Abstract
Introduction
The prevalence of major trauma in the elderly is increasing with ageing western societies. Frailty is now a well-recognised predictor of poor outcome after injury; however, few studies have focused on the progression of frailty and patients’ perceptions of their injuries after discharge.
Aim
We hypothesised that the number of elderly patients that survive major trauma is low and, of those that do, frailty post injury worsens with overall negative views about quality of life. To investigate this, we examined mortality, frailty and patient experience for elderly major trauma admissions to a level 1 trauma centre at one year after admission.
Method
All consecutive patients > 75 with an injury severity score of > 15 were included in the study. Patients were invited to participate in a structured telephone interview to assess change in frailty status as well as assess patient experience after injury.
Results
A total of 79 patients met inclusion criteria; 34 patients had died and 17 were uncontactable; 88% had become more frail (p < 0.05), and more than half commented positively on their overall quality of life following injury.
Conclusions
These findings highlight the elevated mortality in elderly major trauma patients, but also indicate that preconceived opinions on quality of life, post injury, might not be appropriate.
Keywords: Major trauma, frailty, elderly, geriatrics, reported Edmonton Frail Scale
Introduction
Major trauma admissions have been steadily increasing over the last decade.1 Approximately 20,000 cases of major trauma occur every year in England, with approximately 5400 deaths and other life changing injuries resulting in long-term disabilities.2 Although overall major trauma contributes less than 1% to emergency department attendances, it is estimated that costs to the NHS exceed £400 million per year in immediate treatment, with the long-term costs of care being unknown.2 With the rising age of the population, low level falls (<2 m) are now the leading mechanism of injury for major trauma in the UK and the socioeconomic burden of caring for elderly patients with significant injuries is likely to increase further.1
There is a relative paucity of literature specifically focussing on outcomes in elderly trauma. Early studies found that elderly trauma patients have higher mortality and complications compared to younger patients with similar traumatic injuries, with age and injury severity score being independent predictors of poor outcome.3,4 Data collected from the Trauma Audit & Research Network (TARN) highlight that death rates from major trauma increase steeply in older patients during the first year post-injury.5 The report also identifies that co-morbidity has an adverse effect on outcome and that further research focussing on frailty is required.
Frailty is a well-recognised clinical entity, independent of age, co-morbidity and disability. It is defined as a state of reduced physiological reserve, and associated with an increased susceptibility to poor healthcare outcomes.6 Studies have shown that frailty status pre-trauma has a direct effect on outcome following major trauma.7 The Edmonton Frail Scale (EFS) is a simple-to-complete frailty assessment that comprises 10 questions and 1 physical assessment (‘timed up and go’). The EFS has been validated against comprehensive geriatric assessment (CGA), the current gold-standard for frailty assessment, and shown to be reliable and feasible for routine use by non-geriatricians.8 Scores range from 0 (not frail) to 18 (very frail), with scores of 8 or above being defined as frail. EFS has been used in other surgical settings, where patients with scores of 8 or more were likely to have increased post-operative complications and less likely to be discharged home.9 Reported Edmonton Frail Scale (REFS) is an adaptation of EFS, that can be performed in less than 10 minutes by any healthcare professional.10 REFS substitutes the last domain on EFS, the physical performance measure, with three self-assessed physical performance questions (Table 1) and has been cross validated against CGA.10
Table 1.
Reported Edmonton Frail Scale, adapted from Hilmer et al.10
| Domain | Item | 0 Point | 1 Point | 2 Points |
|---|---|---|---|---|
| Cognition | Pre-drawn circle. Add the numbers in the correct positions to make a clock then place the hands to indicate a time of 10 after 11 | No errors | Minor errors | Major errors |
| General health | In the past year, how many times have you been admitted to a hospital? In general, how would you describe your health? | 0 Good/Excellent | 1–2 Fair | >2 Poor |
| Functional independence | With how many of the following activities do you require help? - Meal preparation, shopping, transportation, telephone, housekeeping, laundry, managing money, taking medications | 0–1 | 2–4 | >4 |
| Social support | When you need help, can you count on someone who is willing and able to meet your needs? | Always | Sometimes | Never |
| Medication use | Are you on five or more different prescription medications on a regular basis? At times, do you forget to take your prescription medications? | No No | Yes Yes | |
| Nutrition | Have you recently lost weight | No | Yes | |
| Mood | Do you often feel sad or depressed? | No | Yes | |
| Continence | Have you experienced incontinence | No | Yes | |
| Functional performance | Two weeks ago, were you able to: • Do heavy work around the house like washing windows, walls, or floors without help? • Walk up and down stairs to the second floor without help? • Walk 1 km without help? | Yes Yes Yes | No No No |
We hypothesised that mortality in elderly trauma remains high, despite advances in trauma care, and that frailty post-injury would decline with negative overall views about quality of life. With better understanding of the overall trajectory of injured elderly patients, doctors can provide more reliable advice to patients, relatives and carers about what to expect during admission and after discharge.
