Abstract
After the recognition of the essential role of the immune system in the progression of type 2 diabetes mellitus, more studies are focused on the effects produced by the abnormal differentiation of components of the immune system. In patients suffering from obesity or T2DM, there were alterations in proliferation of T cells and macrophages, and impairment in function of NK cells and B cells, which represented abnormal innate and adaptive immunity. The abnormality of either innate immunity, adaptive immunity, or both was involved and interacted with each other during the progression of T2DM. Although previous studies have revealed the functional involvement of T cells in T2DM, and the regulation of metabolism by the innate or adaptive immune system during the pathogenesis of T2DM, there has been a lack of literature reviewing the relevant role of adaptive and innate immunity in the progression of T2DM. Here, we will review their relevant roles, aiming to provide new thought for the development of immunotherapy in T2DM.
1. Introduction
Type 2 diabetes mellitus (T2DM) is characterized by abnormally elevated levels of blood glucose due to impaired insulin secretion, glucose intolerance, and hyperglycemia. It is also considered as a major burden for healthcare systems worldwide [1]. Nowadays, the pathogenesis of T2DM is considered to be linked to both innate and adaptive immune factors that are recognized as important etiological components in the development of insulin resistance [2]. Epigenetic mechanisms controlling immune cell lineage determination, function, and migration are implicated in obesity and T2DM. Obesity is associated with low-grade inflammation and is responsible for the activation of immune system in patients suffering from T2DM [3]. Increased fat mass in obese patients can induce metabolic dysregulation. It has also been recognized that insulin resistance during obesity is closely related to adipose tissue inflammation [4]. The abnormal proliferation of factors of innate and adaptive immune system was observed during adipose tissue inflammation that may lead to the development of T2DM [3]. For example, impaired NK cell function was observed, particularly with respect to NKG2D expression, which was negatively correlated with HbA1c levels [5]. Moreover, polarization of macrophage to M1 was upregulated, and activation of CD4+ T lymphocytes expressed in visceral adipose tissue of obese mice was elevated [6–8]. Since previous studies have reviewed the functional involvement of T cells in progression of T2DM, or regulation of metabolism by the innate immune system or adaptive immune system during the pathogenesis of T2DM, literature reviewing the relevant role of adaptive and innate immunity in the progression of T2DM in recent years still remains scarce. Therefore, here, we will review the relevant research, aiming to provide new ideas for the subsequent research.
2. T Cells in T2DM
In recent years, it has been reported that T cells play key roles in the progression of T2DM. It indicated that T2DM was associated with overactivated T cells and the activation of the inflammatory pathways [8]. Differentiation of effector T cells is tightly related by the regulation process that influences the production of distinct sets of effector cytokines [9]. T cells are abnormally differentiated in T2DM patients.
2.1. CD4+ T Cells
CD4+ T cells play an important role in the pathology of obesity and insulin resistance. CD4+ effector T cells can be further subdivided into proinflammatory Th1 and Th17 and anti-inflammatory Th2 and Foxp3+ regulatory T (Treg) cell subtypes based on their functionality and the type of cytokine produced [10]. It was reported that the percentage of CD45+ leukocytes increased significantly in obese patients with or without T2DM [11]. The balance between Th2 or Treg and effector T cell subsets such as Th1 or Th17 cells is important for immune homeostasis and the immune response. A large amount of evidence has showed that there was an imbalance in the differentiation in CD4+ T cells in obese T2DM patients.
2.1.1. T Helper (Th) Cells
Th1 cells are differentiated CD4+ T cells characterized by the production of proinflammatory interferon-γ (IFN-γ) [12]. Th2 cells are differentiated from activated CD4+ T cells, which drive the production of key Th2 cell lineage-defining cytokines such as interleukin- (IL-) 4, IL-5, and IL-13 [13]. When CD4+ T cells are encountered by IL-6 and transforming growth factor-β (TGF-β), they tend to differentiate to Th17 cells, which play a pathogenic role in various inflammatory disorders [14].
CD4+ T cells tend to polarize to proinflammatory Th1 cells and Th17 cells in peripheral blood and adipose tissue in patients suffering from T2DM. In contrast, polarization of anti-inflammatory Th2 cells was decreased [15–20]. A recent study [21] showed that Th1/Th2 ratio and levels of cytokines (e.g., IL-4, IL-10, IL-13, and IFN-γ) were significantly elevated, whereas nuclear factor erythroid 2-related factor 2 (Nrf2) and its downstream targets, which act with antioxidant, detoxification, and maintenance of cellular redox homeostasis and glutathione homeostasis and influence mitochondrial biogenesis, were decreased in T2DM patients. The circulatory levels of Nrf2 showed a positive correlation with the levels of Th2 cytokines and negative correlation with the levels of Th1 cytokines [21]. In addition, it showed that CD4+ and CD8+ T cells were infiltrated in both visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT), with proinflammatory Th1 and Th17 cells significantly more frequent in VAT as compared with SAT. The frequency of Th1 cells in SAT and VAT correlated directly with plasma hsCRP concentrations, while the frequency of Th2 correlated inversely with plasma hsCRP concentrations. Furthermore, Th1 cell frequency in SAT also correlated with plasma IL-6 levels [15, 22].
The secretion of cytokines (tumor necrosis factor- (TNF-) α, IFN-γ, and IL-17) and T lymphocytes was drastically upregulated during the pathogenesis of obesity-induced insulin resistance and development of T2DM [23–25]. With respect to the relationship between frequency of lymphocytes and activation of disease, it was found that the frequency of IFN-γ-producing CD3+ T cells was positively correlated with body mass index (BMI) [26]. Previous studies have reported that the frequency of cytokines can be influenced by other types of lymphocytes. B cells support Th17 inflammation in T2DM patients but not in the normal people, whereas monocytes support Th17 inflammation regardless of whether an individual is suffering from T2DM [27]. In addition, the cytokines produced by Th1, IL-2, and TNF-β; the cytokines produced by Th17, IL-17F, and IL-17A; and the cytokines produced by both Th1 and Th17 cells are important for explaining the HbA1c variance [28]. During the progression of T2DM, levels of mRNA and protein of IL-2 and TNF-α in diabetic retinopathy (DR) patients were dramatically higher compared with those of the healthy control group [29]. Moreover, the DR group showed higher IL-2 and TNF-α levels, however lower IL-4 and IL-10 levels than T2DM group without DR [26, 28]. Zhang et al. [30] discovered that levels of vascular endothelial growth factor (VEGF), which is related to the progression of diabetic microvascular disease, were positively correlated with Th1 percentage and the ratio of Th1/Th2. They also found that Th1/Th2 ratio was an independent predictor of VEGF levels in T2DM patients [30]. Angiotensin II increases the activities of T cells and the expression of IFN-γ and IL-17 significantly during the development of carotid atherosclerosis in patients suffering from T2DM [31].
