Abstract
Both childhood maltreatment and impulsivity have been implicated in a broad array of negative public health outcomes and have been much studied in relation to each other. Characterizing this relationship, and the processes underlying it, are important for informing intervention efforts targeting this association and its psychopathological sequelae. The current review presented a systematic meta-analysis of the empirical literature on childhood maltreatment and impulsivity. In all, 55 eligible studies were identified and included in this review. General support was found for a positive association between childhood maltreatment, including its specific subtypes, and general trait impulsivity, with pooled effect sizes ranging from small in the case of childhood sexual abuse (OR = 1.59 [95% CI = 1.38 – 1.84]) to medium-to-large in the case of childhood emotional abuse (OR = 3.10 [95% CI = 2.27 – 4.23]). Support for a relationship between childhood maltreatment and laboratory-based measures of impulsive behavior was generally lacking. The current findings must be interpreted with a degree of caution, given several methodological limitations characterizing much of the empirical literature. Recommendations for addressing these limitations and directions for future research are provided.
Keywords: child abuse, child maltreatment, impulsivity, meta-analysis, neglect
Introduction
Childhood maltreatment, a common form of adverse childhood experiences, consists of several types of abuse and neglect: physical abuse, sexual abuse, emotional abuse, and neglect (Cicchetti & Toth, 2005). This public health concern is quite prevalent. This is particularly true in the United States, where the elevated rate of violent deaths resulting from child abuse stands out as an outlier relative to the rates of this outcome in other high-income countries (Rao & Lux, 2012). Based on self-reported and parent-reported childhood maltreatment, lifetime prevalence rates for physical abuse have been estimated at 22.6% in a recent series of meta-analytical reviews (Stoltenborgh, Bakermans-Kranenburg, Alink, & van IJzendoorn, 2015). With sexual abuse, a marked sex difference is evident, with a lifetime prevalence rate of 7.6% among boys and 18.0% among girls. Although much less work has been conducted on childhood emotional abuse, available estimates place the lifetime prevalence rate for this form of abuse at 36.3%. Similarly the subject of comparative neglect in the empirical literature, childhood neglect is also notably prevalent, with lifetime prevalence rates of 16.3% for physical neglect and 18.4% for emotional neglect.
In addition to its high prevalence rate, childhood maltreatment has been associated with a host of negative public health outcomes, including subsequent engagement in violent behaviors (e.g., bullying, delinquency, intimate partner violence, and weapon-carrying; Duke, Pettingell, McMorris, & Borowsky, 2010), mood disorders (Etain, Henry, Bellivier, Mathieu, & Leboyer, 2008; Infurna et al., 2016), non-suicidal and suicidal self-injury (Dube et al., 2001; Liu, Scopelliti, Pittman, & Zamora, 2018; Maniglio, 2011), as well as substance use disorders (Gilbert et al., 2009; Teicher & Samson, 2013). Moreover, childhood maltreatment experiences appear to be related to an earlier age of onset of several of these clinical phenomena, a more severe course, and worse treatment response (Green et al., 2010; Hill, Pickles, Rollinson, Davies, & Byatt, 2004; Nanni, Uher, & Danese, 2011; Teicher & Samson, 2013; Williams et al., 2014). These deleterious effects of early maltreatment persist well into adulthood (Cicchetti & Toth, 2005; Gilbert et al., 2009). In addition to the toll of childhood maltreatment on social functioning and mental health, its economic burden is substantial, with early maltreatment experiences being associated with unemployment, poverty, and Medicaid usage, as well as lower educational attainment and earnings (Currie & Widom, 2010; Zielinski, 2009). Reflecting the long-term cost to productivity associated with childhood maltreatment, there is a 14% gap by middle age between maltreated individuals and non-maltreated counterparts in probability of employment (Currie & Widom, 2010). Moreover, the estimated lifetime cost is $210,012 per victim of non-fatal maltreatment, and the estimated total lifetime economic cost is $124 billion for all new cases of child maltreatment in a given year (Fang, Brown, Florence, & Mercy, 2012).
Given the magnitude of childhood maltreatment as a public health problem, there is a particular need for a greater understanding of the mediating pathways through which risk is conferred for these negative outcomes. More specifically, although the negative sequelae of childhood maltreatment are well established, the underlying processes of risk remain comparably unclear (Liu, 2017; McLaughlin, 2016). Elucidating these risk processes is of particular importance for their potential to advance our ability to intervene with victims of childhood maltreatment, and thereby to reduce the risk in these individuals for subsequent psychopathology and its attendant societal and economic costs.
One potential mechanism underlying the relation between childhood maltreatment and several mental health outcomes (e.g., suicidal behavior; Braquehais et al. 2010) is impulsivity. Although the research literature on childhood maltreatment and impulsivity, respectively, in relation to mental well-being has been previously subject to review, this has not been the case for the association between early maltreatment experiences and impulsivity. A critical analysis of the empirical literature characterizing this latter relationship is a necessary first step in determining the potential viability of impulsivity as a candidate mechanism through which childhood maltreatment experiences may confer risk for detrimental mental health and socioeconomic outcomes later in life. Thus, the principal objective of the current meta-analytic review is to quantify the strength of the association between overall childhood maltreatment, as well as its specific subtypes, and impulsivity in the empirical literature, with separate analyses conducted for distinct facets of this latter construct. Following this systematic review, a discussion will be provided of methodological considerations, conceptual gaps in the existing literature, along with specific recommendations for clarifying the precise nature of the relationship between maltreatment in childhood and impulsivity, the intention being to inform future study in this area.
Developmental perspectives on childhood maltreatment and impulsivity
Regarding how childhood maltreatment may lead to the development of impulsivity, several possibilities exist. Although it is not within the scope of this paper comprehensively to review all these possibilities, several mutually compatible accounts that merit particular mention include Gershoff’s (2002) process-context model and Vasta’s (1982) dual-component analysis of childhood physical abuse, life history theory, and neurobiological models.
First, an intriguing possibility is that a transactional relationship may exist, with maltreatment leading to increased risk for impulsivity, and impulsive dispositions and associated behavioral difficulties, in turn, taxing parental resources to manage these difficulties, resulting in an elevated likelihood of subsequent emotional and physical maltreatment, particularly when the parents themselves are prone to impulsivity. Furthermore, this likelihood is strengthened by the heritability of impulsivity, with impulsive parents being more likely to engage in undue parenting practices, including abusive behavior, when stressed by child misbehavior, and similarly impulsive offspring themselves being more likely to engage in this misbehavior. Indeed, this possibility is very much congruent with Gershoff’s (2002) process-context model and Vasta’s (1982) dual-component analysis of childhood physical abuse, according to which impulsivity in parental figures who engage in corporal punishment may lead to an escalation of this parenting practice toward abuse, and this may be particularly true when the parents are emotionally activated and confronted with negative internal (e.g., feelings of anger or stress) and external stimulation (e.g., child misbehavior). This possibility may also, in part, account for the often cyclical nature of child maltreatment, with parents who experienced maltreatment during their childhood at greater risk for perpetrating maltreatment with their own offspring (Egeland, Jacobvitz, & Sroufe, 1988).
Second, if childhood maltreatment does indeed confer risk for the development of impulsivity, a question that naturally follows is what accounts for this relationship. An intriguing potential account of this association between early maltreatment experiences and impulsivity may be found in life history theory (Belsky, Schlomer, & Ellis, 2012; Belsky, Steinberg, & Draper, 1991; Del Giudice, Ellis, & Shirtcliff, 2011; Ellis, Figueredo, Brumbach, & Schlomer, 2009). Couched within an evolutionary framework, this theory holds that organisms strategically allocate resources (i.e., time and energy) to different activities across their life cycle. As these resources are finite by nature, it is not possible maximally to devote them to all major life functions (i.e., somatic effort and reproductive effort), and some trade-off between these competing interests is therefore required. Life history strategies fall broadly within a spectrum from “slow” to “fast.” The former is characterized by a stable family environment in early childhood, later reproductive maturity and a preference for more long-term investments and goals, whereas the latter is a more high-risk approach, involving a more difficult rearing environment, earlier age of reproductive maturity and a prioritization of short-term goals in the face of long-term uncertainties.
Importantly, there is no single optimal life history strategy. Rather, it is dependent on the environmental context. Furthermore, phenotypic expression of these life history strategies seems to be both genetically and environmentally determined (Del Giudice et al., 2011). More specifically, and of particular relevance to the current review, extrinsic morbidity-mortality (i.e., external threats to the organism’s well-being) has been identified as a key factor calibrating the development of life history strategies towards the fast end of the spectrum. Indicators of high extrinsic morbidity-mortality include exposure to violence and harsh family environments among others. Harsh environmental contexts during early development have been found to predict an accelerated life history strategy (Belsky et al., 2012). Childhood maltreatment is certainly reflective of a harsh family environment, and thus may contribute toward a preference for a fast life history strategy. Notably consistent with this possibility, among the behavioral traits associated with a life history strategy on the fast end of the continuum are impulsivity and a preference for immediate over delayed rewards (i.e., impulsive choice; Del Giudice et al., 2011; Ellis & Del Giudice, 2014).
Third, adverse early life experiences have been suggested to disrupt normative neural development, particularly in prefrontal cortical regions governing response inhibition (Blair & Raver, 2016; Hart & Rubia, 2012; Pechtel & Pizzagalli, 2011). That is, early maltreatment experiences may lead to abnormal neural development, which in turn, may account for greater impulsive tendencies later in life. Aberrations in the anterior cingulate cortex (ACC), in particular, have been implicated in the neuropathology of childhood maltreatment (Teicher & Samson, 2016). Indeed, reduced myelination in the ACC appears to occur in individuals with a childhood abuse history (Lutz et al., 2017). This finding is of particular relevance here because the ACC is involved in regulating cognitive and motor responses during situations with conflict (Haber & Knutson, 2010), and the deleterious effects of childhood maltreatment on the ACC may be a neurobiological pathway through which early maltreatment experiences may be linked with impulsivity later in life (Lutz et al., 2017; Turecki, 2005). Reduced interior frontal gyrus volumes have also recently identified as another potential neurodevelopmental sequela of early adversities (Luby, Barch, Whalen, Tillman, & Belden, 2017). This is important to note, as the right inferior frontal gyrus has been engaged in performance on certain behavioral measures of impulsivity (i.e., impulsive choice; (Aron, Fletcher, Bullmore, Sahakian, & Robbins, 2003; Bari & Robbins, 2013). The importance of these findings lies, in part, in the possibility that these aberrations in neural development may function as a mediational pathway underlying the link between early adversities and negative health outcomes later in life (Luby et al., 2017).
If aberrant neural development is indeed a consequence of childhood maltreatment and leads to the development of impulsive tendencies, the timing of exposure to maltreatment experiences becomes particularly important and informative. That is, the brain regions most vulnerable to the deleterious effect of maltreatment are the ones undergoing rapid growth at the time of exposure (Pechtel & Pizzagalli, 2011; Teicher et al., 2003). In general, this would involve the hippocampus between birth and age two, the amygdala during early childhood, and the frontal cortex during adolescence (Lupien, McEwen, Gunnar, & Heim, 2009). It therefore stands to reason that aberrant frontal cortical development during adolescence, relative to other periods of development, would be most strongly implicated in the association between contemporaneously experienced maltreatment and impulsivity. As the current studies relating childhood maltreatment to impulsivity did not evaluate the timing of maltreatment exposure, it was not possible to evaluate this hypothesis. Therefore, including assessments of maltreatment experiences more sensitive to the age of occurrence is necessary for future research to provide a more nuanced understanding of this relation.