Method
All patients > 75 years of age admitted to a Level 1 major trauma centre (MTC) in 2013 with ISS > 15 were included in a retrospective analysis of case notes and discharge summaries. General practitioners were contacted to confirm patients were still alive at one year. These survivors were telephoned and asked questions as part of the post-discharge follow-up by two junior doctors, who were not involved in the direct care of the patients during the admission. The patient (or carer if more appropriate) answered a number of questions, including a frailty assessment score based on the REFS, assessing current function, and function pre-injury (retrospective). As the assessment was completed over the phone, the first part of the REFS, clock draw, was not completed. In addition, a semi-structured interview was performed to gauge patients’ perceptions about their admission and life after injury (Table 2). Patients were asked to elaborate on each answer and these were transcribed by the interviewer.
Table 2.
Interview questions used to qualify patients’ experience.
| 1. How do you feel when you think about the accident? |
| 2. How do you feel about life now? |
| 3. Do you ever wish you had not survived the traumatic event? |
To analyse data, unpaired T test, paired T test and Pearson correlation coefficient were used, via commercially available online software (GraphPad QuickCalcs, GraphPad Software, California).
Results
Study population
Overall, 79 patients (40 males) met the study’s eligibility criteria, with patient age at injury ranging from 75 to 101 years (mean age 83 years). At one year, 34/79 (43%) of patients had died, 17 were uncontactable/unwilling to participate, and so 28 patients (15 female) were reviewed and followed up.
Injury severity score and mortality
Injury severity score (ISS) ranged from 16 to 54 (mean 24). The mortality rate was 22% (17 patients) at 30 days and 43% (34 patients) at 12 months. Patients who survived had a mean ISS of 23.9 ± 7.6 (range 16–54), whereas those who had died by 12 months had an average ISS of 25 ± 7.73 (range 16–43) (unpaired t test, T = 0.63, p > 0.5).
Frailty assessment
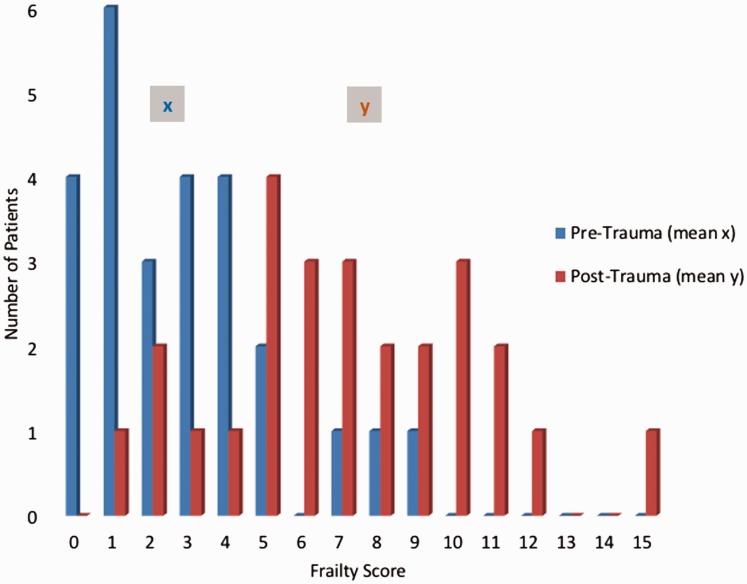
The range of frailty scores pre-trauma was 0–9 points (mean 2.8, median 2.5), following injury, no patient’s score improved and the majority of participants (88%) had become significantly more frail at one year follow-up (Figure 1; T score is 6.6, p < 0.01 using paired t test). The increase in frailty score at one-year ranged from 1 to 15 points (mean 7.3, median 7).
Figure 1.
Frailty scores pre- and post-trauma. x – Pre-Trauma mean score of 2.85. y – Post-trauma mean score of 7.08.
ISS and increasing frailty
The two patients with the highest ISS score, 26 and 38, had the biggest increase in frailty scores (10 points). Pearson correlation coefficient showed a positive trend towards greater frailty decline with higher ISS (R = 0.377 (positive correlation), p = 0.057)
Patient evaluation of quality of life
The majority (57%) of patients were generally satisfied with being alive and surviving the trauma, views also shared amongst patients who were severely restricted post-trauma; examples of positive comments included; ‘very glad to be alive’ and ‘I thank God I survived’. Moreover, the majority of patients were thankful for their care, particularly patients who were discharged back to their own home. One patient had commented that he was able to ‘return to work’, and therefore maintain his independence.