2.1.2. Treg Cells
Treg cells express CD4, CD25, and forkhead family transcription factor Foxp3. They represent a small subset of T lymphocytes constituting only 5–20% of the CD4+ compartment, suppressing effector T cell responses, limiting inflammation, and preventing autoimmunity [14, 32, 33]. CD4+ T cells tend to polarize to Treg cells in vitro when treated with TGF-β, which appears to be dependent upon fatty acid oxidation and cholesterol metabolism rather than glycolysis [34, 35]. Treg cells suppress the levels of effector T cells by various pathways [36], including the inhibition T cell receptor- (TCR-) induced proliferation and IL-2 transcription of conventional T cells (Tcons) [37], the release of anti-inflammatory cytokines like IL-10 and TGF-β [38], the expression of the coinhibitory molecule cytotoxic T lymphocyte antigen-4 (CTLA-4) [39], the expression of the hallmark transcription factor of suppressed CD4+ T cells [40], and the ability to migrate by activation of glycolysis [41].
The balance between Treg and Th1 or Th17 cells is important for immune response in T2DM patients. Treg cells suppress the activities of Th1, Th2, and Th17 cells to improve insulin resistance. It has been reported that the percentage of Treg cells was decreased in peripheral blood of T2DM patients, especially in newly diagnosed patients, which culminates in the progress of inflammation and insulin resistance [42, 43]. It was reported that both Treg/Th17 ratio and Treg/Th1 ratio decreased in patients suffering from T2DM [44]. High levels of insulin in a model of diet-induced obesity impaired the ability of Tregs to suppress inflammatory responses via the AKT/mTOR signaling pathway, which showed lower expression of IL-10 and poor ability to suppress the production of TNF-α [45]. In obese patients also suffering from T2DM, an even lower percentage of Treg cells was revealed [46].
CD39+ Treg cells are responsible for suppressing Th17 cells and are believed to be reduced in number in obese T2DM patients [47]. It was confirmed that CD39 was related to the stability and the suppressive function of Treg cells [19]. It also indicated that, in overweight and obese T2DM patients, the levels of CD4+ IL-17+ cells showed a positive correlation with blood glucose and HbA1c expression levels. CD39hi Treg cells express higher CTLA-4 and produce more IL-10 than CD39low Tregs [19, 45, 47].
2.2. CD8+ T Cells
CD8+ T cells are essential for the adaptive immune response against infections by secreting cytokines, such as IFN-γ and TNF-α. It is well established that CD8+ T cells can also synthesize and express the proinflammatory cytokine IL-17, which is present in inflammatory tissues in various human inflammatory diseases [48]. Previous literature has shown that the accumulation of these cells induces inflammation and insulin resistance [49]. Patients with T2DM or mice with high-fat diet (HFD) seem to have higher percentage of CD8+ cytokine T cells [49–53]; however, the proportion of CD8+ T cells decreased after 120 min of glucose loading [54]. Pathogenic CD8+ T cell subsets, which control hepatic insulin sensitivity and gluconeogenesis, accumulate in the liver of diet-induced obese mice [55]. The accumulation was supported by type I interferon (IFN-I) responses [55]. It has been reported that the concentration of IFN-γ positively correlated with BMI of T2DM patients. In obese individuals, the levels of IFN-γ produced by CD8+ T cells increased when compared with lean individuals, which might modulate the insulin resistance [56]. Diet-induced obesity did not affect the maintenance of preexisting memory CD8+ T cells, including acquisition of a long-term memory phenotype and function [57].
2.3. NKT Cells
NKT cells refer to a large fraction of NK marker+ T cells (“NKT”) which recognize the major histocompatibility complex (MHC) class I-like CD1d protein expressed on the surface of antigen-presenting cells and use an identical “invariant” TCRα chain [58, 59]. Three subgroups of NKT cells can be distinguished according to their antigen specificity and TCR: invariant NKT (iNKT), type II NKT, and NKT-like lymphocytes [60]. iNKT cells are present in large numbers in adipose tissue. Upon activation, iNKT cells can secrete high levels of cytokines, including IL-4 and IFN-γ. But as adipose tissue expands during obesity, the number of iNKT cells decreased, correlating with proinflammatory macrophage infiltration. Mice lacking iNKT cells, when fed on HFD, showed higher weight, larger fat pads, elevated fasting blood glucose (FBG), impaired glucose tolerance test (GTT), and increased insulin resistance compared to wild-type (WT) mice. After weight loss, the abundance of iNKT cells was restored [61], followed by improvement in glucose tolerance and insulin sensitivity. The activation of NKT cells, influenced by M1 macrophages, promoted Th1 responses and inhibited M2 polarization. The expression of CD1d in M2 macrophages could activate NKT cell-mediated immune responses and disrupts the immune balance [62]. The depletion of NKT cells enhances the presence of M1 macrophages in visceral AT and increases insulin resistance and glucose intolerance [63]. It was reported that there was decreased frequency of iNKT cells in VAT and peripheral blood of obese patients [64]. Despite the several studies analyzing the frequency of iNKT cells in T2DM patients, no specific conclusion has been drawn yet [50, 65]. While recent studies identified that the gut microbiota may play a crucial role in iNKT cell development, it can be speculated that T2D alterations of the gut microbiota, and possibly even AT-associated microbiota, affect iNKT cell homeostasis in the gut and AT [66].
3. B Cells in T2DM
B cells have been shown to play a central role in the development of insulin resistance [67], through the production of IgG antibodies and the activation of T cells and macrophages [68]. There were no significant differences between the percentage of B cells in peripheral blood mononuclear cells (PBMCs) of T2DM or obese patients and healthy patients [11]. However, van Beek et al. showed that the expression of activation marker CD38 of B cells was significantly higher on circulating B cells in the obese patients with normal glucose tolerance as compared to obese patients suffering from T2DM [69]. Besides, DeFuria et al. argued that HFD induced a significant increase in the proliferation of B cells in VAT [70]. In patients with obesity or T2DM, DNA methylation, which is likely to be an important mechanism contributing to the interindividual variation in function of immune cells, was proved to stimulate the proliferation of B cells [71]. As we had discussed before, B cells could affect the proliferation of Th17 and the production of proinflammatory cytokines in T2DM patients. It was found that on depletion of CD19+ cells, Th17 proliferation was decreased in T2DM patients but not in individuals without T2DM [27]. Not only obese T2DM patients but also nonobese T2DM patients exhibited significantly high levels of fecal IgG, which is produced by B cells, compared to control individuals with similar BMI [70, 72]. The mice that failed to produce mature B cells showed lower fasting glucose levels and improved glucose tolerance when fed with HFD for 8 weeks compared to HFD-fed WT mice [70]. These results indicated that B cells participated in the process of promoting insulin resistance and glucose intolerance by activating Th1 and Th17 cells and releasing pathogenic antibodies.
