Key Points
Questions
Does an internet-based depression prevention program (competent adulthood transition with cognitive behavioral humanistic and interpersonal training) lower the hazard for depression in at-risk adolescents relative to health education attention control?
Findings
In this randomized clinical trial of adolescents with subsyndromal depression or history of depression randomized to receive internet-based behavioral humanistic interpersonal training or an internet-based general health education control, those who received the CATCH-IT intervention did not evidence fewer episodes of depression in the full intention-to-treat sample, but adolescents with subsyndromal depression may have experienced fewer depressive episodes.
Meaning
Competent adulthood transition with cognitive behavioral humanistic and interpersonal training may be better than health education for preventing depression in adolescents with subsyndromal depression.
Abstract
Importance
Although 13% to 20% of American adolescents experience a depressive episode annually, no scalable primary care model for adolescent depression prevention is currently available.
Objective
To study whether competent adulthood transition with cognitive behavioral humanistic and interpersonal training (CATCH-IT) lowers the hazard for depression in at-risk adolescents identified in primary care, as compared with a general health education (HE) attention control.
Design, Setting, and Participants
This multicenter, randomized clinical trial, a phase 3 single-blind study, compares CATCH-IT with HE. Participants were enrolled from 2012 to 2016 and assessed at 2, 6, 12, 18, and 24 months postrandomization in a primary care setting. Eligible adolescents were aged 13 to 18 years with subsyndromal depression and/or history of depression and no current depression diagnosis or treatment. Of 2250 adolescents screened for eligibility, 446 participants completed the baseline interview, and 369 were randomized into CATCH-IT (n = 193) and HE (n = 176).
Interventions
The internet-based intervention, CATCH-IT, is a 20-module (15 adolescent modules and 5 parent modules) online psychoeducation course that includes a parent program, supported by 3 motivational interviews.
Main Outcomes and Measures
Time to event for depressive episode; depressive symptoms at 6 months.
Results
Of 369 participants (mean [SD] age, 15.4 [1.5] years; 251 women [68%]) included in this trial, 193 were randomized into CATCH-IT and 176 into HE. Among these participants, 28% had both a past episode and subsyndromal depression; 12% had a past episode only, 59% had subsyndromal depression only, and 1% had borderline subsyndromal depression. The outcome of time to event favored CATCH-IT but was not significant with intention-to-treat analyses (unadjusted hazard ratio [HR], 0.59; 95% CI, 0.27-1.29; P = .18; adjusted HR, 0.53; 95% CI, 0.23-1.23; P = .14). Adolescents with higher baseline Center for Epidemiologic Studies Depression scale (CES-D10) scores showed a significantly stronger effect of CATCH-IT on time to event relative to those with lower baseline scores (HR 0.82; 95% CI, 0.67-0.99; P = .04). For example, the hazard ratio for a CES-D10 score of 15 was 0.20 (95% CI, 0.05-0.77), compared with a hazard ratio of 1.44 (95% CI, 0.41-5.03) for a CES-D10 score of 5. In both CATCH-IT and HE groups, depression symptoms declined and functional scores increased.
Conclusions and Relevance
For preventing depressive episodes CATCH-IT may be better than HE for at-risk adolescents with subsyndromal depression. Also CATCH-IT may be a scalable approach to prevent depressive episodes in adolescents in primary care.
Trial Registration
ClinicalTrials.gov Identifier: NCT01893749
This randomized clinical trial evaluates the effect of cognitive behavioral humanistic and interpersonal training vs a general health education attention control on the risk of depression in at-risk adolescents identified in primary care.
Introduction
Approximately 13% to 20% of adolescents experience minor depressive episodes (mDE) or major depressive episodes (MDE) annually.1 These adolescents have a higher incidence of medical illness2 than those without mDE and MDE, and are at higher risk for suicide and recurrent depression.3,4,5 Effective depression prevention programs are essential.6
Promising findings for depression prevention programs are available. A Cochrane meta-analysis of prevention trials favored the intervention group over the control group with an overall risk difference for depressive disorders of −0.03, and for depression symptoms a standard mean difference of −0.21.7 A review noted a 22% risk reduction of depressive episodes for adolescents.7,8 Another meta-analysis involving 19 randomized preventive trials demonstrated significant reduction in depressive symptoms over 2 years among adolescents with higher symptom levels.9 Another review of traditional therapies augmented with computerized communications demonstrated small-to-moderate effect sizes for depressive symptoms.10 A systematic review of primary care-based preventative interventions targeting depression identified 14 randomized clinical trials; only 1 included adolescents, and average effect sizes were small.11 Targeted interventions that show success during trials may not be scalable owing to practical issues such as cost, or prove ineffective in the broader community.12
The primary care internet-based intervention, competent adulthood transition with cognitive behavioral humanistic and interpersonal training (CATCH-IT) addresses the need for a scalable intervention.13,14,15,16 Internet-based interventions are accessible, cost-effective, private, and acceptable because they reduce stigma.12 The CATCH-IT intervention is simple, consumer friendly, and more easily scaled up than more intensive, face-to-face interventions. A randomized clinical trial in China found that CATCH-IT lowered depressive symptoms in adolescents over 12 months.17
We present a multisite randomized clinical trial testing the efficacy of CATCH-IT (version 3) vs an internet-based health education (HE) attention control in primary care. We aimed to prevent the onset of depressive episodes and lower symptoms in adolescents at intermediate-to-high risk for depression. Our primary hypothesis was that adolescents assigned to CATCH-IT relative to HE would have a lower hazard ratio (HR) for mDE or MDE at 6 months. We chose to evaluate group differences at 6 months to examine the potential of CATCH-IT as an immediate, medium-term response to depressive symptoms, given that follow-up intervals for such interventions in adolescents generally range from less than 6 to 12 months.12 We also hypothesize that adolescents in CATCH-IT would show improvement in depressed mood and functional status relative to HE.18
Methods
Study Design and Setting
We conducted a hybrid type 1 effectiveness-implementation trial to test the efficacy of CATCH-IT in a scalable setting and collected information regarding implementation.19 This 2-site (Chicago, Illinois, and Boston, Massachusetts) randomized trial compared CATCH-IT vs HE for preventing depressive episode onset in an intermediate- to high-risk sample of adolescents in primary care. We defined risk status as teens’ current elevated symptoms of depression, history of depressive episode, or both. Depressive episodes are defined as a Depression Severity Rating (DSR) of 3 or more (exhibiting symptoms of subthreshold MDE). At baseline, the participants’ average Center for Epidemiologic Studies Depression scale (CES-D20) score was 16.9. Twelve percent of the sample enrolled with a past MDE only, 60% had current elevated symptoms only, and 28% had both a past MDE and elevated symptoms of depression. Participants were assessed at baseline and at 2 and 6 months postenrollment. Dates of depressive episodes were recorded. Depressive episodes were diagnosed through the use of Kiddie Schedule for Affective Disorders scale (K-SADS) interviews.