Only 29% had negative views or comments on their experience. Ongoing anxiety and frustration since the trauma was evident, particularly relating to the loss of independence and inability to complete previous tasks. This recurrent theme was highlighted by comments including; ‘unable to play golf’ and ‘unable to drive’. One patient who had speech and memory loss as a result of the trauma, reported a perception of ‘loss of sense of purpose’ as he was unable to return to work. This was coupled with a feeling of isolation, as some patients reported on feeling ‘like a prisoner’ and not feeling ‘free’. In addition, approximately a quarter of patients described being ‘low in mood’ and depressed one year on from the trauma. Patients reported being ‘more tearful’ and having a more pessimistic outlook on life since the trauma.
Discussion
Despite advances in trauma care, mortality remains high in elderly trauma. Similar to other studies performed in large cohorts, we identified that the mortality at one-year post-injury remained above 40%. This study found that there was no statistically significant relationship between increasing ISS and increasing mortality but was likely due to a small sample size. There was a statistically significant worsening of frailty one year after hospital admission; before admission, only 8% of our patient group were defined as frail, but this increased to 46% a year after major trauma. This is likely to have significant implications to the individual patient, social services and healthcare infrastructure. These results are in contrast to Day et al.11 who found the vast majority of patients returned to full independence and mobility. The differences may potentially be due to differences in ‘host factors’; Day et al. included younger patients (60 vs. 75 years in this study) and found that age was an important factor influencing survival. Nijboer et al.12 found that ‘host factors,’ such as age, gender and pre-injury medical status, contributed to long-term survival, and not injury severity alone.12 More recently, other research reported that sarcopenia is an independent risk factor for adverse outcomes and increased length of hospital stay.13 There are therefore likely several ‘host factors’ that need to be taken into consideration when reviewing outcomes.
To date there are little qualitative data exploring elderly patients’ experiences after sustaining traumatic injuries. Patients’ experiences mainly included emotional responses of being generally happy about still being alive despite the trauma and residual deficits. Kaufman et al.14 examined different aspects of trauma patients’ experiences during the acute phase and found that their experiences were dependent largely on trauma team members' demeanour, expertise, and efficiency and they valued clear clinical communication. These positive experiences may largely be influenced by the initial, longer term and holistic management provided by the MTC. Patients were grateful for the care they received and were overall very thankful for the MTC and expert management.14
The main negative theme from patients centred around loss of independence and a feeling of isolation as a result of the trauma; both of these could in fact be linked to the worsening level of frailty identified in our study group. As patients were more frail after trauma, they were less able to complete previously routine tasks. Their reliance on family and carers for assistance had increased following trauma and had not improved with their expectations in the months following injury. This caused great frustration to a number of patients, possibly more so given the sudden deterioration as a result of the trauma. This is in contrast to the more gradual decline associated with conditions such as dementia and chronic conditions where patients and relatives are able to gradually adapt to change.
Despite the majority of patients being happy to be alive, a feeling of pessimism or low mood was common; this notion of depression has been highlighted previously in younger trauma patients and this study shows that it occurs in the elderly population.15 At one-year, a quarter of our patients had persistent feelings of low mood, highlighting the need for such outcomes to be anticipated during the admission and a process for follow up and assessment in the community to occur. Several charities and organisations provide psychological support to survivors of trauma and it is important that these resources are easily accessible for elderly as well as young patient groups.
Since the start of this study, there have been significant changes in how success is measured, and the trauma networks have started to look more at quality of life after injury. Despite this, quality of life outcome measures are not routinely collected in major trauma patients as part of TARN; in contrast, the national hip fracture database (NHFD) has recently introduced a quality of life score as part of its assessment which involves patients completing a quality of life assessment (EQ5D). We feel similar scoring needs to become part of the assessment of all major trauma patients, particularly the elderly; such large-scale data collection on quality of life would provide relevant and useful information about patient outcomes and success of treatment, with an opportunity to identify areas of holistic management that could be improved.
There are some design limitations of the study which deserve discussion. The sample size was small with additional loss to follow-up compared to previous multicentre studies using data from large databases. It focused on the anatomic injury as defined by the ISS score and emotional responses, although there are known limitations associated with using ISS, as unlike the New ISS (NISS), it does not take into account multiple injuries within the same body region. In addition, the use of a modified REFS over the phone meant that patients were unable to be scored with regard to clock draw which meant patients’ scores were 2 points less than set out by REFS, which could have affected the overall score. Furthermore, the 12-month follow-up telephone consultations with patients, relatives and carers would have been subject to recall bias. It would have been beneficial to use a standardised, validated patient health outcome assessment tool when looking at patient experience.
