Abstract
In the traditional Medicare program, the use of health care services—particularly postacute care—varies substantially across geographic regions. Less is known about such variations in Medicare Advantage (MA), which is growing rapidly. Insurers that are paid on a risk basis, as in MA, may have incentives and tools to restrain the use of services, which could attenuate geographic variations. In this study of fifty-four million Medicare beneficiaries in the period 2007–13, we found that geographic variations in the use of skilled nursing facility and hospital care in the MA population exceeded those in traditional Medicare, though variations in the use of home health care were greater in traditional Medicare. Within hospital referral regions, the correlations between the use of services in MA and traditional Medicare were moderate to strong. The findings suggest that regional variations in hospital and postacute care reflect local factors that influence beneficiaries’ use of services irrespective of the way they obtain coverage.
John Wennberg and Alan Gittelsohn reported in 1973 that the use of health services, including hospitalizations and tonsillectomies, varied widely across thirteen ostensibly similar communities in Vermont.1 Following this landmark discovery, over four decades of research have documented substantial variations in health care spending and use across US regions.2,3 Further, with some exceptions, some studies have reported weak associations between higher spending and better outcomes, which suggests that reducing the intensity of medical care in high-spending communities could avert billions of dollars in Medicare spending without harming health.4–7
Prior studies of geographic variation have focused largely on the traditional Medicare program or on a voluntary sample of commercial insurers or integrated delivery systems, raising concerns about generalizability to populations with other sources of coverage.2,8–10 There is remarkably little evidence about variation in the use of services in the Medicare Advantage (MA) program, which enrolled 31 percent of the Medicare population as of 2016.11 While private managed care plans are required to provide all Medicare benefits (except for hospice care), they may have the potential to reduce unwarranted variations in care since these entities bear direct financial risk for the cost of services and have tools to constrain utilization that are not fully available in the traditional Medicare program.12,13 For instance, MA plans can use utilization and case management, selectively contract with more efficient providers, and reimburse providers using capitation or other alternatives to fee-for-service. To the extent that these strategies limit the provision of inappropriate care, they may reduce regional variations in care. In contrast, if variations largely reflect local professional norms, physician practice styles, provider supply, and patients’ preferences, and these factors are not substantially influenced by private plans, the magnitude of variations in MA and traditional Medicare may be similar. Further, the use of services for the two insured populations would be highly correlated within regions.14
Using national data for the period 2007–13, this study assessed the use of home health, skilled nursing facility (SNF), and acute hospital care in MA and traditional Medicare; compared geographic variations in both Medicare sectors; and examined the degree to which the use of these services in both sectors was correlated within geographic regions. We focused on home health, SNF, and hospital care since these services are the dominant drivers of spending variations in the Medicare program. In particular, the Institute of Medicine reported that post-acute care accounted for three-quarters of the geographic variations in traditional Medicare spending in the period 2007–09.2 Although post-acute care can also occur in institutional rehabilitation facilities and long-term acute care hospitals, home health and SNF care account for 80 percent of postacute spending in traditional Medicare.14
Study Data And Methods
Study Design And Data Sources
We compared geographic variations in the use of home health, SNF, and hospital care between Medicare Advantage and traditional Medicare. We merged data for 2007–13 from five sources. The Outcome and Assessment Information Set (OASIS) provided information on the use of home health services.15 Information about the use of SNF care was obtained from the national repository of the Minimum Data Set (MDS).16 Data in the two sources are reported for all patients using SNF and home health care, respectively, including both enroll-ees in MA and those in traditional Medicare. We used person-level data from the Healthcare Effectiveness Data and Information Set (HEDIS) and Medicare claims to identify the use of hospital days. HEDIS includes annual summary measures of all acute inpatient hospitalizations and days financed by MA plans. Medicare claims data were used to quantify inpatient hospital use for traditional Medicare beneficiaries. Both of these data sets were linked to the Medicare Beneficiary Summary File to obtain the demographic characteristics of enrollees and assign patients to hospital referral regions (HRRs) by their ZIP code of residence. HRRs represent regional markets for tertiary health care.17 At the time of our analysis, these sources provided the most comprehensive and up-to-date data available for assessing national variations in the use of services in MA and traditional Medicare.
