This review article discusses preclinical and clinical evidence for EGFR tyrosine kinase inhibitors in the treatment of central nervous system metastases, within the context of current treatment options.
Keywords: Brain metastases, Leptomeningeal metastases, Central nervous system metastases, Non‐small cell lung cancer, Epidermal growth factor receptor tyrosine kinase inhibitors
Abstract
Central nervous system (CNS) metastases are a common complication in patients with epidermal growth factor receptor (EGFR)‐mutated non‐small cell lung cancer (NSCLC), resulting in a poor prognosis and limited treatment options. Treatment of CNS metastases requires a multidisciplinary approach, and the optimal treatment options and sequence of therapies are yet to be established. Many systemic therapies have poor efficacy in the CNS due to the challenges of crossing the blood‐brain barrier (BBB), creating a major unmet need for the development of agents with good BBB‐penetrating biopharmaceutical properties. Although the CNS penetration of first‐ and second‐generation EGFR tyrosine kinase inhibitors (TKIs) is generally low, EGFR‐TKI treatment has been shown to delay time to CNS progression in patients with CNS metastases from EGFR‐mutated disease. However, a major challenge with EGFR‐TKI treatment for patients with NSCLC is the development of acquired resistance, which occurs in most patients treated with a first‐line EGFR‐TKI. Novel EGFR‐TKIs, such as osimertinib, have been specifically designed to address the challenges of acquired resistance and poor BBB permeability and have demonstrated efficacy in the CNS. A rational, iterative drug development process to design agents that could penetrate the BBB could prevent morbidity and mortality associated with CNS disease progression. To ensure a consistent approach to evaluating CNS efficacy, special consideration also needs to be given to clinical trial endpoints.
Implications for Practice.
Historically, treatment options for patients who develop central nervous system (CNS) metastases have been limited and associated with poor outcomes. The development of epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) has improved outcomes for patients with EGFR‐mutated disease, and emerging data have demonstrated the ability of these drugs to cross the blood‐brain barrier and elicit significant intracranial responses. Recent studies have indicated a role for next‐generation EGFR‐TKIs, such as osimertinib, in the treatment of CNS metastases. In the context of an evolving treatment paradigm, treatment should be individualized to the patient and requires a multidisciplinary approach.
摘要
在患有表皮生长因子受体(EGFR)突变的非小细胞肺癌(NSCLC)患者中,中枢神经系统(CNS)转移是常见的并发症,可致预后不良并且治疗方案有限。CNS转移的治疗需要多学科方法,而最佳的治疗方案和治疗顺序还有待确定。由于存在穿越血脑屏障(BBB)的挑战,许多全身性治疗在CNS中疗效不佳,导致具有良好BBB穿透性生物制药的开发工作,远远未能满足人们的需求。虽然第一代和第二代EGFR酪氨酸激酶抑制剂(TKIs)的CNS渗透率普遍较低,但EGFR‐TKI治疗已显示延缓了EGFR突变的CNS转移患者的CNS进展。然而,获得性耐药是EGFR‐TKI治疗NSCLC患者的一个主要挑战,大多数接受一线EGFR‐TKI治疗的患者都存在这个问题。新的EGFR‐TKI(如Osimertinib)是专门用来解决获得性抗药性和BBB通透性差的难题,并在CNS中显示了疗效。一个可以穿透BBB的合理迭代的药物开发过程,可以防止CNS疾病进展相关的病损率和死亡率。为了确保评估CNS疗效的一致性,还需要特别考虑临床试验终点。
实践意义
一直以来,向出现中枢神经系统(CNS)转移的患者提供的治疗方案很有限,并且与不良预后相关。表皮生长因子受体(EGFR)酪氨酸激酶抑制剂(TKIs)的发展改善了EGFR突变患者的预后。已经开始有数据显示,这些药物能够跨越血脑屏障,并引起明显的颅内缓解。最近研究表明,新一代EGFR‐TKI(如osimertinib)在治疗CNS转移中起着重要作用。在不断发展的治疗模式中,治疗应针对患者实现个体化,并需要采取多学科方法。
Introduction
Central nervous system (CNS) metastases are common in patients with advanced non‐small cell lung cancer (NSCLC), with a higher incidence observed in patients with epidermal growth factor receptor (EGFR)‐mutated NSCLC, compared with patients with EGFR‐wild type disease, even when adjusted for differences in survival [1], [2]. In patients with EGFR‐mutated disease, the prevalence of brain metastases at first diagnosis is approximately 25%, increasing to around 40% of patients 2 years after diagnosis [3], [4]. Leptomeningeal metastases (LM), the spread of tumor cells into the cerebrospinal fluid (CSF) and the leptomeninges, occur in 9%–15% of patients with EGFR‐mutated disease [2], [5]. Concurrent brain metastases are common, with up 82% of patients with LM experiencing prior or current brain metastases [6], [7]. Brain metastases are associated with a significantly poorer prognosis [8], [9], and the median overall survival (OS) time for patients with LM is just 3.6–4.5 months, despite multimodality treatment [10], [11].
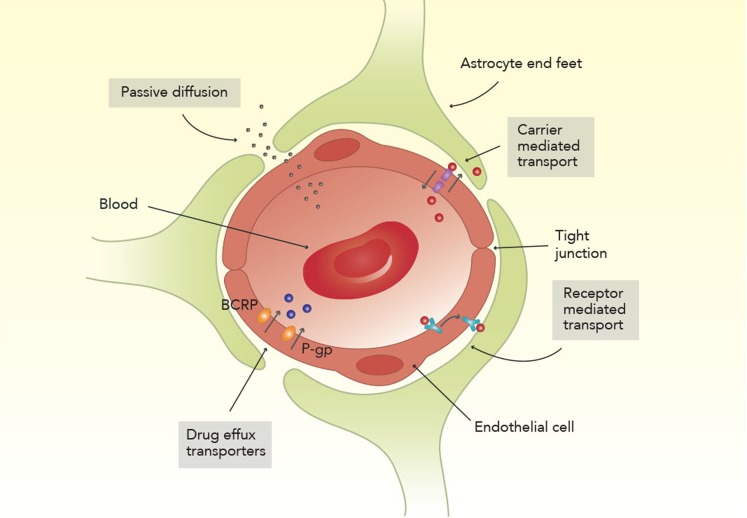
The treatment of CNS metastases is particularly challenging given the limited passage of molecules across the blood‐CSF barrier and blood‐brain barrier (BBB; Fig. 1). Many modern therapeutic agents, including most chemotherapies, are large hydrophilic molecules that are unable to cross the BBB [12], [13]. As such, systemic therapies tend to be ineffective against brain metastases, with response rates for chemotherapy ranging from 15% to 30% [13]. However, for patients with EGFR‐mutated disease, small molecule EGFR tyrosine kinase inhibitors (TKIs) have the potential to elicit CNS responses. This review aims to discuss preclinical and clinical evidence for EGFR‐TKIs in the treatment of CNS metastases, within the context of current treatment options.
Figure 1.
Passage of molecules across the blood‐brain barrier. Endothelial cell tight junctions provide a structural barrier between the blood and the brain. Only small lipophilic molecules with a molecular weight of <400 Da can gain entry to the brain via passive diffusion; the passage of other larger molecules is carrier‐ or receptor mediated [12]. The drug efflux transporter proteins BCRP and P‐gp further restrict the access of therapeutic molecules to the brain by actively transporting them back into circulation [129], [130].
Abbreviations: BCRP, breast cancer‐resistance protein; Da, Dalton; P‐gp, permeability glycoprotein.
Nontargeted Treatment Options for CNS Metastases
In the National Comprehensive Cancer Network (NCCN) Guidelines for NSCLC, recommended options for patients with fewer than three brain metastases include (a) stereotactic radiosurgery (SRS) or (b) surgical resection (if symptomatic or needed for diagnosis) followed by SRS or whole‐brain radiotherapy (WBRT) [14]. Although surgical resection was long considered the standard of care for solitary brain metastasis, SRS is equally as effective in extending patient survival [15]. Factors affecting the choice of surgery versus SRS include tumor size and location, systemic disease status, and the need for relief from symptomatic mass effect or edema [16]. SRS has been shown to be equally as effective in patients with 5–10 brain metastases, compared with patients with 2–4 brain metastases, indicating that SRS is also suitable for patients with extensive brain metastases [17]. However, although SRS provides a high local tumor control rate (84%–93%) [18], [19], it does not provide distant brain control [18], [20].
Traditionally, the NCCN Guidelines for NSCLC have recommended WBRT to target multiple metastases and prevent distant brain failure [21]; however, as extended survival is possible for patients with EGFR‐mutated disease, the treatment‐related toxicities associated with WBRT are of concern. Acute adverse effects, such as nausea and headache, are typically self‐limiting. However, late adverse effects (occurring months or years after treatment) such as neurocognitive decline, leukoencephalopathy, and radiation necrosis are irreversible and may have severe consequences [22], [23]. Results from a recent phase III trial indicate that the addition of WBRT to optimal supportive care does not significantly improve survival or quality of life for patients with brain metastases from NSCLC [24]. However, this study was not specific to patients with EGFR‐mutated disease, in whom the risk‐benefit assessment may differ due to improved systemic prognosis. In line with these results, the NCCN Guidelines for NSCLC have revised recommendations for the treatment of brain metastases by decreasing recommendations for WBRT [14].
