Abstract
Background/Aims:
Behavioral nudges in the food environment increase healthy choices, but it is unknown if they improve diet and health. The ChooseWell 365 study will determine if an automated, personalized worksite intervention to nudge healthier choices improves overall diet and cardiometabolic health.
Design:
Randomized controlled trial of 602 hospital employees who regularly use on-site cafeterias and pay with an employee ID.
Intervention:
The intervention combines an environmental strategy (traffic-light labeling) with objective feedback and personalized nudges (health/lifestyle tips, social norms, incentives) to promote healthy food choices. The ChooseWell 365 software platform automatically generates personalized emails and letters that integrate employees’ weight goals with health, lifestyle, and cafeteria purchasing data. Over one year, the intervention group receives two weekly emails. One provides a log of daily purchases; the second provides personalized health/lifestyle tips. The intervention group receives monthly mailed letters with social norm comparisons and financial incentives for healthier purchases. The one-year intervention will be completed in February 2019; all follow-up will be completed March 2020.
Outcomes:
Weight, cardiometabolic risk factors, and dietary intake at one and two-year followup. Other outcomes include worksite food purchases by study participants and other non-participant employees who are socially connected (inferred from purchasing data) to participants.
Conclusions:
ChooseWell 365 tests a novel strategy to deliver a scalable worksite prevention program that is integrated into the workday. The intervention is personalized but automated and therefore does not require costlier individual counseling. In the future, this program could be applied broadly in other worksite settings.
Keywords: Obesity prevention, dietary intake, worksite, randomized controlled trial, food choice, dietary feedback, social norms, financial incentives, traffic-light labels, behavioral economics
Introduction
Scalable, low-cost interventions to prevent weight gain and improve nutrition are needed to help reverse the rising prevalence of obesity and chronic disease.1-3 In the United States, adults gain an average of 1-2 pounds per year,4,5 and annual obesity-related healthcare costs are estimated close to $200 billion.6 Preventing obesity will require changing physical, social, and cultural norms and environments to promote healthy lifestyles and prevent chronic weight gain.1-3
A worksite, with its established social networks, methods of communication, and shared environments, is ideal for implementing interventions to prevent obesity and improve diet.7,8 Most adults spend half their waking hours at work.9 Employees with obesity have higher costs due to healthcare utilization and lost productivity.10 Most worksite wellness programs are delivered as brief interventions that result in short-term changes in health or behavior, but the long-term health and cost benefits are unknown.11-14 Many programs that have focused on nutrition and physical activity require costly short-term individual or group counseling.11,15,16 To sustain long-term changes in lifestyle behaviors, wellness programs must be integrated into the workday and delivered over time at relatively low cost.
Targeting weight gain prevention and diet quality, rather than weight loss, is a strategy that may be more acceptable and effective among a diverse population of employees. Improving diet quality, independent of weight change, lowers risk of chronic disease.17 Research suggests that preventing weight gain using environmental or individually tailored strategies are promising in worksite, primary care, and community settings.18-21 A worksite healthy food environment positively influences employees’ attitudes toward eating a healthy diet.22-25 Food environment interventions designed using insights from psychology and behavioral economics address the tendency for employees to make unhealthy food choices without considering the long-term effects on health.26 Previous research has demonstrated that behavioral nudges, including traffic-light labels, product placement (choice architecture), and social norms with financial incentives, lead to healthier food choices in a worksite cafeteria.27-30 However, it is unknown if the positive effects of these interventions translate into improvements in overall dietary intake and health.
ChooseWell 365 is a randomized controlled trial of hospital employees that uses the worksite food environment as a platform to deliver a long-term, scalable health promotion program to prevent weight gain and improve dietary intake. The one-year intervention combines cafeteria behavioral strategies (traffic-light labels and choice architecture) with personalized nudges, including social norms, financial incentives, and personalized feedback about employees’ food purchases and health. The intervention is automated using software that integrated employees’ weight goals with their health measurements, medical history, lifestyle behaviors, and worksite food purchasing data. Weight, cardiometabolic risk factors, and dietary outcomes are assessed at the end of the one-year intervention and at two-year follow-up to determine effectiveness of the intervention for improving dietary intake, preventing weight gain, and reducing cardiometabolic risk. If successful, this intervention could be applied broadly in other worksite settings to promote healthy eating and prevent obesity.
Methods
Overview of study design and objectives
Hospital employees who regularly used the on-campus cafeterias were recruited and randomized to the intervention or control groups. Recruitment and baseline evaluation of all participants was completed in February 2018. The one-year intervention period will be completed for all participants by February 2019, and two-year follow up will be completed by March 2020. The three components of the intervention are: 1) automated, personalized nutrition and energy balance feedback based on the employee’s cafeteria food purchases, resting energy expenditure, and weight goal (loss vs. maintenance); 2) monthly social norm messaging about the healthfulness of an employee’s worksite food purchases compared to coworkers; and 3) individualized financial incentives to increase healthy worksite food choices. The project was conceptualized based on an integrated model of social action theory in which employees’ motivation and beliefs about healthy eating are addressed in the context of providing a healthy worksite food environment and personalized feedback for making healthier choices.31,32 The main objectives are to determine if employees in the intervention group improve dietary intake, gain less weight, and improve cardiometabolic health compared to the control group. An exploratory objective will determine if intervention-related changes in study participants’ healthy food choices spread through worksite social networks (identified using food purchasing data) to other employees who visited the cafeterias but did not participate in the trial.33 All outcomes are assessed at the end of the one-year intervention and at two-year follow up. The study was approved by the Partners Institutional Review Board on October 2, 2015.
