Abstract
Propofol is an intravenous hypnotic drug that is used for induction and maintenance of sedation and general anaesthesia. It exerts its effects through potentiation of the inhibitory neurotransmitter γ-aminobutyric acid (GABA) at the GABAA receptor, and has gained widespread use due to its favourable drug effect profile. The main adverse effects are disturbances in cardiopulmonary physiology. Due to its narrow therapeutic margin, propofol should only be administered by practitioners trained and experienced in providing general anaesthesia. Many pharmacokinetic (PK) and pharmacodynamic (PD) models for propofol exist. Some are used to inform drug dosing guidelines, and some are also implemented in so-called target-controlled infusion devices, to calculate the infusion rates required for user-defined target plasma or effect-site concentrations. Most of the models were designed for use in a specific and well-defined patient category. However, models applicable in a more general population have recently been developed and published. The most recent example is the general purpose propofol model developed by Eleveld and colleagues. Retrospective predictive performance evaluations show that this model performs as well as, or even better than, PK models developed for specific populations, such as adults, children or the obese; however, prospective evaluation of the model is still required. Propofol undergoes extensive PK and PD interactions with both other hypnotic drugs and opioids. PD interactions are the most clinically significant, and, with other hypnotics, tend to be additive, whereas interactions with opioids tend to be highly synergistic. Response surface modelling provides a tool to gain understanding and explore these complex interactions. Visual displays illustrating the effect of these interactions in real time can aid clinicians in optimal drug dosing while minimizing adverse effects. In this review, we provide an overview of the PK and PD of propofol in order to refresh readers’ knowledge of its clinical applications, while discussing the main avenues of research where significant recent advances have been made.
Key Points
| Propofol is a potent intravenous hypnotic drug. It exerts its effects through potentiation of the inhibitory neurotransmitter, γ-Aminobutyric acid (GABA). Much experience with its clinical use has been amassed since it was introduced over three decades ago. |
| A general purpose pharmacokinetic (PK) and pharmacodynamic (PD) propofol model recently published by Eleveld and colleagues might replace PK/PD models currently used in clinical practice. |
| Defining the nature of interaction between propofol and other drugs remains a challenge. Response surface model studies can help to elucidate these interactions. |
Introduction
Propofol (2,6-diisopropylphenol) is a potent intravenous hypnotic drug that was developed by Imperial Chemical Industries Limited (London, UK), patented by John (Iain) Glen and Roger James in 1977 [1], and commercially launched in 1986 in Europe and 1989 in the US [2].
Like most anaesthetics, propofol is a γ-aminobutyric acid (GABA) receptor agonist. It has a favourable pharmacokinetic (PK) and pharmacodynamic (PD) profile, which has resulted in it becoming the most commonly used intravenous anaesthetic for the past three decades [2–7]. Rapid and smooth induction with nearly no excitation phenomena, relatively short context-sensitive time, rapid terminal half-life time and low incidence of postoperative nausea and vomiting (PONV) make it a very versatile hypnotic drug. It is used for sedation and anaesthesia for almost all types of surgery, but is particularly well-suited for anaesthesia in patients undergoing ambulatory [8] and neurosurgery where rapid psychomotor recovery are of upmost importance. Its efficacy and utility has also been proven for sedation of patients in the intensive care unit (ICU) [9] and conscious sedation of patients undergoing diagnostic or invasive procedures [10].
The adverse effects of propofol are well-documented, with the most common being pain on injection. Other adverse effects are cardiovascular (bradycardia, hypotension) and metabolic (hyperlipidaemia secondary to infusion of lipid formulation) [11].
Although propofol is well-established in clinical practice, there have been a number of studies published in recent years on the clinical use and pharmacology of the drug. The main aim of this narrative review is to refresh readers’ knowledge of the drug, it’s clinical uses, PK and PD, and to update the reader on the advances in two main fields of research, namely compartmental PK/PD modelling and drug interaction modelling of propofol.
Methods
A MEDLINE database search was performed using PubMed. The following ‘propofol’ Medical Subject Heading (MeSH) terms were used: ‘administration and dosage’ OR ‘adverse effects’ OR ‘blood’ OR ‘cerebrospinal fluid’ OR ‘chemical synthesis’ OR ‘chemistry’ OR ‘contraindications’ OR ‘metabolism’ OR ‘pharmacokinetics’ OR ‘pharmacology’ OR ‘physiology’ OR ‘poisoning’ OR ‘therapeutic use’ OR ‘toxicity’ OR ‘urine’. All articles published after 1 January 1985, in English, with full-text available and relating to human subjects were evaluated for relevancy. A full-text copy was obtained for all relevant publications. A further search of the bibliographies of all relevant articles was performed (also known as the snowball method) to identify any relevant publications missed during the initial search. Finally the ‘Google Scholar’ web search engine was used, with comparable search terms, to complete the literature search.
Drug Formulation
Propofol is insoluble in water [4]. It was first marketed in a formulation containing the surfactant Cremophor EL (polyethoxylated castor oil); however, the vehicle was soon changed to a lipid emulsion because of a high incidence of anaphylactic reactions, thought to be caused by Cremophor® [4]. The Diprivan® (AstraZeneca, London, UK) formulation of propofol came on to the market in 1989 in the US and is still available today worldwide. It is formulated as an Intralipid®-based emulsion (Fresenuis Kabi, Bad Homburg, Germany) and thus contains the same ingredients, namely soybean oil (100 mg/mL), glycerol (22.5 mg/mL), and egg lecithin (12 mg/mL), and of course propofol as the active ingredient [12]. After a series of reports of bacterial contamination of opened ampoules, ethylenediaminetetraacetic acid (EDTA; 0.05 mg/mL) was added to the formulation in 1996 [13], and is still sold in some but not all countries. The solution is isotonic, and neutral pH is achieved by adding sodium hydroxide. The pKa is 11.1 at 20 °C [14]. It has a melting point of 18 °C and should therefore be stored at room temperature. A number of different formulations of propofol are currently available, produced by many different manufacturers.
Most propofol formulations cause pain on injection, which is thought to be due to direct and indirect irritation of venous adventitia by free aqueous propofol through an interaction with TRPV1 and TRPA1 receptors [15, 16]. The free aqueous concentration of propofol is thought to be reduced when it is prepared in a solution containing more medium chain triglycerides than in Intralipid®. Therefore, some manufacturers produced and sold generic propofol formulations, such as Propoven® (Fresenius-Kabi, Bad Homburg, Germany) and Propofol-Lipuro® (B-Braun, Melsungen, Germany), containing more medium and fewer long chain-length fatty acids [17]. Although this reformulation of propofol has reduced the prevalence of pain on injection during the induction of anaesthesia, it still remains a problem in clinical practice [18].
Indications, Contraindications, Drug Dosing Regimen and Adverse Effects
Propofol is used for the induction and maintenance of the hypnotic component of sedation or general anaesthesia. Its use is contraindicated in two patient categories: (1) patients with hypersensitivity to propofol or any of the components of its formulation, and (2) patients with fat metabolism disorders. Since a small number of case reports of anaphylactic and anaphylactoid reactions have been published, the Diprivan® package insert also advises against Diprivan® use in patients with allergies to eggs, egg products, soy beans or soy products [19]. However, in two large retrospective studies, Asserhøj and colleagues were unable to confirm the link between propofol and food allergies [20].
Propofol should only be administered by healthcare professionals trained in the safe care of patients undergoing general anaesthesia. During any procedure involving sedation or anaesthesia with propofol, the anaesthetist should closely monitor, and act on any changes in, the patient’s physiological parameters according to the American Society of Anesthesiologists (ASA) guidelines on minimum monitoring standards [21]. Multiple propofol dosing schemes exist; however, due to considerable variability in the propofol dose necessary to achieve certain clinical endpoints, these should only be regarded as very approximate dosing guidelines. Propofol administration should always be titrated according to clinical effect, which is part of the reason why the clinician should closely monitor the effects and adverse effects of propofol (vide infra). In healthy adults younger than 55 years of age, the Diprivan® package insert advises an induction dose of 2–2.5 mg/kg, administered in boluses of 40 mg every 10 s, titrated to the onset of hypnotic effect, and a maintenance dose of 6–12 mg/kg/h. This dose should be adjusted (reduced) when propofol is administered to less-fit patients undergoing general anaesthesia, such as those fulfilling the ASA physical status categories ASA 3 or 4, or when propofol is used to induce and maintain sedation in critically ill patients in the ICU. For exact dosing guidelines, please refer to the package insert.
The main adverse effects of propofol administration relate to alterations of cardiopulmonary physiology, including loss of airway reflexes, hypoventilation or even apnoea, and hypotension. Any provider of anaesthesia should be trained in managing these adverse effects. A rare but serious adverse effect of propofol administration is the ‘propofol infusion syndrome’ (PRIS), which comprises severe metabolic acidosis, rhabdomyolysis, hyperkalaemia and cardiovascular collapse, and is frequently fatal. PRIS occurs mostly in the setting of prolonged and high-dose propofol infusion administration in children. The Diprivan® package insert advises against administration of propofol > 5 mg/kg/h for more than 48 h. Lastly, there are strong indications, mainly from animal studies [22] and retrospective clinical studies [23], that sedation with GABA agonistic drugs might be responsible for neurotoxicity in paediatric patients, resulting in long-term cognitive deficits; however, clinical significance of these findings is not known and further prospective studies are currently being conducted.
Pharmacokinetics (PK)
Absorption
Propofol is only suitable for intravenous use. It is not suitable for enteral or other routes of administration due to its bitter taste and low oral bioavailability caused by a high first-pass effect and the high hepatic extraction rate (> 90%) [24]. Some researchers have tried to increase the oral bioavailability of propofol, with some success, by administering it in nanoparticles, but this application remains experimental [25].
Distribution
After intravenous administration, propofol is extensively bound to the plasma proteins (predominantly albumin) and erythrocytes. The free fraction is only 1.2–1.7%. As up to 50% of propofol is bound to the erythrocytes [26], many clinical PK investigators measure whole concentrations rather than plasma propofol concentrations.
Propofol readily crosses the blood–brain barrier (BBB) and causes rapid loss of consciousness (sometimes within the time it takes for a drug to pass through the circulation once [27]). The speed of induction depends on patient-related factors (cardiac output being one of the most important factors) and speed of infusion.
Whereas approximately 1% of total plasma propofol is unbound, free fraction of propofol in the CSF is approximately 31% [28]. Equilibrium between blood and brain concentrations is reached after 30 min, resulting in a total blood to CSF propofol ratio of 0.01–0.02 [29]. Placenta transfer is also fast and extensive, with venous blood concentration mother-to-foetus ratios ranging from 0.7 to 0.8 [30]; however, due to its clearance from the neonatal circulation, it has only minimal and short-lived clinical effects in unborn neonates [31] and is thus safe for use during caesarean section [32].
After a single bolus, or short infusion, the time to offset of clinical effects is short because of the fast initial distribution. Redistribution to and from a slow compartment also occurs and is due to the high lipid solubility of propofol. This compartment has a large capacity to absorb propofol, which results in a very large apparent volume of distribution at steady state (Vdss; three to four multiples of total body volume), even in non-obese individuals [33]. Nonetheless, even after prolonged administration, the offset of clinical effects is still reasonably fast compared with other intravenous hypnotics because redistribution of drug from the slow compartment is slow compared with the rates of metabolism and excretion.
The context-sensitive decrement time [34] for propofol is thus generally favourable compared with other hypnotics. For a short infusion (< 3 h), the 80% decrement time is < 50 min, whereas for longer infusions (> 12 h) it increases up to 3.5 h [35].
Metabolism
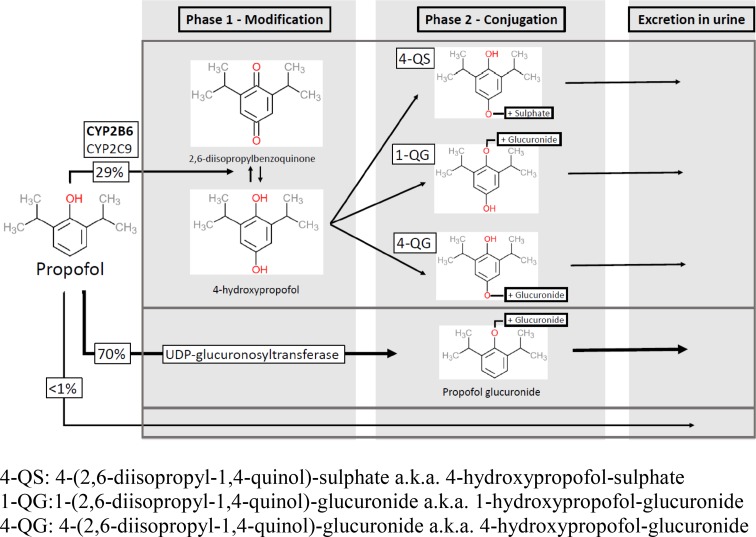
The liver is the main site of propofol metabolism. The majority of propofol (70%) is conjugated to propofol glucuronide by uridine 5′-diphosphate (UDP) glucuronosyltransferase. Approximately 29% of propofol is hydroxylated to 2,6-diisopropyl-1,4-quinol (4-hydroxypropofol). A number of different cytochrome P450 (CYP) P450 isoforms are involved in this step. CYP2B6 and, to a lesser extent, CYP2C9 are the major catalysts. Environmental and genetic influences on the CYP2B6 can, at least partially, explain the interindividual variability in hydroxylation of propofol in liver microsomes [36]. Propofol metabolites are subsequently conjugated to form 4-(2,6-diisopropyl-1,4-quinol)-sulphate, 1-(2,6-diisopropyl-1,4-quinol)-glucuronide and 4-(2,6-diisopropyl-1,4-quinol)-glucuronide [37, 38] (for a graphic representation of the metabolic pathway of propofol see Fig. 1). The major metabolites have no hypnotic activity.
Fig. 1.