There is a lack of standard treatments for patients with LM, from any type of primary cancer, due to insufficient evidence in the literature [25]. The NCCN Guidelines for CNS cancers recommend that patients with LM, from any primary cancer, be stratified into poor‐risk and good‐risk groups. The recommended treatment for patients in the poor‐risk group is palliative/best supportive care and to consider radiotherapy to symptomatic or painful sites for palliation. For patients in the good‐risk group, radiotherapy to bulky disease or symptomatic sites is recommended; a CSF flow scan is strongly recommended to direct further treatment. Depending on the results of CSF flow scans and CSF cytology, further treatment options include intra‐CSF chemotherapy, radiotherapy, and systemic chemotherapy [25].
EGFR‐TKIs
EGFR‐TKIs have a low molecular weight and the potential to cross the BBB more readily than most intravenous chemotherapies. However, first‐ and second‐generation EGFR‐TKIs generally have poor biopharmaceutical properties for BBB penetration due to their affinity for efflux transport proteins such as the adenosine triphosphate‐binding cassette subfamily members B1 and G2 (ABCB1 and ABCG2), hereafter referred to as permeability glycoprotein (P‐gp) and breast cancer‐resistance protein (BCRP), respectively [26], [27], [28] (Fig. 1). Preclinical studies have shown that uptake of EGFR‐TKIs in the brain is low because they do not readily cross the BBB [29], [30]. The CSF penetration of first‐ and second‐generation EGFR‐TKIs is generally low, with average CSF penetration rates of <1%, 1%–3%, and 3%–6% reported for afatinib, gefitinib, and erlotinib, respectively [31], [32], [33], [34]. The CSF penetration of gefitinib is enhanced in patients with brain metastases, compared with patients without brain metastases, potentially due to tumor‐induced BBB disruption [35], [36], raising the question of whether small asymptomatic brain metastases could be treated with an EGFR‐TKI alone. The effect of WBRT on the BBB permeability of EGFR‐TKIs is unclear, with one study reporting an increase in the CSF:plasma ratio of gefitinib following WBRT [35] and another reporting no difference [33].
Despite preclinical data suggesting poor BBB penetrance, EGFR‐TKIs have demonstrated systemic efficacy and CNS activity in patients with brain metastases. In a meta‐analysis of eight clinical studies, EGFR‐TKIs in combination with SRS or WBRT were found to significantly improve objective response rate (ORR), time to CNS progression, and median OS, compared with radiotherapy without EGFR‐TKIs [37]. One phase II study of EGFR‐TKIs for brain metastases reported a systemic ORR of 83%; however, there was a high rate of intracranial disease progression. Of those patients experiencing disease progression, 62% progressed in intracranial lesions only and 19% in both intracranial and extracranial lesions [38]. However, compared with chemotherapy, EGFR‐TKIs are associated with a lower risk of progression in the CNS [39]. EGFR‐TKIs have shown promise in the treatment of LM, with retrospective studies indicating that EGFR‐TKIs can improve survival [2], [10]. An intermittent high dose, known as pulsatile dosing, has been trialed in an attempt to increase EGFR‐TKI concentrations in the CSF and has shown promise in treating patients with CNS metastases that are refractory to treatment with standard‐dose EGFR‐TKIs [40].
A major challenge with EGFR‐TKI treatment is the development of acquired resistance, which occurs in most patients treated with a first‐line first‐ or second‐generation EGFR‐TKI (i.e., gefitinib, erlotinib, afatinib) [41], [42], [43]. Although several mechanisms of resistance to EGFR‐TKI therapy have been identified, in more than 50% of cases, resistance is attributable to the EGFR T790M mutation [44], [45], [46], [47]. However, research conducted using paired biopsies indicates that the distribution of T790M is spatially heterogeneous, with a lower frequency in the CNS compared with thoracic lesions [48], [49]. The comparative rarity of T790M in the CNS may be due to the relatively poor CNS penetration of EGFR‐TKIs [49]. Evidence suggests that mechanisms of resistance in CNS metastases may differ compared with those outside of the CNS [50], [51].
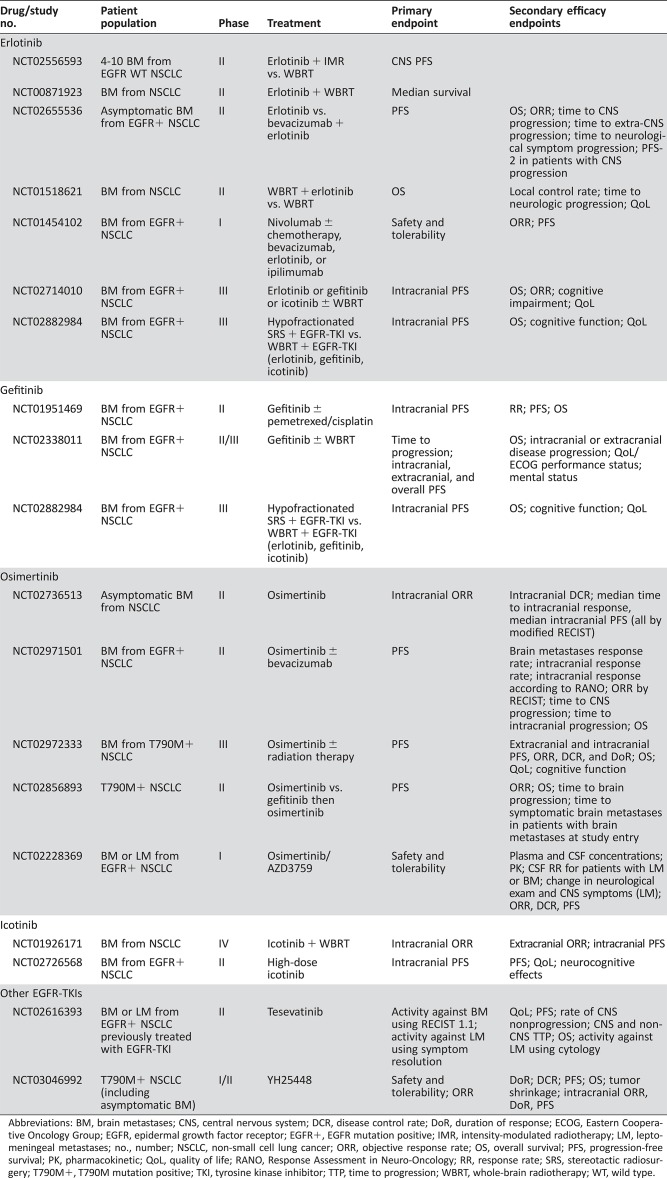
In recent years, novel EGFR‐TKIs, such as osimertinib and AZD3759, have been developed to address the challenges of acquired resistance and poor CNS penetration, respectively, that are experienced with first‐ and second‐generation EGFR‐TKIs [52], [53], [54]. A summary of ongoing clinical trials of EGFR‐TKIs for patients with CNS metastases from NSCLC is listed in Table 1. In the following sections, we discuss evidence for individual EGFR‐TKIs in CNS metastases.
Table 1. Ongoing clinical trials of EGFR‐TKIs for patients with CNS metastases from NSCLC.
Abbreviations: BM, brain metastases; CNS, central nervous system; DCR, disease control rate; DoR, duration of response; ECOG, Eastern Cooperative Oncology Group; EGFR, epidermal growth factor receptor; EGFR+, EGFR mutation positive; IMR, intensity‐modulated radiotherapy; LM, leptomeningeal metastases; no., number; NSCLC, non‐small cell lung cancer; ORR, objective response rate; OS, overall survival; PFS, progression‐free survival; PK, pharmacokinetic; QoL, quality of life; RANO, Response Assessment in Neuro‐Oncology; RR, response rate; SRS, stereotactic radiosurgery; T790M+, T790M mutation positive; TKI, tyrosine kinase inhibitor; TTP, time to progression; WBRT, whole‐brain radiotherapy; WT, wild type.
Gefitinib
Gefitinib is the first EGFR‐TKI to be approved for the treatment of NSCLC, with initial approval granted for third‐line treatment of patients with advanced NSCLC, irrespective of EGFR‐mutation status, and subsequent approvals for first‐line treatment of patients with advanced EGFR‐mutated disease [28], [55], [56]. Preclinical data show that the distribution of [14C]gefitinib in the CNS of nontumor‐bearing mice (AstraZeneca, data on file) and pigmented rats is low [30]. [11C]gefitinib also demonstrated low penetration in the nonhuman primate brain under positron emission tomography (PET) microdosing conditions [30], deemed robust methodology for predicting brain exposure [57]. In in vitro assays and a murine NSCLC brain metastases model, the CNS permeability and efflux ratio of gefitinib increased in a dose‐dependent manner. However, gefitinib is a substrate for P‐gp and, even at the highest dose tested (200 mg/kg), had limited BBB penetration [58]. Gefitinib has been shown to inhibit P‐gp in multidrug‐resistant lung cancer cells, suggesting it may be able to partially overcome this mechanism of drug resistance [59].