Setting and worksite food environment
All participants are employees of Massachusetts General Hospital (MGH) in Boston, Massachusetts, a large teaching hospital with over 26,000 employees. The hospital has 7 food service locations (4 full-service cafeterias, 1 “grab and go” shop, and 2 coffee shops) on the main campus that are owned and operated by the hospital; all food service venues will hereafter be referred to as “cafeterias.” Hospital employees can opt to pay for cafeteria purchases with their employee ID cards using payroll deduction, thus providing the opportunity to track individuals’ purchases. Employees who use their ID cards to pay for cafeteria purchases have the same demographic characteristics as the overall hospital workforce.
The traffic-light labeling system was established in the main hospital cafeteria in 2010 and was implemented in the other cafeterias in 2015. The traffic-light system was designed based on United States Department of Agriculture dietary guidelines.34 Every item is labeled as red, yellow, or green based on an algorithm that factors in calories, saturated fat content, and nutrient density.27 A green rating connotes the highest level of healthfulness and a red item indicates the lowest level. “Choice architecture” changes were also implemented in the main cafeteria in 2010 to make the green-labeled foods and beverages more prominent and convenient for purchase.27 This included re-arranging beverage refrigerators, chip racks, and pre-made sandwiches to have the healthiest choices at eye level and placing baskets of bottled water near food stations. Similar choice architecture changes were implemented in the other 6 cafeterias in 2015. However, choice architecture changes were more limited in the smaller cafeterias because they have less available shelf and refrigerator space for changing the placement of healthy items. The traffic-light labeling and choice architecture interventions have been described previously in detail.27,29 Calories are not consistently listed on menu boards; however, the traffic-light system takes calories into account. Pre-made foods that are packaged by cafeteria staff (i.e. pre-made sandwiches) do have calories and other nutritional information listed on the package. Daily specials offered at all cafeterias also have calorie information and traffic-light ratings accessible to employees through the hospital’s intranet.
Participant recruitment
To be eligible, employees must have been between 20 and 75 years old, used their ID to make purchases in at least one of the cafeterias four or more times a week for at least 6 weeks out of a 12-week period, and been willing to pay for all ongoing cafeteria purchases with their ID cards. Eligible employees were identified with cafeteria purchasing data approximately every 12 weeks during the recruitment period. Exclusion criteria included: desire to gain weight, plans to leave employment in the next year (i.e. retirement, end of training), current pregnancy, history of eating disorder, weight loss surgery in the prior 6 months or in the upcoming year, being a member of MGH cafeteria staff, and participation in a weight-loss study.
Emails were sent to 100-200 randomly selected eligible employees each week asking if they were interested in participating. If the employee did not respond to the first email, a second email was sent over the following two weeks. Non-responsive employees were re-contacted between one and three months later. Employees were screened for eligibility over the phone, and if eligible, scheduled to complete informed consent in person. After completing informed consent, employees were asked to complete an on-line survey and schedule a baseline study visit at the hospital’s Clinical Research Center. Participants were not randomized until they had completed both the survey and visit because they provided important data that could be used for the personalized intervention.
Email access.
For purposes of confidentiality and convenience, all general study communication (i.e. reminders for completing surveys and visits) and intervention messages were delivered through work email. Although most participants accessed work email regularly during the day, some employees did not use a computer at work. Study staff provided instructions to all participants during the consent meeting about how to access the work email through the internet using a smartphone or personal computer.
Cafeteria discount.
As an incentive for participation, all randomized subjects received a 10% discount on cafeteria purchases over the two-year study. Only purchases paid with the employee’s ID badge were eligible for the discount.
Intervention and Attention Control
Intervention development
Prior to starting recruitment, cafeteria items were logged in a database and assigned calorie and associated traffic-light label information. These items were categorized by cafeteria location and item type (e.g. entrée, side, condiment, beverage) to create targeted messages based on employees’ purchasing habits. Using sales data reports, the most frequently sold items were identified and used to develop intervention email tips about cafeteria choices and healthy substitutions.
For most items sold by weight (e.g., frozen yogurt), caloric content was approximated by multiplying the weight by the calories per ounce. Although salad is sold by weight, the salad bar includes different items with varying caloric content, including leafy greens, beans, cheeses, grains, and dressings. Prior to recruitment, we conducted a pilot study to determine the average number of calories per ounce of salad. Study staff approached 127 employees purchasing a salad at lunch time right after paying. These employees completed a brief survey, and the study staff recorded the approximate quantities of each salad item and weighed the salad with a portable scale. The average calories per ounce of salad was determined for men and women and for different age categories. All subgroups had similar mean calories per ounce (35.8 calories per ounce), and therefore this is utilized to calculate salad calories in the trial.
Data Collection
Surveys.
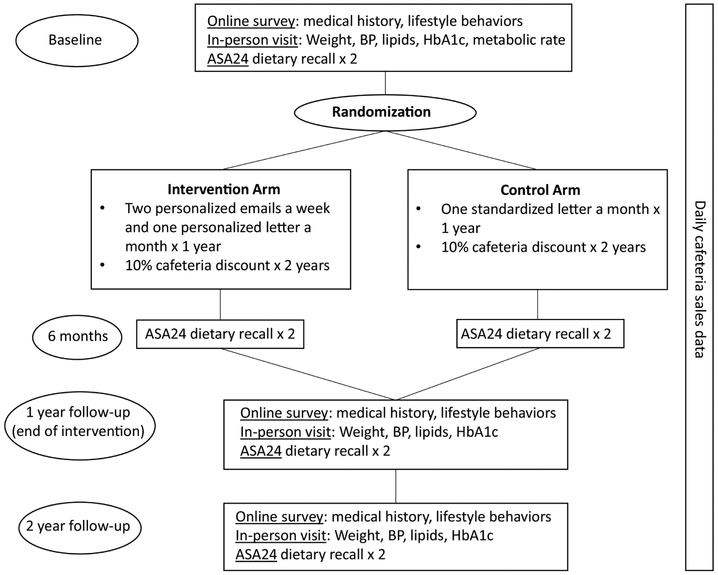
All participants completed a baseline survey electronically to provide demographics, medical history, medications, family history of cardiovascular disease or diabetes, smoking history, eating and activity behaviors, sleep patterns, and weight history. The same survey is repeated at 1 year and 2 years. (Figure 4)
Figure 4.
