Abstract
Objective:
To assess weight trends and diabetes prevalence among US veterans.
Methods:
We used information from the Veterans Affairs (VA) Informatics and Computing Infrastructure (VINCI) Corporate Data Warehouse (CDW) to construct datasets that included demographic data, diabetes status, and weight observations for males and females. Secular and longitudinal trends in mean weight were analyzed.
Results:
4,527,865 patients born from 1915-1984 with weight data during 2000-2014 were included; 36.8% had diabetes. Mean weight at baseline was higher in men and women with diabetes (97 kg and 88 kg, respectively) than in men and women without diabetes (86 kg and 76 kg, respectively). Mean weight increased from 2000-2014 (P < .001) at rates of 0.36 kg/year in women without diabetes, 0.28 kg/year in men with diabetes, 0.25 kg/y in men without diabetes, and 0.22 kg/year in women with diabetes. Weight decreased in those born before 1940, was stable in those born 1940-1949, and increased in those born since 1950.
Conclusions:
Among contemporary veterans, women without diabetes are gaining weight more rapidly than women with diabetes or men. Younger veterans are gaining weight more rapidly than older veterans. Further efforts are needed to prevent weight gain in veterans, especially among women.
Keywords: veterans, diabetes, weight, longitudinal trends, descriptive statistics
Introduction
Weight gain is a critical risk factor for the development of diabetes, its complications, and other chronic diseases. Although obesity and diabetes are public health problems of epidemic proportions, there is incomplete understanding of age-related trends in weight. The prevalence of obesity and diabetes is known to be increasing in United States populations,1-4 and veterans comprise an estimated 14.6% of US adults aged ≥ 21 years,5 but limited data exist on trends in weight and diabetes prevalence in veterans.
A single previous longitudinal study of weight trends in veterans was identified. The Normative Aging Study was a prospective cohort study of healthy male veterans from the Boston, Massachusetts area recruited in 1961-1970, ranging in age from 30 to 78 years at baseline, for whom weight and BMI have been reported.6 More recently, longitudinal trends of obesity and overweight in a prospective study of male and female veterans participating in the Millennium Cohort Study have been reported for 2001-2008.7
The purpose of this study was to evaluate contemporary age-related trends in weight and diabetes prevalence in the United States Veterans Administration (VA) healthcare system, the largest integrated healthcare system in the United States. The VA has an extensive electronic medical records database widely used in epidemiological research in obesity and diabetes. Both secular and longitudinal trends in weight were evaluated, in men and women, with and without diabetes, over a 15-year study period. In terms of secular trends, it was hypothesized that average weight would increase in men and women with and without diabetes from 2000 to 2014, that groups with diabetes would weigh more than groups without diabetes, and that men would weigh more than women. In terms of longitudinal trends, it was hypothesized that as individuals aged, they would gain weight.
Methods
Database.
The Department of Veterans Affairs (VA) Informatics and Computing Infrastructure (VINCI) Clinical Data Warehouse (CDW) was interrogated using structured query language (SQL). Extracted data were analyzed using the VINCI platform. These data used to assess secular and longitudinal trends in body weight in men and women with and without diabetes were obtained from the Institutional Review Board-approved data repository, “VA Diabetes Related Epidemiological Analyses” eIRB #66117.
Study population.
The CDW is a comprehensive source of medical records data, including patient demographics, diagnoses, procedures, medications, and laboratory data.8 The data used for this study comprised essentially all patients in the United States who were seen in an outpatient primary care visit for any reason within the VA healthcare system during 2000-2014. Using a unique patient identifier, demographic, primary care, and laboratory data were extracted with SQL (Oracle Corporation, Redwood Shores, CA) and SAS 9.4 (SAS Corporation, Cary, NC). Excluding persons with birth years outside the range 1915-1984, 5,725,576 unique veterans with at least 4 weight measurements during the study period 2000-2014 were identified (Figure S1).
Concordant with the methods used in previous Atlanta VA research,8,9 patients were classified as having diabetes if they had a least one use of ICD-9 code 250.xx in conjunction with an outpatient visit with a primary care provider (criterion A), or if they had any two uses of the 250.xx ICD-9 codes (criterion B), or if they had been prescribed an antihyperglycemic medication at any time during the study period (criterion C). Individuals who satisfied the diagnostic criteria at any time during the study period were considered to have diabetes for the entire study period. Among the patients with diabetes, at least 1 glycated hemoglobin measurement in each of 4 consecutive calendar years was required for inclusion in the primary analysis dataset.
Weight observations outside the range 0-1000 lb were excluded. Within this range, analyses based on extreme outliers may not be generalizable to other outpatient populations with obesity and/or diabetes. We therefore excluded observations below 80 lb (36.4 kg) (0.09% of the group) or greater than 600 lb (272.7 kg) (0.01% of the group). After excluding 152,870 patients with missing race information, 4,527,865 unique veterans (1,666,346 with diabetes) with 170,066,583 corresponding weight observations were available for the primary analyses (Table 1; Figures 1 and S1).
Table 1.