Institutional review board approval was received from the central site, University of Illinois at Chicago, and local institutional review boards (IRB of Record, Wellesley College, Advocate Healthcare, Franciscan Alliance, Northshore University Health Systems, Northwestern, and Access Healthcare).20 Participants were recruited from 2012 to 2016 through a description of the study during doctor visits, recruitment letters, and posted flyers. Adolescents were screened for risk in-person or by phone. After parental consent, adolescents participated in an eligibility assessment by phone. The parent and adolescent attended an enrollment assessment at their primary care office, when written informed consent from parents and assent from adolescents were obtained, and assessments were administered to confirm eligibility.21 This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline. The protocol, implementation process, and methods have been described in Supplement 1 and elsewhere.18 The study was conducted in clinics in Chicago, northern Indiana, and Boston.
Inclusion and Exclusion Criteria
Adolescents aged 13 to 18 years with elevated levels of depressive symptoms on the CES-D22 (scores 8-17 on the CES-D10 or scores ≥16 on the CES-D20) at screening or at baseline, and/or a history of depression or dysthymia,22,23,24 were eligible. Exclusion criteria included the following: current MDE diagnosis or treatment; past cognitive behavioral therapy; CES-D10 scores of more than 1722; schizophrenia, psychosis, or bipolar disorder; serious medical condition (ie, causing serious disability or dysfunction); significant reading impairment or developmental disability; imminent suicidal risk; and current drug or alcohol abuse.25,26 Criteria were selected to avoid confounding factors in depression etiology or treatment, consistent with the use of CATCH-IT as a preventive intervention.
Randomization
Participants were assigned randomly to CATCH-IT or HE (1:1 allocation) using a computer generated sequence blocked by site and time of entry (random blocks of size 4 and 6), stratified by risk severity (based on CES-D score, prior MDE, or dysthymia), sex and age (13-14 years or 15-18 years).26,27
Blinding
Randomization was concealed from investigators, clinicians, patients, and families until the baseline consent, enrollment, data collection, and assessment were completed. Study participants could not be blinded to their arm assignment. The health care professional was also not blinded, as he or she was expected to conduct 3 motivational interviews (MIs) for CATCH-IT participants. Assessors remained blinded throughout the study. Principal investigators (B.W.V.V. and T.R.G.G.) were blinded to between-group comparisons and group descriptive data until all 6-month follow-up data were collected.
Retention
Challenges related to ongoing study participation were addressed by research staff. Approaches used to maintain contact were birthday cards and regular contact updates.
Outcomes
Occurrence of first depressive episode was determined by the DSR. A score indicating at least subthreshold major depression (a DSR of ≥3) was considered to be a depressive episode. To test for robustness of findings, we also examined data using a DSR cutoff of 4 or more, indicating probable MDE, and a DSR of 5, indicating the presence of MDE.28 Symptom outcomes include the CES-D1022 and Global Assessment Scale (GAS) scores.
CATCH-IT Intervention
The CATCH-IT intervention includes an internet component (15 adolescent modules, based primarily on the Coping with Depression Adolescent Course,29 behavioral activation,30 and interpersonal psychotherapy),31 a brief motivational component (3 physician MIs at 0, 2, and 12 months), and 1 to 3 staff coaching phone calls either at 1 month (Chicago) or at 2 and 4 weeks (Boston), and 18 months. There were also up to 3 check-in calls during weeks 1 through 3 to facilitate website use. The parent internet intervention component (5 modules) is based on an adaptation of the Preventive Intervention Project.32 A description of the intervention has been published.18,33
HE Intervention
The HE intervention is an attention control internet site (14 modules) providing instruction on general health topics. The 14th module discusses mood and mental health treatment, and also addresses mental disorder stigma.14,34 Up to 3 check-in calls (weeks 1-3) were offered to ensure website access. The caregiver internet program (4 modules) is similar.
Intervention Shared Elements
Both interventions were consistent with guidelines for adolescent depression in primary care including the following: training clinicians in depression identification, diagnosis, and treatment; establishing referral relationships; screening; using a formal tool to determine depression risk; assessing depression; interviewing caregivers and adolescents; educating caregivers and adolescents on treatment; establishing treatment plans; and establishing safety plans.35 These steps are closely related to the Chronic Care Model.36 Rates of episodes were extremely low for this high-risk sample. When episodes were identified, adolescents were referred for treatment, and caregivers and pediatricians were notified.
Instruments
Instruments have been described previously.18 The 2-question screener was based on the Patient Health Questionnaire for adolescents.37,38 The K-SADS39,40 is a semistructured interview assessing current and lifetime psychiatric diagnoses in participants aged younger than 18 years, administered to parents and adolescents.39,41 The DSRs are obtained from the Kiddie Longitudinal Interval Follow-up Evaluation41 for each week of the follow-up interval, and GAS ratings were assigned at each assessment. For both the K-SADS and the Kiddie Longitudinal Interval Follow-up Evaluation, precipitating events were reviewed, and episodes secondary to medical concerns were indicated, if they occurred. The CES-D10 measures the frequency of 10 depressive symptoms over the past week, using a 4-point scale; it was completed at baseline, 2, and 6 months.22 Demographic information was collected at baseline, including race and ethnicity, using categories defined by the study team. Fidelity and exposure to the intervention were based on module completion, and completion and rating of the MIs, with 2 trained raters using the MI Treatment Integrity coding manual (version 4.2.1),42 and number of characters typed into the CATCH-IT website.