Future research could involve extending the length of the study or extracting data from TARN, thereby increasing sample size. Gathering information about the patient’s pre-trauma function during their admission or gaining consent to review the patient’s pre-trauma care plan by the General Practitioner (that outlines their pre-morbid function) could contribute to minimising any potential biases. In addition, steps have been made by NHS England to increase the identification of frailty in primary care using electronic frailty scores which could be utilised in assessing pre-morbid frailty in the future.16
Conclusions
Elderly patients who experienced a major trauma event and were admitted to an MTC had a mortality of 43% at one year, with half of those deaths occurring in hospital within 30 days, but the severity of the injury was not directly linked to increasing mortality. Survivors were more frail a year after admission. Patients who survived major trauma tended to have an overall positive outlook, and the extent of the injury and resulting disability did not affect this. However, low mood is a major factor affecting patients’ lives at one-year after trauma and should be anticipated during the admission and reviewed in the community. TARN should collect specific data on frailty and quality of life of elderly trauma patients.
Acknowledgements
None.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Ethical approval was not required as information constituted routine follow up.
Informed consent
Verbal informed consent was obtained from all subjects during the phone consultation.
Trial Registration
Not applicable because information constituted routine care and follow up.
Guarantor
MF.
Contributorship
The authors state equal contribution in the elaboration of this manuscript. LK analysed the data and wrote the manuscript. RK compiled the data. AK analysed the data and wrote the manuscript. GP, MW and SH edited the final manuscript. MF wrote the manuscript and oversaw the project. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Provenance
Not commissioned, externally peer reviewed.
References
- 1.Kehoe A, Smith JE, Edwards A, et al. The changing face of major trauma in the UK. Emerg Med J 2015; 32: 911–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Major trauma care in England, www.nao.org.uk/wp-content/uploads/2010/02/0910213.pdf (2009, accessed 13 February 2018).
- 3.Champion HR, Edin F, Copes WS, et al. Major Trauma in geriatric patients, www.ncbi.nlm.nih.gov/pmc/articles/PMC1349704/pdf/amjph00235-0078.pdf (accessed 1 February 2018).
- 4.Hashmi A, Ibrahim-Zada I, Rhee P, et al. Predictors of mortality in geriatric trauma patients. J Trauma Acute Care Surg 2014; 76: 894–901. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee J, Baxter M, Coats T, et al. Major trauma in older people, www.tarn.ac.uk/content/downloads/3793/Major Trauma in Older People 2017.pdf (2017, accessed 1 July 2018).
- 6.Vermeiren S, Vella-Azzopardi R, Beckwée D, et al. Frailty and the Prediction of negative health outcomes: a meta-analysis. J Am Med Dir Assoc 2016; 17: 1163.e1–1163.e17. [DOI] [PubMed] [Google Scholar]
- 7.Joseph B, Phelan H, Hassan A, et al. The impact of frailty on failure-to-rescue in geriatric trauma patients. J Trauma Acute Care Surg 2016; 81: 1150–1155. [DOI] [PubMed] [Google Scholar]
- 8.Perna S, Francis MDA, Bologna C, et al. Performance of Edmonton Frail Scale on frailty assessment: its association with multi-dimensional geriatric conditions assessed with specific screening tools. BMC Geriatr 2017; 17: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dasgupta M, Rolfson DB, Stolee P, et al. Frailty is associated with postoperative complications in older adults with medical problems. Arch Gerontol Geriatr 2009; 48: 78–83. [DOI] [PubMed] [Google Scholar]
- 10.Hilmer SN, Perera V, Mitchell S, et al. The assessment of frailty in older people in acute care. Aust J Age 2009; 28: 182–188. [DOI] [PubMed] [Google Scholar]
- 11.Day RJ, Vinen J, Hewitt-Falls E. Major trauma outcomes in the elderly. Med J Aust 1994; 160: 675–678. [PubMed] [Google Scholar]
- 12.Nijboer JMM, van der Sluis CK, Dijkstra PU, et al. The value of the trauma mechanism in the triage of severely injured elderly. Eur J Trauma Emerg Surg 2009; 35: 49–55. [DOI] [PubMed] [Google Scholar]
- 13.Deandrade J, Pedersen M, Garcia L, et al. Sarcopenia is a risk factor for complications and an independent predictor of hospital length of stay in trauma patients. J Surg Res 2018; 221: 161–166. [DOI] [PubMed] [Google Scholar]
- 14.Kaufman EJ, Richmond TS, Wiebe DJ, et al. Patient experiences of trauma resuscitation. JAMA Surg 2017; 152: 843–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiseman TA, Curtis K, Lam M, et al. Incidence of depression, anxiety and stress following traumatic injury: a longitudinal study. Scand J Trauma Resusc Emerg Med 2015; 23: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Updated guidance on supporting routine frailty identification and frailty care through the GP, www.england.nhs.uk/wp-content/uploads/2017/04/supporting-guidance-on-frailty-update-sept-2017.pdf (2017, accessed 1 March 2018).