Abstract
Epstein-Barr virus (EBV) is a gamma-herpesvirus that establishes lifelong infection in the majority of people worldwide. EBV uses epigenetic reprogramming to switch between multiple latency states in order to colonize the memory B-cell compartment and to then periodically undergo lytic reactivation upon plasma cell differentiation. This review focuses on recent advances in the understanding of epigenetic mechanisms that EBV uses to control its lifecycle and to subvert the growth and survival pathways that underly EBV-driven B-cell differentiation versus B-cell growth transformation, a hallmark of the first human tumor virus. These include the formation of viral super-enhancers that drive expression of key host dependency factors, evasion of tumor suppressor responses, prevention of plasmablast differentiation, and regulation of the B-cell lytic switch.
Keywords: Lytic reactivation, latency, chromatin, gamma-herpesvirus, tumor virus, super-enhancer
Introduction
Human herpesviruses persistently infect immunocompetent hosts through a biphasic lifecycle that involves latent infection of a long-lived reservoir cell and occasional lytic reactivation. Epstein-Barr virus (EBV) is a ubiquitous human herpesvirus that crosses the tonsillar epithelium, infects B-cells and manipulates growth, survival and differentiation pathways to reach the memory B-cell compartment, the reservoir for lifelong infection [1]. Recent advances continue to shed light on how EBV manipulates epigenetic pathways to reprogram host and viral programs in each of these states.
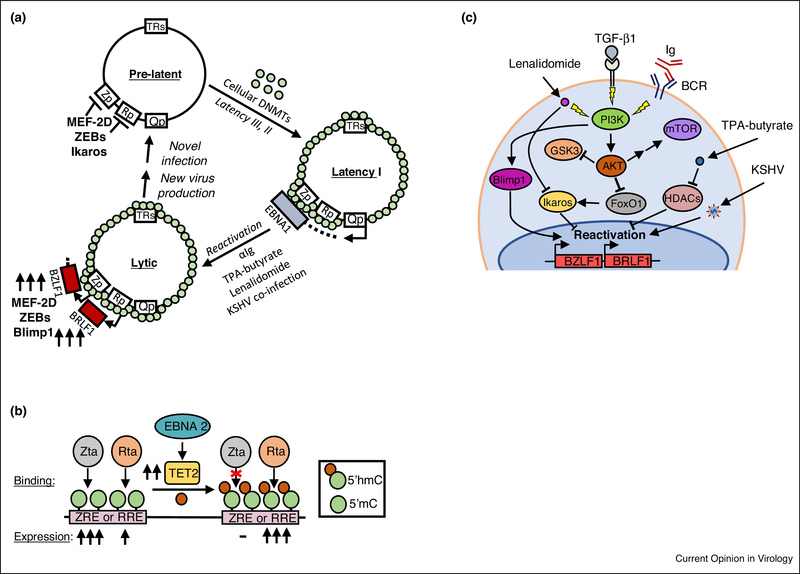
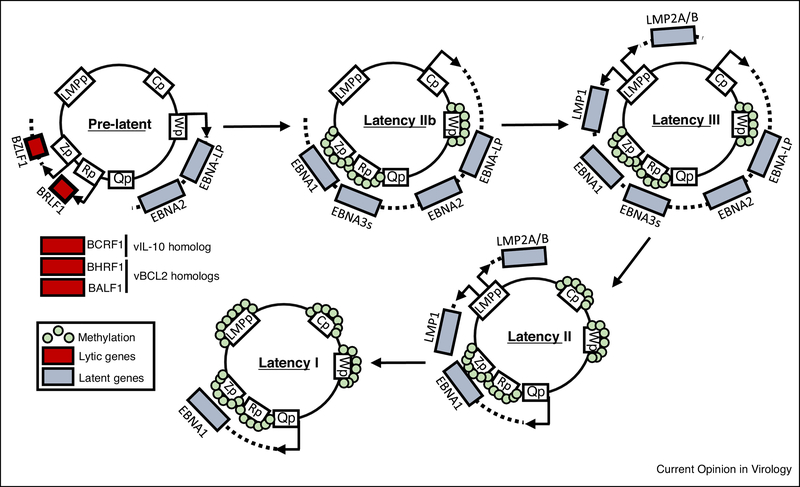
Whereas the lytic cycle promotes virus production and cell-to-cell spread, latency is critical for infected- cell proliferation and survival [2]. Upon B-cell infection, a brief pre-latent state occurs, where lytic transcripts are produced, including those encoding the immediate early transcription factors Zta and Rta, viral BCL2 homologs BHRF1 and BALF1, and the viral IL-10 homolog BCRF1 [3–7]. EBV-encoded miRNAs promote cell cycle and suppress apoptosis [8]. Latency IIb follows, with Epstein Barr nuclear antigens (EBNA) 1, 2 and LP, vBCL2 and non-coding RNAs (ncRNA) expressed (Figure 1). This program drives B-cell hyper-proliferation [4] and transitions to latency III, comprised of six EBNA, two latent membrane protein (LMP) and ncRNAs. In vitro, latency III transforms B-cells into immortalized lymphoblastoid cell lines (LCL). In vivo, EBV instead switches to latency II in immunocompetent hosts upon germinal center entry, where EBNA1, LMP1/2A and ncRNA are expressed. Upon memory cell differentiation, EBV restricts expression to EBNA1 and ncRNAs by the latency I program [2,9,10]. This progression is thought to result from the accumulation of epigenetic silencing marks on viral promoters [11,12] (Figure 1). Reactivation from latency requires de-repression of immediate early genes BZLF1 and BRLF1.
Figure 1. Methylation-dependent expressional changes of the EBV genome during latency progression.