Despite its poor CNS penetration properties, preclinical studies have shown that gefitinib has CNS activity. In mice with EGFR overexpressing intracranial tumors, gefitinib treatment prolonged median survival, compared with no treatment (34 and 18 days, respectively) [29]. Durable responses to gefitinib have been reported in a case series of patients with brain metastases from EGFR‐mutated NSCLC [60]. In a phase II study (n = 41), intracranial ORR with gefitinib was 88%, with 13 patients (32%) experiencing a complete response (CR) [61]. The median time to CNS progression was 14.5 months, with an OS of 21.9 months; however, salvage radiotherapy was required in 49% of patients.
Erlotinib
Erlotinib is a first‐generation EGFR‐TKI recommended as an option for first‐line treatment of advanced EGFR‐mutated NSCLC [14]. As with gefitinib, preclinical studies have demonstrated that erlotinib exposure in the brain is limited [62]. The primary efflux mechanism for erlotinib has been identified as BCRP, with P‐gp having little effect [63]. Although erlotinib penetration of the BBB is normally limited, one case study reports increased accumulation of [11C]erlotinib in brain lesions, compared with the cerebral cortex, of a patient with both brain metastases and LM from NSCLC [64]. Near complete remission of the patient's CNS metastases was achieved within 3 weeks of treatment initiation [64]. It is possible that, in some cases, tumor‐induced disruption of the BBB may allow for increased erlotinib penetration. In a retrospective analysis of 17 patients with brain metastases from EGFR‐mutated NSCLC treated with erlotinib, CNS ORR was 82% and median time to CNS progression was 11.7 months [65]. Of eight patients who did not receive WBRT and were treated with erlotinib alone, six (75%) had objective responses (four CR, two partial responses).
Several case series have reported promising efficacy with high‐dose erlotinib for the treatment of CNS metastases (including LM) refractory to EGFR‐TKIs administered at conventional doses [40], [66], [67]. In a retrospective analysis of nine patients with CNS metastases from EGFR‐mutated NSCLC treated with high‐dose erlotinib (900–1500 mg weekly), six (67%) patients had a partial radiographic response. Median time to CNS progression was 2.7 months and OS was 12 months after initiation of high‐dose erlotinib [40]. Another small case series reported radiographic responses in four of five (80%) evaluable patients treated with high‐dose erlotinib, with one patient showing a CR of both brain metastases and LM [66]. Excluding a patient with prolonged survival who received combination therapy, median OS was 4 months (range 2.5–15 months). The efficacy of high‐dose erlotinib in patients with LM is further discussed in the leptomeningeal metastases section.
Afatinib
Afatinib is a second‐generation EGFR‐TKI and was approved as first‐line treatment for EGFR‐mutated advanced NSCLC in the U.S. in 2013. Preclinical studies of afatinib have shown that exposure in the brain is low, with a brain:plasma maximum observed plasma concentration (Cmax) ratio of <0.36 for a clinically relevant dose of afatinib [30]. However, afatinib has been shown to penetrate the BBB in a murine model of brain metastases from NSCLC and, despite low CNS exposure, cause intracranial tumor regression [68].
The overall response to afatinib in patients with brain metastases has been assessed in subset analyses of phase II and phase III trials. In the phase II LUX‐Lung 2 trial, the ORR was similar between patients with and without brain metastases (65% vs. 60%) [69]. A subgroup analysis of patients with brain metastases included in the phase III LUX‐Lung 3 and LUX‐Lung 6 trials revealed significant improvements in systemic ORR for patients treated with afatinib compared with chemotherapy (70% vs. 20% and 75% vs. 28%, respectively) [70]. The intracranial response rate was not assessed in either study. In an exploratory combined analysis of both studies, progression‐free survival (PFS) was longer with afatinib than with chemotherapy (8.2 vs. 5.4 months; hazard ratio [HR] 0.50; 95% confidence interval [CI] 0.27–0.95; p = .0297). The PFS benefit with afatinib was found to be higher in those patients who received prior WBRT (13.8 vs. 4.7 months) compared with patients who did not (6.9 vs. 5.4 months) [70]. Further studies are required to establish the CNS efficacy of afatinib.
Icotinib
Icotinib is a novel EGFR‐TKI approved for the second‐ or third‐line treatment of advanced NSCLC by the State Food and Drug Administration of the People's Republic of China [71]. Preclinical data on the ability of icotinib to cross the BBB are lacking; however, CSF penetration in patients with brain metastases from NSCLC has been reported as 1.2%–9.7% across three different dose levels (125–500 mg), with a significant correlation between icotinib concentration in the CSF and plasma [72]. WBRT was found to not impact the CSF penetration of icotinib. In a phase III trial (n = 176), icotinib demonstrated superior efficacy over WBRT and chemotherapy for patients with brain metastases from EGFR‐mutated NSCLC [73]. Intracranial PFS was 10 months with icotinib versus 4.8 months with WBRT plus chemotherapy (HR 0.56; 95% CI 0.36–0.90; p = .014). Intracranial ORR was also significantly improved with icotinib, compared with WBRT and chemotherapy (65% vs. 37%, respectively; p = .001), although there was no difference in OS (18 vs. 20.5 months; p = .734).
Osimertinib
Osimertinib is a potent, CNS‐active, irreversible EGFR‐TKI selective for EGFR‐TKI‐sensitizing mutations and the EGFR T790M resistance mutation [30], [52], [74], [75]. Osimertinib initially gained U.S. Food and Drug Administration approval based on a pooled analysis of two phase II studies (AURA extension and AURA2) demonstrating a response rate of 66% in patients with EGFR T790M mutations who were refractory to EGFR‐TKI treatment [76], [77]. Osimertinib is now recommended in the NCCN Guidelines for NSCLC as first‐line treatment for patients with EGFR‐mutated NSCLC and as second‐line treatment for patients with T790M‐positive disease following progression on erlotinib, gefitinib, or afatinib [14]. Preclinical development of osimertinib specifically focused on the assessment of brain penetration and CNS activity. Despite being a substrate of the efflux transporters P‐gp and BCRP, osimertinib is more highly distributed than gefitinib, rociletinib, and afatinib in the mouse brain, with a brain:plasma Cmax ratio of 3.41 versus 0.21, <0.08 and <0.36, respectively [30]. Osimertinib is also highly distributed in the nonhuman primate brain, with greater exposure than rociletinib and gefitinib [30].
In the phase III AURA3 trial, osimertinib demonstrated significantly greater systemic efficacy than chemotherapy in patients with T790M‐positive NSCLC, including those patients with CNS metastases [78]. In a prespecified subgroup analysis, CNS ORR in patients with measurable CNS lesions (n = 46) was 70% with osimertinib, compared with 31% with chemotherapy (p = .015). In patients with measurable and/or nonmeasurable CNS lesions (n = 116), median CNS PFS was significantly longer with osimertinib compared with chemotherapy (11.7 vs. 5.6 months; HR 0.32; 95% CI 0.15–0.69; p = .004) [79]. The recent FLAURA study compared osimertinib with standard‐of‐care EGFR‐TKI (erlotinib or gefitinib) as first‐line therapy in patients with advanced EGFR‐mutated NSCLC; treatment with osimertinib resulted in significantly longer systemic PFS across all predefined subgroups, including those patients with known or treated CNS metastases (median 15.2 vs. 9.6 months; HR 0.47; 95% CI 0.30–0.74; p < .001) [80]. There was a lower incidence of CNS progression events with osimertinib versus standard of care (6% vs. 15%), irrespective of presence or absence of known or treated CNS metastases at study entry. In a subgroup analysis of patients with CNS metastases at baseline, as assessed by neuroradiological blinded independent central review, there was a 52% reduction in the risk of CNS progression with osimertinib (HR 0.48; 95% CI 0.26–0.86; p = .014 [nominally statistically significant]), confirming that osimertinib is superior to erlotinib and gefitinib in the control of CNS metastases [81].
In a subgroup analysis of patients with CNS metastases at baseline, as assessed by neuroradiological blinded independent central review, there was a 52% reduction in the risk of CNS progression with osimertinib, confirming that osimertinib is superior to erlotinib and gefitinib in the control of CNS metastases.
AZD3759
AZD3759 represents a novel class of EGFR‐TKI, which is not a substrate of the efflux transporters P‐gp or BCRP. This compound, which was specifically developed to achieve high exposure both in the plasma and in the CNS by penetrating the BBB, is under investigation for the treatment of CNS metastases from NSCLC [54], [82], [83]. AZD3759 has an unbound brain exposure:unbound plasma ratio of 0.86, indicating similar free exposure in the brain and plasma [83]. In a mouse PC‐9 (EGFR exon 19 deletion) xenograft brain metastases model, AZD3759 induced profound tumor regression and significantly improved survival [53], [82]. The efficacy of AZD3759 in patients with CNS metastases is currently being evaluated in the ongoing phase I BLOOM study (NCT02228369). In an EGFR‐TKI‐naïve cohort, intracranial ORR was 63% (12 of 19 evaluable patients) and systemic ORR 60% (12 of 20 evaluable patients) [84].
