Abstract
Purpose:
Medication-related osteonecrosis of the jaws (MRONJ) is a known complication of antiresorptive medications with surgical and nonsurgical treatment options. The aim of this study was to evaluate the effectiveness of nonsurgical therapy using local wound care on management of MRONJ lesions.
Materials and Methods:
The authors conducted a retrospective cohort study of patients who presented to the University of California–Los Angeles School of Dentistry Oral and Maxillofacial Surgery Clinic for evaluation and treatment of MRONJ. The primary predictor variable was wound care score; secondary predictors were demographics (age, gender), anatomic location, primary condition, and type and time of antiresorptive treatment. Outcomes assessed were disease resolution and time to disease resolution. Statistical analysis was carried out using the Spearman correlation for continuous and ordinal variables or the χ2 test for categorical variables. Time-to-event statistics and Cox proportional hazards models were calculated; a Kaplan-Meier plot was generated to assess time to healing.
Results:
One hundred six patients with 117 MRONJ lesions were treated using local wound care; complete disease resolution was observed 71% of lesions, with an additional 22% of lesions undergoing disease improvement. Wound care score was statistically associated with disease resolution and time to resolution, whereas demographics, anatomic site, condition, and type and time of antiresorptive treatment had no effect on resolution.
Conclusion:
Local wound care increased the likelihood of MRONJ resolution and decreased the time to disease resolution. This strategy can be used in patients who cannot undergo surgery and should be implemented in all patients with MRONJ lesions who are managed nonsurgically.
Antiresorptive agents, such as bisphosphonates and denosumab, are commonly used to treat osteoporosis and bone malignancies.1,2 Although the therapeutic effects have long been documented, side effects, specifically medication-related osteonecrosis of the jaws (MRONJ), can be serious and devastating.3 MRONJ is defined as exposed bone in the oral and maxillofacial region for at least 8 weeks in the presence of antiresorptive or antiangiogenic agents without any history of radiation.4,5
Osteoporosis and low bone density affect more than 50 million Americans older than 50 years, leading to at least 2 million osteoporotic-related fractures.6,7 With the risk of MRONJ in osteoporotic patients estimated at 0.001 to 0.15%, the use of antiresorptive agents in these patients is warranted.5 Similarly, antiresorptive agents have been very effective in decreasing skeletal-related events in patients with cancer.8,9 However, the incidence of MRONJ increases to 1 to 16% in patients on oncologic doses of bisphosphonates or denosumab.5,10 Although antiresorptive agents are central in the management of osteoporosis and osseous malignancy, recent studies have shown that MRONJ markedly decreases quality of life in many affected patients.8,11,12
Once MRONJ is established, current therapies vary and are often dictated by the preference of the treating clinician, as shown by numerous treatment approaches in the literature.13–18 The American Association of Oral and Maxillofacial Surgeons (AAOMS) treatment guidelines include antibacterial mouth rinse and pain control debridement for stages 0 and 1; the more advanced stages 2 and 3 are treated by surgical debridement or resection.4 The American Society for Bone and Mineral Research International Task Force on Osteonecrosis of the Jaws also recommends nonsurgical therapy, reserving surgical therapy for more severe refractory cases.5 Although these clinical guidelines exist, several studies advocate debridement or surgical resection regardless of disease stage, with success rates ranging from 53 to 92%.14–16,19–22 However, more aggressive surgical approaches might not consider the morbidity associated with surgery in medically compromised patients. Studies of nonsurgical treatment also exist, with disease resolution ranging from 18 to 90%.17,18 An overall challenge in comparing clinical approaches in the management of MRONJ is the definition of disease resolution, which can vary from the absence of symptoms to complete mucosal epithelization.
The authors present an alternative approach to traditional nonsurgical therapy and surgical debridement or resection, focusing on local wound care of MRONJ lesions. Disease resolution was defined as complete mucosal coverage, assessed clinically, and lack of bony sequestrum, assessed radiographically. The purpose of this study was to investigate the effectiveness of nonsurgical therapy using local wound care on management of MRONJ. The authors hypothesized that nonsurgical therapy using local wound care could lead to successful disease resolution in patients with MRONJ lesions. The specific aim of this study was to measure the effectiveness of local wound care on disease resolution.