Methodological considerations
In addition to understanding the developmental context in which childhood maltreatment may relate to impulsivity, several important methodological considerations relating to the latter construct should be noted. Impulsivity has been increasingly recognized as a multidimensional construct, with important distinctions existing between different facets of this construct (Cyders & Coskunpinar, 2011; Hamilton, Littlefield, et al., 2015; Hamilton, Mitchell, et al., 2015; Whiteside & Lynam, 2001; Winstanley, Eagle, & Robbins, 2006). It has commonly been assessed using self-report trait measures and state-sensitive laboratory-based indices.1 In line with this conceptual distinction, trait and state-sensitive measures of impulsivity have been consistently observed to be only modestly correlated with each other (Cyders & Coskunpinar, 2011, 2012; Peters & Büchel, 2011; Reynolds, Penfold, & Patak, 2008).
The multidimensional nature of impulsivity is evident among self-report trait measures of this construct, the two most widely used being the Barratt Impulsiveness Scale (BIS; Patton et al. 1995) and the UPPS Impulsive Behavior Scale (as well as its subsequent elaboration, the UPPS-P; Cyders et al., 2007; Whiteside & Lynam, 2001). That is, in addition to a general index of impulsivity, the BIS was designed to assess three dimensions of this construct: (i) motor impulsivity, (ii) non-planning impulsivity, and (iii) attentional impulsivity. Similarly adopting a multidimensional conceptualization of impulsivity, the UPPS-P was developed to reflect five distinct facets of this construct: (i) negative urgency, or a tendency to act impulsively when experiencing negative affect, (ii) lack of premeditation, (iii) lack of perseverance, (iv) sensation-seeking, and (v) positive urgency, or a propensity to act impulsively under conditions of positive affect.
Even among task-based measures, important conceptual distinctions exist (Peters & Büchel, 2011; Robbins, Gillan, Smith, de Wit, & Ersche, 2012; Winstanley, Olausson, Taylor, & Jentsch, 2010). Specifically, in addition to being viewed as state-dependent indices (Cyders & Coskunpinar, 2011; Dougherty, Mathias, Marsh, Moeller, & Swann, 2004; Moeller, Barratt, Dougherty, Schmitz, & Swann, 2001), laboratory-based measures of impulsivity have been conceptualized as reflecting either (i) impulsive action (i.e., behavioral or motor impulsivity) or (ii) impulsive choice (i.e., cognitive impulsivity). Impulsive action is characterized by difficulty in preventing the initiation of a behavior or stopping an already-initiated behavior. Contrastingly, impulsive choice involves the tendency to prefer small immediate rewards over larger delayed ones (for a more thorough discussion of these laboratory-based approaches to measuring impulsivity, see Hamilton, Littlefield, et al., 2015; Hamilton, Mitchell, et al., 2015). Consistent with the view that behavior and cognitive impulsivity are distinct facets of impulsivity, measures of these constructs are modestly correlated with each other (Hamilton, Littlefield, et al., 2015; Lane, Cherek, Rhodes, Pietras, & Tcheremissine, 2003; Reynolds, Ortengren, Richards, & de Wit, 2006), and have been found across multiple studies to possess distinctly different underlying neural correlates (Hamilton, Littlefield, et al., 2015; van Gaalen, Brueggeman, Bronius, Schoffelmeer, & Vanderschuren, 2006; van Gaalen, van Koten, Schoffelmeer, & Vanderschuren, 2006; Whelan et al., 2012; Winstanley et al., 2006).
Given these conceptual distinctions between different facets of impulsivity along with the measures used to index them, several researchers have cautioned against generalizing findings regarding one facet of impulsivity to another, for failure to observe the distinction between them risks obscuring meaningful differences in their relationship with the construct of interest (Cyders & Coskunpinar, 2011; Hamza, Willoughby, & Heffer, 2015; Liu, Trout, Hernandez, Cheek, & Gerlus, 2017). Furthermore, it has been generally recommended that care be taken in the field to specify precisely the aspect of impulsivity assessed in relation to the construct under study (Cyders & Coskunpinar, 2011; Hamza et al., 2015). These distinctions between different facets of impulsivity were therefore observed in the present meta-analysis.
Method
Search strategy and eligibility criteria
A systematic search of the literature was conducted in PsycINFO and MEDLINE to identify studies of potential relevance to the current review. The following search string was applied: (“physical abuse” OR “sex abuse” OR “sexual abuse” OR “emotional abuse” OR “verbal abuse” OR “physical maltreatment” OR “sexual maltreatment” OR “emotional maltreatment” OR “verbal maltreatment” OR “psychological maltreatment” OR “psychological abuse” OR “child abuse” OR “childhood abuse” OR “child maltreatment” OR “childhood maltreatment”) AND (impulsiv* OR “response inhibition” OR “delay discounting” OR “delayed reward” OR “stop signal” OR “continuous performance” OR “attentional control” OR “behavioral control” OR “behavioural control” OR “go/no” OR “go no”). The search results were limited to: (i) English-language publications and (ii) peer-reviewed journal publications since inception to June 15, 2017. The search terms used in the current meta-analysis are based on a review of the search terms used in several prior systematic reviews of childhood maltreatment, which when combined yielded a more extensive set of search terms than in any single prior review, thereby ensuring a more thorough screening of potentially eligible studies. This same approach was adopted to arrive at a final and exhaustive set of search terms for impulsivity. This search strategy yielded a total of 1,062 articles, of which 726 were unique reports. In cases where the eligibility of an article could not be ruled out based on the title and abstract, the full text was also examined.
The study inclusion criteria were: (i) any form of childhood maltreatment was assessed, distinct from other constructs (e.g., adverse childhood experiences, childhood trauma); (ii) childhood maltreatment was analyzed separately from abuse experienced in adulthood; (iii) impulsivity was assessed separately from related constructs (e.g., risk-taking behaviors); and (iv) quantitative data were presented on the association between any form of childhood maltreatment and any aspect of impulsivity.
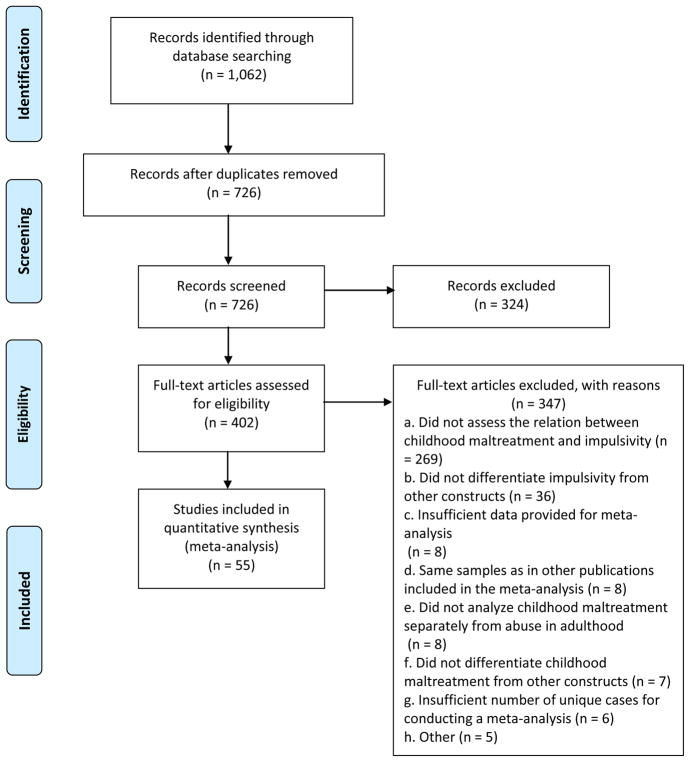
Based on these inclusion criteria, 324 reports were excluded based on their titles and abstracts. Following this initial screen, an additional 341 articles were excluded based on a detailed full-text review, leaving a set of 61 publications satisfying the eligibility criteria. Of these 61 publications, however, it was not possible to include six in the current review, with there being an insufficient number of relevant cases (i.e., fewer than four) for meta-analysis (e.g., cognitive impulsivity in the case of Rohrbeck & Twentyman, 1986), leaving a final set of 55 studies (see Figure 1 for PRISMA flow chart). Studies were excluded based on full-text review because they: (i) did not assess the relationship between childhood maltreatment and impulsivity (n = 269); (ii) did not differentiate impulsivity from other constructs (n = 36); (iii) provided insufficient data for meta-analysis (n = 8)2; (iv) featured a sample that overlapped with that of a study already selected for inclusion and examined the same form of impulsivity in relation to the same outcome of interest (n = 8);3 (v) did not analyze childhood maltreatment separately from abuse in adulthood (n = 8); (vi) did not differentiate childhood maltreatment from other constructs (n = 7); (vii) insufficient number of cases in the literature (i.e., < 3) of the analyses reported in the study for conducting a meta-analysis (n = 6); and (viii) were not quantitative studies (n = 5). Additionally, the titles of the references of all 55 eligible publications included in this meta-analysis were thoroughly reviewed for potential eligibility, with full-text review conducted where warranted. This search yielded no additional eligible studies.
Figure 1.
PRISMA flow chart of literature search
Data extraction
To assess potential moderators, data on seven study characteristics were extracted. These included four sample characteristics: (i) sample age group (i.e., child, adolescent, or adult); (ii) mean age of sample; (iii) sample clinical status (i.e., community versus clinical, at-risk, or mixed); and (iv) percentage of female participants in the study sample. Data for three study design characteristics were also extracted, including: (i) form(s) of childhood maltreatment assessed; (ii) form(s) of impulsivity assessed; and (iii) cross-sectional versus longitudinal analysis. For a subset of 25 of the 55 eligible studies, a second rater independently extracted data on the seven study characteristics. There was at most two discrepancies for any given variable (κs ranged from .65 to 1.). In the one instance where κ = .65 (i.e., age group of the sample), two studies were coded as having adolescent samples by one rater and one by the other. The low κ in this case was a function of the low number of adolescent samples included in this subset, rather than a high discrepancy between coders.
Data analysis
The odds ratio (OR) was used as the primary index of effect size. In cases where ORs were not reported, they were derived whenever possible from available data reported in the study (e.g., means and standard deviations, correlation). All ORs were calculated such that values greater than 1.0 are indicative of a positive association between childhood maltreatment and impulsivity (i.e., childhood maltreatment is associated with greater odds of impulsivity). Conversion of data into ORs and all analyses were conducted with Comprehensive Meta-Analysis Version 3.3.070 (Biostat, 2014). The overall weighted effect size was calculated by pooling ORs across all relevant studies. For all analyses, random-effects models were generated in preference to fixed-effects models, thereby accounting for the high expected heterogeneity across studies resulting from differences in samples, measures, and design. Heterogeneity across the studies was evaluated using the I2 statistic. I2 indicates the percentage of the variance in an effect estimate that is a product of heterogeneity across studies rather than sampling error (i.e., chance). Low heterogeneity is indicated by I2 values of around 25%, and moderate heterogeneity by I2 values of 50%. Substantial heterogeneity that is due to real differences in study samples and methodology is indicated by an I2 value of 75%, suggesting that the observed heterogeneity is more than would be expected with random error (Higgins, Thompson, Deeks, & Altman, 2003). In cases where high heterogeneity is observed, random-effects models are more appropriate than fixed-effects models, as the former accounts for this heterogeneity by incorporating both sampling and study-level errors, with the pooled effect size representing the mean of a distribution of true effect sizes instead of a single true effect size. In contrast, fixed-effects models assume that a single true effect size exists across all studies and any variance detected is due strictly to sampling error. It thus estimates only within-study variance.
High heterogeneity indicates the need for conducting moderator analyses to account for potential sources of this heterogeneity. Each potential moderator was first assessed separately, with an estimate of the effect size at each level of the moderator calculated.
