Abstract
A functional analysis of 167 genes overexpressed in Krebs-2 tumor initiating cells was performed. In the first part of the study, the genes were analyzed for their belonging to one or more of the three groups, which represent the three major phenotypic manifestation of malignancy of cancer cells, namely (1) proliferative self-sufficiency, (2) invasive growth and metastasis, and (3) multiple drug resistance. 96 genes out of 167 were identified as possible contributors to at least one of these fundamental properties. It was also found that substantial part of these genes are also known as genes responsible for formation and/or maintenance of the stemness of normal pluri-/multipotent stem cells. These results suggest that the malignancy is simply the ability to maintain the stem cell specific genes expression profile, and, as a consequence, the stemness itself regardless of the controlling effect of stem niches. In the second part of the study, three stress factors combined into the single concept of “generalized cellular stress,” which are assumed to activate the expression of these genes, were defined. In addition, possible mechanisms for such activation were identified. The data obtained suggest the existence of a mechanism for the de novo formation of a pluripotent/stem phenotype in the subpopulation of “committed” tumor cells.
Keywords: cancer stem cell, TAMRA+ cells, induction of pluripotency, hypoxia, oxidative stress, xenobiotics, carcinogenesis, genes-markers of stemness
Introduction
Hallmarks of cancer: version 2.0
Malignant neoplasms have been known to medicine for several thousand years, and it can assuredly be stated that all this time science has tried to find and formulate the fundamental properties that determine the development of tumors in vivo. The evolution of our ideas regarding the processes of the onset and development of tumors has overcome a very long and difficult way. As the first steps, the primitive macroscopic anatomical descriptions had been made (Yelloly, 1809). With the progress in methodology and instruments development, they gave way to the similar microscopic ones (Creighton, 1882) and even later–to the first attempts to determine the functional properties of tumor cells in vitro (Carrel and Ebeling, 1928). At the late steps, we came to an understanding (well, at least we tend to think so) of the fundamental physiological and molecular-genetic processes of tumor development, which, finally, made it possible to formulate the “Hallmarks of Cancer.”
There are two main points of view on the significant signs of malignancy of cancer and its underlying unit–cancer cells. In the first case, it is asserted that the hallmarks of cancer comprise six biological capabilities acquired during the multistep development of tumors. The hallmarks constitute an organizing principle for rationalizing the complexities of neoplastic disease. They include (1) Self-Sufficiency in Growth Signals, (2) Insensitivity to Antigrowth Signals, (3) Evading Apoptosis, (4) Limitless Replicative Potential, (5) Sustained Angiogenesis, and (6) Tissue Invasion and Metastasis (Hanahan and Weinberg, 2000, 2011).
In the second case, the authors offer an alternative set of key characteristics that determine the malignancy of a cancerous tumor and cancer cells that form it. This variant includes (1) selective growth and proliferative advantages, (2) altered stress response favoring overall survival, (3) vascularization, (4) invasion and metastasis, (5) metabolic rewiring, (6) an abetting microenvironment, and (7) immune modulation (Fouad and Aanei, 2017).
It is easy to note that these two lists both quite clearly overlap, have also quite a fundamental difference. Thus, for example, the authors of the second model do not include immortalization in the list of significant properties that define the behavior of the tumor. This property, in fact, represents a fundamental, extra-hierarchical qualitative event, which, on the one hand, is itself not a manifestation of malignancy, yet, on the other hand, is indispensable for its development.
Since the hallmarks of cancer and cancer cells malignancy, as they are denoted by the authors cited above, seem to be excessively detailed, we in our scrutiny narrowed them down to three more general categories that define the malignant potential at the phenotypic level. The first is the proliferative self-sufficiency as a set of characteristics that provide uncontrolled tumor growth. It comprises both independence from external mitogenic stimuli and immunity to stimuli that cause cell cycle arrest or apoptosis. The second one is invasiveness. It combines such properties as the ability to lyse the basal membrane, an increased capacity for migration, and the ability to adapt to the tissue environment, which is initially uncharacteristic for the tumor cell. And the last, third category is multiple drug resistance. This one is, in fact, a part of a broader detoxification mechanism essential for the survival of cells under aggressive tumor conditions. We also excluded from nomenclature both immortalization (for the reason described above) and sustained angiogenesis (due to ultimate dependence on the tumor context–this feature is essential for solid forms only).
Cancer stem cell: the objectives and subjectives of the paradigm
Along with the definition of the cancer cells malignancy hallmarks and understanding of the mechanisms of tumor progression, data on the high heterogeneity of the tumor cellular mass were accumulated. These data turned out to contradict, to a certain extent, the theory of clonal origin of tumors.
The clonal nature of tumors has been known for a long time: it was first shown for human lymphomas (Fialkow et al., 1967, 1970; Steele, 1970) and subsequently confirmed for other types of tumors (Baylin et al., 1976; Nowell, 1976). At approximately the same time, it was found that tumors are quite heterogeneous and consist of cells that differ, and sometimes to a great extent, both in phenotype, and in physiological, proliferative and tumor-initiating attributes. For glioblastomas, for example, it was shown that tumors contain variable proportions of actively proliferating and nonproliferating tumor cells and that up to 70% of the cells in these tumors are resting (nonproliferating) (Hoshino and Wilson, 1975). However, one of the most convincing and demonstrative essays in terms of evidence of the tumor cells population heterogeneity is the work of Lavrovsky et al. In this essay, multiple clones from several spontaneously established murine sarcomas of CBA, C3H, and Balb/c genotypes were obtained and described. The phenotype of these clones was shown to vary from highly tumorigenic to the so-called pseudonormal. The tumorigenic clones were characterized by rapid multilayer growth and almost complete independence of the serum content, while the pseudonormal ones demonstrated sensitivity to growth factors as well as contact inhibition and the ability to differentiate into adipocytes after prolonged arrest in G0 (Lavrovsky et al., 1992).
Thus, in the early 90s of the last century, a firm paradigm for tumor growth emerged in molecular oncology. It was claimed that tumor growth is driven by a small subpopulation of actively dividing cells, while the rest of the cellular mass, which constitutes the bulk of the tumor, is a kind of ballast formed as a result of high genetic instability of tumor cells (Pathak, 1990).
The further accumulation of knowledge on tumors development has revealed that the cellular composition of tumors is essentially determined by certain internal rules, similar to those for normal organs. As a logical consequence, the previous paradigm has been evolutionary updated. In accordance to this updated paradigm, the tumor is considered an aberrant organ, developing from a subpopulation of poorly differentiated tumor cells with an infinite proliferative potential. For such a type of cells the new term “cancer stem cell” (by analogy with normal stem cells) was invented. And despite the term first being used in 1980 (Mattox and Von Hoff, 1980), the targeted investigation of this phenomenon started only in this millennium, when the term acquired its final meaning as a definition for poorly differentiated cells with indefinite potential for self-renewal that drive tumorigenesis (Reya et al., 2001).
However, in contrast to normal stem cells with their quite objective and clearly formalized criteria of stemness, the definition of stemness for cancer cells remains generally problematic and the search for such criteria is one of the high priority tasks in molecular oncology.
Recently, it was found that a certain subpopulation of Krebs-2 ascites carcinoma cells has the inherent ability to internalize fragments of extracellular double-stranded DNA (hereinafter–TAMRA+ cells). This subpopulation also demonstrates such a fundamental property of cancer stem cells (CSCs) as the ability to induce upon transplantation the development of a new tumor with histological and cellular characteristics similar to the original one. Elimination of these cells leads either to the loss of the grafting potential by the transplant, or to the cure of mice from developed Krebs-2 ascites (Dolgova et al., 2012, 2013, 2014, 2016; Potter et al., 2016b, 2018). Thus, the ability to internalize extracellular double-stranded DNA can be referred to as a valid marker (or, at least, as one of) of cancer cells stemness.
Induction of stemness: alpha and omega of tumor development?
The paradigm of CSC and aberrant organogenesis had resolved the issue of tumors heterogeneity in the context of their clonal origin. But a new question had arisen.
The clonal nature of tumors implies that the entire mass of the tumor is the progeny of a single cell. The rapid and extensive growth of a tumor mass inevitably should lead to a situation, when a progenitor cell, i.e., CSC, remains in the very center of a tumor. It, in turn, should apparently cause either the complete cessation of tumor growth, or such a slowing down of it that is, in fact, almost equivalent to cessation. The tumor growth observed both in experiments and in medical practice is possible only in the presence of an essentially large number of CSCs, more or less evenly distributed throughout the tumor volume. As it is shown by our numerous experiments on mice and cultures of human cancer cells, as well as by the results of other researchers, the content of CSCs in tumor tissue varies from a few hundredths of a percent to several percents, and they are dispersedly scattered throughout a tumor mass or in ascitic fluid (Dolgova et al., 2014; Potter et al., 2016a,b). This means that under regular conditions of tumor tissue development, one CSC ensures the existence and biological activity of about 100–1,000 tumor cells. Assuming all the above, the question is how such a pattern of the CSCs distribution is being formed during the tumor quasi-organ development from a single progenitor.
It is generally accepted that the source of new CSCs, as in the case of normal pluri-/multipotent stem cells, is symmetrical division, as a manifestation of one of the fundamental properties of stemness. The newly formed CSC easily leaves not only its original site of localization in the tumor, but also the formed tumor tissue itself and, without losing its malignant properties, can migrate either to other parts of the growing tumor quasi-organ or to distant parts of the body. In other words, symmetrical division of the progenitor provides a constant supply of new CSCs, which migrate from the primary niche to the periphery of the tumor, creating new growth foci there, and the utmost case of such migrations is metastases.
This hypothesis, which explains the ability of CSCs to increase their population by symmetrical division followed by migration, is supported, in part, by the results we obtained earlier. Daily we estimated the numbers of TAMRA+ cells in Krebs-2 ascites from its onset and until the death of the animals (14 days). A characteristic oscillation in the number of TAMRA+ cells within 3 days accompanied by an increase in the volume of ascitic fluid and the total mass of cancer cells was observed. Along this time span, the number of TAMRA+ cells increased 3-fold and then returned to the baseline. The following model was proposed to explain this observation. The first act of symmetrical division produces two equal CSCs. One of these new CSCs enters the second division producing two daughter cells that both still possess the ability to internalize the TAMRA-labeled DNA probe. After the third division, the progeny of CSC lose their ability to internalize DNA and the percentage of TAMRA+ cells returns to initial value (Potter et al., 2016a,b).
Nevertheless, there are numerous data that suggest the existence of another mechanism for the formation and maintenance of the CSCs population.
Thus, in the study cited above, we found a discrepancy that did not fit into the theory explaining the increase in the number of CSCs as a result of their symmetrical division. It was found that for the majority of the mice analyzed, days of a “peak value” were observed, when the amount of CSCs significantly exceeded the regular threshold values typical for the observed oscillation of the CSCs counts (Potter et al., 2016a,b).
In the also mentioned above work of Lavrovsky et al, the efficacy of tumor formation upon transplantation of the progeny of the obtained clones into syngeneic mice has been evaluated. It was shown that tumors develop both in the case of highly tumorigenic clones, with the properties of CSCs, and in the case of pseudonormal cells, which displayed properties of committed cells. The difference between tumorigenic and pseudonormal clones was only in the incidence of tumor formation and in the time lapse required for this (Lavrovsky et al., 1992).
It is also known that many of immortalized cell lines displaying a “normal” phenotype of committed cells, such as various 3T3 lines, for example, produce tumors upon transplantation into syngeneic or immunodeficient animals (Greig et al., 1985; Melchiori et al., 1992). In other words, the data presented suggest that upon transplantation of “committed” cells of 3T3 type, i.e. possessing an infinite proliferative potential, but not an undifferentiated phenotype, in vivo CSCs can emerge de novo, giving rise to a tumor. Recent evidences support such a model of “dynamic stemness” for, at least, melanomas. Melanoma cells might temporally acquire tumor-initiating properties or switch from a status of tumor-initiating cells to a more differentiated one depending on the tumor context (Tuccitto et al., 2016).
A number of other studies demonstrating the feasibility of tumor cells to transit in both directions from cells of stem-like phenotype to differentiated ones and back again have also been compiled and reviewed (ElShamy and Duhé, 2013; Campos-Sánchez and Cobaleda, 2015).
Numerous observations of “dynamic stemness” allow to hypothesize the emergent nature of, at least, a part of the CSCs population. Accordingly, it is logical to presume that their emergence is associated with certain conditions in the micro- and humoral-environment, leading to the activation of the signaling pathways required for the induction of pluripotent/stem phenotype. Such a hypothesis implies the possibility of a reversible switching of the malignant identity of tumor cells and explains the distribution pattern of CSCs throughout the tumor volume, including its distal regions.
Hallmarks of stemness: pointing the targets
Assuming all the above, it is CSCs that are obviously to be responsible for the implementation of the “tumorigenicity program” and thus have to evince the properties of malignancy to the highest extent, while the role of the remaining mass of tumor cells is still rather speculative.
Previously we have isolated the enriched population of TAMRA+ cells, which, as mentioned above, display all the principal properties of CSCs, and have identified 167 genes overexpressed in these cells relative to TAMRA− cells (see Additional Table 1) (Potter et al., 2017).
In accordance to the proposed model of malignancy that consists of proliferative self-sufficiency, invasiveness and multiple drug resistance, we analyzed all these 167 genes with regard to their possible roles in realization of these fundamental properties. The existing data mining revealed that the genes involved in the formation of TAMRA+ cells malignancy differed in their significance based on their contribution to the one or several attributes of malignancy simultaneously. It also turned out that besides their role as known CSCs markers, a significant part of genes from the list were also markers of stemness in normal pluri-/multipotent stem cells involved in maintaining their stem phenotype.
Upon identification of genes principal for formation and maintenance of the malignant/pluripotent properties of cancer cells, we have attempted to reveal the possible mechanisms of activation of these genes as well as to deduce the conditions essential for such an activation. Analysis of published data has revealed the plausible influence of stress factors on activation of both the identified genes and stem-like phenotype of tumor cells itself. The following analysis of ChIP-Seq data gave us a clue to possible mechanisms of activating effect of “generalized cellular stress.”
The yin and yang of pluripotency
In the following parts of the article we describe a number of well known and generally accepted statements based on multiple experiments with a wide range of models including cellular in vitro models, experimental animals and clinically obtained tumor samples. To prove the majority of these statements we refer to review articles. In cases when the model represents an individual and unique one, we describe it in more details.
Proliferative self-sufficiency
As already mentioned, we consider proliferative self-sufficiency as a complex property. On the one hand, it is defined as the ability of a cell to maintain proliferation under conditions of inaccessibility or deficiency in external mitogenic stimuli. On the other hand, it reflects the ability to keep viability and avoid apoptosis despite the presence of pro-apoptotic signals. It can be achieved by a rather large set of mechanisms, from autocrine synthesis and secretion of growth factors and components of the extracellular matrix (reviewed in Hoelzinger et al., 2007) to blocking the internal mechanisms of the apoptotic program (reviewed in Mallard and Tiralongo, 2017). The main problem we encountered in the analysis and selection of genes contributing to this property is the dependence of the functional properties of their protein products on the overall gene-protein context in each particular case. Often the same protein can act both as a tumor suppressor and as a tumor inducer depending on the type of cells or conditions. As an example, we can refer to the gene Perp, which was overexpressed in TAMRA+ cells, and which we, nevertheless, could not relate to any of the groups due to the lack of direct evidence of its functional effect on the formulated properties. It was shown that in the case of invasive squamous cell carcinoma, Perp functions as a tumor suppressor (Kong et al., 2013), while the Perp−/− mice were more resistant to papilloma development than those of the wild-type, that suggests its pro-oncogenic function (Marques et al., 2005). Moreover, it is a possible case when the protein product of a gene normally functions as a tumor suppressor, but upon the mutation its properties as a tumor suppressor are either lost or even inverted and it acquires pro-oncogenic function as it is shown, for example, for “gain-of-function” mutations of the p53 tumor suppressor gene (Vogiatzi et al., 2016). Since we did not have the opportunity to resolve all these of issues, we decided that the gene is to be included in a certain functional group if in principle there is evidence of its positive impact on the implementation of the corresponding property. As a result, we have selected 82 genes that one way or another participate in formation of the proliferative self-sufficiency of tumor cells (Table 1).
Table 1.
Genes showing elevated expression in TAMRA+ Krebs-2 carcinoma cells relative to TAMRA− cells, the activation of which results in excessive proliferative activity or resistance to apoptosis.
| Gene | Synonyms | Proving reference | |
|---|---|---|---|
| 1 | Abca1 | ABC1, HDLDT1, TGD | Buechler et al., 2002 |
| 2 | Acpp | ACP-3, ACP3, PAP | Liu et al., 2014 |
| 3 | Adrb3 | adrenergic beta-3-receptor | Granneman et al., 2005 |
| 4 | Aldh1a1 | ALDH1, PUMB1, RALDH1 | Meng et al., 2014 |
| 5 | Alox15 | 15-LOX-1 | Deliri et al., 2011 |
| 6 | Amy1 | AMY1A | Mizuno et al., 2015 |
| 7 | Ankrd22 | MGC22805 | Yin et al., 2017 |
| 8 | Arg2 | Arginase, type II | Sousa et al., 2010 |
| 9 | Atp6v0d2 | ATP6D2, FLJ38708, VMA6 | Morimura et al., 2008 |
| 10 | Blnk | BASH, bca, BLNK-s, Ly57, SLP-65, SLP65 | Tan et al., 2001 |
| 11 | Bmper | CRIM3, Cv2 | Heinke et al., 2012 |
| 12 | Cacna1d | CACNL1A2, CCHL1A2, CACH3, CACN4, Cav1.3 | Chen et al., 2014c |
| 13 | Ccr3 | CMKBR3, CC-CKR-3, CD193, CKR3 | Miyagaki et al., 2011 |
| 14 | Cd5l | API6, Spalpha | You et al., 2015 |
| 15 | Cd55 | DAF, CR, CROM, TC | Yin et al., 2015 |
| 16 | Cd200 | MOX1, MOX2, MRC, OX-2 | Jung et al., 2015b |
| 17 | Chrm1 | Acetylcholine receptor, muscarinic 1 | Mannan Baig et al., 2017 |
| 18 | Clec11a | SCGF, CLECSF3, LSLCL, P47 | Hiraoka, 2008 |
| 19 | Cldn1 | ILVASC, SEMP1 | Pope et al., 2014 |
| 20 | Col3a1 | EDS4A | Su et al., 2014 |
| 21 | Col6a2 | Collagen type VI alpha 2 | Cheng et al., 2011 |
| 22 | Comp | EDM1, EPD1, PSACH, MED, THBS5, TSP5 | Hashimoto et al., 2003 |
| 23 | Cp | Ceruloplasmin, ferroxidase | Alcaín and Löw, 1997 |
| 24 | Crabp2 | CRABP-II | Liu et al., 2016b |
| 25 | Cyp7a1 | Cholesterol 7 alpha-monooxygenase | Liu et al., 2016a |
| 26 | Cyp26a1 | CP26, CYP26, P450RAI, P450RAI1 | Osanai et al., 2010 |
| 27 | Ddx3y | DBY | Kotov et al., 2017 |
| 28 | Dusp23 | DUSP25, FLJ20442 | Tang et al., 2010 |
| 29 | Eef1a2 | STN, STNL, EEF1AL, HS1 | Sun et al., 2014 |
| 30 | Eif2s3y | EIF2S3, EIF2G, EIF2, EIF2gamma | Li et al., 2016c |
| 31 | Fam107a | DRR1, TU3A | Asano et al., 2010 |
| 32 | Fblim1 | CAL, FBLP-1, migfilin | Zhao et al., 2009 |
| 33 | Fgfr1 | BFGFR, CD331, CEK, FLG, H2, H3, H4, H5, N-SAM, FLT2, KAL2 | Katoh and Nakagama, 2014 |
| 34 | Fmnl2 | FHOD2, formin-like 2 | Li et al., 2016a |
| 35 | Gas6 | AXLLG, AXSF | Jaluria et al., 2008 |
| 36 | Gata6 | GATA-binding protein 6 | Lin et al., 2012 |
| 37 | Gdf6 | BMP13, KFS, KFS1, SGM1 | Pant et al., 2013 |
| 38 | Gpha2 | GPA2, ZSIG51 | Huang et al., 2016 |
| 39 | Grb10 | Growth factor receptor-bound protein 10 | Kazi and Rönnstrand, 2013 |
| 40 | Hpn | TMPRSS1 | Xing et al., 2011 |
| 41 | Igf1 | IGF-I, IGF1A, IGFI, somatomedin C | Kasprzak et al., 2017 |
| 42 | Igf2 | IGF-II, preptin, somatomedin A | Bergman et al., 2013 |
| 43 | Il10 | CSIF, IL-10, IL10A, TGIF | Masood et al., 1995 |
| 44 | Il17rb | IL17BR, CRL4, EVI27, IL17RH1 | Alinejad et al., 2016 |
| 45 | Itga9 | ALPHA-RLC, ITGA4L, RLC | Zhang et al., 2016a |
| 46 | Itln1 | hIntL, HL-1, ITLN, LFR, omentin | Zhao et al., 2015 |
| 47 | Kcnq2 | BFNC, ENB1, HNSPC, KCNA11, Kv7.2, EBN, EBN1 | Salyer et al., 2013 |
| 48 | Lass4 | CERS4, Trh1, LAG1 homolog, ceramide synthase 4 | Chen et al., 2017 |
| 49 | Lhx4 | Gsh4 | Cha et al., 2014 |
| 50 | Ltbp1 | TGF-beta1-BP-1 | Tritschler et al., 2009 |
| 51 | Lyve1 | XLKD1, LYVE-1 | Huang et al., 2003 |
| 52 | Maged2 | 11B6, BCG1, HCA10, JCL-1, MAGE-D2, MAGED | Papageorgio et al., 2007 |
| 53 | Mmp2 | CLG4, CLG4A, TBE-1 | Chen et al., 2016a |
| 54 | Nfatc2 | NF-ATP, NFAT1, NFATp | Horsley and Pavlath, 2002 |
| 55 | Nrcam | Bravo, NgCAM-related cell adhesion molecule | Conacci-Sorrell et al., 2005 |
| 56 | Nt5e | CALJA, CD73, eN, eNT | Gao et al., 2014 |
| 57 | Nts | Neuromedin N, pro-neurotensin/neuromedin | Hu et al., 2015 |
| 58 | Pde4d | DPDE3 | Powers et al., 2015 |
| 59 | Pdk4 | – | Leclerc et al., 2017 |
| 60 | Per2 | – | Wang et al., 2016c |
| 61 | Pf4 | CXCL4, SCYB4 | Kasper et al., 2007 |
| 62 | Pon1 | Arylesterase 1, ESA | Aldonza et al., 2017 |
| 63 | Prg4 | CACP, bG174L6.2, HAPO, JCAP, MSF, SZP | Oikawa et al., 2017 |
| 64 | Prok2 | BV8, KAL4, MIT1, PK2 | Xin et al., 2013 |
| 65 | Pvrl1 | ED4, HVEC, CD111, CLPED1, HIgR, nectin, OFC7, PRR, PRR1, PVRR1, SK-12 | Bojesen et al., 2012 |
| 66 | Rab15 | – | Matsuo et al., 2014 |
| 67 | Rab37 | – | Dobashi et al., 2009 |
| 68 | Rasgrp3 | CalDAG-GEFIII, GRP3 | Nagy et al., 2014 |
| 69 | Rragd | bA11D8.2.1 | Sasaki et al., 2012 |
| 70 | S100a14 | BCMP84, S100A15 | Wang et al., 2015 |
| 71 | Serpinb1a | ELANH2, anti-elastase, EI, PI2 | Seaborn et al., 2014 |
| 72 | Serpinb2 | PAI2, PLANH2, HsT1201 | Tonnetti et al., 2008 |
| 73 | Slc2a4 | GLUT4 | Garrido et al., 2015 |
| 74 | Slco4a1 | SLC21A12, OATP-E, OATP4A1 | Ban et al., 2017 |
| 75 | Tal1 | TCL5, bHLHa17, SCL | Lacombe et al., 2013 |
| 76 | Tcf7l2 | TCF4, TCF-4 | Shitashige et al., 2008 |
| 77 | Tdo2 | TDO, TPH2 | D'Amato et al., 2015 |
| 78 | Thpo | MGDF, MPLLG, TPO | Chou et al., 2012 |
| 79 | Tnfrsf13c | BAFFR, CD268 | Fu et al., 2009 |
| 80 | Tnn | TNW, TN-N, TN-W | Chiovaro et al., 2015 |
| 81 | Trpv4 | CMT2C, OTRPC4, TRP12, VR-OAC, VRL-2, VROAC | Zhan et al., 2015 |
| 82 | Wnt5a | WNT-5A | Zhou et al., 2017 |
Genes symbols and synonyms are given in accordance to HGNC nomenclature.
Invasiveness and metastasis
Another fundamental property of malignant tumors is their ability of invasive growth and metastasis. This process commonly starts with proteolytic degradation of the basal membrane by metalloproteinases of various types, the increased expression of which is one of the main indicators of invasive tumor growth (reviewed in Jiang et al., 2015). Further, the metastasizing cell must have a number of specific properties. First, it should be able to exist in an unattached state while in the bloodstream or lymphatic vessel. This functional feature overlaps to a significant extent with the previous property to block the apoptosis, in this case–apoptosis caused by the detachment from matrix, the so-called anoykis (reviewed in Taddei et al., 2012). Second, metastasizing cell should be able to settle down and normally proliferate in the initially alien tissue environment, which can be attained through the increased expression of numerous molecules of cell adhesion, often specific for lymphoid cells (reviewed in Chong et al., 2012). And third, the cell should be able to avoid a tissue-specific immune response. This is usually being achieved, either, similarly to the previous case, by expressing specific surface markers, or by synthesizing and secreting immunosuppressive mediators and cytokines (reviewed in Kuol et al., 2017). Another important role in the invasion and metastasis is assigned to proteins that stimulate the migratory function of cells (reviewed in Bordeleau et al., 2014). This group was constituted of 64 genes promoting one or more of mentioned functional properties (Table 2).
Table 2.