Study Population
We included MA and traditional Medicare beneficiaries ages sixty-five and older. Analyses of inpatient days included all enrollees in MA plans that reported HEDIS data. With the exception of private fee-for-service plans and small plans with fewer than 1,000 enrollees, all MA plans must report HEDIS data. Analyses of home health and SNF days included all MA plans, including those that did not report HEDIS data. We excluded 2011 for SNF utilization, as the transition between MDS versions 2.0 and 3.0 occurred in that year. The study population included approximately fifty-four million Medicare beneficiaries during the period 2007–13.
Variables
The principal outcomes were home health days, SNF days, and hospital days, all per 1,000 beneficiary-years. Home health days were defined as the duration between admission and discharge dates for each episode. For people with concurrent episodes from distinct home health providers, we summed home health days for all episodes. Each SNF episode was capped at 100 days following a hospital discharge, consistent with Medicare’s payment policy for SNF services. We included care received in all (freestanding and hospital-based) SNFs and home health facilities. Hospital days were defined as the distinct days in short-stay general hospitals for acute medical and surgical admissions; long-term acute care admissions and other extended care admissions were not included. We used HEDIS and Medicare claims data to obtain information on hospital use for MA and traditional Medicare beneficiaries, respectively.12
We defined MA or traditional Medicare enrollment on the basis of each beneficiary’s first month of Medicare eligibility during the calendar year (typically January). Covariates included age, sex, race/ethnicity (black, white, Hispanic, Asian, or other), ZIP code–level income derived from national census data, enrollment in full Medicaid (defined as of the first month of Medicare eligibility during the measurement year), year, and indicator variables for HRRs.17 In an analysis limited to SNF users, we also included a measure of the ability to perform activities of daily living and a measure of cognition based on the Cognitive Functional Scale. These covariates were obtained from MDS data.18,19 Both covariates are strong predictors of length-of-stay for SNF episodes.19
Analyses Of Utilization Trends In 2007–13
The unit of analysis was the beneficiary-year. We constructed generalized linear models that examined outcomes for MA and traditional Medicare beneficiaries and included the covariates described above. To test whether trends differed between MA and traditional Medicare, we included an interaction term between year and MA enrollment.
Analyses Of Geographic Variation
The analyses of geographic variation used only data from 2013, which included information about 306 HRRs. We estimated expected utilization rates using generalized linear models for MA and traditional Medicare beneficiaries that included the covariates described above. To determine adjusted utilization rates, we multiplied the ratio of observed to expected utilization values for MA and traditional Medicare populations in each HRR by the national mean utilization rate. Using the Spearman rank order test, we assessed the correlation between adjusted utilization rates for each service in MA and traditional Medicare across HRRs.
For each service, we calculated the following relative measures of geographic variation for MA and traditional Medicare: the ninetieth/tenth percentile ratio, which is the level of utilization in the HRR at the ninetieth percentile divided by the level in the HRR at the tenth percentile; and the interquartile ratio, which is the seventy-fifth percentile value divided by the twenty-fifth percentile value. We also calculated the absolute difference between HRRs at the ninetieth and tenth percentiles in level of utilization and between HRRs at the seventy-fifth and twenty-fifth percentiles. These values provide the absolute difference in utilization associated with geographic variations in MA and traditional Medicare.
To test the robustness of the analysis to inclusion of clinical covariates, we compared characteristics and geographic variations in utilization rates among users of SNF care after further adjustment for activities of daily living and Cognitive Functional Scale scores.18,19 We also stratified the analysis by the presence of full Medicaid benefits and performed a sensitivity analysis that excluded HRRs with fewer than 5,000 MA enrollees (n = 41).
Statistical analyses were conducted using Stata/MP, version 14.1. Brown University’s Institutional Review Board approved the study protocol.
Limitations
Our study had several limitations. First, we cannot fully dismiss the possibility that unmeasured differences between MA and traditional Medicare beneficiaries influenced our results. While we adjusted for sociodemo-graphic factors and (for SNF users) functional status, data limitations prohibited a more robust adjustment for beneficiary health status. Thus, this analysis could not determine the extent to which differences between MA and traditional Medicare programs are explained by the selection of healthier enrollees into MA versus management strategies used by MA plans to reduce the use of postacute health services.