Materials and Methods
STUDY DESIGN AND SAMPLE
To address the research question, the authors designed and implemented a retrospective cohort study. The study population was composed of all patients presenting to a single clinician (T.L.A.) at the University of California–Los Angeles (UCLA) School of Dentistry Oral and Maxillofacial Surgery Clinic for evaluation and treatment of MRONJ from June 2008 through July 2017. To be included in the study sample, patients had to be 1) diagnosed with MRONJ, confirmed clinically and radiographically, according to AAOMS guidelines and 2) return for follow-up appointments at the designated recall interval. Exclusion criteria were 1) a failure to return for follow-up appointments (>3 consecutive appointments missed) and 2) a pathologic fracture of the mandible at the initial consultation appointment.
STUDY VARIABLES
The primary predictor variable measured in this study was local wound care score. MRONJ lesions were assessed for the presence of bleeding at the affected site and plaque accumulation on the exposed bone. A scale of 1 to 3 was used for bleeding and plaque accumulation, with scores 1, 2, and 3 representing mild, moderate, and severe, respectively. An overall wound care score from 1 to 6 was assigned by compiling the data measured (points for bleeding + points for plaque accumulation = total wound score). The wound care score used was obtained from the most recent clinic visit. If disease resolution occurred, then the score from the visit before healing was used. Secondary variables assessed were demographics (age, gender), anatomic location, primary condition, and type and time of antiresorptive treatment.
The primary outcome factors evaluated were resolution of disease and time to disease resolution. Disease resolution was defined categorically as disease progression, improvement, or resolution. Disease progression was defined as an increase in disease stage, a larger area of infection or necrotic bone, an increase in inflammation or infection of the exposed area, or pathologic fracture. Disease improvement was defined as lesser disease stage or a decreased area of inflammation or infection. Disease resolution was defined as complete mucosal coverage with a lack of exposed necrotic bone. Time to disease resolution was assessed, defined as a length of time, in months. In patients with disease resolution, this time was defined as the number of months needed for resolution of the disease. In patients without resolution, this was defined as the number of months from the initial clinic visit until the last noted clinical visit.
PATIENT MANAGEMENT AND DATA COLLECTION METHODS
Patients were treated using the AAOMS guidelines, with modifications. No surgical intervention was performed other than removal of a detached mobile sequestrum. Instead, local wound care, defined as mechanical vigorous debridement and cleaning of exposed bone, was used. All patients, at each appointment, regardless of staging or disease progression, were educated on the importance of oral hygiene, including local wound care, and routine dental care. Non-restorable teeth were referred for endodontic treatment, and the crown was sectioned at the gingival level.
Patients were prescribed an antibacterial solution (chlorhexidine 0.12%) but instructed to perform local wound care instead of oral lavage. Specifically, they were instructed to dip a cotton swab or small toothbrush in the chlorhexidine solution and then vigorously and mechanically clean, scrub, and debride the exposed bone or fistula to remove all visible plaque and debris. The clinician confirmed patient understanding after a brief demonstration. Patients were informed that discomfort, bleeding, and irritation, when cleaning, are expected and will subside with continued treatment when inflammation or infection decreases. This information also was relayed to a primary caregiver or family members if the patient was physically limited or a lack of compliance was noted at subsequent appointments. Patients who received antibiotics were given a 3-week regimen of amoxicillin (500 mg orally 3 times per day); if they were allergic to penicillin, then doxycycline (100 mg orally twice per day) was prescribed. A follow-up interval of 1, 2, or 3 months was determined based on disease stage and symptomatology.
Patients with stage 1 and exposed bone but no evidence of infection were given chlorhexidine to be used for local wound care. Patients with stages 2 and 3 and exposed bone, infection, and pain were given a course of antibiotics, analgesic medications, and chlorohexidine to be used for local wound care. Patients did not receive any other medications or growth factors.
Patient records were de-identified before data collection. The records were examined for demographics; underlying condition; type, duration, and dose of antiresorptive use; clinical staging; and sites of disease. Antiresorptive medications were discontinued in only 3 patients (with stage 1 MRONJ for osteoporosis) according to the recommendation of their primary doctor. All others remained on bisphosphonates or denosumab.
DATA ANALYSES
Patient characteristics were compared for healing status (complete, improvement, or progression) using Spearman correlation for continuous and ordinal variables (eg, age, stage) or χ2 test for categorical variables (Tables 1,2). Time to complete healing was compared using Cox proportional hazards (Cox PH) models and summarized against each effect with the estimated hazard ratio (95% confidence interval). A full Cox PH model was completed using all terms (Table 3) to see whether wound score remained relevant after accounting for all other measured patient characteristics. A Kaplan-Meier plot was generated to assess the time to healing in patients with high (≥3) versus low (<3) wound scores (Fig 1). Statistical analyses were run using IBM SPSS 25 (IBM Corp, Armonk, NY). P values less than .05 were considered statistically significant.