Leptomeningeal Disease
The NCCN Guidelines for NSCLC recommend osimertinib (regardless of T790M status) or weekly pulse erlotinib for patients with EGFR‐mutated NSCLC and progressive LM [14]. Osimertinib has shown promising activity in patients with LM, with a number of case studies reporting the efficacy of osimertinib 80 mg once daily for treating patients with refractory LM following prior treatment with EGFR‐TKIs, chemotherapy, SRS, and WBRT [85], [86], [87], [88], [89]. The efficacy of osimertinib 160 mg once daily for patients with heavily pretreated LM is also being assessed in the phase I BLOOM study. In an interim analysis of 23 patients who reached a 12‐week brain imaging assessment, 10 patients had radiological improvement and 13 had stable disease [90]. The efficacy of AZD3759 is being investigated in the same study; in the EGFR‐TKI pretreated cohort, 53% of 17 evaluable patients had confirmed improved or stable LM on radiographic assessment, and two of three patients with concomitant measurable brain metastases achieved confirmed/unconfirmed partial CNS response [91].
Both high‐dose erlotinib and gefitinib have shown promise in treating LM. In a phase II study of erlotinib for patients with LM (n = 21), 35% of 17 patients with EGFR‐mutated disease achieved complete CSF cytological clearance. Median time to LM progression and OS were 2.7 and 4 months, respectively [92]. In a small phase I trial (n = 7) of high‐dose gefitinib (750 mg or 1,000 mg daily) for 2 weeks, followed by 2 weeks of maintenance therapy (500 mg daily), no patients showed radiological improvement. However, four patients had neurological improvement and one had complete CSF cytological clearance. Median PFS and OS were 2.3 and 3.5 months, respectively [93].
Several small studies suggest that erlotinib may be more effective than gefitinib for the treatment of patients with LM [32], [94], [95], and, in a retrospective review of 22 patients who received erlotinib (n = 17) or gefitinib (n = 5) for the treatment of LM from EGFR‐mutated NSCLC, median PFS was longer in patients treated with erlotinib compared with gefitinib (6.6 vs. 2.1 months; p = .07). Median OS with erlotinib was more than double the OS achieved with gefitinib (7.2 vs. 3.0 months; p = .32) [95]. Case studies also suggest that erlotinib may have value in treating patients who have LM progression with gefitinib [34], [96].
There is limited evidence for the efficacy of other EGFR‐TKIs for the treatment of LM. Evidence for the efficacy of afatinib in LM is limited to case reports, which have described successful treatment of LM [97], [98], [99], [100]. In a retrospective review of standard‐ or double‐dose icotinib for LM from NSCLC, 81% of 21 patients had improved Eastern Cooperative Oncology Group performance status, and median OS was 10.1 months [101]. However, as this was a small retrospective study, and patients received additional therapies for the treatment of LM, further studies are required to confirm the potential benefit of icotinib in this setting.
Treating CNS Metastases: Challenges and Future Directions
Clinical Trial Endpoints
The selection of the most appropriate endpoints for clinical trials in patients with CNS metastases is challenging, given the need to account for both CNS and systemic disease. OS may not be an optimal endpoint, as death due to systemic disease progression, despite stable CNS disease, is common [102], [103]. If PFS is used as an endpoint, a clear distinction between CNS, non‐CNS, and systemic PFS should be made. However, an accurate assessment of intracranial PFS can be difficult to achieve after SRS, as radionecrosis can resemble disease recurrence [102]. Furthermore, if systemic disease progression occurs, assessments of CNS progression often ceases, censoring CNS or overall PFS results. As an alternative approach, some studies have employed neurocognitive outcomes as a primary endpoint [104].
RECIST World Health Organization tumor response criteria, and Response Assessment in Neuro‐Oncology (RANO) are commonly used in clinical trials to measure response to treatment. However, patients with CNS metastases have traditionally been excluded from clinical trials, and, when included, there has been a lack of standardization of response assessment [105], [106]. The previously mentioned criteria were not designed to assess CNS response and, therefore, have major limitations in this setting. In particular, unstandardized neuroimaging criteria and nonspecific shrinkage measurements make it difficult to determine a uniformly measured response that can be robustly compared across clinical trials [102]. To address these limitations, additional, specific RANO criteria have been proposed [107]. The RANO criteria for the assessment of brain metastases takes radiographic responses, corticosteroid use, and clinical status into account for response assessment [106]. It is hoped that these criteria will facilitate the development of novel, consistent approaches for the evaluation of CNS metastases.
Traditional efficacy endpoints are challenging to apply in clinical trials of LM as cause of death is usually difficult to determine and patients often have simultaneous progression of both CNS and systemic disease. Consequently, the most suitable endpoint to evaluate treatment efficacy in this population may be time to neurological disease progression.
Traditional efficacy endpoints are challenging to apply in clinical trials of LM as cause of death is usually difficult to determine and patients often have simultaneous progression of both CNS and systemic disease. Consequently, the most suitable endpoint to evaluate treatment efficacy in this population may be time to neurological disease progression [108]. There is currently no validated quantitative radiographic method to assess LM. False‐negative results are common with CSF cytology analysis [109] and neuroimaging [110], [111], making response difficult to determine in these patients. In addition, the absence of a uniform approach to treatment decisions makes the determination of suitable candidates for LM trials difficult. There has been a lack of standardization in clinical trials for LM, with heterogeneity in trial endpoints and response assessments [108]. To address these challenges, the RANO LM working group have developed a consensus proposal for LM response assessment, with the aim of standardizing neurological, CSF cytology, and radiographic assessments [112]. These novel response criteria have not yet been validated and may require further refinement.
Treatment Sequence
The results of the recent FLAURA study, which demonstrate osimertinib's superiority over erlotinib and gefitinib in the first‐line setting [80], raise the question of optimal EGFR‐TKI sequencing. If reserved for those patients with disease progression following first‐line EGFR‐TKIs, osimertinib may extend PFS and offer patients another line of treatment. However, the superior CNS control with osimertinib, and potential to prevent the development of CNS metastases, support its up‐front use. Furthermore, reserving osimertinib for second‐line treatment may limit the patient population that can provide a benefit from this agent. Although more than 50% of patients will have T790M‐positive tumors on progression [44], [45], [46], [47], some may not be suitable for rebiopsy [113] or second‐line therapy. Previous clinical trial reports suggest that as many as 20%–50% of patients with EGFR‐mutated NSCLC do not receive any poststudy treatment after discontinuation, due to aggressive disease progression [114], [115], [116].
The optimal treatment sequence for patients with CNS metastases from EGFR‐mutated NSCLC is not clear. In a retrospective analysis of patients who developed brain metastases before initiating therapy with an EGFR‐TKI (erlotinib in 98% of patients), SRS followed by EGFR‐TKI was associated with a greater OS than WBRT followed by EGFR‐TKI (median 47 vs. 31 months) [117]. However, the use of an up‐front EGFR‐TKI, and deferral of SRS or WBRT, was associated with an inferior OS (median 25 months). To confirm these findings, a prospective randomized trial of SRS followed by EGFR‐TKI, compared with EGFR‐TKI followed by SRS at CNS progression, is needed. Concurrent WBRT and EGFR‐TKI treatment has been shown to be effective in phase II trials of erlotinib, gefitinib, and icotinib for the treatment of brain metastases from NSCLC, with an acceptable tolerability profile. In a phase II trial (n = 21) of gefitinib administered concurrently with WBRT, intracranial ORR was 81% in patients with measurable lesions; median PFS and OS were 10 and 13 months, respectively [118]. Erlotinib administered concurrently with WBRT has demonstrated a CNS ORR of 86% and a median CNS PFS of 8 months in a phase II study (n = 40). For patients with EGFR‐mutated disease, median survival time was 19.1 months [119]. In a study of icotinib plus WBRT (n = 20), intracranial ORR was 80%. Median PFS and OS for patients with EGFR‐mutated disease were 12 and 22 months, respectively [120]. However, given the limitations of WBRT, further research is needed to assess whether the addition of WBRT to EGFR‐TKI treatment improves outcomes, compared with EGFR‐TKI alone for patients with CNS metastases from EGFR‐mutated disease.
Novel Diagnostic Approaches to Assess BBB Penetrance
EGFR‐TKIs with improved BBB‐penetrating properties could have benefits in both treating and preventing CNS metastases [121]; however, developing drugs with good BBB‐penetrating properties and accessing the CNS sanctuary site remains a challenge. Radiolabeling EGFR‐TKIs for PET microdosing studies provides an opportunity to evaluate BBB penetration and brain exposure. To date, this approach has been limited to the preclinical assessment of EGFR‐TKIs [30], [62]. However, such studies can also be performed in healthy volunteers and patients with brain metastases from NSCLC, in whom the BBB may be compromised. Although the tracer doses used in PET microdosing studies do not reflect the brain exposure of therapeutic doses, the utility of this approach for assessing BBB penetration and brain distribution in humans has been established using sertraline [122].