Sample Size
We required 200 participants per intervention condition to achieve 80% power based on a conservative application of our pilot study findings.40 These calculations assumed that in the control group 72% are free from depression after 1-year follow-up, and the second year continues to follow the same exponential rate for controls; for intervention, the hazard is a constant ratio of 0.62, and an attrition rate of 7% for each of the first 4 quarters, and 2% for each of the second 4 quarters (Trial Protocol in Supplement 1).
Statistical Analysis
The trial tested for differences between group medians in website engagement using Wilcoxon rank sum tests. We estimated incidence rates by calculating the number of depressive episodes per 10 000 person-weeks of follow-up. Kaplan-Meier curves were used to estimate the time to first episode distribution for each intervention under 6 different treatment allocations (eTable 1 in Supplement 2). Treatment allocations were developed based on existent literature with regard to threshold effects of adherence as an a priori analytic strategy. The thresholds were applied in the same manner with both interventions with similar numbers of persons identified in each arm. Cox proportional hazard regression was used to estimate the HR comparing CATCH-IT with HE. We present adjusted (sex, ethnicity [Hispanic/nonHispanic], race [white/nonwhite], baseline age, site, and baseline CES-D10 score) and unadjusted HRs. The assumption of proportional hazards was checked by testing the independence between the Schoenfeld residuals and time.43 The trial examined moderating effects of baseline adolescent CES-D10 score as a continuous variable, exhibited across a range of possible CES-D10 values, by including interaction terms in the Cox models. We used linear mixed-effect growth models with random intercepts and slopes to examine differences between group change over time in CES-D10 and GAS. Analyses were adjusted for the covariates listed above. We used propensity scores to account for differences between treatment groups in the per protocol analysis (≥2 modules completed) that could otherwise confound treatment effect estimates controlling for: site, age, sex, ethnicity, race, mother’s education, parents’ marital status, number of siblings, firstborn child, times moved, current GAS score, most severe past GAS score, highest past GAS score, and baseline CES-D10. Analyses were conducted using R statistical software, version 3.3.1 (R Foundation Inc), SAS, version 9.4 (SAS Institute), and Mplus, version 8 (Muthén & Muthén).
Missing Data
The percentages of participants missing each K-SADS or CES-D10 assessment were calculated. We used a logistic regression model to determine whether those missing from follow-up differed from those who were not. We also used multiple imputation to assess the potential for differential follow-up by intervention condition. We constructed 50 data sets for each site and intervention condition with fully saturated specification by condition interacting with the following variables: all CES-D10 and GAS values (0, 2, and 6 months), screening CES-D10, baseline age, sex, ethnicity, race, and maternal education. These were combined into 50 complete imputed data sets and analyzed separately using the growth models described above; results were pooled.
Results
Implementation
We implemented the study in 8 health systems from 31 practices in a defined population of more than 41 000 adolescents. There were 8499 adolescents screened, 2250 phone assessments, 446 enrolled, and 369 randomized. The 2 groups consisted of CATCH-IT (n = 193) and HE (n = 176) (Figure 1). Among these participants, 28% had both a past episode and subsyndromal depression; 12% had a past episode only, 59% had subsyndromal depression only, and 1% had borderline subsyndromal depression
Figure 1. Consort Diagram.
CATCH-IT indicates competent adulthood transition with cognitive behavioral humanistic and interpersonal training; CES-D10, Center for Epidemiologic Studies Depression scale; GAS, Global Assessment Scale; MI, motivational interview.
Sample
Participants were aged 13 to 18 years (mean [SD] age, 15.4 [1.5] years; 251 women [68%]) with history of depression and/or current subsyndromal depressive symptoms. Participants were diverse in self-reported race and ethnicity: 21% Hispanic, 26% non-Hispanic black, 43% non-Hispanic white, 4% Asian, and 6% multiracial or other. Sixty-one percent had married parents, and 53% of the fathers were college graduates. Adolescents were moderately depressed (CES-D10: mean [SD], 9.4 [4.6]), moderately impaired (GAS: mean [SD], 78.1 [9.4%]), had a prior DSR of 3 or more (226 [62%]), and had a prior DSR of 4 or more (144 [40%]) (Table 1).
Table 1. Participant Characteristics at Baseline.