Table 1.
VARIABLES ASSOCIATED WITH DISEASE RESOLUTION AND TIME TO RESOLUTION
| Healing Status | Time to Resolution | |||||
|---|---|---|---|---|---|---|
| Complete Resolution |
Disease Improvement |
Disease Progression |
P Value | Cox Hazard Ratio (95% CI) | Cox P Value | |
| Age (yr) | 72.0 | 71.6 | 70.4 | .489 | 1.00 (0.98–1.02) | .772 |
| Gender, n (%) | .176 | 0.81 (0.49–1.65) | .424 | |||
| Women | 63 (76) | 15 (18) | 5 (6) | |||
| Men | 20 (59) | 10 (29) | 4 (12) | |||
| Anatomic site, n (%) | .949 | 1.01 (0.64–1.59) | .968 | |||
| Maxilla | 30 (70) | 10 (23) | 3 (7) | |||
| Mandible | 53 (72) | 15 (20) | 6 (8) | |||
| Condition, n (%) | .487 | 1.20 (0.77–1.87) | .417 | |||
| Osteoporosis | 34 (75) | 7 (16) | 4 (9) | |||
| Malignancy | 49 (68) | 18 (25) | 5 (7) | |||
| Antiresorptive drug, n (%) | .079 | 0.80 (0.45–1.40) | .434 | |||
| Bisphosphonate | 65 (67) | 24 (24) | 9 (9) | |||
| Alendronate | 31 (72) | 10 (23) | 2 (5) | |||
| Zoledronate | 31 (62) | 13 (26) | 6 (12) | |||
| Other | 3 (60) | 1 (20) | 1 (20) | |||
| Denosumab | 16 (94) | 1 (6) | 0 | |||
| Prolia* | 10 (100) | 0 | 0 | |||
| Xgeva* | 6 (86) | 1 (14) | 0 | |||
| Unknown | 2 (100) | 0 | 0 | |||
| Staging, n (%) | .452 | 0.82 (0.58–1.18) | .286 | |||
| Stage 1 | 47 (72) | 16 (25) | 2 (3) | |||
| Stage 2 | 32 (70) | 9 (20) | 5 (10) | |||
| Stage 3 | 4 (67) | 0 | 2 (33) | |||
| Time on antiresorptive drug (yr) | 5.5 | 3.7 | 4.8 | .819 | 1.01 (0.96–1.06) | .806 |
| Inciting event, n (%) | .269 | — | .686 | |||
| Extraction | 50 (76) | 10 (15) | 6 (9) | |||
| Spontaneous | 16 (68) | 9 (32) | 0 | |||
| Dental disease | 7 (64) | 3 (27) | 1 (9) | |||
| Implant | 7 (64) | 2 (18) | 2 (18) | |||
| Denture | 3 (75) | 1 (25) | 0 | |||
| Wound care score | 2.4 | 3.7 | 4.8 | <.001 | 0.32 (0.22–0.46) | <.001 |
Abbreviation: CI, confidence interval.
Amgen, Inc (Thousand Oaks, CA).
Table 2.
VARIABLES ASSOCIATED WITH WOUND CARE SCORE
| Variable | Spearman | P Value |
|---|---|---|
| Age | −0.07 | .433 |
| Gender | 0.13 | .164 |
| Anatomic site | 0.00 | .981 |
| Condition | −0.10 | .268 |
| Antiresorptive drug | 0.10 | .291 |
| Stage | −0.05 | .595 |
Table 3.
FULL COX PROPORTIONAL HAZARDS MODEL
| Variable | Hazard Ratio (95% CI) | P Value |
|---|---|---|
| Age | 0.99 (0.97–1.01) | .433 |
| Gender | 1.06 (0.59–1.88) | .583 |
| Site | 1.22 (0.75–2.01) | .424 |
| Condition | 1.15 (0.61–2.17) | .656 |
| Antiresorptive drug | 1.06 (0.59–1.91) | .841 |
| Stage | 0.65 (0.41–1.01) | .057 |
| Wound care score | 0.29 (0.20–0.44) | <.001 |
Abbreviation: CI, confidence interval.
FIGURE 1.