A frequent concern in meta-analyses is the possibility of publication bias. Specifically, studies with small effect sizes or non-significant findings are less likely to be published, and consequently may be more likely to be excluded from meta-analyses, resulting in potential inflation of estimates of the overall effect size. To evaluate for potential publication bias, the following publication bias indices were calculated: Orwin’s fail-safe N (Orwin, 1983), Duval and Tweedie’s trim-and-fill analysis (Duval & Tweedie, 2000), and Egger’s regression intercept (Egger, Davey Smith, Schneider, & Minder, 1997). Orwin’s fail-safe N is an index of the robustness of an overall effect size, calculating the number of studies with an effect size of 0 that would be required to reduce the overall effect size in a meta-analysis to non-significance. Duval and Tweedie’s trim-and-fill analysis yields an estimate of the number of missing studies based on asymmetry in a funnel plot of the standard error of each study in a meta-analysis (based on the study’s sample size) against the study’s effect size. This analysis also produces an effect size estimate and confidence interval, adjusting for these missing studies. It should be noted that this procedure assumes homogeneity of effect sizes, and consequently, its results need to be interpreted with caution in cases where significant heterogeneity is present. Finally, Egger’s regression intercept estimates potential publication bias using a linear regression approach assessing study effect sizes relative to their standard error.
Results
Included in the present meta-analysis were 55 publications based on 51 unique samples and assessing the relation between at least one form of childhood maltreatment and at least one aspect of impulsivity. A summary of study details is provided in Table 1. As only one study included an assessment of cognitive impulsivity in relation to childhood maltreatment, it was not possible to include this form of impulsivity in the current meta-analysis. There was similarly an inadequate number of studies of positive urgency for meta-analysis. Finally, although several studies employed a longitudinal design, all analyses of childhood maltreatment in relation to impulsivity were cross-sectional. Therefore, this study design feature was not included in any moderator analyses.
Table 1.
Study characteristics
| Study Author(s) (year) | Na | % Femalea | Mean Agea | Sample | Maltreatment Measure(s) | Form(s) of Maltreatmentb | Impulsivity Measure(s) | Form(s) of Impulsivityb |
|---|---|---|---|---|---|---|---|---|
| Amr et al. (2016) | 58 | 27.0 | 30.3 | Clinical | TAA | CPA, CSA | BIS | Overall, Attention, Motor, NP |
| Arens et al. (2012)1 | 407 | 65.0 | 20.3 | Community | CATS | Overall | UPPS | NU, Persev, Premed, SS |
| Arens et al. (2014) | 600 | 73.0 | 19.6 | Community | CATS | Overall, CPA, CPN, CSA | UPPS | NU |
| Auerbach et al. (2014) | 194 | 74.2 | 15.5 | Clinical | CTQ | Overall | CPT | Behavioral Impulsivity |
| Augsburger et al. (2016) | 94 | 15.0 | 30.1 | At-risk | KERF | Overall | UPPS | NU, Persev, Premed, SS |
| Baltieri (2014) | 315 | 100 | 31.6 | At-risk | SSM | CSA | BIS | Overall |
| Barahmand et al. (2016) | 74 | 0.0 | 17.4 | Clinical | CTQ | Overall, CEA, CEN, CPA, CPN, CSA | BIS | Overall |
| Becker & Grilo (2006)2, c | 458 | 58.0 | 15.8 | Clinical | MACI | Overall | ICS | Overall |
| Becker & Grilo (2007) 2, d | 462 | 42.0 | 15.8 | Clinical | MACI | Overall | ICS | Overall |
| Becker-Blease & Freyd (2008)c | 29 | 48.3 | 9.27 | At-risk | BBTS | Overall | SNAP-IV | Overall |
| Berman & Knight (2015) | 175 | 0.0 | 16.0 | At-risk | MASA | CSA | SSM | Overall |
| Bornovalova et al. (2006) | 93 | 44.0 | 41.5 | Clinical | CTQ | CEA, CEN, CPA, CPN, CSA | MPQ-BF | Overall |
| Bornovalova et al. (2008) | 96 | 48.0 | 14.9 | Community | CTQ | Overall | EIS | Overall |
| Brodsky et al. (2008) | 236 | 85.0 | 45.0 | Clinical | CARE, CDTHI, CEQ | CPA, CSA | BIS | Overall |
| Brown et al. (2017) | 500 | 50.4 | 18.9 | Community | CTQ | CEA, CEN, CPA, CPN, CSA | BIS | Overall |
| Bücker et al. (2012) | 60 | 45.0 | 8.67 | Mixed | SSM, SSR | Overall | CPT | Behavioral Impulsivity |
| Carli et al. (2014) | 1315 | 0.0 | 39.6 | At-risk | CTQ | Overall, CEA, CEN, CPA, CPN, CSA | BIS | Overall |
| Conley & Garza (2011) | 147 | 80.2 | 26.3 | At-risk | SAEQ | CSA | BIS | Overall |
| Daray et al. (2016) | 177 | 100 | 37.6 | Clinical | SSM | CSA | BIS | Overall, Attention, Motor, NP |
| Day et al. (2013)3 | 112 | 39.2 | 16.8 | At-risk | CTQ | CEA, CPA | BIS | Overall |
| De Bellis et al. (2013) | 202 | 56.9 | 12.1 | Mixed | SSM, SSR | Overall | CPT | Behavioral Impulsivity |
| Dworkin et al. (2014) | 649 | 66.6 | NR | Community | SSM | CSA | BIS | Overall |
| Evren et al. (2013) | 200 | 0.0 | 35.3 | Clinical | CTQ | Overall | BIS | Overall |
| Fanning et al. (2014) | 648 | 42.4 | 34.0 | Community | CTQ | CEA, CEN, CPA, CPN, CSA | BIS | Overall |
| Gagnon et al. (2013) | 122 | 65.5 | 23.0 | Community | CTQ | Overall | UPPS | NU, Persev, Premed, SS |
| Gaher et al. (2015)1 | 407 | 65.0 | 20.3 | Community | CATS | CPA, CPN, CSA | UPPS | NU |
| Gowin et al. (2013) | 67 | NR | 31.5 | At-risk | CTQ | Overall | BIS | Overall |
| Gratz et al. (2011) | 225 | 45.0 | 12.1 | Community | CTQ | CEA | EIS | Overall |
| Hahn et al. (2016) | 425 | 71.0 | 19.2 | Community | CATS | Overall | UPPS | NU |
| Hjorth & Ostrov (1982) | 49 | 50.0 | 13.7 | Mixed | SSM, SSR | CPA | OSIQ | Overall |
| Jakubczyk et al. (2013)4 | 304 | 26.0 | 43.5 | Clinical | SSM | CPA, CSA | BIS | Attention, Motor, NP |
| Jakubczyk et al. (2016)4 | 358 | 26.5 | 43.7 | Clinical | SSM | CPA, CSA | BISg | Overall |
| Lee & Park (2016) | 35 | 85.7 | 37.5 | Clinical | CTQ | Overall, CEA, CEN | BIS | Overall |
| Li et al. (2012) | 450 | 55.1 | 33.9 | Clinical | ETISR-SF | Overall | BIS | Overall |
| Lim et al. (2015) | 66 | 33.0 | 17.2 | Mixed | CECA, CTQ, SSR | Overall | SST | Behavioral Impulsivity |
| Liu et al. (2012) | 206 | 0.0 | NR | At-risk | CTQ | Overall | BIS | Overall |
| Lopez-Castroman et al. (2014) | 696 | 71.7 | 39.4 | Clinical | CTQ | Overall, CEA, CEN, CPA, CPN, CSA | BIS | Overall |
| Martins et al. (2014)e | 81 | 72.8 | 37.6 | Clinical | CTQ | Overall, CEA, CEN, CPN | BIS | Overall |
| Minzenberg et al. (2006) | 40 | 88.4 | 35.1 | Clinical | CTQ | CEA, CEN, CPA, CPN, CSA | BIS | Attention, Motor, NP |
| Mirhashem et al. (2017) | 84 | 46.4 | 35.2 | Clinical | CTQ | CPA, CPN, CSA | UPPS-P | NU |
| Narvaez et al. (2012) | 56 | 8.0 | 29.3 | Clinical | CTQ | Overall, CEA, CEN, CPA, CPN, CSA | BIS | Overall |
| Roy (2005) | 268 | 2.2 | 41.3 | Clinical | CTQ | Overall, CEA, CPA, CPN | BIS | Overall |
| Rylands et al. (2012) | 27 | 0.0 | 34.0 | Community | CTQ | Overall | BIS | Overall |
| Schafer et al. (2004)d, f | 1427 | 50.0 | 43.5 | Community | SSM | CPA | SSM | Overall |
| Sergentanis et al. (2014) | 154 | 0.0 | 41.9 | At-risk | SSM | Overall | BIS | Overall |
| Shin et al. (2016) | 333 | 52.5 | 21.7 | Community | CTQ | CPA, CSA | UPPS | NU |
| Somer et al. (2012) | 96 | 41.0 | 34.1 | Clinical | CTQ | Overall, CEA, CEN, CPA, CPN, CSA | BIS | Overall |
| Stetler et al. (2014) | 89 | 0.0 | 31.8 | At.risk | CTQ | Overall, CEA, CEN, CPA, CPN, CSA | BIS | Overall, Attention, Motor, NP |
| Stoltenberg et al. (2012)c | 439 | 64.7 | 22.4 | Community | TAQ | CPA, CSA | BIS | Overall, Attention, |
| Thibodeau et al. (2015) | 1012 | 49.4 | 10.0 | At-risk | SSM, SSR | Overall | CCQ | Motor, NP Overall |
| Thompson & Morrison (2013) | 571 | 0.0 | 18.5 | Community | SSM | CSA | IQ | Overall |
| Veith et al. (2017) | 517 | 67.1 | NR | Community | LONGSCAN sexual abuse/assault measure, VEQ-R | Overall, CPA, CSA | BIS | Attention, Motor, NP |
| Wanklyn et al. (2012)3 | 110 | 39.0 | 16.7 | At-risk | CTQ | Overall, CEN, CPA, CSA | BIS | Overall |
| Wardell et al. (2016) | 232 | 52.5 | 19.7 | Community | CTQ | Overall | UPPS-P | NU, Persev, Premed, SS |
| Wota et al. (2014) | 186 | 48.5 | 45.0 | Clinical | CTQ | Overall, CEA, CEN, CPA, CPN, CSA | BIS | Overall, Attention, Motor, NP |
Note: BBFS = Brief Betrayal Trauma Scale; BIS = Barratt Impulsiveness Scale; CARE = Childhood and Adolescence Review of Experiences; CATS = Child Abuse and Trauma Scale; CCQ = California Child Q-Set; CDTHI = Columbia Demographic and Treatment History Interview; CECA = Childhood Experience of Care and Abuse; CEQ = Childhood Experiences Questionnaire; CPT = Continuous Performance Task; CTQ = Childhood Trauma Questionnaire; EIS = Eysenck Impulsivity Scale; ETISR-SF = Early Trauma Inventory Self Report-Short Form; ICS = Impulsivity Control Scale; IQ = Impulsivity Questionnaire; KERF = Maltreatment and Abuse Chronology of Exposure Scale (German version); LONGSCAN = Longitudinal Studies on Child Abuse and Neglect; MACI = Millon Adolescent Clinical Inventory; MASA = Multidimensional Assessment of Sex and Aggression; MPQ-BF = Multidimensional Personality Questionnaire – Brief Form; NR = not reported; OSIQ = Offer Self-Image Questionnaire; SAEQ = Sexual Abuse Exposure Questionnaire; SNAP-IV = Swanson, Nolan, and Pelham Rating Scale; SSM = study-specific measure; SSR = social service records; SST = Stop-Signal Task; TAA = Trauma Assessment for Adults Brief Revised Version; TAQ = Traumatic Antecedent Questionnaire; UPPS/UPPS-P = UPPS/UPPS-P Impulsive Behavior Scale; VEQ-R = Violent Experiences Questionnaire Revised
CEA = childhood emotional abuse; CEN = childhood emotional neglect; CPA = childhood physical abuse; CPN = childhood physical neglect; CSA = childhood sexual abuse NP = non-planning; NU = negative urgency; Persev = Perseverance; Premed = premeditation; SS = sensation-seeking
Studies with identical superscripts were drawn from same or overlapping samples.