All Patients (2000-2014) by Cohort, Sex, and Diabetes Status (Primary Analysis Dataset)
| Cohort | Age in 2014, y |
Total | F, No DM | F, DM | M, No DM | M, DM |
|---|---|---|---|---|---|---|
| 1915-1919 | 95-99 | 90,373 | 1761 | 470 | 62,209 | 25,933 |
| 1920-1924 | 90-94 | 313,198 | 7989 | 2640 | 199,850 | 102,719 |
| 1925-1929 | 85-89 | 426,474 | 2007 | 847 | 262,333 | 161,287 |
| 1930-1934 | 80-84 | 498,854 | 3610 | 1920 | 288,920 | 204,404 |
| 1935-1939 | 75-79 | 403,176 | 3967 | 2224 | 223,870 | 173,115 |
| 1940-1944 | 70-74 | 498,171 | 6640 | 3793 | 273,641 | 214,097 |
| 1945-1949 | 65-69 | 906,017 | 13,237 | 7331 | 510,436 | 375,013 |
| 1950-1954 | 60-64 | 471,326 | 21,295 | 9899 | 270,580 | 169,552 |
| 1955-1959 | 55-59 | 325,181 | 25,387 | 8826 | 196,085 | 94,883 |
| 1960-1964 | 50-54 | 213,660 | 23,448 | 5971 | 134,402 | 49,839 |
| 1965-1969 | 45-49 | 138,318 | 16,765 | 3187 | 92,779 | 25,587 |
| 1970-1974 | 40-44 | 92,998 | 14,112 | 2153 | 65,146 | 11,587 |
| 1975-1979 | 35-39 | 72,146 | 13,248 | 1424 | 53,050 | 4424 |
| 1980-1984 | 30-34 | 77,973 | 13,848 | 973 | 60,904 | 2248 |
| Total | 30-99 | 4,527,865a | 167,314 | 51,658 | 2,694,205 | 1,614,688 |
Excludes 152,870 individuals with missing data. Grand total = 4,680,735.
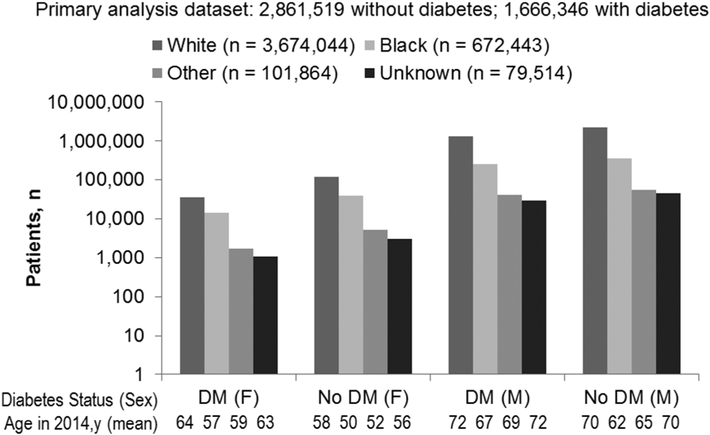
Figure 1.
Demographics of Unique Patients by Race, Sex, and Diabetes Status, Primary Analysis Dataset DM, diabetes mellitus; F, female; M, male.
Survivor dataset.
A dataset limited to individuals (survivors) with weight observations at the endpoints of the full study period (2000 and 2014) was also constructed to eliminate possible selection bias from differing samples at each endpoint. The survivor dataset included 859,945 unique veterans with 51,119,377 weight observations (Table S1, Figure S1). BMI was calculated using the Centers for Disease Control and Prevention formula using height and weight data obtained on the same date.
Statistical analysis.
Secular trends were analyzed by generating descriptive statistics for weight by year of observation, stratified by sex and diabetes status. Means, standard deviations, medians, interquartile ranges, minima, and maxima were computed in pounds, then converted to kilograms.
Longitudinal trends were analyzed using 14 birth cohorts with nonoverlapping 5-year intervals (e.g., 1915-1919, 1920-1924…1980-1984). Weight statistics were calculated for the years 2000 and 2014 for each cohort, stratified by sex and diabetes status. Longitudinal trends were also analyzed for the survivor dataset. BMI trends were analyzed only in the survivor dataset.
SAS/Grid (SAS 9.4) was used for the survivor weight analyses. Some figures were prepared with Excel (Microsoft Corporation, Redmond, WA).
Results
Number of patients and weight observations.
The participants included in the primary analysis dataset were predominantly male (95%), 81% white, 15% black, and 4% other or unknown race. Individuals with diabetes were older than individuals without diabetes, and men were older than women (Figure 1). Among the patients with diabetes, 1,649,540 (59.4%) initially qualified for inclusion according to criterion A, 547,235 (19.7%) according to criterion B, and 580,601 (20.9%) according to criterion C. The distributions of patients by birth cohort in the primary analysis and survivor datasets were comparable (Figure S2).
Secular weight trends.
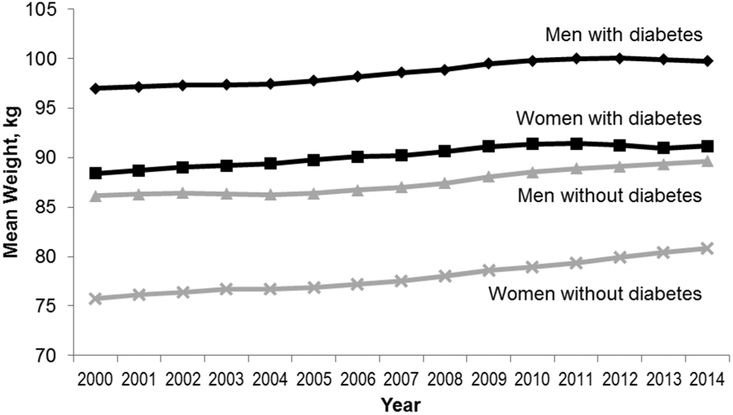
Mean body weight among men and women with and without diabetes increased from 2000 to 2014 (Figure 2 and Tables 2-5). The coefficients of determination (R2) for the fitted regression lines ranged from 0.90 to 0.97 (P < .0001), indicating a progressive trend for weight increase in all groups (Figure S3). Mean weight at baseline was higher in men and women with diabetes (97.0 kg and 88.4 kg, respectively) than in men and women without diabetes (86.2 kg and 75.6 kg, respectively). The highest rate of weight increase was in women without diabetes (0.36 kg/year), followed by men without diabetes (0.28 kg/year), men with diabetes (0.25 kg/year) and women with diabetes (0.22 kg/year). Individuals with diabetes weighed more than individuals without diabetes, however, women with diabetes weighed more than men without diabetes (Figure 2).