4. NK Cells in T2DM
NK cells could recognize and deal with both tumors and viral or bacterial infections, all of which are prevalent in T2D. NK cell dysfunction was considered to lead to an increased risk of several infections and several cancer types [73]. The activity of NK cells is regulated by activating receptors, including NKp30, NKp44, NKp46, NKG2C, and NKG2D, all of which bind ligands present at the surface of tumor cells or infected cells [74]. NK cells could be divided into two main subtypes, one subgroup which mainly plays a role in cytotoxicity by expressing CD56dim CD16bright and another subgroup that mainly secretes cytokines (e.g., TNFα, IFN-γ, IL-8, and IL-10) and expresses CD56bright CD16dim/negative [75]. The number of total NK cells in obese or T2DM patients has exhibited discrepancies among different studies. Some studies have found that obese or T2DM patients exhibited higher number and/or activation of NK cells in the circulation or adipose tissue compared to control subjects [76–78], while a few other studies observed corresponding decreases or no changes at all [79]. Although it is generally recognized that the number of highly cytotoxic CD56dim NK cells decreased in obese individuals, the number of low cytotoxic CD56bright NK cells increased, along with the cytokines, including NKG2D and IFN-γ, produced by NK cells [80]. Berrou et al. has demonstrated that T2DM patients have a decreased frequency of NKp46- and NKG2D-positive NK cells and defects in NK cell function, which was evident from reduced degranulation [5]. Patients with uncontrolled diabetes had the lowest levels of NKG2D expression, and there is a significant inverse correlation between NKG2D-expressing NK cells of diabetic patients and their HbA1c levels. In VAT of HFD mice, NK cells skew macrophage differentiation into a proinflammatory M1 phenotype which further promotes inflammation and the development of obesity-induced insulin resistance [81].
5. Myeloid Cells in T2DM
Innate immunity also includes macrophages, monocytes, neutrophils, eosinophils, and basophils. Macrophages were emphasized to play a key role in the pathological progress of obesity or insulin resistance. Two subtypes of macrophages are present in the adipose tissue: a proinflammatory macrophage type, termed “M1” cultured in the presence of GM-CSF, and an anti-inflammatory macrophage type, termed “M2” in the presence of IL-4. M1-like macrophages showed proinflammatory effects by secreting high levels of proinflammatory markers and cytokines such as TNF, whereas M2-like macrophages exhibited increased secretion of anti-inflammatory cytokines such as IL-4 and IL-10 [82]. Macrophages infiltrated into expanding adipose tissue causing inflammation and linking obesity to insulin resistance. In obese humans, AT macrophages displayed profound proinflammatory (M1) polarization, under the influence of local environmental factors within the adipose tissue, and are thereby thought to be the major source of proinflammatory cytokines and chemokines [83, 84]. These proinflammatory macrophages also secrete chemokines to recruit the next wave of incoming monocytes. Loss of peroxisome proliferator-activated receptor-γ (PPARγ) (induced by IL-4) expression in macrophages can also result in impaired insulin sensitivity in the liver and muscle [85]. Disruption of PPARγ in myeloid cells impairs alternative macrophage activation (M2-like macrophage), thereby playing a key role in the development of diet-induced obesity, insulin resistance, and glucose intolerance.
Furthermore, macrophage activation is mediated by cells involved in adaptive immunity. Th1 and Th17 cells release IFN-γ and IL-17, which stimulate proinflammatory M1 macrophage differentiation, whereas Th2 cells and Treg cells promote anti-inflammatory M2 macrophage polarization via the production of IL-4, IL-10, or IL-13 [23, 86]. Macrophages in adipose tissue were considered as final effector cells, which regulate adipose tissue inflammation [81]. IL-6, which was reported to be increased in obese individuals, and promoted the development of insulin resistance and T2DM [87], could be secreted from macrophages and adipocytes in adipose tissue [88]. Kim et al. reported that expression of lamin A/C, which is a protein meshwork that surrounds and protects the nuclear content, was upregulated in adipose tissue in obese and type 2 diabetes patients. Moreover, lamin A/C expression is specifically upregulated in adipose tissue macrophages (ATMs), particularly in CD11c+ M1 ATMs, due to obesity, which could further promote expression of proinflammatory cytokines by enhancing activity of nuclear factor kappa-light-chain-enhancer of activated B cells (NK-κB) [89].
Beside altered macrophages, monocytes also play a key role in the progression of obesity and insulin resistance in T2DM patients. Patients suffering from T2DM exhibited increased expression of monocyte activation markers (CD11b and CD36). Monocyte surface CD163 expression levels were significantly associated with insulin resistance in type 2 diabetes patients, which showed the pathophysiological role of monocyte CD163 in the development of insulin resistance [90]. Eosinophils and neutrophils also play important roles in the immune regulation of T2DM. T2DM patients exhibited significant decrease in the number of neutrophils and eosinophils [17, 91]. Mice with restored eosinophilia (overexpressing IL-5) demonstrated decreased adiposity and improved insulin sensitivity when fed a high-fat diet [91].
6. Immunotherapy in T2DM
Recently, there have been several studies focusing on immune effect of hypoglycemic drugs or the improvement of glucose and lipid metabolism using immune system modulators. Metformin, which was initially recommended as the drug for T2DM treatment [92], has also been found to downregulate the mRNA levels of NK-kB and IL-1β, thus increasing the insulin sensitivity [93]. Metformin could influence macrophages as well by inducing the expression of reactive oxygen species in macrophages, which led to a phenotypic shift in macrophages toward M2-like macrophages via a partially adenosine monophosphate-activated protein kinase- (AMPK-) independent manner [94].