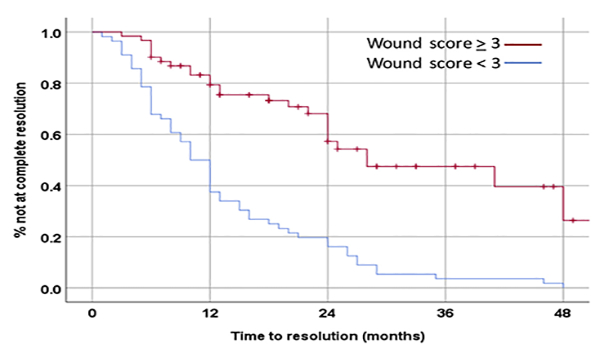
Kaplan-Meier plot of disease resolution status based on wound care score. Poor (≥3) and good (<3) wound care scores were used to assess the percentage of patients with unresolved lesions. Red line represents the percentage of lesions without disease resolution as a function of time in patients with poor wound care scores (≥3). Blue line represents the percentage of lesions without disease resolution as a function of time in patients with good wound care scores (<3).
Results
PATIENT POPULATION AND DEMOGRAPHICS
One hundred six patients with 117 MRONJ sites were included in this retrospective study (Table 1). The average patient age was 71.7 years. Age had no statistically relevant effect on disease resolution. Seventy-one percent of lesions were seen in women; gender had no effect on disease resolution. Similarly, MRONJ prevalence was greater in the mandible. There was no effect on disease resolution based on anatomic location. Sixty-two percent of lesions occurred in patients taking antiresorptive medications for bone malignancies, and the remaining lesions were in osteoporotic patients. The underlying condition had no effect on disease resolution.
Most patients had been treated with a bisphospho-nate, whereas only 15% had taken denosumab. No statistical difference in resolution was observed based on antiresorptive treatment. Interestingly, the duration of antiresorptive treatment had no effect on resolution status. Although most MRONJ lesions resulted from tooth extraction, all lesions healed equally, with no difference among inciting events. At initial presentation, most lesions were stage 1. However, disease stage did not have an effect on disease resolution. Of note, 1 patient with a stage 3 MRONJ lesion in the mandible had a pathologic fracture after 2.5 years of local wound care; however, this patient had very poor compliance with home wound care (score, 6) at all follow-up appointments.
Of importance, wound care score was the only variable associated with disease resolution. Patients with disease resolution had an average wound care score of 2.4, indicating mild levels of plaque and bleeding. In patients with refractory lesions, the average wound care score was 4.8, indicating high levels of bleeding and plaque accumulation. Interestingly, patients with disease improvement had an intermediate score of 3.7. Wound care score was strongly associated with disease resolution (P < .001). Wound care was not associated with any other patient characteristic (Table 2). After adjusting for other patient demographics, wound care score remained highly statistically associated with disease resolution and time to resolution (Table 3). Using Kaplan-Meier analysis, time to resolution was calculated. Patients with good wound care scores (<3) healed at a much faster rate than those with poor wound care scores (≥3). At 24 months of treatment, only 20% of patients with good wound care (score, <3) had unresolved lesions, whereas 60% of those with poor wound care (score, ≥3) had unresolved lesions (Fig 1).
CLINICAL AND RADIOGRAPHIC MANIFESTATIONS OF REPRESENTATIVE CASE
Patient With Stage 2 MRONJ
A 68-year-old man presented to the clinic with complaints of pain and purulent drainage for 8 months after extraction of the right second mandibular molar. On examination, exposed bone on the mucosa lingual to the missing second mandibular molar was noted with associated pain, erythema, and bleeding (Fig 2A). Radiographically, areas of irregular cortication, diffuse trabecular sclerosis, and lack of remodeling were noted in the extraction socket of the missing tooth. However, no bony sequestrum was seen radio-graphically (Fig 2D-D2). After 9 months of wound care, a large area of sequestrum exfoliated, showing epithelized mucosa on the undersurface of the bone (Fig 2B). The underlying tissue was fully epithelized at the 1-week follow-up visit (Fig 2C). The follow-up radiograph displayed a well-defined defect in the socket of the missing mandibular molar, with no evidence of further sequestrum formation (Fig 2E-E2). However, sclerotic and lytic bone changes of the mandible were still apparent, with loss of bony support of the adjacent first mandibular molar.
FIGURE 2.