Genes showing elevated expression in TAMRA+ Krebs-2 carcinoma cells relative to TAMRA− cells, the activation of which results in invasive growth and metastasis.
| Gene | Synonyms | Proving Reference | |
|---|---|---|---|
| 1 | Abca1 | ABC1, HDLDT1, TGD | Zhao et al., 2016 |
| 2 | Abca13 | – | Araújo et al., 2016 |
| 3 | Acpp | ACP-3, ACP3, PAP | Kirschenbaum et al., 2016 |
| 4 | Adamts2 | ADAM-TS2, ADAMTS-3, hPCPNI, NPI, PCINP | Akyol et al., 2015 |
| 5 | Aldh1a1 | ALDH1, PUMB1, RALDH1 | Wang et al., 2017 |
| 6 | Alox15 | 15-LOX-1 | Kerjaschki et al., 2011 |
| 7 | Arg2 | Arginase, type II | Costa et al., 2016 |
| 8 | Asb4 | ASB-4, ankyrin repeat and SOCS box-containing 4 | Au et al., 2014 |
| 9 | Bmper | CRIM3, Cv2 | Heinke et al., 2012 |
| 10 | Cacna1d | CACH3, CACN4, Cav1.3, CACNL1A2, CCHL1A2 | Alinezhad et al., 2016 |
| 11 | Ccr3 | CC-CKR-3, CD193, CKR3, CMKBR3 | Jung et al., 2010 |
| 12 | Cd55 | DAF, CR, CROM, TC | Mikesch et al., 2006 |
| 13 | Cd200 | MOX1, MOX2, MRC, OX-2 | Gorczynski et al., 2011 |
| 14 | Cldn1 | ILVASC, SEMP1 | Mahati et al., 2017b |
| 15 | Col3a1 | EDS4A | Su et al., 2014 |
| 16 | Col6a2 | Collagen type VI alpha 2 | Cheon et al., 2014 |
| 17 | Comp | EDM1, EPD1, PSACH, MED, THBS5, TSP5 | Englund et al., 2016 |
| 18 | Cp | Ceruloplasmin, ferroxidase | Kluger et al., 2004 |
| 19 | Cyp26a1 | CP26, CYP26, P450RAI, P450RAI1 | Osanai and Lee, 2015 |
| 20 | Dock10 | ZIZ3, zizimin3 | Westcott et al., 2015 |
| 21 | Dusp23 | DUSP25 | Tang et al., 2010 |
| 22 | Eef1a2 | STN, STNL, EEF1AL, HS1 | Xu et al., 2013 |
| 23 | Fam107a | DRR1, TU3A | Le et al., 2010 |
| 24 | Fblim1 | CAL, FBLP-1, migfilin | Gkretsi and Bogdanos, 2015 |
| 25 | Fgfr1 | BFGFR, CD331, CEK, FLG, H2, H3, H4, H5, N-SAM, FLT2, KAL2 | Jiao et al., 2015b |
| 26 | Fmnl2 | FHOD2 | Zhu et al., 2011 |
| 27 | Gas6 | AXLLG, AXSF | Wang et al., 2016a |
| 28 | Gata6 | – | Belaguli et al., 2010 |
| 29 | Grb10 | Growth factor receptor-bound protein 10 | Khan et al., 2015 |
| 30 | Gstm3 | GST5 | Meding et al., 2012 |
| 31 | Hpn | TMPRSS1 | Tang et al., 2014 |
| 32 | Igf1 | IGF-I, IGF1A, IGFI, somatomedin C | Lei and Ling, 2015 |
| 33 | Igf2 | IGF-II, preptin, somatomedin A | Lira et al., 2016 |
| 34 | Il10 | CSIF, IL-10, IL10A, TGIF | Zeng et al., 2010 |
| 35 | Il17rb | CRL4, EVI27, IL17RH1, IL17BR | Wu et al., 2015 |
| 36 | Itga9 | ALPHA-RLC, ITGA4L, RLC | Zhang et al., 2016a |
| 37 | Ltbp1 | TGF-beta1-BP-1 | Mercado-Pimentel and Runyan, 2007 |
| 38 | Lyve1 | XLKD1, LYVE-1 | Prevo et al., 2001 |
| 39 | Maged2 | 11B6, BCG1, HCA10, JCL-1, MAGE-D2, MAGED | Kanda et al., 2016 |
| 40 | Mmp2 | CLG4, CLG4A, TBE-1 | Xuan et al., 2015 |
| 41 | Mycbpap | AMAP-1 | Sabe et al., 2009 |
| 42 | Myo1b | myr1 | Ohmura et al., 2015 |
| 43 | Nfatc2 | NF-ATP, NFAT1, NFATp | Jauliac et al., 2002 |
| 44 | Nrcam | Bravo, NgCAM-related cell adhesion molecule | Zhang et al., 2017 |
| 45 | Nt5e | CALJA, CD73, eN, eNT | Wang et al., 2008 |
| 46 | Nts | neuromedin N, pro-neurotensin/neuromedin | Ye et al., 2014 |
| 47 | Pde4d | DPDE3 | Delyon et al., 2017 |
| 48 | Pdk4 | – | Leclerc et al., 2017 |
| 49 | Per2 | – | Li et al., 2016d |
| 50 | Pon1 | Arylesterase 1, ESA | Aldonza et al., 2017 |
| 51 | Ppap2b | PLPP3, LPP3, PAP-2b | Westcott et al., 2015 |
| 52 | Rasgrp3 | CalDAG-GEFIII, GRP3 | Zeng et al., 2014 |
| 53 | S100a14 | BCMP84, S100A15 | Wang et al., 2015 |
| 54 | Selp | GRMP, CD62P, GMP140, PADGEM, PSEL | Stübke et al., 2012 |
| 55 | Serpinb2 | PAI2, PLANH2, HsT1201 | Jin et al., 2017a |
| 56 | Slco4a1 | SLC21A12, OATP-E, OATP4A1 | Ban et al., 2017 |
| 57 | Tal1 | TCL5, bHLHa17, SCL | Correia et al., 2016 |
| 58 | Tcf7l2 | TCF4, TCF-4 | Ravindranath et al., 2008 |
| 59 | Tdo2 | TDO, TPH2 | D'Amato et al., 2015 |
| 60 | Tnn | TNW, TN-N, TN-W | Chiovaro et al., 2015 |
| 61 | Tnxb | TNXB1, TNXB2, TNXBS, XB, XBS | Hu et al., 2009 |
| 62 | Trpv4 | CMT2C, OTRPC4, TRP12, VR-OAC, VRL-2, VROAC | Lee et al., 2017b |
| 63 | Vsig4 | Z39IG | Zhang et al., 2016c |
| 64 | Wnt5a | WNT-5A | Shojima et al., 2015 |
Genes symbols and synonyms are given in accordance to HGNC nomenclature.
Drug resistance
One of important, if not the most important, problems in clinical oncology is the resistance of tumors to antitumor drugs. When in the 50s of the last century this phenomenon had started to be actively investigated, the drug resistance was believed to be an adaptive response that develops as a result of tumor cells selection under long-term exposure to a certain drug. It was generally accepted to associate the drug resistance with an elevated level of expression of enzymes responsible for xenobiotics metabolism, such as P450 family oxygenases (reviewed in Harvey and Morgan, 2014), and specific transmembrane transport proteins providing efflux of xenobiotics and their metabolites (reviewed in Chen et al., 2016b). However, more recent observations have revealed that very often drug resistance is initially intrinsic to a certain subpopulation of tumor cells and is associated not only with the above-mentioned causes (reviewed in Gottesman, 2002). The main effect of antitumor drugs is known to be associated with their either cytostatic or cytotoxic properties, which in turn are mainly realized through DNA damage and should activate apoptotic processes. Accordingly, activation of mechanisms allowing to overcome G1/S arrest or blocking the realization of the apoptotic program, increases the resistance of tumor cells to chemotherapy (Volm, 1998). Moreover, the DNA-damaging effect of chemotherapeutic agents is neutralized by the cellular systems of antioxidative defense (reviewed in Victorino et al., 2014). And, finally, in the very end of the last century, another mechanism of tumors drug resistance—the so-called Cell-Adhesion Mediated Drug Resistance (CAM-DR) was discovered (reviewed in Dalton, 1999). This mechanism, in fact, represents a complex adaptive response that comprises the increased resistance to apoptosis due to anti-apoptotic signals from integrins (Damiano, 2002), reduced tumor permeability for chemotherapeutic agents (Kerbel et al., 1996; Grantab and Tannock, 2012), and formation of syncytium, which also leads to increased drug resistance (Lu and Kang, 2009; Nagler et al., 2011; Mittal et al., 2017). We found the evidences of anticancer therapy resistance inducing activity for 38 genes (Table 3).
Table 3.
Genes showing elevated expression in TAMRA+ Krebs-2 carcinoma cells relative to TAMRA− cells, the activation of which results in increased resistance of cells to xenobiotics and anti-tumor drugs.
| Gene | Synonyms | Proving reference | |
|---|---|---|---|
| 1 | Abca1 | ABC1, HDLDT1, TGD | Hou et al., 2017 |
| 2 | Abca9 | – | Chen et al., 2009 |
| 3 | Abca13 | – | Hlavata et al., 2012 |
| 4 | Aldh1a1 | ALDH1, PUMB1, RALDH1 | Jiang et al., 2016 |
| 5 | Aldh1l1 | FTHFD, 10-fTHF | Hartomo et al., 2015 |
| 6 | Amy1 | AMY1A | Mizuno et al., 2015 |
| 7 | Cd55 | DAF, CR, CROM, TC | Saygin et al., 2017 |
| 8 | Cd200 | MOX1, MOX2, MRC, OX-2 | Jung et al., 2015b |
| 9 | Cldn1 | ILVASC, SEMP1 | Zhao et al., 2017 |
| 10 | Col3a1 | EDS4A | Januchowski et al., 2016 |
| 11 | Col6a2 | Collagen type VI alpha 2 | Januchowski et al., 2016 |
| 12 | Cp | Ceruloplasmin, ferroxidase | Chekhun et al., 2014 |
| 13 | Cyp7a1 | Cholesterol 7 alpha-monooxygenase | Eloranta and Kullak-Ublick, 2005 |
| 14 | Fgfr1 | BFGFR, CD331, CEK, FLG, H2, H3, H4, H5, N-SAM, FLT2, KAL2 | Cole et al., 2010 |
| 15 | Gas6 | AXLLG, AXSF | Wang et al., 2016a |
| 16 | Gstm3 | GST5 | Black et al., 1990 |
| 17 | Grb10 | Growth factor receptor-bound protein 10 | Roszak et al., 2013 |
| 18 | Igf1 | IGF-I, IGF1A, IGFI, somatomedin C | Kikuchi et al., 2015 |
| 19 | Igf2 | IGF-II, preptin, somatomedin A | Wozniak et al., 2015 |
| 20 | Il10 | CSIF, IL-10, IL10A, TGIF | Park et al., 2009 |
| 21 | Lyve1 | XLKD1, LYVE-1 | Qin et al., 2011 |
| 22 | Nfatc2 | NF-ATP, NFAT1, NFATp | Griesmann et al., 2013 |
| 23 | Nt5e | CALJA, CD73, eN, eNT | Loi et al., 2013 |
| 24 | Nts | Neuromedin N, pro-neurotensin/neuromedin | Vias et al., 2007 |
| 25 | Pde4d | DPDE3 | Miklos et al., 2016 |
| 26 | Pdk4 | – | Zhang et al., 2016d |
| 27 | Pf4 | CXCL4, SCYB4 | Han et al., 1997 |
| 28 | Per2 | – | Mitchell and Engelbrecht, 2015 |
| 29 | Pon1 | Arylesterase 1, ESA | Aldonza et al., 2017 |
| 30 | Rasgrp3 | CalDAG-GEFIII, GRP3 | Nagy et al., 2014 |
| 31 | Selp | GRMP, CD62P, GMP140, PADGEM, PSEL | Zheng et al., 2013 |
| 32 | Serpinb2 | PAI2, PLANH2, HsT1201 | Taoka et al., 2015 |
| 33 | Slco4a1 | SLC21A12, OATP-E, OATP4A1 | Brenner et al., 2015 |
| 34 | Tal1 | TCL5, bHLHa17, SCL | Bernard et al., 1998 |
| 35 | Tnn | TNW, TN-N, TN-W | Fukunaga-Kalabis et al., 2010 |
| 36 | Tubb1 | Class VI beta-tubulin | Li et al., 2014 |
| 37 | Vsig4 | Z39IG | Zhang et al., 2016c |
| 38 | Wnt5a | WNT-5A | Hung et al., 2014 |
Genes symbols and synonyms are given in accordance to HGNC nomenclature.
Classification of genes contributing to tamra+ krebs-2 carcinoma cells malignancy with regard to their functional role in the formation of the tumorigenicity hallmarks
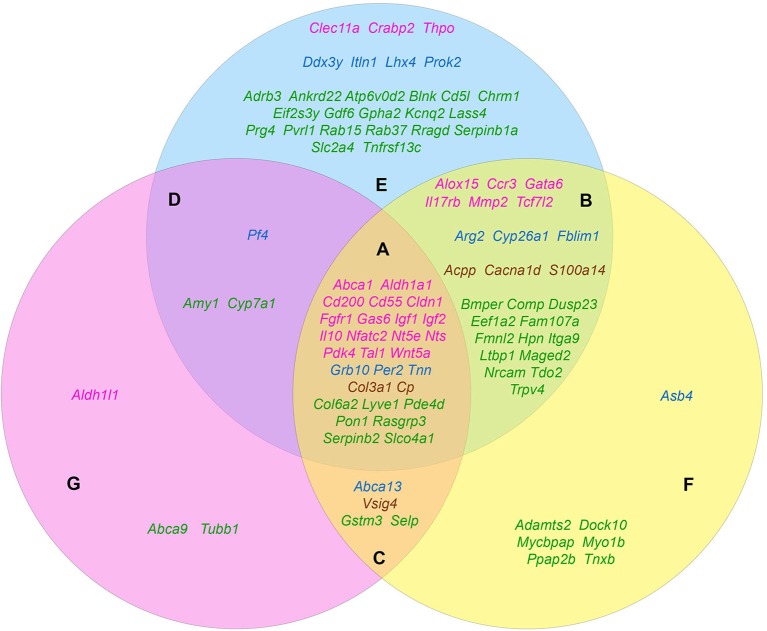
The carried out data mining showed that out of 167 genes we tested, at least 96 belong to at least one of the three groups by their functional role in the formation of the tumorigenic phenotype. Herewith, all these genes in a completely natural way were dispensed into 7 additional groups. Group A (28 genes): Abca1, Aldh1a1, Cd55, Cd200, Cldn1, Col3a1, Col6a2, Cp, Fgfr1, Gas6, Grb10, Igf1, Igf2, Il10, Lyve1, Nfatc2, Nt5e, Nts, Pde4d, Pdk4, Per2, Pon1, Rasgrp3, Serpinb2, Slco4a1, Tal1, Tnn, Wnt5a—genes contributing to the formation of all three features. Group B (25 genes): Acpp, Alox15, Arg2, Bmper, Cacna1d, Ccr3, Comp, Cyp26a1, Dusp23, Eef1a2, Fam107a, Fblim1, Fmnl2, Gata6, Hpn, Il17rb, Itga9, Ltbp1, Maged2, Mmp2, Nrcam, S100a14, Tcf7l2, Tdo2, Trpv4—genes that simultaneously provide proliferative self-sufficiency and invasive growth/metastasis. Group C (4 genes): Abca13, Gstm3, Selp, Vsig4—genes that confer the drug resistance along with the metastatic phenotype. Group D (3 genes): Amy1, Cyp7a1, Pf4—genes responsible for proliferative self-sufficiency and drug resistance. Group E (26 genes): Adrb3, Ankrd22, Atp6v0d2, Blnk, Cd5l, Chrm1, Clec11a, Crabp2, Ddx3y, Eif2s3y, Gdf6, Gpha2, Itln1, Kcnq2, Lass4, Lhx4, Prok2, Prg4, Pvrl1, Rab15, Rab37, Rragd, Serpinb1a, Slc2a4, Thpo, Tnfrsf13c—genes responsible for proliferative self-sufficiency solely. Group F (7 genes): Adamts2, Asb4, Dock10, Mycbpap, Myo1b, Ppap2b, Tnxb—genes-inducers of invasive growth and metastasis. Group G (3 genes): Abca9, Aldh1l1, Tubb1—drug resistance genes (Figure 1).
Figure 1.
The distribution pattern of genes, overexpressed in TAMRA+ Krebs-2 carcinoma cells relative to TAMRA− cells, to functional groups. The blue area corresponds to the proliferative self-sufficiency, yellow, to invasiveness and metastasis; pink, to drug resistance. (A–F) Sections indicate the subgroups of the genes with regard to their multi-functionality: (A) the most multi-functional genes contributing to all three properties; (B) genes contributing to proliferative self-sufficiency and invasive growth/metastasis; (C) genes contributing to drug resistance and metastatic phenotype; (D) genes contributing to proliferative self-sufficiency and drug resistance; (E) genes contributing to proliferative self-sufficiency; (F) genes contributing to invasive growth and metastasis; (G) genes contributing to drug resistance. The genes symbols are indicated in different colors in accordance with their proven functional role in the formation of the stem or stem-like phenotype of normal pluri-/multipotent as well as tumor stem cells: pink denoting genes that are known markers of both normal pluri-/multipotent and tumor stem cells; blue, known markers of normal pluri-/multipotent stem cells; brown, known markers of tumor stem cells; green, genes for which their participation in the formation of stemness has not been proven at all.
Since the genes of the first four groups are “polyfunctional,” i.e., impact two or more properties simultaneously, it is logical to conclude that they contribute significantly greater (in comparison to the genes of the remaining three groups) to the formation of highly tumorigenic phenotype of the TAMRA+ cells. This makes them to be the most plausible candidates for the role of the main genetic markers of CSCs as well as malignancy itself. Moreover, the composed molecular-genetic “portrait,” emphasizing the differences of these cells from the bulk of tumor cells, gives additional reasons to believe that the main properties of tumor malignancy are determined precisely by CSCs.
Formation and maintenance of stemness
Since the term “cancer stem cell” was introduced to designate a certain subpopulation of tumor cells on the basis of their phenotypic and functional similarity to normal pluri-/multipotent stem cells, it was initially assumed that there could be some common molecular-genetic mechanisms that provide such a similarity (Reya et al., 2001). Indeed, such stem cell-specific signaling pathways as, for example, Wnt-, Notch-, and Shh-dependent ones, have been demonstrated to be involved in development of various human and murine tumors (Ellisen et al., 1991; Henrique et al., 1997; Korinek et al., 1998; Chan et al., 1999; Wechsler-Reya and Scott, 1999, 2001; Zhang and Kalderon, 2001).
In this connection, we have considered it to be interesting to search the existing literature for evidences of the functional involvement of the identified genes-inducers of highly tumorigenic phenotype of the TAMRA+ cells in maintaining the stemness of normal pluri-/multipotent cells. In addition, we evaluated the involvement of these genes in the formation and maintenance of the stem-like phenotype of tumor cells.
Based on the screening results, 45 genes were assigned to the category of “stemness markers,” which makes up 46% of the analyzed and 27% of the total (167) genes differentially overexpressed in TAMRA+ cells of the Krebs-2 carcinoma. Herewith, more than half of these genes, namely 27 out of 45, are known to be implicated in maintenance and functional realization of stem properties of both tumor and normal pluripotent cells. However, four of these genes were included in this group with some reservations. Thus, for Cd55 and Il10, no direct contribution to the formation or maintenance of stemness of normal pluri-/multipotent cells was proved, but the essential role in the realization of the reparative functions of mesenchymal and autologous-induced pluripotent stem cells by dint of the immunosuppressive action of the protein products of these genes was demonstrated (Ardianto et al., 2010; Liu et al., 2012; de Almeida et al., 2014; Lee et al., 2015b). The role of Nts in the formation of the pluripotent phenotype has been proved only in the case of the so-called induced pluripotent cells (Cai et al., 2015). And, finally, for Crabp2 there was no direct evidence of its participation in the formation of stemness, but only demonstration of specific expression in normal human amniotic fluid-derived stem cells and in polycythemia vera-derived tumor stem cells (Steidl et al., 2005; Kim et al., 2010). In conjunction with its role in the metabolism of retinoic acids and their derivatives, this makes it to be attractive as a plausible marker of stemness for both tumor and normal stem cells.
Six more genes were identified as established markers of tumor-initiating stem cells. The remaining 12 genes were associated exclusively with normal pluripotent and multipotent stem cells, although, again, with some reservations. So, for Abca13 only specific expression in early human embryonic stem cells, decreasing during consecutive passages has been shown (Barbet et al., 2012), while for Arg2, as well as for the above Cd55 and Il10, its functional role is limited to the immunosuppressive effect necessary to overcome tissue-specific immunity by stem cells as it was shown for human pluripotent cells (Chen et al., 2015b). The results of the screening are summarized in Table 4.
Table 4.
Genes showing elevated expression in TAMRA+ Krebs-2 carcinoma cells relative to TAMRA− cells, and participating in formation and maintenance of stem properties of tumorigenic as well as normal pluri-/multipotent stem cells.
| Gene | Proof for the role in CSCs formation and maintenance | Proof for the role in normal pluri-/multi-potent stem cells formation and maintenance | |
|---|---|---|---|
| 1 | Abca1 | Sun et al., 2015 | Peeters et al., 2006 |
| 2 | Abca13 | N/C | Barbet et al., 2012 |
| 3 | Aldh1a1 | Yang et al., 2014c | Dey et al., 2015 |
| 4 | Aldh1l1 | Hartomo et al., 2015; Wang et al., 2016d | Foo and Dougherty, 2013 |
| 5 | Acpp | Liu et al., 2014 | N/C |
| 6 | Alox15 | Chen et al., 2014d | Kinder et al., 2010 |
| 7 | Arg2 | N/C | Chen et al., 2015b |
| 8 | Asb4 | N/C | Yang et al., 2014b |
| 9 | Cacna1d | Gerber et al., 2013 | N/C |
| 10 | Ccr3 | Long et al., 2012 | Krathwohl, 2004 |
| 11 | Cd55 | Saygin et al., 2017 | Ardianto et al., 2010 |
| 12 | Cd200 | Jung et al., 2015b | Wang et al., 2014 |
| 13 | Cldn1 | Mahati et al., 2017a | Zinner et al., 2013 |
| 14 | Clec11a | Hiraoka, 2008 | Hiraoka et al., 2001 |
| 15 | Col3a1 | Januchowski et al., 2016 | N/C |
| 16 | Cp | Tye et al., 2008; Brandi et al., 2016 | N/C |
| 17 | Crabp2 | Kim et al., 2010 | Steidl et al., 2005 |
| 18 | Cyp26a1 | N/C | Assou et al., 2007 |
| 19 | Ddx3y | Rosinski et al., 2008 | Kotov et al., 2017 |
| 20 | Fblim1 | N/C | Xiao et al., 2012 |
| 21 | Fgfr1 | Ji et al., 2016 | Coutu et al., 2011 |
| 22 | Gas6 | Jin et al., 2017b | Gely-Pernot et al., 2012 |
| 23 | Gata6 | Whissell et al., 2014 | Kubo et al., 2009 |
| 24 | Grb10 | N/C | Li et al., 2017a |
| 25 | Igf1 | Bu et al., 2014 | Li et al., 2010b |
| 26 | Igf2 | Tominaga et al., 2017 | Bendall et al., 2007 |
| 27 | Il10 | Tuccitto et al., 2016 | Liu et al., 2012; de Almeida et al., 2014; Lee et al., 2015b |
| 28 | Il17rb | Bie et al., 2016 | Bie et al., 2017 |
| 29 | Itln1 | N/C | Zhao et al., 2015 |
| 30 | Lhx4 | N/C | Chen et al., 2005 |
| 31 | Mmp2 | Sun et al., 2013; An et al., 2015 | Huang et al., 2011 |
| 32 | Nfatc2 | Perotti et al., 2016 | Kiani et al., 2004 |
| 33 | Nt5e | Katsuta et al., 2016 | Corradetti et al., 2013 |
| 34 | Nts | Zhou et al., 2014 | Cai et al., 2015 |
| 35 | Pdk4 | Song et al., 2015 | Takubo et al., 2013 |
| 36 | Per2 | N/C | Boucher et al., 2016 |
| 37 | Pf4 | N/C | Han et al., 1997; Calaminus et al., 2012; Chen et al., 2014b |
| 38 | Prok2 | N/C | LeCouter et al., 2004 |
| 39 | S100a14 | Leth-Larsen et al., 2012; Ko et al., 2013 | N/C |
| 40 | Tal1 | Gerby et al., 2016 | Baharvand et al., 2006; Souroullas et al., 2009 |
| 41 | Tcf7l2 | Chen et al., 2015a | Quan et al., 2016 |
| 42 | Thpo | Chou et al., 2012 | Kohlscheen et al., 2015 |
| 43 | Tnn | N/C | Tucker et al., 2013 |
| 44 | Vsig4 | Zhang et al., 2016c | N/C |
| 45 | Wnt5a | Zhou et al., 2017 | Hao et al., 2006 |
Malignancy and pluripotency: looking for difference
Identification of such an entity as a CSC has allowed to apply the principles of organogenesis to the development of tumors. From this point of view, the tumor is considered to be an aberrant organ, developing from a tumor cell possessing an infinite proliferative potential and a poorly differentiated stem-like phenotype (Reya et al., 2001). This approach implies the existence of functional analogies between normal stem cells involved in embryogenesis and tumor stem cells. Taking into account the functional purpose of normal pluri-/multipotent cells, their basic physiological properties can be deduced. First, it is obvious that the stem cell must possess a certain degree of proliferative autonomy and increased survival abilities to realize the function of the population self-maintenance. Second, the stem cell must evince active migratory and immunosuppressive functions, as well as the multiple tissue adherence to realize its genesis/reparative/regenerative functions. And third, the stem cell must have a well developed system of detoxification and resistance to xenobiotics, to keep the genome of both its own and the population as a whole intact. i.e., the attributes of stemness and the ones of malignancy, which we defined above, are the same, at least in the first approximation, and, respectively, the molecular-genetic mechanisms that determine these two characteristics can overlap to a significant degree.
Based on Table 4 and Figure 1 data, it can be noted that 21 of the 45 stemness marker genes got into Group A, which includes 28 genes that are most important for the formation of TAMRA+ cells malignancy. That is, this group substantially (75%) consists of the genes essential for the formation and maintenance of stem properties. At this, only two genes are identified as indicators of the stem-like phenotype of tumor cells, while the remaining 19 are necessary for the functioning of normal pluri-/multipotent stem cells. Another 12 genes were included into group B consisting of a total of 25 genes, while the rest were more or less evenly distributed over the remaining five groups.
Thus, the identity of genes determining the malignant properties of tumor-initiating cells and the stem properties of normal pluri-/multipotent stem cells has been revealed. Molecular-genetic identity of tumor-initiating and normal stem cells, as well as their morphophysiological one, gave us a reason to presume the identity of the very properties of malignancy and pluripotency themselves, that can be also designated as the properties of “independent behavior.” Up to the day, a significant number of evidences confirming the presumed behavioral identity of both types of cells has been presented. Thus, for example, it had been shown that transplantation of human embryonic stem cells, as well as of diploid and aneuploid pluripotent ones can lead to the development of tumors, most commonly identified as benign teratomas or malignant teratocarcinomas (Blum and Benvenisty, 2008, 2009). This property is postulated to be the hallmark of all pluripotent stem cell types, which demonstrates their potential to differentiate in all tissue types (reviewed in Dressel, 2011). On the other hand, classical experiments on the inoculation of teratocarcinomas cells into mouse embryos at the early stages of development have shown that, getting into the “right” conditions, malignant cells can differentiate into normal tissue, resulting in the development of a normal mosaic organism (Martin and Evans, 1975; Mintz and Illmensee, 1975; Illmensee and Mintz, 1976).
In other words, all these facts could mean that malignancy and stemness/pluripotency are one and the same entity, and the way this entity could be realized—malignancy or normal stemness—depends on the cellular microenvironment that provides the mentioned “right” location and conditions. And it is the stem cell niche that is apparently to be the appropriate location with appropriate conditions.
Initially, the term “stem cell niche” was proposed by Schofield in 1978 to describe a hypothetical cellular structure that provides conditions for the existence of a stem cell in which it is able to maintain its basic properties of self-renewal and maintenance of an undifferentiated or poorly differentiated state (Schofield, 1978). In its contemporary meaning, the role of the stem niche is dedicated to two basic functions. The first is to maintain the population of stem cells at a certain level by balancing pro-mitogenic and anti-mitogenic signals and providing a specific microenvironment necessary to maintain the undifferentiated state of stem cells (Schofield, 1983; Lin, 2002; Ohlstein et al., 2004; reviewed in Li and Neaves, 2006). The second is to act as a kind of “Maxwell's demon,” allowing niche exit to committed precursor cells, but not stem ones (reviewed in Marthiens et al., 2010). The last function has its reverse. The implication is that if a stem cell leaves the niche for any reason, it must either go back—the so-called “homing” known for hematopoietic stem cells, which can leave the stem niche for a while and then return (Whetton and Graham, 1999), or lose stemness and switch to a committed state, which, finally, ends with differentiation (Voog and Jones, 2010; O'Brien and Bilder, 2013). Simply stated, stem cells could not exist outside the stem cell niche. The main, as well as the only difference between CSCs and normal stem cells which is, in fact, the property of malignancy itself, is the ability to form and maintain stem/pluripotent properties outside a specific niche. This property comprises the defiance to morphogenetic signals from normal cellular and stromal environment and, as a consequence, the ability to form the tumorous stroma as well as the tumor itself in any tissue of the organism independently on the local environmental conditions.
Summarizing the section it should be said that the search for mechanisms providing such “independent behavior” of the CSCs is the principal priority in fundamental molecular oncology for now.
Cancer stem cells: ultima ratio of tumors?
The hypothesis of “dynamic stemness” presumes the inducibility of stem-like phenotype in some subpopulation of “committed” tumor cells. It seems to be logical that such an induction and the following de novo appearance of CSCs occurs rather due to certain changes in cellular humoral or stromal environment. Thus, revealing the genes responsible for the stemness of TAMRA+ cells of the Krebs-2 carcinoma allows, in addition to the above, to deduce both the causes and mechanisms of induction of the stem-like phenotype in some part of the tumor cells.