| Characteristic | All (N = 369) | CATCH-IT (n = 193) | Health Education (n = 176) | |||
|---|---|---|---|---|---|---|
| No. | No. (%) | No. | No. (%) | No. | No. (%) | |
| Age, mean (SD), y | 369 | 15.4 (1.5) | 193 | 15.4 (1.5) | 176 | 15.5 (1.5) |
| Sex | 369 | 193 | 176 | |||
| Male | 118 (32) | 59 (31) | 59 (34) | |||
| Female | 251 (68) | 134 (69) | 117 (66) | |||
| Ethnicity | 369 | 193 | 176 | |||
| Hispanic | 77 (21) | 41 (21) | 36 (20) | |||
| Non-Hispanica | 292 (79) | 152 (79) | 140 (80) | |||
| Race | 369 | 193 | 176 | |||
| White | 201 (54) | 107 (55) | 94 (53) | |||
| Nonwhiteb | 168 (46) | 86 (45) | 82 (47) | |||
| Mother’s education | 359 | 188 | 171 | |||
| Some high school | 12 (3) | 5 (3) | 7 (4) | |||
| High school graduate/GED | 45 (13) | 20 (11) | 25 (15) | |||
| Some college | 87 (24) | 44 (23) | 43 (25) | |||
| College graduate | 215 (60) | 119 (63) | 96 (56) | |||
| Father’s education | 336 | 177 | 159 | |||
| Some high school | 26 (8) | 12 (7) | 14 (9) | |||
| High school graduate/GED | 76 (23) | 36 (20) | 40 (25) | |||
| Some college | 55 (16) | 37 (21) | 18 (11) | |||
| College graduate | 179 (53) | 92 (52) | 87 (55) | |||
| K-SADS | ||||||
| GAS, mean (SD)c | ||||||
| Current | 367 | 78.1 (9.4) | 193 | 78.3 (9.3) | 174 | 78.0 (9.6) |
| Most severe past | 359 | 67.5 (10.9) | 189 | 68.1 (10.3) | 170 | 67.0 (11.5) |
| Highest past | 360 | 82.2 (8.5) | 190 | 82.3 (8.4) | 170 | 82.1 (8.5) |
| DSR, mean (SD)d | ||||||
| Most severe | 364 | 3.1 (1.4) | 189 | 3.1 (1.4) | 175 | 3.2 (1.4) |
| ≥3 | 226 (62) | 113 (60) | 113 (65) | |||
| ≥4 | 144 (40) | 75 (40) | 69 (39) | |||
| Current | 365 | 1.8 (0.9) | 190 | 1.7 (0.9) | 175 | 1.8 (0.9) |
| CES-D20, mean (SD)e | 362 | 16.9 (8.7) | 190 | 17.3 (8.7) | 172 | 16.5 (8.8) |
| CES-D10, mean (SD)f | 362 | 9.4 (4.6) | 190 | 9.5 (4.5) | 172 | 9.4 (4.6) |
| SCARED total score, mean (SD)g | 312 | 25.3 (12.3) | 171 | 25.5 (12.7) | 141 | 25.2 (11.9) |
Abbreviations: CATCH-IT, Competent Adulthood Transition with Cognitive Behavioral Humanistic and Interpersonal Training; CES-D, Center for Epidemiologic Studies Depression scale; DSR, Depression Severity Rating; GAS, Global Assessment Scale; GED, general equivalency diploma; K-SADS, Kiddie Schedule for Affective Disorders scale; SCARED, screen for child and anxiety related disorders.
Participants with missing ethnicity data were coded as non-Hispanic (n = 6).
Participants with missing race data were coded as nonwhite (n = 20; most identified as Hispanic).
Possible range: 1 to 100; a higher score indicates higher functioning.
Possible range: 1 to 6; a higher score indicates more severe depression.
Possible range: 0 to 60; a higher score indicates more severe depression.
Possible range: 0 to 30; a higher score indicates more severe depression.
Possible range: 0 to 82; a higher score indicates greater anxiety.
Fidelity and Intervention Exposure
Intervention use was monitored and recorded. The number of MIs completed was recorded for CATCH-IT participants. Table 2 shows that CATCH-IT adolescents and parents spent more time using the intervention, but CATCH-IT adolescents completed fewer modules than HE adolescents (modules completed: median [interquartile range], 1.0 [4.0] vs 4.0 [14.0], respectively; P = .003). Both study arms received a sizable dose of the interventions, with the combined (parent + adolescent) module completion greater for HE (modules completed: median [interquartile range], 4.0 [8.0] vs 8.0 [17.0], respectively; P < .001). Adolescents and parents included in CATCH-IT typed a mean (SD) of 3071 (4572) and 716 (977) characters, respectively (Table 2). Over 73% of MIs and phone calls were completed. Mean (SD) interview length was 7.7 (4.0) minutes, mean (SD) technical global rating was 3.0 (0.5) on a 1 to 5 scale, and mean (SD) relational global rating was 2.9 (0.6) (eTable 2 in Supplement 2).
Table 2. Fidelity Assessment of Internet Component.
| Website Use | Mean (SD) | Difference CATCH-IT and Health Education, Mean (95% CI) | Median (IQR) | P Valuea | ||
|---|---|---|---|---|---|---|
| CATCH-IT | Health Education | CATCH-IT | Health Education | |||
| Adolescents | ||||||
| No. | 193 | 176 | ||||
| Modules completed, No. | 3.4 (4.7) | 6.8 (6.5) | −3.4 (−4.5 to −2.2) | 1.0 (4.0) | 4.0 (14.0) | .003 |
| Total time on site, min | 100.2 (143.1) | 22.8 (31.0) | 77.4 (55.7 to 99.0) | 39.6 (149.2) | 8.4 (35.1) | <.001 |
| Days visited site | 3.7 (4.5) | 1.4 (1.6) | 2.3 (1.6 to 3.0) | 2.0 (4.0) | 1.0 (2.0) | <.001 |
| Total characters typed, No. | 3071 (4572) | NA | NA | 923 (4469) | NA | NA |
| Adolescents and parents | ||||||
| Modules completed, No. | 5.3 (5.8) | 8.8 (7.3) | −3.5 (−4.8 to −2.1) | 4.0 (8.0) | 8.0 (17.0) | <.001 |
| Total time on site, min | 130.6 (157.9) | 30.6 (35.6) | 100.0 (76.1 to 124.0) | 75.8 (192.2) | 18.9 (40.8) | <.001 |
| Days visited site | 5.2 (5.2) | 2.2 (2.2) | 2.9 (2.1 to 3.8) | 4.0 (6.0) | 2.0 (2.0) | <.001 |
| Total characters typed, No. | 3713 (4932) | NA | NA | 1899 (5792) | NA | NA |
| Parents | ||||||
| No. | 165 | 157 | ||||
| Modules completed, No. | 2.1 (2.0) | 2.2 (1.9) | −0.1 (−0.6 to 0.3) | 2.0 (4.0) | 4.0 (4.0) | .80 |
| Total time on site, min | 32.6 (37.3) | 8.6 (10.0) | 24.0 (17.9 to 30.0) | 22.4 (51.9) | 5.6 (14.9) | <.001 |
| Days visited site | 1.6 (1.6) | 0.9 (1.1) | 0.6 (0.3 to 0.9) | 1.0 (2.0) | 1.0 (1.0) | <.001 |
| Total characters typed, No. | 716 (977) | NA | NA | 101 (1205) | NA | NA |
Abbrevations: CATCH-IT, Competent Adulthood Transition with Cognitive Behavioral Humanistic and Interpersonal Training; IQR, interquartile range; NA, not available.