Consistent with these results, oral anti-CD3 plus glucosylceramide (an NKT cell target antigen) treatment has been shown to induce the production of IL-10 and TGF-β, which were associated with improved levels of glucose while fasting, visceral adipose tissue inflammation, liver enzymes, and hepatic steatosis in ob/ob mice [95]. Similar effects were observed by the induction of TGF-β-dependent CD4+ latency-associated peptide (LAP)-positive Tregs, which decreased the number of CD11b+ F4/80+ macrophages and TNF-α in adipose tissue of leptin-deficient ob/ob mice [96]. Activation of Nrf2 which was reported to be downregulated in PBMCs of T2DM patients, along with skew Th1 and Th2 dominance, could restore cytokine stress and the impaired insulin secretion in pancreatic β-cells [97]. In addition, there have been studies on transgenic mice with respect to the proliferation and function of components of immune system. OX40-KO mice exhibited significantly less body weight and lower fasting glucose levels than WT mice, without obvious adipose tissue inflammation. OX40 deficiency suppresses CD41+ T cell activation and prevents macrophage infiltration in the adipose tissues of obese mice [97]. Li et al. introduced a recombinant adenovirus carrying the protein tyrosine phosphatase nonreceptor type 2 (PTPN2) gene into epididymal white adipose tissue (EWAT) of ApoE−/− mice. The adenovirus reversed the high Th1/Treg and Th17/Treg ratios, macrophage infiltration, the ratio of M1/M2 macrophages, and the expression of proinflammatory cytokines in EWAT of diabetic mice [98].
7. Conclusion
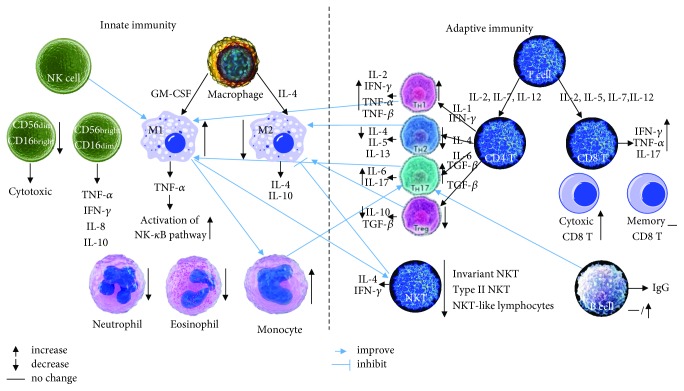
Since there were many similarities in the pathological progress of obesity and T2DM, which are tightly linked, altered proliferation, function, or infiltration of components of adaptive immunity and innate immunity is critical in the progression of T2DM. Obesity and T2DM share similar T cell compartment alterations that may contribute in the metabolic disturbances associated with them. These alterations include increased number of CD45+ T cell, leukocyte shift toward a proinflammatory phenotype, and a reduction in the number of suppressive regulatory T cells and protective NK cells. A higher susceptibility to infections has been observed in patients suffering from obesity and T2D, which indicates a T cell homeostatic dysregulation, NK cell dysfunction, and abnormal polarization of macrophages (Figure 1). Metabolic alterations in patients suffering from obesity and T2DM may further affect differentiation, function, and survival of components of innate immunity and adaptive immunity. Adipokines, such as leptin, increase T cell proliferation and Th1/Th17 cytokine secretion and prevent apoptosis via the mTOR signaling pathway following antigen stimulation [99].
Figure 1.
Role of innate immunity and adaptive immunity in the condition of T2DM, obesity, or adipose tissue of HFD mice.
The cross-talk and dynamics of immune cells initiating and orchestrating AT inflammation and an impaired lipid metabolism at different AT depots in the obese individuals who do not have diabetes or are suffering from type 2 diabetes are still not completely understood. The signals and mechanisms involved in obesity- and/or T2D-mediated modulation of T cell functions remain poorly documented. The mechanisms explaining change in the composition of cytokines secreted by different types of immunocytes are required to be elucidated. There have not been many studies related relationships of immune system and diabetes. The development of a personalized immunotherapy by identifying the metabolic immune checkpoint is highly desirable.
Above all, there has been increasing number of studies linking the immune system to T2DM. It was considered whether T2DM was an autoimmune disease because of the importance of inflammation in the development of insulin resistance, obesity, and T2DM. It is necessary to understand the role of innate immunity and adaptive immunity in obesity and diabetes, which could reveal novel immunotherapeutic approaches to modulate metabolic inflammation and insulin resistance.
Acknowledgments
This work was supported by the Graduate Innovation Fund of Jilin University (no. 2017029) and Innovation Fund in the Molecular Diagnosis and Treatment Engineering, Laboratory of Endocrinology and Metabolism Diseases in Jilin Province (no. 3J117C253428).
Abbreviations
- ATMs:
Adipose tissue macrophages
- AMPK:
Adenosine monophosphate-activated protein kinase
- BMI:
Body mass index
- CTLA-4:
Cytotoxic T lymphocyte antigen-4
- DR:
Diabetic retinopathy
- EWAT:
Epididymal white adipose tissue
- FBG:
Fasting blood glucose
- GTT:
Impaired glucose tolerance test
- HFD:
High-fat diet
- IFN-γ:
Interferon-γ
- IFN-I:
Type I interferon
- IL-4:
Interleukin-4
- IL-5:
Interleukin-5
- IL-6:
Interleukin-6
- IL-10:
Interleukin-10
- IL-13:
Interleukin-13
- IL-17:
Interleukin-17
- iNKT:
Invariant NKT
- MHC:
Major histocompatibility complex
- NK-kB:
Nuclear factor kappa-light-chain-enhancer of activated B cells
- Nrf2:
Nuclear factor erythroid 2-related factor 2
- PBMC:
Peripheral blood mononuclear cell
- PPARγ:
Peroxisome proliferator-activated receptor-γ
- PTPN2:
Protein tyrosine phosphatase nonreceptor type 2
- SAT:
Subcutaneous adipose tissue
- T2DM:
Type 2 diabetes mellitus
- Tcons:
Conventional T cells
- TCR:
T cell receptor
- TGF-β:
Transforming growth factor-β
- Th cell:
T helper cell
- TNF-α:
Tumor necrosis factor-α
- TNF-β:
Tumor necrosis factor-β
- Treg cell:
Regulatory T cell
- VAT:
Visceral adipose tissue
- VEGF:
Vascular endothelial growth factor
- WT:
Wild type.
Contributor Information
Zhenxiang Yu, Email: yuzhenxiang2005@sina.com.
Guixia Wang, Email: gwang168@jlu.edu.cn.
Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- 1.American Diabetes Association. Executive summary: standards of medical care in diabetes—2012. Diabetes care. 2011;35(Supplement 1):S4–10. doi: 10.2337/dc12-s004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldberg R. B. Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. The Journal of Clinical Endocrinology & Metabolism. 2009;94(9):3171–3182. doi: 10.1210/jc.2008-2534. [DOI] [PubMed] [Google Scholar]
- 3.Richardson V. R., Smith K. A., Carter A. M. Adipose tissue inflammation: feeding the development of type 2 diabetes mellitus. Immunobiology. 2013;218(12):1497–1504. doi: 10.1016/j.imbio.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Lee C. H., Lam K. S. L. Obesity-induced insulin resistance and macrophage infiltration of the adipose tissue: a vicious cycle. Journal of Diabetes Investigation. 2018 doi: 10.1111/jdi.12918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berrou J., Fougeray S., Venot M., et al. Natural killer cell function, an important target for infection and tumor protection, is impaired in type 2 diabetes. PLoS One. 2013;8(4, article e62418) doi: 10.1371/journal.pone.0062418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murano I., Barbatelli G., Parisani V., et al. Dead adipocytes, detected as crown-like structures, are prevalent in visceral fat depots of genetically obese mice. Journal of Lipid Research. 2008;49(7):1562–1568. doi: 10.1194/jlr.M800019-JLR200. [DOI] [PubMed] [Google Scholar]
- 7.Shirakawa K., Yan X., Shinmura K., et al. Obesity accelerates T cell senescence in murine visceral adipose tissue. Journal of Clinical Investigation. 2016;126(12):4626–4639. doi: 10.1172/JCI88606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stentz F., Kitabchi A. Activated T lymphocytes in type 2 diabetes: implications from in vitro studies. Current Drug Targets. 2003;4(6):493–503. doi: 10.2174/1389450033490966. [DOI] [PubMed] [Google Scholar]
- 9.Inácio D. P., Amado T., Silva-Santos B., Gomes A. Q. Control of T cell effector functions by miRNAs. Cancer Letters. 2018;427:63–73. doi: 10.1016/j.canlet.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 10.Raphael I., Nalawade S., Eagar T. N., Forsthuber T. G. T cell subsets and their signature cytokines in autoimmune and inflammatory diseases. Cytokine. 2015;74(1):5–17. doi: 10.1016/j.cyto.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verboven K., Wouters K., Gaens K., et al. Abdominal subcutaneous and visceral adipocyte size, lipolysis and inflammation relate to insulin resistance in male obese humans. Scientific Reports. 2018;8(1):p. 4677. doi: 10.1038/s41598-018-22962-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson C. B., Rowell E., Sekimata M. Epigenetic control of T-helper-cell differentiation. Nature Reviews. Immunology. 2009;9(2):91–105. doi: 10.1038/nri2487. [DOI] [PubMed] [Google Scholar]
- 13.Ansel K. M., Djuretic I., Tanasa B., Rao A. Regulation of Th2 differentiation and Il4 locus accessibility. Annual Review of Immunology. 2006;24(1):607–656. doi: 10.1146/annurev.immunol.23.021704.115821. [DOI] [PubMed] [Google Scholar]
- 14.Zhu J., Yamane H., Paul W. E. Differentiation of effector CD4 T cell populations. Annual Review of Immunology. 2010;28(1):445–489. doi: 10.1146/annurev-immunol-030409-101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McLaughlin T., Liu L. F., Lamendola C., et al. T-cell profile in adipose tissue is associated with insulin resistance and systemic inflammation in humans. Arteriosclerosis, Thrombosis, and Vascular Biology. 2014;34(12):2637–2643. doi: 10.1161/ATVBAHA.114.304636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harford K. A., Reynolds C. M., McGillicuddy F. C., Roche H. M. Fats, inflammation and insulin resistance: insights to the role of macrophage and T-cell accumulation in adipose tissue. The Proceedings of the Nutrition Society. 2011;70(4):408–417. doi: 10.1017/S0029665111000565. [DOI] [PubMed] [Google Scholar]
- 17.Nekoua M. P., Fachinan R., Atchamou A. K., et al. Modulation of immune cells and Th1/Th2 cytokines in insulin-treated type 2 diabetes mellitus. African Health Sciences. 2016;16(3):712–724. doi: 10.4314/ahs.v16i3.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lobo T. F., Borges C. d. M., Mattar R., et al. Impaired Treg and NK cells profile in overweight women with gestational diabetes mellitus. American Journal of Reproductive Immunology. 2018;79(3, article e12810) doi: 10.1111/aji.12810. [DOI] [PubMed] [Google Scholar]
- 19.Cortez-Espinosa N., Cortés-Garcia J. D., Martínez-Leija E., et al. CD39 expression on Treg and Th17 cells is associated with metabolic factors in patients with type 2 diabetes. Human Immunology. 2015;76(9):622–630. doi: 10.1016/j.humimm.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Sell H., Habich C., Eckel J. Adaptive immunity in obesity and insulin resistance. Nature Reviews Endocrinology. 2012;8(12):709–716. doi: 10.1038/nrendo.2012.114. [DOI] [PubMed] [Google Scholar]
- 21.Sireesh D., Dhamodharan U., Ezhilarasi K., Vijay V., Ramkumar K. M. Association of NF-E2 related factor 2 (Nrf2) and inflammatory cytokines in recent onset type 2 diabetes mellitus. Scientific Reports. 2018;8(1, article 5126) doi: 10.1038/s41598-018-22913-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chehimi M., Vidal H., Eljaafari A. Pathogenic role of IL-17-producing immune cells in obesity, and related inflammatory diseases. Journal of Clinical Medicine. 2017;6(7):p. 68. doi: 10.3390/jcm6070068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ouchi N., Parker J. L., Lugus J. J., Walsh K. Adipokines in inflammation and metabolic disease. Nature Reviews Immunology. 2011;11(2):85–97. doi: 10.1038/nri2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hotamisligil G., Shargill N., Spiegelman B. Adipose expression of tumor necrosis factor-α: direct role in obesity-linked insulin resistance. Science. 1993;259(5091):87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- 25.Mathis D. Immunological goings-on in visceral adipose tissue. Cell Metabolism. 2013;17(6):851–859. doi: 10.1016/j.cmet.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Francisco C. O., Catai A. M., Moura-Tonello S. C., et al. Cytokine profile and lymphocyte subsets in type 2 diabetes. Brazilian Journal of Medical and Biological Research. 2016;49(4, article e5062) doi: 10.1590/1414-431X20155062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cao Y. L., Zhang F. Q., Hao F. Q. Th1/Th2 cytokine expression in diabetic retinopathy. Genetics and Molecular Research. 2016;15(3):p. 15. doi: 10.4238/gmr.15037311. [DOI] [PubMed] [Google Scholar]