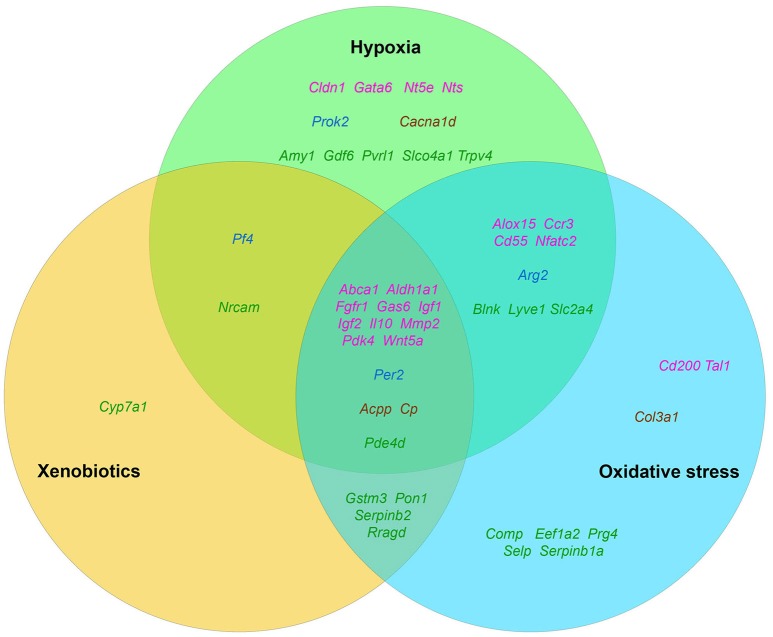
“Generalized cellular stress” as an activator of “stemness genes”
It is well known that tumor growth and development is always accompanied by a number of stress factors. The first of them is the formation of hypoxia foci (Moulder and Rockwell, 1987; reviewed in Bertout et al., 2008). The second one is the oxidative stress, which develops due to various inflammatory and immune reactions (reviewed in Murr et al., 1999; Laviano et al., 2007). And, finally, an increased level of endogenous xenobiotics, such as, for example, kynurenine (Kurz et al., 2011), that are able to activate both AhR (Poormasjedi-Meibod et al., 2016) and other xenosensors. Accordingly, we decided to check the published data in order to find out how much these stress factors are capable of activating the stemness of tumor cells in general as well as the expression of selected “stemness genes” in particular (Figure 2).
Figure 2.
The distribution pattern of genes, overexpressed in TAMRA+ Krebs-2 carcinoma cells relative to TAMRA− cells, with regard to their activation in response to appropriate stimulus. The green area corresponds to hypoxia, blue–to oxidative stress, orange–to xenobiotics. The genes symbols are indicated in different colors in accordance with their proven functional role in the formation of the stem or stem-like phenotype of normal pluri-/multipotent as well as tumor stem cells: pink denoting genes that are known markers of both normal pluri-/multipotent and tumor stem cells; blue–known markers of normal pluri-/multipotent stem cells; brown–known markers of tumor stem cells; green–genes for which their participation in the formation of stemness has not been proven at all.
The fact that hypoxia is a strong stimulus that enhances the aggressive behavior of tumors had been known for a long time (reviewed in Bertout et al., 2008). More recent studies have shown that hypoxia is mandatory for the existence of normal embryonic and other pluri-/multipotent stem cells (Mohyeldin et al., 2010; López-Iglesias et al., 2015; Hammoud et al., 2016), and induces the stem-like phenotype in prostate cancer (Bae et al., 2016), human lung cancer (Iida et al., 2012) and other types of tumors (reviewed in Li and Rich, 2010; Seo et al., 2016). The existing data analysis has revealed that 35 of the 96 genes we have identified as essential for stemness are activated, one way or another, in conditions of local or systemic hypoxia (Table 5, Figure 2).
Table 5.
The results of the analysis of published data on activating effect of the factors of generalized cellular stress for the tested genes that provide a malignant/pluripotent phenotype of the Krebs-2 CSCs.
| Activated genes | Components of generalized cellular stress | ||
|---|---|---|---|
| Hypoxia | Oxidative stress | Xenobiotics | |
| 48 genes | 35 genes | 34 genes | 21 genes |
| Abca1 | Plösch et al., 2010 | Davies et al., 2015 | Ma and Liu, 2012 |
| Acpp | Liu et al., 2014 | Obianime and Roberts, 2009 | Obianime and Roberts, 2009 |
| Aldh1a1 | Hough and Piatigorsky, 2004 | Strzalka-Mrozik et al., 2013 | Hough and Piatigorsky, 2004 |
| Alox15 | Lundqvist et al., 2016 | Jung et al., 2015a | N/C |
| Amy1 | Jam et al., 1978 | N/C | N/C |
| Arg2 | Chen et al., 2014a | Touyz, 2014 | N/C |
| Blnk | Han et al., 2001 | Han et al., 2001 | N/C |
| Cacna1d | Li et al., 2015 | N/C | N/C |
| Ccr3 | Ricciardi et al., 2008 | Michalec et al., 2002 | N/C |
| Cd200 | N/C | Gupta et al., 2014 | N/C |
| Cd55 | Botto et al., 2008 | Iborra et al., 2003 | N/C |
| Cldn1 | Brown et al., 2003 | N/C | N/C |
| Col3a1 | N/C | Luna et al., 2009 | N/C |
| Comp | N/C | Wahba et al., 2016 | N/C |
| Cp | Martin et al., 2005 | Dzugkoeva et al., 2016 | Auslander et al., 2008 |
| Cyp7a1 | N/C | N/C | Lambert et al., 2009 |
| Eef1a2 | N/C | Chen et al., 2000 | N/C |
| Fgfr1 | Ganat et al., 2002; Mouillet et al., 2013 | Alizadeh et al., 2001 | Łazarenkow et al., 2017 |
| Gas6 | Mishra et al., 2012 | Tsai et al., 2016 | Bruchova et al., 2010 |
| Gata6 | Hsiao et al., 2015 | N/C | N/C |
| Gdf6 | Li et al., 2013 | N/C | N/C |
| Gstm3 | N/C | Gibson et al., 2014 | Li et al., 2016b |
| Igf1 | Yang et al., 2015 | Jiao et al., 2015a | Wohlfahrt-Veje et al., 2014 |
| Igf2 | Jögi et al., 2004 | Yang et al., 2014a | Wang et al., 2011 |
| Il10 | Xu et al., 2016 | Joseph Martin and Evan Prince, 2017 | Pacheco et al., 2001; Khalil et al., 2010 |
| Lyve1 | Chaudary et al., 2011 | Jiao et al., 2015a | N/C |
| Mmp2 | Slevin et al., 2009 | Liu et al., 2017 | Kamaraj et al., 2010 |
| Nfatc2 | Wang et al., 2016b | Nomura et al., 2011 | N/C |
| Nrcam | Slevin et al., 2009 | N/C | Gato et al., 2012 |
| Nt5e | Fu and Davies, 2015 | N/C | N/C |
| Nts | Shen and Wang, 1998 | N/C | N/C |
| Pde4d | Pullamsetti et al., 2013 | Kim et al., 2017 | Yeo et al., 2017 |
| Pdk4 | Van Thienen et al., 2017 | Lake et al., 2016 | Luckhurst et al., 2011 |
| Per2 | Peek et al., 2017 | Davis et al., 2017 | Manzella et al., 2013 |
| Pf4 | Shen and Wang, 1994 | N/C | Sithu et al., 2010 |
| Pon1 | N/C | Desai et al., 2014 | Gouédard et al., 2004 |
| Prg4 | N/C | Lee et al., 2015a | N/C |
| Prok2 | LeCouter et al., 2003 | N/C | N/C |
| Pvrl1 | Friedman et al., 2012 | N/C | N/C |
| Rragd | N/C | Sasaki et al., 2012 | Sasaki et al., 2012 |
| Selp | N/C | Takano et al., 2002 | N/C |
| Serpinb1a | N/C | Frühbeck et al., 2010 | N/C |
| Serpinb2 | N/C | Leeuwen et al., 2006; Vo et al., 2011 | Brauze et al., 2017 |
| Slc2a4 | Royer et al., 2000 | Li et al., 2010a | N/C |
| Slco4a1 | Applebaum et al., 2016 | N/C | N/C |
| Tal1 | N/C | Ogino et al., 2014 | N/C |
| Trpv4 | Wu et al., 2017 | N/C | N/C |
| Wnt5a | Chen et al., 2006 | Andersson-Sjöland et al., 2016 | Hrubá et al., 2011 |
Data on the role of oxidative stress in regulation of tumor cells stemness are in general quite contradictory. Numerous studies confirm suppression of the stem-like phenotype of tumor cells under oxidative stress conditions in, for example, in vitro experiments with SUM159 breast cancer cells and pancreatic CSCs of various origin (Cipak et al., 2010; Ma et al., 2017). On the other hand there are numerous quite convincing direct evidences of stemness induction in response to oxidative stress, as, for example, in MCF7 and ZR751 breast cancer cells (Gopal et al., 2016) or in lung cancer cells (Saijo et al., 2016) as well as in a number of other in vitro models (reviewed in Dayem et al., 2010). We found the evidences of oxidative stress activating effect for 34 genes of our list (Table 5, Figure 2).
Finally, we have found data, albeit not numerous, confirming that xenobiotics are also able to induce the stemness of tumor cells. This was shown, for example, for human bronchial epithelial cells (Liu et al., 2016c) and SUM149 inflammatory breast cancer cells (Stanford et al., 2016). As well, xenobiotics turned out to activate the expression of 21 out of 96 genes of stemness of TAMRA+ cells of the Krebs-2 tumor (Table 5, Figure 2).
Thus, the datamining analysis showed that 48 of the 96 genes we designated as potentially important for the formation of the poorly differentiated/stem-like phenotype of tumor cells are activated in response to at least 1 of 3 stress stimuli–hypoxia, oxidative stress, or xenobiotics. Moreover, 14 genes (Aldh1a1, Abca1, Igf1, Igf2, Il10, Gas6, Fgfr1, Wnt5a, Pdk4, Per2, Cp, Pde4d, Mmp2, Acpp) respond with increased expression to all 3 stimuli. It is easy to note that 12 of these 14 genes belong to group A (Figure 1), which contains genes most significant for maintaining stemness/malignancy. Moreover, visual representation of these results in Figure 2 signifies the multiplicity of inducing agents for the majority of stemness-specific genes (pink, blue, and brown denoted ones).
It is known that none of the mentioned stress stimuli exist separately in vivo, instead they are always inextricably linked to each other. So, hypoxia, as well as the presence of xenobiotics, lead to oxidative stress (Netzer et al., 2015; Pizzino et al., 2017). On the other hand, oxidative stress leads to a corruption in metabolism that, in turn, causes the formation of various endogenous xenobiotics such as kynurenine (Ramírez-Ortega et al., 2017; Wigner et al., 2018) or tryptamine-4,5-dione (Jiang et al., 1999; Suga et al., 2017). Therefore, we decided to combine these three stress factors into the single concept of “generalized cellular stress.”
Roads to rome: molecular mechanisms of stemness induction
It is quite obvious that the fact that we have not found any data on the impact of generalized cellular stress on the remaining 48 genes does not mean that there really is no such an influence. Our hypothesis on the role of stress in the activation of stemness could be to some extent supported by data on the presence of regulatory elements that provide the binding of transcription factors and transcriptional activation of these genes in response to factors of generalized cellular stress. To conduct such analysis, we used the open web resource “Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool”: http://amp.pharm.mssm.edu/Enrichr/ (Chen et al., 2013; Kuleshov et al., 2016). Databases of this tool contain an excessive compilation of a huge number of results obtained in the ChIP-Seq (Chromatin ImmunoPrecipitation-Sequencing) experiments. It allows to use the tool not only to determine the degree of sampling enrichment by the criterion of the presence of functional binding sites for certain transcription factors, but also in principle to determine the presence of such sites in the subject genes. So we used the “ChEA 2016” section of the tool to test all 96 “stemness genes” for the presence of binding sites for transcription factors established by experiments on ChIP-Seq analysis. One of the main outcomes of this analysis was that the 72 genes from our list contain binding sites for the SOX2 transcription factor, 59–OCT4/POU5F1, 54–NANOG, 45–KLF4, and 52–c-MYC (Table 6). In fact, only 7 genes out of 96 (Lyve1, Il17rb, Fam107a, Nrcam, Vsig4, Pf4, Amy1, Eif2s3y) contained no binding sites for any of the listed factors.
Table 6.
Results of “ChEA 2016” analysis for 96 ≪stemness genes≫ showing elevated expression in TAMRA+ Krebs-2 carcinoma cells relative to TAMRA− cells, with regard to enrichment with SOX2/OCT4/POU5F1/NANOG/KLF4/c-MYC binding sites.
| TrF | Overlap | P-value | Genes |
|---|---|---|---|
| SOX2 | 21/2564 | 0.009245 | Arg2; Crabp2; Ankrd22; Pde4d; Gata6; Cldn1; Dusp23; Myo1b; Nt5e; Fmnl2; Rab15; Ppap2b; Aldh1a1; Rragd; Pdk4; Maged2; Asb4; S100a14; Gas6; Cd55; Fgfr1 |
| SOX2 | 17/1991 | 0.013342 | Il10; Gstm3; Tcf7l2; Fblim1; Wnt5a; Alox15; Clec11a; Igf1; Tnfrsf13c; Nt5e; Adrb3; Ppap2b; Kcnq2; Rragd; Blnk; Asb4; Fgfr1 |
| SOX2 | 16/2000 | 0.028265 | Il10; Serpinb2; Itln1; Nfatc2; Prg4; Dock10; Selp; Per2; Dusp23; Col3a1; Myo1b; Fmnl2; Tnn; Kcnq2; Lhx4; Cd55 |
| SOX2 | 8/1278 | 0.270262 | Per2; Tcf7l2; Tal1; Rab15; Rragd; Maged2; Pvrl1; Fgfr1 |
| SOX2 | 14/2000 | 0.096132 | Gstm3; Fblim1; Clec11a; Gata6; Itln1; Nfatc2; Cyp7a1; Per2; Lass4; Aldh1a1;Pdk4;Blnk; Gas6; Atp6v0d2 |
| SOX2 | 14/2000 | 0.096132 | Il10; Abca1; Cd5l; Abca9; Cacna1d; Igf1; Cp; Thpo; Rab37; Slco4a1; Tubb1; Maged2; Atp6v0d2; Cd200 |
| SOX2 | 13/2000 | 0.160414 | Il10; Tcf7l2; Aldh1l1; Arg2; Wnt5a; Nfatc2; Cacna1d; Cp; Tal1; Grb10; Lhx4; Acpp; Cd55 |
| SOX2 | 5/863 | 0.399596 | Per2; Gata6; Gdf6; Ltbp1; Itga9 |
| SOX2 | 19/3319 | 0.235257 | Il10; Gstm3; Tcf7l2; Fblim1; Alox15; Clec11a; Wnt5a; Igf1; Tnfrsf13c; Nt5e; Adrb3; Slco4a1; Ppap2b; Kcnq2; Rragd; Blnk; Asb4; Fgfr1; Itga9 |
| SOX2 | 2/497 | 0.692959 | Per2; Myo1b |
| SOX2 | 3/785 | 0.732379 | Il10; Per2; Ppap2b |
| SOX2 | 19/3420 | 0.278900 | Pde4d; Hpn; Nfatc2; Cacna1d; Gdf6; Abca13; Ltbp1; Rasgrp3; Dock10; Fmnl2; Bmper; Tnn; Slco4a1; Rab37; Kcnq2; Aldh1a1; Lhx4; Pvrl1; Ccr3 |
| SOX2 | 10/2000 | 0.495379 | Aldh1l1; Adamts2; Bmper; Rab15; Eef1a2; Hpn; Tubb1; Abca9; Gpha2; Pvrl1 |
| OCT4 | 20/2000 | 0.001144 | Il10; Serpinb2; Wnt5a; Itln1; Prg4; Igf1; Nts; Abca13; Dock10; Selp; Per2; Dusp23; Col3a1; Myo1b; Adamts2; Tnn; Col6a2; Grb10; Lhx4; Cd55 |
| OCT4 | 16/2000 | 0.028265 | Il10; Serpinb2; Itln1; Nfatc2; Prg4; Dock10; Selp; Per2; Dusp23; Col3a1; Myo1b; Fmnl2; Tnn; Kcnq2; Lhx4; Cd55 |
| OCT4 | 13/1992 | 0.157087 | Il10; Gstm3; Tcf7l2; Wnt5a; Alox15; Nfatc2; Nt5e; Adrb3; Kcnq2; Rragd; Asb4; Pvrl1; Fgfr1 |
| OCT4 | 13/2000 | 0.160414 | Tnxb; Cacna1d; Slc2a4; Comp; Adamts2; Tdo2; Adrb3; Slco4a1; Trpv4; Kcnq2; Rragd; Pvrl1; Itga9 |
| OCT4 | 7/2000 | 0.856909 | Tcf7l2; Eef1a2; Hpn; Grb10; Igf1; Acpp; Rasgrp3 |
| POU5F1 | 12/1550 | 0.067193 | Adamts2; Crabp2; Bmper; Thpo; Adrb3; Pde4d; Rragd; Pdk4; Cacna1d; Mycbpap; Asb4; Fgfr1 |
| POU5F1 | 6/622 | 0.078803 | Nt5e; Tal1; Mmp2; Gata6; Maged2; Fgfr1 |
| POU5F1 | 12/2109 | 0.311132 | Il10; Myo1b; Nt5e; Fmnl2; Adrb3; Fblim1; Tal1; Ppap2b; Cacna1d; Maged2; Asb4; Igf1 |
| POU5F1 | 3/753 | 0.705916 | Il10; Per2; Cyp26a1 |
| POU5F1 | 1/567 | 0.937187 | Slco4a1 |
| POU5F1 | 1/555 | 0.933343 | Prok2 |
| POU5F1 | 2/559 | 0.753373 | Cyp26a1; Abca13 |
| POU5F1 | 18/4232 | 0.755639 | Il10; Gstm3; Tcf7l2; Fblim1; Alox15; Wnt5a; Nfatc2; Tnfrsf13c; Nt5e; Adrb3; Slco4a1; Ppap2b; Kcnq2; Rragd; Asb4; Pvrl1; Fgfr1; Itga9 |
| NANOG | 15/1989 | 0.051785 | Tcf7l2; Wnt5a; Igf2; Igf1; Tnfrsf13c; Serpinb1a; Nt5e; Adrb3; Ppap2b; Kcnq2; Rragd; Blnk; Asb4; Pvrl1; Fgfr1 |
| NANOG | 14/2000 | 0.096132 | Il10; Serpinb2; Itln1; Nfatc2; Prg4; Dock10; Selp; Dusp23; Col3a1; Myo1b; Fmnl2; Tnn; Lhx4; Cd55 |
| NANOG | 19/3052 | 0.137575 | Tcf7l2; Wnt5a; Igf2; Igf1; Tnfrsf13c; Ltbp1; Serpinb1a; Nt5e; Adrb3; Rab15; Slco4a1; Ppap2b; Kcnq2; Rragd; Blnk; Asb4; Pvrl1; Itga9; Fgfr1 |
| NANOG | 13/2000 | 0.160414 | Il10; Tcf7l2; Aldh1l1; Arg2; Wnt5a; Nfatc2; Cacna1d; Cp; Tal1; Grb10; Lhx4; Acpp; Cd55 |
| NANOG | 9/1686 | 0.420900 | Tcf7l2; Tdo2; Rab15; Tal1; Mmp2; Gata6; Lhx4; Cldn1; Fgfr1 |
| NANOG | 5/840 | 0.377515 | Clec11a; Blnk; Igf1; Acpp; Itga9 |
| NANOG | 16/3520 | 0.636674 | Pde4d; Igf1; Cp; Lass4; Col3a1; Myo1b; Nt5e; Bmper; Adrb3; Rab37; Ppap2b; Pdk4; Grb10; Pvrl1; Fgfr1; Itga9 |
| NANOG | 11/1908 | 0.307350 | Tcf7l2; Serpinb1a; Adrb3; Fblim1; Ppap2b; Rragd; Igf2; Blnk; Igf1; Itga9; Fgfr1 |
| NANOG | 1/344 | 0.811672 | Igf2 |
| NANOG | 2/542 | 0.737895 | Serpinb1a; Dusp23 |
| NANOG | 3/1232 | 0.940192 | Slco4a1; Blnk; Igf1 |
| NANOG | 8/2000 | 0.756029 | Tcf7l2; Dusp23; Arg2; Tal1; Prok2; Igf1; Gpha2; Ccr3 |
| KLF4 | 12/1211 | 0.013033 | Col3a1; Adamts2; Nt5e; Fblim1; Ankrd22; Gata6; Prok2; Slc2a4; Ltbp1; Cd200; Ccr3; Itga9 |
| KLF4 | 16/2000 | 0.028265 | Il10; Serpinb2; Itln1; Nfatc2; Prg4; Dock10; Selp; Per2; Dusp23; Col3a1; Myo1b; Fmnl2; Tnn; Slco4a1; Lhx4; Cd55 |
| KLF4 | 13/2000 | 0.160414 | Il10; Gstm3; Tcf7l2; Chrm1; Fblim1; Gata6; Cyp26a1; Myo1b; Rab37; Slco4a1; Ppap2b; Pvrl1; Cd55 |
| KLF4 | 8/1502 | 0.433701 | Cyp26a1; Bmper; Tal1; Ppap2b; Gata6; Igf2; S100a14; Cd55 |
| KLF4 | 6/2444 | 0.982047 | Per2; Lass4; Bmper; Col6a2; Tnfrsf13c; Acpp |
| KLF4 | 7/1700 | 0.717649 | Myo1b; Lass4; Slco4a1; Igf2; Nfatc2; Pvrl1; Cd55 |
| KLF4 | 10/2000 | 0.495379 | Comp; Myo1b; Lass4; Slco4a1; Tal1; Pon1; Gata6; Grb10; Lhx4; Pvrl1 |
| CMYC | 16/2000 | 0.028265 | Il10; Serpinb2; Itln1; Nfatc2; Prg4; Dock10; Selp; Per2; Dusp23; Col3a1; Myo1b; Fmnl2; Tnn; Kcnq2; Lhx4; Cd55 |
| MYC | 14/2000 | 0.096132 | Ddx3y; Tnfrsf13c; Gdf6; Rasgrp3; Selp; Cyp26a1; Adamts2; Tal1; Rragd; Blnk; Asb4; Gas6; Pvrl1; Fgfr1 |
| MYC | 16/2979 | 0.354148 | Gstm3; Tcf7l2; Tnxb; Crabp2; Mmp2; Wnt5a; Gata6; Igf2; Igf1; Ltbp1; Adamts2; Thpo; Rab15; Asb4; Lhx4; Cd55 |
| MYC | 3/797 | 0.741816 | Blnk; Nfatc2; Tnfrsf13c |
| MYC | 2/3413 | 1.000000 | Per2; Adrb3 |
| MYC | 6/3868 | 0.999934 | Tcf7l2; Clec11a; Wnt5a; Grb10; Gata6; Gdf6 |
| MYC | 2/1458 | 0.994109 | Lass4; Fgfr1 |
| MYC | 2/746 | 0.877854 | Rab37; Prok2 |
| MYC | 4/1406 | 0.912685 | Mmp2; Ppap2b; Prok2; Tnfrsf13c |
| MYC | 11/2000 | 0.364090 | Ddx3y; Myo1b; Arg2; Slco4a1; Ankrd22; Hpn; Igf2; Grb10; Prg4; Igf1; Rasgrp3 |
SOX2, OCT4/POU5F1, Nanog, KLF4 and c-Myc are known to be the five main transcription factors forming the transcriptional profile of stem cells. Activation of these factors is sufficient for reprogramming a normal somatic cell into a pluripotent/multipotent stem cell, as was first demonstrated on mouse embryonic and adult fibroblast cultures (Takahashi and Yamanaka, 2006; reviewed in Heng et al., 2010). These transcription factors are also shown to be activated under conditions of hypoxia (Li and Rich, 2010; Mathieu et al., 2011; Iida et al., 2012; Bae et al., 2016), oxidative stress (Cullingford et al., 2008; Kang et al., 2009; Kim et al., 2013; Chang et al., 2014; Balvan et al., 2015; Saijo et al., 2016) and in the presence of xenobiotics (Jang et al., 2014; Liu et al., 2016c; Stanford et al., 2016). Thus, the mechanism of formation of the tumor cells stemness can be proposed. This mechanism implies the activation of these key factors under conditions of generalized cellular stress that, in turn, leads to increased expression of specific targets, which probably include also the genes providing the stem-like phenotype of Krebs-2 cells.
In addition, we have decided to check for the possibility of an alternative mechanism of the “stem-genes” activation under conditions of generalized cellular stress independent of SOX2/OCT4/Nanog/KLF4/c-Myc pathway.
The main transcription factors that provide a cellular response to hypoxia are the proteins of the HIF family (hypoxia-inducible factor) (reviewed in Peet et al., 2017). However, the factors such as NFkB, CREB, AP-1, Egr-1, NF-IL6/C/EBPβ, RTEF-1, GATA2, STAT5, ETS1 (reviewed in Cummins and Taylor, 2005) as well as RUNX1 (Lee et al., 2017a) also take a direct part in the regulation of transcription under hypoxia/anoxia. ChIP-Seq enrichment analysis has revealed that 92 of 96 genes contain binding sites for at least one of these transcription factors with the following distribution: CREB1–25 genes, RELA (NFκB)−9 genes, cJUN (AP-1)−31 genes, MAF (AP-1)−15 genes, EGR1–42 genes, C/EBPβ-59 genes, ETS1–11 genes, STAT5–4 genes, GATA2–33 genes, RTEF-1/TEAD4–15 genes, RUNX1/AML1–45 genes (data not shown).
In addition, 88 genes contain a binding site(s) for such xenosensors or their intermediators, as PPARα/δ/γ (58 genes), NFE2L2/NRF2 (14 genes), AHR (6 genes), NR1I2/PXR (9 genes), FOXO1/3 (17 genes) (Klotz and Steinbrenner, 2017), MITF (25 genes) (Huang et al., 2013), EGR1 (42 genes) (Thiel and Cibelli, 2002; Sullivan et al., 2012), as well as for androgen receptor (AR) (55 genes). The last one had been shown to be activated not only by steroid hormones, but also by various xenobiotics, including endogenous ones as well (Araki et al., 2005) (data not shown).
Compared with other components of generalized cellular stress, oxidative stress activates the widest range of transcription factors, among them NFE2L2/NRF2, NFκB, cJUN, MAF, FOXO1/3, STAT1/3, ELK1, MEF2A (Zhang et al., 2016b; Klotz and Steinbrenner, 2017; Nemmiche, 2017; Sies et al., 2017), FLI1 and HOXB4 (Monzen et al., 2011), C/EBPα (Xu et al., 2009; Puri et al., 2012), C/EBPδ (Hour et al., 2010; Banerjee et al., 2016), MYB (Wan et al., 2005), GATA3 (Li et al., 2017b), and IRF8 (Li et al., 2017c; Sakai et al., 2017). It turned out that all 96 genes of our list contain site(s) for at least one of these transcription factors. The most represented factor was FLI1 (56 genes), followed by GATA3 (53 genes) and STAT3 (52 genes). Another 9 factors composed the group of average representation: cJUN−31 genes, IRF8–22 genes, C/EBPα-22 genes, C/EBPδ-21 genes, MYB−19 genes, MAF−15 genes, NFE2L2/NRF2–14 genes, FOXO1 and STAT1–12 genes for each. The remaining 5 factors were low-represented: NFκB/RELA−9 genes, ELK1–8 genes, FOXO3–7 genes, and, finally, HOXB4 and MEF2A−5 genes for each (data not shown).
We draw two principal conclusions from the results of “ChEA 2016” analysis. The first conclusion is that, in fact, all the genes, potentially implicated in maintaining stem-like phenotype of Krebs-2 TAMRA+ cells, can be activated under generalized cellular stress conditions. And the second one is that such an activation can be mediated both by induction of stemness by SOX2, OCT4/POU5F1, Nanog, KLF4, and c-Myc factors, and by direct action of specific mediators of cellular response to hypoxia-xenobiotics-oxidative stress. Yet the presence of binding sites for certain transcription factors does not necessarily ensure the transcriptional activation that depends significantly on general epigenetic/physiological context. It presumes the necessity of complex approach. As we already mentioned above, there are experimental evidences that a number of genes from our list are activated under stress conditions. The analysis of binding sites, respectively, suggests the possible mechanisms of such activation and allows us to extrapolate these mechanisms to other “stem genes.”
If there is a third way: discussion
The issue of the mechanisms of CSCs origination as well as of means they use to self-maintain and increase their population in developing malignant neoplasms is one of the most important for modern oncology, as it is key for the development of methods of antitumor therapy.
The classical model for the formation of CSCs subpopulation is based on the ability of pluripotent cells to divide symmetrically, as the main way of self-renewal of the population (Franco et al., 2016; Rich, 2016). Moreover, CSCs possess the additional ability to retain their “pluripotent” properties outside of the “stem niche” conditions as well as the ability for amoeboid migration characteristic for most of poorly differentiated cells (Sakamoto et al., 2011). It ensures a uniform distribution of the initiating cells newly formed after symmetrical division throughout the tumor volume and, respectively, provides conditions for the continuous exponential growth of the tumor mass.