We focused on home health, SNF, and hospital care since these services are the dominant drivers of spending variations in Medicare.
Second, although we quantified variation at the HRR level, consistent with prior research, consideration of alternative geographic units could yield different findings.20
Finally, our study did not examine the clinical appropriateness of care; nor did it assess the overuse or underuse of these hospital and post-acute care services.
Study Results
Compared with beneficiaries in traditional Medicare, Medicare Advantage beneficiaries were more likely to be female, older, and black or Hispanic, and they were less likely to have full Medicaid benefits (that is, to have dual eligibility). There were minimal changes for most characteristics between 2007 and 2013 for both MA and traditional Medicare beneficiaries. Of note, enrollment in MA increased disproportionately in low-income areas (see online appendix exhibit A1).21 Characteristics of users of SNF care are shown in appendix exhibit A2.21
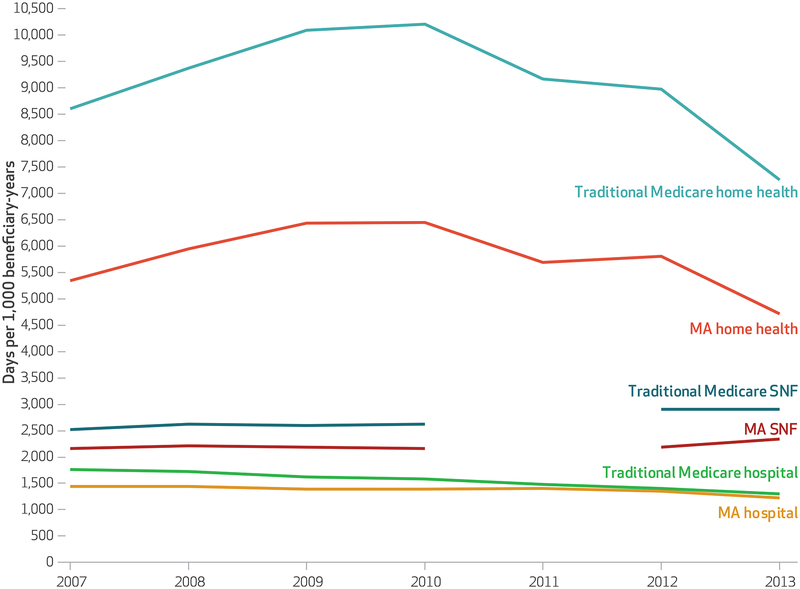
Exhibit 1 shows that there was substantially greater adjusted use of home health and SNF care, but not hospital care, in traditional Medicare compared with MA. In 2007 the use of SNF care per 1,000 beneficiary-years was 2,164 days in MA and 2,521 days in traditional Medicare (absolute difference: 357 days per 1,000 beneficiary-years). In 2013 it was 2,337 days in MA and 2,902 days in traditional Medicare (absolute difference: 565 days per 1,000 beneficiary-years).
Exhibit 1. Adjusted trends in the use of home health, skilled nursing facility (SNF), and hospital care by Medicare Advantage (MA) and traditional Medicare beneficiaries, 2007–13.
Source Authors’ analysis of data for 2007–13 from the Outcome and Assessment Information Set (OASIS), Minimum Data Set (MDS), Healthcare Effectiveness and Data Information Set (HEDIS), Medicare claims, and Medicare Beneficiary Summary File. Notes We excluded 2011 data for SNF days as the transition between MDS versions 2.0 and 3.0 occurred in that calendar year. Estimates adjusted for age, sex, race/ethnicity (black, white, Hispanic, Asian, or other), ZIP code–level income derived from national census data, the presence of full Medicaid benefits (defined in the first month of Medicare eligibility in the measurement year), and indicator variables for hospital referral regions.
In 2007 the use of home health care per 1,000 beneficiary-years was 5,341 days in MA and 8,603 days in traditional Medicare (absolute difference: 3,262 days per 1,000 beneficiary-years). In 2013 it was 4,712 days and 7,257 days, respectively (absolute difference: 2,545 days per 1,000 beneficiary-years). For both MA and traditional Medicare, home health days per 1,000 beneficiary-years increased between 2007 and 2010 and declined thereafter.