- 28.Ip B., Cilfone N. A., Belkina A. C., et al. Th17 cytokines differentiate obesity from obesity-associated type 2 diabetes and promote TNFα production. Obesity. 2016;24(1):102–112. doi: 10.1002/oby.21243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen H., Ren X., Liao N., Wen F. Th17 cell frequency and IL-17A concentrations in peripheral blood mononuclear cells and vitreous fluid from patients with diabetic retinopathy. Journal of International Medical Research. 2016;44(6):1403–1413. doi: 10.1177/0300060516672369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang Q., Fang W., Ma L., Wang Z. D., Yang Y. M., Lu Y. Q. VEGF levels in plasma in relation to metabolic control, inflammation, and microvascular complications in type-2 diabetes. Medicine. 2018;97(15, article e0415) doi: 10.1097/MD.0000000000010415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang K., Jin F., Zhang Z., Sun X. Angiotensin II promotes the development of carotid atherosclerosis in type 2 diabetes patients via regulating the T cells activities: a cohort study. Medical Science Monitor. 2016;22:4000–4008. doi: 10.12659/MSM.900842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zheng Y., Rudensky A. Y. Foxp3 in control of the regulatory T cell lineage. Nature Immunology. 2007;8(5):457–462. doi: 10.1038/ni1455. [DOI] [PubMed] [Google Scholar]
- 33.Dimeloe S., Burgener A. V., Grählert J., Hess C. T-cell metabolism governing activation, proliferation and differentiation; a modular view. Immunology. 2017;150(1):35–44. doi: 10.1111/imm.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Michalek R. D., Gerriets V. A., Jacobs S. R., et al. Cutting edge: distinct glycolytic and lipid oxidative metabolic programs are essential for effector and regulatory CD4+ T cell subsets. Journal of Immunology. 2011;186(6):3299–3303. doi: 10.4049/jimmunol.1003613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berod L., Friedrich C., Nandan A., et al. Erratum: De novo fatty acid synthesis controls the fate between regulatory T and T helper 17 cells. Nature Medicine. 2015;21(4):p. 414. doi: 10.1038/nm0415-414d. [DOI] [PubMed] [Google Scholar]
- 36.Guzma ´n-Flores J. M., Portales-Pe ´rez D. P. Mechanisms of suppression by regulatory T cells (Treg) Gaceta Médica de México. 2013;149(6):630–638. [PubMed] [Google Scholar]
- 37.Thornton A. M., Shevach E. M. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. The Journal of Experimental Medicine. 1998;188(2):287–296. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kleinewietfeld M., Hafler D. A. Regulatory T cells in autoimmune neuroinflammation. Immunological Reviews. 2014;259(1):231–244. doi: 10.1111/imr.12169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.du X., Liu M., Su J., et al. Uncoupling therapeutic from immunotherapy-related adverse effects for safer and effective anti-CTLA-4 antibodies in CTLA4 humanized mice. Cell Research. 2018;28(4):433–447. doi: 10.1038/s41422-018-0012-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y., Su M. A., Wan Y. Y. An essential role of the transcription factor GATA-3 for the function of regulatory T cells. Immunity. 2011;35(3):337–348. doi: 10.1016/j.immuni.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kishore M., Cheung K. C. P., Fu H., et al. Regulatory T cell migration is dependent on glucokinase-mediated glycolysis. Immunity. 2018;48(4):831–832. doi: 10.1016/j.immuni.2018.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jagannathan-Bogdan M., McDonnell M. E., Shin H., et al. Elevated proinflammatory cytokine production by a skewed T cell compartment requires monocytes and promotes inflammation in type 2 diabetes. Journal of Immunology. 2011;186(2):1162–1172. doi: 10.4049/jimmunol.1002615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yuan N., Zhang H. F., Wei Q., Wang P., Guo W. Y. Expression of CD4+ CD25+ Foxp3+ regulatory T cells, interleukin 10 and transforming growth factor β in newly diagnosed type 2 diabetic patients. Experimental and Clinical Endocrinology & Diabetes. 2018;126(2):96–101. doi: 10.1055/s-0043-113454. [DOI] [PubMed] [Google Scholar]
- 44.Zeng L., Lu H., Deng H., Mu P., Li X., Wang M. Noninferiority effects on glycemic control and β-cell function improvement in newly diagnosed type 2 diabetes patients: basal insulin monotherapy versus continuous subcutaneous insulin infusion treatment. Diabetes Technology & Therapeutics. 2012;14(1):35–42. doi: 10.1089/dia.2011.0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Han J. M., Patterson S. J., Speck M., Ehses J. A., Levings M. K. Insulin inhibits IL-10-mediated regulatory T cell function: implications for obesity. Journal of Immunology. 2014;192(2):623–629. doi: 10.4049/jimmunol.1302181. [DOI] [PubMed] [Google Scholar]
- 46.Qiao Y. C., Shen J., He L., et al. Changes of regulatory T cells and of proinflammatory and immunosuppressive cytokines in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Journal of Diabetes Research. 2016;2016:19. doi: 10.1155/2016/3694957.3694957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gu J., Ni X., Pan X., et al. Human CD39hi regulatory T cells present stronger stability and function under inflammatory conditions. Cellular & Molecular Immunology. 2016;14(6):521–528. doi: 10.1038/cmi.2016.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Srenathan U., Steel K., Taams L. S. IL-17+ CD8+ T cells: differentiation, phenotype and role in inflammatory disease. Immunology Letters. 2016;178:20–26. doi: 10.1016/j.imlet.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nishimura S., Manabe I., Nagasaki M., et al. CD8+ effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nature Medicine. 2009;15(8):914–920. doi: 10.1038/nm.1964. [DOI] [PubMed] [Google Scholar]
- 50.Menart-Houtermans B., Rütter R., Nowotny B., et al. Leukocyte profiles differ between type 1 and type 2 diabetes and are associated with metabolic phenotypes: results from the German Diabetes Study (GDS) Diabetes Care. 2014;37(8):2326–2333. doi: 10.2337/dc14-0316. [DOI] [PubMed] [Google Scholar]
- 51.Rausch M. E., Weisberg S., Vardhana P., Tortoriello D. V. Obesity in C57BL/6J mice is characterized by adipose tissue hypoxia and cytotoxic T-cell infiltration. International Journal of Obesity. 2008;32(3):451–463. doi: 10.1038/sj.ijo.0803744. [DOI] [PubMed] [Google Scholar]