Recent evidence suggests EBV latency begins with a pre-latent stage, in which lytic inducers Zta and Rta, along with the vIL-10 homolog BCRF1 and vBCL2 homologs BHRF1 and BALF1 are expressed and enhance transition into viral latency. Upon accumulation of EBNA2 and EBNA-LP, expression from the viral Cp and LMPp promoters is enhanced, leading to induction of all type III latency genes. Repressive methylation of Cp blocks EBNA2 an 3 expression in latency II, where Qp drives EBNA1 and LMPp drives LMP1/2A co-expression. Once repressive methylation is accrued on LMPp, the quiescent latency I is reached, where only EBNA 1 and viral ncRNAs are expressed.
Here, we review recent advances in the understanding of epigenetic contribution to EBV latency states, lytic reactivation, EBV super-enhancers, silencing of tumor suppressors BCL2L11 and PRDM1, and in EBNA3-mediated suppression of LMP1/2A-driven plasmablast differentiation. Space limitations preclude discussion of equally interesting epigenetic mechanisms in EBV-infected epithelial cells [13].
Promoter methylation control latency states
In pre-latency as viral DNA becomes chromatinized, the viral W promoter (Wp) drives EBNA expression [14–16]. Zta preferentially activates early gene promoters with methylated 5’-cytosine residues (5mC) termed meZREs, not widely distributed at this timepoint, preventing progeny virus production at this early timepoint [9,17,18]. Progressive EBV genome compaction and methylation silences leaky lytic transcription [6,14,15,17], while increasing EBNA2 and LP expression activate the C promoter (Cp) to induce EBNA1 and 3 proteins. EBNA2 and host RBP-Jκ activate the unmethylated LMP promoter (LMPp) to induce LMP1 and LMP2A expression, triggering latency III (Figure 2A)[2].
Figure 2. Epigenetic mechanisms affecting the EBV latent-lytic switch.
(A) Schematic diagram depicting repressive methylation (green circles) accrual on the EBV genome by cellular DNA methyltransferases (DMNTs), resulting in latency I. Shown also are selected treatments that can induce lytic gene expression. (B) TET2 conversion of viral genome methylated Z-response element (ZRE) 5’cytosine residues (5mC) into 5’ hydroxymethylation (5’hmC) precludes Zta binding and transactivation. 5’hmC does not affect Rta binding, but surprisingly enhances Rta-mediated activation. (C) PI3K pathway activation stimulates EBV lytic reactivation from latency I. Multiple lytic reactivation stimuli activate PI3K to upregulate Blimp1 and downmodulate Ikaros.
Chromatin conformation has key roles in maintenance of EBV latency [19]. The looping factor CTCF binds to multiple EBV genome sites and is post-translationally regulated by the host enzyme Poly(ADPribose) polymerase (PARP1), which colocalize at specific EBV genomic sites. PARP1 stabilizes CTCF binding to maintain type III latency chromatin configurations [20]. PARP1 and CTCF suppress the BZLF1 promoter [21]. Curiously, knockdown of PARP1, but not CTCF promotes viral reactivation, suggesting that PARP1 may have additional cellular cofactors that act redundantly with or independently of CTCF in lytic switch regulation.
Accumulation of Cp methylation accompanies the shift to latency II, where the Q promoter (Qp) instead drives EBNA1, and a CTCF site insulates Qp from spreading repressive marks [22] (Figure 2A). Cytotoxic T-cell responses exert selective pressure for this antigenic silencing [23], and EBV likely also responds to cellular cues, for example resulting from germinal center entry. Progressive LMPp methylation leads to latency I, reducing immunogenicity [24]. Cellular cues likely contribute to this reprogramming, perhaps resulting from memory cell differentiation, germinal center exit or downmodulation of mitogenic transcription factors [4].
Changes in EBV and host genome methylation patterns in latency III have recently been linked to the host demethylase ten-eleven translocation 2 (TET2), a tumor suppressor that is frequently mutated in hematological cancers [25]. TET2 converts 5-methylcytosine (5mC) into 5-hydroxymethylcytosine (5’hmC) to de-repress target gene expression. Whereas TET2 overexpression results in increased latency III protein expression, TET2 knockdown blocks latency III and triggers lytic expression [24,26]. Building on this hypothesis, latency III expression drives B-cell activation, and TET2 expression is higher in activated B-cells than in germinal center (GC) B-cells. Demethylating agents upregulate latency III transcripts in latency I B-cells. Further supporting key methylation roles, EBNA2, RBP-Jκ and EBF1 induce TET2 expression and then co-occupy key LCL genomic sites with TET2 [24,26].
Epigenetic regulation of EBV lytic reactivation
Reactivation requires immediate early gene de-repression. Zta is homologous to bZIP family transcription factors and binds to AP-1-like Z-response elements (ZREs) [27–29]. Alanine-to-serine substitutions homologous to Zta convert host AP-1 into a TF that binds methylated EBV DNA and that activates some EBV early genes [30], underscoring the close relationship between AP-1 and ZTA. Similarly, Rta binds R-response elements (RREs) with the consensus sequence 5′-GNCCN9GGNG-3′ (where N is any nucleotide). Zta and Rta induce one another as well as EBV early genes [27,31]. As such, Zp and Rp tightly control Zta and Rta expression, respectively [27].
Importantly, repressive H3K27me3 methylation deposited by polycomb-group proteins repress ZREs and RREs. This shielding is important for latency [32], and cellular factors such as MEF2D, ZEB1 and ZEB2 also inhibit early lytic replication by recruiting histone deacetylases to Zp and by negatively regulating cis-acting Zp elements. However, these factors instead enhance lytic induction upon B-cell receptor engagement or TGF-β1 treatment [27].