We observed declines in the rates of hospital care in both MA and traditional Medicare, with the rates for the two populations converging. In 2007 the use of hospital care per 1,000 beneficiary-years was 1,438 days in MA and 1,759 days in traditional Medicare (absolute difference: 321 days per 1,000 beneficiary-years). In 2013 it was 1,228 days and 1,305 days, respectively (absolute difference: 77 days per 1,000 beneficiary-years). Unadjusted trends are shown in appendix exhibit A3.21
Exhibit 2 shows three important findings from our comparisons of geographic variations in MA and traditional Medicare in 2013. First, across services, the home health care sector had the highest levels of geographic variation, followed by SNF and then hospital care.
Exhibit 2.
Geographic variations in use of home health, skilled nursing facility, and hospital care across hospital referral regions (HRRs) in Medicare Advantage and traditional Medicare, 2013
| Medicare Advantage | Traditional Medicare | |||
|---|---|---|---|---|
| Days in: | Ratio | Absolute difference between HRRsa | Ratio | Absolute difference between HRRsa |
| Home Health Care | ||||
| 90th to 10th percentile comparisonb | 4.17 | 5,018 | 4.27 | 7,702 |
| Interquartile comparisonc | 2.07 | 2,391 | 2.22 | 4,001 |
| Skilled Nursing Facility Care | ||||
| 90th to 10th percentile comparisonb | 2.53 | 2,280 | 1.94 | 2,075 |
| Interquartile comparisonc | 1.49 | 1,055 | 1.39 | 1,083 |
| Hospital Care | ||||
| 90th to 10th percentile comparisonb | 2.05 | 914 | 1.71 | 653 |
| Interquartile comparisonc | 1.40 | 440 | 1.34 | 360 |
Source Authors’ analysis of data for 2013 from the Outcome and Assessment Information Set (OASIS), Minimum Data Set (MDS), Healthcare Effectiveness and Data Information Set (HEDIS), Medicare claims, and Medicare Beneficiary Summary File. Note Estimates adjusted for all of the variables listed in exhibit 1 notes except for indicator variables for HRR.
Days per 1,000 beneficiary-years between HRRs with higher and lower utilization.
Utilization in the HRR at the ninetieth percentile, divided by utilization in the HRR at the tenth percentile.
Utilization in the HRR at the seventy-fifth percentile, divided by utilization in the HRR at the twenty-fifth percentile.
Second, geographic variations, as measured by relative differences between HRRs, were greater in MA than traditional Medicare for SNF days and hospital services. For SNF days per 1,000 beneficiary-years, the ratios of utilization between HRRs at the ninetieth and tenth percentiles were 2.53 in MA and 1.94 in traditional Medicare. The absolute difference in utilization between HRRs at the ninetieth and tenth percentiles was 2,280 days per 1,000 beneficiary-years in MA and 2,075 days in traditional Medicare. For hospital days per 1,000 beneficiary-years, the ratios were 2.05 and 1.71, respectively, and the absolute differences were 914 days and 653 days. Comparisons of interquartile ratios for SNF and hospital care also revealed larger magnitudes of geographic variation in MA versus traditional Medicare. Of note, the absolute differences were larger in MA for hospital care and slightly larger in traditional Medicare for SNF care.
Third, for home health care, we observed greater relative variation in the traditional Medicare program compared with MA, as measured by both ratios. The absolute difference in utilization between HRRs in the ninetieth and tenth percentiles was larger in traditional Medicare than in MA. Unadjusted results were largely consistent with adjusted findings (appendix exhibit A4).21
As shown in exhibit 3, there were greater geographic variations in the number of SNF days in the MA population than in the traditional Medicare population, among all users of this service. Of note, the characteristics of users of SNF care in MA and traditional Medicare were similar (appendix exhibit A2).21 In model 1, the ratios of utilization between HRRs at the ninetieth and tenth percentiles per 1,000 users were 1.38 and 1.26 in MA and traditional Medicare, respectively (exhibit 3). Furthermore, variations were greater among beneficiaries with full Medicaid compared to beneficiaries without full Medicaid. Among MA beneficiaries, the ratios were 1.69 for users with and 1.41 for users without full Medicaid. The findings of greater variations in MA versus traditional Medicare were consistent after we included further adjustments for function and cognition. The results were also consistent in a sensitivity analysis that excluded the forty-one HRRs with fewer than 5,000 enrollees in MA plans (appendix exhibit A5).21
Exhibit 3.