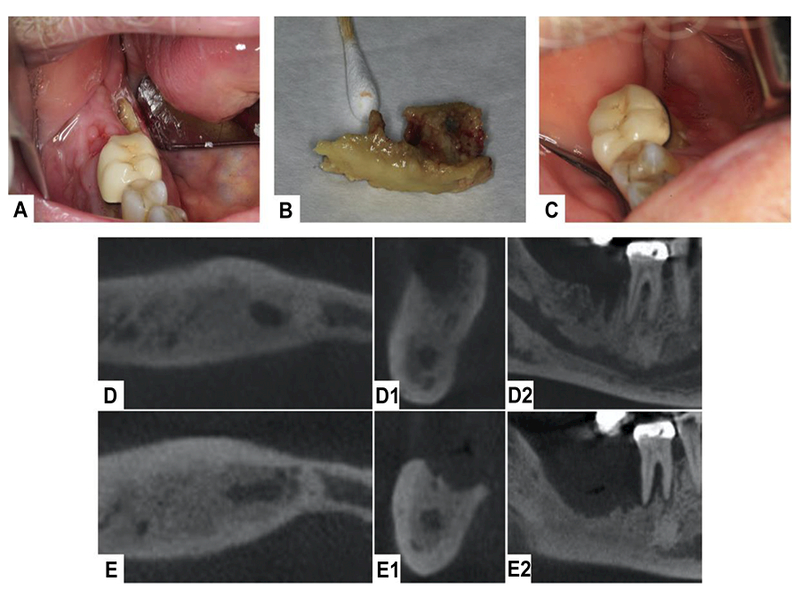
Clinical and radiographic presentation of a patient with stage 2 medication-related osteonecrosis of the jaws. A, Initial clinical presentation shows a small area of bone exposure on the lingual mucosa of the mandibular posterior teeth. B, Exfoliation of necrotic bone after local wound care. C, Clinical healing after exfoliation of necrotic bone. D, D1, D2, Cone-beam computed tomographic examination at the time of initial presentation depicts sclerotic changes in the area of the right posterior mandible, with an unhealed extraction socket. E, E1, E2, Radiographic examination after sequestration shows a well-defined osseous defect, with increased sclerosis and lytic changes, and a loss of periodontal support around the adjacent first mandibular molar.
Discussion
The authors performed a retrospective analysis of local wound care, a novel nonsurgical treatment, for the management of MRONJ lesions. The purpose of this study was to evaluate whether nonsurgical therapy using local wound care could be effective in the treatment of MRONJ lesions. The authors hypothesized that local wound care could lead to disease resolution without the need for surgery in patients with MRONJ. Using local wound care, 71% of MRONJ lesions resolved completely, with an additional 22% showing disease improvement. Specifically, the data show that this nonsurgical management protocol is effective for MRONJ treatment. Indeed, patients with better wound care scores had complete disease resolution at a faster rate than those with poor wound care.
Although studies of MRONJ treatment exist, none focus on local wound care for MRONJ lesions, despite the well-established associations of poor oral hygiene and biofilm with MRONJ development.17,23–25 Similarly, preventative dental measures before antiresorptive treatment are of the utmost importance and known to attenuate MRONJ development.26,27 From these observations, the authors’ treatment protocol centered on local wound care of exposed necrotic bone. Current AAOMS treatment guidelines advocate the use of chlorhexidine as an oral lavage.4 However, this lavage does not remove biofilm from the exposed bone, which acts as a continued source of irritation, inflammation, and often infection. For these reasons, patients in this study were instructed to use a cotton swab or small toothbrush dipped in chlorhexidine and to remove all plaque and debris from the exposed bone, which was defined as local wound care.
To assess the patient’s wound care, the authors assigned a cumulative score measured by the presence of bleeding and plaque. Of importance, patients with disease resolution had a markedly lower wound care score, indicating low levels of plaque and bleeding. In contrast, patients who had refractory disease displayed considerably more bleeding and plaque. Furthermore, patients with better wound care scores underwent disease resolution at a faster rate, with 60% of lesions completely healing within the first year. By 2 years of treatment, disease resolution had been obtained in 80% of patients with good wound care scores. In contrast, patients with poor wound care did not undergo disease resolution at a similar rate. At 1 year of treatment, only 20% of lesions had resolved; at 2 years of treatment, only 40% of lesions had resolved. This suggests that oral hygiene, specifically local wound care of MRONJ lesions, is extremely important for disease resolution in patients with established MRONJ.
In this study, demographics, anatomic site, underlying condition, disease stage, and length and type of antiresorptive treatment had no effect on disease resolution. Initial disease stage had no meaningful effect on resolution. Interestingly, 94% of lesions (16 of 17) in patients on denosumab resolved. Although there are known differences in the pharmacologic effects of bisphosphonates and denosumab, no conclusions can be made because of the small sample of these patients.28,29 Similarly, only 6 patients presented with stage 3 MRONJ lesions; as such, any conclusions made for the treatment of these patients should be limited.