Zta or Rta overexpression triggers lytic reactivation and virus production [33,34]. However, Zta and Rta lytic-inducing effects are not equal in their binding and activation of methylated promoters [35]. Zta only efficiently binds and activates CpG methylated viral promoters, while Rta only efficiently binds and activates unmethylated and perhaps CpG methylated promoters [27,35]. Adding another layer of depth, 5’hmC modification inhibits promoter binding and activation by ZTA [24,36]. Rta binding is unaffected by 5’hmC, yet 5’hmC enhances Rta-mediated promoter activation [36] (Figure 2B). TET2 knockdown enhances immediate-early expression in latency III cells [26].
Curiously, Zta expression triggers lytic reactivation only in a subpopulation of B-cells, for reasons that are incompletely understood. STAT3, which is activated upon EBV entry, contributes to this phenotype, as cells with elevated STAT3 are refractory to reactivation [37]. Mechanistically, STAT3 regulates the KRAB-zinc finger proteins SZF1 and ZNF557 to silence multiple EBV lytic genes, in part through the enzyme TRIM28, which recruits the histone methyltransferase SETDB1, the DNA methyltransferases 3A/B, the NuRD histone deacetylase complex and the heterochromatin amplification factor HP1 [38]. Physiological EBV reactivation triggers are incompletely understood. Differentiation of latently infected memory B-cells into plasma-cells appears to be a major trigger [39]. Further supporting this hypothesis, treatment of latently infected cells with the immunomodulatory agent lenalidomide stimulates reactivation via enhanced PI3K signaling and activation of the downstream AKT and GSK kinases, a pathway also activated by B-cell receptor signaling in plasma cell differentiation. Lenalidomide effects on lytic induction are suppressed by PI3K inhibition, denoting important PI3K roles in this reactivation pathway [40,41]. Lenalidomide also suppresses expression of Ikaros, a host transcription factor positively regulated by PI3K-dependent Forkhead-box-O1 (FoxO1) [40]. Lenalidomide decreases FoxO1 and Ikaros levels and results in enhanced Zta/Rta expression. Ikaros knockdown suppresses EBV reactivation [42] (Figure 2C).
The specific mechanism by which Ikaros suppresses EBV lytic reactivation is currently incompletely understood [40,42]. Adding to the importance of the role of PI3K in lytic reactivation, overexpression of B-lymphocyte-induced maturation protein 1 (Blimp1), a cellular master regulator of plasma cell differentiation, induces lytic reactivation [43]. Blimp1 expression is partly controlled by PI3K activation, as knockout of PTEN, a cellular lipid phosphatase that negatively regulates PI3K, resulted in enhanced Blimp1 expression [44] (Figure 2C). Since lenalidomide induces degradation of IRF4, the major B-cell transcription activator of Blimp1, further studies are needed to assess specific elements of PI3K pathway and additional downstream targets that regulate EBV reactivation, but it stands as an important avenue of investigation.
Primary Effusion Lymphoma (PEL) are typically co-infected with EBV and Kaposi Sarcoma-Associated Herpesvirus (KSHV). Interestingly, EBV co-infection enhances KSHV persistence and tumorigenesis in a humanized mouse model [45]. In this model, co-infection results in a plasma-cell like state reminiscent of PEL, with enhanced EBV lytic gene expression. Coinfected B-cells express Zta, without detectable late gene expression. KSHV may therefore utilize EBV early lytic gene expression to drive cell proliferation and survival [45]. Abortive lytic EBV expression was detected in human PEL tumor samples. Open questions include whether a lack of methylated 5’-cytosine meZREs at PEL early gene promoters underlie the abortive lytic pattern, how KSHV contributes to EBV lytic gene expression, and how EBV lytic genes contribute to transformation.
EBNA and LMP1-activated NF-κB Form Viral Super-Enhancers
Super-enhancers (SE) are particularly strong enhancers that are major determinants of cell identity and malignant states [46,47]. Compared with typical enhancers, SE have significantly larger size, transcription factor density and content and are particularly sensitive to perturbation, such as by BET-bromodomain inhibitors [46]. LCL chromatin immunoprecipitation with deep sequencing (ChIP-Seq) analysis identified SE at host genomic sites [48]. Using LCL EBNA and LMP1-activated NF-κB ChIP-seq datasets [49], two distinct types of viral SE were observed. 888 SE sites are EBNA2 occupied and termed EBNA2 SE, whereas 187 SE are co-occupied by EBNA2, LP, 3A and 3C and five NF-κB subunits and termed EBV SE [48].
To assign EBV SE-promoter linkages, LCL ChIP-seq and Chromatin Interaction Analysis by Paired-End Tag Sequencing (ChIA-PET) datasets [50] were integrated [51]. ChIA-PET defines 3-dimensional genome organization positioned by specific transcription factors, such as CTCF. EBV SE target 544 promoters at an average distance of 438 kilobases (kb), including the host dependency factors CFLAR, IRF4, IRF2 and MYC [51,52]. EBV further upregulates key targets by typical enhancers, including by EBNA2- and RBP-Jκ-bound enhancers [51,53]. RBP-Jκ is important for IRF4 induction by EBNA2 [54], and EBNA2 likewise activates typical enhancers upstream and downstream of MYC [55]. EBNA3C associates with and stabilizes IRF4 [56].
EBV SE often target multiple host genes, and key genes are targeted by multiple EBV SE. For instance, EBV SE 525 and 428 kb upstream each target MYC. While the importance of most EBV SE remain to be established experimentally, deletion of either SE significantly diminishes MYC expression, LCL growth and survival [48]. It will be interesting to determine how EBV upregulates MYC in latency IIb in the absence of LMP1, or in latency II where LMPs but not EBNAs 2 and 3 are expressed.