Geographic variations in the use of skilled nursing facility days per 1,000 beneficiary-years in Medicare Advantage and traditional Medicare across hospital referral regions, 2013
| Model 1a | Model 2b | |||
|---|---|---|---|---|
| Medicare Advantage |
Traditional Medicare |
Medicare Advantage |
Traditional Medicare |
|
| Total Population | ||||
| 90th to 10th percentile ratio | 1.38 | 1.26 | 1.37 | 1.25 |
| Interquartile ratio | 1.19 | 1.13 | 1.17 | 1.12 |
| Beneficiaries With Full Medicaid Benefitsc | ||||
| 90th to 10th percentile ratio | 1.69 | 1.41 | 1.74 | 1.42 |
| Interquartile ratio | 1.31 | 1.20 | 1.29 | 1.21 |
| Beneficiaries Without Full Medicaid Benefitsc | ||||
| 90th to 10th percentile ratio | 1.41 | 1.22 | 1.36 | 1.23 |
| Interquartile ratio | 1.16 | 1.11 | 1.15 | 1.10 |
Source Authors’ analysis of data for 2013 from the Minimum Data Set (MDS) and Medicare Beneficiary Summary File. Note The two ratios are explained in the notes to exhibit 2.
Adjusted for age, sex, race/ethnicity, enrollment in full Medicaid, income, and hospital referral region.
Adjusted for model 1 covariates, functional status, and Cognitive Functional Scale.
Stratified analyses for beneficiaries with and without full Medicaid benefits did not include Medicaid as a covariate in the adjusted models.
The home health care sector had the highest levels of geographic variation, followed by SNF and hospital care.
Utilization in MA and traditional Medicare was highly correlated at the HRR level for all three services, with Spearman correlation coefficients ranging from 0.65 to 0.72 (appendix exhibits A6 and A7).21
Discussion
This comparison of geographic variations in Medicare Advantage and traditional Medicare in the use of home health, SNF, and hospital care has four major findings. First, we found substantially less use of home health and SNF care for MA enrollees, compared with those in traditional Medicare, but similar rates of hospital care use. Second, we found fewer geographic variations in the use of home health care but more variations in the use of SNF and inpatient care in the MA population, compared with the traditional Medicare population. Third, the larger variations in MA versus traditional Medicare remained after adjustments for sociodemographic factors and, in the case of users of SNF care, adjustment for functional status and cognition. Finally, for all three services, we observed a high degree of correlation between utilization in MA and traditional Medicare within HRRs.
Our findings contrast with those of other studies that compared traditional Medicare spending with spending for a younger, commercially insured population.8,13,22,23 However, these studies differ fundamentally from the one presented here, which involves comparisons internal to the Medicare population rather than comparisons of two fundamentally different populations and insurance programs. Our findings may differ from those of earlier comparisons for two main reasons. First, while the use of postacute services, such as skilled nursing and home health care, is the largest driver of geographic variation in traditional Medicare spending,2,23,24 younger commercially insured populations seldom use these services. Second, among commercially insured populations, variations appear to be driven principally by the prices paid for services, rather than the quantity delivered.23 However, there is emerging evidence that, unlike payments in commercial insurance, provider reimbursements in MA plans tend to track those paid by the traditional Medicare program.25,26
Other comparisons of variations between MA and traditional Medicare are more limited than those presented here and have produced mixed findings, with studies finding evidence of higher, lower, and similar magnitudes of variation in MA compared to traditional Medicare.27–29 Because claims from all MA plans have not been available to researchers, prior studies have analyzed data from a voluntary sample of insurers or integrated delivery systems, raising concerns about generalizability to the entire MA population.27,28 By contrast, we extended this research by examining national data on the use of postacute services, since CMS requires OASIS and MDS data to be submitted for all patients, irrespective of their insurance type. Of note, in April 2018 CMS announced the release of encounter-level data for MA plans, beginning with the 2015 calendar year. These data could enhance understanding of the use of health services in the MA program, although their validity and comprehensiveness have not yet been assessed in the peer-reviewed literature.