The model of stemness induction under conditions of generalized cellular stress we have proposed, complements the classical model and allows to resolve certain discrepancies in the available experimental data with the model “symmetrical division-migration.” At this, it should be emphasized that our concept of generalized cellular stress is not limited to the factors listed above and can be extended with such components as inflammation, ionizing radiation, heat shock, etc. Moreover, this model can also possibly explain the carcinogenic effect of chronic oxidative stress, inflammation and the action of carcinogenic xenobiotics through de novo induction of “pluripotency” followed by transformation into malignancy.
Simultaneous existence of two independent and complementary mechanisms for the formation and maintenance of CSCs subpopulation implies that there may be a third and a fourth variant(s). To complete the picture of possible mechanisms of CSCs origination, other hypotheses also need to be mentioned.
One of the hypotheses explains the phenomenon of CSCs de novo emergence due to genetic instability that is inherent characteristic of tumor cells. Formation of cells with a stem-like phenotype evenly dispersed throughout the volume of the tumor mass is believed to be the one of possible consequences of this instability (Lagasse, 2008). However, this explanation has a significant drawback, as it is barely consistent with the fact that tumors retain their histological and biochemical properties, and, accordingly, the overall transcriptional profile during development, as well as upon metastasis and transplantation into model animals (Franzén et al., 1997; Süsskind et al., 2017). This fact testifies to the persistence of a certain “genetic individuality” of cells that drive tumor growth, which to significant extent contradicts the stochastic model of the formation of a tumorigenic population due to genetic instability.
Another possible mechanism for the formation of a pluripotent phenotype in tumor cells could be the phenomenon of “genometastasis” (García-Casas et al., 2017). It is supposed that extracellular double-stranded DNA released from cells that have undergone apoptosis or necrosis, both primary and secondary, can be internalized by cancer cells that have passed the first stages of commitment/differentiation, but still retained such a basic feature of CSC as the ability to capture fragments of extracellular double-stranded DNA. The occurrence of DNA with certain genetic or structural features in internal compartments of such cells can lead to a restoration of the pluripotent potential of the committed cells and their reversible conversion into new CSCs. The proposed “reversive mechanism” does not contradict the proposed concept of the stemness induction under the generalized cellular stress, but, somehow, complements it, since the action of factors of generalized cellular stress is always accompanied by intensive death of cancer cells, which results in an excessive amount of extracellular double-stranded DNA (Wen et al., 2017). This hypothesis addresses the mechanism for retransformation of the early committed progeny of existing CSCs. The main disadvantage of this model, as well as of the previous one, based on genetic instability, is indeterminacy and randomness of the results of events occurring during the “genometastasis” (multiple mutations, random genetic composition of the internalized DNA etc).
Another intriguing model of CSC formation is the “Blebbishield emergency program.” It was found that cancer cells undergoing apoptosis can avoid cell death by evoking this program. During this process, one of the apoptotic bodies becomes a center of aggregation for other ones that results in the formation of so-called “Blebbishield” that, in turn, further transforms into a new CSC. Such a newly formed CSC demonstrates a more aggressive tumorigenic behavior and can even fuse with immunity cells. As a result of all these transformations, the new secondary tumor with significantly more aggressive characteristics arises (Jinesh and Kamat, 2016, 2017).
In general, all the hypotheses considered, starting with genetic instability and ending with the fusion of apoptotic bodies, describe the formation of pluripotent/stem phenotype of tumor cells as a probabilistic event with unpredictable results, somehow or other related to changes in their genetic material. The fluctuations in the percentage of CSCs we have observed in experimental tumors (Potter et al., 2016a) suggests that the main cause of “dynamic stemness” is not genomic but epigenetic changes.
The model we proposed for stemness induction in response to the components of generalized cellular stress, namely hypoxia, oxidative stress and the action of xenobiotics, apparently describes some basic mechanisms of the cellular response to stress. It can be presumed that CSCs serve as a kind of “Emergency service” for tumors, emerging de novo and ensuring their survival under unfavorable conditions. With all this, a number of questions remain, and the main one is why the proportion of CSCs relative to the entire mass of the tumor remains rather low despite the stress conditions? Moreover, it is not clear how long CSCs can sustain a stem-like phenotype, and whether stemness maintenance depends on external conditions or gradually fades regardless of the presence/absence of inducing agents?
Assuming all of the above, we have to admit that the significant majority of existing anti-tumor pharmaceutical and radiotherapy schemes lead to the formation of generalized cellular stress conditions, and, therefore, are likely to induce de novo formation of CSCs in the total mass of nonstem tumor cells (Chang, 2016). Perhaps this explains the fact that despite a certain progress, the overall effectiveness of cancer treatment remains extremely unsatisfactory, and cancer remains one of the leading causes of mortality in the world.
Author contributions
YE performed the analysis, interpreted the data, and drafted the manuscript. AP interpreted the data and drafted the manuscript. EP and ED interpreted the data. OE performed the analysis. OT, AO, and EC participated in the study design. NK coordinated all work. SB conceived the study, participated in its design, coordinated and drafted the manuscript. All authors read and approved the final manuscript.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are gratitude to Dr. Dmitriy Yu. Oshchepkov for critical comments.
Glossary
Abbreviations
- CSC
cancer stem cell
- TAMRA
carboxytetramethylrhodamine, fluorescent dye.
Footnotes
Funding. This study was supported by the State scientific project N 0324-2018-0019 and by the Integration project of the Siberian Branch of the Russian Academy of Sciences Reconstruction, computer analysis and modeling of the structural and functional organization of biomedical-significant gene networks (project N 0324-2018-0021).
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2018.00544/full#supplementary-material
References
- Akyol S., Cömertoglu I., Firat R., Çakmak Ö., Yukselten Y., Erden G., et al. (2015). Effect of insulin on the mRNA expression of procollagen N-proteinases in chondrosarcoma OUMS-27 cells. Oncol. Lett. 10, 1091–1096. 10.3892/ol.2015.3317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcaín F. J., Löw H. (1997). Ceruloplasmin releases pH-induced inhibition of cell proliferation stimulated by growth factors. Redox Rep. 3, 287–293. 10.1080/13510002.1997.11747125 [DOI] [PubMed] [Google Scholar]
- Aldonza M. B. D., Son Y. S., Sung H.-J., Ahn J. M., Choi Y.-J., Kim Y.-I., et al. (2017). Paraoxonase-1 (PON1) induces metastatic potential and apoptosis escape via its antioxidative function in lung cancer cells. Oncotarget 8, 42817–42835. 10.18632/oncotarget.17069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alinejad V., Hossein Somi M., Baradaran B., Akbarzadeh P., Atyabi F., Kazerooni H., et al. (2016). Co-delivery of IL17RB siRNA and doxorubicin by chitosan-based nanoparticles for enhanced anticancer efficacy in breast cancer cells. Biomed. Pharmacother. 83, 229–240. 10.1016/j.biopha.2016.06.037 [DOI] [PubMed] [Google Scholar]
- Alinezhad S., Väänänen R.-M., Mattsson J., Li Y., Tallgrén T., Tong Ochoa N., et al. (2016). Validation of novel biomarkers for prostate cancer progression by the combination of bioinformatics, clinical and functional studies. PLoS ONE 11:e0155901 10.1371/journal.pone.0155901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alizadeh M., Wada M., Gelfman C. M., Handa J. T., Hjelmeland L. M. (2001). Downregulation of differentiation specific gene expression by oxidative stress in ARPE-19 cells. Invest. Ophthalmol. Vis. Sci. 42, 2706–2713. [PubMed] [Google Scholar]
- An H., Kim J. Y., Oh E., Lee N., Cho Y., Seo J. H. (2015). Salinomycin promotes anoikis and decreases the CD44+/CD24-stem-like population via inhibition of STAT3 activation in MDA-MB-231 cells. PLoS ONE 10:e0141919 10.1371/journal.pone.0141919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson-Sjöland A., Karlsson J. C., Rydell-Törmänen K. (2016). ROS-induced endothelial stress contributes to pulmonary fibrosis through pericytes and Wnt signaling. Lab. Investig. 96, 206–217. 10.1038/labinvest.2015.100 [DOI] [PubMed] [Google Scholar]
- Applebaum M. A., Jha A. R., Kao C., Hernandez K. M., DeWane G., Salwen H. R., et al. (2016). Integrative genomics reveals hypoxia inducible genes that are associated with a poor prognosis in neuroblastoma patients. Oncotarget 7, 76816–76826. 10.18632/oncotarget.12713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araki N., Ohno K., Takeyoshi M., Iida M. (2005). Evaluation of a rapid in vitro androgen receptor transcriptional activation assay using AR-EcoScreenTM cells. Toxicol. Vitr. 19, 335–352. 10.1016/j.tiv.2004.10.008 [DOI] [PubMed] [Google Scholar]
- Araújo T. M., Seabra A. D., Lima E. M., Assumpção P. P., Montenegro R. C., Demachki S., et al. (2016). Recurrent amplification of RTEL1 and ABCA13 and its synergistic effect associated with clinicopathological data of gastric adenocarcinoma. Mol. Cytogenet. 9:52. 10.1186/s13039-016-0260-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardianto B., Sugimoto T., Kawano S., Kasagi S., Jauharoh S. N., Kurimoto C., et al. (2010). The HPB-AML-I cell line possesses the properties of mesenchymal stem cells. J. Exp. Clin. Cancer Res. 29:163. 10.1186/1756-9966-29-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asano Y., Kishida S., Mu P., Sakamoto K., Murohara T., Kadomatsu K. (2010). DRR1 is expressed in the developing nervous system and downregulated during neuroblastoma carcinogenesis. Biochem. Biophys. Res. Commun. 394, 829–835. 10.1016/j.bbrc.2010.03.085 [DOI] [PubMed] [Google Scholar]
- Assou S., Le Carrour T., Tondeur S., Ström S., Gabelle A., Marty S., et al. (2007). A meta-analysis of human embryonic stem cells transcriptome integrated into a web-based expression atlas. Stem Cells 25, 961–973. 10.1634/stemcells.2006-0352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Au V., Tsang F. H., Man K., Fan S. T., Poon R. T., Lee N. P. (2014). Expression of ankyrin repeat and SOCS box containing 4 (ASB4) confers migration and invasion properties of hepatocellular carcinoma cells. Biosci. Trends 8, 101–110. 10.5582/bst.8.101 [DOI] [PubMed] [Google Scholar]
- Auslander M., Yudkovski Y., Chalifa-Caspi V., Herut B., Ophir R., Reinhardt R., et al. (2008). Pollution-affected fish hepatic transcriptome and its expression patterns on exposure to cadmium. Mar. Biotechnol. 10, 250–261. 10.1007/s10126-007-9060-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bae K.-M., Dai Y., Vieweg J., Siemann D. W. (2016). Hypoxia regulates SOX2 expression to promote prostate cancer cell invasion and sphere formation. Am. J. Cancer Res. 6, 1078–1088. [PMC free article] [PubMed] [Google Scholar]
- Baharvand H., Ashtiani S. K., Taee A., Massumi M., Valojerdi M. R., Yazdi P. E., et al. (2006). Generation of new human embryonic stem cell lines with diploid and triploid karyotypes. Dev. Growth Differ. 48, 117–128. 10.1111/j.1440-169X.2006.00851.x [DOI] [PubMed] [Google Scholar]
- Balvan J., Gumulec J., Raudenska M., Krizova A., Stepka P., Babula P., et al. (2015). Oxidative stress resistance in metastatic prostate cancer: renewal by self-eating. PLoS ONE 10:e0145016. 10.1371/journal.pone.0145016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ban M. J., Ji S. H., Lee C.-K., Bae S. B., Kim H. J., Ahn T. S., et al. (2017). Solute carrier organic anion transporter family member 4A1 (SLCO4A1) as a prognosis marker of colorectal cancer. J. Cancer Res. Clin. Oncol. 143, 1437–1447. 10.1007/s00432-017-2393-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee S., Aykin-Burns N., Krager K. J., Shah S. K., Melnyk S. B., Hauer-Jensen M., et al. (2016). Loss of C/EBPδ enhances IR-induced cell death by promoting oxidative stress and mitochondrial dysfunction. Free Radic. Biol. Med. 99, 296–307. 10.1016/j.freeradbiomed.2016.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbet R., Peiffer I., Hutchins J. R., Hatzfeld A., Garrido E., Hatzfeld J. A. (2012). Expression of the 49 human ATP binding cassette (ABC) genes in pluripotent embryonic stem cells and in early- and late-stage multipotent mesenchymal stem cells: possible role of ABC plasma membrane transporters in maintaining human stem cell pluripotency. Cell Cycle 11, 1611–1620. 10.4161/cc.20023 [DOI] [PubMed] [Google Scholar]
- Baylin S. B., Gann D. S., Hsu S. H. (1976). Clonal origin of inherited medullary thyroid carcinoma and pheochromocytoma. Science 193, 321–323. 10.1126/science.935869 [DOI] [PubMed] [Google Scholar]
- Belaguli N. S., Aftab M., Rigi M., Zhang M., Albo D., Berger D. H. (2010). GATA6 promotes colon cancer cell invasion by regulating urokinase plasminogen activator gene expression. Neoplasia 12, 856–865. 10.1593/neo.10224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendall S. C., Stewart M. H., Menendez P., George D., Vijayaragavan K., Werbowetski-Ogilvie T., et al. (2007). IGF and FGF cooperatively establish the regulatory stem cell niche of pluripotent human cells in vitro. Nature 448, 1015–1021. 10.1038/nature06027 [DOI] [PubMed] [Google Scholar]
- Bergman D., Halje M., Nordin M., Engström W. (2013). Insulin-like growth factor 2 in development and disease: a mini-review. Gerontology 59, 240–249. 10.1159/000343995 [DOI] [PubMed] [Google Scholar]
- Bernard M., Delabesse E., Novault S., Hermine O., Macintyre E. A. (1998). Antiapoptotic effect of ectopic TAL1/SCL expression in a human leukemic T-cell line. Cancer Res. 58, 2680–2687. [PubMed] [Google Scholar]
- Bertout J. A., Patel S. A., Simon M. C. (2008). The impact of O2 availability on human cancer. Nat. Rev. Cancer 8, 967–975. 10.1038/nrc2540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bie Q., Sun C., Gong A., Li C., Su Z., Zheng D., et al. (2016). Non-tumor tissue derived interleukin-17B activates IL-17RB/AKT/β-catenin pathway to enhance the stemness of gastric cancer. Sci. Rep. 6:25447. 10.1038/srep25447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bie Q., Zhang B., Sun C., Ji X., Barnie P. A., Qi C., et al. (2017). IL-17B activated mesenchymal stem cells enhance proliferation and migration of gastric cancer cells. Oncotarget 8, 18914–18923. 10.18632/oncotarget.14835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black S. M., Beggs J. D., Hayes J. D., Bartoszek A., Muramatsu M., Sakai M., et al. (1990). Expression of human glutathione S-transferases in Saccharomyces cerevisiae confers resistance to the anticancer drugs adriamycin and chlorambucil. Biochem. J. 268, 309–315. 10.1042/bj2680309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum B., Benvenisty N. (2008). The tumorigenicity of human embryonic stem cells. Adv. Cancer Res. 100, 133–158. 10.1016/S0065-230X(08)00005-5 [DOI] [PubMed] [Google Scholar]
- Blum B., Benvenisty N. (2009). The tumorigenicity of diploid and aneuploid human pluripotent stem cells. Cell Cycle 8, 3822–3830. 10.4161/cc.8.23.10067 [DOI] [PubMed] [Google Scholar]
- Bojesen K. B., Clausen O., Rohde K., Christensen C., Zhang L., Li S., et al. (2012). Nectin-1 binds and signals through the fibroblast growth factor receptor. J. Biol. Chem. 287, 37420–37433. 10.1074/jbc.M112.345215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bordeleau F., Alcoser T. A., Reinhart-King C. A. (2014). Physical biology in cancer. 5. The rocky road of metastasis: the role of cytoskeletal mechanics in cell migratory response to 3D matrix topography. AJP Cell Physiol. 306, C110–C120. 10.1152/ajpcell.00283.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botto L., Beretta E., Bulbarelli A., Rivolta I., Lettiero B., Leone B. E., et al. (2008). Hypoxia-induced modifications in plasma membranes and lipid microdomains in A549 cells and primary human alveolar cells. J. Cell. Biochem. 105, 503–513. 10.1002/jcb.21850 [DOI] [PubMed] [Google Scholar]
- Boucher H., Vanneaux V., Domet T., Parouchev A., Larghero J. (2016). Circadian clock genes modulate human bone marrow mesenchymal stem cell differentiation, migration and cell cycle. PLoS ONE 11:e0146674. 10.1371/journal.pone.0146674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandi J., Dalla Pozza E., Dando I., Biondani G., Robotti E., Jenkins R., et al. (2016). Secretome protein signature of human pancreatic cancer stem-like cells. J. Proteomics 136, 1–12. 10.1016/j.jprot.2016.01.017 [DOI] [PubMed] [Google Scholar]
- Brauze D., Zawierucha P., Kiwerska K., Bednarek K., Oleszak M., Rydzanicz M., et al. (2017). Induction of expression of aryl hydrocarbon receptor-dependent genes in human HepaRG cell line modified by shRNA and treated with β-naphthoflavone. Mol. Cell. Biochem. 425, 59–75. 10.1007/s11010-016-2862-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner S., Klameth L., Riha J., Schölm M., Hamilton G., Bajna E., et al. (2015). Specific expression of OATPs in primary small cell lung cancer (SCLC) cells as novel biomarkers for diagnosis and therapy. Cancer Lett. 356, 517–524. 10.1016/j.canlet.2014.09.025 [DOI] [PubMed] [Google Scholar]
- Brown R. C., Mark K. S., Egleton R. D., Huber J. D., Burroughs A. R., Davis T. P. (2003). Protection against hypoxia-induced increase in blood-brain barrier permeability: role of tight junction proteins and NFkappaB. J. Cell Sci. 116, 693–700. 10.1242/jcs.00264 [DOI] [PubMed] [Google Scholar]
- Bruchova H., Vasikova A., Merkerova M., Milcova A., Topinka J., Balascak I., et al. (2010). Effect of maternal tobacco smoke exposure on the placental transcriptome. Placenta 31, 186–191. 10.1016/j.placenta.2009.12.016 [DOI] [PubMed] [Google Scholar]
- Bu Y., Jia Q. A., Ren Z. G., Zhang J. B., Jiang X. M., Liang L., et al. (2014). Maintenance of stemness in oxaliplatin-resistant hepatocellular carcinoma is associated with increased autocrine of IGF1. PLoS ONE 9:e89686. 10.1371/journal.pone.0089686 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Buechler C., Bared S. M., Aslanidis C., Ritter M., Drobnik W., Schmitz G. (2002). Molecular and functional interaction of the ATP-binding cassette transporter A1 with Fas-associated death domain protein. J. Biol. Chem. 277, 41307–41310. 10.1074/jbc.C200436200 [DOI] [PubMed] [Google Scholar]
- Cai Y. N., Dai X. H., Zhang Q. H., Hu R., Dai Z. M. (2015). Gene expression profiling of somatic and pluripotent cells reveals novel pathways involved in reprogramming. Genet. Mol. Res. 14, 12085–12092. 10.4238/2015.October.5.21 [DOI] [PubMed] [Google Scholar]
- Calaminus S. D. J., Guitart A., Sinclair A., Schachtner H., Watson S. P., Holyoake T. L., et al. (2012). Lineage tracing of Pf4-Cre Marks hematopoietic stem cells and their progeny. PLoS ONE 7:e51361. 10.1371/journal.pone.0051361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos-Sánchez E., Cobaleda C. (2015). Tumoral reprogramming: plasticity takes a walk on the wild side. Biochim. Biophys. Acta 1849, 436–447. 10.1016/j.bbagrm.2014.07.003 [DOI] [PubMed] [Google Scholar]
- Carrel A., Ebeling A. H. (1928). The fundamental properties of the fibroblast and the macrophage: III. The malignant fibroblast of sarcoma 10 of the Crocker foundation. J. Exp. Med. 48, 105–123. 10.1084/jem.48.1.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cha N., Liu W., Yang N., Xie S., Gao Y., Chen X., et al. (2014). Oncogenicity of LHX4 in colorectal cancer through Wnt/β-catenin/TCF4 cascade. Tumor Biol. 35, 10319–10324. 10.1007/s13277-014-2210-8 [DOI] [PubMed] [Google Scholar]
- Chan E. F., Gat U., McNiff J. M., Fuchs E. (1999). A common human skin tumour is caused by activating mutations in β- catenin. Nat. Genet. 21, 410–413. 10.1038/7747 [DOI] [PubMed] [Google Scholar]
- Chang J. C. (2016). Cancer stem cells: role in tumor growth, recurrence, metastasis, and treatment resistance. Medicine 95, S20–S25. 10.1097/MD.0000000000004766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Q., Chen B., Thakur C., Lu Y., Chen F. (2014). Arsenic-induced sub-lethal stress reprograms human bronchial epithelial cells to CD61− cancer stem cells. Oncotarget 5, 1290–1303. 10.18632/oncotarget.1789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudary N., Milosevic M., Hill R. P. (2011). Suppression of vascular endothelial growth factor receptor 3 (VEGFR3) and vascular endothelial growth factor C (VEGFC) inhibits hypoxia-induced lymph node metastases in cervix cancer. Gynecol. Oncol. 123, 393–400. 10.1016/j.ygyno.2011.07.006 [DOI] [PubMed] [Google Scholar]
- Chekhun V. F., Lozovska Y. V., Burlaka A. P., Lukyanova N. Y., Todor I. N., Naleskina L. A. (2014). Peculiarities of antioxidant system and iron metabolism in organism during development of tumor resistance to cisplatin. Exp. Oncol. 36, 196–201. [PubMed] [Google Scholar]
- Chen B., Xue J., Meng X., Slutzky J. L., Calvert A. E., Chicoine L. G. (2014a). Resveratrol prevents hypoxia-induced arginase II expression and proliferation of human pulmonary artery smooth muscle cells via Akt-dependent signaling. Am. J. Physiol. Cell. Mol. Physiol. 307, L317–L325. 10.1152/ajplung.00285.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Cao F., Bai L., Liu Y., Xie J., Wang W., et al. (2015a). IKKβ enforces a LIN28B/TCF7L2 positive feedback loop that promotes cancer cell stemness and metastasis. Cancer Res. 75, 1725–1735. 10.1158/0008-5472.CAN-14-2111 [DOI] [PubMed] [Google Scholar]
- Chen E., Proestou G., Bourbeau D., Wang E. (2000). Rapid up-regulation of peptide elongation factor EF-1α protein levels is an immediate early event during oxidative stress-induced apoptosis. Exp. Cell Res. 259, 140–148. 10.1006/excr.2000.4952 [DOI] [PubMed] [Google Scholar]
- Chen E. Y., Tan C. M., Kou Y., Duan Q., Wang Z., Meirelles G., et al. (2013). Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinformatics 14:128. 10.1186/1471-2105-14-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H.-F., Yu C.-Y., Chen M.-J., Chou S.-H., Chiang M.-S., Chou W.-H., et al. (2015b). Characteristic expression of major histocompatibility complex and immune privilege genes in human pluripotent stem cells and their derivatives. Cell Transplant. 24, 845–864. 10.3727/096368913X674639 [DOI] [PubMed] [Google Scholar]
- Chen J., Hersmus N., Van Duppen V., Caesens P., Denef C., Vankelecom H. (2005). The adult pituitary contains a cell population displaying stem/progenitor cell and early-embryonic characteristics. Endocrinology 146, 3985–3998. 10.1210/en.2005-0185 [DOI] [PubMed] [Google Scholar]
- Chen J., Li X., Ma D., Liu T., Tian P., Wu C. (2017). Ceramide synthase-4 orchestrates the cell proliferation and tumor growth of liver cancer in vitro and in vivo through the nuclear factor-κB signaling pathway. Oncol. Lett. 14, 1477–1483. 10.3892/ol.2017.6365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J.-J., Gao Y., Tian Q., Liang Y.-M., Yang L. (2014b). Platelet factor 4 protects bone marrow mesenchymal stem cells from acute radiation injury. Br. J. Radiol. 87:20140184. 10.1259/bjr.20140184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K. G., Valencia J. C., Gillet J.-P., Hearing V. J., Gottesman M. M. (2009). Involvement of ABC transporters in melanogenesis and the development of multidrug resistance of melanoma. Pigment Cell Melanoma Res. 22, 740–749. 10.1111/j.1755-148X.2009.00630.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Fink T., Ebbesen P., Zachar V. (2006). Temporal transcriptome of mouse ATDC5 chondroprogenitors differentiating under hypoxic conditions. Exp. Cell Res. 312, 1727–1744. 10.1016/j.yexcr.2006.02.013 [DOI] [PubMed] [Google Scholar]
- Chen R., Zeng X., Zhang R., Huang J., Kuang X., Yang J., et al. (2014c). Cav1.3 channel α1Dprotein is overexpressed and modulates androgen receptor transactivation in prostate cancers. Urol. Oncol. Semin. Orig. Investig. 32, 524–536. 10.1016/j.urolonc.2013.05.011 [DOI] [PubMed] [Google Scholar]
- Chen S. X., Yin J. F., Lin B. C., Su H. F., Zheng Z., Xie C. Y, et al. (2016a). Upregulated expression of long noncoding RNA SNHG15 promotes cell proliferation and invasion through regulates MMP2/MMP9 in patients with GC. Tumor Biol. 37, 6801–6812. 10.1007/s13277-015-4404-0 [DOI] [PubMed] [Google Scholar]
- Chen Y., Peng C., Abraham S. A., Shan Y., Guo Z., Desouza N., et al. (2014d). Arachidonate 15-lipoxygenase is required for chronic myeloid leukemia stem cell survival. J. Clin. Invest. 124, 3847–3862. 10.1172/JCI66129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z., Shi T., Zhang L., Zhu P., Deng M., Huang C., et al. (2016b). Mammalian drug efflux transporters of the ATP binding cassette (ABC) family in multidrug resistance: a review of the past decade. Cancer Lett. 370, 153–164. 10.1016/j.canlet.2015.10.010 [DOI] [PubMed] [Google Scholar]
- Cheng I. H., Lin Y.-C., Hwang E., Huang H.-T., Chang W.-H., Liu Y.-L., et al. (2011). Collagen VI protects against neuronal apoptosis elicited by ultraviolet irradiation via an Akt/Phosphatidylinositol 3-kinase signaling pathway. Neuroscience 183, 178–188. 10.1016/j.neuroscience.2011.03.057 [DOI] [PubMed] [Google Scholar]