Medians compared using Wilcoxon rank-sum test.
Outcomes
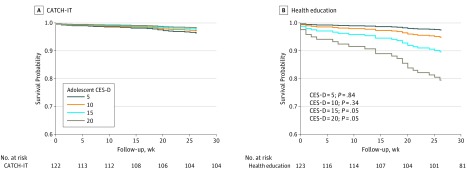
For the primary outcome of time-to-depressive episode (DSR ≥3) using intention-to-treat analyses (N = 369), unadjusted HR was 0.59 (95% CI, 0.27-1.29; P = .18), and adjusted HR was 0.53 (95% CI 0.23-1.23, P = .14). Proportional hazards assumption was met (P = .89). For per protocol analysis (≥2 modules completed on either arm, n = 245) (Figure 2), unadjusted HR was 0.41 (95% CI, 0.17-0.99; P = .05), and adjusted HR was 0.44 (95% CI, 0.18-1.08; P = .07). After adjusting for potential confounders using propensity scores, HR was 0.52 (95% CI, 0.19, 1.42; P = .20). Additional analyses are shown in eTable 3 in Supplement 2, and incidence rates in eTable 4 in Supplement 2. The trial calculated the number needed to treat to indicate the number of adolescents who would need to receive the intervention to prevent 1 additional onset of depressive disorder and found a number needed to treat of 36 for the main effect of CATCH-IT. Adolescents with higher baseline CES-D10 scores showed a significantly stronger effect of CATCH-IT on time to event relative to those with lower baseline scores (HR, 0.82; 95% CI, 0.67-0.99; P = .04) (Figure 3; eTable 5 in Supplement 2). For example, the hazard ratio for a CES-D10 score of 15 was 0.20 (95% CI, 0.05-0.77), compared with a hazard ratio of 1.44 (95% CI, 0.41-5.03) for a CES-D10 score of 5. Sex, ethnicity, race, and age did not predict outcome or interact significantly with the interventions and outcomes. Both CATCH-IT and HE demonstrated reduced depressed mood and improved functional status, with no statistically significant differences at 6 months (eTables 6 and 7 in Supplement 2).
Figure 2. Time to First Depressive Episode for Those Completing 2 or More Modules (Per-Protocol 2 Analysis).
CATCH-IT indicates competent adulthood transition with cognitive behavioral humanistic and interpersonal training.
Figure 3. First Depressive Episode Survival Analysis by Adolescent Baseline CES-D Scores.
CATCH-IT indicates competent adulthood transition with cognitive behavioral humanistic and interpersonal training; and CES-D, Center for Epidemiologic Studies Depression scale.
Missing Data
At least 1 follow-up K-SADS was completed for 85% of the sample, at least 1 follow-up CES-D10 was completed for 80% of the sample, and at least 1 follow-up GAS assessment was completed for 81% of the sample. Dropout between CATCH-IT and HE was different at 2 and 6 months for both K-SADS and CES-D10 (eTable 8A in Supplement 2). At 6 months, K-SADS data were missing for 48 participants (25%) of CATCH-IT and 23 participants (13%) of HE (P = .004), and CES-D10 was missing for 77 participants (40%) of CATCH-IT and 43 participants (24%) of HE (P = .002). Significant predictors of missing K-SADS at 6 months were randomization to CATCH-IT (CATCH-IT vs HE: odds ratio [OR], 2.62; 95% CI, 1.43-4.79; P = .002), living in Chicago (Boston vs Chicago: OR, 0.20; 95% CI, 0.09-0.46; P < .001), age at baseline (OR, 1.23; 95% CI, 1.02-1.49; P = .03), and maternal education (high school graduate or less vs college graduate: OR, 2.99; 95% CI, 1.37-6.53; P = .01) (eTable 8C in Supplement 2). Having a past episode or high CES-D10 at baseline was not associated with missing follow-up.
Discussion
Overall, we observed a nonsignificant decrease in depressive disorders at 6 months in CATCH-IT as compared with HE. Adolescents and parents devoted substantial time to both interventions, and both conditions experienced decreased depressive symptoms and improved functional status. However, higher-risk adolescents demonstrated greater benefit from CATCH-IT, achieving as much as 80% risk reduction with a CES-D10 score of more than 15, but those without symptoms showed no such benefit. While regression to the mean is a possible explanation for the moderating effect of high CES-D on CATCH-IT, other studies have found that preventive effects for depression interventions are stronger for indicated vs universal samples.44 Moreover, the same effect did not emerge for the HE condition—higher CES-D scores did not moderate the effect of the HE condition—suggesting regression to the mean may not explain the group difference found. For the 66% of adolescent and parent pairs who completed at least 2 modules (63% for CATCH-IT and 70% for HE), the unadjusted analysis showed CATCH-IT reduced the risk of mDE and MDE by 59%, but this was not significant after adjustment for demographic factors or after analyses incorporating propensity scoring.
To our knowledge, this is the first clinical trial in adolescents to evaluate whether depressive episodes can be prevented in primary care settings.11 Our finding that the risk of depressive episodes may be reduced for adolescents with subsyndromal depression is consistent with our earlier phase 2 clinical trial, which only included adolescents with subsyndromal depression.45 Results were not significant in the intention-to-treat main effect analysis, but this may be the result of heterogeneity of treatment effect whereby CATCH-IT is favored for those with subsyndromal depression, but not for those with prior depressive episode alone. Perhaps CATCH-IT bored or frustrated adolescents without current symptoms, or conversely, elicited increased surveillance of symptoms or stimulated memories of prior episodes.46,47 Alternatively, adolescents who are not symptomatic may be less motivated to complete CATCH-IT, the more self-directed intervention, and may actually prefer HE, which did not require substantial effort, perhaps even gaining a sense of self-efficacy.34,46,47,48,49 Also, despite spending substantial time engaged with this intervention, the low number of modules completed may have attenuated impact. Additionally, the borderline significant findings favoring CATCH-IT with the completion of 2 modules (eTable 3 in Supplement 2) suggest that there may also be a threshold effect whereby sufficient numbers of modules may need to be completed for CATCH-IT to be more efficacious than HE.