Our finding that MA enrollment was associated with less use of home health and SNF care, but generally similar use of hospital care, is broadly consistent with results of prior studies.12,27,30 We extended this research by demonstrating that the use of hospital care in MA and traditional Medicare had converged by 2013. Further, our results extended those of studies that measured geographic variations in various US and international health systems with diverse approaches to financing and organizing health care delivery.31–34 Like our study, these analyses found that systems with lower overall levels of utilization nevertheless have significant regional variations in use.
Our analysis grouped all MA enrollees together, but there is considerable heterogeneity in the types of MA plans available to enrollees. Plans can vary on the basis of their benefit generosity; tax status; organizational structure; and designation as a Special Needs Plan that enrolls people with Medicaid eligibility, institutional care needs, or chronic conditions. Of note, there are somewhat similar heterogeneities in the traditional Medicare program. Traditional Medicare beneficiaries may be part of an accountable care organization or be included in a bundled payment initiative, both of which involve changes in the method of payment for covered services. Traditional Medicare beneficiaries may also have varying insurance benefits depending on whether they are enrolled in a Part D, retiree, or Medigap plan. Therefore, future work should examine the potential contribution of organizational factors, health plan benefits, and differential market penetration of accountable care organization and bundled payment initiatives to geographic variations in the use of health services.
Decades of studies have reported substantial geographic variations in health care use and spending across the United States, with these findings cited as evidence of waste in the health care system.2,35 Because insurers paid on a risk basis may have stronger incentives and more developed tools to restrain inappropriate utilization, boost efficiency, and detect fraud than the traditional Medicare program does, some observers have contended that variations among those in private insurance plans would be accordingly attenuated.13,36 Our analyses do not support this assertion. Although the overall level of utilization, particularly of postacute care, was lower among MA enrollees, we detected geographic variations in the MA population that exceeded or equaled those of traditional Medicare. Furthermore, within regions, utilization for MA and traditional Medicare beneficiaries was moderately to strongly correlated. Our findings suggest that regional variations in postacute care for older adults likely reflect local factors that operate irrespective of enrollment in health plans of different types.
Supplementary Material
Acknowledgments
Research reported in this article was supported by the National Institute on Aging of the National Institutes of Health (Award Nos. P01AG027296-07S1 and R01AG044374-01). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the National Institutes of Health, Department of Veterans Affairs, or US government.
Contributor Information
Qijuan Li, Qijuan Li is an adjunct assistant professor in the Department of Health Services, Policy, and Practice, Brown University School of Public Health, in Providence, Rhode Island, and director of innovation analytics at SCIO Health Analytics, in West Hartford, Connecticut..
Momotazur Rahman, Momotazur Rahman is an assistant professor in the Department of Health Services, Policy, and Practice, Brown University School of Public Health..
Pedro Gozalo, Pedro Gozalo is an associate professor in the Department of Health Services, Policy, and Practice, Brown University School of Public Health, and a research investigator at the Providence Veterans Affairs (VA) Medical Center..
Laura M. Keohane, Laura M. Keohane is an assistant professor in the Department of Health Policy, Vanderbilt University School of Medicine, in Nashville, Tennessee.
Marsha R. Gold, Marsha R. Gold is senior fellow emeritus at Mathematica Policy Research in Washington, D.C.
Amal N. Trivedi, Amal N. Trivedi (Amal_Trivedi@brown.edu) is an associate professor in the Department of Health Services, Policy, and Practice, Brown University School of Public Health, and a research investigator at the Providence VA Medical Center.