Importantly, disease resolution in the present patients resulted from sequestration of the offending bone, with only 5% of resolved lesions recurring. In addition, wound care therapy duration was shorter for patients who initially presented with radiographic sequestra compared with patients without obvious radiographic signs. Local wound care eliminates the noxious inflammatory environment surrounding exposed bone. In addition, follow-up cone-beam computed tomograms showed that osseous changes, including dense trabeculation, crater-like defects and periosteal bone formation, remained underneath the healed mucosa. These findings suggest that although osteoclast inhibition was central in the initial formation of MRONJ lesions, it was not required for subsequent mucosal healing after exfoliation of the sequestered necrotic bone. Because this abnormal osseous architecture remains under the healed mucosa, it would not be a suitable site for further surgical procedures, such as dental implant placement.
MRONJ management is largely empirical, often focused on treating symptoms, rather than complete disease resolution. Treatment decisions are frequently based on general guidelines, without prospective clinical trials to support a single mode of therapy.4 An increasing number of studies advocate surgical management, with disease resolution reported in 60 to 70% of cases.14–16,19–22 However, recurrence rates are widely varied or unreported.15,30 In addition, the risk of intra- and postoperative complications is increased during surgical treatment.31–34 It is important to note that metastatic cancer has been identified in MRONJ specimens in 5.3% of patients taking antiresorptive agents for malignancies.35 Although rare, this must be considered in patients who undergo nonsurgical therapy.
In contrast, studies of nonsurgical management are few in number and have been less effective in disease management. This is further complicated by varied definitions of disease resolution, such as mucosal healing, lack of symptoms, or disease improvement. Lerman et al36 reported 23% re-epithelization; another study defined disease resolution only as the absence of pain, rather than mucosal healing, which might not be considered true resolution.17 A more recent study reported 65% resolution, but these patients discontinued antiresorptive treatment, which might not be indicated for patients with malignancies or severe osteoporosis.37 A large multicenter study reported 25% disease resolution of 202 patients receiving nonsurgical treatment for MRONJ.38 Furthermore, a systematic review of 97 studies reported that nonsurgical medical management of MRONJ lesions led to resolution in 45% of cases.39 Although no single treatment approach is proven superior, the literature shows that complete disease resolution occurs more often after surgical intervention.38
Although complete disease resolution was achieved in 71% of patients, with an additional 22% undergoing disease improvement, there are limitations to this study. MRONJ is a rare event that occurs in a diverse patient population. Therefore, it is inevitable that this study would include a heterogeneous population. However, the large number of patients allows evaluation of several variables, including the specific antiresorptive agent, disease stage, and primary diagnosis. Similarly, the resolution times might under-represent total treatment time, because some patients were managed by other clinicians before presentation at the UCLA clinic. Furthermore, the retrospective nature of this study is subject to bias. Prospective studies with multiple treatment interventions (nonsurgical vs surgical) would be needed to establish the validity of this approach.
With the large sample and single treatment modality, this study showed that nonsurgical therapy using local wound care is a viable alternative to surgical intervention in patients with stage 1 and 2 disease or patients who cannot tolerate a major surgical procedure. Indeed, prospective studies using this approach will be conducted to confirm the present findings. Although MRONJ is a serious disease with major morbidity, the authors have provided an alternative therapy to surgical treatment that provides disease resolution in most patients. This can be easily implemented and shifts the focus of patient care.
Acknowledgments
This work was supported by grants from the National Institutes of Health/National Institute of Dental and Craniofacial Research (NIH/NIDCR; grant DE09465 to Dr Tetradis; grant DE021444 to Dr Aghaloo). Dr Hadaya was supported by NIH/NIDCR grant T90/R90 DE007296 and F30 DE028171.
Footnotes
Conflict of Interest Disclosures: Drs Tetradis and Aghaloo have served as paid consultants for and received grant support from Amgen, Inc. None of the other authors have a relevant financial relationship(s) with a commercial interest.