Figure 2.
Secular Weight Trends by Year, Sex, and Diabetes Status (Primary Analysis Dataset)
Table 2.
Summary of weight statistics by year of observation, females without diabetes, primary analysis dataset
| Wt Year |
n (wt) | Mean | SD | Median | Q1 | Q3 | Min | Max |
|---|---|---|---|---|---|---|---|---|
| 2000 | 169,039 | 75.76 | 17.47 | 73.26 | 63.05 | 85.73 | 36.29 | 238.46 |
| 2001 | 240,441 | 76.18 | 17.65 | 73.66 | 63.50 | 86.18 | 36.29 | 261.45 |
| 2002 | 285,739 | 76.40 | 17.83 | 73.94 | 63.50 | 86.64 | 36.29 | 253.11 |
| 2003 | 330,642 | 76.68 | 17.89 | 74.39 | 63.78 | 87.09 | 36.29 | 262.18 |
| 2004 | 383,278 | 76.76 | 13.53 | 74.39 | 63.59 | 87.09 | 36.29 | 254.47 |
| 2005 | 421,487 | 76.90 | 18.05 | 74.39 | 63.87 | 87.54 | 36.29 | 252.15 |
| 2006 | 451,965 | 77.20 | 18.24 | 74.84 | 63.96 | 87.91 | 36.29 | 267.00 |
| 2007 | 481,901 | 77.56 | 18.47 | 75.30 | 64.23 | 88.45 | 36.29 | 268.80 |
| 2008 | 533,047 | 78.01 | 18.52 | 75.75 | 64.64 | 88.91 | 36.29 | 270.00 |
| 2009 | 591,615 | 78.62 | 18.58 | 76.30 | 65.20 | 89.68 | 36.29 | 263.00 |
| 2010 | 602,800 | 78.95 | 18.62 | 76.70 | 65.36 | 90.13 | 36.29 | 265.00 |
| 2011 | 614,770 | 79.33 | 18.85 | 77.11 | 65.77 | 90.54 | 36.29 | 270.00 |
| 2012 | 586,246 | 79.93 | 19.09 | 77.79 | 66.09 | 91.22 | 36.29 | 266.00 |
| 2013 | 555,680 | 80.40 | 19.26 | 78.34 | 66.50 | 91.99 | 36.29 | 268.20 |
| 2014 | 540,531 | 80.86 | 19.47 | 78.88 | 66.72 | 92.53 | 36.29 | 272.16 |
Weight values in kg. Max, maximum; Min, minimum; n (wt), number of weight observations; Q1, 25% quartile; Q3, 75% quartile; Wt Year, year of weight observation.
Table 5.
Summary of weight statistics by year of observation, males with diabetes, primary analysis dataset
| Wt Year |
n (wt) | Mean | SD | Median | Q1 | Q3 | Min | Max |
|---|---|---|---|---|---|---|---|---|
| 2000 | 2,272,857 | 96.97 | 20.08 | 94.35 | 83.10 | 107.96 | 36.29 | 272.16 |
| 2001 | 3,196,477 | 97.16 | 20.29 | 94.71 | 83.10 | 108.41 | 36.29 | 272.16 |
| 2002 | 3,874,723 | 97.33 | 20.58 | 94.80 | 83.05 | 108.64 | 36.29 | 272.16 |
| 2003 | 4,503,663 | 97.38 | 20.88 | 94.80 | 83.01 | 108.86 | 36.29 | 272.16 |
| 2004 | 5,022,601 | 97.45 | 21.16 | 94.80 | 82.92 | 109.09 | 36.29 | 272.16 |
| 2005 | 5,337,943 | 97.77 | 21.52 | 95.26 | 83.01 | 109.77 | 36.29 | 272.16 |
| 2006 | 5,541,503 | 98.19 | 21.91 | 95.44 | 83.01 | 110.22 | 36.29 | 272.16 |
| 2007 | 5,686,208 | 98.60 | 22.24 | 95.80 | 83.19 | 110.90 | 36.29 | 272.16 |
| 2008 | 5,989,368 | 98.90 | 21.55 | 96.16 | 83.42 | 111.40 | 36.29 | 272.16 |
| 2009 | 6,357,949 | 99.51 | 22.66 | 96.84 | 83.82 | 112.13 | 36.29 | 272.08 |
| 2010 | 6,254,539 | 99.79 | 22.76 | 97.07 | 83.92 | 112.49 | 36.29 | 272.16 |
| 2011 | 6,135,949 | 100.00 | 22.94 | 97.30 | 83.92 | 112.95 | 36.29 | 272.16 |
| 2012 | 5,793,594 | 100.05 | 23.08 | 97.34 | 83.92 | 113.04 | 36.29 | 272.16 |
| 2013 | 5,486,242 | 99.91 | 23.08 | 97.16 | 83.82 | 112.95 | 36.29 | 272.16 |
| 2014 | 5,327,701 | 99.74 | 23.14 | 97.07 | 83.51 | 112.95 | 36.29 | 272.16 |
Weight values in kg. Max, maximum; Min, minimum; n (wt), number of weight observations; Q1, 25% quartile; Q3, 75% quartile; Wt Year, year of weight observation.
Longitudinal weight trends.