Propofol metabolic pathway. CYP cytochrome P450, UDP uridine 5′-diphosphate
Liver is very efficient at propofol metabolism, with a blood extraction ratio of 90%. Because of this efficiency, propofol metabolism depends critically on maintained hepatic perfusion, and any decreases in hepatic blood flow concomitantly decrease the propofol metabolic rate. The mean clearance of propofol is around 2.2 L/min [33], which is higher than the total liver blood flow. Extrahepatic sites of metabolism account for 40% of total propofol clearance, which has been confirmed during studies of propofol metabolism during the anhepatic stage of liver transplantation [39]. The kidneys contribute significantly to propofol metabolism. They have an extraction ratio of 60–70% [40, 41] and account for up to one-third of total propofol metabolism. The small intestines are also metabolically active, with an extraction ratio of 24% [39]. The role of the lungs is still being debated; some studies suggest an active role of the lungs [42], while others do not [40], or state that the lungs are merely a temporary propofol reservoir and later release propofol from binding sites back into circulation [43].
Elimination and Excretion
After metabolism, 88% of propofol is excreted within 5 days in the urine. Less than 0.3% of administered propofol is excreted unchanged [33]. The phenolic metabolites rarely (< 1% of patients) result in green discolouration of the urine [44].
Propofol is also excreted through exhalation. The amount of propofol excreted this way is extremely small (of the order of a few parts per billion), but the expired concentration correlates with plasma concentrations. Online estimations of propofol plasma concentration, using measurement of expired concentrations, is thus challenging but feasible [45–47]. B. Braun (Melsungen, Germany) has recently launched a commercially available and clinically certified spectrometer, capable of measuring propofol concentration in exhaled air [48].
Population PK Modelling
Noncompartmental Modelling
Most of the older studies of the PK of propofol determined only the noncompartmental PK parameters to characterize the PK of propofol. The ranges of published noncompartmental PK parameters for adults after propofol infusion are Vdss 159–771 L, half-life of fast distribution (T½α) 1.33–4.6 min, half-life of slow distribution (T½β) 27–69.3 min, half-life of elimination (T½γ) 116–834 min, mean residence time (MRT) 102–174 min, total blood clearance (Clb) 1.78–2.28 L/min [49–53]
Compartmental Modelling
A PK model is a mathematical means of describing the PK behaviour (distribution and clearance) of a particular drug in the body. PK models are generally used in two ways. First, they can be used to enable the estimation of the drug concentration in the plasma resulting from a given drug administration profile, thereby being useful in advising drug administration rates. Second, they can be used to calculate the necessary infusion rates required to most efficiently achieve and maintain a given drug concentration in a body compartment (in anaesthesia, the plasma or the effect site are targeted) [54].
The most simple compartmental model contains one compartment and two model parameters, namely the volume of distribution (Vd) and clearance. For many drugs, a one-compartment model can adequately describe the PK and guide drug dosing, but for most drugs used in anaesthesia this is not the case. Therefore, most PK propofol models consist of two or three compartments and a matching number of intercompartmental constants (see Fig. 2 for a diagram of a three-compartment PK and PD model) [55].
Fig. 2.
Overview of a three-compartment pharmacokinetic/pharmacodynamic model
Whether PK models are used to predict achieved concentrations or calculate required infusion rates, a current challenge is to develop models that adequately describe the PK of a widely varying patient population. Obesity is a growing problem, therefore an important issue that needs to be addressed is how to adequately describe patient size so that the PK model compartments and parameters can be effectively scaled to patients with varying sizes and body compositions. A number of different size descriptors exist; body mass index (BMI), ideal body weight (IBW) and adjusted body weight (ABW) are just a few examples. For highly lipophilic drugs, the best size descriptor of volume is probably total body weight (TBW), or another descriptor that incorporates fat mass, while the best size descriptor for clearance is fat free mass [56].
Another challenge is to determine the best way to scale the model compartments and volumes to size (and other) descriptors. Historically, model components were scaled linearly to the size descriptor. This method works well for the intermediate range of sizes but produces erroneous predictions at the extremes of weights, e.g. in small children or morbidly obese adults. Recently, the use of allometric scaling of model components to the size descriptor has become more popular [57]. Allometry is the study of the relationship of size to different anatomical and physiological aspects of an organism. This relationship was first suggested by Snell [58], while the terminology was coined by Huxley and colleagues [59]. Allometric models scale model components to size using a power exponent with an equation in the form of ‘y = bxa’ where ‘y’ is a value of the model component, ‘b’ is a constant, ‘x’ is the value of the size descriptor and ‘a’ is the power exponent (which is commonly 0.75) [60]. Allometric scaling enables generation of universal PK models that are applicable in wide range of patient populations [61, 62]. In general, allometric scaling, often with a power exponent of 0.75, has been shown to apply to multiple biological processes for a wide range of species, from small organisms all the way through to large mammals [63]. However, among neonatal humans, in addition to scaling to size, maturation of enzymatic processes is also an important factor limiting metabolic clearance. Different approaches have been used to deal with this. One approach applied by some groups [60] has been to use different exponents for very young humans. Our group has instead used the same exponent to scale for size, but in addition also applies a sigmoidal function that increases over the course of maturation to the calculation of metabolic clearance in order to correct for the immaturity of metabolic functions in neonates [61, 62].
Although the different models have a similar structure, there are differences in the number of covariates, and in scaling of the volumes and/or clearances in relation to these covariates (see Tables 1 and 2 for study methods and model equations derived from different models). Many models were developed for widely differing patient categories, but, to our knowledge, propofol PK have not been studied in critically ill ICU patients; thus, none of the existing PK models applies to these patients.
Table 1.
Methods
| Principal investigator (publication year) | Population characteristics | Setting | Comedication | Target population | |||||
|---|---|---|---|---|---|---|---|---|---|
| Sex (M/F) | Age (years)a | TBW (kg)a | Height (cm)a | Adults | Obese | Paediatric | |||
| Gepts [49] (1987) | 13/5 | 29–65 | 49–82 | 155–175 | PTN | Glycopyrrolate 0.4 mg IM, lidocaine/bupivacaine intrathecal | X | ||
| Marsh [65] (1991) | Idem Gepts | Idem Gepts | Idem Gepts | Idem Gepts | Idem Gepts | Idem Gepts | X | ||
| Kataria [74] (1994) | 28/25 | 3–11 | 15–61 | NA | PTN | Rocuronium, fentanyl, atropine, bupivacaine, neostigmine + atropine | X | ||
| Short [75] (1994) | 6/4 | 4–7 | 15–22 | NA | PTN | EMLA, N2O, bupivacaine wound infiltration | X | ||
| Schnider [66] (1998) | 13/11 | 26–81 | 44–123 | 155–196 | HV | No comedication administered | X | ||
| Schuttler [52] (2000) | 150/120 | 2–88 | 12–100 | – | PTN and HV | X1 | X | X | |
| Knibbe [78] (2005) | R: 24 C: 6 A: 24 |
R: x C: 1–5 A: 37–73 |
R: 0.25–0.3 C: 10–21 A: 64–93 |
– | R: HV C: PTN A: PTN |
X2 | X | ||
| Paedfusor [73] (2005) | NA | NA | NA | NA | NA | Yes, details not published | X | ||
| van Kralingen [70] (2006) | 20/44 | 48.5 | 55–167 | – | PTN | Lidocaine, fentanyl, atracurium, remifentanil | X | X | |
| Cortinez [69] (2010) | 7/11 | 28–56 | 82–134 | 139–185 | PTN | X3 | X | X | |
| Eleveld [72] (2018) | 672/361 | 0–88 | 0.68–160 | NA | PTN and HV | X4 | X | X | X |
| Sahinovic [149] (2017) | 21/19 | 53 | 81.5 | 175.5 | PTN | Rocuronium | X | ||
X1: multiple datasets were analysed (Schuttler [52], Cockshott [51, 190], Glass [184], White [65, 191], Shafer [74]). Each dataset involved patients receiving different comedications
X2: Multiple datasets were analysed (Cox [192], Knibbe [193], Knibbe [194], Knibbe [195]). Each dataset involved patients receiving different comedications
X3: Multiple datasets were analysed (Schnider [66], Servin [196], Cortínez [69]). Each dataset involved patients receiving different comedications
X4: Data from 30 previously published studies were used. Each dataset involved patients receiving different comedications
HV healthy volunteers, PTN patient, R rat, C children, A adults, NA not available, TBW total body weight, M male, F female, IM intramuscularly
aRange/average
Table 2.
Model equations
| Gepts [49] | Marsh [65] | ||
|---|---|---|---|
| V 1 | 16.92 L | V 1 | 0.228 × TBW |
| V 2 | 35.07 L | V 2 | 0.464 × TBW |
| V 3 | 215.3 L | V 3 | 2.89 × TBW |
| K10 (min−1) | 0.119 | K10 (min−1) | 0.119 |
| K12 (min−1) | 0.114 | K12 (min−1) | 0.112 |
| K13 (min−1) | 0.0419 | K13 (min−1) | 0.042 |
| K21 (min−1) | 0.0550 | K21 (min−1) | 0.055 |
| K31 (min−1) | 0.0033 | K31 (min−1) | 0.0033 |
| Kataria [74] | Short [75] | ||
|---|---|---|---|
| V 1 | 0.41 × TBW | V 1 | 0.432 × TBW |
| V 2 | 0.78 × TBW + 3.1 × AGE − 16 | V 2 | |
| V 3 | 6.9 × TBW | V 3 | |
| CL1 (L min−1) | 0.035 × TBW | K10 (min−1) | 0.0967 |
| CL2 (L min−1) | 0.077 × TBW | K12 (min−1) | 0.1413 |
| CL3 (L min−1) | 0.026 × TBW | K13 (min−1) | 0.0392 |
| K21 (min−1) | 0.1092 | ||
| K31 (min−1) | 0.0049 |
| Schnider [66] | Schuttler [52] | ||
|---|---|---|---|
| V 1 | 4.27 L | V 1 | 9.3 × (TBW/70)0.71 × (Age/30)−0.39 × (1 + BOL × 1.61) |
| V 2 | 18.9 + (− 0.391 × (Age − 53)) L | V 2 | 44.2L × (TBW/70)0.61 × (1 + BOL × 0.73) |
| V 3 | 238 L | V 3 | 266 L |
| CL1 (L min−1) | (1.89 + ((TBM-77) × 0.0456 + ((LBM-59) × − 0.0681) + ((HT-177) × 0.0264) | CL1 (L min−1) | Age ≤ 60: 1.44 L/min × (TBW/70)0.75 Age > 60: 1.44 × (TBW/70)0.75 − (Age − 60) × 0.045 |
| CL2 (L min−1) | 1.29 + (− 0.024) × (Age − 53) | CL2 (L min−1) | 2.25 L/min × (TBW/70)0.62 × (1 + VEN × − 0.40) × (1 + BOL × 2.02) |
| CL3 (L min−1) | 0.836 | CL3 (L min−1) | 0.92 L/min × (TBW/70)0.55 × (1 + BOL × − 0.48) |
| Reference | Males: LBM = 1.1 × WT − 128 × (WT/HT)2; Females: LBM = 1.07 × WT − 148 × (WT/HT)2 |
Reference | VEN = 1 for venous sample and 0 for arterial sample; BOL = 1 for bolus data and 0 for infusion data |
| Knibbe [78] | Paedfusor [73] | ||
|---|---|---|---|
| V 1 | 0.3 × TBW0.98 | V 1 | 0.4584 × TBW |
| V 2 | 1.2 × TBW1.1 | V 2 | V1 × k12/k21 |
| CL1 (L min−1) | 0.071 × WT0.78 | V 3 | V1 × k13/k31 |
| CL2 (L min−1) | 0.062 × WT0.73 | K10 (min−1) | 0.1527 × TBW−0.3 |
| K12 (min−1) | 0.114 | ||
| K13 (min−1) | 0.0419 | ||
| K21 (min−1) | 0.055 | ||
| K31 (min−1) | 0.0033 |
| Kralingen et al. [70] | Cortínez [69] | ||
|---|---|---|---|
| V 1 | 3.03 L | V 1 | 4.48 × (TBW/70) L |
| V 2 | 5.34 L | V 2 | 21.2 × (TBW/70) × e−0.0164 × (Age−50) L |
| V 3 | 116 L | V 3 | 237 × (TBW/70) L |
| CL1 (L min−1) | 2.22 × (TBW/70)0.67 | CL1 (L min−1) | 1.92 × (TBW/70)¾ |
| CL2 (L min−1) | 1.64 | CL2 (L min−1) | 1.45 × (TBW/70)¾ × e−0.0153 × (Age−50) |
| CL3 (L min−1) | 1.86 | CL3 (L min−1) | 0.86 × (TBW/70)¾ |
| Eleveld [72] | Sahinovic [149] | ||
|---|---|---|---|
| V 1 arterial | 6.25 × fcentral(WGT)/fcentral(WGTref) × e0.61 | V 1 | 3.8 × (TBW/70) × e0.205 |
| V 1 venous | V1arterial × (1 + 1.42 × (1 − fcentral(WGT)) | V 2 | 9.21 × (TBW/70) × e0.268 |
| V 2 | 25.5 × WGT/WGTref × faging(− 0.0156) × e0.565 | V 3 | 447 × (TBW/70) |
| V 3 | 273 × fFFM/fFFM,ref × fopiates(− 0.0138) × e0.597 | CL1 (L min−1) | NT: 1.33 × (TBW/70)0.75 × e0.00902 |
| CLmale | 1.79 × (WGT/WGTref)0.75 × fCLmaturation/fCLmaturation,ref × fopiates(− 0.003) × e0.265 | T: 1.33 × (TBW/70)0.75 × 1.444 × e0.00902 | |
| CLfemale | 2.1 × (WGT/WGTref)0.75 × fCLmaturation/fCLmaturation,ref × fopiates(− 0.003) × e0.265 | CL2 (L min−1) | 0.987 × (V2/9.21)0.75 |
| Q2arterial | 1.75(V2/V2ref)0.75 × (1 + 1.3 × (1 − fQ3maturation)) × e0.346 | CL3 (L min−1) | 1.37 × (V3/447)0.75 × e0.192 |
| Q2venous | Q2arterial × 0.68 | ||
| Q3 | 1.11 × (V3/V3ref)0.75 × fQ3maturation/fmaturation,ref × e0.209 | ||
| Reference |
faging(x) = e(x × (AGE-AGEref)) fsigmoid(x, E50, λ) = xλ(xλ + E50λ) |
Reference | T: Patients with brain tumour NT: patients without brain tumour |
|
fcentral(x) = fsigmoid(x, 33.6, 1) fCLmaturation = fsigmoid(PMA, 42.3, 9.06) fQ3maturation = fsigmoid(AGE + 40 weeks, 68.3, 1) fopiates(x) = 1, absence fopiates(x) = e(x × AGE), presence FFMmales = [0.88 + (1 − 0.88)/1 + (AGE/13.4)−12.7] × [9270 × WGT/6680 + 216 × BMI] FFMfemales = [1.11 + (1 − 1.11)/1 + (AGE/7.1)−1.1] × [9270 × WGT/8780 + 244 × BMI] |
CL1 = V1 × K10; CL2 = V2 × K21; CL3 = V3 × K31; V2 = V1 × K12/K21; V3 = V1 × K13/K31
M male, F female, Y young, E elderly, TBW total body weight, FFM fat-free mass, PMA postmenstrual age
Adult Population
Many adult PK models for propofol have been published. Large variability among the model parameters can be found due to differences in study design, drug administration profile and study population used to develop the model [64]. Although numerous multicompartmental mammillary models exist, only two adult models are commonly used in clinical practice for target-controlled infusions (TCIs), namely the Marsh [65] and Schnider [66] models.