References
- 1.Camacho PM, Petak SM, Binkley N, et al. : American Association of Clinical Endocrinologists and American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2016. Endocr Pract 22:1, 2016 [DOI] [PubMed] [Google Scholar]
- 2.Kohno N, Aogi K, Minami H, et al. : Zoledronic acid significantly reduces skeletal complications compared with placebo in Japanese women with bone metastases from breast cancer: A randomized, placebo-controlled trial. J Clin Oncol 23:3314, 2005 [DOI] [PubMed] [Google Scholar]
- 3.Kennel KA, Drake MT: Adverse effects of bisphosphonates: Implications for osteoporosis management. Mayo Clin Proc 84: 632, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruggiero SL, Dodson TB, Fantasia J, et al. : American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 Update. J Oral Maxillofac Surg 72:1938, 2014 [DOI] [PubMed] [Google Scholar]
- 5.Khan AA, Morrison A, Hanley DA, et al. : International Task Force on Osteonecrosis of the Jaw. Diagnosis and management of osteonecrosis of the jaw: A systematic review and international consensus. J Bone Miner Res 30:3, 2015 [DOI] [PubMed] [Google Scholar]
- 6.Burge R, Dawson-Hughes B, Solomon DH, et al. : Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Wright NC, Looker AC, Saag KG, et al. : The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29:2520, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marcus R, Wong M, Heath H III, Stock JL: Antiresorptive treatment of postmenopausal osteoporosis: Comparison of study designs and outcomes in large clinical trials with fracture as an endpoint. Endocr Rev 23:16, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Van Poznak CH, Temin S, Yee GC, et al. : American Society of Clinical Oncology. American Society of Clinical Oncology executive summary of the clinical practice guideline update on the role of bone-modifying agents in metastatic breast cancer. J Clin Oncol 29:1221, 2011 [DOI] [PubMed] [Google Scholar]
- 10.Cafro AM, Barbarano L, Nosari AM, et al. : Osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates: Definition and management of the risk related to zoledronic acid. Clin Lymphoma Myeloma 8:111, 2008 [DOI] [PubMed] [Google Scholar]
- 11.Miksad RA, Lai KC, Dodson TB, et al. : Quality of life implications of bisphosphonate-associated osteonecrosis of the jaw. Oncolo-gist 16:121, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Capocci M, Romeo U, Guerra F, et al. : Medication-related osteo-necrosis of the jaws (MRONJ) and quality of life evaluation: A pilot study. Clin Ter 168:e253, 2017 [DOI] [PubMed] [Google Scholar]
- 13.Epstein MS, Wicknick FW, Epstein JB, et al. : Management of bisphosphonate-associated osteonecrosis: Pentoxifylline and tocopherol in addition to antimicrobial therapy. An initial case series. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110: 593, 2010 [DOI] [PubMed] [Google Scholar]
- 14.Ruggiero SL, Kohn N: Disease stage and mode of therapy are important determinants of treatment outcomes for medication-related osteonecrosis of the jaw. J Oral Maxillofac Surg 73:S94, 2015 [DOI] [PubMed] [Google Scholar]
- 15.Carlson ER, Basile JD: The role of surgical resection in the management of bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 67:85, 2009 [DOI] [PubMed] [Google Scholar]
- 16.Jacobsen C, Metzler P, Obwegeser JA, et al. : Osteopathology of the jaw associated with bone resorption inhibitors: What have we learned in the last 8 years? Swiss Med Wkly 142:w13605, 2012 [DOI] [PubMed] [Google Scholar]
- 17.Marx RE, Sawatari Y, Fortin M, Broumand V: Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: Risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg 63:1567, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Lazarovici TS, Yahalom R, Taicher S, et al. : Bisphosphonate-related osteonecrosis of the jaws: A single-center study of 101 patients. J Oral Maxillofac Surg 67:850, 2009 [DOI] [PubMed] [Google Scholar]
- 19.Kim HY, Lee SJ, Kim SM, et al. : Extensive surgical procedures result in better treatment outcomes for bisphosphonate-related osteonecrosis of the jaw in patients with osteoporosis. J Oral Maxillofac Surg 75:1404, 2017 [DOI] [PubMed] [Google Scholar]
- 20.Vescovi P, Campisi G, Fusco V, et al. : Surgery-triggered and non surgery-triggered Bisphosphonate-related Osteonecrosis of the Jaws (BRONJ): A retrospective analysis of 567 cases in an Italian multicenter study. Oral Oncol 47:191, 2011 [DOI] [PubMed] [Google Scholar]
