Abstract
Aims
Impaired illness awareness or not accepting that one has obesity is an understudied phenomenon that may negatively influence treatment adherence and clinical outcomes. The purpose of this study was to perform a systematic review of available measures of obesity awareness, and subsequently develop and validate a novel scale that measures the core domains of obesity awareness.
Methods
A systematic review of the literature revealed no illness specific measure of subjective obesity awareness. As such, we designed the Obesity Awareness and Insight Scale (OASIS) to assess the following core domains of illness awareness: General Illness Awareness,, Symptom Attribution,, Awareness of Need for Treatment and the Negative Consequences attributable to the illness (www.illnessawarenessscales.com). Participants (n=100) were recruited from an online survey platform to assess the psychometric properties of OASIS.
Results
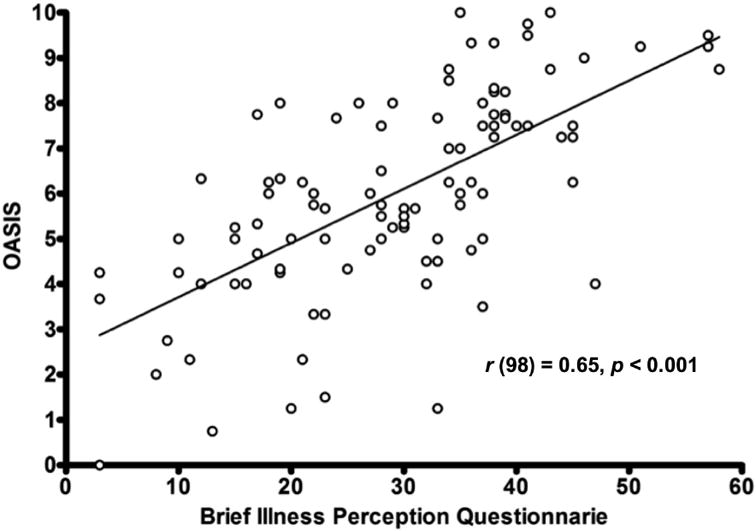
The OASIS demonstrated strong internal consistency (Cronbach's alpha=0.89), convergent (r(98)=0.65, p<0.001) and discriminant validity, and test-retest reliability (intra-class correlation=0.76). An exploratory factor analysis of OASIS revealed a single latent component.
Conclusions
OASIS is an obesity-specific instrument that comprehensively measures subjective obesity awareness. OASIS can be used in epidemiological studies, intervention trials and clinical practice to assess the impact of obesity awareness on treatment adherence and outcomes.
Keywords: Illness awareness, illness denial, insight into illness, obesity, obese
Introduction
Impaired illness awareness or not accepting that one is overweight or has obesity is considered a barrier to healthy lifestyle modifications(1) and a contributor to negative clinical outcomes.(1-3) Yet, despite its presumed role in disease management, impaired obesity awareness is a poorly characterized phenomenon that may represent a meaningful target for intervention to facilitate weight reduction, reduce obesity-related morbidity and mortality, and improve the quality of life of patients and their families.(4-6)
There is a remarkable discrepancy between self-awareness of body weight and actual body weight among obese adults. Despite efforts in recent years to raise the profile of obesity as a public health problem, there has been a decrease in the proportion of obese adults who recognize that they are overweight/obese.(5, 7-10) In one nationwide survey in the United States, although participants self-reported weight loss, there was a net weight gain during the 1-year follow-up period.(10) Similarly, a study in Great Britain comparing cross-sectional surveys from 2007 and 2012 revealed that self-awareness of being significantly overweight declined over this time period.(5) While impaired obesity awareness may represent a major barrier to making lifestyle modifications,(5, 6, 10) accurate weight perception is positively associated with pursuit of weight control.(1)
Although empirical investigations to date suggest that subjective obesity awareness is clinically relevant, it remains a poorly articulated construct. In this work, the term illness awareness refers to one's subjective awareness of having an illness and not one's knowledge of the illness. In other words, subjective illness awareness refers to the individual's acceptance of having obesity, the associated symptoms, negative health consequences, and need for lifestyle modifications independent of one's degree of knowledge about obesity.
Subjective illness awareness has been most rigorously studied in psychotic disorders, particularly schizophrenia where impaired illness awareness and the denial of need for treatment are common features of the disorder.(11, 12) Illness awareness is currently understood as a multidimensional construct that exists on a continuum,(12) incorporating 4 principal domains: (i) General Illness Awareness (e.g., “I am overweight”), (ii) accurate Symptom Attribution to the illness (e.g., “I regularly have back pain due to my weight”), (iii) Awareness of Need for Treatment (e.g., “I would benefit from eating healthy”), and (iv) Awareness of Negative Consequences (e.g., “If I don't lose weight, I may develop diabetes”).(11, 13, 14) This understanding provides a model to assess illness awareness in other medical conditions, such as obesity. For example, an individual who accepts having obesity may, at the same time, deny the need for dietary and other lifestyle modifications despite receiving obesity related education. He/she is likely to have intact general illness awareness, but minimize the negative health consequences of obesity and need for treatment.