How do EBV SE target promoters by long-range interactions? Conditional EBNA2 or 3 allele studies suggest that EBV nuclear antigens may be DNA looping factors. Conditional inactivation of either EBNA2, 3A or 3C significantly reduces EBV SE looping to MYC [48]. EBNA2 recruits the SWI/SNF remodeler BRG1 ATPase to MYC-targeting enhancers, and BRG1 is necessary for their interaction with the MYC promoter [55]. EBNA2 drives cooperative and combinatorial binding of the EBF1 and RBP-Jκ, which then co-occupy newly induced binding sites with EBNA2 [57]. EBNA3 can instead repress or prevent the establishment of chromatin hubs through modulating enhancer-promoter loop formation [58]. Noncoding RNAs Pol II-transcribed from EBV SE also have roles in EBV SE looping to MYC [59].
How EBNA-LP contributes to EBV SE remains to be understood. Recombinant EBV deficient for EBNA-LP transforms B cells from adult donors at reduced efficiency as compared with wildtype EBV and could not fully transform umbilical cord B cells, which died by two weeks post-infection, suggesting epigenetic cell states define EBNA-LP roles [60]. Effects on EBNA2, RBP-Jκ and EBF1 recruitment to viral genome latency promoters were observed. EBNA-LP can also coactivate with the host histone acetyltransferase EP300 [61], an effect that remains to be investigated in the context of EBV SE.
Positive feedback loops enforce expression of key SE targets, such as host microRNA miR-155HG, which is induced by multiple EBV SE and by EBV-SE target IRF4 [51,53]. Similarly, IRF4 and EBNA3C downmodulate BCL6 [62]. ChIP-seq analysis of SE landscapes in pre-latency, latency IIb, II and I phases would undoubtedly reveal interesting shared and unique targets.
EBNA3A, 3C, IRF4 and BATF Epigenetic Regulation of Tumor Suppressor BCL2L11
EBV induces IRF4 and BATF [52], which are key regulators of B-cell differentiation and activation. Genome-wide Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) screens identified BATF and IRF4 as key EBV-induced host dependency factors necessary for LCL, but not EBV+ Burkitt cell survival [52]. CRISPR screens similarly implicated IRF4 as a key PEL dependency factor [63]. The IRF4 DNA motif is enriched at LCL human genome sites occupied by EBNA3C or EBNA3A [64–66], suggesting that EBV may often use IRF4 to target B-cell sites.
BATF and IRF4 bind cooperatively to DNA sites with an AP1-interferon composite element (AICE). BATF and IRF4 are each critical for EBV repression of the tumor suppressor BCL2L11, which encodes the pro-apoptosis factor BIM [52]. Elegant studies identified EBNA-3A, 3C and polycomb as necessary for BCL2L11 suppression [55,67]. How these factors silence BCL2L11 is incompletely understood. Since they co-occupy a B-cell genomic site upstream of the BIM promoter [52], we hypothesize that an IRF4/BATF complex anchors EBNA3A, 3C and polycomb complexes that epigenetically silence BCL2L11.
LCL BCL2L11 knockout (KO) was insufficient to rescue subsequent IRF4 CRISPR KO [52], suggesting additional important LCL IRF4 roles. IRF4 or BATF KO downmodulated expression of c-Myc and its target genes. Since IRF4, BATF and EBNA3A/C co-occupy multiple sites within the EBV SE that loop to MYC, they may have roles in recruiting EBNA3s to these sites and/or SE looping.
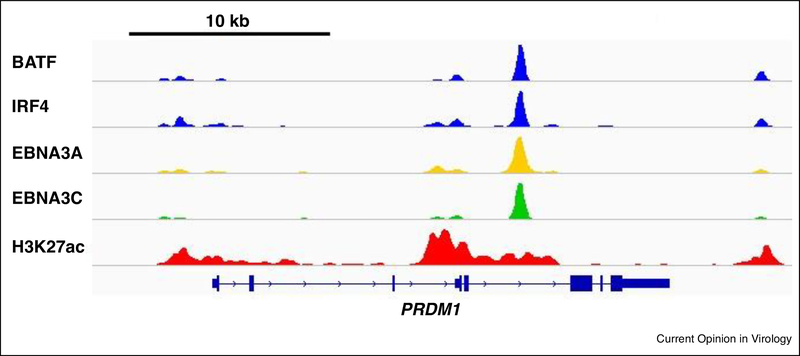
EBNA3A, 3C, IRF4 and BATF Epigenetic Regulation of PRDM1
IRF4 upregulates PRDM1, which encodes the master plasma cell differentiation regulator Blimp1. Since Blimp1 is expressed at low levels in LCLs, how then does EBV block Blimp1 upregulation? EBV null for EBNA3A/3C induces Blimp1 and plasmablast differentiation. EBNA3A/C are necessary to suppress plasmablast differentiation within the first 12 days post-infection, but not thereafter, suggesting that they drive epigenetic commitment to the B-blast fate [68]. Curiously, although Blimp1 and plasma cell differentiation trigger lytic reactivation, lytic antigens are not observed in this model. Further studies are required to identify host and/or viral factors that maintain EBV latency in this setting. Infection of humanized mice with EBNA3A- or EBNA3C-null EBV did not induce plasmablast differentiation, indicating that EBNA3A and 3C have functional redundant roles in maintaining B-lymphoblast state [69].
EBNA3A and 3C were found to co-occupy a PRDM1 locus intronic site[68], but since they do not bind DNA directly, how do they target this site? An overlay of LCL ChIP-seq datasets demonstrates that IRF4 and BATF co-occupy the major EBNA3A/C PRDM1 locus site (Figure 3). We hypothesize that LMP1, LMP2A and EBNA2 first induce a BATF/IRF4 complex to target this site, and to then prevent PRDM1 induction, EBNA3A and C are recruited and drive polycomb proteins to epigenetically silence PRDM1.
Figure 3. Epigenetic silencing of PRDM1 in lymphoblastoid B-cells.