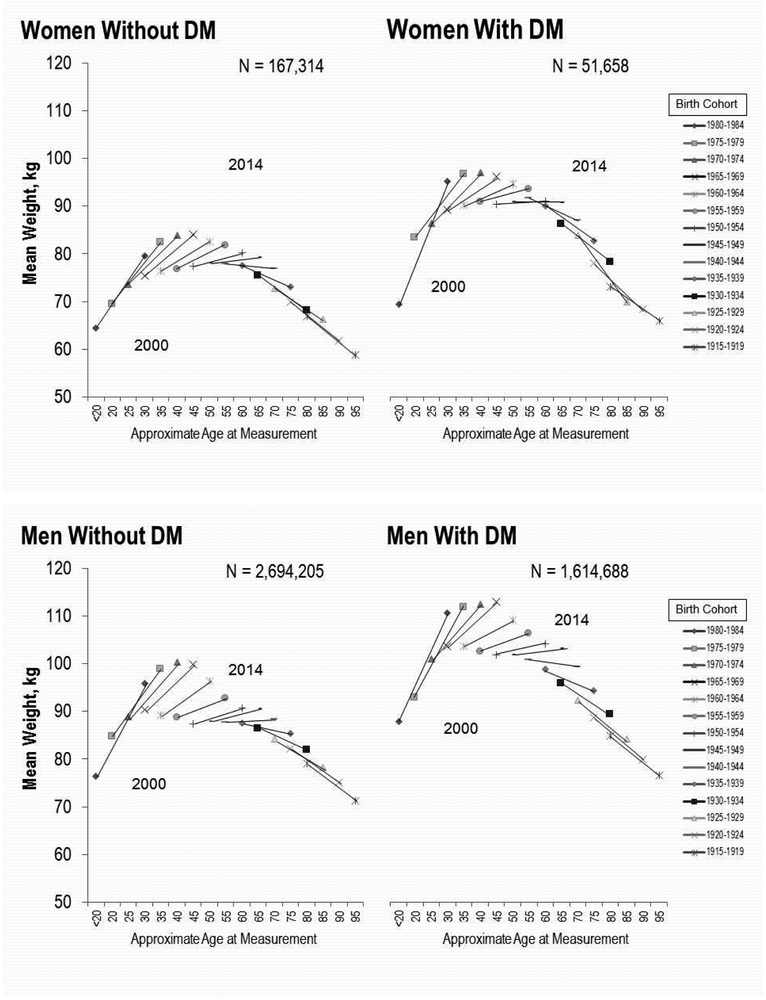
Weight trends varied by birth cohort, sex, and diabetes status. The oldest cohorts (approximately 1915-1919 to 1930-1934) lost weight over the study period, weight was stable in the middle cohorts (approximately 1940-1944 to 1945-1949), and the youngest cohorts (approximately 1950-1954 to 1980-1984) gained weight (Figures 3 and S4). Regardless of sex or diabetes status, older cohorts tended to lose weight, and younger cohorts tended to gain weight, with the most rapid rates of increase observed in the youngest cohorts.
Figure 3.
Longitudinal Weight Trends by Year, Sex, and Diabetes Status (Primary Analysis Dataset)
To assess whether the longitudinal patterns of weight change could be explained by selection bias, the preceding analyses were repeated on the survivor dataset. The results for the survivor dataset show similar trends for mean weight by birth cohort as for the primary analyses (Figures 3, S5, and S6).
BMI trends in the survivor dataset.
From 2000 to 2014, mean BMI increased in women with diabetes (33.1 ± 6.8 kg/m2 to 33.6 ± 7.5 kg/m2, annual rate of change, 0.04 kg/m2), and in women without diabetes (28.4 ± 6.2 kg/m2 to 29.9 ± 6.7 kg/m2, annual rate of change, 0.10 kg/m2), but was essentially unchanged in men without diabetes (28.2 ± 4.8 kg/m2 to 28.2 ± 5.8 kg/m2, annual rate of change, −0.00 kg/m2), and declined slightly in men with diabetes (31.5 ± 5.9 kg/m2 to 31.4 ± 6.8 kg/m2, annual rate of change, −0.01 kg/m2). Women with diabetes had higher BMI than women without diabetes and men regardless of diabetes status. Longitudinally, BMI increased in the younger cohorts, was stable in the middle cohorts, and decreased in the older cohorts (Figure S7).
Diabetes trends.
The proportion of patients with diabetes within each cohort in the primary analysis dataset varied from 4.1% to 43.7% (P < .0001) with a mean prevalence of 36.8% (Figure S8a). The highest prevalence of diabetes was observed in the 1940-1944 birth cohort (43.7%), decreasing to 4.1% in the youngest cohort (birth years 1980-1984). Diabetes was more prevalent in men (37.5%) than in women (23.6%).
In the survivor dataset, the proportion of patients with diabetes varied from 11.5% to 48.8% (P < .0001) with a mean prevalence of 42.6% (Figure S8b); the prevalence of diabetes was higher within 12 of 14 cohorts than in the primary analysis dataset. The highest prevalence of diabetes was observed in the 1940-1944 birth cohort (48.8%), decreasing to 11.5% in the youngest cohort. Diabetes was more prevalent in men (43.4%) than in women (30.4%).
Discussion
The current study differs from other studies examining weight, BMI, and diabetes trends in veterans, with higher weight, BMI, and diabetes prevalence than previously reported, but similar longitudinal patterns.
Prior studies of weight and/or BMI trends in veterans.
The Normative Aging Study considered birth cohorts with the same intervals as the current study, with 15-year trends for weight and BMI.6 The Normative Aging Study included 2280 males, 98% white, with a mean age of 42 years, without chronic disease at baseline.6 The Millennium Cohort Study reported weight change and obesity trends from a nationally representative sample of the US military population which included 42,200 participants, 71% white, of whom 25% were veterans.7 Koepsell et al analyzed obesity and overweight from 1999-2008 in veterans and non-veterans using the nationally representative National Health and Nutrition Examination Survey (NHANES)5; this study provides an important link between obesity trends in veterans and the overall US population.