Depression prevention programs have shown mixed results.12 The only other primary care trial with adolescents demonstrated improvements in explanatory style but not depressed mood.50 Our findings showing that increased participation may predict better outcomes are consistent with prior reports.50,51 The observed risk reduction across multiple outcomes (DSR ≥3, ≥4, and 5; eTable 3 in Supplement 2), even if not statistically significant, is comparable with other trials.7,8,28 While most internet interventions demonstrate favorable changes in depressed mood, this study did not demonstrate between group differences for mood or functional status.10 However, this is similar to the phase 2 clinical trial of CATCH-IT, which demonstrated lower cumulative prevalence of depressive episodes, but not between group differences in depressed mood.38 It is possible the extensive human contact within this trial had an ameliorating effect on mood and strengthened functional status, effectively blurring between group results. A clinical trial of CATCH-IT in Hong Kong that only used self-report instruments demonstrated a significant between group effect (effect size = 0.36) for depressed mood at 12 months.17
This study has a robust prevention design implemented in a population-based model in primary care.52,53 The implementation of our study at 2 sites and 8 health systems has rarely been accomplished in studies of child psychiatric conditions.20 This study fits the model by Curran et al19 of hybrid efficacy and implementation studies and substantially enhances generalizability. The attention control condition, which included guidelines for adolescent depression in primary care and chronic care model elements, no doubt reduced between-group differences.24,36 However, given the need for ethical care of adolescents at risk for depressive episodes, a “no intervention” or “wait list control” condition is not possible.53,54
Limitations
This study had limitations, including the relatively low adherence rate of teens and parents. Module completion for CATCH-IT was consistent with pilot findings. A review of internet-based mental health interventions for youths revealed completion ranged from 24% to 85%, and it was not necessary to complete the entire intervention for positive benefits to emerge.12 In addition, module completion does not correlate with time spent, as the HE modules are significantly shorter than CATCH-IT; overall, CATCH-IT participants spent more time using the intervention. Nevertheless, future research should examine why adolescents did not complete the interventions, and explore strategies for boosting adherence. Also, our incidence rate for depressive disorders was low, thus, increasing the number of participants needed to have adequate power to detect group differences. We do not know for certain whether intervention effects can be attributed to the internet-based modules or to the MIs, although results from our pilot study suggest that adolescents who did not get MIs still evidenced reduced symptoms of depression at follow-up. Other limitations include the findings of differential attrition, which were adjusted analytically, and the fact that researchers enrolled only 92% of the target sample.
Conclusions
Our long-term goal for the CATCH-IT intervention is to provide a first-line program for primary care physicians to offer as part of the guidelines for adolescent depression in primary care, to support adolescents while the need for further intervention can be evaluated. We continue to examine moderators that may explain who responds best to this approach. Future directions include the development of versions for personal devices (eg, tablets and mobile phones), and a version individualized for sexual- and gender-minority teens.
A scalable, population-based approach to preventing depression in adolescents in primary care may be efficacious for adolescents with subsyndromal depression, but not for those with a prior episode alone.
Trial Protocol
eTable 1. Definition for Criteria for Main Outcomes Analyses
eTable 2. MI Fidelity: Mean MITI Summary Scores
eTable 3. Hazard Ratio Estimate and 95% CI for First Depressive Episode Comparing CATCH-IT to Health Education
eTable 4. Incidence of First Depressive Episode by Treatment Group
eTable 5. Adjusted Cox Proportional Hazard Model Results, Including Adolescent Baseline CES-D10 as a Moderator
eTable 6. Depressed Mood
eTable 7. Functional Status
eTable 8. A, Participants With Missing Data: KSADS and CES-D10. B, Predictors of Missing 2-Month Follow-up: Time to Last Assessment <2 Months. C, Predictors of Missing 6-Month Follow-up: Time to Last Assessment <6 Months. D, Predictors of Missing 2-Month CES-D10. E, Predictors of Missing 6-Month CES-D10
Data Sharing Statement
References
- 1.Medicine NRCaIo Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 2.Khalil BA, Gillham JC, Foresythe L, et al. Successful management of short gut due to vanishing gastroschisis - case report and review of the literature. Ann R Coll Surg Engl. 2010;92(5):-. doi: 10.1308/147870810X12659688852437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Georgiades K, Lewinsohn PM, Monroe SM, Seeley JR. Major depressive disorder in adolescence: the role of subthreshold symptoms. J Am Acad Child Adolesc Psychiatry. 2006;45(8):936-944. doi: 10.1097/01.chi.0000223313.25536.47 [DOI] [PubMed] [Google Scholar]
- 4.Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Olino TM. Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychol Med. 2005;35(3):353-365. doi: 10.1017/S0033291704003587 [DOI] [PubMed] [Google Scholar]
- 5.Lewinsohn PM, Rohde P, Klein DN, Seeley JR. Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. J Am Acad Child Adolesc Psychiatry. 1999;38(1):56-63. doi: 10.1097/00004583-199901000-00020 [DOI] [PubMed] [Google Scholar]
- 6.Garber J. Depression in children and adolescents: linking risk research and prevention. Am J Prev Med. 2006;31(6)(suppl 1):S104-S125. doi: 10.1016/j.amepre.2006.07.007 [DOI] [PubMed] [Google Scholar]