Shown are LCL ChIP-seq tracks at the Blimp1-encoding PRDM1 locus for the host transcription factors BATF and IRF4 (blue), EBV EBNA3A (yellow) and EBNA3C (green) and the histone epigenetic mark histone 3 lysine 27 acetyl (H3K27ac, red). A schematic diagram of the PRDM1 gene body is shown at bottom.
Transgenic mouse B-cell LMP2A expression induces IRF4 and enhances B-cell survival, but not plasmablast differentiation [70]. By contrast, conditional GC B-cell LMP1/2A co-expression highlyinduces IRF4 and PRDM1 [71] and upregulates markers of plasmablast differentiation, including CD38 and CD138 [71]. Taken together with EBNA3 models, it appears that sustained LMP1/2A expression in the absence of EBNA3A or 3C drives plasmablast differentiation, which is fatal in mice that lack T and NK-cells [71] or even perforin [72]. In immunocompetent animals, GC B-cell LMP1/2A-coexpression impedes the GC reaction but does not cause lymphoma [71,72].
These mouse models raise the important question of how latency II GC B-cells differentiate into latency I memory cells rather than plasmablasts. Perhaps epigenetic marks from earlier EBV latency states, coexpression of EBNA1 or viral ncRNAs, LMP1/2A expression levels, and/or T/NK-cell immune pressure play roles in guiding infected GC B-cells towards memory cell states. Conversely, epigenetic mechanisms that drive the latency I state typically observed in EBV+ plasmablastic lymphomas remain to be determined.
EBV suppresses Blimp1 by additional mechanisms, including by PRDM1 promoter hypermethylation, upregulation of the functionally-impaired Blimp1-beta isoform [73], and by EBV miR-BHRF1–2 [74]. EBV SE target IRF2 also suppresses PRDM1, apparently independently of EBNA3A/C, since LCL depletion of IRF2 but not EBNA3A/C de-represses PRDM1 [52,68]. CRISPR identified the EBV SE target and IRF2 co-repressor IRF2BP2 as important for LCL growth/survival [52], suggesting possible joint roles in PRDM1 suppression.
Concluding remarks.
Despite recent advances, important epigenetic roles throughout the EBV lifecycle and in EBV oncogenesis remain to be discovered. Humanized mice EBV infection models are rapidly advancing and promise to enable the study of viral and host genome epigenetic changes at key steps of Bcell infection, differentiation and reactivation. For instance, how does EBV alter memory B-cell epigenetic states to maintain latency in vivo? Likewise, how epigenetic mechanisms differ in the host/pathogen interactions between Type-I and II Epstein-Barr strains, and for Type II EBV between B and T-lymphocytes, will be interesting to pursue, including in newly developed humanized mouse models. It will be also be interesting to learn how epigenetic mechanisms underlie cell differentiation state-specific roles of LMP2A [75] and EBNA-LP, and how EBV nuclear antigens and host TFs together form viral super-enhancers.
Overview Figure. Key epigenetic mechanisms regulating EBV and B-cell gene expression.
Upon B-cell infection, the EBV genome rapidly becomes chromatinized to establish latency. During latency III, EBV superenhancers, comprised of four EBNA and five NF-kB transcription factor subunts target key host growth and survival genes, including IRF4. EBNA2-superenhancers. Separately, EBNA3A, 3C and polycomb proteins block expression of tumor suppressors, including PRDM1 (which encodes Blimp1) and BCL2L11 (which encodes BIM). BATF and IRF4 occupy composite AP1-interferon sites and may anchor EBNA3/polycomb complexes. As B-cells transit through the germinal center and differentiate into memory cells, progressive methylation restricts EBV latency gene expression, whereas the TET2 demethylase promotes latency III. Inducing agents trigger PI3K activation and de-repression of the master plasma cell differentiation regulator Blimp to trigger EBV lytic reactivation.
Highlights.
EBNA2 and TET2-mediated DNA demethylation promotes Latency III in B cells
EBNA3A/3C and polycomb prevent plasmablast differentiation driven by LMP1/2A
IRF4, BATF, EBNA3A/3C and polycomb suppress BCL2L11/BIM expression
EBV super-enhancers target 544 LCL genes, typically by long-range interactions
Acknowledgements.