ChooseWell 365 study schema.
Study visits.
Study visits occurred at baseline and will take place at one and two-year follow-up. (Figure 4) Participants fast for 8 hours prior to the visit. Each visit includes measurement of the participant’s weight, height, waist circumference, blood pressure, lipid panel, glucose, and HbA1c. Physical activity was assessed at baseline and will be repeated at follow-up visits with the International Physical Activity Questionnaire.35 At the baseline visit only, resting energy expenditure was measured using the VMAX Encore 29 metabolic cart (Viasys Healthcare, Carefusion, San Diego, CA).36
Automated Self-Administered 24-hour (ASA24) dietary recalls.
Each participant completes two ASA24 dietary recalls on non-consecutive days at each of 4 time points: baseline, 6 months, 1 year, and 2-year follow up. (Figure 4) The ASA24 is a freely-available web-based software tool that is modeled on an interviewer-administered method developed by the United States Department of Agriculture (USDA) and uses multi-level food probes to accurately assess food types and amounts.37 The ASA24 can be administered to large group of individuals and is a valid measure of overall mean intake of nutrients and summary diet measures in an adult population.38,39 Results of the ASA24 recalls will be used to calculate the Health Eating Index-2015 (HEI), a tool to measure compliance with the key, diet-related recommendations of the USDA Guidelines for Americans.40,41 To estimate HEI scores, the two 24-hour dietary recalls from each time point will be combined.42 Participants were compensated $100 after completing the study visit, survey, and two ASA24 dietary recalls at baseline and will be compensated $100 at each follow-up visit (one year and two years) and receive $25 after completing the two ASA24 recalls at 6 months.
Cafeteria purchases.
All items purchased by study participants are tracked in the cafeteria data systems. Purchasing data includes calorie information, the assigned traffic light label, and the time and location of the purchase. Baseline purchasing data on all participants was collected retrospectively for the year prior to their enrollment in the study.
Intervention
Laboratory result letters:
After completion of the baseline visit, participants received a result letter by email that included their “daily calorie budget” which was calculated using the resting energy expenditure, estimated activity level, and self-reported desire to either lose or maintain their weight in the next year. The daily calorie goal for participants who wanted to lose weight were calculated to be 500 calories lower than the daily calorie goal to maintain their weight, although no subject was given a goal of less than 1200 calories per day. The letter also included fasting glucose, lipid profile, and hemoglobin A1C results. A similar letter is mailed to employees after the one and two-year follow-up visits.
Automated, personalized messages:
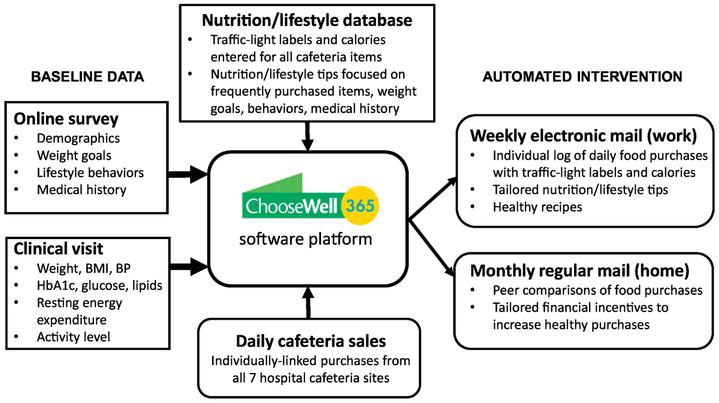
Figure 1 shows the flow of individual data used to create automated, personalized messages during the one-year intervention. Participants in the intervention group receive two weekly emails and monthly letters over one year.
Figure 1.
Flow of study information through the ChooseWell 365 software platform.