The sample size, mean age, and percentage female for participants included in relevant analyses, rather than of the entire study sample, are presented and were incorporated in moderator analyses whenever available. For ease of presentation, whenever the sample size varied across multiple relevant analyses within a study, the largest sample size across these analyses is presented here, and the sample size used in each analysis was retained in the relevant meta-analysis for purposes of obtaining weighted effect sizes.
Several studies included analyses of multiple maltreatment and impulsivity subtypes, for some of which there was an insufficient number of cases in the literature for meta-analysis. For ease of presentation, only the maltreatment and impulsivity subtypes submitted to meta-analysis are presented here.
Separate effects were reported by sex. In cases where the proportion female and/or mean age are not available for relevant analyses, the corresponding values for the overall sample are presented here. Similarly, in cases where separate analyses were conducted by sex, the proportion of the overall sample that was female is presented here.
Three separate effects were reported by race/ethnicity.
Separate analyses were conducted with overall childhood maltreatment as continuous and categorical variables. The effect for maltreatment as a continuous variable was included in the meta-analysis.
Although this study conducted separate analyses by sex, due to non-independence, it was not possible to observe this distinction in the meta-analysis.
This study also assessed childhood sexual abuse in relation to performance on the stop-signal task. As there were not enough studies evaluating this association to conduct a meta-analysis, it was not included in the current review.
Trait impulsivity
General impulsivity
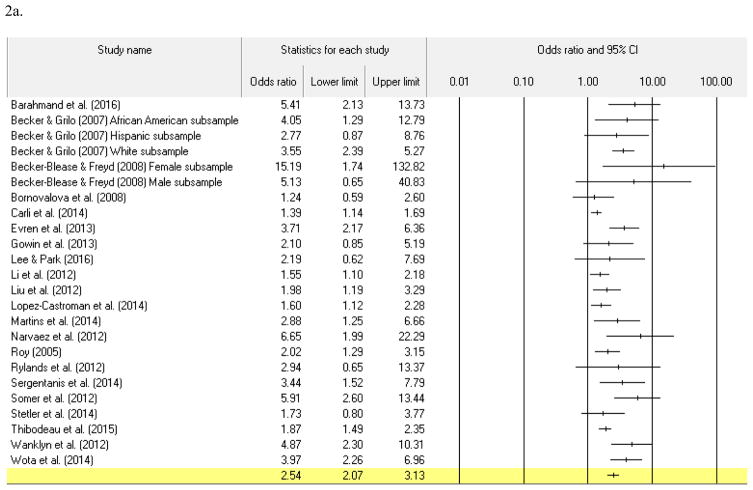
Across 21 studies with 24 unique effects,4 overall childhood maltreatment was positively associated with general trait impulsivity (see Table 2). Heterogeneity was moderately high, indicating the appropriateness of moderator analyses. Age was not a significant moderator of the strength of the association between overall maltreatment and trait impulsivity, regardless of whether age was treated categorically with comparisons made between children, adolescents, and adults (p = .37) or with children and adolescents combined in these comparisons (p = .26). Consistent with these results, age remained a non-significant moderator when analyzed as a continuous variable (b = −.01, p = .41). Similarly, the percentage of female participants in each study was not a significant moderator (b < .01. p = .76). Although only two studies were conducted with community samples, and this low number of effects may yield unstable estimates of effect sizes, exploratory analyses revealed a trend (p = .06) toward larger effects in clinical samples (OR = 2.93 [95% CI = 2.20 – 3.90], p < .001) than in ones drawn from the community (OR = 1.47 [95% CI = 0.76 – 2.86], p = .26). At-risk samples did not differ from community ones in terms of the strength of association between overall childhood maltreatment and general trait impulsivity (p = .30).
Table 2.
Meta-analytic results for childhood maltreatment in relation to general trait impulsivity.
| Effect Size Analyses | Heterogeneity Analyses | Publication Bias Analyses | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| k | OR | 95% CI | p | I2 | p | Orwin’ s fail-safe N | Egger’s regression test p | Trim-and-fill | ||
| OR | 95% CI | |||||||||
| Overall Maltreatment | 24 | 2.54 | 2.07 – 3.13 | <.001 | 65.54% | <.001 | 212 | <.001 | 2.16 | 1.76 – 2.64 |
| Sexual Abuse | 21 | 1.59 | 1.38 – 1.84 | <.001 | 49.00% | <.01 | 82 | .57 | 1.54 | 1.33 – 1.78 |
| Physical Abuse | 21 | 2.05 | 1.72 – 2.44 | <.001 | 65.43% | <.001 | 138 | <.01 | 1.79 | 1.50 – 2.13 |
| Physical Neglect | 13 | 2.08 | 1.71 – 2.54 | <.001 | 53.04% | .01 | 88 | .09 | 1.66 | 1.34 – 2.07 |
| Emotional Abuse | 15 | 3.10 | 2.27 – 4.23 | <.001 | 82.63% | <.001 | 163 | <.01 | 2.59 | 1.95 – 3.43 |
| Emotional Neglect | 13 | 2.17 | 1.58 – 2.99 | <.001 | 81.05% | <.001 | 93 | .04 | 1.98 | 1.46 – 2.69 |
Note: k = number of unique effects; OR = pooled odds ratio; CI = confidence interval
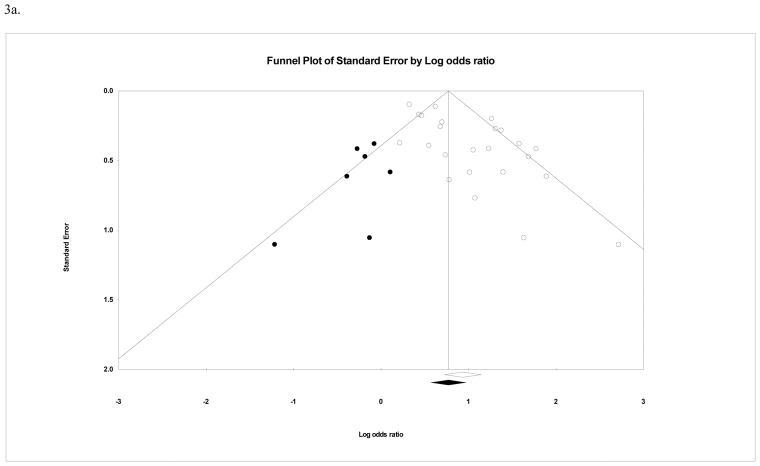
In terms of potential publication bias, Orwin’s fail-safe-N indicated that 212 unpublished studies with an OR of 1.0 would be required to reduce the pooled effect size for the relation between overall maltreatment and general trait impulsivity to 1.1 (an a priori trivial effect size), suggesting that the observed weighted effect size is robust. Egger’s regression test, however, indicated that significant publication bias was present (intercept = 1.97, [95% CI = .99 – 2.95], t(22) = 4.17, p < .001). Additionally, the funnel plot of effect sizes was notably asymmetrical (see Figure 2a). When the trim-and-fill method was used to correct parameter estimates for potential publication bias, the adjusted weighted OR was reduced to 2.16 (95% CI = 1.76 – 2.64).
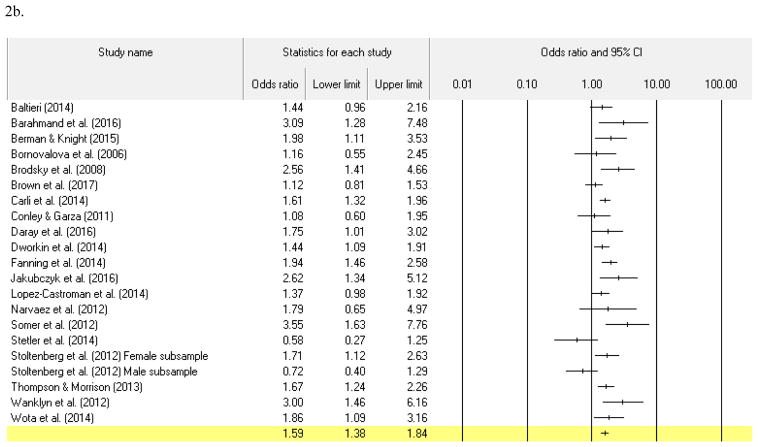
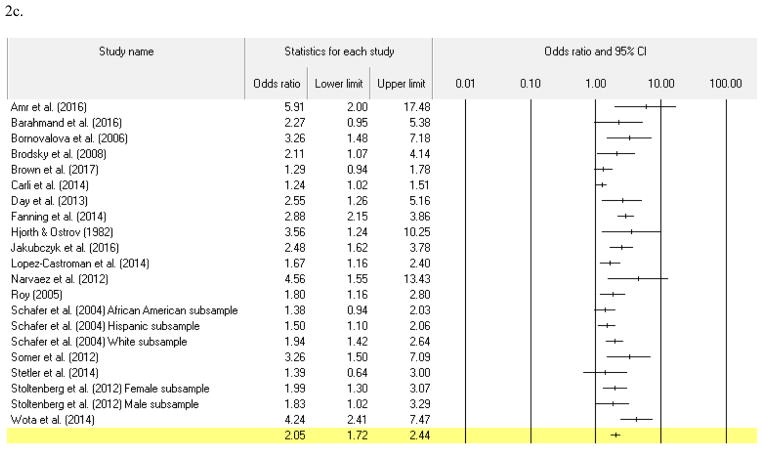
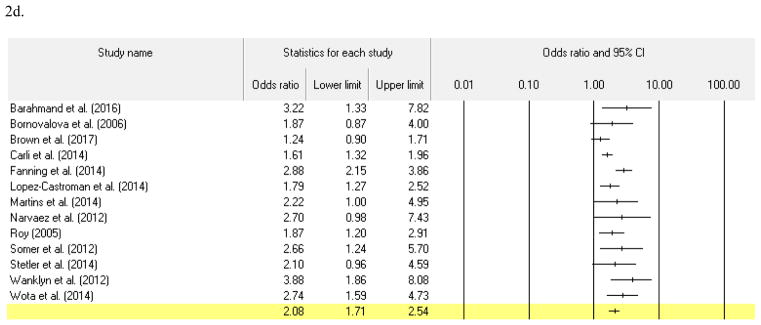
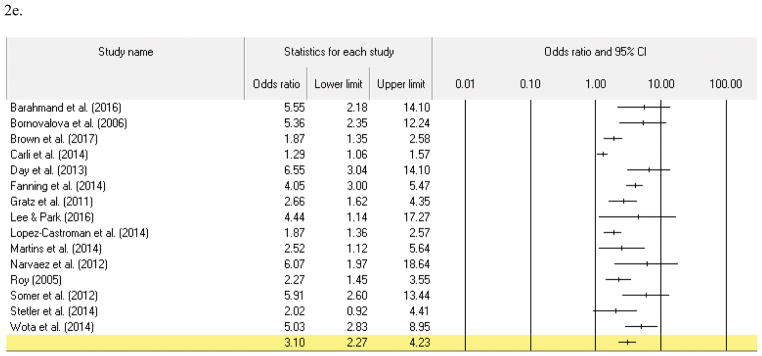
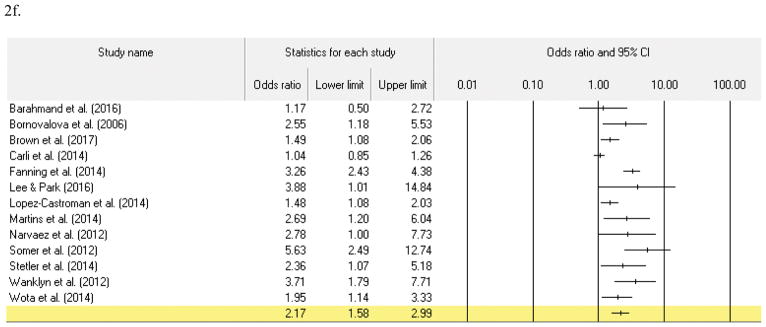
Figure 2. Forest plots for childhood maltreatment in relation to general trait impulsivity.