Prior studies of diabetes prevalence in veterans.
A prior study of veterans investigated secular trends in diabetes prevalence; the subset analyzed in FY2000 (N = 3,332,566) had a similar proportion of males, but fewer whites (60%) and blacks (13%) with more other or unknown race (27%); approximately half of participants were aged 65 years or older.10 Another study (2005-2012) of 1,844,797 veterans investigated outcomes from a lifestyle intervention modeled on the Diabetes Prevention Program (MOVE! Weight Management Program for Veterans); it had slightly fewer males (93%) and whites (78%), but more blacks (18%) and a similar proportion of other races (4%); the mean age at baseline was 53.6 years, similar to the mean age at baseline in the current study (54 years); but the baseline prevalence of diabetes was 23%.9
Secular weight trends.
The two hypotheses with respect to the secular (cross-sectional) trends were confirmed: average weight increased during 2000-2014 in men and women with and without diabetes and individuals with diabetes were heavier than individuals without diabetes. However, women with diabetes were heavier than men without diabetes. In the Millennium Cohort Study, the average weight gain from 2001-2008 was 4.5 - 7.3 kg (0.56 kg/year) for women and 4.0 ± 6.8 kg (0.50 kg/year) for men, more rapid than observed in this study.7 Few studies have reported weight trends specifically in men and women with and without diabetes, but the findings in the current study differ from those observed in the General Practice Research Database (GPRD).11 In men and women with and without diabetes during 1995-2010, individuals with diabetes weighed more than individuals without diabetes, but men were uniformly heavier than women regardless of diabetes status.11 In the year 2000, weight in the current study was consistently higher in all groups than in the GPRD.
Longitudinal weight trends.
Longitudinal trends were not uniform across birth cohorts: as individuals aged, some gained weight and some lost weight. Weight generally decreased in cohorts born before 1940, was stable in cohorts born between 1940 and 1949, and increased in all cohorts born since 1950. The rate of weight increase accelerated progressively from the oldest to the youngest cohorts, and these trends were similar regardless of sex or diabetes status (Figures 3, S4, and S5). The trends for the men without diabetes resembled those reported in the Normative Aging Study for men without chronic disease, insofar as weight increased in the youngest cohorts and decreased in the oldest cohorts (Figure S9).6 The differences in mean weight across birth cohorts in the Normative Aging Study and the most nearly comparable group in this study, men without diabetes, ranged from 8-13 kg.6 Baseline weights in every cohort were higher, and the younger cohorts gained weight more rapidly than participants of the same age in the current study than in the Normative Aging Study.
The differences in weight change between birth cohorts observed during 2000-2014 cannot be explained by selection bias, as the differences between the primary analysis dataset and survivor dataset were minimal (Figures S4, S5, and S6). Weight loss in older adults may be attributed to loss of lean mass with age. The Health, Aging, and Body Composition Study found that approximately one-third of men and women aged 70-79 years lost weight during the following 5 years.12 The effects of weight loss on body composition differed by sex; in men, lean mass loss predominated over fat mass loss, whereas in women, both lean mass and fat mass contributed more equally.
BMI trends.
The mean BMI in the survivor dataset increased from 28.8 kg/m2 to 29.9 kg/m2 during the study period (annual rate of change, 0.01 kg/m2). In the Normative Aging Study, the overall annual rate of change was 0.12 kg/m2, higher than in the current study.6 However, the longitudinal patterns of BMI change in the current study were similar to those in the Normative Aging Study: BMI increased over 15 years in all participants aged 30 to 59 years, but decreased in participants aged ≥ 60 years.6 The average BMI in this study is higher than reported for veterans in the Millennium Cohort, in which the prevalence of obesity (BMI ≥ 30 kg/m2) over 8 years from 16% to 34% in men and 8% to 26% in women.7 In the current study, individuals with diabetes had markedly higher BMI than individuals without diabetes, and women had higher BMI than men. In the 1999-2008 NHANES, after adjusting for age, gender, and race/ethnicity, there were no significant differences in the distribution of BMI between veterans and non-veterans.5 In the 1998-2014 NHANES, among adults aged 20 or older, individuals with diabetes had higher BMI than individuals without diabetes, but women with diabetes had markedly higher BMI than men without diabetes, whereas men and women without diabetes had similar BMI.13
In the 1999-2008 NHANES, BMI at age 25 increased from the oldest to the youngest veterans (23.7, 24.3, and 24.8 kg/m2, respectively), and also increased at faster rates in younger veterans than older veterans (annual change in BMI of 0.13, 0.17, and 0.32 kg/m2, in the groups aged 60-74, 45-59, and 30-44 years, respectively), but veterans were less likely to have body fat < 25% or ≥ 35%.5 Similar patterns of BMI change within birth cohorts were observed in the Global Burden of Disease Study and the Health and Retirement Study.3,14
Diabetes trends.
The crude prevalence of diabetes in the primary analysis dataset is higher than that reported in FY2000 for the VA healthcare system (35.6% vs 19.6%).10 Miller et al found a peak prevalence of diabetes (27.0%) in those born during 1925-1934, lower than the 39.8% prevalence of diabetes for the same birth years in the primary analysis dataset (Figure S10). Although it is likely that there is substantial overlap in the patients included in Miller et al’s FY2000 dataset and patients included in the primary analysis dataset for the year 2000, there are at least two additional factors that may account for the higher prevalence of diabetes in the current study. Firstly, while Miller et al identified patients with diabetes using criteria similar to criteria A-C, unlike the current study they did not impose any restrictions with respect to the number of weight measurements to select patients for analysis. The primary dataset is more likely to include patients with diabetes than the overall VA population because individuals with chronic disease are more likely to have frequent weight measurements than individuals whose contact with the healthcare system is more episodic. Secondly, the methodology used to classify diabetes in the current study will tend to inflate the number of individuals with diabetes relative to Miller et al’s methodology because patients were classified with diabetes if they met criteria A-C at any timeduring the 15-year study period, whereas Miller et al classified patients with diabetes if they met similar criteria only during the year 2000. However, the general pattern of higher diabetes prevalence in the older cohorts, reduced prevalence in the oldest cohorts, and much lower prevalence in the youngest cohorts was observed in both studies. In MOVE!, which used criteria similar to the current study to identify diabetes, and is also likely to have substantial overlap in participants with the current study, the prevalence of diabetes was 38% among lifestyle intervention participants, and 21% among nonparticipants.9 Thus, the prevalence of diabetes among MOVE! participants was similar to the prevalence observed among individuals born between 1925 to 1954 in the primary dataset.