Weekly emails:
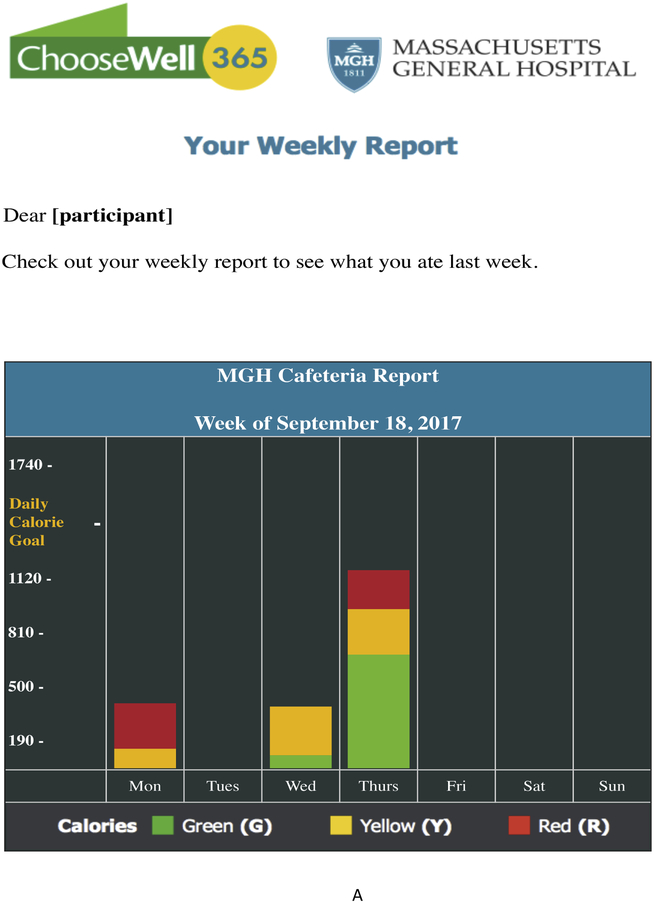
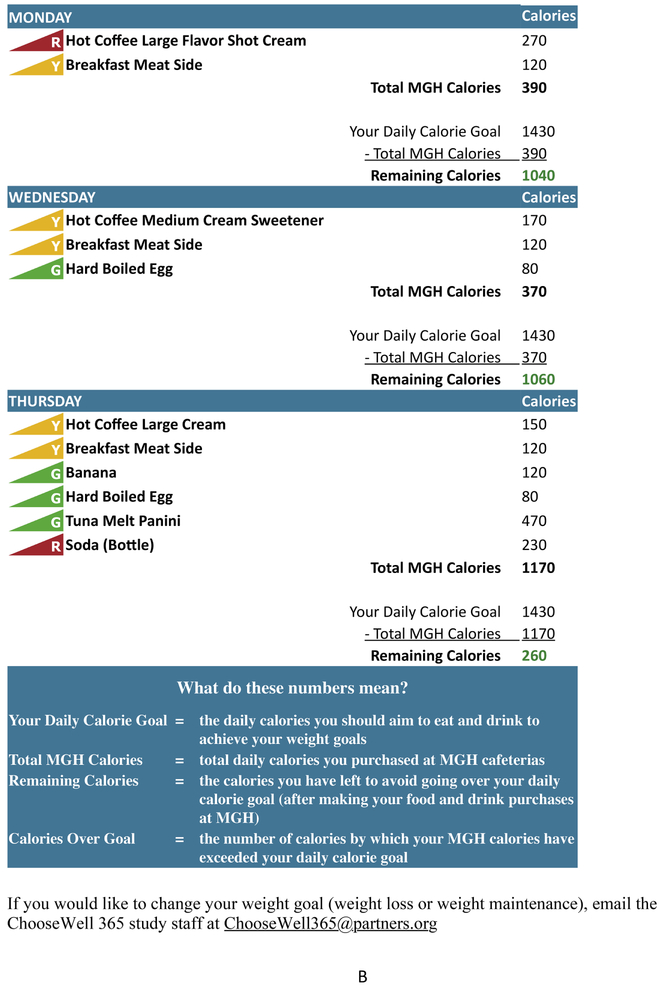
The first email (“Your ChooseWell 365 Weekly Report “) provides a log of all cafeteria items purchased during the week, including the color-label and the caloric content. (Figure 2) At the top of the email is a summary graphic that showed the total calories purchased each day, the proportion of purchased calories that were from foods labeled green, yellow, or red, and the daily calorie goal. Under the graphic, daily purchases are listed with individual item calories, total calories purchased for the day, and the “remaining calories” (daily calorie goal – total purchased calories) for each day. The rationale for providing detailed information about calories purchased with the daily calorie goal is to provide participants with a benchmark to guide their food choices both at work and outside of work.
Figure 2.
ChooseWell 365 intervention email: Weekly Report.
The second email of the week (“Your ChooseWell 365 Weekly Tips”) includes two personalized tips about healthy eating, physical activity, and/or disease prevention. (Supplemental Figure) Prior to recruitment, the study dietitian and physician created a database of over 350 nutrition and lifestyle tips for use in the intervention. The message database was developed based on predetermined domains that the intervention was targeting: weight and energy balance, disease risk (personal and family history of cardiometabolic diseases and risk factors); worksite food purchases (e.g., pizza, salads, sugar-sweetened beverages); home food choices and behaviors (e.g. meal preparation, eating out); barriers to healthy lifestyle (e.g. caring for children, lack of time); and physical activity (e.g. taking stairs, exercise habits). Each participant receives different personalized messages depending on their weekly cafeteria purchases and information collected from the baseline health measurements and survey responses. The tips are automatically compiled and sent through a software platform that integrates cafeteria sales, baseline survey, and visit data. (Figure 1)The algorithm ensures an individual will not receive the same tip within a 15-week period.
Monthly letters:
Monthly letters mailed home provide peer-comparisons of healthy cafeteria purchases plus financial incentives to increase purchases of green-labeled (healthy) cafeteria purchases in the following month. (Figure 3) In a previous study, we demonstrated that this strategy increased the proportion of green-labeled purchases by 2.2 percentage points (p=0.03) over three months.30 Each participant’s letter includes a bar graph demonstrating the proportion of red, yellow, and green items that the employee purchased in the prior month, comparing the employee’s purchases to “all MGH employees” and to the “healthiest MGH employees” (top 10%). The letter also includes a “green goal” to achieve in the following month to earn a financial incentive. A reward could be earned for passing each of three thresholds: 40%, 60%, or 80% green purchases in a month. For example, the October letter would have a “green goal” for the month of October, and the subsequent November letter would include a reward of $20 for each threshold passed during October. The November letter would also include a new goal based on the last threshold crossed. The incentive structure was designed so that employees with the least healthy purchasing patterns at baseline (<40% green) could earn the highest amount of money during the study. Employees who purchase green items at or above the highest threshold (80%) have maintenance of that level as their goal and earn $5 per month to stay at or above 80% green. An employee who starts below the lowest threshold of 40% green could earn a maximum of $115 over the one-year study period ($20 × 3, achieved for passing each threshold in a single month, and $5 × 11 months for remaining at or above the final threshold). The maximum amount that a consistent “healthy eater” could earn during the study is $60 ($5 per month × 12). If an employee earns a $20 reward in one month but does not achieve the new goal in the following month, the employee will earn $5 for staying at or above the most recently crossed threshold. However, employees earn no new reward if they regress and pass the same threshold a second time.