- 7.Merry S, McDowell H, Hetrick S, Bir J, Muller N. Psychological and/or educational interventions for the prevention of depression in children and adolescents. Cochrane Database Syst Rev. 2004;(1):CD003380. [DOI] [PubMed] [Google Scholar]
- 8.Hetrick SE, Cox GR, Witt KG, Bir JJ, Merry SN. Cognitive behavioural therapy (CBT), third-wave CBT and interpersonal therapy (IPT) based interventions for preventing depression in children and adolescents. Cochrane Database Syst Rev. 2016;(8):CD003380. doi: 10.1002/14651858.CD003380.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown CH, Brincks A, Huang S, et al. Two-year impact of prevention programs on adolescent depression: an integrative data analysis approach. Prev Sci. 2018;19(Suppl 1):74-94. doi: 10.1007/s11121-016-0737-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abuwalla Z, Clark MD, Burke B, et al. Long-term telemental health prevention interventions for youth: a rapid review. Internet Interv. 2017;11:20-29. doi: 10.1016/j.invent.2017.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conejo-Cerón S, Moreno-Peral P, Rodríguez-Morejón A, et al. Effectiveness of psychological and educational interventions to prevent depression in primary care: a systematic review and meta-analysis. Ann Fam Med. 2017;15(3):262-271. doi: 10.1370/afm.2031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merry SN. Preventing depression in adolescents: time for a new approach? JAMA Pediatr. 2013;167(11):994-995. doi: 10.1001/jamapediatrics.2013.2862 [DOI] [PubMed] [Google Scholar]
- 13.Gagne RMBL, Wager WW. Principles of Instructional Design. Fort Worth, TX: Harcourt Brace Jovanovich College Publishers; 1992. [Google Scholar]
- 14.Landback J, Prochaska M, Ellis J, et al. From prototype to product: development of a primary care/internet based depression prevention intervention for adolescents (CATCH-IT). Community Ment Health J. 2009;45(5):349-354. doi: 10.1007/s10597-009-9226-3 [DOI] [PubMed] [Google Scholar]
- 15.Van Voorhees BW, Watson N, Bridges J. Development and pilot study of a marketing strategy for primary care/internet based depression prevention intervention for adolescents (CATCH-IT). Prim Care Companion J Clin Psychiatry. 2010;12(3):pii:PCC.09m00791. doi: 10.4088/PCC.09m00791blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Voorhees BW, Ellis JM, Gollan JK, et al. Development and process evaluation of a primary care internet-based intervention to prevent depression in emerging adults. Prim Care Companion J Clin Psychiatry. 2007;9(5):346-355. doi: 10.4088/PCC.v09n0503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ip P, Chim D, Chan KL, et al. Effectiveness of a culturally attuned internet-based depression prevention program for Chinese adolescents: a randomized controlled trial. Depress Anxiety. 2016;33(12):1123-1131. doi: 10.1002/da.22554 [DOI] [PubMed] [Google Scholar]
- 18.Gladstone TG, Marko-Holguin M, Rothberg P, et al. An internet-based adolescent depression preventive intervention: study protocol for a randomized control trial. Trials. 2015;16:203. doi: 10.1186/s13063-015-0705-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217-226. doi: 10.1097/MLR.0b013e3182408812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahoney N, Gladstone T, DeFrino D, et al. Prevention of adolescent depression in primary care: barriers and relational work solutions. Calif J Health Promot. 2017;15(2):1-12. [PMC free article] [PubMed] [Google Scholar]
- 21.Van Voorhees BW, Watson N, Bridges JF, et al. Development and pilot study of a marketing strategy for primary care/internet-based depression prevention intervention for adolescents (the CATCH-IT intervention). Prim Care Companion J Clin Psychiatry. 2010;12(3):PCC.09m00791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radloff LS. The use of the Center for Epidemiologic Studies Depression scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149-166. doi: 10.1007/BF01537606 [DOI] [PubMed] [Google Scholar]
- 23.Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: age at onset, episode duration, and time to recurrence. J Am Acad Child Adolesc Psychiatry. 1994;33(6):809-818. doi: 10.1097/00004583-199407000-00006 [DOI] [PubMed] [Google Scholar]
- 24.Van Voorhees BW, Paunesku D, Gollan J, Kuwabara S, Reinecke M, Basu A. Predicting future risk of depressive episode in adolescents: the Chicago Adolescent Depression Risk Assessment (CADRA). Ann Fam Med. 2008;6(6):503-511. doi: 10.1370/afm.887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Knight JR, Shrier LA, Bravender TD, Farrell M, Vander Bilt J, Shaffer HJ. A new brief screen for adolescent substance abuse. Arch Pediatr Adolesc Med. 1999;153(6):591-596. doi: 10.1001/archpedi.153.6.591 [DOI] [PubMed] [Google Scholar]
- 26.Piantadosi S. Clinical Trials: A Methodologic Perspective. Hoboken, NJ: John Wiley & Sons; 2017. [Google Scholar]
- 27.Pastore DR, Juszczak L, Fisher MM, Friedman SB. School-based health center utilization: a survey of users and nonusers. Arch Pediatr Adolesc Med. 1998;152(8):763-767. doi: 10.1001/archpedi.152.8.763 [DOI] [PubMed] [Google Scholar]
- 28.Garber J, Clarke GN, Weersing VR, et al. Prevention of depression in at-risk adolescents: a randomized controlled trial. JAMA. 2009;301(21):2215-2224. doi: 10.1001/jama.2009.788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clarke GN. The Coping With Stress Course Adolescent: Workbook. Portland, OR: Kaiser Permanente Center for Health Research; 1994. [Google Scholar]
- 30.Jacobson NSMC, Dimdjian S. Behavioral activation treatment for depression: returning to contextual roots. Clin Psychol. 2001;8(3):255-270. [Google Scholar]
- 31.Stuart SRM. Interpersonal Psychotherapy: A Clinicians Guide. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 32.Beardslee WR, Gladstone TR, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in children at risk: evidence of parental and child change. Pediatrics. 2003;112(2):e119-e131. doi: 10.1542/peds.112.2.e119 [DOI] [PubMed] [Google Scholar]