The crude prevalence of diabetes in the primary analysis dataset likely reflects a combination of survivor bias and natural history: diabetes becomes increasingly prevalent with age,1 but diabetes also reduces life expectancy and disability-free life expectancy.15,16 Decreasing diabetes prevalence in the oldest cohorts relative to the peak prevalence may be due to increased mortality (i.e., survivor bias) whereas low prevalence in the youngest cohort is likely due to insufficient age for the expression of diabetes (i.e., natural history). The crude prevalence of diabetes was generally higher in the survivor dataset than in the primary analysis dataset, but followed a similar pattern across birth cohorts.
Strengths.
This is the first report of secular and longitudinal diabetes and weight trends in a large, contemporary veteran population including both men and women. The large size of the datasets permits stratification of results by birth cohorts over a broad range of ages. Even the survivor dataset, at 18% of the size of the primary analysis dataset, had over 850,000 patients available for analysis. In contrast to the Normative Aging Study, the current study examined weight and diabetes prevalence from a much larger number of men and women veterans nationally. In contrast to a prior study of diabetes prevalence in the VA healthcare system, this study is larger, more recent, and examines longitudinal as well as secular trends in diabetes prevalence.10
Limitations.
This study was limited to US veterans and may not be generalizable to nonveteran populations without adjustment for age, sex, and race/ethnicity.5 This study also has some differences from other studies performed in veteran populations. Relative to the Normative Aging Study, this study included more individuals with chronic disease.6 Relative to the participants in the Millennium Cohort Study, the patients in this study were older, and included proportionately more males and more whites.7
Consistent with prior Atlanta VA research,8 subclassification of diabetes by type was not performed. However, the limits placed on ICD-9 codes and age range make it more likely that most individuals diagnosed according to criteria A and B have type 2 diabetes than type 1 diabetes. Of note, individuals with known type 1 diabetes are excluded from military service; all veterans with possible type 1 diabetes therefore have onset at age ≥ 18 years, and are not identified systematically. Women with polycystic ovarian syndrome and individuals with dysglycemia may have been misclassified with diabetes, since criterion C was only applied if a patient had not already been classified with diabetes according to diagnostic codes (criteria A and B). The antihyperglycemic agent metformin may be prescribed for polycystic ovarian syndrome in the absence of diabetes.17 Metformin may also be prescribed to individuals with dysglycemia to prevent the development of type 2 diabetes.18
Weight observations were restricted to the range 80-600 lb since weights outside of this range may reflect disease processes atypical of the clinical course of type 2 diabetes, the most prevalent type of diabetes in adults.1 Individuals with weight observations outside of this range were not omitted from the primary analysis dataset. Truncation is noted in the minimum and maximum values for the weight observations in Tables 2-5. However, the actual number of weight observations affected was small (< 0.1%) and unlikely to affect the results. Moreover, no truncation was observed in the values obtained for the 25% quartile or 75% quartile in men or women, with or without diabetes.
Unforeseen variation in the VA’s terminology for reporting race during 2000-2014 increased the number of subjects with missing data in the race-stratified analyses. A more robust 3-way race classification used black, white, and other, where “other” included all other races as well as unknown, missing, or patients who declined a response.19 Nonetheless, as the individuals with missing data comprised only 3% of the primary analysis dataset, it is unlikely that that their exclusion materially affected the results.
Conclusion
Secular weight trends for men and women with and without diabetes in the VA healthcare system show that average weight increased from 2000 to 2014. As expected, individuals with diabetes weighed more than individuals of the same sex without diabetes. Contrary to expectation, women with diabetes weighed more than men without diabetes throughout the study period. Longitudinal trends revealed varying degrees of weight gain and loss, depending upon birth cohort, with the largest increases in the youngest cohorts and the greatest decreases in the oldest cohorts. The overall prevalence of diabetes in this study was 35.6%, with a minimum prevalence of 4.1% in the 1980-1984 birth cohort and a maximum prevalence of 43.7% in the 1940-1944 birth cohort. From 2000 to 2014, BMI increased in women, and was essentially unchanged or decreased slightly in men. Similar to recent NHANES data, individuals with diabetes had markedly higher BMI than individuals without diabetes, and women with diabetes had higher BMI than men with diabetes. Longitudinally, BMI increased in the youngest cohorts and decreased in the oldest cohorts in patterns similar to those for weight change.
Of note, contemporary male veterans without diabetes are heavier, and are gaining weight more rapidly, than the male veterans without chronic diseases who participated in the Normative Aging Study at similar ages. These findings cannot be explained by selection bias, and they follow patterns across birth cohorts similar to those seen in other longitudinal studies. Given the increased risk of diabetes associated with overweight and obesity, these findings indicate that the future prevalence of diabetes in the VA population may be even higher than in 2000-2014. Accordingly, further efforts are needed to prevent weight gain in the VA population, especially among women.
Supplementary Material
Table 3.