- Cheon D.-J., Tong Y., Sim M.-S., Dering J., Berel D., Cui X., et al. (2014). A collagen-remodeling gene signature regulated by TGF-β signaling is associated with metastasis and poor survival in serous ovarian cancer. Clin. Cancer Res. 20, 711–723. 10.1158/1078-0432.CCR-13-1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiovaro F., Martina E., Bottos A., Scherberich A., Hynes N. E., Chiquet-Ehrismann R. (2015). Transcriptional regulation of tenascin-W by TGF-beta signaling in the bone metastatic niche of breast cancer cells. Int. J. Cancer 137, 1842–1854. 10.1002/ijc.29565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong H. C., Tan C. K., Huang R. L., Tan N. S. (2012). Matricellular proteins: a sticky affair with cancers. J. Oncol. 2012, 1–17. 10.1155/2012/351089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou F.-S., Griesinger A., Wunderlich M., Lin S., Link K. A., Shrestha M., et al. (2012). The thrombopoietin/MPL/Bcl-xL pathway is essential for survival and self-renewal in human preleukemia induced by AML1-ETO. Blood 120, 709–719. 10.1182/blood-2012-01-403212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipak A., Mrakovcic L., Ciz M., Lojek A., Mihaylova B., Goshev I., et al. (2010). Growth suppression of human breast carcinoma stem cells by lipid peroxidation product 4-hydroxy-2-nonenal and hydroxyl radical-modified collagen. Acta Biochim. Pol. 57, 165–71. [PubMed] [Google Scholar]
- Cole C., Lau S., Backen A., Clamp A., Rushton G., Dive C., et al. (2010). Inhibition of FGFR2 and FGFR1 increases cisplatin sensitivity in ovarian cancer. Cancer Biol. Ther. 10, 495–504. 10.4161/cbt.10.5.12585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conacci-Sorrell M., Kaplan A., Raveh S., Gavert N., Sakurai T., Ben-Ze'ev A. (2005). The shed ectodomain of Nr-CAM stimulates cell proliferation and motility, and confers cell transformation. Cancer Res. 65, 11605–11612. 10.1158/0008-5472.CAN-05-2647 [DOI] [PubMed] [Google Scholar]
- Corradetti B., Meucci A., Bizzaro D., Cremonesi F., Lange Consiglio A. (2013). Mesenchymal stem cells from amnion and amniotic fluid in the bovine. Reproduction 145, 391–400. 10.1530/REP-12-0437 [DOI] [PubMed] [Google Scholar]
- Correia N. C., Fragoso R., Carvalho T., Enguita F. J., Barata J. T. (2016). MiR-146b negatively regulates migration and delays progression of T-cell acute lymphoblastic leukemia. Sci. Rep. 6:31894. 10.1038/srep31894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa H., Xu X., Overbeek G., Vasaikar S., Patro C. P., Kostopoulou O. N., et al. (2016). Human cytomegalovirus may promote tumour progression by upregulating arginase-2. Oncotarget 7, 47221–47231. 10.18632/oncotarget.9722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coutu D. L., François M., Galipeau J. (2011). Inhibition of cellular senescence by developmentally regulated FGF receptors in mesenchymal stem cells. Blood 117, 6801–6812. 10.1182/blood-2010-12-321539 [DOI] [PubMed] [Google Scholar]
- Creighton C. (1882). Three cases of tumour arising from skin-glands in the dog, showing the connection between disorder of the glandular structure and function, and cancerous invasion of the connective tissue. Med. Chir. Trans. 65, 53–70.3. Available online at: http://www.ncbi.nlm.nih.gov/pubmed/20896600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullingford T. E., Butler M. J., Marshall A. K., Tham E. L., Sugden P. H., Clerk A. (2008). Differential regulation of Krüppel-like factor family transcription factor expression in neonatal rat cardiac myocytes: effects of endothelin-1, oxidative stress and cytokines. Biochim. Biophys. Acta-Mol. Cell Res. 1783, 1229–1236. 10.1016/j.bbamcr.2008.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins E. P., Taylor C. T. (2005). Hypoxia-responsive transcription factors. Pflügers Arch.-Eur. J. Physiol. 450, 363–371. 10.1007/s00424-005-1413-7 [DOI] [PubMed] [Google Scholar]
- Dalton W. S. (1999). The tumor microenvironment as a determinant of drug response and resistance. Drug Resist. Updat. 2, 285–288. 10.1054/drup.1999.0097 [DOI] [PubMed] [Google Scholar]
- D'Amato N. C., Rogers T. J., Gordon M. A., Greene L. I., Cochrane D. R., Spoelstra N. S., et al. (2015). A TDO2-AhR signaling axis facilitates anoikis resistance and metastasis in triple-negative breast cancer. Cancer Res. 75, 4651–4664. 10.1158/0008-5472.CAN-15-2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damiano J. S. (2002). Integrins as novel drug targets for overcoming innate drug resistance. Curr. Cancer Drug Targets 2, 37–43. 10.2174/1568009023334033 [DOI] [PubMed] [Google Scholar]
- Davies N. A., Watkeys L., Butcher L., Potter S., Hughes M. G., Moir H., et al. (2015). The contributions of oxidative stress, oxidised lipoproteins and AMPK towards exercise-associated PPARγ signalling within human monocytic cells. Free Radic. Res. 49, 45–56. 10.3109/10715762.2014.978311 [DOI] [PubMed] [Google Scholar]
- Davis B. T., Voigt R. M., Shaikh M., Forsyth C. B., Keshavarzian A. (2017). CREB protein mediates alcohol-induced circadian disruption and intestinal permeability. Alcohol. Clin. Exp. Res. 41, 2007–2014. 10.1111/acer.13513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dayem A. A., Choi H.-Y., Kim J.-H., Cho S.-G. (2010). Role of oxidative stress in stem, cancer, and cancer stem cells. Cancers 2, 859–884. 10.3390/cancers2020859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Almeida P., Meyer E. H., Kooreman N. G., Diecke S., Dey D., Sanchez-Freire V., et al. (2014). Transplanted terminally differentiated induced pluripotent stem cells are accepted by immune mechanisms similar to self-tolerance. Nat. Commun. 5:3903. 10.1038/ncomms4903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deliri H., Meller N., Kadakkal A., Malhotra R., Brewster J., Doran A. C., et al. (2011). Increased 12/15-lipoxygenase enhances cell growth, fibronectin deposition, and neointimal formation in response to carotid injury. Arterioscler. Thromb. Vasc. Biol. 31, 110–116. 10.1161/ATVBAHA.110.212068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delyon J., Servy A., Laugier F., André J., Ortonne N., Battistella M., et al. (2017). PDE4D promotes FAK-mediated cell invasion in BRAF-mutated melanoma. Oncogene 36, 3252–3262. 10.1038/onc.2016.469 [DOI] [PubMed] [Google Scholar]
- Desai S., Baker S. S., Liu W., Moya D. A., Browne R. W., Mastrandrea L., et al. (2014). Paraoxonase 1 and oxidative stress in paediatric non-alcoholic steatohepatitis. Liver Int. 34, 110–117. 10.1111/liv.12308 [DOI] [PubMed] [Google Scholar]
- Dey D., Pan G., Varma N. R., Palaniyandi S. S. (2015). Sca-1 + cells from fetal heart with high aldehyde dehydrogenase activity exhibit enhanced gene expression for self-renewal, proliferation, and survival. Oxid. Med. Cell. Longev. 2015, 1–8. 10.1155/2015/730683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobashi S., Katagiri T., Hirota E., Ashida S., Daigo Y., Shuin T., et al. (2009). Involvement of TMEM22 overexpression in the growth of renal cell carcinoma cells. Oncol. Rep. 21, 305–312. 10.3892/or_00000222 [DOI] [PubMed] [Google Scholar]
- Dolgova E. V., Alyamkina E. A., Efremov Y. R., Nikolin V. P., Popova N. A., Tyrinova T. V., et al. (2014). Identification of cancer stem cells and a strategy for their elimination. Cancer Biol. Ther. 15, 1378–1394. 10.4161/cbt.29854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolgova E. V., Efremov Y. R., Orishchenko K. E., Andrushkevich O. M., Alyamkina E. A., Proskurina A. S., et al. (2013). Delivery and processing of exogenous double-stranded DNA in mouse CD34+ hematopoietic progenitor cells and their cell cycle changes upon combined treatment with cyclophosphamide and double-stranded DNA. Gene 528, 74–83. 10.1016/j.gene.2013.06.058 [DOI] [PubMed] [Google Scholar]
- Dolgova E. V., Proskurina A. S., Nikolin V. P., Popova N. A., Alyamkina E. A., Orishchenko K. E., et al. (2012). “Delayed death” phenomenon: a synergistic action of cyclophosphamide and exogenous DNA. Gene 495, 134–145. 10.1016/j.gene.2011.12.032 [DOI] [PubMed] [Google Scholar]
- Dolgova E. V., Shevela E. Y., Tyrinova T. V., Minkevich A. M., Proskurina A. S., Potter E. A., et al. (2016). Nonadherent spheres with multiple myeloma surface markers contain cells that contribute to sphere formation and are capable of internalizing extracellular double-stranded DNA. Clin. Lymphoma Myeloma Leuk. 16, 563–576. 10.1016/j.clml.2016.06.014 [DOI] [PubMed] [Google Scholar]
- Dressel R. (2011). Effects of histocompatibility and host immune responses on the tumorigenicity of pluripotent stem cells. Semin. Immunopathol. 33, 573–591. 10.1007/s00281-011-0266-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzugkoeva F. S., Mozhaeva I. V., Dzugkoev S. G., Margieva O. I., Tedtoeva A. I., Otiev M. A. (2016). Oxidative stress and biochemical markers of endothelial dysfunction and organ damage under conditions of experimental nonferrous metal intoxication. Bull. Exp. Biol. Med. 162, 199–202. 10.1007/s10517-016-3575-z [DOI] [PubMed] [Google Scholar]
- Ellisen L. W., Bird J., West D. C., Soreng A. L., Reynolds T. C., Smith S. D., et al. (1991). TAN-1, the human homolog of the drosophila notch gene, is broken by chromosomal translocations in T lymphoblastic neoplasms. Cell 66, 649–661. 10.1016/0092-8674(91)90111-B [DOI] [PubMed] [Google Scholar]
- Eloranta J. J., Kullak-Ublick G. A. (2005). Coordinate transcriptional regulation of bile acid homeostasis and drug metabolism. Arch. Biochem. Biophys. 433, 397–412. 10.1016/j.abb.2004.09.019 [DOI] [PubMed] [Google Scholar]
- ElShamy W. M., Duhé R. J. (2013). Overview: cellular plasticity, cancer stem cells and metastasis. Cancer Lett. 341, 2–8. 10.1016/j.canlet.2013.06.020 [DOI] [PubMed] [Google Scholar]
- Englund E., Bartoschek M., Reitsma B., Jacobsson L., Escudero-Esparza A., Orimo A., et al. (2016). Cartilage oligomeric matrix protein contributes to the development and metastasis of breast cancer. Oncogene 35, 5585–5596. 10.1038/onc.2016.98 [DOI] [PubMed] [Google Scholar]
- Fialkow P. J., Gartler S. M., Yoshida A. (1967). Clonal origin of chronic myelocytic leukemia in man. Proc. Natl. Acad. Sci. U.S.A. 58, 1468–1471. 10.1073/pnas.58.4.1468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fialkow P. J., Klein G., Gartler S. M., Clifford P. (1970). Clonal origin for individual Burkitt tumours. Lancet 1, 384–386. [DOI] [PubMed] [Google Scholar]
- Foo L. C., Dougherty J. D. (2013). Aldh1L1 is expressed by postnatal neural stem cells in vivo. Glia 61, 1533–1541. 10.1002/glia.22539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fouad Y. A., Aanei C. (2017). Revisiting the hallmarks of cancer. Am. J. Cancer Res. 7, 1016–1036. [PMC free article] [PubMed] [Google Scholar]
- Franco S. S., Szczesna K., Iliou M. S., Al-Qahtani M., Mobasheri A., Kobolák J., et al. (2016). In vitro models of cancer stem cells and clinical applications. BMC Cancer 16:738 10.1186/s12885-016-2774-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzén B., Linder S., Alaiya A. A., Eriksson E., Fujioka K., Bergman A.-C., et al. (1997). Analysis of polypeptide expression in benign and malignant human breast lesions. Electrophoresis 18, 582–587. 10.1002/elps.1150180341 [DOI] [PubMed] [Google Scholar]
- Friedman G. K., Haas M. C., Kelly V. M., Markert J. M., Gillespie G. Y., Cassady K. A. (2012). Hypoxia moderates γ134.5-deleted herpes simplex virus oncolytic activity in human glioma xenoline primary cultures. Transl. Oncol. 5, 200–207. 10.1593/tlo.12115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu L., Lin-Lee Y.-C., Pham L. V., Tamayo A. T., Yoshimura L. C., Ford R. J. (2009). BAFF-R promotes cell proliferation and survival through interaction with IKKβ and NF-κB/c-Rel in the nucleus of normal and neoplastic B-lymphoid cells. Blood 113, 4627–4636. 10.1182/blood-2008-10-183467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu S., Davies K. P. (2015). Opiorphin-dependent upregulation of CD73 (a key enzyme in the adenosine signaling pathway) in corporal smooth muscle cells exposed to hypoxic conditions and in corporal tissue in pre-priapic sickle cell mice. Int. J. Impot. Res. 27, 140–145. 10.1038/ijir.2015.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukunaga-Kalabis M., Martinez G., Nguyen T. K., Kim D., Santiago-Walker A., Roesch A., et al. (2010). Tenascin-C promotes melanoma progression by maintaining the ABCB5-positive side population. Oncogene 29, 6115–6124. 10.1038/onc.2010.350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganat Y., Soni S., Chacon M., Schwartz M. L., Vaccarino F. M. (2002). Chronic hypoxia up-regulates fibroblast growth factor ligands in the perinatal brain and induces fibroblast growth factor-responsive radial glial cells in the sub-ependymal zone. Neuroscience 112, 977–991. 10.1016/S0306-4522(02)00060-X [DOI] [PubMed] [Google Scholar]
- Gao Z. W., Dong K., Zhang H. Z. (2014). The roles of CD73 in cancer. Biomed Res. Int. 2014, 1–9. 10.1155/2014/460654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Casas A., García-Olmo D. C., García-Olmo D. (2017). Further the liquid biopsy: gathering pieces of the puzzle of genometastasis theory. World J. Clin. Oncol. 8, 378–388. 10.5306/wjco.v8.i5.378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido P., Osorio F. G., Morán J., Cabello E., Alonso A., Freije J. M., et al. (2015). Loss of GLUT4 induces metabolic reprogramming and impairs viability of breast cancer cells. J. Cell. Physiol. 230, 191–198. 10.1002/jcp.24698 [DOI] [PubMed] [Google Scholar]
- Gato W. E., Hales D. B., Means J. C. (2012). Hepatic gene expression analysis of 2-aminoanthracene exposed Fisher-344 rats reveal patterns indicative of liver carcinoma and type 2 diabetes. J. Toxicol. Sci. 37, 1001–1016. 10.2131/jts.37.1001 [DOI] [PubMed] [Google Scholar]
- Gely-Pernot A., Coronas V., Harnois T., Prestoz L., Mandairon N., Didier A., et al. (2012). An endogenous vitamin K-dependent mechanism regulates cell proliferation in the brain subventricular stem cell niche. Stem Cells 30, 719–731. 10.1002/stem.1045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber J. M., Gucwa J. L., Esopi D., Gurel M., Haffner M. C., Vala M., et al. (2013). Genome-wide comparison of the transcriptomes of highly enriched normal and chronic myeloid leukemia stem and progenitor cell populations. Oncotarget 4, 715–728. 10.18632/oncotarget.990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerby B., Veiga D. F. T., Krosl J., Nourreddine S., Ouellette J., Haman A., et al. (2016). High-throughput screening in niche-based assay identifies compounds to target preleukemic stem cells. J. Clin. Invest. 126, 4569–4584. 10.1172/JCI86489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson L. A., Lavoie R. A., Bissegger S., Campbell L. M., Langlois V. S. (2014). A positive correlation between mercury and oxidative stress-related gene expression (GPX3 and GSTM3) is measured in female Double-crested Cormorant blood. Ecotoxicology 23, 1004–1014. 10.1007/s10646-014-1243-5 [DOI] [PubMed] [Google Scholar]
- Gkretsi V., Bogdanos D. P. (2015). Experimental evidence of Migfilin as a new therapeutic target of hepatocellular carcinoma metastasis. Exp. Cell Res. 334, 219–227. 10.1016/j.yexcr.2015.03.002 [DOI] [PubMed] [Google Scholar]
- Gopal K., Gupta N., Zhang H., Alshareef A., Alqahtani H., Bigras G., et al. (2016). Oxidative stress induces the acquisition of cancer stem-like phenotype in breast cancer detectable by using a Sox2 regulatory region-2 (SRR2) reporter. Oncotarget 7, 3111–3127. 10.18632/oncotarget.6630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorczynski R. M., Clark D. A., Erin N., Khatri I. (2011). Role of CD200 expression in regulation of metastasis of EMT6 tumor cells in mice. Breast Cancer Res. Treat. 130, 49–60. 10.1007/s10549-010-1259-3 [DOI] [PubMed] [Google Scholar]
- Gottesman M. M. (2002). Mechanisms of cancer drug resistance. Annu. Rev. Med. 53, 615–627. 10.1146/annurev.med.53.082901.103929 [DOI] [PubMed] [Google Scholar]
- Gouédard C., Barouki R., Morel Y. (2004). Dietary polyphenols increase paraoxonase 1 gene expression by an aryl hydrocarbon receptor-dependent mechanism. Mol. Cell. Biol. 24, 5209–5222. 10.1128/MCB.24.12.5209-5222.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granneman J. G., Li P., Zhu Z., Lu Y. (2005). Metabolic and cellular plasticity in white adipose tissue I: effects of β 3 -adrenergic receptor activation. Am. J. Physiol. Metab. 289, E608–E616. 10.1152/ajpendo.00009.2005 [DOI] [PubMed] [Google Scholar]
- Grantab R. H., Tannock I. F. (2012). Penetration of anticancer drugs through tumour tissue as a function of cellular packing density and interstitial fluid pressure and its modification by bortezomib. BMC Cancer 12:214. 10.1186/1471-2407-12-214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greig R. G., Koestler T. P., Trainer D. L., Corwin S. P., Miles L., Kline T., et al. (1985). Tumorigenic and metastatic properties of “normal” and ras-transfected NIH/3T3 cells. Proc. Natl. Acad. Sci. U.S.A. 82, 3698–3701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griesmann H., Ripka S., Pralle M., Ellenrieder V., Baumgart S., Buchholz M., et al. (2013). WNT5A-NFAT signaling mediates resistance to apoptosis in pancreatic cancer. Neoplasia 15, 11–22. 10.1593/neo.121312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Silva T. S., Osizugbo J. E., Tucker L., Spratt H. M., Garg N. J. (2014). Serum-mediated activation of macrophages reflects TcVac2 vaccine efficacy against chagas disease. Infect. Immun. 82, 1382–1389. 10.1128/IAI.01186-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammoud A. A., Kirstein N., Mournetas V., Darracq A., Broc S., Blanchard C., et al. (2016). Murine embryonic stem cell plasticity is regulated through klf5 and maintained by metalloproteinase mmp1 and hypoxia. PLoS ONE 11:e0146281. 10.1371/journal.pone.0146281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han W., Takano T., He J., Ding J., Gao S., Noda C., et al. (2001). Role of BLNK in oxidative stress signaling in B cells. Antioxidants Redox Signal. 3, 1065–1073. 10.1089/152308601317203576 [DOI] [PubMed] [Google Scholar]
- Han Z. C., Lu M., Li J., Defard M., Boval B., Schlegel N., et al. (1997). Platelet factor 4 and other CXC chemokines support the survival of normal hematopoietic cells and reduce the chemosensitivity of cells to cytotoxic agents. Blood 89, 2328–2335. [PubMed] [Google Scholar]
- Hanahan D., Weinberg R. A. (2000). The hallmarks of cancer. Cell 100, 57–70. 10.1016/S0092-8674(00)81683-9 [DOI] [PubMed] [Google Scholar]
- Hanahan D., Weinberg R. A. (2011). Hallmarks of cancer: the next generation. Cell 144, 646–674. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- Hao J., Li T.-G., Qi X., Zhao D.-F., Zhao G.-Q. (2006). WNT/β-catenin pathway up-regulates Stat3 and converges on LIF to prevent differentiation of mouse embryonic stem cells. Dev. Biol. 290, 81–91. 10.1016/j.ydbio.2005.11.011 [DOI] [PubMed] [Google Scholar]
- Hartomo T. B., Van Huyen Pham T., Yamamoto N., Hirase S., Hasegawa D., Kosaka Y., et al. (2015). Involvement of aldehyde dehydrogenase 1A2 in the regulation of cancer stem cell properties in neuroblastoma. Int. J. Oncol. 46, 1089–1098. 10.3892/ijo.2014.2801 [DOI] [PubMed] [Google Scholar]
- Harvey R. D., Morgan E. T. (2014). Cancer, inflammation, and therapy: effects on cytochrome P450-mediated drug metabolism and implications for novel immunotherapeutic agents. Clin. Pharmacol. Ther. 96, 449–457. 10.1038/clpt.2014.143 [DOI] [PubMed] [Google Scholar]
- Hashimoto Y., Tomiyama T., Yamano Y., Mori H. (2003). Mutation (D472Y) in the type 3 repeat domain of cartilage oligomeric matrix protein affects its early vesicle trafficking in endoplasmic reticulum and induces apoptosis. Am. J. Pathol. 163, 101–110. 10.1016/S0002-9440(10)63634-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinke J., Kerber M., Rahner S., Mnich L., Lassmann S., Helbing T., et al. (2012). Bone morphogenetic protein modulator BMPER is highly expressed in malignant tumors and controls invasive cell behavior. Oncogene 31, 2919–2930. 10.1038/onc.2011.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heng J. C., Orlov Y. L., Ng H. H. (2010). Transcription factors for the modulation of pluripotency and reprogramming. Cold Spring Harb. Symp. Quant. Biol. 75, 237–244. 10.1101/sqb.2010.75.003 [DOI] [PubMed] [Google Scholar]
- Henrique D., Hirsinger E., Adam J., Le Roux I., Pourquié O., Ish-Horowicz D., et al. (1997). Maintenance of neuroepithelial progenitor cells by Delta–Notch signalling in the embryonic chick retina. Curr. Biol. 7, 661–670. 10.1016/S0960-9822(06)00293-4 [DOI] [PubMed] [Google Scholar]
- Hiraoka A. (2008). Leukemia cell lines require self-secreted stem cell growth factor (SCGF) for their proliferation. Leuk. Res. 32, 1623–1625. 10.1016/j.leukres.2008.01.003 [DOI] [PubMed] [Google Scholar]
- Hiraoka A., Yano Ki K., Kagami N., Takeshige K., Mio H., Anazawa H., et al. (2001). Stem cell growth factor: in situ hybridization analysis on the gene expression, molecular characterization and in vitro proliferative activity of a recombinant preparation on primitive hematopoietic progenitor cells. Hematol. J. 2, 307–315. 10.1038/sj.thj.6200118 [DOI] [PubMed] [Google Scholar]
- Hlavata I., Mohelnikova-Duchonova B., Vaclavikova R., Liska V., Pitule P., Novak P., et al. (2012). The role of ABC transporters in progression and clinical outcome of colorectal cancer. Mutagenesis 27, 187–196. 10.1093/mutage/ger075 [DOI] [PubMed] [Google Scholar]
- Hoelzinger D. B., Demuth T., Berens M. E. (2007). Autocrine factors that sustain glioma invasion and paracrine biology in the brain microenvironment. J. Natl. Cancer Inst. 99, 1583–1593. 10.1093/jnci/djm187 [DOI] [PubMed] [Google Scholar]
- Horsley V., Pavlath G. K. (2002). NFAT: ubiquitous regulator of cell differentiation and adaptation. J. Cell Biol. 156, 771–774. 10.1083/jcb.200111073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoshino T., Wilson C. B. (1975). Review of basic concepts of cell kinetics as applied to brain tumors. J. Neurosurg. 42, 123–131. 10.3171/jns.1975.42.2.0123 [DOI] [PubMed] [Google Scholar]
- Hou H., Kang Y., Li Y., Zeng Y., Ding G., Shang J. (2017). miR-33a expression sensitizes Lgr5+ HCC-CSCs to doxorubicin via ABCA1. Neoplasma 64, 81–91. 10.4149/neo_2017_110 [DOI] [PubMed] [Google Scholar]
- Hough R. B., Piatigorsky J. (2004). Preferential transcription of rabbit Aldh1a1 in the cornea: implication of hypoxia-related pathways. Mol. Cell. Biol. 24, 1324–1340. 10.1128/MCB.24.3.1324-1340.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hour T.-C., Lai Y.-L., Kuan C.-I., Chou C.-K., Wang J.-M., Tu H.-Y., et al. (2010). Transcriptional up-regulation of SOD1 by CEBPD: a potential target for cisplatin resistant human urothelial carcinoma cells. Biochem. Pharmacol. 80, 325–334. 10.1016/j.bcp.2010.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hrubá E., Vondrácek J., Líbalová H., Topinka J., Bryja V., Soucek K., et al. (2011). Gene expression changes in human prostate carcinoma cells exposed to genotoxic and nongenotoxic aryl hydrocarbon receptor ligands. Toxicol. Lett. 206, 178–188. 10.1016/j.toxlet.2011.07.011 [DOI] [PubMed] [Google Scholar]
- Hsiao K.-Y., Wu M.-H., Chang N., Yang S.-H., Wu C.-W., Sun H. S., et al. (2015). Coordination of AUF1 and miR-148a destabilizes DNA methyltransferase 1 mRNA under hypoxia in endometriosis. Mol. Hum. Reprod. 21, 894–904. 10.1093/molehr/gav054 [DOI] [PubMed] [Google Scholar]
- Hu H. R., Dong Z., Yi L., He X. Y., Zhang Y. L., Liu Y. L., et al. (2015). Function and mechanism of neurotensin (NTS) and its receptor 1 (NTSR1) in occurrence and development of tumors. Zhongguo Zhong Yao Za Zhi 40, 2524–2536. [PubMed] [Google Scholar]
- Hu X., Zhang Y., Zhang A., Li Y., Zhu Z., Shao Z., et al. (2009). Comparative serum proteome analysis of human lymph node negative/positive invasive ductal carcinoma of the breast and benign breast disease controls via label-free semiquantitative shotgun technology. OMICS 13, 291–300. 10.1089/omi.2009.0016 [DOI] [PubMed] [Google Scholar]
- Huang G.-S., Dai L.-G., Yen B. L., Hsu S. H. (2011). Spheroid formation of mesenchymal stem cells on chitosan and chitosan-hyaluronan membranes. Biomaterials 32, 6929–6945. 10.1016/j.biomaterials.2011.05.092 [DOI] [PubMed] [Google Scholar]
- Huang L., Wang C., Zhang Y., Wu M., Zuo Z. (2013). Phenanthrene causes ocular developmental toxicity in zebrafish embryos and the possible mechanisms involved. J. Hazard. Mater. 261, 172–180. 10.1016/j.jhazmat.2013.07.030 [DOI] [PubMed] [Google Scholar]
- Huang S. S., Tang F.-M., Huang Y.-H., Liu I.-H., Hsu S.-C., Chen S.-T., et al. (2003). Cloning, expression, characterization, and role in autocrine cell growth of cell surface retention sequence binding protein-1. J. Biol. Chem. 278, 43855–43869. 10.1074/jbc.M306411200 [DOI] [PubMed] [Google Scholar]
- Huang W.-L., Li Z., Lin T.-Y., Wang S.-W., Wu F.-J., Luo C.-W. (2016). Thyrostimulin-TSHR signaling promotes the proliferation of NIH:OVCAR-3 ovarian cancer cells via trans-regulation of the EGFR pathway. Sci. Rep. 6:27471. 10.1038/srep27471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung T.-H., Hsu S.-C., Cheng C.-Y., Choo K.-B., Tseng C.-P., Chen T.-C., et al. (2014). Wnt5A regulates ABCB1 expression in multidrug-resistant cancer cells through activation of the non-canonical PKA/β-catenin pathway. Oncotarget 5, 12273–12290. 10.18632/oncotarget.2631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iborra A., Mayorga M., Llobet N., Martínez P. (2003). Expression of complement regulatory proteins [membrane cofactor protein (CD46), decay accelerating factor (CD55), and protectin (CD59)] in endometrial stressed cells. Cell. Immunol. 223, 46–51. 10.1016/S0008-8749(03)00127-8 [DOI] [PubMed] [Google Scholar]
- Iida H., Suzuki M., Goitsuka R., Ueno H. (2012). Hypoxia induces CD133 expression in human lung cancer cells by up-regulation of OCT3/4 and SOX2. Int. J. Oncol. 40, 71–79. 10.3892/ijo.2011.1207 [DOI] [PubMed] [Google Scholar]