In the Marsh model, the volumes (V1, V2, V3) are a linear function of patient weight, while the intercompartmental transfer rates (k12, k21, k13, k31) are constant. In contrast, the Schnider model has fixed V1, V3, k13 and k31, and uses age as a covariate in the calculation of V2, k12 and k21, and lean body weight, sex, total body mass and height as covariates of the metabolic clearance.
As indicated above, a benefit of the Schnider model over the Marsh model is that it adjusts the dose and infusion rate according to the patient’s age. This results in smaller bolus doses administered by the TCI pump (on starting, or when the target concentration is increased) in older patients, which might improve haemodynamic stability. A disadvantage of the Schnider model is that the lean body mass equation incorporated into the calculation of k10 can generate paradoxical values, resulting in excessive increases in maintenance infusion rates in the obese [67].
In general, both models have acceptable performance in daily practice, and the choice of model to use is predominantly made based on user experience and the model availability.
Obese Population
Obesity is associated with a number of physiological and pathophysiological changes that can have a significant impact on drug PK. The most important factors affecting PK in obese patients are changes in body composition, haemodynamics, regional blood flow, and liver and kidney function [68].
Older propofol models, such as the Marsh [65] and Schnider [66] models, were developed from studies involving healthy adults with a limited range of weights. Some practitioners still use the Marsh model [65] for TCI propofol administration in obese patients [67], but instead of inputting the TBW, they input an ABW calculated from the TBW and IBW, and calculated as follows:
where IBW is calculated as:
or more simply as:
As mentioned earlier, in severely obese patients, the LBM equation used in the Schnider model generates paradoxically large increases in the k10, when the BMI is > 37 in females and > 42 in males [67]. As a result, commercially available TCI devices programmed with the Schnider model do not allow the user to input parameters that generate BMI values above these limits. Users attempting to use the Schnider model in severely obese patients must either change to a different model, enter a ‘false’ combination of parameters (i.e. a greater height or a lower weight in place of the TBW), or administer propofol by manually controlled infusion.
There are currently a number of propofol models specifically developed for obese patients, such as the Cortínez [69] and van Kralingen [70] models, or a general purpose model that is probably also suitable for use in the obese (the Eleveld allometric model) [61] (see Table 1).
Cortínez et al. [71] have investigated the predictive performance of different PK models in obese patients and concluded that when models were implemented as published (i.e. using the TBW as a weight-scaling measure), the global performance of the Eleveld model [72] was best compared with other models. All models tended to underestimate the propofol plasma concentration. When the user entered the ABW instead of the TBW, the Schnider and Marsh models had the highest accuracy and lowest bias [71].
Paediatric Population
Develop PK models for children is challenging, for many reasons. First, there are ethical challenges with research in children, and, second, as children grow, their size increases, their body composition changes and their organ systems mature, making it difficult to construct a single and accurate PK model.
A number of paediatric PK models for propofol exist, the most well-known being the Paedfusor model [73], Kataria model [74], Short model [75], Schüttler model [52] and the Eleveld ‘general purpose’ model [72]. These models were developed using a range of methodologies. Differences in methodology include the age range of the children enrolled in the study, the study population (healthy children as opposed to children with comorbidities), the sampling site (arterial vs. venous) and the administration regimens used (bolus with or without continuous infusion thereafter). These differences influence the range of patients to which the different models are applicable. For example, the Kataria model was developed from children 3 years of age and older and is thus not validated for use in children younger than 3 years of age.
Sepúlveda et al. [76] and Hara et al. [77] evaluated the predictive performance of these models during short- and long-duration infusions, respectively, and concluded that overall most models overestimate the initial Vd. The relevance is that when they are used to inform dosing schemes designed to achieve a particular plasma concentration, they result in administration of a larger than necessary induction bolus. Most paediatric models performed well during infusions of short duration (up to median of 99 min), while only the Short [75] and Schüttler [52] models showed acceptable performance and the least divergence during infusions of up to 545 min. Overall, the Short model performed the best and the authors concluded that it might be preferable for use during TCI in children.
Unified PK Models
A PK model is only applicable in patients in whom the clinical conditions and patient category match those used in model development. As soon as these begin to diverge, model predictions can be erroneous. Using an inappropriate model during a TCI can lead to unexpected (side) effects. Rational model selection is of critical importance, but given the large number of available models, this is not an easy task. Furthermore, an exact match is often not possible. Even for users knowledgeable in PK, it is difficult to be certain which models to use in patients with overlapping conditions (e.g. patients who are elderly and obese), or in grey zones between conditions (e.g. patients who are moderately obese but otherwise healthy). These difficulties have stimulated the development of unified PK models, which are derived from data collected in a diverse group of patients and clinical conditions, and are thus designed to provide accurate predictive performance well in a wide range of patients and clinical conditions.
The first unified PK model for propofol was published by Schüttler and Ihmsen [52] in 2000. This group developed a general PK model for propofol, applicable in both children and adults, by performing PK analysis on data collected by five different research groups. This analysis yielded a three-compartment PK model with weight, age, method of administration and sampling site as the main covariates. They concomitantly demonstrated that scaling of model compartments and clearances to power exponents (between 0.55 and 0.75) of normalized TBW yielded better model predictions than that of linear scaling. An important obstacle to a broader clinical application of this model is the fact that the user must select a mode of administration (bolus vs. continuous infusion) before using the model, whereas in clinical practice both administration modes are often used.
In 2005, Knibbe and colleagues [78] published an interspecies PK model for propofol, which was a two-compartment model applicable in rats, children and adults. They achieved this impressive task by allometrically scaling volumes and clearances to TBW. In other words, they scaled the volumes and clearances in the model to a power exponent (between 0.73 and 1.1), which allowed them to more realistically estimate the volumes and clearances in a wide range of different bodyweights, from a small rat weighing 0.25 kg to an adult weighing 93 kg.
The most recently published unified PK model for propofol is the ‘general purpose model’ constructed by Eleveld and colleagues [61]. First published in 2014, the PK model was recently expanded with a PD analysis [72]. In the updated version of the model, the authors used PK data derived from 30 previously published studies containing data collected from children of all ages, adults, obese adults, and elderly individuals. They constructed a three-compartment model where weight, age, sex and administration of comedication were covariates. Similar to the work of Schüttler and Ihmsen [52] and Knibbe et al. [78], they also used allometric scaling to normalize bodyweight for clearances (three-quarter power exponent), while volumes were scaled linearly with normalized body weight for V1 and V2, and with normalized fat-free mass for V3. Retrospective analysis of this model performance shows that the model performs at least as good as, or better, than dedicated population models in all populations. Further model evaluation must be performed in prospective studies.
Effects of Patient Characteristics on Propofol Kinetics
One of the main advantages of analysing a larger set of PK and PD data from a wide range of patients is the ability to detect covariate relationships that might remain hidden when a dataset from patients with a narrower range of characteristics is analysed. As a result, Eleveld et al. were able to identify a few, clinically very relevant, correlations. They found a relationship between age and the volume of the peripheral compartments and metabolic clearance. The volume of V2 declines with age, while V3 and metabolic clearance decline only when other medication are concurrently administered. This finding confirms an impression widely shared by practicing anaesthetists that the maintenance infusion rates required for adequate anaesthesia are reduced in older individuals, especially when comedication is administered. Furthermore, they found that the central compartment scales to an Emax function (in other words central compartment volume increase follows a sigmoid function with increasing weight). This suggests that the induction dose of propofol, per kilogram, should be relatively high in low-weight individuals, and relatively low in obese patients, compared with individuals with intermediate weight. This fact is also consistent with the observations of clinical practitioners. Lastly, they reported a higher metabolic clearance in women (of all ages) compared with men, which might explain clinical observations of a more rapid emergence from propofol anaesthesia in women compared with men [79].
Physiologically-Based PK Models
Contrary to compartmental PK models where compartments have no real physiological meaning (or direct correspondence with body parts), compartments in physiologically-based PK models (PBPK) are linked to different body parts connected by the cardiovascular system. Typically, all the major tissues, such as adipose tissue, muscle, brain, heart, kidney, liver, and lung, are represented [80].
An important advantage of PBPK models over compartmental models is the ability of the former to include more parameters specifying sources of physiological and biochemical variability in individuals, thereby reducing the interindividual variability and increasing the individual prediction accuracy. For example, the incorrect assumption of instantaneous mixing of a drug in the central compartment used by compartmental models severely limits their prediction accuracy during the first few minutes of drug infusion. Adaptations to the compartmental models using ‘administration lag time’ and presystemic compartments can improve the prediction accuracy [81], however only PBPK models use cardiac output [82] and blood flow terms to more accurately describe the drug kinetics in greater detail. This even potentially enables them to predict the influence of the effect of changing haemodynamic parameters on drug disposition. The same applies to cerebral blood flow, changes of which can play a major role in propofol PD.
An important disadvantage of PBPK models is the difficulty in collecting the extensive physiological data necessary for model development, and often very limited (if any) improvement in prediction accuracy at a cost of a much more complex and mathematically elaborate model compared with compartmental models [83].
The physiologically-based hybrid recirculatory model published by Upton and Ludbrook [84] is an example of a PBPK propofol model. It incorporates submodels for the lung and brain, and a less detailed ‘lumped model’ for the rest of the body. The prediction accuracy and bias are comparable with that of the major compartmental models [83].
Pharmacodynamics (PD)
Central Nervous System
Hypnotic Effects
Propofol exerts its hypnotic effect through potentiation of the effects of the inhibitory neurotransmitter GABA [85]. It binds to the β-subunit of the postsynaptic GABAA receptor, where it causes an inward directed chloride current that hyperpolarizes the postsynaptic membrane and inhibits neuronal depolarization. This effect is dose-dependent. At low concentrations, propofol potentiates GABA-activated inward chloride currents, while at higher concentrations, it directly activates the channel opening [86]. GABA receptors are ubiquitous throughout the central nervous system [87].
Although our understanding of the actions of propofol at the molecular level is quite extensive, we do not entirely understand how these molecular effects translate into alterations in cellular, synaptic and neural network function, and in turn cause unconsciousness [88]. This knowledge gap is, at least in part, the result of a lack of a generally accepted theory of consciousness. In recent years, cognitive neuroscience has seen a resurgence of interest in this topic, with attempts to integrate anaesthesia and sleep research in order to address this deficiency. This resurgence has revealed several brain areas that play a crucial role in generation of consciousness, and which are extensively influenced by hypnotic drugs.
In the reticular formation of the brainstem [89], there are a number of sleep- and wakefulness-promoting cholinergic and monoaminergic nuclei that exert their effect by influencing higher cortical structures [90]. Their activity and reciprocal influence changes with the level of wakefulness [91]. Local inactivation of wakefulness-promoting areas, such as locus coeruleus and dorsal raphe, enhance anaesthesia, while local activation of various other wakefulness-promoting areas, including pontis oralis and centromedial thalamus, facilitate emergence from anaesthesia. One of the sleep-promoting nuclei is the ventrolateral preoptic area. Lesions in this region enhance wakefulness [92]. These nuclei are extensively affected by clinical concentrations of hypnotic drugs.
The thalamus plays a central role in information processing with the brain. Increasing concentrations of propofol, and thereby increasing levels of sedation, cause a decrease in activity, regional cerebral blood flow and metabolism in the thalamus [93]. There are a number of (mutually nonexclusive) hypotheses on how these changes could lead to or contribute to loss of consciousness [94]. The function of the thalamus as a critical sensory information relay from subcortical structures to the cortex could be impeded by hypnotic drugs [95], although thalamic depression seen after loss of consciousness could merely reflect the decrease in global cortical activity [96]. Hyperpolarization of thalamocortical neurons—and the resulting switching from a tonic firing state in wakefulness to a bursting firing state in unconsciousness—could be a final common pathway through which different hypnotics cause a disruption in thalamocortical and cortico-cortical loops, thereby causing unconsciousness [97].
Finally, the cerebral cortex has long been identified as an important drug effect target for hypnotic drugs. Sleep and anaesthesia studies have consistently demonstrated decreases in cortical activity and cerebral blood flow [98]; however, these changes are not homogeneous across the cortex and across different drugs. The most consistent and largest changes occur in the frontal and posterior parietal cortex [99]. These regions form part of a much wider ‘default mode network’, a functional network thought to be responsible for monitoring of internal environment in humans. Loss of consciousness in non-REM sleep is accompanied by increased modularization of brain activity and reduction in a whole-brain spatiotemporal integration of information [100–102]. This is concordant with the information integration theory of consciousness [103].