Improving illness awareness in obese adults may facilitate treatment initiation and adherence, and potentially result in reductions in obesity-related morbidity and mortality.(4,5, 6) Yet, in order to accomplish this, a valid, reliable measure is required to accurately assess obesity awareness. The aims of this study were: (1) to perform a systematic review of currently available measures of obesity awareness, and (2) to present the development and initial validation of the Obesity Awareness and Insight Scale (OASIS), a novel instrument designed to assess obesity awareness and its core domains in adults.
Methods
Systematic Literature Review
A systematic review of English language publications from 1966 to July 2016 describing assessment instruments for subjective obesity awareness in overweight/obese adults (≥18 years) was conducted using OVID database (Medline®, PsycINFO, and Embase) on August 6th, 2016. The following search terms were used: (“awareness” OR “illness awareness” OR “anosognosia” OR “agnosia” OR “illness perception” OR “denial” OR “insight into illness”) AND (“obesity” OR “overweight” OR “obese”) AND (“assessments” OR “scales” OR “questionnaires”). Duplicates were removed. We excluded studies restricted to body image perception (i.e., satisfaction/dissatisfaction with how one perceives their appearance), psychiatric and neurological disorders, and to other medical conditions, including hypertension, hypercholesterolemia, hyperlipidemia, diabetes, and cardiovascular diseases. Studies focusing on weight gain in pregnant women, children, and adolescents were also omitted. Reference sections of included studies were gleaned for articles overlooked by the search strategy.
Obesity awareness measures were evaluated on the degree to which they assessed the core domains of illness awareness, and other psychometric properties.
Scale Development and Validation
OASIS was developed following the results of our systemic review of the literature (www.illnessawarenessscales.com). (4, 5, 16-20) Item development was guided by existing theoretical models and previously validated scales of illness awareness in other conditions.(11, 13, 21) Nine items were developed for potential inclusion in OASIS, including 3 items for General Illness Awareness, 2 items for Symptom Attribution, 3 items for Awareness of Need for Treatment and 1 item for Awareness of Negative Consequences. Of these, we included both positively and negatively keyed items to limit self-report response bias. For example, where one item measures awareness or acceptance of obesity i.e., “I am overweight”, another item measures denial or impairment of obesity awareness i.e., “I am at a healthy weight”. Each item consists of a 10-point Likert scale,(22) ranging from ‘Strongly Disagree’ to ‘Unsure’ to ‘Strongly Agree’. OASIS average total and subscale scores were derived for each domain. Scale items were reviewed by members from the Bariatric Clinic, Toronto General Hospital, which consists of surgeons, psychiatrists, psychologists, social workers, and nurse practitioners who have expertise in working with patients with obesity.
Data were collected utilizing a digital data collection platform, Research Now (https://www.researchnow.com), which ensures data quality through programmed quality checks. Participants were recruited via email from an online panel of individuals across Canada, excluding Quebec, to minimize recruitment of non-English speaking participants. OASIS was evaluated in 100 adult participants (23-25) representing a broad range of age (M = 58.1, SD = 12.3, range 25 to 78) and region of residence (40% Ontario, 44% Western, and 16% Atlantic provinces). All included participants had checked their weight within 2 weeks of initiating the study. Participants were selected based on quotas for the following 4 overweight/obese categorizations based on calculated body mass index (BMI) mass (kg) / height2 (m): (i) Previously diagnosed and BMI of 25-29.9 (n = 11); (ii) previously diagnosed and BMI ≥ 30 (n = 22); (iii) not previously diagnosed and BMI of 25-29.9 (n = 23); and (iv) not previously diagnosed and BMI ≥ 30 (n = 44). These categorizations and associated sampling were chosen to capture the full spectrum of overweight/obesity awareness, ranging from those with severe impairment to those with intact awareness and recognition of the need for intervention.
Demographic and clinical variables
Participants completed demographic and clinical assessments, which included a medical and psychiatric history, and the following measures: OASIS, Positive and Negative Affect Schedule (PANAS),(26) and Brief Illness Perception Questionnaire (B-IPQ).(16) PANAS is a valid and reliable measure to assess participants' positive and negative emotion states in non-clinical (i.e. non-psychiatric) general adult samples.(26) B-IPQ is a psychometrically validated scale to assess illness perception, which was identified through our systematic review.(16)
Prior to administration of OASIS and other clinical measures, participants were provided with basic education on obesity, including symptoms, health risks, and evidenced-based intervention strategies (Supplemental Material 5). This was done to ensure the assessment of subjective obesity awareness and level of acceptance of the condition, and not participant's degree of knowledge about the disease.