- 21.Nisi M, La Ferla F, Karapetsa D, et al. : Conservative surgical management of patients with bisphosphonate-related osteonecrosis of the jaws: A series of 120 patients. Br J Oral Maxillofac Surg 54: 930, 2016 [DOI] [PubMed] [Google Scholar]
- 22.Graziani F, Vescovi P, Campisi G, et al. : Resective surgical approach shows a high performance in the management of advanced cases of bisphosphonate-related osteonecrosis of the jaws: A retrospective survey of 347 cases. J Oral Maxillofac Surg 70:2501, 2012 [DOI] [PubMed] [Google Scholar]
- 23.Vandone AM, Donadio M, Mozzati M, et al. : Impact of dental care in the prevention of bisphosphonate-associated osteonecrosis of the jaw: A single-center clinical experience. Ann Oncol 23:193, 2012 [DOI] [PubMed] [Google Scholar]
- 24.Vidal-Real C, Perez-Sayans M, Suarez-Penaranda JM, et al. : Osteo-necrosis of the jaws in 194 patients who have undergone intravenous bisphosphonate therapy in Spain. Med Oral Patol Oral Cir Bucal 20:e267, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kumar SK, Gorur A, Schaudinn C, et al. : The role of microbial biofilms in osteonecrosis of the jaw associated with bisphosphonate therapy. Curr Osteoporos Rep 8:40, 2010 [DOI] [PubMed] [Google Scholar]
- 26.Francini F, Pascucci A, Francini E, et al. : Osteonecrosis of the jaw in patients with cancer who received zoledronic acid and bevacizumab. J Am Dent Assoc 142:506, 2011 [DOI] [PubMed] [Google Scholar]
- 27.Migliorati CA, Schubert MM, Peterson DE, Seneda LM: Bisphosphonate-associated osteonecrosis of mandibular and maxillary bone: An emerging oral complication of supportive cancer therapy. Cancer 104:83, 2005 [DOI] [PubMed] [Google Scholar]
- 28.Drake MT, Clarke BL, Khosla S: Bisphosphonates: Mechanism of action and role in clinical practice. Mayo Clin Proc 83:1032, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baron R, Ferrari S, Russell RG: Denosumab and bisphosphonates: Different mechanisms of action and effects. Bone 48: 677, 2011 [DOI] [PubMed] [Google Scholar]
- 30.Klingelhoffer C, Zeman F, Meier J, et al. : Evaluation of surgical outcome and influencing risk factors in patients with medication-related osteonecrosis of the jaws. J Craniomaxillofac Surg 44:1694, 2016 [DOI] [PubMed] [Google Scholar]
- 31.Schrag C, Chang YM, Tsai CY, Wei FC: Complete rehabilitation of the mandible following segmental resection. J Surg Oncol 94: 538, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Seth R, Futran ND, Alam DS, Knott PD: Outcomes of vascularized bone graft reconstruction of the mandible in bisphosphonate-related osteonecrosis of the jaws. Laryngo-scope 120:2165, 2010 [DOI] [PubMed] [Google Scholar]
- 33.Vercruysse H Jr, Backer T, Mommaerts MY: Outcomes of osseous free flap reconstruction in stage III bisphosphonate-related osteonecrosis of the jaw: Systematic review and a new case series. J Craniomaxillofac Surg 42:377, 2014 [DOI] [PubMed] [Google Scholar]
- 34.Reich W, Bilkenroth U, Schubert J, et al. : Surgical treatment of bisphosphonate-associated osteonecrosis: Prognostic score and long-term results. J Craniomaxillofac Surg 43:1809, 2015 [DOI] [PubMed] [Google Scholar]
- 35.Carlson ER, Fleisher KE, Ruggiero SL: Metastatic cancer identified in osteonecrosis specimens of the jaws in patients receiving intravenous bisphosphonate medications. J Oral Maxillofac Surg 71:2077, 2013 [DOI] [PubMed] [Google Scholar]
- 36.Lerman MA, Xie W, Treister NS, et al. : Conservative management of bisphosphonate-related osteonecrosis of the jaws: Staging and treatment outcomes. Oral Oncol 49:977, 2013 [DOI] [PubMed] [Google Scholar]
- 37.Coropciuc RG, Grisar K, Aerden T, et al. : Medication-related osteonecrosis of the jaw in oncological patients with skeletal metastases: Conservative treatment is effective up to stage 2. Br J Oral Maxillofac Surg 55:787, 2017 [DOI] [PubMed] [Google Scholar]
- 38.Hayashida S, Soutome S, Yanamoto S, et al. : Evaluation of the treatment strategies for medication-related osteonecrosis of the jaws (MRONJ) and the factors affecting treatment outcome: A multicenter retrospective study with propensity score matching analysis. J Bone Miner Res 32:2022, 2017 [DOI] [PubMed] [Google Scholar]
- 39.Fliefel R, Troltzsch M, Kuhnisch J, et al. : Treatment strategies and outcomes of bisphosphonate-related osteonecrosis of the jaw (BRONJ) with characterization of patients: A systematic review. Int J Oral Maxillofac Surg 44:568, 2015 [DOI] [PubMed] [Google Scholar]