- 52.Monteiro-Sepulveda M., Touch S., Mendes-Sá C., et al. Jejunal T cell inflammation in human obesity correlates with decreased enterocyte insulin signaling. Cell Metabolism. 2015;22(1):113–124. doi: 10.1016/j.cmet.2015.05.020. [DOI] [PubMed] [Google Scholar]
- 53.Pindjakova J., Sartini C., Lo Re O., et al. Gut dysbiosis and adaptive immune response in diet-induced obesity vs. systemic inflammation. Frontiers in Microbiology. 2017;8:p. 1157. doi: 10.3389/fmicb.2017.01157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Miya A., Nakamura A., Miyoshi H., et al. Impact of glucose loading on variations in CD4+ and CD8+ T cells in Japanese participants with or without type 2 diabetes. Frontiers in Endocrinology. 2018;9:p. 81. doi: 10.3389/fendo.2018.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kintscher U., Hartge M., Hess K., et al. T-lymphocyte infiltration in visceral adipose tissue: a primary event in adipose tissue inflammation and the development of obesity-mediated insulin resistance. Arteriosclerosis, Thrombosis, and Vascular Biology. 2008;28(7):1304–1310. doi: 10.1161/ATVBAHA.108.165100. [DOI] [PubMed] [Google Scholar]
- 56.Luck H., Tsai S., Chung J., et al. Regulation of obesity-related insulin resistance with gut anti-inflammatory agents. Cell Metabolism. 2015;21(4):527–542. doi: 10.1016/j.cmet.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 57.Khan S. H., Hemann E. A., Legge K. L., Norian L. A., Badovinac V. P. Diet-induced obesity does not impact the generation and maintenance of primary memory CD8 T cells. Journal of Immunology. 2014;193(12):5873–5882. doi: 10.4049/jimmunol.1401685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tard C., Rouxel O., Lehuen A. Regulatory role of natural killer T cells in diabetes. Biomedical Journal. 2015;38(6):484–495. doi: 10.1016/j.bj.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lynch L., Michelet X., Zhang S., et al. Regulatory iNKT cells lack expression of the transcription factor PLZF and control the homeostasis of Treg cells and macrophages in adipose tissue. Nature Immunology. 2015;16(1):85–95. doi: 10.1038/ni.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Touch S., Clément K., André S. T cell populations and functions are altered in human obesity and type 2 diabetes. Current Diabetes Reports. 2017;17(9):p. 81. doi: 10.1007/s11892-017-0900-5. [DOI] [PubMed] [Google Scholar]
- 61.Lynch L., Nowak M., Varghese B., et al. Adipose tissue invariant NKT cells protect against diet-induced obesity and metabolic disorder through regulatory cytokine production. Immunity. 2012;37(3):574–587. doi: 10.1016/j.immuni.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang H., Xue R., Zhu S., et al. M2-specific reduction of CD1d switches NKT cell-mediated immune responses and triggers metaflammation in adipose tissue. Cellular & Molecular Immunology. 2018;15(5):506–517. doi: 10.1038/cmi.2017.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Guzik T. J., Skiba D. S., Touyz R. M., Harrison D. G. The role of infiltrating immune cells in dysfunctional adipose tissue. Cardiovascular Research. 2017;113(9):1009–1023. doi: 10.1093/cvr/cvx108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Magalhaes I., Pingris K., Poitou C., et al. Mucosal-associated invariant T cell alterations in obese and type 2 diabetic patients. The Journal of Clinical Investigation. 2015;125(4):1752–1762. doi: 10.1172/JCI78941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Karagianni P., Polyzos S. A., Bougiouklis D., Tsapas A., Paletas K. Investigating the role of natural killer T-cells in gram negative infections of patients with type 2 diabetes mellitus. Hippokratia. 2015;19(3):231–234. [PMC free article] [PubMed] [Google Scholar]
- 66.Magalhaes I., Kiaf B., Lehuen A. iNKT and MAIT cell alterations in diabetes. Frontiers in Immunology. 2015;6:p. 341. doi: 10.3389/fimmu.2015.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Winer D. A., Winer S., Shen L., et al. B cells promote insulin resistance through modulation of T cells and production of pathogenic IgG antibodies. Nature Medicine. 2011;17(5):610–617. doi: 10.1038/nm.2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Winer S., Chan Y., Paltser G., et al. Normalization of obesity-associated insulin resistance through immunotherapy. Nature Medicine. 2009;15(8):921–929. doi: 10.1038/nm.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van Beek L., Lips M. A., Visser A., et al. Increased systemic and adipose tissue inflammation differentiates obese women with T2DM from obese women with normal glucose tolerance. Metabolism. 2014;63(4):492–501. doi: 10.1016/j.metabol.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 70.DeFuria J., Belkina A. C., Jagannathan-Bogdan M., et al. B cells promote inflammation in obesity and type 2 diabetes through regulation of T-cell function and an inflammatory cytokine profile. Proceedings of the National Academy of Sciences. 2013;110(13):5133–5138. doi: 10.1073/pnas.1215840110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Simar D., Versteyhe S., Donkin I., et al. DNA methylation is altered in B and NK lymphocytes in obese and type 2 diabetic human. Metabolism - Clinical and Experimental. 2014;63(9):1188–1197. doi: 10.1016/j.metabol.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 72.Zhou J., Wang Y., He Y., et al. Non-obese type 2 diabetes patients present intestinal B cell dysregulations associated with hyperactive intestinal Tfh cells. Molecular Immunology. 2018;97:27–32. doi: 10.1016/j.molimm.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 73.Joshi N., Caputo G. M., Weitekamp M. R., Karchmer A. W. Infections in patients with diabetes mellitus. The New England Journal of Medicine. 1999;341(25):1906–1912. doi: 10.1056/NEJM199912163412507. [DOI] [PubMed] [Google Scholar]
- 74.Colucci F., Caligiuri M. A., Di Santo J. P. What does it take to make a natural killer? Nature Reviews Immunology. 2003;3(5):413–425. doi: 10.1038/nri1088. [DOI] [PubMed] [Google Scholar]
- 75.Cooper M. A., Fehniger T. A., Caligiuri M. A. The biology of human natural killer-cell subsets. Trends in Immunology. 2001;22(11):633–640. doi: 10.1016/S1471-4906(01)02060-9. [DOI] [PubMed] [Google Scholar]