2a. Overall childhood maltreatment and general trait impulsivity
2b. Childhood sexual abuse and general trait impulsivity
2c. Childhood physical abuse and general trait impulsivity
2d. Childhood physical neglect and general trait impulsivity
2e. Childhood emotional abuse and general trait impulsivity
2f. Childhood emotional neglect and general trait impulsivity
When general trait impulsivity was examined in relation to specific forms of childhood maltreatment, significant associations were found for all maltreatment subtypes, with pooled OR’s ranging from 1.59 (95% CI = 1.38 – 1.84) for childhood sexual abuse to 3.10 (95% CI = 2.27 – 4.23) for childhood emotional abuse. Heterogeneity was significant and ranged from 49.00% (moderate) to 82.63% (high) across these analyses. A summary of these results is presented in Table 2. In moderator analyses, age treated as a categorical variable moderated the association between childhood sexual abuse and general trait impulsivity (p = .03),5 with a larger pooled effect observed for adolescent samples (OR = 2.47, [95% CI = 1.65 – 3.69], p < .001) than in adults (OR = 1.52, [95% CI = 1.32 – 1.76], p < .001). When treated as a continuous variable, however, age no longer moderated the strength of the relationship between childhood sexual abuse and general trait impulsivity (b < .01, p = .52). For the remaining maltreatment subtypes, age did not function as a significant moderator when considered as a categorical or continuous variable (childhood physical abuse: pCategorical = .30, bContinuous < .01, p = .76; childhood physical neglect: bContinuous < .01, p = .99; childhood emotional abuse: pCategorical = .28, bContiunous < .01, p = .69; childhood emotional neglect: bContinuous < .01, p = .99).6 Sex also was not found to moderate the association between maltreatment subtypes and general trait impulsivity (childhood sexual abuse: b < .01, p =.84; childhood physical abuse: b < .01, p = .64; childhood physical neglect: b < .01, p = .99; childhood emotional abuse: b < .01, p = .67; childhood emotional neglect: b < .01, p = .34). Sample type moderated the strength of association with general trait impulsivity in the case of childhood physical abuse (p = .04), for which a larger effect size was observed for clinical samples (OR = 2.56 [95% CI = 1.98 – 3.29], p < .001) than for community ones (OR = 1.78 [95% CI = 1.41 – 2.24], p < .001). Sample type did not moderate the observed associations for any of the remaining maltreatment subtypes (childhood sexual abuse p = .09; childhood emotional abuse p = .60).7
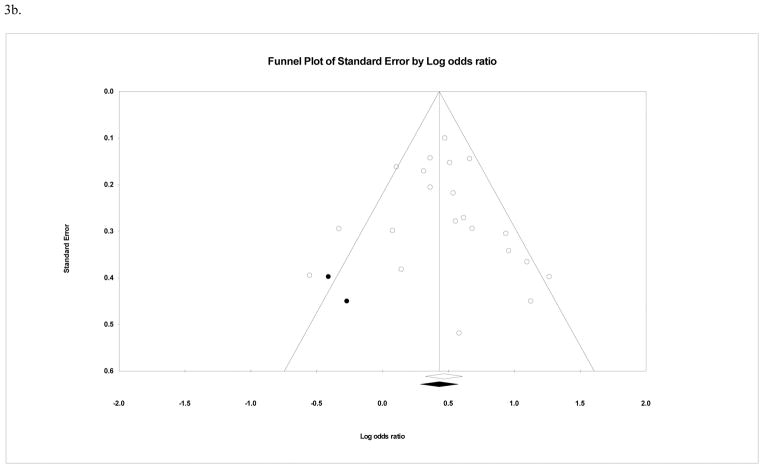
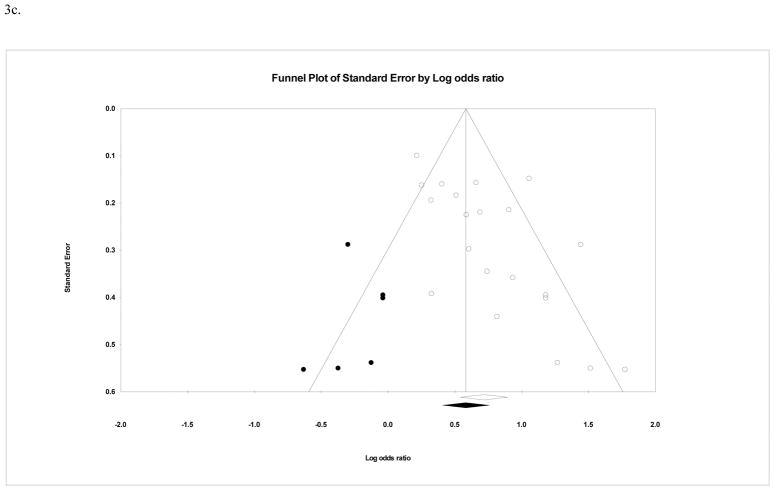
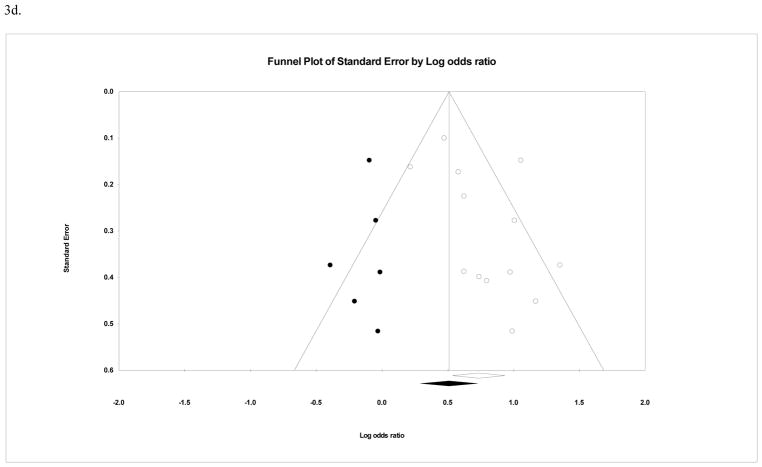
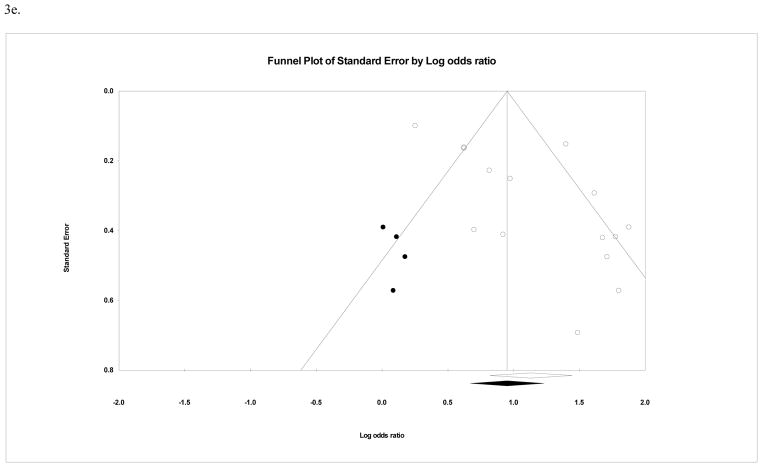
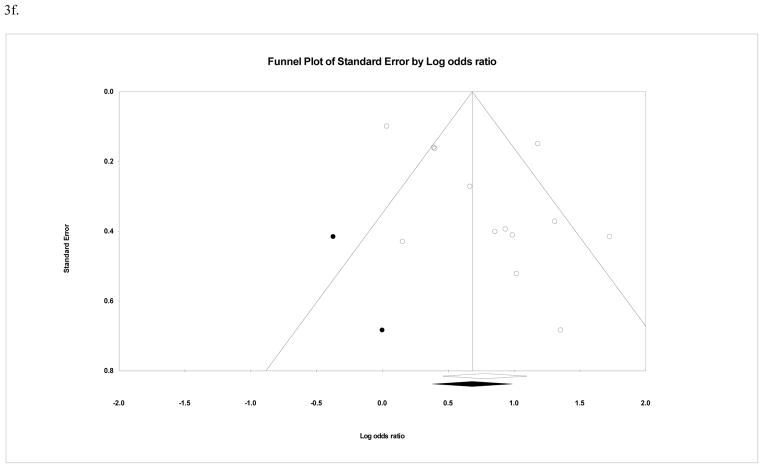
Regarding potential publication bias for studies of maltreatment subtypes, fail-safe n’s ranged from 82 to 212. Egger’s regression test indicated significant publication bias in the case of childhood physical abuse, childhood emotional abuse, and childhood emotional neglect. In general, funnel plots of the effect sizes for maltreatment subtypes were fairly asymmetrical, suggesting the presence of publication bias (see Figures 2b to 2f). Although the trim-and-fill method produced a reduction in estimated effect sizes, significant effects remained for all maltreatment subtypes, with OR’s ranging from 1.54 (95% CI = 1.33 – 1.78) in the case of childhood sexual abuse to 2.59 (95% CI = 1.95 – 3.43) in the case of childhood emotional abuse. These results are summarized in Table 2.
BIS subscales
Comparably fewer studies examined childhood maltreatment in relation to specific subtypes of impulsivity as reflected by the BIS subscales. Apart from childhood physical and emotional neglect, all forms of childhood maltreatment were found to be positively associated with all three BIS subscales, with pooled OR’s ranging from 1.46 (95% CI = 1.03 – 2.07) in the case of childhood sexual abuse and motor impulsivity to 2.72 (85% CI = 1.55 – 4.76) in the case of childhood emotional abuse and motor impulsivity. The one other exception that should be noted is the marginal effect observed between childhood emotional abuse and non-planning impulsivity (OR = 1.90 [95% CI = .99 – 3.63], p = .05). These findings are presented in Table 3.
Table 3.
Meta-analytic results for childhood maltreatment in relation to the Barratt Impulsiveness Scale subscales.
| k | Attentional Impulsivity | Motor Impulsivity | Non-Planning Impulsivity | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | ||
| Overall Maltreatment | 3 | 2.42 | 1.85– 3.17 | <.001 | 2.16 | 1.42 – 3.28 | <.001 | 1.82 | 1.40 – 2.37 | <.001 |
| Sexual Abuse | 8 | 1.50 | 1.07 – 2.10 | .02 | 1.46 | 1.03 – 2.07 | .03 | 1.46 | 1.11 – 1.92 | <.01 |
| Physical Abuse | 8 | 1.99 | 1.41 – 2.83 | <.001 | 2.09 | 1.64 – 2.68 | <.001 | 1.72 | 1.39 – 2.12 | <.001 |
| Physical Neglect | 3 | 1.57 | .80 – 3.06 | .19 | 1.65 | .88 – 3.09 | .12 | 1.50 | .59 – 3.83 | .40 |
| Emotional Abuse | 3 | 2.30 | 1.52 – 3.50 | <.001 | 2.72 | 1.55–4.76 | <.001 | 1.90 | .99 – 3.64 | .05 |
| Emotional Neglect | 3 | 1.87 | .93 – 3.77 | .08 | 1.43 | .95 – 2.15 | .09 | 1.43 | .90 – 2.25 | .13 |
Note: k = number of unique effects; OR = pooled odds ratio; CI = confidence interval
UPPS subscales
Even fewer studies were available for childhood maltreatment in relation to impulsivity as assessed with the UPPS. As shown in Table 4, overall childhood maltreatment was associated with perseverance and negative urgency, but not premeditation or sensation-seeking. Furthermore, the strength of association appeared to be strongest for negative urgency. With only three exceptions, there were too few unique effects for meta-analysis of the association between maltreatment subtypes and the UPPS subscales. In these three cases, negative urgency was positively associated with childhood sexual abuse (OR = 1.60 [95% CI = 1.20 – 2.14], p < .01), childhood physical abuse (OR = 1.98 [95% CI = 1.63 – 2.40], p < .001), and childhood physical neglect (OR = 2.44 [95% CI = 1.39 – 4.30], p < .01).