Amnesia
The amnestic properties of propofol have been extensively described in the literature [104]. Explicit memory seems to be most affected, and in a dose-dependent manner. The most basic form of memory, perceptual priming, seems to be preserved to some degree [105]. The amnestic effects of propofol do not seem to be caused by interference with memory encoding, but a low-dose of propofol has been shown to induce amnesia without any impairments in behaviour [106]. The exact neural mechanism of propofol-induced amnesia in a conscious patient remains to be elucidated.
Anxiolysis
Propofol produces anxiolysis in subhypnotic doses. This has been demonstrated in mice [107] and in patients undergoing propofol sedation while undergoing surgical procedures under regional anaesthesia [108]. Propofol has been proposed as an excellent preoperative anxiolytic drug in day-care surgery, when administered through a patient-controlled anxiolysis system (a patient-controlled analgesia system analogue), as a replacement for benzodiazepine premedication in order to shorten the discharge times [109]. The exact mechanism of this anxiolysis is still not known, but inhibition of 5-HT activity in the hippocampus [110] or nitric oxide synthase in the hypothalamus, amygdala and hippocampus might be the mechanisms involved [111].
Analgesia
There are a number of patient studies describing the analgesic effects of subhypnotic doses of propofol [112, 113]. This effect could be caused by an action of propofol at the spinal level. In animal studies, it has been shown that propofol produces analgesia in mice when administered intraperitoneally, through modulation of spinal GABAA receptors [114], and thereby depresses ventral root potentials in the spinal cord elicited by monosynaptic reflexes or exposure of the spinal cord to substance P [115]. Furthermore, Nishiyama et al. showed that intrathecal injections of propofol had effects on pain perception, but they could not rule out the possibility of neurotoxicity [116].
A recently published meta-analysis comparing postoperative pain after propofol versus inhalation-based anaesthesia did not demonstrate any significant differences, mainly because of substantial heterogeneity among studies published to date [117].
Antiemetic Effect
The antiemetic action of propofol is well known and has been extensively described [118, 119]. Patients receiving anaesthesia with propofol experience significantly less PONV compared with that associated with other hypnotic drugs, irrespective of the use of adjunct drugs, patient characteristics or opiate use. The mechanism behind this effect is not very well understood, but it has been demonstrated that propofol interacts with dopaminergic (D2) receptors in the chemoreceptor trigger zone [120], inhibits the limbic system [121], thereby interacting with cortical reflexes reaching the vomiting centre, and inhibits 5-HT3 receptors located in the central nervous system in a noncompetitive and dose-dependent manner, thereby reducing the incidence and severity of PONV.
Neurophysiological Effects
Propofol decreases cerebral blood flow, intracranial pressure, and cerebral metabolic rate, while maintaining dynamic and static autoregulation [122] and vascular responsiveness to carbon dioxide [123]. These favourable effects on cerebral physiology make propofol an almost ideal hypnotic for anaesthesia during neurosurgery. The evidence for neuroprotective effects of propofol during ischaemia-reperfusion injury is conflicting [124]; however, its role as part of multimodal neuroprotection has been established [125].
Propofol has both pro- and anticonvulsive activity. On the one hand, a number of reports of convulsions and excitatory events such as myoclonus and tremor, during or shortly after the start or end of propofol anaesthesia, have been published [126]; these events might be the result of preferential depression of subcortical regions. On the other hand, the role of propofol as a potent treatment of status epilepticus has been well-established [127, 128].
Cardiovascular System
Propofol has extensive effects on the cardiovascular system. The most prominent effect is systemic blood pressure reduction accompanied by a decrease in cardiac output. This effect is dose-dependent and even occurs at sedative doses. It is more pronounced in elderly and physiologically compromised patients [129]. The effect is, at least partially, mediated by a significant decrease of sympathetic tone accompanied by a decrease in vascular resistance. Furthermore, propofol also inhibits the physiological baroreflex responses, thereby enhancing cardiovascular depression [130].
Cardiac contractility remains preserved. Propofol only has direct negative inotropic actions at concentrations exceeding the clinical range, an effect that is similar in failing and non-failing human hearts. The negative inotropic effect is mediated through a concentration-dependent decrease in the uptake of Ca2+ into the sarcoplasmatic reticulum, which is simultaneously accompanied by an increase of myofilament sensitivity to Ca2+, partially counteracting the effect [131]. The haemodynamic response lags behind the hypnotic effect of propofol. While the hypnotic half-time plasma effect site equilibration time (T½keo) is 2.5 min, independent of age, haemodynamic half-time plasma effect site equilibration time is 5 min in young patients, and up to 10 min in elderly patients [132].
Propofol cardioprotective effects in cardiac surgery is a focus of research. In animal studies, high propofol doses caused dose-dependent attenuation of ischaemia-reperfusion myocardial injury (IRI) by exerting free radical scavenging effects and decreasing lipid peroxidase activity [133]. These cardioprotective effects are less profound than those caused by sevoflurane [134]. A combination of inhaled anaesthetic preconditioning and propofol postconditioning appears to work synergistically in decreasing IRI [135].
Respiratory System
Propofol is a potent ventilatory depressant. It interferes with ventilation in a dose-dependent manner by affecting central chemoreceptor sensitivity, reducing ventilatory responses to hypercapnia and hypoxia [136–138]. In higher doses, propofol causes apnoea. It also changes the pattern of breathing by decreasing the ribcage contribution to tidal volume [139] by causing upper airway relaxation and suppression of upper airway reflexes [140]. Furthermore, it attenuates vagal- and methacholine-induced bronchoconstriction [141] and potentiates hypoxic pulmonary vasoconstriction [142].
Hepatorenal System
Despite the fact that the liver and kidneys are extensively involved in metabolism and excretion of propofol, their function does not appear to be affected by propofol. In human and animal studies, propofol infusion increased hepatic perfusion [143] due to higher arterial [144] and portal venous blood flow [145], while renal perfusion remained essentially unaltered [146]. However, when cardiac output is not maintained, organ perfusion, and thus liver and renal perfusion, could be compromised.
Propofol infusion is known to cause green skin and urine discolouration caused by production of phenol green chromophore. Furthermore, urinary uric acid excretion is increased after propofol infusion, which can result in a cloudy appearance of the urine.
PD Modelling
For propofol, the main clinical effect is loss of consciousness, which is difficult to quantify. Most clinicians consider it to be a continuum of effects, most of which have a binary nature, i.e. present or absent. However, several electroencephalogram (EEG)-based methods of quantifying the depth of anaesthesia have been developed [147, 148]. The most commonly used is the Bispectral index (BIS; Medtronic, Dublin, Ireland), a unitless number between 0 and 100, where 0 represents very high hypnotic drug effect (i.e. no cerebral electrical activity) and 100 represents total absence of the hypnotic drug effect. The BIS monitor is one of the best validated EEG-based monitors for quantifying the drug effect [148]. Several PD studies have been performed, with most of them using a sigmoidal Emax model to characterize the relationship between blood concentration, the concentration in a hypothetical effect site, and the resultant clinical drug effect. Published parameters are in the following ranges: keo, 0.01–0.45 min−1; Ce50, 2.71–3.44 mg L−1; and γ, 1.47–2.961 [65, 67, 71, 149–152].
Drug Interactions
Interactions between drugs occur in the PK, PD, or both [153]. Alterations in the PD (clinically visible) drug dose–effect relationship can be secondary to PK and/or PD interactions; therefore, these interactions are most often not discussed separately when considering clinical applications. Drug interactions can be additive, synergistic or antagonistic [154]. Any anaesthesia provider should be aware of this and adjust the drug dose accordingly.
PK Interactions
PK interactions can result in changes in absorption, distribution, metabolism and elimination.
Absorption
Propofol is only suitable for intravenous administration and thus does not undergo any absorption interactions. Nonetheless, care should be taken when infusing propofol with other drugs. It is well-described that propofol undergoes chemical interactions with a number of frequently used drugs, and should thus not be administered through the same intravenous line with these particular drugs. Of note are interactions with certain antibiotics (e.g. ciprofloxacin, gentamicin, metronidazole) and calcium antagonists (nimodipine, verapamil). A more extensive list of interactions can be found in the summary of product characteristics (SPC) and in the study by Michaels et al. [155]
Distribution
Propofol is extensively bound to plasma proteins. Concomitant infusion with drugs competing for the same plasma binding sites, or use in patients with low plasma proteins, could potentially result in high unbound plasma propofol fraction, causing more profound effects and adverse effects. The clinical significance of this phenomenon is uncertain [156].
Vd and the rate of metabolism of propofol are affected by drugs affecting the cardiovascular system. Drugs that decrease cardiac output and cause a concomitant decrease in hepatic perfusion alter the distribution and metabolism of propofol, e.g. esmolol [157] and in propofol itself [158, 159]
Metabolism
As with many other drugs used in anaesthesia [160, 161], concomitant administration of propofol with other drugs dependent on metabolism by CYP could interfere with its metabolism. In vitro studies demonstrate this possibility, however the results are not directly transposable to the in vivo situation [162].
PD Interactions
Propofol interacts with other intravenous and volatile hypnotic drugs, as well as with opioids. In order to mathematically delineate the interaction between different drugs, their combined effectiveness to reach a certain clinically relevant endpoint is assessed. This combined effectiveness can be explored in an isobolographic analysis using isoboles (or ‘iso-effective’ drug effect dose curves) to show all the dose combinations of drugs resulting in the same clinical effect [163]. The interaction can also be modelled using a response surface modelling technique [164].
Interactions with Hypnotic Drugs
Midazolam
A number of studies have investigated the interaction between propofol and midazolam. All studies confirm, as can be expected based on clinical experience, an interaction, however they do not agree on its nature. The study findings range from an additive to synergistic interaction [165–171]. This discrepancy might be due to study methodologies involving inaccurate PK models, or data collection in a non-steady state.
Dexmedetomidine
Dexmedetomidine is a potent α2 agonist. Multiple studies have investigated its effect on the propofol concentration necessary to reach specific clinical endpoints. When administered preoperatively, dexmedetomidine reduced the propofol dose necessary for sedation and induction of anaesthesia [172, 173]. In adults, a loading dose of 0.1 μg kg−1 administered during a 10-min period reduced the half maximal effective concentration (EC50) of propofol for successful i-gel (Intersurgical, Berkshire, UK) airway insertion from 6.75 to 3.18 µg/mL [174]; a comparable effect was not found in children [175]. The interaction is also evident during and at the end of anaesthesia. Dexmedetomidine reduced propofol use during spinal surgery under propofol–remifentanil anaesthesia, and prolonged recovery times at the end of propofol anaesthesia if it was not stopped early [176, 177]. As with midazolam, a clear interaction model has yet to be developed and a well-designed interaction study needs to be performed, preferably using accurate PK models such as the Eleveld model [61] for propofol and the Hannivoort model for dexmedetomidine [35].
Volatiles
Propofol–sevoflurane interaction studies show an additive interaction, which was demonstrated by studies investigating the effects on clinical endpoints (e.g. loss of consciousness, reaction to laryngoscopy, and reaction to incision), as well as studies measuring the effects on EEG-based parameters from a number of depth of anaesthesia monitors (e.g. Bispectral index, state and response entropy) [178–181]. This additive interaction is not surprising as Sebel et al. demonstrated that propofol and sevoflurane have separate binding sites but converging pathways of action on the GABAα receptor [181, 182].
Interactions with Opioids
Propofol and opioids interact synergistically. This is more pronounced for analgesic drug effects (e.g. loss of response to noxious stimuli) than for hypnotic clinical endpoints, such as loss of responsiveness to verbal commands [154].
Fentanyl significantly decreases the propofol concentration required for loss of consciousness and suppression of responses to noxious stimuli [183]. A ceiling effect of this interaction is seen at fentanyl effect concentrations of 3 ng mL−1, where the propofol plasma concentration necessary for loss of responsiveness to verbal command is decreased by 40% and the concentration necessary for suppression of movement on incision is decreased by 90% compared with when no fentanyl is administered. Further increases in fentanyl concentrations do not increase interaction effects [184].
Sufentanil showed an additive interaction with propofol with respect to loss of responsiveness to verbal command during the induction of anaesthesia. It reduced the propofol concentration necessary for loss of responsiveness in a dose-dependent manner [185]. Hentgen et al. showed that a sufentanil effect site concentration (Ce) of 0.3 ng/mL combined with propofol Ce of 4 ng/mL provides optimal haemodynamic stability during intubation, while a Ce of sufentanil 0.2 ng/mL provides an optimal balance between haemodynamic stability during operation, and a rapid recovery thereafter [186].
Remifentanil is an ultra-short-acting opiate. Its interaction with propofol has been extensively studied in regard to multiple clinical endpoints, and it showed a supra-additive interaction with propofol in regard to hypnotic [187] and analgesic [188] endpoints.
Methods of Drug Delivery
Administration of intravenous hypnotic drugs brings some unique challenges compared with volatile anaesthetics. Multiphasic PK and the inability to continuously measure the achieved drug concentration can present a challenge when trying to achieve a specific drug effect. In the majority of countries worldwide (the US being the main exception), TCI pumps (infusion pumps programmed to infuse a drug guided by a mathematical PK and PD model so as to achieve a predefined plasma or effect site drug concentration expeditiously) are available in order to simplify the administration of propofol [153, 189]. The most well-known PK/PD models for propofol have already been discussed earlier in this article.
Funding
No funding was received in the preparation of this manuscript.
Conflict of interest
Marko M. Sahinovic reports no conflicts of interest. Michel M.R.F. Struys reports his research group/department has received grants and funding from The Medicines Company (Parsippany, NJ, USA), Masimo (Irvine, CA, USA), Fresenius (Bad Homburg, Germany), Acacia Design (Maastricht, The Netherlands), and Medtronic (Dublin, Ireland), as well as honoraria from The Medicines Company (Parsippany, NJ, USA), Masimo (Irvine, CA, USA), Fresenius (Bad Homburg, Germany), Baxter (Deerfield, IL, USA), Medtronic (Dublin, Ireland), and Demed Medical (Temse, Belgium). A.R. Absalom is an editor of the British Journal of Anaesthesia. His research group/department has received grants and funding from The Medicines Company (Parsippany, NJ, USA), Medtronic (Dublin, Ireland), and BD (Franklin Lakes, NJ, USA). He has also received honoraria (paid to the institution) from The Medicines Company (Parsippany, NJ, USA), Janssen Pharmaceutica NV (Beerse, Belgium) and Ever Pharma (Salzburg, Austria).