Summary of weight statistics by year of observation, females with diabetes, primary analysis dataset
| Wt Year |
n (wt) | Mean | SD | Median | Q1 | Q3 | Min | Max |
|---|---|---|---|---|---|---|---|---|
| 2000 | 91,493 | 88.39 | 19.60 | 86.64 | 74.48 | 100.11 | 36.29 | 235.96 |
| 2001 | 125,233 | 88.70 | 19.76 | 86.82 | 74.84 | 100.56 | 36.29 | 259.19 |
| 2002 | 146,148 | 89.01 | 19.98 | 87.09 | 74.84 | 101.10 | 36.29 | 264.45 |
| 2003 | 166,959 | 89.17 | 20.28 | 87.09 | 74.84 | 101.47 | 36.29 | 236.41 |
| 2004 | 188,569 | 89.38 | 20.45 | 87.54 | 74.84 | 101.61 | 36.29 | 252.43 |
| 2005 | 203,532 | 89.77 | 20.72 | 87.54 | 75.30 | 102.06 | 36.29 | 249.48 |
| 2006 | 211,196 | 90.10 | 20.92 | 88.04 | 75.43 | 102.51 | 36.29 | 267.40 |
| 2007 | 222,541 | 90.23 | 20.85 | 88.45 | 75.66 | 102.74 | 36.29 | 270.00 |
| 2008 | 241,035 | 90.64 | 21.11 | 88.81 | 75.89 | 103.10 | 36.29 | 268.50 |
| 2009 | 260,055 | 91.13 | 21.20 | 89.13 | 76.30 | 103.87 | 36.29 | 272.00 |
| 2010 | 257,025 | 91.35 | 21.16 | 89.45 | 76.52 | 104.33 | 36.29 | 272.00 |
| 2011 | 254,308 | 91.39 | 21.11 | 89.59 | 76.66 | 104.33 | 36.29 | 264.50 |
| 2012 | 244,067 | 91.26 | 21.21 | 89.36 | 76.52 | 104.33 | 36.29 | 263.09 |
| 2013 | 231,433 | 90.96 | 21.41 | 89.09 | 76.20 | 103.91 | 36.29 | 272.16 |
| 2014 | 223,240 | 91.15 | 21.42 | 89.36 | 76.20 | 104.10 | 36.29 | 272.16 |
Weight values in kg. Max, maximum; Min, minimum; n (wt), number of weight observations; Q1, 25% quartile; Q3, 75% quartile; Wt Year, year of weight observation.
Table 4.
Summary of weight statistics by year of observation, males without diabetes, primary analysis dataset
| Wt Year |
n (wt) | Mean | SD | Median | Q1 | Q3 | Min | Max |
|---|---|---|---|---|---|---|---|---|
| 2000 | 2,511,015 | 86.16 | 16.77 | 84.37 | 74.84 | 95.26 | 36.29 | 267.44 |
| 2001 | 3,542,600 | 86.32 | 16.90 | 84.46 | 74.84 | 95.71 | 36.29 | 272.16 |
| 2002 | 4,320,137 | 86.42 | 17.07 | 84.73 | 74.84 | 95.71 | 36.29 | 272.16 |
| 2003 | 5,092,248 | 86.36 | 17.33 | 84.60 | 74.84 | 95.85 | 36.29 | 271.70 |
| 2004 | 5,701,941 | 86.27 | 17.43 | 84.37 | 74.53 | 95.85 | 36.29 | 270.75 |
| 2005 | 6,056,617 | 86.39 | 17.69 | 84.51 | 74.39 | 96.16 | 36.29 | 272.16 |
| 2006 | 6,286,166 | 86.71 | 17.98 | 84.82 | 74.57 | 96.62 | 36.29 | 272.16 |
| 2007 | 6,505,014 | 87.00 | 18.27 | 85.09 | 74.75 | 97.07 | 36.29 | 272.16 |
| 2008 | 6,899,626 | 87.42 | 18.53 | 85.37 | 74.84 | 97.52 | 36.29 | 272.16 |
| 2009 | 7,435,229 | 88.09 | 18.81 | 86.18 | 75.30 | 98.43 | 36.29 | 272.16 |
| 2010 | 7,496,083 | 88.55 | 18.98 | 86.50 | 75.71 | 99.11 | 36.29 | 272.00 |
| 2011 | 7,491,058 | 88.91 | 19.21 | 86.77 | 75.75 | 99.66 | 36.29 | 272.16 |
| 2012 | 7,027,508 | 89.12 | 19.48 | 87.00 | 75.75 | 99.79 | 36.29 | 272.00 |
| 2013 | 6,614,960 | 89.36 | 19.74 | 87.09 | 75.84 | 100.24 | 36.29 | 272.16 |
| 2014 | 6,417,009 | 89.65 | 20.06 | 87.41 | 75.93 | 100.70 | 36.29 | 272.16 |
Weight values in kg. Max, maximum; Min, minimum; n (wt), number of weight observations; Q1, 25% quartile; Q3, 75% quartile; Wt Year, year of weight observation.
Study Importance Questions
What is already known about this subject?
Weight gain is a risk factor for many chronic diseases.
Limited data are available on weight trends and diabetes prevalence in contemporary veterans.
What does this study add?
This is the first detailed report on trends in body weight in a large, contemporary veteran population including both men and women.
Body weight and BMI is generally increasing in contemporary veterans, with higher rates of increase in among the youngest veterans, and decreasing weight in the oldest veterans.
Diabetes prevalence is highest among veterans born in the middle of the 20th century, with lower prevalence among younger veterans; regardless of diabetes status, the tendency to gain weight over time, and to be heavier at a younger age, was higher in women than in men.