Table 4.
Meta-analytic results for overall childhood maltreatment in relation to the UPPS subscales.
| k | OR | 95% CI | p | |
|---|---|---|---|---|
| Lack of Premeditation | 4 | 1.40 | .90 – 2.18 | .14 |
| Lack of Perseverance | 4 | 2.08 | 1.62 – 2.68 | <.001 |
| Sensation-Seeking | 4 | 1.06 | .83 – 1.35 | .65 |
| Negative Urgency | 6 | 3.20 | 2.69 – 3.80 | <.001 |
Note: k = number of unique effects; OR = pooled odds ratio; CI = confidence interval
State-sensitive indices of impulsivity: Behavioral impulsivity
Relatively few studies have examined task-based measures of impulsivity in relation to childhood maltreatment. Indeed, a sufficient number of unique effects was available only for overall childhood maltreatment in association with behavioral impulsivity (k = 4). The pooled effect was not significant (OR = 1.07 [95% CI = .52 – 2.18], p = .86).
Discussion
The objective of the current review was to quantify the magnitude of the association between childhood maltreatment and impulsivity in the empirical literature. In the case of general trait impulsivity, there was consistent support for this association, with weighted effect sizes ranging from small to medium-to-large across all forms of maltreatment. Regarding specific facets of impulsivity, a consistent pattern was observed among BIS subscales, with all three facets of impulsivity being specifically associated with childhood abuse (small to medium pooled effects) but not with childhood neglect. The association with impulsivity generally appeared strongest for childhood emotional abuse and weakest for childhood sexual abuse. Indeed, this difference in effect size was significant for general trait impulsivity, with the 95% confidence intervals for childhood emotional and sexual abuse not overlapping. As for the UPPS, the empirical literature is considerably more limited, and consequently there was an insufficient number of studies for meta-analysis with certain maltreatment subtypes (i.e., k ≤ 3). Here, greatest empirical interest has been devoted to negative urgency. Paralleling this trend, the association between overall childhood maltreatment and this facet of impulsivity was significantly stronger than in the case of all other UPPS subscales. Even rarer still are investigations of state-sensitive laboratory-based measure of impulsivity, with meta-analysis currently only possible for behavioral impulsivity. Across the four studies in this area, overall childhood maltreatment was not significantly associated with this form of impulsivity.
Of these findings, that childhood emotional abuse appeared most strongly associated with impulsivity, especially relative to childhood sexual abuse, was perhaps among the most interesting. Why impulsivity appears to have a preferential association with childhood emotional abuse is unclear and a subject for future investigation. One possible explanation may lie in the fact that childhood emotional abuse is the most prevalent form of abuse (Stoltenborgh et al., 2015). It stands to reason that this higher prevalence may in part be a reflection of it also being the most chronic abuse subtype (Glaser, 2002; Stoltenborgh et al., 2015). That is, although both childhood physical and sexual abuse can occur as either isolated incidents or recurrent events, childhood emotional abuse is an inherently chronic phenomenon (Stoltenborgh, Bakermans-Kranenburg, Alink, & IJzendoorn, 2012), and perhaps its greater association with impulsivity is in part a reflection of the impact of this greater chronicity.
The connection in the current review between childhood maltreatment and impulsivity may inform theoretical formulations of the etiology of various forms of psychopathology that have either been theoretically or empirically associated with childhood maltreatment and impulsivity, respectively, including attention deficit/hyperactivity disorder, bipolar disorder, bulimia, substance use disorders, and suicide (Alloy & Abramson, 2010; Bickel, Koffarnus, Moody, & Wilson, 2014; Costello et al., 2002; Fischer, Smith, & Cyders, 2008; Mann et al., 2005; Post & Leverich, 2006; Van Orden et al., 2010; Wenzel & Beck, 2008; Winstanley et al., 2006; Wright, Lipszyc, Dupuis, Thayapararajah, & Schachar, 2014). As just one example, within the interpersonal theory of suicide (Van Orden et al., 2010), both childhood maltreatment and impulsivity are implicated in the etiology of suicidal behavior, but as distinct mechanisms of risk. Specifically, childhood maltreatment and impulsivity are individually associated with risk for this outcome through heightened acquired capability for suicide. Based on the current findings, it may be possible that rather than being separate risk processes, these childhood maltreatment and impulsivity may interrelate in accounting for suicide risk, with the latter mediating the effects of early maltreatment on acquired capability for suicide, and thereby, indirectly, elevated risk for suicidal behavior.
It should also be noted, however, that interpretation of the findings of the current review is constrained by several important methodological limitations prevalent across the existing literature. First, only zero-order effects (i.e., bivariate associations) were included in this meta-analysis, for only four studies, based on three samples, also featured multivariate analyses of childhood maltreatment relative to impulsivity (Jakubczyk et al., 2013, 2016; Lopez-Castroman et al., 2014; Sergentanis et al., 2014). Across these four studies, there was considerable heterogeneity in other variables included in the analyses. Nonetheless, reductions in effect size for overall childhood maltreatment (Sergentanis et al., 2014) and toward non-significance for specific maltreatment subtypes (Jakubczyk et al., 2013; Lopez-Castroman et al., 2014) were observed. Given the paucity of studies in this area and the inconsistency across studies in maltreatment subtypes reduced to non-significant associations with impulsivity, these findings must be regarded as tentative and require replication in future research.
More importantly, just two of the studies included in this review (Jakubczyk et al., 2013, 2016) covaried different forms of childhood maltreatment in evaluating individual maltreatment subtypes in relation to impulsivity. Even in these two cases, only two forms of maltreatment (i.e., physical and sexual abuse) were considered, with the form of childhood abuse most strongly associated with impulsivity in this review (i.e., emotional abuse) absent from consideration. The importance of these observations lies in the fact that maltreatment subtypes have been found frequently to co-occur (Finkelhor, Ormrod, & Turner, 2007; Higgins & McCabe, 2000; Teicher, Samson, Polcari, & McGreenery, 2006), with co-occurrence of subtypes ranging from 35% in large community samples (Edwards, Holden, Felitti, & Anda, 2003) to 90% or higher in more severe samples (Ney, Fung, & Wickett, 1994). Thus, it is uncertain to what degree the estimated effect sizes for maltreatment subtypes in the current meta-analysis reflect unique effects rather than, in part, a function of this high co-occurrence between different forms of maltreatment. Furthermore, although emotional abuse frequently co-occurs with physical and/or sexual abuse, it also often occurs by itself. In contrast, physical and sexual abuse are less likely to occur alone. Therefore, the observed effects for physical and sexual abuse in the current meta-analysis are likely larger than would be the case if the unique effects of each abuse subtype were observed, whereas a smaller reduction in effect size would likely be observed in the case of emotional abuse were its unique effect to be ascertained. Additional studies addressing this issue are therefore required to clarify the strength of the association between individual maltreatment subtypes and impulsivity.
Perhaps the most substantial limitation of the empirical literature to date is that although several of the studies included in this review employed a prospective design, none featured longitudinal analyses of childhood maltreatment in relation to impulsivity. That is, all evaluations of this association have involved retrospective assessments of maltreatment experiences in relation to current measures of impulsivity. From a purely methodological standpoint, this heavy reliance on retrospective recall of maltreatment experiences is a concern insofar as it may lead to systematic under-reporting due to imperfect recall. Indeed, although evidence exists that adults tend to be reasonably reliable in recalling experiences of childhood maltreatment (Bifulco, Brown, Lillie, & Jarvis, 1997), recent work has found a significant level of incongruence between prospectively and retrospectively ascertained data on adverse childhood experiences (Colman et al., 2016), and such discrepancy may potentially affect estimates of the strength of the association between childhood maltreatment and outcomes of interest (Liu, 2017).
Implicit in these cross-sectional assessments of impulsivity with retrospectively recalled childhood maltreatment is the assumption that this relationship is unidirectional in nature, that maltreatment experiences lead to greater impulsivity. This assumption is potentially problematic for several reasons. First, it may be that children with impulsive tendencies are more likely to experience maltreatment. Parents may find these children more challenging to manage, and in some cases, the resulting parental stress (Mash & Johnston, 1990) may lead to an escalation in disciplinary strategies, which could eventually include physical and emotional maltreatment. Such a possibility is not inconsistent with the finding in the present review that childhood sexual abuse, particularly when compared to childhood emotional abuse, was most weakly associated with general trait impulsivity.
A second possibility is that parents’ own impulsive tendencies may be a common factor underlying both risk for offspring impulsivity and child maltreatment. Consistent with this possibility, there is accumulating evidence for moderate genetic influences on impulsivity (Bezdjian, Baker, & Tuvblad, 2011; Niv, Tuvblad, Raine, Wang, & Baker, 2012) and several studies have found parental impulsivity to be associated with physical abuse (Fréchette, Zoratti, & Romano, 2015; Freisthler & Gruenewald, 2013; Price-Wolf, 2015) and neglect of offspring (Schumacher, Slep, & Heyman, 2001).
In summary, support was found in the current meta-analysis for an association between childhood maltreatment and impulsivity, with this relation generally observed to be stronger for emotional abuse, especially relative to sexual abuse. Nonetheless, these findings are qualified by several limitations prevalent throughout the empirical literature. Most notably, there is a need for research concurrently evaluating multiple forms of maltreatment in relation to impulsivity, thereby accounting for the significant level of co-occurrence between maltreatment subtypes and yielding a clearer picture of the unique effect of each form of maltreatment. Research is also particularly needed to extend beyond the current cross-sectional findings by employing longitudinal analyses to lend greater certainty in the temporal relationship between early maltreatment and impulsivity. Additionally, to ensure that this association is not simply a function of a common underlying relationship with parental impulsivity, future studies including an assessment of this construct are required. Finally, in addition to establishing the association between childhood maltreatment experiences and impulsivity, it would be important for future research in this area to elucidate the processes mediating and moderating this relationship for their potential to inform early intervention efforts. Such work is particularly crucial, given the considerable public health burden that has been associated with both early maltreatment experiences and impulsive behaviors.
Figure 3. Funnel plot for effect sizes in the meta-analyses. The vertical line indicates the weighted mean effect. Open circles indicate observed effects for actual studies, and closed circles indicate imputed effects for studies believed to be missing due to publication bias. The clear diamond reflects the unadjusted weighted mean effect size, whereas the black diamond reflects the weighted mean effect size after adjusting for publication bias.
3a. Overall childhood maltreatment and general trait impulsivity
3b. Childhood sexual abuse and general trait impulsivity
3c. Childhood physical abuse and general trait impulsivity
3d. Childhood physical neglect and general trait impulsivity
3e. Childhood emotional abuse and general trait impulsivity
3f. Childhood emotional neglect and general trait impulsivity
Acknowledgments
Preparation of this manuscript was supported in part by the National Institute of Mental Health of the National Institutes of Health under Award Numbers R01MH101138 and R21MH112055. The content is solely the responsibility of the author and does not necessarily represent the official views of the funding agency.
Footnotes
The reference here is to the influence of one’s current affective state on performance on a specific measure of impulsivity, rather than one’s self-reported general disposition toward impulsiveness when experiencing positive or negative affect (e.g., negative urgency). Also note that it is not implied here that these measures are solely state-based. Rather, they are sensitive to both state and trait effects (Peters & Büchel, 2011).
These eight studies were excluded after attempts to contact the study authors did not produce sufficient data for inclusion in the meta-analysis. An additional six studies (Amr, Elsayed, & Ibrahim, 2016; Conley & Garza, 2011; Harden, Carlson, Kretsch, Corbin, & Fromme, 2015; Narvaez et al., 2012; Rylands et al., 2012; Stoltenberg, Anderson, Nag, & Anagnopoulos, 2012) similarly did not report data required for meta-analysis, but were retained after the necessary data were obtained from the study authors.