Contributor Information
Marko M. Sahinovic, Phone: ++31 50 361 3769, Email: M.sahinovic@umcg.nl
Michel M. R. F. Struys, Email: M.M.R.F.Struys@umcg.nl
Anthony R. Absalom, Email: A.R.Absalom@umcg.nl
References
- 1.Glen JB, James R. 2,6-Diisopropylphenol as an anaesthetic agent. London: United States Patent and Trademark Office; 1977. pp. 1–10. [Google Scholar]
- 2.Thompson KA, Goodale DB. The recent development of propofol (DIPRIVAN) Intensive Care Med. 2000;26(Suppl 4):S400–S404. doi: 10.1007/pl00003783. [DOI] [PubMed] [Google Scholar]
- 3.Schüttler J, Schwilden H, editors. Modern anesthetics (handbook of experimental pharmacology) Heidelberg: Springer; 2008. [Google Scholar]
- 4.Baker MT, Naguib M. Propofol: the challenges of formulation. Anesthesiology. 2005;103:860–876. doi: 10.1097/00000542-200510000-00026. [DOI] [PubMed] [Google Scholar]
- 5.Bryson HM, Fulton BR, Faulds D. Propofol. An update of its use in anaesthesia and conscious sedation. Drugs. 1995;50:513–559. doi: 10.2165/00003495-199550030-00008. [DOI] [PubMed] [Google Scholar]
- 6.Fulton B, Sorkin EM. Propofol. An overview of its pharmacology and a review of its clinical efficacy in intensive care sedation. Drugs. 1995;50:636–657. doi: 10.2165/00003495-199550040-00006. [DOI] [PubMed] [Google Scholar]
- 7.Trapani G, Altomare C, Liso G, Sanna E, Biggio G. Propofol in anesthesia. Mechanism of action, structure-activity relationships, and drug delivery. Curr Med Chem. 2000;7:249–271. doi: 10.2174/0929867003375335. [DOI] [PubMed] [Google Scholar]
- 8.Joo HS, Perks WJ. Sevoflurane versus propofol for anesthetic induction: a meta-analysis. Anesth Analg. 2000;91:213–219. doi: 10.1097/00000539-200007000-00040. [DOI] [PubMed] [Google Scholar]
- 9.Liu H, Ji F, Peng K, Applegate RL, Fleming N. Sedation after cardiac surgery: is one drug better than another? Anesth Analg. 2017;124:1061–1070. doi: 10.1213/ANE.0000000000001588. [DOI] [PubMed] [Google Scholar]
- 10.Kochhar GS, Gill A, Vargo JJ. On the horizon: the future of procedural sedation. Gastrointest Endosc Clin N Am. 2016;26:577–592. doi: 10.1016/j.giec.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Marik PE. Propofol: therapeutic indications and side-effects. Curr Pharm Des. 2004;10:3639–3649. doi: 10.2174/1381612043382846. [DOI] [PubMed] [Google Scholar]
- 12.Package insert, Diprivan (Propofol) Injectable Emulsion. Lake Zurich, IL: Fresenius Kabi; 2014.
- 13.Hart B. “Diprivan”: a change of formulation. Eur J Anaesthesiol. 2000;17:71–73. doi: 10.1046/j.1365-2346.2000.00622.x. [DOI] [PubMed] [Google Scholar]
- 14.Pubchem. Propofol. 2017. Available at: https://pubchem.ncbi.nlm.nih.gov/compound/propofol#section=Top.
- 15.Fischer MJM, Leffler A, Niedermirtl F, Kistner K, Eberhardt M, Reeh PW, et al. The general anesthetic propofol excites nociceptors by activating TRPV1 and TRPA1 rather than GABAA receptors. J Biol Chem. 2010;285:34781–34792. doi: 10.1074/jbc.M110.143958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klement W, Arndt JO. Pain on injection of propofol: effects of concentration and diluent. Br J Anaesth. 1991;67:281–284. doi: 10.1093/bja/67.3.281. [DOI] [PubMed] [Google Scholar]
- 17.Allford MA, Mensah JA. Discomfort on injection. Eur J Anaesthesiol. 2006;23:971–974. doi: 10.1017/S0265021506001049. [DOI] [PubMed] [Google Scholar]
- 18.Picard P, Tramèr MR. Prevention of pain on injection with propofol: a quantitative systematic review. Anesth Analg. 2000;90:963–969. doi: 10.1097/00000539-200004000-00035. [DOI] [PubMed] [Google Scholar]
- 19.Hardman JG, Hopkins PM, Struys MMR, editors. Oxford textbook of anaesthesia. Oxford: Oxford University Press; 2017. [Google Scholar]
- 20.Asserhøj LL, Mosbech H, Krøigaard M, Garvey LH. No evidence for contraindications to the use of propofol in adults allergic to egg, soy or peanut. Br J Anaesth. 2016;116:77–82. doi: 10.1093/bja/aev360. [DOI] [PubMed] [Google Scholar]
- 21.American Society for Anesthesiology; Committee for Standards and Practice Parameters. Standards for basic anesthetic monitoring. ASA Standard Guidelines; 2015. p. 1–4. Available at: http://www.asahq.org/quality-and-practice-management/standards-and-guidelines.
- 22.Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876–882. doi: 10.1523/JNEUROSCI.23-03-00876.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jevtovic-Todorovic V, Absalom AR, Blomgren K, Brambrink A, Crosby G, Culley DJ, et al. Anaesthetic neurotoxicity and neuroplasticity: an expert group report and statement based on the BJA Salzburg Seminar. Br J Anaesth. 2013;111:143–151. doi: 10.1093/bja/aet177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raoof AA, Augustijns PR, Verbeeck RK. In vivo assessment of intenstinal, hepatic, and pulmonary first pass metabolism of propofol in the rat. Pharm Res. 1996;13:891–895. doi: 10.1023/a:1016057229478. [DOI] [PubMed] [Google Scholar]
- 25.Uchegbu I, Jones M-C, Corrente F, Godfrey L, Laghezza D, Carafa M, et al. The oral and intranasal delivery of propofol using chitosan amphiphile nanoparticles. Pharm Nanotechnol. 2014;2:65–74. [Google Scholar]
- 26.Mazoit JX, Samii K. Binding of propofol to blood components: implications for pharmacokinetics and for pharmacodynamics. Br J Clin Pharmacol. 1999;47:35–42. doi: 10.1046/j.1365-2125.1999.00860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tarr L, Oppenheimer B, Sager R. The circulation time in various clinical conditions determined by the use of sodium dehydrochlorate. Am Heart J. 1933;8:766. [Google Scholar]
- 28.Dawidowicz AL, Kalitynski R, Fijalkowska A. Free and bound propofol concentrations in human cerebrospinal fluid. Br J Clin Pharmacol. 2003;56:545–550. doi: 10.1046/j.1365-2125.2003.01920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Engdahl O, Abrahams M, Björnsson A, et al. Cerebrospinal fluid concentrations of propofol during anaesthesia in humans. Br J Anaesth. 1998;81:957–959. doi: 10.1093/bja/81.6.957. [DOI] [PubMed] [Google Scholar]
- 30.Dailland P, Cockshott ID, Lirzin JD, Jacquinot P, Jorrot JC, Devery J, et al. Intravenous propofol during cesarean section: placental transfer, concentrations in breast milk, and neonatal effects. A preliminary study. Anesthesiology. 1989;71:827–834. doi: 10.1097/00000542-198912000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Gin T, Yau G, Jong W, Tan P, Leung RKW, Chan K. Disposition of propofol at caesarina section and in the postpartum period. Br J Anaesth. 1991;67:49–53. doi: 10.1093/bja/67.1.49. [DOI] [PubMed] [Google Scholar]
- 32.Tumukunde J, Lomangisi DD, Davidson O, Kintu A, Joseph E, Kwizera A. Effects of propofol versus thiopental on Apgar scores in newborns and peri-operative outcomes of women undergoing emergency cesarean section: a randomized clinical trial. BMC Anesthesiol. 2015;15:63. doi: 10.1186/s12871-015-0044-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Simons P. J., Cockshott I. D., Douglas E. J., Gordon E. A., Hopkins K., Rowland M. Disposition in male volunteers of a subanaesthetic intravenous dose of an oil in water emulsion of14C-propofol. Xenobiotica. 1988;18(4):429–440. doi: 10.3109/00498258809041679. [DOI] [PubMed] [Google Scholar]
- 34.Hughes MA, Glass PS, Jacobs JR. Context-sensitive half-time in multicompartment pharmacokinetic models for intravenous anesthetic drugs. Anesthesiology. 1992;76:334–341. doi: 10.1097/00000542-199203000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Hannivoort LN, Eleveld DJ, Proost JH, Reyntjens KMEM, Absalom AR, Vereecke HEM, et al. Development of an optimized pharmacokinetic model of dexmedetomidine using target-controlled infusion in healthy volunteers. Anesthesiology. 2015;123:357–367. doi: 10.1097/ALN.0000000000000740. [DOI] [PubMed] [Google Scholar]
- 36.Court MH, Duan SX, Hesse LM, Venkatakrishnan K, Greenblatt DJ. Cytochrome P-450 2B6 is responsible for interindividual variability of propofol hydroxylation by human liver microsomes. Anesthesiology. 2001;94:110–119. doi: 10.1097/00000542-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 37.Shioya N, Ishibe Y, Shibata S, Makabe H, Kan S, Matsumoto N, et al. Green urine discoloration due to propofol infusion: a case report. Case Rep Emerg Med. 2011;2011:1–4. doi: 10.1155/2011/242514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mikstacki A, Skrzypczak-Zielinska M, Tamowicz B, Zakerska-Banaszak O, Szalata M, Slomski R. The impact of genetic factors on response to anaesthetics. Adv Med Sci. 2013;58:9–14. doi: 10.2478/v10039-012-0065-z. [DOI] [PubMed] [Google Scholar]
- 39.Takizawa D, Sato E, Hiraoka H, Tomioka A, Yamamoto K, Horiuchi R, et al. Changes in apparent systemic clearance of propofol during transplantation of living related donor liver. Br J Anaesth. 2005;95:643–647. doi: 10.1093/bja/aei243. [DOI] [PubMed] [Google Scholar]
- 40.Hiraoka H, Yamamoto K, Miyoshi S, Morita T, Nakamura K, Kadoi Y, et al. Kidneys contribute to the extrahepatic clearance of propofol in humans, but not lungs and brain. Br J Clin Pharmacol. 2005;60:176–182. doi: 10.1111/j.1365-2125.2005.02393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Takizawa D, Hiraoka H, Goto F, Yamamoto K, Horiuchi R. Human kidneys play an important role in the elimination of propofol. Anesthesiology. 2005;102:327–330. doi: 10.1097/00000542-200502000-00014. [DOI] [PubMed] [Google Scholar]
- 42.Dawidowicz AL, Fornal E, Mardarowicz M, Fijalkowska A. The role of human lungs in the biotransformation of propofol. Anesthesiology. 2000;93:992–997. doi: 10.1097/00000542-200010000-00020. [DOI] [PubMed] [Google Scholar]
- 43.He YL, Ueyama H, Tashiro C, Mashimo T, Yoshiya I. Pulmonary disposition of propofol in surgical patients. Anesthesiology. 2000;93:986–991. doi: 10.1097/00000542-200010000-00019. [DOI] [PubMed] [Google Scholar]
- 44.Bodenham A, Culank LS, Park GR. Propofol infusion and green urine. Lancet. 1987;2:740. doi: 10.1016/s0140-6736(87)91097-x. [DOI] [PubMed] [Google Scholar]
- 45.Takita A, Masui K, Kazama T. On-line monitoring of end-tidal propofol concentration in anesthetized patients. Anesthesiology. 2007;106:659–664. doi: 10.1097/01.anes.0000264745.63275.59. [DOI] [PubMed] [Google Scholar]
- 46.Grossherr M, Hengstenberg A, Meier T, Dibbelt L, Gerlach K, Gehring H. Discontinuous monitoring of propofol concentrations in expired alveolar gas and in arterial and venous plasma during artificial ventilation. Anesthesiology. 2006;104:786–790. doi: 10.1097/00000542-200604000-00024. [DOI] [PubMed] [Google Scholar]
- 47.Colin P, Eleveld DJ, van den Berg JP, Vereecke HEM, Struys MMRF, Schelling G, et al. Propofol breath monitoring as a potential tool to improve the prediction of intraoperative plasma concentrations. Clin Pharmacokinet. 2016;55:849–859. doi: 10.1007/s40262-015-0358-z. [DOI] [PubMed] [Google Scholar]
- 48.B. Braun. Exhaled propofol concentration monitor, Edmon. Available at: https://www.bbraun.com/en/products/b1/edmon.html.