TS is supported by training grant T32 AI007245. BEG is supported by a Burroughs Wellcome Career Award in Medical Sciences, by NIH RO1 AI137337, and by a STARR Cancer Consortium grant. The authors declare no conflict of interest. We thank Liang Wei Wang for assistance with ChIP-seq figure preparation. The authors declare no conflict of interest. We apologize to colleagues whose work we could not cite due to space constraints.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Thorley-Lawson DA: EBV Persistence--Introducing the Virus. Curr Top Microbiol Immunol 2015, 390:151–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Longnecker R, Kieff E and Cohen JI: Epstein-Barr Virus In Fields Virology, edn 6 Edited by Knipe DMaH PM: Lippincott, Williams and Wilkins; 2013:1898–1959. vol 2.] [Google Scholar]
- 3.Price AM, Luftig MA: Dynamic Epstein-Barr virus gene expression on the path to B-cell transformation. Adv Virus Res 2014, 88:279–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Price AM, Luftig MA: To be or not IIb: a multi-step process for Epstein-Barr virus latency establishment and consequences for B cell tumorigenesis. PLoS Pathog 2015, 11:e1004656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halder S, Murakami M, Verma SC, Kumar P, Yi F, Robertson ES: Early events associated with infection of Epstein-Barr virus infection of primary B-cells. PLoS One 2009, 4:e7214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wen W, Iwakiri D, Yamamoto K, Maruo S, Kanda T, Takada K: Epstein-Barr virus BZLF1 gene, a switch from latency to lytic infection, is expressed as an immediate-early gene after primary infection of B lymphocytes. J Virol 2007, 81:1037–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altmann M, Hammerschmidt W: Epstein-Barr virus provides a new paradigm: a requirement for the immediate inhibition of apoptosis. PLoS Biol 2005, 3:e404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seto E, Moosmann A, Gromminger S, Walz N, Grundhoff A, Hammerschmidt W: Micro RNAs of Epstein-Barr virus promote cell cycle progression and prevent apoptosis of primary human B cells. PLoS Pathog 2010, 6:e1001063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalla M, Gobel C, Hammerschmidt W: The lytic phase of epstein-barr virus requires a viral genome with 5-methylcytosine residues in CpG sites. J Virol 2012, 86:447–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pei Y, Lewis AE, Robertson ES: Current Progress in EBV-Associated B-Cell Lymphomas. Adv Exp Med Biol 2017, 1018:57–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schaefer BC, Strominger JL, Speck SH: Host-cell-determined methylation of specific Epstein-Barr virus promoters regulates the choice between distinct viral latency programs. Mol Cell Biol 1997, 17:364–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lieberman PM: Keeping it quiet: chromatin control of gammaherpesvirus latency. Nat Rev Microbiol 2013, 11:863–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott RS: Epstein-Barr virus: a master epigenetic manipulator. Curr Opin Virol 2017, 26:74–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lieberman PM: Epigenetics and Genetics of Viral Latency. Cell Host Microbe 2016, 19:619–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammerschmidt W: The Epigenetic Life Cycle of Epstein-Barr Virus. Curr Top Microbiol Immunol 2015, 390:103–117. [DOI] [PubMed] [Google Scholar]
- 16.Woisetschlaeger M, Strominger JL, Speck SH: Mutually exclusive use of viral promoters in EpsteinBarr virus latently infected lymphocytes. Proc Natl Acad Sci U S A 1989, 86:6498–6502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalla M, Schmeinck A, Bergbauer M, Pich D, Hammerschmidt W: AP-1 homolog BZLF1 of EpsteinBarr virus has two essential functions dependent on the epigenetic state of the viral genome. Proc Natl Acad Sci U S A 2010, 107:850–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhende PM, Seaman WT, Delecluse HJ, Kenney SC: The EBV lytic switch protein, Z, preferentially binds to and activates the methylated viral genome. Nat Genet 2004, 36:1099–1104. [DOI] [PubMed] [Google Scholar]
- 19.Tempera I, Klichinsky M, Lieberman PM: EBV latency types adopt alternative chromatin conformations. PLoS Pathog 2011, 7:e1002180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lupey-Green LN, Caruso LB, Madzo J, Martin KA, Tan Y, Hulse M, Tempera I: PARP1 Stabilizes CTCF Binding and Chromatin Structure to Maintain Epstein Barr Virus Latency Type. J Virol 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lupey-Green LN, Moquin SA, Martin KA, McDevitt SM, Hulse M, Caruso LB, Pomerantz RT, MirandaJL, Tempera I: PARP1 restricts Epstein Barr Virus lytic reactivation by binding the BZLF1 promoter. Virology 2017, 507:220–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tempera I, Wiedmer A, Dheekollu J, Lieberman PM: CTCF prevents the epigenetic drift of EBV latency promoter Qp. PLoS Pathog 2010, 6:e1001048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hislop AD, Taylor GS, Sauce D, Rickinson AB: Cellular responses to viral infection in humans: lessons from Epstein-Barr virus. Annu Rev Immunol 2007, 25:587–617. [DOI] [PubMed] [Google Scholar]
- 24.Wille CK, Li Y, Rui L, Johannsen EC, Kenney SC: Restricted TET2 Expression in Germinal Center Type B Cells Promotes Stringent Epstein-Barr Virus Latency. J Virol 2017, 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ko M, An J, Pastor WA, Koralov SB, Rajewsky K, Rao A: TET proteins and 5-methylcytosine oxidation in hematological cancers. Immunol Rev 2015, 263:6–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu F, Wiedmer A, Martin KA, Wickramasinghe P, Kossenkov AV, Lieberman PM: Coordinate Regulation of TET2 and EBNA2 Control DNA Methylation State of Latent Epstein-Barr Virus. J Virol 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kenney SC, Mertz JE: Regulation of the latent-lytic switch in Epstein-Barr virus. Semin Cancer Biol 2014, 26:60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramasubramanyan S, Kanhere A, Osborn K, Flower K, Jenner RG, Sinclair AJ: Genome-wide analyses of Zta binding to the Epstein-Barr virus genome reveals interactions in both early and late lytic cycles and an epigenetic switch leading to an altered binding profile. J Virol 2012, 86:1249412502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miller G, El-Guindy A, Countryman J, Ye J, Gradoville L: Lytic cycle switches of oncogenic human gammaherpesviruses. Adv Cancer Res 2007, 97:81–109. [DOI] [PubMed] [Google Scholar]