Twenty studies featured overlapping samples. Whenever it remained unclear after inspection of the full text whether two studies reported on overlapping samples, the study authors were contacted to seek clarity on this issue. In cases where two or more studies used the same or overlapping samples but reported on different forms of childhood maltreatment and/or impulsivity, both studies were retained for relevant analyses. In cases where two or more studies used overlapping samples to examine the same forms of childhood maltreatment and impulsivity, the results of analyses based on the largest sample were retained. In the case where two studies assessed the association between childhood maltreatment and impulsivity in different subgroups of the same sample (Becker & Grilo, 2006, 2007), the study that provided analyses of this association in the most number of non-overlapping subgroups was included in the main analysis (Becker & Grilo, 2007), and the other study, which provided analyses of this association in males and females separately, was included in analyses involving sex as a moderator of effect size (Becker & Grilo, 2006).
One study yielded separate effects for males and females (Becker-Blease & Freyd, 2008), and another for three racial groups (Becker & Grilo, 2007).
As none of the analyses for maltreatment subtypes included child samples, the relevant moderator analyses for age were restricted to comparisons between adolescent and adult samples.
Age treated as a categorical variable was not assessed as a moderator for childhood emotional and physical neglect, respectively, as there were only two relevant studies of each neglect subtype featuring adolescent samples.
Sample type was not assessed as a moderator for childhood physical and emotional neglect, as there were insufficient numbers of studies featuring community samples in both cases.
References
- Alloy LB, Abramson LY. The role of the Behavioral Approach System (BAS) in bipolar spectrum disorders. Current Directions in Psychological Science. 2010;19:189–194. doi: 10.1177/0963721410370292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amr M, Elsayed H, Ibrahim IMA. Impulsive behavior and its correlates among patients with schizophrenia in a tertiary care psychiatry setting in Mansoura. Asian Journal of Psychiatry. 2016;22:111–115. doi: 10.1016/j.ajp.2016.06.009. [DOI] [PubMed] [Google Scholar]
- Aron AR, Fletcher PC, Bullmore ET, Sahakian BJ, Robbins TW. Stop-signal inhibition disrupted by damage to right inferior frontal gyrus in humans. Nature Neuroscience. 2003;6:115–116. doi: 10.1038/nn1003. [DOI] [PubMed] [Google Scholar]
- Bari A, Robbins TW. Inhibition and impulsivity: behavioral and neural basis of response control. Progress in Neurobiology. 2013;108:44–79. doi: 10.1016/j.pneurobio.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Becker-Blease KA, Freyd JJ. A preliminary study of ADHD symptoms and correlates: Do abused children differ from nonabused children? Journal of Aggression, Maltreatment & Trauma. 2008;17:133–140. doi: 10.1080/10926770802250736. [DOI] [Google Scholar]
- Becker DF, Grilo CM. Prediction of drug and alcohol abuse in hospitalized adolescents: comparisons by gender and substance type. Behaviour Research and Therapy. 2006;44:1431–1440. doi: 10.1016/j.brat.2005.10.009. [DOI] [PubMed] [Google Scholar]
- Becker DF, Grilo CM. Ethnic differences in the predictors of drug and alcohol abuse in hospitalized adolescents. American Journal on Addictions. 2007;16:389–396. doi: 10.1080/10550490701525343. [DOI] [PubMed] [Google Scholar]
- Belsky J, Schlomer GL, Ellis BJ. Beyond cumulative risk: Distinguishing harshness and unpredictability as determinants of parenting and early life history strategy. Developmental Psychology. 2012;48:662–673. doi: 10.1037/a0024454. [DOI] [PubMed] [Google Scholar]
- Belsky J, Steinberg L, Draper P. Childhood experience, interpersonal development, and reproductive strategy: An evolutionary theory of socialization. Child Development. 1991;62:647–670. doi: 10.1111/j.1467-8624.1991.tb01558.x. [DOI] [PubMed] [Google Scholar]
- Bezdjian S, Baker LA, Tuvblad C. Genetic and environmental influences on impulsivity: A meta-analysis of twin, family and adoption studies. Clinical Psychology Review. 2011;31:1209–1223. doi: 10.1016/j.cpr.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Koffarnus MN, Moody L, Wilson AG. The behavioral- and neuro-economic process of temporal discounting: A candidate behavioral marker of addiction. Neuropharmacology. 2014;76(Pt B):518–527. doi: 10.1016/j.neuropharm.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, Lillie A, Jarvis J. Memories of childhood neglect and abuse: Corroboration in a series of sisters. Journal of Child Psychology and Psychiatry. 1997;38:365–374. doi: 10.1111/j.1469-7610.1997.tb01520.x. [DOI] [PubMed] [Google Scholar]
- Biostat. Comprehensive Meta-Analysis Version 3. Englewood, NJ: Biostat; 2014. [Google Scholar]
- Blair CB, Raver CC. Poverty, stress, and brain development: New directions for prevention and intervention. Academic Pediatrics. 2016;16:S30–S36. doi: 10.1016/j.acap.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braquehais MD, Oquendo MA, Baca-García E, Sher L. Is impulsivity a link between childhood abuse and suicide? Comprehensive Psychiatry. 2010;51:121–129. doi: 10.1016/j.comppsych.2009.05.003. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Colman I, Kingsbury M, Garad Y, Zeng Y, Naicker K, Patten S, Jones PB, et al. Consistency in adult reporting of adverse childhood experiences. Psychological Medicine. 2016;46:543–549. doi: 10.1017/S0033291715002032. [DOI] [PubMed] [Google Scholar]
- Conley TD, Garza MR. Gender and sequelae of child versus adult onset of sexual victimization: Body mass, binge eating, and promiscuity. Journal of Applied Social Psychology. 2011;41:2551–2572. doi: 10.1111/j.1559-1816.2011.00828.x. [DOI] [Google Scholar]
- Costello EJ, Pine DS, Hammen C, March JS, Plotsky PM, Weissman MM, Biederman J, et al. Development and natural history of mood disorders. Biological Psychiatry. 2002;52:529–542. doi: 10.1016/S0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- Currie J, Widom CS. Long-term consequences of child abuse and neglect on adult economic well-being. Child Maltreatment. 2010;15:111–120. doi: 10.1177/1077559509355316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Coskunpinar A. Measurement of constructs using self-report and behavioral lab tasks: Is there overlap in nomothetic span and construct representation for impulsivity? Clinical Psychology Review. 2011;31:965–982. doi: 10.1016/j.cpr.2011.06.001. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Coskunpinar A. The relationship between self-report and lab task conceptualizations of impulsivity. Journal of Research in Personality. 2012;46:121–124. doi: 10.1016/j.jrp.2011.11.005. [DOI] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment. 2007;19:107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- Del Giudice M, Ellis BJ, Shirtcliff EA. Neuroscience and Biobehavioral Reviews. Vol. 35. Elsevier Ltd; 2011. The Adaptive Calibration Model of stress responsivity; pp. 1562–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh DM, Moeller FG, Swann AC. Suicidal behaviors and drug abuse: Impulsivity and its assessment. Drug and Alcohol Dependence. 2004;76:S93–S105. doi: 10.1016/j.drugalcdep.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. JAMA. 2001;286:3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125:e778–786. doi: 10.1542/peds.2009-0597. [DOI] [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the Adverse Childhood Experiences study. American Journal of Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Egeland B, Jacobvitz D, Sroufe LA. Breaking the cycle of abuse. Child Development. 1988;59:1080–1088. doi: 10.2307/1130274. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BJ, Del Giudice M. Beyond allostatic load: Rethinking the role of stress in regulating human development. Development and Psychopathology. 2014;26:1–20. doi: 10.1017/S0954579413000849. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Figueredo AJ, Brumbach BH, Schlomer GL. Fundamental dimensions of environmental risk: The impact of harsh versus unpredictable environments on the evolution and development of life history strategies. Human Nature. 2009;20:204–268. doi: 10.1007/s12110-009-9063-7. [DOI] [PubMed] [Google Scholar]
- Etain B, Henry C, Bellivier F, Mathieu F, Leboyer M. Beyond genetics: Childhood affective trauma in bipolar disorder. Bipolar Disorders. 2008;10:867–876. doi: 10.1111/j.1399-5618.2008.00635.x. [DOI] [PubMed] [Google Scholar]
- Fang X, Brown DS, Florence CS, Mercy JA. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse & Neglect. 2012;36:156–165. doi: 10.1016/j.chiabu.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: A neglected component in child victimization. Child Abuse & Neglect. 2007;31:7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Fischer S, Smith GT, Cyders MA. Another look at impulsivity: a meta-analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clinical Psychology Review. 2008;28:1413–1425. doi: 10.1016/j.cpr.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fréchette S, Zoratti M, Romano E. What is the link between corporal punishment and child physical abuse? Journal of Family Violence. 2015;30:135–148. doi: 10.1007/s10896-014-9663-9. [DOI] [Google Scholar]
- Freisthler B, Gruenewald PJ. Where the individual meets the ecological: a study of parent drinking patterns, alcohol outlets, and child physical abuse. Alcoholism, Clinical and Experimental Research. 2013;37:993–1000. doi: 10.1111/acer.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershoff ET. Corporal punishment by parents and associated child behaviors and experiences: A meta-analytic and theoretical review. Psychological Bulletin. 2002;128:539–579. doi: 10.1037/0033-2909.128.4.539. [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Glaser D. Emotional abuse and neglect (psychological maltreatment): a conceptual framework. Child Abuse & Neglect. 2002;26:697–714. doi: 10.1016/S0145-2134(02)00342-3. [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haber SN, Knutson B. The reward circuit: Linking primate anatomy and human imaging. Neuropsychopharmacology. 2010 doi: 10.1038/npp.2009.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton KR, Littlefield AK, Anastasio NC, Cunningham KA, Fink LHL, Wing VC, Mathias CW, et al. Rapid-response impulsivity: Definitions, measurement issues, and clinical implications. Personality Disorders: Theory, Research, and Treatment. 2015;6:168–181. doi: 10.1037/per0000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton KR, Mitchell MR, Wing VC, Balodis IM, Bickel WK, Fillmore M, Lane SD, et al. Choice impulsivity: Definitions, measurement issues, and clinical implications. Personality Disorders: Theory, Research, and Treatment. 2015;6:182–198. doi: 10.1037/per0000099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza CA, Willoughby T, Heffer T. Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clinical Psychology Review. 2015;38:13–24. doi: 10.1016/j.cpr.2015.02.010. [DOI] [PubMed] [Google Scholar]
- Harden KP, Carlson MD, Kretsch N, Corbin WR, Fromme K. Childhood sexual abuse and impulsive personality traits: Mixed evidence for moderation by DRD4 genotype. Journal of Research in Personality. 2015;55:30–40. doi: 10.1016/j.jrp.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart H, Rubia K. Neuroimaging of child abuse: A critical review. Frontiers in Human Neuroscience. 2012;6:52. doi: 10.3389/fnhum.2012.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins DJ, McCabe MP. Multi-type maltreatment and the long-term adjustment of adults. Child Abuse Review. 2000;9:6–18. doi: 10.1002/(SICI)1099-0852(200001/02)9:1<6::AID-CAR579>3.0.CO;2-W. [DOI] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill J, Pickles A, Rollinson L, Davies R, Byatt M. Juvenile- versus adult-onset depression: Multiple differences imply different pathways. Psychological Medicine. 2004;34:1483–1493. doi: 10.1017/S0033291704002843. [DOI] [PubMed] [Google Scholar]