Conclusion
Despite the challenge of BBB penetration, initial CNS responses in treatment‐naïve patients are common following treatment with EGFR‐TKIs alone. Novel EGFR‐TKIs developed to improve CNS penetration, such as osimertinib, show encouraging efficacy in controlling CNS disease, and personalized biomarker‐driven treatment strategies will continue to maximize benefit to individual patients [78], [123], [124], [125], [126], [127], [128]. Although recent studies suggest that deferring radiotherapy may be associated with comparatively inferior survival, combined treatment approaches have demonstrated efficacy and an adequate safety profile. Therefore, the treatment of CNS metastases from EGFR‐mutant NSCLC requires a multidisciplinary approach to define optimal treatment options or sequence of therapies for individual patients. Given the evolving treatment paradigm for these patients, treatment decisions must be individualized, factoring in the patient's performance status, CNS disease burden, and clinical symptoms in the context of a critical risk‐benefit analysis. Looking to the future, clinical trial endpoints need to clearly differentiate between CNS and systemic disease progression, be tailored to the trial setting, type of therapy under investigation, patient population, and EGFR‐mutation status, and be used consistently across studies. The use of a rational, iterative approach to the drug development process allows the design of agents with the intention of overcoming the BBB and holds promise for preventing morbidity and mortality attributable to CNS disease progression.
Acknowledgments
We acknowledge Rosalie Richards, Ph.D., and Rebecca Plant, M.Sc., of iMed Comms, Macclesfield, an Ashfield Company, part of UDG Healthcare plc, for medical writing support that was funded by AstraZeneca, U.K., in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Footnotes
For Further Reading: Melin J. Khandekar, Zofia Piotrowska, Henning Willers et al. Role of Epidermal Growth Factor Receptor (EGFR) Inhibitors and Radiation in the Management of Brain Metastases from EGFR Mutant Lung Cancers. The Oncologist 2018;23:1054–1062; first published on April 27, 2018.
Implications for Practice: Management of brain metastases in epidermal growth factor receptor (EGFR) mutant lung cancer is a common clinical problem. The question of whether to start initial therapy with an EGFR inhibitor or radiotherapy (either whole‐brain radiotherapy or stereotactic radiosurgery) is controversial. The development of novel EGFR inhibitors with enhanced central nervous system (CNS) penetration is an important advance in the treatment of CNS disease. Multidisciplinary evaluation and evaluation of extracranial disease status are critical to choosing the best treatment option for each patient.
Author Contributions
Conception/design: Manmeet S. Ahluwalia, Kevin Becker, Benjamin P. Levy
Collection and/or assembly of data: Manmeet S. Ahluwalia, Kevin Becker, Benjamin P. Levy
Data analysis and interpretation: Manmeet S. Ahluwalia, Kevin Becker, Benjamin P. Levy
Manuscript writing: Manmeet S. Ahluwalia, Kevin Becker, Benjamin P. Levy
Final approval of manuscript: Manmeet S. Ahluwalia, Kevin Becker, Benjamin P. Levy
Disclosures
Manmeet S. Ahluwalia: Monteris Medical, AstraZeneca, Bristol‐Myers Squibb, CBT Pharmaceuticals, Kadmon Pharmaceuticals, Abbvie, VBI Vaccines (C/A), AstraZeneca, Bristol‐Myers Squibb, Novocure, Novartis, Incyte, Abbvie, Pharmacylics (RF), Elsevier, Prime Oncology (H); Kevin Becker: AstraZeneca (C/A), Genentech/Roche, Bristol‐Myers Squibb (RF); Benjamin P. Levy: AstraZeneca, Eli Lilly, Roche (C/A).
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1. Hsu F, De Caluwe A, Anderson D et al. EGFR mutation status on brain metastases from non‐small cell lung cancer. Lung Cancer 2016;96:101–107. [DOI] [PubMed] [Google Scholar]
- 2. Li YS, Jiang BY, Yang JJ et al. Leptomeningeal metastases in patients with NSCLC with EGFR mutations. J Thorac Oncol 2016;11:1962–1969. [DOI] [PubMed] [Google Scholar]
- 3. Rangachari D, Yamaguchi N, VanderLaan PA et al. Brain metastases in patients with EGFR‐mutated or ALK‐rearranged non‐small‐cell lung cancers. Lung Cancer 2015;88:108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hendriks LE, Smit EF, Vosse BA et al. EGFR mutated non‐small cell lung cancer patients: More prone to development of bone and brain metastases? Lung Cancer 2014;84:86–91. [DOI] [PubMed] [Google Scholar]
- 5. Lee Y, Han JY, Kim HT et al. Impact of EGFR tyrosine kinase inhibitors versus chemotherapy on the development of leptomeningeal metastasis in never smokers with advanced adenocarcinoma of the lung. J Neurooncol 2013;115:95–101. [DOI] [PubMed] [Google Scholar]
- 6. Lee SJ, Lee JI, Nam DH et al. Leptomeningeal carcinomatosis in non‐small‐cell lung cancer patients: Impact on survival and correlated prognostic factors. J Thorac Oncol 2013;8:185–191. [DOI] [PubMed] [Google Scholar]
- 7. Morris PG, Reiner AS, Szenberg OR et al. Leptomeningeal metastasis from non‐small cell lung cancer: Survival and the impact of whole brain radiotherapy. J Thorac Oncol 2012;7:382–385. [DOI] [PubMed] [Google Scholar]
- 8. Bhatt VR, D'Souza SP, Smith LM et al. Epidermal growth factor receptor mutational status and brain metastases in non–small‐cell lung cancer. J Glob Oncol 2016;3:208–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sorensen JB, Hansen HH, Hansen M et al. Brain metastases in adenocarcinoma of the lung: Frequency, risk groups, and prognosis. J Clin Oncol 1988;6:1474–1480. [DOI] [PubMed] [Google Scholar]
- 10. Liao BC, Lee JH, Lin CC et al. Epidermal growth factor receptor tyrosine kinase inhibitors for non‐small‐cell lung cancer patients with leptomeningeal carcinomatosis. J Thorac Oncol 2015;10:1754–1761. [DOI] [PubMed] [Google Scholar]
- 11. Umemura S, Tsubouchi K, Yoshioka H et al. Clinical outcome in patients with leptomeningeal metastasis from non‐small cell lung cancer: Okayama Lung Cancer Study Group. Lung Cancer 2012;77:134–139. [DOI] [PubMed] [Google Scholar]
- 12. Pardridge WM. Drug transport across the blood‐brain barrier. J Cereb Blood Flow Metab 2012;32:1959–1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bartolotti M, Franceschi E, Brandes AA. EGF receptor tyrosine kinase inhibitors in the treatment of brain metastases from non‐small‐cell lung cancer. Expert Rev Anticancer Ther 2012;12:1429–1435. [DOI] [PubMed] [Google Scholar]
- 14.Referenced with permission from the NCCN Clinical Practice Guidelines In Oncology (NCCN Guidelines) for Non‐Small Cell Lung Cancer Version 1.2018. Accessed December 8, 2017. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. https://www.nccn.org/professionals/physician_gls/default.aspx#nscl
- 15. Qin H, Wang C, Jiang Y et al. Patients with single brain metastasis from non‐small cell lung cancer equally benefit from stereotactic radiosurgery and surgery: A systematic review. Med Sci Monit 2015;21:144–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mut M. Surgical treatment of brain metastasis: A review. Clin Neurol Neurosurg 2012;114:1–8. [DOI] [PubMed] [Google Scholar]
- 17. Yamamoto M, Serizawa T, Shuto T et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): A multi‐institutional prospective observational study. Lancet Oncol 2014;15:387–395. [DOI] [PubMed] [Google Scholar]
- 18. Xu Z, Elsharkawy M, Schlesinger D et al. Gamma knife radiosurgery for resectable brain metastasis. World Neurosurg 2013;80:351–358. [DOI] [PubMed] [Google Scholar]
- 19. Bowden G, Kano H, Caparosa E et al. Gamma knife radiosurgery for the management of cerebral metastases from non‐small cell lung cancer. J Neurosurg 2015;122:766–772. [DOI] [PubMed] [Google Scholar]
- 20. Johung KL, Yao X, Li F et al. A clinical model for identifying radiosensitive tumor genotypes in non‐small cell lung cancer. Clin Cancer Res 2013;19:5523–5532. [DOI] [PubMed] [Google Scholar]
- 21.Referenced with permission from the NCCN Clinical Practice Guidelines In Oncology (NCCN Guidelines) for Non‐Small Cell Lung Cancer Version 4.2017) Accessed December 8, 2017. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. https://www.nccn.org/professionals/physician_gls/default.aspx#nscl
- 22. McTyre E, Scott J, Chinnaiyan P. Whole brain radiotherapy for brain metastasis. Surg Neurol Int 2013;4:S236–S244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aoyama H, Tago M, Kato N et al. Neurocognitive function of patients with brain metastasis who received either whole brain radiotherapy plus stereotactic radiosurgery or radiosurgery alone. Int J Radiat Oncol Biol Phys 2007;68:1388–1395. [DOI] [PubMed] [Google Scholar]
- 24. Mulvenna P, Nankivell M, Barton R et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non‐small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): Results from a phase 3, non‐inferiority, randomised trial. Lancet 2016;388:2004–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Referenced with permission from the NCCN Clinical Practice Guidelines In Oncology (NCCN Guidelines) for Central Nervous System Cancer Version 1.2017. Accessed December 8, 2017. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. https://www.nccn.org/professionals/physician_gls/default.aspx#nscl
- 26.CHMP. Committee for Medicinal Products for Human Use (CHMP) assessment report for Giotrif (afatinib). European Medicines Agency 2013.