Figure 3.
ChooseWell 365 intervention monthly letter: Social norms and financial incentive.
Attention Control
Laboratory result letters:
Control group participants received a letter by email after the baseline visit that included only the fasting glucose, lipid profile, and hemoglobin A1C results.
Monthly letters:
The control group does not receive any personalized emails. All control group participants receive the same monthly letters for one year that include standardized healthy lifestyle information, such as the benefits of eating fruits and vegetables and exercising regularly.
Maintenance of nutrition information
Although the traffic-light labeling system has been in place since 2010, new menu items are added frequently and need calorie and traffic-light labels assigned. Each week, prior to sending emails to participants assigned to the intervention, the software program generates a list of all new items with missing nutrition information purchased by study participants to ensure they do not receive reports with missing nutrition data. The study dietician reviews this list at the beginning of the week to update the missing information before the emails are sent and regularly follow up with food service managers to ensure accuracy with item labeling in the cash register database and at the point of sale.
Employee social connections (social network)
Food purchases of employees who used their ID card for cafeteria purchases (>7000 employees) during the study period but who did not participate in the study will included in the social network analysis anonymously using the cafeteria transaction data. Social ties between study participants and non-participants who use the cafeterias (e.g., employees who go to the cafeteria together to get lunch) will be inferred based on a validated algorithm previously developed by the study investigators which uses demographics and time/location of cafeteria purchases by both the study participants and the larger population of employee cafeteria customers.33 Using this validated algorithm, two employees will be considered to be socially connected if the cafeteria database indicates they made purchases at the same cafeteria within a 120 second time window of each other on more than one occasion over 8 weeks. The algorithm then weights ties between employees to a greater or lesser extent based on the number of times a pair of employees are observed to have made purchases at the same time and cafeteria location, the number of different cafeterias at which they were “observed” together, as well as similarity in certain demographic and job characteristics.
Statistical considerations
We consented 656 hospital employees, of whom 602 were randomized between September 2016 and February 2018. Employees who provided consent but were not randomized were older and more likely to be male, but they did not differ from the randomized employees in race, ethnicity, or job type. Participants who completed the baseline visit and survey were randomly assigned to the intervention or control group using a computer-generated block randomization scheme with block sizes of 6. Randomization was stratified by the participant’s response to the survey question asking if they wanted to lose weight or maintain their current weight in the next year. We planned to enroll a total of 600 subjects, and allowing for a 10% attrition rate, the final sample size for analysis is expected to be 540, or approximately 270 per group.
We used data from our prior worksite exercise and nutrition studies to estimate standard deviations for change in weight and cardiometabolic risk factors.43,44 We estimated the standard deviation in weight change at one year to be approximately 2.3 kilograms. With 270 subjects per arm, the study will have 93% power to detect a mean difference as small as 0.7 kilograms between the two study arms with a two-sided significance level of 0.05. Assuming standard deviation for total cholesterol change in one year is 30 mg/dL, the study will have 90% power to detect a mean difference of 8.4 mg/dL. Assuming standard deviation for blood pressure change in one year is 10 mmHg, the study will have 90% power to detect a mean difference of 2.8 mmHg. Assuming standard deviation for HbA1C change in one year is 1.0%, the study will have 90% power to detect a mean difference of 0.28%. A prior study demonstrated a reduced risk of chronic disease with increasing quintiles of HEI scores, and an increase of 5 points in HEI score was sufficient to move a subject into a higher quintile.45 Therefore, we consider a 5-point difference to be a meaningful dietary change. Assuming the standard deviation for change in HEI score is 15, the study will have 97% power to detect a mean difference of 5 between the two study arms with 270 subjects in each arm. Although subjects and study coordinators could not be blinded to assignment, all staff conducting baseline, one, and two-year follow-up visits are blinded to intervention assignment.
The primary outcome is change in weight at the end of one year, and other outcomes include weight change at two years and change in cardiometabolic risk factors (blood pressure, lipids, hemoglobin A1c), cafeteria food purchases, and Healthy Eating Index score at one and two-year follow-up. In an exploratory analysis, we will use cafeteria sales data to identify a network of co-workers connected to study participants and determine whether healthy food purchases among non-study participants over the one-year intervention period are positively correlated with the extent to which they are connected to study participants assigned to the intervention group.
Primary analyses will be performed on an intent-to-treat basis that includes all participants who remained employed at the hospital during the one-year intervention. Leaving employment was expected to occur at random in both groups and to be unrelated to the study outcomes. Study participants who remain employed but do not follow up for assessment visits will be included in final analyses. We will impute missing data, including participants’ weights at one-year follow-up (primary outcome) using multiple imputation and employing all available outcomes assessments and covariates. We will conduct several sensitivity analyses. We will estimate the treatment effect when we include the participants who leave employment, and we will also use alternative strategies to account for missing data, such as complete case analysis and last observation carried forward.46 Analyses of secondary outcomes, including weight at two years, will be analyzed in a similar manner.