Validity
Convergent validity was evaluated using Pearson's correlations between OASIS and B-IPQ.(16) Discriminant validity was evaluated based on the associations between OASIS and PANAS to distinguish the construct of impaired illness awareness from emotional states.
To evaluate factor structure, a parallel analysis was performed to determine the number of components to extract.(27) Eigenvalues extracted from the original data were compared to the eigenvalues generated from a random dataset, which retain the same distributional properties as the original data. Eigenvalues from the original data that exceeded the 95th percentile eigenvalues generated from 1000 random permutations were extracted as components.(28) A principal components analysis was subsequently performed. No rotation was applied. Given that the development of the OASIS is based on an established model of illness awareness, a confirmatory factor analysis would have been ideal. However, the small sample size and the limited number of items created for each domain did not allow for this type of analysis to be carried out.
Reliability
Internal consistency of OASIS was evaluated based on Cronbach's coefficient alpha (α), and corrected item-to-total correlation (CITC). Items with CITC of < 0.25 were excluded to maximize internal consistency.(29)
Participants who agreed to re-take the survey were chosen randomly to assess one-month test-retest reliability using a two-way mixed intra-class correlation coefficient ICC evaluated at the 95% confidence interval.(30, 31) A total of 10 participants were included to detect an ICC of 0.7 at α=0.05 and power of 80%.(32)
Statistical analysis was performed using SPSS statistical software version 23.0 (IBM Corporation, Armonk, NY).
Results
Systematic Literature Review
Our search identified 451 publications. All of the titles and abstracts were read by 2 of the authors (PG, PS). Of these, 438 were deemed unrelated. The remaining full-text articles (n = 13) were reviewed. Six articles were excluded for the following reasons: assessed obesity-related knowledge rather than subjective obesity awareness; utilized measures restricted to body image perception; did not clearly assess subjective awareness (e.g., perception of risk for cancer in overweight/obese persons); or simply did not include a measure or measure description. The remaining 7 full-text articles were retained to assess their psychometric properties and determine the degree to which they assess the core domains of illness awareness (see Supplemental Material 1).(5, 16-20, 33) The findings from each study are summarized in Supplemental Material 2. Detailed descriptions of their psychometric properties can be found in Supplemental Material 3.
The results of our systematic review indicate that there is no comprehensive instrument specific to the assessment of obesity awareness. The currently available measures range from single to multi-domain constructs with dichotomous to multichotomous response options. The majority of the measures appear to assess, at least partially, the General Illness Awareness domain, and some cover other aspects of illness awareness. However, many items are not specific to the core domains of illness awareness, and do not clearly evaluate subjective obesity awareness (Supplemental Material 2). A single measure, B-IPQ, is psychometrically validated and demonstrates good test-retest reliability. However, there are limitations to using B-IPQ for the assessment of obesity awareness. Although illness awareness and illness perceptions are related, the constructs are distinct. B-IPQ was designed to assess a broad a range of illness perception categories (i.e., illness identity, timeline acute/chronic, timeline cyclical, consequences, personal control, treatment control, illness coherence, emotional representations, psychological attributions, risk factors, immunity, and accident or chance (16)), but is not specific to assessing one's subjective awareness and acceptance of having obesity.
Scale Development and Validation
Demographic and clinical characteristics
Table 1 lists the demographic and clinical characteristics of the 100 participants that met our selection criteria. Of these participants, 65 endorsed symptoms associated with obesity. Participants had moderate illness awareness as measured by OASIS average total score (M = 6.0, SD = 2.2). OASIS' correlations with the demographic and clinical variables are presented in Table 2. There was a modest correlation between OASIS and BMI, particularly in the General Illness Awareness and Awareness of Need for Treatment domains, indicating that those with greater obesity awareness had higher BMIs. No associations were observed between OASIS and age, education, age of illness onset, and illness duration.
Table 1. Demographic and clinical characteristics.
| Total sample | |
|---|---|
| N | 100 |
| Gender (% Female) | 31.0% |
| Mean (S.D.) | |
| Age, % ≥ 60 | 58.1 (12.3) 25-78, 49.0% |
| Body Mass Index (BMI) | 32.1 (4.8) 25-48 |
| Education (Years) | 14.6 (2.6) |
| Age of Illness Onset | 39.5 (15.8) |
| Illness Duration (Years) | 15.3 (14.2) |
| OASIS Average Total Scorea | 6.0 (2.2) |
| OASIS Illness Awarenessb | 6.5 (2.4) |
| OASIS Symptom Attributionc | 4.7 (3.0) |
| OASIS Awareness of Need for Treatmentd | 5.7 (2.2) |
| OASIS Awareness of Negative Consequencese | 6.8 (3.0) |
| B-IPQ Total Score | 24.6 (8.9) |
| PANAS Positive Affect Score | 31.6 (7.0) |
| PANAS Negative Affect Score | 17.6 (8.4) |
B-IPQ, Brief-Illness Perception Questionnaire; PANAS, Positive and Negative Affect Schedule.