- 27. de Vries NA, Buckle T, Zhao J et al. Restricted brain penetration of the tyrosine kinase inhibitor erlotinib due to the drug transporters P‐gp and BCRP. Invest New Drugs 2012;30:443–449. [DOI] [PubMed] [Google Scholar]
- 28.EMA. Iressa Summary of Product Characteristics. 2009. Available at http://www.ema.europa.eu/ema/index.jsp%3Fcurl=pages/medicines/human/medicines/001016/human_med_000857.jsp%26murl=menus/medicines/index.jsp. Accessed August 30, 2017.
- 29. Heimberger AB, Learn CA, Archer GE et al. Brain tumors in mice are susceptible to blockade of epidermal growth factor receptor (EGFR) with the oral, specific, EGFR‐tyrosine kinase inhibitor ZD1839 (iressa). Clin Cancer Res 2002;8:3496–3502. [PubMed] [Google Scholar]
- 30. Ballard P, Yates JW, Yang Z et al. Preclinical comparison of osimertinib with other EGFR‐TKIs in EGFR‐mutant NSCLC brain metastases models, and early evidence of clinical brain metastases activity. Clin Cancer Res 2016;22:5130–5140. [DOI] [PubMed] [Google Scholar]
- 31. Hoffknecht P, Tufman A, Wehler T et al. Efficacy of the irreversible ErbB family blocker afatinib in epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI)‐pretreated non‐small‐cell lung cancer patients with brain metastases or leptomeningeal disease. J Thorac Oncol 2015;10:156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Togashi Y, Masago K, Masuda S et al. Cerebrospinal fluid concentration of gefitinib and erlotinib in patients with non‐small cell lung cancer. Cancer Chemother Pharmacol 2012;70:399–405. [DOI] [PubMed] [Google Scholar]
- 33. Fang L, Sun X, Song Y et al. Whole‐brain radiation fails to boost intracerebral gefitinib concentration in patients with brain metastatic non‐small cell lung cancer: A self‐controlled, pilot study. Cancer Chemother Pharmacol 2015;76:873–877. [DOI] [PubMed] [Google Scholar]
- 34. Masuda T, Hattori N, Hamada A et al. Erlotinib efficacy and cerebrospinal fluid concentration in patients with lung adenocarcinoma developing leptomeningeal metastases during gefitinib therapy. Cancer Chemother Pharmacol 2011;67:1465–1469. [DOI] [PubMed] [Google Scholar]
- 35. Zeng YD, Liao H, Qin T et al. Blood‐brain barrier permeability of gefitinib in patients with brain metastases from non‐small‐cell lung cancer before and during whole brain radiation therapy. Oncotarget 2015;6:8366–8376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fidler IJ, Yano S, Zhang RD et al. The seed and soil hypothesis: Vascularisation and brain metastases. Lancet Oncol 2002;3:53–57. [DOI] [PubMed] [Google Scholar]
- 37. Luo S, Chen L, Chen X et al. Evaluation on efficacy and safety of tyrosine kinase inhibitors plus radiotherapy in NSCLC patients with brain metastases. Oncotarget 2015;6:16725–16734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Park SJ, Kim HT, Lee DH et al. Efficacy of epidermal growth factor receptor tyrosine kinase inhibitors for brain metastasis in non‐small cell lung cancer patients harboring either exon 19 or 21 mutation. Lung Cancer 2012;77:556–560. [DOI] [PubMed] [Google Scholar]
- 39. Heon S, Yeap BY, Britt GJ et al. Development of central nervous system metastases in patients with advanced non‐small cell lung cancer and somatic EGFR mutations treated with gefitinib or erlotinib. Clin Cancer Res 2010;16:5873–5882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Grommes C, Oxnard GR, Kris MG et al. “Pulsatile” high‐dose weekly erlotinib for CNS metastases from EGFR mutant non‐small cell lung cancer. Neuro Oncol 2011;13:1364–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mok TS, Wu YL, Thongprasert S et al. Gefitinib or carboplatin‐paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947–957. [DOI] [PubMed] [Google Scholar]
- 42. Rosell R, Carcereny E, Gervais R et al. Erlotinib versus standard chemotherapy as first‐line treatment for European patients with advanced EGFR mutation‐positive non‐small‐cell lung cancer (EURTAC): A multicentre, open‐label, randomised phase 3 trial. Lancet Oncol 2012;13:239–246. [DOI] [PubMed] [Google Scholar]
- 43. Sequist LV, Yang JC, Yamamoto N et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327–3334. [DOI] [PubMed] [Google Scholar]
- 44. Arcila ME, Oxnard GR, Nafa K et al. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid‐based assay. Clin Cancer Res 2011;17:1169–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kuiper JL, Heideman DA, Thunnissen E et al. Incidence of T790M mutation in (sequential) rebiopsies in EGFR‐mutated NSCLC‐patients. Lung Cancer 2014;85:19–24. [DOI] [PubMed] [Google Scholar]
- 46. Li W, Ren S, Li J et al. T790M mutation is associated with better efficacy of treatment beyond progression with EGFR‐TKI in advanced NSCLC patients. Lung Cancer 2014;84:295–300. [DOI] [PubMed] [Google Scholar]
- 47. Wu SG, Liu YN, Tsai MF et al. The mechanism of acquired resistance to irreversible EGFR tyrosine kinase inhibitor‐afatinib in lung adenocarcinoma patients. Oncotarget 2016;7:12404–12413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hata A, Katakami N, Yoshioka H et al. Rebiopsy of non‐small cell lung cancer patients with acquired resistance to epidermal growth factor receptor‐tyrosine kinase inhibitor: Comparison between T790M mutation‐positive and mutation‐negative populations. Cancer 2013;119:4325–4332. [DOI] [PubMed] [Google Scholar]
- 49. Hata A, Katakami N, Yoshioka H et al. Spatiotemporal T790M heterogeneity in individual patients with EGFR‐mutant non‐small‐cell lung cancer after acquired resistance to EGFR‐TKI. J Thorac Oncol 2015;10:1553–1559. [DOI] [PubMed] [Google Scholar]
- 50. Balak MN, Gong Y, Riely GJ et al. Novel D761Y and common secondary T790M mutations in epidermal growth factor receptor‐mutant lung adenocarcinomas with acquired resistance to kinase inhibitors. Clin Cancer Res 2006;12:6494–6501. [DOI] [PubMed] [Google Scholar]
- 51. Brastianos PK, Carter SL, Santagata S et al. Genomic characterization of brain metastases reveals branched evolution and potential therapeutic targets. Cancer Discov 2015;5:1164–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cross DA, Ashton SE, Ghiorghiu S et al. AZD9291, an irreversible EGFR TKI, overcomes T790M‐mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov 2014;4:1046–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zeng Q, Wang J, Cheng Z et al. Discovery and evaluation of clinical candidate AZD3759, a potent, oral active, central nervous system‐penetrant, epidermal growth factor receptor tyrosine kinase inhibitor (EGFR TKI). J Med Chem 2015;58:8200–8215. [DOI] [PubMed] [Google Scholar]
- 54. Yang Z, Guo Q, Wang Y et al. AZD3759, a BBB‐penetrating EGFR inhibitor for the treatment of EGFR mutant NSCLC with CNS metastases. Sci Transl Med 2016;8:368ra172. [DOI] [PubMed] [Google Scholar]
- 55. Cohen MH, Williams GA, Sridhara R et al. FDA drug approval summary: Gefitinib (ZD1839) (Iressa) tablets. The Oncologist 2003;8:303–306. [DOI] [PubMed] [Google Scholar]
- 56.FDA. IRESSA (gefitinib) Highlights of prescribing information. 2015. Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206995s000lbl.pdf. Accessed June 29, 2017.