NOTES
- 1.Wennberg J, Gittelsohn A. Small area variations in health care delivery. Science. 1973;182(4117):1102–8. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Variation in health care spending: target decision making, not geography. Washington (DC): National Academies Press; 2013. Oct. [PubMed] [Google Scholar]
- 3.Cassidy A Health Policy Brief: geographic variation in Medicare spending. Health Affairs [serial on the Internet]. 2014. March 6 [cited 2018 Jun 25]. Available from: https://www.healthaffairs.org/do/10.1377/hpb20140306.633790/full/
- 4.Skinner JS, Fisher ES, Wennberg JE. The efficiency of Medicare [Internet]. Cambridge (MA): National Bureau of Economic Research; 2001. July [cited 2018 Jun 25]. (NBER Working Paper No. 8395). Available from: http://www.nber.org/papers/w8395.pdf [Google Scholar]
- 5.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4): 288–98. [DOI] [PubMed] [Google Scholar]
- 6.Congressional Budget Office. Geographic variation in health care spending [Internet]. Washington (DC): CBO; 2008. February [cited 2018 Jun 25]. (CBO Publication No. 2978). Available from: http://www.cbo.gov/ftpdocs/89xx/doc8972/02-15-GeogHealth.pdf [Google Scholar]
- 7.Cooper RA. States with more health care spending have better-quality health care: lessons about Medicare. Health Aff (Millwood). 2009;28(1): w103–15. DOI: 10.1377/hlthaff.28.1.w103 [DOI] [PubMed] [Google Scholar]
- 8.Chernew ME, Sabik LM, Chandra A, Gibson TB, Newhouse JP. Geographic correlation between large-firm commercial spending and Medicare spending. Am J Manag Care. 2010;16(2):131–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Franzini L, White C, Taychakhoonavudh S, Parikh R, Zezza M, Mikhail O. Variation in inpatient hospital prices and outpatient service quantities drive geographic differences in private spending in Texas. Health Serv Res. 2014;49(6):1944–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henke RM, Karaca Z, Gibson TB, Cutler E, Barrett ML, Levit K, et al. Medicare Advantage and traditional Medicare hospitalization intensity and readmissions. Med Care Res Rev. 2017. March 1 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 11.Jacobson G, Casillas G, Damico A, Neuman T, Gold M. Medicare Advantage 2016 spotlight: enrollment market update [Internet]. San Francisco (CA): Henry J. Kaiser Family Foundation; 2016. May 11 [cited 2018 Jun 25]. Available from: http://kff.org/medicare/issue-brief/medicare-advantage-2016-spotlight-enrollment-market-update/ [Google Scholar]
- 12.Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, Newhouse JP, Ayanian JZ. Analysis of Medicare Advantage HMOs compared with traditional Medicare shows lower use of many services during 2003–09. Health Aff (Millwood). 2012; 31(12):2609–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Philipson TJ, Seabury SA, Lockwood LM, Goldman DP, Lakdawalla DN. Geographic variation in health care: the role of private markets Brookings Papers on Economic Activity [serial on the Internet]. 2010. [cited 2018 Jun 25]. Available from: https://www.brookings.edu/wp-content/uploads/2010/03/2010a_bpea_philipson.pdf [Google Scholar]
- 14.Medicare Payment Advisory Commission. A data book: health care spending and the Medicare program [Internet]. Washington (DC); Med-PAC; 2017. June Section 8, Post-acute care: skilled nursing facilities, home health services, inpatient rehabilitation facilities, long-term care hospitals; [cited 2018 Jun 28]. Available from: http://www.medpac.gov/docs/default-source/data-book/jun17_databooksec8_sec.pdf [Google Scholar]
- 15.Shaughnessy PW, Crisler KS, Schlenker RE. Medicare’s OASIS: standardized outcome and assessment information set for home health care. Home Healthcare Now. 1996;14(7):547–8. [Google Scholar]
- 16.Hawes C, Morris JN, Phillips CD, Mor V, Fries BE, Nonemaker S. Reliability estimates for the Minimum Data Set for nursing home resident assessment and care screening (MDS). Gerontologist. 1995;35(2): 172–8. [DOI] [PubMed] [Google Scholar]
- 17.Dartmouth Atlas of Heath Care. Data by region [Internet]. Lebanon (NH): Trustees of Dartmouth College; c 2018. [cited 2018 Jun 26]. Available from: http://www.dartmouthatlas.org/data/region/ [Google Scholar]
- 18.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999; 54(11):M546–53. [DOI] [PubMed] [Google Scholar]
- 19.Thomas KS, Dosa D, Wysocki A, Mor V. The Minimum Data Set 3.0 Cognitive Function Scale. Med Care. 2017;55(9):e68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Y, Baik SH, Fendrick AM, Baicker K. Comparing local and regional variation in health care spending. N Engl J Med. 2012; 367(18):1724–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. To access the appendix, click on the Details tab of the article online.