- 33.Van Voorhees BW, Gladstone T, Cordel S, et al. Development of a technology-based behavioral vaccine to prevent adolescent depression: a health system integration model. Internet Interventions. 2015;2(3):303-313. doi: 10.1016/j.invent.2015.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Voorhees BW, Fogel J, Houston TK, Cooper LA, Wang NY, Ford DE. Beliefs and attitudes associated with the intention to not accept the diagnosis of depression among young adults. Ann Fam Med. 2005;3(1):38-46. doi: 10.1370/afm.273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zuckerbrot RACA, Jensen PS, Stein R, Laraque D. GLAD-PC Steering Group . Guidelines for adolescent depression in primary care (GLAD-PC): part I. practice preparation, identification, assessment, and initial management [published online February 26, 2018]. Pediatrics. doi: 10.1542/peds.2017-4081 [DOI] [PubMed] [Google Scholar]
- 36.Van Voorhees BW, Walters AE, Prochaska M, Quinn MT. Reducing health disparities in depressive disorders outcomes between non-Hispanic whites and ethnic minorities: a call for pragmatic strategies over the life course. Med Care Res Rev. 2007;64(5 Suppl):157S-194S. doi: 10.1177/1077558707305424 [DOI] [PubMed] [Google Scholar]
- 37.Johnson JG, Harris ES, Spitzer RL, Williams JB. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health. 2002;30(3):196-204. doi: 10.1016/S1054-139X(01)00333-0 [DOI] [PubMed] [Google Scholar]
- 38.Van Voorhees BW, Fogel J, Reinecke MA, et al. Randomized clinical trial of an internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes. J Dev Behav Pediatr. 2009;30(1):23-37. doi: 10.1097/DBP.0b013e3181966c2a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980-988. doi: 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- 40.Kaufman J, Birmaher B, Brent DA, Ryan ND, Rao U. K-SADS-PL. J Am Acad Child Adolesc Psychiatry. 2000;39(10):1208. doi: 10.1097/00004583-200010000-00002 [DOI] [PubMed] [Google Scholar]
- 41.Keller MB, Lavori PW, Friedman B, et al. The longitudinal interval follow-up evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44(6):540-548. doi: 10.1001/archpsyc.1987.01800180050009 [DOI] [PubMed] [Google Scholar]
- 42.Moyers TB, Rowell LN, Manuel JK, Ernst D, Houck JM. The Motivational Interviewing Treatment Integrity code (MITI 4): rationale, preliminary reliability and validity. J Subst Abuse Treat. 2016;65:36-42. doi: 10.1016/j.jsat.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515-526. doi: 10.1093/biomet/81.3.515 [DOI] [Google Scholar]
- 44.Horowitz JL, Garber J, Ciesla JA, Young JF, Mufson L. Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs. J Consult Clin Psychol. 2007;75(5):693-706. doi: 10.1037/0022-006X.75.5.693 [DOI] [PubMed] [Google Scholar]
- 45.Saulsberry A, Marko-Holguin M, Blomeke K, et al. Randomized clinical trial of a primary care internet-based intervention to prevent adolescent depression: one-year outcomes. J Can Acad Child Adolesc Psychiatry. 2013;22(2):106-117. [PMC free article] [PubMed] [Google Scholar]
- 46.Linares IMP. Early interventions for the prevention of PTSD in adults: a systematic literature review. Arch Clin Psychiatry (São Paulo). 2017;44(1):23-29. doi: 10.1590/0101-60830000000109 [DOI] [Google Scholar]
- 47.Iloabachie C, Wells C, Goodwin B, et al. Adolescent and parent experiences with a primary care/Internet-based depression prevention intervention (CATCH-IT). Gen Hosp Psychiatry. 2011;33(6):543-555. doi: 10.1016/j.genhosppsych.2011.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Van Voorhees BW, Ellis J, Stuart S, Fogel J, Ford DE. Pilot study of a primary care internet-based depression prevention intervention for late adolescents. Can Child Adolesc Psychiatr Rev. 2005;14(2):40-43. [PMC free article] [PubMed] [Google Scholar]
- 49.Resnicow K, Davis RE, Zhang G, et al. Tailoring a fruit and vegetable intervention on novel motivational constructs: results of a randomized study. Ann Behav Med. 2008;35(2):159-169. doi: 10.1007/s12160-008-9028-9 [DOI] [PubMed] [Google Scholar]
- 50.Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program. J Abnorm Child Psychol. 2006;34(2):203-219. doi: 10.1007/s10802-005-9014-7 [DOI] [PubMed] [Google Scholar]
- 51.Van Voorhees BW, Mahoney N, Mazo R, et al. Internet-based depression prevention over the life course: a call for behavioral vaccines. Psychiatr Clin North Am. 2011;34(1):167-183. doi: 10.1016/j.psc.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bauer NS, Webster-Stratton C. Prevention of behavioral disorders in primary care. Curr Opin Pediatr. 2006;18(6):654-660. doi: 10.1097/MOP.0b013e3280106239 [DOI] [PubMed] [Google Scholar]
- 53.Bansa M, Brown D, DeFrino D, et al. A little effort can withstand the hardship: fielding an internet-based intervention to prevent depression among urban racial/ethnic minority adolescents in a primary care setting. J Natl Med Assoc. 2018;110(2):130-142. doi: 10.1016/j.jnma.2017.02.006 [DOI] [PubMed] [Google Scholar]
- 54.DeFrino DT, Marko-Holguin M, Cordel S, Anker L, Bansa M, Van Voorhees B. “Why should I tell my business?”: an emerging theory of coping and disclosure in teens. Res Theory Nurs Pract. 2016;30(2):124-142. doi: 10.1891/1541-6577.30.2.124 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable 1. Definition for Criteria for Main Outcomes Analyses
eTable 2. MI Fidelity: Mean MITI Summary Scores
eTable 3. Hazard Ratio Estimate and 95% CI for First Depressive Episode Comparing CATCH-IT to Health Education
eTable 4. Incidence of First Depressive Episode by Treatment Group
eTable 5. Adjusted Cox Proportional Hazard Model Results, Including Adolescent Baseline CES-D10 as a Moderator
eTable 6. Depressed Mood
eTable 7. Functional Status
eTable 8. A, Participants With Missing Data: KSADS and CES-D10. B, Predictors of Missing 2-Month Follow-up: Time to Last Assessment <2 Months. C, Predictors of Missing 6-Month Follow-up: Time to Last Assessment <6 Months. D, Predictors of Missing 2-Month CES-D10. E, Predictors of Missing 6-Month CES-D10
Data Sharing Statement