Discussion
ChooseWell 365 tests a novel worksite intervention that utilizes employees’ food purchases and individual health and behavioral information to provide automated, personalized feedback about food choices, energy balance goals, and health with the primary goal of preventing weight gain and improving diet quality. A total of 602 employees from a large hospital worksite have been enrolled. This is the first randomized controlled trial to test whether personalized feedback about food purchases and health prevents weight gain in a large population of employees. The personalized intervention is automated, using a software platform, and does not include costlier in-person nutrition counseling and education.16 The study has several strengths that will contribute to future knowledge about population-level strategies to prevent obesity, improve dietary intake, and reduce cardiometabolic risk.
The ChooseWell 365 intervention combines personalized behavioral nudges with tailored feedback about employees’ food choices and health. It was conceptualized based on prior studies demonstrating that traffic light labels, choice architecture, and social norms combined with small financial incentives increased healthy food purchases in an employee population.27,29,30 However, the impact of healthier worksite food purchases on health outcomes, such as weight, lipids, and hemoglobin A1C, and overall dietary intake is unknown.
This relatively low-touch and scalable intervention was designed to improve health outcomes by increasing employees’ awareness of their food choices, the association between diet and health, and the impact that small changes in lifestyle may have on weight and cardiometabolic risk factors, such as blood pressure, cholesterol, and blood sugar. At baseline, participants chose a weight goal (loss or maintenance) for the next year. The intervention’s messaging and daily calorie goals are individualized to support the participant’s goal.
The ChooseWell 365 personalized feedback is automated using software that integrates individual data from online surveys, in-person visits, and daily cafeteria purchases. Tracking individuals’ purchases has become a significant component of the modern economy, demonstrating the strong potential for disseminating our findings. While most prior tailored dietary interventions have relied on subjects’ self-reported intake,47,48 the ChooseWell 365 intervention provides dietary feedback based on the employees’ actual food purchases. Employees receive email messages while at work and are therefore able to act on the information by making alterations in worksite food purchases and activities (e.g. taking the stairs) as well as adjusting their calorie consumption and activities outside of work. Monthly letters provide peer comparisons and financial incentives that “nudge” employees to increase their healthy cafeteria choices at work.
A novel objective of this study is to explore the impact of this intervention on the food choices of participants’ worksite social networks to determine if the effect of the intervention spreads among already-existing social connections between co-workers. While some research suggests that unhealthy behaviors spread in a social network,49-51 less is known about whether healthy behaviors and health promotion efforts proliferate in a network.52,53 This will be one of the first studies to determine if the positive effects of a nutrition-based intervention disseminate through socially connected co-workers.
The study aims to prevent disease, and it has power to detect small differences in weight, cholesterol, blood pressure, HbA1c, and dietary intake between the intervention and control groups at the end of the intervention (one year). Two-year follow-up visits will take place to assess whether the effects of the intervention are sustained during the year after it ends. A previous meta-analysis showed that medical costs fell $3.27 for every US dollar spent on workplace wellness programs, but the heterogeneity of programs limited the ability of the meta-analysis to determine which attributes of the program (e.g., nutrition, weight loss) were most important for lowering costs.15 A limitation of interventions that aim to prevent weight gain and cardiometabolic risk factors is that changes in health care use may not take place during the first one to two years; recent worksite wellness studies indicate that at least three years are needed to see a reduction in health care costs.54-56 A unique aspect of the ChooseWell 365 study is the ability to examine the “spillover” effect of the intervention on the healthfulness of cafeteria purchases by employees who are not participating in the intervention. If benefits accrue in those who do not participate in the study but are socially connected to study participants, the cost-effectiveness of the program would increase.
The worksite food environment provides an opportunity to deliver long-term, scalable health promotion programs for prevention of obesity and chronic diseases. ChooseWell 365 aims to prevent employees’ weight gain and improve dietary intake by integrating the intervention into the workday, thus lowering barriers for participation including time and financial burden. In the future, other large employers and institutions could implement a similar program that could be delivered to large populations of employees to prevent weight gain and cardiometabolic disease.
Supplementary Material
Supplemental Figure 1. ChooseWell 365 intervention email: Weekly Tips.
Acknowledgements
We would like to thank the cafeteria staff from the Massachusetts General Hospital Department of Nutrition and Food Services for their effort and dedication to the successful implementation of ChooseWell 365. We would also like to thank the study participants for their time and commitment to the study.
Funding:
ChooseWell 365 is funded by the NIH R01 grants: HL125486 and DK114735. The project was also supported by NIH Grant Number 1UL1TR001102. The NIH had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Trial registration: Clincaltrials.gov Identifier: NCT02660086
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Swinburn B, Egger G. Preventive strategies against weight gain and obesity. Obes Rev. 2002;3(4):289–301. [DOI] [PubMed] [Google Scholar]
- 2.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: Shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. [DOI] [PubMed] [Google Scholar]
- 3.Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of obesity: Science, policy, and action. Lancet. 2011;378(9793):838–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis CE, Jacobs DR,J, McCreath H, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. coronary artery risk development in young adults. Am J Epidemiol. 2000;151(12):1172–1181. [DOI] [PubMed] [Google Scholar]
- 5.Dutton GR, Kim Y, Jacobs DR,J, et al. 25-year weight gain in a racially balanced sample of U.S. adults: The CARDIA study. Obesity (Silver Spring). 2016;24(9):1962–1968. doi: 10.1002/oby.21573 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cawley J, Meyerhoefer C. The medical care costs of obesity: An instrumental variables approach. J Health Econ. 2012;31(1):219–230. doi: 10.1016/j.jhealeco.2011.10.003 [doi]. [DOI] [PubMed] [Google Scholar]
- 7.Anderko L, Roffenbender JS, Goetzel RZ, et al. Promoting prevention through the Affordable Care Act: Workplace wellness. Prev Chronic Dis. 2012;9:E175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carnethon M, Whitsel LP, Franklin BA, et al. Worksite wellness programs for cardiovascular disease prevention: A policy statement from the American Heart Association. Circulation. 2009;120(17):1725–1741. doi: 10.1161/CIRCULATIONAHA.109.192653 [doi]. [DOI] [PubMed] [Google Scholar]
- 9.Bureau of Labor and Statistics. Economic news release: American time use survey - 2016 results. www.bls.gov.doc:5ad8efa6e4b07da0d1231b99. Accessed May 1, 2018.