- 57. Schou M, Varnas K, Lundquist S et al. Large variation in brain exposure of reference CNS drugs: A PET study in nonhuman primates. Int J Neuropsychopharmacol 2015;18:pyv036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chen Y, Wang M, Zhong W et al. Pharmacokinetic and pharmacodynamic study of Gefitinib in a mouse model of non‐small‐cell lung carcinoma with brain metastasis. Lung Cancer 2013;82:313–318. [DOI] [PubMed] [Google Scholar]
- 59. Kitazaki T, Oka M, Nakamura Y et al. Gefitinib, an EGFR tyrosine kinase inhibitor, directly inhibits the function of P‐glycoprotein in multidrug resistant cancer cells. Lung Cancer 2005;49:337–343. [DOI] [PubMed] [Google Scholar]
- 60. Shimato S, Mitsudomi T, Kosaka T et al. EGFR mutations in patients with brain metastases from lung cancer: Association with the efficacy of gefitinib. Neuro Oncol 2006;8:137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Iuchi T, Shingyoji M, Sakaida T et al. Phase II trial of gefitinib alone without radiation therapy for Japanese patients with brain metastases from EGFR‐mutant lung adenocarcinoma. Lung Cancer 2013;82:282–287. [DOI] [PubMed] [Google Scholar]
- 62. Memon AA, Jakobsen S, Dagnaes‐Hansen F et al. Positron emission tomography (PET) imaging with [11C]‐labeled erlotinib: A micro‐PET study on mice with lung tumor xenografts. Cancer Res 2009;69:873–878. [DOI] [PubMed] [Google Scholar]
- 63. Elmeliegy MA, Carcaboso AM, Tagen M et al. Role of ATP‐binding cassette and solute carrier transporters in erlotinib CNS penetration and intracellular accumulation. Clin Cancer Res 2011;17:89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Weber B, Winterdahl M, Memon A et al. Erlotinib accumulation in brain metastases from non‐small cell lung cancer: Visualization by positron emission tomography in a patient harboring a mutation in the epidermal growth factor receptor. J Thorac Oncol 2011;6:1287–1289. [DOI] [PubMed] [Google Scholar]
- 65. Porta R, Sanchez‐Torres JM, Paz‐Ares L et al. Brain metastases from lung cancer responding to erlotinib: The importance of EGFR mutation. Eur Respir J 2011;37:624–631. [DOI] [PubMed] [Google Scholar]
- 66. How J, Mann J, Laczniak AN et al. Pulsatile erlotinib in EGFR‐positive non‐small‐cell lung cancer patients with leptomeningeal and brain metastases: Review of the literature. Clin Lung Cancer 2017;18:354–363. [DOI] [PubMed] [Google Scholar]
- 67. Kuiper JL, Smit EF. High‐dose, pulsatile erlotinib in two NSCLC patients with leptomeningeal metastases–One with a remarkable thoracic response as well. Lung Cancer 2013;80:102–105. [DOI] [PubMed] [Google Scholar]
- 68. Zhang SR, Zhu LC, Jiang YP et al. Efficacy of afatinib, an irreversible ErbB family blocker, in the treatment of intracerebral metastases of non‐small cell lung cancer in mice. Acta Pharmacol Sin 2017;38:233–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Yang JC, Shih JY, Su WC et al. Afatinib for patients with lung adenocarcinoma and epidermal growth factor receptor mutations (LUX‐Lung 2): A phase 2 trial. Lancet Oncol 2012;13:539–548. [DOI] [PubMed] [Google Scholar]
- 70. Schuler M, Wu YL, Hirsh V et al. First‐line afatinib versus chemotherapy in patients with non‐small cell lung cancer and common epidermal growth factor receptor gene mutations and brain metastases. J Thorac Oncol 2016;11:380–390. [DOI] [PubMed] [Google Scholar]
- 71. Shen YW, Zhang XM, Li ST et al. Efficacy and safety of icotinib as first‐line therapy in patients with advanced non‐small‐cell lung cancer. Onco Targets Ther 2016;9:929–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Zhou L, He J, Xiong W et al. Impact of whole brain radiation therapy on CSF penetration ability of Icotinib in EGFR‐mutated non‐small cell lung cancer patients with brain metastases: Results of phase I dose‐escalation study. Lung Cancer 2016;96:93–100. [DOI] [PubMed] [Google Scholar]
- 73. Yang JJ, Zhou C, Huang Y et al. Icotinib versus whole‐brain irradiation in patients with EGFR‐mutant non‐small‐cell lung cancer and multiple brain metastases (BRAIN): A multicentre, phase 3, open‐label, parallel, randomised controlled trial. Lancet Respir Med 2017;5:707–716. [DOI] [PubMed] [Google Scholar]
- 74. Jänne PA, Ahn MJ, Kim DW et al. Phase I study of AZD9291 in patients with EGFR‐TKI‐resistant advanced NSCLC – Updated progression free survival and duration of response data. Ann Oncol 2015;26(suppl 1):i60. [Google Scholar]
- 75. Yang JC, Kim DW, Kim SW et al. Osimertinib activity in patients (pts) with leptomeningeal (LM) disease from non‐small cell lung cancer (NSCLC): Updated results from BLOOM, a phase I study. J Clin Oncol 2016;34(suppl 15):9002a. [Google Scholar]
- 76. Yang J, Ramalingam SS, Jänne PA et al. LBA2_PR: Osimertinib (AZD9291) in pre‐treated pts with T790M‐positive advanced NSCLC: Updated Phase 1 (P1) and pooled Phase 2 (P2) results. J Thoracic Oncol 2016;11(suppl 4):S152–S153. [Google Scholar]
- 77. Ahn MJ, Tsai CM, Yang JC et al. 3083 AZD9291 activity in patients with EGFR‐mutant advanced non‐small cell lung cancer (NSCLC) and brain metastases: Data from Phase II studies. Eur J Cancer 2015;51:S625–S626. [Google Scholar]
- 78. Mok TS, Wu YL, Ahn MJ et al. Osimertinib or platinum–pemetrexed in EGFR T790M–positive lung cancer. N Engl J Med 2017;376:629–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mok T, Ahn MJ, Han JY et al. CNS response to osimertinib in patients (pts) with T790M‐positive advanced NSCLC: Data from a randomized phase III trial (AURA3). J Clin Oncol 2017;35(suppl 15):9005a. [Google Scholar]
- 80. Soria JC, Ohe Y, Vansteenkiste J et al. Osimertinib in untreated EGFR‐mutated advanced non‐small‐cell lung cancer. N Engl J Med 2018;378:113–125. [DOI] [PubMed] [Google Scholar]
- 81. Vansteenkiste J, Reungwetwattana T, Nakagawa K et al. LBA5 CNS response to osimertinib vs standard of care (SoC) EGFR‐TKI as first‐line therapy in patients (pts) with EGFR‐TKI sensitising mutation (EGFRm)‐positive advanced non‐small cell lung cancer (NSCLC): Data from the FLAURA study. Ann Oncol 2017;28(suppl 10):mdx729.007. [Google Scholar]
- 82. Kim D, Yang JC, Chen K et al. AZD3759, an EGFR inhibitor with blood brain barrier (BBB) penetration for the treatment of non‐small cell lung cancer (NSCLC) with brain metastasis (BM): Preclinical evidence and clinical cases. J Clin Oncol 2015;33(suppl 15):8016a. [Google Scholar]
- 83. Tan CS, Cho BC, Soo RA. Next‐generation epidermal growth factor receptor tyrosine kinase inhibitors in epidermal growth factor receptor‐mutant non‐small cell lung cancer. Lung Cancer 2016;93:59–68. [DOI] [PubMed] [Google Scholar]
- 84. Ahn MJ, Kim DW, Cho BC et al. Phase I study (BLOOM) of AZD3759, a BBB penetrable EGFR inhibitor, in patients with TKI‐naïve, EGFRm NSCLC with CNS metastases. J Clin Oncol 2017;35:2006. [Google Scholar]
- 85. Chan OS, Leung WK, Yeung RM. Sustained response to standard dose osimertinib in a patient with plasma T790M‐positive leptomeningeal metastases from primary lung adenocarcinoma. Asia Pac J Clin Oncol 2017;13:428–430. [DOI] [PubMed] [Google Scholar]
- 86. Pareek V, Welch M, Ravera E et al. Marked differences in CNS activity among EGFR inhibitors: Case report and mini‐review. J Thorac Oncol 2016;11:e135–e139. [DOI] [PubMed] [Google Scholar]
- 87. Sakai H, Hayashi H, Iwasa I et al. Successful osimertinib treatment for leptomeningeal carcinomatosis from lung adenocarcinoma with the T790M mutation of EGFR. ESMO Open 2017;2:e000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Takeda T, Itano H, Takeuchi M et al. Osimertinib administration via nasogastric tube in an EGFR‐T790M‐positive patient with leptomeningeal metastases. Respirol Case Rep 2017;5:e00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Uemura T, Oguri T, Okayama M et al. Dramatic intracranial response to osimertinib in a poor performance status patient with lung adenocarcinoma harboring the epidermal growth factor receptor T790M mutation: A case report. Mol Clin Oncol 2017;6:525–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Yang JC, Cho BC, Kim DW et al. Osimertinib for patients (pts) with leptomeningeal metastases (LM) from EGFR‐mutant non‐small cell lung cancer (NSCLC): Updated results from the BLOOM study. J Clin Oncol 2017;35(suppl 15):2020a. [Google Scholar]
- 91. Cho BC, Ahn MJ, Lee JS et al. Phase I study (BLOOM) of AZD3759, a BBB penetrable EGFR inhibitor, in EGFRm NSCLC patients with leptomeningeal metastasis (LM) who progressed after other anti‐cancer therapy. J Clin Oncol 2017;35:2069. [Google Scholar]
- 92. Ota K, Shiraishi Y, Harada T et al. OA08.02. Phase II study of erlotinib in advanced non‐small cell lung cancer patients with leptomeningeal metastasis (LOGIK1101). J Thorac Oncol 2017;12:S271–S272. [Google Scholar]