Acknowledgements
The authors thank Christine Jasien, Atlanta VA Medical Center, who assisted with VINCI data. The contents of this manuscript do not represent the views of the Department of Veterans Affairs, the United States Government, or the Institute of Medical and Nursing Education. This research was performed in partial fulfillment of the requirements for a master’s degree from the Georgia State University School of Public Health. Portions of this paper were previously presented as a poster (192-LB) at the American Diabetes Association 76th Scientific Sessions, June 10-14, 2016, New Orleans, Louisiana.
FUNDING: This material is based upon work supported in part by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences Research and Development.
Footnotes
DISCLOSURES:
Ms. Tamas reports grants from Eli Lilly and Company, grants from Novo Nordisk, Inc., grants from Takeda Pharmaceuticals, Inc., grants from Sanofi US, grants from Boehringer-Ingelheim, grants from AstraZeneca Pharmaceuticals LP, and grants from Merck & Co., Inc, outside the submitted work. Dr. Khakharia has nothing to disclose. Dr. Rothenberg has nothing to disclose. Dr. Phillips reports salary support from the Veterans Health Administration, during the conduct of the study; grants and personal fees from Janssen Pharmaceuticals, personal fees from Profil Institute for Clinical Research, grants from Merck, grants from Amylin, grants from Eli Lilly, grants from Novo Nordisk, grants from Sanofi, grants from PhaseBio, grants from Roche, grants from AbbVie, grants from Vascular Pharmaceuticals, grants from GlaxoSmithKline, grants from Pfizer, grants from Cystic Fibrosis Foundation, and other from DIASYST, outside the submitted work.
References
- 1.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 2015;314(10):1021–1029. [DOI] [PubMed] [Google Scholar]
- 2.Stenholm S, Vahtera J, Kawachi I, et al. Patterns of weight gain in middle-aged and older US adults, 1992–2010. Epidemiology 2015;26:165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walter S, Mejia-Guevara I, Estrada K, Liu SY, Glymour MM. Association of a genetic risk score with body mass index across different birth cohorts. JAMA 2016;316:63–69. [DOI] [PubMed] [Google Scholar]
- 4.Fryar CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity, and extreme obesity among adults: United States, 1960–1962 through 2011–2012 [Web page]. http://www.cdc.gov/nchs/data/hestat/obesity_adult_11_12/obesity_adult_11_12.pdf. Accessed March 4, 2017.
- 5.Koepsell TD, Littman AJ, Forsberg CW. Obesity, overweight, and their life course trajectories in veterans and non-veterans. Obesity (Silver Spring). 2012;20:434–439. [DOI] [PubMed] [Google Scholar]
- 6.Grinker JA, Tucker K, Vokonas PS, Rush D. Body habitus changes among adult males from the Normative Aging Study: relations to aging, smoking history and alcohol intake. Obes Res 1995;3:435–446. [DOI] [PubMed] [Google Scholar]
- 7.Rush T, LeardMann CA, Crum-Cianflone NF. Obesity and associated adverse health outcomes among US military members and veterans: findings from the Millennium Cohort Study. Obesity (Silver Spring) 2016;24:1582–1589. [DOI] [PubMed] [Google Scholar]
- 8.Olson DE, Zhu M, Long Q, et al. Increased cardiovascular disease, resource use, and costs before the clinical diagnosis of diabetes in veterans in the southeastern U.S. J Gen Intern Med 2015;30:749–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson SL, Long Q, Rhee MK, et al. Weight loss and incidence of diabetes with the Veterans Health Administration MOVE! lifestyle change programme: an observational study. Lancet Diabetes Endocrinol 2015;3:173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(suppl 2):B10–B21. [DOI] [PubMed] [Google Scholar]
- 11.Morgan CL, Jenkins-Jones S, Evans M, Barnett AH, Poole CD, Currie CJ. Weight change in people with type 2 diabetes: secular trends and the impact of alternative antihyperglycaemic drugs. Diabetes Obes Metab 2012;14:424–432. [DOI] [PubMed] [Google Scholar]
- 12.Murphy RA, Patel KV, Kritchevsky SB, Houston DK, Newman AB, Koster A, Simonsick EM, Tylvasky FA, Cawthon PM, Harris TB. Weight change, body composition, and risk of mobility disability and mortality in older adults: a population-based cohort study. J Am Geriatr Soc 2014;62:1476–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun X, Du T. Trends in cardiovascular risk factors among U.S. men and women with and without diabetes, 1988–2014. BMC Public Health. 2017;17:893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Z, Liu M. Life years lost associated with diabetes: An individually matched cohort study using the U.S. National Health Interview Survey data. Diabetes Res Clin Pract 2016;118:69–76. [DOI] [PubMed] [Google Scholar]
- 16.Gregg EW, Lin J, Bardenheier B, Chen H, Rejeski WJ, Zhuo X, Hergenroeder AL, Kritchevsky SB, Peters AL, Wagenknecht LE, Ip EH, Espeland MA; Look AHEAD Study Group. Impact of Intensive Lifestyle Intervention on Disability-Free Life Expectancy: The Look AHEAD Study. Diabetes Care. 2018;41:1040–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sirmans SM, Pate KA. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin Epidemiol 2013;6:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herman WH, Pan Q, Edelstein SL, Mather KJ, Perreault L, Barrett-Connor E, Dabelea DM, Horton E, Kahn SE, Knowler WC, Lorenzo C, Pi-Sunyer X, Venditti E, Ye W; Diabetes Prevention Program Research Group. Impact of lifestyle and metformin interventions on the risk of progression to diabetes and regression to normal glucose regulation in overweight or obese people with impaired glucose regulation. Diabetes Care. 2017;40:1668–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gebregziabher M, Lynch CP, Mueller M, et al. Using quantile regression to investigate racial disparities in medication non-adherence. BMC Med Res Methodol 2011;11:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.