- 49.Gepts E, Camu F, Cockshott ID, Douglas EJ. Disposition of propofol administered as constant rate intravenous infusions in humans. Anesth Analg. 1987;66:1256–1263. [PubMed] [Google Scholar]
- 50.Shafer A, Doze VA, Shafer SL, White PF. Pharmacokinetics and pharmacodynamics of propofol infusions during general anesthesia. Anesthesiology. 1988;69:348–356. doi: 10.1097/00000542-198809000-00011. [DOI] [PubMed] [Google Scholar]
- 51.Kirkpatrick T, Cockshott ID, Douglas EJ, Nimmo WS. Pharmacokinetics of propofol (diprivan) in elderly patients. Br J Anaesth. 1988;60:146–150. doi: 10.1093/bja/60.2.146. [DOI] [PubMed] [Google Scholar]
- 52.Schüttler J, Ihmsen H. Population pharmacokinetics of propofol: a multicenter study. Anesthesiology. 2000;92:727–738. doi: 10.1097/00000542-200003000-00017. [DOI] [PubMed] [Google Scholar]
- 53.Wietasch JKG, Scholz M, Zinserling J, Kiefer N, Frenkel C, Knüfermann P, et al. The performance of a target-controlled infusion of propofol in combination with remifentanil: a clinical investigation with two propofol formulations. Anesth Analg. 2006;102:430–437. doi: 10.1213/01.ane.0000189821.81675.b4. [DOI] [PubMed] [Google Scholar]
- 54.Struys MMRF, Sahinovic MM, Lichtenbelt BJ, Vereecke HEM, Absalom AR. Optimizing intravenous drug administration by applying pharmacokinetic/pharmacodynamic concepts. Br J Anaesth. 2011;107:38–47. doi: 10.1093/bja/aer108. [DOI] [PubMed] [Google Scholar]
- 55.Sahinovic MM. Intravenous drug dose optimization and drug effect monitoring in anaesthesia. Groningen: Rijksuniversiteit Groningen; 2017. [Google Scholar]
- 56.Green B, Duffull SB. What is the best size descriptor to use for pharmacokinetic studies in the obese? Br J Clin Pharmacol. 2004;58:119–133. doi: 10.1111/j.1365-2125.2004.02157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Eleveld DJ, Proost JH, Absalom AR, Struys MMRF. Obesity and allometric scaling of pharmacokinetics. Clin Pharmacokinet. 2011;50:751–753. doi: 10.2165/11594080-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 58.Snell O. Die Abhängigkeit des Hirngewichtes von dem Körpergewicht und den geistigen Fähigkeiten. Arch Psychiatr Nervenkr. 1892;23:436–446. [Google Scholar]
- 59.Huxley JS, Needham J, Lerner IM. Terminology of relative growth-rates. Nature. 1941;148:225. [Google Scholar]
- 60.Wang C, Allegaert K, Peeters MYM, Tibboel D, Danhof M, Knibbe CAJ. The allometric exponent for scaling clearance varies with age: a study on seven propofol datasets ranging from preterm neonates to adults. Br J Clin Pharmacol. 2014;77:149–159. doi: 10.1111/bcp.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eleveld DJ, Colin P, Absalom AR, Struys MMRF. Pharmacokinetic-pharmacodynamic model for propofol for broad application in anaesthesia and sedation. Br J Anaesth. 2018;120(5):942–959. doi: 10.1016/j.bja.2018.01.018. [DOI] [PubMed] [Google Scholar]
- 62.Eleveld DJ, Proost JH, Vereecke H, Absalom AR, Olofsen E, Vuyk J, et al. An allometric model of remifentanil pharmacokinetics and pharmacodynamics. Anesthesiology. 2017;126:1005–1018. doi: 10.1097/ALN.0000000000001634. [DOI] [PubMed] [Google Scholar]
- 63.West GB, et al. A general model for the origin of allometric scaling laws in biology. Science. 1997;276:122–126. doi: 10.1126/science.276.5309.122. [DOI] [PubMed] [Google Scholar]
- 64.Proost J. Pharmacokinetic-pharmacodynamic modelling of anesthetic drugs. In: Absalom AR, Mason KP, editors. Total intravenous anesthesia and target controlled infusions. Cham: Springer International Publishing; 2017. [Google Scholar]
- 65.Marsh B, White M, Morton N, Kenny GN. Pharmacokinetic model driven infusion of propofol in children. Br J Anaesth. 1991;67:41–48. doi: 10.1093/bja/67.1.41. [DOI] [PubMed] [Google Scholar]
- 66.Schnider TW, Minto CF, Gambus PL, Andresen C, Goodale DB, Shafer SL, et al. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology. 1998;88:1170–1182. doi: 10.1097/00000542-199805000-00006. [DOI] [PubMed] [Google Scholar]
- 67.Absalom AR, Mani V, De Smet T, Struys MMRF. Pharmacokinetic models for propofol: defining and illuminating the devil in the detail. Br J Anaesth. 2009;103:26–37. doi: 10.1093/bja/aep143. [DOI] [PubMed] [Google Scholar]
- 68.De Baerdemaeker LEC, Mortier EP, Struys MMRF. Pharmacokinetics in obese patients. Contin Educ Anaesth Crit Care Pain. 2004;4:152–155. [Google Scholar]
- 69.Cortínez LI, Anderson BJ, Penna A, Olivares L, Munoz HR, Holford NHG, et al. Influence of obesity on propofol pharmacokinetics: derivation of a pharmacokinetic model. Br J Anaesth. 2010;105:448–456. doi: 10.1093/bja/aeq195. [DOI] [PubMed] [Google Scholar]
- 70.van Kralingen S, Diepstraten J, Peeters MYM, Deneer VHM, van Ramshorst B, Wiezer RJ, et al. Population pharmacokinetics and pharmacodynamics of propofol in morbidly obese patients. Clin Pharmacokinet. 2011;50:739–750. doi: 10.2165/11592890-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 71.Cortínez LI, De la Fuente N, Eleveld DJ, Oliveros A, Crovari F, Sepúlveda P, et al. Performance of propofol target-controlled infusion models in the obese: pharmacokinetic and pharmacodynamic analysis. Anesth Analg. 2014;119:302–310. doi: 10.1213/ANE.0000000000000317. [DOI] [PubMed] [Google Scholar]
- 72.Eleveld DJ, Proost JH, Cortínez LI, Absalom AR, Struys MMRF. A general purpose pharmacokinetic model for propofol. Anesth Analg. 2014;118:1221–1237. doi: 10.1213/ANE.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 73.Absalom AR. “Paedfusor” pharmacokinetic data set. Br J Anaesth. 2005;95:110. doi: 10.1093/bja/aei567. [DOI] [PubMed] [Google Scholar]
- 74.Kataria BK, Ved SA, Nicodemus HF, Hoy GR, Lea D, Dubois MY, et al. The pharmacokinetics of propofol in children using three different data analysis approaches. Anesthesiology. 1994;80:104–122. doi: 10.1097/00000542-199401000-00018. [DOI] [PubMed] [Google Scholar]
- 75.Short TG, Aun CS, Tan P, Wong J, Tam YH, Oh TE. A prospective evaluation of pharmacokinetic model controlled infusion of propofol in paediatric patients. Br J Anaesth. 1994;72:302–306. doi: 10.1093/bja/72.3.302. [DOI] [PubMed] [Google Scholar]
- 76.Sepúlveda P, Cortínez LI, Sáez C, Penna A, Solari S, Guerra I, et al. Performance evaluation of paediatric propofol pharmacokinetic models in healthy young children. Br J Anaesth. 2011;107:593–600. doi: 10.1093/bja/aer198. [DOI] [PubMed] [Google Scholar]
- 77.Hara M, Masui K, Eleveld DJ, Struys MMRF, Uchida O. Predictive performance of eleven pharmacokinetic models for propofol infusion in children for long-duration anaesthesia. Br J Anaesth. 2017;118:415–423. doi: 10.1093/bja/aex007. [DOI] [PubMed] [Google Scholar]
- 78.Knibbe CAJ, Zuideveld KP, Aarts LPHJ, Kuks PFM, Danhof M. Allometric relationships between the pharmacokinetics of propofol in rats, children and adults. Br J Clin Pharmacol. 2005;59:705–711. doi: 10.1111/j.1365-2125.2005.02239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hoymork SC, Raeder J, Grimsmo B, Steen PA. Bispectral index, serum drug concentrations and emergence associated with individually adjusted target-controlled infusions of remifentanil and propofol for laparoscopic surgery. Br J Anaesth. 2003;91:773–780. doi: 10.1093/bja/aeg258. [DOI] [PubMed] [Google Scholar]
- 80.Jones H, Rowland-Yeo K. Basic concepts in physiologically based pharmacokinetic modeling in drug discovery and development. CPT Pharmacomet Syst Pharmacol. 2013;2:e63. doi: 10.1038/psp.2013.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Masui K, Kira M, Kazama T, Hagihira S, Mortier EP, Struys MMRF. Early phase pharmacokinetics but not pharmacodynamics are influenced by propofol infusion rate. Anesthesiology. 2009;111:805–817. doi: 10.1097/ALN.0b013e3181b799c1. [DOI] [PubMed] [Google Scholar]
- 82.Upton RN, Ludbrook GL, Grant C, Martinez AM. Cardiac output is a determinant of the initial concentrations of propofol after short-infusion administration. Anesth Analg. 1999;89:545–552. doi: 10.1097/00000539-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 83.Masui K, Upton RN, Doufas AG, Coetzee JF, Kazama T, Mortier EP, et al. The performance of compartmental and physiologically based recirculatory pharmacokinetic models for propofol. Anesth Analg. 2010;111:368–379. doi: 10.1213/ANE.0b013e3181bdcf5b. [DOI] [PubMed] [Google Scholar]
- 84.Upton RN, Ludbrook G. The performance of compartmental and physiologically based recirculatory pharmacokinetic models for propofol: a comparison using bolus, continuous, and target-controlled infusion data. Anesthesiology. 2005;103:344–352. doi: 10.1213/ANE.0b013e3181bdcf5b. [DOI] [PubMed] [Google Scholar]
- 85.Rudolph U, Antkowiak B. Molecular and neuronal substrates for general anaesthetics. Nat Rev Neurosci. 2004;5:709–720. doi: 10.1038/nrn1496. [DOI] [PubMed] [Google Scholar]
- 86.Sieghart W. Structure and pharmacology of gamma-aminobutyric acidA receptor subtypes. Pharmacol Rev. 1995;47:181–234. [PubMed] [Google Scholar]
- 87.Bormann J. The, “ABC” of GABA receptors. Trends Pharmacol Sci. 2000;21:16–19. doi: 10.1016/s0165-6147(99)01413-3. [DOI] [PubMed] [Google Scholar]
- 88.Adapa RM. Consiousness and anesthesia. In: Absalom AR, Mason KP, editors. Total intravenous anesthesia and target controlled infusions. Cham: Springer International Publishing; 2017. pp. 63–78. [Google Scholar]
- 89.Moruzzi G, Magoun HW. Brain stem reticular formation and activation of the EEG. Electroencephalogr Clin Neurophysiol. 1949;1:455–473. [PubMed] [Google Scholar]
- 90.Saper CB, Fuller PM, Pedersen NP, Lu J, Scammell TE. Sleep state switching. Neuron. 2010;68:1023–1042. doi: 10.1016/j.neuron.2010.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Saper CB, Chou TC, Scammell TE. The sleep switch: hypothalamic control of sleep and wakefulness. Trends Neurosci. 2001;24:726–731. doi: 10.1016/s0166-2236(00)02002-6. [DOI] [PubMed] [Google Scholar]
- 92.Leung LS, Luo T, Ma J, Herrick I. Brain areas that influence general anesthesia. Prog Neurobiol. 2014;122:24–44. doi: 10.1016/j.pneurobio.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 93.Fiset P, Paus T, Daloze T, Plourde G, Meuret P, Bonhomme V, et al. Brain mechanisms of propofol-induced loss of consciousness in humans: a positron emission tomographic study. J Neurosci. 1999;19:5506–5513. doi: 10.1523/JNEUROSCI.19-13-05506.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mashour GA, Alkire MT. Consciousness, anesthesia, and the thalamocortical system. Anesthesiology. 2013;118:13–15. doi: 10.1097/ALN.0b013e318277a9c6. [DOI] [PubMed] [Google Scholar]
- 95.Detsch O, Vahle-Hinz C, Kochs E, Siemers M, Bromm B. Isoflurane induces dose-dependent changes of thalamic somatosensory information transfer. Brain Res. 1999;829:77–89. doi: 10.1016/s0006-8993(99)01341-4. [DOI] [PubMed] [Google Scholar]
- 96.Velly LJ, Rey MF, Bruder NJ, Gouvitsos FA, Witjas T, Regis JM, et al. Differential dynamic of action on cortical and subcortical structures of anesthetic agents during induction of anesthesia. Anesthesiology. 2007;107:202–212. doi: 10.1097/01.anes.0000270734.99298.b4. [DOI] [PubMed] [Google Scholar]
- 97.Alkire MT, Haier RJ, Fallon JH. Toward a unified theory of narcosis: brain imaging evidence for a thalamocortical switch as the neurophysiologic basis of anesthetic-induced unconsciousness. Conscious Cogn. 2000;9:370–386. doi: 10.1006/ccog.1999.0423. [DOI] [PubMed] [Google Scholar]
- 98.Brown EN, Lydic R, Schiff ND. General anesthesia, sleep, and coma. N Engl J Med. 2010;363:2638–2650. doi: 10.1056/NEJMra0808281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kaisti KK, Langsjo JW, Aalto S, Oikonen V, Sipila H, Teras M, et al. Effects of sevoflurane, propofol and adjunct nitrous oxide on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology. 2003;99:603–613. doi: 10.1097/00000542-200309000-00015. [DOI] [PubMed] [Google Scholar]