OASIS Average Total Score excludes item 2 due to poor internal consistency.
OASIS General Illness Awareness includes items 3, 5, and 8.
OASIS Symptom Attribution includes item 1. Item 2 deleted due to poor internal consistency.
OASIS Awareness of Need for Treatment includes items 4, 6, and 9.
OASIS Awareness of Negative Consequences includes item 7.
Table 2. Correlations for the OASIS, B-IPQ, and PANAS.
| OASIS Average Total Score | OASIS General Illness Awareness 1, 2, 3, 4 | OASIS Symptom Attribution 2 | OASIS Awareness of Need for Treatment 3 | OASIS Awareness of Negative Consequences 4 | B-IPQ Total Score | PANAS Positive Affect Score | PANAS Negative Affect Score | |
|---|---|---|---|---|---|---|---|---|
| Age | -0.08 | -0.06 | -0.09 | -0.16 | 0.30 | -0.14 | 0.07 | -0.29* |
| Body Mass Index (BMI) | 0.34* | 0.38** | 0.18 | 0.35* | 0.26* | 0.25* | -0.03 | -0.01 |
| Education (Years) | 0.07 | 0.00 | 0.15 | -0.04 | 0.11 | 0.03 | 0.07 | 0.20* |
| Age of Illness Onset | 0.23 | 0.15 | 0.20 | 0.11 | 0.26 | -0.19 | -0.24 | -0.21 |
| Illness Duration (Years) | -0.26 | -0.07 | -0.24 | -0.22 | -0.22 | 0.11 | 0.34* | 0.04 |
| OASIS Item 1 | 0.81** | 0.55** | - | 0.54** | 0.64** | 0.43** | 0.00 | 0.24 |
| OASIS Item 2† | 0.15 | 0.13 | 0.24 | 0.08 | 0.05 | 0.17 | -0.07 | -0.04 |
| OASIS Item 3 | 0.78** | 0.89** | 0.55** | 0.71** | 0.54** | 0.67** | -0.08 | 0.30* |
| OASIS Item 4 | 0.80** | 0.79** | 0.60** | 0.79** | 0.59** | 0.57** | -0.05 | 0.27* |
| OASIS Item 5 | 0.58** | 0.76** | 0.24* | 0.62** | 0.38** | 0.50** | -0.29 | -0.01 |
| OASIS Item 6 | 0.46** | 0.44** | 0.23 | 0.69** | 0.27* | 0.38** | -0.45** | 0.08 |
| OASIS Item 7 | 0.84** | 0.61** | 0.64** | 0.56** | - | 0.51** | -0.09 | 0.29* |
| OASIS Item 8 | 0.84** | 0.91** | 0.58** | 0.74** | 0.63** | 0.53** | -0.09 | 0.23* |
| OASIS Item 9 | 0.67** | 0.63** | 0.41* | 0.78** | 0.44** | 0.56** | -0.12 | 0.38** |
| OASIS General Illness Awareness 1 | 0.86** | - | 0.55** | 0.81** | 0.61** | 0.66** | -0.17 | 0.21* |
| OASIS Symptom Attribution 2 | 0.81** | 0.55* | - | 0.54* | 0.64* | 0.43** | 0.00 | 0.24 |
| OASIS Awareness of Need for Treatment 3 | 0.84** | 0.81* | 0.54** | - | 0.56** | 0.67** | 0.29* | 0.33* |
| OASIS Awareness of Negative Consequences 4 | 0.84** | 0.61* | 0.64** | 0.56** | - | 0.51* | -0.09 | 0.29* |
| OASIS Average Total Score | - | 0.86** | 0.81** | 0.85** | 0.84** | 0.65** | -0.14 | 0.32* |
| B-IPQ Consequences | 0.69** | 0.68** | 0.49** | 0.72** | 0.53** | 0.86** | -0.32* | 0.44** |
| B-IPQ Timeline | 0.01 | 0.14 | -0.13 | 0.05 | -0.02 | 0.44** | -0.18 | 0.04 |
| B-IPQ Personal control | -0.09 | -0.24* | 0.15 | -0.23* | 0.01 | -0.37** | 0.22* | -0.12 |
| B-IPQ Cure control | 0.38** | 0.38** | 0.35* | 0.35 * | 0.23* | 0.03 | 0.21* | 0.03 |
| B-IPQ Symptom Identity | 0.70** | 0.62** | 0.58** | 0.68** | 0.58** | 0.80** | -0.30* | 0.46** |
| B-IPQ Concern | 0.74** | 0.74** | 0.61** | 0.72* | 0.55** | 0.78** | -0.18 | 0.35* |
| B-IPQ Understanding | 0.16 | 0.14 | 0.11 | 0.06 | 0.21* | 0.21* | 0.13 | -0.16 |
| B-IPQ Emotional response | 0.55** | 0.49** | 0.48** | 0.55** | 0.43** | 0.76** | -0.23* | 0.63** |
| B-IPQ Total score | 0.65** | 0.66** | 0.43* | 0.67** | 0.51** | - | -0.35* | 0.46** |
| PANAS Positive Affect Score | -0.14 | -0.17 | 0.00 | -0.29 * | -0.09 | -0.35* | - | -0.20* |
| PANAS Negative Affect Score | 0.32* | 0.21* | 0.24 | 0.33* | 0.29* | 0.46** | -0.20* | - |
B-IPQ, Brief-Illness Perception Questionnaire; PANAS, Positive and Negative Affect Schedule.