- Illmensee K., Mintz B. (1976). Totipotency and normal differentiation of single teratocarcinoma cells cloned by injection into blastocysts. Proc. Natl. Acad. Sci. U.S.A. 73, 549–553. 10.1073/pnas.73.2.549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaluria P., Konstantopoulos K., Betenbaugh M., Shiloach J. (2008). Egr1 andGas6 facilitate the adaptation of HEK-293 cells to serum-free media by conferring enhanced viability and higher growth rates. Biotechnol. Bioeng. 99, 1443–1452. 10.1002/bit.21707 [DOI] [PubMed] [Google Scholar]
- Jam I., Shoham M., Wolf R. O., Mishkin S. (1978). Elevated serum amylase activity in the absence of clinical pancreatic or salivary gland disease: possible role of acute hypoxemia. Am. J. Gastroenterol. 70, 480–488. [PubMed] [Google Scholar]
- Jang J., Wang Y., Kim H. S., Lalli M. A., Kosik K. S. (2014). Nrf2, a regulator of the proteasome, controls self-renewal and pluripotency in human embryonic stem cells. Stem Cells 32, 2616–2625. 10.1002/stem.1764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Januchowski R., Swierczewska M., Sterzynska K., Wojtowicz K., Nowicki M., Zabel M. (2016). Increased expression of several collagen genes is associated with drug resistance in ovarian cancer cell lines. J. Cancer 7, 1295–1310. 10.7150/jca.15371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jauliac S., López-Rodriguez C., Shaw L. M., Brown L. F., Rao A., Toker A. (2002). The role of NFAT transcription factors in integrin-mediated carcinoma invasion. Nat. Cell Biol. 4, 540–544. 10.1038/ncb816 [DOI] [PubMed] [Google Scholar]
- Ji W., Yu Y., Li Z., Wang G., Li F., Xia W., et al. (2016). FGFR1 promotes the stem cell-like phenotype of FGFR1-amplified non-small cell lung cancer cells through the Hedgehog pathway. Oncotarget 7, 15118–15134. 10.18632/oncotarget.7701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang J., Liu Y., Tang Y., Li L., Zeng R., Zeng S., et al. (2016). ALDH1A1 induces resistance to CHOP in diffuse large B-cell lymphoma through activation of the JAK2/STAT3 pathway. Onco. Targets. Ther. Volume 9, 5349–5360. 10.2147/OTT.S107957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang W. G., Sanders A. J., Katoh M., Ungefroren H., Gieseler F., Prince M., et al. (2015). Tissue invasion and metastasis: molecular, biological and clinical perspectives. Semin. Cancer Biol. 35, S244–S275. 10.1016/j.semcancer.2015.03.008 [DOI] [PubMed] [Google Scholar]
- Jiang X. R., Wrona M. Z., Dryhurst G. (1999). Tryptamine-4,5-dione, a putative endotoxic metabolite of the superoxide- mediated oxidation of serotonin, is a mitochondrial toxin: possible implications in neurodegenerative brain disorders. Chem. Res. Toxicol. 12, 429–436. 10.1021/tx9801615 [DOI] [PubMed] [Google Scholar]
- Jiao H., Natoli R., Valter K., Provis J. M., Rutar M. (2015a). Spatiotemporal cadence of macrophage polarisation in a model of light-induced retinal degeneration. PLoS ONE 10:e0143952. 10.1371/journal.pone.0143952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao J., Zhao X., Liang Y., Tang D., Pan C. (2015b). FGF1–FGFR1 axis promotes tongue squamous cell carcinoma (TSCC) metastasis through epithelial–mesenchymal transition (EMT). Biochem. Biophys. Res. Commun. 466, 327–332. 10.1016/j.bbrc.2015.09.021 [DOI] [PubMed] [Google Scholar]
- Jin T., Suk Kim H., Choi S., Hwang E., Woo J., Suk Ryu H., et al. (2017a). microRNA-200c/141 upregulates SerpinB2 to promote breast cancer cell metastasis and reduce patient survival. Oncotarget 8, 32769–32782. 10.18632/oncotarget.15680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y., Nie D., Li J., Du X., Lu Y., Li Y., et al. (2017b). Gas6/AXL signaling regulates self-renewal of chronic myelogenous leukemia stem cells by stabilizing β-catenin. Clin. Cancer Res. 23, 2842–2855. 10.1158/1078-0432.CCR-16-1298 [DOI] [PubMed] [Google Scholar]
- Jinesh G. G., Kamat A. M. (2016). Blebbishield emergency program: an apoptotic route to cellular transformation. Cell Death Differ. 23, 757–758. 10.1038/cdd.2016.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jinesh G. G., Kamat A. M. (2017). The blebbishield emergency program overrides chromosomal instability and phagocytosis checkpoints in cancer stem cells. Cancer Res. 77, 6144–6156. 10.1158/0008-5472.CAN-17-0522 [DOI] [PubMed] [Google Scholar]
- Jögi A., Vallon-Christersson J., Holmquist L., Axelson H., Borg A., Påhlman S. (2004). Human neuroblastoma cells exposed to hypoxia: induction of genes associated with growth, survival, and aggressive behavior. Exp. Cell Res. 295, 469–487. 10.1016/j.yexcr.2004.01.013 [DOI] [PubMed] [Google Scholar]
- Joseph Martin S., Evan Prince S. (2017). Comparative modulation of levels of oxidative stress in the liver of anti-tuberculosis drug treated Wistar rats by vitamin B12, beta-carotene, and Spirulina fusiformis: role of NF-κB, iNOS, IL-6, and IL-10. J. Cell. Biochem. 118, 3825–3833. 10.1002/jcb.26032 [DOI] [PubMed] [Google Scholar]
- Jung D.-W., Che Z. M., Kim J., Kim K., Kim K.-Y., Williams D., et al. (2010). Tumor-stromal crosstalk in invasion of oral squamous cell carcinoma: a pivotal role of CCL7. Int. J. Cancer 127, 332–344. 10.1002/ijc.25060 [DOI] [PubMed] [Google Scholar]
- Jung J. E., Karatas H., Liu Y., Yalcin A., Montaner J., Lo E. H., et al. (2015a). STAT-dependent upregulation of 12/15-lipoxygenase contributes to neuronal injury after stroke. J. Cereb. Blood Flow Metab. 35, 2043–2051. 10.1038/jcbfm.2015.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung Y.-S., Vermeer P. D., Vermeer D. W., Lee S.-J., Goh A. R., Ahn H.-J., et al. (2015b). CD200: association with cancer stem cell features and response to chemoradiation in head and neck squamous cell carcinoma. Head Neck 37, 327–335. 10.1002/hed.23608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamaraj S., Anandakumar P., Jagan S., Ramakrishnan G., Devaki T. (2010). Modulatory effect of hesperidin on benzo(a)pyrene induced experimental lung carcinogenesis with reference to COX-2, MMP-2 and MMP-9. Eur. J. Pharmacol. 649, 320–327. 10.1016/j.ejphar.2010.09.017 [DOI] [PubMed] [Google Scholar]
- Kanda M., Nomoto S., Oya H., Takami H., Shimizu D., Hibino S., et al. (2016). The expression of melanoma-associated antigen D2 both in surgically resected and serum samples serves as clinically relevant biomarker of gastric cancer progression. Ann. Surg. Oncol. 23, 214–221. 10.1245/s10434-015-4457-8 [DOI] [PubMed] [Google Scholar]
- Kang J., Gemberling M., Nakamura M., Whitby F. G., Handa H., Fairbrother W. G., et al. (2009). A general mechanism for transcription regulation by Oct1 and Oct4 in response to genotoxic and oxidative stress. Genes Dev. 23, 208–222. 10.1101/gad.1750709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper B., Brandt E., Brandau S., Petersen F. (2007). Platelet factor 4 (CXC chemokine ligand 4) differentially regulates respiratory burst, survival, and cytokine expression of human monocytes by using distinct signaling pathways. J. Immunol. 179, 2584–2591. 10.4049/jimmunol.179.4.2584 [DOI] [PubMed] [Google Scholar]
- Kasprzak A., Kwasniewski W., Adamek A., Gozdzicka-Jozefiak A. (2017). Insulin-like growth factor (IGF) axis in cancerogenesis. Mutat. Res. Mutat. Res. 772, 78–104. 10.1016/j.mrrev.2016.08.007 [DOI] [PubMed] [Google Scholar]
- Katoh M., Nakagama H. (2014). FGF receptors: cancer biology and therapeutics. Med. Res. Rev. 34, 280–300. 10.1002/med.21288 [DOI] [PubMed] [Google Scholar]
- Katsuta E., Tanaka S., Mogushi K., Shimada S., Akiyama Y., Aihara A., et al. (2016). CD73 as a therapeutic target for pancreatic neuroendocrine tumor stem cells. Int. J. Oncol. 48, 657–669. 10.3892/ijo.2015.3299 [DOI] [PubMed] [Google Scholar]
- Kazi J. U., Rönnstrand L. (2013). FLT3 signals via the adapter protein Grb10 and overexpression of Grb10 leads to aberrant cell proliferation in acute myeloid leukemia. Mol. Oncol. 7, 402–418. 10.1016/j.molonc.2012.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerbel R. S., St Croix B., Florenes V. A., Rak J. (1996). Induction and reversal of cell adhesion-dependent multicellular drug resistance in solid breast tumors. Hum. Cell 9, 257–264. [PubMed] [Google Scholar]
- Kerjaschki D., Bago-Horvath Z., Rudas M., Sexl V., Schneckenleithner C., Wolbank S., et al. (2011). Lipoxygenase mediates invasion of intrametastatic lymphatic vessels and propagates lymph node metastasis of human mammary carcinoma xenografts in mouse. J. Clin. Invest. 121, 2000–2012. 10.1172/JCI44751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalil A., Villard P.-H., Dao M. A., Burcelin R., Champion S., Fouchier F., et al. (2010). Polycyclic aromatic hydrocarbons potentiate high-fat diet effects on intestinal inflammation. Toxicol. Lett. 196, 161–167. 10.1016/j.toxlet.2010.04.010 [DOI] [PubMed] [Google Scholar]
- Khan F. H., Pandian V., Ramraj S., Aravindan S., Herman T. S., Aravindan N. (2015). Reorganization of metastamiRs in the evolution of metastatic aggressive neuroblastoma cells. BMC Genomics 16:501. 10.1186/s12864-015-1642-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiani A., Habermann I., Haase M., Feldmann S., Boxberger S., Sanchez-Fernandez M. A., et al. (2004). Expression and regulation of NFAT (nuclear factors of activated T cells) in human CD34+ cells: down-regulation upon myeloid differentiation. J. Leukoc. Biol. 76, 1057–1065. 10.1189/jlb.0404259 [DOI] [PubMed] [Google Scholar]
- Kikuchi J., Koyama D., Wada T., Izumi T., Hofgaard P. O., Bogen B., et al. (2015). Phosphorylation-mediated EZH2 inactivation promotes drug resistance in multiple myeloma. J. Clin. Invest. 125, 4375–4390. 10.1172/JCI80325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H. K., Hwang S. H., Abdi S. (2017). Tempol ameliorates and prevents mechanical hyperalgesia in a rat model of chemotherapy-induced neuropathic pain. Front. Pharmacol. 7:532. 10.3389/fphar.2016.00532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M.-C., Cui F.-J., Kim Y. (2013). Hydrogen peroxide promotes epithelial to mesenchymal transition and stemness in human malignant mesothelioma cells. Asian Pac. J. Cancer Prev. 14, 3625–3630. 10.7314/APJCP.2013.14.6.3625 [DOI] [PubMed] [Google Scholar]
- Kim Y. W., Kim H.-J., Bae S.-M., Kim Y. J., Shin J.-C., Chun H.-J., et al. (2010). Time-course transcriptional profiling of human amniotic fluid-derived stem cells using microarray. Cancer Res. Treat. 42, 82–94. 10.4143/crt.2010.42.2.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinder M., Wei C., Shelat S. G., Kundu M., Zhao L., Blair I. A., et al. (2010). Hematopoietic stem cell function requires 12/15-lipoxygenase-dependent fatty acid metabolism. Blood 115, 5012–5022. 10.1182/blood-2009-09-243139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschenbaum A., Izadmehr S., Yao S., O'Connor-Chapman K. L., Huang A., Gregoriades E. M., et al. (2016). Prostatic acid phosphatase alters the RANKL/OPG system and induces osteoblastic prostate cancer bone metastases. Endocrinology 157, 4526–4533. 10.1210/en.2016-1606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klotz L.-O., Steinbrenner H. (2017). Cellular adaptation to xenobiotics: interplay between xenosensors, reactive oxygen species and FOXO transcription factors. Redox Biol. 13, 646–654. 10.1016/j.redox.2017.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluger H. M., Kluger Y., Gilmore-Hebert M., DiVito K., Chang J. T., Rodov S., et al. (2004). cDNA microarray analysis of invasive and tumorigenic phenotypes in a breast cancer model. Lab. Investig. 84, 320–331. 10.1038/labinvest.3700044 [DOI] [PubMed] [Google Scholar]
- Ko C. H., Cheng C. F., Lai C. P., Tzu T. H., Chiu C. W., Lin M. W., et al. (2013). Differential proteomic analysis of cancer stem cell properties in hepatocellular carcinomas by isobaric tag labeling and mass spectrometry. J. Proteome Res. 12, 3573–3585. 10.1021/pr4004294 [DOI] [PubMed] [Google Scholar]
- Kohlscheen S., Wintterle S., Schwarzer A., Kamp C., Brugman M. H., Breuer D. C., et al. (2015). Inhibition of thrombopoietin/Mpl signaling in adult hematopoiesis identifies new candidates for hematopoietic stem cell maintenance. PLoS ONE 10:e0131866. 10.1371/journal.pone.0131866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong C. S., Cao H., Kwok S., Nguyen C. M., Jordan R. C., Beaudry V. G., et al. (2013). Loss of the p53/p63 target PERP is an early event in oral carcinogenesis and correlates with higher rate of local relapse. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 115, 95–103. 10.1016/j.oooo.2012.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korinek V., Barker N., Moerer P., van Donselaar E., Huls G., Peters P. J., et al. (1998). Depletion of epithelial stem-cell compartments in the small intestine of mice lacking Tcf-4. Nat. Genet. 19, 379–383. 10.1038/1270 [DOI] [PubMed] [Google Scholar]
- Kotov A. A., Olenkina O. M., Godneeva B. K., Adashev V. E., Olenina L. V. (2017). Progress in understanding the molecular functions of DDX3Y (DBY) in male germ cell development and maintenance. Biosci. Trends 11, 46–53. 10.5582/bst.2016.01216 [DOI] [PubMed] [Google Scholar]
- Krathwohl M. D. (2004). Chemokines promote quiescence and survival of human neural progenitor cells. Stem Cells 22, 109–118. 10.1634/stemcells.22-1-109 [DOI] [PubMed] [Google Scholar]
- Kubo H., Shimizu M., Taya Y., Kawamoto T., Michida M., Kaneko E., et al. (2009). Identification of mesenchymal stem cell (MSC)-transcription factors by microarray and knockdown analyses, and signature molecule-marked MSC in bone marrow by immunohistochemistry. Genes to Cells 14, 407–424. 10.1111/j.1365-2443.2009.01281.x [DOI] [PubMed] [Google Scholar]
- Kuleshov M. V., Jones M. R., Rouillard A. D., Fernandez N. F., Duan Q., Wang Z., et al. (2016). Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 44, W90–W97. 10.1093/nar/gkw377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuol N., Stojanovska L., Nurgali K., Apostolopoulos V. (2017). The mechanisms tumor cells utilize to evade the host's immune system. Maturitas 105, 8–15.? 10.1016/j.maturitas.2017.04.014 [DOI] [PubMed] [Google Scholar]
- Kurz K., Schroecksnadel S., Weiss G., Fuchs D. (2011). Association between increased tryptophan degradation and depression in cancer patients. Curr. Opin. Clin. Nutr. Metab. Care 14, 49–56. 10.1097/MCO.0b013e328340d849 [DOI] [PubMed] [Google Scholar]
- Lacombe J., Krosl G., Tremblay M., Gerby B., Martin R., Aplan P. D., et al. (2013). Genetic interaction between Kit and Scl. Blood 122, 1150–1161. 10.1182/blood-2011-01-331819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagasse E. (2008). Cancer stem cells with genetic instability: the best vehicle with the best engine for cancer. Gene Ther. 15, 136–142. 10.1038/sj.gt.3303068 [DOI] [PubMed] [Google Scholar]
- Lake A. D., Wood C. E., Bhat V. S., Chorley B. N., Carswell G. K., Sey Y. M., et al. (2016). Dose and effect thresholds for early key events in a PPARα-mediated mode of action. Toxicol. Sci. 149, 312–325. 10.1093/toxsci/kfv236 [DOI] [PubMed] [Google Scholar]
- Lambert C. B., Spire C., Claude N., Guillouzo A. (2009). Dose- and time-dependent effects of phenobarbital on gene expression profiling in human hepatoma HepaRG cells. Toxicol. Appl. Pharmacol. 234, 345–360. 10.1016/j.taap.2008.11.008 [DOI] [PubMed] [Google Scholar]
- Laviano A., Meguid M. M., Preziosa I., Rossi Fanelli F. (2007). Oxidative stress and wasting in cancer. Curr. Opin. Clin. Nutr. Metab. Care 10, 449–456. 10.1097/MCO.0b013e328122db94 [DOI] [PubMed] [Google Scholar]
- Lavrovsky V. A., Guvakova M. A., Lavrovsky Y. V. (1992). High frequency of tumour cell reversion to non-tumorigenic phenotype. Eur. J. Cancer 28, 17–21. 10.1016/0959-8049(92)90375-C [DOI] [PubMed] [Google Scholar]
- Łazarenkow A., Michalska M., Mirowski M., Słomiak K., Nawrot-Modranka J. (2017). The effect of hydrazine derivatives of 3-formylchromones on angiogenic basic fibroblast growth factor and fibroblast growth factor receptor-1 in human melanoma cell line WM-115. Acta Biochim. Pol. 64, 585–590. 10.18388/abp.2017_1565 [DOI] [PubMed] [Google Scholar]
- Le P. U., Angers-Loustau A., de Oliveira R. M., Ajlan A., Brassard C. L., Dudley A., et al. (2010). DRR drives brain cancer invasion by regulating cytoskeletal-focal adhesion dynamics. Oncogene 29, 4636–4647. 10.1038/onc.2010.216 [DOI] [PubMed] [Google Scholar]
- Leclerc D., Pham D. N., Lévesque N., Truongcao M., Foulkes W. D., Sapienza C., et al. (2017). Oncogenic role of PDK4 in human colon cancer cells. Br. J. Cancer 116, 930–936. 10.1038/bjc.2017.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeCouter J., Lin R., Tejada M., Frantz G., Peale F., Hillan K. J., et al. (2003). The endocrine-gland-derived VEGF homologue Bv8 promotes angiogenesis in the testis: localization of Bv8 receptors to endothelial cells. Proc. Natl. Acad. Sci. U.S.A. 100, 2685–2690. 10.1073/pnas.0337667100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeCouter J., Zlot C., Tejada M., Peale F., Ferrara N. (2004). Bv8 and endocrine gland-derived vascular endothelial growth factor stimulate hematopoiesis and hematopoietic cell mobilization. Proc. Natl. Acad. Sci. U.S.A. 101, 16813–16818. 10.1073/pnas.0407697101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K.-Y., Feng P.-H., Ho S.-C., Chuang K.-J., Chen T.-T., Su C.-L., et al. (2015a). Inter-alpha-trypsin inhibitor heavy chain 4: a novel biomarker for environmental exposure to particulate air pollution in patients with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 10, 831–841. 10.2147/COPD.S81611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. H., Manandhar S., Lee Y. M. (2017a). Roles of RUNX in hypoxia-induced responses and angiogenesis. Adv. Exp. Med. Biol. 962, 449–469. 10.1007/978-981-10-3233-2_27 [DOI] [PubMed] [Google Scholar]
- Lee W.-J., Hah Y.-S., Ock S.-A., Lee J.-H., Jeon R.-H., Park J.-S., et al. (2015b). Cell source-dependent in vivo immunosuppressive properties of mesenchymal stem cells derived from the bone marrow and synovial fluid of minipigs. Exp. Cell Res. 333, 273–288. 10.1016/j.yexcr.2015.03.015 [DOI] [PubMed] [Google Scholar]
- Leeuwen D. M., van Agen E., Gottschalk R. W., Vlietinck R., Gielen M., van Herwijnen M. H., et al. (2006). Cigarette smoke-induced differential gene expression in blood cells from monozygotic twin pairs. Carcinogenesis 28, 691–697. 10.1093/carcin/bgl199 [DOI] [PubMed] [Google Scholar]
- Lei T., Ling X. (2015). IGF-1 promotes the growth and metastasis of hepatocellular carcinoma via the inhibition of proteasome-mediated cathepsin B degradation. World J. Gastroenterol. 21, 10137–10149. 10.3748/wjg.v21.i35.10137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leth-Larsen R., Terp M. G., Christensen A. G., Elias D., Kühlwein T., Jensen O. N., et al. (2012). Functional heterogeneity within the CD44 high human breast cancer stem cell-like compartment reveals a gene signature predictive of distant metastasis. Mol. Med. 18, 1109–1121. 10.2119/molmed.2012.00091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., Xie Z., Li Z., Chen S., Li B. (2016a). MicroRNA-613 targets FMNL2 and suppresses progression of colorectal cancer. Am. J. Transl. Res. 8, 5475–5484. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Li C. Y., Renaud H. J., Klaassen C. D., Cui J. Y. (2016b). Age-specific regulation of drug-processing genes in mouse liver by ligands of xenobiotic-sensing transcription factors. Drug Metab. Dispos. 44, 1038–1049. 10.1124/dmd.115.066639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Gao S., Huang H., Liu W., Huang H., Liu X., et al. (2017a). High throughput sequencing identifies an imprinted gene, Grb10, associated with the pluripotency state in nuclear transfer embryonic stem cells. Oncotarget 8, 47344–47355. 10.18632/oncotarget.17185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Zhao L., Zhang Y., Li W., Duan X., Chen J., et al. (2017b). Imbalanced immune responses involving inflammatory molecules and immune-related pathways in the lung of acute and subchronic arsenic-exposed mice. Environ. Res. 159, 381–393. 10.1016/j.envres.2017.08.036 [DOI] [PubMed] [Google Scholar]
- Li L., Neaves W. B. (2006). Normal stem cells and cancer stem cells: the niche matters. Cancer Res. 66, 4553–4557. 10.1158/0008-5472.CAN-05-3986 [DOI] [PubMed] [Google Scholar]
- Li M., Zhao J., Hu Y., Lu H., Guo J. (2010a). Oxygen free radicals regulate energy metabolism via AMPK pathway following cerebral ischemia. Neurol. Res. 32, 779–784. 10.1179/174313209X459174 [DOI] [PubMed] [Google Scholar]
- Li N., Mu H., Zheng L., Li B., Wu C., Niu B., et al. (2016c). EIF2S3Y suppresses the pluripotency state and promotes the proliferation of mouse embryonic stem cells. Oncotarget 7, 11321–11331. 10.18632/oncotarget.7187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Zhang P., Yu X., Zhao Y., Li Q., Zhang Y., et al. (2017c). Lead transiently promotes granulocyte-macrophage progenitor differentiation and subsequently suppresses common myeloid progenitor differentiation. Toxicol. Sci. 160, 268–283. 10.1093/toxsci/kfx176 [DOI] [PubMed] [Google Scholar]
- Li R., Wang Y., Yang Z., He Y., Zhao T., Fan M., et al. (2015). Hypoxia-inducible factor-1α regulates the expression of L-type voltage-dependent Ca(2+) channels in PC12 cells under hypoxia. Cell Stress Chaperones 20, 507–516. 10.1007/s12192-015-0575-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Qin X., Chai S., Qu C., Wang X., Zhang H. (2016d). Modulation of E-cadherin expression promotes migration ability of esophageal cancer cells. Sci. Rep. 6:21713. 10.1038/srep21713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T. S., Cheng K., Lee S. T., Matsushita S., Davis D., Malliaras K., et al. (2010b). Cardiospheres recapitulate a niche-like microenvironment rich in stemness and cell-matrix interactions, rationalizing their enhanced functional potency for myocardial repair. Stem Cells 28, 2088–2098. 10.1002/stem.532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Zhai B., Zhi H., Li Y., Jia L., Ding C., et al. (2014). Association of ABCB1, β tubulin I, and III with multidrug resistance of MCF7/DOC subline from breast cancer cell line MCF7. Tumor Biol. 35, 8883–8891. 10.1007/s13277-014-2101-z [DOI] [PubMed] [Google Scholar]
- Li X., Yang Y., Fang J., Zhang H. (2013). FIZZ1 could enhance the angiogenic ability of rat aortic endothelial cells. Int. J. Clin. Exp. Pathol. 6, 1847–53. [PMC free article] [PubMed] [Google Scholar]
- Li Z., Rich J. N. (2010). Hypoxia and hypoxia inducible factors in cancer stem cell maintenance. Curr. Top. Microbiol. Immunol. 345, 21–30. 10.1007/82_2010_75 [DOI] [PubMed] [Google Scholar]
- Lin H. (2002). The stem-cell niche theory: lessons from flies. Nat. Rev. Genet. 3, 931–940. 10.1038/nrg952 [DOI] [PubMed] [Google Scholar]
- Lin L., Bass A. J., Lockwood W. W., Wang Z., Silvers A. L., Thomas D. G., et al. (2012). Activation of GATA binding protein 6 (GATA6) sustains oncogenic lineage-survival in esophageal adenocarcinoma. Proc. Natl. Acad. Sci. U.S.A. 109, 4251–4256. 10.1073/pnas.1011989109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Zhang R., Wu J., Pu Y., Yin X., Cheng Y., et al. (2017). Interleukin-17A promotes esophageal adenocarcinoma cell invasiveness through ROS-dependent, NF-κB-mediated MMP-2/9 activation. Oncol. Rep. 37, 1779–1785. 10.3892/or.2017.5426 [DOI] [PubMed] [Google Scholar]
- Liu H., Pathak P., Boehme S., Chiang J. Y. (2016a). Cholesterol 7α-hydroxylase protects the liver from inflammation and fibrosis by maintaining cholesterol homeostasis. J. Lipid Res. 57, 1831–1844. 10.1194/jlr.M069807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R.-Z., Li S., Garcia E., Glubrecht D. D., Poon H. Y., Easaw J. C., et al. (2016b). Association between cytoplasmic CRABP2, altered retinoic acid signaling, and poor prognosis in glioblastoma. Glia 64, 963–976. 10.1002/glia.22976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yuan M., Hou K., Zhang L., Zheng X., Zhao B., et al. (2012). Immune characterization of mesenchymal stem cells in human umbilical cord Wharton's jelly and derived cartilage cells. Cell. Immunol. 278, 35–44. 10.1016/j.cellimm.2012.06.010 [DOI] [PubMed] [Google Scholar]
- Liu T. Z., Wang X., Bai Y. F., Liao H. Z., Qiu S. C., Yang Y. Q., et al. (2014). The HIF-2alpha dependent induction of PAP and adenosine synthesis regulates glioblastoma stem cell function through the A2B adenosine receptor. Int. J. Biochem. Cell Biol. 49, 8–16. 10.1016/j.biocel.2014.01.007 [DOI] [PubMed] [Google Scholar]
- Liu Y., Lu R., Gu J., Chen Y., Zhang X., Zhang L., et al. (2016c). Aldehyde dehydrogenase 1A1 up-regulates stem cell markers in benzo[a]pyrene-induced malignant transformation of BEAS-2B cells. Environ. Toxicol. Pharmacol. 45, 241–250. 10.1016/j.etap.2016.06.007 [DOI] [PubMed] [Google Scholar]
- Loi S., Pommey S., Haibe-Kains B., Beavis P. A., Darcy P. K., Smyth M. J., et al. (2013). CD73 promotes anthracycline resistance and poor prognosis in triple negative breast cancer. Proc. Natl. Acad. Sci. U.S.A. 110, 11091–11096. 10.1073/pnas.1222251110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long H., Xie R., Xiang T., Zhao Z., Lin S., Liang Z., et al. (2012). Autocrine CCL5 signaling promotes invasion and migration of CD133+ovarian cancer stem-like cells via NF-κB-mediated MMP-9 upregulation. Stem Cells 30, 2309–2319. 10.1002/stem.1194 [DOI] [PubMed] [Google Scholar]
- López-Iglesias P., Alcaina Y., Tapia N., Sabour D., Arauzo-Bravo M. J., Sainz de la Maza D., et al. (2015). Hypoxia induces pluripotency in primordial germ cells by HIF1α stabilization and Oct4 deregulation. Antioxid. Redox Signal. 22, 205–223. 10.1089/ars.2014.5871 [DOI] [PubMed] [Google Scholar]
- Lu X., Kang Y. (2009). Cell fusion as a hidden force in tumor progression. Cancer Res. 69, 8536–8539. 10.1158/0008-5472.CAN-09-2159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luckhurst C. A., Ratcliffe M., Stein L., Furber M., Botterell S., Laughton D., et al. (2011). Synthesis and biological evaluation of N-alkylated 8-oxybenz[c]azepine derivatives as selective PPARδ agonists. Bioorg. Med. Chem. Lett. 21, 531–536. 10.1016/j.bmcl.2010.10.083 [DOI] [PubMed] [Google Scholar]