- 100.Boly M, Perlbarg V, Marrelec G, Schabus M, Laureys S, Doyon J, et al. Hierarchical clustering of brain activity during human nonrapid eye movement sleep. Proc Natl Acad Sci USA. 2012;109:5856–5861. doi: 10.1073/pnas.1111133109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ferrarelli F, Massimini M, Sarasso S, Casali A, Riedner BA, Angelini G, et al. Breakdown in cortical effective connectivity during midazolam-induced loss of consciousness. Proc Natl Acad Sci USA. 2010;107:2681–2686. doi: 10.1073/pnas.0913008107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Massimini M, Ferrarelli F, Huber R, Esser SK, Singh H, Tononi G. Breakdown of cortical effective connectivity during sleep. Science. 2005;309:2228–2232. doi: 10.1126/science.1117256. [DOI] [PubMed] [Google Scholar]
- 103.Tononi G. An information integration theory of consciousness. BMC Neurosci. 2004;5:42. doi: 10.1186/1471-2202-5-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nordström O, Sandin R. Recall during intermittent propofol anaesthesia. Br J Anaesth. 1996;76:699–701. doi: 10.1093/bja/76.5.699. [DOI] [PubMed] [Google Scholar]
- 105.Andrade J, Deeprose C. Unconscious memory formation during anaesthesia. Best Pract Res Clin Anaesthesiol. 2007;21:385–401. doi: 10.1016/j.bpa.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 106.Veselis RA, Pryor KO, Reinsel RA, Mehta M, Pan H, Johnson R. Low-dose propofol-induced amnesia is not due to a failure of encoding: left inferior prefrontal cortex is still active. Anesthesiology. 2008;109:213–224. doi: 10.1097/ALN.0b013e31817fd8ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kurt M, Bilge SS, Kukula O, Celik S, Kesim Y. Anxiolytic-like profile of propofol, a general anesthetic, in the plus-maze test in mice. Pol J Pharmacol. 2003;55:973–977. [PubMed] [Google Scholar]
- 108.Smith I, Monk TG, White PF, Ding Y. Propofol infusion during regional anesthesia: sedative, amnestic, and anxiolytic properties. Anesth Analg. 1994;79:313–319. doi: 10.1213/00000539-199408000-00020. [DOI] [PubMed] [Google Scholar]
- 109.Ure RW, Dwyer SJ, Blogg CE, White AP. Patient-controlled anxiolysis with propofol. Br J Anaesth. 1991;67:857P–858P. [Google Scholar]
- 110.Matsuo M, Ayuse T, Oi K, Kataoka Y. Propofol produces anticonflict action by inhibiting 5-HT release in rat dorsal hippocampus. NeuroReport. 1997;8:3087–3090. doi: 10.1097/00001756-199709290-00016. [DOI] [PubMed] [Google Scholar]
- 111.Volke V, Kõks S, Vasar E, Bourin M, Bradwejn J, Männistö PT. Inhibition of nitric oxide synthase causes anxiolytic-like behaviour in an elevated plus-maze. NeuroReport. 1995;6:1413–1416. doi: 10.1097/00001756-199507100-00013. [DOI] [PubMed] [Google Scholar]
- 112.Zacny JP, Coalson DW, Young CJ, Klafta JM, Lichtor JL, Rupani G, et al. Propofol at conscious sedation doses produces mild analgesia to cold pressor-induced pain in healthy volunteers. J Clin Anesth. 1996;8:469–474. doi: 10.1016/0952-8180(96)00126-2. [DOI] [PubMed] [Google Scholar]
- 113.Anker-Moller E, Spangsberg N, Arendt-Nielsen L, Schultz P, Krinstensen M, Bjerring P. Subhypnotic doses of thiopentone and propofol cause analgesia to experimentally induced acute pain. Br J Anaesth. 1991;66:185–188. doi: 10.1093/bja/66.2.185. [DOI] [PubMed] [Google Scholar]
- 114.Nadeson R, Goodchild CS. Antinociceptive properties of propofol: involvement of spinal cord gamma-aminobutyric acid(A) receptors. J Pharmacol Exp Ther. 1997;282:1181–1186. [PubMed] [Google Scholar]
- 115.Jewett BA, Gibbs LM, Tarasiuk A, Kendig JJ. Propofol and barbiturate depression of spinal nociceptive neurotransmission. Anesthesiology. 1992;77:1148–1154. doi: 10.1097/00000542-199212000-00016. [DOI] [PubMed] [Google Scholar]
- 116.Nishiyama T, Matsukawa T, Hanaoka K. Intrathecal propofol has analgesic effects on inflammation-induced pain in rats. Can J Anaesth. 2004;51:899–904. doi: 10.1007/BF03018887. [DOI] [PubMed] [Google Scholar]
- 117.Peng K, Liu H-Y, Wu S-R, Liu H, Zhang Z-C, Ji F-H. Does propofol anesthesia lead to less postoperative pain compared with inhalational anesthesia? A systematic review and meta-analysis. Anesth Analg. 2016;123:846–858. doi: 10.1213/ANE.0000000000001504. [DOI] [PubMed] [Google Scholar]
- 118.Borgeat A, Stirnemann HR. Antiemetische Wirkung von propofol. Anaesthesist. 1998;47:918–924. doi: 10.1007/s001010050643. [DOI] [PubMed] [Google Scholar]
- 119.Sneyd JR, Carr A, Byrom WD, Bilski AJ. A meta-analysis of nausea and vomiting following maintenance of anaesthesia with propofol or inhalational agents. Eur J Anaesthesiol. 1998;15:433–445. doi: 10.1046/j.1365-2346.1998.00319.x. [DOI] [PubMed] [Google Scholar]
- 120.Reddi KK. Nature and possible origin of human serum ribonuclease. Biochem Biophys Res Commun. 1975;67:110–118. doi: 10.1016/0006-291x(75)90290-9. [DOI] [PubMed] [Google Scholar]
- 121.CAVAZZUTI M., PORRO C.A., BARBIERI A., GALETTI A. BRAIN AND SPINAL CORD METABOLIC ACTIVITY DURING PROPOFOL ANAESTHESIA. British Journal of Anaesthesia. 1991;66(4):490–495. doi: 10.1093/bja/66.4.490. [DOI] [PubMed] [Google Scholar]
- 122.Strebel S, Lam AM, Matta B, Mayberg TS, Aaslid R, Newell DW. Dynamic and static cerebral autoregulation during isoflurane, desflurane, and propofol anesthesia. Anesthesiology. 1995;83:66–76. doi: 10.1097/00000542-199507000-00008. [DOI] [PubMed] [Google Scholar]
- 123.Fox J, Gelb AW, Enns J, Murkin JM, Farrar JK, Manninen PH. The responsiveness of cerebral blood flow to changes in arterial carbon dioxide is maintained during propofol-nitrous oxide anesthesia in humans. Anesthesiology. 1992;77:453–456. doi: 10.1097/00000542-199209000-00008. [DOI] [PubMed] [Google Scholar]
- 124.Kotani Y, Nakajima Y, Hasegawa T, Satoh M, Nagase H, Shimazawa M, et al. Propofol exerts greater neuroprotection with disodium edetate than without it. J Cereb Blood Flow Metab. 2008;28:354–366. doi: 10.1038/sj.jcbfm.9600532. [DOI] [PubMed] [Google Scholar]
- 125.Fan W, Zhu X, Wu L, Wu Z, Li D, Huang F, et al. Propofol: an anesthetic possessing neuroprotective effects. Eur Rev Med Pharmacol Sci. 2015;19:1520–1529. [PubMed] [Google Scholar]
- 126.Sneyd JR. Excitatory events associated with propofol anaesthesia: a review. J R Soc Med. 1992;85:288–291. doi: 10.1177/014107689208500516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rampil IJ. A primer for EEG signal processing in anesthesia. Anesthesiology. 1998;89:980–1002. doi: 10.1097/00000542-199810000-00023. [DOI] [PubMed] [Google Scholar]
- 128.Samra SK, Sneyd JR, Ross DA, Henry TR. Effects of propofol sedation on seizures and intracranially recorded epileptiform activity in patients with partial epilepsy. Anesthesiology. 1995;82:843–851. doi: 10.1097/00000542-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 129.Hug CC, McLeskey CH, Nahrwold ML, Roizen MF, Stanley TH, Thisted RA, et al. Hemodynamic effects of propofol: data from over 25,000 patients. Anesth Analg. 1993;77:S21–S29. [PubMed] [Google Scholar]
- 130.Ebert TJ. Sympathetic and hemodynamic effects of moderate and deep sedation with propofol in humans. Anesthesiology. 2005;103:20–24. doi: 10.1097/00000542-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 131.Sprung J, Ogletree-Hughes ML, McConnell BK, Zakhary DR, Smolsky SM, Moravec CS. The effects of propofol on the contractility of failing and nonfailing human heart muscles. Anesth Analg. 2001;93:550–559. doi: 10.1097/00000539-200109000-00006. [DOI] [PubMed] [Google Scholar]
- 132.Kazama T, Ikeda K, Morita K, Kikura M, Doi M, Ikeda T, et al. Comparison of the effect-site k(eO)s of propofol for blood pressure and EEG bispectral index in elderly and younger patients. Anesthesiology. 1999;90:1517–1527. doi: 10.1097/00000542-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 133.Xia Z, Godin DV, Ansley DM. Application of high-dose propofol during ischemia improves postischemic function of rat hearts: effects on tissue antioxidant capacity. Can J Physiol Pharmacol. 2004;82:919–926. doi: 10.1139/y04-097. [DOI] [PubMed] [Google Scholar]
- 134.Li F, Yuan Y. Meta-analysis of the cardioprotective effect of sevoflurane versus propofol during cardiac surgery. BMC Anesthesiol. 2015;15:128. doi: 10.1186/s12871-015-0107-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Huang Zhiyong, Zhong Xingwu, Irwin Michael G., Ji Shangyi, Wong Gordon T., Liu Yanan, Xia Zhong-yuan, Finegan Barry A., Xia Zhengyuan. Synergy of isoflurane preconditioning and propofol postconditioning reduces myocardial reperfusion injury in patients. Clinical Science. 2011;121(2):57–69. doi: 10.1042/CS20100435. [DOI] [PubMed] [Google Scholar]
- 136.Nieuwenhuijs D, Sarton E, Teppema L, Dahan A. Propofol for monitored anesthesia care: implications on hypoxic control of cardiorespiratory responses. Anesthesiology. 2000;92:46–54. doi: 10.1097/00000542-200001000-00013. [DOI] [PubMed] [Google Scholar]
- 137.Nieuwenhuijs D, Sarton E, Teppema LJ, Kruyt E, Olievier I, van Kleef J, et al. Respiratory sites of action of propofol: absence of depression of peripheral chemoreflex loop by low-dose propofol. Anesthesiology. 2001;95:889–895. doi: 10.1097/00000542-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 138.Jonsson MM, Lindahl SGE, Eriksson LI. Effect of propofol on carotid body chemosensitivity and cholinergic chemotransduction. Anesthesiology. 2005;102:110–116. doi: 10.1097/00000542-200501000-00019. [DOI] [PubMed] [Google Scholar]
- 139.Yamakage M, Kamada Y, Toriyabe M, Honma Y, Namiki A. Changes in respiratory pattern and arterial blood gases during sedation with propofol or midazolam in spinal anesthesia. J Clin Anesth. 1999;11:375–379. doi: 10.1016/s0952-8180(99)00064-1. [DOI] [PubMed] [Google Scholar]
- 140.McKeating K, Bali IM, Dundee JW. The effects of thiopentone and propofol on upper airway integrity. Anaesthesia. 1988;43:638–640. doi: 10.1111/j.1365-2044.1988.tb04146.x. [DOI] [PubMed] [Google Scholar]
- 141.Kabara S, Hirota K, Hashiba E, Yoshioka H, Kudo T, Sato T, et al. Comparison of relaxant effects of propofol on methacholine-induced bronchoconstriction in dogs with and without vagotomy. Br J Anaesth. 2001;86:249–253. doi: 10.1093/bja/86.2.249. [DOI] [PubMed] [Google Scholar]
- 142.Nakayama M, Murray PA. Ketamine preserves and propofol potentiates hypoxic pulmonary vasoconstriction compared with the conscious state in chronically instrumented dogs. Anesthesiology. 1999;91:760–771. doi: 10.1097/00000542-199909000-00029. [DOI] [PubMed] [Google Scholar]
- 143.Meierhenrich R, Gauss A, Mühling B, Bracht H, Radermacher P, Georgieff M, et al. The effect of propofol and desflurane anaesthesia on human hepatic blood flow: a pilot study. Anaesthesia. 2010;65:1085–1093. doi: 10.1111/j.1365-2044.2010.06504.x. [DOI] [PubMed] [Google Scholar]
- 144.Latte D. Demeure, Bernard J.-M., Blanloeil Y., Peltier P., Francois T., Chatal J.-F. Induction of anaesthesia by propofol and hepatic blood flow in the rabbit. Clinical Physiology. 1995;15(5):515–522. doi: 10.1111/j.1475-097x.1995.tb00540.x. [DOI] [PubMed] [Google Scholar]
- 145.Zhu Tao, Pang Qiying, McCluskey Stuart A., Luo Chaozhi. Effect of propofol on hepatic blood flow and oxygen balance in rabbits. Canadian Journal of Anesthesia/Journal canadien d'anesthésie. 2008;55(6):364–370. doi: 10.1007/BF03021492. [DOI] [PubMed] [Google Scholar]
- 146.Wouters Patrick F., Van de Velde Marc A., Marcus Marco A. E., Deruyter Hendrik A., Van Aken Hugo. Hemodynamic Changes During Induction of Anesthesia with Eltanolone and Propofol in Dogs. Anesthesia & Analgesia. 1995;81(1):125–131. doi: 10.1097/00000539-199507000-00025. [DOI] [PubMed] [Google Scholar]
- 147.Palanca BJ, Mashour GA, Avidan MS. Processed electroencephalogram in depth of anesthesia monitoring. Curr Opin Anaesthesiol. 2009;22:553–559. doi: 10.1097/ACO.0b013e3283304032. [DOI] [PubMed] [Google Scholar]
- 148.Bruhn J, Myles PS, Sneyd R, Struys MMRF. Depth of anaesthesia monitoring: what’s available, what’s validated and what’s next? Br J Anaesth. 2006;97:85–94. doi: 10.1093/bja/ael120. [DOI] [PubMed] [Google Scholar]
- 149.Sahinovic MM, Eleveld DJ, Miyabe-Nishiwaki T, Struys MMRF, Absalom AR. Pharmacokinetics and pharmacodynamics of propofol: changes in patients with frontal brain tumours. Br J Anaesth. 2017;118:901–909. doi: 10.1093/bja/aex134. [DOI] [PubMed] [Google Scholar]