- 30.Lyons DE, Yu KP, Vander Heiden JA, Heston L, Dittmer DP, El-Guindy A, Miller G: Mutant cellular AP1 proteins promote expression of a subset of Epstein-Barr virus late genes in the absence of lytic viral DNA replication. J Virol 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.El-Guindy A, Ghiassi-Nejad M, Golden S, Delecluse HJ, Miller G: Essential role of Rta in lytic DNA replication of Epstein-Barr virus. J Virol 2013, 87:208–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woellmer A, Arteaga-Salas JM, Hammerschmidt W: BZLF1 governs CpG-methylated chromatin of Epstein-Barr Virus reversing epigenetic repression. PLoS Pathog 2012, 8:e1002902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zalani S, Holley-Guthrie E, Kenney S: Epstein-Barr viral latency is disrupted by the immediate-early BRLF1 protein through a cell-specific mechanism. Proc Natl Acad Sci U S A 1996, 93:9194–9199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ragoczy T, Heston L, Miller G: The Epstein-Barr virus Rta protein activates lytic cycle genes and can disrupt latency in B lymphocytes. J Virol 1998, 72:7978–7984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woellmer A, Hammerschmidt W: Epstein-Barr virus and host cell methylation: regulation of latency, replication and virus reactivation. Curr Opin Virol 2013, 3:260–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wille CK, Nawandar DM, Henning AN, Ma S, Oetting KM, Lee D, Lambert P, Johannsen EC, Kenney SC: 5-hydroxymethylation of the EBV genome regulates the latent to lytic switch. Proc Natl Acad Sci U S A 2015, 112:E7257–7265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li X, Bhaduri-McIntosh S: A Central Role for STAT3 in Gammaherpesvirus-Life Cycle and -Diseases. Front Microbiol 2016, 7:1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li X, Burton EM, Koganti S, Zhi J, Doyle F, Tenenbaum SA, Horn B, Bhaduri-McIntosh S: KRAB-ZFP Repressors Enforce Quiescence of Oncogenic Human Herpesviruses. J Virol 2018, 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laichalk LL, Thorley-Lawson DA: Terminal differentiation into plasma cells initiates the replicative cycle of Epstein-Barr virus in vivo. J Virol 2005, 79:1296–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones RJ, Iempridee T, Wang X, Lee HC, Mertz JE, Kenney SC, Lin HC, Baladandayuthapani V, Dawson CW, Shah JJ, et al. : Lenalidomide, Thalidomide, and Pomalidomide Reactivate the Epstein-Barr Virus Lytic Cycle through Phosphoinositide 3-Kinase Signaling and Ikaros Expression. Clin Cancer Res 2016, 22:4901–4912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu X, Cohen JI: The role of PI3K/Akt in human herpesvirus infection: From the bench to the bedside. Virology 2015, 479-480:568–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iempridee T, Reusch JA, Riching A, Johannsen EC, Dovat S, Kenney SC, Mertz JE: Epstein-Barr virus utilizes Ikaros in regulating its latent-lytic switch in B cells. J Virol 2014, 88:4811–4827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reusch JA, Nawandar DM, Wright KL, Kenney SC, Mertz JE: Cellular differentiation regulator BLIMP1 induces Epstein-Barr virus lytic reactivation in epithelial and B cells by activating transcription from both the R and Z promoters. J Virol 2015, 89:1731–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Setz CS, Hug E, Khadour A, Abdelrasoul H, Bilal M, Hobeika E, Jumaa H: PI3K-Mediated Blimp-1 Activation Controls B Cell Selection and Homeostasis. Cell Rep 2018, 24:391–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McHugh D, Caduff N, Barros MHM, Ramer PC, Raykova A, Murer A, Landtwing V, Quast I, Styles CT,Spohn M, et al. : Persistent KSHV Infection Increases EBV-Associated Tumor Formation In Vivo via Enhanced EBV Lytic Gene Expression. Cell Host Microbe 2017, 22:61–73 e67. [DOI] [PubMed] [Google Scholar]
- 46.Whyte WA, Orlando DA, Hnisz D, Abraham BJ, Lin CY, Kagey MH, Rahl PB, Lee TI, Young RA: Master transcription factors and mediator establish super-enhancers at key cell identity genes. Cell 2013, 153:307–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hnisz D, Schuijers J, Lin CY, Weintraub AS, Abraham BJ, Lee TI, Bradner JE, Young RA: Convergence of developmental and oncogenic signaling pathways at transcriptional super-enhancers. Mol Cell 2015, 58:362–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou H, Schmidt SC, Jiang S, Willox B, Bernhardt K, Liang J, Johannsen EC, Kharchenko P, Gewurz BE,Kieff E, et al. : Epstein-Barr virus oncoprotein super-enhancers control B cell growth. Cell Host Microbe 2015, 17:205–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhao B, Barrera LA, Ersing I, Willox B, Schmidt SC, Greenfeld H, Zhou H, Mollo SB, Shi TT, Takasaki K,et al. : The NF-kappaB genomic landscape in lymphoblastoid B cells. Cell Rep 2014, 8:15951606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tang Z, Luo OJ, Li X, Zheng M, Zhu JJ, Szalaj P, Trzaskoma P, Magalska A, Wlodarczyk J, Ruszczycki B,et al. : CTCF-Mediated Human 3D Genome Architecture Reveals Chromatin Topology for Transcription. Cell 2015, 163:1611–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jiang S, Zhou H, Liang J, Gerdt C, Wang C, Ke L, Schmidt SCS, Narita Y, Ma Y, Wang S, et al. : The Epstein-Barr Virus Regulome in Lymphoblastoid Cells. Cell Host Microbe 2017, 22:561–573 e564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ma Y, Walsh MJ, Bernhardt K, Ashbaugh CW, Trudeau SJ, Ashbaugh IY, Jiang S, Jiang C, Zhao B, Root DE, et al. : CRISPR/Cas9 Screens Reveal Epstein-Barr Virus-Transformed B Cell Host Dependency Factors. Cell Host Microbe 2017, 21:580–591 e587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wood