- Luna C., Li G., Qiu J., Epstein D. L., Gonzalez P. (2009). Role of miR-29b on the regulation of the extracellular matrix in human trabecular meshwork cells under chronic oxidative stress. Mol. Vis. 15, 2488–2497. Available online at: http://www.molvis.org/molvis/v15/a266/ [PMC free article] [PubMed] [Google Scholar]
- Lundqvist A., Sandstedt M., Sandstedt J., Wickelgren R., Hansson G. I., Jeppsson A., et al. (2016). The arachidonate 15-lipoxygenase enzyme product 15-HETE is present in heart tissue from patients with ischemic heart disease and enhances clot formation. PLoS ONE 11:e0161629. 10.1371/journal.pone.0161629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Liu D. (2012). Activation of pregnane X receptor by pregnenolone 16 α-carbonitrile prevents high-fat diet-induced obesity in AKR/J mice. PLoS ONE 7:e38734. 10.1371/journal.pone.0038734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Yu W., Shrivastava A., Alemi F., Lankachandra K., Srivastava R. K., et al. (2017). Sanguinarine inhibits pancreatic cancer stem cell characteristics by inducing oxidative stress and suppressing sonic hedgehog-Gli-Nanog pathway. Carcinogenesis 38, 1047–1056. 10.1093/carcin/bgx070 [DOI] [PubMed] [Google Scholar]
- Mahati S., Bolati D., Yang Y., Mao R., Zhang H., Bao Y. (2017a). TMPRSS4 promotes cancer stem cell traits by regulating CLDN1 in hepatocellular carcinoma. Biochem. Biophys. Res. Commun. 490, 906–912. 10.1016/j.bbrc.2017.06.139 [DOI] [PubMed] [Google Scholar]
- Mahati S., Xiao L., Yang Y., Mao R., Bao Y. (2017b). miR-29a suppresses growth and migration of hepatocellular carcinoma by regulating CLDN1. Biochem. Biophys. Res. Commun. 486, 732–737. 10.1016/j.bbrc.2017.03.110 [DOI] [PubMed] [Google Scholar]
- Mallard B. W., Tiralongo J. (2017). Cancer stem cell marker glycosylation: nature, function and significance. Glycoconj. J. 34, 441–452. 10.1007/s10719-017-9780-9 [DOI] [PubMed] [Google Scholar]
- Mannan Baig A., Khan N. A., Effendi V., Rana Z., Ahmad H. R., Abbas F. (2017). Differential receptor dependencies. Anticancer. Drugs 28, 75–87. 10.1097/CAD.0000000000000432 [DOI] [PubMed] [Google Scholar]
- Manzella N., Bracci M., Staffolani S., Strafella E., Rapisarda V., Valentino M., et al. (2013). Styrene altered clock gene expression in serum-shocked cultured human fibroblasts. Biosci. Biotechnol. Biochem. 77, 1296–1298. 10.1271/bbb.120944 [DOI] [PubMed] [Google Scholar]
- Marques M. R., Horner J. S., Ihrie R. A., Bronson R. T., Attardi L. D. (2005). Mice lacking the p53/p63 target gene Perp are resistant to papilloma development. Cancer Res. 65, 6551–6556. 10.1158/0008-5472.CAN-05-0366 [DOI] [PubMed] [Google Scholar]
- Marthiens V., Kazanis I., Moss L., Long K., Ffrench-Constant C. (2010). Adhesion molecules in the stem cell niche - more than just staying in shape? J. Cell Sci. 123, 1613–1622. 10.1242/jcs.054312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin F., Linden T., Katschinski D. M., Oehme F., Flamme I., Mukhopadhyay C. K., et al. (2005). Copper-dependent activation of hypoxia-inducible factor (HIF)-1: implications for ceruloplasmin regulation. Blood 105, 4613–4619. 10.1182/blood-2004-10-3980 [DOI] [PubMed] [Google Scholar]
- Martin G. R., Evans M. J. (1975). Differentiation of clonal lines of teratocarcinoma cells: formation of embryoid bodies in vitro. Proc. Natl. Acad. Sci. U.S.A. 72, 1441–1445. 10.1073/pnas.72.4.1441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masood R., Zhang Y., Bond M., Scadden D., Moudgil T., Law R., et al. (1995). Interleukin-10 is an autocrine growth factor for acquired immunodeficiency syndrome-related B-cell lymphoma. Blood 85, 3423–3430. Available online at: http://www.bloodjournal.org/content/85/12/3423.long?sso-checked=true [PubMed] [Google Scholar]
- Mathieu J., Zhang Z., Zhou W., Wang A. J., Heddleston J. M., Pinna C. M., et al. (2011). HIF induces human embryonic stem cell markers in cancer cells. Cancer Res. 71, 4640–4652. 10.1158/0008-5472.CAN-10-3320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuo T., Dat le T., Komatsu M., Yoshimaru T., Daizumoto K., Sone S., et al. (2014). Early growth response 4 is involved in cell proliferation of small cell lung cancer through transcriptional activation of its downstream genes. PLoS ONE 9:e113606. 10.1371/journal.pone.0113606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattox D. E., Von Hoff D. D. (1980). Culture of human head and neck cancer stem cells using soft agar. Arch. Otolaryngol. 106, 672–674. 10.1001/archotol.1980.00790350014005 [DOI] [PubMed] [Google Scholar]
- Meding S., Balluff B., Elsner M., Schöne C., Rauser S., Nitsche U., et al. (2012). Tissue-based proteomics reveals FXYD3, S100A11 and GSTM3 as novel markers for regional lymph node metastasis in colon cancer. J. Pathol. 228, 459–470. 10.1002/path.4021 [DOI] [PubMed] [Google Scholar]
- Melchiori A., Colacci A., Lollini P. L., De Giovanni C., Carlone S., Grilli S., et al. (1992). Induction of invasive and experimental metastasis potential in BALB/c 3T3 cells by benzo(a)pyrene transformation. Invasion Metastasis 12, 1–11. [PubMed] [Google Scholar]
- Meng E., Mitra A., Tripathi K., Finan M. A., Scalici J., McClellan S., et al. (2014). ALDH1A1 maintains ovarian cancer stem cell-like properties by altered regulation of cell cycle checkpoint and DNA repair network signaling. PLoS ONE 9:e107142. 10.1371/journal.pone.0107142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercado-Pimentel M. E., Runyan R. B. (2007). Multiple transforming growth factor-beta isoforms and receptors function during epithelial-mesenchymal cell transformation in the embryonic heart. Cells Tissues Organs 185, 146–156. 10.1159/000101315 [DOI] [PubMed] [Google Scholar]
- Michalec L., Choudhury B. K., Postlethwait E., Wild J. S., Alam R., Lett-Brown M., et al. (2002). CCL7 and CXCL10 orchestrate oxidative stress-induced neutrophilic lung inflammation. J. Immunol. 168, 846–52. 10.4049/jimmunol.168.2.846 [DOI] [PubMed] [Google Scholar]
- Mikesch J.-H., Schier K., Roetger A., Simon R., Buerger H., Brandt B. (2006). The expression and action of decay-accelerating factor (CD55) in human malignancies and cancer therapy. Cell. Oncol. 28, 223–232. 10.1155/2006/814816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklos W., Heffeter P., Pirker C., Hager S., Kowol C., van Schoonhoven S., et al. (2016). Loss of phosphodiesterase 4D mediates acquired triapine resistance via Epac-Rap1-Integrin signaling. Oncotarget 7, 84556–84574. 10.18632/oncotarget.11821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mintz B., Illmensee K. (1975). Normal genetically mosaic mice produced from malignant teratocarcinoma cells. Proc. Natl. Acad. Sci. U.S.A. 72, 3585–3589. 10.1073/pnas.72.9.3585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra A., Wang J., Shiozawa Y., McGee S., Kim J., Jung Y., et al. (2012). Hypoxia stabilizes GAS6/Axl signaling in metastatic prostate cancer. Mol. Cancer Res. 10, 703–712. 10.1158/1541-7786.MCR-11-0569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell M. I., Engelbrecht A. M. (2015). Circadian rhythms and breast cancer: the role of Per2 in doxorubicin-induced cell death. J. Toxicol. 2015:392360. 10.1155/2015/392360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal K., Donthamsetty S., Kaur R., Yang C., Gupta M. V., Reid M. D., et al. (2017). Multinucleated polyploidy drives resistance to Docetaxel chemotherapy in prostate cancer. Br. J. Cancer 116, 1186–1194. 10.1038/bjc.2017.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyagaki T., Sugaya M., Murakami T., Asano Y., Tada Y., Kadono T., et al. (2011). CCL11-CCR3 interactions promote survival of anaplastic large cell lymphoma cells via ERK1/2 activation. Cancer Res. 71, 2056–2065. 10.1158/0008-5472.CAN-10-3764 [DOI] [PubMed] [Google Scholar]
- Mizuno S., Hanamura I., Ota A., Karnan S., Narita T., Ri M., et al. (2015). Overexpression of salivary-type amylase reduces the sensitivity to bortezomib in multiple myeloma cells. Int. J. Hematol. 102, 569–578. 10.1007/s12185-015-1859-0 [DOI] [PubMed] [Google Scholar]
- Mohyeldin A., Garzón-Muvdi T., Quiñones-Hinojosa A. (2010). Oxygen in stem cell biology: a critical component of the stem cell niche. Cell Stem Cell 7, 150–161. 10.1016/j.stem.2010.07.007 [DOI] [PubMed] [Google Scholar]
- Monzen S., Tashiro E., Kashiwakura I. (2011). Megakaryocytopoiesis and thrombopoiesis in hematopoietic stem cells exposed to ionizing radiation. Radiat. Res. 176, 716–724. 10.1667/RR2725.1 [DOI] [PubMed] [Google Scholar]
- Morimura T., Fujita K., Akita M., Nagashima M., Satomi A. (2008). The proton pump inhibitor inhibits cell growth and induces apoptosis in human hepatoblastoma. Pediatr. Surg. Int. 24, 1087–1094. 10.1007/s00383-008-2229-2 [DOI] [PubMed] [Google Scholar]
- Mouillet J.-F., Donker R. B., Mishima T., Cronqvist T., Chu T., Sadovsky Y. (2013). The unique expression and function of miR-424 in human placental trophoblasts1. Biol. Reprod. 89:25. 10.1095/biolreprod.113.110049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulder J. E., Rockwell S. (1987). Tumor hypoxia: its impact on cancer therapy. Cancer Metastasis Rev. 5, 313–341. 10.1007/BF00055376 [DOI] [PubMed] [Google Scholar]
- Murr C., Fuith L. C., Widner B., Wirleitner B., Baier-Bitterlich G., Fuchs D. (1999). Increased neopterin concentrations in patients with cancer: indicator of oxidative stress? Anticancer Res. 19, 1721–1728. [PubMed] [Google Scholar]
- Nagler C., Hardt C., Zänker K. S., Dittmar T. (2011). Co-cultivation of murine BMDCs with 67NR mouse mammary carcinoma cells give rise to highly drug resistant cells. Cancer Cell Int. 11:21. 10.1186/1475-2867-11-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagy Z., Kovács I., Török M., Tóth D., Vereb G., Buzás K., et al. (2014). Function of RasGRP3 in the formation and progression of human breast cancer. Mol. Cancer 13, 96. 10.1186/1476-4598-13-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemmiche S. (2017). Oxidative signaling response to cadmium exposure. Toxicol. Sci. 156, 4–10. 10.1093/toxsci/kfw222 [DOI] [PubMed] [Google Scholar]
- Netzer N., Gatterer H., Faulhaber M., Burtscher M., Pramsohler S., Pesta D. (2015). Hypoxia, oxidative stress and fat. Biomolecules 5, 1143–1150. 10.3390/biom5021143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomura M., Yoshimura Y., Kikuiri T., Hasegawa T., Taniguchi Y., Deyama Y., et al. (2011). Platinum nanoparticles suppress osteoclastogenesis through scavenging of reactive oxygen species produced in RAW264.7 cells. J. Pharmacol. Sci. 117, 243–252. 10.1254/jphs.11099FP [DOI] [PubMed] [Google Scholar]
- Nowell P. C. (1976). The clonal evolution of tumor cell populations. Science 194, 23–28. 10.1126/science.959840 [DOI] [PubMed] [Google Scholar]
- Obianime A. W., Roberts I. I. (2009). Antioxidants, cadmium-induced toxicity, serum biochemical and the histological abnormalities of the kidney and testes of the male Wistar rats. Niger. J. Physiol. Sci. 24, 177–185. [DOI] [PubMed] [Google Scholar]
- O'Brien L. E., Bilder D. (2013). Beyond the niche: tissue-level coordination of stem cell dynamics. Annu. Rev. Cell Dev. Biol. 29, 107–136. 10.1146/annurev-cellbio-101512-122319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogino T., Kobuchi H., Fujita H., Matsukawa A., Utsumi K. (2014). Erythroid and megakaryocytic differentiation of K562 erythroleukemic cells by monochloramine. Free Radic. Res. 48, 292–302. 10.3109/10715762.2013.865840 [DOI] [PubMed] [Google Scholar]
- Ohlstein B., Kai T., Decotto E., Spradling A. (2004). The stem cell niche: theme and variations. Curr. Opin. Cell Biol. 16, 693–699. 10.1016/j.ceb.2004.09.003 [DOI] [PubMed] [Google Scholar]
- Ohmura G., Tsujikawa T., Yaguchi T., Kawamura N., Mikami S., Sugiyama J., et al. (2015). Aberrant myosin 1b expression promotes cell migration and lymph node metastasis of HNSCC. Mol. Cancer Res. 13, 721–731. 10.1158/1541-7786.MCR-14-0410 [DOI] [PubMed] [Google Scholar]
- Oikawa K., Mizusaki A., Takanashi M., Ozaki T., Sato F., Kuroda M., et al. (2017). PRG4 expression in myxoid liposarcoma maintains tumor cell growth through suppression of an antitumor cytokine IL-24. Biochem. Biophys. Res. Commun. 485, 209–214. 10.1016/j.bbrc.2017.02.055 [DOI] [PubMed] [Google Scholar]
- Osanai M., Lee G. H. (2015). The retinoic acid-metabolizing enzyme CYP26A1 upregulates fascin and promotes the malignant behavior of breast carcinoma cells. Oncol. Rep. 34, 850–858. 10.3892/or.2015.4042 [DOI] [PubMed] [Google Scholar]
- Osanai M., Sawada N., Lee G.-H. (2010). Oncogenic and cell survival properties of the retinoic acid metabolizing enzyme, CYP26A1. Oncogene 29, 1135–1144. 10.1038/onc.2009.414 [DOI] [PubMed] [Google Scholar]
- Pacheco K. A., Tarkowski M., Sterritt C., Negri J., Rosenwasser L. J., Borish L. (2001). The influence of diesel exhaust particles on mononuclear phagocytic cell-derived cytokines: IL-10, TGF-beta and IL-1 beta. Clin. Exp. Immunol. 126, 374–383. 10.1046/j.1365-2249.2001.01698.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pant S. D., March L. D., Famulski J. K., French C. R., Lehmann O. J., Waskiewicz A. J. (2013). Molecular mechanisms regulating ocular apoptosis in zebrafish gdf6a mutants. Investig. Ophthalmol. Vis. Sci. 54, 5871–5879. 10.1167/iovs.12-11315 [DOI] [PubMed] [Google Scholar]
- Papageorgio C., Brachmann R., Zeng J., Culverhouse R., Zhang W., McLeod H. (2007). MAGED2: a novel p53-dissociator. Int. J. Oncol. 31, 1205–1211. 10.3892/ijo.31.5.1205 [DOI] [PubMed] [Google Scholar]
- Park Y. H., Sohn S. K., Kim J. G., Lee M. H., Song H. S., Kim M. K., et al. (2009). Interaction between BCL2 and interleukin-10 gene polymorphisms alter outcomes of diffuse large B-cell lymphoma following rituximab plus CHOP chemotherapy. Clin. Cancer Res. 15, 2107–2115. 10.1158/1078-0432.CCR-08-1588 [DOI] [PubMed] [Google Scholar]
- Pathak S. (1990). Cytogenetic abnormalities in cancer: with special emphasis on tumor heterogeneity. Cancer Metastasis Rev. 8, 299–318. 10.1007/BF00052606 [DOI] [PubMed] [Google Scholar]
- Peek C. B., Levine D. C., Cedernaes J., Taguchi A., Kobayashi Y., Tsai S. J., et al. (2017). Circadian clock interaction with HIF1α mediates oxygenic metabolism and anaerobic glycolysis in skeletal muscle. Cell Metab. 25, 86–92. 10.1016/j.cmet.2016.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peet D. J., Kittipassorn T., Wood J. P., Chidlow G., Casson R. J. (2017). HIF signalling: the eyes have it. Exp. Cell Res. 356, 136–140. 10.1016/j.yexcr.2017.03.030 [DOI] [PubMed] [Google Scholar]
- Peeters S. D., van der Kolk D. M., de Haan G., Bystrykh L., Kuipers F., de Vries E. G., et al. (2006). Selective expression of cholesterol metabolism genes in normal CD34+CD38– cells with a heterogeneous expression pattern in AML cells. Exp. Hematol. 34, 622–630. 10.1016/j.exphem.2006.01.020 [DOI] [PubMed] [Google Scholar]
- Peixoto Lira R. C., Fedatto P. F., Marco Antonio D. S., Leal L. F., Martinelli C. E., De Castro M., et al. (2016). IGF2 and IGF1R in pediatric adrenocortical tumors: roles in metastasis and steroidogenesis. Endocr. Relat. Cancer 23, 481–493. 10.1530/ERC-15-0426 [DOI] [PubMed] [Google Scholar]
- Perotti V., Baldassari P., Molla A., Vegetti C., Bersani I., Maurichi A., et al. (2016). NFATc2 is an intrinsic regulator of melanoma dedifferentiation. Oncogene 35, 2862–2872. 10.1038/onc.2015.355 [DOI] [PubMed] [Google Scholar]
- Pizzino G., Irrera N., Cucinotta M., Pallio G., Mannino F., Arcoraci V., et al. (2017). Oxidative stress: harms and benefits for human health. Oxid. Med. Cell. Longev. 2017, 1–13. 10.1155/2017/8416763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plösch T., Gellhaus A., Van Straten E. M., Wolf N., Huijkman N. C., Schmidt M., et al. (2010). The liver X receptor (LXR) and its target gene ABCA1 are regulated upon low oxygen in human trophoblast cells: a reason for alterations in preeclampsia? Placenta 31, 910–918. 10.1016/j.placenta.2010.07.009 [DOI] [PubMed] [Google Scholar]
- Poormasjedi-Meibod M. S., Salimi Elizei S., Leung V., Baradar Jalili R., Ko F., Ghahary A. (2016). Kynurenine modulates MMP-1 and type-I collagen expression via aryl hydrocarbon receptor activation in dermal fibroblasts. J. Cell. Physiol. 231, 2749–2760. 10.1002/jcp.25383 [DOI] [PubMed] [Google Scholar]
- Pope J. L., Bhat A. A., Sharma A., Ahmad R., Krishnan M., Washington M. K., et al. (2014). Claudin-1 regulates intestinal epithelial homeostasis through the modulation of Notch-signalling. Gut 63, 622–634. 10.1136/gutjnl-2012-304241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter E. A., Dolgova E. V., Proskurina A. S., Efremov Y. M., Minkevich A. R., Rozanov A. S., et al. (2017). Gene expression profiling of tumor-initiating stem cells from mouse Krebs-2 carcinoma using a novel marker of poorly differentiated cells. Oncotarget 8, 9425–9441. 10.18632/oncotarget.14116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter E. A., Dolgova E. V., Proskurina A. S., Efremov Y. R., Taranov O. S., Nikolin V. P., et al. (2016a). Development of the therapeutic regimen based on the synergistic activity of cyclophosphamide and doublestranded DNA preparation which results in complete cure of mice engrafted with Krebs-2 ascites. Vavilov J. Genet. Breed. 20, 723–735. 10.18699/VJ16.162 [DOI] [Google Scholar]
- Potter E. A., Dolgova E. V., Proskurina A. S., Minkevich A. M., Efremov Y. R., Taranov O. S., et al. (2016b). A strategy to eradicate well-developed Krebs-2 ascites in mice. Oncotarget 7, 11580–11594. 10.18632/oncotarget.7311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter E. A., Proskurina A. S., Ritter G. S., Dolgova E. V., Nikolin V. P., Popova N. A., et al. (2018). Efficacy of a new cancer treatment strategy based on eradication of tumor-initiating stem cells in a mouse model of Krebs-2 solid adenocarcinoma. Oncotarget 9, 28486–28499. 10.18632/oncotarget.25503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers G. L., Hammer K. D., Domenech M., Frantskevich K., Malinowski R. L., Bushman W., et al. (2015). Phosphodiesterase 4D inhibitors limit prostate cancer growth potential. Mol. Cancer Res. 13, 149–160. 10.1158/1541-7786.MCR-14-0110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prevo R., Banerji S., Ferguson D. J., Clasper S., Jackson D. G. (2001). Mouse LYVE-1 is an endocytic receptor for hyaluronan in lymphatic endothelium. J. Biol. Chem. 276, 19420–19430. 10.1074/jbc.M011004200 [DOI] [PubMed] [Google Scholar]
- Pullamsetti S. S., Banat G. A., Schmall A., Szibor M., Pomagruk D., Hänze J., et al. (2013). Phosphodiesterase-4 promotes proliferation and angiogenesis of lung cancer by crosstalk with HIF. Oncogene 32, 1121–1134. 10.1038/onc.2012.136 [DOI] [PubMed] [Google Scholar]
- Puri N., Sodhi K., Haarstad M., Kim D. H., Bohinc S., Foglio E., et al. (2012). Heme induced oxidative stress attenuates sirtuin1 and enhances adipogenesis in mesenchymal stem cells and mouse pre-adipocytes. J. Cell. Biochem. 113, 1926–1935. 10.1002/jcb.24061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin Z., Dai L., Bratoeva M., Slomiany M. G., Toole B. P., Parsons C. (2011). Cooperative roles for emmprin and LYVE-1 in the regulation of chemoresistance for primary effusion lymphoma. Leukemia 25, 1598–1609. 10.1038/leu.2011.144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan Y., Zhang X., Xu S., Li K., Zhu F., Li Q., et al. (2016). Tcf7l2 localization of putative stem/progenitor cells in mouse conjunctiva. Am. J. Physiol. Physiol. 311, C246–C254. 10.1152/ajpcell.00014.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramírez-Ortega D., Ramiro-Salazar A., González-Esquivel D., Ríos C., Pineda B., Pérez de la Cruz V. (2017). 3-Hydroxykynurenine and 3-hydroxyanthranilic acid enhance the toxicity induced by copper in rat astrocyte culture. Oxid. Med. Cell. Longev. 2017, 1–12. 10.1155/2017/2371895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravindranath A., O'Connell A., Johnston P. G., El-Tanani M. K. (2008). The role of LEF/TCF factors in neoplastic transformation. Curr. Mol. Med. 8, 38–50. 10.2174/156652408783565559 [DOI] [PubMed] [Google Scholar]
- Reya T., Morrison S. J., Clarke M. F., Weissman I. L. (2001). Stem cells, cancer, and cancer stem cells. Nature 414, 105–111. 10.1038/35102167 [DOI] [PubMed] [Google Scholar]
- Ricciardi A., Elia A. R., Cappello P., Puppo M., Vanni C., Fardin P., et al. (2008). Transcriptome of hypoxic immature dendritic cells: modulation of chemokine/receptor expression. Mol. Cancer Res. 6, 175–185. 10.1158/1541-7786.MCR-07-0391 [DOI] [PubMed] [Google Scholar]
- Rich J. N. (2016). Cancer stem cells: understanding tumor hierarchy and heterogeneity. Medicine 95, S2–S7. 10.1097/MD.0000000000004764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosinski K. V., Fujii N., Mito J. K., Koo K. K. W., Xuereb S. M., Sala-Torra O., et al. (2008). DDX3Y encodes a class I MHC-restricted H-Y antigen that is expressed in leukemic stem cells. Blood 111, 4817–4826. 10.1182/blood-2007-06-096313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roszak J., Smok-Pieniazek A., Nocun M., Stepnik M. (2013). Characterization of arsenic trioxide resistant clones derived from Jurkat leukemia T cell line: focus on PI3K/Akt signaling pathway. Chem. Biol. Interact. 205, 198–211. 10.1016/j.cbi.2013.07.011 [DOI] [PubMed] [Google Scholar]
- Royer C., Lachuer J., Crouzoulon G., Roux J., Peyronnet J., Mamet J., et al. (2000). Effects of gestational hypoxia on mRNA levels of Glut3 and Glut4 transporters, hypoxia inducible factor-1 and thyroid hormone receptors in developing rat brain. Brain Res. 856, 119–128. 10.1016/S0006-8993(99)02365-3 [DOI] [PubMed] [Google Scholar]
- Sabe H., Hashimoto S., Morishige M., Ogawa E., Hashimoto A., Nam J.-M., et al. (2009). The EGFR-GEP100-Arf6-AMAP1 signaling pathway specific to breast cancer invasion and metastasis. Traffic 10, 982–993. 10.1111/j.1600-0854.2009.00917.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saijo H., Hirohashi Y., Torigoe T., Horibe R., Takaya A., Murai A., et al. (2016). Plasticity of lung cancer stem-like cells is regulated by the transcription factor HOXA5 that is induced by oxidative stress. Oncotarget 7, 50043–50056. 10.18632/oncotarget.10571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sáinz N., Rodríguez A., Catalán V., Becerril S., Ramírez B., Gómez-Ambrosi J., et al. (2010). Leptin administration downregulates the increased expression levels of genes related to oxidative stress and inflammation in the skeletal muscle of ob/ob mice. Mediators Inflamm. 2010:784343. 10.1155/2010/784343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai E., Morita M., Ohuchi M., Kido M. A., Fukuma Y., Nishishita K., et al. (2017). Effects of deficiency of Kelch-like ECH-associated protein 1 on skeletal organization: a mechanism for diminished nuclear factor of activated T cells cytoplasmic 1 during osteoclastogenesis. FASEB J. 31, 4011–4022. 10.1096/fj.201700177R [DOI] [PubMed] [Google Scholar]
- Sakamoto Y., Prudhomme S., Zaman M. H. (2011). Viscoelastic gel-strip model for the simulation of migrating cells. Ann. Biomed. Eng. 39, 2735–2749. 10.1007/s10439-011-0360-z [DOI] [PubMed] [Google Scholar]
- Salyer S. A., Olberding J. R., Distler A. A., Lederer E. D., Clark B. J., Delamere N. A., et al. (2013). Vacuolar ATPase driven potassium transport in highly metastatic breast cancer cells. Biochim. Biophys. Acta-Mol. Basis Dis. 1832, 1734–1743. 10.1016/j.bbadis.2013.04.023 [DOI] [PubMed] [Google Scholar]
- Sasaki H., Shitara M., Yokota K., Hikosaka Y., Moriyama S., Yano M., et al. (2012). RagD gene expression and NRF2 mutations in lung squamous cell carcinomas. Oncol. Lett. 4, 1167–1170. 10.3892/ol.2012.938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saygin C., Wiechert A., Rao V. S., Alluri R., Connor E., Thiagarajan P. S., et al. (2017). CD55 regulates self-renewal and cisplatin resistance in endometrioid tumors. J. Exp. Med. 214, 2715–2732. 10.1084/jem.20170438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield R. (1978). The relationship between the spleen colony-forming cell and the haemopoietic stem cell. Blood Cells 4, 7–25. [PubMed] [Google Scholar]
- Schofield R. (1983). The stem cell system. Biomed. Pharmacother. 37, 375–380. [PubMed] [Google Scholar]
- Seaborn T., Ravni A., Au R., Chow B. K., Fournier A., Wurtz O., et al. (2014). Induction of serpinb1a by PACAP or NGF is required for PC12 cells survival after serum withdrawal. J. Neurochem. 131, 21–32. 10.1111/jnc.12780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo E. J., Kim D. K., Jang I. H., Choi E. J., Shin S. H., Lee S. I., et al. (2016). Hypoxia-NOTCH1-SOX2 signaling is important for maintaining cancer stem cells in ovarian cancer. Oncotarget 7, 55624–55638. 10.18632/oncotarget.10954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen D., Wang Y. (1994). Effects of hypoxia on platelet activation in pilots. Aviat. Space. Environ. Med. 65, 646–648. [PubMed] [Google Scholar]
- Shen D., Wang Y. (1998). Changes of plasma level of neurotensin, somatostatin, and dynorphin A in pilots under acute hypoxia. Mil. Med. 163, 120–121. 10.1093/milmed/163.2.120 [DOI] [PubMed] [Google Scholar]
- Shitashige M., Hirohashi S., Yamada T. (2008). Wnt signaling inside the nucleus. Cancer Sci. 99, 631–637. 10.1111/j.1349-7006.2007.00716.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shojima K., Sato A., Hanaki H., Tsujimoto I., Nakamura M., Hattori K., et al. (2015). Wnt5a promotes cancer cell invasion and proliferation by receptor-mediated endocytosis-dependent and -independent mechanisms, respectively. Sci. Rep. 5:8042. 10.1038/srep08042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sies H., Berndt C., Jones D. P. (2017). Oxidative stress. Annu. Rev. Biochem. 86, 715–748. 10.1146/annurev-biochem-061516-045037 [DOI] [PubMed] [Google Scholar]