OASIS General Illness Awareness includes items 3, 5, and 8.
OASIS Symptom Attribution includes item 1. Item 2 deleted due to poor internal consistency.
OASIS Awareness of Need for Treatment includes items 4, 6, and 9.
OASIS Awareness of Negative Consequences includes item 7.
Grey highlight indicates that this item was deleted from the scale due to poor internal consistency.
p< 0.05.
p ≤ 0.0002, Bonferroni correction for multiple comparisons.
Validity
OASIS average total (see Figure 1) and subscale scores were correlated with B-IPQ total score, and also significantly associated with most B-IPQ items, i.e., consequences, identity, concern, and emotional response, which indicates good convergent validity. PANAS Positive Affect scores were not correlated with OASIS average total or subscale scores. PANAS Negative Affect scores were modestly associated with OASIS average total scores (see Table 2), suggestive of good discriminant validity.
Figure 1. Convergence (r) for OASIS average total score with the Brief Illness Perception Questionnaire (B-IPQ) total score.
One component emerged from the parallel analysis of all 9 OASIS items (Supplemental Material 4 presents the scree plot). The first 3 eigenvalues generated from actual data were 4.72, 1.31, and 0.87. The 3 95th percentile eigenvalues generated from random data were 1.61, 1.39, and 1.23.
The single component extracted explained 52.5% of the variance in OASIS. The Kaiser-Meyer-Olkin measure of sampling adequacy was 0.85. The factor loadings for the single latent component, CITCs, and the domain for each item are presented in Table 3.
Table 3. OASIS factor loadings and internal reliability.
| Expected Domain | Items | Factor Loading (Principle Component Method) | Corrected Item-To-Total Correlation (CITC) |
|---|---|---|---|
| Symptom Attribution | 1. My experiences are due to being overweight or obese | 0.717 | 0.628 |
| Symptom Attribution † | 2. My experiences are due to other reasons than my weight regardless of what other people think (e.g. doctors, family, friends, etc.). | 0.140 | 0.134 |
| General Illness Awareness | 3. I have an excessive amount of body fat. | 0.856 | 0.759 |
| Awareness of Need for Treatment | 4. I NEED to make or maintain healthy life style changes to improve my diet and increase the amount I exercise. | 0.890 | 0.792 |
| General Illness Awareness | 5.I am at a healthy weight. | 0.618 | 0.555 |
| Awareness of Need for Treatment | 6. I can safely carry on my current lifestyle (i.e. eating and exercising as I currently do). | 0.456 | 0.401 |
| Awareness of Negative Consequences | 7. My weight has led or can lead to negative health consequences (e.g. high cholesterol, hypertension, diabetes, heart disease, depression, etc.). | 0.912 | 0.824 |
| General Illness Awareness | 8. I am overweight or have obesity (i.e. Body Mass Index greater than 25 = overweight; Body Mass Index greater than 30 = obese). | 0.898 | 0.805 |
| Awareness of Need for Treatment | 9. I need weight loss treatment. | 0.661 | 0.517 |
Cronbach's alpha excluding item 2 is 0.862.
Grey highlight indicates that this item was deleted from the scale due to poor internal consistency
Reliability
The CITCs for each item were > 0.25, except item 2 (see Table 3). Cronbach's α for OASIS with item 2 deleted was 0.89, indicating strong internal consistency.(34)
The ICC for one-month test-retest reliability for OASIS total score was 0.76 at the 95% confidence interval.