- 150.Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, et al. The influence of age on propofol pharmacodynamics. Anesthesiology. 1999;90:1502–1516. doi: 10.1097/00000542-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 151.Billard V, Gambus PL, Chamoun N, Stanski DR, Shafer SL. A comparison of spectral edge, delta power, and bispectral index as EEG measures of alfentanil, propofol, and midazolam drug effect. Clin Pharmacol Ther. 1997;61:45–58. doi: 10.1016/S0009-9236(97)90181-8. [DOI] [PubMed] [Google Scholar]
- 152.Seo JH, Goo EK, Song IA, Park SH, Park HP, Jeon YT, et al. Influence of a modified propofol equilibration rate constant (k(e0)) on the effect-site concentration at loss and recovery of consciousness with the Marsh model. Anaesthesia. 2013;68:1232–1238. doi: 10.1111/anae.12419. [DOI] [PubMed] [Google Scholar]
- 153.Sahinovic MM, Absalom AR, Struys MMRF. Administration and monitoring of intravenous anesthetics. Curr Opin Anaesthesiol. 2010;23:734–740. doi: 10.1097/ACO.0b013e3283404579. [DOI] [PubMed] [Google Scholar]
- 154.van den Berg JP, Vereecke HEM, Proost JH, Eleveld DJ, Wietasch JKG, Absalom AR, et al. Pharmacokinetic and pharmacodynamic interactions in anaesthesia. A review of current knowledge and how it can be used to optimize anaesthetic drug administration. Br J Anaesth. 2017;118:44–57. doi: 10.1093/bja/aew312. [DOI] [PubMed] [Google Scholar]
- 155.Michaels MR, Stauffer GL, Haas DP. Propofol compatibility with other intravenous drug products: two new methods of evaluating IV emulsion compatibility. Ann Pharmacother. 1996;30:228–232. doi: 10.1177/106002809603000303. [DOI] [PubMed] [Google Scholar]
- 156.Schmidt S, Gonzalez D, Derendorf H. Significance of protein binding in pharmacokinetics and pharmacodynamics. J Pharm Sci. 2010;99:1107–1122. doi: 10.1002/jps.21916. [DOI] [PubMed] [Google Scholar]
- 157.Wilson ES, McKinlay S, Crawford JM, Robb HM. The influence of esmolol on the dose of propofol required for induction of anaesthesia. Anaesthesia. 2004;59:122–126. doi: 10.1111/j.1365-2044.2004.03460.x. [DOI] [PubMed] [Google Scholar]
- 158.Vuyk J. Pharmacokinetic and pharmacodynamic interactions between opioids and propofol. J Clin Anesth. 1997;9:23S–26S. doi: 10.1016/s0952-8180(97)00117-7. [DOI] [PubMed] [Google Scholar]
- 159.Perry S, Whelan E, Shay S, Wood A, Wppd M. Effect if I.V. anesthesia with propofol on drug distribution and metabolism in the dog. Br J Anaesth. 1991;66:66–72. doi: 10.1093/bja/66.1.66. [DOI] [PubMed] [Google Scholar]
- 160.Friedericy HJ, Bovill JG. The role of the cytochrome P450 system in drug interactions in anaesthesia. Baillieres Clin Anaesthesiol. 1998;12:213–228. [Google Scholar]
- 161.Vuyk J, Mertens MJ, Olofsen E, Burm AG, Bovill JG. Propofol anesthesia and rational opioid selection: determination of optimal EC50-EC95 propofol-opioid concentrations that assure adequate anesthesia and a rapid return of consciousness. Anesthesiology. 1997;87:1549–1562. doi: 10.1097/00000542-199712000-00033. [DOI] [PubMed] [Google Scholar]
- 162.Le Guellec C, Lacarelle B, Villard PH, Point H, Catalin J, Durand A. Glucuronidation of propofol in microsomal fractions from various tissues and species including humans: effect of different drugs. Anesth Analg. 1995;81:855–861. doi: 10.1097/00000539-199510000-00034. [DOI] [PubMed] [Google Scholar]
- 163.Berenbaum MC. What is synergy? Pharmacol Rev. 1989;41:93–141. [PubMed] [Google Scholar]
- 164.Minto CF, Schnider TW, Short TG, Gregg KM, Gentilini A, Shafer SL. Response surface model for anesthetic drug interactions. Anesthesiology. 2000;92:1603–1616. doi: 10.1097/00000542-200006000-00017. [DOI] [PubMed] [Google Scholar]
- 165.Short TG, Plummer JL, Chui PT. Hypnotic and anaesthetic interactions between midazolam, propofol and alfentanil. Br J Anaesth. 1992;69:162–167. doi: 10.1093/bja/69.2.162. [DOI] [PubMed] [Google Scholar]
- 166.Short TG, Chui PT. Propofol and midazolam act synergistically in combination. Br J Anaesth. 1991;67:539–545. doi: 10.1093/bja/67.5.539. [DOI] [PubMed] [Google Scholar]
- 167.Fidler M, Kern SE. Flexible interaction model for complex interactions of multiple anesthetics. Anesthesiology. 2006;105:286–296. doi: 10.1097/00000542-200608000-00011. [DOI] [PubMed] [Google Scholar]
- 168.Vinik HR, Bradley EL, Kissin I. Triple anesthetic combination: propofol-midazolam-alfentanil. Anesth Analg. 1994;78:354–358. doi: 10.1213/00000539-199402000-00026. [DOI] [PubMed] [Google Scholar]
- 169.Wilder-Smith OH, Ravussin P, Decosterd L, Despland P, Bissonnette B. Midazolam premedication reduces propofol dose requirements for multiple anesthetic endpoints. Can J Anaesth. 2001;48:439–445. doi: 10.1007/BF03028305. [DOI] [PubMed] [Google Scholar]
- 170.McClune S, McKay AC, Wright PM, Patterson CC, Clarke RS. Synergistic interaction between midazolam and propofol. Br J Anaesth. 1992;69:240–245. doi: 10.1093/bja/69.3.240. [DOI] [PubMed] [Google Scholar]
- 171.Lichtenbelt BJ, Olofsen E, Dahan A, van Kleef JW, Struys MMRF, Vuyk J. Propofol reduces the distribution and clearance of midazolam. Anesth Analg. 2010;110:1597–1606. doi: 10.1213/ANE.0b013e3181da91bb. [DOI] [PubMed] [Google Scholar]
- 172.Dutta S, Karol MD, Cohen T, Jones RM, Mant T. Effect of dexmedetomidine on propofol requirements in healthy subjects. J Pharm Sci. 2001;90:172–181. doi: 10.1002/1520-6017(200102)90:2<172::aid-jps8>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 173.Peden CJ, Cloote AH, Stratford N, Prys-Roberts C. The effect of intravenous dexmedetomidine premedication on the dose requirement of propofol to induce loss of consciousness in patients receiving alfentanil. Anaesthesia. 2001;56:408–413. doi: 10.1046/j.1365-2044.2001.01553.x. [DOI] [PubMed] [Google Scholar]
- 174.Jang Y-E, Kim Y-C, Yoon H-K, Jeon Y-T, Hwang J-W, Kim E, et al. A randomized controlled trial of the effect of preoperative dexmedetomidine on the half maximal effective concentration of propofol for successful i-gel insertion without muscle relaxants. J Anesth. 2015;29:338–345. doi: 10.1007/s00540-014-1949-9. [DOI] [PubMed] [Google Scholar]
- 175.Hammer GB, Sam WJ, Chen MI, Golianu B, Drover DR. Determination of the pharmacodynamic interaction of propofol and dexmedetomidine during esophagogastroduodenoscopy in children. Paediatr Anaesth. 2009;19:138–144. doi: 10.1111/j.1460-9592.2008.02823.x. [DOI] [PubMed] [Google Scholar]
- 176.Ngwenyama NE, Anderson J, Hoernschemeyer DG, Tobias JD. Effects of dexmedetomidine on propofol and remifentanil infusion rates during total intravenous anesthesia for spine surgery in adolescents. Paediatr Anaesth. 2008;18:1190–1195. doi: 10.1111/j.1460-9592.2008.02787.x. [DOI] [PubMed] [Google Scholar]
- 177.Ohtani N, Kida K, Shoji K, Yasui Y, Masaki E. Recovery profiles from dexmedetomidine as a general anesthetic adjuvant in patients undergoing lower abdominal surgery. Anesth Analg. 2008;107:1871–1874. doi: 10.1213/ane.0b013e3181887fcc. [DOI] [PubMed] [Google Scholar]
- 178.Coppens MJ, Versichelen LFM, Mortier EP. Struys MMRF. Do we need inhaled anaesthetics to blunt arousal, haemodynamic responses to intubation after i.v. induction with propofol, remifentanil, rocuronium? Br J Anaesth. 2006;97:835–841. doi: 10.1093/bja/ael254. [DOI] [PubMed] [Google Scholar]
- 179.Diz JC, Del Río R, Lamas A, Mendoza M, Durán M, Ferreira LM. Analysis of pharmacodynamic interaction of sevoflurane and propofol on Bispectral Index during general anaesthesia using a response surface model. Br J Anaesth. 2010;104:733–739. doi: 10.1093/bja/aeq081. [DOI] [PubMed] [Google Scholar]
- 180.Harris RS, Lazar O, Johansen JW, Sebel PS. Interaction of propofol and sevoflurane on loss of consciousness and movement to skin incision during general anesthesia. Anesthesiology. 2006;104:1170–1175. doi: 10.1097/00000542-200606000-00011. [DOI] [PubMed] [Google Scholar]
- 181.Schumacher PM, Dossche J, Mortier EP, Luginbuehl M, Bouillon TW, Struys MMRF. Response surface modeling of the interaction between propofol and sevoflurane. Anesthesiology. 2009;111:790–804. doi: 10.1097/ALN.0b013e3181b799ef. [DOI] [PubMed] [Google Scholar]
- 182.Sebel LE, Richardson JE, Singh SP, Bell SV, Jenkins A. Additive effects of sevoflurane and propofol on gamma-aminobutyric acid receptor function. Anesthesiology. 2006;104:1176–1183. doi: 10.1097/00000542-200606000-00012. [DOI] [PubMed] [Google Scholar]
- 183.Kazama T, Ikeda K, Morita K. Reduction by fentanyl of the Cp50 values of propofol and hemodynamic responses to various noxious stimuli. Anesthesiology. 1997;87:213–227. doi: 10.1097/00000542-199708000-00007. [DOI] [PubMed] [Google Scholar]
- 184.Smith Chris, McEwan Angus I., Jhaveri Rajiv, Wilkinson Michael, Goodman David, Smith L. Richard, Canada Andrew T., Glass Peter S. A. The Interaction of Fentanyl on the Cp50 of Propofol for Loss of Consciousness and Skin Incision. Anesthesiology. 1994;81(4):820–828. [PubMed] [Google Scholar]
- 185.Schraag S, Mohl U, Bothner U, Georgieff M. Interaction modeling of propofol and sufentanil on loss of consciousness. J Clin Anesth. 1999;11:391–396. doi: 10.1016/s0952-8180(99)00076-8. [DOI] [PubMed] [Google Scholar]
- 186.Hentgen E, Houfani M, Billard V, Capron F, Ropars J-M, Travagli JP. Propofol-sufentanil anesthesia for thyroid surgery: optimal concentrations for hemodynamic and electroencephalogram stability, and recovery features. Anesth Analg. 2002;95:597–605. doi: 10.1097/00000539-200209000-00019. [DOI] [PubMed] [Google Scholar]
- 187.Bouillon TW, Bruhn J, Radulescu L, Andresen C, Shafer TJ, Cohane C, et al. Pharmacodynamic interaction between propofol and remifentanil regarding hypnosis, tolerance of laryngoscopy, bispectral index, and electroencephalographic approximate entropy. Anesthesiology. 2004;100:1353–1372. doi: 10.1097/00000542-200406000-00006. [DOI] [PubMed] [Google Scholar]
- 188.Kern SE, Xie G, White JL, Egan TD. A response surface analysis of propofol-remifentanil pharmacodynamic interaction in volunteers. Anesthesiology. 2004;100:1373–1381. doi: 10.1097/00000542-200406000-00007. [DOI] [PubMed] [Google Scholar]
- 189.Kuizenga MH, Vereecke HEM, Struys MMRF. Model-based drug administration. Curr Opin Anaesthesiol. 2016;29:475–481. doi: 10.1097/ACO.0000000000000356. [DOI] [PubMed] [Google Scholar]
- 190.Saint-Maurice C, Cockshott ID, Douglas EJ, Ricjard MO, Harmey JL. Pharmacokinetics of propofol in young children after a single dose. Br J Anaesth. 1989;63:667–670. doi: 10.1093/bja/63.6.667. [DOI] [PubMed] [Google Scholar]
- 191.White M, Kenny GNC. Intravenous propofol anaesthesia using a computerised infusion system. Anaesthesia. 1990;45:204–209. doi: 10.1111/j.1365-2044.1990.tb14685.x. [DOI] [PubMed] [Google Scholar]
- 192.Cox EH, Knibbe CAJ, Koster VS, Langemeijer MWE, Tukker EE, Lange R, et al. Influence of different fat emulsion-based intravenous formulations on the pharmacokinetics and pharmacodynamics of propofol. Pharm Res. 1998;15:442–448. doi: 10.1023/a:1011980432646. [DOI] [PubMed] [Google Scholar]
- 193.Knibbe CAJ, Melenhorst-de Jong G, Mestrom M, Rademaker CMA, Reijnvaan AFA, Zuideveld KP, et al. Pharmacokinetics and effects of propofol 6% for short-term sedation in paediatric patients following cardiac surgery. Br J Clin Pharmacol. 2002;54:415–422. doi: 10.1046/j.1365-2125.2002.01652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Knibbe CA, Aarts LP, Kuks PF, Voortman HJ, Lie-A-Huen L, Bras LJ, et al. Pharmacokinetics and pharmacodynamics of propofol 6% SAZN versus propofol 1% SAZN and Diprivan-10 for short-term sedation following coronary artery bypass surgery. Eur J Clin Pharmacol. 2000;56:89–95. doi: 10.1007/s002280050726. [DOI] [PubMed] [Google Scholar]
- 195.Knibbe CAJ, Zuideveld KP, DeJongh J, Kuks PFM, Aarts LPHJ, Danhof M. Population pharmacokinetic and pharmacodynamic modeling of propofol for long-term sedation in critically ill patients: a comparison between propofol 6% and propofol 1% Clin Pharmacol Ther. 2002;72:670–684. doi: 10.1067/mcp.2002.129500. [DOI] [PubMed] [Google Scholar]
- 196.Servin F, Farinotti R, Haberer JP, Desmonts JM. Propofol infusion for maintenance of anesthesia in morbidly obese patients receiving nitrous oxide. A clinical and pharmacokinetic study. Anesthesiology. 1993;78:657–665. doi: 10.1097/00000542-199304000-00008. [DOI] [PubMed] [Google Scholar]