- Infurna MR, Reichl C, Parzer P, Schimmenti A, Bifulco A, Kaess M. Associations between depression and specific childhood experiences of abuse and neglect: A meta-analysis. Journal of Affective Disorders. 2016;190:47–55. doi: 10.1016/j.jad.2015.09.006. [DOI] [PubMed] [Google Scholar]
- Jakubczyk A, Brower KJ, Kopera M, Krasowska A, Michalska A, Łoczewska A, Majewska A, et al. Physical pain and impulsivity in alcohol-dependent patients. Addiction Research & Theory. 2016;24:458–465. doi: 10.3109/16066359.2016.1164844. [DOI] [Google Scholar]
- Jakubczyk A, Klimkiewicz A, Mika K, Bugaj M, Konopa A, Podgórska A, Brower KJ, et al. Psychosocial predictors of impulsivity in alcohol-dependent patients. Journal of Nervous and Mental Disease. 2013;201:43–47. doi: 10.1097/NMD.0b013e31827aaf9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane SD, Cherek DR, Rhodes HM, Pietras CJ, Tcheremissine OV. Relationships among laboratory and psychometric measures of impulsivity: Implications in substance abuse and dependence. Addictive Disorders & Their Treatment. 2003;2:33–40. doi: 10.1097/00132576-200302020-00001. [DOI] [Google Scholar]
- Liu RT. Childhood adversities and depression in adulthood: Current findings and future directions. Clinical Psychology: Science and Practice. 2017;24:140–153. doi: 10.1111/cpsp.12190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Scopelliti KM, Pittman SK, Zamora AS. Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. Lancet Psychiatry. 2018;5:51–64. doi: 10.1016/S2215-0366(17)30469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Trout ZM, Hernandez EM, Cheek SM, Gerlus N. A behavioral and cognitive neuroscience perspective on impulsivity, suicide, and non-suicidal self-injury: Meta-analysis and recommendations for future research. Neuroscience & Biobehavioral Reviews. 2017;83:440–450. doi: 10.1016/J.NEUBIOREV.2017.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Castroman J, Jaussent I, Beziat S, Guillaume S, Baca-Garcia E, Genty C, Olié E, et al. Increased severity of suicidal behavior in impulsive aggressive patients exposed to familial adversities. Psychological Medicine. 2014;44:3059–3068. doi: 10.1017/S0033291714000646. [DOI] [PubMed] [Google Scholar]
- Luby JL, Barch D, Whalen D, Tillman R, Belden A. Association Between Early Life Adversity and Risk for Poor Emotional and Physical Health in Adolescence. JAMA Pediatrics. 2017;171:1168–1175. doi: 10.1001/jamapediatrics.2017.3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Lutz PE, Tanti A, Gasecka A, Barnett-Burns S, Kim JJ, Zhou Y, Chen GG, et al. Association of a history of child abuse with impaired myelination in the anterior cingulate cortex: Convergent epigenetic, transcriptional, and morphological evidence. American Journal of Psychiatry. 2017;174:1185–1194. doi: 10.1176/appi.ajp.2017.16111286. [DOI] [PubMed] [Google Scholar]
- Maniglio R. The role of child sexual abuse in the etiology of suicide and non-suicidal self-injury. Acta Psychiatrica Scandinavica. 2011;124:30–41. doi: 10.1111/j.1600-0447.2010.01612.x. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Hegerl U, et al. Suicide prevention strategies: A systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- Mash EJ, Johnston C. Determinants of parenting stress: Illustrations from families of hyperactive children and families of physically abused children. Journal of Clinical Child Psychology. 1990;19:313–328. doi: 10.1207/s15374424jccp1904_3. [DOI] [Google Scholar]
- McLaughlin KA. Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child and Adolescent Psychology. 2016;45:361–382. doi: 10.1080/15374416.2015.1110823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. American Journal of Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. American Journal of Psychiatry. 2011;169:141–151. doi: 10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- Narvaez JCM, Magalhães PVS, Trindade EK, Vieira DC, Kauer-Sant’anna M, Gama CS, von Diemen L, et al. Childhood trauma, impulsivity, and executive functioning in crack cocaine users. Comprehensive Psychiatry. 2012;53:238–244. doi: 10.1016/j.comppsych.2011.04.058. [DOI] [PubMed] [Google Scholar]
- Ney PG, Fung T, Wickett AR. The worst combinations of child abuse and neglect. Child Abuse & Neglect. 1994;18:705–714. doi: 10.1016/0145-2134(94)00037-9. [DOI] [PubMed] [Google Scholar]
- Niv S, Tuvblad C, Raine A, Wang P, Baker LA. Heritability and longitudinal stability of impulsivity in adolescence. Behavior Genetics. 2012;42:378–392. doi: 10.1007/s10519-011-9518-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orwin RG. A Fail-safe N for effect size in meta-analysis. Journal of Educational Statistics. 1983;8:157–159. doi: 10.2307/1164923. [DOI] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. Journal of Clinical Psychology. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::AID-JCLP2270510607>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: An integrated review of human literature. Psychopharmacology. 2011;214:55–70. doi: 10.1007/s00213-010-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters J, Büchel C. The neural mechanisms of inter-temporal decision-making: Understanding variability. Trends in Cognitive Sciences. 2011;15:227–239. doi: 10.1016/j.tics.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Post RM, Leverich GS. The role of psychosocial stress in the onset and progression of bipolar disorder and its comorbidities: The need for earlier and alternative modes of therapeutic intervention. Development and Psychopathology. 2006;18:1181–1211. doi: 10.1017/S0954579406060573. [DOI] [PubMed] [Google Scholar]
- Price-Wolf J. Social support, collective efficacy, and child physical abuse: does parent gender matter? Child Maltreatment. 2015;20:125–135. doi: 10.1177/1077559514562606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao S, Lux AL. The epidemiology of child maltreatment. Paediatrics and Child Health. 2012;22:459–464. doi: 10.1016/j.paed.2012.09.002. [DOI] [Google Scholar]
- Reynolds B, Ortengren A, Richards JB, de Wit H. Dimensions of impulsive behavior: Personality and behavioral measures. Personality and Individual Differences. 2006;40:305–315. doi: 10.1016/j.paid.2005.03.024. [DOI] [Google Scholar]
- Reynolds B, Penfold RB, Patak M. Dimensions of impulsive behavior in adolescents: Laboratory behavioral assessments. Experimental and Clinical Psychopharmacology. 2008;16:124–131. doi: 10.1037/1064-1297.16.2.124. [DOI] [PubMed] [Google Scholar]
- Robbins TW, Gillan CM, Smith DG, de Wit S, Ersche KD. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends in Cognitive Sciences. 2012;16:81–91. doi: 10.1016/j.tics.2011.11.009. [DOI] [PubMed] [Google Scholar]
- Rohrbeck CA, Twentyman CT. Multimodal assessment of impulsiveness in abusing, neglecting, and nonmaltreating mothers and their preschool children. Journal of Consulting and Clinical Psychology. 1986;54:231–236. doi: 10.1037/0022-006X.54.2.231. [DOI] [PubMed] [Google Scholar]
- Rylands AJ, Hinz R, Jones M, Holmes SE, Feldmann M, Brown G, McMahon AW, et al. Pre- and postsynaptic serotonergic differences in males with extreme levels of impulsive aggression without callous unemotional traits: A positron emission tomography study using 11C-DASB and 11C-MDL100907. Biological Psychiatry. 2012;72:1004–1011. doi: 10.1016/j.biopsych.2012.06.024. [DOI] [PubMed] [Google Scholar]
- Schumacher JA, Slep AMS, Heyman RE. Risk factors for child neglect. Aggression and Violent Behavior. 2001;6:231–254. doi: 10.1016/S1359-1789(00)00024-0. [DOI] [Google Scholar]
- Sergentanis TN, Sakelliadis EI, Vlachodimitropoulos D, Goutas N, Sergentanis IN, Spiliopoulou CA, Papadodima S. Does history of childhood maltreatment make a difference in prison? A hierarchical approach on early family events and personality traits. Psychiatry Research. 2014;220:1064–1070. doi: 10.1016/j.psychres.2014.10.019. [DOI] [PubMed] [Google Scholar]
- Stoltenberg SF, Anderson C, Nag P, Anagnopoulos C. Association between the serotonin transporter triallelic genotype and eating problems is moderated by the experience of childhood trauma in women. International Journal of Eating Disorders. 2012;45:492–500. doi: 10.1002/eat.20976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, van IJzendoorn MH. The universality of childhood emotional abuse: A meta-analysis of worldwide prevalence. Journal of Aggression, Maltreatment & Trauma. 2012;21:870–890. doi: 10.1080/10926771.2012.708014. [DOI] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, van IJzendoorn MH. The prevalence of child maltreatment across the globe: Review of a series of meta-analyses. Child Abuse Review. 2015;24:37–50. doi: 10.1002/car.2353. [DOI] [Google Scholar]
- Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neuroscience and Biobehavioral Reviews. 2003;27:33–44. doi: 10.1016/s0149-7634(03)00007-1. [DOI] [PubMed] [Google Scholar]
- Teicher MH, Samson JA. Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. American Journal of Psychiatry. 2013;170:1114–1133. doi: 10.1176/appi.ajp.2013.12070957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Samson JA. Enduring neurobiological effects of childhood abuse and neglect. Journal of Child Psychology and Psychiatry. 2016;57:241–66. doi: 10.1111/jcpp.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Samson JA, Polcari A, McGreenery CE. Sticks, stones, and hurtful words: Relative effects of various forms of childhood maltreatment. American Journal of Psychiatry. 2006;163:993–1000. doi: 10.1176/appi.ajp.163.6.993. [DOI] [PubMed] [Google Scholar]
- Turecki G. Dissecting the suicide phenotype: The role of impulsive-aggressive behaviours. Journal of Psychiatry and Neuroscience. 2005 [PMC free article] [PubMed] [Google Scholar]
- van Gaalen MM, Brueggeman RJ, Bronius PFC, Schoffelmeer ANM, Vanderschuren LJMJ. Behavioral disinhibition requires dopamine receptor activation. Psychopharmacology. 2006;187:73–85. doi: 10.1007/s00213-006-0396-1. [DOI] [PubMed] [Google Scholar]
- van Gaalen MM, van Koten R, Schoffelmeer ANM, Vanderschuren LJMJ. Critical involvement of dopaminergic neurotransmission in impulsive decision making. Biological Psychiatry. 2006;60:66–73. doi: 10.1016/j.biopsych.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasta R. Physical child abuse: A dual-component analysis. Developmental Review. 1982;2:125–149. doi: 10.1016/0273-2297(82)90007-7. [DOI] [Google Scholar]
- Wenzel A, Beck AT. A cognitive model of suicidal behavior: Theory and treatment. Applied and Preventive Psychology. 2008;12:189–201. doi: 10.1016/j.appsy.2008.05.001. [DOI] [Google Scholar]
- Whelan R, Conrod PJ, Poline JB, Lourdusamy A, Banaschewski T, Barker GJ, Bellgrove MA, et al. Adolescent impulsivity phenotypes characterized by distinct brain networks. Nature Neuroscience. 2012;15:920–925. doi: 10.1038/nn.3092. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. doi: 10.1016/S0191-8869(00)00064-7. [DOI] [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJV, Hackmann A, et al. Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: A randomized dismantling trial. Journal of Consulting and Clinical Psychology. 2014;82:275–286. doi: 10.1037/a0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstanley CA, Eagle DM, Robbins TW. Behavioral models of impulsivity in relation to ADHD: Translation between clinical and preclinical studies. Clinical Psychology Review. 2006;26:379–395. doi: 10.1016/j.cpr.2006.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstanley CA, Olausson P, Taylor JR, Jentsch JD. Insight into the relationship between impulsivity and substance abuse from studies using animal models. Alcoholism, Clinical and Experimental Research. 2010;34:1306–1318. doi: 10.1111/j.1530-0277.2010.01215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright L, Lipszyc J, Dupuis A, Thayapararajah SW, Schachar R. Response inhibition and psychopathology: A meta-analysis of go/no-go task performance. Journal of Abnormal Psychology. 2014;123:429–439. doi: 10.1037/a0036295. [DOI] [PubMed] [Google Scholar]
- Zielinski DS. Child maltreatment and adult socioeconomic well-being. Child Abuse & Neglect. 2009;33:666–678. doi: 10.1016/j.chiabu.2009.09.001. [DOI] [PubMed] [Google Scholar]