Discussion
With the increasing global prevalence of obesity and related complications,(35-38) further investigation of obesity awareness (www.illnessawarenessscales.com) is necessary to refine our understanding of its role in treatment outcomes. To accomplish this, a valid measure of subjective illness awareness specific to obesity is essential. The lack of such a scale led to the development and psychometric validation of OASIS, a novel, easy-to-use, comprehensive measure of subjective obesity awareness. OASIS contains 8-items each using a 10-point Likert scale to assess the core domains of illness awareness in obesity. OASIS takes approximately 2 minutes to complete. The results of psychometric testing provide preliminary support for the validity and reliability of OASIS.
The results of our systematic review suggest that currently available measures range from single to multi-domain constructs and differ in their effectiveness in evaluating the core domains of illness awareness in obesity. Since illness awareness exists on a continuum, the use of dichotomous and multiple-choice questions rather than rating scales (i.e., Likert-type items) may limit expression and response range. Of the seven measures we encountered, only B-IPQ is a psychometrically validated instrument in a number of chronic illnesses; however, it is not obesity-specific.
OASIS and its subscales demonstrate good convergent validity with the B-IPQ total score, and discriminant validity with the PANAS Positive and Negative Affect scores. Of note, OASIS average total score and subscale scores were not correlated with the B-IPQ items that do not directly assess illness awareness (i.e., timeline, personal control, and understanding). For example, the B-IPQ item, “How much control do you feel you have over your illness?” may assess perceived ‘control’ over their illness, whereas the OASIS item “I NEED to make or maintain healthy life style changes to improve my diet and increase the amount I exercise” is specific to awareness of need for dietary and other lifestyle modifications.
OASIS and its subscales were positively correlated with BMI. This suggests that individuals with higher BMI are more subjectively aware of having obesity, the health consequences, and need for lifestyle modifications. At the same time, this indicates the importance of acquiring subjective obesity awareness at the early stages of weight gain to motivate individuals to engage in healthier lifestyle behaviors to prevent progression.(19)
Although 2 items were initially designed to measure Symptom Attribution, item 2 was excluded due to weak internal consistency. The other remaining item to measure Symptom Attribution demonstrated good internal consistency, and convergent and discriminant validity, indicating the need for this domain in this population.
The single-factor solution is consistent with previously validated measures of illness awareness in other conditions.(39, 40) Although clinically distinct, factor analyses tend to suggest that the hypothesized domains represent a single latent component. Despite the lack of empirical support for a multidimensional structure, these rationally derived domains are theoretically subsumed within overall illness awareness. As OASIS is designed based on an established theoretical model, a confirmatory factor analysis would have been ideal. However, the limited number of items created for each domain in combination with the sample size did not allow for this to be performed. We balanced the need between adopting traditional psychometric principles and developing an instrument that is sufficiently concise for clinical utility. Having fewer than 4 domains as well as critical items linked to key outcomes (e.g., Awareness of Negative Consequences) might permit for both. Future research evaluating this hierarchical structure, and the predictive utility of overall illness awareness and specific domains, will be a valuable addition to the literature.
Our study has a few limitations. First, specific to the systematic review, although we performed a comprehensive search, we may have excluded relevant articles that used other terms related to subjective illness awareness. Additionally, our search was limited to English language publications, possibly excluding relevant measures in other languages. Second, regarding the psychometric assessment of OASIS, a possible limitation is the use of a digital data collection platform, which will exclude individuals without access to or those who are not familiar with the use of a computer. Further, there may be a selection bias toward motivated participants. That being said, studies report no differences in reliability or validity between online or clinically based surveys.(41) Moreover, the platform used in this study ensures data quality through programmed quality checks. A third limitation may stem from our selection criteria for overweight/obese categorizations. Particularly, if participants were not previously diagnosed as being overweight/obese, it is possible that they have lower obesity awareness scores due to lack of knowledge about the condition or affirmation from a medical professional. In order to minimize the influence of knowledge on subjective illness awareness, participants were provided with background information on obesity, including clear definitions of obesity, associated symptoms, treatment options, and consequences prior to completing study measures (Supplemental Material 5). Last, the results of OASIS are not generalizable to children or adolescents with obesity.
Conclusion
In summary, OASIS provides a novel, disease-specific instrument to measure subjective obesity awareness. As the first study to validate a scale of its kind, OASIS may be utilized in epidemiology studies to investigate the true extent to which subjective obesity awareness is associated with clinical outcomes. Furthermore, OASIS may be useful for neuroimaging and neurophysiology studies investigating the neural correlates of obesity awareness, and prospective intervention studies targeting impaired obesity awareness.