- 22.Baker LC, Fisher ES, Wennberg JE. Variations in hospital resource use for Medicare and privately insured populations in California. Health Aff (Millwood). 2008;27(2):w123–34. DOI: 10.1377/hlthaff.27.2.w123. [DOI] [PubMed] [Google Scholar]
- 23.Cooper Z, Craig S, Gaynor M, Van Reenen J. The price ain’t right? Hospital prices and health spending on the privately insured [Internet]. Cambridge (MA): National Bureau of Economic Research; 2015. December [revised 2018 May; cited 2018 Jul 2]. (Working Paper No. 21815). Available from: http://www.nber.org/papers/w21815.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mechanic R Post-acute care—the next frontier for controlling Medicare spending. New Engl J Med. 2014;370(8):692–4. [DOI] [PubMed] [Google Scholar]
- 25.Berenson RA, Ginsburg PB, Christianson JB, Yee T. The growing power of some providers to win steep payment increases from insurers suggests policy remedies may be needed. Health Aff (Millwood). 2012;31(5):973–81. [DOI] [PubMed] [Google Scholar]
- 26.Trish E, Ginsburg P, Gascue L, Joyce G. Physician reimbursement in Medicare Advantage compared with traditional Medicare and commercial health insurance. JAMA Intern Med. 2017;177(9):1287–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Curto V, Einav L, Finkelstein A, Levin JD, Bhattacharya J. Healthcare spending and utilization in public and private Medicare [Internet]. Cambridge (MA): National Bureau of Economic Research; 2017. January [cited 2018 Jun 26]. (NBER Working Paper No. 23090). Available from: http://www.nber.org/papers/w23090.pdf [Google Scholar]
- 28.Matlock DD, Groeneveld PW, Sidney S, Shetterly S, Goodrich G, Glenn K, et al. Geographic variation in cardiovascular procedure use among Medicare fee-for-service vs Medicare Advantage beneficiaries. JAMA. 2013;310(2):155–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Waxman DA, Min L, Setodji CM, Hanson M, Wenger NS, Ganz DA. Does Medicare Advantage enrollment affect home healthcare use? Am J Manag Care. 2016;22(11): 714–20. [PubMed] [Google Scholar]
- 30.Huckfeldt PJ, Escarce JJ, Rabideau B, Karaca-Mandic P, Sood N. Less intense postacute care, better outcomes for enrollees in Medicare Advantage than those in fee-for-service. Health Aff (Millwood). 2017;36(1):91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McWilliams JM, Dalton JB, Landrum MB, Frakt AB, Pizer SD, Keating NL.Geographic variation in cancer-related imaging: Veterans Affairs health care system versus Medicare. Ann Intern Med. 2014;161(11): 794–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McPherson K, Wennberg JE, Hovind OB, Clifford P. Small-area variations in the use of common surgical procedures: an international comparison of New England, England, and Norway. N Engl J Med. 1982; 307(21):1310–4. [DOI] [PubMed] [Google Scholar]
- 33.Stiefel M, Feigenbaum P, Fisher ES. The Dartmouth Atlas applied to Kaiser Permanente: analysis of variation at the end of life. Perm J 2008; 12(1):4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ashton CM, Petersen NJ, Souchek J, Menke TJ, Yu HJ, Pietz K, et al. Geographic variations in utilization rates in Veterans Affairs hospitals and clinics. N Engl J Med. 1999; 340(1):32–9. [DOI] [PubMed] [Google Scholar]
- 35.Gawande A The cost conundrum persists. New Yorker: [serial on the Internet]. 2010. February 18 [cited 2018 Jun 26]. Available from: https://www.newyorker.com/news/news-desk/the-cost-conundrum-persists [Google Scholar]
- 36.Book RA. Medicare variation revisited: is something wrong with McAllen, Texas, or is something wrong with Medicare? [Internet]. Washington (DC): Heritage Foundation; 2011. January 4 [cited 2018 Jun 22]. Available from: https://www.heritage.org/health-care-reform/report/medicare-variation-revisited-something-wrong-mcallen-texas-or-something [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.