- Sithu S. D., Srivastava S., Siddiqui M. A., Vladykovskaya E., Riggs D. W., Conklin D. J., et al. (2010). Exposure to acrolein by inhalation causes platelet activation. Toxicol. Appl. Pharmacol. 248, 100–110. 10.1016/j.taap.2010.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slevin M., Krupinski J., Rovira N., Turu M., Luque A., Baldellou M., et al. (2009). Identification of pro-angiogenic markers in blood vessels from stroked-affected brain tissue using laser-capture microdissection. BMC Genomics 10:113. 10.1186/1471-2164-10-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song K., Kwon H., Han C., Zhang J., Dash S., Lim K., et al. (2015). Active glycolytic metabolism in CD133(+) hepatocellular cancer stem cells: regulation by MIR-122. Oncotarget 6, 40822–40835. 10.18632/oncotarget.5812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souroullas G. P., Salmon J. M., Sablitzky F., Curtis D. J., Goodell M. A. (2009). Adult hematopoietic stem and progenitor cells require either Lyl1 or Scl for survival. Cell Stem Cell 4, 180–186. 10.1016/j.stem.2009.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa M. S., Latini F. R., Monteiro H. P., Cerutti J. M. (2010). Arginase 2 and nitric oxide synthase: pathways associated with the pathogenesis of thyroid tumors. Free Radic. Biol. Med. 49, 997–1007. 10.1016/j.freeradbiomed.2010.06.006 [DOI] [PubMed] [Google Scholar]
- Stanford E. A., Wang Z., Novikov O., Mulas F., Landesman-Bollag E., Monti S., et al. (2016). The role of the aryl hydrocarbon receptor in the development of cells with the molecular and functional characteristics of cancer stem-like cells. BMC Biol. 14:20. 10.1186/s12915-016-0240-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele M. W. (1970). Clonal origin for individual Burkitt tumours. Lancet 1:677. [DOI] [PubMed] [Google Scholar]
- Steidl U., Schroeder T., Steidl C., Kobbe G., Graef T., Bork S., et al. (2005). Distinct gene expression pattern of malignant hematopoietic stem and progenitor cells in polycythemia vera. Ann. N. Y. Acad. Sci. 1044, 94–108. 10.1196/annals.1349.013 [DOI] [PubMed] [Google Scholar]
- Strzalka-Mrozik B., Prudlo L., Kimsa M. W., Kimsa M. C., Kapral M., Nita M., et al. (2013). Quantitative analysis of SOD2, ALDH1A1 and MGST1 messenger ribonucleic acid in anterior lens epithelium of patients with pseudoexfoliation syndrome. Mol. Vis. 19, 1341–1349. Available online at: http://www.molvis.org/molvis/v19/1341/ [PMC free article] [PubMed] [Google Scholar]
- Stübke K., Wicklein D., Herich L., Schumacher U., Nehmann N. (2012). Selectin-deficiency reduces the number of spontaneous metastases in a xenograft model of human breast cancer. Cancer Lett. 321, 89–99. 10.1016/j.canlet.2012.02.019 [DOI] [PubMed] [Google Scholar]
- Su B., Zhao W., Shi B., Zhang Z., Yu X., Xie F., et al. (2014). Let-7d suppresses growth, metastasis, and tumor macrophage infiltration in renal cell carcinoma by targeting COL3A1 and CCL7. Mol. Cancer 13:206. 10.1186/1476-4598-13-206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suga N., Murakami A., Nakamura Y., Ishisaka A., Kitamoto N., Ito M., et al. (2017). Cytotoxic and cytoprotective effects of tryptamine-4,5-dione on neuronal cells: a double-edged sword. Free Radic. Res. 51, 545–553. 10.1080/10715762.2017.1331038 [DOI] [PubMed] [Google Scholar]
- Sullivan B. P., Cui W., Copple B. L., Luyendyk J. P. (2012). Early growth response factor-1 limits biliary fibrosis in a model of xenobiotic-induced cholestasis in mice. Toxicol. Sci. 126, 267–274. 10.1093/toxsci/kfr311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun D. X., Liao G. J., Liu K. G., Jian H. (2015). Endosialin-expressing bone sarcoma stem-like cells are highly tumor-initiating and invasive. Mol. Med. Rep. 12, 5665–5670. 10.3892/mmr.2015.4218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun M., Zhou W., Zhang Y. Y., Wang D. L., Wu X. L. (2013). CD44+ gastric cancer cells with stemness properties are chemoradioresistant and highly invasive. Oncol. Lett. 5, 1793–1798. 10.3892/ol.2013.1272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Du C., Wang B., Zhang Y., Liu X., Ren G. (2014). Up-regulation of eEF1A2 promotes proliferation and inhibits apoptosis in prostate cancer. Biochem. Biophys. Res. Commun. 450, 1–6. 10.1016/j.bbrc.2014.05.045 [DOI] [PubMed] [Google Scholar]
- Süsskind D., Hurst J., Rohrbach J. M., Schnichels S. (2017). Novel mouse model for primary uveal melanoma: a pilot study. Clin. Experiment. Ophthalmol. 45, 192–200. 10.1111/ceo.12814 [DOI] [PubMed] [Google Scholar]
- Taddei M. L., Giannoni E., Fiaschi T., Chiarugi P. (2012). Anoikis: an emerging hallmark in health and diseases. J. Pathol. 226, 380–393. 10.1002/path.3000 [DOI] [PubMed] [Google Scholar]
- Takahashi K., Yamanaka S. (2006). Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676. 10.1016/j.cell.2006.07.024 [DOI] [PubMed] [Google Scholar]
- Takano M., Meneshian A., Sheikh E., Yamakawa Y., Wilkins K. B., Hopkins E. A., et al. (2002). Rapid upregulation of endothelial P-selectin expression via reactive oxygen species generation. Am. J. Physiol. Circ. Physiol. 283, H2054–H2061. 10.1152/ajpheart.01001.2001 [DOI] [PubMed] [Google Scholar]
- Takubo K., Nagamatsu G., Kobayashi C. I., Nakamura-Ishizu A., Kobayashi H., Ikeda E., et al. (2013). Regulation of glycolysis by Pdk functions as a metabolic checkpoint for cell cycle quiescence in hematopoietic stem cells. Cell Stem Cell 12, 49–61. 10.1016/j.stem.2012.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan J. E., Wong S. C., Gan S. K., Xu S., Lam K. P. (2001). The adaptor protein BLNK is required for b cell antigen receptor-induced activation of nuclear factor-kappa B and cell cycle entry and survival of B lymphocytes. J. Biol. Chem. 276, 20055–20063. 10.1074/jbc.M010800200 [DOI] [PubMed] [Google Scholar]
- Tang J. P., Tan C. P., Li J., Siddique M. M., Guo K., Chan S. W., et al. (2010). VHZ is a novel centrosomal phosphatase associated with cell growth and human primary cancers. Mol. Cancer 9:128. 10.1186/1476-4598-9-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang X., Mahajan S. S., Nguyen L. T., Béliveau F., Leduc R., Simon J. A., et al. (2014). Targeted inhibition of cell-surface serine protease Hepsin blocks prostate cancer bone metastasis. Oncotarget 5, 1352–1362. 10.18632/oncotarget.1817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taoka Y., Matsumoto K., Ohashi K., Minamida S., Hagiwara M., Nagi S., et al. (2015). Protein expression profile related to cisplatin resistance in bladder cancer cell lines detected by two-dimensional gel electrophoresis. Biomed. Res. 36, 253–261. 10.2220/biomedres.36.253 [DOI] [PubMed] [Google Scholar]
- Thiel G., Cibelli G. (2002). Regulation of life and death by the zinc finger transcription factor Egr-1. J. Cell. Physiol. 193, 287–292. 10.1002/jcp.10178 [DOI] [PubMed] [Google Scholar]
- Tominaga K., Shimamura T., Kimura N., Murayama T., Matsubara D., Kanauchi H., et al. (2017). Addiction to the IGF2-ID1-IGF2 circuit for maintenance of the breast cancer stem-like cells. Oncogene 36, 1276–1286. 10.1038/onc.2016.293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonnetti L., Netzel-Arnett S., Darnell G. A., Hayes T., Buzza M. S., Anglin I. E., et al. (2008). SerpinB2 protection of retinoblastoma protein from calpain enhances tumor cell survival. Cancer Res. 68, 5648–5657. 10.1158/0008-5472.CAN-07-5850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touyz R. M. (2014). Linking LOX-1 and arginase II through mitochondria: a novel paradigm in endothelial dysfunction. Circ. Res. 115, 412–414. 10.1161/CIRCRESAHA.114.304550 [DOI] [PubMed] [Google Scholar]
- Tritschler I., Gramatzki D., Capper D., Mittelbronn M., Meyermann R., Saharinen J., et al. (2009). Modulation of TGF-β activity by latent TGF-β-binding protein 1 in human malignant glioma cells. Int. J. Cancer 125, 530–540. 10.1002/ijc.24443 [DOI] [PubMed] [Google Scholar]
- Tsai W.-B., Long Y., Park J.-R., Chang J. T., Liu H., Rodriguez-Canales J., et al. (2016). Gas6/Axl is the sensor of arginine-auxotrophic response in targeted chemotherapy with arginine-depleting agents. Oncogene 35, 1632–1642. 10.1038/onc.2015.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuccitto A., Tazzari M., Beretta V., Rini F., Miranda C., Greco A., et al. (2016). Immunomodulatory factors control the fate of melanoma tumor initiating cells. Stem Cells 34, 2449–2460. 10.1002/stem.2413 [DOI] [PubMed] [Google Scholar]
- Tucker R. P., Ferralli J., Schittny J. C., Chiquet-Ehrismann R. (2013). Tenascin-C and tenascin-W in whisker follicle stem cell niches: possible roles in regulating stem cell proliferation and migration. J. Cell Sci. 126, 5111–5115. 10.1242/jcs.134650 [DOI] [PubMed] [Google Scholar]
- Tye S. L., Gilg A. G., Tolliver L. B., Wheeler W. G., Toole B. P., Maria B. L. (2008). Hyaluronan regulates ceruloplasmin production by gliomas and their treatment-resistant multipotent progenitors. J. Child Neurol. 23, 1221–1230. 10.1177/0883073808321066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Lee W. H., Choong L. Y., Jin T. H., Mon N. N., Chong S., Liew C. S., et al. (2017b). TRPV4 plays a role in breast cancer cell migration via Ca2+-dependent activation of AKT and downregulation of E-cadherin cell cortex protein. Oncogenesis 6:e338 10.1038/oncsis.2017.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Thienen R., Masschelein E., D'Hulst G., Thomis M., Hespel P. (2017). Twin resemblance in muscle HIF-1α responses to hypoxia and exercise. Front. Physiol. 7:676. 10.3389/fphys.2016.00676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vias M., Burtt G., Culig Z., Veerakumarasivam A., Neal D. E., Mills I. G. (2007). A role for neurotensin in bicalutamide resistant prostate cancer cells. Prostate 67, 190–202. 10.1002/pros.20518 [DOI] [PubMed] [Google Scholar]
- Victorino V. J., Pizzatti L., Michelletti P., Panis C. (2014). Oxidative stress, redox signaling and cancer chemoresistance: putting together the pieces of the puzzle. Curr. Med. Chem. 21, 3211–3226. 10.2174/0929867321666140601164647 [DOI] [PubMed] [Google Scholar]
- Vo T. K. D., de Saint-Hubert M., Morrhaye G., Godard P., Geenen V., Martens H. J., et al. (2011). Transcriptomic biomarkers of the response of hospitalized geriatric patients admitted with heart failure. Comparison to hospitalized geriatric patients with infectious diseases or hip fracture. Mech. Ageing Dev. 132, 131–139. 10.1016/j.mad.2011.02.002 [DOI] [PubMed] [Google Scholar]
- Vogiatzi F., Brandt D. T., Schneikert J., Fuchs J., Grikscheit K., Wanzel M., et al. (2016). Mutant p53 promotes tumor progression and metastasis by the endoplasmic reticulum UDPase ENTPD5. Proc. Natl. Acad. Sci. U.S.A. 113, E8433–E8442. 10.1073/pnas.1612711114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volm M. (1998). Multidrug resistance and its reversal. Anticancer Res. 18, 2905–2917. [PubMed] [Google Scholar]
- Voog J., Jones D. L. (2010). Stem cells and the niche: a dynamic duo. Cell Stem Cell 6, 103–115. 10.1016/j.stem.2010.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahba M. G., Messiha B. A., Abo-Saif A. A. (2016). Protective effects of fenofibrate and resveratrol in an aggressive model of rheumatoid arthritis in rats. Pharm. Biol. 54, 1705–1715. 10.3109/13880209.2015.1125931 [DOI] [PubMed] [Google Scholar]
- Wan J., Badham H. J., Winn L. (2005). The role of c-MYB in benzene-initiated toxicity. Chem. Biol. Interact. 153–154, 171–178. 10.1016/j.cbi.2005.03.037 [DOI] [PubMed] [Google Scholar]
- Wang C., Jin H., Wang N., Fan S., Wang Y., Zhang Y., et al. (2016a). Gas6/Axl axis contributes to chemoresistance and metastasis in breast cancer through Akt/GSK-3β/β- catenin signaling. Theranostics 6, 1205–1219. 10.7150/thno.15083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Liu X., Li T., Liu C., Zhao Y. (2011). Increased hepatic Igf2 gene expression involves C/EBPβ in TCDD-induced teratogenesis in rats. Reprod. Toxicol. 32, 313–321. 10.1016/j.reprotox.2011.06.117 [DOI] [PubMed] [Google Scholar]
- Wang J., Nikhil K., Viccaro K., Chang L., White J., Shah K. (2017). Phosphorylation-dependent regulation of ALDH1A1 by Aurora kinase A: insights on their synergistic relationship in pancreatic cancer. BMC Biol. 15:10. 10.1186/s12915-016-0335-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Zhu Z., Huang Y., Wang P., Luo Y., Gao Y., et al. (2014). The subtype CD200-positive, chorionic mesenchymal stem cells from the placenta promote regeneration of human hepatocytes. Biotechnol. Lett. 36, 1335–1341. 10.1007/s10529-014-1468-7 [DOI] [PubMed] [Google Scholar]
- Wang L., Zhou X., Zhou T., Ma D., Chen S., Zhi X., et al. (2008). Ecto-5′-nucleotidase promotes invasion, migration and adhesion of human breast cancer cells. J. Cancer Res. Clin. Oncol. 134, 365–372. 10.1007/s00432-007-0292-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P., Xu J., Hou Z., Wang F., Song Y., Wang J., et al. (2016b). miRNA-34a promotes proliferation of human pulmonary artery smooth muscle cells by targeting PDGFRA. Cell Prolif. 49, 484–493. 10.1111/cpr.12265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Ao Y., Yang K., Tang H., Chen D. (2016c). Circadian clock gene Per2 plays an important role in cell proliferation, apoptosis and cell cycle progression in human oral squamous cell carcinoma. Oncol. Rep. 35, 3387–3394. 10.3892/or.2016.4724 [DOI] [PubMed] [Google Scholar]
- Wang X., Yang J., Qian J., Liu Z., Chen H., Cui Z. (2015). S100A14, a mediator of epithelial-mesenchymal transition, regulates proliferation, migration and invasion of human cervical cancer cells. Am. J. Cancer Res. 5, 1484–1495. [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Li K., Guo X., Li X., Bu Y., Bai X., et al. (2016d). The prognostic roles of ALDH1 isoenzymes in gastric cancer. Onco. Targets. Ther. 9, 3405–3414. 10.2147/OTT.S102314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler-Reya R., Scott M. P. (2001). The developmental biology of brain tumors. Annu. Rev. Neurosci. 24, 385–428. 10.1146/annurev.neuro.24.1.385 [DOI] [PubMed] [Google Scholar]
- Wechsler-Reya R. J., Scott M. P. (1999). Control of neuronal precursor proliferation in the cerebellum by Sonic Hedgehog. Neuron 22, 103–114. 10.1016/S0896-6273(00)80682-0 [DOI] [PubMed] [Google Scholar]
- Wen F., Curlango-Rivera G., Huskey D. A., Xiong Z., Hawes M. C. (2017). Visualization of extracellular DNA released during border cell separation from the root cap. Am. J. Bot. 104, 970–978. 10.3732/ajb.1700142 [DOI] [PubMed] [Google Scholar]
- Westcott J. M., Prechtl A. M., Maine E. A., Dang T. T., Esparza M. A., Sun H., et al. (2015). An epigenetically distinct breast cancer cell subpopulation promotes collective invasion. J. Clin. Invest. 125, 1927–1943. 10.1172/JCI77767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whetton A. D., Graham G. J. (1999). Homing and mobilization in the stem cell niche. Trends Cell Biol. 9, 233–238. 10.1016/S0962-8924(99)01559-7 [DOI] [PubMed] [Google Scholar]
- Whissell G., Montagni E., Martinelli P., Hernando-Momblona X., Sevillano M., Jung P., et al. (2014). The transcription factor GATA6 enables self-renewal of colon adenoma stem cells by repressing BMP gene expression. Nat. Cell Biol. 16, 695–707. 10.1038/ncb2992 [DOI] [PubMed] [Google Scholar]
- Wigner P., Czarny P., Galecki P., Su K. P., Sliwinski T. (2018). The molecular aspects of oxidative and nitrosative stress and the tryptophan catabolites pathway (TRYCATs) as potential causes of depression. Psychiatry Res. 262, 566–574. 10.1016/j.psychres.2017.09.045 [DOI] [PubMed] [Google Scholar]
- Wohlfahrt-Veje C., Audouze K., Brunak S., Antignac J. P., le Bizec B., Juul A., et al. (2014). Polychlorinated dibenzo-p-dioxins, furans, and biphenyls (PCDDs/PCDFs and PCBs) in breast milk and early childhood growth and IGF1. Reproduction 147, 391–399. 10.1530/REP-13-0422 [DOI] [PubMed] [Google Scholar]
- Wozniak M., Duś-Szachniewicz K., Ziółkowski P. (2015). Insulin-like growth factor-2 is induced following 5-aminolevulinic acid-mediated photodynamic therapy in SW620 human colon cancer cell line. Int. J. Mol. Sci. 16, 23615–23629. 10.3390/ijms161023615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu H.-H., Hwang-Verslues W. W., Lee W.-H., Huang C.-K., Wei P.-C., Chen C.-L., et al. (2015). Targeting IL-17B–IL-17RB signaling with an anti–IL-17RB antibody blocks pancreatic cancer metastasis by silencing multiple chemokines. J. Exp. Med. 212, 333–349. 10.1084/jem.20141702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Q.-F., Qian C., Zhao N., Dong Q., Li J., Wang B.-B., et al. (2017). Activation of transient receptor potential vanilloid 4 involves in hypoxia/reoxygenation injury in cardiomyocytes. Cell Death Dis. 8:e2828. 10.1038/cddis.2017.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao G., Cheng H., Cao H., Chen K., Tu Y., Yu S., et al. (2012). Critical role of filamin-binding LIM protein 1 (FBLP-1)/migfilin in regulation of bone remodeling. J. Biol. Chem. 287, 21450–21460. 10.1074/jbc.M111.331249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin H., Lu R., Lee H., Zhang W., Zhang C., Deng J., et al. (2013). G-protein-coupled receptor agonist BV8/prokineticin-2 and STAT3 protein form a feed-forward loop in both normal and malignant myeloid cells. J. Biol. Chem. 288, 13842–13849. 10.1074/jbc.M113.450049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing P., Li J. G., Jin F., Zhao T. T., Liu Q., Dong H. T., et al. (2011). Clinical and biological significance of hepsin overexpression in breast cancer. J. Investig. Med. 59, 803–810. 10.2310/JIM.0b013e31821451a1 [DOI] [PubMed] [Google Scholar]
- Xu C., Hu D. M., Zhu Q. (2013). eEF1A2 promotes cell migration, invasion and metastasis in pancreatic cancer by upregulating MMP-9 expression through Akt activation. Clin. Exp. Metastasis 30, 933–944. 10.1007/s10585-013-9593-6 [DOI] [PubMed] [Google Scholar]
- Xu L., Wang X., Wang J., Liu D., Wang Y., Huang Z., et al. (2016). Hypoxia-induced secretion of IL-10 from adipose-derived mesenchymal stem cell promotes growth and cancer stem cell properties of Burkitt lymphoma. Tumor Biol. 37, 7835–7842. 10.1007/s13277-015-4664-8 [DOI] [PubMed] [Google Scholar]
- Xu Y., Saegusa C., Schehr A., Grant S., Whitsett J. A., Ikegami M. (2009). C/EBPα is required for pulmonary cytoprotection during hyperoxia. Am. J. Physiol. Cell. Mol. Physiol. 297, L286–L298. 10.1152/ajplung.00094.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xuan X., Li S., Lou X., Zheng X., Li Y., Wang F., et al. (2015). Stat3 promotes invasion of esophageal squamous cell carcinoma through up-regulation of MMP2. Mol. Biol. Rep. 42, 907–915. 10.1007/s11033-014-3828-8 [DOI] [PubMed] [Google Scholar]
- Yang B., Wagner J., Damaschke N., Yao T., Wuerzberger-Davis S. M., Lee M. H., et al. (2014a). A novel pathway links oxidative stress to loss of insulin growth factor-2 (IGF2) imprinting through NF-κB activation. PLoS ONE 9:e88052. 10.1371/journal.pone.0088052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C.-S., Chang K.-Y., Rana T. M. (2014b). Genome-wide functional analysis reveals factors needed at the transition steps of induced reprogramming. Cell Rep. 8, 327–337. 10.1016/j.celrep.2014.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Ren Y., Yu X., Qian F., Bian B.-S., Xiao H. L., et al. (2014c). ALDH1A1 defines invasive cancer stem-like cells and predicts poor prognosis in patients with esophageal squamous cell carcinoma. Mod. Pathol. 27, 775–783. 10.1038/modpathol.2013.189 [DOI] [PubMed] [Google Scholar]
- Yang Q., Sun M., Ramchandran R., Raj J. U. (2015). IGF-1 signaling in neonatal hypoxia-induced pulmonary hypertension: role of epigenetic regulation. Vascul. Pharmacol. 73, 20–31. 10.1016/j.vph.2015.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Y., Long X., Zhang L., Chen J., Liu P., Li H., et al. (2014). NTS/NTR1 co-expression enhances epithelial-to-mesenchymal transition and promotes tumor metastasis by activating the Wnt/β-catenin signaling pathway in hepatocellular carcinoma. Oncotarget 7, 70303–70322. 10.18632/oncotarget.11854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yelloly J. (1809). A case of tumour in the brain, with remarks on the propagation of nervous influence. Med. Chir. Trans. 1, 183–223. 10.1177/095952870900100116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo C. D., Kim Y. A., Lee H. Y., Kim J. W., Kim S. J., Lee S. H., et al. (2017). Roflumilast treatment inhibits lung carcinogenesis in benzo(a)pyrene-induced murine lung cancer model. Eur. J. Pharmacol. 812, 189–195. 10.1016/j.ejphar.2017.07.004 [DOI] [PubMed] [Google Scholar]
- Yin H., Li C., Wang S., Guo Q., Ren X., Jiang G. (2015). Silencing of CD59 enhanced the sensitivity of HT29 cells to 5-Fluorouracil and Oxaliplatin. J. Infect. Chemother. 21, 8–15. 10.1016/j.jiac.2014.08.020 [DOI] [PubMed] [Google Scholar]
- Yin J., Fu W., Dai L., Jiang Z., Liao H., Chen W., et al. (2017). ANKRD22 promotes progression of non-small cell lung cancer through transcriptional up-regulation of E2F1. Sci. Rep. 7:4430. 10.1038/s41598-017-04818-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- You Q., Wu Y., Yao N., Shen G., Zhang Y., Xu L., et al. (2015). Interaction of AIM with insulin-like growth factor-binding protein-4. Int. J. Mol. Med. 36, 833–838. 10.3892/ijmm.2015.2262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng L., O'Connor C., Zhang J., Kaplan A. M., Cohen D. A. (2010). IL-10 promotes resistance to apoptosis and metastatic potential in lung tumor cell lines. Cytokine 49, 294–302. 10.1016/j.cyto.2009.11.015 [DOI] [PubMed] [Google Scholar]
- Zeng X., Hu Z., Wang Z., Tao J., Lu T., Yang C., et al. (2014). Upregulation of RASGRP3 expression in prostate cancer correlates with aggressive capabilities and predicts biochemical recurrence after radical prostatectomy. Prostate Cancer Prostatic Dis. 17, 119–125. 10.1038/pcan.2013.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhan L., Yang Y., Ma T.-T., Huang C., Meng X.-M., Zhang L., et al. (2015). Transient receptor potential vanilloid 4 inhibits rat HSC-T6 apoptosis through induction of autophagy. Mol. Cell. Biochem. 402, 9–22. 10.1007/s11010-014-2298-6 [DOI] [PubMed] [Google Scholar]
- Zhang J., Na S., Liu C., Pan S., Cai J., Qiu J. (2016a). MicroRNA-125b suppresses the epithelial–mesenchymal transition and cell invasion by targeting ITGA9 in melanoma. Tumor Biol. 37, 5941–5949. 10.1007/s13277-015-4409-8 [DOI] [PubMed] [Google Scholar]
- Zhang J., Wang X., Vikash V., Ye Q., Wu D., Liu Y., et al. (2016b). ROS and ROS-mediated cellular signaling. Oxid. Med. Cell. Longev. 2016, 1–18. 10.1155/2016/4350965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X.-H., Qian Y., Li Z., Zhang N.-N., Xie Y.-J. (2016c). Let-7g-5p inhibits epithelial-mesenchymal transition consistent with reduction of glioma stem cell phenotypes by targeting VSIG4 in glioblastoma. Oncol. Rep. 36, 2967–2975. 10.3892/or.2016.5098 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Kalderon D. (2001). Hedgehog acts as a somatic stem cell factor in the Drosophila ovary. Nature 410, 599–604. 10.1038/35069099 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Sui F., Ma J., Ren X., Guan H., Yang Q., et al. (2017). Positive feedback loops between NrCAM and major signaling pathways contribute to thyroid tumorigenesis. J. Clin. Endocrinol. Metab. 102, 613–624. 10.1210/jc.2016-1677 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Zhang Y., Geng L., Yi H., Huo W., Talmon G., et al. (2016d). Transforming growth factor β mediates drug resistance by regulating the expression of pyruvate dehydrogenase kinase 4 in colorectal cancer. J. Biol. Chem. 291, 17405–17416. 10.1074/jbc.M116.713735 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Zhao J., Zhang Y., Ithychanda S. S., Tu Y., Chen K., Qin J., et al. (2009). Migfilin interacts with Src and contributes to cell-matrix adhesion-mediated survival signaling. J. Biol. Chem. 284, 34308–34320. 10.1074/jbc.M109.045021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao L.-R., Du Y.-J., Chen L., Liu Z.-G., Jia X.-Y., Pan Y.-H., et al. (2015). Omentin-1 promotes the growth of neural stem cells via activation of Akt signaling. Mol. Med. Rep. 11, 1859–1864. 10.3892/mmr.2014.2937 [DOI] [PubMed] [Google Scholar]
- Zhao W., Prijic S., Urban B. C., Tisza M. J., Zuo Y., Li L., et al. (2016). Candidate antimetastasis drugs suppress the metastatic capacity of breast cancer cells by reducing membrane fluidity. Cancer Res. 76, 2037–2049. 10.1158/0008-5472.CAN-15-1970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z., Li J., Jiang Y., Xu W., Li X., Jing W. (2017). CLDN1 increases grug resistance of non-small cell lung cancer by activating autophagy via up-regulation of ULK1 phosphorylation. Med. Sci. Monit. 23, 2906–2916. 10.12659/MSM.904177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y., Yang J., Qian J., Qiu P., Hanabuchi S., Lu Y., et al. (2013). PSGL-1/selectin and ICAM-1/CD18 interactions are involved in macrophage-induced drug resistance in myeloma. Leukemia 27, 702–710. 10.1038/leu.2012.272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Yi L., Ouyang Q., Xu L., Cui H., Xu M. (2014). Neurotensin signaling regulates stem-like traits of glioblastoma stem cells through activation of IL-8/CXCR1/STAT3 pathway. Cell. Signal. 26, 2896–2902. 10.1016/j.cellsig.2014.08.027 [DOI] [PubMed] [Google Scholar]
- Zhou Y., Kipps T. J., Zhang S. (2017). Wnt5a signaling in normal and cancer stem cells. Stem Cells Int. 2017:5295286 10.1155/2017/5295286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X. L., Zeng Y. F., Guan J., Li Y. F., Deng Y. G., Bian X. W., et al. (2011). FMNL2 is a positive regulator of cell motility and metastasis in colorectal carcinoma. J. Pathol. 224, 377–388. 10.1002/path.2871 [DOI] [PubMed] [Google Scholar]
- Zinner B., Gyöngyösi B., Babarczi E., Kiss A., Sobel G. (2013). Claudin 1 expression characterizes human uterine cervical reserve cells. J. Histochem. Cytochem. 61, 880–888. 10.1369/0022155413501324 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.