Supplementary Material
Acknowledgments
The authors would like to thank Wanna Mar, research coor- dinator. The research was partially supported by Centre for Addiction and Mental Health (CAMH) Research (PG), CAMH Foundation grant, Ontario Mental Health Foundation (OMHF) - Type A Grant (AGG), and National Institutes of Health RO1MH084886-01A2 (AGG).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003-2008 Study. Int J Obes (Lond) 2011;35(8):1063–70. doi: 10.1038/ijo.2010.229. [DOI] [PubMed] [Google Scholar]
- 2.Swift JA, Glazebrook C, Anness A, Goddard R. Obesity-related knowledge and beliefs in obese adults attending a specialist weight-management service: implications for weight loss over 1 year. Patient Education & Counseling. 2009;74(1):70–6. doi: 10.1016/j.pec.2008.07.045. [DOI] [PubMed] [Google Scholar]
- 3.Burroughs VJ, Nonas C, Sweeney CT, Rohay JM, Harkins AM, Kyle TK, et al. Self-reported comorbidities among self-described overweight African-American and Hispanic adults in the United States: results of a national survey. Obesity. 2008;16(6):1400–6. doi: 10.1038/oby.2008.61. [DOI] [PubMed] [Google Scholar]
- 4.Oksel E, Gunduzoglu NC, Topcu S. The Perception of Obese Persons: Cross Cultural Considerations. Holistic Nursing Practice. 2015;29(4):225–31. doi: 10.1097/HNP.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 5.Johnson F, Beeken RJ, Croker H, Wardle J. Do weight perceptions among obese adults in Great Britain match clinical definitions? Analysis of cross-sectional surveys from 2007 and 2012. BMJ Open. 2014;4(11):e005561. doi: 10.1136/bmjopen-2014-005561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.den Engelsen C, Vos RC, Rijken M, Rutten GE. Comparison of perceptions of obesity among adults with central obesity with and without additional cardiometabolic risk factors and among those who were formally obese, 3 years after screening for central obesity. BMC Public Health. 2015;15:1214. doi: 10.1186/s12889-015-2544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson F, Cooke L, Croker H, Wardle J. Changing perceptions of weight in Great Britain: comparison of two population surveys. BMJ. 2008;337:a494. doi: 10.1136/bmj.a494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson-Taylor WL, Fisher RA, Hubbard VS, Starke-Reed P, Eggers PS. The change in weight perception of weight status among the overweight: Comparison of NHANES III (1988-1994) and 1999-2004 NHANES. International Journal of Behavioral Nutrition and Physical Activity. 2008;5(9) doi: 10.1186/1479-5868-5-9. no pagination. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salcedo V, Gutierrez-Fisac JL, Guallar-Castillon P, Rodriguez-Artalejo F. Trends in overweight and misperceived overweight in Spain from 1987 to 2007. International Journal of Obesity. 2010;34(12):1759–65. doi: 10.1038/ijo.2010.96. [DOI] [PubMed] [Google Scholar]
- 10.Wetmore CM, Mokdad AH. In denial: misperceptions of weight change among adults in the United States. Prev Med. 2012;55(2):93–100. doi: 10.1016/j.ypmed.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 11.Amador XF, Strauss DH, Yale SA, Gorman JM. Awareness of illness in schizophrenia. Schizophr Bull. 1991;17(1):113–32. doi: 10.1093/schbul/17.1.113. [DOI] [PubMed] [Google Scholar]
- 12.Cooke MA, Peters ER, Kuipers E, Kumari V. Disease, deficit or denial? Models of poor insight in psychosis. Acta psychiatrica Scandinavica. 2005;112(1):4–17. doi: 10.1111/j.1600-0447.2005.00537.x. [DOI] [PubMed] [Google Scholar]
- 13.David AS. Insight and psychosis. The British journal of psychiatry: the journal of mental science. 1990;156:798–808. doi: 10.1192/bjp.156.6.798. [DOI] [PubMed] [Google Scholar]
- 14.Gerretsen P, Plitman E, Rajji TK, Graff-Guerrero A. The effects of aging on insight into illness in schizophrenia: a review. Int J Geriatr Psychiatry. 2014;29(11):1145–61. doi: 10.1002/gps.4154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams AR, Olfson M, Galanter M. Assessing and improving clinical insight among patients “in denial”. JAMA Psychiatry. 2015;72(4):303–4. doi: 10.1001/jamapsychiatry.2014.2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 17.Agrawal P, Gupta K, Mishra V, Agrawal S. A study on body-weight perception, future intention and weight-management behaviour among normal-weight, overweight and obese women in India. Public Health Nutr. 2014;17(4):884–95. doi: 10.1017/S1368980013000918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sivalingam SK, Ashraf J, Vallurupalli N, Friderici J, Cook J, Rothberg MB. Ethnic Differences in the Self-Recognition of Obesity and Obesity-Related Comorbidities: A Cross-Sectional Analysis. Journal of General Internal Medicine. 2011;26(6):616–20. doi: 10.1007/s11606-010-1623-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tol J, Swinkels IC, De Bakker DH, Veenhof C, Seidell JC. Overweight and obese adults have low intentions of seeking weight-related care: A cross-sectional survey. BMC Public Health. 2014;14(1):582. doi: 10.1186/1471-2458-14-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Truesdale KP, Stevens J. Do the obese know they are obese? North Carolina medical journal. 2008;69(3):188–94. [PMC free article] [PubMed] [Google Scholar]