- 76.Guo H., Xu B., Gao L., et al. High frequency of activated natural killer and natural killer T-cells in patients with new onset of type 2 diabetes mellitus. Experimental Biology and Medicine. 2012;237(5):556–562. doi: 10.1258/ebm.2012.011272. [DOI] [PubMed] [Google Scholar]
- 77.O’Rourke R. W., Gaston G. D., Meyer K. A., White A. E., Marks D. L. Adipose tissue NK cells manifest an activated phenotype in human obesity. Metabolism. 2013;62(11):1557–1561. doi: 10.1016/j.metabol.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Viel S., Besson L., Charrier E., et al. Alteration of natural killer cell phenotype and function in obese individuals. Clinical Immunology. 2017;177:12–17. doi: 10.1016/j.clim.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 79.Lynch L. A., O'Connell J. M., Kwasnik A. K., Cawood T. J., O'Farrelly C., O'Shea D. B. Are natural killer cells protecting the metabolically healthy obese patient? Obesity. 2009;17(3):601–605. doi: 10.1038/oby.2008.565. [DOI] [PubMed] [Google Scholar]
- 80.Bähr I., Jahn J., Zipprich A., Pahlow I., Spielmann J., Kielstein H. Impaired natural killer cell subset phenotypes in human obesity. Immunologic Research. 2018;66(2):234–244. doi: 10.1007/s12026-018-8989-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lee B. C., Kim M. S., Pae M., et al. Adipose natural killer cells regulate adipose tissue macrophages to promote insulin resistance in obesity. Cell Metabolism. 2016;23(4):685–698. doi: 10.1016/j.cmet.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gordon S., Martinez F. O. Alternative activation of macrophages: mechanism and functions. Immunity. 2010;32(5):593–604. doi: 10.1016/j.immuni.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 83.Lumeng C. N., DelProposto J. B., Westcott D. J., Saltiel A. R. Phenotypic switching of adipose tissue macrophages with obesity is generated by spatiotemporal differences in macrophage subtypes. Diabetes. 2008;57(12):3239–3246. doi: 10.2337/db08-0872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kratz M., Coats B. R., Hisert K. B., et al. Metabolic dysfunction drives a mechanistically distinct proinflammatory phenotype in adipose tissue macrophages. Cell Metabolism. 2014;20(4):614–625. doi: 10.1016/j.cmet.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Odegaard J. I., Ricardo-Gonzalez R. R., Goforth M. H., et al. Macrophage-specific PPARγ controls alternative activation and improves insulin resistance. Nature. 2007;447(7148):1116–1120. doi: 10.1038/nature05894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tiemessen M. M., Jagger A. L., Evans H. G., van Herwijnen M. J. C., John S., Taams L. S. CD4+CD25+Foxp3+ regulatory T cells induce alternative activation of human monocytes/macrophages. Proceedings of the National Academy of Sciences. 2007;104(49):19446–19451. doi: 10.1073/pnas.0706832104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lowe G., Woodward M., Hillis G., et al. Circulating inflammatory markers and the risk of vascular complications and mortality in people with type 2 diabetes and cardiovascular disease or risk factors: the ADVANCE study. Diabetes. 2014;63(3):1115–1123. doi: 10.2337/db12-1625. [DOI] [PubMed] [Google Scholar]
- 88.Febbraio M. A., Pedersen B. K. Muscle-derived interleukin-6: mechanisms for activation and possible biological roles. FASEB Journal. 2002;16(11):1335–1347. doi: 10.1096/fj.01-0876rev. [DOI] [PubMed] [Google Scholar]
- 89.Kim Y., Bayona P. W., Kim M., et al. Macrophage lamin A/C regulates inflammation and the development of obesity-induced insulin resistance. Frontiers in Immunology. 2018;9:p. 696. doi: 10.3389/fimmu.2018.00696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kawarabayashi R., Motoyama K., Nakamura M., et al. The association between monocyte surface CD163 and insulin resistance in patients with type 2 diabetes. Journal of Diabetes Research. 2017;2017:8. doi: 10.1155/2017/6549242.6549242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wu D., Molofsky A. B., Liang H. E., et al. Eosinophils sustain adipose alternatively activated macrophages associated with glucose homeostasis. Science. 2011;332(6026):243–247. doi: 10.1126/science.1201475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Inzucchi S. E., Bergenstal R. M., Buse J. B., et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2012;55(6):1577–1596. doi: 10.1007/s00125-012-2534-0. [DOI] [PubMed] [Google Scholar]
- 93.Xu X., Lin S., Chen Y., et al. The effect of metformin on the expression of GPR109A, NF-κB and IL-1β in peripheral blood leukocytes from patients with type 2 diabetes mellitus. Annals of Clinical & Laboratory Science. 2017;47(5):556–562. [PubMed] [Google Scholar]
- 94.Bułdak Ł., Łabuzek K., Bułdak R. J., et al. Metformin affects macrophages’ phenotype and improves the activity of glutathione peroxidase, superoxide dismutase, catalase and decreases malondialdehyde concentration in a partially AMPK-independent manner in LPS-stimulated human monocytes/macrophages. Pharmacological Reports. 2014;66(3):418–429. doi: 10.1016/j.pharep.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 95.Zhang C., Xiao C., Wang P., et al. The alteration of Th1/Th2/Th17/Treg paradigm in patients with type 2 diabetes mellitus: relationship with diabetic nephropathy. Human Immunology. 2014;75(4):289–296. doi: 10.1016/j.humimm.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 96.Ilan Y., Maron R., Tukpah A. M., et al. Induction of regulatory T cells decreases adipose inflammation and alleviates insulin resistance in ob/ob mice. Proceedings of the National Academy of Sciences. 2010;107(21):9765–9770. doi: 10.1073/pnas.0908771107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu B., Yu H., Sun G., et al. OX40 promotes obesity-induced adipose inflammation and insulin resistance. Cellular and Molecular Life Sciences. 2017;74(20):3827–3840. doi: 10.1007/s00018-017-2552-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Li Y., Zhou H., Wang F., et al. Overexpression of PTPN2 in visceral adipose tissue ameliorated atherosclerosis via T cells polarization shift in diabetic Apoe−/− mice. Cellular Physiology and Biochemistry. 2018;46(1):118–132. doi: 10.1159/000488415. [DOI] [PubMed] [Google Scholar]
- 99.Procaccini C., de Rosa V., Galgani M., et al. Leptin-induced mTOR activation defines a specific molecular and transcriptional signature controlling CD4+ effector T cell responses. Journal of Immunology. 2012;189(6):2941–2953. doi: 10.4049/jimmunol.1200935. [DOI] [PubMed] [Google Scholar]