_versions Accessed May25, 2018
- 26.Yao X, Stewart EA, Laughlin-Tommaso SK, Heien HC, Borah BJ. Medical therapies for heavy menstrual bleeding in women with uterine fibroids: A retrospective analysis of a large commercially insured population in the USA. BJOG 2017;124:322–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taran FA, Brown HL, Stewart EA. Racial diversity in uterine leiomyoma clinical studies. Fertil Steril 2010;94:1500–1503 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.