- 21.Gerretsen P, Remington G, Borlido C, Quilty L, Hassan S, Polsinelli G, et al. The VAGUS insight into psychosis scale - Self-report and clinician-rated versions. Psychiatry research. 2014;220(3):1084–9. doi: 10.1016/j.psychres.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Preston CC, Colman AM. Optimal number of response categories in rating scales: reliability, validity, discriminating power, and respondent preferences. Acta Psychologica. 2000;104(1):1–15. doi: 10.1016/s0001-6918(99)00050-5. [DOI] [PubMed] [Google Scholar]
- 23.Everitt BS. Multivariate analysis: the need for data, and other problems. The British journal of psychiatry: the journal of mental science. 1975;126:237–40. doi: 10.1192/bjp.126.3.237. [DOI] [PubMed] [Google Scholar]
- 24.Nunnally JC. Psychometric theory. McGraw-Hill; 1978. [Google Scholar]
- 25.MacCallum RC, Widaman KF, Zhang S, Hong S. Sample size in factor analysis. Psychological Methods. 1999;4(1):84–99. [Google Scholar]
- 26.Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. The British journal of clinical psychology / the British Psychological Society. 2004;43(Pt 3):245–65. doi: 10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- 27.O'Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and velicer's MAP test. Behavior research methods, instruments, & computers: a journal of the Psychonomic Society, Inc. 2000;32(3):396–402. doi: 10.3758/bf03200807. [DOI] [PubMed] [Google Scholar]
- 28.Quilty LC, Ayearst L, Chmielewski M, Pollock BG, Bagby RM. The Psychometric Properties of the Personality Inventory for DSM-5 in an APA DSM-5 Field Trial Sample. Assessment. 2013;20(3):362–9. doi: 10.1177/1073191113486183. [DOI] [PubMed] [Google Scholar]
- 29.Clark LA, Watson D. Constructing Validity: Basic Issues in Objective Scale Development. Psychological Assessment. 1995;7(3):309–19. doi: 10.1037/pas0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fleiss JL. The design and analysis of clinical experiments. xiv. New York: Wiley; 1986. p. 432. [Google Scholar]
- 31.Marx RG, Menezes A, Horovitz L, Jones EC, Warren RF. A comparison of two time intervals for test-retest reliability of health status instruments. Journal of Clinical Epidemiology. 2003;56(8):730–5. doi: 10.1016/s0895-4356(03)00084-2. [DOI] [PubMed] [Google Scholar]
- 32.Bujang MA. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: a review. 2017:1–11. [Google Scholar]
- 33.Oksel E, Gündüzoğlu NÇ, Topçu S. The Perception of Obese Persons: Cross Cultural Considerations. Holistic Nursing Practice. 2015;29(4):225–31. doi: 10.1097/HNP.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 34.Cortina J. What is coefficient alpha? An examination of theory and applications. Journal of Applied Psychology. 1993:98–104. [Google Scholar]
- 35.Kirunda BE, Fadnes LT, Wamani H, Van den Broeck J, Tylleskar T. Population-based survey of overweight and obesity and the associated factors in peri-urban and rural Eastern Uganda. BMC Public Health. 2015;15:1168. doi: 10.1186/s12889-015-2506-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bancej C, Jayabalasingham B, Wall RW, Rao DP, Do MT, de Groh M, et al. Evidence Brief--Trends and projections of obesity among Canadians. Health Promotion and Chronic Disease Prevention in Canada. 2015;35(7):109–12. doi: 10.24095/hpcdp.35.7.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oksel E, Gunduzoglu NC, Topcu S. The Perception of Obese Persons: Cross Cultural Considerations. Holist Nurs Pract. 2015;29(4):225–31. doi: 10.1097/HNP.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 39.Sanz M, Constable G, Lopez-Ibor I, Kemp R, David AS. A comparative study of insight scales and their relationship to psychopathological and clinical variables. Psychological medicine. 1998;28(2):437–46. doi: 10.1017/s0033291797006296. [DOI] [PubMed] [Google Scholar]
- 40.Lincoln TM, Lullmann E, Rief W. Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr Bull. 2007;33(6):1324–42. doi: 10.1093/schbul/sbm002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Risko EF, Quilty LC, Oakman JM. Socially Desirable Responding on the Web: Investigating the Candor Hypothesis. Journal of personality assessment. 2006;87(3):269–76. doi: 10.1207/s15327752jpa8703_08. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