- 93. Jackman DM, Cioffredi LA, Jacobs L et al. A phase I trial of high dose gefitinib for patients with leptomeningeal metastases from non‐small cell lung cancer. Oncotarget 2015;6:4527–4536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Lee E, Keam B, Kim DW et al. Erlotinib versus gefitinib for control of leptomeningeal carcinomatosis in non‐small‐cell lung cancer. J Thorac Oncol 2013;8:1069–1074. [DOI] [PubMed] [Google Scholar]
- 95. Kashima J, Okuma Y, Miwa M et al. Retrospective analysis of survival in patients with leptomeningeal carcinomatosis from lung adenocarcinoma treated with erlotinib and gefitinib. Jpn J Clin Oncol 2017;47:357–362. [DOI] [PubMed] [Google Scholar]
- 96. Tetsumoto S, Osa A, Kijima T et al. Two cases of leptomeningeal metastases from lung adenocarcinoma which progressed during gefitinib therapy but responded to erlotinib. Int J Clin Oncol 2012;17:155–159. [DOI] [PubMed] [Google Scholar]
- 97. Sekine A, Kato T, Iwasawa T et al. Promising effects of afatinib on leptomeningeal carcinomatosis derived from erlotinib‐resistant lung adenocarcinoma. Intern Med 2016;55:2457–2461. [DOI] [PubMed] [Google Scholar]
- 98. Tamiya M, Shiroyama T, Nishihara T et al. Afatinib successfully treated leptomeningeal metastasis during erlotinib treatment in a patient with EGFR‐mutant (Exon18:G719S) lung adenocarcinoma as a second‐line chemotherapy. Asia Pac J Clin Oncol 2016;13:e531–e533. [DOI] [PubMed] [Google Scholar]
- 99. Ghosn M, Assi T, Rassy EE et al. An unexpected response to second line EGFR inhibitor in relapsing leptomeningeal carcinomatosis from lung adenocarcinoma raises questions on differential mechanisms of action of these agents. Bull Cancer 2017;104:385–387. [DOI] [PubMed] [Google Scholar]
- 100. Kawaguchi Y, Hanaoka J, Hayashi H et al. Clinical efficacy of afatinib treatment for a patient with leptomeningeal carcinomatosis. Chemotherapy 2016;62:147–150. [DOI] [PubMed] [Google Scholar]
- 101. Gong L, Xiong M, Huang Z et al. Icotinib might be effective for the treatment of leptomeningeal carcinomatosis in non‐small cell lung cancer with sensitive EGFR mutations. Lung Cancer 2015;89:268–273. [DOI] [PubMed] [Google Scholar]
- 102. Preusser M, Winkler F, Collette L et al. Trial design on prophylaxis and treatment of brain metastases: Lessons learned from the EORTC Brain Metastases Strategic Meeting 2012. Eur J Cancer 2012;48:3439–3447. [DOI] [PubMed] [Google Scholar]
- 103. Chamberlain MC, Kormanik P. Carcinoma meningitis secondary to non‐small cell lung cancer: Combined modality therapy. Arch Neurol 1998;55:506–512. [DOI] [PubMed] [Google Scholar]
- 104. Chang EL, Wefel JS, Hess KR et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole‐brain irradiation: A randomised controlled trial. Lancet Oncol 2009;10:1037–1044. [DOI] [PubMed] [Google Scholar]
- 105. McCoach CE, Berge EM, Lu X et al. A brief report of the status of central nervous system metastasis enrollment criteria for advanced non‐small cell lung cancer clinical trials: A review of the ClinicalTrials.gov Trial Registry. J Thorac Oncol 2016;11:407–413. [DOI] [PubMed] [Google Scholar]
- 106. Lin NU, Lee EQ, Aoyama H et al. Response ssessment criteria for brain metastases: Proposal from the RANO group. Lancet Oncol 2015;16:e270–e278. [DOI] [PubMed] [Google Scholar]
- 107. Huang RY, Wen PY. Response Assessment in Neuro‐Oncology criteria and clinical endpoints. Magn Reson Imaging Clin N Am 2016;24:705–718. [DOI] [PubMed] [Google Scholar]
- 108. Chamberlain M, Soffietti R, Raizer J et al. Leptomeningeal metastasis: A Response Assessment in Neuro‐Oncology critical review of endpoints and response criteria of published randomized clinical trials. Neuro Oncol 2014;16:1176–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Glass JP, Melamed M, Chernik NL et al. Malignant cells in cerebrospinal fluid (CSF): The meaning of a positive CSF cytology. Neurology 1979;29:1369–1375. [DOI] [PubMed] [Google Scholar]
- 110. Pauls S, Fischer AC, Brambs HJ et al. Use of magnetic resonance imaging to detect neoplastic meningitis: Limited use in leukemia and lymphoma but convincing results in solid tumors. Eur J Radiol 2012;81:974–978. [DOI] [PubMed] [Google Scholar]
- 111. Chamberlain MC. Comprehensive neuraxis imaging in leptomeningeal metastasis: A retrospective case series. CNS Oncol 2013;2:121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Chamberlain M, Junck L, Brandsma D et al. Leptomeningeal metastases: A RANO proposal for response criteria. Neuro Oncol 2016;19:484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Redig AJ, Costa DB, Taibi M et al. Prospective study of repeated biopsy feasibility and acquired resistance at disease progression in patients with advanced EGFR mutant lung cancer treated with erlotinib in a phase 2 trial. JAMA Oncol 2016;2:1240–1242. [DOI] [PubMed] [Google Scholar]
- 114. Douillard JY, Ostoros G, Cobo M et al. First‐line gefitinib in Caucasian EGFR mutation‐positive NSCLC patients: A phase‐IV, open‐label, single‐arm study. Br J Cancer 2014;110:55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Yang JC, Wu YL, Schuler M et al. Afatinib versus cisplatin‐based chemotherapy for EGFR mutation‐positive lung adenocarcinoma (LUX‐Lung 3 and LUX‐Lung 6): Analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol 2015;16:141–151. [DOI] [PubMed] [Google Scholar]
- 116. Yang JJ, Zhou Q, Yan HH et al. A phase III randomised controlled trial of erlotinib vs gefitinib in advanced non‐small cell lung cancer with EGFR mutations. Br J Cancer 2017;116:568–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Magnuson WJ, Lester‐Coll NH, Wu AJ et al. Management of brain metastases in tyrosine kinase inhibitor‐naive epidermal growth factor receptor‐mutant non‐small‐cell lung cancer: A retrospective multi‐institutional analysis. J Clin Oncol 2017;35:1070–1077. [DOI] [PubMed] [Google Scholar]
- 118. Ma S, Xu Y, Deng Q et al. Treatment of brain metastasis from non‐small cell lung cancer with whole brain radiotherapy and Gefitinib in a Chinese population. Lung Cancer 2009;65:198–203. [DOI] [PubMed] [Google Scholar]
- 119. Welsh JW, Komaki R, Amini A et al. Phase II trial of erlotinib plus concurrent whole‐brain radiation therapy for patients with brain metastases from non‐small‐cell lung cancer. J Clin Oncol 2013;31:895–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Fan Y, Huang Z, Fang L et al. A phase II study of icotinib and whole‐brain radiotherapy in Chinese patients with brain metastases from non‐small cell lung cancer. Cancer Chemother Pharmacol 2015;76:517–523. [DOI] [PubMed] [Google Scholar]
- 121. Heon S, Yeap BY, Lindeman NI et al. The impact of initial gefitinib or erlotinib versus chemotherapy on central nervous system progression in advanced non‐small cell lung cancer with EGFR mutations. Clin Cancer Res 2012;18:4406–4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Shin KH, Kim KP, Lim KS et al. A positron emission tomography microdosing study with sertraline in healthy volunteers. Int J Clin Pharmacol Ther 2012;50:224–232. [DOI] [PubMed] [Google Scholar]
- 123. Brahmer J, Reckamp KL, Baas P et al. Nivolumab versus docetaxel in advanced squamous‐cell non‐small‐cell lung cancer. N Engl J Med 2015;373:123–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Borghaei H, Paz‐Ares L, Horn L et al. Nivolumab versus docetaxel in advanced nonsquamous non‐small‐cell lung cancer. N Engl J Med 2015;373:1627–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Herbst RS, Baas P, Kim DW et al. Pembrolizumab versus docetaxel for previously treated, PD‐L1‐positive, advanced non‐small‐cell lung cancer (KEYNOTE‐010): A randomised controlled trial. Lancet 2016;387:1540–1550. [DOI] [PubMed] [Google Scholar]
- 126. Antonia SJ, Kim SW, Spira AI et al. Safety and clinical activity of durvalumab (MEDI4736), an anti‐PD‐L1 antibody, in treatment‐naïve patients with advanced non–small‐cell lung cancer. J Clin Oncol 2016;34:9029a. [Google Scholar]
- 127. Fehrenbacher L, Spira A, Ballinger M et al. Atezolizumab versus docetaxel for patients with previously treated non‐small‐cell lung cancer (POPLAR): A multicentre, open‐label, phase 2 randomised controlled trial. Lancet 2016;387:1837–1846. [DOI] [PubMed] [Google Scholar]
- 128. Kelly K, Patel MR, Infante JR et al. Avelumab (MSB0010718C), an anti‐PD‐L1 antibody, in patients with metastatic or locally advanced solid tumors: Assessment of safety and tolerability in a phase I, open‐label expansion study. J Clin Oncol 2015;33:3044a. [Google Scholar]
- 129. Schinkel AH. P‐Glycoprotein, a gatekeeper in the blood‐brain barrier. Adv Drug Deliv Rev 1999;36:179–194. [DOI] [PubMed] [Google Scholar]
- 130. Agarwal S, Hartz AM, Elmquist WF et al. Breast cancer resistance protein and P‐glycoprotein in brain cancer: Two gatekeepers team up. Curr Phar Des 2011;17:2793–2802. [DOI] [PMC free article] [PubMed] [Google Scholar]