CD, Carvell T, Gunnell A, Ojeniyi OO, Osborne C, West MJ: Enhancer control of miR-155 expression in Epstein-Barr virus infected B cells. J Virol 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Glaser LV, Rieger S, Thumann S, Beer S, Kuklik-Roos C, Martin DE, Maier KC, Harth-Hertle ML,Gruning B, Backofen R, et al. : EBF1 binds to EBNA2 and promotes the assembly of EBNA2 chromatin complexes in B cells. PLoS Pathog 2017, 13:e1006664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wood CD, Veenstra H, Khasnis S, Gunnell A, Webb HM, Shannon-Lowe C, Andrews S, Osborne CS,West MJ: MYC activation and BCL2L11 silencing by a tumour virus through the large-scale reconfiguration of enhancer-promoter hubs. Elife 2016, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Banerjee S, Lu J, Cai Q, Saha A, Jha HC, Dzeng RK, Robertson ES: The EBV Latent Antigen 3C Inhibits Apoptosis through Targeted Regulation of Interferon Regulatory Factors 4 and 8. PLoS Pathog 2013, 9:e1003314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lu F, Chen HS, Kossenkov AV, DeWispeleare K, Won KJ, Lieberman PM: EBNA2 Drives Formation of New Chromosome Binding Sites and Target Genes for B-Cell Master Regulatory Transcription Factors RBP-jkappa and EBF1. PLoS Pathog 2016, 12:e1005339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McClellan MJ, Wood CD, Ojeniyi O, Cooper TJ, Kanhere A, Arvey A, Webb HM, Palermo RD, HarthHertle ML, Kempkes B, et al. : Modulation of enhancer looping and differential gene targeting by Epstein-Barr virus transcription factors directs cellular reprogramming. PLoS Pathog 2013, 9:e1003636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liang J, Zhou H, Gerdt C, Tan M, Colson T, Kaye KM, Kieff E, Zhao B: Epstein-Barr virus superenhancer eRNAs are essential for MYC oncogene expression and lymphoblast proliferation. Proc Natl Acad Sci U S A 2016, 113:14121–14126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Szymula A, Palermo RD, Bayoumy A, Groves IJ, Ba Abdullah M, Holder B, White RE: Epstein-Barr virus nuclear antigen EBNA-LP is essential for transforming naive B cells, and facilitates recruitment of transcription factors to the viral genome. PLoS Pathog 2018, 14:e1006890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang C, Zhou H, Xue Y, Liang J, Narita Y, Gerdt C, Zheng AY, Jiang R, Trudeau S, Peng CW, et al. : Epstein-Barr Virus Nuclear Antigen Leader Protein Coactivates EP300. J Virol 2018, 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pei Y, Banerjee S, Jha HC, Sun Z, Robertson ES: An essential EBV latent antigen 3C binds Bcl6 for targeted degradation and cell proliferation. PLoS Pathog 2017, 13:e1006500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Patil A, Manzano M, Gottwein E: CK1alpha and IRF4 are essential and independent effectors of immunomodulatory drugs in primary effusion lymphoma. Blood 2018, 132:577–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang A, Welch R, Zhao B, Ta T, Keles S, Johannsen E: Epstein-Barr Virus Nuclear Antigen 3 (EBNA3) Proteins Regulate EBNA2 Binding to Distinct RBPJ Genomic Sites. J Virol 2015, 90:2906–2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jiang S, Willox B, Zhou H, Holthaus AM, Wang A, Shi TT, Maruo S, Kharchenko PV, Johannsen EC, Kieff E, et al. : Epstein-Barr virus nuclear antigen 3C binds to BATF/IRF4 or SPI1/IRF4 composite sites and recruits Sin3A to repress CDKN2A. Proc Natl Acad Sci U S A 2014, 111:421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schmidt SC, Jiang S, Zhou H, Willox B, Holthaus AM, Kharchenko PV, Johannsen EC, Kieff E, Zhao B: Epstein-Barr virus nuclear antigen 3A partially coincides with EBNA3C genome-wide and is tethered to DNA through BATF complexes. Proc Natl Acad Sci U S A 2015, 112:554–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Allday MJ: EBV finds a polycomb-mediated, epigenetic solution to the problem of oncogenic stress responses triggered by infection. Front Genet 2013, 4:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Styles CT, Bazot Q, Parker GA, White RE, Paschos K, Allday MJ: EBV epigenetically suppresses the B cell-to-plasma cell differentiation pathway while establishing long-term latency. PLoS Biol 2017, 15:e2001992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Murer A, McHugh D, Caduff N, Kalchschmidt J, Barros M, Zbinden A, Capaul R, Niedobitek G, Allday M, Chijioke O, et al. : EBV persistence without its EBNA3A and 3C oncogenes in vivo. PLoS Pathog 2018, 14:e1007039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Minamitani T, Yasui T, Ma Y, Zhou H, Okuzaki D, Tsai CY, Sakakibara S, Gewurz BE, Kieff E, Kikutani H: Evasion of affinity-based selection in germinal centers by Epstein-Barr virus LMP2A. Proc Natl Acad Sci U S A 2015, 112:11612–11617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Minamitani T, Ma Y, Zhou H, Kida H, Tsai CY, Obana M, Okuzaki D, Fujio Y, Kumanogoh A, Zhao B, et al. : Mouse model of Epstein-Barr virus LMP1- and LMP2A-driven germinal center B-cell lymphoproliferative disease. Proc Natl Acad Sci U S A 2017, 114:4751–4756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wirtz T, Weber T, Kracker S, Sommermann T, Rajewsky K, Yasuda T: Mouse model for acute EpsteinBarr virus infection. Proc Natl Acad Sci U S A 2016, 113:13821–13826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vrzalikova K, Leonard S, Fan Y, Bell A, Vockerodt M, Flodr P, Wright KL, Rowe M, Tao Q, Murray PG: Hypomethylation and Over-Expression of the Beta Isoform of BLIMP1 is Induced by EpsteinBarr Virus Infection of B Cells; Potential Implications for the Pathogenesis of EBV-Associated Lymphomas. Pathogens 2012, 1:83–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ma J, Nie K, Redmond D, Liu Y, Elemento O, Knowles DM, Tam W: EBV-miR-BHRF1–2 targets PRDM1/Blimp1: potential role in EBV lymphomagenesis. Leukemia 2016, 30:594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mancao C, Hammerschmidt W: Epstein-Barr virus latent membrane protein 2A is a B-cell receptor mimic and essential for B-cell survival. Blood 2007, 110:3715–3721. [DOI] [PMC free article] [PubMed] [Google Scholar]