- 10.Van Nuys K, Globe D, Ng-Mak D, Cheung H, Sullivan J, Goldman D. The association between employee obesity and employer costs: Evidence from a panel of U.S. employers. Am J Health Promot. 2014;28(5):277–285. doi: 10.4278/ajhp.120905-QUAN-428 [doi]. [DOI] [PubMed] [Google Scholar]
- 11.Anderson LM, Quinn TA, Glanz K, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. Am J Prev Med. 2009;37(4):340–357. [DOI] [PubMed] [Google Scholar]
- 12.Engbers LH, van Poppel MN, Chin A Paw MJ, van Mechelen W. Worksite health promotion programs with environmental changes: A systematic review. Am J Prev Med. 2005;29(1):61–70. [DOI] [PubMed] [Google Scholar]
- 13.Pelletier KR. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: Update VII 2004-2008. J Occup Environ Med. 2009;51(7):822–837. [DOI] [PubMed] [Google Scholar]
- 14.Thorndike AN. Workplace interventions to reduce obesity and cardiometabolic risk. Curr Cardiovasc Risk Rep. 2011;5:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baicker K, Cutler D, Song Z. Workplace wellness programs can generate savings. Health affairs. 2010;29(2):1–8. [DOI] [PubMed] [Google Scholar]
- 16.Fitzgerald S, Kirby A, Murphy A, Geaney F, Perry IJ. A cost-analysis of complex workplace nutrition education and environmental dietary modification interventions. BMC Public Health. 2017;17(1):7. doi: 10.1186/s12889-016-3988-7 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sotos-Prieto M, Bhupathiraju SN, Mattei J, et al. Association of changes in diet quality with total and cause-specific mortality. N Engl J Med. 2017;377(2):143–153. doi: 10.1056/NEJMoa1613502 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lemon SC, Wang ML, Wedick NM, et al. Weight gain prevention in the school worksite setting: Results of a multi-level cluster randomized trial. Prev Med. 2014;60:41–47. doi: 10.1016/j.ypmed.2013.12.010 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bennett GG, Foley P, Levine E, et al. Behavioral treatment for weight gain prevention among black women in primary care practice: A randomized clinical trial. JAMA Intern Med. 2013;173(19):1770–1777. doi: 10.1001/jamainternmed.2013.9263 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolfenden L, Wyse R, Nichols M, Allender S, Millar L, McElduff P. A systematic review and meta-analysis of whole of community interventions to prevent excessive population weight gain. Prev Med. 2014;62:193–200. doi: 10.1016/j.ypmed.2014.01.031 [doi]. [DOI] [PubMed] [Google Scholar]
- 21.Beauchamp A, Backholer K, Magliano D, Peeters A. The effect of obesity prevention interventions according to socioeconomic position: A systematic review. Obes Rev. 2014;15(7):541–554. doi: 10.1111/obr.12161 [doi]. [DOI] [PubMed] [Google Scholar]
- 22.Engbers LH, van Poppel MN, Chin AP, van Mechelen W. The effects of a controlled worksite environmental intervention on determinants of dietary behavior and self-reported fruit, vegetable and fat intake. BMC Public Health. 2006;6:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raulio S, Roos E, Prattala R. School and workplace meals promote healthy food habits. Public Health Nutr. 2010;13(6):987–992. [DOI] [PubMed] [Google Scholar]
- 24.Lowe MR, Tappe KA, Butryn ML, et al. An intervention study targeting energy and nutrient intake in worksite cafeterias. Eat behav. 2010;11(3):144–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sonnenberg L, Gelsomin E, Levy DE, Riis J, Barraclough S, Thorndike AN. A traffic light food labeling intervention increases consumer awareness of health and healthy choices at the point-of-purchase. Preventive medicine. 2013;57:253–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roberto CA, Kawachi I, eds. Behavioral economics and public health. New York, New York: Oxford University Press; 2016. [Google Scholar]
- 27.Thorndike AN, Sonnenberg L, Riis J, Barraclough S, Levy DE. A 2-phase labeling and choice architecture intervention to improve healthy food and beverage choices. Am J Public Health. 2012;102(3):527–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levy DE, Riis J, Sonnenberg LM, Barraclough SJ, Thorndike AN. Food choices of minority and low-income employees: A cafeteria intervention. Am J Prev Med. 2012;43(3):240–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thorndike AN, Riis J, Sonnenberg LM, Levy DE. Traffic-light labels and choice architecture: Promoting healthy food choices. Am J Prev Med. 2014;46:143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thorndike AN, Riis J, Levy DE. Social norms and financial incentives to promote employees' healthy food choices: A randomized controlled trial. Prev Med. 2016;86:12–18. doi: 10.1016/j.ypmed.2016.01.017 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ewart CK. Social action theory for a public health psychology. Am Psychol. 1991;46(9):931–946. [DOI] [PubMed] [Google Scholar]
- 32.Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Communication Theory. 2003;13(2):164–183. [Google Scholar]
- 33.Levy D, Pachucki M, O'Malley J, Porneala B, Yaqubi A, Thorndike A. Abstract P314: Healthy food choices are correlated in a large employee social network. Circulation. 2018;137(Suppl 1):AP314 http://circ.ahajournals.org/content/137/Suppl_1/AP314.abstract. [Google Scholar]
- 34.U.S. Department of Agriculture and U.S Department of Health and Human Services, ed. Dietary Guidelines for Americans, 2010. 7th edition ed. Washington D.C.: U.S. Government Printing Office; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. [DOI] [PubMed] [Google Scholar]
- 36.Compher C, Frankenfield D, Keim N, Roth-Yousey L, Evidence Analysis WG. Best practice methods to apply to measurement of resting metabolic rate in adults: A systematic review. J Am Diet Assoc. 2006;106(6):881–903. doi: S0002-8223(06)00146-5 [pii]. [DOI] [PubMed] [Google Scholar]
- 37.National Cancer Institute. ASA24 automated self-administered 24 hour dietary assessment tool. Division of Cancer Control and Population Sciences, Epidemiology and Genomics Research Program: https://epi.grants.cancer.gov/asa24/. Accessed June 1, 2018.
- 38.Frankenfeld CL, Poudrier JK, Waters NM, Gillevet PM, Xu Y. Dietary intake measured from a self-administered, online 24-hour recall system compared with 4-day diet records in an adult US population. J Acad Nutr Diet. 2012;112(10):1642–1647. [DOI] [PubMed] [Google Scholar]
- 39.Subar AF, Kirkpatrick SI, Mittl B, et al. The automated self-administered 24-hour dietary recall (ASA24): A resource for researchers, clinicians, and educators from the National Cancer Institute. J Acad Nutr Diet. 2012;112(8):1134–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the healthy eating index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. doi: S2212-2672(18)30838-4 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reedy J, Lerman JL, Krebs-Smith SM, et al. Evaluation of the healthy eating index-2015. J Acad Nutr Diet. 2018;118(9):1622–1633. doi: S2212-2672(18)30836-0 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Freedman LS, Guenther PM, Krebs-Smith S, Dodd KW, Midthune D. A population's distribution of healthy eating index-2005 component scores can be estimated when more than one 24-hour recall is available. J Nutr. 2010;140(8):1529–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thorndike AN, Healey E, Sonnenberg L, Regan S. Participation and cardiovascular risk reduction in a voluntary worksite nutrition and physical activity program. Preventive medicine. 2011;52:164–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thorndike AN, Sonnenberg L, Healey E, Myint-U K, Kvedar JC, Regan S. Prevention of weight gain following a worksite nutrition and exercise program: A randomized controlled trial. Am J Prev Med. 2012;43(1):27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6):1009–1018. doi: 10.3945/jn.111.157222 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Batterham MJ, Tapsell LC, Charlton KE. Analyzing weight loss intervention studies with missing data: Which methods should be used? Nutrition. 2013;29(7-8):1024–1029. doi: 10.1016/j.nut.2013.01.017 [doi]. [DOI] [PubMed] [Google Scholar]
- 47.Broekhuizen K, Kroeze W, van Poppel MN, Oenema A, Brug J. A systematic review of randomized controlled trials on the effectiveness of computer-tailored physical activity and dietary behavior promotion programs: An update. Ann Behav Med. 2012;44(2):259–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Teasdale N, Elhussein A, Butcher F, et al. Systematic review and meta-analysis of remotely delivered interventions using self-monitoring or tailored feedback to change dietary behavior. Am J Clin Nutr. 2018;107(2):247–256. doi: 10.1093/ajcn/nqx048 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. [DOI] [PubMed] [Google Scholar]
- 50.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pachucki MA, Jacques PF, Christakis NA. Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011;101(11):2170–2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aral S, Nicolaides C. Exercise contagion in a global social network. Nat Commun. 2017;8:14753. doi: 10.1038/ncomms14753 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang J, Brackbill D, Yang S, Becker J, Herbert N, Centola D. Support or competition? how online social networks increase physical activity: A randomized controlled trial. Prev Med Rep. 2016;4:453–458. doi: 10.1016/j.pmedr.2016.08.008 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Naydeck BL, Pearson JA, Ozminkowski RJ, Day BT, Goetzel RZ. The impact of the Highmark employee wellness programs on 4-year healthcare costs. J Occup Environ Med. 2008;50(2):146–156. doi: 10.1097/JOM.0b013e3181617855 [doi]. [DOI] [PubMed] [Google Scholar]
- 55.Henke RM, Goetzel RZ, McHugh J, Isaac F. Recent experience in health promotion at Johnson & Johnson: Lower health spending, strong return on investment. Health Aff (Millwood). 2011;30(3):490–499. doi: 10.1377/hlthaff.2010.0806 [doi]. [DOI] [PubMed] [Google Scholar]
- 56.Jones D, Molitor D, Reif J. What do workplace wellness programs do? Evidence from the Illinois workplace wellness study. National Bureau of Economic Research Working Paper Series. 2018; No. 24229. http://www.nber.org/papers/w24229.pdf. doi: 10.3386/w24229. Accessed October 18, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. ChooseWell 365 intervention email: Weekly Tips.